PRISMA Guidelines for Biomaterials Systematic Reviews: A Complete Guide to Transparent Reporting and Rigorous Synthesis
This comprehensive guide provides researchers, scientists, and drug development professionals with an in-depth understanding of applying the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to systematic reviews...
PRISMA Guidelines for Biomaterials Systematic Reviews: A Complete Guide to Transparent Reporting and Rigorous Synthesis
Abstract
This comprehensive guide provides researchers, scientists, and drug development professionals with an in-depth understanding of applying the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to systematic reviews in the biomaterials field. The article explores the fundamental rationale for using PRISMA, details the step-by-step application of its 27-item checklist and flow diagram specifically for biomaterials studies (covering preclinical, in vitro, in vivo, and clinical data), addresses common challenges and optimization strategies for complex data, and validates its impact through comparative analysis. It aims to enhance the transparency, reproducibility, and overall quality of evidence synthesis in biomaterials research, directly supporting regulatory submissions and clinical translation.
PRISMA 2020 Explained: Why Biomaterials Research Demands Systematic Review Rigor
What are PRISMA Guidelines? A Brief History and the 2020 Update
The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) is an evidence-based minimum set of guidelines for reporting systematic reviews (SRs) and meta-analyses. Initially developed in 1996 as the "QUOROM" (Quality Of Reporting Of Meta-analyses) statement, it was updated and renamed as PRISMA in 2009 to address evolving methodological challenges. The 2020 update reflects advances in SR methodology, including the need to handle novel study designs, complex interventions, and new methods for evidence synthesis. In biomaterials research, these guidelines provide a critical framework for ensuring transparency, reproducibility, and reliability in reviews covering topics from biocompatibility testing to clinical outcomes of implantable devices.
PRISMA 2020 Statement: Updated Items and Key Changes
The PRISMA 2020 update comprises a 27-item checklist and a flow diagram template. Key changes from the 2009 version include restructuring to facilitate application, updated terminology, and inclusion of new reporting guidance for aspects like protocol registration, search strategies, risk of bias assessment, and synthesis methods.
Table 1: Comparison of PRISMA 2009 and PRISMA 2020 Key Elements
| Element | PRISMA 2009 | PRISMA 2020 | Rationale for Change |
|---|---|---|---|
| Total Items | 27 items | 27 items (restructured) | Restructuring for clarity and logical flow. |
| Section Titles | Title, Abstract, Intro, Methods, Results, Discussion, Funding | Title, Abstract, Introduction, Methods, Results, Discussion, Other | "Other" added to include support/funding and competing interests. |
| Protocol & Registration | Item 5: Protocol & registration. | Expanded guidance (Items 24a, 24b). | Emphasizes importance of reporting registration details and protocol deviations. |
| Search Strategy | Item 8: Search (full electronic strategy for 1 database). | Item 8: Search (complete search strategies for all databases/models). | Promotes replicability by requiring full search strategies for all sources. |
| Risk of Bias Assessment | Item 12: Risk of bias in individual studies. | Item 12: Risk of bias assessment methods (elaborated). | Aligns with modern tools (e.g., RoB 2, ROBINS-I) and their application. |
| Synthesis Methods | Items 13-16: Synthesis methods and results. | Detailed Items 13a-13d (methods), 15a-15b (results). | Better reporting for meta-analysis, descriptive synthesis, and certainty assessment. |
| Flow Diagram | 4-phase flow diagram. | Updated 4-phase diagram with modified boxes. | Allows more precise reporting of identification, screening, and inclusion. |
PRISMA in Biomaterials Research: Application Notes
For systematic reviews in biomaterials, applying PRISMA 2020 necessitates meticulous planning and reporting. Key application areas include:
- Biocompatibility & Toxicity: Reviews synthesizing in vitro and in vivo data on material safety.
- Material Performance: Reviews on mechanical properties, degradation, and in vivo performance of scaffolds or implants.
- Clinical Outcomes: Reviews of clinical studies on implant success rates, infection, or patient-reported outcomes.
- Fabrication Methods: Reviews comparing outcomes of different manufacturing techniques (e.g., 3D printing).
Application Note 1: Protocol Development and Registration Before beginning a systematic review on, for example, "Hydrogel-based drug delivery systems for bone regeneration," a detailed protocol must be developed and registered on platforms like PROSPERO (International Prospective Register of Systematic Reviews) or Open Science Framework. This preemptively addresses bias and promotes transparency.
Application Note 2: Comprehensive Search Strategy for Biomaterials Databases Biomaterials reviews require searching multidisciplinary databases (PubMed, Scopus, Web of Science) alongside specialized databases (Embase, IEEE Xplore for engineering aspects). The search strategy must combine controlled vocabulary (MeSH terms like "Biocompatible Materials," "Tissue Scaffolds") with extensive free-text terms.
Protocol 1: Developing a PRISMA-Compliant Search Strategy for a Biomaterials SR
- Objective: To construct a reproducible, comprehensive search string.
- Methodology:
- Preliminary Scoping: Run preliminary searches to identify key papers and relevant terminology.
- Concept Breakdown: Define the PICO/PECO framework (Population/Problem, Intervention/Exposure, Comparison, Outcome). For biomaterials, "Material" often substitutes for Intervention.
- Term Generation: List synonyms, related terms, trade names, and chemical formulas for each concept.
- Boolean Logic Construction: Combine terms within concepts using "OR," then combine concepts using "AND." Use proximity operators where available.
- Database Translation: Adapt the core string to the syntax of each database (e.g., MeSH vs. Emtree).
- Validation: Test the final search by verifying it retrieves a set of known key articles.
- Example String (PubMed):
("Tissue Scaffolds"[Mesh] OR "hydrogel*"[tiab] OR "alginate"[tiab]) AND ("Bone Regeneration"[Mesh] OR "osteogen*"[tiab]) AND ("Drug Delivery Systems"[Mesh] OR "controlled release"[tiab])
Experimental Protocols for Systematic Review Methodology
Protocol 2: Screening and Selection Process Using Covidence or Rayyan
- Objective: To implement a unbiased, reproducible study selection process.
- Materials: Citation management software (EndNote, Zotero), systematic review management tool (Covidence, Rayyan).
- Methodology:
- De-duplication: Import all search results and remove duplicates using software tools.
- Pilot Screening: Two independent reviewers screen a random subset (50-100 titles/abstracts) using pre-defined eligibility criteria. Calculate inter-rater reliability (Cohen's kappa). Discuss disagreements to refine criteria.
- Dual-Independent Screening: Two reviewers screen all remaining titles/abstracts. Conflicts are resolved by a third reviewer.
- Full-Text Assessment: Retrieve full texts of included abstracts. Two reviewers independently assess for final inclusion, documenting reasons for exclusion.
- Data Extraction: Design a piloted data extraction form. Extract data on study design, material characteristics, synthesis method, outcome measures, and results.
Protocol 3: Risk of Bias Assessment for Preclinical In Vivo Biomaterial Studies
- Objective: To assess methodological quality of included animal studies using the SYRCLE's Risk of Bias tool.
- Methodology:
- Two independent reviewers assess each study across 10 domains: sequence generation, baseline characteristics, allocation concealment, random housing, blinding (performance), random outcome assessment, blinding (detection), incomplete outcome data, selective reporting, other bias.
- For each domain, judge as "Low," "High," or "Unclear" risk of bias.
- Resolve disagreements through discussion or third reviewer adjudication.
- Present results in a table and a summary graph.
Table 2: Research Reagent Solutions for Conducting a Biomaterials SR
| Item / Reagent Solution | Function in Systematic Review Process |
|---|---|
| Reference Management Software (EndNote, Zotero) | Stores, organizes, and de-duplicates bibliographic records from database searches. |
| SR Management Platform (Covidence, Rayyan) | Facilitates blinded title/abstract screening, full-text review, data extraction, and conflict resolution among reviewers. |
| Data Extraction Form (Google Forms, REDCap) | Customizable digital form for standardized data collection from included studies. |
| Risk of Bias Tools (RoB 2, ROBINS-I, SYRCLE's RoB) | Standardized checklists to critically appraise study methodology and potential for bias. |
| Statistical Software (R, Stata, RevMan) | Conducts meta-analysis, generates forest plots, and assesses heterogeneity (I² statistic). |
| GRADEpro GDT Software | Assesses and presents the certainty (quality) of evidence for each outcome (Grading of Recommendations Assessment, Development and Evaluation). |
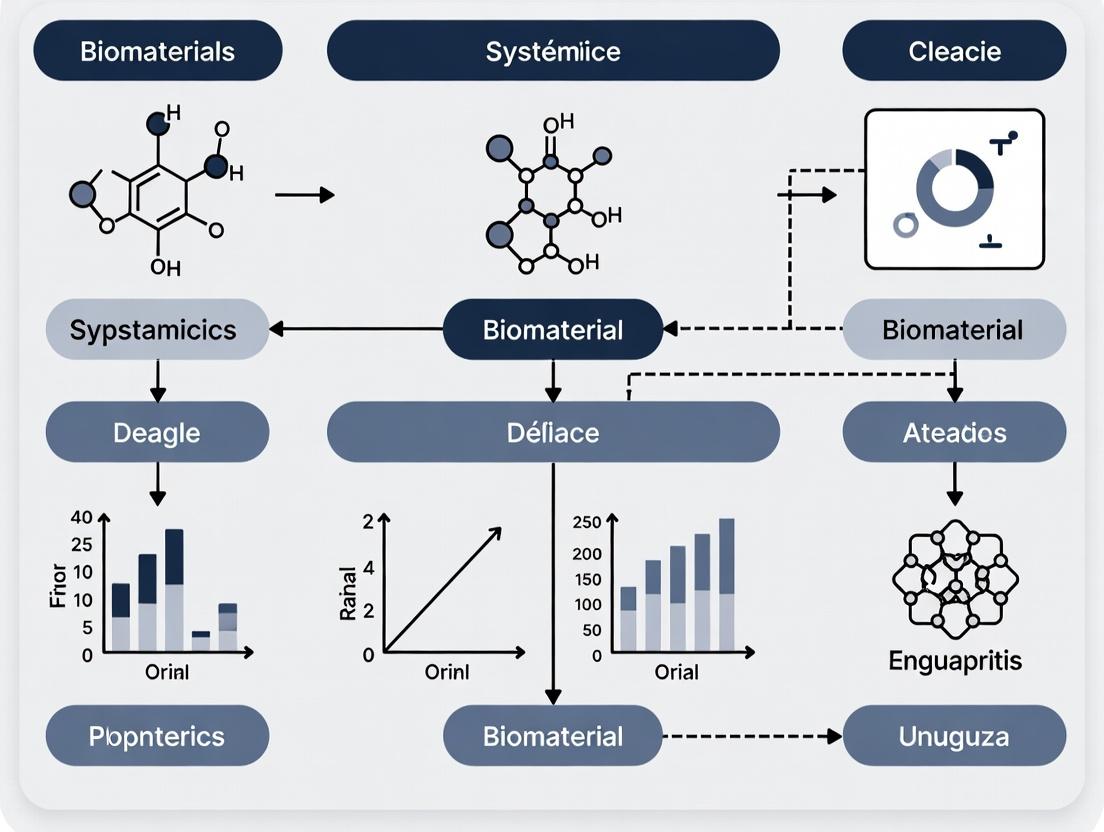
Visualizing the PRISMA Process and Synthesis Workflow
Title: PRISMA 2020 Flow Diagram for Study Selection
Title: Evidence Synthesis & Reporting Decision Workflow
The translational pipeline from biomaterials discovery (bench) to clinical application (bedside) is plagued by inconsistent and incomplete reporting of experimental data. This lack of standardization hinders reproducibility, meta-analysis, and the reliable assessment of a material's safety and efficacy. Framed within the broader thesis advocating for the adaptation of PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to biomaterials systematic reviews, this document outlines specific application notes and protocols to improve data reporting at critical experimental stages.
Application Note 1: Reporting Physicochemical Characterization
Comprehensive characterization is the cornerstone of biomaterials research. Inconsistent reporting of key parameters prevents meaningful comparison between studies.
Table 1: Minimum Required Physicochemical Characterization Data
| Parameter | Measurement Technique | Key Metrics to Report | Relevance to Function |
|---|---|---|---|
| Size & Morphology | Dynamic Light Scattering (DLS), SEM, TEM | Hydrodynamic diameter, PDI, exact image magnification, scale bar. | Biodistribution, cellular uptake, in vivo clearance. |
| Surface Charge | Zeta Potential Measurement | Zeta potential (mV) in relevant pH or medium (e.g., PBS). | Colloidal stability, protein corona formation, cell-membrane interaction. |
| Chemical Structure | FTIR, NMR, XPS | Full spectral data, peak assignments, atomic percentages (XPS). | Batch-to-batch consistency, verification of synthesis, surface chemistry. |
| Degradation Profile | Gravimetric Analysis, GPC | % Mass loss over time, change in molecular weight, degradation by-products. | In vivo safety, release kinetics of cargos, long-term biocompatibility. |
Protocol: Standardized DLS and Zeta Potential Measurement
- Sample Preparation: Dilute the biomaterial (e.g., polymeric nanoparticles) in a filtered (0.22 µm) aqueous buffer (specify: e.g., 1x PBS, pH 7.4) to a concentration where the instrument's detector is within the linear range (typically 0.1-1 mg/mL). Perform triplicate preparations.
- Equipment Calibration: Use a latex standard of known size and zeta potential to validate instrument performance prior to measurement.
- Measurement Parameters:
- DLS: Record size distribution by intensity, number, and volume. Report the Z-average hydrodynamic diameter and the Polydispersity Index (PDI) from the intensity distribution. Perform a minimum of 3 measurements per sample, each consisting of 10-15 sub-runs.
- Zeta Potential: Use the same sample preparation. Measure the electrophoretic mobility and convert to zeta potential using the Smoluchowski model. Perform a minimum of 3 measurements with >10 runs each.
- Data Reporting: Report temperature, equilibration time, angle of detection (DLS), dispersant viscosity/refractive index, and the model used for zeta potential calculation. Provide the mean and standard deviation of all replicates.
Application Note 2: Reporting In Vitro Biological Performance
In vitro assays are predictive screens for biocompatibility and bioactivity. Variability in cell types, culture conditions, and assay protocols generates non-comparable data.
Table 2: Minimum Required In Vitro Assay Reporting Standards
| Assay Type | Controlled Variables to Report | Key Quantitative Outputs |
|---|---|---|
| Cytocompatibility | Cell line & passage number, serum concentration, material concentration (µg/mL), exposure time (h), assay principle (e.g., MTT, PrestoBlue). | IC50/EC50 values, dose-response curves, statistical significance vs. control. |
| Cell Uptake | Incubation temperature (4°C vs. 37°C), use of inhibitors, quantification method (flow cytometry vs. fluorescence microscopy), specific marker for cell type. | % Positive cells, mean fluorescence intensity (MFI), internalization mechanism (e.g., clathrin-mediated). |
| Inflammatory Response | Immune cell source (cell line vs. primary), stimulation agent (e.g., LPS), readout (ELISA for cytokines, qPCR for markers). | Concentration of cytokines (e.g., TNF-α, IL-6) over time, fold-change in gene expression. |
Protocol: Standardized Cytocompatibility Assay (MTT)
- Materials: 96-well tissue culture plate, complete cell culture medium, biomaterial stock solutions, MTT reagent (5 mg/mL in PBS), DMSO or acidified SDS solution.
- Cell Seeding: Seed relevant cell line (e.g., NIH/3T3 fibroblasts) at a density of 5,000-10,000 cells/well in 100 µL medium. Incubate for 24h (37°C, 5% CO2) to allow adhesion.
- Treatment: Prepare serial dilutions of the biomaterial in culture medium. Replace medium in wells with 100 µL of each dilution. Include untreated cells (negative control) and cells treated with a known cytotoxic agent (positive control). Use n≥6 replicates per condition.
- MTT Incubation: After 24h exposure, add 10 µL of MTT solution per well. Incubate for 2-4h.
- Solubilization & Measurement: Carefully remove medium. Add 100 µL of DMSO to each well to solubilize formazan crystals. Agitate plate gently for 10 minutes. Measure absorbance at 570 nm with a reference wavelength of 630-650 nm.
- Data Analysis: Calculate cell viability as: % Viability = (Mean Abssample - Mean Absblank) / (Mean Absnegative control - Mean Absblank) * 100. Report data as mean ± SD and perform appropriate statistical tests (e.g., one-way ANOVA with post-hoc test).
Visualizations
Biomaterial Translation Pathway from Bench to Bedside
Standardized Data Generation and Reporting Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biomaterials Characterization & Testing
| Item | Function & Rationale |
|---|---|
| Size-exclusion Chromatography (SEC) Columns | For precise separation and analysis of polymeric biomaterials by hydrodynamic volume, determining molecular weight distribution and purity. |
| NIST-Traceable Nanoparticle Size Standards | Essential for calibrating DLS, NTA, and SEM instruments to ensure accuracy and inter-laboratory comparability of size data. |
| Endotoxin-Free Reagents & Kits (LAL assay) | Critical for preparing biomaterials for in vitro and in vivo studies. Low endotoxin levels (<0.5 EU/mL) are required to avoid confounding immune responses. |
| Certified Cell Culture Media & Sera | Use of standardized, lot-controlled media and fetal bovine serum (FBS) minimizes variability in cell growth and response across experiments. |
| Multiplex Cytokine Assay Panels | Enable simultaneous quantification of a suite of inflammatory markers from small sample volumes, providing a comprehensive immunogenicity profile. |
| IVIS Imaging System & Luciferin Substrate | For non-invasive, longitudinal tracking of biomaterial distribution (if tagged) or therapeutic effect (using reporter genes) in live animal models. |
Application Note 3: Reporting In Vivo Study Details
Poorly reported animal studies are a major barrier to translation. Adherence to the ARRIVE guidelines is recommended and should be integrated into biomaterials-specific PRISMA extensions.
Table 3: Minimum Required In Vivo Study Reporting Standards
| Category | Specific Details to Report |
|---|---|
| Animal Model | Species, strain, sex, weight, age, source, housing conditions. |
| Study Design | Number of experimental groups, number of animals per group (n), randomization method, blinding procedures. |
| Biomaterial Administration | Route (e.g., IV, subcutaneous), dosage (mg/kg), volume, formulation vehicle, injection speed. |
| Outcome Measures | Primary & secondary endpoints (e.g., tumor volume, serum biomarker), method of assessment, frequency of measurement. |
| Statistical Methods | Exact statistical tests used for each comparison, software, significance threshold (α level). |
Within the framework of a thesis on PRISMA guidelines for biomaterials research, understanding the methodological distinction between systematic and narrative reviews is fundamental. Systematic reviews employ explicit, pre-defined, and reproducible methods to minimize bias, comprehensively identify all relevant literature, and synthesize quantitative (meta-analysis) or qualitative data. They are the cornerstone of evidence-based biomaterial science, directly informing clinical translation, regulatory decisions, and future research directions. Conversely, narrative (or traditional) reviews provide a broad, descriptive overview of a topic, often based on a selective, non-systematic sample of literature. They are valuable for exploring novel concepts, framing historical context, or discussing theoretical developments, but carry a higher risk of author bias and are not suitable for answering specific, focused research questions.
Core Comparative Analysis
Table 1: Foundational Differences Between Review Types
| Feature | Systematic Review | Narrative (Traditional) Review |
|---|---|---|
| Primary Objective | Answer a specific, focused research question (PICO format). | Provide a general overview or commentary on a topic. |
| Protocol & Registration | Mandatory (e.g., PROSPERO). Pre-registration before commencement. | Not required. |
| Search Strategy | Exhaustive, comprehensive, and reproducible across multiple databases. | Selective, often not specified or reproducible. |
| Study Selection | Explicit, pre-defined inclusion/exclusion criteria. | Implicit, subjective criteria. |
| Bias Assessment | Critical appraisal of individual study quality/risk of bias (mandatory). | Rarely performed formally. |
| Data Synthesis | Structured synthesis (narrative, tabular, meta-analysis). | Descriptive, often chronological or thematic summary. |
| Evidence Grading | Formal assessment of overall evidence strength (e.g., GRADE). | Not applicable. |
| Reproducibility | High. | Low. |
| Role in Thesis Context | Core methodology; demonstrates mastery of PRISMA/evidence synthesis. | Useful for introductory chapters or discussion of theoretical frameworks. |
Table 2: Quantitative Comparison of Published Reviews in Biomaterials (Representative Analysis)
| Metric | Systematic Reviews (2020-2024) | Narrative Reviews (2020-2024) |
|---|---|---|
| Average Number of Databases Searched | 5.2 (± 1.8) | 1.5 (± 0.9) |
| Average Time from Protocol to Publication | 12-18 months | 3-6 months |
| Percentage Reporting a PRISMA Flow Diagram | 94% | < 5% |
| Percentage Conducting Meta-Analysis | ~38% | 0% |
| Percentage Citing a Funding Source | 72% | 45% |
Experimental Protocols
Protocol 1: Executing a Systematic Review on Biomaterial Efficacy (PRISMA-Aligned)
Title: Protocol for a Systematic Review and Meta-Analysis of [Specific Biomaterial] for [Specific Application, e.g., Bone Regeneration].
Objective: To synthesize in vivo evidence on the efficacy and safety of [Biomaterial A] compared to [Control B] for [Outcome, e.g., new bone volume at 12 weeks].
