Predicting and Controlling Biomaterial-Host Interactions: A Roadmap to Overcome Response Variability
This article addresses the critical challenge of variability in host responses to biomaterials, a major hurdle in clinical translation for researchers and drug development professionals.
Predicting and Controlling Biomaterial-Host Interactions: A Roadmap to Overcome Response Variability
Abstract
This article addresses the critical challenge of variability in host responses to biomaterials, a major hurdle in clinical translation for researchers and drug development professionals. It explores the foundational biological sources of this variability, from individual immune profiles to biomaterial physicochemical properties. The scope encompasses novel methodological frameworks like 'bottom-up' biomaterial design and AI-driven predictive modeling, alongside troubleshooting strategies for immune modulation and personalization. Finally, it evaluates advanced in silico and in vitro validation techniques designed to reliably predict in vivo performance and facilitate comparative analysis of next-generation biomaterials.
Decoding the Sources of Variability: From Biological Systems to Material Properties
Frequently Asked Questions (FAQs)
Q1: Why is understanding macrophage polarization (M1/M2) critical for the success of my biomaterial implant?
Macrophage polarization is a pivotal determinant of biomaterial fate. The dynamic equilibrium between pro-inflammatory M1 and pro-healing M2 phenotypes directly dictates the balance between destructive inflammation and constructive tissue regeneration [1] [2].
- M1 Macrophages: Induced by stimuli like LPS and IFN-γ, they are characterized by the production of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) and markers like iNOS and CD80. They initiate necessary inflammatory responses but can lead to chronic inflammation, fibrous encapsulation, and implant failure if their activity is prolonged [3] [4].
- M2 Macrophages: Induced by signals like IL-4 and IL-13, they express markers like CD206 and CD163 and secrete anti-inflammatory cytokines (IL-10, TGF-β). They promote tissue repair, angiogenesis, and biomaterial integration [3] [2] [4].
A successful biomaterial facilitates a timely transition from a dominant M1 phenotype in the early stages to a dominant M2 phenotype in the later stages of healing [2].
Q2: Which physical properties of a biomaterial can I modify to influence macrophage behavior?
The physical cues of biomaterials are potent immunomodulators that can be engineered to guide macrophage polarization, offering a powerful strategy to reduce research variability stemming from ill-defined material properties [2].
- Stiffness: Macrophages tend to polarize toward an M1 phenotype on stiffer substrates and toward an M2 phenotype on softer substrates that mimic the elasticity of native tissues [2] [5].
- Topography and Surface Roughness: Micropatterned and nano-rough surfaces generally promote an anti-inflammatory M2 phenotype, while smooth surfaces can exacerbate pro-inflammatory M1 responses [2].
- Pore Architecture: Three-dimensional scaffold architectures, particularly those with larger pore sizes (e.g., 50×50×20 μm³), have been shown to promote an M2-like expression profile, whereas smaller pores can increase M1-associated markers [2] [6].
- Hydrophilicity: Hydrophilic surfaces typically reduce foreign body reactions and favor M2 polarization, while hydrophobic surfaces can increase protein denaturation and promote M1 responses [2].
Q3: My in vivo results do not match my in vitro predictions regarding the host response. What are the common culprits for this discrepancy?
This is a central challenge in translational research. Key culprits include:
- Oversimplified In Vitro Models: Standard in vitro cultures often use extreme polarizing conditions (e.g., high-dose LPS or IL-4) and lack the complexity of the in vivo immune cell crosstalk (e.g., with T cells, neutrophils) and dynamic cytokine milieu [2].
- Serum Protein Adsorption: The "protein corona" that instantly forms on a biomaterial upon implantation in vivo can completely mask the engineered surface properties you tested in vitro, altering how immune cells recognize the material [7].
- Mechanical Mismatch: The mechanical mismatch between your implant and the surrounding tissue creates a mechanical microenvironment not captured in standard 2D cultures, significantly influencing macrophage mechanosensing and response [8].
Q4: What are the key signaling pathways involved in macrophage polarization that I should analyze to validate my biomaterial's immunomodulatory effects?
Biomaterials influence macrophage fate through specific signaling pathways. Analyzing these is key to validating your material's design and ensuring consistent outcomes. The table below summarizes the core pathways.
Table 1: Key Signaling Pathways in Macrophage Polarization
| Pathway | Primary Inducers | Key Transcription Factors | Resulting Phenotype & Output |
|---|---|---|---|
| NF-κB / MAPK [1] [4] | LPS, TNF-α, DAMPs/PAMPs [1] | NF-κB, AP-1 | M1 Phenotype: Pro-inflammatory cytokine production (TNF-α, IL-1β, IL-6) [4]. |
| JAK-STAT1 [3] [4] | IFN-γ | STAT1 | M1 Phenotype: iNOS expression, antimicrobial activity [3] [4]. |
| JAK-STAT6 [3] [4] | IL-4, IL-13 | STAT6, PPARγ | M2 Phenotype (M2a): Tissue repair, fibrosis, expression of CD206, arginase-1 [3] [4]. |
| PI3K-Akt [4] | Growth factors, IL-4 | Akt, mTOR | Dual Role: Can support both M1 (glycolysis) and M2 (metabolic reprogramming) polarization depending on context [4]. |
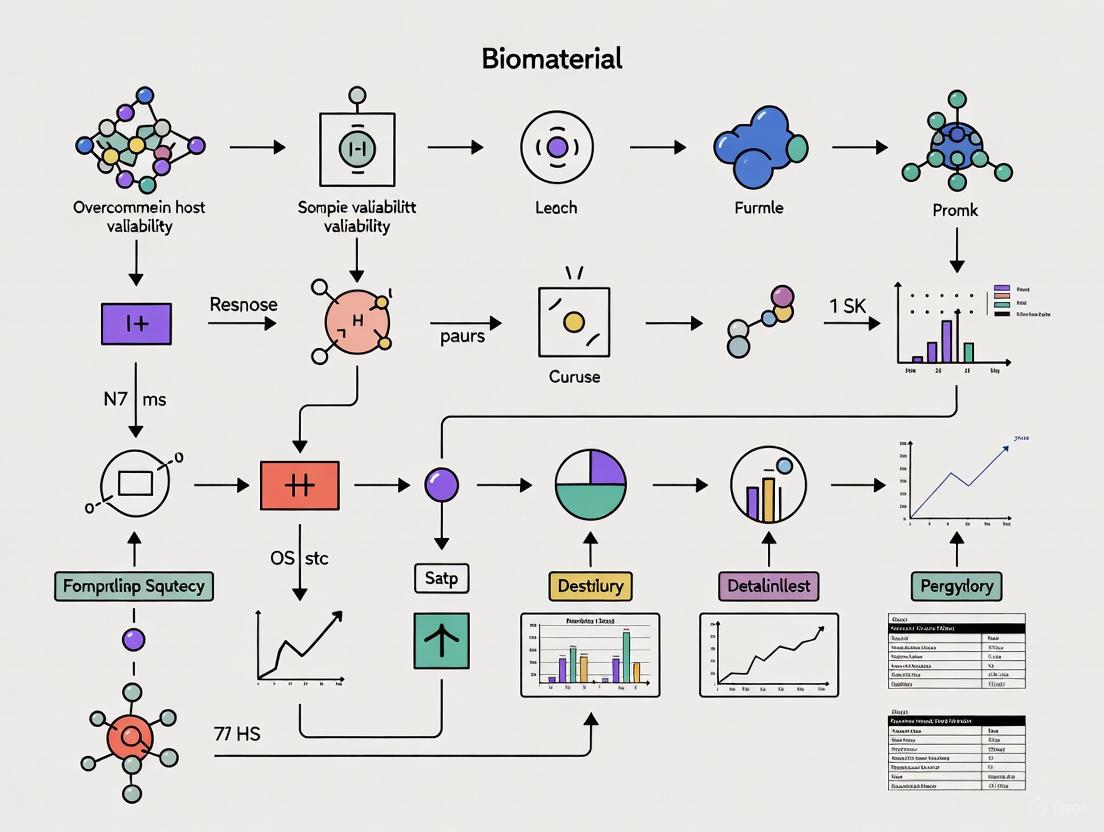
The following diagram illustrates the logical relationship and crosstalk between these key signaling pathways in macrophage polarization.
Troubleshooting Guides
Issue: Uncontrolled Foreign Body Reaction and Fibrosis
A persistent pro-inflammatory response often leads to dense fibrous capsule formation, isolating the implant and causing failure [7] [5].
Investigation and Resolution Protocol:
Characterize the Immune Microenvironment:
- Method: Implant your biomaterial in a relevant animal model. At multiple time points (e.g., 3, 7, 14, 28 days), explant the tissue and perform:
- Immunohistochemistry (IHC)/Immunofluorescence (IF): Stain for M1 (iNOS, CD80) and M2 (CD206, ARG1) markers to quantify the M1/M2 ratio spatially and temporally [7].
- RNA Analysis: Use qPCR on explanted tissue to analyze the expression of key pro-inflammatory (TNF-α, IL-1β) and anti-inflammatory (IL-10, TGF-β) cytokines [1].
- Method: Implant your biomaterial in a relevant animal model. At multiple time points (e.g., 3, 7, 14, 28 days), explant the tissue and perform:
Modify Biomaterial Physicochemical Properties:
- Action: If analysis confirms chronic M1 dominance, redesign your biomaterial.
- Reduce Stiffness: If possible, tune the scaffold's elastic modulus to better match the target tissue [2].
- Alter Surface Topography: Introduce micro/nano-scale roughness or specific patterns known to promote M2 polarization [2] [5].
- Incorporate Bioactive Cues: Functionalize the material with anti-inflammatory cytokines (e.g., IL-4) or specific ECM-derived peptides (e.g., RGD) to actively steer macrophages toward an M2 phenotype [1] [8].
- Action: If analysis confirms chronic M1 dominance, redesign your biomaterial.
Issue: High Variability in Macrophage Response Between Experimental Batches
Inconsistent outcomes can stem from uncontrolled variables in biomaterial fabrication or cell culture.
Investigation and Resolution Protocol:
Audit Your Material Characterization:
- Action: For every new batch of biomaterial, rigorously characterize:
- Documentation: Maintain a detailed log of all fabrication parameters (e.g., polymer lot, crosslinking time, temperature).
Standardize Your Cell-Based Assays:
- Cell Source: Use a consistent and well-characterized source of macrophages (e.g., primary human monocyte-derived macrophages from a specific donor pool or a specific cell line like THP-1). Document passage numbers and differentiation protocols meticulously [3].
- Serum Control: Use the same lot of fetal bovine serum (FBS) for an entire study to minimize variability introduced by serum-derived factors [7].
- Stimulation Consistency: Prepare stock solutions of polarizing agents (LPS, IFN-γ, IL-4) in single-use aliquots to avoid freeze-thaw cycles and degradation.
The following workflow diagram outlines a standardized experimental approach to minimize variability from material fabrication through to data analysis.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Macrophage-Biomaterial Studies
| Reagent/Material | Function in Experiments | Key Considerations |
|---|---|---|
| THP-1 Cell Line | A human monocytic cell line; can be differentiated into macrophages using PMA. | Provides a renewable, consistent cell source. Must ensure consistent differentiation protocols. Response may differ from primary cells [3]. |
| Primary Human Monocytes | Isolated from peripheral blood, these differentiate into macrophages (e.g., with M-CSF). | More physiologically relevant. High donor-to-donor variability must be accounted for in experimental design [3] [4]. |
| Polarizing Cytokines (IL-4, IL-13, IFN-γ, LPS) | Used to polarize macrophages toward specific (M1 or M2) phenotypes in vitro. | Use high-purity, endotoxin-free reagents. Aliquot to preserve activity. Concentration and timing are critical [3] [2] [4]. |
| Anti-CD68 / Anti-Iba1 Antibodies | Pan-macrophage markers for identifying total macrophage population in tissue sections (IHC/IF) [9]. | Validate antibodies for your specific species and application (IHC vs. IF). |
| Anti-iNOS / Anti-CD206 Antibodies | Classic markers for identifying M1 (iNOS) and M2 (CD206) polarized macrophages via IHC/IF or flow cytometry [2] [4]. | Be aware that macrophages exist on a spectrum; using multiple markers is more reliable than a single one. |
| Polycaprolactone (PCL) | A common synthetic, biodegradable polymer used to fabricate 3D scaffolds for tissue engineering. | Easily tunable mechanical properties and architecture. Hydrophobic surface may need modification to enhance biocompatibility [7]. |
| Decellularized ECM Scaffolds | Natural biomaterials derived from tissues, retaining complex biochemical cues. | Highly bioactive and can promote favorable M2 polarization. Potential for batch-to-batch variability and immunogenicity if not properly decellularized [8] [7]. |
| RGD Peptide | A fibronectin-derived peptide used to functionalize biomaterial surfaces to promote cell adhesion. | Enhances integrin-mediated macrophage adhesion, which can influence polarization fate. The density and spatial presentation are critical [8]. |
| Sulfo Cy5.5-N3 | Sulfo Cy5.5-N3, MF:C46H53N6NaO10S3, MW:969.1 g/mol | Chemical Reagent |
| Resveratrol-3-O-beta-D-glucuronide-13C6 | Resveratrol-3-O-beta-D-glucuronide-13C6, MF:C20H20O9, MW:410.32 g/mol | Chemical Reagent |
Troubleshooting Guide: Frequently Asked Questions
FAQ 1: Our in vivo implant study shows high variability in fibrotic capsule thickness between test animals. What are the primary factors driving this outcome variability, and how can we control for them?
Several interrelated factors contribute to variability in fibrosis outcomes. To control for them, focus on the following:
- Biomaterial Surface Properties: The chemical, physical, and morphological characteristics of your biomaterial surface are a primary modulator of the FBR [10] [11]. Surface properties dictate the initial adsorption of host proteins (like fibrinogen and fibronectin), which in turn influences subsequent immune cell adhesion and activation [11]. Standardize and thoroughly characterize your material's surface properties (e.g., roughness, wettability, chemistry) between batches.
- Host Immune Cell Heterogeneity: The FBR is driven by a dynamic network of cells, notably macrophages and fibroblasts, which are not uniform populations [12] [13]. The balance between pro-inflammatory (M1) and pro-healing (M2) macrophages, as well as the activity of different fibroblast subpopulations, can significantly impact the degree of fibrosis [12] [11]. Use flow cytometry and transcriptional analysis to characterize the immune cell profile at the implant interface rather than relying solely on histological endpoints.
- Surgical Technique and Implantation Site: Inconsistent surgical procedures, including the degree of tissue injury and implantation technique, can introduce significant variability [11]. Implement a standardized surgical protocol and consider the specific physiological environment of the implantation site.
FAQ 2: We are observing inconsistent monocyte adhesion and macrophage fusion on our biomaterials in vitro. What could be causing this, and how can we improve the consistency of our cell culture models?
Inconsistencies in in vitro cell behavior often stem from the protein layer that spontaneously forms on the material prior to cell interaction.
- Protein Adsorption and the Vroman Effect: The types, concentrations, and conformations of proteins adsorbed to your biomaterial from the cell culture medium are critical determinants of cell adhesion [11]. This layer is dynamic, with proteins adsorbing and desorbing over time (the Vroman Effect). To improve consistency:
- Pre-condition materials: Pre-incubate all material samples in the relevant protein solution (e.g., serum) for a standardized duration before adding cells.
- Use defined media: Whenever possible, use cell culture media with defined protein compositions to reduce batch-to-batch variability of serum.
- Characterize the adsorbed layer: Utilize techniques like immunofluorescence or quartz crystal microbalance to confirm the consistency of the protein layer on your material surfaces.
FAQ 3: What are the key molecular and cellular markers we should track to reliably stage the Foreign Body Response in our animal models?
Reliable staging requires monitoring a combination of cellular and molecular markers across the timeline of the FBR. The table below summarizes key indicators.
Table 1: Key Markers for Staging the Foreign Body Response
| Stage of FBR | Timeline | Key Cellular Players | Characteristic Molecular Markers |
|---|---|---|---|
| Acute Inflammation | First ~1-7 days | Neutrophils, Mast Cells, M1 Macrophages | TNF-α, IL-6, IL-1β, Histamine [12] [11] |
| Chronic Inflammation / FBGC Formation | ~1-4 weeks | Monocytes, M1/M2 Macrophages, Foreign Body Giant Cells (FBGCs) | IL-4, IL-13, CCL2 (MCP-1), iNOS (M1), CD206 (M2) [12] [11] |
| Granulation Tissue & Fibrosis | ~2 weeks onward | Myofibroblasts, Endothelial Cells, Macrophages | TGF-β1, α-SMA (alpha-smooth muscle actin), Collagen I/III, PDGF [12] [14] |
FAQ 4: How can we leverage computational tools to predict and manage variability in biomaterial-host interactions?
Machine learning (ML) is an emerging powerful tool to navigate the complex parameter space of biomaterial design and host response.
- Handling Multi-dimensional Data: ML can identify non-intuitive relationships between a biomaterial's input parameters (e.g., composition, surface topography, stiffness) and its in vivo output properties (e.g., extent of fibrosis, capsule thickness) [15].
- Accelerating Discovery: Supervised learning models can be trained on existing experimental data to predict the biological performance of new, untested biomaterials, drastically reducing the need for extensive and costly in vivo experimentation [15]. Start by building a structured dataset of your material properties and corresponding experimental outcomes to serve as a foundation for such models.
FAQ 5: What are the most promising strategic approaches for designing biomaterials that mitigate the FBR?
Current strategies focus on actively modulating the immune response rather than simply being inert.
- Immunomodulation: Incorporate anti-inflammatory cytokines (e.g., IL-10) or specific metabolic inhibitors into the biomaterial to steer the local immune microenvironment toward a pro-regenerative, anti-fibrotic state [14].
- Mechanical Property Tuning: Cells sense and respond to mechanical cues. Designing materials with stiffness that discourages fibroblast-to-myofibroblast transition and dense collagen deposition can reduce fibrosis [13].
- Surface Engineering: Creating non-fouling surfaces that minimize protein adsorption (e.g., using zwitterionic hydrogels) can reduce the initial trigger for the FBR cascade [14]. Bio-inspiration, such as creating microtopographies that discourage FBGC formation, is also a viable path.
Experimental Protocols & Methodologies
Protocol 1: Isolating and Analyzing Peri-Implant Cells for FBR Staging
This protocol is adapted from recent studies investigating cellular drivers of fibrosis, including the role of skeletal stem cells and fibroblast subpopulations [12] [14].
Objective: To isolate and characterize the key cellular populations (immune cells and fibroblasts) from the tissue-biomaterial interface for precise staging of the FBR.
Materials:
- Explanted Sample: The biomaterial implant and the surrounding fibrous capsule tissue.
- Dissociation Reagents: Collagenase Type I and DNAse I in a suitable buffer like PBS or RPMI.
- Cell Staining: Fluorescently conjugated antibodies against F4/80 (macrophages), CD206 (M2 macrophage marker), α-SMA (myofibroblasts), and CD90 (fibroblasts). A viability dye (e.g., propidium iodide) is essential.
- Equipment: GentleMACS or similar tissue dissociator, flow cytometer, cell culture incubator.
Step-by-Step Methodology:
- Explanation & Tissue Processing: Surgically explain the biomaterial with its enclosing fibrous capsule. Gently separate the capsule tissue from the biomaterial surface using a scalpel, ensuring all interfacial tissue is collected.
- Enzymatic Digestion: Mince the tissue finely and place it in a digestion cocktail containing Collagenase Type I (e.g., 2 mg/mL) and DNAse I (e.g., 0.1 mg/mL). Digest for 30-60 minutes at 37°C with constant agitation. Using a GentleMACS dissociator can improve yield and consistency.
- Cell Isolation: Pass the digested tissue through a 70 µm cell strainer to obtain a single-cell suspension. Centrifuge to pellet the cells and lyse any red blood cells if necessary.
- Cell Staining & Flow Cytometry: Resuspend the cell pellet in FACS buffer. Incubate with antibody cocktails designed to identify your cell populations of interest (e.g., macrophages, fibroblasts). Include isotype controls. Analyze the stained cells using a flow cytometer.
- Data Analysis: Use flow cytometry software to identify and quantify the percentages of different cell populations (e.g., F4/80+ macrophages, F4/80+CD206+ M2 macrophages, CD90+α-SMA+ myofibroblasts). This provides a quantitative snapshot of the FBR stage.
Protocol 2: Quantifying Fibrotic Outcomes via Histomorphometry
Objective: To quantitatively assess the extent of fibrosis and capsule formation around an implanted biomaterial.
Materials:
- Tissue Sections: Formalin-fixed, paraffin-embedded (FFPE) tissue sections containing the implant site.
- Staining Reagents: Hematoxylin and Eosin (H&E) for general morphology. Picrosirius Red for collagen deposition.
- Equipment: Light microscope, polarized light microscope (for Picrosirius Red), image analysis software (e.g., ImageJ, QuPath).
Step-by-Step Methodology:
- Tissue Sectioning: Section FFPE blocks to a thickness of 5-7 µm. Ensure sections are taken from the central region of the implant.
- Staining:
- Perform H&E staining following standard protocols to visualize overall tissue structure and cellularity.
- Perform Picrosirius Red staining to specifically highlight collagen fibrils.
- Image Acquisition:
- For H&E, capture bright-field images at standardized magnifications (e.g., 40x, 100x).
- For Picrosirius Red, capture images under both bright-field and polarized light. Under polarized light, thick, mature collagen fibers appear orange/red, while thinner, newer fibers appear green.
- Image Analysis:
- Capsule Thickness: Using H&E images, take multiple, perpendicular measurements of the fibrous capsule from the implant surface to the outer edge of normal tissue. Calculate the average and standard deviation.
- Collagen Deposition & Maturity: Using Picrosirius Red images, use color thresholding in image analysis software to quantify the total area of birefringence (both red and green) as a percentage of the total tissue area. The ratio of red (mature) to green (new) collagen can provide insight into the maturity of the fibrotic tissue.
Visualizing the FBR Cascade: Signaling Pathways and Experimental Workflow
FBR Signaling Pathway
FBR Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents
This table details key reagents and their functions for investigating the Foreign Body Response.
Table 2: Key Research Reagents for FBR Investigation
| Research Reagent | Function / Target in FBR | Example Application |
|---|---|---|
| Recombinant IL-4 / IL-13 | Cytokines that drive macrophage fusion into Foreign Body Giant Cells (FBGCs) [11]. | Used in in vitro models to induce and study FBGC formation on biomaterial surfaces. |
| TGF-β1 Inhibitors | Blocks Transforming Growth Factor-beta 1 signaling, a master regulator of fibroblast activation and collagen production [12]. | In vivo administration or local release from biomaterials to test reduction of fibrotic capsule formation. |
| Anti-α-SMA Antibody | Immunostaining for Alpha-Smooth Muscle Actin, a marker for activated myofibroblasts [13]. | Identifying and quantifying the key effector cells in fibrotic encapsulation via immunohistochemistry. |
| Picrosirius Red Stain | Binds to collagen fibrils; allows for quantification of total collagen deposition and maturity under polarized light [12]. | Histological assessment of fibrosis extent and maturity around explanted biomaterials. |
| Fluorophore-conjugated Antibodies (F4/80, CD206, CD3) | Cell surface markers for macrophages (F4/80), M2 macrophages (CD206), and T-cells (CD3) [11]. | Flow cytometric immunophenotyping of the inflammatory cell infiltrate at the implant site. |
| Collagenase Type I/II | Enzymes for the digestion of collagenous tissue in the fibrous capsule. | Essential for creating single-cell suspensions from explanted tissue for downstream flow cytometry or cell culture. |
| Rediocide C | Rediocide C, MF:C46H54O13, MW:814.9 g/mol | Chemical Reagent |
| Geninthiocin | Geninthiocin, MF:C50H49N15O15S, MW:1132.1 g/mol | Chemical Reagent |
Troubleshooting Guide: Common Biomaterial Experiment Challenges
This guide addresses frequent issues encountered in biomaterials research, helping you identify potential causes and corrective actions to reduce variability in your results.
Table 1: Troubleshooting Guide for Biomaterial Experiments
| Problem | Potential Causes | Suggested Solutions |
|---|---|---|
| High Protein Fouling | Suboptimal surface chemistry or energy; experimental conditions not mimicking physiological state [16]. | Tailor surface chemistry/functional groups; use controlled biofluid sources and physiological conditions (concentration, pH, ionic strength) [17] [16]. |
| Poor Cell Adhesion | Non-adhesive protein layer (e.g., albumin); insufficient surface roughness or inappropriate functional groups [18] [16]. | Modify surface with RGD peptides or collagen; optimize nano/micro-scale topography to promote focal adhesion [18] [19]. |
| Uncontrolled/Overly Fast Degradation | Biomaterial chemical composition (e.g., ester groups) highly susceptible to hydrolysis; mismatch between degradation rate and tissue healing [20]. | Select materials with stable moieties (e.g., amides) or crosslinking; design degradation profile to match tissue regeneration time [20] [19]. |
| Severe Foreign Body Reaction & Fibrosis | Material surface properties trigger sustained inflammation; surface topography promotes pro-fibrotic macrophage response [7] [21]. | Design surfaces with anti-fibrotic chemical moieties; modulate topography/chemistry to promote pro-regenerative M2 macrophage polarization [7] [17]. |
| Irreproducible Degradation Data | Mistaking material dissolution for degradation; relying only on inferential techniques (e.g., gravimetry) without chemical confirmation [20]. | Employ multiple, complementary techniques (e.g., SEC, NMR) to confirm chemical breakdown; follow ASTM guidelines precisely [20]. |
Frequently Asked Questions (FAQs)
1. Why is my biomaterial triggering a severe inflammatory response? A severe inflammatory response is often linked to your biomaterial's surface properties. The chemical composition, topography, and surface energy directly influence initial protein adsorption, which in turn dictates immune cell activation. Furthermore, the degradation products of your material can be immunogenic. To mitigate this, focus on modulating surface chemistry and topography to promote a favorable immune response, such as encouraging anti-inflammatory M2 macrophage polarization [7] [17] [21].
2. How can I accurately measure biomaterial degradation without expensive equipment? While gravimetric analysis (mass loss) and scanning electron microscopy (SEM) for surface morphology are common and cost-effective starting points, they can be misleading as they infer but do not confirm degradation. For conclusive evidence, these physical methods should be combined with techniques that monitor chemical changes. Solution viscosity can indicate molecular weight changes, and pH tracking of the degradation medium can confirm hydrolytic processes. Be aware that ASTM guidelines recommend methods like SEC for definitive molar mass evaluation [20].
3. What is the optimal surface roughness for promoting bone integration (osseointegration)? For bone tissue engineering, studies suggest that surface roughness at the nanoscale increases extracellular matrix (ECM) protein adsorption, which promotes osteoblast attachment and differentiation. While cell infiltration can occur with pores as small as 40 μm, optimal bone formation has been observed with larger pore diameters, around 325 μm, which allows for even cell distribution and reduces peripheral cell accumulation [18].
4. My experimental fouling results are inconsistent. What critical parameters should I control? Inconsistent fouling results often stem from variations in experimental conditions. To improve reproducibility, strictly control and document these parameters:
- Protein Source and Concentration: Use consistent, fresh biofluids, as age can alter protein conformation. Concentrations can dramatically affect adsorption profiles [16].
- Ionic Strength and pH: These affect protein charge and stability, thereby influencing adsorption [16].
- Temperature: Conduct experiments at physiological temperature (37°C) when possible [16].
- Characterization Technique: Be aware that the method itself (e.g., fluorescent labeling) can alter protein behavior [16].
Essential Experimental Protocols
Protocol 1: Comprehensive In Vitro Degradation Assessment
This protocol provides a multi-faceted approach to assess biomaterial degradation, moving beyond simple mass loss.
Workflow Overview
Materials & Reagents
- Degradation Medium: Phosphate Buffered Saline (PBS), simulated body fluid (SBF), or enzymatic buffers [20].
- Sterile Containers: For incubation of samples.
- Analytical Balances: Precision of 0.1% of total sample weight is recommended [20].
- Oven or Desiccator: For drying samples to a constant weight [20].
- Characterization Equipment: SEM, Size Exclusion Chromatography (SEC), FTIR, NMR, viscometer.
Step-by-Step Procedure
- Pre-degradation Characterization: Record the initial dry mass, molecular weight, and chemical structure (via FTIR/NMR) of your biomaterial samples [20].
- Immersion: Immerse pre-weighed samples in the degradation medium (e.g., PBS at pH 7.4) in sterile containers. Maintain a consistent surface-area-to-volume ratio [20].
- Incubation: Place containers in an incubator at 37°C. The pH should be monitored and maintained at 7.4, unless testing for a specific biological environment [20].
- Sampling: Remove samples in triplicate at predetermined timepoints (e.g., days 1, 7, 14, 28, etc.). Gently rinse samples and dry to a constant weight before analysis [20].
- Post-sampling Analysis:
- Gravimetric Analysis: Measure mass loss:
(Initial Mass - Dry Mass at Time t) / Initial Mass * 100%. - Surface Morphology: Use SEM to visualize surface erosion, cracking, or porosity changes.
- Molecular Weight: Use SEC or solution viscosity to track the reduction in polymer chain length.
- Chemical Analysis: Use FTIR or NMR to confirm the breakage of chemical bonds (e.g., ester groups) and identify degradation by-products [20].
- Gravimetric Analysis: Measure mass loss:
Protocol 2: Systematic Evaluation of Protein Fouling
This protocol standardizes the critical initial step of protein adsorption to improve experimental consistency.
