Navigating the Maze: Overcoming Standardization Challenges in Biomaterial Testing Protocols
This article addresses the critical standardization challenges confronting researchers and developers in the biomaterials field.
Navigating the Maze: Overcoming Standardization Challenges in Biomaterial Testing Protocols
Abstract
This article addresses the critical standardization challenges confronting researchers and developers in the biomaterials field. It explores the foundational international standards and regulatory frameworks governing biomaterial testing, examines methodological complexities in applying these standards to advanced materials, provides strategies for troubleshooting common optimization hurdles, and outlines robust validation and documentation requirements. Aimed at scientists, researchers, and drug development professionals, this comprehensive review synthesizes current practices, identifies persistent gaps between standardized protocols and innovative material systems, and discusses future directions for creating more predictive and efficient testing paradigms that can keep pace with technological advancement while ensuring patient safety and regulatory compliance.
The Regulatory Landscape: Core Standards and Evolving Frameworks for Biomaterial Testing
ISO 10993 and Its Critical Role in Biological Evaluation
Frequently Asked Questions (FAQs)
Q1: What is the core purpose of the ISO 10993 series for a researcher?
The ISO 10993 series provides a framework for the biological evaluation of medical devices within a risk management process [1] [2]. Its purpose is to ensure that a device is safe for its intended use by assessing the potential for adverse biological reactions—such as toxicity, irritation, or sensitization—resulting from contact between the device materials and the human body [3]. For researchers, it shifts the approach from a standardized checklist of tests to a science-based, risk-informed justification for the testing strategy [4] [3].
Q2: What are the "Big Three" biocompatibility tests and are they always required?
The "Big Three" tests are cytotoxicity, sensitization, and irritation assessments [5]. These are considered fundamental and are required for almost all medical devices, regardless of the device's category, nature of patient contact, or duration of use [5]. Cytotoxicity testing, for example, evaluates the potential for device materials to cause cell death or inhibit cell growth using in vitro methods [6] [5].
Q3: What is the difference between "extractables" and "leachables" in material characterization?
- Extractables: Chemical constituents that can be released from a material under controlled, exaggerated laboratory conditions (e.g., using strong solvents or high temperatures) [3].
- Leachables: Substances that are released from the device under normal clinical conditions of use and can come into contact with the patient [3].
The identification and quantification of these substances, as guided by ISO 10993-18, form the basis for a toxicological risk assessment and are critical for the biological safety evaluation [7] [3].
Q4: How has the concept of "foreseeable misuse" been integrated into the biological evaluation?
Recent updates to the standards require that the biological risk assessment considers how a device might be used outside its intended purpose [8] [9]. A key example is "use for longer than the period intended by the manufacturer, resulting in a longer duration of exposure" [8]. This means researchers must now consider systematic misuse scenarios, informed by post-market surveillance data or clinical literature, during the design of the biological evaluation plan [8].
Q5: My device is chemically equivalent to an existing device. Can I avoid new biological testing?
Demonstrating biological equivalence is a recognized pathway to reduce or avoid animal testing [7]. However, under regulations like the EU MDR, the requirements are strict. You must demonstrate not only that the devices have the same materials and intended use but also that they have "similar release characteristics of substances, including degradation products and leachables" [7]. This requires a comprehensive chemical characterization and a detailed justification for any differences, making biological equivalence one of the most challenging arguments to substantiate [7].
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent or Variable Cytotoxicity Results
- Problem: Cell cultures show variable levels of cell death (lysis) or morphological changes between test runs [6].
- Investigation Protocol:
- Review Sample Preparation: Confirm that the surface-area-to-volume ratio for extractions is consistent and follows ISO 10993-12 guidelines [5]. Slight variations can significantly alter the concentration of extractables.
- Verify Extraction Conditions: Ensure temperature and duration of extraction are rigorously controlled (e.g., 37°C for 24 hours) [6].
- Check Cell Culture Health: Use low-passage-number cells and confirm that control cultures are healthy and confluent. The use of antibiotics in the culture medium can prevent interference from microbial contamination on the test material [6].
- Solution: Standardize the entire workflow from sample preparation to cell seeding. Use well-defined positive and negative controls in every test run to validate the system's performance [6] [5].
Challenge 2: Justifying the Omission of a Standard Test (e.g., Sensitization)
- Problem: A researcher wants to justify that a sensitization test is not needed for their device.
- Investigation Protocol:
- Conduct a Thorough Chemical Characterization: Perform a complete extractables and leachables study per ISO 10993-18 [7] [4]. This is a prerequisite for a science-based justification.
- Perform a Toxicological Risk Assessment: A qualified toxicologist must evaluate all identified leachable substances against established thresholds (e.g., Dose-Based Threshold, DBT) for sensitization potential [10] [3].
- Leverage Existing Clinical Data: If the device is part of a family or has a well-established material with significant clinical history, this data can be used to support the justification, provided it specifically addresses the sensitization endpoint [10].
- Solution: Document the entire process in a Biological Evaluation Plan (BEP) and Report (BER). The justification must be based on analytical data and toxicological risk assessment, not merely on the fact that a material is "well-known" [4] [3].
Challenge 3: Determining the Correct Contact Duration for a Complex Device
- Problem: A device is intended for brief contact but is routinely used multiple times on the same patient. The correct duration category (limited, prolonged, long-term) is unclear.
- Investigation Protocol:
- Define the Exposure Scenario: Determine if the contact is "daily" or "intermittent" based on the standard's definitions. A "contact day" is any day in which contact occurs, irrespective of the length of time within that day [8].
- Calculate Total Exposure Period: For multiple exposures, the total exposure period is the number of calendar days from the first to the last use on a single patient [8].
- Consider Foreseeable Misuse: Evaluate if the device could reasonably be left in place or used for longer than stated in the instructions for use [8] [9].
- Solution: A device used intermittently over 10 days, even if each contact is brief, has a total exposure period of 10 days, placing it in the "prolonged" duration category (≥24 hours to 30 days) [8]. Justify the final categorization in the BEP.
Key Research Reagent Solutions
The following table details essential materials and methods used in biocompatibility testing, as referenced in the ISO 10993 standards.
Table: Essential Reagents and Analytical Methods for Biocompatibility Testing
| Reagent / Method | Function in Biological Evaluation | Key Application Notes |
|---|---|---|
| Cell Cultures (L929, Balb 3T3) | Used in in vitro cytotoxicity testing (ISO 10993-5) to assess cell viability and morphological damage [5]. | Mammalian fibroblast cell lines are standard. Culture health is critical for reproducible results [6]. |
| Extraction Media (Saline, Culture Medium, Vegetable Oil) | Simulate the elution of leachables from a device under different physiological conditions (polar, non-polar) [5] [3]. | The choice of media is critical and should reflect the nature of bodily fluids the device will contact [3]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | An analytical method for the identification and quantification of non-volatile extractables and leachables [3]. | Highly effective for characterizing a wide range of organic compounds released from device materials. |
| Gas Chromatography-Mass Spectrometry (GC-MS) | An analytical method for identifying and quantifying volatile and semi-volatile organic leachables [3]. | Complements LC-MS to provide a comprehensive profile of substances that can migrate from the device. |
| MTT / XTT Assay Kits | Colorimetric assays that measure cell metabolic activity as an indicator of cell viability and cytotoxicity [5]. | Provides quantitative data on cytotoxicity; a reduction in activity indicates compromised cell health. |
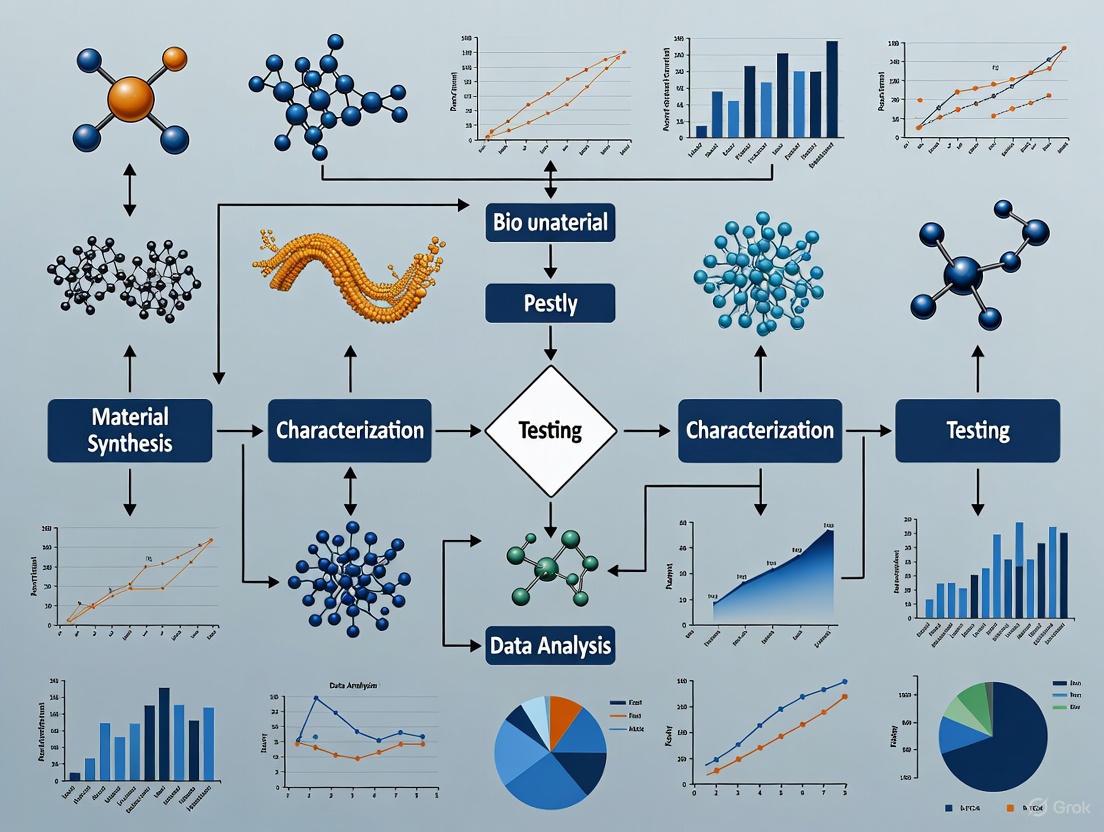
Experimental Workflow and Risk Assessment Pathways
The following diagram illustrates the integrated, risk-based biological evaluation process for a medical device as outlined in the ISO 10993 series, particularly the updated ISO 10993-1:2025.
Biological Evaluation Workflow
The updated standards embed the biological evaluation firmly within a risk management framework (aligning with ISO 14971) [8] [4]. This process is iterative, requiring re-evaluation if risks are deemed unacceptable or if new information (e.g., from post-market surveillance) becomes available [8].
The following diagram outlines the critical decision-making process for determining the necessary testing based on the device's contact nature and duration.
Testing Decision Tree
ASTM International Standards for Material-Specific Testing
ASTM International develops and publishes voluntary consensus technical standards that are critical for a wide range of materials, products, systems, and services [11]. For biomaterials, these standards provide essential specifications and test methods for evaluating the design, performance, and biocompatibility of medical devices, implants, and tissue-engineered medical products (TEMPs) [12]. Within the broader thesis on standardization challenges in biomaterial testing protocols, understanding and properly implementing these ASTM standards is fundamental to ensuring material safety, efficacy, and regulatory compliance while addressing inconsistencies in testing methodologies across research institutions and industries.
Standards by Material Category
ASTM International organizes its standards across multiple volumes, with Section 13 specifically dedicated to Medical Devices and Services [13]. The tables below summarize key ASTM standards relevant to different biomaterial categories.
Metallic Biomaterials Standards
Table 1: Selected ASTM Standards for Metallic Biomaterials
| Standard Number | Standard Title | Primary Application |
|---|---|---|
| F136-13(2021)e1 [14] | Specification for Wrought Titanium-6Aluminum-4Vanadium ELI (Extra Low Interstitial) Alloy for Surgical Implant Applications | Orthopedic and trauma implants |
| F138-13 [15] | Specification for Wrought 18Chromium-14Nickel-2.5Molybdenum Stainless Steel Alloy Bar and Wire for Surgical Implants | Corrosion-resistant surgical implants |
| F2063-18 [14] | Specification for Wrought Nickel-Titanium Shape Memory Alloys for Medical Devices and Surgical Implants | Devices utilizing shape memory effect |
| F1108-21 [14] | Specification for Titanium-6Aluminum-4Vanadium Alloy Castings for Surgical Implants | Cast orthopedic implants |
| F648-21 [14] | Specification for Ultra-High-Molecular-Weight Polyethylene Powder and Fabricated Form for Surgical Implants | Bearing surfaces in joint replacements |
Polymeric Biomaterials Standards
Table 2: Selected ASTM Standards for Polymeric Biomaterials
| Standard Number | Standard Title | Primary Application |
|---|---|---|
| F648-21 [14] | Specification for Ultra-High-Molecular-Weight Polyethylene Powder and Fabricated Form for Surgical Implants | Bearing surfaces in joint replacements |
| F997-18 [14] | Specification for Polycarbonate Resin for Medical Applications | Medical device components |
| F702-18 [14] | Specification for Polysulfone Resin for Medical Applications | Medical device components |
| F3333-20 [14] | Specification for Chopped Carbon Fiber Reinforced (CFR) Polyetheretherketone (PEEK) Polymers for Surgical Implant Applications | Load-bearing orthopedic implants |
Tissue-Engineered Medical Products (TEMPs) Standards
Table 3: Selected ASTM Standards for TEMPs and Biomaterials [16]
| Standard Number | Standard Title | Primary Application |
|---|---|---|
| F2150-19 [14] | Guide for Characterization and Testing of Biomaterial Scaffolds Used in Regenerative Medicine and TEMPs | Scaffold evaluation |
| F2212-25 [16] | Guide for Characterization of Type I Collagen as Starting Material for Surgical Implants and TEMPs | Collagen characterization |
| F2900-25 [16] | Guide for Characterization of Hydrogels Used in Regenerative Medicine | Hydrogel assessment |
| F3659-24 [16] | Guide for Bioinks Used in Bioprinting | Bioprinting materials |
| F2027-25 [16] | Guide for Characterization and Testing of Raw/Starting Materials for TEMPs | Raw material qualification |
| F2347-24 [16] | Guide for Characterization and Testing of Hyaluronan as Starting Materials | Hyaluronan-based products |
| F3368-19 [14] | Guide for Cell Potency Assays for Cell Therapy and Tissue Engineered Products | Cell functionality assessment |
Troubleshooting Common Experimental Challenges
Sample Preparation and Handling
FAQ: How should I prepare test samples for ASTM biocompatibility testing to ensure consistent and reproducible results?
Sample preparation is a critical first step detailed in standards like ISO 10993-12:2021, which is often referenced in ASTM-guided workflows [5]. Inconsistent extraction procedures are a primary source of inter-laboratory variability.
- Problem: Inconsistent cytotoxicity results between testing batches.
- Solution:
- Extraction Vehicle Selection: Use appropriate extraction vehicles as specified in the standard and relevant to your device's clinical use. Common vehicles include [5]:
- Physiological saline
- Vegetable oil
- Cell culture medium with serum
- Surface Area-to-Volume Ratio: Precisely calculate the surface area or weight of your sample and maintain the specified ratio with the extraction vehicle. Deviations can drastically alter leachable concentrations.
- Extraction Time and Temperature: Strictly adhere to the prescribed conditions (e.g., 24 ± 2 hours at 37 ± 1°C). Document any deviations as they can impact the profile of extracted chemicals.
- Aseptic Technique: For tests requiring sterility, ensure all preparation steps are performed under aseptic conditions to prevent microbial contamination that confounds results.
- Extraction Vehicle Selection: Use appropriate extraction vehicles as specified in the standard and relevant to your device's clinical use. Common vehicles include [5]:
Biocompatibility Testing
FAQ: Why are my in vitro cytotoxicity results (e.g., MTT assay) highly variable even with controlled sample preparation?
The "Big Three" biocompatibility tests—cytotoxicity, irritation, and sensitization—are required for nearly all medical devices [5]. Cytotoxicity testing, per ASTM F813 and ISO 10993-5, evaluates the material's potential to cause cell death or damage [12] [5].
- Problem: High variability in quantitative cell viability readings (e.g., MTT, XTT, Neutral Red Uptake).
- Solution:
- Cell Line and Passage Number: Use the recommended cell lines (e.g., L929 fibroblasts, Balb 3T3) and control the passage number. High-passage cells can lose sensitivity. Maintain consistent seeding density and confirm cell viability is >90% before starting the assay [5].
- Positive and Negative Controls: Always include concurrent controls. A negative control (e.g., high-density polyethylene) and a positive control (e.g., organotin-stabilized PVC) are essential for validating the test system's responsiveness [5].
- Assay Interference: Some materials can interfere with assay metrics. For example, materials that are themselves redox-active can interfere with MTT formazan production. Perform an interference check by incubating the material extract with the assay reagent in the absence of cells.
- Acceptance Criteria: While ISO 10993-5 does not define strict acceptance criteria, a cell viability of ≥70% is generally considered a positive sign, especially when testing neat extract. However, the final assessment must consider the device's nature and intended use [5].
Mechanical Testing
FAQ: My polymer scaffold's compressive modulus results show high standard deviation. How can I improve the reliability of my mechanical testing data?
Standards like ASTM D695 (compressive properties of rigid plastics) and ISO 604 provide frameworks, but methodological rigor is key [15].
- Problem: High standard deviation in compressive modulus measurements for porous polymer scaffolds.
- Solution:
- Specimen Geometry and Parallelism: Ensure test specimens have parallel end faces. Non-parallel surfaces induce uneven stress distribution. The height-to-diameter ratio should comply with the standard to prevent buckling.
- Hydration State: For biomaterials intended for hydrated use (in vivo), test them in their hydrated state. Mechanical properties of hydrogels and many polymers are highly dependent on water content. Control hydration time precisely.
- Crosshead Speed: The strain rate significantly influences the measured modulus. Strictly adhere to the crosshead speed specified in the standard (e.g., 1 mm/min for many polymers). Document any deviation.
- Preload: Apply a minimal, standardized preload to ensure full contact between the specimen and the platens before starting the test. This establishes a consistent "zero" point.
Experimental Protocols for Key Tests
Cytotoxicity Testing by Extraction (Based on ISO 10993-5 / ASTM F813)
Principle: This test assesses the cytotoxic potential of a biomaterial by exposing cultured mammalian cells to an extract of the material and evaluating cell damage and inhibition of cell growth [5].
Materials and Reagents:
- L929 fibroblast or Balb 3T3 cell line
- Appropriate cell culture medium (e.g., Dulbecco's Modified Eagle Medium with serum)
- Extraction vehicles: physiological saline, vegetable oil, culture medium without serum
- MTT reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-2H-tetrazolium bromide)
- Solvent for formazan crystals (e.g., Isopropanol, DMSO)
- Multi-well plate reader (spectrophotometer)
Methodology:
- Sample Preparation: Prepare the material extract per ISO 10993-12 using a surface area-to-volume ratio of 3 cm²/mL or 0.1 g/mL for irregular materials. Perform extraction at 37°C for 24 hours [5].
- Cell Culture: Grow L929 cells in complete medium to 80% confluence. Harvest and seed cells into 96-well plates at a density of 1 x 10â´ cells/well. Incubate for 24 hours to allow cell attachment.
- Exposure: Aspirate the culture medium from the wells. Add the material extract (neat or diluted) to the test wells. Include negative control wells (extraction vehicle alone) and positive control wells (e.g., latex or zinc diethyldithiocarbamate). Incubate the plates for 24 ± 2 hours at 37°C in a 5% CO₂ atmosphere [5].