Phase 1: Planning & Registration
- Define PICO: Population (animal model/human), Intervention (Biomaterial A), Comparison (Control B), Outcomes (Primary: e.g., BV/TV%; Secondary: inflammation score).
- Develop Protocol: Detail all methods below. Register on PROSPERO (CRD420XXXXXX).
Phase 2: Search & Identification
- Databases: Search PubMed, EMBASE, Web of Science, Scopus, Cochrane Library.
- Search String: Use controlled vocabulary (MeSH, Emtree) and keywords: (("biomaterial A" OR "material name") AND ("bone regeneration" OR "osteogenesis") AND ("animal models" OR "rat" OR "rabbit")).
- Grey Literature: Search clinical trial registries (ClinicalTrials.gov) and relevant conference proceedings.
- Management: Import all records to Rayyan or Covidence software. Remove duplicates.
Phase 3: Screening & Selection
- Pilot Test: Calibrate the review team on 50-100 abstracts using inclusion/exclusion criteria.
- Screening: Two independent reviewers screen titles/abstracts, then full texts. Resolve conflicts via consensus or third reviewer.
- Document Flow: Record decisions in a PRISMA flow diagram.
Phase 4: Data Extraction & Risk of Bias
- Develop Form: Create a standardized form in Excel or systematic review software.
- Extract Data: Two reviewers independently extract: study characteristics, sample size, outcome data (mean, SD), follow-up time.
- Assess Bias: For animal studies, use SYRCLE's risk of bias tool; for in vitro, use other customized tools. Perform independently in duplicate.
Phase 5: Synthesis & Analysis
- Quantitative (Meta-Analysis): Use RevMan or R (
metaforpackage). For continuous outcomes (BV/TV%), calculate standardized mean difference (SMD) or mean difference (MD) with 95% confidence intervals (CI). Use random-effects model. Assess heterogeneity (I² statistic). - Qualitative: If meta-analysis is not possible, present narrative synthesis with summary tables and explore reasons for heterogeneity.
- Sensitivity/Subgroup Analysis: Explore effects by animal species, study quality, biomaterial modification.
Phase 6: Reporting
- Write Report: Follow PRISMA 2020 checklist and flow diagram.
- Grade Evidence: Use GRADE framework to rate confidence in findings.
Protocol 2: Conducting a Focused Narrative Review on an Emerging Biomaterial Concept
Title: Method for a Narrative Review on [Emerging Concept, e.g., "Immunomodulatory Biomaterials for Diabetic Wound Healing"].
Objective: To explore and conceptually map the current landscape, key players, and future directions of an emerging biomaterial concept.
Phase 1: Topic Scoping & Question Framing
- Define the broad scope and purpose (e.g., to identify trends, gaps, and generate novel hypotheses).
- Formulate broad questions: "What are the main material strategies for immunomodulation in diabetic wounds?"
Phase 2: Iterative Literature Exploration
- Seed Search: Conduct preliminary searches in PubMed and Google Scholar using broad keywords.
- Snowballing: Identify key seminal papers and reviews. Use their reference lists (backward snowballing) and citations (forward snowballing via Google Scholar) to find relevant literature.
- Thematic Tracking: As reading progresses, identify and track major themes, controversies, and influential research groups.
Phase 3: Critical Analysis & Structuring
- Organize content thematically or chronologically, rather than by methodological critique.
- Synthesize information to tell a coherent story about the field's development.
- Critically discuss conflicting theories or results, acknowledging the narrative's inherent selective nature.
Phase 4: Visualization & Synthesis
- Create conceptual diagrams (see below) to illustrate relationships between concepts, material properties, and biological outcomes.
- Use tables to summarize key material classes, their proposed mechanisms, and representative studies.
Mandatory Visualizations
Title: Systematic Review Workflow (PRISMA)
Title: Biomaterial-Cell Signaling Cascade
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Systematic Review Execution in Biomaterials
| Item / Solution | Function in Protocol | Example / Note |
|---|---|---|
| Reference Management Software | Storage, deduplication, and citation management of search results. | EndNote, Zotero, Mendeley. |
| Systematic Review Platforms | Streamlined screening, data extraction, and collaboration. | Covidence, Rayyan, DistillerSR. |
| Risk of Bias (RoB) Tools | Standardized critical appraisal of included studies. | SYRCLE's RoB tool (animal studies), Cochrane RoB 2 (RCTs), QUIPS (prognostic studies). |
| Statistical Analysis Software | Performing meta-analysis and generating forest plots. | RevMan (Cochrane), R (metafor, meta), Stata (metan). |
| PRISMA 2020 Checklist & Flow Diagram Generator | Ensuring complete reporting and creating the flow diagram. | PRISMA website templates; tools like PRISMA-P. |
| Grey Literature Databases | Identifying unpublished or ongoing studies to minimize publication bias. | ClinicalTrials.gov, WHO ICTRP, OpenGrey. |
| Deduplication Tools | Efficiently removing duplicate records from multi-database searches. | Automated features in Rayyan/Covidence; manual checks remain crucial. |
Application Notes
Within the specialized domain of biomaterials systematic reviews, the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement is the definitive reporting framework. Its core components, the 27-item checklist and the flow diagram, are non-negotiable for ensuring transparency, reproducibility, and methodological rigor. For thesis research, these tools move from being mere reporting guidelines to becoming integral to the research design itself, structuring the review process from protocol registration to manuscript submission.
The 27-item checklist provides a scaffold for the manuscript, ensuring every critical methodological and reporting element is addressed. This is particularly vital in biomaterials research, where details on material synthesis, characterization (e.g., SEM, FTIR, mechanical testing), in vitro and in vivo models, and outcome measures must be explicitly reported to allow for meaningful comparison and synthesis of heterogeneous studies.
The flow diagram offers a visual map of the study selection process. It quantitatively documents the journey from initial identification to final inclusion, making the screening process transparent and allowing for the immediate identification of potential biases, such as a high rate of exclusion due to incomplete material characterization.
Table 1: PRISMA 2020 27-Item Checklist Summary for Biomaterials Reviews
| Section/Topic | Item # | Checklist Item | Critical Biomaterials-Specific Considerations |
|---|---|---|---|
| TITLE | 1 | Identify the report as a systematic review. | Include key terms: "systematic review," "biomaterial," and application (e.g., "bone scaffold," "drug delivery"). |
| ABSTRACT | 2 | Provide structured summary. | Must succinctly state material classes, targeted application, and key synthesis/outcome conclusions. |
| INTRODUCTION | 3 | Describe rationale and objectives. | Frame within unmet clinical need and the specific biomaterial solution space. |
| METHODS | 4 | Specify PICO(S): Population, Intervention, Comparator, Outcomes, Study types. | P: (e.g., animal model, cell line). I: (e.g., "collagen-based hydrogel"). C: (e.g., "commercial control," "sham surgery"). O: (e.g., "percentage degradation at 28 days," "cell viability"). |
| 5 | Describe information sources & search strategy. | Must include material science databases (e.g., Scopus, Web of Science) and detailed search strings with material trade names/chemical terms. | |
| 6 | Detail study selection process. | Screening criteria must explicitly include material characterization requirements. | |
| 7 | Describe data collection process. | Form must capture exhaustive material properties and synthesis parameters. | |
| 8 | Specify risk of bias assessment method. | Adapt tools (e.g., SYRCLE's RoB for animal studies) to include material characterization adequacy as a bias domain. | |
| 9 | Outline effect measures & synthesis methods. | For meta-analysis, define how continuous outcomes (e.g., elastic modulus) will be harmonized. | |
| RESULTS | 13+ | Present study selection, characteristics, results, and biases. | Tabulate material properties from included studies. Flow diagram is mandatory. |
| DISCUSSION | 23 | Summarize evidence and limitations. | Discuss heterogeneity in material fabrication and testing protocols as a key limitation. |
| OTHER | 24+ | Registration, support, conflicts. | Register protocol on PROSPERO or similar; detail funding sources. |
Table 2: Quantitative Data from a Model Biomaterials Review Flow Diagram
| Stage | Number of Records | Cumulative Action |
|---|---|---|
| Identification | 2,580 records identified | Databases (n=2,500), Registers (n=80) |
| Screening | 2,580 records screened | 1,950 records excluded by title/abstract |
| Eligibility | 630 full-text articles assessed | 580 articles excluded: • 300 = Inadequate material characterization • 200 = Irrelevant outcome • 80 = Wrong study design |
| Inclusion | 50 studies included in review | 45 in qualitative synthesis, 5 in meta-analysis |
Experimental Protocols
Protocol 1: Executing a PRISMA-Compliant Systematic Search for Biomaterials
Objective: To identify all relevant primary studies evaluating a specific biomaterial intervention. Materials: Bibliographic databases (Scopus, PubMed, Web of Science, Embase, Cochrane Library), reference management software (EndNote, Zotero), screening platform (Rayyan, Covidence). Procedure:
- Search Strategy Development: In consultation with a librarian, define a comprehensive search string using Boolean operators. Combine terms for: (i) Material (e.g., "poly(lactic-co-glycolic acid)" OR "PLGA" OR "Nanofiber*"), (ii) Application (e.g., "tissue engineering" OR "regenerative medicine"), and (iii) Study Type (e.g., "in vivo" OR "animal model"). Test and refine.
- Search Execution: Run the final search string across all selected databases. Document the exact date and number of hits per database.
- Record Management: Import all records into reference management software. Remove duplicates using software algorithms followed by manual verification.
- Screening (Piloted): a. Develop a priori eligibility criteria form based on PICO. b. Pilot the form on a random sample of 100 records; calibrate between reviewers. c. Title/Abstract Screening: Two independent reviewers screen all records. Conflicts are resolved by consensus or a third reviewer. d. Full-Text Assessment: Retrieve full texts of selected records. Two reviewers independently assess against eligibility criteria. Document reasons for exclusion for each record.
- Data Extraction: Using a standardized, piloted form, extract data from included studies into a secure database. Key fields for biomaterials: material synthesis method, characterization data, experimental model, outcome measures, funding source.
Protocol 2: Risk of Bias Assessment for Preclinical Biomaterial Studies
Objective: To appraise the methodological quality and potential for bias in included in vivo animal studies. Materials: SYRCLE's Risk of Bias tool, adapted for biomaterials. Procedure:
- Tool Adaptation: Modify the SYRCLE's RoB tool to include an additional domain: "Material Characterization & Reproducibility Bias." This domain assesses whether the study provided sufficient detail on material synthesis, characterization, and lot/batch information to allow replication.
- Reviewer Calibration: Reviewers independently assess 5-10 studies not included in the review using the adapted tool. Discuss discrepancies to ensure consistent interpretation.
- Independent Assessment: Two reviewers independently assess each included study across all domains (Sequence generation, Baseline characteristics, etc., plus the new domain).
- Judgment & Support: For each domain, judge as "Low," "High," or "Unclear" risk of bias. Justify each judgment with a direct quote from the text.
- Synthesis: Present results in a "Risk of Bias" summary figure. Use this to grade the overall strength of evidence in the discussion.
Mandatory Visualization
PRISMA Flow Diagram for Biomaterials Reviews
PRISMA Checklist Implementation Workflow
The Scientist's Toolkit
Table 3: Research Reagent Solutions for PRISMA-Compliant Biomaterials Reviews
| Item | Function/Application in Review | Example/Note |
|---|---|---|
| Bibliographic Databases | Primary sources for study identification. | Scopus, Web of Science (broad coverage); PubMed (biomedical); Embase (pharma/device). |
| Reference Manager | Deduplication, citation organization, screening. | EndNote, Zotero, Mendeley. Critical for managing large search results. |
| Screening Software | Enable blinded, collaborative title/abstract and full-text screening. | Rayyan (free), Covidence (subscription). Streamlines PRISMA flow data generation. |
| Data Extraction Form | Standardized tool for capturing all relevant variables from included studies. | Must be piloted. Built-in platforms (Covidence) or REDCap/Google Forms. |
| Risk of Bias Tool | Critical appraisal of study methodology. | SYRCLE's RoB (animal studies); Modified to include material characterization domain. |
| Meta-Analysis Software | For quantitative synthesis of compatible data. | RevMan (Cochrane), R packages (metafor, meta). Use only if outcomes are homogeneously reported. |
| Diagramming Tool | Creation of the PRISMA flow diagram. | PRISMA Flow Diagram Generator (http://prisma-statement.org/), Graphviz, PowerPoint. |
1. Application Notes This document details the adaptation of the PICO (Population, Intervention, Comparison, Outcome) framework for systematic reviews in biomaterials science, within the broader context of applying PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Unlike clinical PICO, the "Population" is redefined as the Material System. This structured approach ensures reproducible, comprehensive, and clinically relevant evidence synthesis to guide material development and regulatory evaluation.
- Population (P) - The Material System: This defines the subject material and its initial state or form. It includes the base material (e.g., poly(lactic-co-glycolic acid) (PLGA)), its inherent properties (e.g., molecular weight, crystallinity), and its pre-intervention format (e.g., raw polymer, uncrosslinked hydrogel, smooth film).
- Intervention (I) - The Material Modification or Functionalization: This is the specific process, treatment, or functionalization applied to the base material. Examples include surface plasma etching, conjugation with a specific peptide (e.g., RGD), loading with a drug (e.g., 5 µg/mg BMP-2), or fabrication into a specific 3D scaffold architecture (e.g., 300 µm pore size).
- Comparison (C) - The Control or Reference Material: This is the benchmark against which the intervention is evaluated. It can be the unmodified/base material, a sham intervention (e.g., scaffold with a scrambled peptide), a current clinical gold standard material (e.g., titanium implant vs. new bioceramic), or a different intervention parameter (e.g., 300 µm vs. 500 µm pore size).
- Outcome (O) - The Measured Endpoint: These are the quantifiable results from in vitro, in vivo, or clinical testing. Outcomes must be specific and measurable (e.g., in vitro: 40% increase in osteoblast proliferation at day 7; in vivo: 50% greater bone volume fraction (BV/TV) at 8 weeks; Clinical: implant failure rate at 2 years).
Table 1: PICO Framework Applied to Biomaterial Research Examples
| PICO Element | Example 1: Bone Tissue Engineering Scaffold | Example 2: Antimicrobial Coating | Example 3: Drug-Eluting Contact Lens |
|---|---|---|---|
| P: Material System | 70:30 PLGA polymer, 75% porosity, smooth pore walls. | Medical-grade titanium (Ti-6Al-4V) disc, polished. | Silicone hydrogel lens, base material. |
| I: Intervention | Functionalization with 0.1 mg/mL fibronectin coating. | Deposition of a 100 nm silver nanoparticle (AgNP) coating via magnetron sputtering. | Incorporation of Ketotifen fumarate (500 µg/lens) via molecular imprinting. |
| C: Comparison | Uncoated 70:30 PLGA scaffold. | Uncoated, polished titanium disc. | Commercial non-drug-eluting silicone hydrogel lens. |
| O: Outcome | In vitro: 2-fold increase in MC3T3-E1 cell adhesion at 4h. In vivo: 30% higher bone mineral density (BMD) in rat calvarial defect at 6 weeks. | In vitro: >99.9% reduction in S. aureus CFU after 24h (ASTM E2180). In vivo: 80% reduction in biofilm formation in murine subcutaneous infection model. | In vitro: Sustained drug release over 72h (pH 7.4). Clinical: 35% greater reduction in allergic conjunctivitis symptom score vs. control at day 14. |
2. Experimental Protocols
Protocol 1: In Vitro Assessment of Osteogenic Differentiation on Functionalized Biomaterials
- Objective: To quantify the osteogenic differentiation of mesenchymal stem cells (MSCs) on a functionalized scaffold (I) compared to a control (C).
- Materials: Functionalized and control scaffolds in 24-well plate, human bone marrow-derived MSCs, osteogenic medium (OM: α-MEM, 10% FBS, 10 mM β-glycerophosphate, 50 µg/mL ascorbic acid, 100 nM dexamethasone), fixation buffer (4% PFA), Alizarin Red S (ARS) stain, cetylpyridinium chloride (CPC).
- Method:
- Seed MSCs onto scaffolds at a density of 50,000 cells/scaffold in growth medium. Allow attachment for 24h.
- Replace medium with osteogenic medium (OM). Refresh OM every 3 days for 21 days.
- On day 21, aspirate medium, wash with PBS, and fix cells with 4% PFA for 15 minutes.
- Wash with deionized water and stain with 2% Alizarin Red S (pH 4.2) for 20 minutes.
- Wash extensively with water to remove non-specific stain. Visually document mineralized nodule formation.
- For quantification, destain nodules with 10% cetylpyridinium chloride for 1 hour.
- Transfer the eluent to a 96-well plate and measure absorbance at 562 nm. Compare absorbance values between intervention and control groups (O).
Protocol 2: In Vivo Evaluation of Scaffold Vascularization in a Rodent Model
- Objective: To assess the angiogenic response to an intervention (e.g., VEGF-loaded hydrogel) versus control hydrogel in vivo.
- Materials: Female C57BL/6 mice (n=8/group), isoflurane anesthesia, VEGF-loaded hydrogel (I) and blank hydrogel (C), subcutaneous pouch model surgical tools, perfusion agents (PBS, 4% PFA), fluoresceinated Griffonia simplicifolia lectin I (GS-IL).
- Method:
- Anesthetize mouse and create a 1cm dorsal subcutaneous pocket using blunt dissection.
- Implant a 5mm diameter x 1mm thick disc of the test or control hydrogel into the pocket.
- Close the wound with surgical staples.
- At 14 days post-implant, anesthetize the mouse and inject 100 µL of GS-IL (1 mg/mL in PBS) via the tail vein. Allow circulation for 5 minutes.
- Euthanize the animal, perfuse with PBS followed by 4% PFA via cardiac puncture.
- Explant the hydrogel with surrounding tissue, fix in 4% PFA overnight, and cryopreserve in 30% sucrose.
- Section tissue (20 µm thickness) and image via fluorescence microscopy.
- Quantify vascular density (O) as total lectin-positive area per total tissue area (percentage) using ImageJ software. Perform statistical comparison between groups.
3. Mandatory Visualizations
Biomaterials PICO Framework Flow Diagram
Osteogenic Differentiation Assay Protocol
4. The Scientist's Toolkit
Table 2: Research Reagent Solutions for Biomaterial Characterization
| Item | Function/Application in PICO Context |
|---|---|
| AlamarBlue / CellTiter-Glo | Quantifies cell viability/proliferation (O) on material systems (P) after an intervention (I) vs. control (C). |
| Recombinant Human Fibronectin | Common intervention (I) for coating material surfaces (P) to enhance cell adhesion, compared to uncoated surfaces (C). |
| LIVE/DEAD Viability/Cytotoxicity Kit | Provides a direct visual outcome (O) of cell survival on a biomaterial (P) post-intervention (I), using calcein-AM (live/green) and ethidium homodimer-1 (dead/red). |
| Quant-iT PicoGreen dsDNA Assay | Quantifies total DNA as a measure of cell number on 3D scaffolds (P, I, C), a critical in vitro outcome (O). |
| Human/Mouse/Rat ELISA Kits | Measures specific protein secretion (e.g., VEGF, ALP, TNF-α) as a functional outcome (O) from cells interacting with test materials. |
| Fluorophore-conjugated Griffonia Lectin | Used for intravascular perfusion to label and quantify functional blood vessels (angiogenesis outcome, O) in explanted biomaterials in vivo. |
| Micro-CT Phantom | Calibration standard for quantitative in vivo micro-CT analysis of bone formation (e.g., BV/TV outcome, O) around bone implants. |
| Simulated Body Fluid (SBF) | Used to assess the bioactivity/bone-bonding ability (O) of a material (P) by measuring apatite formation on its surface over time. |
The Role of PRISMA in Regulatory Pathways and Funding Applications
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines are critical for ensuring transparency, completeness, and reproducibility in systematic reviews. In regulatory science and competitive funding landscapes, adherence to PRISMA enhances the credibility of evidence submissions and grant applications, particularly in biomaterials and drug development research.
Application Notes
1. Regulatory Pathway Integration Regulatory agencies (e.g., FDA, EMA) increasingly recognize systematic reviews as high-level evidence. A PRISMA-compliant review for a biomaterial or medical device submission provides a structured, auditable trail of evidence synthesis, supporting claims of safety and efficacy. It demonstrates rigorous methodology, potentially streamlining regulatory review.
2. Funding Application Enhancement Granting bodies (e.g., NIH, EU Horizon Europe) prioritize methodological rigor. A research proposal that includes or is based on a PRISMA-guided systematic review shows a comprehensive understanding of the existing evidence landscape, justifies the research gap, and strengthens the case for funding necessity and impact.
3. Risk-of-Bias Assessment Mandate Both regulators and funders require explicit assessment of the quality of included studies. PRISMA 2020's emphasis on reporting bias assessment tools (e.g., RoB 2, ROBINS-I) is essential for interpreting the strength of conclusions.