Materials & Reagents
- Protein Solution: Single protein (e.g., fibrinogen, albumin) or complex biofluid (e.g., blood serum). Use consistent, fresh sources [16].
- Buffer: e.g., PBS. Control ionic strength and pH meticulously [16].
- Detection Method: Radiolabels, fluorescent labels, or colorimetric assays (e.g., Micro BCA).
Step-by-Step Procedure
- Surface Preparation: Prepare biomaterial samples with identical surface properties and dimensions.
- Solution Incubation: Incubate samples with the protein solution under controlled conditions (37°C, static or flow conditions) for a set time [16].
- Rinsing: Gently rinse samples with buffer to remove loosely associated proteins.
- Protein Detection:
- Labeled Proteins: Directly measure radioactivity or fluorescence from the surface.
- Unlabeled Proteins: Elute adsorbed proteins using a detergent (e.g., 1% SDS) and quantify the concentration in the eluent using a colorimetric assay [16].
- Data Normalization: Normalize the amount of adsorbed protein to the surface area of the sample (e.g., ng/cm²).
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials and Their Functions in Biomaterial Characterization
| Research Reagent / Material | Primary Function in Experimentation |
|---|---|
| Phosphate Buffered Saline (PBS) | Standard aqueous medium for in vitro degradation studies, simulating physiological pH and ionic strength [20]. |
| Size Exclusion Chromatography (SEC) | Analytical technique to monitor changes in the molecular weight distribution of a biodegradable polymer over time [20]. |
| Fourier Transform Infrared (FTIR) Spectroscopy | Detects changes in chemical bonds and functional groups on the biomaterial surface before and after degradation or protein interaction [20]. |
| RGD Peptide | A cell-adhesive peptide ligand that can be grafted onto biomaterial surfaces to promote specific integrin-mediated cell attachment [19]. |
| Enzymatic Buffers (e.g., with Lysozyme) | Used to study enzyme-mediated degradation pathways relevant to the in vivo environment [20]. |
| Acellular Dermal Matrix (e.g., HADM, PADM) | A natural biomaterial used as a positive control in in vivo studies for effective tissue integration and mild inflammatory response [7]. |
| Eupenifeldin | Eupenifeldin, MF:C33H40O7, MW:548.7 g/mol |
| Rabdoserrin A | Rabdoserrin A, MF:C20H26O5, MW:346.4 g/mol |
Advanced Strategy: Integrating Design of Experiments (DoE) and Machine Learning
To systematically overcome variability and optimize biomaterial properties, move beyond traditional one-factor-at-a-time approaches.
Relationship Between DoE, ML, and Biomaterial Development
- Adopt a DoE Workflow: Begin by using statistical Design of Experiments (DoE) to plan your studies. This involves identifying key factors (e.g., polymer composition, pore size, crosslinking density) and their levels, then running a controlled set of experiments to model their relationship with responses (e.g., degradation rate, tensile strength, cell viability). This maximizes information while minimizing the number of experimental runs [22].
- Leverage Machine Learning: For highly complex and multi-dimensional data (e.g., from high-throughput characterization), machine learning (ML) can identify non-linear relationships and hidden patterns that traditional statistics might miss. ML models can predict optimal biomaterial compositions and properties, drastically accelerating the discovery pipeline [15] [22].
- Combine Both Methods: Use DoE to generate high-quality, structured initial data. Then, apply ML to build predictive models from this data, which can then inform the next, more refined, round of experimental design. This synergistic approach is a powerful future direction for the field [15] [22].
Core Mechanisms: How Host Factors Influence Biomaterial Response
FAQ: Why do age and sex cause variability in host responses to biomaterials?
Biological sex and age are significant sources of variability in immune responses, which directly influence how a host reacts to an implanted biomaterial. These factors affect cytokine production, immune cell populations, and the overall inflammatory environment [23].
- Sex-Based Differences: Females typically mount stronger innate and adaptive immune responses than males. This includes higher antibody responses, interferon activity, and T cell numbers. This can make females more susceptible to autoimmune diseases but also leads to more robust responses to biomaterials, vaccines, and infections [23] [24].
- Age-Based Differences: Aging is associated with immunosenescence, which includes a decline in naive T cells and dysregulation of the tissue microenvironment. Older individuals often exhibit delayed macrophage recruitment and altered proinflammatory profiles following implantation [23].
- The Estrogen Paradox: In some diseases, such as pulmonary arterial hypertension (PAH), sex hormones create a complex phenomenon. For example, estrogen may contribute to increased disease susceptibility in females while also conferring a survival advantage, a situation that can be modeled using advanced biomaterial systems [25].
FAQ: What is the clinical evidence that these factors matter?
Numerous clinical and pre-clinical observations confirm the critical role of host factors. For instance, the immune response to six common biomaterials (e.g., agarose, alginate, chitosan, CMC, GelMA, and collagen) showed clear sex and age-related heterogeneity in transcriptomic profiles after blood contact [23]. Furthermore, in respiratory diseases like PAH, a clear sexual dimorphism exists, with females being four times more likely to be diagnosed but having better survival rates than males [25].
Troubleshooting Guides for Common Experimental Challenges
Challenge: Inconsistent Cell Activation in Response to Biomaterial Stiffness
Problem: When studying fibroblast activation on hydrogels of varying stiffness, results are inconsistent and not reproducible.
Solution: Consider the sex of the cell source and the composition of the serum used in your culture media.
- Step 1: Report Cell Sex. Always note the biological sex of the primary cells used. Male and female human pulmonary arterial adventitial fibroblasts (hPAAFs) respond differently to identical mechanical cues [25].
- Step 2: Standardize Serum Source. Fetal Bovine Serum (FBS) has batch-to-batch variability and undefined levels of sex hormones. For greater consistency, use human serum pooled by sex and age.
- Example: Female hPAAFs showed a stiffness-dependent activation profile only when cultured in younger female serum (from donors <50 years old) or when older female serum was supplemented with estradiol. Male hPAAFs, however, responded to stiffness increases regardless of serum composition [25].
- Step 3: Use Dynamic Biomaterials. Employ biomaterials that can mimic disease progression, such as dynamically stiffening PEGαMA hydrogels, to model how cells respond to changes in their mechanical environment [25].
Challenge: Unpredictable Immune Reactions to Implanted Biomaterials
Problem: An implant elicits a highly variable immune response (e.g., severe inflammation or fibrosis) across a test population.
Solution: Stratify test subjects by age and sex during pre-clinical evaluation and select biomaterial type based on the desired immune response.
- Step 1: Pre-screen Biomaterial Immunogenicity. Use an ex vivo human whole blood incubation model to profile the immune response to different biomaterials across donors of different ages and sexes [23].
- Step 2: Select Biomaterials by Immune Profile. Research shows that biomaterial ingredients elicit specific immune responses. For example:
- Step 3: Incorporate Immune Modulators. Engineer biomaterials to release immunomodulatory factors, such as anti-inflammatory cytokines, to promote a tolerogenic immune response and mitigate adverse reactions [26].
Key Experimental Protocols
Detailed Protocol: Ex Vivo Analysis of Blood-Biomaterial Interactions
This protocol, adapted from a 2021 study, details how to profile the immuno-biocompatibility of a biomaterial while accounting for donor age and sex [23].
1. Blood Collection and Preparation:
- Collect venous blood from healthy human volunteers, stratified into age/sex groups (e.g., young group: 20-39 years old; elderly group: 40-59 years old). Include at least 5 males and 5 females per group.
- Use anticoagulants like sodium citrate or EDTA. Keep samples at room temperature and process within 2 hours.
2. Biomaterial Coating:
- Prepare biomaterial solutions (e.g., 0.5% w/w in appropriate solvents).
- Coat well plates with 100 µL of each solution and allow them to dry under sterile conditions.
3. Whole Blood Incubation:
- Add 1 mL of fresh whole blood to each coated well.
- Incubate for 4-6 hours at 37°C with 5% CO₂.
4. RNA Sequencing and Analysis:
- Collect blood post-incubation for RNA extraction.
- Perform RNA-seq and subsequent bioinformatic analysis (e.g., PCA, differential gene expression, leukocyte profiling) to identify ingredient-, sex-, and age-specific immune signatures.
Detailed Protocol: Testing Cell Response to Dynamic Stiffening
This protocol describes a method to study sex-specific fibroblast activation in response to microenvironment stiffening, mimicking disease progression [25].
1. PEGαMA Hydrogel Synthesis and Fabrication:
- Synthesize PEGαMA from 8-arm PEG-OH and ethyl 2-(bromomethyl)acrylate.
- Fabricate soft hydrogels (~1-5 kPa) that replicate healthy tissue stiffness using photopolymerization.
2. Cell Seeding and Culture:
- Seed male and female human pulmonary arterial adventitial fibroblasts (hPAAFs) onto the soft hydrogels.
- Culture cells in media supplemented with defined sera (e.g., FBS, or human serum pooled by sex and age).
3. Dynamic Stiffening:
- After cell adhesion, perform a secondary photopolymerization reaction to stiffen the hydrogel to a modulus exceeding 10 kPa, mimicking diseased tissue.
4. Analysis of Fibroblast Activation:
- Quantify activation by measuring the expression and organization of alpha-smooth muscle action (αSMA) via immunostaining and image analysis.
- Compare activation levels between male and female cells on soft vs. stiffened substrates under different serum conditions.
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential Research Reagents for Studying Host Factor Variability
| Reagent / Material | Function / Relevance | Example Application / Note |
|---|---|---|
| PEGαMA (Poly(ethylene glycol)-alpha methacrylate) | Forms dynamically stiffening hydrogels. | Allows in vitro mimicking of progressive tissue stiffening, as seen in fibrotic diseases [25]. |
| Human Serum (Sex & Age Pooled) | Physiologically relevant culture supplement. | Reveals sex-specific cell responses; superior to FBS which has undefined hormones [25] [23]. |
| Primary Cells (with defined sex) | Biologically relevant model system. | Using cells from both sexes is critical, as responses can be opposite [25] [24]. |
| RNA-Sequencing | Transcriptomic profiling tool. | Identifies genome-wide, sex- and age-specific host responses to biomaterials [23]. |
| Collagen & GelMA | Protein-based biomaterials. | Known to upregulate NKT cell pathways and activate adaptive immunity [26] [23]. |
| Chitosan & Alginate | Polysaccharide-based biomaterials. | Tend to induce stronger innate inflammatory responses [26] [23]. |
| Pyralomicin 1b | Pyralomicin 1b, MF:C20H19Cl2NO7, MW:456.3 g/mol | Chemical Reagent |
| Methotrexate Hydrate | Methotrexate Hydrate, MF:C20H24N8O6, MW:472.5 g/mol | Chemical Reagent |
Table 2: Summary of Sex-Biased Immune Responses to Pathogens in Humans [24]
| Pathogen Type | Pathogen Example | Observed Sex Bias | Notes |
|---|---|---|---|
| Virus | Hepatitis B & C (HBV, HCV) | Higher prevalence & severity in males | [24] |
| Virus | Herpes Simplex Virus (HSV1/2) | Higher prevalence in females | [24] |
| Virus | HIV-1 | Female-biased transmission (Male-to-female) | Varies with regional socioeconomic factors [24] |
| Bacteria | Helicobacter pylori | Higher infection rate in males | [24] |
| Bacteria | Borrelia burgdorferi (Lyme) | Initial infection higher in males; reinfection higher in females | [24] |
| Parasite | Leishmania spp. (Visceral) | Higher susceptibility in males | [24] |
| Fungus | Cryptococcus spp. | Higher disease incidence in males | Observed in both HIV+ and HIV- cohorts [24] |
Table 3: Age and Sex-Based Transcriptomic Responses to Biomaterials [23]
| Biomaterial Category | Example Materials | Key Immune Findings | Impact of Age & Sex |
|---|---|---|---|
| Polysaccharide-based | Chitosan, Alginate, Agarose, CMC | Induced strong innate immune responses. | Significant age-related differences were observed. |
| Protein-based | GelMA, Collagen Type I | Upregulated NKT cell pathway and adaptive immune responses. | Showed fewer differences by sex and age compared to polysaccharides. |
Signaling Pathways and Experimental Workflows
Diagram 1: Host Factor Impact Pathway
Diagram 2: Ex Vivo Blood Test Workflow
Troubleshooting Guides
Troubleshooting Inherent Differentiation Biases
Problem: Unexpected lineage specification despite defined soluble factors.
- Potential Cause: The mechanical properties (stiffness) of your culture substrate are biasing stem cell fate.
- Solution: Match substrate stiffness to your target tissue. For example, use soft substrates (~0.2 kPa) to promote neurogenic or adipogenic outcomes, and stiffer substrates (10-100 kPa) to promote osteogenic outcomes [27]. Utilize polyacrylamide or polydimethylsiloxane (PDMS) hydrogels with tunable elastic moduli for precise control.
- Potential Cause: The surface topography or geometry is providing conflicting cues.
- Solution: Employ microgrooved or nanogrooved substrates to guide cell alignment and fate. For enhanced osteogenic differentiation of human adipose stem cells (hASCs), consider using titanium dioxide (TiOâ‚‚) nanotubes with 70 nm grooves [28].
- Potential Cause: The cell adhesion ligand density is insufficient or inappropriate, failing to support necessary integrin signaling.
- Solution: Optimize the surface density of adhesion peptides like RGD. Ensure a sufficient density of GRGDSP to support cell adhesion and potentiate growth factor signaling [29].
Problem: Low efficiency of directed differentiation towards a target cell type.
- Potential Cause: The culture system does not support biologically driven assembly or proper morphogenesis.
- Solution: For tissues requiring complex 3D architecture, use 3D culture systems like embryoid bodies (EBs). Precisely control the size and shape of cell aggregates, as EB size critically influences lineage specification [29].
- Potential Cause: Lack of synergy between adhesive cues and soluble morphogenic cues.
- Solution: Co-present cell adhesion ligands (e.g., RGD) with specific growth factor receptor-binding peptides (e.g., BMP-receptor binding peptide) on your material surface to create synergistic signaling contexts [29].
Troubleshooting Epigenetic Memory
Problem: Induced pluripotent stem cells (iPSCs) exhibit a differentiation bias towards their cell type of origin.
- Potential Cause: Incomplete epigenetic reprogramming, leaving residual tissue-specific DNA methylation signatures [30].
- Solution:
- Serial Reprogramming: Differentiate the iPSCs and then reprogram them again.
- Chromatin-Modifying Drugs: Treat iPSCs with drugs like histone deacetylase (HDAC) inhibitors or DNA methyltransferase inhibitors to reset the epigenetic landscape [30].
- Extended Culture: Culture iPSCs for extended passages (e.g., beyond passage 6) to allow for gradual erosion of the epigenetic memory.
- Solution:
Problem: Primary cells lose their phenotype after 2D expansion prior to 3D culture.
- Potential Cause: Cells have developed a "mechanical memory" of the stiff 2D culture substrate, which is maintained through epigenetic modifications like H3K9me3, locking them in a de-differentiated state [31].
- Solution:
- Limit Expansion: Keep 2D expansion phases as short as possible. For chondrocytes, recovery is possible after 8 population doublings but is lost after 16 [31].
- Epigenetic Disruption: Use inhibitors of epigenetic modifiers during or after expansion to disrupt the unfavorable mechanical memory. Suppressing or increasing H3K9me3 levels can help partially restore the native chromatin architecture [31].
- Use Soft Substrates: Culture cells on substrates that mimic the stiffness of their native tissue environment during expansion to prevent the acquisition of a non-physiological mechanical memory.
- Solution:
Problem: Unstable cell phenotype after transfer from a synthetic material to a 3D hydrogel.
- Potential Cause: The material-induced epigenetic state is not maintained in the new environment.
- Solution: Pre-condition cells on a material that promotes a transcriptionally active chromatin state (euchromatin) for the desired lineage. Cells cultured on micropatterned, flexible substrates show increased histone acetylation and decreased HDAC activity, which may prime them for differentiation [28] [27].
Frequently Asked Questions (FAQs)
Q1: What is "inherent differentiation bias" in the context of stem cell-material interactions? A1: Inherent differentiation bias refers to the tendency of stem cells to preferentially differentiate into certain lineages based on physical and chemical cues from the material they are cultured on, independent of soluble factors. This includes biases imposed by substrate stiffness, topography, and ligand presentation. For example, mesenchymal stem cells (MSCs) cultured on stiff substrates (100 kPa) produce a secretome that promotes their own proliferation, while those on soft substrates (0.2 kPa) produce a secretome that promotes osteogenesis and adipogenesis [32]. Similarly, iPSCs can retain an "epigenetic memory" of their tissue of origin, making them differentiate more efficiently into related lineages [30].
Q2: How do material cues lead to long-term epigenetic memory? A2: Material cues are transduced from the extracellular matrix, through the cytoskeleton, and directly to the nucleus via structures like the LINC complex. This force transmission can alter chromatin architecture by modifying histones (e.g., acetylation, methylation) and DNA methylation. These epigenetic marks can be maintained over multiple cell divisions, creating a memory of the initial mechanical environment. For instance, prolonged 2D culture on stiff plastic increases H3K9me3 levels, a repressive mark, which suppresses the native chondrocyte phenotype even after the cells are moved to a 3D soft hydrogel [27] [31].
Q3: My differentiation protocol is highly variable. Which material properties should I control first? A3: To reduce variability, prioritize standardizing these three material properties, as they are potent regulators of cell fate:
- Stiffness (Elastic Modulus): Use hydrogels to precisely mimic the stiffness of your target tissue.
- Topography: Introduce controlled micro- or nano-scale patterns to guide cell shape and differentiation.
- Ligand Density: Use well-defined chemistries to present a consistent density of cell adhesion peptides (e.g., RGD) across experimental batches.
Q4: Can I erase an undesirable mechanical memory in my cells? A4: Yes, emerging strategies involve using small molecule inhibitors targeting epigenetic enzymes like HDACs or histone methyltransferases/demethylases. Treating cells with these inhibitors can disrupt the established chromatin state, effectively "erasing" the mechanical memory and making cells more receptive to new differentiation cues [31] [30].
Q5: Why should I consider using 3D cultures over 2D systems? A5: 3D cultures more faithfully recapitulate the complex and dynamic signaling present during natural morphogenesis. They allow for "biologically driven assembly," where stem cells self-organize into higher-order structures with minimal external patterning cues. The 3D context also provides more physiologically relevant mechanical and spatial signals that can reduce aberrant epigenetic memory and improve differentiation efficiency [29] [33].
Data Presentation
Table 1: Impact of Substrate Stiffness on MSC Paracrine Activity and Differentiation
| Substrate Stiffness | Secretome Effect on MSC Proliferation | Secretome Effect on MSC Differentiation | Effect on Macrophage Phagocytosis | Effect on Angiogenesis | Key Secretory Factors |
|---|---|---|---|---|---|
| 0.2 kPa (Soft) | No promotion | Promotes osteogenesis and adipogenesis | Most beneficial effects | Promotes | Elevated IL-6 [32] |
| 100 kPa (Stiff) | Boosts proliferation | No promotion | Less beneficial effects | Less beneficial | Elevated OPG, TIMP-2, MCP-1, sTNFR1 [32] |
Table 2: Epigenetic Modifications Induced by Material Cues
| Material Cue | Cell Type | Observed Epigenetic Change | Functional Outcome |
|---|---|---|---|
| Micropatterned/ Flexible Substrates [28] [27] | Mesenchymal Stem Cells (MSCs) | ↑ Histone H3 acetylation, ↓ HDAC activity | Increased gene transcription; Enhanced reprogramming and differentiation |
| TiO₂ Nanogrooves [28] | Human Adipose Stem Cells (hASCs) | ↑ H3K4 trimethylation, inhibition of demethylase RBP2 | Promotion of osteogenic differentiation |
| Prolonged 2D Culture (Stiff Substrate) [31] | Primary Chondrocytes | ↑ H3K9me3 (repressive mark) | Loss of chondrocyte phenotype; Mechanical memory |
| Nanotopographical Substrates [28] | Embryonic Stem Cells (ESCs) | Altered DNA methylation in regions related to MSCs and osteogenic progenitors | Influence on early cell fate decisions |
Experimental Protocols
Protocol 1: Assessing Epigenetic Memory via Chondrocyte Re-differentiation
Purpose: To evaluate the persistence of mechanical memory after 2D expansion by measuring the recovery of the chondrocyte phenotype in a 3D hydrogel [31].
- 2D Expansion: Expand primary chondrocytes on standard tissue culture plastic (TCP) for a defined number of population doublings (PDs). For example, use 8 PDs (recoverable memory) and 16 PDs (long-term memory) as critical time points.
- 3D Encapsulation: Harvest the expanded cells and encapsulate them in a soft, chondropermissive 3D hydrogel (e.g., agarose or a soft PEG-based hydrogel at a stiffness of ~2-5 kPa).
- Culture: Maintain constructs in a defined chondrogenic medium (e.g., with TGF-β3) for 14-21 days.
- Analysis:
- Gene Expression: Quantify expression of chondrogenic genes (e.g., ACAN, COL2A1, SOX9) via qRT-PCR. Compare to freshly isolated chondrocytes and a no-expansion control.
- Histology: Process constructs for histology and stain for sulfated glycosaminoglycans (sGAG) with Alcian Blue or Safranin-O.
- Epigenetic Analysis: Perform immunostaining or ChIP-qPCR for H3K9me3 on the 2D-expanded cells and recovered 3D constructs to correlate phenotype with chromatin state.
Protocol 2: Testing Synergy between Adhesion and Growth Factor Cues
Purpose: To investigate the combined effect of cell adhesion ligand density and a tethered growth factor peptide on stem cell fate [29].
- Surface Functionalization: Prepare self-assembled monolayers (SAMs) or a similar platform with varying densities of the cell adhesion peptide GRGDSP (e.g., 0, low, medium, high density).
- Combinatorial Presentation: On each adhesion density background, co-present a fixed density of a specific growth factor receptor-binding peptide, such as a BMP-receptor binding peptide (BR-BP).
- Cell Seeding and Culture: Seed human Mesenchymal Stem Cells (hMSCs) onto the functionalized surfaces. Culture in a basal medium without exogenous BMP-2 to isolate the effect of the tethered cues.
- Analysis:
- Morphology: Quantify cell spreading and surface coverage after 24 hours.
- Differentiation: After 7-14 days, assess early osteogenic differentiation by staining for alkaline phosphatase (ALP) activity and quantifying expression of osteogenic genes (e.g., Runx2, Osteocalcin).
Signaling Pathway and Experimental Workflow Visualizations
Diagram 1: Mechano-Epigenetic Signaling Pathway
Diagram Title: Material Cues to Epigenetic Change Pathway
Diagram 2: Mechanical Memory Experiment Workflow
Diagram Title: Mechanical Memory Testing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Studying Stem Cell-Material Interactions
| Reagent / Material | Function / Property | Application Example |
|---|---|---|
| Polyacrylamide Hydrogels [32] [27] | Tunable elastic modulus (0.1 kPa to 100+ kPa); can be functionalized with adhesion ligands. | Studying the effect of substrate stiffness on stem cell differentiation and paracrine activity. |
| Polydimethylsiloxane (PDMS) [28] | Flexible polymer; can be molded with microgrooves; gas-permeable. | Creating micropatterned substrates to study effects of topography and strain on histone acetylation. |
| RGD Peptide [29] | Synthetic peptide containing Arg-Gly-Asp sequence; binds to cell surface integrins. | Functionalizing synthetic materials to enable specific cell adhesion and study integrin-mediated signaling. |
| Titanium Dioxide (TiOâ‚‚) Nanotubes [28] | Nanoscale topography (e.g., 70 nm grooves); bioactive. | Promoting osteogenic differentiation of human adipose-derived stem cells (hASCs). |
| Thermoresponsive Hydrogels (e.g., Poly(N-isopropylacrylamide)) [28] | Allows for gentle cell harvest by lowering temperature without enzymatic digestion. | Harvesting cells while preserving their epigenetic state and mechanical memory for downstream analysis. |
| Histone Deacetylase (HDAC) Inhibitors (e.g., Valproic Acid, Trichostatin A) [30] | Small molecules that increase global histone acetylation by inhibiting deacetylases. | Resetting epigenetic memory in iPSCs or disrupting unfavorable mechanical memory. |
| Rhodirubin B | Rhodirubin B, MF:C42H55NO15, MW:813.9 g/mol | Chemical Reagent |
| Pgla tfa | Pgla tfa, MF:C90H163F3N26O24S, MW:2082.5 g/mol | Chemical Reagent |
Engineering Solutions: From 'Bottom-Up' Design to Integrin-Targeting and AI
Frequently Asked Questions (FAQs)
Q1: What exactly is the "bottom-up" biomaterial design paradigm, and how does it differ from traditional approaches?
The bottom-up biomaterial design paradigm is a strategic framework that starts by first understanding the fundamental biological properties and microenvironmental needs of specific cells, and then engineering cell-instructive biomaterials from the molecular level upward to support them [34]. This approach fundamentally shifts away from conventional methods that often try to adapt cells to pre-existing, off-the-shelf materials. Instead, it prioritizes designing biomaterials that are tailored to address key biological challenges such as differentiation variability, functional maturity of derived cells, and the survival of therapeutic cell populations in hostile microenvironments [34]. By replicating lineage-specific mechanical, chemical, and spatial cues, these tailored biomaterials enhance differentiation fidelity, reprogramming efficiency, and functional integration.
Q2: My biomaterial implant is triggering a strong foreign body response and fibrosis. How can a bottom-up approach help mitigate this?
A bottom-up approach addresses this by actively designing materials to modulate the immune response, rather than just being passive scaffolds. This involves several key strategies informed by the principles of the paradigm [35] [36]:
- Immune-Instructive Surfaces: Modifying surface properties like roughness, topography, and chemistry can significantly influence immune cell interactions. For example, specific nanopatterning can reduce the foreign body reaction and improve integration [36].
- Controlled Release of Immunomodulators: Biomaterials can be engineered to release bioactive molecules that actively shape the immune environment. For instance, releasing agents that promote a shift in macrophage phenotype from pro-inflammatory (M1) to anti-inflammatory and pro-regenerative (M2) can reduce chronic inflammation and fibrosis [35].
- Mechanical Property Matching: The stiffness and elasticity of the biomaterial should match the target tissue. Softer materials that mimic the brain's mechanical properties, for example, have been shown to lead to a reduced inflammatory reaction [36].
Q3: I am working with induced pluripotent stem cells (iPSCs). How can this paradigm help with issues like inconsistent differentiation and tumorigenic risk?
The bottom-up paradigm directly tackles these challenges by creating engineered microenvironments that provide precise control over stem cell fate [34] [37].
- Overcoming Epigenetic Memory: iPSCs can retain a "memory" of their original cell type, which can bias differentiation. A bottom-up design uses tailored biomaterial cues—such as specific adhesion ligands, controlled stiffness, and spatial patterning—to more robustly guide cells toward the desired lineage, overcoming this inherent bias [34].
- Ensuring Functional Maturity and Safety: By replicating critical aspects of the native stem cell niche, these biomaterials promote more complete differentiation and functional maturation of derived cells. This reduces the risk of residual undifferentiated pluripotent cells persisting and forming teratomas [34]. Using defined, biomaterial-based systems also avoids the variability and xenogeneic risks associated with tumor-derived matrices like Matrigel [33].
Q4: What are some key material properties I should prioritize when designing a bottom-up biomaterial for neural regeneration?
For neural applications, the biomaterial should mimic the delicate and complex environment of the nervous system. Key properties to prioritize include [37]:
- Electrical Conductivity: Using conductive polymers like polypyrrole, polythiophene, and polyaniline can help neurites grow and enhance cellular activity by facilitating the transmission of electrical impulses crucial for nerve signaling.
- Mechanical Compatibility: Neural tissue is soft. The scaffold should be malleable, flexible, and structurally sound to match the mechanical properties of the brain without causing compression or irritation.
- Biocompatibility and Surface Erodibility: Materials like polyglycerol sebacate (PGS) are beneficial because they are surface-erodible and elastomeric, providing consistent contact-guidance for nerve regeneration over time.
- Support for 3D Growth: The material should facilitate the creation of a porous, three-dimensional structure that supports axonal ingrowth and cell infiltration.
Troubleshooting Guides
Problem 1: Inconsistent Cell Differentiation Outcomes in 3D Biomaterial Scaffolds
A core promise of the bottom-up paradigm is controlling cell fate, but variability in differentiation can still occur.
Step 1: Identify the Problem Confirm that differentiation is inconsistent across multiple batches of scaffolds and with different cell donors, not just a one-time experimental error.
Step 2: List Possible Explanations
- Inhomogeneous Scaffold Properties: Variability in porosity, stiffness, or ligand distribution within the scaffold.
- Improper Biochemical Cue Presentation: Inconsistent concentration, stability, or spatial distribution of growth factors or adhesion peptides.
- Inadequate Mass Transport: Poor diffusion of nutrients, oxygen, or signaling molecules to cells in the scaffold's core.
- Cell-Seeding Inconsistency: Uneven cell distribution or varying initial cell viability.
Step 3: Collect Data & Experimentation
- For Explanation 1: Characterize scaffold uniformity using scanning electron microscopy (SEM) to assess pore structure and use atomic force microscopy (AFM) to map mechanical properties across different regions of the scaffold.
- For Explanation 2: Use immunofluorescence to check the spatial distribution of key biofunctionalized ligands (e.g., RGD peptides). Employ ELISA assays to quantify the release kinetics of loaded growth factors from multiple scaffold batches.
