Preventing Fibrotic Encapsulation of Breast Implants: Molecular Mechanisms, Biomaterial Innovations, and Therapeutic Strategies
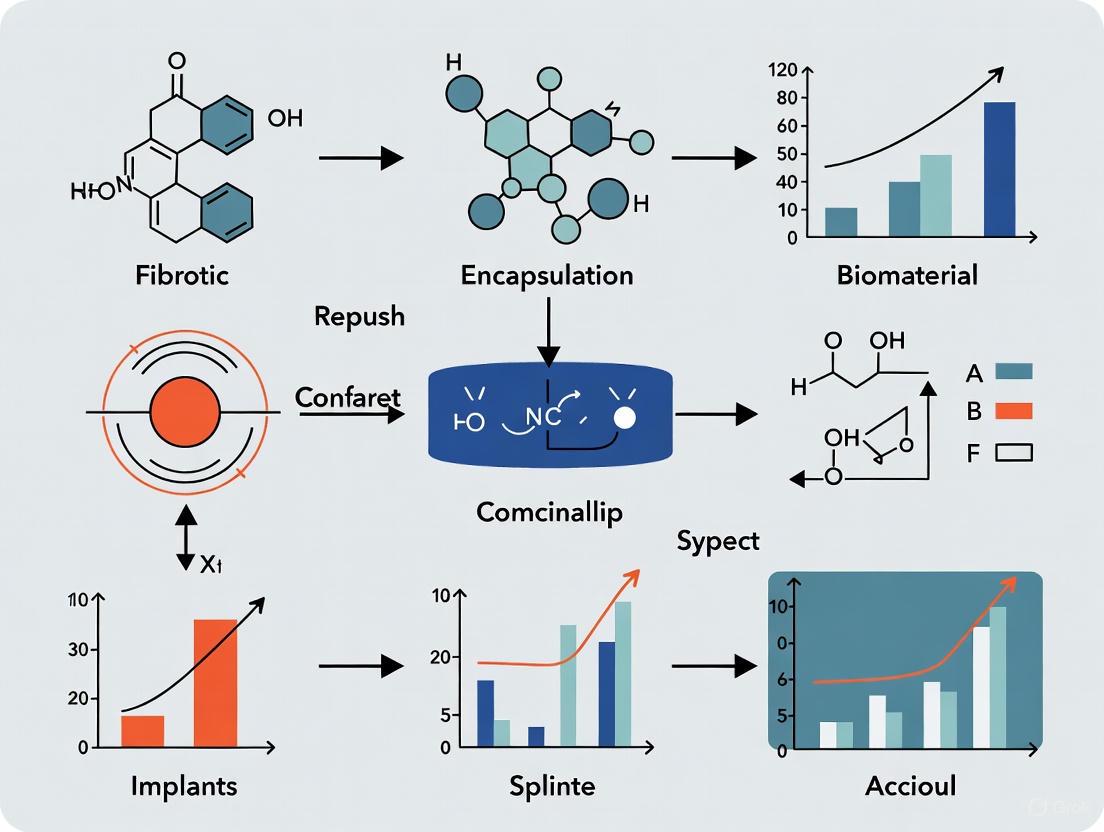
This review provides a comprehensive analysis of the pathophysiological mechanisms and emerging strategies to prevent fibrotic encapsulation of breast implants, a major complication leading to capsular contracture.
Preventing Fibrotic Encapsulation of Breast Implants: Molecular Mechanisms, Biomaterial Innovations, and Therapeutic Strategies
Abstract
This review provides a comprehensive analysis of the pathophysiological mechanisms and emerging strategies to prevent fibrotic encapsulation of breast implants, a major complication leading to capsular contracture. Tailored for researchers, scientists, and drug development professionals, we synthesize foundational science on the foreign body response, exploring the critical roles of mechanical signaling, TGF-β activation, and immune cell interplay. The article details methodological advances in biomaterial engineering, including surface topography, soft coatings, and immunomodulatory approaches. We further evaluate troubleshooting for clinical challenges and validate strategies through comparative analysis of preclinical and clinical data, offering a roadmap for developing next-generation implants and targeted anti-fibrotic therapies.
Decoding the Foreign Body Response: Cellular and Molecular Drivers of Implant Fibrosis
{css}
/* Technical Support Center: The Fibrotic Cascade */
Fibrotic Cascade Technical Support Center
Troubleshooting Guides
Low Cell Yield from Capsule Tissue Digestion
Problem: After enzymatic digestion of breast implant capsule tissue, the resulting cell yield is low, hindering subsequent analysis.
- Check Tissue Processing: Ensure the tissue is thoroughly minced into fragments smaller than 1 mm before digestion to maximize surface area for enzyme action [1].
- Verify Enzyme Activity: Confirm that the collagenase solution was freshly prepared or properly aliquoted and stored to prevent loss of activity. The standard concentration used is 0.75 mg/mL [1].
- Optimize Digestion Time: The standard digestion period is 1 hour at 37°C. Over-digestion can damage cells, while under-digestion reduces yield [1].
- Validate Cell Sorting Markers: When sorting fibroblast subpopulations, ensure the use of validated antibody panels. A common combination is CD26 (a fibrogenic marker) with vimentin (a pan-fibroblast marker) for identification [1].
High Background in Immunofluorescence (IF) Staining
Problem: High background fluorescence obscures specific signal when staining for markers like α-SMA or CD26 in capsular tissue sections.
- Confirm Antibody Compatibility: Ensure the secondary antibody is specific to the host species of the primary antibody and is not cross-reacting with other tissue elements [2].
- Optimize Blocking: Use an appropriate blocking solution (e.g., 1% Power Block) for at least 2 hours at room temperature to reduce non-specific binding [1].
- Titrate Antibodies: The concentration of both primary and secondary antibodies may need optimization. A common starting dilution for primary antibodies is 1:200 [1].
- Include Controls: Always run negative controls (omitting the primary antibody) to distinguish specific staining from background [2].
Frequently Asked Questions (FAQs)
Q1: What are the key cellular players in the fibrotic cascade around breast implants? A1: The process involves an orchestrated response from immune cells and structural cells. Initially, neutrophils and macrophages respond to the implant. Subsequently, fibroblasts are activated and can differentiate into myofibroblasts, which are the primary collagen-producing cells responsible for capsule formation and contraction. A specific subpopulation of pro-fibrotic fibroblasts marked by CD26 has been identified as being particularly responsible for collagen production [1] [3] [4].
Q2: What is the central signaling pathway driving myofibroblast differentiation? A2: The Transforming Growth Factor-beta (TGF-β) pathway is the prototypical driver. It operates through both canonical (Smad-dependent) and non-canonical (e.g., MAPK/JNK/p38) signaling pathways to activate the genetic program for myofibroblast differentiation, leading to increased expression of α-SMA, collagens, and fibronectin [5] [3].
Q3: How does implant surface topography influence the fibrotic response? A3: Surface texture is a critical determinant of the host immune response. Roughness influences protein adsorption, immune cell activation, and cytokine profiles. Implants with an average roughness of ~4 µm have been shown to elicit less inflammation and thinner fibrous capsules compared to rougher surfaces, which can trigger a stronger pro-fibrotic TH1/TH17 immune response [6].
Q4: What are the essential controls for a reliable fibroblast activation experiment? A4:
- Positive Control: Treat fibroblasts with a known activator like TGF-β (e.g., 2-10 ng/mL) to ensure the system can detect differentiation.
- Negative Control: Use untreated fibroblasts to establish a baseline activation state.
- Technical Control: Include a housekeeping gene (e.g., GAPDH, β-actin) in gene expression analyses (qPCR) to normalize data [5].
The table below consolidates key quantitative findings from recent research on capsular fibrosis.
Table 1: Key Experimental Findings in Capsular Fibrosis Research
| Parameter | Finding | Experimental Context | Source |
|---|---|---|---|
| CD26+ Fibroblast Collagen Production | Produced more collagen than CD26- fibroblasts | Cell sorting and culture from human breast capsules | [1] |
| Critical Surface Roughness (Ra) | ~4 µm associated with least inflammation and fibrosis | Comparison of silicone implants in patients | [6] |
| Enzymatic Digestion Concentration | 0.75 mg/mL collagenase | Digestion of human breast capsule tissue for FACS | [1] |
| Primary Antibody Dilution (IF) | 1:200 | Immunofluorescence on human breast capsule sections | [1] |
| Key Gene Expression in CD26+ Fibroblasts | Increased IL8, TGF-β1, COL1A1, TIMP4 | qPCR on sorted fibroblast populations from human capsules | [1] |
Experimental Protocols
Protocol: Flow Cytometry Analysis of Capsular Fibroblasts
This protocol details the process for isolating and characterizing fibroblast subpopulations from human breast implant capsule tissue [1].
1. Tissue Digestion:
- Thoroughly mince the freshly obtained capsule specimen into fragments <1 mm.
- Enzymatically digest the tissue using 0.75 mg/mL collagenase from Clostridium histolyticum in a digest buffer (e.g., with 5% FBS and DNase I).
- Incubate for 1 hour at 37°C with gentle agitation (120 rpm).
2. Cell Sorting (FACS):
- Resuspend the resulting single-cell suspension.
- Incubate cells with fluorescently conjugated antibodies against target surface markers (e.g., anti-CD26 to identify pro-fibrotic fibroblasts, anti-vimentin as a pan-fibroblast marker).
- Use a fluorescence-activated cell sorter to isolate the CD26-positive and CD26-negative fibroblast populations for downstream functional assays.
3. Downstream Analysis:
- Culture the sorted fibroblasts to assess collagen production.
- Extract RNA to analyze gene expression of fibrotic markers (e.g., IL8, TGF-β1, COL1A1, TIMP4) via qPCR.
Protocol: Immunofluorescence Staining for Myofibroblasts
This protocol is used to visualize and confirm the presence of activated myofibroblasts in capsular tissue sections [1].
1. Tissue Preparation:
- Fix capsule tissue specimens immediately in 4% paraformaldehyde for 16 hours at 4°C.
- Cryoprotect by immersing in 30% sucrose for 5 days before embedding in OCT compound.
- Section the OCT blocks into 6-μm thick slices using a cryostat.
2. Staining Procedure:
- Permeabilize tissue sections with 0.2% Triton X-100 for 30 minutes.
- Block sections with 1% blocking solution for 2 hours at room temperature.
- Incubate with primary antibodies (e.g., anti-α-SMA for myofibroblasts, anti-CD26) diluted in blocking solution (1:200) for 18 hours at 4°C.
- Wash sections and incubate with appropriate fluorescent secondary antibodies (e.g., diluted 1:4000) for 1 hour at room temperature.
- Mount slides with a DAPI-containing medium to counterstain nuclei.
3. Imaging:
- Image the stained sections using a confocal microscope.
- Analyze for co-localization of markers (e.g., α-SMA and CD26) to identify activated pro-fibrotic fibroblast populations.
Pathway and Workflow Visualizations
The Core Fibrotic Signaling Pathway
Fibroblast Isolation & Analysis Workflow
The Scientist's Toolkit
Table 2: Essential Research Reagents for Fibrosis Studies
| Reagent / Material | Function / Application | Example / Note |
|---|---|---|
| Collagenase | Enzymatic digestion of fibrous capsule tissue to isolate cells. | From Clostridium histolyticum; used at 0.75 mg/mL [1]. |
| Anti-CD26 Antibody | Identification and sorting of a pro-fibrotic fibroblast subpopulation. | Rabbit anti-CD26; used for Immunohistochemistry and FACS [1]. |
| Anti-α-SMA Antibody | Marker for activated myofibroblasts; key indicator of fibrosis. | Used in immunofluorescence to visualize contractile cells [1] [3]. |
| Anti-Vimentin Antibody | Pan-fibroblast marker; identifies the general fibroblast population. | Goat anti-vimentin; often used in co-staining with CD26 [1]. |
| TGF-β1 Cytokine | Positive control to induce myofibroblast differentiation in vitro. | Typical working concentration of 2-10 ng/mL [5]. |
| Silicone Implants (Various Ra) | To study the effect of surface topography on the foreign body response. | Implants with defined roughness (e.g., Ra ~4µm vs. Ra ~60µm) [6]. |
| Sulfatroxazole | Sulfatroxazole | High-Purity Antibacterial Agent | Sulfatroxazole is a potent synthetic antibacterial compound for research use only (RUO). Explore its mechanism and applications. Not for human or veterinary use. |
| N-Acetylhistidine | N-Acetyl-L-histidine|High-Purity Research Compound | N-Acetyl-L-histidine for research applications. Study its role as a molecular water pump in models. For Research Use Only. Not for human consumption. |
FAQs: Immune Mechanisms in Capsular Fibrosis
1. What are the key macrophage phenotypes involved in the foreign body reaction to breast implants, and how do they influence capsular contracture?
The foreign body reaction (FBR) to breast implants is characterized by a dynamic interplay of macrophage phenotypes, primarily the pro-inflammatory M1 and the pro-repair M2 macrophages [7] [8].
- M1 Macrophages (CD68+NOS2+): Dominant in the acute inflammatory phase post-implantation. They are classically activated by bacterial components (e.g., via TLR4) or T-cell-derived IFN-γ. M1 macrophages boost inflammation by releasing cytokines like TNF-α, IL-1β, IL-6, and IL-8, and contribute to tissue damage via reactive oxygen species (ROS) and degradative enzymes [7] [9]. Sustained M1 activation is profibrotic.
- M2 Macrophages (CD68+CD206+): Predominant later in the FBR, activated by IL-4 and IL-13. They dampen inflammation and orchestrate tissue repair and fibrosis by producing vascular endothelial growth factor (VEGF) and the master fibrotic regulator, Transforming Growth Factor-beta (TGF-β) [7] [8]. A controlled M2 response is necessary for normal healing, but persistent activity drives excessive fibrosis.
An imbalance, particularly a prolonged M1-dominated response often linked to biofilm presence or chronic inflammation, leads to sustained cytokine release and TGF-β-driven fibroblast activation, resulting in capsular contracture [7] [8].
2. Which T-cell subsets are associated with promoting or preventing capsular contracture?
Both innate and adaptive immunity are involved in fibrogenesis, with specific T-helper (Th) cell subsets playing distinct roles [10] [8].
- Pro-Fibrotic Subsets: Th1 (secreting IFN-γ) and Th17 (secreting IL-17) responses are pro-inflammatory and associated with the M1 macrophage phenotype. Contracted capsules show greater infiltrates of Th1/Th17 T cells and express higher levels of TGF-β, IL-1, IL-6, and IL-17, directly contributing to capsular fibrosis [8]. Th2 cells (secreting IL-4 and IL-13) are linked to the M2 macrophage phenotype and are also involved in profibrotic wound repair [8].
- Anti-Fibrotic Subsets: A dominant Th2 response is generally considered profibrotic in other organ systems [11]. However, within the context of breast implant capsules, the Th2-driven M2 macrophage activation is stated to lead to less capsular contracture, highlighting the complexity and context-dependency of these pathways [8]. The role of regulatory T cells (Tregs) in breast capsules is less defined, though in other fibrotic diseases they often exhibit anti-fibrotic effects [10].
3. What are the primary experimental models for studying immune responses to implant surfaces?
- In Vivo Models: Rodent models (e.g., Wistar rats) are widely used to study capsule formation around implanted devices [12]. Researchers can control variables like implant surface topography (smooth, macrotextured, nanotextured), placement, and administration of therapeutic compounds.
- In Vitro Models: These involve culturing macrophages (e.g., cell lines like RAW 264.7 or primary human macrophages) with implant surface materials or conditioned media. This allows for controlled investigation of specific signaling pathways and cytokine production in response to different surface chemistries and topographies [9].
- Human Tissue Analysis: Capsular tissues from revision surgeries are analyzed using histology, immunohistochemistry, and molecular biology techniques to characterize immune cell infiltrates and cytokine profiles, providing direct human pathological data [7] [8].
4. Our histology shows a thick, collagen-dense capsule. What immune profiling should we perform to understand the driving mechanism?
Focus your analysis on key immune cells and fibrotic markers.
- Immunohistochemistry (IHC)/Immunofluorescence (IF): Quantify cell populations using specific antibodies.
- Western Blot/Quantitative PCR (qPCR): Analyze protein and gene expression levels of key cytokines and fibrotic mediators.
Table 1: Key Targets for Immune Profiling of Fibrotic Capsules
| Target | Cell Type / Process | Significance in Capsular Contracture |
|---|---|---|
| CD68 / NOS2 | M1 Macrophages | Indicates pro-inflammatory, profibrotic activation [7] |
| CD206 | M2 Macrophages | Indicates pro-repair, fibrotic activation [7] |
| CD3 / CD4 | T-Lymphocytes | General T-cell infiltration [8] |
| IFN-γ | Th1 Cells | Pro-inflammatory cytokine, linked to M1 polarization [8] |
| IL-17 | Th17 Cells | Pro-inflammatory, profibrotic cytokine [8] |
| TGF-β1 | Fibrosis Master Regulator | Potent driver of fibroblast-to-myofibroblast transition and collagen production [7] [12] |
| α-SMA | Myofibroblasts | Activated fibroblast responsible for contraction and ECM deposition [12] |
| Collagen I | Extracellular Matrix (ECM) | Primary component of the fibrous capsule [12] |
Troubleshooting Guides
Problem: Inconsistent macrophage polarization in in vitro assays.
- Potential Cause 1: Inadequate or variable stimulation. LPS and IFN-γ are required for robust M1 polarization, while IL-4 and IL-13 are essential for M2 polarization [9]. Check cytokine activity and concentrations.
- Solution: Use fresh, high-purity cytokines at established concentrations (e.g., 20-100 ng/mL LPS + 20-50 ng/mL IFN-γ for M1; 20-50 ng/mL IL-4 for M2). Include positive controls (e.g., known M1/M2 marker analysis via qPCR or flow cytometry).
- Potential Cause 2: Cell culture conditions affecting responsiveness. Serum batches can vary and contain polarizing factors.
- Solution: Use a consistent, well-characterized serum batch. Consider using serum-free media formulations designed for macrophage culture during the polarization stage.
Problem: High variability in capsule thickness in an animal model.
- Potential Cause 1: Surgical technique inconsistency leading to varying degrees of tissue trauma, bleeding, or contamination.
- Solution: Standardize the surgical procedure, including pocket creation, implant handling, and closure. Implement strict aseptic techniques to prevent subclinical infection, a known trigger for contracture [13] [8].
- Potential Cause 2: Uncontrolled implant movement or positioning.
- Solution: Ensure a properly sized pocket and consistent implant placement. Studies show implant movement varies with surface type, which can influence the FBR [12].
Experimental Protocols
Protocol 1: Evaluating the Effect of Implant Surface Topography on Capsule Formation (In Vivo)
This protocol is based on a study comparing smooth, macrotextured, and nanotextured implants [12].
- Animal and Grouping: Utilize 48 Wistar rats. Randomly divide them into 3 experimental groups (n=16 per group): Group A (Smooth implant), Group B (Macrotextured implant), Group C (Nanotextured implant). Each group is further divided into 4-week and 12-week endpoints.
- Implantation Surgery: Perform sterile surgery to insert one implant into a subcutaneous pocket on the rat's back. Administer standard post-operative analgesics.
- Tissue Harvest: At each endpoint, euthanize the animals and carefully explant the implant with the surrounding capsular tissue intact.
- Analysis:
- Histology: Fix tissue in formalin, embed in paraffin, and section. Perform:
- Immunohistochemistry (IHC): Stain sections for α-SMA (myofibroblasts) and TGF-β1 to assess fibrotic activity [12].
- Western Blot: Homogenize capsule tissue to quantify protein expression levels of TGF-β1 and other fibrosis markers [12].
Table 2: Key Reagents for Implant-Capsule Interaction Studies
| Research Reagent | Function/Application |
|---|---|
| Silicone Implants (Smooth, Macro, Nano) | The foreign body to trigger the FBR; variable topography is the independent variable [12]. |
| Anti-CD68 / Anti-NOS2 Antibodies | IHC/IF markers for identifying pro-inflammatory M1 macrophages [7]. |
| Anti-CD206 Antibodies | IHC/IF markers for identifying pro-repair M2 macrophages [7]. |
| Anti-α-SMA Antibody | Marker for activated myofibroblasts, the key contractile cell in fibrosis [12]. |
| Anti-TGF-β1 Antibody | Detects the master regulator of fibrosis via IHC or Western Blot [12]. |
| LPS & IFN-γ | In vitro stimulants for polarizing macrophages to the M1 phenotype [9]. |
| IL-4 & IL-13 | In vitro stimulants for polarizing macrophages to the M2 phenotype [9]. |
Protocol 2: In Vitro Macrophage Polarization in Response to Implant Surface Microparticles
- Macrophage Culture: Use a human macrophage cell line (e.g., THP-1 differentiated with PMA) or primary human monocyte-derived macrophages.
- Particle Generation & Treatment: Generate silicone microparticles from implant materials. Co-culture macrophages with varying concentrations of particles in culture media.
- Polarization Stimulation: After particle exposure, stimulate the cells with standard M1 (LPS + IFN-γ) or M2 (IL-4) polarizing cytokines for 24-48 hours.
- Analysis:
- qPCR: Isolate RNA and analyze expression of M1 markers (TNF-α, IL-1β, IL-6) and M2 markers (Arg1, Mrc1, Fizz1) [9].
- ELISA: Collect cell culture supernatant and measure secretion of key cytokines like TNF-α (M1) or TGF-β (M2/fibrosis).
- Flow Cytometry: Harvest cells and stain for surface markers CD80/86 (M1) and CD206 (M2) for quantification of populations.
Signaling Pathway Visualizations
Macrophage Polarization Signaling
T-cell Macrophage Crosstalk
FAQs: Troubleshooting Common Experimental Challenges
Q1: In my 2D culture, TGF-β treatment does not consistently induce myofibroblast differentiation. What could be the issue?
The inconsistency often stems from inadequate activation of latent TGF-β or the absence of necessary mechanical tension.
- Problem: Latent TGF-β requires activation before it can bind to its receptors. In 2D cultures without sufficient mechanical force or the correct integrins, this activation may not occur.
- Solution: Ensure proper TGF-β activation. You can use commercially available active TGF-β1. Alternatively, to study physiological activation, pre-coat plates with an RGD-containing peptide (e.g., from fibronectin) or use a cell line that expresses relevant integrins like αVβ6 or αVβ8 [14] [15]. Confirming the presence of mechanical tension in your culture system is also critical.
Q2: My 3D fibrotic microtissue model is not demonstrating sufficient collagen alignment and contraction. How can I improve it?
The key is to provide topographical guidance and ensure the presence of mechanically activated cells.
- Problem: Randomly polymerized collagen gels lack the directional cues found in fibrotic tissues, leading to disorganized matrix deposition.
- Solution: Incorporate microfabricated structures (like micropillar arrays) into your 3D model to guide tissue alignment and measure contractile forces [16]. Co-culture fibroblasts with pro-fibrotic macrophages (M2-like), as their interaction significantly enhances collagen alignment and tissue contraction through integrin-mediated mechanotransduction [16].
