Titanium vs. PCL in 3D Printed Bone Scaffolds: A Comparative Analysis for Biomedical Researchers
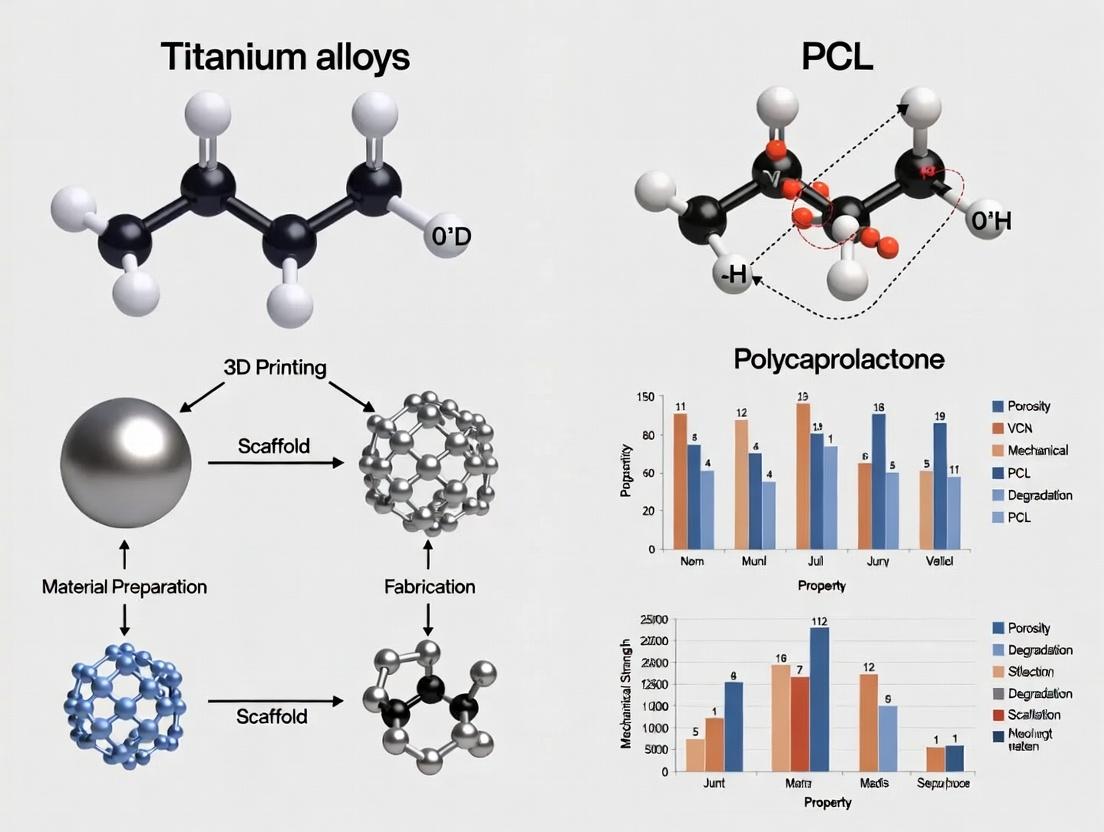
This article provides a comprehensive, evidence-based analysis of two prominent materials in 3D-printed bone tissue engineering: titanium alloys and polycaprolactone (PCL).
Titanium vs. PCL in 3D Printed Bone Scaffolds: A Comparative Analysis for Biomedical Researchers
Abstract
This article provides a comprehensive, evidence-based analysis of two prominent materials in 3D-printed bone tissue engineering: titanium alloys and polycaprolactone (PCL). Tailored for researchers and biomedical professionals, we explore the fundamental properties, manufacturing methodologies, and critical challenges associated with each material. The content systematically compares their mechanical performance, biocompatibility, degradation profiles, and clinical translation potential, synthesizing the latest research to inform material selection and scaffold design for advanced regenerative medicine applications.
Understanding the Building Blocks: Core Properties of Titanium Alloys and PCL for Bone Regeneration
Application Notes for Bone Scaffold Research
The selection of titanium alloys for 3D-printed bone scaffolds is predicated on their superior mechanical properties, biocompatibility, and corrosion resistance compared to bioresorbable polymers like Polycaprolactone (PCL). This analysis is framed within a thesis investigating the trade-offs between permanent metallic and temporary polymeric scaffolds for bone regeneration and drug delivery.
Ti-6Al-4V (Grade 5): The long-standing benchmark. Its strength and proven history make it suitable for load-bearing orthopedic implants. However, concerns regarding potential aluminum and vanadium ion release and a higher elastic modulus than cortical bone necessitate surface modifications for optimal osteointegration.
Ti-6Al-4V ELI (Grade 23): The "Extra Low Interstitial" version. Reduced oxygen, nitrogen, carbon, and iron content enhance ductility, fracture toughness, and biocompatibility. This makes it the preferred choice for critical applications like spinal fusion cages and maxillofacial implants, where improved fatigue resistance is crucial.
Newer Beta Alloys (e.g., Ti-15Mo, Ti-Nb-Ta-Zr): Developed to address the modulus mismatch of alpha-beta alloys. Comprised primarily of beta-stabilizing elements (Mo, Nb, Ta), these alloys offer a lower elastic modulus closer to that of bone, reducing stress shielding. Their excellent corrosion resistance and inherent biocompatibility position them as the next-generation materials for non-load-bearing or low-load scaffold designs, often fabricated via Electron Beam Melting (EBM) or selective laser melting (SLM).
Contrast with PCL: PCL scaffolds, fabricated via fused deposition modeling (FDM) or melt electrospinning writing, offer tunable degradation (≈2-4 years) and are excellent for sustained drug release. However, their low mechanical strength restricts use to non-load-bearing defects. The permanent, robust titanium scaffold provides immediate structural support, while surface functionalization (e.g., hydroxyapatite coating, polymer dip-coating) can be used to incorporate drug-eluting capabilities.
Quantitative Property Comparison
Table 1: Mechanical and Physical Properties of Titanium Alloys vs. Cortical Bone and PCL
| Material | Elastic Modulus (GPa) | Yield Strength (MPa) | Ultimate Tensile Strength (MPa) | Fatigue Strength (MPa, @10⁷ cycles) | Approx. Density (g/cm³) | Primary Fabrication for Scaffolds |
|---|---|---|---|---|---|---|
| Cortical Bone | 10 - 30 | 30 - 70 | 70 - 150 | 20 - 40 | 1.8 - 2.0 | - |
| PCL Polymer | 0.2 - 0.5 | 10 - 20 | 20 - 50 | N/A | 1.14 | FDM / Electrospinning |
| Ti-6Al-4V (wrought) | 110 - 114 | 850 - 900 | 900 - 1000 | 500 - 600 | 4.43 | SLM / EBM |
| Ti-6Al-4V ELI | 101 - 110 | 795 - 875 | 860 - 965 | 550 - 620 | 4.43 | SLM / EBM |
| Ti-15Mo (β-alloy) | 78 - 82 | 540 - 870 | 690 - 1020 | 450 - 550 | ~4.95 | EBM / SLM |
| Ti-35Nb-5Ta-7Zr (β-alloy) | ~55 | ~530 | ~590 | ~300 | ~6.0 | SLM |
Table 2: Biological & Chemical Performance Indicators
| Material | Corrosion Resistance (PBS, 37°C) | Ion Release Profile | Osteoblast Adhesion & Proliferation | Osseointegration Potential (in vivo) | Typical Surface Modification for Scaffolds |
|---|---|---|---|---|---|
| PCL | Degrades via hydrolysis | Caprolactone monomers | Moderate; requires bioactivation (e.g., RGD coating) | Low; forms fibrous capsule unless modified | Plasma treatment, Hydroxyapatite blending |
| Ti-6Al-4V | Excellent (passive TiO₂ layer) | Trace Al, V ions detected | High | High (Gold Standard) | Acid-etching, Anodization (TiO₂ nanotubes), HA coating |
| Ti-6Al-4V ELI | Excellent | Minimal ion release | Very High | Very High | Similar to Ti-64, with enhanced results |
| Newer Beta Alloys | Excellent | Primarily benign ions (Nb, Ta, Zr) | High to Very High | High; enhanced by lower modulus | Anodization, Calcium-Phosphate deposition |
Experimental Protocols
Protocol 1: In Vitro Osteogenic Differentiation on 3D-Printed Scaffolds
Objective: To assess the osteoinductive potential of Ti-6Al-4V ELI vs. PCL scaffolds with surface modifications. Materials: Sterile 3D-printed scaffolds (Ø10mm x 2mm), Human Mesenchymal Stem Cells (hMSCs), Osteogenic Differentiation Media (OM: DMEM, 10% FBS, 10mM β-glycerophosphate, 50µg/mL ascorbic acid, 100nM dexamethasone), Alizarin Red S stain. Procedure:
- Pre-conditioning: Sterilize Ti scaffolds via autoclaving. Etch Ti scaffolds in 1:1 mixture of 98% H₂SO₄ and 30% H₂O₂ for 1 hr at 60°C, rinse 3x with sterile DI water. Coat experimental group with nanoscale hydroxyapatite via electrochemical deposition.
- Seeding: Seed hMSCs at a density of 50,000 cells/scaffold in standard growth media. Allow adhesion for 6 hrs.
- Differentiation: After 24 hrs, replace media with OM. Refresh media every 3 days.
- Analysis (Day 21): Fix cells with 4% PFA for 15 min. Stain with 2% Alizarin Red S (pH 4.2) for 20 min. Wash extensively. For quantification, destain with 10% cetylpyridinium chloride for 1 hr and read absorbance at 562 nm.
- Data Normalization: Report as nmoles of Alizarin Red S per µg of total DNA (measured via PicoGreen assay).
Protocol 2: Dynamic Mechanical Loading of Scaffold-Bone Constructs
Objective: To evaluate stress shielding and bone adaptation in a simulated femoral defect model. Materials: 3D-printed Ti-6Al-4V and Ti-35Nb-5Ta-7Zr scaffolds (porosity: 70%, pore size: 500µm), PCL scaffolds (porosity: 70%), Bioreactor with cyclic compression capability, Bone analog (polyurethane foam mimicking cancellous bone). Procedure:
- Construct Assembly: Pot cylindrical scaffolds (Ø6mm x 15mm) into a standardized bone analog defect using biocompatible epoxy, creating a press-fit model.
- Bioreactor Setup: Mount constructs in bioreactor chambers filled with cell culture media maintained at 37°C, 5% CO₂.
- Loading Regime: Apply a sinusoidal compressive load at 1 Hz for 1 hour daily. Use a peak stress of 5 MPa (approximating human gait) for 28 days. Include unloaded controls.
- Strain Measurement: Use embedded strain gauges on the bone analog to measure deformation. Calculate the load transfer ratio (Strain in construct/Strain in native analog).
- Post-analysis: Micro-CT scanning to assess bone analog density changes at the implant interface. Higher density indicates positive remodeling; lower density indicates stress shielding.
Diagrams
Research Workflow for Scaffold Comparison
Ti Scaffold Osteogenic Signaling Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Titanium vs. PCL Scaffold Research
| Item | Function & Rationale |
|---|---|
| Ti-6Al-4V ELI Powder (Grade 23, 15-45µm) | Feedstock for SLM/EBM printing. ELI grade ensures high purity for reproducible biocompatibility studies. |
| Medical Grade PCL Filament (MW ~80,000 Da) | Feedstock for FDM printing. Medical grade ensures consistent viscosity, purity, and degradation profile. |
| α-Minimal Essential Media (α-MEM) with 10% FBS | Standard culture medium for bone-forming cells (osteoblasts, hMSCs). Provides essential nutrients and growth factors. |
| Osteogenic Supplement Cocktail (Dexamethasone, Ascorbic Acid, β-Glycerophosphate) | Induces and supports the osteogenic differentiation of stem cells on test scaffolds. |
| AlamarBlue or PrestoBlue Cell Viability Reagent | Resazurin-based assay for non-destructive, quantitative monitoring of cell proliferation on 3D scaffolds over time. |
| Alizarin Red S Solution (pH 4.1-4.3) | Histochemical stain that binds to calcium deposits. The gold standard for quantifying mineralization in vitro. |
| RGD Peptide Solution (Arg-Gly-Asp) | Coating for PCL scaffolds to enhance integrin-mediated cell adhesion, mimicking the natural extracellular matrix. |
| Simulated Body Fluid (SBF, 10x Concentrate) | Used in bioactivity tests. Formation of bone-like apatite on a material surface in SBF indicates high osteoconductivity. |
| Hydrofluoric & Nitric Acid Etching Solution | For controlled surface roughening of titanium to enhance mechanical interlocking and cellular response. |
| Micro-CT Calibration Phantom | Essential for quantitative analysis of bone ingrowth into scaffold pores and mineral density in in vivo models. |
Within the paradigm of bone tissue engineering, the search for optimal scaffold materials juxtaposes permanent metallic solutions, like titanium alloys, against biodegradable polymers. Polycaprolactone (PCL) emerges as a key biodegradable contender, offering a unique balance of prolonged degradation, biocompatibility, and tunable mechanics suitable for facilitating bone regeneration.
Key Characteristics and Quantitative Data
Table 1: Core Characteristics of PCL vs. Titanium Alloys (Ti-6Al-4V) for Bone Scaffolds
| Characteristic | Polycaprolactone (PCL) | Titanium Alloy (Ti-6Al-4V) |
|---|---|---|
| Degradation Profile | Hydrolytic & enzymatic; 2-4 years in vivo | Essentially non-degradable; bioinert |
| Young's Modulus | 0.2 - 0.8 GPa | ~110 GPa |
| Tensile Strength | 10 - 50 MPa | ~1000 MPa |
| Melting Point | 60°C | ~1650°C |
| 3D Print Method | Fused Deposition Modeling (FDM), Melt Electrospinning Writing (MEW) | Selective Laser Melting (SLM), Electron Beam Melting (EBM) |
| Biocompatibility | Excellent; supports cell adhesion & proliferation | Excellent; osteoconductive |
| Bioactivity | Inert; requires surface modification/ composites (e.g., hydroxyapatite) for bone bonding | Intrinsically osteoconductive; forms bone-bonding apatite layer |
| Resorption Outcome | Replaced by native tissue | Permanent implant; potential stress shielding |
Table 2: Optimized 3D Printing Parameters for PCL Bone Scaffolds (FDM)
| Parameter | Typical Value Range | Functional Impact |
|---|---|---|
| Nozzle Temperature | 80 - 120°C | Ensures complete melting & flow. |
| Build Plate Temperature | 40 - 60°C | Improves layer adhesion and prevents warping. |
| Print Speed | 5 - 20 mm/s | Balances resolution and structural integrity. |
| Nozzle Diameter | 100 - 400 µm | Determines strut diameter and pore size. |
| Layer Height | 100 - 300 µm | Affects z-axis resolution and print time. |
| Infill Pattern/ Porosity | 50-70% porosity (grid, hexagonal) | Critical for nutrient diffusion, cell infiltration, and mechanical compliance. |
Application Notes and Protocols
Protocol 1: Fabrication of PCL Scaffolds via FDM for Osteogenesis Studies
Objective: To manufacture reproducible, porous PCL scaffolds for in vitro osteogenic differentiation assays.
Materials (Research Reagent Solutions):
- Medical-grade PCL Pellet: (e.g., Purac Capa 6500) – Raw material with defined molecular weight for consistent melt viscosity.
- Solvent: Chloroform – For preparing PCL coatings or cleaning equipment.
- Cell Culture Media: Alpha-MEM – Basal medium for bone cell culture.
- Osteogenic Supplements: β-glycerophosphate, Ascorbic Acid, Dexamethasone – Induces osteogenic differentiation of mesenchymal stem cells (MSCs).
- AlamarBlue or MTT Reagent: Colorimetric assay for quantifying cell viability/proliferation.
- Alizarin Red S Stain: Dye for detecting and quantifying calcium-rich deposits (mineralization).
Methodology:
- Printer Setup & Calibration:
- Load PCL filament into the FDM printer. Ensure feedstock is dry.
- Level the build plate. Set parameters as per Table 2 (e.g., 90°C nozzle, 45°C plate).
- Design & Slicing:
- Design a 3D model (e.g., disc, 10mm diameter x 2mm height) with CAD software.
- Use slicing software to generate a porous structure (e.g., 0/90° laydown pattern, 60% porosity).
- Export G-code and upload to the printer.
- Printing:
- Execute print in a controlled environment (low draft).
- Allow scaffold to cool gradually on the build plate.