- Viability Assessment (MTT Assay):
- After incubation, add MTT solution to each well.
- Incubate for 2-4 hours to allow formazan crystal formation.
- Carefully aspirate the medium and solubilize the formazan crystals with isopropanol.
- Measure the absorbance of each well at 570 nm using a plate reader [5].
- Data Analysis: Calculate the percentage of cell viability relative to the negative control. Cell viability ≥70% is generally considered a positive indicator, but the result must be interpreted in the context of the device's intended use [5].
Compression Testing of Porous Polymer Scaffolds (Based on ASTM D695 / ISO 604)
Principle: This test determines the compressive properties of a rigid or semi-rigid plastic scaffold, which is critical for applications in load-bearing tissue engineering, such as bone regeneration.
Materials and Reagents:
- Universal Testing Machine (UTM) with compression platens
- Phosphate Buffered Saline (PBS) for hydration
- Calipers for dimensional measurement
Methodology:
- Specimen Preparation: Fabricate cylindrical specimens with a height-to-diameter ratio as specified in the standard (e.g., 2:1). Ensure the end faces are flat and parallel. Measure and record the exact dimensions of each specimen.
- Conditioning: For biomaterials intended for hydrated use, condition the specimens by immersing them in PBS at 37°C for 24 hours prior to testing to achieve equilibrium swelling.
- Test Setup: Mount the specimen centrally on the lower platen of the UTM. Ensure the specimen's long axis is aligned with the direction of the applied force. Lower the upper platen until it just makes contact with the specimen.
- Application of Preload: Apply a small preload (e.g., 0.05 N) to ensure full contact between the specimen and the platens. This point is defined as zero displacement.
- Testing: Compress the specimen at a constant crosshead speed (e.g., 1 mm/min for many polymers) until a predetermined strain or specimen failure is reached. Record the force and displacement data throughout the test.
- Data Analysis:
- Convert force-displacement data to stress-strain data.
- The compressive modulus is calculated as the slope of the initial linear portion of the stress-strain curve.
- Compressive strength is typically taken as the maximum stress sustained by the specimen before failure (or at a specific strain offset for materials that do not fail catastrophically).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for Biomaterial Testing
| Item | Function/Application | Key Considerations |
|---|---|---|
| L929 Fibroblast Cell Line [5] | In vitro cytotoxicity testing (ISO 10993-5) | Standardized cell model; control passage number to maintain sensitivity. |
| Balb 3T3 Cell Line [5] | In vitro cytotoxicity testing (ISO 10993-5) | An alternative fibroblast cell line; ensure mycoplasma-free status. |
| MTT/XTT Reagents [5] | Colorimetric assays for quantitative cell viability. | MTT requires solubilization; XTT is ready-to-use. Check for material interference. |
| High-Density Polyethylene (HDPE) [5] | Negative control sample for biocompatibility tests. | Provides a baseline for non-cytotoxic response. |
| Zinc Diethyldithiocarbamate or Latex [5] | Positive control sample for biocomotoxicity tests. | Validates the responsiveness of the test system. |
| Cell Culture Media & Sera | Maintaining cell lines for in vitro assays. | Use consistent batches; serum-free options may be needed for specific extract tests. |
| Phosphate Buffered Saline (PBS) | Extraction vehicle and general washing buffer. | A polar extraction medium for hydrophilic compounds. |
| Vegetable Oil | Extraction vehicle (non-polar). | A non-polar extraction medium for lipophilic compounds. |
| Ultra-High-Molecular-Weight Polyethylene (UHMWPE) [14] | Reference material for wear and mechanical tests. | Well-characterized material for comparative studies (e.g., ASTM F648). |
| Type I Collagen [16] | Raw material for TEMPs and scaffold fabrication (e.g., ASTM F2212). | Source (bovine, porcine, recombinant) and purity are critical parameters. |
| HPH-15 | HPH-15, MF:C19H31N3S4, MW:429.7 g/mol | Chemical Reagent |
| Pth (1-44) (human) | Pth (1-44) (human), MF:C225H366N68O61S2, MW:5064 g/mol | Chemical Reagent |
The successful implementation of ASTM International standards for material-specific testing is paramount for overcoming standardization challenges in biomaterial research. By adhering to detailed protocols for sample preparation, biocompatibility assessment, and mechanical testing, researchers can generate reliable, reproducible, and comparable data. This technical support center provides foundational guidance for troubleshooting common experimental issues, thereby enhancing research quality and accelerating the development of safe and effective biomaterials for clinical applications.
FDA Guidance and Regional Regulatory Variations
This technical support center provides troubleshooting guides and FAQs to help researchers navigate the complex landscape of biomaterials testing regulations, directly addressing common experimental challenges.
Frequently Asked Questions
Q1: What are the core biocompatibility tests required for most medical devices? The "Big Three" biocompatibility tests—cytotoxicity, irritation, and sensitization assessment—are standard requirements for nearly all medical devices regardless of category, patient contact, or duration of use [5]. These tests evaluate fundamental biological responses to ensure device safety. Cytotoxicity testing assesses whether materials cause harm to living cells, irritation testing evaluates localized inflammatory responses, and sensitization testing identifies potential allergic reactions [5]. The International Organization for Standardization (ISO) 10993 series provides detailed guidance on conducting these assessments within a risk management framework [17] [5].
Q2: How do FDA requirements align with international standards like ISO 10993? The FDA generally aligns with ISO 10993 standards but maintains specific interpretations and additional requirements [5]. While FDA recognizes many ISO 10993 standards, it doesn't fully recognize all parts and provides supplementary guidance documents [5]. For example, the FDA's recently issued draft guidance "Chemical Analysis for Biocompatibility Assessment of Medical Devices" expands on ISO 10993-18:2020 with more specific recommendations for chemical characterization [18]. Manufacturers must provide biocompatibility data that satisfies both ISO standards and FDA's specific interpretations for regulatory submissions [5].
Q3: What alternative methods to animal testing does the FDA accept? The FDA encourages alternative methods to animal testing, particularly through chemical characterization combined with toxicological risk assessment [18]. According to recent draft guidance, acceptable approaches include targeted analysis (quantifying expected constituents), non-targeted analysis (identifying unknown chemicals in device extracts), and simulated-use or leachables studies that refine exposure estimates [18]. This aligns with the principles of Replacement, Reduction, and Refinement (3Rs) mandated by Directive 2010/63/EU in the European Union [5].
Q4: What are the key differences in biomaterials regulations across major markets? Major regulatory regions maintain distinct frameworks with varying emphasis, though all reference ISO 10993 standards:
- United States (FDA): Requires premarket submissions with biocompatibility data based on ISO 10993 with specific modifications and interpretations [17] [5].
- European Union (MDR): Mandates CE marking under the Medical Device Regulation which references ISO 10993 standards, with oversight by notified bodies rather than national health authorities [17] [5].
- Japan (PMDA): Follows "Guidelines for Basic Biological Tests of Medical Materials and Devices" which resembles ISO 10993 but recommends modified tests and sample preparations [17].
- Canada (Health Canada): Aligns with international standards through Medical Devices Regulations but maintains country-specific requirements [5].
Q5: What are common pitfalls in chemical characterization for biocompatibility? The FDA identifies several methodological challenges in recent draft guidance: variability in testing methodologies across laboratories, inappropriate extraction conditions that underestimate tissue exposure, insufficient chemical identification, and inadequate data reporting [18]. To address these, FDA recommends specific quality assurance parameters like performing extractions in triplicate, choosing conditions that simulate worst-case scenarios, and implementing detailed workflows for identifying unknown extractables [18].
Regional Regulatory Variations Comparison
Table 1: Key Regional Regulatory Variations for Biomaterials Testing
| Region/Authority | Primary Regulation | Guidance Foundation | Notable Specific Requirements |
|---|---|---|---|
| United States (FDA) | Food, Drug, and Cosmetic Act [17] | ISO 10993-1 with modifications [17] [5] | Detailed chemical characterization per draft guidance [18] |
| European Union | Medical Device Regulation (MDR) [5] | ISO 10993 series [5] | CE marking through notified bodies [17] |
| Japan (PMDA) | PMDA Regulations [5] | Modified ISO 10993 approach [17] | Different sample preparations and test modifications [17] |
| Canada (Health Canada) | Medical Devices Regulations [5] | ISO 10993 standards [5] | Country-specific submission requirements [5] |
| International | Various national regulations [5] | ISO 10993 series [5] | Lack of complete harmonization causes ambiguity [5] |
Table 2: Recent FDA Guidance Documents Relevant to Biomaterials (2024-2025)
| Guidance Topic | Status | Issue Date | Key Focus |
|---|---|---|---|
| Chemical Analysis for Biocompatibility Assessment of Medical Devices [19] | Draft | 09/19/2024 | Methodological approaches for chemical analysis [19] |
| Considerations for the Use of Artificial Intelligence | Draft | 01/07/2025 | AI support for regulatory decision-making [20] |
| Alternative Tools: Assessing Drug Manufacturing Facilities | Final | 09/12/2025 | CGMP for pharmaceutical quality [20] |
| Control of Nitrosamine Impurities in Human Drugs | Final | 09/05/2024 | Pharmaceutical quality and impurities [20] |
| Real-World Data: Assessing EHR and Claims Data | Final | 07/25/2024 | Supporting regulatory decisions with real-world evidence [20] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Biomaterials Testing
| Reagent/Material | Function/Application | Standard/Protocol Reference |
|---|---|---|
| Extraction Solvents (physiological saline, vegetable oil, DMSO, ethanol) [17] | Extract leachable components from test materials under standardized conditions [17] | ISO 10993-12:2021 [5] |
| Cell Cultures (Balb 3T3, L929, Vero cells) [5] | In vitro cytotoxicity testing using mammalian cell lines [5] | ISO 10993-5:2009 [5] |
| Viability Assays (MTT, XTT, Neutral Red Uptake) [5] | Quantitative measurement of cell survival and proliferation [5] | ISO 10993-5:2009 [5] |
| Reference Materials | Positive and negative controls for test validation [5] | ISO 10993-12:2021 [5] |
| Limulus Amebocyte Lysate | Detection of bacterial endotoxins/pyrogens [17] | Bacterial endotoxin testing [17] |
| Epi-cryptoacetalide | Epi-cryptoacetalide, MF:C18H22O3, MW:286.4 g/mol | Chemical Reagent |
| Stearidonoyl glycine | Stearidonoyl glycine, MF:C20H31NO3, MW:333.5 g/mol | Chemical Reagent |
Experimental Protocols: Key Methodologies
Cytotoxicity Testing (ISO 10993-5:2009)
Purpose: Assess whether medical device materials or extracts cause harm to living cells [5].
Methodology:
- Sample Preparation: Prepare extracts using physiological saline, vegetable oil, or cell culture medium as extraction solvents following ISO 10993-12:2021 [5]. Use surface area to volume ratios of 1.25-6 cm²/mL [17].
- Extraction Conditions: Conduct extraction at 37°C for 24 hours for cytotoxicity testing [17].
- Cell Culture Exposure: Expose cultured mammalian cells (Balb 3T3, L929, or Vero cell lines) to extracts for approximately 24 hours [5].
- Assessment Endpoints:
- Cell viability measured via MTT, XTT, or Neutral Red Uptake assays
- Morphological changes observed microscopically
- Cell detachment and lysis evaluation [5]
- Acceptance Criteria: While ISO 10993-5 doesn't define specific criteria, ≥70% cell viability (cell survival) is generally considered favorable, especially when testing neat extract [5].
Chemical Characterization (FDA Draft Guidance 2024)
Purpose: Identify and quantify chemical constituents in device extracts as an alternative to some biological testing [18].
Methodology:
- Information Gathering: Compose comprehensive device information including materials, manufacturing processes, and clinical use conditions [18].
- Test Article Selection: Use final, sterile finished devices representative of mass production [18].
- Extraction Studies:
- Perform extractions in triplicate for statistical significance
- Use exaggerated conditions to simulate worst-case scenarios
- Employ both polar and non-polar extraction media [18]
- Analytical Techniques:
- Targeted Analysis: Fully quantify expected constituents
- Non-Targeted Analysis: Identify and semi-quantify unknown extractables [18]
- Data Analysis and Reporting: Create comprehensive test reports with method summaries, protocol deviations, and detailed results with toxicological risk assessment [18].
Experimental Workflow Visualization
Biocompatibility Assessment Workflow
Global Regulatory Strategy Development
The Drive to Reduce Animal Testing and Develop Alternative Models
Troubleshooting Guides and FAQs for New Approach Methodologies (NAMs)
Common Experimental Challenges and Solutions
Q1: Our organ-on-a-chip model shows inconsistent barrier function across devices. What could be causing this variability?
A: Variability in microphysiological systems often stems from these key factors:
- Cell source and passage number: Primary cells beyond passage 5 may lose functionality, while iPSC-derived cells require rigorous differentiation quality control. Standardize using cells between passages 3-5 for consistent results.
- Microfluidic flow rates: Laminar flow must be maintained between 50-100 μL/min for most organ models. Calibrate pumps weekly and document shear stress calculations (typically 0.5-2 dyne/cm² for endothelial barriers).
- Extracellular matrix batch variability: Test each new Matrigel or collagen batch with a transepithelial electrical resistance (TEER) validation assay before experimental use. Acceptable coefficient of variation should be <15% across three devices.
- Media composition: Growth factor concentrations can degrade; prepare fresh aliquots weekly and document lot numbers for all serum-free components.
Q2: Our in silico toxicity predictions don't align with traditional in vivo data. How should we resolve these discrepancies?
A: Discrepancies often reveal human-specific biological responses that animal models cannot capture. Follow this validation protocol:
- Confirm human biological relevance: Use the FDA's ISTAND program evaluation framework to determine if your model better predicts human responses [21]. The Emulate Liver-Chip, for instance, demonstrated 87% sensitivity and 100% specificity for drug-induced liver injury detection where animal models failed [21].
- Utilize the Integrated Chemical Environment (ICE): Compare predictions against the ICE database's curated human-relevant toxicity data [22].
- Implement orthogonal validation: Run parallel tests using two additional NAMs (e.g., high-throughput screening and 3D spheroid models) to build a weight-of-evidence approach [22].
Q3: We're encountering difficulties qualifying alternative methods under ISO 10993-1:2025. What documentation is essential?
A: The 2025 standard requires robust integration with risk management frameworks [8]. Essential documentation includes:
- Biological evaluation plan: Must now include "reasonably foreseeable misuse" scenarios and total exposure period calculations, not just intended use [8].
- Risk estimation rationale: Document severity and probability of biological harm using ISO 14971 methodology, including how chemical characterization data informs these assessments [8].
- NAMs validation evidence: Provide data comparing your method's performance against traditional endpoints with statistical analysis of sensitivity, specificity, and reproducibility [8] [22].
Q4: How do we address regulatory concerns about novel biomaterials that lack animal testing data?
A: FDA's 2025 roadmap emphasizes a "totality-of-evidence" approach [23] [21]:
- Implement a tiered testing strategy: Begin with in chemico and in silico assessments, progress to increasingly complex in vitro models, and use animals only as a last resort [22].
- Leverage the FDA's ISTAND program: Qualify your Drug Development Tools through this pilot program, as demonstrated by the first Organ-on-a-Chip acceptance in September 2024 [21].
- Provide mechanistic data: Include transcriptomics, proteomics, and high-content imaging to demonstrate understanding of material-biological interactions at a molecular level [24].
Quantitative Comparison of Alternative Methods
Table 1: Performance Metrics of Validated Non-Animal Methods
| Method Type | Key Application | Validation Status | Throughput | Relative Cost | Regulatory Acceptance |
|---|---|---|---|---|---|
| Organ-on-a-Chip | Drug-induced liver injury prediction | Peer-reviewed; 87% sensitivity, 100% specificity [21] | Medium | High | Accepted into FDA ISTAND program [21] |
| In silico (AI/ML) toxicity prediction | Predictive toxicology | OECD QSAR framework; >80% concordance for many endpoints [22] | High | Low | Accepted as part of weight-of-evidence |
| High-throughput screening | Chemical prioritization | Tox21 program; >10,000 chemicals tested [22] | Very High | Medium | Accepted for prioritization |
| 3D organoids | Disease modeling | Research use; characterizing heterogeneity [22] | Medium | Medium | Early-stage qualification |
| Human-based in vitro | Biocompatibility testing | ISO 10993-1:2025 aligned for specific endpoints [8] | Medium-High | Medium | Increasing acceptance |
Table 2: Regulatory Timeline for Alternative Methods Implementation
| Timeframe | Regulatory Developments | Impact on Testing Requirements |
|---|---|---|
| Short-term (2025) | FDA roadmap implementation; ISO 10993-1:2025 adoption | Animal testing becomes "the exception rather than the rule"; increased acceptance of NAMs data in INDs [23] [8] |
| Mid-term (2026-2027) | Standards development for NAMs qualification; expanded ISTAND qualifications | Specific NAMs recognized as valid for particular contexts of use; reduced requirements for animal data [21] |
| Long-term (2028+) | Widespread adoption of qualified NAMs across regulatory agencies | Animal testing primarily for complex systemic effects not addressable by current NAMs [23] [22] |
Experimental Protocols for Key Alternative Methods
Protocol 1: Establishing a Multi-Organ Microphysiological System
Purpose: To create a connected liver-cardiac model for preclinical toxicity assessment.
Materials:
- Organ-on-a-chip platform with 2+ tissue chambers
- Primary human hepatocytes (commercial source, passage 2-4)
- iPSC-derived cardiomyocytes (30+ days differentiated)
- Serum-free organ-specific media
- TEER measurement apparatus
- Analytical platform for metabolite analysis (LC-MS recommended)
Methodology:
- Device preparation: Coat liver chamber with collagen I (50μg/mL) and cardiac chamber with fibronectin (25μg/mL). Incubate at 37°C for 2 hours.
- Cell seeding: Seed hepatocytes at 5×10ⵠcells/cm² in liver chamber. Seed cardiomyocytes at 1×10ⶠcells/cm² in cardiac chamber. Maintain static conditions for 6 hours to facilitate attachment.
- System initiation: After cell attachment, initiate flow at 50μL/hour, gradually increasing to 100μL/hour over 48 hours.
- Functional validation: Measure albumin production (hepatocytes) and beat rate (cardiomyocytes) daily for 7 days to establish baseline functionality.
- Test compound exposure: Introduce compounds through the circulatory mimetic channel at clinically relevant concentrations. Include a minimum of n=6 chips per treatment group.
- Endpoint assessment: At 24, 48, and 72 hours post-exposure, measure:
- Metabolic activity (MTT assay)
- Tissue-specific function markers
- Histological changes
- Transcriptomic changes if applicable
Troubleshooting note: If one tissue shows premature failure, check for media compatibility—custom formulations may be necessary to support multiple tissue types.
Protocol 2: Computational Prediction of Biomaterial Biocompatibility
Purpose: To predict the biocompatibility of novel polymers using in silico methods.
Materials:
- Chemical structure of test material (SMILES format)
- Access to toxicity prediction software (OECD QSAR Toolbox, EPA TEST, or commercial platforms)
- Chemical properties database (PubChem, ChemIDplus)
- Historical biocompatibility data for similar structures
Methodology:
- Descriptor calculation: Compute physicochemical descriptors including logP, molecular weight, polar surface area, and H-bond donors/acceptors.
- Read-across analysis: Identify structurally similar compounds with existing toxicity data using the OECD QSAR Toolbox. Apply a similarity threshold of >70% for reliable prediction.
- Toxicity endpoint prediction: Run QSAR models for:
- Cytotoxicity (baseline toxicity prediction)
- Sensitization potential (protein binding models)
- Genotoxicity (structural alerts for DNA reactivity)
- Dose-response modeling: Estimate the probable concentration at which effects may occur using hierarchical clustering of historical dose-response data for analogous structures.