Q3: How can I specifically inhibit integrin-mediated TGF-β activation without affecting other pathways?
Target the specific integrins or the mechanical link they provide.
- Solution: Utilize small molecule inhibitors or blocking antibodies against specific integrins. For example, Cilengitide targets αV-containing integrins. To specifically disrupt the mechanical link between integrins and the cytoskeleton, use low concentrations of ROCK inhibitors (e.g., Y-27632) or myosin II inhibitors (e.g., blebbistatin) [17] [16]. This prevents the generation of contractile force required for integrin-mediated TGF-β activation.
Q4: What are the best markers to confirm a pro-fibrotic phenotype in my in vitro model?
A combination of markers for activated fibroblasts, ECM, and immune cells is most reliable.
- Solution: The table below summarizes key markers for a pro-fibrotic phenotype.
Table 1: Key Markers for Profibrotic Phenotype Analysis
| Cell Type | Marker | Significance |
|---|---|---|
| Myofibroblast | α-SMA (Alpha-Smooth Muscle Actin) | Gold standard for fibroblast-to-myofibroblast differentiation [18] [16] [3]. |
| Collagen I, Fibronectin (especially EDA+ isoform) | Indicates elevated ECM production [18] [17]. | |
| Pro-fibrotic Macrophage | CD206, Arginase-1 | Associated with M2/pro-fibrotic polarization [16]. |
| Integrin αM (CD11b) / β2 (CD18) | Indicates mechanical activation [16]. | |
| General Pathway | Phospho-Smad2/3 | Indicates active canonical TGF-β signaling [18] [19]. |
| CTGF (Connective Tissue Growth Factor) | Key downstream mediator of TGF-β's fibrotic effects [18]. |
Experimental Protocols for Key Assays
Protocol 1: Assessing Integrin-Mediated TGF-β Activation in a Co-culture System
This protocol is designed to study how mechanically activated macrophages contribute to TGF-β activation and fibroblast differentiation in a 3D microtissue, relevant to the fibrotic capsule microenvironment.
- Objective: To investigate the role of macrophage-fibroblast crosstalk in driving TGF-β activation and fibrosis.
Materials:
- Normal Human Lung Fibroblasts (NHLFs) or human dermal fibroblasts.
- Human peripheral blood monocytes.
- Recombinant IL-4 and IL-13 (to polarize monocytes to M2 macrophages).
- Type I collagen solution.
- Micropillar-based microtissue molds (e.g., spiral or diamond patterns).
- Anti-integrin β2 (CD18) blocking antibody or ROCK inhibitor (Y-27632).
- Antibodies for immunofluorescence: α-SMA, Collagen I, CD206.
Method:
- Microtissue Formation: Mix NHLFs with collagen I and seed into micropillar molds. Allow fibroblasts to remodel the matrix for 3-5 days, forming an aligned microtissue [16].
- Macrophage Polarization and Seeding: Differentiate monocytes into M2 macrophages using IL-4 and IL-13 (e.g., 20 ng/mL each for 48 hours). Seed these macrophages onto the pre-formed fibroblast microtissues.
- Experimental Inhibition: To test the role of mechanotransduction, treat co-cultures with an integrin β2 blocking antibody or ROCK inhibitor.
- Analysis: After 3-7 days of co-culture, fix microtissues and perform immunofluorescence staining for α-SMA, collagen I, and CD206. Analyze the degree of cell and collagen alignment, and quantify α-SMA intensity. Measure contractile force generation by tracking micropillar deflection [16].
Protocol 2: Quantifying Myofibroblast Differentiation in a Stiffness-Controlled 2D System
This protocol examines how substrate stiffness synergizes with soluble factors to drive fibrosis.
- Objective: To evaluate the combined effect of substrate mechanics and TGF-β on fibroblast activation.
Materials:
- Polyacrylamide hydrogels of tunable stiffness (e.g., 1 kPa mimicking healthy tissue, 50 kPa mimicking fibrotic tissue).
- Sulfo-SANPAH for crosslinking collagen I to the hydrogel surface.
- Human fibroblasts.
- Latent or active TGF-β1.
Method:
- Hydrogel Preparation: Fabricate polyacrylamide hydrogels with compliant (1 kPa) and stiff (50 kPa) substrates. Coat the surface with type I collagen using the crosslinker Sulfo-SANPAH.
- Cell Seeding and Treatment: Plate fibroblasts onto the hydrogels. Treat cells with either latent TGF-β or active TGF-β.
- Analysis: After 48-72 hours, fix and stain for α-SMA and paxillin (to visualize focal adhesions). The number of α-SMA-positive stress fibers and the size of focal adhesions will be significantly greater on stiff substrates, especially in the presence of TGF-β, demonstrating mechanical potentiation of the fibrotic response [17].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating Mechanical Profibrotic Signaling
| Reagent / Tool | Function / Target | Experimental Application |
|---|---|---|
| Recombinant TGF-β1 (Active) | Directly activates TGF-β receptors. | Positive control for inducing Smad2/3 phosphorylation and myofibroblast differentiation [18] [15]. |
| Latent TGF-β Complex | Requires activation for function. | Studying physiological TGF-β activation mechanisms via integrins or proteases [18] [14]. |
| Cilengitide | Small molecule inhibitor of αV integrins. | Blocking integrins αVβ3, αVβ5, and αVβ6 to inhibit integrin-mediated TGF-β activation [20]. |
| Integrin β2 (CD18) Blocking Antibody | Inhibits leukocyte-specific integrins. | Disrupting macrophage mechanical activation and their pro-fibrotic crosstalk with fibroblasts [16]. |
| Y-27632 (ROCK Inhibitor) | Inhibits Rho-associated kinase (ROCK). | Reducing cellular contractility; blocks force-mediated TGF-β activation and myofibroblast contraction [17] [16] [3]. |
| Pirfenidone | FDA-approved anti-fibrotic drug. | Multi-target inhibitor; used to validate fibrotic models. Recently shown to inhibit macrophage mechanical activation via ROCK2 [16]. |
| Tunable Stiffness Hydrogels | Mimics compliant or stiff tissue environments. | Essential for studying the role of matrix mechanics in potentiating TGF-β signaling and fibroblast activation [17]. |
| Micropillar Arrays | Measures cellular contractile forces. | Quantifying the contractile output of myofibroblasts and the contribution of mechanical force to fibrosis [16]. |
| Cyclo(Ala-Phe) | Cyclo(Ala-Phe), CAS:14474-78-3, MF:C12H14N2O2, MW:218.25 g/mol | Chemical Reagent |
| 3-Methyladipic acid | 3-Methyladipic Acid|High-Purity Research Chemical | 3-Methyladipic acid, a key metabolite in Refsum disease research. This product is for Research Use Only (RUO). Not for human or veterinary diagnostic or therapeutic use. |
Pathway Diagrams for Core Signaling Mechanisms
TGF-β Activation and Signaling
Macrophage-Fibroblast Profibrotic Crosstalk
Capsular fibrosis, specifically capsular contracture (CC), is the most common complication following breast implant surgery, often leading to pain, implant distortion, and the need for revision surgery [21] [3]. While the formation of a thin, soft fibrous capsule is a normal foreign body response, the progressive tightening and contraction that defines CC is a pathological process [3]. A growing body of evidence implicates subclinical biofilm infections as a primary etiological factor in this process [21] [22]. Biofilms are structured communities of microorganisms encased in a self-produced polymeric matrix that adhere to a surface, such as a breast implant [21]. These biofilm communities are highly resistant to antibiotics and host immune responses, leading to a state of chronic, low-grade inflammation that can drive excessive fibroblast activation and collagen deposition, resulting in clinical contracture [21] [3] [22]. This technical support guide is designed to assist researchers in investigating this critical biofilm-infection connection to develop effective preventative and therapeutic strategies.
FAQs: Biofilms and Implant-Related Fibrosis
What is the clinical evidence linking biofilms to capsular contracture? Multiple clinical studies have directly cultured bacteria from implants and capsules explanted due to contracture. The table below summarizes key clinical evidence:
Table: Clinical Evidence of Biofilms in Capsular Contracture
| Study Focus | Author | Key Finding | Level of Evidence |
|---|---|---|---|
| Presence of Biofilms | Virden et al. [21] | Correlation between positive bacterial cultures on silicone shells and development of CC. | 3 (Case-control) |
| Presence of Biofilms | Pajkos et al. [21] | Identification of biofilms via sonication and scanning electron microscopy (SEM) on explanted devices. | 3 (Case-control) |
| Presence of Biofilms | Schreml et al. [21] | Bacterial colonization confirmed via culture in patients with CC. | 3 (Case-control) |
Which bacterial species are most commonly associated with biofilms on breast implants? The biofilm community on mammary implants is often polymicrobial, but certain commensal skin bacteria are frequently identified [21]. The most common organisms include:
- Staphylococcus epidermidis: A major part of the skin flora and the most frequently identified species on explanted breast implants [21].
- Staphylococcus aureus: Another common skin commensal with strong biofilm-forming capabilities [21].
- Propionibacterium acnes: A skin and gut commensal that may gain access to the implant during surgery, particularly with peri-areolar incisions [21].
How do biofilms on implants drive the process of fibrotic encapsulation? Biofilms induce a persistent foreign body reaction. The innate immune system recognizes biofilm components, triggering a chronic inflammatory cascade. This involves sustained activation of macrophages, which release pro-fibrotic cytokines like Transforming Growth Factor-beta (TGF-β) [3] [22]. TGF-β is a master regulator that drives the differentiation of fibroblasts into myofibroblasts, which are characterized by the expression of α-smooth muscle actin (α-SMA) and are responsible for excessive collagen production and tissue contraction, leading to a thick, constrictive capsule [3].
Why are biofilm-related infections so resistant to antibiotic treatment? Biofilms confer resistance through multiple, overlapping mechanisms [21]:
- Physical Barrier: The extracellular polymeric substance (EPS) matrix limits antibiotic penetration.
- Altered Microenvironments: Gradients in nutrients, oxygen, and pH within the biofilm create heterogeneous populations of bacteria, including dormant, persister cells that are highly tolerant to antibiotics.
- Upregulated Stress Responses: Bacteria in a biofilm state differentially express genes, including those for multidrug efflux pumps and antibiotic-degrading enzymes like β-lactamases.
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent Biofilm Formation In Vitro
- Problem: High variability in biofilm biomass between experimental replicates.
- Solution:
- Standardize Inoculum: Use a defined growth medium (e.g., Tryptic Soy Broth with 1% glucose [23]) and carefully control the initial bacterial concentration (e.g., half McFarland density diluted to ~5x10^5 CFU/mL) [23].
- Control Surface Properties: Ensure the material used for in vitro assays (e.g., silicone discs) has consistent surface topography and chemistry, as these are critical factors for bacterial adhesion [24] [3].
- Include Controls: Always include a known strong biofilm-forming strain (e.g., S. aureus ATCC 25923) and a non-biofilm forming negative control in every assay run [23].
Challenge 2: Differentiating Between Planktonic and Biofilm Antimicrobial Resistance
- Problem: An agent shows efficacy against free-floating (planktonic) bacteria but fails against a established biofilm.
- Solution: Employ specific assays designed for biofilms.
- Minimum Biofilm Eliminating Concentration (MBEC) Assay: This is the standard method. After forming a biofilm in a 96-well plate, treat it with serial dilutions of the antimicrobial agent. The MBEC is the lowest concentration that eliminates the visible biofilm [23]. The XTT colorimetric assay can be used to quantify metabolic activity of biofilm-resident bacteria post-treatment [23].
- Data Interpretation: Note that MBEC values are often orders of magnitude higher than the Minimum Inhibitory Concentration (MIC) for planktonic cells. For example, one study on S. aureus found strains susceptible to ceftiofur in the planktonic state but resistant in the biofilm state [23].
Challenge 3: Modeling the Complex Host Immune Response to Biofilms In Vivo
- Problem: Simple rodent models may not fully recapitulate the human foreign body response and fibrotic cascade.
- Solution:
- Use Larger Animal Models: Porcine (pig) skin and immune responses are closer to humans, making them valuable for preclinical studies [21].
- Incorplicate Key Read-Outs: Beyond quantifying bacterial load, analyze the explanted tissue and capsule for:
- Histology: Collagen density (Trichrome stain), immune cell infiltration (H&E), and myofibroblast presence (α-SMA immunohistochemistry) [3] [22].
- Cytokine Profiling: Measure levels of pro-fibrotic cytokines (e.g., TGF-β, IL-17) and pro-inflammatory markers (e.g., IL-1, TNF-α) in peri-implant tissue [3] [22].
Key Experimental Protocols
Protocol: Quantitative Analysis of Biofilm Formation via Colorimetric Assay
This protocol, adapted from Stepanović et al. and used in mastitis research, is a cornerstone for in vitro biofilm quantification [23].
Workflow Diagram: Biofilm Quantification Assay
Materials:
- Tissue culture-treated 96-well plate (e.g., JET BIOFIL) [23]
- Tryptic Soy Broth (TSB) with 1% glucose [23]
- Bouin's reagent or equipment for air-drying at 60°C [23]
- 0.1% Crystal Violet solution
- 95% Ethanol
- Microplate reader (e.g., Epoch, BioTek) [23]
Procedure:
- Inoculation: Dilute a fresh bacterial culture 2:200 in TSB + 1% glucose. Pipette 200 µL into designated wells. Include control wells with sterile broth only [23].
- Incubation: Incubate the plate aerobically for 24 hours at 37°C [23].
- Washing: Gently discard the supernatant from each well. Wash the wells three times with phosphate-buffered saline (PBS) to remove non-adherent planktonic cells. Let the plate air-dry.
- Fixing: Fix the adhered biofilms by adding Bouin's reagent for 1 hour or by air-drying the plate at 60°C for 1 hour [23].
- Staining: Add 0.1% crystal violet solution to each well for 5-15 minutes.
- Destaining: Rinse the plate thoroughly under running tap water until the control wells appear clear. Air-dry the plate.
- Solubilization: Add 200 µL of 95% ethanol to each well to solubilize the dye bound to the biofilm. Allow it to sit for 10-30 minutes with gentle shaking.
- Measurement: Transfer 125 µL of the solubilized dye from each well to a new plate (or measure directly if the plate is compatible). Measure the optical density (OD) at 570 nm using a microplate reader [23].
Data Analysis: Calculate the cut-off value (ODc) as the average OD of the negative control plus three times its standard deviation. Categorize biofilm formation as follows [23]:
- None: OD ≤ ODc
- Weak: ODc < OD ≤ 2xODc
- Moderate: 2xODc < OD ≤ 4xODc
- Strong: OD > 4xODc
Protocol: Molecular Detection of Biofilm-Associated Genes
Understanding the genetic basis of biofilm formation in clinical isolates is crucial.
Materials:
- PCR reagents (Taq polymerase, dNTPs, buffer, MgClâ‚‚)
- Primers for target genes (e.g., icaA, icaD, fnbA, fnbB, bap) [23]
- Thermocycler
- Gel electrophoresis equipment
Procedure:
- DNA Extraction: Extract genomic DNA from your bacterial isolates using a standard boiling or commercial kit method.
- PCR Amplification: Set up PCR reactions with specific primers and cycling conditions as previously described for each target gene [23].
- Gel Electrophoresis: Run the PCR products on an agarose gel, visualize under UV light, and score for the presence or absence of the target amplicon.
Table: Common Biofilm-Associated Genes in Staphylococci
| Gene | Function / Encodes For | Reported Frequency in S. aureus Isolates |
|---|---|---|
| icaD | Intercellular adhesion locus (polysaccharide synthesis) | 75% [23] |
| fnbA | Fibronectin-binding protein A (initial attachment) | 43.8% [23] |
| fnbB | Fibronectin-binding protein B (initial attachment) | 31.2% [23] |
| bap | Biofilm-associated protein | 25% [23] |
| icaA | Intercellular adhesion locus | 9.4% [23] |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Biofilm and Fibrosis Research
| Item | Function / Application | Example / Note |
|---|---|---|
| Silicone Discs/Sheets | In vitro substrate for biofilm growth; mimics implant material. | Ensure consistent surface topography (smooth vs. textured) as it influences bacterial adhesion [24] [3]. |
| Tryptic Soy Broth (TSB) + 1% Glucose | Standardized rich medium for promoting biofilm growth of Staphylococci. | The added glucose enhances production of extracellular polysaccharides [23]. |
| Crystal Violet | A basic dye used for the colorimetric quantification of total biofilm biomass. | Standard, cost-effective method; cannot distinguish between live and dead cells [23]. |
| XTT Assay Kit | Colorimetric assay to measure the metabolic activity of cells within a biofilm. | Used for determining MBEC and assessing viability after antimicrobial treatment [23]. |
| Anti-α-SMA Antibody | Primary antibody for immunohistochemistry to identify activated myofibroblasts in fibrous capsules. | A key marker for the profibrotic cellular phenotype [3]. |
| Anti-TGF-β Antibody | For detecting levels of this master regulatory cytokine in tissue sections (IHC) or supernatants (ELISA). | Central to the pro-fibrotic signaling pathway [3] [22]. |
| PCR Primers for icaADBC | To detect the genetic potential of staphylococcal isolates to produce a polysaccharide biofilm matrix. | The ica locus is critical for biofilm accumulation in many strains [23]. |
| Cyclo(Tyr-Val) | Cyclo(Tyr-Val), MF:C14H18N2O3, MW:262.30 g/mol | Chemical Reagent |
| L-Serine-13C3 | L-Serine-13C3, MF:C3H7NO3, MW:108.071 g/mol | Chemical Reagent |
Visualizing the Fibrotic Signaling Pathway Induced by Biofilms
The following diagram integrates the key molecular and cellular events, from bacterial adhesion to clinical contracture, as described in the literature [3] [22].
Mechanism Diagram: Biofilm-Induced Fibrotic Encapsulation
Biomaterial Engineering and Pharmacological Disruption of Profibrotic Pathways
Troubleshooting Guide: Common Experimental Challenges in Surface Engineering
FAQ 1: Why does my in vitro macrophage assay not show a clear difference in cytokine expression between smooth and textured surfaces?
- Potential Cause: The surface properties of your test samples, specifically the hydrophilicity, may have degraded over time due to hydrocarbon contamination from the air, a process known as "biological aging." This can diminish the expected cellular response [25].
- Solution: Implement a surface activation protocol immediately prior to experiments. Techniques like UV photofunctionalization have been shown to restore surface hydrophilicity and remove hydrocarbon contaminants, revitalizing the bioactivity of the surface and ensuring a more robust cellular response [25].
FAQ 2: How can I ensure the surface topography of my experimental implants is consistent and accurately characterized?
- Potential Cause: Inconsistent fabrication methods or inadequate surface characterization. Manufacturing techniques for textured implants can be crude, and surfaces are often poorly characterized [26].
- Solution:
- Standardize Fabrication: For research-grade samples, use precise methods like anodic oxidation for nano-textures or certified sandblasting/acid-etching for micro-textures [27].
- Comprehensive Characterization: Employ a combination of:
- Scanning Electron Microscopy (SEM): For qualitative evaluation of micro- and nano-morphology [28] [12].
- Laser Confocal Microscopy / White Light Interferometry: For accurate 3D quantitative characterization of surface roughness parameters (e.g., S₠- average height, Sᵈʳ - developed interfacial area ratio) [28] [12] [26].
- Energy-Dispersive X-ray (EDX) Analysis: To verify the chemical and elemental composition of the surface [28].
FAQ 3: My animal model shows high variance in capsular thickness. What factors should I control?
- Potential Cause: Uncontrolled surgical variables or implant movement (rotation) within the pocket, which is influenced by surface topography [12].
- Solution:
- Surgical Precision: Standardize the implant pocket size and location across all subjects to minimize confounding variables.
- Account for Surface-Dependent Movement: Be aware that different topographies exhibit different levels of mobility. A study found that nanotexture and smooth surface implants had significantly increased movement compared to macrotexture implants. This variable should be measured and accounted for in your analysis [12].
The following tables summarize key quantitative findings from preclinical studies on implant surface topography.
Table 1: Impact of Surface Topography on Capsule Formation in a Rodent Model (12 Weeks Post-Implantation) [12]
| Surface Topography | Capsule Thickness (µm) | Collagen Fiber Density (%) | Myofibroblast Infiltration (%) | TGF-β1 Expression (Optical Density) | Implant Movement (Change in Location) |
|---|---|---|---|---|---|
| Smooth | 415.07 ± 19.74 | 67.8 ± 3.4 | 42.8 ± 3.4 | 0.95 ± 0.04 | 38.75° ± 15.56° |
| Macrotexture(Roughness: ~100 µm) | 261.53 ± 5.7 | 62.2 ± 6.1 | 25.2 ± 6.1 | 0.91 ± 0.05 | 3.50° ± 1.73° |
| Nanotexture(Roughness: ~6 µm) | 232.48 ± 14.10 | 46.2 ± 3.3 | 16.2 ± 3.3 | 0.80 ± 0.09 | 76.00° ± 24.01° |
Table 2: Comparison of Micro-scale vs. Nano-scale Surface Modifications [27]
| Aspect | Micro-Scale Modifications | Nano-Scale Modifications |
|---|---|---|
| Feature Size | 1 - 100 micrometers (µm) | 1 - 100 nanometers (nm) |
| Common Methods | Sandblasting, Acid Etching, Plasma Spraying | Anodization, Sol-Gel Coating, Chemical Vapour Deposition |
| Key Advantage | Cost-effective, extensive long-term clinical data | Enhanced protein adsorption, faster healing, biomimetic |
| Key Limitation | May trap bacteria; less efficient protein interaction | Higher cost, limited long-term data, complex manufacturing |
| Impact on Fibrosis | Higher capsule thickness and collagen density | Reduced capsule thickness and collagen density |
Detailed Experimental Protocols
Protocol 1: In Vivo Evaluation of Capsule Formation
This protocol is adapted from a study investigating capsule formation around implants with different surface topographies in a rodent model [12].
- Study Groups and Implants: Assign subjects into groups (e.g., n=8 per group). Use commercially available or custom-fabricated silicone implants with well-characterized surfaces:
- Surgical Implantation: Perform aseptic surgery to insert one implant per subject into a defined subcutaneous pocket. Standardize pocket size and location precisely across all subjects.
- Post-Op Monitoring and Measurement: At defined endpoints (e.g., 4 and 12 weeks):
- Implant Location: Periodically measure and record implant rotation or movement from the original position [12].
- Euthanasia and Explantation: Euthanize subjects and carefully retrieve the implant with the surrounding capsular tissue intact.
- Histological Processing and Staining:
- Immunohistochemical (IHC) Staining:
- Perform IHC staining for key fibrotic markers such as α-Smooth Muscle Actin (α-SMA) to identify myofibroblasts and TGF-β1 to assess pro-fibrotic signaling [12].
- Western Blot Analysis:
- Homogenize capsular tissue and use Western Blot to quantitatively compare the protein expression levels of fibrotic markers like TGF-β1 across the different study groups [12].