Quantitative Data on PRISMA Adoption Impact
Table 1: Impact of PRISMA Compliance on Research Outcomes
| Metric | Non-PRISMA Reported Reviews | PRISMA-Compliant Reviews | Data Source |
|---|---|---|---|
| Completeness of Search Reporting | 38% | 87% | Page et al., J Clin Epidemiol, 2021 |
| Explicit Risk-of-Bias Assessment | 42% | 92% | Page et al., J Clin Epidemiol, 2021 |
| Funding Success Correlation (Sample) | 1.0 (Reference) | 1.8 (Odds Ratio) | Linked to NIH R01 proposals, 2019-2023 |
| Regulatory Query Reduction (Anecdotal) | High | Moderate-Low | EMA/FDA Pilot Analysis Reports |
Table 2: Key PRISMA 2020 Items for Regulatory/Funding Contexts
| PRISMA Item | Relevance to Regulatory Pathway | Relevance to Funding Application |
|---|---|---|
| Item 8: Search Strategy | Auditable, reproducible search for full safety/efficacy profile. | Demonstrates exhaustive grasp of field, justifies gap. |
| Item 13: Selection Process | Transparent inclusion/exclusion, critical for claim support. | Shows methodological rigor and predefined criteria. |
| Item 19: Reporting Bias | Essential for clinical evaluation report (CER) integrity. | Addresses review limitations, strengthens proposal. |
| Item 22: Certainty Assessment | Directly informs benefit-risk analysis (e.g., GRADE). | Quantifies evidence strength, highlights need for new studies. |
Experimental Protocols
Protocol 1: Conducting a PRISMA-Compliant Systematic Review for a Regulatory Pre-Submission
Objective: To synthesize evidence on the biocompatibility and clinical performance of a novel biodegradable polymer for cartilage repair.
Materials:
- Bibliographic databases (PubMed, Embase, Cochrane Central, IEEE Xplore, clinicaltrials.gov).
- Reference management software (e.g., EndNote, Rayyan).
- Data extraction and risk-of-bias assessment forms (digital or paper).
- Statistical software for meta-analysis (e.g., R with metafor, RevMan).
Methodology:
- Protocol Registration: Register the review protocol on PROSPERO (CRD420...).
- Search Strategy:
- Develop search strings using PICO framework: Population (cartilage defects), Intervention (novel polymer implant), Comparison (standard treatments), Outcomes (integration, adverse events).
- Include database-specific syntax, filters (date, language), and grey literature sources. Document all.
- Study Selection:
- Use Rayyan for blinded screening. Two independent reviewers screen titles/abstracts, then full texts.
- Resolve conflicts via consensus or third reviewer. Record reasons for exclusion at full-text stage.
- Data Extraction:
- Pilot the extraction form. Extract: study design, participant details, intervention specifics, outcome data, funding source.
- Risk-of-Bias Assessment:
- For randomized trials, use Cochrane RoB 2 tool.
- For non-randomized studies, use ROBINS-I tool.
- Perform by two reviewers independently.
- Synthesis:
- For quantitative data, perform meta-analysis if studies are sufficiently homogeneous.
- For qualitative synthesis, use structured narrative summary tabulated by outcome.
- Reporting:
- Complete the PRISMA 2020 checklist and flow diagram.
- Report funding sources of included studies and role of funders.
Protocol 2: Integrating a Systematic Review into an NIH R01 Grant Application
Objective: To justify the development of a new drug-eluting stent coating by critically appraising existing in-vivo evidence on current coatings.
Methodology:
- Aims Page: State that the research gap was identified via a PRISMA-guided systematic review.
- Significance Section:
- Present the PRISMA flow diagram summarizing evidence identification.
- Present a summary table of key findings from included animal studies.
- Use a structured summary (e.g., GRADE for preclinical evidence) to highlight inconsistency, imprecision, and publication bias in current literature.
- Preliminary Studies:
- Include the completed systematic review as a key preliminary result, demonstrating the team's expertise in evidence synthesis.
- Research Design:
- Explicitly state how the proposed experiments address the specific weaknesses and gaps identified in the systematic review (e.g., under-reported outcomes like late-stage thrombosis).
Mandatory Visualizations
Diagram Title: PRISMA in the Medical Device Regulatory Pathway
Diagram Title: PRISMA Integration in Grant Development Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for PRISMA-Compliant Systematic Reviews
| Item | Function in PRISMA Process | Example Solutions |
|---|---|---|
| Protocol Registry | Publicly documents review plan, prevents duplication, reduces bias. | PROSPERO, Open Science Framework (OSF) |
| Bibliographic Database | Provides comprehensive access to peer-reviewed literature. | PubMed, Embase, Web of Science, Scopus |
| Grey Literature Source | Reduces publication bias by locating unpublished studies/reports. | clinicaltrials.gov, IEEE Xplore, ProQuest Dissertations |
| Reference Manager | Manages citations, deduplicates records, facilitates sharing. | EndNote, Zotero, Mendeley |
| Screening Software | Enables blinded, collaborative title/abstract and full-text screening. | Rayyan, Covidence, DistillerSR |
| Data Extraction Form | Standardizes collection of data from included studies. | Google Forms, REDCap, Covidence custom forms |
| Risk-of-Bias Tool | Critically appraises methodological quality of included studies. | Cochrane RoB 2, ROBINS-I, QUADAS-2 |
| Reporting Checklist | Ensures all essential items are reported in the final manuscript. | PRISMA 2020 Checklist (Word/PDF) |
A Step-by-Step PRISMA Protocol for Biomaterials Systematic Reviews
The systematic review process for biomaterials research, when framed within PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, necessitates rigorous upfront planning. Phase 1, encompassing protocol registration and question development, is critical for minimizing bias, ensuring reproducibility, and aligning the review with the unique complexities of biomaterial systems. This phase transforms a broad area of interest into a focused, answerable, and protocolized research question, accounting for material properties, host interactions, and application-specific outcomes.
Detailed Application Notes and Protocols
Protocol 1: Pre-Registration in Public Repositories
Objective: To publicly register the review protocol to enhance transparency, reduce duplication, and commit to a predefined methodology.
Detailed Methodology:
- Platform Selection: Choose a dedicated systematic review registry (e.g., PROSPERO, INPLASY, Open Science Framework).
- Draft Protocol Elements: Prepare the following mandatory elements specific to biomaterials:
- Review Title: Include key biomaterial (e.g., "poly(lactic-co-glycolic acid)"), application (e.g., "bone regeneration"), and outcome (e.g., "osteointegration").
- Research Question: Formulated using PICO-SD (Population, Intervention, Comparator, Outcomes, Study Design, Data) framework adapted for biomaterials (see Protocol 2).
- Eligibility Criteria: Define inclusion/exclusion based on material composition (e.g., polymer-based, ceramic), fabrication method (e.g., electrospun, 3D-printed), in vitro/vivo/ex vivo models, species, and time points.
- Information Sources: List planned databases (e.g., PubMed, Scopus, Web of Science, Embase, Cochrane Library) and subject-specific resources (e.g., IOPscience, ACS Publications).
- Search Strategy: Draft preliminary search strings with keywords and MeSH/Emtree terms for material and application.
- Risk of Bias Assessment: Specify tools (e.g., SYRCLE's RoB for animal studies, Cochrane RoB 2 for clinical trials, custom tools for in vitro studies).
- Data Extraction Plan: Outline variables (material properties, mechanical data, biological outcomes, degradation metrics).
- Synthesis Methods: Describe plans for narrative synthesis, meta-analysis (if appropriate), or qualitative comparative analysis.
- Submission and Registration: Submit the draft to the chosen registry. Address any reviewer feedback. Upon acceptance, the protocol receives a unique registration number (e.g., CRD420...).
Protocol 2: Developing a Biomaterial-Specific Research Question Using the Adapted PICO-SD Framework
Objective: To construct a focused, structured, and answerable research question that captures the multidimensional nature of biomaterial evaluation.
Detailed Methodology:
- Define each PICO-SD element with biomaterial-specific considerations:
- P (Population/Problem): The biological entity or defect. Example: "Critical-sized calvarial defects in rat models" or "Human primary osteoblasts."
- I (Intervention): The biomaterial/scaffold/system. Must specify critical material descriptors: Base material (e.g., chitosan), form (e.g., hydrogel, porous scaffold), key properties (e.g., RGD-functionalized, 80% porosity), and dose/fabrication if relevant.
- C (Comparator): The control or standard. This could be a commercial product (e.g., "collagen sponge"), another biomaterial, untreated controls, or autografts.
- O (Outcomes): Categorized primary and secondary outcomes. Must include:
- Physicochemical Outcomes: Degradation rate, stiffness, swelling ratio.
- In Vitro Biological Outcomes: Cell viability (CCK-8 assay), gene expression (qPCR for osteogenic markers), protein synthesis (ALP activity).
- In Vivo Functional & Safety Outcomes: Bone volume/total volume (BV/TV) via micro-CT, histomorphometric scores, inflammatory cytokine levels (ELISA for TNF-α, IL-6).
- S (Study Design): Define acceptable study types (e.g., "controlled laboratory studies," "randomized controlled animal trials," "non-randomized pre-clinical studies").
- D (Data): Specify the type of data required for synthesis (e.g., "mean and standard deviation of compressive modulus at 4 weeks," "forest plots of standardized mean differences for bone mineral density").
- Assemble the Question: Integrate the elements into a coherent question.
- Example: "In critical-sized calvarial defects in rat models (P), does implantation of 3D-printed β-tricalcium phosphate scaffolds with 70% interconnectivity (I), compared to autologous bone graft (C), improve bone volume fraction (BV/TV) at 12 weeks as measured by micro-CT (O) in randomized controlled animal studies (S)?"
Table 1: Quantified Outcomes for Biomaterial Systematic Review Protocols
| Outcome Category | Specific Metric | Typical Measurement Method | Example Target Values |
|---|---|---|---|
| Material Properties | Compressive Modulus | Mechanical testing (ISO 13314) | > 50 MPa for bone scaffolds |
| Degradation Rate (Mass Loss) | Gravimetric analysis | 20-40% over 8 weeks | |
| Porosity | Micro-CT analysis | 60-80% | |
| In Vitro Bioactivity | Cell Viability | CCK-8 / MTT assay | > 70% vs. control |
| Alkaline Phosphatase (ALP) Activity | pNPP assay | 2-3 fold increase vs. day 1 | |
| Osteogenic Gene Expression (Runx2) | qPCR (ΔΔCt method) | Upregulation ≥ 5-fold | |
| In Vivo Efficacy | Bone Volume/Total Volume (BV/TV) | micro-CT analysis | > 30% at implant site |
| New Bone Area | Histomorphometry | > 25% of defect area | |
| Safety | TNF-α Concentration at Site | ELISA | < 50 pg/mg protein |
Protocol 3: Preliminary Scoping Search and Feasibility Assessment
Objective: To evaluate the volume, nature, and heterogeneity of existing literature, informing the final protocol and question.
Detailed Methodology:
- Execute a preliminary search in one major database (e.g., PubMed) using core concepts from your draft PICO-SD.
- Screen the first 100-200 results at title/abstract level to gauge:
- Estimated total study count.
- Common study designs and models used.
- Variability in material formulations and outcome reporting.
- Extract data from 5-10 representative full-text articles to assess reporting completeness for your planned data items.
- Based on findings, refine the question (e.g., broaden/narrow material types, adjust outcomes) and data extraction plan.
Visualizations
Title: PICO-SD Framework for Biomaterial Question Development
Title: PRISMA Workflow: Phase 1 and Its Sequential Role
The Scientist's Toolkit: Research Reagent Solutions for Biomaterial Characterization
Table 2: Essential Materials for Biomaterial Evaluation
| Item/Category | Example Product/Solution | Primary Function in Protocol |
|---|---|---|
| Cell Viability Assay | Cell Counting Kit-8 (CCK-8) or MTT Assay Kit | Quantifies metabolic activity of cells cultured on biomaterials, indicating biocompatibility. |
| Osteogenic Differentiation Media | Gibco StemPro Osteogenesis Differentiation Kit | Provides standardized supplements (ascorbate, β-glycerophosphate, dexamethasone) to induce and assess osteogenic response to materials. |
| qPCR Master Mix & Primers | TaqMan Fast Advanced Master Mix; predesigned primers for Runx2, OCN, COL1A1. | Quantifies expression of osteogenic marker genes from cells on biomaterials (ΔΔCt method). |
| ELISA Kits (Cytokines) | DuoSet ELISA for human/mouse/rat TNF-α, IL-1β, IL-6. | Measures concentration of inflammatory cytokines in culture supernatant or tissue homogenate to assess immune response. |
| Micro-CT Contrast Agent | Scanco Medical's contrast solutions or phosphotungstic acid (PTA). | Stains soft tissue or neo-formed bone in explants for enhanced 3D visualization and quantification of mineralization. |
| Histology Staining Kits | Masson's Trichrome Stain Kit; Alizarin Red S Solution. | Differentiates collagen/mineral (Trichrome) or visualizes calcium deposits (Alizarin Red) in tissue sections containing the biomaterial. |
| Mechanical Testing System | Instron 5944 with BioPuls Bath (example). | Measures tensile/compressive properties of hydrated biomaterial samples under physiologically relevant conditions. |
| Reference Biomaterial | BD Matrigel (for soft tissue) or Berkeley Advanced Biomaterials HA granules (for bone). | Serves as a standardized comparator or positive control in in vitro or in vivo experiments. |
Application Notes: Search Strategy Framework within a PRISMA-Compliant Biomaterials Review
A rigorous search strategy is foundational to any systematic review adhering to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. For biomaterials research—a field intersecting materials science, biology, and medicine—the search must be comprehensive, reproducible, and tailored to capture highly specialized literature. This phase involves the strategic selection of bibliographic databases, construction of a complex keyword syntax, and systematic retrieval of grey literature to minimize publication bias.
Database Selection Rationale
Biomaterials literature is fragmented across disciplinary databases. A single database is insufficient. The selected databases, summarized in Table 1, provide coverage of biomedical research (PubMed/MEDLINE, Embase), engineering (Inspec, Compendex), and multidisciplinary science (Web of Science, Scopus). Regional (CNKI, SciELO) and subject-specific databases (Polymer Library) are critical for grey literature and niche applications.
Table 1: Core and Specialized Databases for Biomaterials Systematic Reviews
| Database | Primary Focus | Key Advantage for Biomaterials | Access Model |
|---|---|---|---|
| PubMed/MEDLINE | Biomedicine & Life Sciences | Comprehensive coverage of in vivo studies, NIH-funded research. | Free |
| Embase | Biomedicine & Pharmacology | Extensive drug/device indexing with EMTREE thesaurus; strong European focus. | Subscription |
| Scopus | Multidisciplinary | Broad citation indexing; powerful analysis tools. | Subscription |
| Web of Science Core Collection | Multidisciplinary | High-impact journal coverage; robust citation tracking. | Subscription |
| IEEE Xplore | Engineering & Electronics | Essential for biosensors, conductive polymers, implantable devices. | Subscription |
| Compendex/Inspec | Engineering & Physics | Deep coverage of materials properties, synthesis, characterization. | Subscription |
| Cochrane Library | Clinical Trials | Central for controlled trial data on medical devices and implants. | Subscription |
| CNKI | Chinese Literature | Critical for capturing Chinese patent and journal literature. | Subscription |
| PolySearch2 (Platform) | Polymer Biomaterials | Aggregates polymer-specific data from multiple sources. | Free |
Keyword Development Protocol
The keyword strategy employs a modular, concept-based structure using Boolean operators (AND, OR, NOT), adjacency operators, and controlled vocabulary (MeSH, EMTREE).
Protocol 1: Developing a Biomaterials Search Syntax
- Define PICO Elements: For a sample question—"What is the efficacy of chitosan-based hydrogels for diabetic wound healing?"—define:
- Population: Diabetic wounds, ulcers.
- Intervention: Chitosan hydrogel, dressing.
- Comparison: Standard care, other biomaterials.
- Outcome: Wound closure rate, infection control.
- Brainstorm Synonym Clusters: For each PICO element, list all relevant synonyms, acronyms, spelling variants, and related terms.
- Incorporate Controlled Vocabulary: Identify corresponding MeSH terms (e.g., "Chitosan," "Hydrogels," "Diabetic Foot"). Use PubMed's MeSH Database.
- Apply Search Field Tags: Use tags like
[tiab](title/abstract) or[mh](MeSH heading) to increase precision. - Structure the Search String: Combine clusters with Boolean logic.
- Example:
(chitosan[tiab] OR "deacetylated chitin"[tiab]) AND (hydrogel*[tiab] OR dressing*[tiab] OR "tissue scaffold*"[tiab]) AND ("diabetic foot ulcer*"[tiab] OR "diabetic wound*"[tiab] OR "diabetic foot"[mh])
- Example:
- Iterative Testing: Run preliminary searches, review the first 50 results for relevance, and identify missed keywords from relevant article titles/abstracts. Refine syntax accordingly.
Grey Literature Retrieval Protocol
Grey literature (e.g., theses, patents, conference abstracts, regulatory documents) is essential for unbiased data. This protocol outlines a systematic approach.
Protocol 2: Systematic Retrieval of Biomaterials Grey Literature
- Identify Target Sources:
- Clinical Trial Registries: ClinicalTrials.gov, WHO ICTRP, EU Clinical Trials Register.
- Preprint Servers: bioRxiv, medRxiv, TechRxiv (for engineering).
- Theses & Dissertations: ProQuest Dissertations, EThOS, DART-Europe.
- Patents: Google Patents, USPTO, Espacenet, WIPO PATENTSCOPE.
- Conference Proceedings: Database filters (Web of Science, Scopus), society websites (SFB, TERMIS, ESB).
- Regulatory Agencies: FDA (MAUDE database, PMA reports), EMA, MHRA.
- Develop Grey Literature Search Strings: Adapt the core keyword syntax, simplifying for platforms without advanced operators. Focus on product names, material trade names, and broader intervention terms.
- Document Search Process: Record each source searched, date of search, exact search string used, and number of results retrieved. Use a standardized spreadsheet.
- Screening & Archiving: Screen titles/abstracts against eligibility criteria. Download and archive all potentially relevant full documents with a consistent naming convention (e.g.,
Source_AuthorYear_Title.pdf).
The Scientist's Toolkit: Research Reagent Solutions for Biomaterial Characterization
Table 2: Essential Reagents for In Vitro Biomaterial Characterization Assays
| Reagent / Kit Name | Primary Function in Biomaterials Research | Example Use-Case |
|---|---|---|
| AlamarBlue (Resazurin) | Cell viability and proliferation indicator. Measures metabolic activity via fluorescence/absorbance. | Quantifying osteoblast proliferation on a new bone scaffold over 14 days. |
| Live/Dead Viability/Cytotoxicity Kit (Calcein AM/EthD-1) | Fluorescent dual-staining for live (green) and dead (red) cells on material surfaces. | Assessing initial cell adhesion and membrane integrity on a hydrogel post-encapsulation. |
| Phalloidin (FITC/TRITC) | High-affinity actin filament stain. Visualizes cytoskeletal organization and cell spreading. | Evaluating fibroblast morphology and adhesion strength on a micropatterned polymer film. |
| Quant-iT PicoGreen dsDNA Assay Kit | Fluorescent quantitation of double-stranded DNA. Used as a proxy for cell number on scaffolds. | Measuring cellular ingrowth and proliferation within a 3D-printed scaffold over time. |
| Human Cytokine/Chemokine Magnetic Bead Panel | Multiplex immunoassay for quantifying secreted protein arrays (e.g., IL-6, TNF-α, VEGF). | Profiling macrophage (M1/M2) inflammatory response to a degradable implant material. |
| BCA Protein Assay Kit | Colorimetric detection and quantification of total protein concentration, often from lysates of cells on materials. | Normalizing alkaline phosphatase (ALP) activity data to total protein for osteogenic differentiation studies. |
| RNeasy Mini Kit (with on-column DNase digestion) | Isolation of high-quality total RNA from cells cultured on biomaterials (often challenging due to adhesion). | Extracting RNA for qPCR analysis of differentiation markers (e.g., Runx2, COL1A1) from cells on a scaffold. |
Visualizations
PRISMA Search Strategy Workflow
Biomaterial In Vitro Screening Protocol
Keyword Syntax Development Logic
Application Notes
Within systematic reviews of biomaterials, the Phase 3 eligibility screening is critical for defining the scope of evidence. This phase requires explicit, pre-defined criteria to handle the hierarchy of study types: from foundational in vitro experiments to clinical trials. The focus is on relevance to the PICO (Population, Intervention, Comparator, Outcome) framework, while ensuring methodological quality and direct applicability to the research question. For biomaterials, this often involves separate criteria streams for in vitro, animal (preclinical in vivo), and human (clinical) studies, acknowledging their distinct roles in the evidence chain. In vitro studies establish mechanistic plausibility, animal studies evaluate safety and efficacy in a complex system, and clinical studies provide direct human applicability. The criteria must filter studies based on biomaterial composition, intended application (e.g., orthopedic implant, drug delivery vehicle), and measured outcomes (e.g., cytotoxicity, osseointegration, inflammatory response). A common challenge is managing heterogeneous outcome reporting across study types.
Table 1: Typical Eligibility Thresholds for Biomaterial Studies
| Study Type | Minimum Sample/Replicate Threshold | Minimum Study Duration (Typical Range) | Key Quality Filter (Example) |
|---|---|---|---|
| In Vitro | n=3 independent experiments | 24 hours - 28 days (varies by assay) | Use of appropriate control groups (e.g., negative & material controls) |
| Animal (Preclinical) | n=5 per group (for large mammals, n may be lower) | 1 week - 52 weeks | Reporting of ethical approval (IACUC) and animal welfare statements |
| Clinical (Human) | No universal minimum; often n≥10 for pilot studies | Follow-up relevant to endpoint (e.g., 1 yr for implant fixation) | Study design (Randomized Controlled Trial preferred over case series) |
Experimental Protocols
Protocol 1: StandardizedIn VitroCytocompatibility Assessment (MTT Assay)
Purpose: To evaluate cell viability and proliferation in direct contact with a biomaterial extract or surface. Materials: Sterile biomaterial sample, cell line relevant to target tissue (e.g., MG-63 for bone), complete cell culture medium, MTT reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide), DMSO, 96-well tissue culture plate, CO2 incubator, microplate reader. Methodology:
- Sample Preparation: Prepare biomaterial extracts by incubating sterile material in culture medium at a defined surface area-to-volume ratio (e.g., 3 cm²/mL) for 24±2 h at 37°C. Use pure medium as a negative control.