- Post-processing:
- Sterilize scaffolds by immersion in 70% ethanol for 30 minutes, followed by UV irradiation per side for 15 minutes.
- Rinse 3x with sterile phosphate-buffered saline (PBS).
- Cell Seeding (Under Aseptic Conditions):
- Pre-wet scaffolds in culture medium for 1 hour.
- Seed with human MSCs at a density of 5 x 10^4 cells/scaffold in a low-attachment plate.
- After 2 hours, add osteogenic media. Refresh media every 3 days.
- Analysis:
- Monitor proliferation weekly (AlamarBlue).
- Assess mineralization at day 21-28 (Alizarin Red S staining and quantification via cetylpyridinium chloride extraction).
Title: PCL Scaffold Fabrication & Cell Culture Workflow
Protocol 2: Coating PCL Scaffolds with Hydroxyapatite (HAp) for Enhanced Bioactivity
Objective: To deposit a biomimetic, osteoconductive HAp layer on PCL scaffolds via simulated body fluid (SBF) incubation.
Materials:
- 10x Simulated Body Fluid (SBF): Prepared according to Kokubo protocol – Supersaturated solution mimicking ionic blood plasma for apatite nucleation.
- 5.0M Sodium Hydroxide (NaOH): For adjusting and maintaining SBF pH at 7.4.
- Medical-grade PCL Scaffold: From Protocol 1.
Methodology:
- Surface Activation:
- Treat PCL scaffolds with 5.0M NaOH for 1 hour to hydrolyze surface and increase hydrophilicity.
- Rinse thoroughly with deionized water until neutral pH.
- SBF Preparation:
- Prepare 1x SBF by serial dilution of 10x stock, buffered to pH 7.4 at 36.5°C using HCl/NaOH.
- Coating Incubation:
- Immerse activated scaffolds in SBF (Scaffold volume : SBF volume ≈ 1:100).
- Incubate at 36.5°C for 7-14 days without agitation.
- Refresh SBF solution every 48 hours to maintain ion concentration.
- Harvesting:
- Carefully remove scaffolds and rinse gently with deionized water to remove loosely bound crystals.
- Dry overnight in a desiccator.
- Characterization:
- Analyze coating morphology via scanning electron microscopy (SEM).
- Confirm HAp composition via energy-dispersive X-ray spectroscopy (EDS) peaks for Calcium (Ca) and Phosphorus (P).
Title: Hydroxyapatite Coating Protocol on PCL
Signaling Pathway Context: PCL/HAp Scaffold Osteoinduction
PCL itself is not osteoinductive, but when combined with HAp or osteogenic cells, it facilitates key bone-forming pathways.
Title: PCL/HAp-Induced Osteogenic Signaling
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for PCL Bone Scaffold Research
| Reagent/Material | Function & Rationale |
|---|---|
| Medical-grade PCL (Capa 6500) | High-purity, biocompatible polymer with consistent Mn (~50,000) for reproducible melt processing. |
| Simulated Body Fluid (SBF) | Induces biomimetic apatite coating on polymers, enhancing bioactivity and osteoconduction. |
| β-Glycerophosphate | Osteogenic media component; provides phosphate source for alkaline phosphatase (ALP) to generate mineral deposits. |
| Alizarin Red S | Histochemical stain that binds to calcium; standard for quantifying in vitro mineralization. |
| Type I Collase Solution | Enzymatic digestion for harvesting cells from 3D scaffolds or digesting mineral for Alizarin Red quantification. |
| Fetal Bovine Serum (FBS) | Essential supplement for cell culture media; provides growth factors and proteins for MSC attachment and expansion. |
| Dexamethasone | Synthetic glucocorticoid in osteogenic media; induces MSC commitment to osteoblast lineage via glucocorticoid receptor signaling. |
| Phalloidin (F-actin stain) | Fluorescent dye for visualizing cytoskeletal organization and cell morphology on scaffold struts via confocal microscopy. |
This document, framed within a thesis comparing 3D-printed titanium alloys to polycaprolactone (PCL) for bone scaffolds, outlines the core functional requirements for an ideal bone scaffold and provides detailed application notes and protocols for their evaluation. The objective is to guide researchers in matching material properties to specific clinical and experimental needs.
Core Functional Requirements & Quantitative Comparison
The ideal bone scaffold must satisfy a multi-faceted set of mechanical, biological, and processing requirements. The following table summarizes key quantitative targets and compares two prominent 3D-printable materials: Titanium Alloy (Ti-6Al-4V) and Polycaprolactone (PCL).
Table 1: Quantitative Requirements & Material Comparison for Bone Scaffolds
| Requirement Category | Specific Parameter | Ideal Target Range | Titanium Alloy (Ti-6Al-4V) | Polycaprolactone (PCL) |
|---|---|---|---|---|
| Mechanical | Compressive Modulus | 0.05 - 20 GPa (Trabecular to Cortical) | 110 - 120 GPa | 0.4 - 0.6 GPa (Neat) |
| Mechanical | Compressive Strength | 2 - 200 MPa | 500 - 1000 MPa* | 10 - 50 MPa* |
| Structural | Porosity | 50 - 90% | Highly tunable via design | Highly tunable via design |
| Structural | Pore Size | 100 - 600 μm (for bone ingrowth) | Achievable via SLM/EBM | Achievable via FDM/Melt Electrospinning |
| Biological | Degradation Rate | Match bone regeneration rate (months-years) | Non-degradable (Bioinert) | ~2-4 years in vivo (Tunable) |
| Biological | Surface Chemistry | Osteoconductive/ Osteoinductive | Requires coating (e.g., HA) for bioactivity | Requires modification/blending for bioactivity |
| Manufacturing | Feature Resolution | < 100 μm for microarchitecture | ~30-100 μm (SLM) | ~100-300 μm (FDM) |
Note: Scaffold effective strength is highly dependent on porosity and architecture. Ti-6Al-4V values are for solid material; PCL values are for porous constructs.
Detailed Experimental Protocols
Protocol: In Vitro Osteogenic Differentiation Assay
Purpose: To evaluate the osteoconductivity and bioactivity of scaffold materials (e.g., coated Ti-6Al-4V vs. PCL-composite).
Materials:
- Sterile test scaffolds (Ø 5mm x 2mm height).
- Human Mesenchymal Stem Cells (hMSCs), passage 3-5.
- Osteogenic Differentiation Medium: α-MEM, 10% FBS, 10 mM β-glycerophosphate, 50 µg/mL ascorbic acid, 100 nM dexamethasone.
- Control: Expansion Medium (α-MEM, 10% FBS).
- 24-well low-attachment plates.
Procedure:
- Sterilization: Autoclave Ti-6Al-4V scaffolds (dry cycle). Sterilize PCL scaffolds in 70% ethanol for 30 min, followed by PBS rinses.
- Seeding: Pre-wet scaffolds in medium. Seed hMSCs at 50,000 cells/scaffold in 20 µL of expansion medium. Incubate for 2 hours (37°C, 5% CO₂) to allow adhesion, then add 1 mL of medium per well.
- Induction: After 24 hours, replace medium with Osteogenic or Control Medium. Change medium every 3 days.
- Analysis:
- Day 7 & 14: Alkaline Phosphatase (ALP) activity assay (use pNPP substrate, measure absorbance at 405 nm). Normalize to total DNA content.
- Day 21 & 28: Alizarin Red S (ARS) staining for calcium deposits. Quantify by dissolving stain with 10% cetylpyridinium chloride and measuring absorbance at 562 nm.
- Statistical Analysis: Perform ANOVA with post-hoc Tukey test (n=6, p<0.05).
Protocol: Mechanical Characterization of Porous Scaffolds
Purpose: To determine the effective compressive modulus and strength of 3D-printed porous scaffolds.
Materials:
- Cylindrical scaffolds (Ø 8mm x 10mm height, n=5 per group).
- Universal Testing Machine (e.g., Instron 5944) with a 1 kN load cell.
- Two parallel, hardened steel compression plates.
Procedure:
- Conditioning: Store scaffolds in PBS at 37°C for 48 hours prior to testing to simulate hydrated state.
- Setup: Calibrate the machine. Place scaffold centered on the lower plate. Set crosshead speed to 0.5 mm/min.
- Compression Test: Apply compressive load until scaffold is compressed to ~50% of its original height or until catastrophic failure. Record force vs. displacement data.
- Data Analysis:
- Calculate Engineering Stress (σ) = Force / Original Cross-sectional Area.
- Calculate Engineering Strain (ε) = Displacement / Original Height.
- Generate stress-strain curve.
- Determine Compressive Modulus (E) as the slope of the initial linear elastic region (typically 0-5% strain).
- Determine Compressive Strength at Yield as the stress at the 0.2% offset yield point.
Diagrams
Title: Ideal Bone Scaffold Requirement Categories
Title: Scaffold Development & Testing Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Bone Scaffold Research
| Item | Function & Application | Example/Supplier Note |
|---|---|---|
| hMSCs (Human Mesenchymal Stem Cells) | Gold-standard primary cell line for evaluating osteogenic differentiation potential on scaffolds. | Lonza, Thermo Fisher. Use low passage number (P3-P5). |
| Osteogenic Supplement Kit | Provides standardized concentrations of β-glycerophosphate, ascorbic acid, and dexamethasone for consistent differentiation assays. | Thermo Fisher (A1007201), Sigma (SCR028). |
| AlamarBlue or MTS Reagent | Colorimetric/fluorometric assays for quantifying metabolically active cells on scaffolds (cytocompatibility). | Thermo Fisher (DAL1100), Promega (G3580). |
| Alizarin Red S Solution | Histochemical stain for detecting and quantifying calcium phosphate deposits (mineralization). | Sigma (A5533). Requires pH adjustment to 4.2. |
| Osteocalcin (OCN) ELISA Kit | Quantifies osteocalcin, a late-stage osteogenic differentiation marker, in cell culture supernatants. | Abcam (ab195214), R&D Systems (DY1419). |
| Simulated Body Fluid (SBF) | Solution ionically similar to human plasma. Used for in vitro bioactivity testing (apatite formation on surfaces). | Prepare via Kokubo's method or commercial kits (e.g., ChemCruz). |
| Micro-CT Scanner (e.g., SkyScan) | For high-resolution 3D analysis of scaffold porosity, pore size distribution, and mineralized tissue ingrowth ex vivo. | Bruker, Scanco Medical. |
| 3D Bioprinter/FDM Printer | For fabricating scaffolds with controlled architecture. FDM for PCL, SLM/EBM for Ti alloys. | FDM: CELLINK BIO X; Metal: EOS M 100. |
| Hydroxyapatite (HA) Nanopowder | For blending with PCL or coating Ti surfaces to enhance osteoconductivity and surface bioactivity. | Sigma (677418), particle size < 200 nm. |
| RGD Peptide Solution | Cell-adhesive peptide used to functionalize the surface of synthetic polymers (like PCL) to improve cell attachment. | Merck (CC1052), typically cyclic RGDfK. |
Application Notes
This document provides application notes for the selection of permanent titanium (Ti-6Al-4V) alloy versus temporary polycaprolactone (PCL) scaffolds in bone regeneration. The decision framework is situated within a thesis on 3D-printed patient-specific bone constructs, focusing on the dichotomy between permanent structural support and transient, bioactive resorption.
Permanent Titanium Alloy (Ti-6Al-4V) Scaffolds:
- Primary Rationale: Selected for large, critical-size load-bearing defects (e.g., mandibular reconstruction, spinal fusion) where indefinite mechanical integrity is paramount.
- Key Advantage: Superior and enduring yield strength and fatigue resistance match or exceed cortical bone, preventing catastrophic failure.
- Clinical Consideration: Risk of stress-shielding over long periods due to high stiffness modulus. Requires secondary surgery for removal if problematic. Excellent osseointegration via direct bone-on-implant contact but is bioinert without surface functionalization.
Temporary Resorbable PCL Scaffolds:
- Primary Rationale: Indicated for non-critical or moderate-size defects where the natural bone healing cycle (3-12 months) can eventually assume load. The scaffold provides temporary mechanical support and a template for guided bone regeneration.
- Key Advantage: Biodegradability (typical resorption profile: 2-4 years) eliminates need for implant removal. Degradation products are metabolically benign. Easily functionalized with bioceramics (e.g., hydroxyapatite, β-Tricalcium Phosphate) or drugs.
- Clinical Consideration: Mechanical properties are inferior to titanium and cortical bone, limiting use to low-load or load-sharing applications. Degradation kinetics and mechanical decay must be meticulously matched to new bone formation rates to avoid collapse.
Table 1: Core Material Properties Comparison
| Property | Ti-6Al-4V (ELI, ASTM F136) | PCL (Medical Grade) | Human Cortical Bone |
|---|---|---|---|
| Young's Modulus (GPa) | 110 - 125 | 0.4 - 0.8 | 15 - 20 |
| Tensile/Compressive Yield Strength (MPa) | 795 - 950 | 20 - 40 | 130 - 180 |
| Porosity Range for Osteoconduction | 50-70% (designed) | 60-80% (designed) | N/A (Natural Structure) |
| Fatigue Strength (MPa, 10⁷ cycles) | ~500 | < 10 | ~70 |
| Degradation Profile | Non-resorbable (Corrosion possible) | 2 - 4 years (Hydrolytic) | N/A |
Table 2: In Vivo Performance Metrics Summary
| Performance Metric | 3D-Printed Ti-6Al-4V Scaffold | 3D-Printed PCL+HA Composite Scaffold |
|---|---|---|
| Time to Initial Osseointegration | 4 - 8 weeks | 2 - 4 weeks |
| Bone Ingrowth Depth at 12 weeks | 1.0 - 1.8 mm | 1.5 - 2.5 mm |
| Peak Inflammation Period | 2 - 4 weeks (acute) | 4 - 8 weeks (chronic, degradation-driven) |
| Typical Study Duration (Pre-clinical) | 12 - 52 weeks | 24 - 104 weeks (to track resorption) |
Experimental Protocols
Protocol 1: In Vitro Degradation and Mechanical Decay of PCL Scaffolds
Objective: To characterize the mass loss, change in pH, and compressive modulus of 3D-printed PCL scaffolds under simulated physiological conditions.
- Scaffold Fabrication: Print PCL and PCL+20% HA (w/w) scaffolds (Φ10mm x 5mm) via fused deposition modeling (FDM). Sterilize using 70% ethanol and UV light.
- Degradation Medium: Prepare phosphate-buffered saline (PBS, pH 7.4) with 0.02% sodium azide. Add 100 U/ml penicillin-streptomycin.
- Incubation: Immerse scaffolds (n=6 per group) in 10 ml medium per scaffold. Maintain at 37°C in an orbital shaker at 60 rpm.
- Sampling & Analysis:
- Time Points: 1, 4, 12, 24, 52 weeks.
- Mass Loss: Rinse retrieved scaffolds, dry to constant weight. Calculate percentage mass remaining.
- pH Monitoring: Record pH of incubation medium at each time point.
- Mechanical Testing: Perform unconfined compression test on wet samples to determine elastic modulus and yield strength.
- Morphology: Assess pore structure and surface erosion via scanning electron microscopy (SEM).
Protocol 2: In Vivo Osseointegration Comparison in a Rabbit Femoral Condyle Model
Objective: To compare early-stage bone ingrowth and osteogenesis for porous Ti-6Al-4V vs. PCL-TCP scaffolds.
- Scaffold Preparation: Fabricate cylindrical scaffolds (Φ4mm x 6mm). Ti scaffolds: clean and autoclave. PCL-TCP scaffolds: sterilize via ethylene oxide.
- Animal Model: Use 36 skeletally mature New Zealand White Rabbits (approved by IACUC). Create bilateral, non-critical-size defects (Φ4mm x 6mm) in femoral condyles.
- Implantation: Randomly implant Ti-6Al-4V (left) and PCL-TCP (right) scaffolds. Allow free movement post-op.
- Termination & Analysis: Euthanize groups (n=6) at 2, 6, and 12 weeks.
- Micro-CT: Quantify bone volume/total volume (BV/TV) within scaffold pores and adjacent bone.
- Histology: Process undecalcified (Ti) and decalcified (PCL) sections for Van Gieson's picro fuchsin (for bone) and H&E (for cellular detail) staining. Score osteointegration using a standardized scale.
- Biomechanics: Perform push-out test on a subset of samples to measure interfacial shear strength.