- Data Analysis: Use image analysis software to quantify staining results. Perform statistical analysis (e.g., ANOVA) to compare capsule thickness, collagen density, and marker expression between groups.
Protocol 2: Fabrication and In Vitro Testing of a Biomimetic Breast Tissue-Derived Surface
This protocol outlines the creation of a novel, biomimetic implant surface derived from human breast tissue and its initial in vitro validation [26].
- Surface Characterization and Modeling:
- Tissue Sampling: Obtain human breast adipose tissue samples with appropriate ethical approval and informed consent [26].
- Imaging: Image the tissue surface using Scanning Electron Microscopy (SEM) to observe the native topography, which typically appears as a layer of close-packed spheres (adipocytes) with a web of extracellular matrix fibers [26].
- 3D Profiling: Use Laser Confocal Microscopy to generate a high-resolution three-dimensional map of the adipose surface texture [26].
- Statistical Modeling: Analyze the surface measurement data to create a statistical model of the topography (e.g., "modelled adipose" surface) [26].
- Surface Fabrication:
- In Vitro Macrophage Response Assay:
- Cell Culture: Use a human macrophage cell line (e.g., THP-1 cells). Differentiate monocytes into macrophages prior to seeding [26].
- Seeding: Seed macrophages onto the novel biomimetic surfaces and control surfaces (e.g., smooth silicone) [26].
- Analysis:
- Cell Morphology: Use SEM to assess macrophage morphology and adhesion on the different surfaces [26].
- Gene Expression: After a set incubation period (e.g., 48 hours), extract RNA and perform Quantitative PCR (qPCR) to analyze the expression of key cytokines and polarization markers (e.g., IL-1β, TNF-α, IL-6 for pro-inflammatory M1 phenotype; IL-10, TGF-β for pro-fibrotic M2 phenotype) [26].
- Cytokine Secretion: Collect cell culture supernatant and use Enzyme-Linked Immunosorbent Assay (ELISA) to quantify the secretion of proteins like TNF-α and IL-6 [26].
- Evaluation: A favorable, less fibrotic response is indicated by a downregulation of pro-inflammatory cytokines (IL-1β, TNF-α, IL-6) and/or a shift in macrophage polarization towards the M2 phenotype in response to the biomimetic surface compared to controls [26].
Foreign Body Response (FBR) Pathway
Integrated Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Investigating Implant Surfaces
| Item | Function/Application in Research |
|---|---|
| Medical-Grade Silicone (PDMS) | The base material for fabricating experimental breast implant shells and testing novel surface topographies [26]. |
| THP-1 Human Monocyte Cell Line | A widely used model for in vitro studies of the human immune response. Can be differentiated into macrophages to test surface-induced inflammatory and fibrotic responses [26]. |
| Antibodies for IHC/Western Blot | Essential for detecting and quantifying key proteins involved in fibrosis. Critical targets include α-SMA (for myofibroblasts) and TGF-β1 (a master regulator of fibrosis) [12]. |
| ELISA Kits (TNF-α, IL-6, IL-1β) | Used to quantitatively measure the secretion of pro-inflammatory cytokines from macrophages cultured on different implant surfaces, indicating the intensity of the foreign body response [26]. |
| PCR Primers & Reagents | For quantitative PCR (qPCR) analysis of gene expression changes in cells exposed to different surfaces. Key genes include those for fibrotic markers and cytokines [26]. |
| Histology Stains (H&E, Masson's Trichrome) | Standard dyes used on tissue sections to visualize overall capsule structure (H&E) and to quantify collagen deposition and density (Masson's Trichrome) [12]. |
| Scanning Electron Microscope (SEM) | Instrument for high-resolution imaging of surface micro- and nano-morphology to ensure topographical features are as designed and to inspect cell morphology on surfaces [28] [12] [26]. |
| 3D Surface Profilometer | Instrument for quantitative, three-dimensional analysis of surface roughness parameters (e.g., Sâ‚, Sᵈʳ), which are critical for correlating topography with biological outcomes [28] [12]. |
| Cauloside D | Cauloside D, MF:C53H86O22, MW:1075.2 g/mol |
| Bromo-PEG7-Boc | Bromo-PEG7-Boc, MF:C21H41BrO9, MW:517.4 g/mol |
This technical support center provides resources for researchers investigating the use of soft silicone layers to mitigate the fibrotic encapsulation of breast implants. Fibrotic encapsulation, or capsular contracture, is a common complication where a thickened collagen capsule forms around the implant, potentially leading to pain, hardening, and deformity [29] [30]. The underlying mechanism involves a foreign body response (FBR) that activates myofibroblasts, which are scar-forming cells [31]. The mechanical properties of the implant surface, specifically its elastic modulus, play a critical role in driving this activation [30].
The foundational study by Noskovicova et al. demonstrated that coating conventionally stiff silicone implants (elastic modulus ~2 MPa) with a soft silicone layer (elastic modulus ~2 kPa) significantly reduced collagen deposition and myofibroblast activation in a murine model [30]. The proposed mechanism is that soft surfaces reduce intracellular stress in fibroblasts, minimizing the recruitment of αv and β1 integrins and subsequent activation of pro-fibrotic Transforming Growth Factor-beta (TGF-β) signaling pathways [30]. This resource center consolidates experimental protocols, troubleshooting guides, and key reagents to facilitate replication and advancement of this promising approach.
The following diagram illustrates the core signaling pathway involved in this process, contrasting the cellular responses to stiff versus soft silicone surfaces.
Diagram 1: Signaling Pathway in Fibrotic Encapsulation. This diagram contrasts the pro-fibrotic cellular response triggered by stiff silicone surfaces with the suppressed response from soft surfaces or pharmacological inhibition.
Troubleshooting Common Experimental Problems
Q1: Our soft silicone coatings are exhibiting incomplete or non-uniform curing, leading to tacky surfaces and compromised mechanical integrity. What are the causes and solutions?
A: Incomplete curing is a frequent issue that can invalidate modulus measurements and biological results.
- Cause (Incorrect Mixing Ratios): Two-part silicone systems require precise stoichiometric ratios for complete cross-linking. Deviations disrupt the polymerization network [32].
- Solution: Always use a high-precision digital scale to measure components. For critical applications, consider using pre-measured kits from suppliers to ensure consistency [32].
- Cause (Insufficient Curing Time/Temperature): Rushing the process or using incorrect temperatures prevents the material from reaching its ultimate physical properties [33] [32].
- Solution: Strictly follow the manufacturer's data sheet for recommended curing times and temperatures. Note that elevated temperatures accelerate curing, but the reaction coordinate (a function of time and temperature) must be calculated to ensure full cure [33]. Allow the material to cure at a stable, controlled room temperature for the full recommended duration before testing or use.
- Cause (Material Incompatibility): The soft coating material may be chemically incompatible with the stiffer substrate silicone.
- Solution: Ensure both the base implant and soft coating are from the same silicone chemistry family (e.g., platinum-catalyzed). Perform adhesion tests on small samples before full-scale fabrication.
Q2: We are encountering air bubbles trapped within our soft silicone layers during fabrication. How can this be prevented?
A: Air bubbles create defects that act as stress concentrators and can be misinterpreted as biological voids in histology.
- Cause (Poor Mixing & Pouring Technique): Aggressive stirring or rapid pouring of the liquid prepolymer introduces and traps air [34] [32].
- Solution: Mix the components slowly and deliberately to minimize air entrainment. Pour the mixture in a thin, steady stream against the side of the mold container [32].
- Cause (Inadequate Degassing): Failing to remove entrained air before curing is a primary cause.
- Solution: Implement vacuum degassing. Place the mixed silicone in a vacuum chamber immediately after mixing and apply a vacuum until the volume stops expanding and bubbles collapse (typically 2-5 minutes) [34] [32].
Q3: The adhesion between our soft silicone layer and the underlying stiff substrate is weak, leading to delamination during handling or implantation.
A: Weak interfacial adhesion is a critical failure point for layered implants.
- Cause (Overcuring of the First Layer): If the base silicone implant is fully cured (its reaction coordinate Ï„ >> 1), it presents a chemically inert surface with few available sites for the soft coating to bond with [33].
- Solution: Employ a staged curing process. Apply the soft coating while the base substrate is only partially cured (the "green stage"), allowing polymer chains to cross-link across the interface. The reaction coordinate framework can be used to determine the optimal window for bonding [33].
- Cause (Absence of a Mechanical Interlock): A perfectly smooth interface provides little surface area for adhesion.
- Solution: Modify the surface topography of the stiff substrate before applying the soft layer. This can be achieved by using textured molds or lightly abrading the surface to create micro-scale anchors.
Q4: Our in-vivo experiments show high variability in capsule thickness despite using soft layers. What factors beyond modulus could be influencing this?
A: Fibrotic encapsulation is a multifactorial process. Key considerations include:
- Cause (Subclinical Infection/Biofilm): Bacterial contamination, even at levels that do not cause clinical infection, is a well-documented trigger for chronic inflammation and capsular contracture [29].
- Solution: Adhere to strict aseptic surgical techniques during implantation. Some studies suggest the use of antibiotic irrigation or antimicrobial-coated implants, though their efficacy is an area of active research [29].
- Cause (Implant Surface Topography): While your focus is modulus, surface texture (smooth, micro-textured, nano-textured) independently modulates the immune response. Nano-textured surfaces have shown promise in reducing myofibroblast infiltration and promoting a more favorable immune profile [29].
- Solution: Control for surface topography in your experimental design. Consider using implants with identical topography but varying modulus to isolate the mechanical effect.
Frequently Asked Questions (FAQs) for Researchers
Q1: What is the quantitative evidence that soft silicone layers reduce fibrosis?
A: The primary evidence comes from a key murine model study which reported that a soft silicone layer (~2 kPa) on a stiff substrate (~2 MPa) significantly reduced collagen deposition and myofibroblast activation compared to stiff implants alone. Furthermore, pharmacological inhibition of the mechanical activation of TGF-β via the small molecule CWHM-12 produced a similar anti-fibrotic effect [30].
Q2: How does implant elastic modulus mechanically activate TGF-β?
A: On stiff surfaces, fibroblasts generate high intracellular contractile forces. This mechanical stress promotes the recruitment of αv and β1 integrins to focal adhesions. These integrins bind to the Latency-Associated Peptide (LAP) of latent TGF-β, inducing a conformational change that releases active TGF-β, which then drives myofibroblast differentiation and fibrosis [30]. Soft surfaces reduce the cellular contractile forces, preventing this mechano-activation pathway.
Q3: Are there pharmacological strategies that mimic the effect of soft surfaces?
A: Yes, the small-molecule inhibitor CWHM-12 antagonizes the binding of αv integrin to LAP. In the referenced study, treatment with CWHM-12 suppressed active TGF-β signaling, myofibroblast activation, and fibrotic encapsulation around stiff subcutaneous implants in mice, effectively producing a "chemical softening" effect [30].
Q4: How can we accurately measure the elastic modulus of our silicone layers?
A: The gold standard is to use a dynamic mechanical analyzer (DMA) or a tensile tester to perform uniaxial or biaxial tensile tests on pure, bulk samples of the cured material. For thin coatings, nanoindentation may be more appropriate. Ensure samples are fully cured and tested under standardized environmental conditions. The table below summarizes key quantitative findings from the literature.
Table 1: Quantitative Effects of Implant Surface Properties on Fibrotic Outcomes
| Implant Type / Treatment | Elastic Modulus | Key Measured Outcome | Experimental Model | Source |
|---|---|---|---|---|
| Conventional Silicone (Control) | ~2 MPa | Baseline collagen deposition & myofibroblast activation | Mouse subcutaneous implant | [30] |
| Soft Silicone-Coated | ~2 kPa | Reduced collagen & myofibroblast activation | Mouse subcutaneous implant | [30] |
| CWHM-12 Treatment (on stiff implant) | N/A (Pharmacological) | Suppressed TGF-β signaling & fibrosis | Mouse subcutaneous implant | [30] |
| L-Microtextured Implant | N/A (Topography) | Increased tissue remodeling, reduced myofibroblasts | Human study (n=30, 5 groups) | [29] |
| Smooth Implant | N/A (Topography) | Highest incidence of capsular contracture | Human study (n=30, 5 groups) | [29] |
Detailed Experimental Protocols
Protocol: Fabricating Soft Silicone-Coated Implants
This protocol describes the creation of a model implant with a tunable soft surface layer.
Materials:
- Base Silicone Elastomer (e.g., for stiff core, ~2 MPa)
- Soft Silicone Elastomer (e.g., for coating, Shore A hardness <30, target modulus ~2 kPa)
- Precision Digital Scale
- Vacuum Chamber and Pump
- Mold (e.g., disk-shaped for standardized testing)
- Curing Oven (if temperature-accelerated)
Method:
- Fabricate Stiff Core: Mix the base silicone components in the precise ratio recommended by the manufacturer. Degas in a vacuum chamber until no bubbles remain. Pour into the mold and cure partially. The key is to bring the reaction coordinate (Ï„) of the base to a point just before full gelation to ensure optimal adhesion for the next layer [33].
- Apply Soft Coating: Mix the soft silicone components thoroughly. Degas the mixture completely. Pour the soft silicone directly onto the partially cured stiff core.
- Co-Curing: Allow the layered structure to cure fully together. This enables polymer chains from both layers to interdiffuse and cross-link at the interface, creating a strong bond.
- Post-Processing: Demold the final implant and inspect for defects like bubbles or delamination. Store in a clean, dry environment until implantation.
The workflow for this fabrication process and the subsequent in-vivo validation is outlined below.
Diagram 2: Experimental Workflow for Implant Fabrication and Validation. This diagram outlines the key steps from creating the layered silicone implant to its in-vivo evaluation and final data analysis.
Protocol: Quantifying the Foreign Body Response In-Vivo
Materials:
- Experimental Implants (Soft-coated) & Control Implants (Stiff)
- Animal Model (e.g., C57BL/6 mice, approved by IACUC)
- Surgical tools, sutures, anesthetic, analgesic
- Tissue fixation and processing equipment
- Antibodies for immunohistochemistry (e.g., α-SMA for myofibroblasts, CD68 for macrophages, CD31 for vasculature)
Method:
- Implantation: Following approved ethical guidelines, implant disks of test and control materials subcutaneously in the dorsum of the animal. Each animal can host multiple implants in separate pockets.
- Explanation: At predetermined endpoints (e.g., 2, 4, and 8 weeks), euthanize the animals and carefully explant the constructs with the surrounding capsular tissue.
- Histological Processing: Fix tissues in formalin, embed in paraffin, and section. Perform standard staining (e.g., H&E for general morphology, Masson's Trichrome for collagen).
- Immunohistochemistry (IHC): Stain sections with specific antibodies to identify key cell types and activation states.
- Quantitative Analysis:
- Capsule Thickness: Measure at multiple points around the implant circumference from H&E or Trichrome stains.
- Collagen Density: Quantify the blue-stained area in Trichrome sections using image analysis software (e.g., ImageJ).
- Myofibroblast Presence: Count α-SMA positive cells at the implant-tissue interface.
- Immune Cell Profiling: Quantify M1 (pro-inflammatory) vs. M2 (pro-repair) macrophage polarization using specific markers.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Materials for Investigating Soft Silicone Layers
| Reagent / Material | Function / Role in Research | Example / Specification |
|---|---|---|
| Soft Silicone Elastomer | Creates the low-modulus surface layer to reduce mechanical activation. | Look for a Shore 00 hardness rating or an Elastic Modulus in the low kPa range (e.g., ~2 kPa). "Gel-type" soft SR with Shore A below 30 is also relevant [35] [30]. |
| Stiff Silicone Substrate | Serves as the base implant material and experimental control. | Standard medical-grade silicone with an Elastic Modulus of ~1-3 MPa [30]. |
| CWHM-12 Inhibitor | A small-molecule pharmacological tool to inhibit αv integrin binding to LAP, suppressing TGF-β activation. | Used for in-vivo studies to mimic the "soft surface" effect chemically and validate the mechano-transduction pathway [30]. |
| α-SMA Antibody | Primary antibody for Immunohistochemistry to identify and quantify activated myofibroblasts. | Critical for measuring the terminal effector cell in the fibrotic response. |
| TGF-β Signaling Assay Kits | To quantify the level of active TGF-β signaling in the peri-implant tissue (e.g., via pSMAD2/3 levels). | Validates the molecular mechanism linking mechanics to cell activation. |
| Vacuum Degassing Chamber | Essential equipment for removing air bubbles from liquid silicone before curing to ensure defect-free samples. | Prevents experimental artifacts and ensures consistent mechanical properties [34] [32]. |
| 3-epi-Digitoxigenin | 3-epi-Digitoxigenin, CAS:545-52-8, MF:C23H34O4, MW:374.5 g/mol | Chemical Reagent |
| Phytochelatin 5 | Phytochelatin 5 (PC5) | Research-grade Phytochelatin 5, a heavy metal-detoxifying plant peptide. For Research Use Only (RUO). Not for human or veterinary diagnostic or therapeutic use. |
Scientific Background: TGF-β Signaling in Fibrotic Encapsulation
The fibrotic encapsulation of medical implants, such as silicone breast implants, is a common complication that often necessitates revision surgery. This process, known as the Foreign Body Response (FBR), is a complex immune reaction that culminates in the formation of a dense, collagenous capsule around the implant, a process clinically recognized as capsular contracture [36] [3]. Central to this pathological fibrosis is the cytokine Transforming Growth Factor-Beta (TGF-β).
Upon implant placement, tissue injury initiates a wound healing response. Platelets are among the first responders, releasing growth factors including TGF-β, which orchestrates subsequent inflammatory and proliferative phases [36]. The persistence of the implant leads to chronic inflammation, characterized by the activation of macrophages. These macrophages attempt to phagocytose the implant; when unsuccessful, "frustrated phagocytosis" occurs, leading to their fusion into foreign body giant cells (FBGCs) and sustained pro-inflammatory signaling [36] [3]. A critical event is the shift in macrophage polarization from a pro-inflammatory (M1) phenotype to a pro-fibrotic (M2) phenotype. M2 macrophages are a major source of active TGF-β [3].
TGF-β drives fibrosis by activating resident fibroblasts, prompting their differentiation into myofibroblasts. These cells are identified by the expression of α-smooth muscle actin (α-SMA) and are responsible for excessive deposition and remodeling of extracellular matrix (ECM) proteins, primarily collagen types I and III, which form the fibrous capsule [3]. The primary signaling pathway for TGF-β involves the binding to and activation of transmembrane TGF-β receptor I (TGF-βRI) and II (TGF-βRII) complexes, which then phosphorylate downstream SMAD transcription factors (SMAD2/3) that translocate to the nucleus to initiate pro-fibrotic gene expression [15] [37]. Given its pivotal role, the TGF-β pathway presents a prime therapeutic target for mitigating fibrotic encapsulation.
The following diagram illustrates the key cellular and molecular events in the foreign body response and the points of intervention for TGF-β-targeting therapies:
Targeting the Pathway: Mechanisms of TGF-β Inhibition
Two primary therapeutic strategies for inhibiting TGF-β signaling are Small-Molecule TGF-βRI Inhibitors and Integrin Antagonists. Their mechanisms of action are distinct yet converge on the same goal of reducing fibrotic signaling.
A. Small-Molecule TGF-βRI Inhibitors
These compounds are designed to directly target the intracellular kinase domain of the TGF-β receptor I (TGF-βRI, also known as ALK5), competitively inhibiting its ATP-binding site. This blockade prevents the receptor from phosphoryating its downstream SMAD2/3 proteins, thereby interrupting the canonical pro-fibrotic signaling cascade [38]. Structural biology and X-ray crystallography have been instrumental in designing these inhibitors for high selectivity and potency [38] [39].
B. Integrin Antagonists
Integrins are cell surface receptors that play a crucial role in the activation of TGF-β. TGF-β is secreted in a latent complex (LLC) bound to the extracellular matrix. Specific integrins, notably αVβ6 and αVβ8, are key mediators of latent TGF-β activation. The αVβ6 integrin, expressed on epithelial cells, binds to the RGD motif in the Latency-Associated Peptide (LAP) and exerts mechanical force to change LAP's conformation, releasing the active TGF-β cytokine. The αVβ8 integrin, expressed on immune cells like macrophages, employs proteolytic activation via membrane-type MMPs (e.g., MMP14) to liberate active TGF-β [15] [37]. Antagonists blocking these integrins prevent the initial release of active TGF-β, acting further upstream in the pathway [40].
The diagram below details the TGF-β signaling pathway and the precise points of inhibition for these two classes of therapeutics:
Research Reagent Solutions
The table below summarizes key reagents used in research targeting the TGF-β pathway for anti-fibrotic studies.
| Reagent Category | Example(s) | Primary Function / Mechanism |
|---|---|---|
| Small-Molecule TGF-βRI Inhibitors | Galunisertib (LY2157299), SB-431542, CWHM-12 (representative class) [38] | Selective ATP-competitive inhibitors of the TGF-βRI (ALK5) kinase, blocking downstream SMAD2/3 phosphorylation. |
| Integrin Antagonists | Anti-αVβ6/αVβ8 mAbs, Cilengitide (RGD-mimetic) [40] [37] | Block integrin-mediated activation of latent TGF-β complexes, preventing the release of the active cytokine. |
| SMAD Reporter Assays | SMAD-responsive luciferase constructs (CAGA box, SBE) [38] | Measure the transcriptional activity of the canonical TGF-β/SMAD signaling pathway in cells. |
| Antibodies for Fibrosis Markers | Anti-α-SMA, Anti-Collagen I/III, Anti-phospho-Smad2/3 [3] | Detect and quantify myofibroblast differentiation, ECM deposition, and pathway activation via IHC, IF, or Western Blot. |
| Latent TGF-β Activation Kits | Commercial ELISA-based kits | Quantify levels of active vs. total TGF-β in cell culture supernatants or tissue lysates. |
Experimental Protocols
A. Protocol 1: Assessing Anti-Fibrotic Efficacy in anIn VitroFibroblast Activation Assay
This protocol is used to test the efficacy of TGF-β inhibitors on preventing fibroblast-to-myofibroblast differentiation.
- Cell Seeding: Plate human dermal fibroblasts (e.g., HDFs) in multi-well plates (e.g., 12 or 24-well) at a density of 5 x 10^4 cells/mL in standard growth medium. Allow cells to adhere overnight.
- Pre-treatment (Optional): Pre-incubate cells with your test compounds (e.g., TGF-βRI inhibitor or integrin antagonist) for 1-2 hours. Prepare a dilution series of the inhibitor in serum-free or low-serum medium.
- Stimulation: Replace the medium with fresh medium containing 2-5 ng/mL of recombinant active TGF-β1 to induce differentiation. Maintain the same concentration of your test inhibitor in the treatment wells. Include controls:
- Negative Control: Cells in medium only (no TGF-β1, no inhibitor).
- Positive Control: Cells with TGF-β1 only (no inhibitor).
- Vehicle Control: Cells with TGF-β1 + DMSO/equivalent solvent.