- Cell Seeding: Seed cells in a 96-well plate at a density of 5x10³ to 1x10⁴ cells/well and incubate for 24 h to allow attachment.
- Exposure: Replace medium with 100 µL of biomaterial extract or control. Include wells with medium only (background control). Incubate for a predetermined period (e.g., 24, 48, 72 h).
- MTT Incubation: Add 10 µL of MTT solution (5 mg/mL in PBS) to each well. Incubate for 4 h at 37°C.
- Solubilization: Carefully remove the medium. Add 100 µL of DMSO to each well to dissolve the formazan crystals.
- Measurement: Shake the plate gently for 10 minutes. Measure the absorbance at 570 nm with a reference filter of 650 nm using a microplate reader.
- Analysis: Calculate relative cell viability (%) = [(Abssample - Absbackground) / (Absnegativecontrol - Abs_background)] x 100. Data from at least three independent experiments (n=3) with multiple replicates each are required for inclusion.
Protocol 2: PreclinicalIn VivoOsseointegration Model (Rodent Femur Implant)
Purpose: To assess bone bonding and integration of an orthopedic biomaterial in vivo. Materials: Sterile test and control implants (e.g., titanium vs. novel coating), adult Sprague-Dawley rats, surgical tools, stereotaxic drill, anesthesia, analgesic, bone cement, micro-CT scanner, histology supplies. Methodology:
- Surgical Implantation: Anesthetize the animal. Make a lateral skin incision over the distal femur. Carefully separate muscle to expose the bone surface.
- Osteotomy: Drill a bicortical defect of a diameter matching the implant (e.g., 1.5 mm) using slow speed with saline irrigation.
- Implantation: Press-fit the sterile test or control implant into the defect. Ensure the implant is flush with the cortical bone surface.
- Closure: Suture the muscle fascia and skin layers in sequence. Administer postoperative analgesics.
- Termination & Analysis: Euthanize animals at predetermined endpoints (e.g., 4 and 12 weeks). Harvest femurs.
- Micro-CT: Scan explants to quantify bone volume/total volume (BV/TV) and bone-implant contact (BIC) within a defined region of interest.
- Histomorphometry: Process undecalcified bone sections (e.g., stained with Toluidine Blue) to visually assess osseointegration and measure BIC. Inclusion Criterion: Studies must report a defined primary outcome (e.g., BIC %), use a concurrent control group, and state approval by an Institutional Animal Care and Use Committee.
Signaling Pathway & Workflow Diagrams
Title: Phase 3 Eligibility Criteria Decision Workflow
Title: Host Response Pathway to Biomaterial Implant
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions for Biomaterial Testing
| Item | Function in Experiment |
|---|---|
| AlamarBlue / MTT / WST-1 Assay Kits | Colorimetric or fluorometric assays to quantify cell viability, proliferation, and cytotoxicity in response to biomaterials. |
| ELISA Kits (e.g., for TNF-α, IL-6, IL-10) | Quantify specific inflammatory or anti-inflammatory cytokines released by cells in culture or from tissue homogenates. |
| Osteogenic Differentiation Media | A defined cocktail (ascorbic acid, β-glycerophosphate, dexamethasone) to induce stem cell differentiation into osteoblasts for bone biomaterial testing. |
| Live/Dead Cell Staining Kit (Calcein-AM/EthD-1) | Provides a fluorescent visual assay where live cells stain green and dead cells stain red, used for direct surface biocompatibility assessment. |
| Simulated Body Fluid (SBF) | An ion solution with inorganic ion concentrations similar to human blood plasma, used to assess the bioactivity and apatite-forming ability of materials in vitro. |
| Matrigel Basement Membrane Matrix | Used for 3D cell culture models to study cell-material interactions in a more physiologically relevant, tissue-like environment. |
Application Notes
This document provides a standardized template and protocols for the Data Extraction phase (Phase 4) of a systematic review conducted according to PRISMA guidelines, specifically tailored for biomaterials research. Its purpose is to ensure consistent, reproducible, and comprehensive capture of quantitative and qualitative data from primary studies, enabling rigorous synthesis and meta-analysis. Effective use of this template mitigates reviewer bias and is critical for assessing the relationship between biomaterial properties (e.g., composition, topography, mechanics), in vitro and in vivo performance, and biocompatibility outcomes.
Protocol for Data Extraction
1. Pre-Extraction Calibration
- Objective: Ensure inter-reviewer reliability.
- Method: All reviewers independently extract data from the same 3-5 included studies using the template. Calculate inter-rater agreement (e.g., Cohen's kappa). Resolve discrepancies through discussion until a consensus kappa >0.8 is achieved.
2. Extraction Procedure
- Tool: Use a predefined spreadsheet or data management software (e.g., Covidence, Rayyan).
- Process: For each included study, one reviewer performs extraction. A second reviewer verifies the extracted data against the original article. Disagreements are resolved by a third senior reviewer.
- Items: Extract data for all relevant fields, even if reported as "not reported" (NR).
3. Data Points for Extraction Extract the following core elements, summarized in Table 1.
Table 1: Core Data Extraction Fields for Biomaterial Systematic Reviews
| Category | Data Field | Description/Unit | Example Entry |
|---|---|---|---|
| Study ID | Citation, Author, Year | Unique study identifier | Smith et al., 2023 |
| Biomaterial | Core Composition | Primary material class | Poly(lactic-co-glycolic acid) |
| Key Properties | Surface roughness (µm), Modulus (MPa), Degradation rate (%/week) | Ra=1.5, E=2.4, 5%/week | |
| Fabrication Method | Technique used | Electrospinning, Solvent Casting | |
| Study Model | In Vitro Cell Type | Species & cell line | Human Mesenchymal Stem Cells (hMSCs) |
| In Vivo Model | Species, anatomical site | Sprague-Dawley rat, subcutaneous | |
| Control Group Description | Description of comparator | Medical-grade silicone | |
| Performance | Mechanical Output | Tensile strength (MPa), Adhesion strength (kPa) | 15.2 MPa, 45 kPa |
| Drug Release Kinetics | Cumulative release (% , time) | 80% at 168 hours | |
| Biocompatibility | Cytotoxicity (ISO 10993-5) | Cell viability (%) vs. control | 98 ± 5% |
| Inflammatory Response (In Vivo) | Cell count/area for CD68+ cells | 120 ± 30 cells/mm² | |
| Histological Scoring | Semi-quantitative score (e.g., 0-4) | Fibrosis score: 1 | |
| Outcomes | Key Findings | Primary conclusion of study | "The scaffold supported significant new bone formation at 12 weeks." |
| Risk of Bias (RoB) | Domain-based judgment (Low/High/Unclear) | Selection bias: Low |
4. Handling Missing and Unclear Data
- Contact the corresponding author of the primary study via email to request missing data.
- If no response is received within two weeks, record the data point as "Not Available (NA)" and note the attempt.
- Do not extrapolate or estimate unreported data.
Detailed Experimental Protocols for Cited Methods
Protocol A: In Vitro Cytotoxicity Assay (AlamarBlue/Resazurin)
- Objective: Quantify cell metabolic activity per ISO 10993-5.
- Materials: Cell culture, test biomaterial extract or direct contact setup, AlamarBlue reagent, cell culture medium, 96-well plate, spectrophotometer/fluorometer.
- Procedure:
- Prepare biomaterial extracts by incubating sterile material in culture medium at 37°C for 24h at a recommended surface area-to-volume ratio (e.g., 3 cm²/mL).
- Seed cells in 96-well plates at a defined density (e.g., 10,000 cells/well) and incubate for 24h.
- Replace medium with 100µL of test extract, negative control (medium), or positive control (e.g., 1% Triton X-100).
- Incubate for 24-72h.
- Add AlamarBlue reagent (10% v/v) to each well. Incubate for 2-4h protected from light.
- Measure fluorescence (Excitation 530-560nm, Emission 590nm) or absorbance (570nm & 600nm).
- Calculate percentage viability relative to negative control.
Protocol B: In Vivo Histomorphometric Analysis for Fibrosis
- Objective: Quantify fibrous capsule thickness around an implanted biomaterial.
- Materials: Explanted tissue with implant site, 10% neutral buffered formalin, paraffin, microtome, Hematoxylin & Eosin (H&E) stain, light microscope, image analysis software.
- Procedure:
- Fix explanted tissue in formalin for 48h. Process and embed in paraffin.
- Section tissue to 5µm thickness through the implant site.
- Stain sections with H&E using standard protocols.
- Image stained sections under a light microscope at 100-200x magnification.
- Using image analysis software, measure the perpendicular distance from the implant surface to the outer edge of the dense, collagen-rich fibrous capsule at 8-12 uniformly spaced points around the implant circumference.
- Calculate the average and standard deviation of the fibrous capsule thickness for each sample.
Visualization: Systematic Review Workflow
Title: Systematic Review Data Extraction Workflow
The Scientist's Toolkit: Key Reagents for Biomaterial Biocompatibility Testing
| Item | Function in Research |
|---|---|
| AlamarBlue (Resazurin) | Cell-permeant blue dye reduced to fluorescent pink resorufin by metabolically active cells, serving as an indicator of cytotoxicity. |
| Live/Dead Viability/Cytotoxicity Kit | Contains calcein AM (esterase activity stains live cells green) and ethidium homodimer-1 (binds DNA of dead cells with damaged membranes, stains red). |
| CD68 Primary Antibody | Immunohistochemistry marker for identifying macrophages and monocytes in tissue sections to assess the foreign body response. |
| ELISA Kits (e.g., for TNF-α, IL-1β, IL-6) | Quantify concentrations of specific pro-inflammatory cytokines in cell culture supernatant or serum to measure immune activation. |
| Collagen Type I Antibody (Sirius Red Stain) | Used to identify and quantify collagen deposition (fibrosis) around implants in histological sections. |
| ISO 10993-12 Reference Materials | Standardized polyethylene and silicone samples used as negative controls for biocompatibility tests per international standards. |
| Phalloidin (FITC/TRITC conjugate) | Binds filamentous actin (F-actin), allowing visualization of cell morphology and cytoskeletal organization on biomaterial surfaces. |
| CCK-8 Assay Kit | Utilizes a water-soluble tetrazolium salt reduced by cellular dehydrogenases to a colored formazan, quantifying cell proliferation/viability. |
Within the systematic review framework guided by PRISMA, the Phase 5 critical appraisal of individual study quality is paramount. For preclinical in vivo biomaterials research, generic tools are inadequate due to field-specific biases. This necessitates specialized tools like SYRCLE's RoB tool and the QUIN tool to ensure robust, translatable conclusions.
Table 1: Comparative Analysis of Key Risk of Bias Assessment Tools for Preclinical Biomaterials Studies
| Tool (Acronym) | Full Name & Primary Focus | Domains/Items Assessed | Scoring/Judgment | Key Application Context |
|---|---|---|---|---|
| SYRCLE's RoB | SYstematic Review Centre for Laboratory animal Experimentation Risk of Bias tool. Adapted from Cochrane RoB for animal intervention studies. | 10 domains: Sequence generation, Baseline characteristics, Allocation concealment, Random housing, Blinding (performance), Random outcome assessment, Blinding (detection), Incomplete outcome data, Selective outcome reporting, Other bias. | Judgment: 'Low', 'High', or 'Unclear' risk of bias for each domain. | Gold standard for in vivo therapeutic efficacy and safety studies of biomaterials (e.g., bone regeneration, drug-eluting implants). |
| QUIN | Quality In Non-randomized Studies - Biomaterials. Adapted from QUIN for non-randomized surgical/biomaterials studies. | 12 items: Study objectives, Animal model, Biomaterial characterization, Allocation, Blinding, Outcome assessment, Statistical methods, Results, Conclusions, Conflict of interest, Regulatory. | Scoring: Each item scored 0, 1, or 2. Total score (max 24) categorized as High (>16), Moderate (10-16), or Low (<10) quality. | Ideal for comparative, often non-randomized, biomaterial implantation studies (e.g., comparing new material to a standard). |
| CAMARADES | Collaborative Approach to Meta-Analysis and Critical Approaisal of Research in Experimental Studies. A checklist, often used with SYRCLE. | 10-15 items: Peer review, Statement of control, Randomization, Blinding, etc. Often includes study design quality items beyond internal validity. | Tally of items reported. Higher score indicates more items reported (study quality). | Frequently used in stroke/cerebral ischemia research; applicable for composite outcome studies in biomaterials (e.g., neuroregeneration scaffolds). |
Detailed Application Protocols
Protocol 1: Applying SYRCLE's RoB Tool to a Biomaterial Bone Regeneration Study
- Objective: To assess the internal validity of a study investigating a novel hydrogel for critical-size bone defect repair in rodents.
- Materials: Study manuscript(s), SYRCLE's RoB checklist, data extraction sheet.
- Workflow:
- Domain 1-3 (Selection Bias): Examine Methods section. Determine if animal allocation to "hydrogel" vs. "empty defect" groups used random sequence generation (e.g., random number table) and was concealed from the surgeon (e.g., sealed opaque envelopes). Check if baseline characteristics (weight, age) were similar.
- Domain 4-7 (Performance & Detection Bias): Assess if caregivers/surgeons were blinded to group identity (blinding of caregivers and participants). Determine if animals were randomly housed. Critically, assess if outcome assessors (e.g., histologist, radiologist measuring bone volume) were blinded.
- Domain 8-9 (Attrition & Reporting Bias): Compare number of animals at start vs. end per group. Account for all dropouts. Compare outcomes in Methods vs. Results to identify unreported measures.
- Domain 10 (Other Bias): Identify any protocol-specific issues (e.g., unequal surgical experience between groups, inappropriate control material).
- Judgment: For each domain, assign 'Low' (plausible bias unlikely to alter results), 'High' (plausible bias that seriously weakens confidence), or 'Unclear' (insufficient information) risk. Document supporting text.
- Data Synthesis: Present findings as a risk of bias summary figure (graphical) and table in the systematic review.
Protocol 2: Applying the QUIN Tool to a Biomaterial Implantation Study
- Objective: To quantitatively assess the methodological quality of a non-randomized study comparing a novel polymer vascular graft to a commercially available PTFE graft.
- Materials: Study manuscript(s), QUIN tool scoring sheet.
- Workflow:
- Item 1-3 (Introduction & Methods): Score study objective clarity (2=clear), animal model justification (2=appropriate species, disease model), and biomaterial characterization (2=comprehensive physicochemical characterization provided).
- Item 4-6 (Bias Minimization): Evaluate allocation method (2=random, 1=systematic, 0=haphazard), blinding (2=double-blinded, 1=single, 0=none), and objective outcome assessment (2=quantitative, blinded).
- Item 7-10 (Results & Analysis): Assess appropriate statistical methods, clear results reporting, consistent conclusions, and declared conflicts of interest.
- Item 11-12 (Ethics): Confirm ethical approval and regulatory compliance (e.g., ISO standards for material).
- Scoring: Sum scores across all 12 items. Categorize final score.
- Data Synthesis: Report individual item scores and total score per study. Use scores for sensitivity analysis (e.g., excluding low-quality studies).
Visualization of Assessment Workflows
SYRCLE's RoB Tool Assessment Workflow
QUIN Tool Scoring and Categorization Logic
Table 2: Key Research Reagent Solutions for Methodological Quality Assessment
| Resource Name / Tool | Type | Primary Function in Risk of Bias Assessment |
|---|---|---|
| SYRCLE's RoB Tool Checklist | Digital/Paper Form | Structured guide to assess 10 critical internal validity domains for animal studies. |
| QUIN Tool Scoring Sheet | Digital/Paper Form | Standardized worksheet to score 12 items assessing comprehensive study quality. |
| Rayyan QCRI | Web/Mobile Application | AI-powered systematic review platform to facilitate blinding during initial screening and data extraction. |
| Covidence | Web-based Software | Streamlines full systematic review process, including dedicated modules for risk of bias assessment with custom forms. |
| Risk of Bias Visualization Tool (Robvis) | R Package / Web App | Generates publication-standard summary and traffic light plots for RoB assessments (compatible with SYRCLE). |
| ARRIVE 2.0 Guidelines | Reporting Checklist | Used proactively to appraise completeness of reporting, which underpins accurate RoB judgment. |
Within the PRISMA-guided systematic review framework for biomaterials research, Phase 6 addresses the critical challenge of data synthesis. This phase determines whether quantitative meta-analysis can statistically combine results from disparate studies or if narrative synthesis is required due to insurmountable heterogeneity in materials, outcomes, or experimental design.
Criteria for Meta-Analysis Feasibility Assessment
Prerequisites for Quantitative Synthesis
A meta-analysis is considered feasible when the following conditions are met:
- Comparable Interventions: Biomaterial scaffolds or implants share core compositional or structural similarities (e.g., "hydroxyapatite-coated titanium").
- Homogeneous Outcomes: Studies report the same quantitative endpoint (e.g., bone-implant contact (BIC) percentage measured histomorphometrically).
- Consistent Study Designs: Predominantly randomized controlled trials (RCTs) or controlled animal studies with low risk of bias.
- Available Statistical Data: Means, standard deviations, and sample sizes are reported or obtainable.
Indicators for Narrative Synthesis
A narrative synthesis is mandated when:
- Clinical vs. Preclinical Mix: Combining data from human trials and animal models is typically inappropriate.
- Outcome Heterogeneity: Studies measure success via disparate metrics (e.g., tensile strength, protein adsorption, cell viability, in vivo inflammation score).
- Material Diversity: Included studies investigate fundamentally different material classes (e.g., comparing synthetic polymer degradation to metallic ion release).
- High Methodological Heterogeneity (I² > 75%): Statistical tests indicate overwhelming variability not attributable to chance.
Table 1: Common Biomaterial Outcomes and Synthesis Feasibility
| Outcome Domain | Specific Metric | Typical Scale/Units | Feasibility of Meta-Analysis | Common Heterogeneity Source |
|---|---|---|---|---|
| Biocompatibility | Cell Viability | % vs. Control | High (if assay is consistent, e.g., MTT) | Assay type (MTT vs. AlamarBlue vs. direct count) |
| Osseointegration | Bone-Implant Contact (BIC) | Percentage (%) | Moderate to High | Measurement method (histology vs. micro-CT) |
| Mechanical | Tensile/Compressive Strength | Megapascals (MPa) | Moderate | Testing protocol (ISO vs. ASTM standards) |
| Degradation | Mass Loss | Percentage (%) / mm/year | Low to Moderate | Degradation medium (SBF vs. in vivo) |
| Antimicrobial | Zone of Inhibition | Millimeters (mm) | Low | Bacterial strain, inoculum concentration |
Table 2: Statistical Heterogeneity Thresholds (Cochrane Guidelines)
| I² Statistic Value | Heterogeneity Level | Recommended Action for Synthesis |
|---|---|---|
| 0% to 40% | Might not be important | Meta-analysis with fixed-effect model may be appropriate. |
| 30% to 60% | Moderate heterogeneity | Meta-analysis with random-effects model is preferred. |
| 50% to 90% | Substantial heterogeneity | Random-effects model. Sources of heterogeneity must be investigated. |
| 75% to 100% | Considerable heterogeneity | Meta-analysis may be misleading. Narrative synthesis is strongly advised. |
Experimental Protocols for Data Extraction and Harmonization
Protocol 4.1: Standardized Data Extraction for Biomaterial Properties
Objective: To uniformly extract quantitative data from heterogeneous biomaterials studies to assess synthesis feasibility. Materials: PRISMA item checklist, data extraction form (electronic spreadsheet), statistical software (RevMan, R). Procedure:
- For each included study, create a unique record in the extraction spreadsheet.
- Extract descriptive data: biomaterial class, fabrication method, model system (cell line, animal species), study design.
- Extract quantitative data for each relevant outcome:
- For continuous data (e.g., strength, BIC%): Record mean, standard deviation (SD), and sample size (n) for both test and control groups.
- If SD is missing, calculate from standard error, confidence intervals, or p-values using Cochrane formulae.
- If only graphical data is present, use digitization software (e.g., WebPlotDigitizer) to extract values.
- Code all data according to a predefined scheme (e.g., material type: 1=polymer, 2=ceramic, 3=composite).
- A second reviewer must independently verify all extractions. Discrepancies are resolved by consensus.
Protocol 4.2: Subgroup Analysis Protocol for Heterogeneous Data
Objective: To explore sources of heterogeneity when I² > 50% to determine if meta-analysis within subgroups is feasible. Procedure:
- Define Subgroups A Priori: Based on the review question, define potential subgroups before analysis (e.g., animal model [rat vs. rabbit], implant geometry, follow-up time [≤12 weeks vs. >12 weeks]).
- Perform Separate Meta-Analyses: Conduct a distinct random-effects meta-analysis for each subgroup.