- Uncertainty quantification: Apply the Applicability Domain Index to determine prediction reliability. Reject predictions with ADI <0.7.
- Experimental design prioritization: Use computational results to focus in vitro testing on predicted endpoints of concern.
Validation: Compare predictions against limited in vitro testing (minimum 3 endpoints) to establish model accuracy for your specific chemical space.
Research Reagent Solutions for Alternative Methods
Table 3: Essential Materials for Implementing New Approach Methodologies
| Reagent/Category | Specific Examples | Function | Key Considerations |
|---|---|---|---|
| Cells | Primary human hepatocytes, iPSC-derived cells, primary human keratinocytes | Provide human-relevant biological responses | Verify donor information, passage number, and functional validation data [22] |
| Extracellular Matrices | Matrigel, collagen I, fibrin, synthetic PEG-based hydrogels | Mimic tissue microenvironment | Test lot-to-lot variability; consider defined synthetic matrices for standardization [25] |
| Specialized Media | Organ-specific differentiation media, serum-free toxicity testing media | Support tissue-specific functions | Document all growth factors and supplements; check stability data [22] |
| Microphysiological Systems | Organ-on-a-chip platforms, 3D bioprinters, transwell systems | Provide physiological context with flow and tissue-tissue interfaces | Select systems with demonstrated reproducibility and available historical data [21] |
| Detection Assays | TEER electrodes, transepithelial electrical resistance; high-content imaging systems | Functional and structural assessment | Validate assays for 3D culture formats; establish baseline ranges [25] |
| Computational Tools | QSAR software, PBPK modeling platforms, AI/ML prediction tools | In silico prediction and data integration | Verify using known compounds before applying to novel materials [22] [24] |
Workflow Visualization
Gaps in Standards for Emerging Technologies (Nanomaterials, 3D-Printed Scaffolds)
Frequently Asked Questions (FAQs)
Q1: What are the key regulatory challenges for documenting novel nanomaterials? The regulatory landscape for nanomaterials is complex and varies significantly by region, creating a major challenge for standardization. In the European Union, REACH regulation has stringent, evolving reporting requirements for nanomaterials, including specific provisions for surface-treated nanomaterials [26]. Canada has expanded its mandatory reporting requirements with thresholds that differ from those for conventional chemicals [26]. The United States currently lacks nano-specific regulations, but regulatory bodies like OSHA are increasingly scrutinizing nanomaterial Safety Data Sheets (SDS) under existing frameworks like the Hazard Communication Standard [26]. This regulatory patchwork necessitates tailored documentation strategies for different markets.
Q2: Why do traditional Safety Data Sheet (SDS) templates fail for nanomaterials? Traditional SDS templates are inadequate because they do not capture the unique properties that govern nanomaterial behavior and toxicity. Key shortcomings include:
- Inadequate Hazard Identification: Traditional acute toxicity data may not reflect nano-specific respiratory hazards [26].
- Insufficient Composition Details: Standard templates lack fields for critical parameters like particle size distribution, surface area, shape, and surface chemistry [26].
- Generic Exposure Controls: Recommendations for standard fume hoods and gloves are often ineffective for controlling nanoparticle exposure [26].
Q3: What are the critical mechanical performance gaps in standardizing 3D-printed bone scaffolds? Standardization is challenged by the complex interplay between scaffold geometry, material composition, and processing parameters, all of which significantly influence mechanical performance [27]. For instance, studies on PLA+ scaffolds show that mechanical responses like displacement and strain vary dramatically with the lattice geometry (Gyroid, Diamond, Lidinoid) and wall thickness under the same compressive load [27]. This lack of a unified predictive model for how design choices affect mechanical outcomes is a major gap. Furthermore, balancing mechanical strength with necessary porosity for biological functions like cell migration and vascularization remains a significant challenge [28] [27].
Q4: Which 3D printing technologies are most relevant for bone scaffold fabrication, and how does the choice impact standardization? The choice of printing technology introduces variability that complicates standardization. The most common technologies include:
- Extrusion-Based Printing: Includes Fused Deposition Modeling (FDM) for thermoplastics and Direct Ink Writing (DIW) for pastes/hydrogels. Fidelity in DIW heavily depends on the ink's viscoelastic properties [28].
- Laser-Based Printing: Includes Stereolithography (SLA) and Digital Light Processing (DLP), which use light to polymerize resins with high resolution [28]. Each technology has a distinct processing window, material compatibility, and impact on the final scaffold's structural fidelity, mechanical properties, and bioactivity, creating a barrier to establishing universal standards [28].
Q5: How can researchers address the lack of specific toxicological data for nanomaterials? A transparent "weight of evidence" approach is recommended. This involves:
- Building a Data Matrix: Systematically gathering all available data (e.g., from in vitro studies, read-across from similar materials) and explicitly identifying data gaps [26].
- Documenting Reasoning: Clearly stating the justification for hazard classifications and including statements in the SDS such as: "Limited toxicity data available specifically for this nanomaterial form" [26].
- Leveraging Consortia Data: Utilizing resources like the OECD Test Guidelines for nanomaterials and ECHA's appendices to inform assessments [26].
Troubleshooting Guides
Problem 1: Inconsistent Mechanical Performance in 3D-Printed Scaffolds
Issue: Printed scaffolds exhibit unexpected mechanical failure, excessive deformation, or high batch-to-batch variability.
| Potential Cause | Diagnostic Steps | Solution & Recommended Protocol |
|---|---|---|
| Suboptimal Geometric Configuration [27] | Analyze scaffold design using Finite Element Analysis (FEA) to identify stress concentration points. | Optimize architecture using computational modeling. Studies show Gyroid lattices often outperform Diamond and Lidinoid in mechanical integrity [27]. |
| Incorrect Printing Parameters for Material [28] | Review layer height, nozzle temperature, and printing speed against material supplier specifications. | Adopt a systematic experimental design like a Taguchi L27 Orthogonal Array to identify the optimal parameter set for mechanical performance [27]. |
| Uncontrolled Porosity and Pore Size [28] [27] | Characterize scaffold porosity and pore size using micro-CT scanning. | Design scaffolds with a controlled pore size range of 700–900 μm and ensure high interconnectivity to balance mechanical and biological needs [27]. |
| Inadequate Material Selection [28] | Evaluate the degradation profile and mechanical strength (e.g., compressive modulus) of the polymer. | Select advanced materials like PLA+ for enhanced toughness over standard PLA, or use polymer-ceramic composites to improve osteoconductivity and strength [28] [27]. |
Problem 2: Regulatory Compliance and Hazard Communication for Nanomaterials
Issue: Safety Data Sheets (SDS) for nanomaterials are rejected by regulators or customers for insufficient characterization.
| Potential Cause | Diagnostic Steps | Solution & Recommended Protocol |
|---|---|---|
| Insufficient Particle Characterization [26] | Audit Section 9 (Physical/Chemical Properties) of the SDS for missing nano-specific data. | Incorporate specific measurements: particle size distribution (e.g., D50), BET surface area, and detailed shape/morphology descriptions [26]. |
| Poorly Defined Exposure Controls [26] | Review exposure control plans for engineering controls and PPE specific to nanomaterials. | Specify "HEPA-filtered local exhaust ventilation" instead of "fume hoods" and detail effective glove types (e.g., "double nitrile, 0.18mm") [26]. |
| Inadequate Hazard Identification [26] | Check if GHS classification is based on data for the bulk material, not the nano-form. | Classify based on available nano-specific data. Use clear statements about data gaps and apply a conservative, evidence-based classification [26]. |
| Omitted Information on Composition [26] | Verify that all nanomaterials are listed with specific CAS numbers or detailed descriptions. | Disclose all nano-ingredients. Use precise descriptions like "titanium dioxide (anatase, silica-modified, 15-25 nm)" if a specific CAS is unavailable [26]. |
Data Presentation
| Lattice Geometry | Wall Thickness (mm) | Compressive Load (kN) | Displacement (mm) | Strain (×10â»Â²) | Notable Performance |
|---|---|---|---|---|---|
| Lidinoid | 1.0 | 9 | 2.15 | 7.1 | Highest deformability |
| Diamond | 1.5 | 6 | 0.98 | 3.3 | Intermediate performance |
| Gyroid | 2.0 | 3 | 0.36 | 1.2 | Superior mechanical integrity, least deformation |
| Gyroid | 1.0 | 9 | 1.45 | 4.8 | Maintains relative strength at high load |
| Parameter Category | Specific Data Required | Example Entry for an SDS | Rationale |
|---|---|---|---|
| Particle Size & Distribution | D50 value, range (e.g., 90% of particles between) | "D50 = 45 nm with 90% of particles between 30-65 nm" | Governs deposition, biological uptake, and toxicity. |
| Surface Area | BET surface area measurement | "BET Surface Area: 225 m²/g" | Critical for reactivity and dose-metric assessment. |
| Shape & Morphology | Descriptive morphology, aspect ratio | "High-aspect ratio needle-like structures" | Indicates potential asbestos-like pathogenicity. |
| Surface Chemistry | Description of coatings or modifications | "Surface-treated with silica" | Significantly alters biological interactions and toxicity. |
| Dispersion Stability | Stability behavior in relevant media | "Dispersion agglomerates in high ionic strength solutions" | Informs safe handling and risk under use conditions. |
Experimental Protocols
Objective: To systematically optimize the mechanical performance of 3D-printed bone scaffolds by evaluating geometric and loading parameters.
Methodology:
- Scaffold Design: Create three distinct Triply Periodic Minimal Surface (TPMS) lattice geometries (e.g., Lidinoid, Diamond, Gyroid) within a fixed design envelope (e.g., 30×30×30 mm³).
- Parameter Variation: Define varying wall thicknesses (e.g., 1.0, 1.5, 2.0 mm). Calculate the resulting porosity for each design.
- Experimental Design: Employ a Taguchi L27 Orthogonal Array to efficiently arrange the experiments (geometry × thickness × compressive load (e.g., 3, 6, 9 kN)).
- Mechanical Testing: Subject scaffolds to compression testing according to standards (e.g., ASTM). Record key responses: displacement and strain.
- Predictive Modeling: Train a Back-propagation Artificial Neural Network (BPANN) model using experimental data to predict scaffold behavior across a wider parameter space. Validate model accuracy (e.g., target R² > 0.99).
- Validation: Perform Finite Element Analysis (FEA) simulations to validate both experimental and BPANN-predicted results, creating a robust optimization framework.
Objective: To prepare a comprehensive and regulatory-compliant SDS for a nanomaterial, addressing its unique properties and potential hazards.
Methodology:
- Comprehensive Characterization: Prior to classification, fully characterize the nanomaterial's physical and chemical properties (see Table 2 for required data).
- Data Gap Analysis: Build a "data matrix" spreadsheet to inventory all available toxicological data (in vivo, in vitro) and explicitly identify data gaps.
- Hazard Classification: Use a "weight of evidence" approach. For data gaps, apply read-across from similar materials and expert judgment. Document all reasoning transparently.
- SDS Authoring - Critical Sections:
- Section 2: Hazard Identification: Clearly state data limitations. Emphasize respiratory hazards, which are common for nanomaterials.
- Section 3: Composition: List all nano-ingredients with specific CAS numbers or detailed descriptions, including concentration.
- Section 8: Exposure Controls: Specify "HEPA-filtered local exhaust ventilation" and test and specify PPE (e.g., glove type and thickness).
- Section 9: Physical Properties: Include all nano-specific parameters from Step 1.
- Section 11: Toxicological Information: Summarize all data, prioritize routes of exposure (e.g., inhalation), and contextualize in vitro vs. in vivo findings.
- Review and Documentation: Assemble a team (material scientist, toxicologist, safety engineer) to review the SDS. Maintain a separate file with all data sources and decision rationales.
Workflow Visualization
Experimental Protocol Development Workflow
Nanomaterial SDS Authoring Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Material/Reagent | Function in Research |
|---|---|
| PLA+ (Polylactic Acid Plus) | A primary thermoplastic polymer for extrusion printing; offers enhanced toughness and reduced brittleness compared to standard PLA, better mimicking bone mechanics [27]. |
| Bioactive Ceramics | Materials like hydroxyapatite or tricalcium phosphate; incorporated as fillers in polymer composites to provide osteoconductivity and improve compressive strength [28]. |
| Photocurable Resins | Used in laser-based printing (SLA/DLP) to create high-resolution scaffolds; often require post-processing for biocompatibility [28]. |
| Surface Modification Agents | Molecules (e.g., peptides, PEG) used to functionalize scaffold surfaces, improving cell adhesion, reducing immune rejection, or controlling degradation [28]. |
| Autotaxin-IN-7 | Autotaxin-IN-7, MF:C26H24N6O4, MW:484.5 g/mol |
| P162-0948 | P162-0948, MF:C20H15FN4O2, MW:362.4 g/mol |
| Resource/Platform | Function in Research |
|---|---|
| ECHA's Appendix for Nanoforms | Provides critical guidance for complying with the European Union's REACH regulation for nanomaterials, essential for market access in the EU [26]. |
| NIOSH Current Intelligence Bulletins | Offers authoritative, science-based recommended exposure limits (RELs) for specific nanomaterials (e.g., titanium dioxide), informing safe lab practices [26]. |
| OECD Test Guidelines | Provides internationally agreed-upon testing methods for the safety assessment of nanomaterials, ensuring data reliability and regulatory acceptance [26]. |
From Theory to Practice: Implementing Testing Protocols Across Material Classes
Test Selection Based on Contact Duration and Body Contact Type
This technical support guide provides a structured framework for selecting appropriate biocompatibility tests for medical devices and biomaterials, directly addressing key challenges in standardizing biomaterial testing protocols.
Biocompatibility Testing Framework
How are medical devices categorized for biocompatibility testing?
Device categorization is the first critical step and is based on the nature of body contact and contact duration [29] [30].
- Surface Devices: Contact body surfaces only.
- Intact Skin: Devices like electrodes, compression garments.
- Mucosal Membranes: Devices like endotracheal tubes, contact lenses.
- Breached or Compromised Surfaces: Devices like wound dressings on broken skin.
- External Communicating Devices: Contact internal tissues or body fluids via a external path.
- Blood Path, Indirect: Devices like administration sets, which contact blood indirectly.
- Tissue/Bone/Dentin: Devices like laparoscopic surgery tools or dental restoration materials.
- Circulating Blood: Devices like central venous catheters or blood oxygenators.
- Implant Devices: Placed entirely inside the body.
- Tissue/Bone: Devices like orthopedic implants or pacemakers.
- Blood: Devices like vascular grafts or heart valves [29].
How does contact duration influence test selection?
The duration a device contacts the body directly influences the extent of biological evaluation required. The three standardized categories are [29] [30]:
- Limited: ≤ 24 hours (e.g., hypodermic needles, single-use surgical instruments).
- Prolonged: >24 hours to 30 days (e.g., temporary indwelling catheters, some wound dressings).
- Long-term/Permanent: >30 days (e.g., joint replacements, permanent implants).
Test Selection Tables by Device Category
The following tables summarize the biological effects that must be evaluated based on your device's categorization and contact duration. These requirements are derived from the FDA's modified matrix based on ISO 10993-1 [29].
= Endpoint for consideration.
Surface Devices
| Biological Effect | Intact Skin | Mucosal Membrane | Breached/Compromised Surface |
|---|---|---|---|
| Limited Contact (≤24 hours) | |||
| Cytotoxicity | |||
| Sensitization | |||
| Irritation or Intracutaneous Reactivity | |||
| Acute Systemic Toxicity | |||
| Material-Mediated Pyrogenicity | |||
| Prolonged Contact (>24h to 30 days) | |||
| Subacute/Subchronic Toxicity | |||
| Implantation | |||
| Long-term/Permanent Contact (>30 days) | |||
| Genotoxicity | |||
| Chronic Toxicity | |||
| Carcinogenicity |
External Communicating Devices
| Biological Effect | Blood Path, Indirect | Tissue/Bone/Dentin | Circulating Blood |
|---|---|---|---|
| Limited Contact (≤24 hours) | |||
| Cytotoxicity | |||
| Sensitization | |||
| Irritation or Intracutaneous Reactivity | |||
| Acute Systemic Toxicity | |||
| Material-Mediated Pyrogenicity | |||
| Genotoxicity | * | ||
| Hemocompatibility | |||
| Prolonged Contact (>24h to 30 days) | |||
| Subacute/Subchronic Toxicity | |||
| Genotoxicity | |||
| Implantation | |||
| Hemocompatibility | |||
| Long-term/Permanent Contact (>30 days) | |||
| Genotoxicity | |||
| Implantation | |||
| Hemocompatibility | |||
| Chronic Toxicity | |||
| Carcinogenicity |
Note: *For all devices used in extracorporeal circuits [29].
Implant Devices
| Biological Effect | Tissue/Bone | Blood |
|---|---|---|
| Limited Contact (≤24 hours) | ||
| Cytotoxicity | ||
| Sensitization | ||
| Irritation or Intracutaneous Reactivity | ||
| Acute Systemic Toxicity | ||
| Material-Mediated Pyrogenicity | ||
| Genotoxicity | ||
| Implantation | ||
| Hemocompatibility | ||
| Prolonged Contact (>24h to 30 days) | ||
| Subacute/Subchronic Toxicity | ||
| Genotoxicity | ||
| Implantation | ||
| Hemocompatibility | ||
| Long-term/Permanent Contact (>30 days) | ||
| Genotoxicity | ||
| Implantation | ||
| Hemocompatibility | ||
| Chronic Toxicity | ||
| Carcinogenicity |
Troubleshooting FAQs
Our device is made of a common polymer. Do we still need to perform all tests listed in the matrix?
Not necessarily. The FDA provides a policy for devices contacting intact skin made from common materials (identified in Attachment G of its guidance) where you may provide specific information in your submission instead of a full biocompatibility evaluation [29] [31]. However, this is specific to intact skin devices. For all other device categories and materials, you must address every endpoint in the matrix, but not always with new testing. You can use existing data, chemical characterization, or a scientific rationale to justify why a test is not needed [29] [4]. If you use novel materials or manufacturing processes, additional testing is typically required [29].
We are testing a biodegradable material. Which additional factors must we consider?
For any device or material intended to degrade in the body, you must provide degradation information as part of your biological evaluation [29]. This includes identifying and quantifying the degradation products (leachables) and assessing their biological safety (e.g., cytotoxicity, systemic toxicity, genotoxicity). Understanding the full degradation profile is critical, as some byproducts may have toxicological effects not evident from testing the parent material [32].
Why is there variability in cytotoxicity results between different labs testing the same material?
A core standardization challenge in cytotoxicity testing lies in the choice of cell lines and protocols. Many labs use immortalized cell lines (e.g., L-929 mouse fibroblasts) which are tumor-derived and may not represent the behavior of primary human cells. Furthermore, results can be influenced by factors like [32]:
- Cell origin and type: Tumor-derived vs. primary cells.
- Culture conditions: Media composition and exposure time.
- Endpoint measurement: Qualitative (microscopic evaluation) vs. quantitative (e.g., MTT assay) methods. Adhering to standardized protocols like those in ISO 10993-5 and carefully documenting all methodological details is crucial for reproducibility [33] [34].
What are the key considerations for testing a device that contacts blood?
For blood-contacting devices (especially those contacting circulating blood), hemocompatibility testing is mandatory [29]. This involves a battery of tests to evaluate the device's interaction with blood, assessing the potential for [33] [34]:
- Thrombogenicity: Formation of blood clots.
- Hemolysis: Destruction of red blood cells.
- Platelet activation.
- Complement system activation. The specific tests required depend on the device's contact duration and the nature of blood contact (indirect vs. circulating) [29] [30].