Visualizations
Material Selection Decision Flow
PCL Scaffold Degradation & Bone Regeneration Pathway
The Scientist's Toolkit
Table 3: Essential Research Reagents & Materials
| Item | Function in Research | Specification / Rationale |
|---|---|---|
| Ti-6Al-4V ELI Powder | Raw material for SLM/DMLS 3D printing. | Grade 23, ASTM F136. Low interstitial elements (O, N) enhance ductility and fatigue resistance. |
| Medical Grade PCL Pellets | Raw material for FDM/Extrusion-based 3D printing. | Inherent viscosity ~1.8 dL/g. Certificates for biocompatibility (ISO 10993) and high purity. |
| β-Tricalcium Phosphate (β-TCP) Powder | Bio-ceramic additive for PCL composite. | Enhances osteoconductivity and buffer acidic degradation products. Typical blend: 20-30% w/w. |
| Simulated Body Fluid (SBF) | In vitro bioactivity and apatite formation test. | Ion concentration equal to human blood plasma, per Kokubo protocol. |
| AlamarBlue / MTS Assay Kit | Quantify in vitro cytocompatibility and cell proliferation on scaffolds. | Water-soluble, non-toxic resazurin-based assay. Preferred over MTT for 3D scaffolds. |
| Osteogenic Differentiation Media | Induce osteogenic lineage in mesenchymal stem cells (MSCs) in vitro. | Contains Dexamethasone, β-glycerophosphate, and Ascorbic Acid. |
| Polyclonal Anti-Osteocalcin Antibody | Immunohistochemical staining for mature osteoblasts in explanted tissue. | Key marker for terminal osteogenic differentiation and bone mineralization. |
| Micro-CT Calibration Phantom | Calibrate Hounsfield Units to mineral density for bone quantification. | Essential for accurate, reproducible BV/TV and BMD measurements in vivo. |
From Powder to Polymer: Advanced Manufacturing Techniques for Titanium and PCL Scaffolds
Application Notes: SLM vs. EBM for Ti-6Al-4V in Bone Scaffold Research
In the context of a thesis comparing 3D printing titanium alloys (Ti-6Al-4V) versus Polycaprolactone (PCL) for bone scaffolds, SLM and EBM represent the primary metal additive manufacturing (AM) modalities. Their capabilities for producing complex, porous, and load-bearing metallic structures make them critical for orthopaedic implant research.
Core Differentiators:
- Atmosphere: SLM operates under an inert argon or nitrogen atmosphere. EBM requires a high vacuum (<1×10⁻³ mbar). This makes EBM unsuitable for volatile material integration but superior for reactive metals.
- Energy Source & Speed: SLM uses a focused Nd:YAG or fiber laser, typically with a smaller spot size (50-100 µm) and slower build rates. EBM uses a focused electron beam, with a larger spot size (~100-200 µm) and faster build rates due to higher energy input and preheating.
- Preheating & Residual Stress: EBM preheats the powder bed to 600-700°C, resulting in near stress-free, ductile parts with a coarse alpha-lath microstructure. SLM parts have high cooling rates, leading to fine acicular α' martensite, higher strength, but significant residual stress requiring post-build heat treatment.
- Surface & Accuracy: SLM produces parts with higher surface finish and finer feature resolution, suitable for intricate scaffold geometries. EBM parts have a rougher, sintered surface which may be beneficial for bone on-growth but requires post-processing for precision fit.
- Porosity Control: Both techniques can generate controlled porosity via unit cell design (e.g., gyroid, diamond). SLM offers higher precision in pore geometry. EBM's powder sintering can lead to slightly varying pore sizes.
Summary for Bone Scaffold Context: EBM-produced Ti-6Al-4V may be preferable for bulk, load-bearing scaffold sections where ductility and minimal residual stress are critical. SLM is better suited for patient-specific, high-resolution, complex porous networks that mimic trabecular bone architecture. Both are compared to PCL, which offers biodegradability and drug-eluting potential but lacks the mechanical strength for major load-bearing applications.
Quantitative Data Comparison
Table 1: Process & Mechanical Property Comparison for Ti-6Al-4V
| Parameter | Selective Laser Melting (SLM) | Electron Beam Melting (EBM) | PCL (FDM/DLP) |
|---|---|---|---|
| Beam Type | Laser (Fiber/Nd:YAG) | Electron Beam | N/A (Extruder/UV Light) |
| Atmosphere | Inert Gas (Ar, N₂) | High Vacuum (<10⁻³ mbar) | Ambient or Nitrogen |
| Build Temp. | 80-200°C (Plate) | 600-700°C (Powder Bed) | Ambient or <100°C |
| Typical Layer Thickness | 20-50 µm | 50-70 µm | 100-200 µm |
| Tensile Strength (As-built) | 1100-1300 MPa | 900-1050 MPa | 20-50 MPa |
| Elongation at Break (As-built) | 5-10% | 10-15% | 300-1000% |
| Surface Roughness (Ra) | 10-25 µm | 25-40 µm | 10-30 µm |
| Minimum Feature Size | ~100 µm | ~200 µm | ~200-500 µm |
| Residual Stress | Very High | Low | Negligible |
| Biocompatibility | Excellent | Excellent | Excellent, Biodegradable |
Table 2: In-Vitro Osteogenic Response (Typical Range from Literature)
| Material & Process | Cell Viability (MG-63, % vs Control) | Alkaline Phosphatase Activity (Day 14, % Increase) | Calcium Deposition (Day 21, µg/cm²) |
|---|---|---|---|
| Ti-6Al-4V (SLM, acid-etched) | 95-110% | 180-250% | 45-65 |
| Ti-6Al-4V (EBM, as-built) | 90-105% | 150-220% | 40-60 |
| PCL (Porous Scaffold) | 85-100% | 120-180% | 30-50 |
| Tissue Culture Plastic (Control) | 100% | 100% | 5-10 |
Experimental Protocols
Protocol 1: Fabrication of Ti-6Al-4V Porous Scaffolds via SLM
Objective: To manufacture Ti-6Al-4V bone scaffold with defined gyroid porosity for mechanical and biological testing. Materials: Gas-atomized Ti-6Al-4V ELI powder (20-63 µm), SLM machine (e.g., EOS M 290, SLM Solutions 280), argon gas. Methodology:
- Design: Design a 10x10x10 mm cube with a gyroid lattice structure using CAD (e.g., nTopology, Materialise Magics). Target porosity: 70%. Pore size: 500 µm. Export as .stl file.
- File Preparation: Import .stl into machine software. Orient part to minimize supports. Apply standard Ti-6Al-4V parameter set (e.g., laser power 175 W, scan speed 1200 mm/s, hatch distance 110 µm, layer thickness 30 µm). Generate support structures for overhangs >45°.
- Machine Setup: Ensure argon atmosphere <0.1% O₂. Preheat build plate to 80°C. Recoat powder bed with fresh, dried powder.
- Build Execution: Initiate build. Monitor O₂ levels and process stability throughout.
- Post-Processing: Remove part from plate via wire EDM. Remove supports via grinding. Perform stress relief annealing (750°C for 2h, furnace cool under argon). Clean via ultrasonic cleaning in ethanol.
- Characterization: Measure dimensions, porosity (micro-CT), and surface roughness.
Protocol 2: In-Vitro Osteogenic Differentiation Assay on AM Scaffolds
Objective: To assess the osteogenic potential of MC3T3-E1 pre-osteoblasts on SLM/EBM Ti-6Al-4V vs. PCL scaffolds. Materials: Sterilized scaffolds (autoclaved for Ti, UV/ethanol for PCL), MC3T3-E1 cell line, α-MEM media, Osteogenic media (α-MEM + 10% FBS, 10 mM β-glycerophosphate, 50 µg/mL ascorbic acid, 100 nM dexamethasone), AlamarBlue (resazurin), ALP assay kit (pNPP), Alizarin Red S. Methodology:
- Seeding: Place scaffolds in 24-well plate. Seed cells at 50,000 cells/scaffold in 50 µL drops. Allow 2h attachment, then add 1 mL growth media. Incubate (37°C, 5% CO₂).
- Proliferation (Day 1,3,7): Aspirate media. Add 10% AlamarBlue in phenol-free media (1 mL/well). Incubate 4h. Measure fluorescence (Ex560/Em590). Calculate % reduction vs blank scaffold control.
- Differentiation: On Day 3, switch to osteogenic media. Change media every 3 days.
- ALP Activity (Day 14): Lyse cells in 0.1% Triton X-100. Incubate lysate with pNPP substrate (30 min, 37°C). Stop with 0.1M NaOH. Measure absorbance at 405 nm. Normalize to total protein (BCA assay).
- Mineralization (Day 21): Fix cells with 70% ethanol (1h). Stain with 2% Alizarin Red S (pH 4.2, 20 min). Wash. For quantification, dissolve bound stain in 10% cetylpyridinium chloride. Measure absorbance at 562 nm.
Visualization Diagrams
Workflow for AM Titanium Scaffold R&D
Osteogenic Signaling Pathway in Scaffold Assays
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for AM Titanium Scaffold Research
| Item | Function in Research | Example/Notes |
|---|---|---|
| Ti-6Al-4V ELI Powder (Grade 23) | Feedstock for SLM/EBM. ELI (Extra Low Interstitial) grade offers higher purity and fracture toughness, critical for implants. | Size: 20-63 µm. Supplier: AP&C, TLS Technik. |
| AlamarBlue / Resazurin | Cell viability and proliferation assay. Measures metabolic activity via fluorescence. Non-destructive, allowing longitudinal study. | Thermo Fisher Scientific, Sigma-Aldrich. |
| pNPP (p-Nitrophenyl Phosphate) | Substrate for colorimetric Alkaline Phosphatase (ALP) activity assay, a key early osteogenic differentiation marker. | Sold in ALP assay kits (e.g., Abcam, Sigma). |
| Alizarin Red S | Dye that binds to calcium deposits. Used for semi-quantitative and quantitative assessment of late-stage mineralization. | 2% solution, pH 4.1-4.3. |
| Osteogenic Media Supplements | Induces osteoblast differentiation. β-Glycerophosphate (phosphate source), Ascorbic Acid (collagen synthesis), Dexamethasone (glucocorticoid inducer). | Prepare fresh ascorbic acid aliquots. |
| Cell Line: MC3T3-E1 Subclone 4 | A well-characterized murine pre-osteoblast cell line, standard for in-vitro osteogenesis studies. | ATCC CRL-2593. |
| Micro-CT Scanner (e.g., SkyScan) | Non-destructive 3D analysis of scaffold porosity, pore size distribution, and interconnectivity. | Critical for pre-biological characterization. |
Application Notes
This document provides detailed application notes and protocols for three polymer processing techniques employed in the fabrication of polycaprolactone (PCL) scaffolds for bone tissue engineering. This work is contextualized within a broader thesis comparing 3D-printed titanium alloy scaffolds with biodegradable PCL constructs, focusing on the trade-offs between mechanical integrity, bioactivity, degradation kinetics, and manufacturing precision for in vitro and preclinical studies.
Fused Deposition Modeling (FDM) for PCL is a robust, accessible extrusion-based method ideal for producing scaffolds with defined macro-architectures (pore sizes 300-800 µm) and good compressive strength. It is best suited for in vitro mechanobiology studies or as a control for shape and initial mechanical performance against metal scaffolds. Its limitations include moderate resolution and anisotropic properties.
Selective Laser Sintering (SLS) enables the creation of complex, high-resolution PCL scaffolds with superior surface roughness and mechanical properties closer to isotropy compared to FDM. It is highly applicable for generating intricate, patient-specific scaffold geometries that mimic cancellous bone architecture, providing a more relevant comparison to the geometric fidelity achievable with titanium laser powder bed fusion.
Melt Electrospinning Writing (MEW) is a high-resolution additive manufacturing technique that produces ultrafine, precisely arranged PCL fibers (diameters 5-50 µm). It excels in creating scaffolds with biomimetic topographical cues at the cellular scale, ideal for investigating cell-material interactions, differentiation, and infiltration. Its comparison to metal scaffolds is less direct but crucial for understanding the role of micro-architecture in biological integration.
Quantitative Comparison of PCL Fabrication Techniques
Table 1: Summary of key process parameters and scaffold outcomes for PCL fabrication methods relevant to bone scaffold research.
| Parameter | Fused Deposition Modeling (FDM) | Selective Laser Sintering (SLS) | Melt Electrospinning Writing (MEW) |
|---|---|---|---|
| Typical Fiber/Feature Size | 200 - 500 µm | 80 - 150 µm (laser spot) | 5 - 50 µm |
| Pore Size Range | 300 - 800 µm | 200 - 600 µm | 50 - 300 µm |
| Porosity Range | 40 - 60% | 50 - 70% | 60 - 90% |
| Compressive Modulus (PCL) | 30 - 150 MPa | 50 - 200 MPa | 1 - 20 MPa |
| Key Process Temperature | Nozzle: 80 - 120°C | Powder Bed: 50 - 60°C; Laser: N/A | Nozzle: 80 - 120°C; Collector: RT |
| Build Rate | Medium (1-10 cm³/hr) | Slow (0.1-2 cm³/hr) | Very Slow (0.01-0.5 cm³/hr) |
| Resolution/Accuracy | Low-Medium | High | Very High |
| Primary Advantage | Cost-effective; Good mechanicals | Complex geometry; Good surface finish | High resolution; Biomimetic topography |
| Primary Disadvantage | Anisotropy; Limited resolution | Powder recycling; Thermal history | Slow speed; Delicate structures |
Table 2: Biological performance indicators for PCL scaffolds fabricated via different routes in bone tissue engineering contexts.
| Performance Indicator | FDM PCL Scaffolds | SLS PCL Scaffolds | MEW PCL Scaffolds |
|---|---|---|---|
| MC3T3-E1/hMSC Viability | High (>90% at 7 days) | High (>90% at 7 days) | Very High (>95% at 7 days) |
| Alkaline Phosphatase Activity | Moderate (2-3 fold increase) | Moderate-High (3-4 fold increase) | High (4-5 fold increase) |
| Mineralization (Ca²⁺ Deposition) | Moderate | High | High (aligned fiber guidance) |
| Protein Adsorption Capacity | Standard | Enhanced (higher surface roughness) | Very High (high surface area) |
| Degradation Rate (in vitro) | Slow (2-4 years in vivo) | Slow (2-4 years in vivo) | Tunable (increased surface area accelerates) |
Experimental Protocols
Protocol 1: FDM Fabrication of PCL Bone Scaffolds
Objective: To fabricate porous PCL scaffolds with a rectilinear grid structure for comparative mechanical testing against Ti-6Al-4V scaffolds. Materials:
- PCL pellets (Mn 45,000-80,000 g/mol)
- Desktop FDM 3D printer (e.g., modified RepRap)
- Heated build plate
- Slicing software (e.g., Cura, Simplify3D)
Methodology:
- Material Preparation: Dry PCL pellets at 40°C in a vacuum oven for 4 hours to remove moisture.
- Filament Extrusion: Use a single-screw extruder to produce 1.75 mm diameter filament. Parameters: Heated zones: 80°C, 95°C, 100°C; puller speed adjusted for consistent diameter (±0.05 mm).
- 3D Model & Slicing: Design a 10x10x5 mm³ cube with 0/90° laydown pattern in CAD. Import to slicer. Key parameters:
- Layer height: 0.2 mm
- Nozzle diameter: 0.4 mm
- Nozzle temperature: 100°C
- Build plate temperature: 45°C
- Printing speed: 20 mm/s
- Infill density: 60% (rectilinear)
- Pore size (designed): 400 µm
- Printing: Load PCL filament. Initiate print with skirt adhesion. Allow scaffold to cool on build plate post-print.
- Post-Processing: Inspect under light microscope. Clean with compressed air. Sterilize for cell culture using 70% ethanol (2 hr) followed by UV exposure (30 min per side).
Protocol 2: SLS Fabrication of PCL Bone Scaffolds
Objective: To fabricate complex, porous PCL scaffolds with high dimensional accuracy for in vitro osteogenesis studies. Materials:
- PCL powder (particle size 50-100 µm, Cryogenically milled and sieved)
- Benchtop SLS printer (e.g., Sinterit Lisa, Formlabs Fuse 1)
- Powder handling tools
Methodology:
- Powder Preparation: Dry PCL powder at 40°C in vacuum for 6 hours. Sieve (63 µm mesh) to ensure uniform particle distribution.
- 3D Model & Preparation: Design a 10 mm diameter x 5 mm height cylindrical scaffold with gyroid pore architecture (porosity ~65%). Convert to STL.
- Machine Setup: Load powder into feed cartridge. Set powder bed pre-heat temperature to 55°C (just below PCL melting point ~60°C).