- Incubation: Culture the cells for 48-72 hours.
- Analysis:
- Protein Analysis (Western Blot): Lyse cells and analyze lysates via Western Blot for fibrotic markers: α-SMA (key outcome), phospho-Smad2/3 (pathway activation), and total Smad2/3 (loading control). Compare band intensity between treated and control groups [3].
- Immunofluorescence (IF): Fix cells, permeabilize, and stain for α-SMA (primary antibody) with a fluorescent secondary antibody. Use DAPI for nuclei. Visualize and quantify fluorescence intensity or the percentage of α-SMA-positive cells using fluorescence microscopy [3].
- Gene Expression (qRT-PCR): Extract RNA, synthesize cDNA, and perform qPCR for genes such as ACTA2 (α-SMA), COL1A1, and COL3A1. Normalize to housekeeping genes (e.g., GAPDH, ACTB) and express as fold-change relative to the positive control [3].
B. Protocol 2: Evaluating Compound Efficacy in anIn VivoMouse Model of Implant Fibrosis
This protocol outlines the key steps for testing anti-TGF-β therapies in an animal model of fibrotic encapsulation.
- Implant Preparation:
- Use small discs of medical-grade silicone (e.g., 5mm diameter).
- For localized drug delivery, implants can be coated with a matrix (e.g., poloxamer hydrogel, fibrin sealant) containing the test inhibitor (e.g., a TGF-βRI inhibitor) or a vehicle control [3].
- Surgery:
- Anesthetize mice according to your institutional animal care protocol.
- Make a small dorsal incision and create a subcutaneous pocket.
- Insert the prepared silicone implant into the pocket.
- Close the wound with sutures or clips.
- Administer post-operative analgesics.
- Systemic Dosing (Alternative to Coating): If testing systemic administration, begin dosing via intraperitoneal (IP) injection or oral gavage according to the compound's pharmacokinetic profile, starting on the day of surgery and continuing for the study duration.
- Study Duration and Endpoint: Maintain animals for 2-8 weeks to allow for mature capsule formation.
- Tissue Harvest and Analysis:
- Euthanize mice and carefully explant the silicone disc with the surrounding fibrous capsule intact.
- Capsule Thickness Measurement: Fix explants in formalin, process for paraffin embedding, and section. Stain with Hematoxylin and Eosin (H&E) for general histology and Masson's Trichrome or Picrosirius Red to visualize collagen. Measure capsule thickness in multiple locations per section using image analysis software [36] [3].
- Immunohistochemistry (IHC): Perform IHC on tissue sections for α-SMA (to identify myofibroblasts) and phospho-Smad2/3 (to confirm pathway inhibition in the treatment group) [3].
- Hydroxyproline Assay: Hydrolyze a portion of the capsule and use a hydroxyproline assay as a biochemical measure of total collagen content [3].
Troubleshooting Guide & FAQs
Q1: My test compound shows excellent efficacy in the in vitro fibroblast activation assay but fails to reduce capsule thickness in vivo. What could be the reason?
- A1: This is a common translational challenge. Consider the following:
- Bioavailability: The compound may have poor penetration into the dense, avascular fibrotic tissue surrounding the implant. Check the compound's distribution profile.
- Pharmacokinetics (PK): The half-life of the compound in vivo might be too short to maintain effective concentrations at the target site. Conduct PK studies to guide dosing frequency.
- Redundancy in Pathways: In vivo, multiple parallel pro-fibrotic pathways (e.g., PDGF, IL-13) may be activated, which can compensate for the inhibited TGF-β pathway. Consider combination therapies.
- Timing of Intervention: The therapeutic window may have been missed. Administering the inhibitor during the early inflammatory phase might be more effective than during later fibrotic stages.
Q2: In my in vitro assays, I observe high variability in α-SMA expression between technical replicates when stimulating with TGF-β. How can I improve consistency?
- A2:
- Cell Passage Number: Use fibroblasts at low, consistent passage numbers (e.g., P3-P8). High-passage cells can senesce and lose their responsiveness to TGF-β.
- Serum Batch: Use the same batch of fetal bovine serum (FBS) for an entire study, as different lots can have varying levels of endogenous growth factors that influence baseline fibroblast activity.
- TGF-β Preparation: Always use a fresh aliquot of recombinant TGF-β and ensure it is properly diluted and mixed to achieve a uniform concentration across all wells. Avoid repeated freeze-thaw cycles.
- Cell Density: Ensure cells are seeded at a highly consistent density to achieve uniform confluence at the time of stimulation.
Q3: What are the key controls needed for a rigorous in vivo implant study?
- A3: A well-designed study should include:
- Sham Control: Animals undergo the same surgical procedure without implant insertion to account for baseline wound healing.
- Vehicle-Control Implant Group: Animals receiving an implant coated with/dosed with the delivery vehicle only (e.g., DMSO, saline).
- Treatment Group(s): Animals receiving the implant with the active test compound.
- Reference Compound Group (if available): Animals treated with a known anti-fibrotic agent (e.g., a glucocorticoid like Triamcinolone) to validate the model's responsiveness [3].
Q4: How can I confirm that an integrin antagonist is working in my system and not just causing general cytotoxicity?
- A4:
- Viability Assay: Perform a standard cell viability assay (e.g., MTT, CCK-8) alongside your functional assay to rule out cytotoxic effects at the working concentration.
- Measure Active TGF-β: Use an ELISA specific for active TGF-β (not total TGF-β) on cell culture supernatants. A successful αVβ6/αVβ8 antagonist should significantly reduce the level of active TGF-β detected after latent complex stimulation, without affecting cell viability [37].
- Downstream Readout: Confirm reduced phosphorylation of Smad2/3, which is a specific downstream event of TGF-β pathway activation.
This technical support center is designed for researchers working within the field of breast implant bioengineering, specifically focusing on the challenge of preventing fibrotic encapsulation. Fibrosis, or capsular contracture, remains a primary cause of implant failure, often necessitating revision surgery. This process is driven by an excessive foreign body response (FBR), a complex cascade initiated upon implantation. At the heart of this response are macrophages, innate immune cells with remarkable plasticity. Their polarization state—toward pro-inflammatory (M1) or pro-healing (M2) phenotypes—critically influences whether the outcome is destructive fibrosis or harmonious integration [3] [36] [41]. This resource provides targeted troubleshooting guides, FAQs, and detailed protocols to aid in the development and testing of immunomodulatory surface coatings designed to steer macrophage responses toward positive outcomes and mitigate fibrotic encapsulation.
Core Concepts & Troubleshooting Guides
The Macrophage Polarization Balance in FBR
Understanding the default FBR sequence is essential for diagnosing issues in coating performance. The following diagram outlines the key cellular events following implantation.
Troubleshooting Guide: Uncontrolled M1-Driven Inflammation
- Problem: Histological analysis shows persistent M1 macrophages (iNOS+, TNF-α+, IL-1β+) and thick, dense collagen capsules around the implant.
- Potential Cause & Solution:
- Cause 1: Coating surface chemistry promotes excessive adsorption of pro-inflammatory proteins like fibrinogen.
- Solution: Modify coating with anti-fouling polymers (e.g., PEG, zwitterions) to reduce non-specific protein adsorption [3] [41].
- Cause 2: Surface topography presents micro-scale features that physically frustrate macrophages, preventing phagocytosis.
- Solution: Re-engineer surface topography to include nanoscale features or specific roughness that promotes M2 polarization. Rough-hydrophilic titanium surfaces have been shown to skew macrophages toward an M2 phenotype [42] [36].
- Cause 3: The coating is releasing cytotoxic degradation products or contaminants (e.g., endotoxins).
- Solution: Implement rigorous material purification and sterility checks. Use in vitro cytotoxicity assays (e.g., with RAW 264.7 cells) before in vivo testing.
Signaling Pathways in Macrophage Polarization
A key mechanism by which coatings exert their effect is by interacting with specific signaling pathways that control macrophage polarization. The following diagram summarizes the major pathways involved in M1 and M2 activation.
Troubleshooting Guide: Inadequate M2 Polarization
- Problem: Coating fails to induce a sufficient M2 response in vitro or in vivo, with low expression of markers like CD206, Arg1, and IL-10.
- Potential Cause & Solution:
- Cause 1: Coating lacks specific biochemical cues to activate M2 pathways (e.e., IL-4/STAT6).
- Solution: Functionalize the surface with immobilized M2-inducing cytokines (e.g., IL-4, IL-13) or use coatings that release these factors in a controlled manner [9].
- Cause 2: The physical cues from the surface (e.g., stiffness, topography) are insufficient to trigger mechanotransduction pathways that promote M2 polarization.
- Solution: Tune the elastic modulus of the coating to mimic that of native breast tissue (~1 kPa). Incorporate specific topological cues known to promote an anti-inflammatory phenotype [36].
- Cause 3: The coating is too hydrophobic, which is associated with a pro-inflammatory M1 response.
- Solution: Increase surface hydrophilicity through plasma treatment or chemical grafting. Rough-hydrophilic titanium surfaces have demonstrated a clear shift toward M2 polarization compared to smooth-hydrophobic ones [42].
Frequently Asked Questions (FAQs)
Q1: What are the key surface properties of a biomaterial that influence macrophage polarization? The three key properties are topography, chemistry (including wettability and charge), and stiffness. Topography (e.g., rough vs. smooth) directly affects cell adhesion and shape, which in turn influences phenotype. Surface chemistry determines the initial "molecular fingerprint" of adsorbed proteins, which is the first signal immune cells encounter. Stiffness that mimics healthy, soft tissue is generally associated with reduced inflammation and fibrosis [3] [36] [41].
Q2: How can I quantitatively assess the success of an immunomodulatory coating in an animal model? A multi-faceted approach is critical. Key quantitative metrics include:
- Histomorphometry: Measure capsular thickness from H&E stained sections.
- Immunohistochemistry/Immunofluorescence: Quantify the ratio of M2 (CD206, Arg1) to M1 (iNOS, CD86) macrophages within the peri-implant tissue.
- Gene Expression Analysis: Use qPCR on harvested capsule tissue to measure expression of pro-fibrotic (TGF-β, Collagen I) and pro-inflammatory (TNF-α, IL-1β) genes.
- Functional Assessment: For bone-adjacent implants, measure Bone-to-Implant Contact (BIC) via micro-CT or histology [42].
Q3: My in vitro macrophage culture results do not seem to translate to my in vivo model. What could be the reason? This is a common challenge. The simplified in vitro environment lacks the complexity of the in vivo milieu. Key differences include:
- The Protein Corona: In vivo, the implant is immediately coated with a complex mixture of serum proteins, which may differ significantly from the single protein solutions often used in vitro.
- Cellular Crosstalk: In vivo, macrophages interact with many other cell types (e.g., T cells, fibroblasts, mesenchymal stem cells) that profoundly influence their polarization. An in vitro finding that adoptive transfer of M2 macrophages improves outcomes highlights the importance of the broader cellular environment [42] [9].
- Mechanical and Dynamic Environment: In vivo, cells experience fluid flow and mechanical stresses absent in static culture. Always validate key in vitro findings in a biologically complex model.
Q4: Are there any clinical or pre-clinical examples where modulating macrophage response has improved implant outcomes? Yes. Clinically, textured implants were initially introduced partly to disrupt the linear scar formation of capsular contracture, though the association of some highly textured implants with BIA-ALCL has complicated this picture [43] [44]. In pre-clinical studies, rough-hydrophilic titanium implants have been shown to skew macrophages toward an M2-like phenotype, leading to increased bone-to-implant contact in osseointegration models [42]. Furthermore, the adoptive transfer of in vitro-generated M2 macrophages into macrophage-competent mice has been shown to reduce the pro-inflammatory environment and improve implant integration [42].
Experimental Protocols & Data Presentation
Detailed Protocol: In Vitro Macrophage Polarization Assay on Coated Surfaces
This protocol is used to screen coating strategies for their ability to direct macrophage polarization.
Material Preparation:
- Prepare your coated samples and uncoated controls (e.g., smooth silicone) in 24-well plate formats. Sterilize via UV irradiation or ethanol wash.
- Blocking: Incubate samples with 1% Bovine Serum Albumin (BSA) in PBS for 1 hour to block non-specific binding sites.
Cell Seeding and Culture:
- Use a murine macrophage cell line (e.g., RAW 264.7) or primary bone marrow-derived macrophages (BMDMs).
- Seed cells at a density of 1 x 10^5 cells/well in standard culture medium and allow to adhere for 6 hours.
- Replace medium with polarization-inducing medium:
- M0 (Control): Base medium only.
- M1 (Positive Control): Base medium + 100 ng/mL LPS + 20 ng/mL IFN-γ.
- Test Group: Base medium only (the coating itself provides the polarizing stimulus).
Incubation and Harvest:
- Incubate cells for 48 hours.
- For RNA Extraction: Lyse cells directly in TRIzol reagent for subsequent RNA extraction and qPCR analysis.
- For Protein Analysis: Lyse cells in RIPA buffer for Western blotting or cytokine analysis via ELISA.
- For Immunofluorescence: Fix cells with 4% PFA for 15 minutes and permeabilize with 0.1% Triton X-100.
Analysis:
- qPCR Markers:
- M1: iNOS (Nos2), TNF-α, IL-1β, IL-6.
- M2: Arg1, Ym1 (Chi3l3), Fizz1 (Retnla), CD206 (Mrc1).
- Protein/IF Markers: Use antibodies against iNOS (M1) and CD206 or Arg1 (M2).
- ELISA: Measure secretion of TNF-α (M1) and IL-10 (M2) in the culture supernatant.
- qPCR Markers:
Quantitative Data from Key Studies
The following tables summarize critical quantitative findings from the literature, which can serve as benchmarks for your own experimental results.
Table 1: Impact of Macrophage Manipulation on Implant Integration Outcomes (Pre-clinical Model)
| Experimental Group | Key Finding (vs. Control) | Measurement Technique | Reference |
|---|---|---|---|
| Macrophage Ablation | ↑ Neutrophils; ↓ T cells & MSCs; compromised healing | Flow Cytometry, Histology | [42] |
| Adoptive Transfer of M1 Macrophages | ↑ Inflammatory cells; ↓ Bone-to-Implant Contact | Histomorphometry | [42] |
| Adoptive Transfer of M2 Macrophages | ↓ Pro-inflammatory environment; ↑ Bone-to-Implant Contact | Cytokine Assay, Histomorphometry | [42] |
| Rough-Hydrophilic Titanium Implant | Skewed macrophage polarization to M2-like phenotype | qPCR, Cytokine Secretion | [42] |
Table 2: Cytokine Profiles of Polarized Human Macrophages
| Macrophage Phenotype | Characteristic Cytokines & Mediators | Primary Functions | Reference |
|---|---|---|---|
| M1 (Classically Activated) | TNF-α, IL-1β, IL-6, IL-12, IL-23, ROS, NO | Pathogen clearance, Pro-inflammatory response, Initiation of adaptive immunity, Potent Antigen Presentation | [9] [41] |
| M2 (Alternatively Activated) | IL-10, TGF-β, CCL17, CCL18, Arg1 | Immunosuppression, Tissue repair & remodeling, Fibrosis promotion, Resolution of inflammation | [42] [9] [41] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Macrophage and FBR Research
| Item | Function/Application in Research | Example & Notes |
|---|---|---|
| RAW 264.7 Cell Line | Murine macrophage line for high-throughput in vitro screening of coating effects on polarization. | Easy to culture and transfect. Results should be validated in primary cells. |
| Primary BMDMs | Gold standard for in vitro studies, providing a more physiologically relevant model than cell lines. | Isolated from mouse femurs and tibias and differentiated with M-CSF. |
| Polarizing Cytokines | To generate positive controls for M1 (LPS + IFN-γ) and M2 (IL-4, IL-13, IL-10) phenotypes in vitro. | Use high-purity, carrier-protein-free reagents for reliable results. |
| Antibodies for Flow/IF | To identify and quantify macrophage populations and polarization states. | M1: anti-iNOS, anti-CD86. M2: anti-CD206, anti-Arginase-1. |
| ELISA Kits | To quantitatively measure cytokine secretion (e.g., TNF-α, IL-1β for M1; IL-10, TGF-β for M2). | Essential for functional validation of polarization. |
| MaFIA Mouse Model | (Macrophage Fas-Induced Apoptosis) Allows for inducible ablation of macrophages to study their specific role in FBR in vivo. | Critical for establishing causality of macrophage function [42]. |
| Acellular Dermal Matrix (ADM) | A biologic scaffold used in reconstruction to provide a supportive, immunomodulatory interface between implant and host tissue. | Can reduce capsular contracture; modulates the host immune response [3] [44]. |
| Jatrophane 3 | Jatrophane 3, MF:C43H53NO14, MW:807.9 g/mol | Chemical Reagent |
| (Z)-Aconitic acid | (Z)-Aconitic acid, MF:C94H82N4O2S4, MW:1427.9 g/mol | Chemical Reagent |
Addressing Clinical Variability and Overcoming Translational Hurdles
The foreign body response (FBR) to breast implants represents a complex immunological cascade that can lead to fibrotic encapsulation, the most common long-term complication in implant-based breast surgery [45]. Capsular fibrosis (CF) occurs when the scar tissue naturally forming around the implant becomes unusually hard, causing pain, anatomical displacement, and often requiring surgical intervention [46]. Recent advances in immunomics—the comprehensive study of immune system responses using high-throughput technologies—now enable researchers to move beyond descriptive histology toward predictive modeling of individual patient risk. The incidence of capsular contracture ranges from 10% to 20%, with recurrence rates as high as 54% following conventional revision surgery [46]. This technical support framework provides methodologies for stratifying patient risk through immunomic profiling, enabling targeted anti-fibrotic interventions.
The foundational science underlying this approach recognizes that breast implants inevitably trigger a foreign body response, a sophisticated biological process involving precise sequences of protein adsorption, immune cell recruitment, and fibroblast activation [45]. The implant surface properties, including topography, hydrophobicity, and charge, establish an initial "molecular fingerprint" that dictates subsequent cellular interactions and ultimately dictates the extent of fibrotic encapsulation [45]. By mapping these immunological pathways at the individual patient level, researchers can now identify key biomarkers predictive of adverse fibrotic outcomes, creating opportunities for personalized prophylactic strategies.
Technical Support Center
Troubleshooting Guides
Guide 1: Inconsistent Flow Cytometry Results in Implant Patient Immunophenotyping
- Problem: High inter-patient variability in lymphocyte subpopulation measurements obscures significant findings.
- Solution: Implement the standardized panel from [47] with strict pre-analytical protocols:
- Sample Collection: Collect 5mL peripheral blood in EDTA tubes via standard venipuncture.
- Processing Timeline: Transport to laboratory within 24 hours and process immediately.
- Antibody Panel: Use clones anti-CD3 Leu-4 SK7, anti-CD4 Leu-3a SK3, anti-CD8 Leu-2a SK1, anti-CD16+56 Leu-11c + Leu-19 B73.1 MY31, anti-CD19 Leu-12 4G7, anti-CD25 IL-2Rα 2A3, and anti-CD45 Hle-1 2D1.
- Staining Protocol: Incubate 100μL blood with 10μL antibodies at room temperature (out of direct light) for 15 minutes.
- Erythrocyte Lysis: Use FACSLyse solution (2mL) followed by two PBS washes and centrifugation at 3500 rpm for 10 minutes.
- Fixation: Resuspend cell pellet in 0.5mL PBS for fixation.
- Gating Strategy: Gate lymphocytes by forward and right-angle light scattering [47].
Guide 2: Poor Quality Capsular Tissue for Transcriptomic Analysis
- Problem: RNA degradation in periprosthetic capsular tissue compromises transcriptome studies.
- Solution:
- Harvesting Technique: Collect tissue samples using sharp dissection to minimize mechanical stress.
- Stabilization: Immediately place tissue in RNAlater stabilization solution.
- Storage Conditions: Flash-freeze in liquid nitrogen for long-term storage at -80°C.
- Documentation: Record implant location (subpectoral/subglandular), time since implantation, and Baker score for all samples.
- Reference Methodology: Consult the RNA sequencing approach from [48] which analyzed over 28,000 genomic markers in breast tissue adjacent to implants.
Guide 3: Detecting Subtle Macrophage Polarization Shifts
- Problem: Standard immunohistochemistry fails to quantify continuum of macrophage phenotypes in fibrotic capsules.
- Solution: Employ multiplex immunofluorescence with validated markers:
- M1 Macrophages: CD68+/CD80+/CD86+/IL-1β+
- M2 Macrophages: CD68+/CD163+/CD206+/IL-10+
- Quantification Method: Use automated image analysis software to calculate M1:M2 ratio across multiple high-power fields.
- Validation: Correlate with TGF-β1 expression levels as key pro-fibrotic mediator [45].
- Temporal Analysis: Sample at multiple timepoints (15, 30, 90 days) to track polarization dynamics [49].
Frequently Asked Questions (FAQs)
Q1: What is the most reliable method for detecting subclinical silicone exposure in periprosthetic tissue?
A1: SEM and TEM analysis provides the highest sensitivity for identifying silicone fragments and their cellular context. The methodology in [49] successfully detected silicone particles and associated coccoid bacteria as early as 30 days post-implantation. Key findings include:
- Silicone fragments preferentially accumulate in implant surface concavities
- Fragment presence correlates with bacterial colonization and histiocytic infiltration
- Sample preparation requires critical point drying to preserve ultrastructure
Q2: Does implant rupture cause measurable systemic immune activation?
A2: Current evidence suggests rupture does not significantly alter systemic immunity. A comprehensive study of 67 women (16 with ruptured implants, 51 with intact implants) found:
- No significant differences in antibody levels against breast-related antigens (CEA, MUC-1, ER, HER-2, mammaglobin-A)
- Only one immune-related differentially expressed gene (MS4A1) in local breast tissue
- No evidence for immune-related changes explaining autoimmune-like symptoms [50]
Q3: What are the key temporal phases of the foreign body response that should be sampled for comprehensive immunomic profiling?
A3: The FBR progresses through five distinct phases that should be sampled strategically [45]:
- Protein adsorption (minutes to hours): Sample immediately for proteomic analysis of corona composition
- Acute inflammation (days): Focus on neutrophil and monocyte recruitment markers
- Chronic inflammation (weeks): Analyze macrophage and lymphocyte populations
- Foreign body giant cell formation (weeks to months): Evaluate fusion-related proteins (DC-STAMP, MMPs)
- Fibrosis (months to years): Assess collagen deposition, myofibroblast differentiation, and TGF-β signaling
Q4: How can researchers distinguish Breast Implant Illness (BII) from other autoimmune conditions in study populations?