- For Explanation 3: Section the scaffold and perform live/dead staining to see if cell death is localized to the interior, indicating diffusion limitations.
Step 4: Implement the Fix Based on the data, potential fixes include:
- Optimizing fabrication parameters (e.g., electrospinning, 3D bioprinting) for greater consistency.
- Using dual-crosslinking or different biofunctionalization strategies to ensure uniform and stable cue presentation.
- Incorporating sacrificial materials or channels during fabrication to create vascular-like networks for improved perfusion.
Problem 2: Uncontrolled or Mismatched Biomaterial Degradation
The degradation profile of a biomaterial is critical for its success and must match the rate of new tissue formation.
Step 1: Identify the Problem Observe either a complete loss of structural integrity too early, a persistent implant that hinders tissue remodeling, or an inflammatory reaction to degradation products.
Step 2: List Possible Explanations
- Bulk Erosion vs. Surface Erosion: Bulk-eroding polymers (e.g., PLGA) can lead to sudden collapse and acidic byproduct accumulation, while surface erosion offers more controlled degradation.
- Enzyme-Mediated Degradation: Overexpression of specific enzymes (e.g., MMPs) at the implant site can cause unexpectedly rapid degradation.
- Material Crystallinity and MW: Higher crystallinity and molecular weight generally slow down degradation.
Step 3: Collect Data & Experimentation
- Perform in vitro degradation studies in PBS and in enzyme solutions (e.g., collagenase for natural polymers) to track mass loss, molecular weight change, and pH shift over time.
- Analyze the mechanical properties (e.g., compressive modulus) of the scaffold weekly to correlate degradation with function loss.
Step 4: Implement the Fix
- Switch to a surface-eroding polymer (e.g., polyanhydrides) or blend polymers to fine-tune the degradation profile.
- Design the material to be enzyme-responsive, so degradation is directly linked to cell-mediated remodeling activities [35]. For example, incorporate MMP-cleavable crosslinkers.
- Adjust the crystallinity and initial molecular weight during polymer synthesis.
Key Biomaterial Properties and Their Design Considerations
Table 1: Key properties for bottom-up biomaterial design and their impact on biological response.
| Property | Goal in Bottom-Up Design | Technical Considerations |
|---|---|---|
| Mechanical Stiffness | Match target tissue to direct stem cell lineage and reduce foreign body response [8] [36]. | Tune polymer crosslinking density, polymer concentration, or composite with ceramics. Softer materials (~0.1-1 kPa) for brain, stiffer (~10-30 kPa) for bone. |
| Biodegradation Rate | Synchronize with new tissue formation rate to provide temporary, supportive niche. | Choose between surface-eroding (e.g., PGS [37]) or bulk-eroding (e.g., PLGA) polymers. Incorporate enzyme-sensitive linkages. |
| Bioactivity | Present specific biochemical cues to instruct cell adhesion, proliferation, and differentiation. | Functionalize with adhesion peptides (e.g., RGD [8]), incorporate glycosaminoglycan mimetics, or create systems for controlled release of growth factors. |
| Immunomodulation | Actively shape a pro-regenerative immune microenvironment [35] [36]. | Modify surface topography/chemistry; incorporate controlled release of cytokines (e.g., IL-4) or drugs to promote M2 macrophage polarization. |
| Electrical Conductivity | Support excitable tissues like nerve and muscle by facilitating electrical signal propagation [37]. | Use conductive polymers (e.g., polypyrrole), or incorporate graphene/carbon nanotubes into insulating biodegradable polymers. |
Experimental Protocols for Key Analyses
Protocol 1: Assessing Integrin-Mediated Signaling in Cells on Engineered Surfaces
Purpose: To verify that your biomaterial is successfully engaging specific integrin receptors to activate pro-regenerative intracellular signaling pathways, a core principle of bottom-up design [8].
Materials:
- Biomaterial scaffold or 2D film
- Relevant cell type (e.g., mesenchymal stem cells, fibroblasts)
- Antibodies for immunofluorescence: anti-integrin (e.g., β1 subunit), anti-phospho-FAK (Tyr397), anti-vinculin, and corresponding fluorescent secondary antibodies
- Cell culture reagents
- Confocal microscope
Method:
- Cell Seeding: Seed cells at a sub-confluent density onto the biomaterial test substrate and a control substrate (e.g., tissue culture plastic).
- Fixation and Permeabilization: After 4-24 hours, rinse cells with PBS and fix with 4% paraformaldehyde for 15 minutes. Permeabilize with 0.1% Triton X-100 for 5 minutes.
- Immunostaining: Block with 1% BSA for 1 hour. Incubate with primary antibodies (diluted in blocking buffer) overnight at 4°C. Wash and incubate with secondary antibodies for 1 hour at room temperature. Use phalloidin to stain F-actin and DAPI for nuclei.
- Imaging and Analysis: Image using a confocal microscope. Analyze for:
- Focal Adhesion Formation: Look for co-localization of vinculin and phospho-FAK with the ends of F-actin stress fibers.
- Integrin Clustering: Assess the presence and size of integrin clusters at the cell-material interface.
- Signal Activation: Compare the intensity and distribution of phospho-FAK staining between test and control materials, indicating activation of downstream signaling.
Protocol 2: Quantifying Macrophage Polarization in Response to an Immunomodulatory Biomaterial
Purpose: To determine if your biomaterial can actively modulate the host immune response by driving macrophages toward a pro-regenerative (M2) phenotype, a key strategy for overcoming variability in host responses [35] [36].
Materials:
- Biomaterial sample (sterile)
- Primary human or murine macrophages (e.g., THP-1-derived macrophages)
- Cell culture media
- LPS (for M1 polarization control), IL-4 (for M2 polarization control)
- RNA extraction kit, qPCR reagents
- Antibodies for flow cytometry: anti-CD86 (M1 marker), anti-CD206 (M2 marker)
Method:
- Macrophage Culture and Stimulation: Differentiate and seed macrophages onto the biomaterial and control surfaces. Include control groups stimulated with LPS (M1) and IL-4 (M2).
- Gene Expression Analysis (qPCR): After 24-48 hours, extract total RNA. Perform qPCR to analyze the expression of:
- M1 markers: TNF-α, iNOS (NOS2), IL-1β
- M2 markers: ARG1, CD206 (MRC1), IL-10
- Normalize to housekeeping genes (e.g., GAPDH). A shift toward M2 marker expression on the test biomaterial indicates successful immunomodulation.
- Surface Marker Analysis (Flow Cytometry): Harvest cells from the biomaterial surface (using gentle scraping or enzymatic digestion). Stain cells with fluorescently-labeled antibodies against CD86 and CD206. Analyze using flow cytometry to quantify the percentage of cells in M1 vs. M2 states.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key reagents and materials for bottom-up biomaterial research.
| Item | Function in Bottom-Up Design | Example Applications |
|---|---|---|
| RGD Peptide | A key integrin-binding peptide used to biofunctionalize materials and promote specific cell adhesion [8]. | Enhancing osteogenic differentiation on bone scaffolds; improving endothelial cell attachment on vascular grafts. |
| Matrix Metalloproteinase (MMP)-Cleavable Peptide Crosslinker | Creates enzyme-responsive materials that degrade in response to cell-secreted enzymes, facilitating cell migration and tissue remodeling [35]. | Designing injectable hydrogels for 3D cell culture; creating scaffolds that allow patient-specific invasion rates. |
| Conductive Polymers (e.g., Polypyrrole) | Provides electrical conductivity to biomaterials, supporting the function of electrically excitable tissues [37]. | Nerve guidance conduits; cardiac patches for myocardial infarction. |
| Hyaluronic Acid (HA) | A natural glycosaminoglycan that can be chemically modified to create hydrogels that mimic the native extracellular matrix. | Liver organoid culture [33]; wound healing dressings. |
| Polycaprolactone (PCL) | A synthetic, biodegradable polymer known for its good mechanical properties and slow degradation rate. Often used in composites. | Electrospun scaffolds for bone and neural tissue engineering [37]. |
| Endophenazine C | Endophenazine C, MF:C25H28N2O7, MW:468.5 g/mol | Chemical Reagent |
| Yadanzioside L | Yadanzioside L, MF:C34H46O17, MW:726.7 g/mol | Chemical Reagent |
Key Signaling Pathways and Experimental Workflows
Integrin Signaling Pathway
Troubleshooting Workflow
Harnessing Integrin-Targeting Motifs to Direct Cell Fate and Enhance Integration
Integrins, a superfamily of heterodimeric transmembrane adhesion receptors, serve as fundamental mediators of bidirectional communication between cells and their extracellular matrix (ECM). These receptors, composed of α and β subunits that form 24 unique combinations in humans, recognize specific ECM components and orchestrate essential cellular processes including adhesion, migration, proliferation, differentiation, and survival [38] [39] [40]. The dynamic interplay between integrins and their ligands forms the molecular foundation for tissue development, homeostasis, and regeneration, establishing them as prime targets for therapeutic intervention in regenerative medicine [8] [40].
The central premise of harnessing integrin-targeting motifs lies in their ability to precisely direct cell fate and enhance biomaterial integration by recapitulating key aspects of native ECM signaling. Specific recognition motifs, particularly the Arg-Gly-Asp (RGD) sequence found in numerous ECM proteins, demonstrate high binding affinity for several integrins, including αvβ3, αvβ5, αvβ6, αvβ8, and α5β1 [39] [41]. This specific binding capability provides a powerful tool for engineering biomaterials that can actively instruct cellular behavior rather than merely serving as passive scaffolds [8].
Within the context of overcoming variability in biomaterial host responses, integrin-targeting strategies offer promising approaches to enhance signaling specificity and reduce unpredictable outcomes. By precisely controlling integrin engagement through engineered motifs, researchers can potentially direct more consistent cellular responses, improve biomaterial integration, and ultimately achieve more predictable therapeutic outcomes in regenerative medicine applications [8] [40].
Technical Troubleshooting Guide: Common Experimental Challenges
Biomaterial-Cell Interaction Issues
Problem: Poor cell adhesion to engineered biomaterials Solution: Optimize integrin-binding motif presentation
- Verify motif density: Use quantitative methods (e.g., ELISA, fluorescence tagging) to confirm RGD surface concentration. Optimal density typically ranges from 1-10 fmol/cm² but requires empirical determination for specific cell types [8] [41].
- Check spatial arrangement: Ensure motifs are accessible, not sterically hindered by polymer chains. Incorporate flexible linkers (e.g., PEG spacers) of appropriate length (typically 3.5-13 nm) to enhance accessibility [8].
- Confirm motif orientation: Use chemoselective conjugation strategies (e.g., click chemistry, maleimide-thiol) rather than random conjugation to control ligand orientation [8].
- Validate integrin specificity: Include control surfaces with scrambled peptide sequences (e.g., RGE) to distinguish specific integrin-mediated adhesion from non-specific binding [39].
Problem: Inconsistent differentiation outcomes across experimental replicates Solution: Standardize integrin signaling pathway activation
- Characterize integrin expression profile: Perform flow cytometry to identify which integrin subunits (αv, β1, β3, β5, etc.) your target cell population expresses before designing biomaterials [38] [40].
- Control substrate mechanics: Match biomaterial stiffness to target tissue physiology (e.g., ~0.1-1 kPa for neural tissue, ~10-30 kPa for mesenchymal precursors, ~25-40 kPa for osteogenic differentiation) [8] [40].
- Modulate co-receptor engagement: Incorporate secondary binding sites (e.g., PHSRN synergic site for α5β1 integrin) alongside primary RGD motifs to enhance signaling specificity [8].
- Monitor pathway activation: Implement standard controls for key downstream effectors (FAK, ERK, AKT) via Western blot to verify consistent integrin signaling across experiments [42] [8].
Biomaterial Performance Challenges
Problem: Unpredictable host immune response to implanted biomaterials Solution: Engineer immunomodulatory integrin engagement
- Select anti-inflammatory integrin ligands: Prioritize motifs that promote M2 macrophage polarization (e.g., laminin-derived peptides engaging α6β1) over those stimulating pro-inflammatory responses [1].
- Control degradation kinetics: Tune biomaterial degradation rates to match tissue ingrowth (days for acute inflammation resolution, weeks for functional integration) to prevent persistent foreign body response [8].
- Incorporate multi-functional motifs: Include integrin-binding sequences known to modulate immune cell activity (e.g., α4β1-binding peptides for lymphocyte regulation) alongside adhesion motifs [40].
- Validate in relevant models: Test materials in systems with competent immune components (e.g., co-cultures with macrophages) rather than solely in simplified cell systems [1].
Problem: Limited functional integration with host tissue Solution: Enhance bidirectional mechanotransduction
- Design dynamic mechanical properties: Develop materials with stress-relaxing behavior that permit cell-mediated remodeling rather than purely elastic substrates [8].
- Incorporate protease-sensitive domains: Include matrix metalloproteinase (MMP)-cleavable sequences to enable cell-directed material degradation and replacement with native ECM [8].
- Implement graded interface design: Create biomaterials with spatially varying integrin ligand density to guide seamless tissue integration at the implant-host interface [8] [40].
- Ensure vascularization support: Include αvβ3 and αvβ5 integrin-binding motifs to promote endothelial cell adhesion and angiogenic signaling for proper nutrient transport [39].
Integrin Signaling Pathways: Mechanisms and Experimental Monitoring
Core Integrin Signaling Cascade
The following diagram illustrates the fundamental signaling pathway activated upon integrin engagement with ECM motifs, highlighting key nodes for experimental monitoring:
Lineage-Specific Integrin Signaling
The diagram below illustrates how integrin signaling directs mesenchymal stem cell fate toward adipogenic, chondrogenic, and osteogenic lineages through distinct pathway activation:
Quantitative Analysis of Integrin Signaling Components
Table 1: Key downstream effectors in integrin-mediated differentiation pathways
| Signaling Component | Adipogenesis | Chondrogenesis | Osteogenesis | Detection Method |
|---|---|---|---|---|
| FAK phosphorylation | Decreased at Tyr397 | Variable | Increased at Tyr397 | Phospho-specific Western blot |
| ERK/MAPK activity | Moderate activation | Strong activation (via Src) | Strong activation | Phospho-ERK ELISA/Western |
| Wnt/β-catenin | Activated (inhibits differentiation) | Not primary pathway | Activated (promotes differentiation) | β-catenin nuclear localization |
| Key transcription factors | PPARγ, CEBPα | SOX9 | RUNX2, OSX | Immunofluorescence, qPCR |
| Characteristic markers | AP2, AdipoQ | Collagen II, Aggrecan | Osteocalcin, Alkaline phosphatase | qPCR, enzymatic assay |
Research Reagent Solutions: Essential Tools for Integrin Research
Table 2: Key research reagents for manipulating and monitoring integrin signaling
| Reagent Category | Specific Examples | Function/Application | Considerations for Use |
|---|---|---|---|
| Integrin-binding peptides | RGD, LDV, PHSRN, IKVAV | Promote specific integrin engagement | Optimize density (1-10 fmol/cm²); include spacer arms |
| Function-blocking antibodies | Anti-β1 (AIIB2), Anti-αvβ3 (LM609), Anti-α5β1 (JBS5) | Inhibit specific integrin function | Verify species cross-reactivity; use IgG isotype controls |
| Activating antibodies | TS2/16 (β1 integrin), AG89 (β3 integrin) | Stimulate integrin signaling | Can induce unphysiological clustering |
| Chemical inhibitors | FAK inhibitor (PF-573228), Src inhibitor (PP2), RGD-based cyclic inhibitors | Block specific signaling nodes | Monitor off-target effects on related kinases |
| Natural ECM controls | Fibronectin, Laminin, Vitronectin, Collagen I/IV | Positive controls for adhesion | Batch variability; use same source across experiments |
| Fluorescent ligands | RGD-Cy5, RGD-FITC, Fibronectin-Alexa conjugates | Quantify binding and internalization | Control for non-specific binding with RGE analogs |
| Integrin expression vectors | α5-GFP, β1-mCherry, dominant-negative constructs | Modulate integrin expression levels | Account for transfection efficiency differences |
Frequently Asked Questions: Expert Solutions
Q1: How do I determine the optimal density of RGD peptides for my specific cell type and application?
A1: The optimal density requires empirical determination but follows these guidelines: Start with a density gradient ranging from 0.1 to 20 fmol/cm². Most cell types show maximal adhesion between 1-10 fmol/cm². For stem cell differentiation, lower densities (1-4 fmol/cm²) often favor maintenance, while higher densities (4-10 fmol/cm²) typically promote differentiation. Always include a negative control (scrambled peptide like RGE) and positive control (fibronectin-coated surface) for validation. Use quantitative methods like radioactive labeling, fluorescence quantification, or ELISA to verify surface density rather than relying on initial conjugation concentrations [8] [41].
Q2: What are the key differences between using short peptide motifs versus full ECM proteins for integrin targeting?
A2: Short peptides (e.g., RGD) offer precise control over integrin engagement, batch-to-batch consistency, and resistance to denaturation, but lack the context of native ECM which presents multiple binding sites simultaneously. Full ECM proteins (e.g., fibronectin) provide physiological complexity and synergistic sites (like PHSRN which enhances α5β1 binding to RGD), but exhibit batch variability and potential pathogen transmission. For reductionist studies of specific integrin functions, peptides are preferable. For applications requiring robust, physiological cell responses, full proteins or engineered multi-domain constructs often perform better [8] [40].
Q3: Why do I sometimes observe different cellular responses to the same integrin-targeting motif on different biomaterial substrates?
A3: Cellular responses depend on the integration of multiple cues beyond just the biochemical motif. Key factors include:
- Substrate stiffness: The same integrin engagement on stiff (>10 kPa) versus soft (<1 kPa) substrates activates different downstream pathways despite identical ligand presentation.
- Ligand mobility: Mobile ligands that permit integrin clustering typically enhance signaling compared to immobilized ligands.
- Topographical cues: Nanoscale patterning of motifs influences integrin clustering and signaling efficacy.
- Co-presented factors: The presence of growth factors or other ECM components dramatically alters integrin signaling outcomes. Always characterize the complete material microenvironment rather than focusing solely on the integrin ligand itself [8] [40].
Q4: How can I specifically target particular integrin heterodimers when many recognize similar motifs?
A4: Several strategies enhance specificity:
- Use constrained cyclic peptides: Cyclic RGDfC shows >10-fold higher specificity for αvβ3 over αvβ5 compared to linear RGD.
- Leverage synergistic sites: The FNIII9-10 fragment containing both RGD and PHSRN specifically engages α5β1 with minimal binding to other RGD-recognizing integrins.
- Employ affinity tuning: Lower-affinity RGD analogs can discriminate between integrins with different binding affinities.
- Utilize spatial patterning: Nanoscale spatial organization of motifs can selectively engage specific integrins based on their clustering requirements. Validate specificity using function-blocking antibodies against specific integrin subunits in adhesion inhibition assays [39] [41].
Q5: What are the best practices for verifying that observed cellular responses are truly integrin-mediated?
A5: Implement a multi-faceted validation approach:
- Inhibition controls: Use function-blocking antibodies against specific integrin subunits or RGD competitive inhibitors to confirm response abrogation.
- Genetic approaches: Employ siRNA/shRNA knockdown of specific integrin subunits or express dominant-negative constructs.
- Signaling validation: Monitor phosphorylation of direct integrin effectors like FAK (Tyr397) and Src family kinases.
- Specificity controls: Always include scrambled peptide controls (e.g., RGE) and validate that mutations in the core motif abolish activity.
- Multiple cell type testing: Confirm expected cell-type-specific responses based on known integrin expression profiles [38] [8] [40].
Advanced Methodologies: Experimental Protocols
Quantitative Biomaterial Functionalization Protocol
This protocol describes a standardized method for conjugating integrin-targeting peptides to biomaterial surfaces with precise density control:
Materials:
- Aminated biomaterial surface (e.g., PLA, PLGA, PEG)
- Sulfo-SMCC crosslinker (Thermo Scientific)
- Thiol-containing RGD peptide (e.g., GCGYGRGDSPG)
- Ellman's reagent for thiol quantification
- Reaction buffer: 0.1 M phosphate, 0.15 M NaCl, 10 mM EDTA, pH 7.2
Procedure:
- Surface activation: Incubate aminated surfaces with 2 mM Sulfo-SMCC in reaction buffer for 1 hour at room temperature with gentle agitation.
- Washing: Rinse surfaces 3× with reaction buffer to remove unreacted crosslinker.
- Peptide conjugation: Incubate with thiol-containing RGD peptide at varying concentrations (0.01-1 mM) for 4 hours at room temperature.
- Quantification: Use Ellman's reagent to measure free thiol concentration before and after conjugation to calculate immobilized peptide density.
- Validation: Verify bioactivity using cell adhesion assays with appropriate controls.
Troubleshooting notes: If conjugation efficiency is low, increase Sulfo-SMCC concentration or extend activation time. If cell response is suboptimal, incorporate a PEG spacer (e.g., MW 3400) between surface and peptide [8] [41].
Integrin Signaling Activation Assay
This protocol provides a standardized approach to monitor integrin pathway activation in response to biomaterial engagement:
Materials:
- Cells of interest (e.g., mesenchymal stem cells)
- Functionalized biomaterials and appropriate controls
- Lysis buffer: RIPA buffer supplemented with protease and phosphatase inhibitors
- Phospho-specific antibodies: anti-FAK (Tyr397), anti-Src (Tyr418), anti-ERK1/2 (Thr202/Tyr204)
- Total protein antibodies for normalization
Procedure:
- Cell seeding: Plate cells on functionalized biomaterials at standardized density (e.g., 10,000 cells/cm²).
- Timing optimization: Conduct time course experiments (15 min to 24 hours) to identify peak phosphorylation times for your specific system.
- Protein extraction: Lyse cells at predetermined time points in ice-cold lysis buffer.
- Western blotting: Separate proteins by SDS-PAGE, transfer to membranes, and probe with phospho-specific antibodies.
- Normalization: Strip and reprobe membranes with total protein antibodies for normalization.
- Quantification: Use densitometry to calculate phosphorylation ratios relative to total protein and control surfaces.
Key considerations: Include both positive (fibronectin-coated) and negative (RGE-functionalized or non-adhesive) controls. Use serum-free conditions during adhesion to isolate integrin-specific signaling from growth factor pathways [42] [8] [40].
Technical Troubleshooting Guide
Inconsistent Material Responsiveness
Problem: Biomaterial fails to respond consistently to intended stimuli in biological environments.
| Potential Cause | Diagnostic Tests | Solution |
|---|---|---|
| Interference from Biofouling | Measure protein adsorption (e.g., using Bradford assay); Analyze surface topography via AFM. | Incorporate anti-fouling polymers (e.g., PEG); Use topography-patterned surfaces. |
| Shielded Stimulus | Measure local pH with microsensors; Quantify local enzyme concentration (ELISA). | Design amplifiers (e.g., enzyme-triggered cascade systems); Use stimuli with deeper tissue penetration (e.g., NIR, US). |
| Inaccurate Trigger Threshold | Characterize material transition point in vitro in simulated physiological conditions. | Re-engineer material chemistry to adjust trigger threshold (e.g., modulate polymer LCST). |
Experimental Protocol: Validating pH-Responsiveness in Simulated Microenvironments
- Prepare Buffer Solutions: Create a series of phosphate-buffered saline (PBS) solutions simulating physiological (pH 7.4), mildly acidic (e.g., pH 6.5-6.8 for tumor microenvironments), and significantly acidic (pH 5.0-5.5 for endosomal compartments) conditions.
- Incubate Material: Place a precise mass (e.g., 10 mg) of the smart biomaterial, such as a pH-sensitive hydrogel nanoparticle, into each buffer solution. Maintain a constant temperature (37°C).
- Monitor Response: At predetermined time points, measure:
- Swelling/Degradation: Gravimetric analysis for hydrogels or dynamic light scattering (DLS) for nanoparticle size change.
- Payload Release: Use UV-Vis spectroscopy or HPLC to quantify the release of a model drug (e.g., doxorubicin) encapsulated within the material.
- Data Analysis: Plot the percentage of swelling, degradation, or drug release against time for each pH. A successful material will show minimal change at pH 7.4 and significant, reproducible changes at target acidic pHs.
Uncontrolled or Burst Release of Therapeutics
Problem: The biomaterial releases its payload too quickly or prematurely, before encountering the target stimulus.
| Potential Cause | Diagnostic Tests | Solution |
|---|---|---|
| Poorly Crosslinked Matrix | Perform swelling ratio studies; Conduct rheology to measure storage (G') and loss (G") moduli. | Optimize crosslinking density; Use dual crosslinking strategies (covalent and ionic). |
| Premature Degradation | Incubate material in serum or relevant biological fluids; Analyze molecular weight change via GPC. | Switch to more stable, hydrolysis-resistant chemical linkers; Add protective surface coatings. |
| Non-Specific Diffusion | Perform drug release studies in non-stimulus conditions (e.g., pH 7.4, no enzyme). | Re-design material with a more stable "shell"; Use prodrugs that require a specific stimulus for activation. |
Experimental Protocol: Assessing Release Kinetics
- Dialysis Tubing Method: Place the drug-loaded biomaterial into a dialysis bag (with an appropriate molecular weight cutoff). Immerse the bag in a large volume of release medium (PBS, pH 7.4) under sink conditions.
- Sampling: At regular intervals, withdraw a small aliquot (e.g., 1 mL) from the external release medium and replace it with fresh pre-warmed buffer.
- Analysis: Quantify the drug concentration in the aliquots using a pre-established calibration curve (UV-Vis, HPLC, or fluorescence).
- Modeling: Fit the cumulative release data to kinetic models (e.g., zero-order, first-order, Higuchi) to understand the release mechanism. A desired sustained release profile will show a slow, controlled release over an extended period.
Inadequate Immune Integration and Foreign Body Response
Problem: The material triggers a prolonged pro-inflammatory response or fibrotic encapsulation, isolating it from the host tissue.
| Potential Cause | Diagnostic Tests | Solution |
|---|---|---|
| Surface Properties | Quantify macrophage polarization via flow cytometry (CD86 for M1, CD206 for M2); Measure levels of pro-inflammatory cytokines (e.g., TNF-α, IL-6) via ELISA. | Functionalize surface with anti-inflammatory cytokines (e.g., IL-4) or "self" peptides; Tune surface roughness/porosity. |
| Uncontrolled Degradation Products | Collect and analyze degradation media (e.g., using LC-MS); Co-culture with immune cells to assess cytotoxicity and activation. | Purify raw materials to remove contaminants; Switch to degradable units that produce metabolically benign products (e.g., lactic acid, succinate). |
Experimental Protocol: Evaluating Macrophage Polarization In Vitro
- Cell Culture: Use a murine macrophage cell line (e.g., RAW 264.7) or primary bone marrow-derived macrophages (BMDMs). Culture in appropriate media.
- Material Exposure: Seed macrophages on the surface of the biomaterial or in a Transwell co-culture system. Include controls: M0 (unpolarized), M1 (stimulated with LPS and IFN-γ), and M2 (stimulated with IL-4 and IL-13).
- Analysis (48-72 hours post-exposure):
- Flow Cytometry: Harvest cells and stain for surface markers: CD86 (M1) and CD206 (M2).
- Cytokine ELISA: Collect cell culture supernatant and measure the concentration of TNF-α/IL-6 (M1) and IL-10/TGF-β (M2).
- Gene Expression: Isolve RNA and perform qPCR for M1 (iNOS, IL-1β) and M2 (Arg1, Ym1) gene markers.
- Interpretation: A pro-regenerative material will promote a significant shift towards an M2-like phenotype compared to the M0 and M1 controls.
Frequently Asked Questions (FAQs)
Q1: What are the main categories of stimuli that smart biomaterials respond to? Smart biomaterials are classified based on the origin of the trigger stimulus. External/Physical stimuli are applied from outside the body and include light (e.g., NIR), magnetic fields, ultrasound, and electric fields [43] [44]. Internal/Chemical & Biological stimuli are inherent to the pathological or physiological microenvironment and include pH, specific enzymes (e.g., MMPs), reactive oxygen species (ROS), and temperature gradients [43] [44] [45]. Some advanced systems are multi-responsive, designed to react to multiple triggers for enhanced precision [43].
Q2: My pH-sensitive hydrogel responds too slowly in the target acidic environment. How can I improve its response time? Slow response kinetics are often a diffusion-limited problem. You can:
- Increase Porosity: Modify your fabrication method (e.g., using porogens or cryogelation) to create a more macroporous network, facilitating faster proton diffusion.
- Reduce Material Dimensions: Switch from a bulk hydrogel to hydrogel microparticles or nanoparticles, dramatically increasing the surface-area-to-volume ratio.
- Modify Polymer Chemistry: Incorporate more hydrophilic and ionizable groups into the polymer backbone to enhance water uptake and swelling speed upon protonation.
Q3: How can I confirm that my material is working via its intended mechanism in vivo and not just through passive release? This requires careful experimental design with appropriate controls.
- Use a Control Material: Design and synthesize a control material that is structurally identical but lacks the responsive element (e.g., a non-cleavable linker instead of an enzyme-cleavable one).
- In Vivo Imaging: If possible, label your material and its payload with different fluorophores or contrast agents. Use non-invasive imaging to track whether the material accumulates at the target site and whether the payload is released specifically there.
- Pharmacokinetic/Pharmacodynamic (PK/PD) Studies: Compare the biodistribution and efficacy of the drug delivered by the smart material versus the free drug or the drug delivered by the non-responsive control material. A successful smart material will show higher target site accumulation and reduced off-target effects.