Detailed Experimental Protocols
Cytotoxicity Testing (ISO 10993-5)
Purpose: To evaluate the potential for device materials to cause cell death or inhibit cell growth.
Method Selection:
- Direct Contact Method: Ideal for low-density materials. A piece of the test material is placed directly onto a confluent layer of cells (e.g., L-929 fibroblasts) and incubated for 24-72 hours. Cytotoxicity is indicated by zones of malformed, degenerative, or lysed cells under and around the test sample [33].
- Agar Diffusion Method: Suitable for high-density materials. A thin layer of agar is placed over the cells. The test material or an extract dried on filter paper is placed on the agar surface. After incubation, a zone of cell lysis under the material indicates cytotoxicity [33].
- MEM Elution (Extract) Method: Uses extracts of the device prepared with various solvents (e.g., saline, serum) to simulate clinical use. The extracts are applied to the cell culture, and after incubation, cells are examined for effects. This method allows for semi-quantitative analysis [33].
- Quantitative MTT Assay: A colorimetric method that measures the reduction of a yellow tetrazolium salt by mitochondrial enzymes in living cells. The resulting purple formazan can be quantified spectrophotometrically. This method provides a numerical value for cell viability and is less subject to analyst interpretation [33].
Sensitization Testing (ISO 10993-10)
Purpose: To determine if device extracts contain chemicals that can cause allergic reactions after repeated or prolonged exposure.
Method Selection:
- Guinea Pig Maximization Test (GPMT): Considered the most sensitive. The test material extract is intradermally injected with Freund's Complete Adjuvant (an immune stimulant) during the induction phase. After a challenge exposure, the skin reaction is scored for redness and swelling (erythema and edema). Recommended for devices with internal or externally communicating contact [33].
- Closed Patch Test: Used for devices contacting only unbroken skin. The test material or extract is applied topically to the shaved skin of guinea pigs repeatedly during the induction phase, followed by a challenge dose. The skin sites are graded for allergic response [33].
- Murine Local Lymph Node Assay (LLNA): An alternative method that measures the proliferation of lymphocytes in the lymph nodes draining the application site. From an animal welfare perspective, the LLNA is often preferred as it reduces animal suffering and can provide quantitative data [33].
Genotoxicity Testing (ISO 10993-3)
Purpose: To assess the potential of device extracts to cause genetic damage (gene mutations, chromosomal aberrations).
Standard Battery: A battery of tests is required, typically including:
- Ames Test (Bacterial Reverse Mutation Assay): An in vitro test using specific strains of Salmonella typhimurium and Escherichia coli to detect point mutations. It is a required initial test for all devices with prolonged or permanent contact [33] [34].
- In vitro Mouse Lymphoma Assay or Chromosomal Aberration Test: These in vitro tests use mammalian cells to detect chromosomal damage (clastogenicity).
- In vivo Micronucleus Test: An in vivo test where animals (typically mice) are treated with the device extract, and the bone marrow or peripheral blood is examined for the presence of micronuclei (small, extranuclear bodies containing chromosomal fragments), which indicate chromosomal damage [33]. For devices with long-term exposure, an Ames test plus two in vivo methods are generally required [33].
Test Selection Workflow
This diagram outlines the logical decision process for selecting biocompatibility tests.
The Scientist's Toolkit: Essential Reagents & Materials
| Item | Function in Biocompatibility Testing |
|---|---|
| L-929 Mouse Fibroblast Cell Line | A standard cell line used for in vitro cytotoxicity testing (e.g., MEM Elution, Agar Diffusion assays) [32]. |
| Salmonella typhimurium TA98, TA100, etc. | Specific bacterial strains used in the Ames Test for detecting reverse mutations and assessing genotoxic potential [33]. |
| Complete Freund's Adjuvant (CFA) | An immune stimulant used in the Guinea Pig Maximization Test to enhance the sensitization response for more reliable detection of weak allergens [33]. |
| Dimethyl Sulfoxide (DMSO) & Sodium Chloride | Common solvents used to prepare extracts of device materials for elution-based tests (cytotoxicity, sensitization, systemic toxicity) [33]. |
| MTT Reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) | A yellow tetrazolium salt used in quantitative cytotoxicity assays. It is reduced to a purple formazan by metabolically active cells, providing a colorimetric measure of cell viability [33]. |
| Glp-Asn-Pro-AMC | Glp-Asn-Pro-AMC, MF:C24H27N5O7, MW:497.5 g/mol |
| 5-Methylnonanoyl-CoA | 5-Methylnonanoyl-CoA, MF:C31H54N7O17P3S, MW:921.8 g/mol |
A technical guide for researchers navigating standardization challenges in biomaterial testing.
This technical support center article addresses frequently asked questions and common experimental challenges related to the "Big Three" biocompatibility tests—cytotoxicity, sensitization, and irritation. These tests form the cornerstone of the biological safety evaluation for nearly all medical devices and are critical for regulatory approval globally [5].
FAQs: Core Concepts and Regulatory Context
Q1: What are the "Big Three" biocompatibility tests and why are they so critical?
The "Big Three" refers to the trio of cytotoxicity, irritation, and sensitization assessments. These tests are a standard requirement for almost every medical device entering the market, irrespective of its category, nature of patient contact, or duration of use [5]. They are the first line of defense in ensuring that a device material does not cause immediate cell death, skin irritation, or allergic reactions upon contact with the body.
Q2: How do international standards like ISO 10993 guide our testing protocols?
The ISO 10993 series of standards provides a globally harmonized framework for the biological evaluation of medical devices. Key standards include:
- ISO 10993-1: Provides an overarching framework for evaluation and testing within a risk management process [35] [8].
- ISO 10993-5: Specifies test methods and protocols for cytotoxicity testing [5].
- ISO 10993-10: Covers test methods for irritation and skin sensitization [5].
Other major regulatory bodies, including the US FDA and the European Union under its MDR, align their expectations with these ISO standards, though often with specific national deviations or additional guidance [5] [36].
Q3: Our device is made from "biocompatible" materials. Do we still need to perform this testing?
Yes, testing is likely still required. The FDA does not maintain a list of pre-approved "biocompatible materials" [35]. A material's safety is evaluated in the context of its specific intended use, patient contact duration, and the device's overall design. While data from predicate devices or supplier materials can reduce the testing burden, a comprehensive biological evaluation plan rooted in risk management is mandatory [35].
Q4: What is the single biggest standardization challenge in this field today?
The most significant challenge is the fragmented research landscape and significant variability in in vitro culture conditions and read-outs, which complicates cross-study comparisons [37]. This lack of standardized protocols is a major hurdle in adopting new approach methodologies (NAMs) and is a primary focus of ongoing research and standards development [5] [37].
Q5: How is the upcoming ISO 10993-1:2025 standard changing our approach?
The 2025 revision deeply embeds the biological evaluation process within a formal risk management framework, as defined in ISO 14971 [8]. Key changes include:
- Mandating the consideration of reasonably foreseeable misuse (e.g., using a device longer than intended) in the biological risk assessment.
- Providing more precise definitions for determining total exposure period, especially for devices with multiple or intermittent patient contact.
- Requiring an assessment of bioaccumulation potential for chemicals present in the device [8].
Troubleshooting Guides for Experimental Challenges
Challenge 1: Inconsistent Cytotoxicity Results
Problem: Variable results in cell viability assays (e.g., MTT, XTT) between test runs or laboratories.
Investigation & Resolution:
| Potential Cause | Investigation Steps | Recommended Corrective Actions |
|---|---|---|
| Extract Preparation Variability | Audit extraction parameters (solvent, temperature, duration, surface area-to-volume ratio) per ISO 10993-12. [5] | Standardize extraction protocols across all batches. Use controls with known reactivity. |
| Cell Line Instability | Check cell line authentication and passage number. Monitor mycoplasma contamination. | Use low-passage cells from a reputable source. Maintain consistent culture conditions. |
| Assay Interference | Test device extracts with assay reagents in a cell-free system. | Switch to an alternative assay (e.g., from MTT to Neutral Red Uptake if interference is confirmed). [5] |
Challenge 2: Non-Standardized FBGC Formation for Implantation Studies
Problem: Difficulty in reproducing in vitro foreign body giant cell (FBGC) formation, leading to poor predictive value for the in vivo foreign body response.
Investigation & Resolution:
- Root Cause: The research landscape is marked by significant variability in critical parameters, including cell origin and type, culture media and sera, fusion-inducing factors, and seeding density [37].
- Solution: While a universally accepted standard is not yet available, researchers are urged to adopt internal, rigorously documented protocols. A recent review proposes guidelines to improve reproducibility, focusing on standardizing the use of fusion-inducing factors like IL-4 and IL-13 and consistent quantification methods [37].
Challenge 3: Justifying Test Selection to Regulatory Bodies
Problem: Defending the choice, scope, or omission of certain "Big Three" tests during regulatory submission.
Investigation & Resolution:
- Proactive Planning: Develop a robust Biological Evaluation Plan (BEP) early in the device development process. The BEP should not just be a test checklist; it must be a risk-based rationale that considers the device's intended use, material chemistry, and clinical history [35] [8].
- Leverage All Data: Justify your testing strategy with a combination of data: chemical characterization, toxicological risk assessment, existing scientific literature, and clinical data from predicate devices [35]. Engage regulators in pre-submission discussions to align on your strategy.
The Scientist's Toolkit: Essential Reagents & Materials
The following table details key reagents and materials used in standard in vitro "Big Three" testing.
Table: Key Research Reagent Solutions for "Big Three" Biocompatibility Testing
| Item | Function in Testing | Application Notes |
|---|---|---|
| L929 or Balb/c 3T3 Fibroblasts | Standardized cell lines used for cytotoxicity testing. | Assess cell viability and morphological changes after exposure to device extracts. [5] |
| MTT / XTT Assay Kits | Colorimetric assays that measure cell metabolic activity as a marker of viability. | Common quantitative methods endorsed by ISO 10993-5. [5] |
| Neutral Red Dye | A vital dye taken up by living lysosomes; used in cytotoxicity testing. | An alternative endpoint for quantifying cell viability. [5] |
| Extraction Solvents | Vehicles to leach chemicals from a device for testing. | Typically include physiological saline, vegetable oil, and cell culture medium with serum. [5] |
| Recombinant IL-4 / IL-13 | Cytokines used to induce macrophage fusion into FBGCs in vitro. | Critical but variably applied reagents in non-standardized implantation simulation models. [37] |
| pGlu-Pro-Arg-MNA | pGlu-Pro-Arg-MNA, MF:C23H32N8O7, MW:532.5 g/mol | Chemical Reagent |
| Avenanthramide D | Avenanthramide D, CAS:53901-55-6, MF:C16H13NO4, MW:283.28 g/mol | Chemical Reagent |
Experimental Workflow and Signaling Pathways
Cytotoxicity Testing Workflow
The following diagram outlines the core decision-making and experimental process for assessing cytotoxicity according to ISO 10993-5.
Key Signaling in Foreign Body Response
This diagram illustrates the core cellular process of Foreign Body Giant Cell (FBGC) formation, a key event in the reaction to implanted materials, highlighting areas of protocol variability.
Table: Acceptability Criteria for Common Cytotoxicity Assays (based on ISO 10993-5) [5]
| Assay Type | Measured Endpoint | General Acceptance Guideline | Notes |
|---|---|---|---|
| MTT / XTT | Metabolic Activity (Cell Viability) | Typically ≥ 70% cell survival vs. control | A qualitative assessment of cell morphology is also required. |
| Neutral Red Uptake | Lysosomal Integrity & Viability | Typically ≥ 70% cell survival vs. control | Measures the ability of living cells to incorporate and bind the dye. |
| Qualitative Morphology | Cell Lysis, Detachment, Morphology | No excessive signs of toxicity | Graded relative to control cultures. |
Table: Global Regulatory Landscape for "Big Three" Testing [5]
| Region / Country | Primary Regulatory Body | Key Standard / Regulation | Notable Consideration |
|---|---|---|---|
| United States | FDA (Food and Drug Administration) | FDA Guidance + ISO 10993 | Does not fully recognize all ISO standards; review specific guidance. |
| European Union | - | MDR (EU 2017/745) + ISO 10993 | Requires strict adherence to the 3Rs (Replacement, Reduction, Refinement) for animal testing. [5] |
| Japan | PMDA (Pharmaceuticals and Medical Devices Agency) | ISO 10993 | Requirements are aligned with international standards. |
| Canada | Health Canada | Medical Devices Regulations (MDR) + ISO 10993 | Aligns with international standards. |
| International | ISO | ISO 10993 Series | The globally harmonized base standard for biological evaluation. |
FAQs and Troubleshooting Guides
Surface Analysis
Q1: How can I accurately measure the surface zeta potential of my dental implant material to predict protein interaction?
A: The Surface Zeta Potential analysis is a key method for this task. You can use a surface zeta potential analyzer (e.g., SurPASS 3) to study the interaction of proteins in solution with the implant material. This technique combines the determination of adsorption kinetics with the characteristics of the adsorbed surface layer. In-depth knowledge in this field will enable you to develop dental implants that are resistant to bacterial biofilm formation and thus help diminish the risk for infections or implant failure [38].
- Troubleshooting Tip: If you are getting inconsistent readings, ensure that the dedicated sample holders for specific geometries (e.g., hollow fiber membranes for hemodialysis membranes) are used to correctly characterize the surface of interest [38].
Q2: What is the best method to verify the adhesion quality of a coating on a stent?
A: Scratch testing is one of the few methods that can verify the adhesion of a coating and thereby ensure a sufficiently long lifetime of the implant. To make sure stents behave as required and are not damaged in the body, adhesion and scratch resistance of the coating are measured with a nano scratch tester. The critical load, which is the load at which the coating fails, is determined in this test [38].
- Troubleshooting Tip: Properly mount the stent on the tester as per established protocols to avoid artifacts in the measurement of the critical load [38].
Q3: My hydrogel friction tests are yielding inconsistent data. What could be the cause?
A: Testing of hydrogels is perceived as complicated due to the difficulty of mounting them and because minor changes in the pressures exerted can significantly influence tribological properties. Use a tribometer with a special sample holder for hydrogels. This setup allows optimal adaptation to real-life conditions in terms of contact pressure, sliding velocities, and temperature, and has high sensitivity when measuring friction over a broad range of sliding velocities [38].
- Troubleshooting Tip: Ensure that the normal force and sliding velocity are meticulously controlled and documented, as these parameters are critical for reproducible results with soft, compliant materials like hydrogels.
Mechanical Testing
Q4: How can I determine the mechanical properties of a small or thin biomaterial sample, like a tissue-engineered scaffold or a coating?
A: For small samples, thin specimens, or coatings, nanoindentation is the preferred technique. It provides both elastic modulus and hardness data without the need for large sample volumes. A calibrated Berkovich indenter tip is used, and the load-displacement data during the indentation process is analyzed to determine mechanical properties [39]. This method is also ideal for measuring properties of sensitive materials like contact lenses and human tissues [38].
- Troubleshooting Tip: For accurate and reproducible results, sample preparation is key. An extremely rough surface may reduce the accuracy of indentation data; a proven method for polishing samples is recommended. The testing equipment also needs to be isolated from vibrations [39].
Q5: What are the key mechanical tests required for a vascular stent to meet regulatory standards?
A: A robust testing profile for a vascular stent includes [40]:
- Material Testing: Evaluate the raw nitinol wire for elongation, tensile strength, and shape memory by loading and unloading in a cyclic test per ASTM F2516.
- Flexibility Testing: Subject the stent to a three-point bend test per ASTM F2606 to generate a force-displacement curve.
- Tortuosity Testing: Quantify the frictional forces to simulate pushing the stent through the vascular system.
- Radial Force Testing: Evaluate the radial strength, chronic outward force, and compression resistance to ensure efficacy once implanted.
- Durability Testing: Subject the device to millions of fatigue loading cycles (e.g., 400 million cycles per ASTM F2477) to simulate years of in vivo service.
Q6: When performing a standard microhardness test (Vickers/Knoop), my results have high variability. How can I improve this?
A: Traditional microhardness test methods optically analyze the indented impression, which can convolute data with operator bias. To improve reliability, consider using instrumented indentation with a Berkovich indenter. Using a nanoindenter for microhardness testing with forces ranging up to 1 N, and performing an array of indents using dynamic measurements yields accurate and reliable microhardness data with no operator bias [39]. Furthermore, ensure the testing environment is controlled and free from vibrations [39].
Standardized Experimental Protocols
Protocol 1: Nanoindentation for Elastic Modulus and Hardness
Objective: To determine the elastic modulus and hardness of a biomaterial sample using nanoindentation.
Materials:
- Nanoindenter with a calibrated Berkovich diamond indenter tip
- Sample of interest, properly mounted and polished
- Standard reference sample for calibration (e.g., fused silica)
Method:
- Calibration: Calibrate the indenter tip area function and instrument frame stiffness using the standard reference sample.
- Approach: The calibrated indenter tip approaches the surface of the sample until contact is established.
- Loading: The force is linearly increased at a specified rate, and the tip indents into the sample surface. Record the load-displacement data.
- Dwell: A short dwell time occurs at the maximum force to account for material creep.
- Unloading: The sample is unloaded at a specified rate. The stiffness is measured at the initial point of unloading.
- Analysis: The resulting load-displacement data, along with the known area function of the indenter tip, are used to calculate the elastic modulus and hardness of the material [39].
Protocol 2: Scratch Testing for Coating Adhesion
Objective: To determine the critical load (adhesion strength) of a coating on a substrate (e.g., a stent).
Materials:
- Nano scratch tester
- Coated sample, securely mounted
- Microscope for post-test analysis
Method:
- Mounting: Securely mount the sample (e.g., stent) in the scratch tester as per the manufacturer's guidelines [38].
- Testing: Draw a rounded diamond stylus across the coated surface under a progressively increasing normal load.
- Data Collection: Simultaneously record the applied normal load, frictional force, and acoustic emissions (if available).
- Post-Test Analysis: Use microscopy (optical or SEM) to observe the scratch track and identify the exact point of coating failure (e.g., cracking, delamination).