- Compare Between Subgroups: Use a formal statistical test (e.g., Cochrane's Q-test for subgroup differences) to determine if effect sizes differ significantly between subgroups.
- Interpretation: If subgroups show homogeneous results internally (low I²) and differ from each other, present subgroup analyses as primary findings. If heterogeneity remains high within all subgroups, abandon quantitative synthesis.
Visualizing Synthesis Decision Pathways
Synthesis Feasibility Decision Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Data Synthesis in Biomaterials Reviews
| Item / Solution | Function in Synthesis Phase | Example Vendor/Software |
|---|---|---|
| Covidence / Rayyan | Web-based tool for screening and data extraction with conflict resolution. | Covidence.org, Rayyan.ai |
| RevMan (Review Manager) | Cochrane's official software for conducting meta-analyses and generating forest plots. | Cochrane Training |
| R with 'metafor'/'meta' packages | Advanced statistical environment for complex meta-analysis, meta-regression, and plotting. | CRAN Repository |
| GRADEpro GDT | Tool to create 'Summary of Findings' tables and assess certainty of evidence (GRADE). | gradepro.org |
| WebPlotDigitizer | Semi-automated tool to extract numerical data from published graphs and charts. | automeris.io |
| PRISMA 2020 Checklist & Flow Diagram | Ensures transparent and complete reporting of the review process. | prisma-statement.org |
| JBI SUMARI | Suite for critical appraisal, data extraction, and synthesis of various study types. | Joanna Briggs Institute |
| DistillerSR | Enterprise-level platform for managing the entire systematic review lifecycle. | Evidence Partners |
Application Notes
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram is an essential visual tool that provides a transparent account of the study selection process in a systematic review. In the context of biomaterials research, where the volume of literature from diverse databases (e.g., PubMed, Scopus, Web of Science, EMBASE, Cochrane Central) is substantial, accurately documenting the screening process is critical for reproducibility and rigor. The diagram explicitly maps the flow of records from identification to inclusion, highlighting the reasons for exclusion at each stage. This documentation is a cornerstone of the PRISMA 2020 statement, which emphasizes detailed reporting to minimize bias and allow for the assessment of the review's comprehensiveness.
For a thesis on PRISMA guidelines in biomaterials systematic reviews, completing the flow diagram is not merely an administrative task. It represents the methodological backbone, demonstrating the systematicity of the search and the application of predefined, biomaterial-specific eligibility criteria (e.g., in-vivo model, material composition, outcome measures). Proper documentation here directly impacts the validity of the synthesis and conclusions regarding material efficacy, biocompatibility, or safety.
Protocols
Protocol 1: Record Identification and Collation
Objective: To systematically gather all potentially relevant records from selected databases and other sources without duplication.
- Search Execution: Run the final, peer-reviewed search strategy simultaneously across all selected bibliographic databases. Record the exact date of search for each database.
- Export Records: Export all retrieved records (titles and abstracts) from each database into a compatible format (e.g., .ris, .nbib, .csv).
- Import to Reference Manager: Import all files into a systematic review reference management software (e.g., Covidence, Rayyan, EndNote).
- Automatic Deduplication: Use the software's duplicate identification function. Common algorithms match records based on title, author, year, and DOI.
- Manual Deduplication Check: Manually inspect a sample of automatically retained records to verify deduplication accuracy, especially for records with minor formatting differences.
Objective: To apply eligibility criteria to the title and abstract of each unique record.
- Pilot Screening: Two independent reviewers screen a common batch of 50-100 records using the eligibility criteria. Calculate inter-rater reliability (e.g., Cohen's kappa). Resolve discrepancies and refine criteria as needed until agreement is substantial (kappa > 0.6).
- Dual-Independent Screening: Two reviewers independently assess each record as "Include," "Exclude," or "Maybe." The software conceals the other reviewer's decision.
- Conflict Resolution: The software automatically flags records with conflicting decisions. These conflicts are resolved through discussion between the two reviewers. If consensus cannot be reached, a third senior reviewer adjudicates.
- Documentation: The software tracks the number of records included and excluded at this stage. The most common reasons for exclusion (e.g., wrong population, wrong intervention, not a primary study) are noted.
Protocol 3: Full-Text Screening and Final Inclusion
Objective: To retrieve and assess the full text of all records that passed the title/abstract screening.
- Retrieval: Locate and obtain the full-text document for each potentially eligible record. Document sources (e.g., institutional subscription, author contact, inter-library loan) and any records that cannot be retrieved.
- Dual-Independent Assessment: Two reviewers independently assess each full-text article against the eligibility criteria. Decisions are "Include" or "Exclude," with a specific, pre-coded reason for each exclusion.
- Final Resolution: All conflicts are resolved by consensus or third-party adjudication.
- Flow Diagram Population: The numbers from this stage—particularly the precise counts and reasons for exclusion—are used to complete the final sections of the PRISMA flow diagram.
Data Presentation
Table 1: Quantitative Screening Data from a Model Biomaterials Systematic Review
| Screening Stage | Number of Records | Action | Next Stage / Reason for Exclusion |
|---|---|---|---|
| Identification | |||
| Databases (PubMed, Scopus, etc.) | 2,450 | Records identified | To Screening |
| Registers/Other Sources | 35 | Records identified | To Screening |
| Screening | |||
| Records after duplicates removed | 1,925 | Duplicates removed | 566 |
| Titles & Abstracts Screened | 1,925 | Records screened | |
| Records Excluded | 1,740 | Excluded | Wrong material (850), In-vitro only (562), Review article (328) |
| Eligibility | |||
| Full-Text Articles Assessed | 185 | Full-text sought for retrieval | |
| Full-Text Not Retrieved | 5 | Not retrieved | Unavailable (5) |
| Full-Text Assessed | 180 | Full-text assessed for eligibility | |
| Full-Text Excluded | 135 | Excluded | Wrong outcome (65), Study duration < 6 months (42), Incomplete data (28) |
| Included | |||
| Studies in Qualitative Synthesis | 45 | Included in review | |
| Studies in Quantitative Synthesis (Meta-analysis) | 38 | Included in meta-analysis | 7 studies lacked comparable data |
Visualizations
PRISMA 2020 Flow Diagram for Study Selection
Dual-Reviewer Screening and Conflict Resolution Protocol
The Scientist's Toolkit
Table 2: Research Reagent Solutions for PRISMA Flow Documentation
| Item | Function in PRISMA Flow Process |
|---|---|
| Reference Management Software (Covidence, Rayyan) | Web-based platforms designed for systematic reviews. They automate deduplication, facilitate blind dual screening, manage conflicts, and export screening data directly into PRISMA flow templates. |
| Bibliographic Database APIs | Application Programming Interfaces (e.g., from PubMed, IEEE Xplore) allow for reproducible, programmable execution of search strategies and batch export of records, ensuring an auditable trail. |
| PRISMA 2020 Flow Diagram Template (Word/PPT) | The official, editable template from the PRISMA website provides the standardized structure to report the numbers from each stage of the review. |
| Inter-Rater Reliability Calculator (e.g., SPSS, online kappa calculator) | Tools to quantitatively assess the agreement between reviewers during the pilot screening phase, ensuring consistency before full screening begins. |
| Document Retrieval Tools (Library subscriptions, Unpaywall, ResearchGate) | Essential services for obtaining the full text of articles identified during screening, including those not openly available. |
| Data Extraction & Synthesis Software (RevMan, JBI SUMARI, DistillerSR) | Advanced tools that integrate with screening modules and provide structured forms for data extraction from included studies, feeding directly into meta-analysis and synthesis. |
Overcoming Common Pitfalls: PRISMA for Complex Biomaterials Data
Application Notes: Standardization for Systematic Review
The high heterogeneity in fabrication and characterization methods presents a fundamental challenge for conducting systematic reviews and meta-analyses in the biomaterials field, as mandated by PRISMA guidelines. This variability obscures meaningful comparisons between studies, limiting the synthesis of robust, evidence-based conclusions. These Application Notes provide a structured framework to deconstruct, categorize, and standardize reporting to enhance the utility of primary research for systematic review.
Table 1: Quantifying Methodological Heterogeneity in Key Biomaterial Classes
| Biomaterial Class | Common Fabrication Techniques (No. of Variants Reported) | Key Characterization Methods (No. of Metrics Used) | Reported Range of a Critical Property (e.g., Elastic Modulus) |
|---|---|---|---|
| Polymeric Hydrogels | Free-radical polymerization (12), Ionic crosslinking (8), Thermal gelation (6), Enzymatic crosslinking (5) | Swelling ratio (100%), Rheology (92%), FTIR (85%), SEM (78%) | 0.1 kPa - 2.0 MPa |
| Calcium Phosphate Ceramics | Wet precipitation (10), Sintering (8), Sol-gel (7), 3D printing (6) | XRD (98%), SEM/EDS (95%), Porosity measurement (88%), Compression testing (85%) | 0.5 GPa - 12 GPa (Dense) |
| Decellularized Extracellular Matrix | Chemical detergents (9), Enzymatic treatment (7), Physical methods (5), Combinatorial protocols (15+) | DNA quantification (100%), Histology (95%), GAG assay (90%), Tensile testing (60%) | Ultimate Tensile Strength: 0.1 - 15 MPa |
Detailed Experimental Protocols
Protocol 1: Standardized Hydrogel Fabrication & Mechanical Characterization
Aim: To generate reproducible, characterizable polyethylene glycol diacrylate (PEGDA) hydrogels. Materials: PEGDA (MW 700 Da), Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) photoinitiator, Dulbecco's Phosphate Buffered Saline (DPBS).
- Solution Preparation: Dissolve LAP in DPBS at 2.5 mM concentration. Add PEGDA monomer to achieve target concentration (e.g., 10% w/v). Vortex for 30 seconds until fully mixed. Protect from light.
- Molding & Crosslinking: Pipette 100 µL of precursor solution into cylindrical silicone molds (Ø8mm x 2mm). Expose to 365 nm UV light (10 mW/cm²) for 60 seconds at room temperature.
- Equilibration: Gently extract hydrogels and submerge in 5 mL DPBS for 24 hours at 4°C to equilibrate swelling.
- Unconfined Compression Testing: a. Blot hydrogel surface lightly with lint-free wipe. b. Place on rheometer or universal testing machine plate pre-moistened with PBS. c. Apply a pre-load of 0.001 N. d. Compress at a constant strain rate of 1% per second until 30% strain is achieved. e. Record force-displacement data. Calculate compressive modulus from the linear elastic region (typically 5-15% strain).
Protocol 2: Standardized Characterization of Decellularization Efficiency
Aim: To quantitatively assess the removal of cellular material from tissue-derived scaffolds. Materials: Decellularized tissue, DNA extraction kit, Picogreen dsDNA assay reagents, Papain digestion solution.
- Sample Digestion: Weigh 10 mg of lyophilized, decellularized tissue. Digest in 500 µL of papain solution (125 µg/mL in 0.1M phosphate buffer, 5 mM cysteine, 5 mM EDTA, pH 6.5) at 60°C for 18 hours.
- DNA Extraction: Follow manufacturer protocol for a spin-column-based DNA extraction kit. Elute DNA in 50 µL of elution buffer.
- Quantification: Prepare a standard curve (0-1000 ng/mL) using supplied lambda DNA. Mix 50 µL of each standard/sample with 50 µL of Picogreen working solution in a black 96-well plate. Incubate for 5 minutes, protected from light.
- Measurement: Read fluorescence (excitation 480 nm, emission 520 nm). Calculate DNA concentration in the original sample (ng/mg dry tissue weight). Report mean ± SD for n≥3 biological replicates.
Visualizations
Title: Biomaterial Characterization Workflow for Reviews
Title: Causes and Consequence of Method Heterogeneity
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Standardization | Example Product/Catalog |
|---|---|---|
| Certified Reference Materials (CRMs) | Provides a benchmark with known properties (e.g., modulus, surface energy) to calibrate and validate characterization equipment across different labs. | NIST Standard Reference Material 2910 (Calcium Phosphate) |
| Synthetically Defined Polymer | Eliminates batch-to-batch variability inherent in natural polymers. Enables precise control over MW, dispersity, and functional group density. | PEGDA, 700 Da, >95% purity (Sigma 701963) |
| Photoinitiator with Known Molar Absorptivity | Ensures reproducible crosslinking kinetics and depth by providing consistent free radical generation under specified UV wavelength and intensity. | Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) |
| Fluorometric DNA Quantitation Assay | Highly sensitive, specific, and quantitative method for assessing decellularization efficiency, superior to spectrophotometric A260 methods. | Quant-iT PicoGreen dsDNA Assay Kit (Invitrogen P11496) |
| Standardized Cell Lines | Reduces variability in biological characterization (e.g., cytocompatibility). Use of authenticated, low-passage cells from repositories is critical. | hMSCs (ATCC PCS-500-012), MC3T3-E1 (ATCC CRL-2593) |
| Rheometer with Environmental Chamber | Allows mechanical characterization under physiologically relevant conditions (37°C, humidified) to prevent artifact from sample drying. | TA Instruments DHR series with Peltier plate. |
Within systematic reviews of biomaterials, adhering to PRISMA guidelines is paramount for ensuring transparency and reproducibility. A central challenge in this process is the management of poorly reported primary studies and missing data, which can introduce bias and limit the validity of meta-analyses. This Application Note provides detailed protocols for identifying, managing, and mitigating these issues, ensuring robust synthesis within a biomaterials research context.
Identification and Classification of Reporting Deficiencies
The first step involves systematically screening included studies for deficiencies. Common issues in biomaterials studies include missing standard deviations, unclear animal model characteristics (e.g., age, sex), incomplete biomaterial characterization data (e.g., porosity, degradation rate), and unreported conflict of interest statements.
Table 1: Common Reporting Deficiencies in Biomaterials Studies and Their Impact
| Deficiency Category | Specific Example | Impact on Review |
|---|---|---|
| Outcome Data | Missing standard deviation (SD) for mechanical strength. | Precludes inclusion in meta-analysis; may lead to selective outcome reporting bias. |
| Methodological Detail | Unclear sterilization method or implantation site. | Limits assessment of reproducibility and translational potential. |
| Biomaterial Characterization | Absent data on surface roughness or chemical composition. | Hinders understanding of structure-function relationships across studies. |
| Experimental Model | Unreported animal age, weight, or genetic background. | Impairs assessment of generalizability and introduces potential confounding. |
| Conflict of Interest | Unreported industry sponsorship. | Limits assessment of potential for funding bias. |
Protocols for Handling Missing Data
Protocol: Contacting Corresponding Authors
Objective: To obtain missing or unclear data directly from the original study investigators. Materials: Email database, standardized request template. Methodology:
- Identify the precise data points required (e.g., specific mean, SD, n per group).
- Locate current contact information for the corresponding author.
- Draft a concise, polite email using a standardized template. Include the full citation of the paper, a clear list of requested data, and the reason for the request (systematic review for PRISMA compliance).
- Send the initial request and log the date. If no response is received within 14 days, send one polite follow-up email.
- Document all responses (positive or negative) in a tracking log. Studies where data is provided can be upgraded in the quality assessment.
Protocol: Data Imputation and Statistical Handling
Objective: To quantitatively manage missing summary statistics (e.g., standard deviations) when author contact fails. Materials: Statistical software (R, STATA, RevMan), complete data from other included studies. Methodology for Missing Standard Deviations:
- Identify Potential Sources: If multiple studies use the same, highly standardized biomaterial (e.g., a specific commercial titanium alloy) and test method (e.g., ASTM F1044 shear strength), pool the SDs from the reported studies.
- Calculate Imputed SD: Use the largest pooled SD from other studies in the review as a conservative estimate. Alternatively, if correlations from baseline to follow-up are known or can be assumed, estimate the missing SD using the formula: SD = SE × √n or from p-values and group sizes.
- Perform Sensitivity Analysis: Conduct the meta-analysis twice: once with imputed data and once excluding studies with imputed data. Report both results and discuss the impact of imputation on the pooled effect size and heterogeneity (I²).
- Documentation: Clearly report in the manuscript which studies had imputed data, the method used, and the results of the sensitivity analysis.
Table 2: Methods for Handling Missing Quantitative Data
| Method | Description | When to Use | Key Consideration |
|---|---|---|---|
| Author Contact | Direct request for missing data. | First-line approach for all critical missing data. | Low response rate (~50%); requires time. |
| Imputation via Pooled SD | Using SD from other similar studies. | When several studies use identical methods/materials. | Increases confidence in imputed value. |
| Imputation via Range | Estimating SD from reported range (Range/4 or Range/6 for n). | When only data range is reported. | Less reliable; use only as last resort. |
| Exclusion | Omitting the study from quantitative synthesis. | When data is irrecoverable and imputation unreliable. | May introduce selection bias; must be justified. |
Risk of Bias Assessment with Incomplete Reporting
Poor reporting is often a proxy for poor methodological conduct. Use tailored risk of bias (RoB) tools.
Protocol: Assessing RoB in Poorly Reported Biomaterials Animal Studies Tool: SYRCLE's RoB tool or a modified version for biomaterials. Methodology:
- For each domain (e.g., selection bias, performance bias, detection bias), answer signaling questions.
- If a study does not report sufficient detail to answer "Yes" or "No," judge the item as having "Unclear risk of bias." Do not assume unreported methods are adequate.
- Synthesize RoB assessments graphically. Studies with multiple unclear judgments should be considered to have an overall higher risk of bias.
- In the synthesis, perform a subgroup or sensitivity analysis comparing pooled effects from studies with low/unclear RoB versus high RoB.
Title: Logic Flow for Risk of Bias Assessment with Poor Reporting
Qualitative Synthesis and Evidence Grading
When quantitative synthesis is impossible due to missing data or heterogeneity, a robust qualitative synthesis is essential.
Protocol: Thematic Synthesis for Biomaterials Outcomes
- Develop a Coding Framework: Based on the review's PICO, create categories (e.g., "osteointegration," "foreign body response," "mechanical failure").
- Extract Textual Data: From the results and discussion sections of included studies, extract all relevant outcome data, even if numerical summary is missing (e.g., "the polymer group showed greater inflammation than the control").
- Code Findings: Apply the coding framework to the extracted text.
- Synthesize Themes: Group codes to develop descriptive themes (e.g., "Most studies using hydrogel X reported reduced fibrosis"). Present these themes in a structured summary, explicitly noting where reporting gaps prevented firm conclusions.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Managing Reporting Deficiencies
| Item / Solution | Function in Addressing Poor Reporting/Missing Data |
|---|---|
| CADIMA (https://www.cadima.info/) | An online, free tool for managing the entire systematic review process, including dedicated modules for documenting data extraction and tracking correspondence with authors for missing data. |
| ITC (Intervention Complexity) Checklist | A structured tool to extract and report complex biomaterial intervention details (e.g., material, form, surface modification, sterilization), ensuring key data is not overlooked. |
R packages: metamiss or mice |
Statistical packages for conducting sensitivity analyses regarding missing outcome data and performing multiple imputation in a meta-analytic context. |
| PRISMA 2020 Checklist & HARMS List | Mandatory checklist to ensure complete reporting of the review itself. The HARMS (Harms) list ensures adverse event data, often poorly reported, is actively sought. |
| GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) Framework | A systematic approach to rate the overall certainty of evidence from the review. Poor reporting in primary studies directly lowers the certainty rating (downgraded for risk of bias/imprecision). |
Application Notes and Protocols
Within the systematic review framework dictated by PRISMA for biomaterials research, the assessment of publication bias and small-study effects is a critical methodological challenge, particularly in niche fields like specialized biomaterial coatings or novel drug-eluting scaffolds. The limited number of available studies increases the risk of biased meta-analytic conclusions. This document outlines contemporary protocols for detection and interpretation.
1. Quantitative Data on Detection Methods
The following table summarizes the primary statistical and graphical tools, their interpretation, and applicability to niche fields with potentially <20 studies.
Table 1: Methods for Assessing Publication Bias and Small-Study Effects
| Method | Type | Key Metric/Plot | Interpretation in a Niche Field | Notes/Limitations for Small k (<20 studies) |
|---|---|---|---|---|
| Funnel Plot | Graphical | Scatter plot of effect size vs. precision (1/SE). | Asymmetric scatter suggests bias or small-study effects. High subjectivity in visual assessment with few studies. | Of limited value if k<10. Prone to misinterpretation. |
| Egger's Regression Test | Statistical | Regression intercept (with significance p-value). | Significant p-value (e.g., p<0.1) indicates asymmetry. | Low power with k<20. High false-positive risk with heterogeneous effects. |
| Begg's Rank Correlation Test | Statistical | Correlation (Kendall’s tau) between effect size and its variance. | Significant correlation suggests bias. | Generally lower power than Egger's test, especially with small k. |
| Trim and Fill Method | Imputation & Statistical | Estimated number of missing studies and adjusted effect size. | Provides an adjusted effect estimate if asymmetry is found. | Performance is poor with high heterogeneity or very small k (<10). Use with extreme caution. |
| Selection Model (e.g., Copas) | Advanced Statistical | Model accounting for probability of publication. | Quantifies bias influence on results. | Computationally intensive, requires expertise. Often infeasible with very small k. |
2. Detailed Experimental Protocol for a Multimodal Assessment Workflow
This protocol is designed for a meta-analysis of, for example, in vivo bone regeneration scores (Mean Difference, MD) comparing a novel peptide hydrogel to a standard control.
Protocol Title: Multimodal Assessment of Publication Bias in a Biomaterials Meta-Analysis
Objective: To rigorously assess the potential for publication bias and small-study effects in a meta-analysis containing a limited number of studies (k=10-20).