Q4: What are the key molecular biology techniques to assess host response to my biomaterial? Essential techniques for evaluating biocompatibility and cellular responses at the molecular level include [46]:
- Polymerase Chain Reaction (PCR/qPCR): To detect and quantify changes in gene expression of inflammatory markers (e.g., TNF-α, IL-6), fibrosis-associated genes (e.g., Collagen I), and regeneration markers.
- Immunocytochemistry (ICC) & Immunohistochemistry (IHC): To visualize and localize specific protein targets (e.g., cell surface markers on immune cells, transcription factors like YAP/TAZ) within and around the material.
- Enzyme-Linked Immunosorbent Assay (ELISA): To quantitatively measure the secretion levels of specific cytokines and growth factors in the tissue homogenate or culture supernatant.
- Flow Cytometry: To immunophenotype and quantify different immune cell populations (e.g., M1 vs. M2 macrophages) recruited to or influenced by the implant.
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in Smart Biomaterial Research | Example Application |
|---|---|---|
| Poly(N-isopropylacrylamide) (PNIPAAm) | A temperature-responsive polymer exhibiting a Lower Critical Solution Temperature (LCST) near 32°C. Undergoes reversible swelling/deswelling. | Injectable, in-situ gelling systems for cell delivery or drug depot formation [47]. |
| pH-Sensitive Linkers | Chemical bonds (e.g., hydrazone, acetal, β-thiopropionate) that remain stable at pH 7.4 but hydrolyze in acidic environments. | Targeted drug release in tumor microenvironments (pH ~6.5-6.8) or inflammatory sites [43] [47]. |
| Matrix Metalloproteinase (MMP)-Cleavable Peptides | Short peptide sequences (e.g., VPMS↓MRGG) that are specifically cleaved by MMPs overexpressed in remodeling tissues and tumors. | Creating hydrogels that degrade on-demand to release cells or drugs in response to local cellular activity [47]. |
| Black Phosphorus (BP) Nanosheets | A photoresponsive nanomaterial that generates heat and reactive oxygen species upon Near-Infrared (NIR) light irradiation. | Photothermal therapy and light-triggered drug release for bone tumor ablation and subsequent bone regeneration [43]. |
| Azobenzene Crosslinkers | Molecules that undergo reversible cis-trans isomerization upon exposure to specific light wavelengths, changing their molecular length. | Creating hydrogels with reversibly tunable stiffness for mechanobiology studies [48]. |
| Parasin I TFA | Parasin I TFA, MF:C84H155F3N34O26, MW:2114.3 g/mol | Chemical Reagent |
| Antifungal agent 87 | Antifungal agent 87, MF:C14H14O4, MW:246.26 g/mol | Chemical Reagent |
Essential Signaling Pathways and Experimental Workflows
Material-Driven Macrophage Polarization Pathway
Stimuli-Responsive Drug Release Workflow
Leveraging Decellularized Extracellular Matrix (dECM) for Native-like Scaffolds
FAQs: Core Concepts and Host Response
Q1: What are the primary immunological advantages of using dECM scaffolds over synthetic alternatives? dECM scaffolds offer significant immunological benefits because they are derived from natural extracellular matrices, which are largely conserved across species, and the decellularization process removes major immunogenic components. Unlike synthetic scaffolds that can trigger a foreign body response (FBR) leading to chronic inflammation and fibrotic encapsulation, dECM scaffolds are recognized as "self" components [49]. They primarily stimulate an indirect pathway of allorecognition, which is less vigorous and avoids acute rejection. Furthermore, a properly prepared dECM can promote a shift in macrophage polarization toward the reconstructive M2 phenotype and encourage T cell polarization toward a regulatory (T reg) phenotype, fostering a regenerative environment instead of an inflammatory one [49].
Q2: Despite decellularization, why do some dECM scaffolds still provoke an immune response? Immune responses to dECM scaffolds are often triggered by residual elements and processing-induced damage [49]. Key etiologies include:
- Residual Cellular Antigens: Incomplete removal of major histocompatibility complex (MHC) molecules and minor histocompatibility antigens can activate the adaptive immune system [49].
- Damage-Associated Molecular Patterns (DAMPs): These are danger signals released when cells and the ECM are damaged during harsh decellularization or implantation. DAMPs include nuclear and mitochondrial DNA, reactive oxygen species (ROS), and fragmented ECM components like hyaluronic acid [49]. They are recognized by pattern recognition receptors (PRRs) on innate immune cells, triggering a pro-inflammatory response (e.g., release of IL-1, IL-6, TNF) that can lead to graft destruction [49].
- Xenogeneic Antigens: When using animal-derived tissues, epitopes like the alpha-gal epitope can cause rejection if not thoroughly removed [50].
- Cytotoxicity from Processing: Residual chemical detergents from the decellularization process can cause cytotoxicity and exacerbate inflammatory responses [49].
Q3: What is the role of decellularization quality in determining the host response? The quality of decellularization is the most critical factor in dictating the host response. An ineffective process leaves immunogenic cellular material, while an overly aggressive process can destroy the native ECM's structural and biochemical integrity, generating DAMPs and compromising the scaffold's mechanical and bio-instructive properties [49] [50]. The ultimate goal is to find a balance that achieves complete cell removal while maximally preserving the native ECM's composition, architecture, and bound signaling molecules [50].
Troubleshooting Guides
Problem: Inconsistent or Incomplete Decellularization
Potential Causes and Solutions:
| Cause | Diagnostic Tests | Solution and Optimization |
|---|---|---|
| Inefficient Decellularization Agent | - DNA quantification (e.g., picogreen assay): >50 ng mg dry weight residual DNA indicates poor decellularization [50].- Histology (H&E, DAPI staining): Visual identification of residual nuclear material. | Switch or combine agents. Non-ionic detergents (Triton X-100) are milder but may leave cytoplasm; ionic detergents (SDS) are more effective but can denature ECM proteins; zwitterionic detergents (CHAPS) offer a middle ground [50]. |
| Inadequate Perfusion or Agitation | - Visual inspection for uneven coloration.- Sampling from multiple tissue regions for DNA/histology. | For porous tissues: Use perfusion-based decellularization to ensure uniform agent delivery. For dense tissues: Increase agitation speed or duration. |
| High Native Lipid Content | - Lipid-specific stains (e.g., Oil Red O). | Incorporate lipase enzymes into the protocol to catalyze the cleavage of ester bonds in lipids [50]. |
Detailed Protocol: Apoptosis-Assisted Decellularization This method aims to minimize DAMP generation by avoiding sudden cell necrosis.
- Induction: Treat the tissue with a mild apoptotic stimulus (e.g., serum starvation, UV exposure).
- Incubation: Incubate the tissue under physiological conditions for 12-48 hours to allow endogenous caspases to initiate programmed cell death.
- Rinsing: Use a mild non-ionic detergent (e.g., 0.1% Triton X-100) in a hypotonic buffer to rinse out cellular debris without aggressive ECM disruption [49].
- Nuclease Treatment: Immerse the tissue in a solution containing DNase and RNase (e.g., 100 U/mL in Mg²⺠buffer) for 12-24 hours to fragment and remove nucleic acids [50].
- Final Rinse: Rinse extensively with deionized water and PBS to remove all enzymes and cellular remnants.
Problem: Poor In Vivo Integration and Host Cell Recruitment
Potential Causes and Solutions:
| Cause | Diagnostic Tests | Solution and Optimization |
|---|---|---|
| Loss of Bioactive Cues | - ELISA/Western Blot: Quantify retention of key Growth Factors (e.g., VEGF, FGF).- In vitro cell migration assay: Assess chemotactic potential. | Use gentler decellularization methods (e.g., using zwitterionic detergents). Consider recapitulation strategies by soaking the dECM in a cocktail of critical GFs post-decellularization [50]. |
| Excessive Crosslinking | - Enzymatic degradation assay: Measure resistance to collagenase.- Mechanical testing: Check for unnaturally high stiffness. | Optimize crosslinking parameters (concentration, duration). Use carbodiimide (EDC) crosslinking instead of glutaraldehyde to reduce cytotoxicity. Explore non-chemical methods like dehydrothermal treatment [49]. |
| Presence of DAMPs | - ELISA for HMGB1 or S100 proteins.- qPCR for pro-inflammatory cytokine upregulation in cultured macrophages. | Implement a final "clean-up" step using washing buffers with scavengers for DAMPs (e.g., albumin). Ensure all nucleic acids are thoroughly removed with nucleases [49]. |
Detailed Protocol: Assessing Macrophage Polarization In Vitro This protocol evaluates the immunomodulatory potential of your dECM.
- dECM Conditioning: Culture the dECM scaffold in standard cell culture medium for 24-48 hours to create a conditioned medium.
- Cell Seeding: Isolate primary human or murine monocytes, differentiate them into naïve macrophages (M0), and seed them in a 24-well plate.
- Treatment: Treat the macrophages with the dECM-conditioned medium. Use standard media as a negative control and media with LPS/IFN-γ as a positive M1 (inflammatory) control.
- Analysis: After 48 hours, analyze polarization via:
- qPCR: Measure gene expression markers for M1 (iNOS, TNF-α, IL-6) and M2 (Arg1, CD206, IL-10) phenotypes.
- Flow Cytometry: Stain for M1 (e.g., CD80) and M2 (e.g., CD206) surface markers.
- A successful dECM scaffold will promote a significant upregulation of M2 markers compared to the M1 control [49].
Key Signaling Pathways in dECM Immunogenicity
The following diagram illustrates the key immune pathways triggered by a dECM scaffold, highlighting the critical role of residual antigens and DAMPs.
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential reagents and their functions for developing and evaluating dECM scaffolds.
| Reagent Category | Specific Examples | Function in dECM Research |
|---|---|---|
| Decellularization Agents | SDS (Ionic Detergent): Effective for cell lysis and DNA removal. Can be harsh on ECM structure. [50]Triton X-100 (Non-ionic Detergent): Milder agent for cell lysis, good for cytoplasmic removal. [50]CHAPS (Zwitterionic Detergent): Balanced option, maintains ECM structure better than SDS. [50] | Disrupt cell membranes and lipid-protein interactions to solubilize and remove cellular material while aiming to preserve the native ECM. |
| Enzymes | DNase/RNase: Catalyze the cleavage of phosphodiester bonds in DNA/RNA. Essential for removing immunogenic genetic material. [50]Trypsin: Protease that cleaves peptide bonds; often used with EDTA to dissociate cells. [50] | Degrade and remove specific cellular components (nucleic acids, proteins) that are not eliminated by detergents alone. |
| Crosslinkers | Glutaraldehyde: Traditional crosslinker, can cause cytotoxicity. [49]EDC (Carbodiimide): Zero-length crosslinker, less cytotoxic, promotes amine-carboxyl linkage. [49] | Enhance the mechanical stability and resistance to degradation of the dECM scaffold. Can mask residual antigens. |
| Assessment Kits | Picogreen Assay: Fluorescent quantitation of double-stranded DNA. Critical for validating decellularization. [50]ELISA Kits: For quantifying residual growth factors (e.g., VEGF, FGF) or DAMPs (e.g., HMGB1). | Provide quantitative data to ensure the scaffold meets quality control standards for decellularization and bioactivity. |
| Sterilization Methods | Peracetic Acid, Ethylene Oxide, Gamma Irradiation | Eliminate microbial contamination. Method choice significantly impacts ECM integrity and immunogenicity; requires optimization. [49] [50] |
| Norfloxacin | Norfloxacin, CAS:68077-27-0; 70458-96-7, MF:C16H18FN3O3, MW:319.33 g/mol | Chemical Reagent |
| BU-2313 A | BU-2313 A, MF:C27H35NO9, MW:517.6 g/mol | Chemical Reagent |
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions (FAQs)
FAQ 1: How can we improve the predictive accuracy of AI models for biomaterial-host interactions when our dataset is limited? Limited data is a common challenge. To improve model accuracy, we recommend:
- Data Augmentation: Artificially expand your dataset using techniques like SMOTE for numerical data or adding noise to existing data within physiological ranges.
- Transfer Learning: Leverage pre-trained models developed for large, public biomaterial or biological response datasets (e.g., from the Protein Data Bank) and fine-tune them on your specific, smaller dataset [51].
- Utilize Multimodal AI: Integrate smaller datasets from different sources (e.g., mechanical properties, genomic data, simple imaging) to create a more holistic model that can uncover complex relationships not visible in single-data models [51].
FAQ 2: Our experimental results for biomaterial degradation do not match the AI's predictions. What could be the cause? A discrepancy between prediction and experiment often stems from the "black-box" nature of some complex models and variability in experimental conditions.
- Troubleshooting Steps:
- Audit Training Data: Check if the model was trained on data that adequately covers the experimental conditions (e.g., pH, enzyme concentrations, mechanical stress) you are testing.
- Increase Interpretability: Employ interpretability techniques like SHAP (SHapley Additive exPlanations) to understand which input features (e.g., polymer molecular weight, cross-linking density) the model is heavily relying on for its predictions. This can reveal if the model is using spurious correlations [52] [53].
- Validate Experimentally: Confirm that your experimental protocols for measuring degradation (e.g., mass loss, release profile) are consistent and reproducible.
FAQ 3: What are the best AI approaches for inverse design—finding a biomaterial formulation that meets a specific set of biological and mechanical criteria? Inverse design is a key strength of AI in biomaterials. The following approaches are recommended:
- Generative Models: Use models like Generative Adversarial Networks (GANs) or Variational Autoencoders (VAEs) to generate novel biomaterial designs (e.g., polymer structures, composite formulations) that possess your target properties [52].
- Reinforcement Learning (RL): Implement RL algorithms where the "agent" explores the vast design space of material parameters. The agent receives rewards for proposing designs that meet your target criteria, learning to optimize formulations through this computational trial-and-error process [53].
- High-Throughput Screening Coupled with ML: Use AI to screen large in silico libraries of material compositions. Train a model on a subset of known data, and then use it to predict the performance of millions of virtual candidates, prioritizing the most promising for synthesis [54].
FAQ 4: How can we manage and integrate heterogeneous data types (e.g., imaging, genomics, mechanical tests) for a multimodal AI project? Effective data integration is critical for multimodal AI.
- Methodology:
- Standardization: Create a standardized data pre-processing pipeline for each data modality (e.g., normalize imaging data, align genomic sequences, scale mechanical properties).
- Feature Extraction: Use specialized AI models to extract key features from each data type: Convolutional Neural Networks (CNNs) for medical or material images, and Recurrent Neural Networks (RNNs) for sequential data like genomic information or time-series degradation data [51].
- Data Fusion: Fuse the extracted features into a unified representation in the middle or late stages of the AI model architecture, allowing the network to learn cross-modal relationships [51].
Troubleshooting Common Experimental Issues
Issue: High Variability in Cell Response Data on AI-Designed Scaffolds
- Potential Cause: The AI model may be overfitting to a limited set of cell culture conditions (e.g., a single cell line, specific serum concentration) and failing to generalize.
- Solution:
- Retrain with Expanded Data: Incorporate training data that captures a wider range of biological variability, such as different cell donors, passage numbers, and culture media compositions [53].
- Incorporate Noise: Intentionally add controlled variability to the training data to make the model more robust.
- Experimental Validation: Always validate AI predictions with in vitro experiments using multiple cell lines or primary cells to ensure biological relevance [54].
Issue: Poor Printability or Structural Failure of AI-Optimized Bioinks during 3D Bioprinting
- Potential Cause: The AI model optimized for biological performance (e.g., cell adhesion) may have proposed a material with unsuitable rheological properties for the specific biofabrication process.
- Solution:
- Multi-Objective Optimization: Reformulate the AI's task to simultaneously optimize for both biological and mechanical/printing parameters (e.g., viscosity, shear-thinning behavior, cross-linking time) [54].
- Integrate Process Parameters: Include biofabrication process parameters (e.g., nozzle diameter, printing pressure, temperature) as input features in the AI model to better predict printability outcomes [54].
Summarized Data Tables
Table 1: AI Model Types and Their Applications in Biomaterials Design
| AI Model Type | Primary Function | Specific Application in Biomaterials | Key Advantage |
|---|---|---|---|
| Supervised Learning [52] [53] | Predicts an output from labeled input data. | Predicting degradation rates of polymers [52] [53]. | High accuracy for well-defined prediction tasks. |
| Unsupervised Learning [52] [53] | Finds hidden patterns in unlabeled data. | Clustering different protein adsorption profiles on material surfaces [52]. | Discovers novel patterns without pre-existing labels. |
| Reinforcement Learning [53] | Learns optimal decisions through trial-and-error feedback. | Optimizing the composition of a hydrogel for controlled drug release [53]. | Ideal for iterative design optimization. |
| Deep Learning (DL) [54] [52] | Processes complex data through multi-layered neural networks. | Analyzing medical images to design patient-specific implants [51]. | Automates feature extraction from raw, complex data. |
| Multimodal AI [51] | Integrates diverse data types (e.g., images, genomics). | Designing a bone scaffold by combining CT scan data, genomic markers for osteoporosis, and mechanical test data [51]. | Provides a holistic view for personalized solutions. |
Table 2: Essential Research Reagent Solutions for AI-Driven Biomaterials Research
| Reagent / Material | Function in Experiment | Relevance to AI Integration |
|---|---|---|
| Protein Data Bank (PDB) Datasets [51] | Provides 3D protein structures for training AI models like AlphaFold. | Enables AI-driven prediction of biomaterial-protein interactions and biological compatibility [51]. |
| Specific Cell Lines (e.g., MSC, HUVEC) | Model biological host response (e.g., adhesion, differentiation, inflammation). | Generates standardized biological response data for training and validating AI prediction models [54] [53]. |
| Functionalized Hydrogels | Mimic the extracellular matrix; used for 3D cell culture and bioprinting. | Serves as a tunable material platform for high-throughput screening to generate data for AI models [55] [53]. |
| High-Throughput Screening Assays | Rapidly test cell viability, proliferation, and differentiation on numerous material compositions. | Generates the large-scale, consistent datasets required to train robust and accurate AI models [52]. |
| Fluorescent Markers & Imaging Dyes | Visualize and quantify cell-material interactions (e.g., cell spreading, apoptosis). | Provides rich, quantitative image data that can be analyzed by Convolutional Neural Networks (CNNs) to automate response evaluation [51]. |
Detailed Experimental Protocols
Protocol 1: High-Throughput Screening of Polymer Libraries for Cytocompatibility
Objective: To generate a large, consistent dataset on polymer cytocompatibility for training a supervised AI model to predict host response.
Materials:
- Library of polymer compositions (e.g., varying ratios of PGA, PLA, PCL)
- 96-well or 384-well cell culture plates
- Standard cell line (e.g., human fibroblasts)
- Cell viability assay kit (e.g., MTT, AlamarBlue)
- Automated liquid handling system
- Plate reader
Methodology:
- Polymer Preparation: Synthesize or acquire the polymer library. Create thin films or microparticles of each polymer composition.
- Plate Coating: Use an automated liquid handler to coat the wells of the culture plate with the different polymer compositions, ensuring consistency. Include control wells (tissue culture plastic for positive control, a toxic material for negative control).
- Cell Seeding: Seed a predetermined number of cells into each well using the automated system.
- Incubation: Culture cells for a standardized period (e.g., 24, 48, 72 hours).
- Viability Assay: Perform the cell viability assay according to the manufacturer's protocol, using the plate reader for quantification.
- Data Curation: Compile the results into a structured dataset. Each entry should include the polymer's physicochemical descriptors (e.g., molecular weight, hydrophobicity, composition ratios) as input features and the normalized cell viability as the output label [52] [53].
Protocol 2: Integrating Multimodal Data for Personalized Bone Scaffold Design
Objective: To combine patient-specific clinical imaging and AI to design an optimized, bioinspired scaffold for bone regeneration.
Materials:
- Patient CT scan data (DICOM format)
- AI software platform (e.g., Python with TensorFlow/PyTorch, specialized biomaterial software)
- 3D bioprinter
- Osteoconductive bioink (e.g., hydroxyapatite-loaded alginate)
Methodology:
- Image Processing:
- Input the patient's CT scan into a Convolutional Neural Network (CNN) trained for medical image segmentation.
- The CNN automatically identifies and segments the bone defect geometry, outputting a 3D model [51].
- Mechanical Optimization:
- Use the 3D model in a Finite Element Analysis (FEA) simulation to map mechanical stress distributions under load.
- Train a separate AI model (e.g., a reinforcement learning agent) to optimize the scaffold's internal porous architecture to match the native bone's mechanical properties and minimize stress shielding [55].
- Biomaterial Selection:
- Digital Design & Fabrication:
- The final, optimized scaffold design is converted into a G-code file and fabricated using a 3D bioprinter and the selected bioink [54].
Workflow and Relationship Visualizations
Troubleshooting Immune Rejection and Optimizing for Personalized Outcomes
Fundamental Concepts of Macrophage Polarization
What is macrophage polarization and why is it critical in biomaterial research?
Macrophage polarization is the process by which macrophages adopt different functional phenotypes—primarily the pro-inflammatory M1 or anti-inflammatory M2 state—in response to specific environmental signals within their microenvironment [56] [57]. This plasticity is a hallmark of macrophages and represents a continuum of functional states rather than simply two fixed categories [56] [58].
In the context of biomaterial implantation and tissue engineering, the host immune response initiates with M1 macrophages, which are crucial for early-stage inflammatory responses and pathogen clearance. However, a timely transition to M2 macrophages is essential for promoting tissue repair and regeneration [56] [1]. A persistent M1 response can lead to chronic inflammation and tissue damage, while an improperly timed M2 polarization may result in fibrotic encapsulation of implanted materials [56]. Therefore, understanding and controlling this balance is fundamental to overcoming variability in host responses to biomaterials.
What are the key functional differences between M1 and M2 macrophages?
The table below summarizes the characteristic features of M1 and M2 macrophage phenotypes:
| Feature | M1 (Pro-inflammatory) | M2 (Anti-inflammatory / Pro-healing) |
|---|---|---|
| Activating Stimuli | IFN-γ, LPS, TNFα [56] [57] | IL-4, IL-13, IL-10 [56] [57] |
| Characteristic Surface Markers | CD80, CD86, MHC II [59] | CD206, CD163, Dectin-1 [57] [59] |
| Key Secreted Cytokines & Mediators | TNFα, IL-1β, IL-6, IL-12, iNOS, ROS [57] [59] | IL-10, TGF-β, Ornithine, Polyamines [57] |
| Primary Functions | Pathogen clearance, tumor cytotoxicity, immunostimulation [57] | Tissue repair, immunoregulation, angiogenesis, parasite containment [56] [57] |
| Metabolic Pathway | Glycolysis [59] | Oxidative Phosphorylation, Fatty Acid Oxidation [59] |
Key Signaling Pathways Governing M1-M2 Polarization
The polarization of macrophages is directed by a complex interplay of intracellular signaling pathways. The following diagram illustrates the core signaling networks that regulate the balance between the M1 and M2 phenotypes.
How do these signaling pathways influence polarization outcomes?
The diagram above illustrates the major signaling cascades. Key regulatory mechanisms include:
- NF-κB Pathway: A central driver of M1 polarization. Signals through Toll-like Receptors (TLR4) by pathogens or damage (LPS) activate IKK, which leads to the degradation of IκB and the nuclear translocation of NF-κB (p65/p50) to transcribe pro-inflammatory genes [57] [59].
- JAK-STAT Pathway: This is a pivotal axis. STAT1 activation by IFN-γ promotes M1 genes, while STAT6 activation by IL-4/IL-13 and STAT3 activation by IL-10 drive M2 polarization [57] [59]. The balance between STAT1 and STAT6/STAT3 activation is a critical control point.
- IRF Family: IRF5 is induced by TLR signaling and promotes M1 responses. In contrast, IRF4, which is upregulated by STAT6, inhibits IRF5 and promotes the M2 phenotype [57].
- PPARγ and KLF4: These are key transcription factors for M2 polarization. PPARγ controls oxidative metabolism and M2 gene expression, while KLF4 promotes M2 functions by suppressing NF-κB [57].
- Negative Feedback: Molecules like SOCS1 and SOCS3 are induced by inflammatory signaling (e.g., STAT1) and provide negative feedback to prevent excessive M1 polarization [57].
Experimental Protocols for Modulating PolarizationIn Vitro
What is a standard protocol for polarizing human macrophages toward M1 and M2 phenotypes?
This protocol is commonly used for differentiating and polarizing macrophages from human monocytic cell lines (like THP-1) or primary monocytes.
Protocol 1: Differentiation and Polarization of Human Macrophages
| Step | Procedure | Reagents & Concentrations | Duration | Key Notes |
|---|---|---|---|---|
| 1. Monocyte Differentiation | Culture THP-1 cells or isolated PBMCs. | THP-1: 100 ng/mL PMAPBMCs: 50 ng/mL M-CSF | 24-48 hours | PMA treatment for THP-1 cells induces adherence and differentiation into macrophage-like cells. |
| 2. Resting Phase | Replace medium with fresh, cytokine-free medium. | Basic growth medium (e.g., RPMI-1640 with serum) | 24 hours | Allows cells to stabilize in a resting, M0 state. |
| 3. M1 Polarization | Stimulate resting macrophages with M1-inducing cues. | Standard: 100 ng/mL LPS + 20 ng/mL IFN-γAlternative: 20 ng/mL IFN-γ alone | 24-48 hours | LPS+IFN-γ is a potent classic activation signal. |
| 4. M2 Polarization | Stimulate resting macrophages with M2-inducing cues. | M2a (IL-4): 20 ng/mL IL-4M2a (IL-13): 20 ng/mL IL-13M2c (Deactivation): 20 ng/mL IL-10 | 24-48 hours | IL-4 and IL-13 induce the "alternative activation" M2a subtype. |
How can I validate the success of macrophage polarization in my experiments?
It is crucial to confirm phenotype shifts using a combination of techniques. The table below outlines standard validation methods and their expected outcomes.
Table: Key Methods for Phenotype Validation
| Method | M1 Marker Examples | M2 Marker Examples | Technical Considerations |
|---|---|---|---|
| Gene Expression (qPCR) | iNOS (NOS2), IL-1β, IL-12, TNFα | Arg1, FIZZ1 (RETNLA), YM1 (CHI3L1), CD206, CCL17 | Fast, quantitative. Use a panel of markers for confidence. |
| Surface Marker Analysis (Flow Cytometry) | CD80, CD86, MHC-II | CD206, CD163, CD200R | Direct protein-level detection on live cells. |
| Cytokine Secretion (ELISA/Cytometric Bead Array) | High TNFα, IL-12, IL-6 in supernatant | High IL-10, TGF-β in supernatant | Measures functional secretory output. |
| Functional Assays | Nitrite (Griess assay) measurement | Arginase activity assay | iNOS produces NO (measured as nitrite), while Arg1 consumes arginine. |
The Scientist's Toolkit: Research Reagent Solutions
A curated list of essential reagents for studying macrophage polarization is provided below.
| Reagent Category | Specific Examples | Primary Function in Polarization |
|---|---|---|
| Polarizing Cytokines | Recombinant Human/Mouse IFN-γ, IL-4, IL-13, IL-10 | Directly induces polarization toward M1 (IFN-γ) or M2 (IL-4, IL-13, IL-10) phenotypes [56] [57]. |
| TLR Agonists | Ultrapure LPS (from E. coli or S. minnesota) | Activates TLR4 signaling to strongly drive M1 polarization, often used in synergy with IFN-γ [57]. |
| Signal Transduction Inhibitors | BAY 11-7082 (IKK inhibitor), Stattic (STAT3 inhibitor), AS1517499 (STAT6 inhibitor) | Chemically probes specific signaling pathways (NF-κB, JAK-STAT) to validate their role in polarization [59]. |
| Metabolic Modulators | 2-Deoxy-D-glucose (2-DG, glycolysis inhibitor), Etomoxir (CPT1 inhibitor, blocks FAO) | Investigates the critical link between metabolic reprogramming and macrophage phenotype [59]. |
| Validation Antibodies | Anti-CD86 (M1), Anti-CD206 (M2), Anti-iNOS (M1), Anti-Arginase-1 (M2) | Essential for flow cytometry, western blot, or immunofluorescence to confirm phenotype. |
Troubleshooting Common Experimental Challenges
FAQ 1: Why do my macrophages not show a clear M1/M2 phenotype after stimulation?
Potential Causes and Solutions:
- Insufficient Polarization Time: Ensure stimulation lasts at least 24 hours; some markers peak at 48 hours.
- Inadequate Cytokine Concentration: Titrate your cytokines (e.g., IL-4, IFN-γ) to find the optimal concentration for your specific cell source.
- Resting State Not Achieved: If starting from a monocyte line, ensure proper differentiation and a 24-hour resting period in base medium before polarization.
- Cell Health Issues: Check for mycoplasma contamination and ensure cells are not over-confluent, which can alter their responsiveness.
- Marker Selection: Use a panel of at least 2-3 markers for each phenotype to get a confident readout, as the expression can be heterogeneous.
FAQ 2: How can I achieve a sequential M1-to-M2 phenotype switch in my biomaterial study?
This is a key challenge for mimicking the natural healing process. The following workflow diagram outlines a general strategy for designing such an experiment.
Key Considerations for Sequential Polarization:
- Biomaterial-Based Strategies: Instead of a simple cytokine wash, "smart" biomaterials can be engineered to control the spatial and temporal release of chemical cues. For instance, scaffolds can be designed to release an M1-inducing factor initially, followed by a delayed release of M2-promoting factors like IL-4 or IL-10 [56].