- Determination: Correlate the failure point with the recorded normal load to determine the critical load (Lc) [38].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in biomaterial characterization and testing.
| Research Reagent / Material | Function in Experiment |
|---|---|
| Berkovich Indenter Tip | A three-sided pyramidal diamond indenter used in nanoindentation to probe mechanical properties on a nano- to micro-scale [39]. |
| Complete Freund's Adjuvant (CFA) | An immune response enhancer used in the Guinea Pig Maximization Test to evaluate the sensitization potential of a material or its extracts [33]. |
| MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide) | A yellow tetrazole that is reduced to purple formazan in living cells, used in colorimetric assays to quantify cell viability and cytotoxicity [33]. |
| Microbubbles | Injectable ultrasound contrast agents used to enhance the contrast of small blood vessels, allowing for the assessment of vascularization in tissue engineering constructs [41]. |
| Fluorogenic Peptide Substrates | Molecules used in enzyme activity assays that release a fluorescent signal upon cleavage by a specific enzyme, allowing for the quantification of enzymatic activity [42]. |
| Bovine Type I Collagen Matrix | A natural biopolymer scaffold derived from animal tissue, frequently used in tissue engineering (e.g., skin, cartilage) for its superior biological activity compared to many synthetic polymers [43]. |
| Salmonella typhimurium Strains | Specific bacterial strains used in the Ames test to detect point mutations and evaluate the genotoxic potential of a material or its extractable chemicals [33]. |
| pacFA Ceramide | pacFA Ceramide, MF:C33H59N3O3, MW:545.8 g/mol |
| Itic-4F | Itic-4F, MF:C94H78F4N4O2S4, MW:1499.9 g/mol |
Data Presentation: Standardized Testing Summaries
Table 1: Common In Vivo Biocompatibility Tests and Their Applications
| Test Name | Key Objective | Typical Model System | Primary Readout / Endpoint |
|---|---|---|---|
| Guinea Pig Maximization Test [33] | Determine sensitization potential (allergic response) | Guinea Pig | Skin reaction (erythema and edema) after challenge dose |
| Murine Local Lymph Node Assay (LLNA) [33] | Determine sensitization potential quantitatively | Mouse | Proliferation of T-lymphocytes in draining lymph nodes |
| Intracutaneous Test [33] | Estimate local irritation potential | Rabbit | Scores for erythema and edema at injection sites |
| Acute Systemic Toxicity Test [33] | Detect leachable chemicals causing systemic effects | Mouse | Observation of toxic signs (e.g., lethargy, convulsions) after extract injection |
| Ames Test [33] | Assess genotoxicity (point mutations) | Salmonella typhimurium | Reversion of histidine-dependent mutations |
Table 2: Comparison of Mechanical Testing Techniques for Biomaterials
| Technique | Typical Load Range | Key Measured Properties | Ideal for Sample Types | Standard Guidance |
|---|---|---|---|---|
| Nanoindentation [39] | µN to mN | Hardness, Elastic Modulus | Thin films, coatings, small volumes, tissues, hydrogels | ISO 14577 |
| Microhardness (Vickers/Knoop) [39] | < 10 N | Hardness | Small samples, thin specimens, plated surfaces | ASTM E384 |
| Tensile/Compression Test [40] | N to kN | Elastic Modulus, Yield Strength, Fracture Toughness | Bulk materials, standard "dog-bone" specimens | ASTM F2516 (for nitinol) |
| Scratch Testing [38] | mN to N | Critical Load (Adhesion strength) | Coatings on substrates (e.g., stents, implants) | ASTM C1624 (adapted for biomaterials) |
| Tribological Testing [38] | Variable | Coefficient of Friction, Wear | Surfaces in relative motion (e.g., catheters, artificial joints) | Custom simulations of in-service conditions |
Experimental Workflow Visualization
Biomaterial Testing Workflow
Cytotoxicity Testing Pathway
Frequently Asked Questions (FAQs) and Troubleshooting Guide
This technical support resource addresses common challenges researchers face when developing biomimetic models for physiological microenvironments, framed within the critical context of standardizing biomaterial testing protocols.
FAQ Category: Foundational Concepts and Design
1. Why is incorporating multiple cell types considered a "design requirement" for biomimetic microvascular models? A biomimetic model's physiological relevance depends on re-creating the multi-cellular complexity of a real network. The coordinated functions of different cell types are not just background; they are active participants in processes like angiogenesis and remodeling.
- Endothelial Cells regulate angiogenesis, acting as migrating tip cells and proliferating stalk cells during sprouting [44].
- Pericytes stabilize capillaries, deposit basement membrane components, and secrete growth factors like VEGF to guide sprout outgrowth [44].
- Smooth Muscle Cells regulate vessel diameter and initiate angiogenesis by detaching from vessels in response to molecular signals [44].
- Macrophages guide capillary sprouting via matrix degradation, facilitate pruning, and can exhibit phenotypic overlap with pericytes [44].
- Troubleshooting Tip: If your model shows unstable vessel structures or poor angiogenic response, assess the presence and spatial organization of these supporting perivascular cells. Their absence is a common point of failure.
2. What are the key mechanical properties of the extracellular matrix (ECM) I should replicate beyond simple stiffness? Focusing solely on substrate stiffness (elastic modulus) is a common oversimplification. Tissues exhibit complex mechanical behaviors that must be decoupled in your model [45].
- Viscoelasticity: Tissues exhibit time-dependent stress relaxation. This viscous behavior can be tuned independently from stiffness using entrapped linear polymers (e.g., linear polyacrylamide in a crosslinked gel) and significantly affects cell spreading and phenotype [45].
- Viscoplasticity: This refers to irreversible deformation. Cells can plastically remodel their surroundings, and materials with higher plasticity have been shown to promote cancer cell spreading and invasiveness independent of modulus [45].
- Fiber Architecture: It is critical to decouple stiffness from fiber density and crosslink density. Studies show that stiffening a collagen gel by increasing fiber density decreases angiogenic sprouting, while stiffening via non-enzymatic glycation (which increases crosslinks without increasing fiber density) can enhance it [45].
- Troubleshooting Tip: If cells in your 3D model are not behaving as in vivo, characterize your hydrogel's stress relaxation and plastic remodeling capabilities. A highly elastic, non-relaxing synthetic gel may not provide the correct mechanical cues, even if the stiffness matches.
FAQ Category: Standardization and Reproducibility
3. Our in vitro foreign body giant cell (FBGC) assays are highly variable between labs. What are the key sources of this inconsistency? The research landscape for FBGC formation is fragmented, leading to challenges in reproducibility. A recent review identified critical variables that require standardization [37].
- Cell Source: The origin and type of cells (e.g., primary monocytes vs. macrophage cell lines) used from the monocyte/macrophage lineage significantly impact results.
- Culture Conditions: Variability in culture media, serum supplements, and the specific fusion-inducing factors (e.g., cytokines like IL-4 or IL-13) creates major cross-study discrepancies.
- Seeding Density and Surface: The initial cell density and the nature of the culture surface (e.g., tissue culture plastic vs. specific biomaterials) influence fusion efficiency and outcomes.
- Solution: Advocate for and adopt standardized protocols within your research community. The field is calling for guidelines to improve reproducibility and reliability in FBGC research [37].
4. How does the new ISO 10993-1:2025 standard impact the biological evaluation of my biomaterial? The 2025 update represents a significant shift, more deeply integrating the biological evaluation process into a risk management framework aligned with ISO 14971 [8].
- Risk Estimation: You must now perform biological risk estimation based on the severity and probability of biological harm, a concept that is new to formal biological safety evaluations [8].
- Foreseeable Misuse: The evaluation must now consider "reasonably foreseeable misuse," such as a device being used for longer than the manufacturer's intended period. This can no longer be controlled solely by the instructions for use and may change your device's categorization and required testing [8].
- Contact Duration Definition: The calculation of exposure duration is more complex. The concept of "transitory" contact is gone, and any contact within a day counts as a full "contact day." For devices with multiple exposures, the "total exposure period" is the number of days from the first to the last use, which can quickly move a device from a "limited" to a "prolonged" duration category [8].
Experimental Protocols for Key Assessments
Protocol 1: Inducing In Vitro Foreign Body Giant Cell (FBGC) Formation This protocol is synthesized from the analysis of common methods, highlighting steps critical for standardization [37].
Objective: To generate FBGCs from human monocytes in vitro to study the foreign body response to a biomaterial.
Methodology:
- Cell Isolation and Culture: Isolate primary human peripheral blood mononuclear cells (PBMCs) from buffy coats via density gradient centrifugation. Differentiate monocytes into macrophages by culturing in RPMI-1640 medium supplemented with 10% heat-inactivated fetal bovine serum (FBS) and 50 ng/mL Macrophage Colony-Stimulating Factor (M-CSF) for 7 days.
- FBGC Induction: After differentiation, stimulate macrophages to fuse by adding a combination of 20 ng/mL Interleukin-4 (IL-4) and 20 ng/mL Interleukin-13 (IL-13) to the culture medium.
- Seeding: Seed the stimulated macrophages at a standardized density of 100,000 cells/cm² directly onto the test biomaterial or a control surface (e.g., tissue culture plastic).
- Maintenance: Culture the cells for up to 14 days, refreshing the medium and cytokines every 2-3 days.
- Quantification and Analysis: At endpoint, fix cells and stain for multinucleated cells (e.g., using H&E or a fluorescent nuclear stain). FBGCs are typically defined as cells containing three or more nuclei. Quantify the fusion index: (Number of nuclei in multinucleated cells / Total number of nuclei) × 100%.
Key Reagents:
- Primary human PBMCs
- M-CSF, IL-4, and IL-13 cytokines
- Test biomaterial scaffold
Troubleshooting:
- Low Fusion Efficiency: Confirm cytokine activity and concentration. Optimize seeding density; excessive confluency can inhibit fusion.
- High Variability: Strictly control the source and lot of serum, as components can greatly influence fusion. Use consistent cell passage numbers if using cell lines.
Protocol 2: Tuning Hydrogel Viscoelasticity Independently of Stiffness This protocol allows for the independent manipulation of viscous and elastic properties in a hydrogel system [45].
Objective: To create a polyacrylamide hydrogel with tunable stress relaxation (viscoelasticity) without altering its baseline elastic modulus.
Methodology:
- Base Gel Preparation: Prepare a standard crosslinked polyacrylamide (PAAm) hydrogel solution. A typical formulation includes 7.5% acrylamide and 0.1% bis-acrylamide crosslinker in an aqueous buffer.
- Incorporating Viscoelastic Element: To introduce viscoelasticity, dissolve a specific weight percentage (e.g., 0% to 2%) of linear polyacrylamide (LPA) polymer into the PAAm solution before polymerization. The LPA is not crosslinked and acts as an entrapped viscous element.
- Polymerization: Add ammonium persulfate (APS) and Tetramethylethylenediamine (TEMED) to initiate free-radical polymerization. Cast the solution between glass plates spaced to the desired thickness.
- Characterization: Use rheometry to confirm that the storage modulus (G', elasticity) remains constant across samples while the loss modulus (G", viscosity) increases with higher LPA concentrations.
- Cell Culture: Seed cells (e.g., hepatic stellate cells or fibroblasts) on the hydrogel surface and assess morphological changes (e.g., cell spreading). Increased viscosity has been shown to attenuate cell spreading and promote a more quiescent phenotype [45].
Key Reagents:
- Acrylamide monomer
- N,N'-Methylenebis(acrylamide) (bis-acrylamide) crosslinker
- Linear polyacrylamide (LPA)
- APS and TEMED
Data Presentation
Table 1: Key Mechanisms for Biomimetic Drug Carriers to Cross the Blood-Brain Barrier (BBB)
Table summarizing strategic approaches for neurological applications, derived from analysis of BBB structure and transport mechanisms [46].
| Mechanism | Principle | Example Strategy | Key Consideration |
|---|---|---|---|
| Receptor-Mediated Transcytosis (RMT) | Ligand binds specific receptor on endothelial cell, triggering vesicular transport across the cell. | Nanoparticles functionalized with Transferrin (Tf) to target Tf Receptor (TfR). | High selectivity and efficiency; potential receptor saturation. |
| Carrier-Mediated Endocytosis (CME) | Utilizes membrane transport proteins for essential nutrients. | Conjugation of drugs to glucose analogs for transport via GLUT1. | Saturable and selective for specific molecular structures. |
| Adsorptive-Mediated Endocytosis (AME) | Relies on electrostatic interaction between positive charge and negative cell surface. | Cationic albumin or cell-penetrating peptides conjugated to nanocarriers. | Less specific than RMT; potential for higher non-specific uptake. |
| Cell-Mediated Transcytosis (CMT) | Uses immune cells as "vehicles" to carry drugs across the BBB. | Loading nanoparticles into monocytes/macrophages that naturally infiltrate the CNS. | Leverages biology; dependent on carrier cell function and state. |
Table 2: The Scientist's Toolkit: Essential Reagents for Biomimetic Microenvironment Research
A curated list of critical materials and their functions for constructing advanced in vitro models.
| Research Reagent / Material | Function in Biomimetic Models | Key Rationale |
|---|---|---|
| Primary Cells (Microvascular Endothelial Cells, Pericytes) | Form the core cellular components of vascular networks [44]. | Origin (micro- vs. macrovessel) is critical; primary cells maintain more physiological phenotypes than cell lines. |
| Stem Cell Populations | Serve as heterogeneous cell sources capable of self-assembly or differentiation into vascular networks [44]. | Enables bottom-up construction of complex tissues and patient-specific modeling. |
| Interleukins (e.g., IL-4, IL-13) | Key cytokines to induce macrophage fusion into Foreign Body Giant Cells (FBGCs) in vitro [37]. | Essential for standardizing assays that predict the foreign body response to implants. |
| Viscoelastic Hydrogel Components (e.g., Linear Polyacrylamide) | Tunes the time-dependent mechanical properties (stress relaxation) of the synthetic ECM [45]. | Allows decoupling of stiffness and viscosity, which independently and profoundly influence cell fate. |
| Dynamic Hydrogel Crosslinkers (e.g., photodegradable moieties) | Enables in situ, user-controlled stiffening or softening of the cell culture substrate [45]. | Permits investigation of how temporal changes in mechanics, mimicking disease progression, guide cell behavior. |
| Fura-5F AM | Fura-5F AM, MF:C43H44FN3O24, MW:1005.8 g/mol | Chemical Reagent |
Visualizations
Diagram 1: Cell-Microenvironment Interaction in Angiogenesis
Diagram 2: Experimental Workflow for Standardized FBGC Assay
Troubleshooting Guide: Common Experimental Challenges in Biomaterial Testing
Problem 1: Inconsistent Foreign Body Giant Cell (FBGC) Formation In Vitro
- Problem Description: Significant variability in FBGC formation rates when testing the immune response to a new biodegradable polymer, making cross-study comparisons difficult [37].
- Possible Explanations:
- Variability in cell origin and type (e.g., different monocyte/macrophage sources).
- Inconsistencies in culture conditions (media, sera, fusion-inducing factors).
- Differences in cell seeding density or culture surface properties.
- Investigation & Resolution:
- Standardize Cell Source: Use a consistent, well-characterized cell line or primary cell donor source.
- Control Culture Conditions: Adhere to a defined protocol for culture media, serum batches, and concentrations of fusion-inducing cytokines like IL-4 or GM-CSF [37].
- Validate Read-Outs: Use standardized methods for quantifying FBGC formation, such as consistent microscopy fields and nuclear count thresholds.
- Preventive Strategy: Develop and adhere to a detailed, standardized operating procedure (SOP) for FBGC induction, documenting all reagent sources and lot numbers [37].
Problem 2: Misinterpreting Biomaterial Degradation Results
- Problem Description: Observed mass loss in a polymeric scaffold is mistakenly attributed to degradation when it might be simple dissolution or fragmentation [47].
- Possible Explanations:
- Gravimetric analysis (weight loss) alone is used without chemical confirmation.
- The solubility of the polymer in the degradation medium is not accounted for.
- The test does not distinguish between surface erosion and bulk dissolution.
- Investigation & Resolution:
- Employ Chemical Analysis: Use techniques like Gel Permeation Chromatography (GPC) to confirm changes in molecular weight or NMR/FTIR to identify chemical by-products [47].
- Combine Multiple Techniques: Correlate mass loss with data on mechanical property changes (e.g., loss of tensile strength) and morphological changes (via SEM).
- Confirm By-Products: Use chromatography or mass spectrometry to identify and quantify degradation by-products, confirming actual breakdown [47].
- Preventive Strategy: Follow a multi-parameter assessment strategy as outlined in the diagram below, moving beyond simple gravimetric analysis to confirm chemical degradation.
Problem 3: Biocompatibility Test Failures Due to Leachables
- Problem Description: A new orthopedic implant material fails cytotoxicity or sensitization tests due to unexpected leachable substances [48] [49].
- Possible Explanations:
- Inadequate material characterization before biocompatibility testing.
- Leachables from additives, plasticizers, or residues from manufacturing (e.g., from 3D printing).
- Changes in material properties after sterilization.
- Investigation & Resolution:
- Conduct Thorough Material Characterization: Perform detailed analysis of the material's composition before biological testing [48].
- Simulate Worst-Case Scenarios: Use extraction conditions that mimic the end-use environment and include sterilization in the testing workflow [49].
- Employ Sensitive Analytical Techniques: Ensure Analytical Evaluation Thresholds (AETs) are sensitive enough to detect low levels of leachables and assign confidence levels to compound identification [48].
- Preventive Strategy: Integrate biocompatibility assessment early in the material selection process and re-evaluate after any changes to manufacturing or sterilization methods [49].
Problem 4: Low Mechanical Strength of Biodegradable Polymer Constructs
- Problem Description: A 3D-printed porous scaffold from a biodegradable polymer lacks the mechanical integrity for load-bearing orthopedic applications.
- Possible Explanations:
- Intrinsically low mechanical properties of the polymer.
- Suboptimal 3D printing parameters leading to structural defects.
- Mechanical mismatch with native bone tissue.
- Investigation & Resolution:
- Material Selection: Consider polymer composites or copolymers to enhance strength. For metals, explore biodegradable alloys like magnesium [50].
- Optimize Printing Parameters: For 3D-printed structures, calibrate printing temperature, speed, and layer height to improve layer adhesion and reduce porosity.
- Design Optimization: Use computer-aided design (CAD) to create architectures (e.g., graded porosity) that better mimic the mechanical properties of bone [50].
- Preventive Strategy: Select materials with an elastic modulus close to that of bone (e.g., magnesium alloys, ~45 GPa) to reduce stress shielding and perform mechanical testing early in the development cycle [51] [50].
Frequently Asked Questions (FAQs)
Q1: What are the key standardization challenges when comparing biodegradation rates of metals and polymers? The primary challenge is the lack of unified, conclusive protocols. Standard techniques like gravimetric analysis can mistake solubility for degradation, and methods like SEM only infer but do not confirm degradation [47]. Furthermore, the current ASTM guidelines need updating to include real-time, non-invasive monitoring and do not fully account for the different degradation mechanisms between metals (e.g., corrosion) and polymers (e.g., hydrolysis, enzymatic cleavage) [47].
Q2: Why is my in vitro immune response data not translating to in vivo models? This is often due to oversimplified in vitro models that fail to capture the complexity of the in vivo environment. A major factor is the significant variability in methods used to induce immune cells like FBGCs in vitro, including cell origin, culture media, and inducing factors [37]. To improve translation, adopt more standardized and physiologically relevant in vitro protocols that better simulate the dynamic immune response.
Q3: How can I proactively manage biocompatibility risks when selecting a new biomaterial? Avoid a reactive approach. Integrate biocompatibility assessment early in the material selection process, not after the design is finalized [49]. Conduct thorough material characterization early on, understand the regulatory history of similar materials, and consider how manufacturing (like 3D printing) and sterilization might alter the material and create leachables [48] [49].
Q4: What are the advantages of using 3D printing for orthopedic biomaterials? 3D printing enables the fabrication of patient-specific implants with complex, customized geometries that match anatomical defects [50]. It allows for the creation of controlled porous structures that can promote bone ingrowth and, for metals, helps design implants with a modulus similar to bone to reduce stress-shielding [50].