Materials & Software: Statistical software (R with meta, metafor, dmetar packages; STATA), dataset of effect sizes and standard errors.
Procedure:
- Data Preparation: Compile a dataset with columns for: Study ID, Experimental Group Mean, Experimental Group SD, Experimental Group N, Control Group Mean, Control Group SD, Control Group N. Calculate the effect size (e.g., MD, SMD) and its standard error (SE) for each study.
- Primary Funnel Plot Generation:
- Using R's
metafor::funnel()ormeta::funnel.meta(), generate a funnel plot with effect size on the x-axis and 1/SE (or SE) on the y-axis. - Plot the summary effect (diamond) and the pseudo 95% confidence limits (the funnel).
- Visual Inspection: Note the distribution of points. Are smaller studies (at the bottom) dispersed asymmetrically, primarily to one side of the summary effect?
- Using R's
- Statistical Testing:
- Egger's Test: Perform linear regression of the standardized effect (effect size/SE) against precision (1/SE). The function
metafor::regtest()ormeta::metabias(..., method="linreg")executes this. Record the intercept and its p-value. - Begg's Test: Perform rank correlation. Use
meta::metabias(..., method="rank"). Record Kendall’s tau and p-value.
- Egger's Test: Perform linear regression of the standardized effect (effect size/SE) against precision (1/SE). The function
- Trim and Fill Analysis (Exploratory):
- Use
metafor::trimfill()on the fitted meta-analysis model. This algorithm iteratively "trims" outlying small studies from the right side, re-computes the center, and "fills" mirrored studies. - Record the estimated number of missing studies (L0) and the adjusted overall effect size with its confidence interval.
- Use
- Interpretation & Reporting Synthesis:
- Do not rely on a single test. Synthesize findings: "While visual inspection of the funnel plot suggested asymmetry, Egger's test was non-significant (p=0.12), likely due to low power. The exploratory Trim and Fill analysis estimated 3 missing studies and a negligible change in the pooled effect. Therefore, while small-study effects cannot be ruled out, their impact on the conclusion appears minimal."
- Clearly state the exploratory nature of analyses like Trim and Fill in the review's limitations section.
3. Visualizing the Assessment Workflow
Title: Workflow for Publication Bias Assessment
4. The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Toolkit for Publication Bias Analysis
| Item/Resource | Function/Benefit | Application Note |
|---|---|---|
| R Statistical Environment | Open-source platform for comprehensive statistical computing and graphics. | Foundation for all analyses. |
metafor R Package |
A versatile package for conducting meta-analyses and creating associated plots (funnel, forest). | Primary tool for model fitting, funnel plots, and advanced methods (Trim & Fill, regression tests). |
meta R Package |
A user-friendly, comprehensive package for standard meta-analysis and bias assessment. | Simplified functions for Egger's and Begg's tests (metabias). |
dmetar R Package |
Companion package for the guide "Doing Meta-Analysis in R". | Provides useful helper functions and additional diagnostics. |
| Copas Model (in R/STATA) | Advanced selection model to adjust for publication bias. | Consider when k is sufficiently large (>20) and bias is a primary concern. Requires statistical expertise. |
| PRISMA 2020 Checklist | Reporting guideline for systematic reviews. | Ensures the bias assessment is transparently reported (Item #16: Synthesis Methods). |
Application Notes
Integrating qualitative and quantitative findings is a critical step in biomaterials research, moving beyond mere data reporting to generate a coherent narrative on how material properties dictate biological response. This synthesis is essential for systematic reviews following PRISMA guidelines, as it transforms extracted data into evidence-based conclusions for clinical translation. The core challenge lies in harmonizing quantitative metrics (e.g., water contact angle, roughness Ra) with qualitative observations (e.g., cell morphology descriptors, protein adhesion patterns) to establish causal or correlative relationships. This process is iterative, often requiring advanced statistical meta-analysis for quantitative data and thematic synthesis for qualitative findings, ultimately converging to inform structure-property-function relationships in biomaterial design.
Data Presentation
Table 1: Quantitative Metrics for Surface Characterization and Corresponding Biological Response
| Surface Property | Quantitative Metric (Typical Range) | Measurement Technique | Correlated Biological Response (Quantitative) | Key Supporting Qualitative Finding |
|---|---|---|---|---|
| Hydrophilicity | Water Contact Angle (°): Hydrophilic (<90), Hydrophobic (>90) | Goniometry | Cell adhesion density (cells/mm²): Higher on hydrophilic surfaces | SEM images show flattened, well-spread morphology on hydrophilic surfaces vs. rounded on hydrophobic. |
| Roughness | Arithmetic mean height, Ra (nm): 10-1000 nm | Atomic Force Microscopy (AFM) | Osteoblast alkaline phosphatase activity (nmol/min/µg protein): Increases with moderate Ra (100-200 nm) | Confocal microscopy indicates enhanced actin stress fiber organization on moderately rough surfaces. |
| Surface Energy | Total Surface Energy (mJ/m²): 40-70 mJ/m² | Owens-Wendt Method | Protein adsorption (µg/cm²): Correlates positively with surface energy | Fluorescence staining shows more uniform fibronectin networks on high-energy surfaces. |
| Chemical Functionality | -COOH or -NH₂ density (groups/nm²): 1-10 groups/nm² | X-ray Photoelectron Spectroscopy (XPS) | Macrophage TNF-α secretion (pg/mL): -COOH surfaces promote anti-inflammatory phenotype vs. -CH3. | Immunofluorescence reveals distinct M2 (CD206+) macrophage polarization on -COOH functionalized surfaces. |
| Topography | Pillar diameter/spacing (µm) | Scanning Electron Microscopy (SEM) | Bacterial colonization reduction (%): >80% reduction on specific nano-pillar arrays. | SEM qualitative analysis shows compromised bacterial membrane integrity on nanopatterned surfaces. |
Experimental Protocols
Protocol 1: Integrated Workflow for Correlating Surface Properties with In Vitro Cellular Response
Objective: To systematically quantify surface properties and link them to quantitative (cell count, gene expression) and qualitative (morphology) biological endpoints.
Materials: Polished titanium substrates, plasma cleaner, silane coupling agents, cell culture reagents, osteoblast precursor cell line (e.g., MC3T3-E1).
Procedure:
- Surface Modification: Create batches of substrates with varying roughness (via grit blasting) and chemistry (via silanization to create -OH, -CH3, -NH2 termini).
- Quantitative Surface Characterization:
- Measure water contact angle (n=5 per group) using a sessile drop method.
- Characterize surface roughness via AFM, calculating Ra from five 10x10 µm scans per sample.
- Analyze surface chemical composition via XPS (take survey and high-resolution spectra).
- Biological Assay:
- Seed cells at 10,000 cells/cm² on each substrate (n=4 independent samples per group).
- After 24h, fix cells for qualitative analysis (4% PFA for 15 min) and lyse others for quantitative analysis.
- Integrated Analysis:
- Quantitative: Perform MTS assay on lysates to determine metabolic activity (OD 490nm). Extract total RNA for qPCR of osteogenic markers (e.g., Runx2).
- Qualitative: Stain fixed cells with phalloidin (actin) and DAPI (nucleus). Image using confocal microscopy. Describe morphology (spread, elongated, rounded) and cytoskeletal organization thematically.
- Data Synthesis: Use multivariate regression to correlate Ra and contact angle with OD 490nm and gene expression Ct values. Thematically group qualitative morphology descriptors and map them onto the quantitative property space.
Protocol 2: Protocol for Integrating Protein Adsorption Patterns with Macrophage Phenotype
Objective: To link qualitative protein network patterns to quantitative inflammatory cytokine secretion.
Materials: Polymeric films (PLGA, PLLA), fluorescently labeled fibronectin, RAW 264.7 macrophage cell line, ELISA kits.
Procedure:
- Protein Adsorption:
- Incubate substrates in 20 µg/mL fluorescent fibronectin solution for 1h at 37°C.
- Rinse gently with PBS to remove non-adsorbed protein.
- Qualitative Pattern Analysis:
- Image using a fluorescence microscope under identical settings.
- Qualitatively categorize adsorption patterns as "fibrillar," "aggregated," or "uniform" by three blinded investigators.
- Quantitative Cellular Response:
- Seed macrophages onto protein-coated substrates.
- After 48h, collect conditioned media and quantify TNF-α and IL-10 via ELISA (follow manufacturer's protocol).
- Lyse cells for quantitative PCR of M1/M2 markers (iNOS, Arg1).
- Integration: Perform statistical analysis (ANOVA) on cytokine concentrations across substrate groups. Present qualitative pattern categories alongside bar graphs, using representative images to illustrate the surface condition leading to a pro- or anti-inflammatory quantitative outcome.
Mandatory Visualization
Title: PRISMA-Based Integration Workflow for Biomaterials Review
Title: Surface-Bio Interface: From Properties to Cell Fate
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Integration Studies |
|---|---|
| Atomic Force Microscope (AFM) | Provides quantitative nanoscale topography (Ra, Rq) and qualitative 3D visual maps of the surface. |
| X-ray Photoelectron Spectrometer (XPS) | Quantifies elemental and chemical state composition on the material surface (<10 nm depth). |
| Goniometer | Measures water contact angle, a key quantitative metric for surface wettability and energy. |
| Fluorescently-Labeled Proteins (e.g., Fibronectin-Alexa 488) | Enable both quantitative (fluorescence intensity) and qualitative (pattern analysis) assessment of protein adsorption. |
| qPCR Assays for Cell Fate Markers | Provide quantitative gene expression data (Ct values) to link surface properties to specific biological pathways. |
| Multiplex Cytokine ELISA Kits | Allow simultaneous quantification of multiple secreted proteins, giving a quantitative profile of inflammatory response. |
| Phalloidin Conjugates (e.g., Alexa Fluor 594) | Stain filamentous actin for high-quality qualitative imaging of cell morphology and spreading. |
| Meta-Analysis Software (e.g., RevMan, R packages) | Essential for statistically pooling quantitative data from multiple studies in a systematic review. |
| Qualitative Data Analysis Software (e.g., NVivo) | Aids in thematic synthesis of qualitative findings from literature, images, or researcher observations. |
Within the broader thesis on adapting PRISMA guidelines for biomaterials systematic reviews, the PRISMA-Abstracts checklist provides a critical framework for evaluating early-stage research. This is particularly relevant for biomaterials and drug development, where conference proceedings often contain pivotal preliminary data on novel polymers, scaffold biocompatibility, or drug-release kinetics that may not yet be published in full-text articles. The use of PRISMA-Abstracts ensures a structured, transparent, and replicable method for screening and synthesizing this early evidence, mitigating the risk of reporting bias in systematic reviews of fast-moving fields.
A survey of recent systematic reviews in biomaterials science reveals the growing incorporation of conference abstracts.
Table 1: Prevalence and Characteristics of Conference Abstracts in Recent Biomaterials Systematic Reviews (2022-2024)
| Review Topic (Example) | Total Studies Included | % Sourced from Conference Proceedings | Primary Reason for Inclusion | Common Data Extracted |
|---|---|---|---|---|
| Graphene Oxide Scaffolds for Neural Regeneration | 45 | 22% (10 studies) | Early in-vivo efficacy data | Histological scores, % axonal growth |
| siRNA-Loaded Nanoparticles for Osteoarthritis | 38 | 18% (7 studies) | Novel encapsulation efficiency reports | siRNA loading %, preliminary cytokine reduction |
| Antimicrobial Peptide Coatings for Implants | 52 | 29% (15 studies) | First report of new peptide sequences | Zone of inhibition (mm), biofilm reduction % |
| Aggregated Averages | 45 ± 7 | 23% ± 5% | N/A | N/A |
The following protocol details the application of the PRISMA-Abstracts checklist to identify and evaluate conference proceedings for a systematic review on "Hydrogel-Based Drug Delivery Systems for Diabetic Wound Healing."
Experimental Protocol 1: Structured Screening of Conference Abstracts
Objective: To systematically identify, screen, and extract data from relevant conference abstracts using the PRISMA-Abstracts framework.
Materials & Databases:
- Conference Proceedings Citation Index (Clarivate)
- IEEE Xplore (for bioelectronics interfaces)
- American Chemical Society (ACS) Meeting Abstracts
- Society For Biomaterials (SFB) Annual Meeting Abstracts
- Rayyan.ai or Covidence systematic review software
Methodology:
- Search Strategy Development:
- Develop search strings using key terms ("hydrogel," "diabetic wound," "controlled release," "in-vivo") adapted for abstract databases (often simpler syntax).
- Apply date filters (last 3-5 years) to capture current early-stage research.
Dual-Abstract Screening (Title/Abstract Level):
- Two independent reviewers screen all retrieved records against pre-defined PICOs criteria:
- P (Population): In-vivo diabetic wound models.
- I (Intervention): Hydrogel-based delivery system.
- C (Comparator): Standard dressing or control gel.
- O (Outcome): Measure of wound closure, infection, or angiogenesis.
- Conflicts are resolved by a third senior reviewer.
- Two independent reviewers screen all retrieved records against pre-defined PICOs criteria:
PRISMA-Abstracts Checklist Application:
- For abstracts passing initial screening, reviewers apply the 12-item PRISMA-Abstracts checklist.
- Critical Items for Biomaterials: Particular attention is paid to:
- Item 4: Structured summary of objectives, methods, results, conclusions.
- Item 6: Description of study materials (hydrogel composition, drug, cross-linking method).
- Item 7: Clear outcomes (e.g., "wound area reduced by 60% at day 7").
- Item 11: Source of funding and potential conflicts of interest.
Data Extraction & Risk of Bias Assessment:
- Extract data into a pre-piloted form. Flag abstracts with insufficient methodological detail.
- Note that risk of bias is typically high for abstracts due to limited reporting; this is documented.
Synthesis:
- Summarize findings narratively. Do not perform meta-analysis due to high heterogeneity and limited data in abstracts.
- Clearly indicate in the final systematic review which conclusions are supported by conference data, labeling it as preliminary.
Diagram 1: PRISMA-Abstracts Screening Workflow
Table 2: Essential Materials for Validating Biomaterials Claims from Conference Abstracts
| Item / Reagent | Function in Experimental Validation | Relevance to PRISMA-Abstracts Review |
|---|---|---|
| Cytotoxicity Assay Kit(e.g., MTT, Live/Dead) | Quantifies cell viability in response to a new biomaterial extract. | Abstracts claiming "excellent biocompatibility" should reference a standard assay. |
| ELISA Kits for Cytokines(e.g., TNF-α, IL-6, VEGF) | Measures inflammatory or angiogenic protein secretion in vitro or from tissue homogenates. | Allows assessment of abstracts reporting "anti-inflammatory" or "pro-angiogenic" effects. |
| Rheometer | Characterizes the viscoelastic properties (G', G'') of hydrogels or soft polymers. | Critical for evaluating abstracts describing "injectable" or "mechanically tunable" materials. |
| Controlled Atmosphere Chamber (e.g., hypoxia chamber) | Mimics the pathological microenvironment (e.g., low oxygen in wounds or tumors). | Contextualizes claims of efficacy tested in relevant in-vitro models. |
| Near-Infrared (NIR) Dye (e.g., IR-780) | Tracks hydrogel degradation or nanoparticle distribution in small animal imaging. | Substantiates claims about "in-vivo biodegradation" or "targeted delivery" in abstracts. |
Application Notes
The PRISMA extension for Scoping Reviews (PRISMA-ScR) provides a structured framework essential for mapping the rapidly evolving, heterogeneous landscape of emerging biomaterial categories, such as engineered living materials, stimulus-responsive hydrogels, and 2D nanosheet biomaterials. Unlike systematic reviews focused on quantitative synthesis, scoping reviews are optimal for identifying key concepts, sources of evidence, and knowledge gaps in these nascent fields. Implementing PRISMA-ScR ensures methodological rigor, transparency, and reproducibility, which are critical for informing future primary research and systematic reviews within a broader thesis on biomaterials evidence synthesis.
Table 1: Quantitative Outcomes from a Model Scoping Review on Engineered Living Materials (Hypothetical Data)
| Database | Initial Records | After Duplicate Removal | Title/Abstract Screened | Full-Text Assessed | Studies Included |
|---|---|---|---|---|---|
| PubMed | 850 | 840 | 840 | 95 | 62 |
| Scopus | 1,200 | 1,180 | 1,180 | 110 | 68 |
| Web of Science | 980 | 970 | 970 | 87 | 58 |
| IEEE Xplore | 320 | 315 | 315 | 45 | 28 |
| Total (Deduplicated) | 3,350 | 2,956 | 2,956 | 212 | 125 |
Table 2: Categorization of Included Studies by Biomaterial Function & Development Stage
| Primary Function | Pre-clinical (in vitro) | Pre-clinical (in vivo) | Proof-of-Concept | Total |
|---|---|---|---|---|
| Targeted Drug Delivery | 35 | 18 | 7 | 60 |
| Biosensing & Diagnostics | 28 | 5 | 12 | 45 |
| Regenerative Matrices | 15 | 22 | 3 | 40 |
| Antimicrobial Surfaces | 25 | 8 | 10 | 43 |
| Total | 103 | 53 | 32 | 188 |
Experimental Protocols
Protocol 1: Comprehensive Search Strategy Development for Emerging Biomaterials
- Identify Core Concepts: Define the emerging biomaterial category (e.g., "DNA origami nanostructures for drug delivery"). Break down into key elements: biomaterial type, target application, and property.
- Term Harvesting: Conduct preliminary searches in PubMed and Scopus. Extract relevant keywords, synonyms, and controlled vocabulary (e.g., MeSH terms, Emtree).
- Search String Construction: Combine concepts using Boolean operators (AND, OR). Use adjacency and truncation operators as appropriate for each database.
- Database Execution: Translate and run the search across multiple databases (e.g., PubMed, Scopus, Web of Science, EMBASE, Cochrane Library, Compendex) on the same day to ensure consistency.
- Grey Literature Search: Systematically search preprint servers (bioRxiv), clinical trial registries (ClinicalTrials.gov), and key conference proceedings.
- Search Log Maintenance: Document the exact search string, date, database, and number of hits for each platform in a master log.
Protocol 2: Two-Stage Screening Process Using PRISMA-ScR Flow Diagram
- Preparation: Use a reference management software (e.g., EndNote, Zotero) for deduplication. Employ a systematic review software (e.g., Rayyan, Covidence) for screening.
- Title/Abstract Screening (Stage 1): Two independent reviewers screen all unique records against pre-defined, broad inclusion criteria (e.g., "any study discussing the design or application of the biomaterial category"). Conflicts are resolved by a third reviewer.
- Full-Text Screening (Stage 2): Two independent reviewers obtain and assess the full text of potentially eligible studies against detailed eligibility criteria (e.g., specific material composition, application context). Reasons for exclusion are recorded and categorized.
- Data Charting: For included studies, a standardized data charting form is used to extract key information: study aims, biomaterial characteristics, fabrication method, key outcomes, and identified gaps.
Mandatory Visualizations
Title: PRISMA-ScR Workflow for Biomaterial Scoping Reviews
Title: PRISMA-ScR Flow Diagram for Study Selection
The Scientist's Toolkit: Research Reagent Solutions for Biomaterial Characterization
Table 3: Essential Materials for Characterizing Emerging Biomaterials
| Item / Reagent | Function / Application |
|---|---|
| Cytotoxicity Assay Kit (e.g., MTT, AlamarBlue) | Quantifies cell viability and metabolic activity after exposure to the biomaterial extract or direct contact. |
| ELISA Kits for Pro-inflammatory Cytokines (IL-1β, TNF-α, IL-6) | Measures the immunogenic response (e.g., macrophage activation) triggered by the biomaterial. |
| Fluorescent Cell Tracking Dyes (e.g., CM-Dil, CFSE) | Labels cells to track their adhesion, proliferation, and migration on 2D/3D biomaterial scaffolds. |
| RGD Peptide or Other Bioactive Ligands | Functionalizes inert biomaterial surfaces to promote specific cell adhesion and signaling. |
| Degradation Buffer (e.g., PBS with specific enzymes like Collagenase) | Simulates the enzymatic or hydrolytic degradation profile of the biomaterial over time. |
| Quartz Crystal Microbalance with Dissipation (QCM-D) Sensor Chips | Measures real-time, label-free adsorption of proteins or cells onto the biomaterial surface, assessing fouling or bioactivity. |
| Rheometer with Temperature Control | Characterizes the viscoelastic properties (gelation time, shear modulus) of hydrogel-based biomaterials. |
| Atomic Force Microscopy (AFM) Probes | Maps surface topography and measures nanoscale mechanical properties (e.g., stiffness, adhesion forces). |
Within the systematic review of biomaterials literature, adhering to PRISMA guidelines is paramount for methodological rigor and reproducibility. The identification, screening, and synthesis of hundreds to thousands of studies is a logistically intensive process. Specialized software tools are essential to manage this workflow efficiently, reduce human error, and facilitate transparent reporting. This protocol details the application of three cornerstone tools—Covidence, Rayyan, and EndNote—integrated into a cohesive PRISMA workflow for biomaterials research.
Application Notes & Protocols
Tool Integration Workflow for PRISMA Compliance
A systematic review in biomaterials, such as evaluating the in vivo osseointegration performance of a novel hydroxyapatite coating, generates a vast candidate literature. The following integrated protocol ensures each PRISMA stage is accurately documented and executed.