- Critical Timing: Literature suggests that the M1 phase is necessary initially but should subside after a few days. A sustained M1 response hinders healing. The timing of the switch is critical for therapeutic success [56].
- Validation: When testing your system, it is essential to measure markers for both phenotypes over a time course to confirm that M1 markers decrease while M2 markers increase.
Variability can arise from multiple sources, making experimental consistency paramount.
- Cell Source: Macrophages derived from different donors (PBMCs), different cell lines (THP-1 vs. U937), or from different tissues can have inherent genetic and epigenetic differences that affect their polarization capacity [58].
- Culture Conditions: Serum batch variability, media composition, and cell density can significantly influence polarization outcomes. Using defined, serum-free media where possible can reduce this variability.
- Reagent Quality: The activity and endotoxin level of recombinant cytokines can vary between manufacturers and lots. Use high-quality, validated reagents and aliquot them to avoid freeze-thaw cycles.
- Developmental Origin: Remember that macrophages originate from at least two developmental pathways—embryonic-derived (self-renewing tissue-resident) and bone marrow-derived monocytes—which can lead to functionally distinct populations [58]. The source of your macrophages (e.g., a cell line vs. a tissue-resident population) is an important variable.
Fibrotic encapsulation is a common pathological process where an excessive amount of fibrous connective tissue is deposited into the extracellular matrix (ECM) space surrounding an implanted biomaterial [60]. This process represents the final common pathway of the foreign body reaction (FBR), a complex immune-mediated response that can compromise the functionality and longevity of medical implants [61]. The formation of a dense, avascular collagenous network around implants blocks communication between the device and host tissue, leading to device failure and necessitating replacement surgeries that cost healthcare systems billions annually [61].
Understanding and mitigating fibrotic encapsulation is particularly crucial within the broader context of overcoming variability in biomaterial host responses. The clinical success of implantable devices—from breast implants and glucose sensors to neural electrodes and drug delivery systems—heavily depends on achieving consistent and predictable tissue integration while minimizing the fibrotic response [61]. This technical support guide addresses the key challenges researchers face when designing anti-fibrotic strategies and provides practical solutions for evaluating material-based approaches.
Key Mechanisms and Signaling Pathways in Fibrosis
Cellular Players in Fibrotic Encapsulation
The foreign body response involves a coordinated sequence of cellular events beginning immediately after implantation:
- Protein Adsorption: Within minutes, blood plasma proteins (primarily albumin and fibrinogen) adsorb to the material surface, undergoing conformational changes that create recognition patterns for immune cells [62] [61].
- Neutrophil Infiltration: As first responders, neutrophils arrive at the implantation site within two days, secreting pro-inflammatory lipid mediators like cysteinyl leukotrienes (CysLTs) that regulate their own recruitment and stimulate fibroblast migration [62].
- Macrophage Polarization and Fusion: The acute inflammatory phase transitions to chronic inflammation approximately one week post-implantation, characterized by monocyte infiltration and macrophage activation [62] [61]. Macrophages attempt to phagocytose the implant, and in the case of non-degradable materials, fuse to form foreign body giant cells (FBGCs) [61].
- Fibroblast Activation and Myofibroblast Differentiation: Activated by cytokines and chemokines from immune cells, and under mechanical tension from weak focal adhesion to the material surface, fibroblasts differentiate into myofibroblasts [61]. This process is characterized by α-smooth muscle actin (α-SMA) expression in intracytoplasmic stress fibers and secretion of collagen types I and III [60] [61].
Molecular Signaling Pathways
The transformation of normal wound healing into pathological fibrosis involves several key molecular pathways:
- TGF-β/Smad Signaling: Transforming growth factor-beta (TGF-β1) is a master regulator of fibrosis, activating intracellular signaling through TGF-β receptors and Smad proteins (particularly Smad3) [60]. This pathway drives fibroblast-to-myofibroblast differentiation and upregulates collagen production [62] [60].
- MMP/TIMP Imbalance: Matrix metalloproteinases (MMPs) and their inhibitors (TIMPs) regulate ECM remodeling. An imbalance with increased TIMP activity promotes fibrosis by preventing collagen degradation in various organs [60].
- Rho/ROCK Pathway: When ECM adhesion is insufficient, fibroblasts enhance contractility via the Rho/ROCK signaling pathway, which synergistically interacts with TGF-β signaling to drive myofibroblast differentiation [62].
- Additional Molecular Mediators: Other significant contributors include Th2-type cytokines (IL-4, IL-5, IL-13, IL-21), angiogenic factors (VEGF), growth factors (CTGF, PDGF), and components of the renin-angiotensin-aldosterone system (Angiotensin II) [60].
Figure 1: Cellular and Molecular Pathways in Fibrotic Encapsulation. This diagram illustrates the sequential cellular events and key molecular signaling pathways that drive the foreign body response and subsequent fibrotic capsule formation around implanted biomaterials. Dashed lines represent molecular signaling influences on cellular processes.
Frequently Asked Questions (FAQs) on Anti-Fibrotic Material Design
FAQ 1: What material surface properties most significantly impact the foreign body response?
Multiple surface properties collectively influence the foreign body response, with surface topography, chemistry, and mechanical stiffness being particularly significant [61]. Optimized surface topography at micro/nano levels can tune protein adsorption, focal cell adhesion, and ultimately regulate fibrotic capsule formation [61]. For instance, enhanced textural complexity significantly alters the pathological progression of FBR, promoting tissue ingrowth that disrupts fibrous capsule architecture while improving tissue integration [62]. Compared to smooth-surface implants, textured implants release particulate debris that undergoes macrophage phagocytosis, triggering adaptive immune responses that differ from those elicited by smooth surfaces [62].
Surface chemistry modifications that increase hydrophilicity have demonstrated significant benefits. Zwitterionic polymer coatings substantially reduce protein adsorption and macrophage attachment, leading to thinner fibrous capsules in rodent models [61]. Methacryloyloxyethyl phosphorylcholine (MPC) polymer coatings mimic the outer cell membrane structure, creating a superhydrophilic surface that resists protein adsorption and subsequent immune cell recognition [62].
The mechanical properties of implants, particularly stiffness, should match the target tissue for optimal integration [36]. Softer materials that better mimic brain tissue, for example, lead to reduced inflammatory reactions compared to stiffer counterparts [36]. This principle applies across various tissue types, highlighting the importance of mechanical compatibility in implant design.
FAQ 2: How can I determine if my surface modification effectively reduces fibrosis in vivo?
Comprehensive evaluation of anti-fibrotic efficacy requires multiple assessment methods spanning histological, molecular, and functional analyses:
Histological Analysis: Standard hematoxylin and eosin (H&E) staining provides initial assessment of overall tissue architecture and inflammatory cell infiltration, while Masson's Trichrome or Picrosirius Red staining specifically highlight collagen deposition and distribution [63]. The collagen layer thickness at the implant-tissue interface serves as a key quantitative metric, with significantly thinner layers indicating successful anti-fibrotic strategies [63].
Immunofluorescence Staining: Multiplex immunofluorescence for specific cell markers enables precise identification of immune cell populations involved in the FBR, including neutrophils (neutrophil elastase), macrophages (CD68 for pan-macrophages; iNOS and vimentin for pro-inflammatory M1 macrophages; CD206 for anti-inflammatory M2 macrophages), T cells (CD3), and fibroblasts (αSMA) [63]. Quantification of cell numbers in the collagenous layer at the implant-tissue interface over a standardized width (e.g., 500 μm) provides robust comparative data [63].
Molecular Analysis: Quantitative PCR (qPCR) analysis of immune-cell-related genes (including Nos2, Arg1, Cd68, Cd3e) and Luminex quantification of inflammatory cytokines (G-CSF, IL-12p70, etc.) offer insights into the molecular mechanisms underlying observed morphological differences [63]. RNA sequencing can provide comprehensive transcriptome profiles of the tissue response to different material surfaces [63].
FAQ 3: What are the most promising emerging technologies for preventing fibrotic encapsulation?
Several innovative approaches show significant promise for preventing fibrotic encapsulation:
Adhesive Implant-Tissue Interfaces: Recent groundbreaking research demonstrates that creating adhesive interfaces between implants and tissues can virtually eliminate observable fibrous capsule formation across diverse organs [63]. These interfaces achieve highly conformal integration with tissue surfaces, reducing infiltration of inflammatory cells into the implant-tissue interface compared to non-adhesive interfaces [63]. Poly(vinyl alcohol)-based and chitosan-based adhesive interfaces have both shown capability to prevent observable fibrous capsule formation for up to 84 days in rodent models [63].
Biomimetic Surface Strategies: Surfaces that mimic natural tissue structures or incorporate bioactive signals from the extracellular matrix can actively direct favorable immune responses [61]. Decellularized extracellular matrix (dECM) coatings retain structurally and chemically intact native ECM components that promote constructive tissue remodeling instead of scar formation [62].
3D-Printed and Additively Manufactured Implants: Additive manufacturing enables creation of implants with precisely controlled porosity and architecture that promotes vascularization and tissue integration while minimizing fibrosis [62]. Macroscale salt leaching techniques combined with 3D printing can create optimized surface textures that reduce FBR [62].
Drug-Eluting Systems with Advanced Therapeutics: Beyond traditional anti-inflammatories, next-generation systems deliver specific immunomodulatory agents such as colony-stimulating factor 1 receptor inhibitors that alter macrophage polarization from pro-inflammatory to anti-inflammatory states [36]. Genetic approaches using small interfering RNA (siRNA) and microRNA (miRNA) precisely target and regulate genes or pathways involved in inflammation [36].
Troubleshooting Guide: Common Experimental Challenges
Challenge 1: Inconsistent Fibrosis Measurement Across Samples
Problem: High variability in capsule thickness measurements between samples within the same experimental group, compromising data reliability.
Solutions:
- Implement standardized sampling protocols with multiple sectioning levels (at least 3-5 sections per implant) and systematic measurement intervals (e.g., every 100-200 μm along the implant interface) [63].
- Utilize automated image analysis systems with threshold-based collagen detection instead of manual measurements to reduce bias and improve consistency.
- Employ a blinded evaluation approach where the pathologist is unaware of sample group assignments during analysis to prevent unconscious bias [63].
- Include internal controls in each processing batch to account for technical variability in staining intensity.
Challenge 2: Poor Long-Term Stability of Anti-Fibrotic Coatings
Problem: Surface modifications or drug-eluting coatings degrade or delaminate before completing their intended functional duration.
Solutions:
- Implement accelerated aging studies to predict coating stability, including cyclic mechanical stress testing and in vitro degradation assays in physiologically relevant media.
- Consider cross-linking strategies or interpenetrating network hydrogels that maintain adhesion stability for extended periods (up to 12 weeks demonstrated in recent studies) [63].
- Incorporate stability testing as a standard part of coating characterization, including adhesion strength measurements via peel tests and examination of coating integrity after implantation using scanning electron microscopy.
Challenge 3: Translational Gaps Between In Vitro and In Vivo Findings
Problem: Promising in vitro anti-fibrotic results fail to translate to in vivo efficacy.
Solutions:
- Develop more physiologically relevant in vitro models, including macrophage-fibroblast co-culture systems that better mimic the cellular crosstalk in FBR [7].
- Utilize humanized mouse models that better recapitulate human immune responses when evaluating anti-fibrotic strategies intended for clinical translation [63].
- Implement preliminary in vivo screening with multiple time points (e.g., 3, 7, 14, 28 days) to capture the dynamic evolution of the FBR before committing to longer-term studies [63].
Experimental Protocols for Evaluating Anti-Fibrotic Strategies
Protocol for Histological Quantification of Fibrotic Encapsulation
This standardized protocol enables consistent evaluation and quantification of fibrotic capsules around implanted materials:
Materials Needed:
- Tissue samples with explanted materials
- 10% neutral buffered formalin
- Ethanol series (70%, 95%, 100%)
- Xylene or xylene substitute
- Paraffin embedding medium
- Microtome
- Glass slides
- Masson's Trichrome stain kit or Picrosirius Red stain kit
- Light microscope with digital camera
- Image analysis software (ImageJ/FIJI with appropriate plugins)
Procedure:
- Tissue Processing: Fix explanted tissue with surrounding capsule in 10% neutral buffered formalin for 24-48 hours at 4°C.
- Dehydration and Embedding: Process tissues through graded ethanol series (70%, 95%, 100%), clear in xylene, and infiltrate with paraffin using standard histological protocols.
- Sectioning: Section tissues at 4-5 μm thickness using a microtome, ensuring sections are taken from multiple levels through the implant site (minimum of 3 levels spaced 200-300 μm apart).
- Staining: Perform Masson's Trichrome staining following manufacturer's protocol (nuclei dark red, cytoplasm red, collagen blue) or Picrosirius Red staining (collagen appears birefringent under polarized light).
- Imaging: Capture digital images at standardized magnifications (40x, 100x, 200x) ensuring consistent lighting and exposure across all samples.
- Quantification:
- Using image analysis software, calibrate measurements using the image scale bar.
- Draw perpendicular lines from the implant surface to the outer capsule edge at systematic intervals (every 100 μm for a minimum of 10 measurements per section).
- For Picrosirius Red, use polarized light microscopy and quantify both capsule thickness and collagen birefringence intensity as measures of collagen organization and density.
- Statistical Analysis: Express results as mean thickness ± standard deviation, performing appropriate statistical tests (e.g., one-way ANOVA with post-hoc testing for multiple groups).
Protocol for Immunofluorescence Analysis of Foreign Body Response
This protocol enables detailed characterization of cellular populations and their phenotypes within the fibrotic capsule:
Materials Needed:
- Paraffin-embedded tissue sections (prepared as above)
- Antigen retrieval solution (citrate buffer, pH 6.0, or Tris-EDTA buffer, pH 9.0)
- Blocking solution (5% normal serum from host species of secondary antibodies)
- Primary antibodies against target antigens (see Table 1 for recommendations)
- Fluorochrome-conjugated secondary antibodies
- DAPI (4',6-diamidino-2-phenylindole) for nuclear counterstaining
- Fluorescent mounting medium
- Confocal or fluorescence microscope
Procedure:
- Deparaffinization and Rehydration: Bake slides at 60°C for 30 minutes, then deparaffinize in xylene and rehydrate through graded ethanol series to distilled water.
- Antigen Retrieval: Perform heat-induced epitope retrieval using appropriate buffer (consult antibody datasheet) in a microwave or pressure cooker (e.g., 95-100°C for 20 minutes).
- Blocking: Incubate sections with blocking solution containing 5% normal serum and 0.1-0.3% Triton X-100 for 1 hour at room temperature to prevent non-specific binding.
- Primary Antibody Incubation: Apply optimized concentrations of primary antibodies diluted in blocking solution and incubate overnight at 4°C in a humidified chamber.
- Secondary Antibody Incubation: After washing, apply appropriate fluorochrome-conjugated secondary antibodies diluted in blocking solution and incubate for 1-2 hours at room temperature protected from light.
- Counterstaining and Mounting: Apply DAPI (1 μg/mL) for 5 minutes to visualize nuclei, then wash and mount with fluorescent mounting medium.
- Imaging and Analysis: Acquire images using confocal or fluorescence microscopy with consistent settings across all samples. Quantify positively stained cells within a standardized area (e.g., 500 μm width from implant interface) using image analysis software.
Table 1: Key Antibodies for Characterizing Foreign Body Response
| Target | Cell Type/Marker | Recommended Clones/Sources | Dilution Range |
|---|---|---|---|
| α-SMA | Myofibroblasts | Abcam clone 1A4, Dako clone asm-1 | 1:200-1:500 |
| CD68 | Pan-macrophages | BioRad clone FA-11, Dako clone KP1 | 1:100-1:300 |
| iNOS | M1 macrophages | Abcam clone 2C1, Santa Cruz sc-7271 | 1:100-1:200 |
| CD206 | M2 macrophages | Abcam clone 15-2, BioRad MCA2235A647 | 1:200-1:400 |
| CD3 | T lymphocytes | Abcam clone SP7, Dako A0452 | 1:100-1:200 |
| Neutrophil Elastase | Neutrophils | Abcam clone 2B6, Dako M0752 | 1:200-1:500 |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents for Investigating Fibrotic Encapsulation
| Category | Specific Reagents/Materials | Function/Application | Key Considerations |
|---|---|---|---|
| Surface Modification | Zwitterionic polymers (e.g., MPC) | Create superhydrophilic surfaces that resist protein adsorption | Maintain coating stability during implantation; ensure uniform coverage |
| Poly(vinyl alcohol)-based adhesives | Form adhesive implant-tissue interfaces that prevent fibrous capsule formation | Optimize cross-linking density for balance of adhesion and biocompatibility | |
| Decellularized ECM (dECM) coatings | Provide bioactive signals that promote constructive tissue remodeling | Standardize dECM sourcing and processing to minimize batch-to-batch variability | |
| Pharmacological Agents | Triamcinolone acetonide (glucocorticoid) | Potent anti-inflammatory that inhibits fibroblast proliferation and collagen synthesis | Control release kinetics to maintain therapeutic concentrations without systemic effects |
| Tranilast (anti-allergic/anti-fibrotic) | Suppresses TGF-β1 release and collagen deposition by fibroblasts | Monitor potential hepatotoxicity at high doses in preclinical models | |
| Rho/ROCK pathway inhibitors (e.g., Y-27632) | Block mechanical tension-driven myofibroblast differentiation | Optimize local delivery to minimize effects on surrounding tissue contractility | |
| Characterization Tools | Picrosirius Red stain | Specific collagen detection with birefringence under polarized light | Use consistent microscope settings for quantitative birefringence comparisons |
| Multiplex Luminex assays | Simultaneous quantification of multiple inflammatory cytokines | Include standards in each plate to normalize between assay runs | |
| RNA sequencing | Comprehensive transcriptomic profiling of tissue response | Plan for adequate replication (n≥3) per experimental group for statistical power |
Figure 2: Experimental Workflow for Evaluating Anti-Fibrotic Strategies. This diagram outlines a comprehensive approach for developing and testing material-based strategies to mitigate fibrotic encapsulation, incorporating in vitro screening, appropriate animal models, and multi-modal analysis to generate translatable findings.
Mitigating fibrotic encapsulation requires a multifaceted approach that addresses the complex interplay between material properties and biological responses. The most promising strategies emerging from current research include creating adhesive implant-tissue interfaces that prevent inflammatory cell infiltration [63], designing surface topographies that direct favorable immune responses [61], and developing controlled release systems for specific immunomodulatory agents [36]. As the field advances, the focus is shifting from merely minimizing the foreign body response to actively orchestrating tissue responses that promote integration and regeneration.
For researchers working to overcome variability in biomaterial host responses, standardization of evaluation methods across laboratories will be crucial for generating comparable data and accelerating progress. The protocols and troubleshooting guides provided here offer a foundation for consistent assessment of anti-fibrotic strategies. Future directions will likely include the development of smart implants that can autonomously respond to their microenvironment and personalized approaches that account for individual variations in immune responses [36]. By systematically applying these material-based approaches and assessment methodologies, researchers can contribute to the next generation of implants that successfully achieve long-term functional integration with host tissues.
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ Category: Addressing Tumorigenicity
Question: What is the fundamental link between stem cell pluripotency and tumorigenicity? The abilities to self-renew and differentiate, which define stem cells, are mechanistically linked to tumorigenic potential. The core molecular programming for pluripotency shares key components with oncogenic pathways. Genes commonly used for reprogramming, such as Myc and KLF4, are established oncogenes, while other factors like Sox2, Nanog, and Oct3 are also linked to tumorigenesis. The teratoma assay, a standard test for pluripotency, is itself a tumor formation assay, highlighting this intrinsic connection [64].
Question: Are pluripotency and tumorigenicity inseparably coupled? Evidence suggests they are highly related but may be separable. A fundamental principle is that greater pluripotency and self-renewal often correlate with a higher probability of causing tumors. Conversely, reducing tumorigenicity may inevitably reduce "stemness." However, not all stem cells within the same culture form tumors, indicating that pluripotency and tumorigenicity, while deeply intertwined, may have distinct molecular features that can be targeted individually [64].
Question: What are the primary safety concerns regarding tumorigenicity in clinical applications? The risk varies by cell source. Adult stem cells (e.g., bone marrow mononuclear cells) have a low tumorigenic risk, and no related cancers have been reported in cardiac clinical trials. The risk is higher for pluripotent cells; Embryonic Stem Cell (ESC) and Induced Pluripotent Stem Cell (iPSC)-derived cardiomyocytes can form tumors. However, improved cardiac differentiation protocols have significantly reduced this risk. The minimal threshold for tumor formation from undifferentiated cells appears to be high (on the order of 100,000 cells), partly due to the generally poor survival of transplanted cells [65].
FAQ Category: Resolving Differentiation Inconsistency
Question: Why is there such high variability in differentiation efficiency between protocols and cell lines? Differentiation inconsistency arises from multiple factors:
- Protocol Variations: Strategies for differentiating stem cells into terminal fates (e.g., neurons) are based on developmental biology, but variations in the composition, concentration, and timing of signaling molecules lead to markedly different results [66].
- Cell Line Differences: Inherent variations in differentiation efficiency exist between different stem cell lines, which is particularly critical when using patient-specific iPSCs for disease modeling [66].
- Culture Methods: Novel methods like three-dimensional cultures and hypoxic conditions can influence differentiation outcomes but are not always standardized [66].
- Critical Parameters: For neural induction, the quality of the starting hPSCs and the initial plating density are crucial. Excessive differentiation in the starting culture or a confluency that is too low or too high will reduce induction efficiency [67].
Question: Our lab is differentiating basal forebrain cholinergic neurons (BFCNs). The efficiency is low and inconsistent. What are the key factors we should optimize? BFCN differentiation is complex. To improve efficiency, ensure your protocol recapitulates key developmental stages and check the following:
- Growth Factors: BMP9 induces and maintains the cholinergic phenotype, while FGF2 and BDNF stimulate cholinergic differentiation. NGF is critical for maturation and survival [66].
- Morphogens: Efficient patterning requires high Sonic Hedgehog (SHH) for ventralization and low Wnt signaling [66].
- Transcription Factors: The expression of key transcription factors like NKX2.1, LHX8, and ISL1 is a hallmark of correct lineage specification. One study achieved 94% purity in BFCN cultures by overexpressing LHX8 and GBX1 and using fluorescence-activated cell sorting [66].
- Characterization: Mature BFCNs are identified by markers like ChAT, vAChT, and p75NTR, and exhibit specific electrophysiological profiles (e.g., slow spiking activity of 4–10 Hz) [66].
Question: We encounter high cell death during neural stem cell (NSC) culture and differentiation. What are we doing wrong? NSCs and differentiating neurons are fragile. Common pitfalls and solutions include:
- Incorrect Thawing: Thaw cells quickly (not longer than 2 minutes at 37°C). Do not centrifuge primary neurons upon thawing [67].
- Osmotic Shock: After thawing, transfer cells to a pre-rinsed tube and add pre-warmed medium drop-wise while swirling the tube. Do not add the full medium volume at once [67].
- Improper Coating: For adherent NSC culture, ensure tissue culture plates are properly coated with Geltrex, fibronectin, or poly-L-ornithine/laminin as required [67].
- Old or Incorrect Medium: Check the expiration date of supplements like B-27. B-27-supplemented medium is stable for only two weeks at 4°C. Also, ensure you are using the correct B-27 supplement for your application [67].
Troubleshooting Guides
Troubleshooting Differentiation Inefficiency
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| High, uncontrolled differentiation in starting hPSC culture | Overgrown colonies; old culture medium; prolonged time outside incubator. | Passage cells at ~85% confluency. Remove differentiated areas before passaging. Ensure medium is fresh (<2 weeks old at 2-8°C). Minimize time plates are out of incubator (<15 min) [68]. |
| Poor cell survival after passaging or during neural induction | Cells are overly confluent during passaging; dissociation into single cells is too harsh; no protective agent used. | For passaging, avoid using overly confluent cultures. For sensitive cell lines or neural induction, use a ROCK inhibitor (Y-27632) during passaging to prevent apoptosis [67] [68]. |
| Low efficiency in cardiac differentiation with CHIR99021 | Inconsistent cell cycle status and confluency at differentiation initiation. | Standardize the cell seeding density and ensure uniform confluency at the start of differentiation. The efficiency of GSK3β inhibitors like CHIR99021 is highly dependent on the cell's state [69]. |
| Failed neural induction | Differentiated hPSCs in starting culture; incorrect initial plating density. | Remove all differentiated cells from hPSC culture before induction. Plate cells as small clumps (not single cells) at a recommended density of 2–2.5 x 10^4 cells/cm² [67]. |
Quantitative Data: Key Challenges in Clinical Translation
The table below summarizes major hurdles and supporting data from the literature, which should inform the design of pre-clinical safety studies.
| Clinical Hurdle | Key Quantitative Findings & Observations | Context & Implications |
|---|---|---|
| Poor Cell Engraftment & Survival | Only ~5% of delivered stem cells engraft within 24 hours in human studies; long-term survival is even lower [65]. | Explains the limited and inconsistent therapeutic benefits seen in clinical trials (e.g., only 2-5% LVEF improvement in heart failure trials). Strategies to enhance survival are critical [65]. |
| Tumorigenicity Risk from PSCs | The minimal threshold for tumor formation from undifferentiated hESCs/hiPSCs is estimated to be on the order of >10^5 cells [65]. | While a concern, the risk is mitigated by poor cell survival and advanced differentiation protocols that deplete undifferentiated cells. |
| Dose-Response Inconsistency | Clinical studies show conflicting results: one study found low-dose CD34+ cells more effective for angina, while another found a positive relationship between cell dose and myocardial perfusion [65]. | Highlights that delivered dose does not equal retained dose. Cell fate imaging is needed to understand the true dose-response relationship. |
| In Vivo Teratoma Assay | This is the gold-standard assay for assessing both pluripotency and tumorigenic potential [64]. | A positive result confirms pluripotency but also indicates a safety risk. For therapy, cells must be unable to form teratoma in mice [64]. |
The Scientist's Toolkit: Essential Reagents & Materials
| Item | Function / Explanation | Example Application |
|---|---|---|
| ROCK Inhibitor (Y-27632) | A small molecule that significantly improves the survival of human pluripotent stem cells (hPSCs) after single-cell dissociation and freezing/thawing by inhibiting apoptosis [67] [68]. | Used during passaging, cryopreservation, and post-thaw plating to increase cell viability and attachment efficiency. |
| BDNF & NGF | Brain-Derived Neurotrophic Factor (BDNF) and Nerve Growth Factor (NGF) are critical neurotrophins. BDNF stimulates cholinergic differentiation, while NGF controls maturation and survival of specific neurons like BFCNs [66]. | Essential components in differentiation media for basal forebrain cholinergic neurons (BFCNs). |
| B-27 Supplement | A serum-free supplement optimized for the long-term survival and maintenance of neurons and neural stem cells in culture. | Used in neural differentiation and neural stem cell culture media. Its correct use and freshness are critical for cell health [67]. |
| CHIR99021 | A highly selective and potent inhibitor of Glycogen Synthase Kinase 3 (GSK-3). It activates Wnt/β-catenin signaling, a pathway critical for initiating the differentiation of various cell lineages, including cardiomyocytes [69]. | Used as the first step in many directed differentiation protocols, such as cardiac differentiation from hPSCs. |
| Geltrex/Matrigel | Commercially available basement membrane extracts rich in laminin, collagen, and other proteins. They provide a defined substrate that supports the attachment and growth of hPSCs and neural cells in feeder-free culture systems [67] [68]. | Used to coat tissue culture plates for the adherent culture of hPSCs and neural stem cells. |
| Essential 8 Medium | A defined, xeno-free culture medium formulated for the feeder-free growth and expansion of hPSCs. It is a simplified formulation that supports consistent cell growth [67]. | Used for the routine maintenance and passaging of human embryonic and induced pluripotent stem cells. |
Experimental Protocols & Workflows
Detailed Protocol: Assessing Tumorigenicity via the Teratoma Assay
Purpose: The teratoma assay is a critical in vivo test used to confirm the pluripotency of stem cell lines by demonstrating their ability to differentiate into tissues of all three germ layers (ectoderm, mesoderm, and endoderm). Concurrently, it is a direct test of a cell line's tumorigenic potential, making it a cornerstone of pre-clinical safety assessment [64].
Methodology:
- Cell Preparation: Harvest the stem cells (e.g., hESCs or hiPSCs) at the log phase of growth. Ensure a high viability count (>90%). Prepare a cell suspension in an appropriate, cold injection vehicle (e.g., PBS mixed with a basement membrane matrix like Matrigel).
- Host Animal Immunosuppression: Use an immunodeficient mouse model (e.g., SCID, NOD-SCID) to prevent xenogeneic rejection of the human cells. The choice of model is critical, as a false negative (no teratoma) could be due to host immune rejection rather than a lack of tumorigenicity in the cells [64].
- Injection: Load the cell suspension (typically containing 1-5 million cells per site) into a syringe. Inject the cells intramuscularly into the hind limb muscle, subcutaneously into the dorsal flank, or under the testis capsule. The intramuscular route is often preferred for easier subsequent analysis.
- Monitoring and Endpoint: Monitor the animals regularly for tumor formation over a period of 8-16 weeks. The endpoint is typically when the tumor reaches a predetermined size (e.g., 1.5 cm in diameter) or at the end of the study period.
- Histological Analysis:
- Euthanize the animal and surgically resect the resulting teratoma.
- Fix the tissue in 4% paraformaldehyde or 10% neutral buffered formalin.
- Process, embed in paraffin, and section.