Comparative Data: Orthopedic Metals vs. Biodegradable Polymers
Table 1: Key Property Comparison for Orthopedic Application
| Property | Traditional Metals (e.g., Ti, SS) | Biodegradable Polymers (e.g., PLLA, Chitosan) | Biodegradable Metals (e.g., Mg) |
|---|---|---|---|
| Primary Function | Permanent structural support [51] | Temporary scaffold, drug delivery [52] | Temporary mechanical support [50] |
| Biodegradable | No (Corrodes over long periods) [51] | Yes (Hydrolytic/Enzymatic cleavage) [52] | Yes (Corrosion in bodily fluid) [50] |
| Elastic Modulus | 110-200 GPa (High, causes stress shielding) [51] | 1-5 GPa (Low, often too flexible for load-bearing) [51] | ~45 GPa (Close to cortical bone) [50] |
| Key Advantage | High mechanical strength [51] | Tunability, biocompatibility [52] | Avoids secondary surgery, osteogenic potential [50] |
| Key Challenge | Stress shielding, implant loosening, need for removal [51] | Low mechanical strength, inconsistent degradation rates [47] [52] | Rapid/uneven degradation, gas release [50] |
Table 2: Standardized Testing Protocols & Common Pitfalls
| Test Type | Standard Methodology | Common Pitfalls & Troubleshooting |
|---|---|---|
| Biodegradation Assessment | Immersion in simulated body fluid (e.g., PBS, pH 7.4); Gravimetric analysis; GPC/SEC for molecular weight [47]. | Pitfall: Mistaking solubility for degradation. Solution: Combine gravimetry with chemical analysis (NMR, HPLC) to confirm breakdown [47]. |
| Cytotoxicity (ISO 10993-5) | Extracting material in cell culture media and exposing to mammalian cells (e.g., L929 fibroblasts). | Pitfall: Leachables from processing or sterilization cause false positives. Solution: Thorough material characterization and testing post-sterilization [48] [49]. |
| FBGC Formation (In Vitro) | Culture of macrophages (e.g., THP-1) with cytokines (IL-4/GM-CSF) to induce fusion [37]. | Pitfall: High variability between labs. Solution: Standardize cell source, cytokine concentration, and culture duration. Use quantitative read-outs [37]. |
| Mechanical Testing | Tensile/compressive tests per ASTM standards to determine modulus, strength, and elongation. | Pitfall: Data doesn't represent in vivo performance. Solution: Test in conditions simulating the physiological environment (e.g., 37°C, hydrated) [51]. |
Experimental Protocols
Protocol 1: Multi-Parameter Biomaterial Degradation Assessment
This protocol goes beyond simple mass loss to provide a comprehensive view of degradation [47].
- Pre-degradation Characterization: Characterize the initial material's weight, molecular weight (via GPC), chemical structure (via FTIR), and mechanical properties.
- Immersion Study: Immerse samples in a degradation medium (e.g., PBS at pH 7.4, with or without enzymes like lysozyme) and maintain at 37°C under agitation.
- Periodic Sampling: At predetermined time points, remove samples from the medium.
- Analysis:
- Physical: Rinse, dry, and weigh samples for gravimetric analysis. Observe surface morphology via SEM.
- Chemical: Analyze the molecular weight of the material via GPC. Analyze the degradation medium for chemical by-products using techniques like NMR or HPLC.
- Mechanical: Perform tensile or compressive tests to monitor changes in strength and modulus.
Protocol 2: Standardized In Vitro FBGC Formation Assay
This protocol aims to reduce variability in assessing the foreign body response [37].
- Cell Preparation: Differentiate human monocytic THP-1 cells into macrophages using PMA.
- FBGC Induction: Seed macrophages on the material surface or tissue culture plastic. Add a standardized concentration of recombinant human IL-4 (e.g., 20 ng/mL) and GM-CSF to the culture medium to induce fusion.
- Culture Maintenance: Culture cells for 7-14 days, refreshing media and cytokines every 2-3 days.
- Quantification: Fix and stain cells (e.g., for actin and nuclei). Image using fluorescence microscopy. Quantify FBGCs by defining them as cells containing three or more nuclei. Report results as FBGCs per field or percentage of total nuclei within FBGCs.
Visual Workflows and Diagrams
Diagram Title: Multi-Parameter Degradation Assessment Workflow
Diagram Title: Biomaterial Selection Logic for Orthopedics
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Biomaterial Testing
| Item | Function/Application | Key Considerations |
|---|---|---|
| IL-4 & GM-CSF | Cytokines used to induce macrophage fusion and FBGC formation in vitro [37]. | Batch-to-batch variability can affect results; requires concentration optimization. |
| Simulated Body Fluids (PBS, SBF) | Buffered solutions used as degradation media to mimic the physiological environment [47]. | pH must be carefully maintained at 7.4; enzymatic addition (e.g., lysozyme) may be required. |
| THP-1 Cell Line | A human monocytic cell line that can be differentiated into macrophages, used for standardized immune response assays [37]. | Passage number and differentiation protocol (PMA concentration) must be consistent. |
| Alkaline Phosphatase (ALP) | A common biochemical marker for osteogenic activity and bone formation in cell-biomaterial interaction studies. | Activity should be normalized to total protein content; can be used to assess bioactivity of implants. |
| Gel Permeation Chromatography (GPC) | An analytical technique to determine the molecular weight distribution of polymers, crucial for confirming degradation [47]. | Requires appropriate standards; sample preparation must not alter the polymer. |
Solving Real-World Challenges: Optimization Strategies for Complex Biomaterials
Addressing Material Variability and Testing Complexity
Troubleshooting Guides
Guide 1: Addressing Inconsistent Biocompatibility Test Results
Problem: Significant variability in cytotoxicity results is observed when testing the same biomaterial batch across different labs or even different plates within the same lab.
Solution: Inconsistent results often stem from non-standardized sample preparation and test conditions. The following steps can help identify and mitigate the root causes.
- Troubleshooting Steps:
- Verify Extract Preparation: Confirm that extraction parameters (temperature, duration, surface area-to-volume ratio) strictly adhere to ISO 10993-12 guidelines [5] [17]. Inconsistent extraction is a primary source of variability.
- Audit Cell Culture Health: Ensure the use of a healthy, low-passage cell line (e.g., L929 or Balb 3T3 fibroblasts) and confirm that control cells exhibit >90% viability before assay initiation [5].
- Validate Assay Reagents: Use freshly prepared or properly aliquoted reagents. For example, MTT solution can degrade if stored improperly or for too long, leading to reduced signal [5].
- Inspect Testing Apparatus: If using direct contact methods on material samples, ensure a consistent and well-sealed contact area. Novel systems like the ClicKit-Well can standardize the testing surface and prevent leakage, minimizing errors associated with sample placement in traditional well plates [53].
- Review Environmental Controls: Document and verify that incubation conditions (temperature, COâ‚‚, humidity) are stable throughout the test duration, as fluctuations can affect cell metabolism and assay endpoints [53].
Preventive Measures: Implement a rigorous protocol for sample preparation and maintain detailed device history records (DHR) for each test batch to ensure full traceability [54].
Guide 2: Managing the Complexity of Mechanical Testing for Biological Materials
Problem: Mechanical tests on soft, hydrating biomaterials or tissue-engineered constructs yield data with high noise and poor reproducibility.
Solution: The inherent properties of biomaterials—such as being soft, hydrating, anisotropic, and heterogenous—require specialized approaches distinct from those used for traditional industrial materials [55].
- Troubleshooting Steps:
- Optimize Grip and Fixture: Prevent sample slippage or damage at the clamps using sandpaper-coated grips, multipoint puncture fixation, or clamping to firmly attached tabs [55].
- Maintain Physiological Conditions: Conduct tests in a controlled environmental chamber that maintains the sample at 37°C and 100% humidity to prevent artifactual changes in material properties due to drying [55].
- Employ Full-Field Strain Analysis: Use digital image correlation (DIC) or similar image-based strain analysis techniques to quantify local strains. This is crucial for heterogeneous materials where mechanical properties vary across the specimen [55].
- Account for Anisotropy: Design tests to characterize material properties in multiple directions (e.g., axial, circumferential) if the biomaterial has a defined fiber orientation or layered structure [55].
- Validate Sensor Sensitivity: Ensure the testing system is calibrated for the expected force range, which can be orders of magnitude lower than for metals or plastics, requiring precise control over force and displacement [55].
Frequently Asked Questions (FAQs)
FAQ 1: What are the "Big Three" biocompatibility tests, and are they always required?
Answer: The "Big Three" refers to the core battery of tests for nearly all medical devices: cytotoxicity, sensitization, and irritation [5]. These assessments are a fundamental part of the biological evaluation according to ISO 10993-1. However, the necessity for testing is determined by a risk-based assessment of the final finished device, considering its nature of body contact and contact duration. If a device has no direct or indirect tissue contact, biocompatibility testing may not be needed [31] [5].
FAQ 2: How does the upcoming ISO 10993-1:2025 standard change how we determine "duration of contact"?
Answer: The 2025 update introduces more nuanced definitions, moving beyond a simple summation of seconds. Key changes include:
- Contact Day: Any contact within a 24-hour period counts as one full day of contact.
- Total Exposure Period: For devices with multiple exposures, the duration is the total number of calendar days from the first to the last use on a single patient.
- Foreseeable Misuse: You must now consider systematic misuse, such as using a device longer than intended, which could change the categorization from "prolonged" to "long-term" contact [8]. This more rigorous framework demands careful justification of the exposure scenario in the biological evaluation plan.
FAQ 3: Our new polymer is biodegradable. Why is its testing considered more complex than for a permanent implant?
Answer: Biodegradable materials introduce time-varying properties, adding layers of testing complexity:
- Dynamic Properties: Mechanical strength and mass change over time, requiring testing at multiple time points to simulate the entire degradation profile [25].
- Degradation Byproducts: You must identify and assess the biocompatibility of all chemical leachables and degradation products, not just the base polymer [43] [25].
- Bioactivity: The material should not be inert. Testing must verify that its interaction with biological systems positively stimulates target cells for tissue regeneration, rather than provoking an adverse foreign body response [43].
FAQ 4: What is the single most critical document for ensuring traceability during a regulatory audit?
Answer: The Device History Record (DHR) is critical for production traceability. It is a compilation of records proving the device was manufactured according to the Device Master Record (DMR) and includes data like dates of manufacture, quantity produced, and unique device identifiers (UDIs) for each batch [54]. For the design and development phase, the Design History File (DHF) provides the comprehensive audit trail [54].
Standardized Experimental Protocols
Protocol 1: In Vitro Cytotoxicity Testing by Extract Method (Based on ISO 10993-5)
This protocol evaluates the potential of a biomaterial to cause cell death using extracts of the test material.
1. Principle: Extracts of the test material are prepared and applied to cultured mammalian cells. After a defined exposure period, cell damage is quantified by measuring parameters such as cell viability, morphological changes, and cell lysis [5].
2. Workflow Diagram:
3. Materials and Reagents:
- Cell Line: L929 mouse fibroblasts or other validated lines (e.g., Balb 3T3) [5].
- Extraction Media: Serum-supplemented cell culture medium (for polar extracts) and vegetable oil or dimethyl sulfoxide (for non-polar extracts) as appropriate [5] [17].
- Viability Assay Kit: MTT, XTT, or Neutral Red uptake assay reagents [5].
- Equipment: COâ‚‚ incubator, biological safety cabinet, inverted microscope, multi-well plate reader.
4. Key Steps:
- Sample Preparation: Prepare the material extract per ISO 10993-12, using a surface area-to-volume ratio of 3-6 cm²/mL. Extract at 37°C for 24 hours [5] [17].
- Cell Seeding: Seed cells in a 96-well plate and culture until subconfluent.
- Exposure: Replace the culture medium with the material extract. Include a negative control (fresh medium) and a positive control (e.g., latex extract or phenol solution) [5].
- Incubation: Incubate the plate for 24 hours at 37°C and 5% CO₂.
- Viability Assessment: Perform the MTT assay by adding the MTT reagent, incubating for 2-4 hours, solubilizing the formazan crystals, and measuring the absorbance at 570 nm [5].
- Morphological Assessment: Examine cells under a microscope for signs of toxicity, such as rounding, detachment, or lysis.
5. Data Interpretation: Calculate the percentage of cell viability relative to the negative control. A reduction in cell viability to <70% is generally considered a sign of potential cytotoxicity and warrants further investigation, though acceptance criteria should be risk-based [5].
Protocol 2: Chemical Characterization for Biological Risk Assessment
This protocol identifies and quantifies leachable substances from a biomaterial, forming the basis for a toxicological risk assessment.
1. Principle: The material is extracted using simulating solvents, and the extracts are analyzed using analytical techniques to identify and quantify chemical constituents. The data is used to assess the potential biological risks of each leachable [54] [8].
2. Workflow Diagram:
3. Materials and Reagents:
- Extraction Solvents: Polar (e.g., saline, water) and non-polar (e.g., hexane, ethanol) solvents to simulate different physiological conditions [17].
- Analytical Standards: Certified reference standards for suspected leachables (e.g., polymer monomers, plasticizers, antioxidants).
- Equipment: Liquid Chromatograph with Mass Spectrometry (LC-MS), Gas Chromatograph with Mass Spectrometry (GC-MS), Inductively Coupled Plasma Mass Spectrometry (ICP-MS) for metals.
4. Key Steps:
- Extraction: Extract the material under accelerated conditions (e.g., 50-70°C for 72 hours) to obtain a worst-case scenario of leachables [17].
- Analysis: Screen the extracts using LC-MS and GC-MS to separate and tentatively identify organic leachables. Use ICP-MS for inorganic elements.
- Quantification: Quantify the identified substances using calibrated methods with reference standards.
- Risk Assessment: For each identified substance, calculate the estimated daily exposure dose and compare it to established safety thresholds (e.g., Allowable Limit, PDE) derived from toxicological data. This process is central to the risk management framework emphasized in ISO 10993-1:2025 [8].
5. Data Interpretation: The biological risk is considered controlled if the total estimated exposure for all leachables remains below the relevant toxicological thresholds. If a risk is identified, material reformulation or process changes are required.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key materials and reagents essential for standardized biomaterial testing.
| Item Name | Function/Application in Testing | Key Considerations |
|---|---|---|
| L929 Fibroblasts | Standardized cell line for cytotoxicity testing (ISO 10993-5) [5]. | Use low passage number; maintain consistent culture conditions to ensure assay reproducibility. |
| MTT Reagent | (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-2H-tetrazolium bromide); used to quantitatively assess cell viability [5]. | Light-sensitive; prepare fresh solutions or aliquot and freeze. Ensure proper solubilization of formazan product. |
| Reference Materials | Materials with known biological reactivity (e.g., USP plastic classes) used as controls in biocompatibility tests [17]. | Essential for validating test method performance and comparing results across different labs. |
| ClicKit-Well System | A deformable, perforated frame that creates standardized wells directly on a material sample for in-vitro testing [53]. | Minimizes errors from sample geometry and placement in traditional well plates, improving data consistency. |
| Extraction Solvents | A panel of solvents (saline, culture medium, vegetable oil, ethanol) used to prepare material extracts [5] [17]. | Coverage of polar and non-polar chemicals ensures a comprehensive assessment of leachable substances. |
The shift from traditional immortalized cell lines to human primary cells represents a significant evolution in preclinical research, particularly for biomaterial testing. While cell lines offer convenience, primary cells provide unparalleled physiological relevance, more accurately mimicking the in vivo environment. This transition, however, introduces new challenges in standardization, protocol development, and technical handling. This technical support center is designed to help researchers, scientists, and drug development professionals overcome these hurdles, providing actionable troubleshooting guides and FAQs to ensure the generation of reliable, human-relevant data.
Frequently Asked Questions (FAQs)
What are the primary advantages of using human primary cells over immortalized cell lines?
Human primary cells are isolated directly from human tissue and retain the genetic and phenotypic stability of their tissue of origin. Unlike immortalized cell lines—which are often cancer-derived and genetically modified for infinite division—primary cells have a finite lifespan, which helps prevent the genetic drift and proteomic changes commonly seen in long-cultured cell lines [56]. This makes them superior for modeling normal physiology and disease states, leading to more translational research outcomes and data that are more predictive of human in vivo responses [57] [58] [56].
My primary cells are senescing too quickly. What could be the cause?
Premature senescence in primary cells is frequently linked to their fundamental biological nature and specific culture conditions. Key factors to investigate include:
- The Hayflick Limit: Primary cells have a predetermined, finite number of cell divisions before they naturally enter senescence [58].
- Culture Conditions: Suboptimal conditions are a common culprit. This includes using inappropriate growth media that lacks necessary tissue-specific cytokines and growth factors, or consistently passaging cells at very high densities (e.g., 100% confluence). Post-confluent cells may differentiate and senesce more rapidly [58].
- Handling Stress: Excessive exposure to proteolytic enzymes like trypsin during subculturing or overly harsh centrifugation can damage cells and accelerate aging [58].
How can I improve the reproducibility of my experiments when using primary cells?
Reproducibility is challenged by the inherent donor-to-donor variability of primary cells [57]. To improve consistency:
- Source Commercially Available Primary Cells: Reputable suppliers provide cells that are performance-tested, quality-controlled, and pre-screened for viruses, ensuring a standardized and safe starting material [58].
- Use Standardized Culture Systems: Utilize a complete system from a single vendor, including the cells, basal media, and cell-specific growth kits. These components are tested together for optimal reliability [58].
- Consider Advanced Alternative Models: New technologies like ioCells (human iPSC-derived cells programmed with opti-ox technology) are designed to offer human relevance with less than 2% gene expression variability across lots, directly addressing the reproducibility challenge [57].
Are there specific biomaterial properties that are critical to test with primary cells?
Yes, when evaluating biomaterials for applications like tissue engineering, the composition and a broad range of material properties significantly influence primary cell behavior and tissue outcomes. Critical properties to evaluate include [59]:
- Surface characteristics
- Degradation rate
- Mechanical strength
These properties can impact primary cell functions such as immune defense, sensory perception, vascularization, and reparative dentinogenesis, underscoring the need for robust and standardized evaluation methods [59].
Troubleshooting Guides
Issue 1: Low Post-Thaw Viability of Cryopreserved Primary Cells
Problem: A high percentage of cells are non-viable upon thawing, leading to poor attachment and growth.
Solution:
- Thawing Protocol:
- Rapid Thaw: Immerse the cryovial directly in a 37°C water bath until only a small ice crystal remains (approximately 1-2 minutes) [60] [58].
- Immediate Dilution: Gently transfer the cell suspension to a tube containing a larger volume (e.g., 10 mL) of pre-warmed complete growth medium. This quickly dilutes the cytotoxic cryoprotectant (e.g., DMSO).
- Gentle Centrifugation: Centrifuge at 200-250 x g for 5 minutes to pellet the cells. Carefully remove the supernatant containing the DMSO [60].
- Resuspend and Plate: Resuspend the cell pellet in fresh, pre-warmed growth medium and seed them into a culture vessel [60].
- Preventative Measures:
- Use a controlled-rate freezing device to freeze cells slowly at -1°C per minute before long-term storage in liquid nitrogen. This minimizes lethal ice crystal formation within the cells [60] [58].
- For certain sensitive primary cells, plate them directly upon thawing and allow them to attach for 24 hours before changing the medium to remove residual DMSO [58].
Issue 2: Failure to Attach to the Culture Surface
Problem: Cells remain in suspension and do not form a monolayer.
Solution:
- Verify Surface Coating: Ensure the culture vessel is appropriately coated with extracellular matrix proteins (e.g., collagen, fibronectin) if required by your specific cell type.
- Check Cell State: Confirm the cells were thawed correctly and that post-thaw viability was assessed.
- Assess Culture Conditions:
- Inspect Seeding Density: Seed cells at the recommended density; a too-low density can inhibit attachment and growth.
Issue 3: Inconsistent Results Between Experiments
Problem: High variability in data obtained from different batches of primary cells.
Solution:
- Minimize Technical Variability:
- Account for Biological Variability:
- For donor-specific studies, plan to use cells from multiple donors (n≥3) to understand population-wide effects.
- For consistent screening work, consider using genetically defined, human iPSC-derived cells like ioCells, which offer high batch-to-batch consistency [57].
- Quality Control: Only use primary cells from suppliers that provide comprehensive data, including sterility testing, viability checks, and cell-specific marker expression profiles [58].