A4: A systematic review of 6,048 women with BII identified key characteristics [51]:
- Symptom onset typically occurs 6.4 years post-implantation
- Most common symptoms: fatigue (58.3%), joint pain (51%), muscle pain (44%)
- Explantation leads to symptom improvement in 81.9% of cases after 12.3 years average implantation
- Differentiating biomarkers may include ANA positivity (24%) and capsular inflammation (58.4%)
- Consider comorbid fibromyalgia (12%) and pre-existing autoimmune conditions (20.7%) as confounding factors
Quantitative Data Synthesis
Table 1: Peripheral Blood Immune Cell Dynamics Following Breast Implantation [47]
| Immune Parameter | Preoperative (Mean % ± SD) | 3 Months Postoperative (Mean % ± SD) | 12 Months Postoperative (Mean % ± SD) | P-value |
|---|---|---|---|---|
| Lymphocytes | 31.24 ± 4.89 | 33.26 ± 5.78 | 33.31 ± 5.11 | 0.375 |
| Polymorphonuclear cells | 60.36 ± 6.16 | 58.49 ± 6.91 | 58.16 ± 4.65 | 0.461 |
| Monocytes | 5.75 ± 1.64 | 5.19 ± 1.89 | 5.67 ± 1.66 | 0.468 |
| T-helper lymphocytes (CD3+/CD4+) | 43.17 ± 7.31 | 41.93 ± 7.61 | 42.07 ± 6.38 | 0.789 |
| Cytotoxic T lymphocytes (CD3+/CD8+) | 27.25 ± 5.94 | 28.27 ± 5.93 | 27.90 ± 4.27 | 0.801 |
Table 2: Clinical Characteristics of Breast Implant Illness Populations [51]
| Parameter | Pooled Prevalence (%) | Mean Timeframe | Notes |
|---|---|---|---|
| Symptom improvement post-explantation | 81.9% | - | Based on systematic review of 33 studies |
| Time to symptom onset | - | 6.4 years | From implantation to first symptoms |
| Time to explantation | - | 12.3 years | From implantation to removal |
| Most common symptoms: Fatigue | 58.3% | - | - |
| Joint pain | 51.0% | - | - |
| Muscle pain | 44.0% | - | - |
| Capsular contracture | 44.4% | - | Medical reason for explantation |
| ANA positivity | 24.0% | - | Potential autoimmune association |
| Pre-existing autoimmune conditions | 20.7% | - | Confounding factor |
| Implant rupture | 21.4% | - | - |
| Psychiatric illness history | 16.5% | - | Confounding factor |
| Fibromyalgia | 12.0% | - | Overlapping symptom complex |
Table 3: Advanced Imaging Applications in Capsular Fibrosis Research [49]
| Technique | Resolution | Primary Applications in CF Research | Key Findings |
|---|---|---|---|
| Scanning Electron Microscopy (SEM) | 3D surface visualization | • Implant-tissue interface analysis• Collagen architecture• Bacterial biofilm detection | • Architectural shift in collagen from unidirectional to multidirectional by day 90• Silicone fragments with coccoid bacteria at day 30• Increased histiocytes at later timepoints |
| Transmission Electron Microscopy (TEM) | 0.2 nm | • Intracellular visualization• Collagen fiber organization• Organelle-level changes in immune cells | • Increased collagen concentration over time (15-90 days)• Multidirectional collagen arrangement in established fibrosis |
| Light Microscopy | Varies with magnification | • Initial tissue assessment• Cellularity evaluation• Guide for further analysis | • Identification of lymphocytic infiltration at inner capsular surface• Visualization of smooth muscle cells and fibroblasts |
Experimental Protocols
Protocol: Flow Cytometric Immunophenotyping of Implant Patients
Purpose: To quantify lymphocyte subpopulations in peripheral blood of patients with silicone breast implants for systemic immune monitoring [47].
Materials:
- EDTA blood collection tubes
- Monoclonal antibodies: CD3, CD4, CD8, CD16/CD56, CD19, CD25, CD45
- FACSLyse solution (Becton Dickinson)
- Phosphate-buffered saline (PBS)
- FACScan flow cytometer with CellQuest V3.1 software
Procedure:
- Collect 5mL peripheral blood in EDTA tubes via venipuncture
- Within 24 hours, add 100μL blood to tubes with 10μL fluorescent-conjugated antibodies
- Incubate 15 minutes at room temperature, protected from light
- Add 2mL FACSLyse solution, incubate for erythrocyte lysis
- Centrifuge at 3500 rpm for 10 minutes
- Wash with 2mL PBS, repeat centrifugation
- Resuspend cell pellet in 0.5mL PBS for fixation
- Analyze by flow cytometry with lymphocyte gating by forward/side scatter
- Collect data from ≥10,000 events per sample
Analysis: Compare preoperative (baseline) with 3-month and 12-month postoperative timepoints using repeated measures ANOVA.
Protocol: Ultrastructural Analysis of Periprosthetic Capsules
Purpose: To characterize cellular behavior and extracellular matrix composition in capsular fibrosis using SEM and TEM [49].
Materials:
- Scanning Electron Microscope (e.g., JEOL JSM-7500F)
- Transmission Electron Microscope
- Critical point dryer
- Sputter coater
- Uranyl acetate and lead citrate for staining
- Glutaraldehyde and osmium tetroxide for fixation
SEM Procedure:
- Fix capsular tissue samples in 2.5% glutaraldehyde in 0.1M cacodylate buffer
- Post-fix in 1% osmium tetroxide for 1 hour
- Dehydrate through graded ethanol series (30%-100%)
- Critical point dry using liquid COâ‚‚
- Mount on aluminum stubs and sputter coat with gold-palladium
- Image at accelerating voltages of 5-15 kV
TEM Procedure:
- Fix tissue samples in 2.5% glutaraldehyde followed by 1% osmium tetroxide
- Dehydrate through ethanol series and embed in epoxy resin
- Cut ultrathin sections (70-90 nm) using ultramicrotome
- Stain with uranyl acetate and lead citrate
- Examine at 80 kV accelerating voltage
Key Observations:
- Collagen architecture (unidirectional vs. multidirectional)
- Cellular infiltration (histiocytes, lymphocytes, foreign body giant cells)
- Silicone fragment presence and associated bacteria
- ECM density and composition
Signaling Pathways and Experimental Workflows
Foreign Body Response to Fibrosis Pathway
Immunomic Risk Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for Breast Implant Immunomics
| Research Tool | Specific Application | Function/Utility | Example References |
|---|---|---|---|
| Flow Cytometry Antibodies | Peripheral blood immunophenotyping | Quantification of lymphocyte subpopulations (T-cells, B-cells, NK cells) and activation markers | CD3, CD4, CD8, CD16/56, CD19, CD25 [47] |
| SEM/TEM Equipment | Capsular ultrastructure analysis | High-resolution imaging of implant-tissue interface, collagen architecture, and cellular infiltration | [49] |
| RNA Sequencing | Transcriptomic profiling | Genome-wide analysis of gene expression in periprosthetic tissue; identification of fibrotic pathways | Analysis of >28,000 genomic markers [48] |
| Macrophage Polarization Markers | Immunohistochemistry/IF | Differentiation of M1 (pro-inflammatory) vs M2 (pro-fibrotic) macrophage populations in capsules | CD68, CD80, CD163, CD206, iNOS, Arg1 [45] |
| Cytokine Assays | Inflammation monitoring | Measurement of pro-fibrotic cytokines (TGF-β, IL-4, IL-13, PDGF) in serum and tissue | TGF-β emphasis [45] |
| Bacterial Detection Kits | Biofilm analysis | Identification of bacterial colonization (S. epidermidis) associated with capsule formation | Coccoid bacteria detection [49] |
| Automated Image Analysis Software | Collagen quantification | Digital pathology assessment of collagen density, orientation, and capsule thickness | Collagen architectural shift analysis [49] |
| Machine Learning Algorithms | Predictive modeling | Integration of multi-omics data for patient stratification and fibrosis risk prediction | Adaptive Boosting (Adaboost) [52] |
| FPR1 antagonist 2 | FPR1 Antagonist 2 | Bench Chemicals |
Fibrotic encapsulation is a physiological response where the body forms a protective tissue capsule around a foreign object, such as a breast implant [7]. While this process is normal, excessive fibrosis can lead to capsular contracture, a complication characterized by tissue hardening, pain, and implant distortion, which remains a primary challenge in long-term implant success [7] [29]. This guide explores how surgical technique and implant placement choices directly influence the molecular and cellular pathways driving this fibrotic response, providing researchers with frameworks for experimental investigation.
The foreign body reaction (FBR) proceeds through defined biological phases: immediate blood-material interactions, provisional matrix formation, acute and chronic inflammation, foreign body giant cell formation, and finally, fibrous capsule development [7] [3]. Surgical decisions can modulate each stage, making understanding these mechanisms crucial for developing anti-fibrotic strategies.
Key Biological Mechanisms and Pathways
Cellular Players in Fibrosis
The fibrotic process involves coordinated interactions between multiple immune and structural cells:
- Macrophages: Central regulators transitioning from pro-inflammatory M1 phenotypes (secreting TNF-α, IL-1, IL-6) to pro-fibrotic M2 phenotypes (secreting TGF-β) that drive tissue remodeling [7] [3].
- Fibroblasts: Differentiate into myofibroblasts under TGF-β stimulation, expressing α-smooth muscle actin (α-SMA) and secreting collagen types I and III to form the fibrous capsule [3].
- T-Lymphocytes: Particularly IL-17-secreting CD4+ T cells and γδ+ T cells, which promote fibrotic progression through cytokine signaling [3].
- Foreign Body Giant Cells (FBGCs): Formed from macrophage fusion, these cells create an acidic microenvironment and release degradative factors that can contribute to implant damage [7].
Molecular Signaling Pathways
The diagram below illustrates the core signaling pathways driving fibrotic encapsulation, highlighting potential therapeutic intervention points.
Impact of Surgical Variables: Experimental Data
Surgical technique significantly influences fibrotic outcomes through multiple mechanistic pathways. The following table summarizes key surgical variables and their documented impact on capsule formation.
Table 1: Surgical Variables and Their Impact on Fibrotic Outcomes
| Surgical Variable | Experimental/Cinical Findings | Proposed Mechanism | Effect on Capsule Pathology |
|---|---|---|---|
| Incision Site [29] | Periareolar incisions associated with 5.36% CC rate vs. 1.64% for inframammary fold | Greater bacterial exposure through mammary ducts | ↑ Inflammation → ↑ Fibrosis risk |
| Pocket Location [29] [44] | Submuscular placement reduces CC risk vs. subglandular | Vascularized tissue barrier reduces inflammation | ↓ CC rates in reconstructive surgery |
| Implant Surface [29] [3] | Textured implants show lower CC incidence than smooth surfaces | Tissue ingrowth disrupts fibrous capsule organization | Alters collagen density & orientation |
| Procedural Contamination [53] | Bacterial biofilm above threshold level triggers CC | Chronic inflammation via T-cell response | Direct correlation with contracture severity |
The Scientist's Toolkit: Essential Reagents & Models
This section details critical reagents, model systems, and experimental methodologies for investigating fibrotic encapsulation.
Table 2: Essential Research Reagents and Experimental Models
| Reagent/Model | Research Application | Key Function/Mechanism |
|---|---|---|
| Triamcinolone acetonide [3] | Pharmacologic coating on implants | Glucocorticoid that inhibits inflammatory cascades |
| Tranilast [3] | Anti-fibrotic drug delivery | Suppresses TGF-β release and collagen synthesis |
| Acellular Dermal Matrix (ADM) [29] [44] | Implant coverage in surgical models | Provides structural barrier, modulates host response |
| Mouse/Porcine Implant Models [7] [53] | In vivo fibrosis studies | Recapitulates human FBR for therapeutic testing |
| CD30 Immunohistochemistry [44] | BIA-ALCL detection in capsule tissue | Diagnostic marker for lymphoma in chronic inflammation |
| α-SMA Staining [3] | Myofibroblast identification | Marker for activated fibroblasts in fibrotic capsules |
| Capsule Histology Scoring [7] [29] | Fibrosis severity quantification | Collagen density, cellularity, and thickness metrics |
Experimental Workflow for Fibrosis Assessment
The following diagram outlines a comprehensive experimental workflow for evaluating fibrotic encapsulation in preclinical models.
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q: What are the primary molecular targets for preventing myofibroblast differentiation in capsular fibrosis? A: The central molecular target is the TGF-β signaling pathway [3]. Both Smad-dependent and Smad-independent (including Rho/ROCK) pathways drive fibroblast-to-myofibroblast differentiation. Experimental approaches include TGF-β neutralizing antibodies, ROCK inhibitors, and targeting senescent cells that secrete pro-fibrotic factors.
Q: How does implant surface topography influence the immune response at the molecular level? A: Surface topography directly affects immune cell polarization [29] [3]. Nanotextured surfaces promote immunosuppressive FOXP3+ T cells and M2 macrophage phenotypes, reducing fibrotic responses. In contrast, smooth surfaces trigger stronger myofibroblast activation and form denser collagen bundles.
Q: What is the relationship between bacterial biofilm and the pathogenesis of capsular contracture? A: Biofilm formation creates chronic inflammation that drives fibrosis [53]. Bacteria bound to the implant surface resist host defenses, stimulating persistent T-cell responses and cytokine release (particularly IL-1, IL-6, TNF-α). This inflammatory milieu activates fibroblasts and promotes collagen deposition.
Q: Which animal models best recapitulate human capsular contracture for therapeutic testing? A: Porcine models demonstrate direct correlation between bacterial load and contracture severity [53]. Rodent models are valuable for investigating molecular mechanisms and immune cell contributions [3]. Each model offers advantages: porcine for biofilm studies and surgical technique refinement, murine for genetic and pathway manipulation.
Technical Issue Resolution
Table 3: Troubleshooting Common Experimental Challenges
| Experimental Challenge | Potential Cause | Solution |
|---|---|---|
| High variability in capsule thickness measurements | Inconsistent harvesting techniques; orientation during processing | Implement standardized dissection protocols; use suture markers for consistent orientation during embedding |
| Poor RNA quality from capsule tissue | High collagen content; rapid RNA degradation | Immediate stabilization in RNAlater; implement mechanical disruption protocols; use specialized high-fibrosis RNA kits |
| Inconsistent histology scoring | Subjective assessment criteria; multiple reviewers | Develop standardized scoring system with reference images; implement blinded review; calculate inter-rater reliability |
| Failure to detect cytokine differences | Insensitive assays; inappropriate timepoints | Use multiplex cytokine arrays; perform time-course experiments focusing on early inflammatory phase (1-4 weeks) |
| Animal model not developing contracture | Species/strain selection; implant surface characteristics | Use established porcine models with textured implants; consider bacterial contamination models to induce stronger FBR |
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary biological mechanisms driving fibrotic encapsulation? The formation of a fibrous capsule is a pathological foreign body reaction (FBR) that unfolds in six key stages: (i) blood-biomaterial interaction and provisional matrix formation, (ii) acute inflammation, (iii) chronic inflammation, (iv) formation of foreign body giant cells (FBGCs), (v) fibrous capsule formation, and (vi) in the case of contracture, pathological contraction of this capsule [3]. This process is driven by a complex interplay of immune cells. The initial acute inflammatory phase is characterized by the recruitment of polymorphonuclear leukocytes (PMNs), which secrete pro-inflammatory cysteinyl leukotrienes (CysLTs) [3]. If the foreign body persists, the response transitions to chronic inflammation, dominated by macrophages. The polarization of these macrophages into pro-fibrotic (M1) and pro-resolving (M2) phenotypes is critical; a persistent M1 response exacerbates inflammation and fibrosis [3]. Key cells such as fibroblasts are then driven by cytokines, including Transforming Growth Factor-Beta (TGF-β), to differentiate into myofibroblasts. These myofibroblasts, characterized by α-smooth muscle actin (α-SMA) expression, secrete and contract collagen, leading to the formation of a dense, avascular collagenous capsule that can tighten and deform [3].
FAQ 2: Which patient-specific and surgical factors are most strongly linked to an increased risk of capsular contracture? Clinical evidence has identified several significant risk factors. A 2025 retrospective study of 212 patients found that a positive smoking history, implant oversizing, and postoperative hematoma formation were independent risk factors for capsular contracture [54] [55]. The associated odds ratios from this study are summarized in Table 1 below. Beyond these, surgical factors play a crucial role. The surgical approach matters, with periareolar incisions associated with a higher incidence of contracture compared to inframammary fold incisions, likely due to the higher bacterial load from transected mammary ducts [56]. The placement of the implant also influences risk, as subglandular placement has been associated with a higher risk of contracture compared to submuscular placement [56]. Furthermore, subclinical infection and biofilm formation on the implant surface are considered major contributors to the chronic inflammatory response that leads to contracture [56].
FAQ 3: How do implant surface characteristics influence the foreign body response and subsequent fibrosis? Implant surface topography is a key modulator of the host immune response and a critical area of innovation. Textured surfaces were initially developed to disrupt the linear alignment of collagen fibers, thereby preventing the contraction of the capsule [54]. However, the relationship between texture and contracture is complex, with clinical studies showing conflicting results [54] [57]. The type of texture is crucial; macrotextured implants have been linked to bicapsular formation and Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) [56]. In contrast, emerging data suggests that nanostructured implants demonstrate superior biocompatibility, resulting in the minimum capsular thickness, reduced collagen density, and less myofibroblast infiltration [56]. These surfaces appear to balance roughness and mobility, potentially reducing the risk of both contracture and malignancy. Surface properties also influence the immune response; for instance, coarse-textured implants may favor the anti-fibrotic M2 macrophage phenotype, thereby minimizing the fibrotic response [56].
Troubleshooting Guide for Common Experimental and Clinical Challenges
Problem: High Rate of Capsular Contracture in Preclinical Model
- Potential Cause 1: Bacterial contamination and biofilm formation on the implant.
- Solution: Implement rigorous aseptic surgical protocols. Consider irrigating the implant pocket with an antibiotic solution (e.g., a combination of cephalosporin and gentamicin) [54] [55]. Utilize antimicrobial coatings on the implant itself, such as silver nanoparticles (NAg) or other antibacterial technologies, in experimental settings [3].
- Potential Cause 2: Excessive implant-to-pocket size mismatch (oversizing) leading to sustained tension.
- Solution: Utilize preoperative planning systems to select an implant volume that matches the patient's anatomical dimensions. In a clinical context, avoid implant oversizing, defined as a volume exceeding the recommended capacity by 20% or more [54] [55].
- Potential Cause 3: Post-operative hematoma.
- Solution: Ensure meticulous hemostasis during surgery. The use of post-operative negative pressure drainage tubes until drainage is minimal (e.g., <30 ml/24 hours) can help prevent hematoma formation [54] [55].
Problem: Inconsistent Fibrotic Readouts in Animal Studies
- Potential Cause: Variable host response to different implant surface topographies.
- Solution: Standardize and carefully document the implant surface characteristics (smooth, microtextured, macrotextured, nanotextured) across all experimental groups. Be aware that animal models may not perfectly replicate human fibrotic responses to different textures [56]. Ensure that capsule analysis includes multiple metrics: histological assessment of collagen density and alignment, immunohistochemical staining for key markers (α-SMA, TGF-β, CD68), and measurement of capsular thickness.
Detailed Experimental Protocols
Protocol 1: Histopathological Evaluation and Scoring of Fibrotic Capsules This protocol is essential for standardizing the analysis of fibrotic tissue in both preclinical and clinical studies.
- Tissue Harvest: After explantation, the fibrous capsule should be carefully dissected from the surrounding tissue.
- Sectioning: Divide the capsule into standardized segments (e.g., anterior, posterior, medial, lateral) for comprehensive analysis.
- Fixation and Staining: Fix tissue segments in formalin and embed in paraffin. Section and stain with:
- Hematoxylin and Eosin (H&E): For general histology and cellularity assessment.
- Masson's Trichrome or Picrosirius Red: To visualize and quantify collagen deposition and fiber alignment.
- Immunohistochemistry (IHC): Perform IHC staining for critical fibrotic markers:
- α-Smooth Muscle Actin (α-SMA): To identify activated myofibroblasts.
- Transforming Growth Factor-Beta (TGF-β): A key pro-fibrotic cytokine.
- CD68: To identify macrophage infiltration and distribution.
- Scoring System: Establish a semi-quantitative scoring system (e.g., 0-3) for parameters such as inflammatory cell density, myofibroblast presence, collagen density, and capsule thickness. This allows for comparative statistical analysis [3] [56].
Protocol 2: In Vitro Assessment of Macrophage-Implant Material Interactions This methodology helps to decode the initial immune response to new implant materials or coatings.
- Material Preparation: Sterilize the test biomaterial (e.g., silicone discs with different surface topographies or coatings) and place them in a multi-well culture plate.
- Cell Seeding: Isulate and differentiate human monocyte-derived macrophages, or use a monocytic cell line (e.g., THP-1) differentiated into macrophages. Seed the cells onto the material surfaces.
- Polarization and Stimulation: Polarize macrophages towards M1 (using LPS and IFN-γ) or M2 (using IL-4 and IL-13) phenotypes in the presence of the test material.
- Analysis:
- Gene Expression: Use qPCR to analyze the expression of M1 markers (e.g., TNF-α, IL-1β) and M2 markers (e.g., CD206, TGF-β).
- Protein Secretion: Use ELISA to measure the secretion of pro-fibrotic (e.g., IL-17, TGF-β) and anti-fibrotic cytokines in the supernatant.
- Cell Morphology: Use scanning electron microscopy (SEM) to visualize macrophage adhesion and fusion into foreign body giant cells (FBGCs) [3].
Visualizing Key Signaling Pathways and Workflows
Fibrotic Encapsulation Signaling Network
Experimental Workflow for Implant Fibrosis Research
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Investigating Fibrotic Encapsulation
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| Nanostructured Silicone Implants [56] | Test substrate for modulating foreign body response. | Minimal capsular thickness; reduced collagen density and myofibroblast infiltration. |
| Acellular Dermal Matrix (ADM) [3] | Bioactive scaffold used to reduce fibrosis in experimental and clinical settings. | Retains structurally intact extracellular matrix (collagen, elastin); placed between implant and tissue. |
| TGF-β Neutralizing Antibodies [3] | To inhibit the primary pro-fibrotic signaling pathway in vitro and in vivo. | Targets a key cytokine driving fibroblast-to-myofibroblast differentiation. |
| α-SMA (Alpha-Smooth Muscle Actin) Antibody [3] | Immunohistochemical marker for identifying activated myofibroblasts in tissue sections. | Critical for quantifying the primary effector cells in capsular contracture. |
| CD68 Antibody [56] | Pan-macrophage marker for visualizing and quantifying macrophage infiltration in the fibrous capsule. | Essential for assessing the innate immune response to the implant. |
| Rho/ROCK Pathway Inhibitors (e.g., Y-27632) [3] | Pharmacologic agents to target Smad-independent fibrotic signaling pathways. | Inhibits fibroblast contractility and activation. |
| 3D Bioprinting / Imprinting Technologies [3] [56] | Fabrication of implants with precise surface topographies (high contact points, low roughness). | Enables creation of biomimetic surfaces designed to promote natural tissue integration. |
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary material-related reasons for the failure of medical implants and drug delivery systems? Material failures are responsible for 36% of medical device failures. The four most common reasons are [58]:
- Improper Materials Selection: The material's properties are unfit for the biological environment, leading to issues like inadequate strength, chemical incompatibility with drugs, or leaching of substances into the body [58].