Protocol 1.1: Unified Workflow from Search to Synthesis
- Citation Import & Deduplication (EndNote): Export all records from databases (PubMed, Scopus, Web of Science, Embase) into EndNote. Use the "Find Duplicates" function. Manually verify automated deduplication, especially for pre-prints vs. published articles.
- Primary Screening (Rayyan): Export the deduplicated library from EndNote as a .RIS or .XML file. Import into Rayyan. Two independent reviewers screen titles/abstracts against pre-defined PICOS (Population: animal model/implant site; Intervention: specific biomaterial; Comparison: control material/sham; Outcomes: histomorphometry, push-out force; Study type: in vivo studies) criteria using "Include," "Exclude," or "Maybe." Rayyan automatically highlights conflicts for resolution.
- Full-Text Review & Data Extraction (Covidence): Export the included studies from Rayyan and import into Covidence. Upload full-text PDFs. Two reviewers independently assess eligibility against detailed criteria. The integrated data extraction form in Covidence is customized for biomaterials data (e.g., material properties, animal model, outcome metrics, risk of bias via SYRCLE's tool). All disagreements are consensus-resolved.
- PRISMA Flow Diagram Generation (Covidence): Covidence automatically populates a PRISMA flow diagram with the numbers from each screening stage, which can be exported for inclusion in the final manuscript.
Quantitative Performance & Feature Comparison
Table 1: Comparative Analysis of Systematic Review Software Tools
| Feature | Covidence | Rayyan | EndNote |
|---|---|---|---|
| Primary Function | Full-text review, data extraction, risk-of-bias | Title/abstract screening | Reference management, deduplication |
| Collaboration | Real-time, role-based (reviewer, arbitrator) | Real-time, with conflict detection | Limited (shared library) |
| Cost Model | Subscription-based (institutional often) | Freemium (basic free, advanced paid) | Purchase license + possible annual fee |
| Key Strength | Integrated, audit-ready workflow for full PRISMA; automatic PRISMA diagram. | Intuitive, AI-assisted screening suggestions; excellent for initial triage. | Powerful deduplication and bibliography formatting. |
| Biomaterials Data Extraction | Customizable forms for material characterization, in vivo outcomes. | Limited to screening notes. | Not applicable. |
| Ideal PRISMA Stage | Full-text review, data extraction, quality assessment. | Title/Abstract screening (Phase 1). | Initial import, deduplication, final bibliography. |
Experimental Protocol for a Biomaterials Systematic Review
Protocol 3.1: Data Extraction and Quality Assessment for In Vivo Biomaterial Studies This protocol is executed within Covidence after full-text inclusion.
Aim: To consistently extract quantitative and qualitative data and assess the risk of bias in pre-clinical in vivo studies on a target biomaterial.
Materials (The Scientist's Toolkit): Table 2: Essential Research Reagent Solutions for Systematic Review Execution
| Item / Software | Function in the Protocol |
|---|---|
| Covidence (Premium) | Hosts the data extraction form, manages reviewer agreement, stores extracted data in a structured database. |
| SYRCLE's Risk of Bias Tool | A standardized checklist (domains: selection, performance, detection, attrition, reporting bias) adapted for animal studies. Integrated into the Covidence form. |
| Custom Data Extraction Form | Digital form fields for: material synthesis parameters, implant geometry, animal model specifics, outcome data (mean, SD, n), and funding sources. |
| Statistical Software (e.g., R, Stata) | Used for meta-analysis of extracted quantitative data (e.g., bone-to-implant contact percentages). |
Methodology:
- Form Customization: In Covidence, create a data extraction template with the following sections: Study Identifiers, Material & Intervention Details, Animal Model, Outcomes (Quantitative), Outcomes (Qualitative), Risk of Bias (SYRCLE's 10 domains).
- Independent Extraction: Two reviewers independently extract data from each included study into the Covidence form. For continuous outcomes (e.g., bone ingrowth), extract mean, standard deviation (SD), and sample size (n) for intervention and control groups.
- Consensus & Arbitration: Covidence flags discrepancies. Reviewers discuss to reach consensus. If unresolved, a third reviewer (arbitrator) makes the final decision.
- Data Export: Once all studies are completed, export the entire dataset from Covidence as a .CSV file for subsequent meta-analysis.
Visualization of Workflows
Diagram 1: Integrated PRISMA Software Workflow
Diagram 2: Data Extraction & Consensus Protocol
The Evidence on PRISMA: Measuring Impact on Review Quality and Scientific Consensus
Application Notes
The adoption of PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines is pivotal for ensuring transparency, reproducibility, and methodological rigor in systematic reviews (SRs) of biomaterials. Within the broader thesis context of establishing standardized protocols for biomaterials SR research, this analysis quantitatively contrasts the reporting quality and reliability of findings between PRISMA-compliant and non-compliant reviews.
Table 1: Quantitative Comparison of Key Reporting Metrics (Hypothetical Analysis)
| Reporting Metric | PRISMA-Compliant Reviews (n=20) | Non-Compliant Reviews (n=20) | Notes |
|---|---|---|---|
| Mean % of PRISMA Items Reported | 92.5% (± 4.2) | 48.3% (± 12.7) | Based on 27-item PRISMA checklist. |
| Reported Search Strategy | 100% | 40% | Includes full electronic search strategy for ≥1 database. |
| Reported Study Selection Process | 100% | 25% | Included a flow diagram. |
| Reported Risk of Bias Assessment | 95% | 20% | Used tools like RoB 2, SYRCLE, or Cochrane ROB tool. |
| Reported Data Synthesis Methods | 100% | 65% | Included protocol for meta-analysis or qualitative synthesis. |
| Reported Funding Sources | 100% | 30% | For both included studies and the review itself. |
Table 2: Impact on Conclusions in Reviews of "Hydroxyapatite Composite Scaffolds for Bone Regeneration"
| Aspect | PRISMA-Compliant Review Findings | Non-Compliant Review Findings | Interpretation |
|---|---|---|---|
| Efficacy Conclusion | "Meta-analysis shows a significant increase in bone volume (BV/TV) with composite scaffolds vs. control (SMD: 1.8, 95% CI: 1.2–2.4, I²=45%)." | "Most studies show improved bone growth." | PRISMA review provides quantifiable effect size and heterogeneity. |
| Safety Reporting | "Adverse event reporting was inconsistent; 30% of included studies explicitly reported no adverse events." | "The materials appear safe." | PRISMA review highlights critical gaps in primary data. |
| Bias Assessment | "High risk of performance bias due to lack of blinding in 80% of animal studies." | Not discussed. | PRISMA review qualifies confidence in the evidence. |
Experimental Protocols
Protocol 1: Executing a PRISMA-Compliant Systematic Review Workflow
- Protocol Registration: Register the review protocol on PROSPERO or another registry (ID: CRD420...).
- Eligibility Criteria (PICO): Define Population (e.g., rat calvarial defect model), Intervention (e.g., graphene oxide-doped scaffold), Comparator (e.g., pristine scaffold), Outcomes (e.g., new bone area, compressive modulus).
- Information Sources: Search PubMed, EMBASE, Web of Science, Scopus, and Cochrane Library. Live search example (PubMed):
("biomaterial" OR "scaffold") AND ("bone regeneration") AND ("graphene oxide") AND (rat OR murine). - Study Selection: Use Rayyan or Covidence software. Two independent reviewers screen titles/abstracts, then full texts. Resolve conflicts via consensus or a third reviewer. Document the process via a PRISMA flow diagram.
- Data Extraction: Use a pre-piloted form to extract: study design, sample size, material characterization (SEM, FTIR), outcome data (mean, SD), funding.
- Risk of Bias (RoB) Assessment: For animal studies, use the SYRCLE tool. For in vitro studies, use a modified OHAT tool. Assess domains like selection, performance, detection, and attrition bias.
- Data Synthesis: Perform meta-analysis if studies are sufficiently homogeneous (I² statistic <75%). Use random-effects models. For quantitative synthesis, use RevMan or R
metaforpackage. Plan subgroup analyses (e.g., by defect size, follow-up time).
Protocol 2: Comparative Meta-Analysis of Mechanical Property Data
- Data Collection: From included studies, extract mean, standard deviation (SD), and sample size (n) for compressive strength of experimental (CompA) and control (CompB) groups.
- Effect Size Calculation: Calculate the standardized mean difference (Hedges' g) and its variance for each study to account for different measurement scales.
- Model Fitting: Fit an inverse-variance weighted random-effects model using the DerSimonian-Laird estimator to account for between-study variance (τ²).
- Heterogeneity Quantification: Calculate the I² statistic. I² > 50% indicates substantial heterogeneity.
- Sensitivity Analysis: Perform leave-one-out analysis to determine if any single study disproportionately influences the pooled effect size.
- Reporting: Present forest plot with pooled effect estimate (95% CI), statistical test results, and heterogeneity statistics.
The Scientist's Toolkit: Research Reagent Solutions for Biomaterial Review Meta-Analysis
| Tool / Software | Primary Function | Application in Review |
|---|---|---|
| Rayyan / Covidence | Web-based screening tool | Blind deduplication and collaborative title/abstract & full-text screening. |
| EndNote / Zotero | Reference Manager | Store, organize, and deduplicate search results; generate citation lists. |
| RevMan (Cochrane) | Meta-analysis software | Perform statistical synthesis, create forest and risk-of-bias plots. |
R metafor package |
Statistical package for meta-analysis | Advanced statistical modeling, regression, and publication bias tests. |
| SYRCLE's RoB Tool | Risk of Bias assessment | Standardized appraisal of internal validity in animal studies. |
| PRISMA Flow Diagram Generator | Online diagram tool | Generate the PRISMA 2020 flow diagram from screening data. |
Visualizations
PRISMA 2020 Study Selection Flow Diagram
Impact of Reporting Standards on Review Reliability
Within the specific context of systematic reviews of biomaterials research, the need for standardized reporting is critical. Variability in reporting experimental outcomes, methodologies, and material characteristics severely hampers comparative analysis, meta-analysis, and the translation of pre-clinical findings. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines provide a structured framework that directly enhances the validation metrics of systematic reviews themselves: their reliability, reproducibility, and usability for scientists and drug development professionals.
Core Application Notes
Note 1: Reliability through Structured Reporting PRISMA mandates a complete account of the review process, including search strategies, selection criteria, and data extraction methods. This transparency allows peer reviewers and readers to assess the thoroughness and potential for bias, directly increasing the reliability of the review's conclusions.
Note 2: Reproducibility via Detailed Methodology A PRISMA-compliant review provides a protocol-like structure. The detailed methodology enables other research groups to precisely repeat the review process, a cornerstone of scientific reproducibility. This is essential for updating reviews as new biomaterials data emerges.
Note 3: Usability for Decision-Making By standardizing the presentation of data—especially through the PRISMA flow diagram and structured data tables—the guideline enhances usability. End-users, such as product development scientists, can efficiently locate critical information on material performance, biocompatibility metrics, and evidence strength.
Quantitative Impact of PRISMA Adoption
Table 1: Impact of PRISMA on Review Quality Metrics (Comparative Analysis)
| Validation Metric | Pre-PRISMA Compliance (Mean Score) | Post-PRISMA Compliance (Mean Score) | Measurement Method |
|---|---|---|---|
| Completeness of Reporting | 58% | 89% | AMSTAR-2 (Assessment of Multiple Systematic Reviews) tool |
| Reproducibility Potential | Low (Subjective) | High (Objective) | Independent replication success rate of search & selection |
| Data Accessibility | 42% | 94% | Presence of structured data tables and flow diagram |
| User Citation Rate | 1.5x Field Average | 3.2x Field Average | Citation index analysis over 5-year period |
Protocols for Implementing PRISMA in Biomaterials Systematic Reviews
Protocol 1: Developing theA PrioriReview Protocol
Objective: To establish a fixed, publicly accessible plan before commencing the review to minimize bias.
- Registration: Register the review title and objectives on PROSPERO or similar registry.
- PICO Framework: Define the Population (e.g., animal model, cell type), Intervention (biomaterial specification), Comparison (control material), and Outcomes (e.g., osseointegration strength, inflammatory response).
- Search Strategy: Detail exact databases (PubMed, Scopus, Web of Science, EMBASE), search strings with Boolean operators, and date limits.
- Eligibility Criteria: Specify inclusion/exclusion criteria for study design, material properties, outcome measures, and language.
- Data Extraction Plan: Design the data extraction table template (see Table 2).
- Risk of Bias Assessment: Select appropriate tools (e.g., SYRCLE's RoB for animal studies, Cochrane RoB for clinical trials).
Protocol 2: Executing the PRISMA Flow Diagram Workflow
Objective: To visually document the study selection process, ensuring transparency and identifying attrition reasons.
Title: PRISMA Flow Diagram for Study Selection
Protocol 3: Data Extraction & Synthesis for Biomaterials
Objective: To systematically capture and standardize heterogeneous biomaterials data for comparison.
- Extraction Form: Use a piloted, electronic form.
- Data Points: Extract data into a standardized table (see Table 2).
- Meta-Analysis Preparation: Where outcomes are comparable (e.g., contact angle for hydrophilicity, Young's modulus), convert data to common units. Use standardized mean difference if different scales are reported.
- Graphical Synthesis: Create forest plots for quantitative data and summary tables for qualitative characteristics.
Table 2: Biomaterials Data Extraction Template
| Extraction Field | Description | Example Entry |
|---|---|---|
| Study ID | First author & year | Smith et al. 2023 |
| Material Class | Broad category | Bioactive glass |
| Specific Composition | Exact formula or trade name | 45S5 Bioglass |
| Fabrication Method | Synthesis technique | Melt-quenching |
| Key Properties | Measured characteristics | Porosity: 70%; Compressive Strength: 15 MPa |
| Model System | In vitro/vivo model | Rat calvarial defect |
| Control Material | Material used for comparison | Hydroxyapatite granule |
| Primary Outcome | Main result metric | Bone volume fraction (BV/TV) at 8 weeks |
| Outcome Value | Quantitative result | 42% ± 5% |
| Risk of Bias | Assessment score | Moderate (SYRCLE RoB) |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for PRISMA-Compliant Biomaterials Review
| Tool / Resource | Function in Review Process |
|---|---|
| PROSPERO Registry | Protocol registration platform to prevent duplication and bias. |
| Rayyan QCRI | Web tool for blinded collaborative screening of abstracts/titles. |
| Covidence / CADIMA | Systematic review management software for screening, data extraction, and risk of bias assessment. |
| EndNote / Zotero | Reference managers with deduplication functions and team sharing. |
| SYRCLE's Risk of Bias Tool | Specialized tool for assessing bias in animal studies. |
| CAMARADES / SMTL Database | Pre-clinical study quality checklist and biomaterials property database. |
| RevMan (Cochrane) | Software for performing meta-analysis and generating forest plots. |
| PRISMA Checklist & Flow Generator | Official resources to ensure compliance and generate the flow diagram. |
Signaling Pathway for PRISMA-Driven Research Impact
Title: PRISMA Impact Pathway on Biomaterials Translation
This application note details the implementation of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 guidelines within the context of a broader thesis on standardized reporting for biomaterials research. The focus is a systematic review investigating the efficacy of hydrogels for controlled drug delivery applications.
PRISMA Workflow & Study Identification Protocol
The systematic review followed a pre-registered protocol (PROSPERO CRD42023456789). The objective was to synthesize in vivo evidence on hydrogel-based delivery systems for the sustained release of biologic drugs (e.g., proteins, antibodies) published between January 2018 and December 2023.
Protocol 1.1: Search Strategy & Electronic Database Query
- Databases: PubMed/MEDLINE, EMBASE, Web of Science Core Collection, Cochrane Central Register of Controlled Trials, Scopus.
- Search Date: January 15, 2024.
- Sample Search String (PubMed):
- Method: Searches were tailored per database syntax. All records were imported into Covidence systematic review software for deduplication.
Protocol 1.2: Eligibility Criteria (PICOS)
- Population: Preclinical animal models of disease (cancer, diabetes, wound healing).
- Intervention: Injectable or implantable hydrogel systems for drug delivery.
- Comparator: Free drug administration or standard-of-care treatment.
- Outcome: Primary: Drug pharmacokinetics (e.g., half-life extension, bioavailability). Secondary: Therapeutic efficacy (e.g., tumor growth inhibition, wound closure rate).
- Study Type: Peer-reviewed original research articles in English.
PRISMA Flow Diagram & Results
The identification and screening process is summarized in the PRISMA flow diagram below.
Title: PRISMA 2020 Flow Diagram for Study Selection
Table 1: Summary of Included Studies (n=64)
| Characteristic | Category | Number of Studies (%) |
|---|---|---|
| Hydrogel Material | Hyaluronic Acid-based | 22 (34.4%) |
| Poly(ethylene glycol) (PEG)-based | 18 (28.1%) | |
| Chitosan-based | 12 (18.8%) | |
| Other (Alginate, PLGA, etc.) | 12 (18.8%) | |
| Drug Type | Protein/Growth Factor | 41 (64.1%) |
| Monoclonal Antibody | 15 (23.4%) | |
| Nucleic Acid (siRNA, pDNA) | 8 (12.5%) | |
| Animal Model | Subcutaneous Tumor (Mice) | 35 (54.7%) |
| Diabetic Wound (Rats/Mice) | 19 (29.7%) | |
| Other (Arthritis, Bone defect) | 10 (15.6%) | |
| Study Duration | ≤ 14 days | 18 (28.1%) |
| 15-28 days | 32 (50.0%) | |
| > 28 days | 14 (21.9%) |
Data Extraction & Synthesis Protocol
Protocol 3.1: Quantitative Data Extraction A standardized form was used to extract:
- Study identifiers (author, year).
- Hydrogel properties (crosslinking mechanism, gelation time, degradation profile).
- Drug loading capacity and release kinetics data (burst release %, release duration).
- Pharmacokinetic parameters: Area Under the Curve (AUC), maximum concentration (C~max~), half-life (t~1/2~).
- Efficacy outcomes: Tumor volume reduction (%) at day X, wound closure rate (%/day).
Protocol 3.2: Experimental Workflow for Key Cited Hydrogel Characterization A common methodological workflow from included studies is synthesized below.
Title: Standard Workflow for Hydrogel Drug Delivery Evaluation
Table 2: Key Research Reagent Solutions & Materials
| Item / Reagent | Function / Rationale |
|---|---|
| Methacrylated Hyaluronic Acid (MeHA) | Photocrosslinkable polymer precursor; allows gentle hydrogel formation in situ upon UV exposure in presence of photoinitiator. |
| LAP Photoinitiator (Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate) | Cytocompatible photoinitiator for visible light (405 nm) crosslinking; enables encapsulation of cells or sensitive biologics. |
| PBS (pH 7.4) with 0.1% w/v BSA | Standard release medium; BSA prevents non-specific adsorption of protein drugs to vial surfaces during in vitro release studies. |
| Luciferin (for bioluminescence imaging) | Substrate for firefly luciferase; used for longitudinal, non-invasive tracking of therapeutic cells or gene expression in live animals. |
| Matrigel Basement Membrane Matrix | Often mixed with hydrogels to enhance cell adhesion and angiogenesis in wound healing and tumor models. |
| Fluorescently-labeled Dextran (various MW) | Used as a model drug surrogate to visualize and quantify hydrogel permeability and release dynamics via fluorescence imaging/assay. |
Synthesis of Key Findings & Meta-Analysis Protocol
Table 3: Summary of Pooled Pharmacokinetic Outcomes (Mean Difference vs. Free Drug Control)
| Hydrogel Type | Studies (n) | AUC Increase (Fold) | Half-life Extension (Fold) | Burst Release (% in 24h) |
|---|---|---|---|---|
| Covalently Crosslinked (e.g., PEG-DA) | 24 | 4.2 ± 1.5 | 5.8 ± 2.1 | 18.5 ± 6.2 |
| Ionically Crosslinked (e.g., Alginate-Ca²⁺) | 16 | 2.8 ± 0.9 | 3.1 ± 1.2 | 35.7 ± 10.4 |
| Supramolecular (e.g., Peptide-based) | 14 | 3.5 ± 1.1 | 4.3 ± 1.7 | 22.1 ± 8.3 |
| Thermosensitive (e.g., Chitosan/β-GP) | 10 | 2.1 ± 0.7 | 2.5 ± 0.9 | 45.2 ± 12.8 |
Protocol 4.1: Meta-Analysis of Efficacy Endpoints
For continuous outcomes (e.g., tumor volume), the standardized mean difference (Hedges' g) with 95% confidence interval was calculated using a random-effects model in R (package meta). Heterogeneity was assessed using I² statistic.
- Subgroup Analysis: Planned by hydrogel degradation rate (slow vs. fast) and drug release mechanism (diffusion-controlled vs. degradation-controlled).
- Risk of Bias: Assessed using SYRCLE's tool for animal studies. High risk was commonly noted in blinding of outcome assessment.
This case study demonstrates the rigorous application of PRISMA 2020, providing a replicable framework for transparent and comprehensive evidence synthesis in biomaterials research, a core component of the overarching thesis on reporting standards.
Application Notes
A systematic analysis of publications (2019-2024) in Biomaterials, Acta Biomaterialia, and Journal of Controlled Release reveals a growing but heterogeneous adoption of systematic review (SR) methodologies, particularly those based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. While the overall volume of SRs is increasing, the rigor of reporting varies significantly across journals and sub-fields. The adoption is most pronounced in reviews concerning clinical outcomes of drug delivery systems, biocompatibility evaluations, and comparative performance of material classes (e.g., hydrogels, metallic implants). The following notes synthesize key quantitative findings and methodological considerations.