- Stain sections with Hematoxylin and Eosin (H&E).
- Examine under a microscope for the presence of well-differentiated tissues representing all three germ layers, such as:
- Ectoderm: Neural tissue, pigmented cells (retinal epithelium), stratified squamous epithelium.
- Mesoderm: Cartilage, bone, muscle, adipose tissue.
- Endoderm: Respiratory epithelium, intestinal epithelium, secretory glands.
Interpretation: The formation of a teratoma containing tissues from the three germ layers confirms the pluripotency of the injected cells. For regenerative medicine, the goal is to use cell populations that have lost this capacity, meaning they should not form a teratoma in this assay [64].
Signaling Pathways in Stem Cell Fate
The diagram below illustrates the core molecular dilemma linking the networks of pluripotency and tumorigenicity.
Figure 1: Shared Molecular Machinery between Pluripotency and Tumorigenicity. Key transcription factors and regulators (e.g., Myc, KLF4) are critical for maintaining stem cell pluripotency but are also established oncogenes or linked to tumorigenesis, creating a fundamental challenge for safe therapeutic application [64].
Experimental Workflow for Differentiating Basal Forebrain Cholinergic Neurons
This workflow outlines the key stages for generating BFCNs from human pluripotent stem cells based on developmental principles.
Figure 2: BFCN Differentiation Workflow. The step-wise differentiation of human pluripotent stem cells into functional basal forebrain cholinergic neurons, mirroring in vivo development. Key markers for each stage and optional steps to enhance purity are shown [66].
Frequently Asked Questions
FAQ: Why is it important to consider a patient's age and sex when selecting a biomaterial?
The immune system undergoes significant changes with age (immunosenescence) and exhibits fundamental differences between sexes. These variations can dramatically alter how the body responds to an implanted biomaterial. For instance, men experience accelerated immune aging, including sharper declines in naive T cells and B cells, leading to a more pro-inflammatory baseline. Women often mount stronger immune responses, which, while offering better vaccine protection, can also predispose them to stronger inflammatory reactions to implants. Using a "one-size-fits-all" biomaterial ignores these biological realities, potentially leading to suboptimal integration, chronic inflammation, or implant failure [70] [71] [72].
FAQ: What are the key age-related immune changes that impact biomaterial integration?
Aging affects both the innate and adaptive arms of the immune system. Key changes include a shift in T-cell populations from naive to effector memory phenotypes, a decline in B cell function, and altered monocyte and dendritic cell activity. These changes contribute to "inflammaging"—a state of chronic, low-grade inflammation that can disrupt the delicate balance of the bone healing process. The table below summarizes critical age-related immune changes relevant to biomaterial response [70] [1] [72].
Table 1: Key Age-Related Immune Changes Impacting Biomaterial Response
| Immune Component | Change with Age | Potential Impact on Biomaterials |
|---|---|---|
| CD8+ Naive T Cells | Significant decrease starting from age 38 [70] | Reduced ability to mount new, adaptive immune responses to implants. |
| CD4+ Naive T Cells | Decrease later in life (age 69+) [70] | Similar reduced adaptive capacity. |
| B Cells (Plasmablasts) | Decrease above age 67 [70] | Impaired antibody production and humoral immunity. |
| Dendritic Cells (DCs) | Decreased numbers in late age (pDC: 75+; cDC: 81+) [70] | Weakened bridge between innate and adaptive immunity. |
| Innate Immune Cells (e.g., Monocytes) | Increased baseline inflammatory activity ("inflammaging") [71] | Higher risk of prolonged pro-inflammatory response to the implant. |
FAQ: How do sex-based immune differences influence the host response to biomaterials?
Sex differences are present throughout life and affect immune cell composition and function. Studies show that males and females have different proportions of key immune cells, such as B cells, T cells, and monocytes, both in early life and old age. These differences mean the immune systems of older men and women operate and respond to threats—including biomaterials—differently. For example, older women tend to have more active adaptive immunity, while older men have more active innate immunity [71] [73] [72].
Table 2: Key Sex-Based Immune Differences Relevant to Biomaterial Response
| Immune Parameter | Sex-Associated Difference | Potential Impact on Biomaterials |
|---|---|---|
| B Cell Proportions | Females have higher B cell proportions than males, a difference that becomes significant in older age [72]. | May lead to stronger antibody-mediated responses to biomaterials in females. |
| Naive T Cell Proportions | Women have higher proportions of naive CD4+ T cells compared to men [72]. | May influence the type and scale of the adaptive immune response to the implant. |
| Immune System Aging | Men experience accelerated immune aging; age-related changes are greater in magnitude and happen sooner [71]. | Biomaterials may encounter a more aged, inflammatory environment earlier in male patients. |
| Response to Vaccines/Therapies | Women respond more strongly to some vaccines (e.g., PCV13) [71]. | Suggests female immune systems may be more responsive to bioactive components in biomaterials. |
FAQ: What experimental strategies can I use to account for age and sex in my biomaterials research?
The most critical step is to include both sexes and a range of ages in your in vivo studies and ex vivo models. For in vitro work, you can use primary immune cells isolated from male and female donors of different ages. An advanced strategy is to employ an ex vivo human whole blood model, where blood from stratified donors is incubated with different biomaterials, followed by transcriptomic analysis (RNA-seq) to map ingredient-, sex-, and age-specific immune responses [23].
FAQ: My research focuses on bone regeneration. What specific immune cells should I monitor?
In bone regeneration, macrophages are the central orchestrators of the immune response. Their polarization from a pro-inflammatory (M1) phenotype to a pro-healing (M2) phenotype is crucial for successful repair. Other key cells include T lymphocytes (especially Th17 cells and regulatory T cells), B lymphocytes, and their associated cytokines (e.g., RANKL, OPG, TNF-α, IL-10). Your biomaterial strategy should aim to modulate the local immune microenvironment towards a pro-regenerative (M2) state [1].
Troubleshooting Guides
Problem: Excessive Inflammation or Fibrosis Around the Implant
- Potential Cause: The biomaterial is inducing a strong pro-inflammatory (M1) macrophage response that is not resolving, potentially exacerbated by an aged immune system ("inflammaging") or sex-based differences in innate immunity.
- Solution:
- Redesign Material Properties: Tune the physical properties of your biomaterial. Surface topography, stiffness, and wettability can directly influence macrophage polarization. Softer substrates often promote M2 polarization.
- Incorporate Bioactive Cues: Design biomaterials to release anti-inflammatory cytokines (e.g., IL-4, IL-10) or drugs (e.g., rapamycin) in a controlled manner to steer the immune response toward an M2, pro-regenerative state [1] [74].
- Stratify by Sex and Age: Analyze your results separately for male and female animals, and across age groups. A material that works in young males might cause fibrosis in older females due to their different immune baselines [71].
Problem: Inconsistent Performance of a Biomaterial Across Preclinical Models
- Potential Cause: The study design does not account for age and sex as biological variables, leading to high variability and masking the biomaterial's true efficacy in specific subpopulations.
- Solution:
- Standardize Experimental Cohorts: Use age- and sex-matched animals in your studies. Include groups that represent the target clinical population (e.g., older, post-menopausal females for an osteoporosis application).
- Use Advanced Profiling: Characterize the immune status of your models at baseline and post-implantation using techniques like flow cytometry, RNA-seq, or ATAC-seq. This will help you link biomaterial performance to specific immune profiles [70] [72].
- Employ an Ex Vivo Screening Model: Before moving to complex in vivo studies, use a human whole blood model from donors of different ages and sexes to screen biomaterial formulations for desirable immune activation profiles [23].
Problem: Poor Osteogenesis and Bone Healing Despite Using Osteoinductive Biomaterials
- Potential Cause: The local immunomodulatory microenvironment is not supportive of bone formation. In aged individuals or certain sex contexts, there may be a dysregulation of key cells (e.g., T cells) and cytokines that disrupt the balance between osteoclasts and osteoblasts.
- Solution:
- Target the Immuno-Microenvironment: Design biomaterials that co-deliver osteoinductive factors (e.g., BMP-2) and immunomodulatory factors (e.g., TGF-β) to simultaneously promote bone growth and create a favorable immune environment [1].
- Monitor Key Immune-Bone Axis Players: In your experiments, measure the levels of RANKL, OPG, IL-17, and TNF-α in the implant area. An imbalance in these signals can inhibit healing even with a potent osteoinductive material [1].
Experimental Protocols
Protocol 1: Ex Vivo Human Whole Blood Model for Screening Biomaterial-Induced Immune Responses
This protocol, adapted from a 2021 study, allows for high-throughput screening of biomaterial-immune interactions across donor age and sex [23].
- Objective: To assess the transcriptomic immune response of different biomaterials using whole blood from stratified human donors.
- Reagents & Materials:
- Biomaterials of interest (e.g., agarose, alginate, chitosan, GelMA, collagen)
- Fresh whole blood from healthy human donors (collected in sodium heparin tubes)
- RNA stabilization reagent (e.g., PAXgene Blood RNA tubes)
- RNA extraction kit
- RNA-seq library preparation kit
- Cell culture well plates
- Procedure:
- Donor Stratification: Collect blood from healthy volunteers stratified into groups by age (e.g., young: 20-39, elderly: 40-59) and sex (5 males and 5 females per group) [23].
- Biomaterial Coating: Coat well plates with the biomaterials of interest. A suggested starting point is 100 μL of a 0.5% (w/w) biomaterial solution per well [23].
- Blood Incubation: Add fresh whole blood to the biomaterial-coated wells and incubate for a predetermined time (e.g., 4-24 hours) under standard cell culture conditions (37°C, 5% CO₂).
- RNA Collection and Sequencing: After incubation, collect blood and stabilize RNA. Perform total RNA extraction, followed by RNA-seq library preparation and sequencing.
- Data Analysis: Perform differential gene expression analysis, pathway enrichment analysis (e.g., KEGG, GO), and immune cell deconvolution to identify age-, sex-, and ingredient-specific response signatures.
Protocol 2: Flow Cytometry Analysis of Key Immune Cell Populations in a Rodent Implantation Model
This protocol provides a methodology for characterizing the local and systemic immune response to an implanted biomaterial.
- Objective: To quantify changes in innate and adaptive immune cell populations following biomaterial implantation in a sex- and age-stratified rodent model.
- Reagents & Materials:
- Single-cell suspension from implant site (e.g., digested tissue) or peripheral blood
- Flow cytometry buffer (PBS + 2% FBS)
- Fluorescently conjugated antibodies (see "Research Reagent Solutions" below)
- Flow cytometer
- Procedure:
- Cell Harvesting: At the experimental endpoint, harvest the biomaterial implant with the surrounding tissue. Process the tissue into a single-cell suspension using enzymatic digestion (e.g., collagenase). Collect peripheral blood as a systemic reference.
- Cell Staining: Aliquot cells and stain with pre-titrated antibody panels. Include a viability dye to exclude dead cells.
- Panel 1 (Innate Cells): CD45, CD11b, Ly6G, Ly6C, F4/80. This allows identification of granulocytes, monocytes, and macrophages.
- Panel 2 (T Cells): CD45, CD3, CD4, CD8, CD44, CD62L. This allows identification of naive, central memory, and effector memory T cells.
- Panel 3 (B Cells): CD45, CD19, B220, IgD, CD38.
- Data Acquisition and Analysis: Acquire data on a flow cytometer. Analyze using flow cytometry software, gating on live, single cells to determine the frequency of each cell population. Compare results between experimental groups (e.g., young vs. old, male vs. female) and against a sham or naive control.
The Scientist's Toolkit
Table 3: Essential Research Reagents for Immune-Biomaterial Studies
| Reagent / Tool | Function / Application |
|---|---|
| High-Parameter Flow Cytometry | Simultaneous quantification of multiple immune cell surface and intracellular markers to deeply phenotype the immune response at the implant site [70] [72]. |
| RNA Sequencing (RNA-seq) | Unbiased transcriptomic profiling to discover age-, sex-, and biomaterial-specific gene expression signatures and pathways [23] [72]. |
| ATAC-seq (Assay for Transposase-Accessible Chromatin with sequencing) | Mapping epigenomic changes and chromatin accessibility in immune cells in response to biomaterials and aging [72]. |
| DNA Methylation (DNAm) Deconvolution Algorithms | Computational estimation of immune cell type proportions from bulk tissue or blood DNAm data, useful for longitudinal studies [73]. |
| Cytokine/Chemokine Multiplex Assays | Measuring concentrations of multiple soluble inflammatory mediators in serum or tissue homogenate to assess the systemic and local inflammatory state. |
| Stimuli-Responsive Polymers (e.g., pH-, enzyme-sensitive) | Base materials for constructing "smart" biomaterials that release their payload in response to specific microenvironmental cues [47]. |
Visualizing Workflows and Pathways
Diagram: Ex Vivo Screening Workflow for Personalized Biomaterials
Diagram: Key Signaling in the Bone Immunomodulatory Microenvironment
Optimizing Biodegradation Rates to Match Tissue Regeneration and Avoid Premature Failure
This technical support resource is designed to assist researchers in navigating the critical challenge of aligning biomaterial degradation with the timeline of tissue regeneration. The inherent variability in host responses to implanted materials can lead to two primary failure modes: premature degradation, which causes mechanical failure before new tissue matures, and persistent implantation, where slow degradation leads to chronic inflammation or fibrous encapsulation [7]. This guide provides targeted troubleshooting advice, data, and protocols to help you design more predictable and successful regenerative therapies.
Quantitative Data on Biomaterial Degradation
Understanding the degradation kinetics of common biomaterials is the first step in selecting the right polymer for your specific application and target tissue regeneration window. The data below summarizes key findings from recent studies.
Table 1: Experimental Degradation Kinetics of Common Biomaterials
| Polymer | Study Model / Conditions | Key Degradation Metrics | Associated Change in Mechanical Properties |
|---|---|---|---|
| Polycaprolactone (PCL) with 4% HA [75] | 3D-printed airway support on porcine trachea, 2 years | • Mass Loss: <1% (1 yr); ~10% (2 yrs)• Mol. Weight (Mn) Loss: 25% (1 yr); 50% (2 yrs) | • Elastic Modulus: Increased from 146.7 MPa to 291.7 MPa (1 yr) and 362.5 MPa (2 yrs).• Failure Mode: Transitioned to brittle failure by 2 years. |
| Polylactic Acid (PLA) [76] | In vitro / Industrial Composting | • Degrades efficiently only under industrial composting conditions (e.g., >50°C).• Degradation in natural environments (soil, marine) is significantly slower. | • Tensile Strength: 45-60 MPa (initial, for PLLA).• Elastic Modulus: 0.35-0.5 GPa (initial). Properties are highly dependent on crystallinity. |
| Bio-degradable Materials (General) [7] | In vivo implantation | • Degradation rate is a primary factor influencing the host's immune response (e.g., macrophage polarization to M1/M2 phenotypes). | • A mismatch in mechanical properties with native tissue can lead to inadequate tissue integration and fibrous encapsulation. |
Troubleshooting Guide: Common Experimental Challenges
Problem: Inconsistent Degradation Rates BetweenIn VitroandIn VivoModels
Q: My in vitro degradation tests show perfect 6-month degradation, but my small animal model shows almost no degradation after a year. What factors am I missing?
A: This common discrepancy often arises from oversimplified in vitro conditions that fail to replicate the complex biological environment [75].
- Root Cause 1: Lack of Enzymatic and Cellular Activity.
- Solution: Supplement your in vitro degradation medium with relevant enzymes (e.g., esterases, MMPs) or use cell-culture conditioned media to better simulate the inflammatory and remodeling phases of healing [8].
- Root Cause 2: Ignoring the Target Tissue Microenvironment.
- Solution: Recognize that degradation is tissue-dependent. A subcutaneous implant model may yield different kinetics than an intramuscular or tracheal one [75]. Where possible, use an implantation site that mimics your target clinical application.
Problem: Premature Mechanical Failure of Scaffold
Q: The scaffold I'm testing for bone repair loses its structural integrity and collapses much earlier than the rate of mass loss suggests it should. Why?
A: This phenomenon, known as hydrolytic embrittlement, occurs when the polymer's molecular weight decreases significantly, reducing its toughness long before actual mass loss is observed [75].
- Root Cause: Bulk Erosion and Molecular Weight Drop.
- Solution:
- Monitor Molecular Weight: Use Gel Permeation Chromatography (GPC) to track the reduction in number-average molecular weight (Mn) throughout your experiment, not just mass loss.
- Material Selection: Consider using polymers with slower degradation profiles like PCL for applications requiring longer mechanical support [75].
- Composite Design: Reinforce your polymer scaffold with ceramic components like hydroxyapatite (HA) to help maintain mechanical strength as the polymer degrades [75].
- Solution:
Problem: Chronic Inflammatory Response or Fibrous Encapsulation
Q: My scaffold shows good biocompatibility in vitro, but upon implantation, it triggers a chronic inflammatory response and becomes encapsulated in fibrous tissue, isolating it from the host.
A: This is a classic sign of a mismatch between the biomaterial and the host's immune system [7].
- Root Cause 1: Excessive or Prolonged Degradation Products.
- Solution: Modify the polymer's composition or structure to control the release rate of acidic byproducts. A sudden, localized drop in pH can exacerbate inflammation.
- Root Cause 2: Improper Surface Characteristics.
Essential Experimental Protocols
Protocol: MonitoringIn VitroHydrolytic Degradation
This protocol provides a standardized method for initial screening of degradation kinetics.
Objective: To characterize the mass loss, molecular weight change, and mechanical property evolution of a biomaterial under simulated physiological conditions.
Materials:
- Research Reagent Solutions:
- Phosphate Buffered Saline (PBS): Provides a neutral pH ionic environment.
- Sodium Azide: A bacteriostatic agent to prevent microbial growth that could confound results.
- Enzymatic Solutions: E.g., Esterase or Collagenase, to simulate enzymatic degradation.
Methodology:
- Sample Preparation: Pre-weigh (Wâ‚€) and sterilize polymer scaffolds of standardized dimensions (e.g., 5mm diameter x 2mm thick disks).
- Immersion: Immerse each sample in 10-20 mL of PBS (pH 7.4) containing 0.02% sodium azide. Maintain at 37°C under gentle agitation.
- Sampling Interval: Remove samples in triplicate at predetermined time points (e.g., 1, 4, 12, 24 weeks).
- Analysis:
- Mass Loss: Rinse retrieved samples, dry thoroughly, and weigh (Wð‘¡). Calculate percentage mass loss:
(Wâ‚€ - Wð‘¡)/Wâ‚€ × 100%. - Molecular Weight: Analyze dry samples using Gel Permeation Chromatography (GPC) to determine the change in molecular weight distribution.
- Mechanical Testing: Perform compressive or tensile tests to track changes in elastic modulus, strength, and strain at failure.
- Mass Loss: Rinse retrieved samples, dry thoroughly, and weigh (Wð‘¡). Calculate percentage mass loss:
- Advanced Simulation: Run a parallel set of samples in PBS supplemented with relevant enzymes at physiological concentrations.
Protocol: Assessing Immune Response to Degradation ProductsIn Vitro
Objective: To evaluate the potential of degradation products to modulate the immune response.
Materials:
- Research Reagent Solutions:
- Macrophage Cell Line: E.g., RAW 264.7 or primary bone-marrow derived macrophages.
- Cell Culture Media: RPMI or DMEM with serum.
- ELISA Kits: For quantifying cytokine profiles (e.g., TNF-α for M1 response; IL-10 for M2 response).
Methodology:
- Leachate Preparation: Incubate a known mass/surface area of your biomaterial in cell culture media for 24-72 hours. Filter the supernatant to sterilize.
- Cell Culture: Seed macrophages in well plates and allow them to adhere.
- Treatment: Expose cells to the material leachate (e.g., 50% leachate, 50% fresh media). Use Lipopolysaccharide (LPS) and Interleukin-4 (IL-4) as controls for M1 and M2 polarization, respectively.
- Analysis:
- Gene Expression: After 24-48 hours, perform RT-qPCR to analyze M1 (iNOS, CD86) and M2 (Arg1, CD206) marker genes.
- Protein Secretion: Use ELISA on the culture supernatant to quantify pro-inflammatory (TNF-α, IL-6) and anti-inflammatory (IL-10) cytokines [7].
Key Signaling Pathways in Degradation and Regeneration
The degradation process is not passive; it actively influences tissue regeneration through dynamic biochemical signaling.
Biodegradation Signaling Pathways
Research Reagent Solutions
Table 2: Essential Materials for Biomaterial Degradation and Host Response Studies
| Reagent / Material | Function / Role in Research | Specific Example |
|---|---|---|
| Polycaprolactone (PCL) | A slow-degrading polyester used for applications requiring extended mechanical support (e.g., bone, tracheal repair) [75]. | 3D-printed PCL-HA composites for airway stents [75]. |
| Polylactic Acid (PLA) | A versatile, bio-based polyester; degrades faster than PCL but requires specific conditions (industrial composting) for rapid breakdown [76]. | PLLA screws or scaffolds for tissue fixation and engineering. |
| RGD Peptide | A cell-adhesive peptide motif used to biofunctionalize material surfaces, enhancing cell integration and mitigating foreign body response [8]. | Covalent grafting of RGD onto PCL or PLA surfaces to improve fibroblast/osteoblast adhesion. |
| Hydroxyapatite (HA) | A bioactive ceramic used in composites to improve bone bonding (osteoconductivity) and modulate the degradation profile of polymers [75]. | PCL-HA composite for bone tissue engineering. |
| Tin(II) Octanoate (Sn(Oct)â‚‚) | A common catalyst used in the ring-opening polymerization (ROP) of lactide and other cyclic esters to create high molecular-weight polymers like PLA [76]. | Catalyst for synthesizing PLA via ROP. |
| Matrix Metalloproteinases (MMPs) | Enzymes crucial for ECM remodeling in vivo. Used in vitro to create more biologically relevant degradation environments [8]. | MMP-1 or MMP-2 added to in vitro degradation buffers to simulate inflammatory conditions. |
Advanced Models and Metrics: Validating Biomaterial Performance and Biocompatibility
Core Concepts and Recent Advances
How have recent regulatory updates, like ISO 10993-1:2025, changed the requirements for advanced biocompatibility testing?
The 2025 update to ISO 10993-1 represents a significant shift, moving from a checklist approach to a risk-management-focused paradigm deeply aligned with ISO 14971. This changes how you design advanced assays in several key ways [77]:
- Integration with Risk Management: Your biological evaluation plan must now be an integral part of the device's overall risk management file. It should clearly identify biological hazards, hazardous situations, and the potential for biological harm, estimating risk based on severity and probability [77].
- Foreseeable Misuse: You must now consider "reasonably foreseeable misuse" during categorization and testing. For example, if a device is intended for short-term use but could systematically be used for a longer period, your testing must account for the prolonged exposure scenario [77].
- Refined Exposure Assessment: The concept of "transitory" contact is removed. The standard now uses detailed definitions for "total exposure period" and "contact day," and mandates considering bioaccumulation. If a leachable chemical is known to bioaccumulate, the contact duration should be considered long-term unless justified otherwise [77].
What are the key limitations of standard biocompatibility tests that advanced assays aim to overcome?
Standard tests, while essential for regulatory approval, often fall short in predicting complex in vivo outcomes. Advanced assays address these gaps [78]:
- Predicting Dynamic Host Responses: Standard tests are often static, whereas advanced assays aim to mimic the dynamic reciprocity between the biomaterial and the host environment, including immune responses and tissue remodeling processes [8].
- Detecting Subtle or Complex Failure Modes: Conventional tests may not detect issues like subtle inflammatory cascades, interfacial debonding in complex multi-material structures, or the long-term effects of chronic inflammation [79] [78].
- Evaluating Modern Biomaterial Complexity: The anisotropic, heterogeneous, and layered nature of advanced biomaterials (e.g., bio-composites, functionally graded materials) challenges conventional inspection and testing methods [79].
Troubleshooting Advanced Assays
We are encountering high variability in our in vitro host response assays (e.g., cytokine secretion). What are the primary sources of this variability and how can we control for them?
High variability often stems from inconsistencies in material preparation, cell culture conditions, or assay endpoints. The table below outlines common sources and mitigation strategies.
Table: Troubleshooting Variability in In Vitro Host Response Assays
| Source of Variability | Specific Issue | Corrective Action |
|---|---|---|
| Material Preparation | Inconsistent surface topography or chemistry between batches. | Implement rigorous surface characterization (e.g., SEM, XPS) for each batch used in experiments [78]. |
| Extraction Process | Non-standardized extraction ratios, time, or temperature. | Adhere strictly to ISO 10993-12 guidelines. Use qualified extraction vehicles and maintain precise, documented control over extraction parameters [80]. |
| Cell System | Use of low-passage vs. high-passage cells; donor-to-donor variability in primary cells. | Standardize cell passage numbers; use pooled primary cell sources where possible to minimize donor-specific effects. |
| Assay Endpoints | Inconsistent timing of endpoint measurement (e.g., cytokine peak vs. baseline). | Perform time-course experiments to identify the optimal and most reproducible timepoint for each specific endpoint [8]. |
Our non-destructive testing (NDT) results for a composite implant are inconsistent with destructive physical analysis. What could explain this discrepancy?
Discrepancies between NDT and destructive analysis are common and often point to specific limitations of the NDT method or the material's inherent complexity [79] [81]:
- Anisotropic Signal Propagation: The anisotropic nature of composite materials causes ultrasonic or electromagnetic waves to travel at different speeds in different directions, leading to mode conversion and distorted signals that may not accurately represent the defect [79] [81].
- Signal Attenuation in Heterogeneous Materials: Layered architectures and internal boundaries scatter and attenuate NDT signals (e.g., ultrasound), reducing penetration and resolution. A defect might be visible in a cross-sectional destructive analysis but be obscured in an NDT signal [79].
- Calibration and Reference Errors: Developing a calibration procedure for an anisotropic, heterogeneous material is challenging. Using an inappropriate reference block can lead to inaccurate quantitative readings [81].
- Defect Orientation: Some NDT methods are highly sensitive to defects oriented in a specific direction. A delamination parallel to the sensor might be invisible, whereas a cross-section reveals it clearly [79].
Actionable Protocol: To resolve this, employ a multimodal NDT approach. Correlate the initial NDT method (e.g., Ultrasonic Testing) with a complementary technique. For interfacial defects like delamination, capacitive sensing can be highly effective as it detects variations in dielectric properties through insulating materials. For internal voids, micro-CT (XCT) provides high-resolution 3D data, though it may be limited by sample size [79] [81].
Advanced Experimental Protocols
Protocol 1: Non-Destructive Evaluation of Delamination in a Layered Biomaterial Composite using Capacitive Sensing
This protocol leverages capacitive sensing for high-sensitivity, non-contact detection of interfacial defects.
- Principle: Exploits differences in dielectric permittivity between the intact composite material and air-filled delaminations. A coplanar capacitive sensor creates an fringing electric field that interacts with the material's dielectric properties [79].
- Workflow Diagram:
- Key Research Reagent Solutions:
- Coplanar Capacitive Sensor Array: The core component for generating and measuring fringing capacitance. Function: Non-contact interrogation of dielectric properties [79].
- Precision Motion Stage: Allows for automated raster scanning of the sensor over the sample. Function: Ensures consistent, high-resolution data collection [79].
- Vector Network Analyzer (VNA) or Impedance Analyzer: Provides the electrical signal and measures the complex impedance/capacitance. Function: High-precision measurement of the sensor's response [79].
- Dielectric Reference Standards: Materials with known permittivity. Function: Calibration of the sensor system for quantitative assessment [79].
Protocol 2: Evaluating Integrin-Mediated Signaling in Response to a Biomaterial Surface
This destructive assay provides deep mechanistic insight into the host cell response at the biomaterial interface.
- Principle: Analyzes the activation of key signaling pathways (FAK, MAPK/ERK) downstream of integrin-ECM ligand binding when cells adhere to a novel biomaterial surface [8].
- Workflow Diagram:
- Key Research Reagent Solutions:
- Phospho-Specific Antibodies: Anti-p-FAK (Tyr397) and anti-p-ERK. Function: Enable specific detection of the activated (phosphorylated) signaling proteins [8].
- Total Protein Antibodies: Anti-FAK and Anti-ERK. Function: Serve as loading controls for data normalization and interpretation [8].
- ECM Protein-Coated Controls: Surfaces coated with Collagen I or Fibronectin. Function: Provide a positive control for robust integrin signaling activation [8].
- RGD Peptide Functionalized Surfaces: Used as an experimental variable. Function: Specifically engages integrins αvβ3 and α5β1 to test specific cell-adhesion hypotheses [8].