- In-Service Degradation: The material breaks down in the body faster than anticipated due to factors like enzymatic activity, pH, or mechanical stress [58].
- Reagent or Raw Material Stability: The quality of the raw materials or reagents used is inconsistent or does not meet specifications, affecting the final device's performance [58].
- Manufacturing Process Incompatibility: The manufacturing process (e.g., molding, sterilization) negatively alters the material's properties, causing weaknesses or degradation [58].
FAQ 2: Why is fibrotic encapsulation a major challenge for breast implants and drug-releasing biomaterials? Fibrotic encapsulation is a natural foreign body reaction (FBR). For breast implants, it can lead to capsular contracture, causing pain, hardening, and deformity [29]. For drug delivery systems, the dense, avascular collagenous capsule can act as a physical barrier, impeding the controlled release of therapeutic agents and reducing treatment efficacy [3].
FAQ 3: What key biomaterial properties influence drug release kinetics and longevity? The release of drugs, especially fragile proteins, from a biomaterial is a complex process. Key properties and mechanisms include [59]:
- Degradation Rate: The speed at which the material breaks down controls the release of encapsulated drugs.
- Porosity and Swelling: A material's ability to absorb water and its pore structure affect how quickly drugs diffuse out.
- Material Composition: Both natural (e.g., chitosan, collagen) and synthetic (e.g., PLGA, PEG) polymers offer different advantages and challenges in terms of biocompatibility, tunability, and release profiles [60] [59].
Troubleshooting Guides
Problem: Inconsistent or Burst Release of Therapeutics from Biomaterial Potential Cause & Solution:
- Cause: Inadequate material-protein binding or rapid degradation of the biomaterial matrix [59].
- Solution: Explore stimuli-responsive materials designed for controlled release. Optimize the cross-linking density of hydrogels to better sequester the drug and reduce initial burst release [59].
Problem: Excessive Fibrotic Encapsulation of Implanted Biomaterial Potential Cause & Solution:
- Cause: A cascade of biological events triggered by the foreign body response, including chronic inflammation, macrophage activation, and fibroblast differentiation into collagen-producing myofibroblasts [3].
- Solution:
- Surface Modification: Use textured or nanostructured implant surfaces, which have been shown to reduce capsular contracture compared to smooth surfaces in breast implants [29].
- Pharmacological Intervention: Apply drug-eluting coatings. The glucocorticoid triamcinolone acetonide (TA) has been shown to significantly reduce capsule thickness and collagen density [3].
- Bioactive Coatings: Utilize Acellular Dermal Matrix (ADM), which retains a natural extracellular matrix structure that can modulate the host response and reduce fibrosis [3].
Problem: Premature Degradation or Structural Failure of Biomaterial Potential Cause & Solution:
- Cause: The in-service environment (e.g., enzymatic activity, mechanical load) is harsher than the material was selected for [58].
- Solution: Conduct thorough in vitro and in vivo testing under conditions that mimic the actual physiological environment. Perform failure analysis and life assessments during the design phase to select materials with suitable biostability [58].
Experimental Protocols & Data Presentation
Protocol 1: Assessing In-Vitro Drug Release from a Polymeric Hydrogel This protocol outlines a method to profile the release kinetics of a therapeutic protein from a hydrogel.
- Hydrogel Fabrication: Prepare a PEG-based hydrogel using UV light-initiated crosslinking. Incorporate the model protein (e.g., Bovine Serum Albumin) into the precursor solution before gelation.
- Release Study Setup: Immerse each hydrated hydrogel disk in a sealed vial containing phosphate-buffered saline (PBS) as the release medium. Maintain at 37°C under gentle agitation.
- Sampling and Analysis: At predetermined time points, collect a sample of the release medium and replace it with fresh PBS to maintain sink conditions. Quantify the protein concentration using a spectrophotometer or HPLC.
- Data Modeling: Plot cumulative release over time and fit the data to mathematical models (e.g., Higuchi, Korsmeyer-Peppas) to understand the release mechanism (diffusion or degradation-controlled).
Table 1: Common Biomaterial Platforms for Sustained Drug Release [60] [59]
| Material Platform | Key Characteristics | Common Applications | Key Challenges |
|---|---|---|---|
| Poly(Lactic-co-Glycolic Acid) (PLGA) | Biodegradable, tunable degradation rate, FDA-approved for many uses. | Controlled release microspheres, implants for CNS drug delivery [60]. | Acidic degradation products can affect drug stability; burst release can be an issue. |
| Poly(Ethylene Glycol) (PEG) Hydrogels | Highly hydrophilic, biocompatible, can be functionalized. | Protein delivery, 3D cell culture, tissue engineering [59]. | Poor protein sequestration in traditional hydrogels can lead to burst release. |
| Extracellular Vesicles (EVs) | Natural lipid bilayer, high biocompatibility, low immunogenicity. | Targeted drug delivery for neurodegenerative diseases [60]. | Standardization of isolation, loading efficiency, and scalable production. |
| Solid Lipid Nanoparticles (SLNs) | Improves stability of lipophilic drugs, composed of physiological lipids. | Drug delivery for CNS diseases [60]. | Potential for unpredictable gelation and relatively low drug loading capacity. |
Table 2: Strategies to Mitigate Fibrotic Encapsulation of Implants [3] [29]
| Strategy Category | Specific Example | Mechanism of Action | Evidence of Efficacy |
|---|---|---|---|
| Surface Topography | Nanostructured surfaces | Promotes tissue ingrowth, disrupts continuous collagen capsule, modulates immune response toward anti-inflammatory M2 macrophages [3] [29]. | Shows minimum capsular thickness and reduced myofibroblast infiltration in breast implant studies [29]. |
| Drug-Eluting Coatings | Triamcinolone Acetonide (TA) | Potent glucocorticoid that suppresses local inflammation and fibroblast activity [3]. | Significant reduction in capsule thickness and collagen density around silicone implants in animal models [3]. |
| Bioactive Therapies | Acellular Dermal Matrix (ADM) | Provides a natural ECM scaffold that modulates host response, promoting integration and reducing foreign body reaction [3]. | Used in breast augmentation to lower incidence of capsular contracture [3]. |
| Surgical Optimization | Inframammary fold incision | Reduces bacterial contamination from mammary ducts compared to periareolar incision [29]. | Clinical studies show lower rates of capsular contracture with this surgical approach [29]. |
Signaling Pathways in Fibrosis
The following diagram illustrates the key cellular and molecular pathways driving fibrotic encapsulation, integrating targets for therapeutic intervention.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biomaterial and Anti-Fibrosis Research
| Research Reagent | Function / Rationale |
|---|---|
| PLGA Nanoparticles | A versatile, biodegradable polymer system for creating sustained-release formulations for drugs targeting fibrotic pathways [60]. |
| Triamcinolone Acetonide (TA) | A glucocorticoid used in research coatings to potently suppress the inflammatory phase of the foreign body response and subsequent fibrosis [3]. |
| Tranilast | An anti-allergic and anti-fibrotic drug that can be incorporated into biomaterial coatings to inhibit collagen deposition and fibroblast proliferation [3]. |
| Acellular Dermal Matrix (ADM) | A bioengineered scaffold used to study how a natural extracellular matrix structure can modulate host integration and reduce the fibrotic response [3]. |
| PEG-Based Hydrogels | A tunable, hydrophilic polymer system for creating 3D cell cultures and studying drug release kinetics in a controlled environment [59]. |
| TGF-β Neutralizing Antibodies | Used to experimentally inhibit the primary cytokine driving fibroblast-to-myofibroblast differentiation, confirming its role in the fibrotic cascade [3]. |
| Rho/ROCK Pathway Inhibitors | Small molecule inhibitors (e.g., Y-27632) used to investigate the role of this critical Smad-independent pathway in myofibroblast contractility [3]. |
Preclinical to Clinical Translation: Evaluating Efficacy and Safety of Anti-Fibrotic Strategies
In Vitro and Murine Model Validation of Novel Anti-Fibrotic Compounds
Capsular contracture (CC) remains one of the most prevalent and challenging complications following breast implant surgery, characterized by excessive fibrotic tissue formation around the implant [29]. This pathological foreign body response leads to breast hardening, pain, and deformity, often requiring additional surgical intervention [29] [31]. The underlying mechanism shares common features with organ fibrosis, particularly the activation of myofibroblasts and excessive deposition of extracellular matrix (ECM) components such as collagen type I and III [61] [31]. Despite advancements in implant technology, there is no established gold-standard treatment to prevent fibrotic encapsulation, highlighting the critical need for novel anti-fibrotic strategies [62]. This technical support document provides validated experimental protocols and troubleshooting guidance for researchers developing and testing new anti-fibrotic compounds aimed at preventing this debilitating complication.
FAQs: Experimental Design and Compound Selection
Q1: What are the key considerations when selecting in vitro models for initial anti-fibrotic compound screening?
Primary human dermal fibroblasts (HDFs) and cardiac fibroblasts (HCFs) serve as excellent primary cell models for initial screening [61] [63]. When establishing your assay, focus on quantifying expression of collagen type I alpha 1 (COL1A) and collagen type III alpha 1 (COL3A) as primary endpoints, as these are clinically relevant markers of fibrotic activity [61]. Ensure your assay includes appropriate fibroblast activation stimuli, such as TGF-β, to mimic the profibrotic environment [64]. For breast implant-specific research, consider that implant surface characteristics significantly influence fibroblast response, with smooth surfaces triggering stronger myofibroblast activation compared to textured alternatives [29].
Q2: How do I determine the optimal dosing regimen for in vivo validation studies?
The timing of therapeutic interventions is crucial for accurate efficacy assessment. In bleomycin-induced models, avoid the initial acute inflammatory phase (first 7 days) and focus on the fibrotic phase [65]. Research demonstrates that treatment windows from day 7-28 or day 14-28 are optimal for assessing anti-fibrotic effects rather than earlier timepoints [65]. For compound screening, include nintedanib (60 mg/kg orally, once daily) or pirfenidone as reference controls to benchmark your compound's performance against clinically approved agents [65].
Q3: What are the most relevant endpoints for assessing anti-fibrotic efficacy in murine models?
Beyond standard histology, incorporate multiple quantitative endpoints: measure the expression of fibrotic markers (α-SMA, collagen I, fibronectin) via RT-qPCR and immunofluorescence [66] [64]. Utilize micro-CT imaging to derive morphological biomarkers of fibrosis, including mean lung attenuation and aeration compartments [65]. For breast implant research, assess both collagen density and organization, as second-harmonic generation imaging can reveal favorable collagen organization indicative of more compliant capsules [62].
Q4: How can I mitigate graft-versus-host disease (GvHD) in humanized mouse models?
The hematopoietic stem cell (HSC)-humanized model demonstrates stable multilineage engraftment without GvHD development, unlike PBMC-humanized models which develop GvHD approximately 5 weeks post-reconstitution [67]. For long-term studies, prioritize the HSC-humanized model established by engrafting immunodeficient mice with human CD34+ cells from umbilical cord blood [67].
Troubleshooting Guides
Poor In Vitro Potency
| Problem | Possible Causes | Solutions |
|---|---|---|
| Lack of anti-fibrotic activity in primary human fibroblasts | • Insufficient compound solubility• Inadequate cellular uptake• Off-target mechanism | • Perform structure-activity relationship (SAR) studies with targeted modifications to core scaffold [64]• Test chemical similars of lead compounds (e.g., lycorine similars) for improved efficacy [63]• Implement controlled-release delivery systems like electrospun fibers [62] |
| High cytotoxicity at effective concentrations | • Non-specific cellular toxicity• Narrow therapeutic window | • Evaluate cytotoxicity on human iPS-derived cardiomyocytes [63]• Determine EC5 and EC95 values using multiplex toxicity assays [63]• Explore combination therapies with synergistic agents (e.g., omega-3 + montelukast) [62] |
| Inconsistent results across fibroblast donors | • Donor-specific biological variability• Differences in passage number | • Use fibroblasts from multiple donors and pool results [63]• Standardize passage numbers (recommended: passages 3-7)• Include internal controls in each experiment |
Murine Model Challenges
| Problem | Possible Causes | Solutions |
|---|---|---|
| Spontaneous fibrosis resolution in BLM model | • Single bleomycin administration• Evaluation at incorrect timepoints | • Utilize triple bleomycin administration protocol (days 0, 2, 4) to establish longer-lasting fibrosis [65]• Conduct terminal endpoint at day 28 instead of day 21 [65] |
| Failure to translate in vitro results to in vivo efficacy | • Species-specific differences in drug metabolism• Inadequate human immune component | • Employ humanized mouse models with HSC engraftment [67]• Verify compound stability and metabolism in mouse serum• Use micro-CT to identify optimal treatment window [65] |
| Excessive mortality in BLM model | • Bleomycin dose too high• Infection from immunosuppression | • Administer bleomycin via oropharyngeal aspiration (50 μL volume) [67] [65]• Provide acidified water (pH 2.5-3.0) to inhibit Pseudomonas infection [67] |
Quantitative Data from Recent Anti-Fibrotic Studies
Table 1: Efficacy Data of Novel Anti-Fibrotic Compounds in Preclinical Models
| Compound | Model System | Key Efficacy Findings | Reference |
|---|---|---|---|
| Ellagic acid, Gallic acid, Syringic acid (from Rosa roxburghii) | In vitro: fibroblast cultures; In vivo: BLM-induced pulmonary fibrosis in mice | • Inhibited fibroblast migration• Attenuated intracellular ROS overproduction• Downregulated α-SMA and collagen I expression• Superior efficacy in ethyl acetate fraction | [66] |
| Deramiocel (CDC therapy) | In vitro: human dermal fibroblasts; In vivo: DMD patients (HOPE-2 trial) | • Conditioned media suppressed COL1A and COL3A expression• Dose-dependent anti-fibrotic activity• 71% slowing of skeletal muscle decline (PUL score)• 107% slowing of cardiac disease progression (LVEF) | [61] |
| Pirfenidone derivative 10b | In vitro: LL29 and DHLF cells; In vivo: BLM-induced pulmonary fibrosis in mice | • Robust suppression of fibrotic markers (FN1, α-SMA, collagen1α1) at 50-100 μM• Mitigated alveolar wall thickening and collagen deposition• Significantly restored lung function• Modulated SMAD3/SMAD7 signaling pathway | [64] |
| PCL-ω3-MTKS fibers | In vitro: drug release studies; In vivo: rat mini-implant model | • Controlled and prolonged release profile (90 days)• Significant reduction in fibrotic capsule thickness• Improved collagen organization• Synergistic efficacy of omega-3 and montelukast | [62] |
| Lycorine similar (lyco-s) | In vitro: human cardiac fibroblasts; ex vivo: human myocardial slices | • Inhibited HCF proliferation at concentrations 100-fold lower than lycorine• Nearly complete shutdown of ECM production• Low cytotoxicity on human iPS-derived cardiomyocytes• Strong anti-fibrotic gene regulation | [63] |
Table 2: Experimental Parameters for Anti-Fibrotic Compound Validation
| Parameter | Optimal Conditions | Validation Methods |
|---|---|---|
| In vitro dosing | 24-72 hour treatment; dose range 1-100 μM | • BrdU incorporation assay [63]• WST-1 cell proliferation assay [63]• Caspase activation and LDH release for toxicity [63] |
| In vivo dosing | • BLM model: treatment days 7-28 or 14-28 [65]• Nintedanib control: 60 mg/kg orally, once daily [65] | • Micro-CT imaging at days 0, 7, 14, 21, 28 [65]• Histopathology (Masson's trichrome, H&E) [67]• BALF cell analysis [65] |
| Fibrosis assessment | • Gene expression: COL1A1, COL3A1, α-SMA, FN1 [61] [64]• Protein level: immunofluorescence, Western blot [64] [68]• Histology: collagen deposition, capsule thickness [62] | • RT-qPCR for fibrotic markers [64]• Immunofluorescence for α-SMA, collagen I [66]• Second-harmonic generation imaging for collagen organization [62] |
| Humanized model engraftment | • HSC-humanized: 3×10ⴠCD34+ cells via intrahepatic injection [67]• PBMC-humanized: 1×10ⷠPBMCs via tail vein injection [67] | • FACS analysis of human immune cell populations [67]• Assessment of multilineage engraftment (T cells, B cells) [67] |
Experimental Protocols
In Vitro Potency Assay for Anti-Fibrotic Activity
This protocol adapts the validated approach used to evaluate Deramiocel's anti-fibrotic activity [61]:
Cell Culture: Maintain primary human dermal fibroblasts (HDFs) in fibroblast growth medium (FGM-3) containing 1 ng/mL bFGF, 5 μg/mL insulin, 1% penicillin-streptomycin, and 10% FBS in fibroblast basal medium [63]. Use cells between passages 3-7 for consistency.
Compound Treatment: Seed 96-well plates with 7,500 HDFs/well in 0.1% gelatin-coated plates. After 24 hours, replace medium with serial dilutions of test compounds in FGM-3 containing 1.6% DMSO and 1% BrdU.
Proliferation Assessment: After 24-hour incubation, wash cells twice with DPBS and incubate with anti-BrdU:POD antibody for 60 minutes at room temperature. Measure absorbance at 370nm with reference at 490nm.
Viability Validation: In parallel plates, treat cells with compound dilutions for 24 hours, then replace medium with 10% WST-1 in FGM-3. Incubate for 60 minutes at 37°C in the dark and measure absorbance at 450nm with reference at 630nm.
Quality Control: Calculate Z' factor (≥0.5) and signal window (≥2) for assay validation. Categorize compounds as "active" if n≥3 repetitions and EC50<10μM in both assays [63].
Bleomycin-Induced Lung Fibrosis Model for Anti-Fibrotic Compound Validation
This protocol utilizes the longer-lasting triple bleomycin administration model optimized for anti-fibrotic drug discovery [65]:
Animal Preparation: Use 7-8 week old male C57Bl/6 mice. Acclimatize for 7-10 days upon arrival with standard housing conditions (room temperature 20-24°C, relative humidity 40-70%, 12h light-dark cycle).
Fibrosis Induction: Anesthetize mice with 2.5% isoflurane. Administer bleomycin hydrochloride (diluted in 50μL saline) via oropharyngeal aspiration on days 0, 2, and 4. Control animals receive saline only.
Compound Administration: Randomize bleomycin-treated mice into experimental groups. Begin compound administration on day 7 or day 14, continuing through day 28. Administer reference control nintedanib at 60 mg/kg orally once daily.
Micro-CT Imaging: At days 0, 7, 14, 21, and 28, anesthetize mice with 2% isoflurane and scan thoraxes using micro-CT with the following parameters: X-ray tube current 88μA, voltage 90kV, total angle 360°, scan length 4 minutes. Reconstruct images with 50μm isotropic voxel size.
Endpoint Analysis: On day 28, collect bronchoalveolar lavage fluid (BALF) for cell count analysis. Harvest lungs for histology (Masson's trichrome staining) and molecular analysis (RNA and protein extraction for fibrotic marker expression).
Humanized Mouse Model of Pulmonary Fibrosis
This protocol establishes a clinically relevant platform for evaluating human-targeted therapies [67]:
HSC-Humanized Mouse Generation:
- Obtain 4-day-old NOD.Cg-PrkdcscidIL2γgtm1 Sug/JicKoat (NOG) mouse pups.
- Irradiate pups with appropriate dose for immune suppression.
- Isolate CD34+ cells from human umbilical cord blood by Ficoll-Paque density gradient centrifugation and magnetic bead separation.
- Resuspend HSCs in 50μL PBS and administer 3×10ⴠCD34+ cells per mouse via intrahepatic injection.
Engraftment Validation:
- After 12-16 weeks, collect peripheral blood and analyze by FACS for human immune cell populations.
- Confirm multilineage engraftment (T cells: ~20%, B cells: ~57%) before proceeding with fibrosis induction.
Fibrosis Induction and Compound Testing:
- Administer bleomycin via oropharyngeal aspiration to humanized mice.
- Begin compound treatment on day 7, continue to day 21.
- Include nintedanib control (40 mg/kg, once daily by oral gavage).
Signaling Pathways and Experimental Workflows
Anti-Fibrotic Compound Screening Workflow
Diagram 1: Anti-Fibrotic Compound Screening Workflow. This workflow outlines the sequential process for identifying and validating novel anti-fibrotic compounds, with feedback loops for optimizing compounds with poor activity or high toxicity. SAR: Structure-Activity Relationship; hiPS-CM: human induced pluripotent stem cell-derived cardiomyocytes; BLM: bleomycin; HSC: hematopoietic stem cell.
Key Anti-Fibrotic Signaling Pathways
Diagram 2: Key Anti-Fibrotic Signaling Pathways and Intervention Points. This diagram illustrates major profibrotic signaling pathways and the mechanisms by which various anti-fibrotic compounds inhibit these pathways. Compounds highlighted in green represent intervention points for novel anti-fibrotic agents.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Anti-Fibrotic Studies
| Reagent/Cell Line | Specific Function | Application Notes |
|---|---|---|
| Primary Human Dermal Fibroblasts (HDFs) | Principal effector cells for fibrosis; produce ECM components | • Obtain from multiple donors (Promocell #C-12375)• Culture in FGM-3 medium with bFGF and insulin [63]• Use passages 3-7 for consistency |
| Primary Human Cardiac Fibroblasts (HCFs) | Heart-specific fibroblasts for cardiac fibrosis research | • Multiple donors recommended• Assess collagen I/III expression as primary endpoint [61]• Test in ex vivo living myocardial slices [63] |
| Bleomycin Hydrochloride | Induces pulmonary fibrosis in murine models | • Administer via oropharyngeal aspiration (50μL volume) [65]• Triple administration (days 0, 2, 4) for longer-lasting fibrosis [65]• Dose range: 1.5-2.0 U/kg per administration |
| Nintedanib (Reference Control) | Tyrosine kinase inhibitor; approved anti-fibrotic agent | • Use 60 mg/kg orally, once daily for in vivo studies [65]• Benchmark for compound efficacy• Prepare fresh in appropriate vehicle for each administration |
| Pirfenidone (Reference Control) | Anti-fibrotic agent; modulates TGF-β signaling | • Use 500 μM as in vitro reference [64]• Benchmark for novel pirfenidone derivatives [64] |
| CD34+ Hematopoietic Stem Cells | Generation of humanized mouse models | • Isolate from umbilical cord blood [67]• Inject 3×10ⴠcells via intrahepatic route [67]• Validate engraftment after 12-16 weeks by FACS |
| Anti-Collagen I/III Antibodies | Detection of key ECM components in fibrosis | • Use for immunofluorescence and Western blot [66] [61]• Quantify expression changes post-treatment |
| Anti-α-SMA Antibody | Marker for activated myofibroblasts | • Key indicator of myofibroblast differentiation [66] [64]• Use for immunofluorescence quantification |
| TGF-β1 | Potent activator of fibroblast-to-myofibroblast differentiation | • Use at 2-5 ng/mL to stimulate fibroblast activation [64]• Essential for in vitro fibrosis models |
| Masson's Trichrome Stain | Histological detection of collagen deposition | • Standard for fibrosis assessment in tissue sections [67] [68]• Quantify blue-stained collagen areas |
Fibrotic encapsulation is a complex biological process and a common host response to any implanted medical device, including breast implants. This natural healing reaction can lead to the development of a dense collagenous capsule around the implant [3]. In a significant subset of patients, this process can progress to capsular contracture, a pathological hardening and tightening of the capsule that results in breast firmness, pain, and aesthetic deformity [69] [44]. This condition remains one of the most frequent and challenging complications in both aesthetic and reconstructive breast surgery, often necessitating reoperation [69].