- Printing Parameters:
- Laser power: 2.5 W (for 1060 nm diode laser)
- Scan speed: 1.5 m/s
- Layer thickness: 0.1 mm
- Hatch spacing: 0.1 mm
- Chamber atmosphere: Nitrogen (optional, to prevent oxidation)
- Print Execution: Run build job. Allow chamber to cool slowly to room temperature after completion to minimize warping.
- Post-Processing: Carefully de-powder the part using soft brushes and compressed air. Recover un-sintered powder for future use (up to 50% recycle ratio with fresh powder topping). Sterilize with ethylene oxide gas.
Protocol 3: MEW Fabrication of PCL Bone Scaffolds
Objective: To fabricate highly aligned, micro-fibrous PCL meshes for studying contact guidance of osteoblasts. Materials:
- Medical grade PCL (Mn 45,000 g/mol)
- MEW apparatus: Syringe pump, high-voltage supply (0-30 kV), heated metal nozzle (blunt-end, Gauge 20-23), temperature-controlled stage, XYZ motion collector.
- Solvent (optional, for cleaning): Dichloromethane.
Methodology:
- Polymer Melt Preparation: Load PCL pellets into a glass syringe barrel. Heat in an oven at 120°C for 1 hour to form a homogeneous, air-bubble-free melt.
- Apparatus Setup: Assemble heated syringe onto pump. Connect to heated nozzle (maintained at 105°C). Set collector (aluminum foil on grounded stage) distance to 5-10 mm from nozzle tip. Set syringe pump to a low flow rate (e.g., 50 µL/hr).
- Process Optimization & Printing: Apply high voltage (8-12 kV) to the nozzle. A stable, straight jet is required. Once stable, initiate programmed collector motion.
- Voltage: 10 kV
- Collector Distance: 8 mm
- Nozzle Temp: 105°C
- Flow Rate: 60 µL/hr
- Collector Speed: 500 mm/min (to achieve 100 µm fiber spacing)
- Pattern: Unidirectional lanes for 10 layers, rotating 90° per layer for a grid.
- Collection: After printing, carefully detach the scaffold from the collector. Anneal at 60°C for 15 minutes to improve inter-layer bonding.
- Sterilization: Due to delicate structure, use low-pressure plasma sterilization (Argon gas, 5 min) or antibiotic/antimycotic solution immersion (24 hr).
Visualizations
Thesis Evaluation Workflow for PCL Scaffolds
FDM Process Flow for PCL Scaffolds
SLS Process Flow for PCL Scaffolds
MEW Process Flow for PCL Scaffolds
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key materials and reagents for fabricating and evaluating PCL bone scaffolds.
| Item Name | Specification / Example | Primary Function in Research |
|---|---|---|
| Medical Grade PCL | Mn 45,000-80,000; CAPA 6500 | Raw biomaterial for scaffold fabrication. High Mn provides suitable mechanical strength & degradation time (~2-4 years). |
| Titanium Alloy Powder | Ti-6Al-4V, Grade 23, 15-45 µm | Control/comparison material for metal scaffold fabrication via laser powder bed fusion. |
| Dulbecco's Modified Eagle Medium (DMEM) | High glucose, with L-glutamine | Base cell culture medium for maintaining osteoblast precursors (e.g., MC3T3-E1, hMSCs). |
| Fetal Bovine Serum (FBS) | Qualified, Heat-inactivated | Essential supplement for cell culture medium to promote cell growth and differentiation. |
| Osteogenic Inducers | Ascorbic acid (50 µg/mL), β-glycerophosphate (10 mM), Dexamethasone (100 nM) | Chemical cocktail to induce osteogenic differentiation of stem cells on scaffolds. |
| AlamarBlue/CCK-8 Assay Kit | Pre-mixed reagent | Colorimetric assay for quantifying cell viability and proliferation on 3D scaffolds. |
| Alizarin Red S Solution | 2% (w/v), pH 4.1-4.3 | Stain for detecting and quantifying calcium deposits (mineralization) during osteogenesis. |
| Phosphate Buffered Saline (PBS) | 1X, sterile, without Ca²⁺/Mg²⁺ | Washing buffer for cell cultures and assays. |
| Paraformaldehyde (PFA) | 4% in PBS | Fixative for preserving cell morphology on scaffolds for imaging (SEM, fluorescence). |
| Critical Point Dryer | E.g., Samdri-PVT-3D | Instrument for preparing delicate hydrated samples (like cell-seeded MEW scaffolds) for SEM without structural collapse. |
| Micro-CT System | E.g., SkyScan 1272 | Non-destructive 3D imaging for quantifying scaffold porosity, pore size distribution, and interconnectivity. |
| Universal Mechanical Tester | E.g., Instron 5944 | For performing compressive/tensile tests on scaffolds to compare mechanical properties with titanium. |
Within the broader research thesis comparing 3D-printed titanium alloys (e.g., Ti-6Al-4V) versus polycaprolactone (PCL) for bone scaffold applications, Design for Additive Manufacturing (DfAM) is paramount. The core challenge is to engineer scaffolds that mimic the complex, hierarchical porosity of natural bone to facilitate osteointegration, vascularization, and mechanical stability. This document provides application notes and protocols for designing, manufacturing, and characterizing scaffolds with optimal porosity and pore architecture for bone regeneration.
Quantitative Comparison of Titanium vs. PCL Scaffold Parameters
The table below summarizes target and achieved parameters from recent studies for both material systems.
Table 1: Target vs. Achieved Scaffold Parameters for Ti-6Al-4V and PCL
| Parameter | Target Range (Bone Scaffold) | Typical Ti-6Al-4V (SLM/DMLS) | Typical PCL (FDM/MEW) | Key Functional Impact |
|---|---|---|---|---|
| Total Porosity | 50-90% | 60-80% | 70-90% | Influences cell migration, nutrient diffusion, and mechanical strength. |
| Pore Size | 100-600 µm (osteoconduction) | 300-600 µm | 200-500 µm | Critical for cell seeding, tissue ingrowth, and vascularization. |
| Pore Interconnectivity | >95% | >99% (from design) | 90-98% (can have residual support) | Ensures uniform tissue formation and prevents necrotic cores. |
| Strut/Feature Resolution | N/A | 50-200 µm | 100-300 µm | Determines architectural fidelity and surface area for cell attachment. |
| Elastic Modulus (Compressive) | 0.1-2 GPa (cancellous bone) | 1-5 GPa | 0.05-0.5 GPa | Match to host bone to reduce stress shielding (Ti) or provide adequate support (PCL). |
| Surface Area/Volume Ratio | High for cell attachment | Medium (smooth struts) | High (often textured) | Directly influences initial protein adsorption and cell adhesion. |
DfAM Protocols for Porosity Optimization
Protocol 3.1: Computational Design of Graded Porosity Scaffolds
Objective: To design a scaffold with a radially graded porosity, denser at the periphery for mechanical stability and more porous at the core for enhanced bioactivity.
Materials & Software:
- CAD Software (e.g., nTopology, Rhinoceros 3D with Grasshopper)
- TPMS (Triply Periodic Minimal Surface) unit cell library (e.g., Gyroid, Diamond, Schwarz P).
- Target porosity profile data.
Methodology:
- Define Geometry: Start with the outer boundary of the scaffold defect site.
- Select & Map TPMS Unit Cell: Select a Gyroid unit cell. Use a function to map the cell size (and thus porosity) relative to the radial distance from the center.
- Generate Lattice: Apply the graded TPMS field to the scaffold volume. The porosity (Φ) is controlled by the equation: Φ = 1 - (Volume of Solid TPMS / Volume of Bounding Cube).
- Boolean and Export: Perform a Boolean intersection of the graded lattice with the scaffold boundary. Export the final model as an STL or 3MF file for printing.
Protocol 3.2: Manufacturing & Post-Processing
A. For Titanium Alloy (Ti-6Al-4V) via Selective Laser Melting (SLM):
- Machine Preparation: Calibrate the SLM system (e.g., EOS M 290). Use a pre-alloyed Ti-6Al-4V powder (particle size 15-45 µm).
- Build Parameters: Orient scaffold to minimize support (typically vertical). Use a contour scanning strategy. Key parameters: Laser Power = 120-150 W, Scan Speed = 800-1200 mm/s, Hatch Distance = 80-110 µm, Layer Thickness = 30 µm.
- Post-Processing: Perform stress-relief annealing at 650°C for 3 hours in argon. Remove from build plate via wire EDM. Apply surface finishing via grit blasting (Al₂O₃, 250 µm) and acid etching (e.g., in 5% HF solution for 2-5 minutes) to increase surface roughness and bioactivity.
B. For Polycaprolactone (PCL) via Melt Electrowriting (MEW):
- Machine Preparation: Load medical-grade PCL (Mn 80,000) into a syringe, heat to 80-95°C. Use a stainless-steel nozzle (22-27G).
- Printing Parameters: Apply a high voltage (3-8 kV) between nozzle and collector. Use a pressurized air system (0.5-3 bar) for polymer extrusion. Key parameters: Collector speed = 200-1000 mm/min, Nozzle-to-collector distance = 3-8 mm, Temperature = 85°C.
- Post-Processing: After printing, scaffolds may be annealed at 55°C for 30 minutes to improve crystallinity and mechanical stability. Sterilize using ethylene oxide or low-dose gamma irradiation.
Characterization Protocols
Protocol 4.1: Micro-CT Analysis for Pore Architecture
Objective: To quantitatively analyze total porosity, pore size distribution, and interconnectivity. Equipment: Micro-CT scanner (e.g., SkyScan 1272). Method:
- Scanning: Mount scaffold on stage. Set voltage to 60 kV (PCL) or 100 kV (Ti), current accordingly. Use a 0.5 mm Al filter. Perform a 360° rotation with a rotation step of 0.4°. Achieve pixel size < 1/3 of minimum strut size.
- Reconstruction: Use NRecon software with standardized beam hardening and ring artifact correction.
- Analysis (CTAn):
- Binarization: Apply a global threshold to segment solid from void.
- 3D Analysis: Calculate total porosity (Po(tot)).
- Pore Size: Use sphere-fitting algorithm for local thickness measurement.
- Interconnectivity: Perform a pore isolation operation. Interconnectivity (%) = [Po(tot) - Po(iso)] / Po(tot) * 100, where Po(iso) is isolated porosity.
Protocol 4.2: In Vitro Biological Evaluation
Objective: To assess cell-scaffold interaction in terms of adhesion, proliferation, and osteogenic differentiation. Cell Line: Human Mesenchymal Stem Cells (hMSCs). Method:
- Sterilization & Pre-conditioning: Sterilize Ti scaffolds by autoclaving; PCL by ethanol immersion and UV exposure. Pre-soak in culture medium for 24h.
- Seeding: Seed scaffolds at a density of 50,000 cells/scaffold using the droplet method. Incubate for 2 hours before adding medium.
- Proliferation (Day 1, 3, 7): Use AlamarBlue assay. Incubate scaffolds in 10% AlamarBlue reagent for 3 hours. Measure fluorescence (Ex560/Em590).
- Osteogenic Differentiation:
- Culture: Maintain in osteogenic medium (with β-glycerophosphate, ascorbic acid, dexamethasone).
- Analysis (Day 14, 21):
- ALP Activity: Quantify using pNPP assay, normalize to total protein (BCA).
- Mineralization: Stain with Alizarin Red S, quantify by elution with cetylpyridinium chloride.
Visualizing the Osteogenic Signaling Pathway in Scaffolds
Diagram Title: Osteogenic Signaling in Porous Scaffolds
Experimental Workflow for Scaffold Evaluation
Diagram Title: Scaffold DfAM to Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Bone Scaffold Research
| Item | Function in Research | Example/Specification |
|---|---|---|
| Ti-6Al-4V ELI Powder | Metallic base material for high-strength, permanent scaffolds. | Grade 23, spherical, 15-45 µm diameter (for SLM). |
| Medical Grade PCL | Biodegradable polymer base material for temporary scaffolds. | Mn 80,000, inherent viscosity ~1.8 dL/g. |
| hMSCs | Primary cell model for in vitro osteogenesis studies. | Human Bone Marrow-derived, passage 4-6. |
| Osteogenic Supplement | Induces stem cell differentiation into osteoblast lineage. | Contains dexamethasone, ascorbate, and β-glycerophosphate. |
| AlamarBlue Reagent | Fluorescent indicator for quantifying cell viability and proliferation. | Resazurin-based, non-toxic, allows longitudinal study. |
| pNPP Substrate | Chromogenic substrate for quantifying Alkaline Phosphatase (ALP) activity. | Used in ALP assay as an early osteogenic marker. |
| Alizarin Red S | Dye that binds to calcium deposits for visualization and quantification of mineralization. | 2% solution (pH 4.1-4.3) for staining. |
| Micro-CT Calibration Phantom | Ensures accuracy and consistency of micro-CT quantitative measurements. | Hydroxyapatite phantom with known density. |
Application Notes
Within the thesis research on 3D-printed titanium alloy (Ti-6Al-4V) versus polycaprolactone (PCL) scaffolds for bone regeneration, post-processing is a critical determinant of the scaffold's final biomechanical properties, bioactivity, and clinical safety. For metallic alloys, post-processing aims to relieve residual stresses, enhance fatigue resistance, and create osteoconductive surfaces. For biodegradable polymers like PCL, the focus is on enhancing surface cell interactions without compromising structural integrity. Sterilization bridges the research-to-clinic gap, where method selection must preserve material properties while ensuring asepsis.
Data Presentation
Table 1: Comparative Effects of Post-Processing on Ti-6Al-4V vs. PCL Scaffolds
| Parameter | Ti-6Al-4V (Typical Values Post-Processing) | PCL (Typical Values Post-Processing) | Notes |
|---|---|---|---|
| Heat Treatment Temp. | 650-850°C (Annealing/HIP) | 50-60°C (Annealing) | HIP: Hot Isostatic Pressing. PCL temp. must remain below its melting point (~60°C). |
| Residual Stress Reduction | >90% reduction via HT | 70-80% reduction | Critical for fatigue life in metals; prevents creep in polymers. |
| Surface Roughness (Sa) | 1-5 µm (as-printed) → 0.5-2 µm (polished) or 10-50 µm (acid-etched) | 5-15 µm (as-printed) → Can be increased via hydrolysis | Roughness promotes osteoblast adhesion. Etching Ti creates micro/nano topography. |
| Hydrophilicity (Water Contact Angle) | 70-90° (native) → <10° (plasma treatment) | 70-110° (native) → 40-70° (NaOH treatment) | Hydrophilic surfaces enhance protein adsorption and cell attachment. |
| Recommended Sterilization | Autoclave (Steam), Dry Heat, Gamma Irradiation | Ethylene Oxide, Low-Temperature Plasma, Gamma Irradiation (with caution) | Gamma can degrade PCL mechanical properties >25 kGy. |
Table 2: Sterilization Protocol Impact on Material Properties
| Sterilization Method | Ti-6Al-4V Compatibility | PCL Compatibility | Key Parameters & Effects |
|---|---|---|---|
| Autoclave (Steam) | Excellent. No degradation. | Poor. Melts/deforms. | 121°C, 15-20 psi, 20 min. Standard for metals. |
| Dry Heat | Excellent. | Poor. Thermal deformation. | 160-180°C, 120 min. For heat-stable metals. |
| Ethylene Oxide (EtO) | Good. Residual gas must be aerated. | Excellent. Method of choice. | 37-55°C, 1-6 hrs exposure + 8-12 hrs aeration. |
| Gamma Irradiation | Excellent. | Conditional. Cross-linking/scission. | 25-40 kGy standard dose. >25 kGy reduces PCL Mw and strength. |
| Low-Temperature Plasma (H2O2) | Good. No residue. | Good. Minimal damage. | 45-50°C, 45-55 min. Complex geometries may be challenging. |
Experimental Protocols
Protocol 1: Stress-Relief Heat Treatment for Ti-6Al-4V Lattice Scaffolds
Objective: To relieve internal residual stresses from the laser powder bed fusion (LPBF) process without significantly altering microstructure.
- Place the as-printed Ti-6Al-4V scaffold in a vacuum or argon-purged tube furnace.
- Ramp temperature from room temperature to 650°C at a rate of 5°C per minute.
- Hold at 650°C for 2 hours.
- Allow to furnace-cool to below 200°C before removing.
- Characterize residual stress via X-ray diffraction (sin²ψ method) and compare yield strength via compression testing to as-printed controls.
Protocol 2: Alkaline Hydrolysis for PCL Surface Modification
Objective: To introduce carboxyl and hydroxyl groups onto PCL scaffold surfaces, enhancing hydrophilicity and protein adsorption.