The following workflow outlines the logical steps for diagnosing and resolving the most common issues encountered when working with primary cells:
Essential Research Reagents and Materials
The following table details key reagents and materials essential for successful primary cell culture, along with their specific functions in supporting cell health and experimental consistency.
| Reagent/Material | Function & Importance in Primary Cell Culture |
|---|---|
| Complete Growth Medium | A basal medium supplemented with tissue-specific growth factors, cytokines, and hormones. Critical for maintaining cell phenotype and proliferation, as primary cells have fastidious nutrient requirements [58]. |
| Cryoprotectant (e.g., DMSO) | Permeates the cell to lower the freezing point and prevent lethal intracellular ice crystal formation during cryopreservation. Typically used at 5-10% concentration [60]. |
| Extracellular Matrix (ECM) Coating | Proteins like collagen or fibronectin that coat the culture surface, mimicking the in vivo basement membrane. Essential for the attachment and survival of anchorage-dependent primary cells [58]. |
| Cell Detachment Agent | A proteolytic enzyme (e.g., trypsin) often combined with EDTA, used to gently dissociate adherent cells from the culture surface for subculturing. Low concentrations are vital to avoid damaging sensitive primary cells [58]. |
| Defined Supplements (e.g., FBS) | Serum or defined supplements provide a source of proteins, lipids, and attachment factors. Low-serum or serum-free formulations are often preferred to ensure consistency and avoid undefined components [58]. |
Supporting Data and Market Context
The growing recognition of the value of primary cells is reflected in the market data and quantitative comparisons with traditional models. The table below summarizes a direct comparison of key features across different cell models to aid in experimental planning.
Table 1: Comparative Analysis of Cell Model Features for Experimental Planning [57]
| Feature | Animal Primary Cells | Immortalized Cell Lines | ioCells (iPSC-derived) |
|---|---|---|---|
| Biological Relevance | Closer to native morphology and function | Often non-physiological (e.g., cancer-derived) | Human-specific and characterised for functionality |
| Reproducibility | High variability (donor-to-donor) | Reliable, but prone to genetic drift | High consistency (<2% gene expression variability) |
| Scalability | Low yield, difficult to expand | Easily scalable | Consistent at scale (billions per run) |
| Ease of Use | Technically complex, time-intensive | Simple to culture | Ready-to-use, no special handling required |
| Human Origin | Typically rodent-derived | Often non-human | Derived from human iPSCs |
Table 2: Human Primary Cell Culture Market Snapshot (2025-2032) [61]
| Segment | Projected Market Share in 2025 | Key Driver |
|---|---|---|
| Overall Market Value | USD 4.10 Billion (2025) | Rising prevalence of chronic diseases and adoption of personalized medicines [61]. |
| Product Type | Primary Cells (32.1%) | Critical role in advancing cellular research and therapeutics development [61]. |
| Application | Cell & Gene Therapy (41.3%) | Rising demand for clinically-relevant cells as building blocks for advanced therapies [61]. |
| Region | North America (41.5%) | Strong research infrastructure and presence of leading pharmaceutical companies [61]. |
Integration of In Silico Modeling and Machine Learning
The integration of in silico modeling and machine learning (ML) is transforming biomaterial testing protocols, offering powerful tools to accelerate discovery and enhance predictive accuracy. However, this rapidly evolving field presents significant standardization challenges. Researchers and developers encounter inconsistencies in model validation, data quality requirements, and regulatory acceptance. This technical support center addresses these hurdles through targeted troubleshooting guides and FAQs, providing clear methodologies to standardize your experimental workflows and improve the reliability of your computational approaches.
Troubleshooting Guides
Guide 1: Addressing Data Quality and Availability Issues
Problem: Machine learning models for biomaterial design are producing unreliable or non-generalizable predictions.
Explanation: The performance of ML models is heavily dependent on the quality, quantity, and consistency of training data. In biomaterials, data is often scarce, inconsistently generated across labs, or lacks standardized formatting, leading to the "curse of dimensionality" where too many features exist relative to data points [62].
Solution:
- Step 1: Implement data preprocessing protocols. Use feature selection algorithms to reduce dimensionality and focus on the most critical material attributes (e.g., composition, surface topography, porosity) [62] [63].
- Step 2: Employ data augmentation techniques. Utilize generative adversarial networks (GANs) to create synthetic data that expands your training set, improving model robustness [64] [63].
- Step 3: Adopt standardized data formats. Align experimental data collection with FAIR principles (Findable, Accessible, Interoperable, Reusable) to ensure consistency and enable data mining from public repositories [65].
Guide 2: Managing Model Interpretability and Validation
Problem: A "black-box" ML model provides a promising prediction for a new biomaterial, but the underlying reasoning is unclear, making validation and regulatory approval difficult.
Explanation: Complex models like deep neural networks can be difficult to interpret. For biomaterials, understanding the structure-function relationship is crucial, and regulators require transparent evidence for safety and efficacy claims [63] [54].
Solution:
- Step 1: Integrate the Adverse Outcome Pathway (AOP) framework. Use AOPs as a biological scaffold to organize knowledge and link ML-predicted molecular interactions (Molecular Initiating Events) to adverse outcomes of regulatory concern [66].
- Step 2: Apply explainable AI (XAI) techniques. Use tools like SHAP (SHapley Additive exPlanations) to identify which input features (e.g., polymer flexibility index, surface wettability) most influenced the model's output [62] [63].
- Step 3: Validate with orthogonal in silico methods. Corroborate ML predictions with mechanistic modeling, such as molecular dynamics simulations, to provide evidence for structural stability and interaction dynamics, as demonstrated in PMMA-biomolecule studies [67].
Guide 3: Bridging the Gap Between In Silico and Clinical Translation
Problem: Successful in silico results fail to predict biomaterial performance in pre-clinical or clinical settings.
Explanation: This often stems from a failure to account for inter-individual physiological variability (e.g., age, organ function, genetics) and the complexities of the biological environment in the models [64].
Solution:
- Step 1: Utilize virtual populations in PBPK/QST models. Incorporate physiological variability by using existing virtual populations for specific groups (e.g., pediatrics, geriatrics, patients with renal impairment) to simulate a wider range of real-world responses [64].
- Step 2: Incorporate real-world data (RWD). Feed clinical data from electronic health records or post-market surveillance back into your models to iteratively refine and validate them against human outcomes [65] [64].
- Step 3: Establish a continuous validation loop. Create a workflow where in silico predictions inform targeted in vitro (e.g., 3D tissue models, organ-on-a-chip) and pre-clinical studies, the results of which then refine the computational models [68].
Frequently Asked Questions (FAQs)
FAQ 1: What are the most suitable machine learning algorithms for predicting biomaterial-biomolecule interactions?
The choice of algorithm depends on your data and the problem type. For classification tasks (e.g., predicting biocompatibility: compatible/non-compatible), Support Vector Machines (SVM) and Random Forests are often effective [63]. For regression tasks (e.g., predicting a continuous value like degradation rate), linear regression, ridge regression, and gradient boosting machines are commonly used [63]. For complex pattern recognition in high-dimensional data, Deep Learning (DL) models, a subset of ML, can be powerful but require larger datasets [63].
FAQ 2: How can we standardize the validation process for an in silico model to meet regulatory expectations?
A robust validation strategy is multi-faceted. First, ensure external validation by testing the model on a completely independent dataset not used in training. Second, establish context of use by clearly defining the model's purpose and limitations. Third, employ modular verification by validating sub-models (e.g., a molecular docking simulation) independently. Finally, maintain comprehensive documentation in a Design History File (DHF), detailing all design inputs, outputs, and validation activities, as required for medical devices [54]. Regulatory agencies are increasingly receptive to well-validated in vitro and computational models as part of the evidence package [68].
FAQ 3: Our molecular dynamics simulations are computationally expensive and slow down our workflow. How can we optimize this?
Consider a multi-fidelity modeling approach. Use coarse-grained models for initial, rapid screening to identify promising candidates. Then, apply more detailed and computationally intensive all-atom molecular dynamics simulations only to the top candidates [67]. Furthermore, you can use ML surrogate models trained on the results of a limited number of full simulations to quickly predict outcomes for new, similar materials, drastically reducing computation time [69] [70].
FAQ 4: How can we effectively integrate data from diverse sources (e.g., high-throughput experimentation, literature mining) for machine learning?
The AOP framework is an excellent tool for this integration. It provides a structured "biological space" to organize disparate data [66]. Key Events (KEs) from AOPs, such as specific protein receptor bindings or cellular responses, can serve as standardized nodes. Data from various sources can be mapped onto these KEs, creating a unified and biologically meaningful dataset for training ML models that predict adverse outcomes along a known causal pathway [66].
Standardized Experimental Protocols
Protocol 1: Molecular Docking and Dynamics for Biocompatibility Assessment
This protocol provides a methodology for evaluating the binding affinities and interactions of a biomaterial (or its monomeric units) with biological targets, a key aspect of assessing biocompatibility at a molecular level [67].
1. Receptor and Ligand Preparation:
- Receptor Selection: Identify and select protein receptors relevant to your biomaterial's application (e.g., RANKL, Fibronectin for bone metabolism). Obtain their 3D structures from the Protein Data Bank (PDB) or AlphaFold database [67].
- Active Site Identification: Use computational tools like CASTp 3.0 to identify the active binding sites on your selected receptors [67].
- Ligand Preparation: Construct the 3D molecular structure of your biomaterial/compound. Perform energy minimization using a force field (e.g., MM2) in molecular modeling software (e.g., Chem3D) to obtain a stable, low-energy conformation [67].
2. Molecular Docking Simulation:
- Software: Utilize docking software like HADDOCK.
- Method: Employ a Lamarckian genetic algorithm to explore the conformational space of the ligand-receptor interaction. Perform the docking calculation to predict the binding pose, affinity, and steric features of the complex [67].
3. Molecular Dynamics (MD) Simulation:
- Software: Use MD packages like GROMACS.
- Method: Solvate the docked complex in a water box, add ions to neutralize the system, and run a dynamics simulation for a sufficient time (e.g., 100 nanoseconds). This step evaluates the stability of the complex and the dynamic interactions over time [67].
4. Analysis and Pharmacophore Modeling:
- Analyze the MD trajectories for root-mean-square deviation (RMSD) to assess stability.
- Use a tool like LigandScout for pharmacophore modeling to identify critical functional groups (e.g., carbonyl groups) involved in binding, which informs on biocompatibility [67].
Protocol 2: Developing a QST Model for Drug-Induced Toxicity Prediction
This protocol outlines the steps for creating a Quantitative Systems Toxicology (QST) model to predict organ-specific toxicity, such as Drug-Induced Liver Injury (DILI), in specific populations like postmenopausal women [64].
1. Systems Model Construction:
- Define the Scope: Identify the biological system (e.g., liver), the toxicity (e.g., DILI), and the key physiological pathways involved (e.g., oxidative stress, bile acid transport).
- Gather Mechanistic Data: Mine literature and databases for quantitative data on the rates and dynamics of the key events in the chosen pathways.
2. Virtual Population Generation:
- Identify Key Variability: Determine the physiological parameters that vary in the target population (e.g., for postmenopausal women, consider hormone levels, body composition, liver enzyme activity).
- Incorporate Real-World Data (RWD): Use RWD from electronic health records or clinical trials to define the statistical distributions of these parameters and create a virtual population that reflects real-world variability [64].
3. Model Simulation and Validation:
- Run Simulations: Execute the QST model with the virtual population to simulate the incidence and severity of the adverse outcome (e.g., DILI) across a range of drug exposures.
- Validate Predictions: Compare the model's predictions against existing clinical data or dedicated in vitro studies (e.g., using human liver organoids) to assess its predictive accuracy [64] [68].
4. Application and Refinement:
- Use the validated model to simulate the toxicological risk of new drug candidates in the target virtual population.
- Establish a feedback loop where new experimental and clinical data are continuously used to refine and update the model [64].
Essential Visualizations
Diagram 1: Integrated In Silico and Experimental Workflow
This diagram illustrates a standardized, iterative workflow for biomaterial development that integrates in silico modeling and machine learning with experimental validation.
Diagram 2: Adverse Outcome Pathway Framework for Biomarker Identification
This diagram shows how the AOP framework organizes knowledge from molecular events to adverse outcomes, aiding in the identification and validation of biomarkers for biomaterial testing.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key software tools, databases, and frameworks essential for conducting integrated in silico and machine learning research in biomaterials.
Table: Essential Computational Tools for Integrated Biomaterial Research
| Tool Name | Type | Primary Function | Relevance to Standardization |
|---|---|---|---|
| GROMACS [67] | Software Package | Molecular Dynamics (MD) Simulation | Provides a standardized, open-source platform for simulating biomaterial-biological molecule interactions and assessing structural stability. |
| HADDOCK [67] | Software Package | Molecular Docking | Uses standardized algorithms (e.g., Lamarckian genetic) to predict binding affinities and poses, enabling comparative studies. |
| AOP-Wiki / AOP-KB [66] | Knowledge Base | Adverse Outcome Pathway Repository | Offers a curated, collaborative framework for organizing toxicological knowledge, crucial for standardizing the biological context of ML models. |
| LigandScout [67] | Software Tool | Pharmacophore Modeling | Identifies essential interaction features in a compound, helping to standardize assessments of biocompatibility. |
| Protein Data Bank (PDB) [67] | Database | 3D Protein Structures | Provides standardized, high-quality structural data for receptors, essential for consistent molecular docking studies. |
| Chem3D / MM2 Force Field [67] | Modeling Software & Force Field | 3D Structure Modeling & Energy Minimization | Standardizes the initial preparation of ligand (biomaterial) structures, ensuring simulations start from an energetically stable conformation. |
| Virtual Populations [64] | Data Resource | Simulated Patient Cohorts | Provides standardized demographic and physiological data for PBPK/QST models, improving the translation of results to specific human populations. |
Multi-modal Imaging and Non-Destructive Testing Methods
Technical Support Center: Troubleshooting & FAQs
FAQ: General Principles
Q1: What is the primary advantage of using a multi-modal approach over a single technique?
- A: Multi-modal imaging synergizes the strengths of individual techniques to provide comprehensive data. For example, Micro-CT offers excellent 3D structural data but lacks molecular specificity. Fluorescence imaging provides high sensitivity for specific biomarkers but has limited depth penetration. By combining them, you can precisely co-localize a fluorescently-tagged cellular event (e.g., inflammation) within a 3D scaffold structure, overcoming the limitations of each method.
Q2: How do I choose the right combination of modalities for my biomaterial study?
- A: The choice depends on your key research question and the properties of your biomaterial. Refer to the table below for a comparative guide.
| Modality | Spatial Resolution | Penetration Depth | Key Measurable Parameters | Best for Biomaterial Properties |
|---|---|---|---|---|
| Micro-CT | 1-50 µm | 1-10 cm (sample dependent) | Volume, Porosity, Morphology, Degradation | Scaffold architecture, mineral content, integration with host bone. |
| MRI | 10-100 µm | mm - cm | Water content, Diffusion, Soft Tissue Contrast | Hydrogel swelling, pore interconnectivity, soft tissue integration. |
| Ultrasound | 50-500 µm | mm - cm | Elasticity, Density, Viscosity | Mechanical integrity, non-invasive monitoring in vivo. |
| Fluorescence Imaging | 1-5 µm | < 1 cm | Biomarker Expression, Cell Viability, Drug Release | Cellular infiltration, inflammatory response, targeted drug delivery. |
| Raman Spectroscopy | 0.5-1 µm | µm - mm | Chemical Composition, Crystallinity | Polymer degradation, protein secondary structure, drug distribution. |
Troubleshooting Guide: Common Experimental Issues
Issue #1: Poor Signal-to-Noise Ratio in Fluorescence Imaging of a Deep-Tissue Scaffold.
- Problem: The fluorescent signal from cells within a thick ( > 500 µm) polymer scaffold is weak and obscured by background noise.
- Solution:
- Reagent Check: Use near-infrared (NIR) fluorophores (e.g., Cy5.5, ICG) which experience less scattering and absorption by tissue compared to visible light fluorophores.
- Sample Preparation: Ensure thorough clearing of the sample using optical clearing agents (e.g., CUBIC, ScaleS) to reduce light scattering.
- Instrument Calibration: Confirm that your imaging system (e.g., Confocal, Light Sheet) is calibrated for the specific fluorophore's excitation/emission wavelengths. Use high-sensitivity detectors (e.g., GaAsP PMTs).
- Experimental Protocol (Ex Vivo):
- Fixation: Perfuse and fix the explanted scaffold-tissue construct with 4% PFA for 24 hours.
- Clearing: Immerse the sample in CUBIC-1 reagent at 37°C for 3-7 days with gentle agitation.
- Staining & Washing: Incubate with primary/secondary antibodies conjugated to an NIR fluorophore. Perform all washes in the clearing reagent.
- Imaging: Mount the cleared sample and image using a light sheet fluorescence microscope for rapid, high-contrast 3D acquisition.
Issue #2: Difficulty Correlating Micro-CT and Histology Data Accurately.
- Problem: It is challenging to precisely match a 2D histological slice with its exact corresponding location in the 3D Micro-CT volume.
- Solution: Implement a fiduciary marker system.
- Embedding: Before embedding in paraffin or resin, drill micro-holes (using a micro-drill) or place inert, radio-opaque pins (e.g., tungsten) at known, asymmetric positions in the sample block.
- Imaging: Perform Micro-CT scanning. The pins will appear as high-density landmarks in the 3D volume.
- Sectioning: During sectioning for histology, the pins will create visible holes or marks on the slices.
- Registration: Use the landmarks in both datasets for precise 2D-to-3D co-registration using software like 3D Slicer or Amira.
- Experimental Protocol:
- After explantation, use a 200 µm diameter tungsten drill bit to create three asymmetric fiducial marks around the sample.
- Scan the sample via Micro-CT (e.g., 10 µm voxel size, 70 kVp).
- Process, embed, and section the sample following standard histological protocols.
- Digitize the histological slides and use the fiducial marks to align the 2D section with the 3D Micro-CT data.
Issue #3: Inconsistent Results in Ultrasound Elastography Measurements.
- Problem: Measured Young's modulus values for the same hydrogel biomaterial vary significantly between experiments.
- Solution:
- Coupling: Ensure consistent and complete acoustic coupling between the transducer and the sample. Use a standardized amount of ultrasound gel and apply consistent, minimal pressure.
- Calibration: Regularly calibrate the ultrasound system using phantoms with known mechanical properties.
- Environmental Control: Perform all measurements in a temperature-controlled environment, as hydrogel stiffness is highly temperature-sensitive.
- Experimental Protocol:
- Sample Preparation: Prepare hydrogel discs (e.g., 10mm diameter, 3mm height) in a standardized mold.
- Temperature Equilibration: Place samples in a PBS bath at 37°C for 1 hour before testing.
- Measurement: Use a high-frequency ultrasound system (e.g., 40 MHz) with a shear wave elastography module. Apply a thin, uniform layer of gel. Take five measurements at different locations on each sample and report the mean ± standard deviation.
The Scientist's Toolkit: Essential Reagents & Materials
| Item | Function / Application |
|---|---|
| NIR Fluorophores (e.g., Cy7, IRDye 800CW) | Enables deep-tissue fluorescence imaging by minimizing light absorption and scattering. |
| Optical Clearing Agents (e.g., CUBIC, ScaleA2) | Renders biological tissues transparent by matching refractive indices, allowing deeper light penetration. |
| Radio-Opaque Contrast Agents (e.g., Iohexol, Gold Nanoparticles) | Enhances X-ray absorption in Micro-CT, used for visualizing soft biomaterials or vascularization. |
| Fiduciary Markers (e.g., Tungsten Pins, Carbon Fiber) | Provides physical reference points for accurate spatial correlation between different imaging modalities. |
| Ultrasound Phantoms with Known Stiffness | Calibrates ultrasound elastography systems to ensure quantitative accuracy of mechanical measurements. |
| Heavy Metal Stains (e.g., Phosphotungstic Acid) | Stains soft biomaterials and tissues for higher contrast in Micro-CT and electron microscopy. |
Visualization: Experimental Workflows
Multi-modal Imaging Workflow
Correlative Micro-CT & Fluorescence
Life Cycle Analysis and Sustainable Assessment Integration
Troubleshooting Common LCA Challenges in Biomaterial Development
FAQs: Addressing Critical Methodology Issues
Q1: How can we account for scaling effects when assessing early-stage bio-based technologies? Early-stage bio-based technologies often operate at lab or pilot scale, which doesn't represent optimized industrial conditions. This makes robust comparison with fossil-based alternatives challenging. Implement a combined ex-ante and prospective LCA framework that modifies process inventories and projects them to future industrial scale. This approach can reduce climate change impact estimates significantly—from 105–471 kg CO₂-eq./kg of polymer to 9–14 kg CO₂-eq./kg after scaling projections, with process synergies (like solvent recovery) contributing up to 83% reduction [71].