Table: Comparison of Advanced Non-Destructive Testing (NDT) Techniques for Biomaterials
| Technique | Physical Principle | Best For Detecting | Key Advantage | Key Limitation | Approx. Resolution |
|---|---|---|---|---|---|
| Phased Array Ultrasonic Testing (PAUT) | High-frequency sound waves | Internal voids, delamination, porosity | High penetration in polymers; can inspect complex geometries | Challenging with highly attenuative/ anisotropic materials; requires couplant | 50 - 500 µm [79] [81] |
| Capacitive Sensing | Fringing electric fields / Dielectric properties | Delamination, moisture ingress, variation in composite layup | Non-contact; high sensitivity to interfacial defects; works through insulators | Limited penetration depth; sensitive to environmental factors | 10 - 200 µm [79] |
| Infrared Thermography (IRT) | Surface temperature mapping / Heat flow | Subsurface delamination, disbonds | Rapid inspection of large areas; non-contact | Surface emissivity effects; limited depth penetration | 100 µm - 5 mm [79] [81] |
| Micro-CT (XCT) | X-ray attenuation / 3D tomography | Internal 3D structure, porosity, fiber orientation | Excellent 3D visualization; quantitative volumetric data | Limited sample size; higher cost; requires safety measures | 1 - 10 µm [81] |
Table: Key Signaling Pathways in Biomaterial-Host Interaction
| Pathway | Key Initiating Event | Primary Readouts | Significance in Biocompatibility |
|---|---|---|---|
| FAK/Src | Integrin clustering and adhesion to surface | Phosphorylation of FAK (Tyr397), Paxillin | Drives initial cell adhesion, spreading, and migration; critical for tissue integration [8]. |
| MAPK/ERK | Growth factor release / Integrin signaling | Phosphorylation of ERK1/2 | Regulates cell proliferation and differentiation; sustained activation can indicate a pro-regenerative response [8]. |
| PI3K/Akt | Integrin signaling / Growth factors | Phosphorylation of Akt (Ser473) | Promotes cell survival; protects against apoptosis in the stressful implant microenvironment [8]. |
| NF-κB | Pro-inflammatory cytokine signaling (e.g., TNF-α) / Pattern Recognition Receptors | Nuclear translocation of p65 subunit; IκBα degradation | Master regulator of inflammatory response; sustained activation indicates chronic inflammation and potential implant failure [78]. |
Technical Support Center
Frequently Asked Questions (FAQs) & Troubleshooting Guides
This section addresses common challenges in developing immunocompetent 3D in vitro models, providing evidence-based solutions to reduce experimental variability and enhance the reliability of your data on biomaterial-host interactions.
FAQ 1: Why does my 3D co-culture model show high variability in immune cell recruitment and activation?
- Problem: Inconsistent results in immune cell behavior when co-cultured with stromal cells in a 3D biomaterial scaffold.
- Background: The activation and polarization of immune cells, such as macrophages, are highly sensitive to the local microenvironment. Variability often stems from inconsistencies in the biomaterial's physical and chemical properties [7].
- Solution:
- Characterize Biomaterial Properties: Before each experiment, document key properties of your biomaterial scaffold, such as surface texture, stiffness (elastic modulus), and degradation rate, as these directly influence immune cell response [7].
- Standardize Cell Seeding: Use a defined protocol for immune cell incorporation. Ensure consistent cell numbers, viability, and seeding method (e.g., pre-mixing with hydrogel vs. subsequent perfusion).
- Monitor Soluble Factors: Regularly assay culture medium for key cytokines (e.g., IL-4, IL-13, IFN-γ) using multiplex assays to ensure the inflammatory milieu is as intended [7].
FAQ 2: How can I prevent my 3D model from failing to replicate key features of the human immune response seen in vivo?
- Problem: The model lacks physiological relevance, failing to show critical processes like relevant macrophage polarization (M1/M2) or proper neutrophil extravasation.
- Background: Simple 3D static cultures often lack the dynamic interactions and mechanical forces present in living tissues [82] [83].
- Solution:
- Incorporate Microfluidics: Utilize organ-on-a-chip (OOC) platforms to introduce fluid flow and mechanical cues like cyclic strain. This has been shown to activate biological pathways that are dormant in static models, significantly enhancing physiological relevance [83].
- Use Primary or iPSC-Derived Cells: Whenever possible, use primary human immune cells or those derived from induced pluripotent stem cells (iPSCs) to better mimic human-specific immune responses compared to immortalized cell lines [84].
- Include Multiple Immune Cell Types: Move beyond monocultures. Develop tri-cultures that include, for example, epithelial cells, fibroblasts, and macrophages to better simulate the cross-talk that dictates immune responses in vivo [85].
FAQ 3: What are the best methods for analyzing complex cell-cell and cell-biomaterial interactions within my 3D model without destroying it?
- Problem: Standard endpoint analysis methods (e.g., histology, RNA extraction) require sacrificing the model, preventing longitudinal studies and increasing inter-model variability.
- Background: Understanding the dynamics of host response requires non-invasive monitoring over time [82].
- Solution:
- Non-Invasive Imaging: Use confocal microscopy with live-cell stains or genetically encoded fluorescent reporters to track cell migration, viability, and interactions in real-time.
- Analyze Spent Media: Collect and analyze conditioned media periodically for metabolic markers (e.g., glucose/lactate), cytokines, and other secreted factors to infer cellular activity without disturbing the model [85].
- Integrate Biosensors: Employ OOC platforms that are compatible with embedded biosensors to continuously monitor parameters like oxygen tension (hypoxia) and pH, which are crucial indicators of the tissue and immune status [83].
FAQ 4: My model shows poor reproducibility between batches of biomaterial scaffolds. How can I improve consistency?
- Problem: Experimental outcomes change significantly when using different batches of the same biomaterial (e.g., hydrogels like Matrigel, or synthetic polymers).
- Background: Natural hydrogels can have batch-to-batch variations in composition, which alter the biochemical and mechanical signals presented to cells [86].
- Solution:
- Rigorous Pre-screening: Implement a quality control protocol for each new batch of biomaterial. This can include rheology to test stiffness, SDS-PAGE for protein composition, and a pilot cell culture experiment to confirm expected cell behavior.
- Shift to Synthetic Materials: Consider using defined synthetic or semi-synthetic hydrogels where the composition and mechanical properties can be precisely controlled and reproduced [86].
- Detailed Documentation: Meticulously record the batch number, lot number, and all QC data for every biomaterial used, allowing you to trace and account for variability in your results.
Detailed Experimental Protocols
The following protocols are curated to help you establish robust and reproducible immunocompetent 3D models for studying host responses to biomaterials.
Protocol 1: Establishing a Co-culture Model with Immune Cells in a 3D Scaffold
This protocol outlines the steps for creating a foundational 3D model containing stromal and immune cells to study biomaterial interactions [7] [85].
- Objective: To create a reproducible 3D co-culture system for assessing initial immune cell response to a biomaterial.
- Materials:
- Biomaterial scaffold (e.g., Collagen-Chitosan scaffold, PCL scaffold, Matrigel)
- Relevant stromal cells (e.g., fibroblasts, mesenchymal stem cells)
- Immune cells (e.g., primary monocyte-derived macrophages, THP-1 cell line)
- Cell culture medium (appropriate for all cell types)
- Cytokines for immune cell polarization (e.g., IFN-γ for M1, IL-4/IL-13 for M2)
- Methodology:
- Scaffold Preparation: Hydrate or prepare the biomaterial scaffold according to the manufacturer's instructions in a suitable well plate or microfluidic device. Ensure sterility.
- Stromal Cell Seeding: Seed the stromal cells into the scaffold at a pre-optimized density. Allow cells to adhere and proliferate for 24-48 hours to establish a baseline tissue structure.
- Immune Cell Incorporation:
- Option A (Pre-mixing): Gently mix the immune cells with the liquid biomaterial before gelation. This embeds the cells uniformly throughout the scaffold.
- Option B (Perfusion/Seeding): After the scaffold is established, carefully add immune cells in suspension on top of the scaffold, allowing them to migrate into the 3D structure. For OOC models, introduce cells through the vascular channel [83].
- Immune Polarization: After immune cell incorporation, add specific cytokine cocktails to the culture medium to polarize macrophages towards M1 (pro-inflammatory) or M2 (pro-healing) phenotypes [7].
- Maintenance: Culture the co-culture system, changing the medium as required, and monitor daily for signs of contamination or cell death.
Table 1: Key Parameters for 3D Co-culture Setup
| Parameter | Typical Range / Example | Considerations for Reproducibility |
|---|---|---|
| Stromal Cell Density | 1-5 million cells/mL [85] | Optimize for your specific scaffold porosity and size. |
| Immune-to-Stromal Cell Ratio | 1:10 to 1:2 | Varies based on research question (homeostasis vs. inflammation). |
| Scaffold Stiffness | 150 Pa - 5.7 kPa [87] | Matches the stiffness of the native tissue being modeled. |
| Polarization Cytokine Exposure | 20-50 ng/mL for 24-48 hours [7] | Titrate concentration and time to achieve desired polarization without cytotoxicity. |
Protocol 2: Integrating a 3D Model with a Microfluidic Organ-on-a-Chip Platform
This protocol describes adapting a 3D culture for an OOC system to introduce fluid flow and study dynamic processes like immune cell recruitment [83] [84].
- Objective: To create a dynamic model that simulates vascular perfusion and immune cell extravasation into a 3D tissue compartment.
- Materials:
- Organ-Chip device (e.g., Emulate Chip-S1 or Chip-R1)
- Extracellular matrix (ECM) hydrogel (e.g., Corning Matrigel)
- Endothelial cells (e.g., HUVECs)
- Tissue-specific cells (e.g., hepatocytes, epithelial cells)
- Immune cells (e.g., monocytes, neutrophils)
- Microfluidic perfusion system
- Methodology:
- Chip Priming and Coating: Sterilize the chip and coat the tissue channel with an appropriate ECM hydrogel to create the 3D tissue scaffold.
- Tissue Channel Seeding: Seed the tissue-specific cells into the ECM matrix in the tissue channel and allow them to form a 3D structure under static conditions for 1-3 days.
- Vascular Channel Lining: Seed endothelial cells into the separate vascular channel and allow them to form a confluent, tight monolayer under perfusion with low flow rate (e.g., 0.1-1.0 µL/min).
- Immune Cell Recruitment Assay:
- Introduce immune cells into the medium perfusing the vascular channel.
- Activate the endothelium or the tissue compartment by introducing an inflammatory cytokine (e.g., TNF-α) via the perfusion medium.
- Use live-cell imaging to monitor and quantify the adhesion of immune cells to the endothelium and their subsequent transmigration into the 3D tissue compartment.
- Troubleshooting Tip: If immune cells do not adhere or migrate, verify the activation of the endothelium by measuring surface adhesion molecule (e.g., ICAM-1, VCAM-1) expression and confirm the functionality of the chemokine gradient.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Immunocompetent 3D Model Development
| Reagent / Material | Function / Application | Example Products / Components |
|---|---|---|
| Basement Membrane Matrix | Provides a biologically active scaffold for organoid and 3D tissue growth; rich in ECM proteins. | Corning Matrigel [87] |
| Synthetic Hydrogels | Defined, tunable scaffolds for 3D culture; allow precise control over mechanical and biochemical properties. | Polycaprolactone (PCL), Polyethylene glycol (PEG)-based hydrogels [7] |
| Microfluidic Organ-Chips | Platforms to incorporate fluid flow, mechanical forces, and multiple tissue interfaces for enhanced physiological relevance. | Emulate Chip-S1 (Stretchable), Chip-R1 (Rigid) [83] |
| Cell Culture Assay Kits | Provide all necessary reagents and protocols for specific readouts, standardizing analysis across experiments. | Luminex xMAP (multiplex cytokine analysis), Metabolic assay kits (e.g., MTT, ATP) [86] |
| Primary Human Immune Cells | Provide human-relevant immune responses critical for predicting clinical outcomes. | Primary monocytes, macrophages, neutrophils from human donors [84] |
Visualizing Workflows and Signaling
The following diagrams illustrate key experimental setups and biological pathways relevant to immunocompetent 3D models.
Diagram 1: Immunocompetent Organ-on-a-Chip Workflow
Diagram 2: Macrophage Polarization in Biomaterial Response
Technical Support Center
Troubleshooting Guides & FAQs
FAQ 1: My multi-modal data (e.g., CT, genomics) does not align properly after acquisition. What are the primary causes and solutions?
Answer: Misalignment between multi-modal datasets is a common challenge caused by differences in spatial resolution, field-of-view, and sample deformation during preparation or transfer between instruments [88]. To resolve this:
- Implement Co-registration Algorithms: Use software tools that minimize discrepancies by aligning pixel intensities, contours, or features. Select visually distinct structures shared across modalities as fiducial markers to guide this process [88].
- Standardize Sample Preparation: For sequential imaging, use fiducial markers visible across all modalities. When combining in-vivo and ex-vivo images, be aware that organ size and structure can change post-extraction; maintaining physiological conditions ex-vivo can mitigate this [88].
- Leverage Published Frameworks: Frameworks like MCANet successfully fuse features from different anatomical regions (e.g., lungs, adipose tissue) using cross-attention mechanisms, providing a model for handling disparate data sources [89].
FAQ 2: How can I improve the predictive accuracy of my model for host response to biomaterials?
Answer: Low predictive accuracy often stems from overlooking the complexity of the immune response. Enhance your model by:
- Adopting a Multi-Modal Approach: Integrate diverse data types. For instance, combine histological images with spatial transcriptomics data to gain a more comprehensive view of the Tumor Microenvironment (TME) or host-biomaterial interface [90] [88]. One study showed that integrating radiology, pathology, and clinical information predicted therapy response with an AUC of 0.91 [90].
- Incorporating Immunomodulatory Factors: Account for specific immune cell activities. The polarization of pro-inflammatory macrophages (MPs) to anti-inflammatory states is a critical determinant of biomaterial acceptance versus rejection and can be targeted using specific agents like colony-stimulating factor 1 receptor inhibitors [36].
- Including Material Properties: Model inputs should include biomaterial properties known to influence the host response, such as surface topography, chemistry, and stiffness [36] [21].
FAQ 3: What strategies can I use to track the host immune response to an implant in real-time?
Answer: Real-time monitoring is an advanced goal that requires careful design.
- Develop and Use Multimodal Nanosensors: These sensors can be designed to achieve real-time monitoring within the tissue microenvironment [90].
- Employ Multimodal Contrast Agents: Use probes detectable by multiple imaging techniques. Examples include:
- Gadolinium-loaded quantum dots for combined MRI and fluorescence imaging (note: potential toxicity limits use to animal models) [88].
- Targeted US-MP micro-bubbles combined with ultrasound and multiphoton imaging to study vessel healing [88].
- Fluorinated probes for MRI, followed by high-resolution Raman imaging on ex-vivo tissue [88].
- Utilize Multimodal Imaging Platforms: Leverage hybrid platforms like PET/MRI scanners for simultaneous data acquisition, providing correlated anatomical and functional data [88].
FAQ 4: My computational model for tissue engineering is too slow and does not span the entire biofabrication process. How can I optimize it?
Answer: This indicates a need for more efficient and comprehensive computational strategies.
- Move Beyond Single-Stage Models: Many existing models focus on a single biofabrication stage. To improve efficiency and relevance, develop computational methods that span multiple stages and components of the biofabrication process, from design to tissue maturation [91].
- Use Accurate Biofabrication Process Models: Base your computational design on accurate models that encompass both biological and technological aspects. This intelligent design approach moves away from inefficient trial-and-error paradigms [91].
- Consider a Two-Stage Deep Learning Architecture: For complex tasks like predicting acute kidney injury from CT images, a two-stage framework (e.g., MCANet) can be effective. The first stage uses a lightweight network (e.g., ResNet-18) for feature extraction, while the second employs a deeper network (e.g., ResNet-101) for global classification, balancing cost and power [89].
Table 1: Performance Metrics of Multi-Modal Models in Healthcare
| Model / Approach | Data Modalities Integrated | Clinical Application | Key Performance Metric | Result |
|---|---|---|---|---|
| MCANet [89] | Chest CT (Lungs, Epicardial & Subcutaneous Adipose Tissue) | Prediction of AKI in Pneumonia-Associated Sepsis | Accuracy (External Test Set) | 0.981 |
| AUC (External Test Set) | 0.99 | |||
| Multimodal Fusion [90] | Radiology, Pathology, Clinical Data | Prediction of Anti-HER2 Therapy Response | AUC | 0.91 |
| LightGBM Model [89] | Imaging & Clinical Features | Prediction of AKI Onset Time | Accuracy (External Test Set) | 0.8409 |
| Multimodal Model [89] | Deep Features, Radiomics, Clinical Data | Prediction of AKI | Accuracy (External Test Set) | 0.9773 |
| AUC (External Test Set) | 0.961 |
Table 2: Biomaterial Properties and Their Immunomodulatory Impact
| Material Property | Immune System Interaction | Potential Outcome | Research Reagent / Strategy |
|---|---|---|---|
| Surface Topography (e.g., nanopatterning) [36] | Influences adhesion and activation of immune cells (e.g., MPs). | Can reduce fibrosis and Foreign Body Reaction (FBR); improves integration [36]. | Nanostructured surfaces |
| Chemical Composition (Bioactive) [36] | Can induce tailored tissue responses; degradation products may cause chronic inflammation. | Enhanced integration with host tissue (bioactivity); risk of fibrous encapsulation [36]. | Bioactive Glass (BaG), Biodegradable Polymers |
| Mechanical Properties (e.g., Stiffness) [36] | Affects MP polarization; should match target tissue. | Softer materials for brain implants reduce inflammatory reaction [36]. | Soft hydrogels, Tuned elastomers |
| Controlled Drug Release [36] | Local delivery of immunomodulators (e.g., anti-inflammatory drugs, siRNA). | Shifts MPs from pro-inflammatory to anti-inflammatory state; promotes regeneration [36]. | Drug-eluting scaffolds, siRNA-loaded nanoparticles |
Detailed Experimental Protocols
Protocol 1: A Two-Stage Deep Learning Framework for Multi-Modal Image Integration (Based on MCANet) [89]
Objective: To extract and fuse informative imaging features from multiple anatomical regions to predict a clinical outcome (e.g., sepsis-associated acute kidney injury).
Methodology:
- Data Collection & Preparation:
- Collect multi-modal patient data, such as chest CT images, clinical records, and laboratory data at admission.
- Define a region of interest (ROI) for feature extraction (e.g., lungs, epicardial adipose tissue, T4-level subcutaneous adipose tissue).
- Stage 1 - Region-Specific Feature Extraction:
- Use a lightweight convolutional neural network (CNN) like ResNet-18 to process 2D CT slices from each ROI.
- This stage is designed for efficiency, extracting distinct feature maps from each anatomical region at a low computational cost.
- Stage 2 - Multi-Scale Feature Fusion and Classification:
- Fuse the extracted features using a Multiscale Feature Attention Network (MSFAN) that employs cross-attention mechanisms. This enhances interactions and contextual understanding between features from different regions.
- The fused feature set is then fed into a deeper, more powerful classifier like ResNet-101 to model complex, global patterns and perform the final classification task.
- Model Evaluation:
- Evaluate performance using standard metrics: AUC, Accuracy, Precision, Recall, and F1-score on both internal and external test sets.
- Employ explainability techniques like Grad-CAM for visual interpretation of the model's decision-making focus.
Protocol 2: Standardized In-Vitro Evaluation of Biomaterial-Host Immune Response [21]
Objective: To systematically and reliably assess the immunomodulatory potential and regenerative capacity of biomaterials (e.g., hydrogels) before in-vivo studies.
Methodology:
- Biomaterial Preparation and Sterilization:
- Synthesize and fabricate the biomaterial according to the desired properties (e.g., hydrogel composition, stiffness).
- Ensure rigorous sterilization and, critically, test for endotoxin contamination, as endotoxins can significantly skew the immune response and lead to false results [21].
- Immune Cell Culture and Exposure:
- Culture immortalized or primary immune cells relevant to the host response, such as macrophages (MPs).
- Expose the cells to the biomaterial extract or co-culture them directly on the biomaterial surface.
- Multi-Modal Response Assessment:
- Gene Expression Analysis: Use qPCR to measure the expression of key pro-inflammatory (e.g., TNF-α, IL-1β) and anti-inflammatory (e.g., IL-10, TGF-β) markers.
- Protein Secretion Profiling: Use ELISA or multiplex immunoassays to quantify the secretion of corresponding cytokines and chemokines into the culture medium.
- Cell Phenotype Characterization: Use flow cytometry or immunocytochemistry to identify cell surface markers indicative of MP polarization (e.g., pro-inflammatory M1 vs. anti-inflammatory M2 phenotypes) [36].
- Functional Regeneration Assay:
- Co-culture the primed immune cells with regenerative cells (e.g., stem cells, fibroblasts) or use the conditioned medium from step 3.
- Assess downstream regenerative outcomes, such as stem cell differentiation, fibroblast proliferation, or extracellular matrix deposition, to link the immune response to functional tissue repair [21].
Workflow & Pathway Visualizations
Host Response Pathways
Multi-Modal Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Multi-Modal Biomaterial and Imaging Research
| Item | Function / Application |
|---|---|
| ResNet-18 / ResNet-101 [89] | Pre-trained convolutional neural networks for efficient (ResNet-18) and deep (ResNet-101) feature extraction from medical images. |
| Multiscale Feature Attention Network (MSFAN) [89] | A network module using cross-attention mechanisms to fuse features from different anatomical regions or modalities, enhancing model performance. |
| Grad-CAM [89] | An explainable AI technique that produces visual explanations for decisions from CNN-based models, highlighting important regions in an image. |
| Fiducial Markers [88] | Physical markers visible across multiple imaging modalities (e.g., CT, MRI, microscopy) used to align and co-register datasets accurately. |
| Multimodal Contrast Agents [88] | Probes (e.g., Gadolinium quantum dots, fluorinated compounds) detectable by more than one imaging technique to track cells or processes across scales. |
| Colony Stimulating Factor 1 Receptor (CSF1R) Inhibitor [36] | An immunomodulatory agent that selectively targets MP differentiation and activation, helping to shift the immune response toward a pro-regenerative state. |
| Bioactive Glass (BaG) [36] | A class of biomaterials that bond with host tissue and can be tailored to induce specific, desirable tissue responses instead of being passive. |
| Small Interfering RNA (siRNA) [36] | Used for precise genetic modulation of inflammatory pathways locally at the implant site, offering a refined control over the host immune response. |
Frequently Asked Questions
Q1: Why does the same biomaterial implant cause different immune responses in different patients? The host immune response to a biomaterial is highly individualistic due to several factors. The innate immune system recognizes materials as foreign, triggering inflammatory responses and activating immune cells like macrophages. However, the specific outcome depends on the material's surface properties (e.g., charge, hydrophobicity), the patient's unique immune system genetics, and environmental factors. This variability is a key challenge in predicting in vivo performance from in vitro tests [26] [92].
Q2: Our polymer scaffold is degrading too quickly in vivo, leading to mechanical failure. What are the key factors controlling degradation? The degradation rate of polymers is influenced by both material-intrinsic and host-specific factors. Intrinsically, the chemical composition (e.g., ester bonds in PLGA, lactic acid in PLA), crystallinity, and molecular weight are critical. In the host, the local pH, enzyme concentrations (e.g., MMPs), and inflammatory cell activity at the implantation site can drastically accelerate degradation. This is a common source of variability, as the inflammatory milieu differs between individuals and anatomical sites [26] [93].
Q3: How can we pre-clinically screen for the problem of "mechanically mismatched" implants causing stress shielding? Stress shielding occurs when a rigid implant (like a traditional metal alloy) bears all the mechanical load, preventing the surrounding bone from experiencing normal stress and leading to bone resorption. To screen for this:
- In vitro: Use mechanical testers to match the implant's effective stiffness (Young's modulus) to that of the target native tissue (e.g., ~10-30 GPa for cortical bone).
- In vivo (animal models): Utilize micro-CT imaging over time (e.g., 4, 8, 12 weeks) to quantify bone mineral density (BMD) in the peri-implant region compared to a contralateral control. A significant decrease in BMD indicates stress shielding [93] [8].
Q4: Our ceramic bone graft is performing well in a young animal model but fails in an aged model. What could be the cause? This is a classic example of how host physiology impacts biomaterial success. Aged organisms often have a diminished capacity for tissue regeneration and a altered, often chronically inflamed, immune environment (inflammaging). Your ceramic graft might rely on a robust osteogenic and angiogenic response that is compromised in the aged host. Re-evaluating your material in models that reflect the age and co-morbidities of your target patient population is crucial [92] [94].
Q5: What are the key considerations for designing a "retrievable" biomaterial for clinical trials? Respect for persons and the right to withdraw is a fundamental ethical principle. If a biomaterial is designed for maximal integration, retrieval may not be feasible. For clinical trials, you must:
- Design for Retrievability: Consider encapsulation strategies (e.g., in a mesh bag) or limit the degree of bio-integration in early-stage trials.
- Informed Consent: Clearly communicate the permanence (or retrievability) of the implant to the patient during the consent process, explaining why such a design is necessary [94].
Troubleshooting Guides
Problem: Uncontrolled and Variable Inflammatory Response to Implant
Issue: The biomaterial elicits a severe or chronic foreign body reaction (FBR), leading to excessive fibrosis (fibrous encapsulation), implant failure, or patient discomfort. The severity is inconsistent across test subjects.
Diagnosis & Analysis:
- Histopathological Analysis: Excise the implant and surrounding tissue at multiple time points (e.g., 1, 2, and 4 weeks). Section and stain with H&E for general morphology and Masson's Trichrome for collagen deposition.
- Immunohistochemistry (IHC): Stain for immune cell markers:
- CD68: To identify macrophages.
- iNOS (M1 macrophage): Indicates pro-inflammatory phenotype.
- CD206 (M2 macrophage): Indicates pro-healing/anti-inflammatory phenotype.
- A high M1/M2 ratio indicates a persistent inflammatory state.
- Cytokine Profiling: Use ELISA or multiplex assays on tissue homogenates or serum to quantify pro-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6).
Solutions:
- For Polymers/Ceramics: Modify the surface topography to include micro- or nano-scale features known to promote a favorable immune response. A surface with specific pore sizes (e.g., 30-40 μm) can promote vascularization and reduce capsule thickness [8].
- For All Material Classes: Incorporate anti-inflammatory cytokines (e.g., IL-4, IL-10) or small molecule drugs (e.g., Dexamethasone) into a coating or the bulk material for localized, controlled release to modulate the immune response [26].
- Material Selection: Consider switching to or blending with "immunomodulatory" natural biomaterials like chitosan or hyaluronic acid, which have demonstrated abilities to modulate macrophage polarization toward the M2 state [26].
Problem: Premature Degradation and Loss of Mechanical Strength
Issue: The biodegradable material (polymer or metal) degrades too quickly in the physiological environment, failing to provide mechanical support for the required healing period.
Diagnosis & Analysis:
- Mass Loss Measurement: Weigh the implant (
M_i) before implantation. After explantation, carefully clean and dry it, then weigh again (M_e). Calculate percentage mass loss:(M_i - M_e)/M_i * 100. - Mechanical Testing: After explantation, perform tensile or compressive tests on the retrieved implant and compare the values to its pre-implantation mechanical properties (e.g., Young's modulus, ultimate tensile strength).
- Surface Morphology: Use Scanning Electron Microscopy (SEM) to visualize surface pitting, cracking, or erosion patterns.
Solutions:
- For Biodegradable Metals (e.g., Mg-alloys):
- Alloying: Adjust the composition with elements like Zinc (Zn), Calcium (Ca), or rare earth elements to reduce the corrosion rate.
- Surface Coating: Apply a protective, slow-degrading coating such as calcium phosphate.
- For Biodegradable Polymers (e.g., PLA, PCL):
- Cross-linking: Increase the cross-link density of the polymer network to slow down hydrolysis and enzyme penetration.
- Copolymer Blending: Create a copolymer with a slower-degrading monomer (e.g., blending PGA with the more hydrophobic PCL) to tune the degradation profile [93].
- Structural Reinforcement: Incorporate ceramic nanoparticles (e.g., hydroxyapatite) into the polymer matrix to improve strength and slow degradation.
Comparative Data Tables
Table 1: Key Properties and Host Responses of Major Biomaterial Classes
Table summarizing the intrinsic properties and typical in vivo responses for metals, polymers, ceramics, and composites.
| Material Class | Key Subtypes & Examples | Tensile Strength (MPa) | Young's Modulus (GPa) | Degradation Timeline | Key Host Response Challenges |
|---|---|---|---|---|---|
| Metals | Stainless Steel, Titanium (Ti6Al4V), Cobalt-Chrome | 500 - 1200+ | 100 - 230 | Non-degradable (permanent) | Stress-shielding (due to high stiffness), Corrosion releasing metal ions, potential for toxicity or allergy [93] [95]. |
| Polymers | Non-degradable: PE, PMMADegradable: PLA, PCL, PLGA | 20 - 100 | 0.5 - 5 | Weeks to Years (tunable) | Inflammatory response to degradation byproducts (acidic for PLA/PGA), creep deformation, potential for excessive fibrous encapsulation [26] [93]. |
| Ceramics | Alumina, Zirconia (Bioinert)Hydroxyapatite, TCP (Bioactive) | 100 - 900 (Compressive) | 70 - 400 | Non-degradable to years (resorbable) | Brittleness and low fracture toughness, variable resorption rates, potential for poor tissue adhesion if not bioactive [95] [8]. |
| Composites | PLA/Hydroxyapatite, PCL/Bioglass, Carbon Fiber/Epoxy | Wide range (tailorable) | Wide range (tailorable) | Tunable | Interface failure between phases, complex and variable degradation profiles, potential for unknown immune responses to new material combinations [93] [8]. |
Table 2: Statistical Analysis of Degradation and Biocompatibility in Alloys
Meta-analysis data comparing different classes of metallic biomaterials, highlighting trends in mechanical and degradation properties [93].
| Alloy Class | Abbreviation | Typical Tensile Strength (MPa) | Relative Degradation Rate (in vivo) | Key Biocompatibility Notes |
|---|---|---|---|---|
| Biodegradable Low Entropy | BLE | Low | Low | Provides a baseline but often lacks sufficient strength. |
| Biodegradable Medium Entropy | BME | Medium | Highest | Offers a balance of strength and rapid degradation, suitable for temporary fixtures. |
| Biodegradable High Entropy | BHE | High | Medium | Promising for high-strength applications requiring moderate degradation. |
| Non-Biodegradable Medium Entropy | NBME | Highest | N/A (Very Slow) | Used for permanent implants where degradation is undesirable. |
Experimental Protocols
Protocol 1: High-Throughput Screening of Cell-Biomaterial Interactions
Objective: To rapidly assess the cytotoxicity and cell adhesion properties of a library of new material compositions (e.g., polymer-ceramic composites) in a statistically robust manner [96].