- Immerse the 3D-printed PCL scaffold in 5M sodium hydroxide (NaOH) aqueous solution.
- Incubate at 37°C for 90 minutes under gentle agitation.
- Carefully remove the scaffold and rinse extensively with distilled water (5x, 5 minutes each) to remove all NaOH residue.
- Dry under vacuum for 24 hours.
- Characterize via water contact angle measurement and ATR-FTIR to confirm hydrolysis product formation (broad -OH stretch ~3400 cm⁻¹).
Protocol 3: Sterilization Validation for PCL Composite Scaffolds via Ethylene Oxide
Objective: To effectively sterilize PCL-based scaffolds without compromising chemical or mechanical integrity.
- Pre-condition scaffolds in a controlled humidity chamber (50-60% RH) for 12 hours.
- Load scaffolds into an EtO sterilization chamber, ensuring no overlapping.
- Execute cycle: Pre-vacuum, humidity injection (to 50-60% RH), EtO gas injection (500-600 mg/L), exposure at 37°C for 3 hours.
- Perform deep vacuum cycles to evacuate EtO gas.
- Transfer scaffolds to a validated aerator at 50°C for 12 hours.
- Validate sterility using USP <71> and assess residual EtO/ECH per ISO 10993-7. Test mechanical properties vs. non-sterilized controls.
Mandatory Visualization
Ti-6Al-4V Post-Processing Workflow
PCL Scaffold Post-Processing Workflow
Scaffold Sterilization Method Decision Tree
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Scaffold Post-Processing Research
| Item / Reagent | Function in Research | Example Use Case |
|---|---|---|
| Tube Furnace (Argon/Vacuum) | Provides controlled high-temperature environment for stress relief and sintering of metals. | Heat treatment of Ti-6Al-4V scaffolds. |
| Sodium Hydroxide (NaOH) Pellets | Alkaline agent for hydrolyzing ester bonds in PCL, creating hydrophilic surface groups. | Surface modification of PCL scaffolds (5M solution). |
| Hydrofluoric-Nitric Acid (HF-HNO3) Mix | Acid mixture for etching titanium alloys to create controlled micro-scale topography. | Surface roughening of Ti-6Al-4V for osseointegration. |
| Ethylene Oxide Sterilization Kit | Gas-based, low-temperature sterilization system for temperature-sensitive polymers. | Terminal sterilization of PCL-based composite scaffolds. |
| Plasma Surface Treater (O2 or Ar Plasma) | Generates reactive plasma to clean and functionalize surfaces, increasing energy. | Enhancing wettability of both Ti and PCL surfaces pre-coating. |
| Simulated Body Fluid (SBF) | Biomimetic solution to assess apatite-forming ability (bioactivity) of a modified surface. | Testing bioactivity of hydroxyapatite-coated Ti scaffolds. |
| X-ray Diffractometer (XRD) | Analyzes crystallographic structure, phase composition, and residual stress in materials. | Verifying phase changes in Ti-6Al-4V post-heat treatment. |
| Goniometer | Measures static water contact angle to quantify surface wettability/hydrophilicity. | Quantifying success of NaOH treatment on PCL. |
Navigating Material-Specific Challenges: Strategies to Optimize Titanium and PCL Scaffold Performance
Within the thesis comparing 3D-printed titanium alloys versus polycaprolactone (PCL) for bone scaffolds, a critical challenge for titanium is its high elastic modulus (∼110 GPa), leading to stress shielding and subsequent bone resorption. This document outlines application notes and protocols for two synergistic strategies: reducing the bulk modulus through porous lattice design and enhancing the surface bioactivity to promote osseointegration.
Table 1: Comparative Properties of Scaffold Materials and Designs
| Parameter | Solid Ti-6Al-4V | Porous Ti-6Al-4V Lattice (This Work) | PCL Scaffold | Cortical Bone |
|---|---|---|---|---|
| Elastic Modulus (GPa) | 110 - 115 | 2 - 20 (Tunable by design) | 0.2 - 0.4 | 10 - 30 |
| Porosity (%) | 0 | 60 - 80 | 70 - 90 | 5 - 10 (Haversian) |
| Average Pore Size (µm) | N/A | 400 - 700 | 250 - 500 | 100 - 300 (Osteon) |
| Yield Strength (MPa) | 850 - 1100 | 50 - 300 | 10 - 30 | 100 - 150 |
| Primary Fabrication Method | Machining, Casting | Laser Powder Bed Fusion (L-PBF) | Fused Deposition Modeling (FDM) | - |
Table 2: Surface Modification Techniques & Outcomes
| Technique | Process Summary | Key Outcome Metrics | Effect on Osteogenesis |
|---|---|---|---|
| Acid-Alkali (A-A) Treatment | Immersion in 5M NaOH, 60°C, 24h; then 5M HCl, 60°C, 24h. | Forms nanoscale network, Contact Angle: <10° (superhydrophilic) | Induces apatite formation in SBF; upregulates Runx2 expression. |
| Anodic Oxidation (AO) | In 1M H₃PO₄ + 0.5% HF, 10-20V, 1h. | Creates TiO₂ nanotubes (∼100 nm dia., ∼1 µm length). | Enhances mesenchymal stem cell (MSC) adhesion and alkaline phosphatase (ALP) activity by ∼200%. |
| Biomimetic Coating | Immersion in 5x Simulated Body Fluid (SBF), 37°C, 7 days. | Deposits carbonated hydroxyapatite (HAp) layer (∼20 µm thick). | Provides direct osteoconductive surface; enables BMP-2 peptide grafting. |
Experimental Protocols
Protocol 1: Design and Fabrication of Low-Modulus Porous Titanium Lattice via L-PBF
Objective: To fabricate a titanium scaffold with an elastic modulus <20 GPa. Materials:
- Ti-6Al-4V ELI powder (20-63 µm particle size).
- Commercial L-PBF system (e.g., EOS M 290, SLM Solutions 280).
- CAD software (e.g., nTopology, Materialise Magics) with gyroid or dodecahedron unit cell.
Procedure:
- Lattice Design: Using CAD software, design a 10x10x10 mm³ scaffold based on a triply periodic minimal surface (e.g., gyroid) unit cell. Set the target porosity to 70% and pore size to 600 µm.
- Support Generation & Slicing: Generate minimal supports for overhangs using auto-generation tools. Slice the model into layers (typically 30 µm thickness).
- Powbed Preparation: Load the build chamber with Ti-6Al-4V powder under argon atmosphere. Ensure oxygen level <0.1%.
- L-PBF Parameters: Set key parameters: Laser power = 170 W, Scan speed = 1200 mm/s, Hatch distance = 0.11 mm, Layer thickness = 30 µm. Use a stripe or chessboard scan pattern.
- Fabrication & Depowdering: Execute the build. After completion, carefully remove the scaffold from the build plate via wire EDM and ultrasonicate in ethanol to remove sintered powder.
Protocol 2: Combined Acid-Alkali and Anodic Oxidation Surface Treatment
Objective: To create a hierarchical nano-micro structured, bioactive surface on 3D-printed porous titanium. Materials:
- Fabricated porous Ti scaffold (from Protocol 1).
- 5M Sodium Hydroxide (NaOH) solution.
- 5M Hydrochloric Acid (HCl) solution.
- Electrolyte: 1M Phosphoric Acid (H₃PO₄) with 0.5wt% Hydrofluoric Acid (HF).
- DC Power Supply, Platinum cathode.
Procedure:
- Cleaning: Sonicate scaffolds in acetone, ethanol, and deionized water (DIW) for 15 min each. Dry in oven at 60°C.
- Acid-Alkali Treatment:
- Immerse scaffolds in 5M NaOH solution at 60°C for 24 hours.
- Rinse gently with DIW.
- Immerse in 5M HCl solution at 60°C for 24 hours.
- Rinse thoroughly with DIW and dry at 40°C.
- Anodic Oxidation:
- Assemble a two-electrode cell with the scaffold as the anode and a Pt mesh as the cathode, immersed in the H₃PO₄/HF electrolyte (0°C).
- Apply a constant DC voltage of 15V for 60 minutes.
- Rinse the scaffold copiously with DIW and dry in air.
- Post-treatment: Anneal the treated scaffold in a furnace at 450°C for 2 hours to crystallize the amorphous TiO₂ layer into anatase phase.
Protocol 3: In Vitro Osteogenic Differentiation Assay
Objective: To evaluate the bioactivity of modified titanium scaffolds versus controls. Materials: Human Bone Marrow Mesenchymal Stem Cells (hBM-MSCs), Osteogenic medium (OM), ALP assay kit (e.g., Sigma-Aldrich), Alizarin Red S (ARS) stain.
Procedure:
- Scaffold Sterilization: Sterilize scaffolds (untreated Ti, A-A+AO treated Ti, PCL control) in 70% ethanol for 2h, then UV irradiate for 1h per side.
- Cell Seeding: Seed hBM-MSCs at a density of 5x10⁴ cells per scaffold in a 48-well plate. Allow attachment for 4h in growth medium, then add OM.
- ALP Activity (Day 7): Lyse cells in 0.2% Triton X-100. Measure ALP activity using p-nitrophenyl phosphate substrate. Normalize to total protein content (BCA assay).
- Mineralization Assay (Day 21): Fix cells with 4% PFA for 15 min. Stain with 2% ARS solution (pH 4.2) for 20 min. Wash extensively. Quantify by eluting stain with 10% cetylpyridinium chloride and measuring absorbance at 562 nm.
- Gene Expression (qPCR, Day 14): Extract RNA, synthesize cDNA. Perform qPCR for osteogenic markers (Runx2, OPN, OCN) normalized to GAPDH.
Visualizations
Title: Stress Shielding vs. Modulus Reduction
Title: Surface Bioactivation Signaling Pathway
Title: Integrated Scaffold Development Workflow
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions & Materials
| Item | Function/Application | Key Notes |
|---|---|---|
| Ti-6Al-4V ELI Powder | Raw material for L-PBF fabrication of scaffolds. | Use gas-atomized, spherical powder (20-63 µm). ELI grade ensures low interstitial elements. |
| 5x Simulated Body Fluid (5x SBF) | Accelerated biomimetic hydroxyapatite coating. | Higher ion concentration vs. 1x SBF reduces coating time from 28 to ~7 days. |
| Osteogenic Differentiation Medium | Induces osteogenesis in hBM-MSCs in vitro. | Typically contains Dexamethasone, Ascorbic Acid, and β-Glycerophosphate. |
| Alkaline Phosphatase (ALP) Assay Kit | Quantifies early osteogenic differentiation (Day 7-10). | Measures hydrolysis of pNPP to colored p-nitrophenol. Normalize to total protein. |
| Alizarin Red S (ARS) Solution | Stains calcium deposits for late-stage mineralization (Day 21-28). | Quantification possible via dye elution and spectrophotometry. |
| RiboNucleic Acid (RNA) Isolation Kit | Extracts high-quality RNA from cells on scaffolds for qPCR. | Must include steps to disrupt cell-scaffold matrix. |
Within the research thesis "Comparative Analysis of 3D-Printed Titanium Alloy vs. Poly(ε-caprolactone) (PCL) Scaffolds for Critical-Sized Bone Defect Regeneration," this document addresses a core experimental challenge. While titanium alloys offer superior mechanical strength and osteointegration, PCL provides a biodegradable, accessible alternative suitable for drug-eluting scaffolds. The primary limitations impeding PCL's translation are its inadequate mechanical strength for load-bearing sites and intrinsic hydrophobicity, which hinders cell adhesion and protein adsorption. These application notes detail protocols to engineer PCL-based composite scaffolds that mitigate these weaknesses.
Application Notes: Strategies and Quantitative Data
2.1 Strategies for Mechanical Reinforcement
| Strategy | Additive/Technique | Key Outcome (Quantitative) | Reference Year |
|---|---|---|---|
| Polymer Blending | Poly(L-lactic acid) (PLLA) | Tensile modulus increased from ~250 MPa (pure PCL) to ~680 MPa (70/30 PCL/PLLA). | 2023 |
| Ceramic Composite | Nano-hydroxyapatite (nHA) | Compressive strength increased by ~150% (from 8 MPa to ~20 MPa) with 20% nHA loading. | 2024 |
| Structural Design | Triply Periodic Minimal Surface (TPMS) Gyroid | Yield strength of designed PCL/nHA gyroid scaffold reached ~32 MPa, mimicking trabecular bone. | 2024 |
| Nanofiber Reinforcement | Cellulose Nanocrystals (CNC) | Addition of 3 wt% CNC increased Young's modulus by 95% and tensile strength by 110%. | 2023 |
2.2 Strategies for Hydrophilicity Enhancement
| Strategy | Method | Key Outcome (Quantitative) | Reference Year |
|---|---|---|---|
| Surface Plasma Treatment | O₂/Ar Plasma, 100W, 5 min | Water contact angle reduced from 108° to 35°, effect sustained for 7 days post-treatment. | 2023 |
| Wet Chemical Etching | 5M NaOH, 60°C, 30 min | Contact angle reduced to 55°, with significant surface pitting increasing protein adsorption by 300%. | 2024 |
| Bioactive Coating | Polydopamine (PDA) Coating | Contact angle reduced to ~20°, followed by immobilization of collagen or BMP-2 peptide. | 2023 |
| Copolymer Integration | PCL-PEG-PCL Triblock Copolymer | Bulk hydrophilicity improved; water absorption increased from 5% (PCL) to >45%. | 2024 |
Experimental Protocols
Protocol 3.1: Fabrication of PCL/nHA Composite Filament for FDM Objective: Produce a homogeneous composite filament with 20% nHA for enhanced osteoconductivity and strength.
- Materials: PCL pellets (Mn 80,000), nano-hydroxyapatite powder (<200 nm), dichloromethane (DCM).
- Procedure: a. Dissolve 80g PCL pellets in 500mL DCM via magnetic stirring (12h). b. Disperse 20g nHA in 100mL DCM via probe sonication (30 min, pulse mode). c. Combine solutions and stir for 6h. Pour into a PTFE tray and let DCM evaporate (48h). d. Vacuum-dry the composite cake at 40°C for 24h to remove residual solvent. e. Feed dried composite into a twin-screw extruder (temperature profile: 80-100-110°C) to produce 1.75 mm filament. f. Spool filament and store in a desiccator.
Protocol 3.2: Alkaline Hydrolysis for Permanent Surface Hydrophilization Objective: Create a micro-rough, hydrophilic PCL surface to enhance initial cell attachment.
- Materials: 3D-printed PCL scaffold, Sodium hydroxide (NaOH) pellets, deionized water, phosphate-buffered saline (PBS).
- Procedure: a. Prepare a 5M NaOH solution in deionized water. b. Immerse PCL scaffolds in the solution, ensuring full submersion. c. Incubate at 60°C for 30 minutes in a water bath. d. Carefully remove scaffolds and rinse 5x in fresh PBS to neutralize pH. e. Soak scaffolds in DI water for 2h, changing water every 30 min. f. Lyophilize for 24h and characterize via water contact angle and SEM.
Protocol 3.3: Polydopamine Coating for Biofunctionalization Objective: Apply a universal, adhesive coating to anchor bioactive molecules.
- Materials: 3D-printed PCL scaffold, Dopamine hydrochloride, Tris buffer (10mM, pH 8.5).
- Procedure: a. Prepare a 2 mg/mL dopamine solution in Tris buffer. Filter (0.22 µm). b. Place scaffolds in the solution with gentle agitation (e.g., rocker). c. React for 24h at room temperature. Observe solution darkening. d. Retrieve scaffolds and rinse extensively with DI water until runoff is clear. e. Dry at 37°C for 12h. Coated scaffolds can be used directly or further immersed in a solution of the desired peptide (e.g., RGD) for 12h to enable covalent grafting.