The foreign body reaction (FBR) that drives fibrous capsule formation is a multi-stage process involving: (i) blood-biomaterial interaction and provisional matrix formation, (ii) acute inflammation, (iii) chronic inflammation, (iv) formation of foreign body giant cells (FBGCs), and (v) fibrous capsule maturation [3]. Key cellular players include neutrophils, macrophages, fibroblasts, and T-cells, with critical molecular mediators including TGF-β, IL-17, matrix metalloproteinases (MMPs), and tissue inhibitors of metalloproteinases (TIMPs) [3]. The interplay between these cells and signaling pathways ultimately drives fibroblast differentiation into myofibroblasts, which deposit a dense, avascular collagen network that characterizes the mature fibrous capsule [3].
Implant surface topography—specifically, the choice between textured and smooth surfaces—has been extensively investigated as a critical modifiable factor in mitigating the FBR and subsequent capsular contracture. This meta-analysis synthesizes clinical evidence and explores the underlying biological mechanisms through which surface texture influences fibrotic outcomes.
Summarized Clinical Outcome Data
Table 1: Comparative Clinical Outcomes of Smooth vs. Textured Implants
| Complication Type | Smooth Implants | Textured Implants | Notes & Context |
|---|---|---|---|
| Capsular Contracture (Overall) | Up to 51.7% [69]; 2.4%-18.9% (Primary Augmentation) [44] | Reported rates vary widely; some studies show lower rates [70] | A widely cited meta-analysis reported no significant difference in rates for subpectoral placement [70]. Lista et al. (2020) reported similar rates in the subglandular plane (1.6% smooth vs. 3.3% textured) [70]. |
| Capsular Contracture (10-Year Core Study) | 18.9% (Augmentation) [70] | No significant difference from smooth [70] | Large 2014 manufacturer (Allergan) core study found no statistically significant difference between textured and smooth devices [70]. |
| Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) | Risk is effectively zero; no published cases in patients with only smooth implants [70] | Causative link established; finite risk, with some estimates at ~3/1000 [70] | The risk difference is categorical, not relative. Textured implants are considered causative for BIA-ALCL [70]. The disease carries a ~5% risk of mortality [70]. |
| Implant Malrotation | Minimal risk [70] | Risk of rotation exists, particularly for anatomical shaped devices [70] | This is a specific complication related to the stability of anatomical implants, which require texture to maintain position. |
| Other Complications (Rippling, Malposition, Double Capsules) | Textured implants (specifically Allergan Biocell) associated with higher rates of malposition, malrotation, seroma, rippling, rupture, pain, and double capsules [70] |
Biological Mechanisms of Topographical Influence
The surface topography of an implant is a primary determinant of the host immune response. Textured surfaces, characterized by their specific surface area and architecture, are designed to modulate the FBR.
Tissue Integration and Inflammatory Response
Textured implants promote tissue ingrowth into the surface pores, which disrupts the formation of a continuous, aligned collagenous capsule. This ingrowth anchors the implant, potentially reducing micromovement, and creates a more disorganized, less contractile capsule architecture [3]. In contrast, smooth implants often develop a denser, more aligned capsule with a higher likelihood of contraction.
The cellular response also differs. Compared to smooth-surface implants, textured implants may release particulate debris that undergoes macrophage phagocytosis. This process can paradoxically trigger both pro-inflammatory and pro-healing cytokine expression, influencing the subsequent fibrotic pathway [3]. The polarization of macrophages—the primary arbiters of the FBR—is critical. A shift from pro-inflammatory M1 macrophages to pro-healing M2 phenotypes is essential for natural wound healing; the presence of an implant can delay this transition, sustaining inflammation [3].
Signaling Pathways in Fibrosis
The key signaling pathway driving fibrosis, regardless of implant texture, is the TGF-β (Transforming Growth Factor-Beta) pathway. Activated macrophages and fibroblasts release TGF-β, which synergistically activates both Smad-dependent and Smad-independent (including Rho/ROCK) pathways in fibroblasts [3]. This activation drives fibroblast differentiation into myofibroblasts, which are characterized by the expression of α-smooth muscle actin (α-SMA) and are responsible for the excessive secretion and contraction of collagen, primarily types III and I [3]. The Rho/ROCK pathway is particularly involved in enhancing cellular contractility, especially when adhesion to the material surface is unstable [3].
Diagram: Key Signaling Pathways in Fibrous Capsule Formation
Detailed Experimental Protocols
Protocol: Subcutaneous Implant Rodent Model for Fibrosis Assessment
This model is the gold standard for preliminary assessment of implant biocompatibility and the FBR [71].
- Material Preparation: Sterilize implant samples (e.g., smooth silicone, textured silicone) via UV radiation (30 min per side) or autoclaving.
- Animal Surgery: Anesthetize rodents (e.g., C57BL/6 mice) and shave the dorsal area. Make a ~1 cm midline incision.
- Implant Placement: Create subcutaneous pockets by blunt dissection on each side of the incision. Insert one test material per pocket (e.g., smooth on one side, textured on the other for within-animal control).
- Closure: Close the incision with surgical sutures or clips.
- Endpoint Analysis: Euthanize animals at predetermined time points (e.g., 2, 4, and 12 weeks).
- Histology: Excise the implant with the surrounding tissue, fix in formalin, and process for paraffin sectioning. Stain with:
- H&E: For general capsule morphology and cellularity.
- Masson's Trichrome or Picrosirius Red: For visualization and quantification of collagen deposition and capsule thickness.
- Immunohistochemistry (IHC): For specific cell types (e.g., CD68 for macrophages, α-SMA for myofibroblasts) and signaling molecules (e.g., TGF-β).
- Gene Expression Analysis: Isolve RNA from peri-implant tissue and perform qRT-PCR for fibrotic markers (e.g.,
Acta2(α-SMA),Col1a1,Col3a1,Tgfb1,Mmp9,Timp1).
- Histology: Excise the implant with the surrounding tissue, fix in formalin, and process for paraffin sectioning. Stain with:
Protocol: In Vitro Macrophage-Implant Surface Interaction Assay
This assay evaluates the direct inflammatory response of immune cells to different implant surfaces.
- Surface Preparation: Place sterile implant material samples (e.g., 1 cm² discs of smooth and textured silicone) in the wells of a culture plate.
- Cell Seeding: Differentiate human monocytic cell line (THP-1) into macrophages using Phorbol 12-myristate 13-acetate (PMA). Seed the resulting macrophages onto the material samples at a defined density.
- Culture and Stimulation: Culture cells for 24-72 hours. Optionally, stimulate with a known inflammatory trigger like LPS.
- Analysis:
- Cytokine Profiling: Collect cell culture supernatant and analyze using ELISA or a multiplex immunoassay for pro-inflammatory (e.g., IL-1β, TNF-α, IL-6) and pro-fibrotic (e.g., TGF-β) cytokines.
- Cell Morphology and Adhesion: Fix and stain cells on the material surface (e.g., Phalloidin for F-actin, DAPI for nuclei) and image using fluorescence or confocal microscopy to assess cell adhesion, spreading, and FBGC formation.
- Gene Expression: Lyse cells directly on the material and perform qRT-PCR for polarization markers (e.g.,
CD86for M1,CD206for M2).
Diagram: Experimental Workflow for Implant Biocompatibility
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Investigating the FBR
| Reagent / Material | Function / Application | Specific Examples & Notes |
|---|---|---|
| Implant Material Samples | The primary test substrate for in vitro and in vivo experiments. | Medical-grade smooth and textured silicone sheets or mini-implants; Polyurethane-coated implants [44]. |
| Cell Culture Models | In vitro assessment of immune cell response. | THP-1 human monocyte line (differentiated with PMA into macrophages); Primary human peripheral blood mononuclear cells (PBMCs) or isolated monocytes. |
| Cytokine Detection Kits | Quantification of soluble inflammatory and fibrotic mediators. | ELISA or Multiplex Arrays for TGF-β, IL-1β, TNF-α, IL-6, IL-10. Critical for profiling macrophage polarization [3]. |
| Histology Stains & Antibodies | Visualization and quantification of capsule structure and cellular components. | H&E (general morphology); Masson's Trichrome (collagen); IHC Antibodies for α-SMA (myofibroblasts), CD68 (macrophages), CD3 (T-cells) [3]. |
| qRT-PCR Reagents | Measurement of gene expression related to fibrosis and inflammation. | Primers/Probes for ACTA2 (α-SMA), COL1A1, COL3A1, TGFB1, MMP9, TIMP1, IL17A [3]. |
| Animal Models | Preclinical in vivo assessment of the FBR and capsular contracture. | Mouse or Rat Subcutaneous Implant Model [71]. The UTJ (Utero-Tubal Junction) in non-human primates represents an immune-privileged site for comparative studies [71]. |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: The clinical data on capsular contracture rates for textured vs. smooth implants seems conflicting. What is the key takeaway for a researcher?
A1: You are correct that the data is heterogeneous. The key is to recognize that the surgical plane of placement is a critical confounding variable. Early studies demonstrating a benefit for texture often used subglandular placement. More recent, high-level evidence, including a widely cited meta-analysis, shows that when implants are placed in the subpectoral plane (now preferred by many surgeons), the significant difference in capsular contracture rates between smooth and textured devices disappears [70]. Furthermore, recent large core studies with 10-year follow-up have found no significant difference in capsular contracture rates [70]. Your experimental design should account for this variable if using an in vivo model.
Q2: From a biological mechanism standpoint, why wouldn't textured implants conclusively prevent fibrosis?
A2: While texture promotes tissue ingrowth and disrupts the organized collagen capsule, it also presents a larger surface area and can release particulate debris through abrasion. This debris can undergo phagocytosis by macrophages, triggering a chronic, low-grade inflammatory response and the release of pro-fibrotic cytokines like TGF-β, which can paradoxically drive the fibrotic process [3]. The net effect on capsule formation is a balance between the anti-fibrotic effect of tissue integration and the pro-fibrotic effect of the sustained foreign body response.
Q3: What are the most reliable endpoints for quantifying capsular contracture in a pre-clinical rodent model?
A3: The most translational endpoints are histomorphometric:
- Capsule Thickness: Measure at multiple standardized points around the implant on Masson's Trichrome-stained sections.
- Cellularity: Quantify the density of nuclei within the capsule.
- Collagen Density: Can be quantified from Trichrome or Picrosirius Red-stained sections using polarized light or image analysis software.
- Myofibroblast Presence: Score the intensity and distribution of α-SMA staining via IHC. Supplement these with molecular analyses like qRT-PCR for fibrotic genes from the peri-implant tissue.
Q4: Our in vitro data shows a strong pro-inflammatory response to a textured surface. Does this mean it will perform worse in vivo?
A4: Not necessarily. An initial robust inflammatory response is part of the normal healing process. The critical factor is how the response resolves. A material that promotes a transition from a pro-inflammatory (M1) to a pro-healing/remodeling (M2) macrophage phenotype may still lead to a favorable outcome in vivo, despite a strong initial in vitro reaction [3]. Therefore, in vitro models should aim to assess macrophage polarization over time, not just initial cytokine release.
Q5: Beyond surface texture, what are other promising research directions for preventing fibrotic encapsulation?
A5: The field is exploring several innovative strategies, including:
- Surface Modifications: Creating "anti-fouling" surfaces that minimize protein adsorption, or coatings with bioactive molecules (e.g., TGF-β inhibitors) [3].
- Pharmacological Interventions: Local drug delivery from the implant surface using coatings eluting anti-fibrotic agents (e.g., Tranilast) or immunomodulators [3].
- Bioactive Coatings: Using Acellular Dermal Matrix (ADM) or other decellularized matrices to create a more natural tissue-implant interface [3].
- Microenvironment Studies: Investigating immune-privileged sites (e.g., the uterine cavity) to identify endogenous factors that dampen the FBR [71].
Frequently Asked Questions (FAQs)
FAQ 1: What is the clinical and histological evidence linking the Baker and Wilflingseder classification systems? A 2007 comparative study demonstrated a statistically significant positive correlation (p < 0.05) between the clinical Baker score and the histological Wilflingseder score [72]. The study found that increasing Baker grade was associated with greater capsular thickness and more severe inflammatory reactions within the capsule, characterized by a higher number of silicone particles and silicone-loaded macrophages [72]. This provides a direct histopathological link between what is observed clinically and the underlying tissue changes.
FAQ 2: How has the Wilflingseder classification evolved to incorporate modern molecular findings? The original Wilflingseder classification has been modified to include contemporary immunohistochemical and histological understandings [73]. The updated parameters assess [72] [73]:
- Capsule thickness and cell layers
- Thickness of the inner synovial metaplasia
- Collagen structure and fiber organization
- Presence and quantity of histiocytes
- Infiltration of inflammatory cells (lymphocytes, plasma cells, granulocytes) This modification allows for a more objective classification of histological changes that reflect current knowledge in capsular contracture development.
FAQ 3: What molecular mechanisms drive the progression of fibrotic encapsulation? Fibrotic encapsulation is a staged foreign body response (FBR). Key mechanisms include [3]:
- Protein Adsorption: Plasma proteins (albumin, fibrinogen) immediately adsorb to the implant surface.
- Acute Inflammation: Neutrophils are recruited and secrete pro-inflammatory cysteinyl leukotrienes (CysLTs).
- Chronic Inflammation & FBGC Formation: Macrophages polarize into pro-inflammatory M1 phenotypes, secreting cytokines like IL-1. Persistent frustration leads to foreign body giant cell (FBGC) formation.
- Fibrotic Cascade: Activated macrophages and T-cells (e.g., Th17) release TGF-β and IL-17. This, in concert with mechanical signaling via the Rho/ROCK pathway, drives fibroblast-to-myofibroblast differentiation. Myofibroblasts then deposit dense collagen (primarily type I and III), forming the avascular, fibrous capsule [3].
FAQ 4: What is the role of bacterial biofilm in capsular contracture, and how is it detected? Biofilms are considered a significant contributor to capsular contracture by provoking a chronic, low-grade inflammatory response [13]. However, evidence suggests they are not the sole cause [74]. Advanced detection methodologies include [74]:
- Specialized Cultures: Using anaerobic and aerobic culture conditions.
- Molecular Techniques: Real-time PCR (rtPCR) and 16S rRNA gene sequencing to identify bacterial DNA.
- Microscopy: Scanning Electron Microscopy (SEM) and live:dead staining combined with fluorescent microscopy to visualize biofilm morphology and viability.
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent Correlation Between Clinical Grade and Histological Findings
- Problem: A patient has a high Baker grade (III-IV) but the histological analysis shows only mild fibrosis, or vice versa.
- Solution:
- Standardize Sampling: Ensure capsular tissue biopsies are taken from the area where the capsule is thickest, as capsule thickness is heterogeneous [75]. Take multiple measurements and record the average.
- Expand Histological Analysis: Do not rely on a single parameter. Use the modified Wilflingseder classification, which includes multiple factors like synovial metaplasia, inflammatory cell infiltration, and collagen structure, providing a more comprehensive assessment [73].
- Check for Subclinical Infection: Employ biofilm detection protocols (e.g., PCR, SEM) to identify a potential infectious cause that may not be evident from standard H&E staining [74].
Challenge 2: Low Yield or Contamination in Biofilm Analysis
- Problem: Cultures are consistently negative, or molecular analysis reveals only contaminating bacteria (e.g., Micrococcineae from skin flora) [74].
- Solution:
- Aseptic Explantation: Use a no-touch technique during explantation and immediately place specimens in anaerobic transport packs to preserve fastidious bacteria [74].
- Multi-Modal Detection: Do not rely on culture alone. Combine culture with rtPCR and SEM to increase sensitivity. Culture-negative samples may still show positive signals with molecular or microscopic methods [74].
- Incorporate Controls: Include a known positive control (e.g., a sample from a frank Grade IV contracture) to validate your biofilm detection workflow [74].
Challenge 3: Poor Quality of Capsular Tissue for Histology and Molecular Analysis
- Problem: Tissue sections are torn, stained poorly, or yield low-quality RNA/DNA.
- Solution:
- Proper Fixation: Ensure prompt and adequate fixation of tissue specimens to prevent autolysis and preserve morphology [76].
- Optimal Processing: Follow a standardized tissue processing workflow to avoid artifacts like under-processing (causing soft tissue) or over-processing (causing brittle tissue) [76].
- Dedicated Storage: For molecular analysis, immediately preserve a portion of the sample in a specialized reagent like RNAlater to stabilize RNA and DNA for subsequent PCR analysis [74].
Quantitative Data Tables
| Baker Grade | Clinical Presentation | Mean Capsular Thickness Trend | Key Histological Features (Wilflingseder) |
|---|---|---|---|
| I | Breast is soft and natural | Thinnest | Minimal inflammation, organized collagen, few histiocytes. |
| II | Breast slightly firm but looks normal | Increased | Mild synovial metaplasia, presence of histiocytes and some inflammatory cells. |
| III | Breast is firm and appears abnormal | Moderately Thick | Moderate to severe inflammation, synovial metaplasia, higher density of silicone particles and macrophages. |
| IV | Breast is hard, painful, and abnormal | Thickest | Dense hyaline fibrosis, significant silicone deposition, foreign body granulomas, calcification possible. |
Note: A 2007 study confirmed a positive correlation (p<0.05) between Baker grade and the histological Wilflingseder score. Capsular thickness also positively correlates with implantation time and patient age at implantation [72] [75].
| Parameter | Score 0 | Score 1 | Score 2 | Score 3 |
|---|---|---|---|---|
| Capsule Thickness | <0.1 mm | 0.1 - 0.5 mm | 0.5 - 1.0 mm | >1.0 mm |
| Synovial Metaplasia | Absent | Thin, 1-3 cell layers | Moderate, 4-10 cell layers | Thick, >10 cell layers |
| Inflammatory Cell Infiltrate | None | Mild (Scattered cells) | Moderate (Focal aggregates) | Severe (Dense, band-like) |
| Collagen Architecture | Loose, parallel fibers | Moderately organized | Dense, bundled | Very dense, hyalinized |
| Histiocytes / FBGCs | None | Occasional | Numerous | Sheets / Dense clusters |
Experimental Protocols
Protocol 1: Comprehensive Histomorphological Analysis of Capsular Tissue
Objective: To prepare and evaluate breast implant capsules using the modified Wilflingseder classification.
Materials:
- Capsular tissue biopsy
- 10% Neutral Buffered Formalin
- Automated tissue processor
- Paraffin embedding station
- Microtome
- Slides and coverslips
- Hematoxylin and Eosin (H&E) stain
- Special stains (e.g., Masson's Trichrome for collagen)
Methodology:
- Grossing: Immediately after explantation, biopsy a ~2.5 cm² section of the capsule from the thickest area [74] [75]. Record the location.
- Fixation: Immerse tissue in sufficient 10% Neutral Buffered Formalin for 24-48 hours to ensure complete penetration and prevent autolysis [76].
- Processing: Dehydrate the tissue through a graded series of alcohols, clear with xylene, and infiltrate with paraffin wax using an automated processor [76].
- Embedding and Sectioning: Orient the tissue in a paraffin block and section at 4-5 μm thickness using a microtome. Float sections on a water bath and mount on glass slides [76].
- Staining: Perform routine H&E staining. Employ special stains as needed (e.g., Masson's Trichrome to differentiate collagen morphology).
- Analysis: Examine slides under light microscopy by two independent, blinded investigators. Score each parameter from Table 2 to generate a composite Wilflingseder score. Correlate this score with the pre-operative Baker grade [72] [73].
Protocol 2: Multi-Modal Biofilm Detection on Explanted Prostheses
Objective: To detect and characterize bacterial biofilm on explanted breast implants and adjacent tissues.
Materials:
- Explanted prosthesis, capsule, and ADM samples
- Anaerobic and aerobic bacterial transport packs
- RNAlater solution
- Sheep's blood agar, chocolate agar, pre-reduced Brucella blood agar plates
- PCR reagents and equipment, 16S rRNA primers
- Scanning Electron Microscope (SEM)
- Live/Dead BacLight Bacterial Viability Kit
Methodology:
- Specimen Collection: Aseptically collect matched biopsies from the implant surface, capsule, and ADM (if present). Divide each sample for different analyses [74].
- Microbiological Culture:
- Vortex the implant in saline or mince the tissue.
- Plate the resulting material on the various agar plates.
- Incubate aerobically (5% COâ‚‚) for 3 days and anaerobically for 5 days [74].
- Molecular Detection (qPCR/16s rRNA sequencing):
- Place a tissue piece in RNAlater.
- Extract total DNA.
- Perform real-time quantitative PCR (qPCR) with pan-bacterial 16S rRNA primers.
- For positive samples, perform 16S rRNA gene sequencing (e.g., targeting V1-V2 regions) to classify bacterial taxonomy [74].
- Microscopic Evaluation:
- Live/Dead Staining: Apply cell permeable and impermeable fluorescent dyes to fresh, unfixed tissue to visualize viable bacteria under a fluorescent microscope [74].
- SEM: Fix a sample in glutaraldehyde, dehydrate, critical-point dry, and sputter-coat with gold. Image to visualize biofilm ultrastructure [74].
Signaling Pathways and Experimental Workflows
Diagram 1: Core Fibrotic Encapsulation Signaling Pathway
Core pathway from foreign body response to fibrosis.
Diagram 2: Integrated Analysis Workflow
Integrated workflow for histopathological correlation study.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Capsular Contracture Research
| Reagent / Material | Function in Research | Specific Example / Note |
|---|---|---|
| RNAlater | Stabilizes and protects RNA/DNA in tissue samples for subsequent molecular studies. | Critical for preserving genetic material for qPCR and 16S rRNA sequencing from capsular biopsies [74]. |
| 16S rRNA Primers | Allows amplification of bacterial DNA for identification and taxonomic classification. | Used to detect subclinical infection and biofilm-forming bacteria; targets conserved bacterial genes [74]. |
| Anti-α-SMA Antibody | Marker for immunohistochemical identification of myofibroblasts. | Key indicator of active fibrosis in capsular tissue; cells positive for α-SMA are contractile [3]. |
| Live/Dead BacLight Stain | Fluorescent viability assay to distinguish live vs. dead bacteria in a biofilm. | Uses membrane-permeant (green) and -impermeant (red) dyes; visualized with fluorescence microscopy [74]. |
| Acellular Dermal Matrix (ADM) | Biological scaffold used in revision surgery and as a research model. | Studied to understand its ability to modulate the host response and reduce capsular contracture compared to capsule [74]. |
| Masson's Trichrome Stain | Histological stain that differentially colors collagen fibers blue and muscle fibers red. | Essential for evaluating collagen architecture, density, and organization in capsular tissue [76]. |
For researchers focused on preventing fibrotic encapsulation of breast implants, a deep understanding of the regulatory landscape is not merely administrative—it is scientifically crucial. The U.S. Food and Drug Administration's (FDA) post-market surveillance data and labeling requirements constitute a rich, often underutilized, repository of real-world evidence on implant performance and complications. This technical support center is designed to bridge the gap between regulatory science and laboratory research, providing troubleshooting guides, standardized protocols, and analytical frameworks to help researchers leverage these resources effectively. By framing your fundamental research on fibrotic encapsulation within this structured regulatory context, you enhance both the translational potential and regulatory alignment of your scientific discoveries.