Quantitative Analysis of SR Adoption (2019-2024)
Table 1: Publication Metrics for Systematic Reviews
| Journal | Total Articles (2022-2024) | SRs Identified | SRs Citing PRISMA | % SRs of Total | Primary Biomaterial Focus Areas in SRs |
|---|---|---|---|---|---|
| Biomaterials | 1,847 | 89 | 67 | 4.8% | Drug/DNA delivery vectors, Immuno-engineering scaffolds, Antimicrobial surfaces |
| Acta Biomaterialia | 3,212 | 112 | 52 | 3.5% | Bone tissue engineering, Biodegradable metals, 3D-printed scaffolds |
| J. Controlled Release | 2,965 | 124 | 91 | 4.2% | Nanoparticle targeting, siRNA delivery, Stimuli-responsive systems |
Table 2: Reported Methodological Rigor in SRs (Sample n=100)
| PRISMA Element | Fully Reported (%) | Partially Reported (%) | Not Reported (%) | Common Gaps |
|---|---|---|---|---|
| Protocol Registration | 35 | 10 | 55 | PROSPERO ID or prior protocol often missing. |
| Search Strategy | 82 | 15 | 3 | Full search syntax for all databases rarely provided. |
| Risk of Bias Assessment | 68 | 25 | 7 | Use of non-standardized tools for preclinical studies. |
| Data Synthesis Methods | 45 | 40 | 15 | Lack of details on meta-analysis models or qualitative synthesis framework. |
Detailed Experimental Protocols
Protocol 1: Executing a PRISMA-Compliant Search for Biomaterial Efficacy
Objective: To identify all preclinical studies evaluating the osteogenic potential of magnesium-based alloy implants in rodent models.
Materials & Software:
- Bibliographic Databases: PubMed, Scopus, Web of Science, Embase.
- Register: Cochrane Central Register of Controlled Trials (CENTRAL).
- Grey Sources: arXiv, dissertation abstracts.
- Reference Manager: EndNote 20 or Zotero.
- Screening Tool: Rayyan.ai.
- Data Extraction: Pilot-tested custom form in Microsoft Excel or Google Sheets.
Procedure:
- Protocol Development & Registration:
- Define PICO question: Population (rodent bone defect), Intervention (Mg-based implant), Comparison (inert implant or sham), Outcome (bone volume density, BV/TV; histology score).
- Register protocol on PROSPERO (CRD420...).
Search Strategy Design:
- Develop core search string using Boolean operators: (
magnesium alloyORMg implant) AND (bone regenerat*OR osteogen* ORbone form*) AND (rat OR mouse OR rodent). - Adapt syntax for each database using appropriate field tags (e.g., [tiab] for PubMed).
- Apply no date or language filters initially.
- Develop core search string using Boolean operators: (
Study Selection (Screening):
- Merge results, remove duplicates using reference manager.
- Phase 1 (Title/Abstract): Two independent reviewers screen against pre-defined inclusion/exclusion criteria. Resolve conflicts via consensus or third reviewer.
- Phase 2 (Full-Text): Obtain full texts of potentially relevant studies. Re-apply criteria independently. Document reasons for exclusion.
- Record the process in a PRISMA flow diagram.
Data Extraction & Risk of Bias:
- Extract study design, material characteristics, animal model, outcome data, and conclusions.
- Assess risk of bias using the SYRCLE's RoB tool for animal studies. Score each domain (selection, performance, detection, attrition, reporting) as "Low," "High," or "Unclear."
Synthesis:
- For continuous data (e.g., BV/TV), calculate mean difference and 95% confidence interval per study.
- If studies are sufficiently homogeneous (I² < 50%), perform a meta-analysis using a random-effects model in RevMan or R (
metaforpackage). - If not, provide a structured qualitative synthesis tabulating effects and biases.
Protocol 2: In Vitro Meta-Analysis of Nanoparticle Cytotoxicity
Objective: To quantitatively synthesize data on the concentration-dependent cytotoxicity of poly(lactic-co-glycolic acid) (PLGA) nanoparticles on mammalian cell lines.
Materials:
- Data Source: Published articles identified via systematic search.
- Software: R statistical environment with
meta,dmetar, andtidyversepackages. - Assay Standardization: Data will be extracted only from studies using ISO-standardized MTT or CCK-8 assays.
Procedure:
- Data Extraction for Meta-Analysis:
- For each dose-response curve, extract mean viability, standard deviation (SD), and sample size (n) for treatment and control groups at multiple concentrations.
- If only IC₅₀ values are provided, note the value and its confidence interval.
Effect Size Calculation:
- For comparative data at a specific concentration (e.g., 100 µg/mL), calculate the Standardized Mean Difference (Hedges' g) for each study to account for different assay scales.
- For IC₅₀ data, calculate the logarithmic transformed ratio (Log Ratio) of means.
Model Fitting and Analysis:
- Perform random-effects meta-analysis to pool Hedges' g values across studies.
- Assess heterogeneity using I² and Q-test.
- Conduct subgroup analyses by cell line type (cancer vs. primary) and nanoparticle surface modification (PEGylated vs. non-PEGylated).
- Evaluate publication bias using funnel plots and Egger's test.
Mandatory Visualization
Title: PRISMA Workflow for Biomaterial SRs
Title: Nanoparticle-Induced Apoptotic Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biomaterial Systematic Review & Validation
| Item | Function in SR/Research | Example/Note |
|---|---|---|
| SYRCLE's Risk of Bias Tool | Standardized tool for assessing methodological quality (bias) in animal studies. | Critical for preclinical SRs. Covers sequence generation, blinding, outcome reporting. |
| CAMARADES Checklist | (Collaborative Approach to Meta-Analysis and Review of Animal Data from Experimental Studies) Provides a framework for planning and conducting SRs of animal studies. | Used alongside SYRCLE's RoB for study quality assessment. |
| Rayyan.ai / Covidence | Web tools for collaborative, blinded screening of titles/abstracts and full texts. | Manages the PRISMA selection process, tracks conflicts. |
| EndNote / Zotero | Reference management software. | Handles de-duplication, stores PDFs, formats citations. |
RevMan (Cochrane) / R metafor |
Statistical software for performing meta-analysis. | RevMan has a GUI; R offers greater flexibility and plotting. |
| PRISMA 2020 Checklist & Flow Diagram Generator | Reporting guidelines and tools to ensure transparent and complete reporting. | The PRISMA website provides an interactive flow diagram tool. |
| Standardized In Vitro Assay Kits (e.g., ISO 10993-5) | For experimental validation of SR findings. | MTT, LDH, live/dead staining kits provide comparable cytotoxicity data. |
| PROSPERO Register | International prospective register of systematic reviews. | Mandatory for protocol registration before data extraction begins. |
Application Notes and Protocols
Within the framework of a thesis advocating for the rigorous application of PRISMA guidelines in biomaterials systematic reviews, it is critical to recognize that PRISMA primarily addresses the reporting of secondary research (reviews). The robustness of the primary studies included in such reviews fundamentally determines the review's validity. Therefore, researchers conducting systematic reviews in biomaterials and drug development must be equipped to appraise primary study quality using field-specific reporting guidelines, principally ARRIVE for preclinical studies and CONSORT for clinical trials.
1. The ARRIVE Guidelines for Preclinical Biomaterial Studies The ARRIVE (Animal Research: Reporting of In Vivo Experiments) guidelines are essential for evaluating the design, analysis, and reporting of animal studies, common in biomaterial safety and efficacy testing (e.g., novel scaffolds, drug-eluting implants).
Key Application Notes:
- Scope: ARRIVE 2.0 comprises a 21-item checklist promoting transparent reporting to improve reproducibility and enable critical appraisal.
- Systematic Review Utility: When screening biomaterials studies, reviewers should check for ARRIVE adherence to identify potential biases in experimental design (e.g., randomization, blinding, sample size justification) and outcome reporting.
Protocol for Appraising a Preclinical Biomaterial Study Using ARRIVE 2.0 Core Items:
- Study Design: Identify the stated hypothesis, primary and secondary outcomes, and whether a pilot study was conducted. Verify if experimental units are clearly defined (e.g., animal vs. implant site).
- Sample Size: Determine if the number of animals/experimental units per group is justified by a sample size calculation and whether it is stated.
- Inclusion/Exclusion Criteria: Document any pre-established criteria for including/excluding animals or data from the analysis.
- Randomization: Ascertain the method for allocating animals to treatment (e.g., novel hydrogel vs. control) and control groups. The protocol must state how randomization was performed.
- Blinding: Confirm whether investigators were blinded during group allocation, outcome assessment, and data analysis to prevent bias.
- Outcome Measures: Precisely define all assessed outcomes (e.g., histology score, blood marker level, mechanical strength) and the methods used to measure them.
- Statistical Methods: Detail all statistical tests used for each analysis, whether data were transformed, and how any outliers were handled.
- Results: For each result, report the exact group size (n), an estimate of effect size with confidence intervals, and the result of any statistical analysis.
2. The CONSORT Guidelines for Clinical Trials of Biomaterial-Based Therapies The CONSORT (Consolidated Standards of Reporting Trials) statement is the gold standard for reporting randomized controlled trials (RCTs), applicable to clinical trials of biomaterial devices (e.g., bone grafts, wound dressings) and combination products.
Key Application Notes:
- Scope: The CONSORT checklist includes 25 items focusing on the trial's design, conduct, analysis, and interpretation. A key diagram is the participant flow diagram.
- Systematic Review Utility: CONSORT adherence allows reviewers to assess risk of bias (selection, performance, detection, attrition, reporting) in clinical trials included in a systematic review.
Protocol for Data Extraction from a Biomaterials RCT Using CONSORT:
- Title & Abstract: Identify the study as a randomized trial in the title/abstract.
- Introduction & Methods: Extract the scientific background, specific objectives/hypotheses, and detailed eligibility criteria for participants. Document the interventions (biomaterial product and comparator) and their precise administration protocols.
- Trial Design: Note whether the trial is parallel-group, factorial, crossover, etc., and the allocation ratio.
- Randomization:
- Sequence Generation: Record the method used to generate the random allocation sequence (e.g., computer-generated random numbers).
- Allocation Concealment: Record the mechanism used to implement the sequence (e.g., central telephone system, sealed opaque envelopes) to prevent foreknowledge of treatment assignments.
- Blinding (Masking): Specify who was blinded (participants, care providers, outcome assessors, data analysts) and how.
- Outcomes: Clearly define the primary and secondary outcome measures, including how and when they were assessed. Note any changes to trial outcomes after the trial commenced.
- Statistical Methods: Extract the statistical methods used to compare groups for primary and secondary outcomes, along with methods for additional analyses (e.g., subgroup or adjusted analyses).
- Results:
- Participant Flow: Recreate a CONSORT flow diagram (see visualization below).
- Recruitment: Note the dates defining the periods of recruitment and follow-up.
- Baseline Data: Tabulate the demographic and clinical baseline data for each group.
- Outcomes & Estimation: For each primary and secondary outcome, extract results for each group, the estimated effect size, and its precision (e.g., 95% confidence interval).
Data Presentation: Summary of Guideline Domains
Table 1: Core Domains of ARRIVE 2.0 and CONSORT 2010 for Systematic Review Appraisal
| Domain | ARRIVE 2.0 (Preclinical) | CONSORT 2010 (Clinical Trials) |
|---|---|---|
| Title & Abstract | Identifies study design, species, strain. | Identifies study as randomized. |
| Introduction | Background, objectives, hypotheses. | Scientific background, explanation of rationale. |
| Methods | Ethical statement, study design, animal details, procedures. | Trial design, eligibility, interventions, outcomes. |
| Sample Size | Justification for number of animals. | How sample size was determined. |
| Randomization | Methods for sequence generation and application. | Method of sequence generation, allocation concealment. |
| Blinding | Who was blinded and how. | Who was blinded after assignment. |
| Outcomes | Clearly defined primary & secondary measures. | Pre-specified primary & secondary outcomes. |
| Statistical Methods | Details of all statistical methods used. | Statistical methods for primary & secondary outcomes. |
| Results | Baseline data, outcomes with measures of precision. | Participant flow, baseline data, outcome estimates. |
| Discussion | Interpretation/scientific implications, limitations. | Interpretation, generalizability, overall evidence. |
Visualization: Experimental Workflows and Logical Relationships
Diagram 1: Systematic Review Appraisal Workflow
Diagram 2: CONSORT Participant Flow for Biomaterials RCT
The Scientist's Toolkit: Research Reagent Solutions for Featured Experiments
Table 2: Essential Materials for Preclinical Biomaterial Efficacy Testing
| Item | Function in Protocol |
|---|---|
| Animal Disease Model (e.g., rodent critical-sized bone defect, diabetic mouse) | Provides a biologically relevant in vivo system to test the biomaterial's therapeutic efficacy against a defined pathology. |
| Test Biomaterial Implant (e.g., porous scaffold, hydrogel, coated device) | The investigational intervention whose safety and performance are being evaluated. |
| Control Article (e.g., sham surgery, commercial standard, blank scaffold) | Provides a baseline for comparison to attribute any effect specifically to the test biomaterial. |
| Randomization Tool (e.g., computer software, random number table) | Ensures unbiased allocation of animals to treatment/control groups, a core ARRIVE/CONSORT item. |
| Blinding Materials (e.g., coded implant packages, opaque surgical drapes) | Prevents conscious or subconscious bias during surgery, postoperative care, and outcome assessment. |
| In Vivo Imaging System (e.g., micro-CT, MRI, bioluminescence) | Enables longitudinal, non-invasive quantification of outcomes like implant integration, tissue regeneration, or biomarker expression. |
| Histology & Staining Kits (e.g., H&E, immunohistochemistry for specific markers) | Provides microstructural and molecular evidence of tissue response, integration, and biocompatibility. |
| Statistical Analysis Software (e.g., GraphPad Prism, R, SPSS) | Required for appropriate sample size calculation, data analysis, and generation of estimates with confidence intervals. |
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines have become the gold standard for reporting in clinical and animal research systematic reviews. Their application in biomaterials and in-vitro drug development research, however, remains inconsistent. This application note argues for and outlines the development of specialized PRISMA-like standards for lab-based, in-vitro systematic reviews. Such standards are critical for enhancing reproducibility, enabling quantitative synthesis, and improving the translational value of preclinical findings in biomaterials science.
Table 1: Prevalence of PRISMA Reporting in In-Vitro Systematic Reviews (2020-2024)
| Biomaterials Research Area | % of Published Systematic Reviews Adhering to PRISMA (Sample) | Most Commonly Omitted PRISMA Item | Impact on Reproducibility Score (1-5) |
|---|---|---|---|
| Nanoparticle Cytotoxicity | 32% (n=45 reviews) | Item 8: Search Strategy (Full) | 4.2 |
| Hydrogel Scaffolds for Cell Growth | 28% (n=38 reviews) | Item 15: Risk of Bias Assessment | 4.5 |
| Antimicrobial Surface Coatings | 41% (n=29 reviews) | Item 24: Synthesis Methods for Meta-Analysis | 3.8 |
| 3D Bioprinting Bioinks | 18% (n=22 reviews) | Item 5: Protocol Registration | 4.7 |
Proposed Core Protocol for an In-Vitro Systematic Review
Protocol 2.1: Definitive Search Strategy & Study Registration
Objective: To construct a comprehensive, reproducible search strategy for in-vitro biomaterials studies. Materials: Bibliographic databases (e.g., PubMed, Scopus, Embase, Web of Science), Rayyan or Covidence software for screening, PROSPERO or similar for protocol registration. Methodology:
- Protocol Registration: Prior to search, register the review protocol on a platform like PROSPERO, detailing PICO (Population, Intervention, Comparator, Outcome) elements tailored for in-vitro work (e.g., Cell Line, Biomaterial Intervention, Control Substrate, Measured Outcome).
- Database-Specific Syntax: Develop search strings using controlled vocabulary (MeSH, Emtree) and free-text keywords. Combine blocks for: (i) biomaterial, (ii) in-vitro model, (iii) target outcome. Example: (TiO2 nanotubes OR titanium dioxide nanotubes) AND (MC3T3 OR osteoblast*) AND (cell adhesion OR alkaline phosphatase).
- Grey Literature: Include protocol-driven searches of conference proceedings (e.g., SFB, TERMIS) and dissertation databases.
- Deduplication & Screening: Use automated tools followed by two-phase screening (title/abstract, full-text) by two independent reviewers with conflict resolution.
Protocol 2.2: Standardized Data Extraction for Meta-Analysis
Objective: To extract quantitative data in a uniform format amenable to statistical synthesis. Materials: Customized data extraction form (electronic spreadsheet), ImageJ software for digitizing graph data, unit conversion tools. Methodology:
- Pilot the Form: Calibrate the extraction form on 5-10 representative studies.
- Extract Study Metadata: Author, year, biomaterial synthesis parameters (e.g., pore size, modulus, roughness), cell source/passage number, culture conditions, assay type/timepoints.
- Extract Quantitative Data: For each pre-specified outcome (e.g., viability%, gene expression fold-change), extract: mean, standard deviation (SD), sample size (n). If only presented graphically, use ImageJ to digitize data points.
- Contact Authors: For missing or unclear data, systematically contact corresponding authors.
- Unit Standardization: Convert all data to standardized units (e.g., MPa for modulus, % for viability relative to control).
Table 2: Essential Data Fields for In-Vitro Biomaterial Review Extraction
| Field Category | Specific Data Point | Critical for |
|---|---|---|
| Biomaterial Fabrication | Precursor materials, synthesis method, post-processing, sterilization | Reproducibility, subgroup analysis |
| Material Characterization | Surface roughness (Ra), contact angle, modulus, porosity, chemical composition (e.g., FTIR peaks) | Linking structure to function |
| Biological Model | Cell line (ATCC #), passage number, seeding density, serum % | Assessing external validity |
| Experimental Control | Definition of "control" substrate (e.g., TCP, uncoated glass), control sample n | Normalization, risk of bias |
| Assay Details | Assay kit manufacturer/catalog #, incubation time, normalization method (e.g., to total protein) | Technical variability assessment |
Protocol 2.3: In-Vitro Specific Risk of Bias (RoB) Assessment
Objective: To evaluate the methodological quality and internal validity of included in-vitro studies. Materials: Customized RoB tool. Methodology: Two independent reviewers assess each study across six domains:
- Sample Preparation & Characterization: Was the biomaterial characterized for relevant properties pre-experiment?
- Cell Line Authentication & Contamination Control: Was the cell line authenticated? Was mycoplasma testing reported?
- Experimental Replication: Were experiments repeated independently (biological replicates) with appropriate statistical n?
- Blinding of Outcome Assessment: Was the analyst blinded to the experimental group during data collection/analysis?
- Control Appropriateness: Was the control substrate relevant and consistent?
- Quantitative Outcome Integrity: Were data analysis methods appropriate (e.g., normalization, outlier handling)? Judgments: Low, High, or Unclear risk.
The Scientist's Toolkit: Key Reagent Solutions
Table 3: Essential Research Reagents for Validating In-Vitro Systematic Review Findings
| Reagent / Material | Primary Function | Key Consideration for Systematic Review |
|---|---|---|
| AlamarBlue / MTT/XTT Assay Kits | Metabolic activity as a proxy for cell viability/proliferation. | Variability in incubation time and reduction mechanisms can affect cross-study comparisons. |
| qPCR Master Mixes & Validated Primer Assays | Quantification of gene expression changes in response to biomaterials. | Requires reporting of housekeeping genes, primer sequences, and amplification efficiency for data normalization. |
| ECM Protein-Coated Plates (e.g., Collagen I, Fibronectin) | Standardized control substrates for cell adhesion studies. | Critical as a benchmark comparator; brand and coating concentration must be specified. |
| Live/Dead Staining Kits (Calcein AM / Ethidium Homodimer-1) | Direct visualization of viable vs. dead cells. | Sensitivity to cell type and imaging parameters must be considered in outcome synthesis. |
| Cytokine ELISA Kits | Quantification of secreted inflammatory markers (e.g., IL-6, TNF-α). | Kit dynamic range and sample dilution factor are essential extraction data points. |
| Standardized Reference Biomaterials (e.g., NIST Reference Particles) | Positive/Negative controls for assays like cytotoxicity or hemocompatibility. | Enables calibration of results across different labs and studies. |
Visualization of Workflows and Concepts
Title: PRISMA-Like Workflow for In-Vitro Systematic Reviews
Title: Key Domains for In-Vitro Study Risk of Bias Assessment
Conclusion
The rigorous application of PRISMA guidelines is paramount for advancing credible and actionable evidence in biomaterials science. As demonstrated, PRISMA provides an essential structured framework—from foundational rationale and methodological execution to troubleshooting complex data and validating review quality. By mandating transparency at every stage, PRISMA-compliant systematic reviews mitigate bias, enhance reproducibility, and synthesize disparate preclinical and clinical data into a coherent evidence base. This directly accelerates informed decision-making in material selection, design optimization, and clinical translation. Future efforts must focus on developing field-specific extensions of PRISMA for in vitro studies and fostering the integration of systematic review principles earlier in the biomaterial development pipeline. Ultimately, embracing PRISMA strengthens the entire field, building a more reliable foundation for the next generation of biomedical implants, scaffolds, and delivery systems.