Diagrams and Visualizations
Title: Research Strategy for Overcoming PCL Limitations
Title: PCL/nHA Composite Filament Fabrication Workflow
Title: Surface Modification via Polydopamine Coating
The Scientist's Toolkit
| Research Reagent/Material | Function in PCL Scaffold Enhancement |
|---|---|
| Nano-Hydroxyapatite (nHA) | Bioactive ceramic filler; improves compressive strength, modulus, and osteoconductivity. |
| Poly(L-lactic acid) (PLLA) | Blending polymer; increases tensile modulus and degradation rate of PCL composite. |
| Dopamine Hydrochloride | Precursor for polydopamine (PDA) coating; enables surface hydrophilization and secondary biomolecule immobilization. |
| Tris Buffer (pH 8.5) | Alkaline buffer for PDA polymerization; provides optimal conditions for oxidative self-assembly. |
| Sodium Hydroxide (NaOH) | Strong base for alkaline hydrolysis; etches PCL surface to create micro-roughness and carboxyl groups. |
| Cellulose Nanocrystals (CNC) | Bio-based nanofiller; significantly enhances tensile properties and can modify degradation. |
| O₂/Ar Gas Mix | Feedstock gas for plasma treatment; introduces polar oxygen-containing groups on PCL surface. |
Within the paradigm of developing optimal bone scaffolds, a critical comparison exists between 3D-printed titanium alloys and biodegradable polymers like polycaprolactone (PCL). Titanium offers superior mechanical strength but is permanent, can cause stress shielding, and requires revision surgery in growing patients. PCL, a biocompatible and FDA-approved polyester, provides a tunable temporary scaffold that promotes bone regeneration via gradual resorption. The central challenge for PCL is predicting and controlling its degradation rate to match the bone healing timeline (typically 3-12 months). This application note details strategies to tailor PCL's composition and architecture to achieve predictable resorption profiles, enabling its reliable use as an alternative to permanent metallic implants in non-load-bearing applications.
Key Factors Influencing PCL Degradation Rate
PCL degrades primarily via bulk hydrolysis of its ester linkages, a process influenced by intrinsic material properties and extrinsic environmental conditions.
Table 1: Factors Governing PCL Degradation Kinetics
| Factor | Mechanism of Influence | Typical Range/Options | Impact on Degradation Rate |
|---|---|---|---|
| Molecular Weight (Mw) | Chain length determines number of hydrolyzable bonds. | Low Mw: 10-30 kDa; High Mw: 50-100 kDa | Lower Mw = Faster degradation |
| Crystallinity | Dense crystalline regions are less permeable to water than amorphous regions. | 40-70% | Higher crystallinity = Slower degradation |
| Co-polymer Composition | Introduction of faster-degrading monomers (e.g., lactide, glycolide) alters backbone hydrophilicity and stability. | PCL-PLA, PCL-PGA, PCL-PLGA | More hydrophilic comonomer = Faster degradation |
| Scaffold Architecture (Porosity & Pore Size) | Higher surface area increases water penetration and mass loss. | Porosity: 60-80%; Pore Size: 200-500 μm | Higher porosity/smaller pores = Faster degradation |
| 3D Printing Parameters | Influences crystallinity, porosity, and mechanical strain. | Nozzle Temp., Print Speed, Layer Height | Higher temp/speed can increase crystallinity, slowing degradation. |
| In Vivo Environment | Enzymatic activity (e.g., lipases) and local pH accelerate hydrolysis. | Physiological (pH 7.4) vs. Inflammatory (pH <7) | Enzymatic presence & lower pH = Faster degradation |
Experimental Protocols for Tailoring and Assessing Degradation
Protocol 2.1: Synthesis of PCL-based Copolymers for Tunable Hydrolysis
Objective: To synthesize PCL-PLA triblock copolymers with varying block lengths to modulate degradation. Materials: ε-Caprolactone, L-Lactide, Stannous octoate (catalyst), Toluene (anhydrous), Methanol. Procedure:
- Purification: Dry ε-caprolactone and L-lactide over calcium hydride overnight and distill under vacuum.
- Reaction Setup: In a flame-dried Schlenk flask under argon, add predetermined molar ratios of ε-caprolactone and L-lactide (e.g., 80:20, 50:50 PCL:PLA).
- Polymerization: Add stannous octoate catalyst (0.1 wt% of monomers). Seal and immerse in an oil bath at 130°C for 24 hours with magnetic stirring.
- Termination & Precipitation: Cool the flask, dissolve the viscous product in minimal toluene, and precipitate into a 10-fold excess of cold methanol.
- Recovery: Filter the polymer, wash with fresh methanol, and dry under vacuum at 40°C to constant weight. Characterize by GPC (Mw) and NMR (composition).
Protocol 2.2: Fabrication of Architecture-Controlled Scaffolds via Fused Deposition Modeling (FDM)
Objective: To 3D-print PCL scaffolds with designed pore architectures to study structure-degradation relationships. Materials: PCL filament (1.75 mm diameter), FDM 3D printer (e.g., desktop model), Slicing software (e.g., Cura). Procedure:
- Design: Create 3D models (e.g., 10x10x3 mm cubes) with controlled pore geometries (e.g., 0/90° vs. 0/60/120° laydown patterns) using CAD software.
- Slicing: Import model into slicing software. Set parameters: Nozzle Diameter: 0.4 mm, Layer Height: 0.2 mm, Printing Temperature: 90-100°C, Bed Temperature: 50°C, Print Speed: 20 mm/s.
- Architecture Variation: Generate two distinct G-code files:
- Architecture A: Rectilinear infill, 60% density, 400 μm effective pore size.
- Architecture B: Gyroid infill, 80% density, 300 μm effective pore size.
- Printing: Load PCL filament, preheat printer, and execute prints. Store scaffolds in a desiccator.
Protocol 2.3:In VitroDegradation Study (ASTM F1635 Standard)
Objective: To quantitatively monitor mass loss, molecular weight change, and mechanical property decay over time. Materials: PBS (pH 7.4), Sodium azide (0.02% w/v), Thermostatic shaking water bath, Vacuum oven, GPC, Micro-CT. Procedure:
- Baseline Characterization: Weigh (W₀), scan via micro-CT for initial porosity, and test a subset for initial mechanical properties (compressive modulus).
- Immersion: Place individual scaffolds (n=5 per time point) in 20 mL of PBS with sodium azide (to prevent microbial growth). Incubate at 37°C in a shaking water bath (60 rpm).
- Sampling: Retrieve samples at predetermined intervals (e.g., 1, 3, 6, 9, 12 months).
- Analysis:
- Mass Loss: Rinse samples with DI water, dry to constant weight (Wₐ). Calculate mass remaining: (Wₐ/W₀)*100%.
- Molecular Weight: Dissolve a portion of dried sample in THF, analyze via GPC to track Mw reduction.
- Morphology: Image via SEM to observe surface erosion, pore coalescence.
- Mechanics: Perform compressive testing on hydrated samples.
Table 2: Typical Degradation Data for PCL Variants (12-month in vitro)
| PCL Formulation | Initial Mw (kDa) | Porosity (%) | Mass Remaining (%) | Mw Retention (%) | Time to 50% Mass Loss (Est.) |
|---|---|---|---|---|---|
| High Mw PCL Homopolymer | 80 | 70 | ~95 | ~65 | >36 months |
| Low Mw PCL Homopolymer | 15 | 70 | ~85 | ~40 | ~24 months |
| PCL-PLA (70:30) Copolymer | 50 | 70 | ~75 | ~30 | ~18 months |
| High Mw PCL (Architecture A) | 80 | 60 | ~97 | ~70 | >36 months |
| High Mw PCL (Architecture B) | 80 | 80 | ~90 | ~60 | ~30 months |
Visualization of Key Concepts
Diagram 1: Strategy for PCL Resorption Control (83 chars)
Diagram 2: PCL Hydrolysis & Resorption Pathway (84 chars)
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagent Solutions for PCL Degradation Studies
| Item | Function/Brief Explanation | Example Supplier/Catalog |
|---|---|---|
| Polycaprolactone (PCL) Pellets/Filament | Raw polymer material. Varying Mw grades (e.g., 14kDa, 45kDa, 80kDa) allow baseline rate studies. | Sigma-Aldrich, Corbion Purac |
| L-Lactide & Glycolide Monomers | For synthesizing PCL copolymers (e.g., PCL-PLA) to accelerate degradation via more hydrolytically active segments. | Sigma-Aldrich, Polysciences |
| Stannous Octoate (Tin(II) 2-ethylhexanoate) | Standard catalyst for ring-opening polymerization (ROP) of lactones and lactides. Must be handled under inert atmosphere. | Sigma-Aldrich |
| Phosphate Buffered Saline (PBS), pH 7.4 | Standard medium for in vitro hydrolysis studies, simulating physiological ionic strength and pH. | Thermo Fisher, Gibco |
| Lipase from Pseudomonas cepacia | Enzyme used to model enzymatic degradation in vitro, as PCL is susceptible to enzymatic hydrolysis by certain lipases. | Sigma-Aldrich |
| Size Exclusion/GPC Columns (e.g., PLgel Mixed-C) | For measuring changes in molecular weight (Mw, Mn) and polydispersity (Đ) over degradation time. | Agilent Technologies |
| AlamarBlue or PrestoBlue Cell Viability Reagent | For assessing cytocompatibility of degradation products via metabolic activity assays on osteoblast cells (e.g., MC3T3-E1). | Thermo Fisher |
| Simulated Body Fluid (SBF) | Ion concentration similar to human blood plasma. Used to assess apatite formation (bioactivity) on degrading scaffolds. | Prepared per Kokubo protocol or commercial kits. |
Within the thesis research comparing laser powder bed fusion (LPBF) of Ti-6Al-4V and fused deposition modeling (FDM) of polycaprolactone (PCL) for bone scaffolds, controlling manufacturing defects is paramount to achieving scaffolds with predictable mechanical properties, degradation profiles, and biological performance. This Application Note details critical protocols for characterizing and mitigating three universal defect classes: porosity, residual stress, and dimensional inaccuracy.
Table 1: Defect Characteristics, Implications, and Control Targets for Ti-6Al-4V vs. PCL Scaffolds
| Defect Type | Ti-6Al-4V (LPBF) Typical Range & Target | PCL (FDM) Typical Range & Target | Primary Impact on Scaffold Function |
|---|---|---|---|
| Porosity (Unintended) | Range: 0.1-2.0 vol% Target: <0.5% (dense struts) | Range: 1-5 vol% (inter-filament gaps) Target: <1% (fully dense struts) | Mechanical fatigue strength; barrier to cell migration if pore size <~10µm. |
| Designed Macro-Porosity | Pore Size: 300-800 µm Porosity: 50-80% Accuracy: ± 50 µm | Pore Size: 300-800 µm Porosity: 50-80% Accuracy: ± 100 µm | Osseointegration, vascularization, permeability. |
| Residual Stress | Range: 200-1000 MPa (tensile, near surface) Target: <200 MPa (post-process) | Range: 5-20 MPa (shrinkage-induced) Target: Minimal via annealing | Ti: Part distortion, stress-corrosion cracking. PCL: Warpage, layer delamination. |
| Dimensional Accuracy | Linear Error: ± 20-100 µm Strut Diameter Error: ± 25-50 µm | Linear Error: ± 50-200 µm Strut Diameter Error: ± 50-150 µm | Fit with defect site; designed permeability/stiffness. |
| Surface Roughness (Ra) | As-built: 15-30 µm Target: 5-20 µm (for bioactivity) | As-built: 5-15 µm Target: 5-20 µm | Influences initial cell adhesion and osteogenic differentiation. |
Table 2: Process Parameters for Defect Mitigation
| Parameter | Ti-6Al-4V LPBF Protocol | PCL FDM Protocol | Rationale |
|---|---|---|---|
| Key Energy Density | 60-90 J/mm³ (e.g., P=200W, v=800mm/s, h=80µm, t=30µm) | N/A | Optimizes melt pool stability, minimizes keyhole & lack-of-fusion pores. |
| Nozzice/Bed Temp | Pre-heated build plate (~200°C) | Nozzle: 90-110°C Bed: 45-60°C | Reduces thermal gradient (Ti) and improves layer adhesion (PCL). |
| Scan Strategy | Stripes or islands with 67° rotation between layers | Raster Angle: ±45° alternation | Manages heat distribution and residual stress in Ti; improves interlayer strength in PCL. |
| Inert Atmosphere | Argon, <100 ppm O₂ | Not Required | Prevents oxidation-induced defects in Ti alloy. |
| Post-Processing | Stress Relief: 650-800°C, 2-4h, Argon HIP: 920°C, 100 MPa, 2h | Annealing: 55-60°C, 1-2h, in fixture | Relieves residual stresses (Ti), closes internal pores (Ti via HIP), reduces PCL warpage. |
Experimental Protocols for Defect Characterization
Protocol 3.1: Quantification of Porosity & Pore Morphology
Objective: To accurately measure and classify the porosity (both designed and unintended) in Ti-6Al-4V and PCL scaffolds. Materials: Micro-computed tomography (µCT) system, image analysis software (e.g., ImageJ, Avizo), metallographic/polishing setup for Ti, critical point dryer for PCL. Procedure:
- Sample Preparation: Ti-6Al-4V: Cut representative section, mount in resin, grind, and polish to a 1µm finish. PCL: Dehydrate scaffold in graded ethanol series and critical point dry to preserve architecture.
- µCT Scanning: Scan both sample types at a resolution of at least 5µm/voxel. Use a beam energy of 70 kV for PCL and 100 kV for Ti. Apply a 0.5 mm Al filter for Ti to reduce beam hardening.
- Image Reconstruction & Segmentation: Reconstruct 3D volume. Apply a global thresholding algorithm (e.g., Otsu's method) to segment solid material from pores.
- Analysis:
- Calculate total porosity (%) = (Total pore volume / Total scaffold volume) * 100.
- Use connected component analysis to separate designed macro-pores (>100µm) from unintended micro-pores (<50µm).
- For Ti, report pore sphericity; spherical pores suggest gas entrapment, irregular shapes indicate lack-of-fusion.
Protocol 3.2: Measurement of Residual Stress via the Contour Method
Objective: To map 2D residual stress fields in a cross-section of a Ti-6Al-4V scaffold. Materials: Wire electrical discharge machining (EDM), coordinate measuring machine (CMM) or high-resolution laser scanner, finite element analysis (FEA) software, stress-relieved reference sample. Procedure:
- Specimen Cutting: Carefully cut the scaffold or a representative bulk sample using wire EDM. The cut must be slow and cool to avoid introducing new stresses.
- Surface Profiling: Measure the topography of the cut surface using a CMM or laser scanner with sub-micron resolution. This measures the 2D displacement field caused by stress relaxation.
- Inverse FEA: Input the measured displacement field into an elastic FEA model of the specimen. The software inversely calculates the original residual stress field that, when released, would produce the measured displacements.
- Validation: Compare results with X-ray diffraction (XRD) stress measurements at specific surface points.
Protocol 3.3: Protocol for Assessing Dimensional Accuracy
Objective: To quantify deviations between as-designed (CAD) and as-built scaffold geometries. Materials: High-resolution 3D scanner (e.g., structured light, laser), digital calipers, metrology software (e.g., Geomagic Control). Procedure:
- Reference Model: Export the original scaffold CAD file (STL format).
- 3D Scanning: Scan the manufactured scaffold from multiple angles. For Ti, apply a thin matte white coating if necessary. For translucent PCL, apply a developer spray.
- Alignment & Comparison: Align the scan data (point cloud) to the CAD model using a best-fit algorithm. Perform a 3D deviation analysis.
- Quantification: Report:
- Global Accuracy: Root mean square (RMS) error of all points.
- Critical Feature Accuracy: Average error and standard deviation for strut diameters, pore diameters, and overall scaffold dimensions.
- Form Error: Visual heat map of deviations.
Diagrams for Defect Formation and Control Workflows
Diagram Title: Porosity Defect Cause & Control Flow
Diagram Title: Residual Stress Path & Mitigation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Defect Analysis in Scaffold Research
| Item | Function & Specification | Application Note |
|---|---|---|
| Standardized Ti-6Al-4V Powder | Spherical gas-atomized powder, 15-45 µm diameter, low oxygen content (<0.1 wt%). | Ensures consistent flowability and melt pool dynamics in LPBF, minimizing porosity sources. |
| Medical Grade PCL Filament | High purity, consistent diameter (e.g., 1.75 ± 0.05 mm), defined molecular weight (Mw ~80 kDa). | Reduces filament diameter variation-induced gaps and ensures predictable viscosity & crystallization stress. |
| µCT Calibration Phantom | Phantom with known density and pore size standards (e.g., 100-800 µm rods). | Essential for quantitative, repeatable porosity and pore size distribution measurements. |
| Conductive Mounting Resin | Epoxy resin filled with copper or carbon particles. | For metallographic preparation of Ti scaffolds, allows for subsequent SEM/EDX analysis without charging. |
| Critical Point Dryer (CPD) | System using CO₂ as transition fluid. | Prevents collapse of PCL scaffold's porous microstructure during dehydration prior to high-resolution imaging. |
| Structured Light 3D Scanner | Scanner with <10 µm resolution and volumetric accuracy. | For non-contact, high-resolution 3D digitization of complex scaffold geometry for accuracy assessment. |
| Stress-Relief Annealing Furnace | Tube furnace capable of 1000°C with argon gas purging. | For controlled stress relief of Ti-6Al-4V scaffolds per Protocol 3.2, preventing oxidation. |
| Image Analysis Software (Fiji/ImageJ) | Open-source software with BoneJ plugin suite. | For segmentation and quantitative analysis of µCT data (porosity, strut thickness, connectivity). |
Head-to-Head Analysis: Validating Mechanical, Biological, and Clinical Performance of Titanium vs. PCL Scaffolds
This document provides Application Notes and Protocols for the mechanical benchmarking of 3D-printed bone scaffolds. The work is framed within a broader thesis comparing Titanium alloys (e.g., Ti-6Al-4V) with the bioresorbable polymer Polycaprolactone (PCL) for bone regeneration applications. Key mechanical parameters—Compressive Strength, Elastic Modulus, Fatigue Resistance, and Anisotropy—are critical for ensuring scaffolds mimic native bone, provide structural support, and influence cellular responses. Standardized testing is essential for meaningful comparison between these fundamentally different material systems.