Q1: How can I access quantitative, long-term safety data on capsular contracture rates for specific implant types?
A: The FDA's Post-Approval Studies (PAS) Database provides detailed, long-term safety outcomes for all approved breast implants. These studies are a mandatory condition of device approval and contain longitudinal data on local complications, including capsular contracture rates, reoperations, and explantations, stratified by implant type and patient indication. For example, searching the PAS for Mentor MemoryGel implants (P030053) reveals 7-year cumulative incidence rates for capsular contracture (Baker Grades III/IV) of 7.2% for primary augmentation patients and 18.0% for revision-augmentation patients [77]. This data serves as a critical benchmark for evaluating the potential efficacy of novel anti-fibrotic strategies against current clinical outcomes.
Q2: What specific risk information related to fibrosis and the Foreign Body Response (FBR) must be included in breast implant labeling?
A: Per FDA guidance issued in September 2020, breast implant labeling must include a Boxed Warning and a Patient Decision Checklist [78] [79]. These documents explicitly communicate the risk of capsular contracture and the potential for systemic symptoms (often grouped under "Breast Implant Illness"). The labeling conveys that the device's lifespan is limited and that additional surgeries may be required to treat complications like hardening of the implant [80]. For researchers, this mandated content precisely identifies the clinical fibrotic complications that your work aims to mitigate.
Q3: My research suggests a novel biomaterial coating reduces myofibroblast activation. How can I position these findings within the current regulatory context?
A: Your findings should be contextualized using the FDA's recognized pathophysiological framework of the FBR. The agency's resources acknowledge that the FBR is a complex process leading to fibrous encapsulation, and that implant surface properties govern initial protein adsorption, which in turn orchestrates immune cell activation and fibrosis [36]. When presenting your data, explicitly map your biomaterial's mechanism of action onto the phases of the FBR as delineated in FDA-accepted scientific reviews [36]. Furthermore, propose how the efficacy of your coating could be monitored using endpoints already collected in PAS, such as capsular contracture rates and reoperation frequencies, to facilitate future regulatory evaluation.
Q4: What are the documented limitations of current post-market surveillance data that might affect my retrospective analysis?
A: Key limitations you must account for in your experimental design include:
- Low Follow-up Rates: Some large PAS have historically suffered from low follow-up rates (e.g., ~20% at 7 years in one study), which can introduce bias and limit the interpretation of long-term safety [77].
- Data Gaps: Medical Device Reports (MDRs) are a passive surveillance system, leading to potential underreporting and often containing incomplete data on implant specifics and patient history [80] [81].
- Non-Mandatory Registries: Participation in registries like the National Breast Implant Registry (NBIR) is voluntary for surgeons, which may result in data sets that are not fully representative [81].
Troubleshooting Guides for Common Research Challenges
Challenge 1: Translating In Vitro Findings to Predict In Vivo Efficacy
| Symptom | Potential Root Cause | Recommended Action |
|---|---|---|
| A novel surface treatment shows excellent anti-fibrotic properties in 2D cell culture but fails in a small animal model. | The in vitro environment does not replicate the complex, dynamic immune response and mechanical forces present in vivo. | 1. Consult FBR Phase Models: Design your in vivo experiments to specifically target and analyze distinct phases of the Foreign Body Response, such as the acute inflammatory phase or the FBGC formation phase [36].2. Benchmark Against Clinical Data: Compare the characteristics of the fibrous capsule formed in your model (e.g., thickness, collagen density, myofibroblast presence) with known clinical data and manufacturer PAS data on capsular contracture [77] [82]. |
Challenge 2: Identifying Clinically Relevant Endpoints for Grant Applications
| Symptom | Potential Root Cause | Recommended Action |
|---|---|---|
| Difficulty justifying the clinical relevance of a proposed molecular biomarker for fibrosis. | The biomarker's connection to patient-centered outcomes or established regulatory endpoints is not clearly defined. | 1. Leverage PAS Data: Reference specific quantitative endpoints from PAS, such as "Kaplan-Meier estimated cumulative incidence of reoperation" due to capsular contracture, which was 11.7% for primary augmentation at 7 years in one cohort [77].2. Correlate with Baker Grades: Propose a validation strategy to correlate your novel biomarker with the clinical gold standard, the Baker classification system for capsular contracture, used in PAS and clinical practice [55]. |
Challenge 3: Interpreting Conflicting Data on Implant Surface Properties
| Symptom | Potential Root Cause | Recommended Action |
|---|---|---|
| Published literature presents conflicting conclusions on how surface texture influences fibrosis. | Study outcomes are confounded by multiple variables, including surgical technique, patient population, and implant location. | 1. Review Regulatory History: Understand that textured implants (specifically Allergan's BIOCELL) were voluntarily recalled in 2019 due to their link to BIA-ALCL, shifting the risk-benefit calculus for texture-related modifications [83] [80].2. Focus on Mechanism: Redirect research focus from empirical texture observations to the fundamental molecular mechanisms by which surface topography modulates macrophage polarization (M1 vs. M2 phenotypes) and subsequent fibroblast activity, a pathway acknowledged by the FDA's scientific sources [36]. |
Research Reagent Solutions for Fibrosis and FBR Studies
| Item | Function/Application in Fibrosis Research | Example/Note |
|---|---|---|
| Macrophage Polarization Assays | To quantify the shift from pro-inflammatory (M1) to pro-fibrotic (M2) phenotypes, which is a central event in the FBR driving fibrosis [36]. | Use cytokine cocktails (e.g., IFN-γ+LPS for M1; IL-4+IL-13 for M2) and analyze via flow cytometry (CD86, iNOS, CD206, ARG1) or qPCR. |
| Histological Staining for Capsule Assessment | To characterize the composition, thickness, and cellularity of the fibrotic capsule in in vivo models. | Masson's Trichrome (collagen), Picrosirius Red (collagen birefringence), α-SMA immunohistochemistry (myofibroblasts), H&E (general morphology). |
| Foreign Body Giant Cell (FBGC) Markers | To identify and quantify the formation of FBGCs, a hallmark of the chronic inflammatory phase of the FBR [36]. | Staining for multinucleated cells (H&E) and specific markers like CD68/CD163. |
| Cytokine Profiling Arrays | To measure the levels of key pro-fibrotic cytokines (e.g., TGF-β, PDGF, TNF-α) in peri-implant fluid or cell culture supernatants. | Commercially available multiplex ELISA kits allow simultaneous measurement of multiple analytes from small sample volumes. |
| FDA's PAS Database | To access real-world, long-term clinical data on complication rates for benchmarking and contextualizing preclinical findings [83] [77] [82]. | Publicly accessible via accessdata.fda.gov. Search by manufacturer (e.g., Mentor, Allergan) or approval number (e.g., P030053). |
Visualizing the Foreign Body Response to Breast Implants
The following diagram illustrates the key cellular and molecular phases of the Foreign Body Response (FBR), which leads to fibrotic encapsulation, as detailed in FDA-cited scientific literature [36]. This roadmap is essential for identifying potential targets for therapeutic intervention.
Diagram Title: Phases of the Foreign Body Response to Breast Implants
Experimental Protocols from Post-Approval Studies
Protocol 1: Analyzing Long-Term Complication Rates from PAS Data
This methodology outlines how to extract and analyze quantitative fibrosis-related data from the FDA's PAS database for use in comparative effectiveness research.
1. Objective: To determine the cumulative incidence of capsular contracture requiring reoperation for a specific breast implant model over a 7-10 year period.
2. Data Source: FDA PAS Database (e.g., for Mentor MemoryGel, Application P030053/PAS001; for Allergan Natrelle, P020056/PAS001) [77] [82].
3. Methodology:
- Data Extraction: Navigate to the PAS database and identify the study report for the implant of interest. Locate the "Final Safety Findings" or "Interim Results" section.
- Outcome Measures: Extract Kaplan-Meier estimated cumulative incidence rates for key endpoints:
Capsular Contracture (Baker Grades III/IV)Reoperation(and the specific reason for reoperation, e.g., "capsular contracture")Implant Removal
- Stratification: Record data stratified by patient indication (Primary Augmentation, Revision-Augmentation, Primary Reconstruction, Revision-Reconstruction), as complication profiles differ significantly between these groups [77].
- Statistical Note: The PAS often uses Kaplan-Meier analysis to account for variable patient follow-up times. Note the follow-up rate at the time of analysis, as low rates may affect reliability.
4. Application: The extracted data provides a clinical benchmark. For instance, if your novel anti-fibrotic hydrogel demonstrates a 60% reduction in capsule thickness in a rodent model, you can contextualize this by referencing the clinical contracture rates your technology aims to improve upon.
Protocol 2: Clinical Correlation of Risk Factors for Capsular Contracture
This protocol is based on a retrospective clinical study that identified independent risk factors for capsular contracture, providing a framework for validating pre-clinical findings [55].
1. Objective: To assess the impact of specific patient and surgical factors on the development of capsular contracture.
2. Study Design: Retrospective cohort study.
3. Patient Population:
- Inclusion Criteria: Patients undergoing primary breast augmentation with silicone implants, complete clinical records, minimum 12-month follow-up.
- Exclusion Criteria: Prior breast surgery, concurrent reconstructive procedures, systemic autoimmune disorders affecting wound healing.
4. Data Collection and Variables:
- Outcome Variable: Capsular contracture graded by the Baker classification system (I-IV) by blinded, board-certified surgeons.
- Independent Variables:
- Patient demographics (age, BMI)
- Smoking history
- Implant characteristics (size, surface texture)
- Surgical details (approach, plane)
- Postoperative events (hematoma, drainage volume)
- Experimental Variable: If applicable, implant oversizing, defined as volume exceeding preoperative planning recommendation by ≥20% [55].
5. Statistical Analysis:
- Perform univariate analysis (t-tests, chi-square) to identify variables associated with capsular contracture.
- Enter significant variables into a multivariate logistic regression model to identify independent risk factors, reported as Odds Ratios (OR) with 95% Confidence Intervals (CI). The referenced study found smoking (OR=2.95), implant oversizing (OR=6.00), and hematoma (OR=14.60) to be significant independent risk factors [55].
The following tables consolidate key long-term safety data from FDA Post-Approval Studies, providing a critical resource for evaluating the clinical significance of fibrotic complications.
Table 1: Seven-Year Cumulative Incidence of Key Complications in Mentor MemoryGel Silicone Implants [77]
| Patient Indication | Any Complication or Reoperation | Capsular Contracture Baker II | Capsular Contracture Baker III/IV | Implant Removal | Reoperation |
|---|---|---|---|---|---|
| Primary Augmentation | 35.9% | 8.7% | 7.2% | 6.2% | 11.7% |
| Revision-Augmentation | 50.8% | 20.2% | 18.0% | 12.5% | 18.9% |
| Primary Reconstruction | 53.4% | 12.3% | 12.7% | 15.9% | 24.7% |
| Revision-Reconstruction | 58.5% | 16.1% | 18.3% | 17.4% | 26.6% |
Table 2: Top Reasons for Reoperation and Explantation at 7 Years (Mentor MemoryGel) [77]
| Patient Indication | Primary Reason for Reoperation | % of Procedures | Primary Reason for Explantation | % of Procedures |
|---|---|---|---|---|
| Primary Augmentation | Capsular Contracture (Gr II/III/IV) | 26.8% | Patient Requested Size Change | 58.9% |
| Revision-Augmentation | Capsular Contracture (Gr II/III/IV) | 31.1% | Patient Requested Size Change | 44.8% |
| Primary Reconstruction | Asymmetry | 22.1% | Asymmetry | 26.4% |
| Revision-Reconstruction | Asymmetry | 24.4% | Asymmetry | 31.2% |
Conclusion
The prevention of fibrotic encapsulation is pivoting from a purely mechanical approach to a sophisticated understanding of immunology and mechanobiology. Key takeaways confirm that softening implant surfaces, disrupting the mechanical activation of TGF-β via integrin inhibition, and steering macrophage polarization are potent strategies to reduce fibrosis. The successful clinical application of textured implants, despite recent challenges, validates the principle that surface properties dictate biological response. Future directions must focus on personalized immunomodulation, the development of smart biomaterials with active therapeutic release, and rigorous preclinical models that better recapitulate the human immune response. Bridging these interdisciplinary insights from foundational molecular research to clinical validation will be paramount for developing the next generation of bio-integrative breast implants.
References
- 1. Pro-Fibrotic CD26-Positive Fibroblasts Are Present in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7317086/]
- 2. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 3. Decoding Fibrotic Encapsulation in Plastic Surgery implants [https://www.sciencedirect.com/science/article/abs/pii/S0927776525006988]
- 4. Fibroblast and myofibroblast in normal tissue repair and... activation [https://www.nature.com/articles/s41580-024-00716-0?error=cookies_not_supported&code=4a6d272e-7113-4052-812c-fd0d3adc7603]
- 5. and Myofibroblasts -Mitochondrial and metabolic control of... Fibrosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC7982967/]
- 6. Silicone implant surface microtopography modulates ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1342895/full]
- 7. Implant-based breast surgery and capsular formation [https://pmc.ncbi.nlm.nih.gov/articles/PMC10632565/]
- 8. Current Concepts in Capsular Contracture [https://pmc.ncbi.nlm.nih.gov/articles/PMC8432999/]
- 9. Macrophages in immunoregulation and therapeutics [https://www.nature.com/articles/s41392-023-01452-1]
- 10. T Cells in Fibrosis and Fibrotic Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7333347/]
- 11. CD4+T and CD8+T cells profile in lung inflammation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1562892/full]
- 12. Impact on capsule formation for three different types of ... [https://www.nature.com/articles/s41598-022-17320-x]
- 13. What is capsular contracture and how can it be treated? [https://www.plasticsurgery.org/news/blog/what-is-capsular-contracture-and-how-can-it-be-treated]
- 14. Cross Talk among TGF-β Signaling Pathways, Integrins, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3220354/]
- 15. TGF-β signaling in health, disease and therapeutics [https://www.nature.com/articles/s41392-024-01764-w]
- 16. Modeling mechanical activation of macrophages during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10980276/]
- 17. Role of integrins in the development of fibrosis ... [https://www.frontiersin.org/journals/ophthalmology/articles/10.3389/fopht.2023.1274797/full]
- 18. TGF-β signaling in fibrosis - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4408550/]
- 19. The pivotal role of TGF-β/Smad pathway in fibrosis ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1649179/full]
- 20. Integrins in cardiac fibrosis [https://pubmed.ncbi.nlm.nih.gov/35872324/]
- 21. The Relationship of Bacterial Biofilms and Capsular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5127460/]
- 22. SMI-Capsular Fibrosis and Biofilm Dynamics: Molecular ... [https://www.mdpi.com/1422-0067/25/21/11675]
- 23. Characterization of Biofilm Formation Ability, Virulence Factors and... [https://ijvm.ut.ac.ir/article_82768.html]
- 24. Oral Microorganisms and Biofilms : New Insights to Defeat the Main... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9781395/]
- 25. The 3D theory of osseointegration: material, topography, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317956/]
- 26. Development, fabrication and evaluation of a novel ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706116306481]
- 27. Micro vs. Nano Surface Modifications for Implants [https://completesmilesbv.com.au/micro-vs-nano-surface-modifications-for-implants/]
- 28. Dental implant surface morphology, chemical composition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9932231/]
- 29. Advances in Etiology and Prevention of Capsular Contracture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12031949/]
- 30. Suppression of the fibrotic encapsulation of silicone ... [https://profiles.wustl.edu/en/publications/suppression-of-the-fibrotic-encapsulation-of-silicone-implants-by/]
- 31. Preventing fibrotic encapsulation | Nature Reviews Materials [https://www.nature.com/articles/s41578-021-00338-4]
- 32. How to Troubleshoot Common Issues in Silicone Molding [https://www.siliconeplus.net/blog/How-to-Troubleshoot-Common-Issues-in-Silicone-Molding_b8296]
- 33. Understanding silicone elastomer curing and adhesion for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12266107/]
- 34. Troubleshooting Common Silicone Molding Problems and ... [https://www.nicerapid.com/blog/troubleshooting-common-silicone-molding-problems-and-mistakes/]
- 35. Modulating the Configurations of “Gel-Type†Soft Silicone ... [https://www.mdpi.com/2310-2861/9/9/686]
- 36. Biomimetic optimization of silicone breast implant integration [https://pmc.ncbi.nlm.nih.gov/articles/PMC12484225/]
- 37. Transforming growth factor-β receptors [https://www.nature.com/articles/s41401-024-01235-6]
- 38. Structural insights and clinical advances in small-molecule ... [https://www.sciencedirect.com/science/article/pii/S2950329925000141]
- 39. Structure-guided engineering of TGF-βs for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7797196/]
- 40. Emerging therapeutic opportunities for integrin inhibitors [https://www.nature.com/articles/s41573-021-00284-4]
- 41. Investigating Immunomodulatory Biomaterials for Preventing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10741225/]
- 42. Adoptive Transfer of Immunomodulatory Macrophages ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11486562/]
- 43. Breast Implant Safety [https://www.plasticsurgery.org/patient-safety/breast-implant-safety]
- 44. Recognizing and Managing Breast Implant Complications [https://pmc.ncbi.nlm.nih.gov/articles/PMC12067747/]
- 45. Frontiers | Biomimetic optimization of silicone breast implant integration: insights into wound healing and the foreign body response [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1668930/full]
- 46. BD Announces Milestone in Clinical Trial for Use of ... [https://news.bd.com/2025-03-20-BD-Announces-Milestone-in-Clinical-Trial-for-Use-of-Bioabsorbable-GalaFLEX-LITE-TM-Scaffold-in-Breast-Implant-Revision-Surgery,1]
- 47. Early Systemic Immune Response to Silicone Breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11884710/]
- 48. Breast implant silicone exposure induces immunogenic ... [https://www.sciencedirect.com/science/article/pii/S0142961224005611]
- 49. SEM and TEM for identification of capsular fibrosis and cellular behavior around breast implants – a descriptive analysis | BMC Molecular and Cell Biology | Full Text [https://bmcmolcellbiol.biomedcentral.com/articles/10.1186/s12860-021-00364-8]
- 50. Rupture Of Breast Implants Does Not Cause Systemic Or ... [https://ps-rc.org/meeting/program/2025/7.cgi]
- 51. Breast Implant Illness: Symptoms, Outcomes with ... [https://link.springer.com/article/10.1007/s00266-025-05142-x]
- 52. Personalized Risk Assessment of Hepatic Fibrosis after ... [https://www.mdpi.com/2077-0383/12/20/6489]
- 53. How to prevent complications in breast augmentation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5409896/]
- 54. Analysis of risk factors for capsular contracture after breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12129903/]
- 55. Analysis of risk factors for capsular contracture after breast ... [https://www.frontiersin.org/journals/surgery/articles/10.3389/fsurg.2025.1596993/full]
- 56. Advances in Etiology and Prevention of Capsular ... [https://link.springer.com/article/10.1007/s00266-024-04500-5]
- 57. The history and development of breast implants - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7450417/]
- 58. 4 Most Common Reasons for Medical Device Material Failures [https://inside.battelle.org/blog-details/4-most-common-reasons-for-medical-device-material-failures]
- 59. Biomaterials for Protein Delivery: Opportunities and ... [https://www.mdpi.com/2072-666X/15/4/533]
- 60. Challenges in Biomaterial-Based Drug Delivery Approach for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7795247/]
- 61. A Novel In Vitro Potency Assay Demonstrating the Anti- ... [https://www.mdpi.com/2227-9059/13/11/2652]
- 62. Electrospun polycaprolactone fibers encapsulating omega ... [https://pubmed.ncbi.nlm.nih.gov/40412454/]
- 63. Development and characterization of anti-fibrotic natural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8891108/]
- 64. Design and Synthesis of Novel Pirfenidone Analogues for ... [https://pubmed.ncbi.nlm.nih.gov/40969868/]
- 65. Micro-CT-assisted identification of the optimal time-window ... [https://www.nature.com/articles/s41598-024-65030-3]
- 66. Screening and validation of active components in Rosa ... [https://pubmed.ncbi.nlm.nih.gov/40154178/]
- 67. Establishment of a humanized mouse model of pulmonary ... [https://www.nature.com/articles/s41598-025-18370-7]
- 68. The first step for understanding the molecular mechanism ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1610165/full]
- 69. Risks and Complications of Breast Implants [https://www.fda.gov/medical-devices/breast-implants/risks-and-complications-breast-implants]
- 70. Perception of Risk and the Choice Between Smooth ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278739/]
- 71. Effect of tissue microenvironment on fibrous capsule formation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8135119/]
- 72. Clinical and morphological conditions in capsular ... [https://pubmed.ncbi.nlm.nih.gov/17572576/]
- 73. a comparison of two implants according to a modification ... [https://pubmed.ncbi.nlm.nih.gov/22729961/]
- 74. Histologic, Molecular, and Clinical Evaluation of Explanted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4649701/]
- 75. Histological analysis of silicone breast implant capsules ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961202004295]
- 76. Troubleshooting Histopathology & Tissue Processing [https://www.leicabiosystems.com/en-nl/knowledge-pathway/troubleshooting-routine-histology-a-guide-on-how-to-avoid-common-mistakes/]
- 77. Post-Approval Studies (PAS) Database - accessdata.fda.gov [https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma_pas.cfm?c_id=72&t_id=90325]
- 78. Breast Implants [https://www.fda.gov/medical-devices/implants-and-prosthetics/breast-implants]
- 79. Labeling for Approved Breast Implants [https://www.fda.gov/medical-devices/breast-implants/labeling-approved-breast-implants]
- 80. FDA Releases New Updates on the Safety and ... [https://bisanonprofit.org/blog/breast-implant-safety-alliance-bisa-fda-releases-new-updates-on-the-safety-and-effectiveness-of-breast-implants]
- 81. Conflicting interpretations and FDA reputation: the case of ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1475992/full]
- 82. Post-Approval Studies (PAS) Database - accessdata.fda.gov [https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma_pas.cfm?c_id=73&t_id=90235]
- 83. Breast Implant Postmarket Safety Information [https://www.fda.gov/medical-devices/breast-implants/breast-implant-postmarket-safety-information]