Materials:
- Material Library: An array of material samples (e.g., as thin films or in well-plates) with systematic variation in composition.
- Cells: Relevant cell line (e.g., MC3T3-E1 pre-osteoblasts for bone materials, NIH/3T3 fibroblasts for soft tissue).
- Reagents: Cell culture medium, fetal bovine serum (FBS), Phosphate Buffered Saline (PBS), AlamarBlue or MTT reagent, Calcein-AM/Ethidium homodimer-1 (Live/Dead stain), 4% paraformaldehyde.
Methodology:
- Sterilization: Sterilize all material samples (e.g., under UV light for 30 minutes per side).
- Seeding: Seed cells onto the material surfaces at a standardized density (e.g., 10,000 cells/cm²) in a 96-well plate format. Include tissue culture plastic (TCP) as a positive control.
- Incubation: Culture cells for 1, 3, and 7 days under standard conditions (37°C, 5% CO₂).
- Viability Assay (Day 1, 3, 7):
- Add AlamarBlue reagent (10% v/v) to the culture medium.
- Incubate for 2-4 hours.
- Transfer the supernatant to a new plate and measure fluorescence (Ex/Em ~560/590 nm).
- Live/Dead Staining (Endpoint):
- Wash samples with PBS.
- Incubate with Calcein-AM (2 µM, labels live cells green) and Ethidium homodimer-1 (4 µM, labels dead cells red) for 30 minutes.
- Image using a fluorescence microscope or high-content imaging system.
- Data Analysis: Normalize fluorescence data to the TCP control. Use statistical software (e.g., ANOVA with post-hoc testing) to identify material compositions that significantly enhance cell viability and adhesion compared to controls.
Protocol 2: In Vivo Assessment of Osseointegration and Immune Response
Objective: To evaluate the bone-bonding strength and quantify the local immune cell response to an orthopaedic implant in a rodent model [26] [8].
Materials:
- Implants: Test material (e.g., a new porous titanium coating) and a control material (e.g., smooth titanium).
- Animal Model: Rats or rabbits (approved by IACUC).
- Reagents: Ketamine/Xylazine anesthetic, 10% Neutral Buffered Formalin, decalcification solution (e.g., EDTA), paraffin, primary antibodies (e.g., anti-CD68, anti-iNOS, anti-CD206), DAB staining kit.
Methodology:
- Surgery: Perform a critical-sized defect or implant placement in the femoral condyle or tibia of the animal under aseptic conditions (n ≥ 5 per group).
- Sacrifice & Harvest: Euthanize animals at 4 and 12 weeks post-implantation. Harvest the femur with the implant in situ.
- Sample Processing:
- For Histology: Fix samples in formalin for 48 hours. Decalcify in EDTA for 2-3 weeks. Process and embed in paraffin. Section into 5 µm thick slices.
- For Mechanical Push-in Test: At 12 weeks, a separate set of implants can be tested by applying a vertical load to the implant until failure to quantify bone-implant bonding strength.
- Staining & Analysis:
- H&E and Masson's Trichrome: Assess general tissue morphology, inflammation, and bone formation at the interface.
- Immunohistochemistry (IHC): Stain sections for CD68, iNOS, and CD206. Quantify the number of positive cells in 3-5 high-power fields (HPF) adjacent to the implant.
- Data Analysis: Report bone-implant contact (BIC%) from histology and ultimate push-in force. Statistically compare the M1/M2 macrophage ratio between test and control groups. A successful implant will show higher BIC%, higher push-in force, and a lower M1/M2 ratio over time.
Signaling Pathways in Host-Biomaterial Interaction
Integrin-Mediated Cell Adhesion Pathway
Diagram Title: Integrin-Mediated Cell Adhesion and Signaling
This pathway illustrates how cells interact with the extracellular matrix (ECM) of a biomaterial. Upon binding to ECM proteins like collagen, integrin receptors cluster and activate intracellular signaling hubs called focal adhesions. This triggers the FAK/SRC pathway, which regulates cytoskeletal dynamics for cell adhesion and migration. Parallel activation of the PI3K/Akt pathway promotes cell survival, while the MAPK/ERK pathway regulates gene expression for proliferation. Biomaterial surface properties directly influence this signaling [26] [8].
Immune Response to Biomaterials
Diagram Title: Macrophage Polarization in Foreign Body Response
This diagram outlines the key immune response to an implanted biomaterial. Proteins from blood and tissue immediately adsorb onto the material's surface. This layer recruits immune cells, primarily macrophages. These macrophages can polarize into different functional states: the pro-inflammatory M1 phenotype (driven by factors like IFN-γ), which releases cytokines that can lead to chronic inflammation and fibrosis; or the pro-healing M2 phenotype (driven by IL-4/IL-13), which promotes tissue repair and integration. The material's properties heavily influence this balance [26].
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for Biomaterials Host Response Research
| Item | Function & Application |
|---|---|
| Primary Cells (e.g., HUVECs, Osteoblasts) | Provide a more physiologically relevant model than cell lines for studying cell-material interactions, angiogenesis, and bone formation. Isolated directly from tissue [8]. |
| Recombinant Cytokines (e.g., IL-4, TGF-β1) | Used in vitro to polarize immune cells (e.g., driving macrophages to M2 state with IL-4) or to induce differentiation of stem cells (e.g., osteogenesis with BMP-2) [26]. |
| Matrix Metalloproteinase (MMP) Assay Kits | Quantify the activity of MMP enzymes (e.g., MMP-2, MMP-9) in tissue homogenates or cell culture supernatant. Critical for monitoring ECM remodeling around degradable implants [8]. |
| AlamarBlue / MTT Reagents | Colorimetric or fluorometric indicators of cell metabolic activity. The standard for in vitro cytotoxicity and proliferation screening on new material surfaces [96]. |
| Decellularized ECM (dECM) Powder | Serves as a biologically active coating or bioink component to create a native-like, pro-regenerative microenvironment for cells in vitro and in vivo [26] [33]. |
| RGD Peptide | A synthetic peptide sequence (Arg-Gly-Asp) that can be covalently grafted to material surfaces to promote specific integrin-mediated cell adhesion, improving biointegration [8]. |
| Anti-CD68 / iNOS / CD206 Antibodies | Key tools for Immunohistochemistry (IHC) to identify and quantify total macrophages (CD68), pro-inflammatory M1 macrophages (iNOS), and pro-healing M2 macrophages (CD206) in tissue sections [26]. |
Frequently Asked Questions & Troubleshooting Guides
Biomaterial Integration & Host Response
Q: Our biomaterial implant shows excessive fibrous capsule formation in vivo. What key material properties should we investigate?
A: Excessive fibrotic encapsulation is often a sign of a suboptimal host response. Your investigation should focus on these key material properties and their characterization:
- Biocompatibility and Cytocompatibility: Ensure the material supports cell growth and function without eliciting a severe adverse response. Standardized in vitro tests (e.g., ISO 10993) for cell viability and proliferation are crucial first steps [97].
- Surface Characteristics: The material's surface is the primary interface with host tissue. Modifications that enhance cellular adhesion and tissue integration can mitigate the foreign body reaction. Check surface properties like roughness, charge, and chemical functional groups [98] [97].
- Degradation Behavior: The degradation rate should match the tissue regeneration pace. A material that degrades too slowly can sustain a chronic inflammatory response, while one that degrades too quickly may not provide adequate support. Monitor degradation products, as they can also be immunogenic [98] [97].
Troubleshooting Guide: High Fibrous Capsule Thickness
| Observation | Potential Cause | Investigation & Resolution Strategies |
|---|---|---|
| Thick, avascular capsule | Chronic inflammation from poor biocompatibility or toxic leachates. | 1. Review Material Purity: Analyze synthesis and sterilization processes for potential contaminants [99].2. Test Degradation Products: Assess the cytotoxicity of material breakdown products in vitro [98].3. Modify Surface Chemistry: Apply coatings (e.g., with cell-adhesive peptides like RGD) to improve integration [98] [35]. |
| Rapid capsule formation | Material is perceived as a foreign body, triggering a severe initial immune response. | 1. Characterize Mechanical Mismatch: Ensure the material's stiffness (Young's modulus) is comparable to the target native tissue to avoid stress shielding [97].2. Incorporate Immunomodulatory Cues: Use "smart" biomaterials that release anti-inflammatory cytokines (e.g., IL-4) to promote a pro-regenerative immune cell (M2 macrophage) phenotype [35]. |
Assessing Angiogenic Potential
Q: When evaluating angiogenesis in 3D hydrogels, we observe poor endothelial cell sprouting and non-lumenized structures. Is this a problem with our cells or the matrix?
A: This is a common challenge, particularly with synthetic biomaterials. The issue likely lies with the physical properties of your hydrogel matrix. Follow this troubleshooting path:
- First, Verify Your Assumptions and Controls: Confirm that your endothelial cells are healthy and that your pro-angiogenic growth factor cocktails are active. Always include a positive control, such as a low-concentration (e.g., 3-4 mg/mL) fibrin or collagen type I hydrogel, which are known to support robust sprouting [100] [101].
- Investigate Matrix Porosity: A critical factor is the hydrogel's permeability, which is a measure of its porosity. Nanoscale pore sizes in many synthetic hydrogels can physically restrict collective cell migration and lumen formation.
- Solution: Increase matrix microporosity. Research shows that incorporating sacrificial gelatin microgels into a synthetic dextran-based hydrogel can create cell-scale pores, enabling the formation of lumenized, multicellular sprouts in vitro and enhancing cell invasion in vivo [101].
Troubleshooting Guide: Poor Angiogenic Sprouting
| Observation | Potential Cause | Investigation & Resolution Strategies |
|---|---|---|
| Minimal cell invasion | Insufficient matrix degradation or lack of adhesive ligands. | 1. Incorporate Proteolytic Sites: Use crosslinkers that are sensitive to Matrix Metalloproteinases (MMPs) secreted by invading cells [35].2. Add Bioactive Ligands: Functionalize the hydrogel with peptides (e.g., RGD) to promote integrin-mediated cell adhesion and migration [101]. |
| Sprouts lack lumens | Excessive matrix density or nanoscale porosity physically restrains cells. | 1. Modulate Matrix Density: Titrate the polymer concentration downward. In collagen and fibrin, higher density can increase sprouting but decrease invasion speed [101].2. Engineer Microporosity: Use the composite materials approach with sacrificial microgels to increase pore size [101]. |
Quantification and Benchmarking
Q: How can we quantitatively benchmark our new bio-ink against existing materials for printability and cell compatibility?
A: Developing simple, quantitative protocols is essential for fair comparison. You can benchmark based on the following three criteria, as demonstrated for PEGDA and GelMA bio-inks [102]:
- 1. Cell Sedimentation: Measure the homogeneity of cell distribution within the ink cartridge over time (e.g., one hour). Gel-phase inks like GelMA and shear-thinning RAPID inks prevent appreciable sedimentation, while sol-phase inks like pure PEGDA experience significant settling [102].
- 2. Cell Viability During Printing: Print cells at a constant flow rate and immediately test for membrane integrity (e.g., using a live/dead assay). In one study, less than 10% of cells were damaged in PEGDA and GelMA, while a novel RAPID ink saw less than 4% damage [102].
- 3. Cell Viability After Curing: Expose cells to the ink-specific curing conditions (e.g., light for photopolymerizing inks, ionic solution for alginate) for a set time and test viability. Over 50% of cells near the edges of PEGDA and GelMA droplets were damaged after curing, compared to fewer than 20% for RAPID inks cured in CaClâ‚‚ [102].
Quantitative Benchmarking Data
| Bio-ink Type | Cell Sedimentation (after 1 hour) | Acute Cell Damage (during extrusion) | Cell Damage Post-Curing (5-minute exposure) |
|---|---|---|---|
| PEGDA | Significant settling | < 10% | > 50% (near droplet edges) |
| PEGDA with Xanthan Gum | Prevented settling | Data Not Available | Data Not Available |
| GelMA | Prevented settling | < 10% | > 50% (near droplet edges) |
| RAPID Inks | Prevented settling | < 4% | < 20% (near droplet edges) |
| Hydrogel Type | Protein Concentration | Young's Modulus | Permeability (Porosity) | EC Sprout Morphology (in vitro) | Implant Stability (in vivo) |
|---|---|---|---|---|---|
| Collagen I | 3 mg/mL | Low | High (Microporous) | Lumenized, multicellular | Rapidly resorbed |
| Collagen I | 6 mg/mL | Medium | Medium | Lumenized, multicellular | Rapidly resorbed |
| Fibrin | 5 mg/mL | Low | High (Microporous) | Lumenized, multicellular | Rapidly resorbed |
| Fibrin | 15 mg/mL | Medium | Medium | Lumenized, multicellular | Rapidly resorbed |
| Dextran (DexVS) | 10 wt% | High | Low (Nanoporous) | Few, non-lumenized sprouts | Stable size & shape |
| Microporous DexVS | 10 wt% + Microgels | High | Engineered Microporosity | Lumenized, multicellular | Stable size & shape |
Detailed Experimental Protocols
This protocol assesses cell compatibility during the bioprinting process itself, not just long-term after culture.
A. Cell Sedimentation Assay
- Prepare Bio-ink: Mix your cell suspension (e.g., 3T3 fibroblasts) with the bio-ink polymer precursor to achieve the desired cell density.
- Load and Wait: Load the cell-laden bio-ink into a standard printing cartridge. Allow it to stand undisturbed for one hour at room temperature.
- Sample and Count: Carefully sample the bio-ink from the top and bottom of the cartridge. Dissociate or lyse the bio-ink as needed and count the cell concentration in each sample using a hemocytometer or automated cell counter.
- Analyze: A homogeneous cell distribution (similar counts top and bottom) indicates good resistance to sedimentation.
B. Cell Viability During Extrusion
- Print into Viability Assay: Set up a constant, moderate flow rate (e.g., 75 µL/min). Extrude the cell-laden bio-ink directly into a container holding a cell membrane integrity dye, such as propidium iodide.
- Immediate Analysis: The dye will immediately stain cells with compromised membranes. Count the percentage of stained (dead) cells versus the total number of cells to quantify acute shear-induced damage.
C. Cell Viability After Curing
- Print and Cure: Print small droplets of the cell-laden bio-ink and subject them to the standard curing conditions (e.g., UV light for photocrosslinking, CaClâ‚‚ solution for ionic crosslinking) for a defined period (e.g., 5 minutes).
- Assess Viability: After curing, incubate the constructs with a live/dead viability assay (e.g., calcein-AM/propidium iodide). Image the droplets using fluorescence microscopy, paying special attention to cells near the edges which experience the harshest curing conditions.
- Quantify: Calculate the percentage of dead cells in the vulnerable outer regions of the droplet.
This microfluidics-based protocol allows for high-throughput, quantitative comparison of angiogenic sprouting in different biomaterials.
- Device Fabrication: Use standard soft lithography to create polydimethylsiloxane (PDMS) microfluidic devices. The design should feature a central gel chamber flanked by two media channels.
- Hydrogel Loading and Polymerization:
- Insert a gelatin-coated needle into the gel chamber to pre-form a channel.
- Inject the hydrogel precursor solution (e.g., collagen, fibrin, or DexVS mixed with endothelial cells if desired) into the central chamber and allow it to polymerize.
- Hydrate the gel overnight to dissolve the gelatin coating and remove the needle, leaving behind a hollow, cylindrical channel.
- Cell Seeding:
- Introduce a suspension of human umbilical vein endothelial cells (HUVECs) into the hollow channel. The cells will adhere to the channel wall, forming a confluent endothelial monolayer that mimics a parent blood vessel.
- Inducing Sprouting:
- Establish a stable chemokine gradient by flowing a medium containing pro-angiogenic factors (e.g., VEGF) through one adjacent media channel and a basal medium through the other.
- Imaging and Quantification:
- After 2-5 days, image the 3D sprouting using confocal microscopy.
- Quantify key morphometric parameters, including:
- Invasion Depth: Distance from the parent vessel to the sprout tip.
- Sprout Diameter: Average width of the sprouts.
- Number of Sprouts: Per unit length of the parent vessel.
- Lumenization: Assessed via cross-sectional imaging or perfusion with a fluorescent dye.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function & Application |
|---|---|
| Gelatin Methacrylate (GelMA) | A widely used, UV-light-polymerizable bio-ink derived from denatured collagen. It is cell-adhesive and forms a gel-phase material that prevents cell sedimentation [102]. |
| Poly(ethylene glycol) diacrylate (PEGDA) | A synthetic, bio-inert hydrogel precursor. Often modified with cell-adhesive peptides (e.g., RGD) and is commonly used as a benchmark material for its high porosity when crosslinked [102]. |
| Type I Collagen | A natural ECM protein extracted from tissues. Forms a microporous hydrogel at neutral pH that supports robust endothelial cell tubulogenesis and sprouting, serving as a gold-standard for angiogenesis assays [100] [101]. |
| Fibrin | A natural hydrogel formed from the polymerization of fibrinogen, a key protein in blood clotting. Models a wound-healing ECM and is highly supportive of angiogenic sprouting [100] [101]. |
| Matrix Metalloproteinase (MMP)-Sensitive Peptides | Crosslinkers (e.g., containing the sequence VPM) that allow cells to degrade and remodel their surrounding matrix, which is crucial for 3D cell migration and invasion in processes like angiogenesis [35]. |
| RGD Peptide | A tri-peptide (Arg-Gly-Asp) sequence found in many ECM proteins. It is conjugated to biomaterials (especially synthetic ones) to promote integrin-mediated cell adhesion [101]. |
| Sacrificial Gelatin Microgels | Micron-sized particles of crosslinked gelatin. When mixed into a hydrogel precursor, they create a composite material. After polymerization, the gelatin is dissolved, leaving behind interconnected micropores that facilitate cell migration and nutrient diffusion [101]. |
Experimental Workflows & Conceptual Diagrams
Biomaterial Integration and Host Response Pathways
Angiogenesis-on-a-Chip Experimental Workflow
Conclusion
Overcoming variability in biomaterial host responses necessitates a paradigm shift from a one-size-fits-all approach to a predictive, personalized framework. The integration of a 'bottom-up' design philosophy with AI-powered informatics and advanced, immunocompetent validation models provides a robust roadmap. Future progress hinges on multidisciplinary collaboration to translate these strategies into clinically viable solutions, ultimately enabling the development of next-generation biomaterials that reliably and predictably integrate with the host for improved therapeutic outcomes in regenerative medicine and drug development.
References
- 1. Research Progress on Biomaterials with Immunomodulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12412535/]
- 2. Physical cues in biomaterials modulate macrophage ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1640560/full]
- 3. Biomaterial Strategies of Macrophage Behaviour in Bone ... [https://link.springer.com/article/10.1007/s40883-025-00443-8]
- 4. Macrophage Signaling Pathways in Health and Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171086/]
- 5. "The Impact of Biomaterial Characteristics on Macrophage ... [https://jdc.jefferson.edu/otofp/83/]
- 6. Engineering macrophage responses through 3D scaffold ... [https://www.sciencedirect.com/science/article/pii/S2590006425008993]
- 7. Biological responses to biomaterials: a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12068782/]
- 8. Biomaterials in tissue repair and regeneration: key insights ... [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2025.1565810/full]
- 9. Immune cell diversity and regenerative markers reveal ... [https://www.nature.com/articles/s41598-025-11679-3]
- 10. Molecular Signaling in Biomaterial-induced Foreign Body ... [https://pubmed.ncbi.nlm.nih.gov/40981767/]
- 11. FOREIGN BODY REACTION TO BIOMATERIALS - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2327202/]
- 12. Exploring the Overlooked Roles and Mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10081717/]
- 13. Macrophages and fibroblasts in foreign body reactions [https://www.sciencedirect.com/science/article/pii/S2590006423002430]
- 14. Overcoming immune hurdles to implant longevity [https://www.nature.com/articles/s41551-024-01276-6]
- 15. Biomaterials by design: Harnessing data for future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8628044/]
- 16. Controlling Experimental Parameters to Improve ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2020.604236/full]
- 17. Biological responses to physicochemical properties of ... [https://pubs.rsc.org/en/content/articlehtml/2020/cs/d0cs00103a]
- 18. Biomaterial-directed cell behavior for tissue engineering - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7839921/]
- 19. 4.2 Biocompatibility and Host Response [https://fiveable.me/biomedical-engineering-i/unit-4/biocompatibility-host-response/study-guide/0K6Ib7u93f43oouQ]
- 20. A review of biomaterial degradation assessment ... [https://www.nature.com/articles/s41529-024-00487-1]
- 21. Interplay between biomaterials and the immune system [https://www.sciencedirect.com/science/article/pii/S1742706122007255]
- 22. Design of Experiments in the Advancement of Biomaterial [https://encyclopedia.pub/entry/40331]
- 23. The personalized application of biomaterials based on age ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961221005342]
- 24. Gene-Specific Sex Effects on Susceptibility to Infectious ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.712688/full]
- 25. Dynamically stiffening biomaterials reveal age- and sex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11063519/]
- 26. exploring the interplay between natural biomaterials and host ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10627157/]
- 27. Material Cues as Potent Regulators of Epigenetics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5409508/]
- 28. When epigenetics meets bioengineering—A material ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5785488/]
- 29. Context clues: the importance of stem cell-material ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3970235/]
- 30. Epigenetic memory in induced pluripotent stem cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3150836/]
- 31. Mechanical memory stored through epigenetic remodeling ... [https://www.sciencedirect.com/science/article/pii/S0006349523001571]
- 32. Substrate mechanical properties bias MSC paracrine ... [https://www.sciencedirect.com/science/article/pii/S1742706123003732]
- 33. Current advances and prospects in biomaterials-guided ... [https://www.sciencedirect.com/science/article/pii/S2666138125000131]
- 34. Bottom-up Biomaterial strategies for creating tailored stem ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1581292/full]
- 35. Smart biomaterials: as active immune modulators to shape pro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12558899/]
- 36. Engineering the Immune Response to Biomaterials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12097135/]
- 37. Exploration of biomaterial and stem cell-based strategies for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07266-9]
- 38. Therapeutic Use of Integrin Signaling in Melanoma Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468206/]
- 39. Integrin Targeting and Beyond: Enhancing Cancer ... [https://www.mdpi.com/1424-8247/17/11/1556]
- 40. Insight into the role of Integrins and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11541888/]
- 41. Targeting tumor microenvironment with RGD- ... [https://www.sciencedirect.com/science/article/pii/S0304383525001004]
- 42. Integrin signaling pathways in mesenchymal stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395929/]
- 43. Recent advances in smart stimuli-responsive biomaterials ... [https://www.nature.com/articles/s41413-021-00180-y]
- 44. Stimuli-responsive smart materials: Bridging the gap ... [https://www.sciencedirect.com/science/article/abs/pii/S2405886625000314]
- 45. Smart Biomaterials in Wound Healing: Advances, ... [https://www.mdpi.com/2306-5354/12/11/1178]
- 46. Essential molecular biology methods in biomaterials ... [https://www.explorationpub.com/Journals/ebmx/Article/101344]
- 47. Smart biomaterials: as active immune modulators to shape ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1669399/full]
- 48. Reversible control of biomaterial properties for dynamically ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8159151/]
- 49. Immunogenicity of decellularized extracellular matrix scaffolds [https://pmc.ncbi.nlm.nih.gov/articles/PMC9912640/]
- 50. Decellularized extracellular matrix biomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10622743/]
- 51. Multimodal AI in Biomedicine: Pioneering the Future of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195918/]
- 52. Artificial Intelligence in Biomaterials: A Comprehensive ... [https://www.mdpi.com/2076-3417/14/15/6590]
- 53. The Role of Artificial Intelligence in Biomaterials Science [https://pmc.ncbi.nlm.nih.gov/articles/PMC12526772/]
- 54. AI-guided biomaterials and biofabrication strategies for ... [https://www.sciencedirect.com/science/article/pii/S3050562325001795]
- 55. Future Frontiers in Bioinspired Implanted Biomaterials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12422076/]
- 56. Delivery strategies to control inflammatory response [https://pmc.ncbi.nlm.nih.gov/articles/PMC4945478/]
- 57. Molecular Mechanisms That Influence the Macrophage M1 ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2014.00614/full]
- 58. Macrophages: Subtypes, Distribution, Polarization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12290311/]
- 59. Macrophage polarization in cancer and beyond: from ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525003386]
- 60. Mediators leading to fibrosis - how to measure and control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2946622/]
- 61. Advanced strategies to thwart foreign body response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9472022/]
- 62. Decoding Fibrotic Encapsulation in Plastic Surgery implants [https://www.sciencedirect.com/science/article/abs/pii/S0927776525006988]
- 63. Adhesive anti-fibrotic interfaces on diverse organs [https://www.nature.com/articles/s41586-024-07426-9]
- 64. Deconstructing Stem Cell Tumorigenicity: A Roadmap to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2733374/]
- 65. Potential Strategies to Address the Major Clinical Hurdles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5378463/]
- 66. Common pitfalls of stem cell differentiation: a guide to ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5002043/]
- 67. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 68. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 69. Unraveling the Inconsistencies of Cardiac Differentiation ... [https://www.sciencedirect.com/science/article/pii/S2213671118301504]
- 70. Age- and sex-associated differences in immune cell populations [https://pmc.ncbi.nlm.nih.gov/articles/PMC12309924/]
- 71. Sex Differences in Immune System Aging and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10751359/]
- 72. Sexual-dimorphism in human immune system aging [https://www.nature.com/articles/s41467-020-14396-9]
- 73. Biological sex impacts immune cell proportions and ... [https://www.nature.com/articles/s42003-025-08844-9]
- 74. Biomaterial Strategies for Selective Immune Tolerance [https://pmc.ncbi.nlm.nih.gov/articles/PMC10015875/]
- 75. Investigation of the biodegradation kinetics and associated ... [https://pubmed.ncbi.nlm.nih.gov/40154121/]
- 76. Biodegradable Plastics as Sustainable Alternatives [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471672/]
- 77. ISO 10993-1:2025 Updates —Top 10 Biological Evaluation ... [https://namsa.com/resources/blog/iso-10993-12025top-10-biological-evaluation-essentials-in-the-update/]
- 78. Advanced testing and biocompatibility strategies for ... [https://biotechsustainablematerials.biomedcentral.com/articles/10.1186/s44316-024-00018-7]
- 79. Non-Destructive Testing and Evaluation of Hybrid and ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12196977/]
- 80. Regulatory Guidelines For Biocompatibility Safety Testing [https://www.mddionline.com/regulatory-quality/regulatory-guidelines-for-biocompatibility-safety-testing]
- 81. Recent Trends in Non-Destructive Testing Approaches for ... [https://www.mdpi.com/1996-1944/18/13/3146]
- 82. The Evolution of Anticancer 3D In Vitro Models: The Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11853635/]
- 83. In Vitro Human Models Grow Up [https://emulatebio.com/press/in-vitro-human-models-grow-up/]
- 84. Beyond Animals: Revolutionizing Drug Discovery with Human ... [https://wyss.harvard.edu/news/beyond-animals-revolutionizing-drug-discovery-with-human-relevant-models/]
- 85. Better models, better treatment? a systematic review of ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1569211/full]
- 86. 3D Cell Cultures: Next Generation & New Challenges [https://drug-dev.com/cell-culture-market-3d-cell-cultures-next-generation-new-challenges/]
- 87. 3D Cell Culture Summit Roadshow 2025 [https://www.corning.com/worldwide/en/products/life-sciences/news-events/events/2025/09/3d-summit-2025.html]
- 88. Multimodal bioimaging across disciplines and scales [https://www.nature.com/articles/s44303-024-00010-w]
- 89. Integrating Multi-Modal Imaging Features for Early ... [https://www.sciencedirect.com/science/article/pii/S1076633225007445]
- 90. Multimodal Integration in Health Care - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370271/]
- 91. Computational methods for biofabrication in tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10818159/]
- 92. Top Mistakes in Experimental Design for Biologists [https://bigomics.ch/blog/common-mistakes-biologists-make-when-designing-experiments-and-analyzing-data/]
- 93. Material synthesis and design optimization of biomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11954756/]
- 94. Navigating ethical challenges in the development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9530811/]
- 95. Understanding the Different Types of Materials [https://aprcomposites.com.au/materials-science/materials-engineering/types-of-materials/]
- 96. Evolving biomaterials design from trial and error to ... [https://www.sciencedirect.com/science/article/abs/pii/S174270612500176X]
- 97. In Depth on Biomaterials in Life Sciences | Reports [https://boydbiomedical.com/knowledge-center/reports/in-depth-on-biomaterials-in-life-sciences?hsLang=en]
- 98. Extracellular matrix-based biomaterial scaffolds and the ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961216001009]
- 99. How to Troubleshoot Experimental Protocols in the Lab [https://www.linkedin.com/advice/1/what-some-strategies-troubleshooting-experimental-jekfe]
- 100. State-of-the-Art Methods for Evaluation of Angiogenesis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8077227/]
- 101. Direct comparison of angiogenesis in natural and synthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8595798/]
- 102. Quantitative criteria to benchmark new and existing bio- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5811195/]