Table 1: Typical Mechanical Properties of 3D-Printed Scaffold Materials vs. Bone
| Material / Tissue | Fabrication Method | Compressive Strength (MPa) | Elastic Modulus (GPa) | Fatigue Limit (Cycles, MPa) | Key Notes |
|---|---|---|---|---|---|
| Cortical Bone | N/A | 130-180 | 15-25 | >10⁷ @ 70 MPa | Anisotropic, direction-dependent. |
| Cancellous Bone | N/A | 2-12 | 0.05-0.5 | N/A | Highly porous. |
| Ti-6Al-4V (SLM/DMLS) | Powder Bed Fusion | 900-1200 | 110-120 | 10⁷ @ ~500 MPa (R=-1) | High strength, high stiffness, low anisotropy with optimized parameters. |
| PCL (FDM) | Fused Deposition Modeling | 2-15 | 0.2-0.5 | 10⁴-10⁵ @ 2-4 MPa | Highly process-dependent, viscoelastic, significant anisotropy. |
| PCL (SLS) | Selective Laser Sintering | 10-25 | 0.4-0.8 | 10⁵-10⁶ @ 5-8 MPa | Improved strength over FDM, reduced anisotropy. |
Table 2: Key Sources of Anisotropy in Additively Manufactured Scaffolds
| Source | Effect on Ti-6Al-4V | Effect on PCL |
|---|---|---|
| Build Direction | Moderate: Columnar grain growth can cause ~10-15% strength variance. | High: Layer adhesion is critical; Z-direction strength can be 50% lower. |
| Scan Strategy | Low-Moderate: Affects residual stress and texture. | Not Applicable (for FDM). |
| Road/Raster Angle | Not Applicable (for PBF). | High: Off-axis loading relative to raster direction reduces strength. |
| Porosity/Architecture | High: Dominates effective properties. Can be designed isotropically (e.g., cubic) or anisotropically (e.g., orthogonal). | High: Same as metal, but layer-driven defects amplify anisotropy. |
Experimental Protocols
Protocol 1: Quasi-Static Compression Test for Scaffolds
Objective: To determine the compressive yield strength, ultimate compressive strength, and apparent elastic modulus of porous scaffold structures. Materials: Universal testing machine (e.g., Instron, Zwick), 3D-printed scaffold samples (cube or cylinder, minimum 5 replicates), calipers. Procedure:
- Sample Preparation: Fabricate scaffolds with defined porosity (e.g., 70%) and pore size (e.g., 500 µm). Measure exact sample dimensions (height, cross-sectional area).
- Mounting: Place the sample centrally on the lower platen of the testing machine. Ensure the loading axis aligns with the intended scaffold orientation (e.g., build direction).
- Test Parameters:
- Pre-load: 1 N.
- Loading rate: 0.5 mm/min (strain rate ~0.005/min).
- Stop criterion: 80% strain or catastrophic failure.
- Data Analysis:
- Elastic Modulus: Calculate the slope of the linear elastic region (typically 20-70% of peak stress) on the stress-strain curve.
- Yield Strength: Use the 0.2% offset method.
- Ultimate Compressive Strength: Identify the maximum stress attained.
Protocol 2: Cyclic Compression Fatigue Test
Objective: To assess the resistance to cyclic loading and determine an S-N (Wöhler) curve. Materials: Servohydraulic testing machine with cyclic capability, environmental chamber (optional, for 37°C/PBS), scaffold samples. Procedure:
- Sample Preparation: As per Protocol 1.
- Test Setup: Use a sinusoidal waveform. Select an R-ratio (σmin/σmax) of 0.1 for tension-compression or use compression-compression (R=10) to prevent buckling.
- Test Execution:
- Test a series of samples at different stress amplitudes (e.g., 50%, 60%, 70% of UCS).
- Frequency: 2-5 Hz for PCL (to minimize hysteresis heating); up to 10 Hz for Ti alloys.
- Run until sample failure (defined by a 20% drop in peak load or visible fracture) or until a run-out limit (e.g., 5 million cycles).
- Data Analysis: Plot stress amplitude (S) vs. cycles to failure (N) on a log scale to generate the S-N curve. Report the endurance limit, if identified.
Protocol 3: Assessment of Elastic Anisotropy
Objective: To quantify directional dependence of the elastic modulus. Materials: Universal testing machine or nanoindentation system, scaffolds designed with identical unit cells. Procedure (Macro-scale):
- Design: Fabricate scaffold cubes with a defined, symmetric lattice (e.g., cubic or diamond).
- Orientation: Test separate sample sets with primary loading axis aligned along the X (print plane), Y (print plane), and Z (build direction) axes.
- Testing: Perform compression tests as in Protocol 1 for each orientation (n≥3 per orientation).
- Analysis: Calculate the Elastic Modulus (E) for each direction. Anisotropy Index (AI) can be calculated as: AI = (Emax - Emin) / E_average. An AI of <0.1 indicates near isotropy.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Equipment for Mechanical Benchmarking
| Item | Function & Relevance |
|---|---|
| Universal Testing Machine | Applies controlled tensile/compressive forces; essential for generating stress-strain data. |
| Servohydraulic Fatigue Tester | Applies cyclic loads; required for fatigue life (S-N) determination. |
| Environmental Chamber | Maintains 37°C in phosphate-buffered saline (PBS); simulates physiological conditions for polymer testing (PCL is viscoelastic). |
| 3D Digital Image Correlation (DIC) System | Non-contact optical method to measure full-field strain, crucial for identifying local deformations and anisotropy. |
| High-Resolution Micro-CT Scanner | Quantifies as-built porosity, pore size distribution, and detects internal defects critical for fatigue initiation. |
| Nanoindenter | Measures local modulus and hardness of individual struts, especially important for assessing fusion quality in PCL. |
| Phosphate-Buffered Saline (PBS), pH 7.4 | Standard immersion medium for simulating in vitro physiological conditions during testing. |
| ISO 13314:2011 / ASTM F4515 | Standard for compression testing of porous metals; guides sample geometry and test method. |
| ASTM F2902 | Guide for assessing degradation of absorbable polymeric scaffolds, relevant for PCL in fluid. |
Diagrams
Diagram 1: Workflow for Scaffold Mechanical Benchmarking
Diagram 2: Key Factors Influencing Mechanical Performance
Within the broader thesis comparing 3D-printed titanium alloy (Ti-6Al-4V) versus polycaprolactone (PCL) scaffolds for bone regeneration, assessing biocompatibility is paramount. This document provides detailed application notes and protocols for evaluating three core components: Osteointegration (direct structural and functional connection between living bone and scaffold), Osteoconduction (scaffold's ability to support bone growth along its surface), and the Inflammatory Response (immune reaction post-implantation). The inherent properties of titanium (bioinert, high strength) and PCL (biodegradable, tunable) demand distinct yet parallel evaluation frameworks.
Table 1: Key Material Properties Influencing Biocompatibility
| Property | 3D-Printed Ti-6Al-4V | 3D-Printed PCL | Ideal Bone Scaffold | Test Standard |
|---|---|---|---|---|
| Elastic Modulus (GPa) | 110-115 | 0.4-0.8 | 10-30 (Cortical Bone) | ASTM E111 |
| Surface Roughness (Ra, μm) | 10-30 (after etching) | 5-15 (as printed) | 1-10 (for cell adhesion) | ISO 4287 |
| Porosity (%) | 50-70 | 60-80 | 50-90 | ASTM D792 |
| Degradation Rate | Negligible (corrodes slowly) | 10-30% mass loss/year in vivo | Matches bone growth rate | ISO 10993-13 |
| In Vitro Cell Viability (%) | >90% (hMSCs, day 7) | 85-95% (hMSCs, day 7) | >70% | ISO 10993-5 |
Table 2: Typical In Vivo Outcomes (Rodent Femur Model, 12 Weeks)
| Metric | Ti-6Al-4V Scaffold | PCL Scaffold | Measurement Method |
|---|---|---|---|
| Bone-Implant Contact (BIC) % | 60-75% | 40-55% | Histomorphometry |
| New Bone Area (%) | 35-50% | 25-40% | Micro-CT / Histology |
| Peak Inflammatory Response | Week 2 (neutrophils/macrophages) | Week 1-2 (higher macrophage density) | Immunohistochemistry (CD68+) |
| Trabecular Number (1/mm) | 3.5-4.2 | 2.8-3.5 | Micro-CT analysis |
| Push-out Strength (MPa) | 15-25 | 5-12 | Biomechanical testing |
Experimental Protocols
Protocol 3.1:In VitroOsteoconduction & Osteogenic Differentiation
Aim: To assess the scaffold's ability to support mesenchymal stem cell (MSC) adhesion, proliferation, and osteogenic differentiation. Materials: Sterilized Ti-6Al-4V and PCL scaffolds (Ø5mm x 2mm), human MSCs (hMSCs), osteogenic media (OM: basal media + 10mM β-glycerophosphate, 50µg/mL ascorbic acid, 100nM dexamethasone), control media (basal media), alamarBlue assay, OsteoImage mineralization stain, qPCR reagents. Procedure:
- Seed hMSCs onto scaffolds at 50,000 cells/scaffold in 96-well plates. Allow 2h for adhesion, then add media.
- Proliferation: At days 1, 3, 7, incubate with 10% alamarBlue for 4h. Measure fluorescence (Ex560/Em590). Use scaffolds without cells as blank.
- Differentiation: Culture sets of scaffolds in OM or control media for 14 and 21 days. Change media twice weekly.
- Mineralization Assay: At day 21, wash scaffolds, perform OsteoImage staining per manufacturer's protocol. Quantify fluorescence (Ex492/Em520) or visualize via confocal microscopy.
- Gene Expression: At day 14, extract RNA (TRIzol). Perform qPCR for RUNX2, ALPL, SPP1 (osteopontin), and BGLAP (osteocalcin). Normalize to GAPDH. Use 2^(-ΔΔCt) method.
Protocol 3.2:In VivoOsteointegration & Inflammatory Response (Rodent Model)
Aim: To evaluate bone bonding and the temporal immune response to implanted scaffolds. Materials: 8-week-old male Sprague-Dawley rats, sterilized scaffolds (Ø1.5mm x 2mm), surgical tools, isoflurane anesthesia, analgesia, embedding resin, micro-CT system, histology supplies, antibodies for IHC (CD68 for macrophages, TRAP for osteoclasts, Osteocalcin for osteoblasts). Procedure:
- Surgery: Create bilateral critical-size defects in femoral condyles. Press-fit one scaffold type per defect (randomized). Suture muscle and skin. Administer post-op analgesia.
- Time Points: Euthanize groups at 2 days, 1, 2, 4, and 12 weeks post-op (n=6/time point/group).
- Micro-CT Analysis: Scan excised femora at 10µm resolution. Reconstruct and analyze: Bone Volume/Tissue Volume (BV/TV) within 500µm of scaffold, Trabecular Thickness (Tb.Th), and Bone-Implant Contact (BIC) using thresholding software (e.g., CTAn).
- Histology: Dehydrate, embed in methyl methacrylate (for Ti) or paraffin (for PCL). Section (5µm). Stain with H&E, Masson's Trichrome.
- Histomorphometry: Calculate BIC (%) and new bone area (%) from stained sections using software (e.g., ImageJ).
- Inflammatory Response: Perform IHC on early time-point (2d, 1w, 2w) sections. Quantify CD68+ and TRAP+ cells per mm² in peri-implant region.
Protocol 3.3:In VitroMacrophage Polarization Assay
Aim: To characterize the acute inflammatory response by assessing macrophage phenotype (M1 pro-inflammatory vs. M2 pro-healing) on material surfaces. Materials: RAW 264.7 macrophage cell line or primary bone marrow-derived macrophages (BMDMs), serum-free media, LPS (for M1 polarization), IL-4 (for M2 polarization), RNA/DNA extraction kits, ELISA kits for TNF-α (M1) and IL-10 (M2). Procedure:
- Seed macrophages onto material discs (Ti, PCL, control TCP) at 100,000 cells/cm² in serum-free media.
- After 24h, stimulate with LPS (100ng/mL) + IFN-γ (20ng/mL) for M1, or IL-4 (20ng/mL) for M2. Use unstimulated cells as M0 control.
- Gene Expression: At 24h post-stimulation, extract RNA. Analyze M1 markers (iNOS, CD86, TNF-α) and M2 markers (Arg1, CD206, IL-10) via qPCR.
- Protein Secretion: At 48h, collect supernatant. Quantify TNF-α and IL-10 via ELISA.
- Morphology: Image cells via SEM or fluorescence (actin staining) to observe elongated (M2) vs. spread (M1) morphology.
Diagrams
Temporal Phases of Scaffold Biocompatibility
Macrophage Polarization Pathways on Ti vs. PCL
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents & Materials for Biocompatibility Testing
| Item | Function & Rationale | Example Product/Catalog |
|---|---|---|
| Human Mesenchymal Stem Cells (hMSCs) | Primary cells for in vitro osteogenic differentiation assays; gold standard for bone regeneration studies. | Lonza PT-2501; ATCC PCS-500-012 |
| OsteoImage Mineralization Assay | Fluorescently labels hydroxyapatite deposits; quantifies in vitro osteoconduction/ mineralization. | Lonza PA-1503 |
| alamarBlue Cell Viability Reagent | Resazurin-based assay for non-destructive, longitudinal tracking of cell proliferation on 3D scaffolds. | Thermo Fisher Scientific DAL1025 |
| CD68 Antibody (IHC) | Pan-macrophage marker for identifying and quantifying the inflammatory infiltrate in vivo. | Abcam ab955 |
| TRAP Stain Kit | Detects tartrate-resistant acid phosphatase activity, identifying osteoclasts on bone-scaffold interface. | Sigma-Aldrich 387A-1KT |
| Rat TNF-α & IL-10 ELISA Kits | Quantify key pro-inflammatory (M1) and anti-inflammatory (M2) cytokines in serum or homogenates. | R&D Systems DY510, DY522 |
| Methyl Methacrylate (MMA) Embedding Kit | For hard tissue (bone+Ti) histology; preserves bone-scaffold interface for sectioning. | Sigma-Aldrich GER1120-1EA |
| Micro-CT Calibration Phantom | Hydroxyapatite phantom with known density for accurate BMD and BV/TV quantification. | Scanco Medical HA Phantom |
| qPCR Primers for Osteogenesis | Validate osteogenic differentiation (RUNX2, ALPL, SPP1, BGLAP) and housekeeping genes. | Qiagen; Custom from IDT |
| LPS (E. coli O111:B4) & Recombinant IL-4 | Standard agonists for in vitro polarization of macrophages to M1 and M2 phenotypes, respectively. | Sigma-Aldrich L2630; PeproTech 200-04 |
Thesis Context: Within research comparing 3D-printed titanium alloys to polycaprolactone (PCL) scaffolds for bone regeneration, a pivotal challenge is the mismatch between the slow degradation of PCL and the rate of new bone formation. This document details protocols to characterize PCL scaffold degradation and concurrent bone ingrowth, enabling the optimization of scaffold architecture and composition to synchronize these processes.
Protocol:In VitroHydrolytic Degradation Kinetics of 3D-Printed PCL Scaffolds
Objective: To quantitatively monitor mass loss, molecular weight change, and morphological changes of PCL scaffolds under simulated physiological conditions.
Materials & Reagents:
- PCL Scaffolds: 3D-printed via fused deposition modeling (FDM) or melt electrospinning writing (MEW). Standard dimensions: 10mm diameter x 3mm height, 60% porosity, 400µm pore size.
- Phosphate-Buffered Saline (PBS): 0.1M, pH 7.4, sterile.
- Sodium Azide: 0.02% w/v in PBS to inhibit microbial growth.
- Analytical Balance: Precision ±0.01 mg.
- Gel Permeation Chromatography (GPC) system with refractive index detector.
- Scanning Electron Microscope (SEM).
- Incubator: Maintained at 37°C.
Procedure:
- Initial Characterization: Weigh each scaffold (W₀). Determine initial molecular weight (Mₙ₀, Mₚ₀) via GPC. Image pore morphology via SEM.
- Immersion: Immerse individual scaffolds in 20 mL of PBS with sodium azide in sealed containers (n=5 per time point).
- Incubation: Place containers in an incubator at 37°C.
- Sampling: Retrieve scaffolds at predetermined time points (e.g., 1, 3, 6, 9, 12 months).
- Analysis:
- Mass Loss: Rinse retrieved scaffolds with DI water, lyophilize for 48h, and weigh (Wₜ). Calculate mass remaining (%) = (Wₜ / W₀) * 100.
- Molecular Weight: Dissolve dried scaffolds in tetrahydrofuran (THF) and analyze via GPC to determine Mₙₜ and Mₚₜ.
- Morphology: Image via SEM to observe surface erosion, pore wall thinning, and pore size change.
Table 1: Representative In Vitro Degradation Data for PCL Scaffolds (60% Porosity)
| Time Point (Months) | Mass Remaining (%) | Number-Avg Mol. Wt. (Mₙ) Retention (%) | Pore Size Change (SEM Observation) |
|---|---|---|---|
| 0 | 100.0 ± 0.5 | 100.0 ± 2.0 | 400 ± 25 µm, smooth walls |
| 3 | 99.5 ± 0.8 | 92.5 ± 3.1 | No significant change |
| 6 | 98.8 ± 1.2 | 85.3 ± 4.5 | Slight surface pitting |
| 9 | 97.0 ± 1.5 | 75.8 ± 5.2 | Increased pitting, pore rounding |
| 12 | 94.5 ± 2.0 | 65.0 ± 6.0 | Visible pore wall thinning |
Protocol:In VivoEvaluation of Bone Ingrowth in a Critical-Size Calvarial Defect Model
Objective: To histomorphometrically quantify new bone formation within PCL scaffolds implanted in a bone defect, correlating it with scaffold degradation stage.
Materials & Reagents:
- Animal Model: Sprague-Dawley rats (or similar), 8-10 weeks old.
- PCL Scaffolds: Sterilized by ethylene oxide gas.
- Osteoconductive Control: 3D-printed titanium alloy scaffold (Ti-6Al-4V, equivalent geometry).
- Surgical Tools: Trephine bur (8mm diameter for rat calvaria).
- Fixative: 10% Neutral Buffered Formalin.
- Decalcification Solution: 10% EDTA, pH 7.4.
- Embedding Medium: Paraffin or polymethyl methacrylate (PMMA) for undecalcified sections.
- Stains: Hematoxylin & Eosin (H&E), Masson's Trichrome, von Kossa.
Procedure:
- Surgery: Create two bilateral 8mm full-thickness critical-size defects in the rat calvarium. Implant a PCL scaffold in one defect and a Ti-alloy scaffold in the contralateral defect (n=6-8 per group/time point).
- Post-Op & Euthanasia: Monitor animals. Euthanize at 4, 12, 26, and 52 weeks.
- Harvest & Process: Harvest calvaria blocks, fix in formalin for 48h.
- Option A (Decalcified): Decalcify in EDTA for 14 days, paraffin-embed, section at 5µm.
- Option B (Undecalcified): Dehydrate in graded ethanol, embed in PMMA, section using a diamond saw (~50µm).
- Staining & Imaging: Stain sections (H&E for general morphology, Masson's Trichrome for collagen/bone, von Kossa for mineralized tissue). Image using brightfield microscopy.
- Histomorphometry: Using image analysis software (e.g., ImageJ), quantify:
- Bone Ingrowth (%): (New bone area within scaffold pores / total pore area) x 100.
- Scaffold Remnant Area (%): (Remaining scaffold area / initial implant area) x 100.
- Bone-Scaffold Contact (%): (Length of new bone in direct contact with scaffold / total scaffold perimeter) x 100.
Table 2: Representative In Vivo Bone Ingrowth vs. Scaffold Degradation
| Time Point (Weeks) | PCL Scaffold Mass Remaining (%) * | Bone Ingrowth in PCL (%) | Bone Ingrowth in Ti-Alloy (%) |
|---|---|---|---|
| 4 | ~99 | 5.2 ± 1.8 | 12.5 ± 2.1* |
| 12 | ~98 | 15.8 ± 3.5 | 25.4 ± 3.0* |
| 26 | ~96 | 28.5 ± 4.2 | 32.1 ± 3.8 |
| 52 | ~90 | 35.0 ± 5.0 | 38.5 ± 4.5 |
Estimated from *in vitro correlation. *Ti-alloy shows faster early bone apposition due to superior osteoconductivity and stiffness.
The Scientist's Toolkit: Key Research Reagents & Materials
| Item Name | Function/Benefit in PCL/Bone Research |
|---|---|
| Medical-Grade PCL (Mn 80,000) | Standard polymer with consistent viscosity for 3D printing and predictable ~2-4 year full degradation timeline. |
| β-Tricalcium Phosphate (β-TCP) Powder | Osteoconductive ceramic additive. Blended with PCL to enhance bioactivity and buffer acidic degradation products. |
| Recombinant Human BMP-2 | Potent osteoinductive growth factor. Can be incorporated into PCL scaffolds to accelerate bone ingrowth, offsetting slow degradation. |
| Alizarin Red S Stain | Histochemical stain that binds calcium deposits. Used to identify and quantify early mineralized nodule formation in vitro. |
| Osteogenic Media (DMEM, FBS, Ascorbate, β-Glycerophosphate, Dexamethasone) | Standard cocktail to induce osteogenic differentiation of mesenchymal stem cells (MSCs) seeded on scaffolds in vitro. |
| Micro-CT Scanner (e.g., SkyScan) | Non-destructive 3D imaging to quantify bone volume/tissue volume (BV/TV) and scaffold degradation in vivo over time. |
| Polymerase Chain Reaction (PCR) Assays for Osteogenic Markers (RUNX2, OPN, OCN) | Molecular biology tool to quantify the expression of genes indicating osteoblast differentiation on degrading PCL scaffolds. |
Signaling Pathways in Osteogenesis on Degrading PCL
Title: Osteogenic Response to PCL Degradation Signals
Experimental Workflow for Critical Timeline Analysis
Title: Workflow to Correlate Degradation & Bone Ingrowth
Current Applications in Bone Scaffold Technology
Clinical Applications of 3D-Printed Implants
| Application Area | Material (Primary) | FDA Clearance/Approval Status (as of 2024) | Key Clinical Indication Example |
|---|---|---|---|
| Craniomaxillofacial (CMF) Reconstruction | Ti-6Al-4V (Titanium Alloy) | 510(k) Cleared (Multiple systems, e.g., DePuy Synthes PROPHECY, Stryker TRUMATCH) | Mandibular reconstruction, orbital floor repair |
| Spinal Fusion Cages | PEEK, Titanium Alloy | 510(k) Cleared (e.g., Medtronic CAPSTONE, NuVasive Modulus) | Lumbar interbody fusion |
| Patient-Specific Orthopedic Implants | Ti-6Al-4V, Co-Cr Alloys | 510(k) Cleared via FDA's PSI Guidance | Complex joint revision surgery, bone tumor resection |
| Resorbable Bone Void Fillers | PCL, PCL/β-TCP composites | 510(k) Cleared (e.g., OsteoFab by Oxford Performance Materials) | Filling cranial defects, foot/ankle fusion |
Comparative Performance Metrics: Ti-6Al-4V vs. PCL Scaffolds
| Parameter | Ti-6Al-4V Scaffolds | PCL-based Scaffolds | Measurement Method / Standard |
|---|---|---|---|
| Ultimate Compressive Strength | 500 - 1100 MPa | 2 - 50 MPa | ASTM F452 / ISO 13314 |
| Elastic Modulus | 110 - 120 GPa | 0.2 - 4 GPa | Uniaxial tensile/compressive test |
| Porosity (designed for bone ingrowth) | 50 - 80% | 60 - 90% | Micro-CT analysis |
| Fatigue Strength (10^7 cycles) | 350 - 500 MPa | 1 - 10 MPa | Rotating beam fatigue test |
| In Vitro Osteoblast Proliferation Rate (Day 7) | 120-150% vs. control | 180-250% vs. control (with bioactive coating) | AlamarBlue / MTT assay |
| Complete Degradation Time | Non-degradable | ~24 - 48 months | In vivo implantation (mass loss %) |
| Typical Lead Time for Patient-Specific Implant | 10 - 14 days | 5 - 7 days | From imaging to sterilization |
Regulatory Hurdles and Pathways
Key Regulatory Milestones for Clinical Translation
| Regulatory Stage | Description & Requirements | Typical Timeline | Estimated Cost (USD) |
|---|---|---|---|
| Preclinical (Bench) | Biocompatibility (ISO 10993), Mechanical testing, In vitro cell studies. | 6 - 12 months | $200,000 - $500,000 |
| Preclinical (In Vivo) | Large animal model (e.g., sheep femoral defect). Histology, micro-CT, biomechanical push-out test. | 12 - 24 months | $500,000 - $1.5M |
| Regulatory Submission (e.g., FDA 510(k)) | Demonstration of Substantial Equivalence to a predicate device. Full technical file. | 90-150 days (FDA review) | $100,000 - $500,000 (excluding testing) |
| First-in-Human / Pilot Clinical Study | Small cohort (10-30 patients). Safety & feasibility endpoints. Often requires IDE. | 2 - 3 years | $2M - $5M |
| Pivotal Clinical Trial | Larger, randomized controlled trial for PMA or De Novo classification. | 3 - 5 years | $10M - $30M+ |
Critical Standards for Additively Manufactured Implants
| Standard | Title | Key Requirements for Ti-6Al-4V & PCL |
|---|---|---|
| ASTM F3001 | Standard Specification for Additive Manufacturing Titanium-6 Aluminum-4 Vanadium ELI (Extra Low Interstitial) with Powder Bed Fusion | Chemical composition, microstructure, mechanical properties, post-processing. |
| ASTM F2027 | Standard Guide for Characterization and Testing of Raw or Starting Materials for Porous and Non-porous Medical Devices | Applies to PCL resin feedstock for printing. Requires viscosity, molecular weight, thermal analysis. |
| ISO 10993-1 | Biological evaluation of medical devices | Biocompatibility testing matrix (Cytotoxicity, Sensitization, Irritation, Systemic Toxicity, Implantation). |
| ISO 13485 | Quality management systems for medical devices | Mandatory for design, development, production, and servicing of scaffolds. |
Detailed Experimental Protocols
Protocol 1: In Vitro Osteogenic Differentiation on 3D-Printed Scaffolds
Objective: To assess the osteogenic potential of MC3T3-E1 pre-osteoblasts cultured on Ti-6Al-4V vs. PCL scaffolds.
Materials:
- Scaffolds: Sterilized (autoclaved Ti, ethanol/UV for PCL), 8mm diameter x 4mm height.
- Cells: MC3T3-E1 Subclone 4 (ATCC CRL-2593).
- Medium: α-MEM, 10% FBS, 1% Pen/Strep. Osteogenic Supplement: 50 µg/mL Ascorbic Acid, 10 mM β-glycerophosphate, 100 nM Dexamethasone.
- Assay Kits: AlamarBlue (Viability), Quant-iT PicoGreen dsDNA (Proliferation), SensoLyte pNPP Alkaline Phosphatase (ALP) Assay.
Procedure:
- Seeding: Pre-wet scaffolds in medium. Seed cells at 5 x 10^4 cells/scaffold in low-attachment 24-well plates. Centrifuge plates (500 rpm, 5 min) to enhance cell infiltration.
- Culture: Maintain in growth medium for 24h, then switch to osteogenic medium. Refresh medium every 48h.
- Analysis:
- Day 3, 7, 14: Perform AlamarBlue assay (10% v/v in medium, 2h incubation, measure fluorescence Ex/Em 560/590).
- Day 7, 14, 21: Harvest scaffolds (n=4/timepoint). Lyse cells in 0.1% Triton X-100.
- Use PicoGreen assay for total DNA content (follow manufacturer's protocol).
- Use pNPP assay on same lysate for ALP activity. Normalize ALP to total DNA.
- Statistical Analysis: Two-way ANOVA with Tukey's post-hoc test (factors: Material, Time). p < 0.05 considered significant.
Protocol 2: In Vivo Ovine Critical-Sized Defect Model
Objective: To evaluate bone regeneration and scaffold integration for GMP-grade Ti-6Al-4V vs. PCL-TCP scaffolds.
Materials:
- Animal Model: Mature female sheep (n=8/group), bilateral femoral condyle defects.
- Scaffolds: Sterile, cylindrical (Ø6mm x 10mm). Ti: porous lattice (500µm pore). PCL: 70/30 PCL/β-TCP composite.
- Key Instruments: Surgical drill, dental burr, periosteal elevator, suture.
Procedure:
- Surgery: General anesthesia. Aseptic preparation. Lateral parapatellar arthrotomy to expose femoral condyle. Create a bicortical critical-sized defect (6mm) using drill and burr under saline irrigation.
- Implantation: Press-fit implant into defect. Close fascia and skin in layers. Administer post-op analgesia and antibiotics.
- Termination: Euthanize at 12 weeks.
- Analysis:
- Micro-CT: Scan explanted condyle. Quantify Bone Volume/Total Volume (BV/TV) within region of interest (1mm perimeter around scaffold). Analyze bone-implant contact (BIC%) for Ti group.
- Histology: Dehydrate, embed in methyl methacrylate (Ti) or paraffin (PCL). Section (5-10µm). Stain with Toluidine Blue & Basic Fuchsin (for mineralized bone) and Masson's Trichrome (for collagen). Perform histomorphometry.
The Scientist's Toolkit: Research Reagent Solutions
| Item / Kit | Supplier Examples | Function in Bone Scaffold Research |
|---|---|---|
| AlamarBlue Cell Viability Reagent | Thermo Fisher, Bio-Rad | Fluorescent indicator of metabolic activity for in vitro cytocompatibility screening on scaffold materials. |
| Quant-iT PicoGreen dsDNA Assay | Thermo Fisher | Ultra-sensitive fluorescent quantification of double-stranded DNA, enabling precise cell proliferation measurement on 3D scaffolds. |
| SensoLyte pNPP Alkaline Phosphatase Assay Kit | AnaSpec | Colorimetric (405nm) detection of early osteogenic differentiation marker ALP in cell lysates from scaffolds. |
| Osteogenesis Assay Kit (MilliporeSigma) | MilliporeSigma | Multiplexed measurement of ALP activity and calcium deposition (Alizarin Red S) for late-stage osteogenesis confirmation. |
| Live/Dead Viability/Cytotoxicity Kit | Thermo Fisher | Simultaneous staining with Calcein AM (green, live) and Ethidium homodimer-1 (red, dead) for 3D confocal imaging of cell distribution and viability. |
| Rat/Mouse Osteocalcin EIA Kit | Immunotopics | Enzyme immunoassay for quantifying osteocalcin, a late-stage bone formation marker, in cell culture supernatant or serum from animal studies. |
| µCT Angiogenesis Analysis Software (e.g., CTAn) | Bruker | Advanced software for quantifying 3D microvascular structure within and around implanted scaffolds from contrast-enhanced micro-CT data. |
Diagrams and Visualizations
Title: Regulatory Pathway for Bone Scaffolds
Title: Material Choice Dictates Clinical Application
Title: Fabrication Workflow for PCL vs. Ti Scaffolds
Conclusion
The choice between titanium alloys and PCL for 3D-printed bone scaffolds is not a simple binary but a strategic decision dictated by the specific clinical scenario. Titanium alloys offer unparalleled mechanical integrity and permanence, ideal for large load-bearing defects, yet require optimization to mitigate stress shielding. PCL presents a versatile, biodegradable alternative that supports natural bone remodeling but demands careful engineering to overcome its inherent mechanical and hydrophobic limitations. Future research directions converge on hybrid and composite materials, multi-material 3D printing, and advanced surface functionalization to create next-generation scaffolds that combine the strengths of both material families. The ultimate goal is a new paradigm of patient-specific, bioactive implants that seamlessly integrate with host bone, accelerating the translation of additive manufacturing from bench to bedside in orthopedics and maxillofacial surgery.