Q2: What are the main challenges in standardizing biomaterial testing protocols? Standardization requires metrological traceability, ensuring measurements are comparable across time, place, and procedures. Key challenges include:
- Lack of clearly defined measurands (analytes to be measured)
- Insufficient reference methods and materials
- Non-commutable reference materials that lead to inaccurate results
- Complex harmonization needs when full standardization isn't possible [72]
Q3: How do we manage uncertainty in biocompatibility testing? Materials and biological responses are inherently variable. Implement these strategies:
- Use confidence levels as quantifiable measures of certainty for compound identification
- Apply robust analytical methodologies sensitive enough to meet Analytical Evaluation Thresholds (AETs)
- Employ multiple scientifically validated methods tailored to device characteristics
- Document rationales for confidence levels with supporting data [48]
Q4: What documentation is essential for biomaterial validation? Comprehensive documentation demonstrates regulatory compliance and ensures quality:
- Design History File (DHF): Chronicles design and development processes
- Device Master Record (DMR): Manufacturing instructions and specifications
- Device History Record (DHR): Production batch records
- Testing/Inspection Records: Biocompatibility, mechanical, and chemical stability results
- Risk Management Documentation: Assessments, mitigation plans, and post-market surveillance [54]
Quantitative Data Tables for LCA Impact Reduction
Table 1: Environmental Impact Reduction Through Combined LCA Approaches
| Impact Category | Lab-Scale Impact | After Ex-Ante LCA | Additional Reduction with Prospective LCA | Total Reduction |
|---|---|---|---|---|
| Climate Change | 105-471 kg COâ‚‚-eq./kg polymer | 9-14 kg COâ‚‚-eq./kg polymer | Up to 56% by 2050 | 83-97% |
| Freshwater Eutrophication | Not specified | Not specified | Up to 99% | Up to 99% |
| Photochemical Oxidant Formation | Not specified | Not specified | Up to 99% | Up to 99% |
| Marine Eutrophication | Not specified | Not specified | Up to 98% | Up to 98% |
Source: [71]
Table 2: Standardization vs. Harmonization Approaches
| Aspect | Standardization | Harmonization |
|---|---|---|
| Reference System | SI-traceable reference methods/materials | Conventionally agreed reference system |
| Measurand Definition | Clearly defined | May not be clearly defined |
| Traceability | To higher-order reference system | To agreed-upon conventional reference |
| Applicability | Limited number of well-defined analytes | Broader range of complex biomaterials |
| Example | CDC Hormones Standardization Program | IFCC approach for Thyroid-Stimulating Hormone |
Source: [72]
Experimental Protocol: Ex-Ante LCA for Early-Stage Biomaterials
Objective: Project environmental impacts of lab-scale biomaterial production to industrial scale for accurate comparison with conventional materials.
Methodology:
- Inventory Development: Compile complete material and energy inputs/outputs from lab-scale processes
- Process Modification: Identify and model scale-up effects including:
- Equipment efficiency improvements
- Energy integration opportunities
- Mass and heat recovery systems
- Process optimization and yield improvements
- Synergy Identification: Identify process synergies such as solvent recovery systems
- Background System Projection: Model future changes in background systems (energy grid, transportation)
- Impact Assessment: Calculate environmental impacts using standardized LCA methods (ISO 14040/14044)
Critical Controls:
- Maintain consistent functional unit across all comparisons
- Include uncertainty analysis for scaling factors
- Validate projections with expert consultation and sensitivity analysis
- Use site-specific data where available, generic data where necessary [71]
Troubleshooting Guide: Systematic Problem-Solving Framework
When encountering unexpected LCA results or biomaterial testing failures, follow this structured approach:
Identify the Problem
- Define the specific discrepancy without presuming causes
- Compare expected versus actual results quantitatively
- Verify the experimental system is functioning properly
List Possible Explanations
- Consider all components: materials, methods, equipment, operators
- Include both obvious and subtle potential causes
- Document without pre-judgment
Collect Data Systematically
- Review controls: positive, negative, and procedural
- Verify storage conditions and expiration dates of reagents
- Compare procedures with established protocols
- Check equipment calibration and maintenance records
Eliminate Explanations
- Use data to rule out incorrect hypotheses
- Prioritize based on probability and testability
- Document rationale for elimination
Test Remaining Hypotheses
- Change only one variable at a time
- Design experiments to isolate specific factors
- Include appropriate controls in each test
Identify Root Cause
Workflow Visualization: LCA Integration Framework
LCA Integration Workflow from Lab to Industrial Scale
Research Reagent Solutions for Biomaterial Assessment
Table 3: Essential Materials for Biomaterial Testing and LCA
| Reagent/Material | Function | Application Context |
|---|---|---|
| Reference Measurement Procedures | Higher-order analytical methods for value assignment | Standardization of clinical measurements [72] |
| Commutable Reference Materials | Ensure traceability established appropriately | Calibration verification across measurement procedures [72] |
| Single-Donor Serum Panels | Authentic patient samples for comparability assessment | Verification of measurement uniformity across methods [72] |
| ISO 10993-1 Biological Evaluation | Standardized biocompatibility testing framework | Assessment of medical device biological safety [31] |
| Validated Analytical Methods | Techniques meeting Analytical Evaluation Thresholds | Accurate compound identification in extracts [48] |
Standardization Pathway for Biomaterial Testing
Standardization Pathway for Comparable Results
Troubleshooting Biocompatibility Testing Issues
Common Problem: Failure to meet Analytical Evaluation Thresholds (AETs)
Symptoms:
- Inconsistent results across testing batches
- Inability to detect compounds at required concentrations
- Regulatory questions about testing sensitivity
Solution Protocol:
- Methodology Enhancement
- Implement advanced analytical techniques with greater sensitivity
- Validate methods for specific device characteristics
- Use multiple complementary analytical approaches
Uncertainty Management
- Assign and justify confidence levels for each identification
- Document rationale for confidence determinations
- Incorporate worst-case scenario testing
Material Characterization
- Conduct early and thorough material analysis
- Verify supplier-provided material specifications
- Anticipate potential extraction compounds [48]
Validation: Test revised methodologies with control materials of known composition and concentration to verify AET compliance before proceeding with device testing.
Documentation Checklist for Biomaterial Validation
- Design History File (DHF) with complete design inputs/outputs
- Device Master Record (DMR) with manufacturing specifications
- Device History Record (DHR) for each production batch
- Biocompatibility testing per ISO 10993-1 requirements
- Material characterization reports
- Risk management documentation
- Sterilization validation records (if applicable)
- Stability testing data
- Clinical evaluation reports (if applicable)
- Post-market surveillance plan [31] [54]
Ensuring Safety and Efficacy: Validation, Documentation, and Comparative Analysis
Analytical, Clinical, and Biological Validation Requirements
This technical support center provides troubleshooting guides and frequently asked questions (FAQs) for researchers navigating the complex landscape of validation in biomaterials research. The content is framed within the broader context of standardizing testing protocols, addressing common pitfalls in analytical, clinical, and biological validation.
## Troubleshooting Guide: Biological Evaluation of Medical Devices
Q1: Our biological evaluation results were questioned by a regulatory body for not adequately considering "reasonably foreseeable misuse." How should we have addressed this?
A1: The 2025 update to ISO 10993-1 explicitly integrates concepts from risk management standards (ISO 14971), making the consideration of reasonably foreseeable misuse a mandatory part of the biological risk assessment [8]. Your evaluation plan should have:
- Defined Misuse Scenarios: Systematically identified use of the device outside its intended purpose, such as use for a longer duration than specified in the Instructions for Use (IFU) or in an unintended anatomical location [8].
- Utilized Available Data: Incorporated post-market surveillance data and clinical literature from similar devices to predict systematic misuse patterns [8].
- Expanded Testing Scope: Justified the duration of exposure and categorization of the device based on the total exposure period from all potential uses, including misuse, not just the ideal use case [8].
Q2: How do we correctly determine the "contact duration" for a device with potential for multiple uses?
A2: The ISO 10993-1:2025 standard provides specific definitions for calculating exposure. The process is more nuanced than simple stopwatch timing [8].
- Key Definitions:
- Contact Day: Any day in which the device contacts tissues, irrespective of the length of time within that day.
- Total Exposure Period: The number of contact days between the first and last use of a medical device on a single patient [8].
- Calculation Method:
- For daily contact devices, the total exposure period is the number of calendar days from first to last use.
- For intermittent contact devices (with at least 24 hours between contacts), sum the number of contact days.
- Critical Consideration: A single exposure is a minimum of one day. Two exposures can move a device from "limited" (≤24 hours) to "prolonged" (24 hours to 30 days) duration [8].
Determining Device Contact Duration
## Troubleshooting Guide: Analytical Method Validation
Q3: Our analytical method validation for a biomaterial's degradation byproducts failed during a technology transfer to a new lab. Which parameters are most critical to ensure robustness?
A3: Failure during transfer often indicates insufficient assessment of precision and robustness. Per ICH Q2(R2) and Q14 guidelines, you must demonstrate the method is fit-for-purpose across different environments [75] [76].
- Critical Parameters to Re-check:
- Intermediate Precision: Test the method on different days, with different analysts, and using different equipment. The %RSD (Relative Standard Deviation) for repeatability and intermediate precision should be predefined and justified (e.g., often ≤2% for assay methods) [76].
- Robustness: Deliberately vary method parameters (e.g., pH, temperature, flow rate in HPLC) within a realistic range to ensure the method's reliability. ICH Q14 now encourages a more formal, science-based approach to this [75].
- Specificity: Prove the method can unequivocally quantify the analyte (e.g., a specific degradation byproduct) in the presence of other potential components like impurities, excipients, or the biomaterial matrix itself [76].
Q4: What is the modern, proactive approach to analytical procedure development that can prevent validation failures later?
A4: The latest ICH guidelines (Q2(R2) and Q14) advocate for a lifecycle management approach, moving away from a one-time "check-the-box" validation [75].
- Implement an Analytical Target Profile (ATP): Before development, define a prospective summary of the method's required performance characteristics (e.g., "The method must quantify impurity X with an accuracy of 98-102% and a precision of ≤2% RSD") [75] [76].
- Adopt a Risk-Based Approach: Use quality risk management (ICH Q9) to identify potential sources of variability during development. This informs your robustness studies and control strategy [75].
- Enhanced Approach: ICH Q14 describes an "enhanced approach" to development that, while requiring deeper initial understanding, allows for more flexible post-approval changes through a well-defined control strategy [75].
### Core Validation Parameters & Acceptance Criteria (ICH Q2(R2))
This table summarizes the key parameters required to validate an analytical method [75] [76].
| Parameter | Definition | Typical Acceptance Criteria Example |
|---|---|---|
| Accuracy | Closeness of results to the true value. | Percent recovery of 98-102%. |
| Precision | Degree of scatter in repeated measurements. | %RSD ≤ 2% for repeatability. |
| Specificity | Ability to measure analyte amidst interfering components. | No interference from placebo or known impurities. |
| Linearity | Direct proportionality of response to analyte concentration. | Correlation coefficient (r) > 0.998. |
| Range | Interval between upper and lower analyte levels with suitable performance. | Defined by linearity, accuracy, and precision data. |
| LOD/LOQ | Lowest amount detectable/quantifiable. | Signal-to-noise ratio of 3:1 for LOD, 10:1 for LOQ. |
| Robustness | Reliability under small, deliberate parameter changes. | Method meets system suitability upon variation. |
## Troubleshooting Guide: Clinical and Biomarker Validation
Q5: We have a novel biomarker for detecting a specific reaction to a biomaterial, but we are facing challenges with sensitivity and specificity in clinical samples. What are the common causes and solutions?
A5: Sensitivity (ability to detect true positives) and specificity (ability to avoid false positives) are major hurdles in translating biomarkers to the clinic [77].
- Common Causes:
- Matrix Effects: Components in blood or other biological fluids can interfere with the assay. This is a known limitation for immunoassays and spectrophotometry [77].
- Cross-Reactivity: The assay detects molecules similar to the target biomarker, leading to false positives. Immunoassays can have cross-reactivity rates up to 15% in complex samples [77].
- Insufficient Sensitivity of Platform: Spectrophotometry lacks the sensitivity to detect low-abundance biomarkers crucial for early disease diagnosis [77].
- Potential Solutions:
- Platform Shift: Move to more specific techniques like Mass Spectrometry (MS), which can offer up to 1,000 times lower detection limits for some analytes compared to spectrophotometry [77].
- Method Development: Invest in extensive optimization to minimize interference and cross-reactivity during the analytical procedure development phase, as guided by ICH Q14 [75].
- Multi-Omics Verification: Use a multi-omics approach (e.g., genomics, proteomics) to confirm the biomarker's identity and relationship to the biological event, creating a more comprehensive and reliable signature [24].
### Comparison of Analytical Techniques in Clinical Biochemistry
This table compares common techniques used for biomarker analysis, highlighting their pros and cons [77].
| Technology | Advantages | Limitations | Throughput | Relative Cost |
|---|---|---|---|---|
| Spectrophotometry | Simple, inexpensive | Low sensitivity & specificity, matrix interference | High | Low |
| Immunoassays | High specificity, wide analyte range | Cross-reactivity, interference from heterophilic antibodies | High | Medium |
| Chromatography/MS | Highly specific and sensitive | Expensive, complex sample prep, requires skill | Low-Medium | High |
| Lab-on-a-Chip (μTAS) | Portable, fast, low sample volume | Limited multiplexing, some matrix issues | High | Medium-High |
## Frequently Asked Questions (FAQs)
Q: What is the single most significant change in the ISO 10993-1:2025 standard? A: The most significant change is its deep alignment with the risk management framework of ISO 14971. Biological evaluation is now formally presented as a risk management process, requiring the identification of biological hazards, hazardous situations, and harms, followed by risk estimation and control [8].
Q: We are developing a new polymeric implant. What is the most critical documentation we need to maintain? A: Comprehensive documentation is the backbone of quality and compliance [54]. The most critical records include the Design History File (DHF) (chronicling design development), the Device Master Record (DMR) (the manufacturing blueprint), and the Device History Record (DHR) (the production batch record). Additionally, thorough risk management documentation and all testing/inspection records are essential [54].
Q: How is Artificial Intelligence (AI) expected to impact biomarker analysis? A: By 2025, AI and Machine Learning (ML) are expected to revolutionize biomarker analysis through predictive analytics for forecasting disease progression, automated data interpretation to speed up discovery, and enabling highly personalized treatment plans by analyzing individual patient biomarker profiles [24].
Q: What is the role of "real-world evidence" in biomarker validation? A: Regulatory bodies are increasingly recognizing real-world evidence to understand biomarker performance in diverse, real-world clinical populations and settings, complementing data from controlled clinical trials [24].
## The Scientist's Toolkit: Essential Research Reagent Solutions
This table details key materials and their functions in biomaterials testing and validation [78].
| Item / Material Class | Function in Validation | Common Examples |
|---|---|---|
| Titanium & Alloys | Bone implant material testing; assessing osseointegration and mechanical strength. | Orthopedic and dental implants. |
| Calcium Phosphates | Bioactive coatings to promote bone growth; used in testing bioactivity and integration. | Hydroxyapatite coatings on metal implants. |
| Polyethylene (PE) | Testing for wear resistance and low-friction properties in joint replacements. | Acetabular cups in hip implants. |
| Silicones | Used in validation of soft, flexible devices for stability and biocompatibility. | Catheters, tubing, breast implants. |
| Cell Lines (e.g., L929) | In vitro cytotoxicity testing per ISO 10993-5 to determine baseline biocompatibility. | Fibroblast cells for elution tests. |
Analytical Method Lifecycle
Understanding DHF, DMR, and DHR
For researchers and scientists developing biomedical devices, maintaining stringent documentation is a critical regulatory requirement. The Design History File (DHF), Device Master Record (DMR), and Device History Record (DHR) form a interconnected system that chronicles a device's journey from concept to commercial production [79] [80].
The following table summarizes the core purpose, content, and regulatory focus of each file.
| File | Full Name | Primary Focus & Purpose | Key Contents | Regulatory Requirement (FDA 21 CFR Part 820) |
|---|---|---|---|---|
| DHF | Design History File | Documents the history of the design process, proving the device was developed according to user needs and regulatory controls [79] [80]. | Design & development plans, user needs, design inputs/outputs, verification & validation protocols/reports, design reviews, risk management file, design change records [79] [80] [81]. | § 820.30 (Design Controls) [80]. |
| DMR | Device Master Record | Serves as the "recipe" or blueprint for manufacturing the device. It ensures every unit is built and tested identically [79] [81]. | Device specifications (e.g., drawings, formulations), production process specifications, quality assurance procedures, packaging/labeling specs, installation/servicing methods [79] [81]. | § 820.181 (Device Master Record) [80]. |
| DHR | Device History Record | Provides the production history for each batch, lot, or unit, proving it was manufactured in accordance with the DMR [79] [80]. | Dates of manufacture, quantity manufactured and released, acceptance records, primary identification label/labeling, Unique Device Identifier (UDI) [79] [81]. | § 820.184 (Device History Record) [80]. |
The Role of Risk Management Files
The Risk Management File is a crucial component integrated throughout the DHF. It provides systematic evidence that risks have been identified, evaluated, and controlled [80]. It demonstrates a proactive approach to safety throughout the product lifecycle [54].
Key Documentation:
- Risk Management Plan: Outlines the strategy for risk management activities.
- Risk Assessment Reports: Documents the identification of potential harms and the estimation of associated risks.
- Risk Mitigation Plans: Details the measures taken to reduce risks to an acceptable level.
- Post-Market Surveillance Plans: Describes the ongoing monitoring of the device's performance and safety in the market [54].
The Document Interrelationship
The relationship between the DHF, DMR, and DHR is sequential and interconnected. The design process (DHF) produces the manufacturing instructions (DMR), which in turn generates the production proof (DHR) [79].
Frequently Asked Questions (FAQs)
1. Our pre-clinical biomaterial test results are inconsistent. Could this be a DHF documentation issue? Yes, inconsistent results often stem from poorly defined design inputs and outputs in the DHF. For biomaterials, key performance characteristics like biocompatibility, mechanical strength, and degradation rate must be translated into precise, measurable design inputs [54] [25]. Your verification and validation protocols within the DHF must then reference standardized testing methods to ensure reproducibility [37].
- Troubleshooting Guide:
- Symptom: High variability in mechanical strength data from in vitro fatigue testing.
- Potential Cause: Design inputs for tensile strength and fatigue resistance are not specific to the physiological environment.
- Solution: Revisit design inputs to ensure they account for in vivo conditions (e.g., temperature, pH, cyclic loading). Update the DHF to include more rigorous verification protocols that simulate these conditions [54] [25].
2. How do we demonstrate that our manufacturing process consistently produces a biomaterial with the required properties? This is the core purpose of the DMR and DHR. The DMR must contain the validated process specifications for creating the biomaterial, including equipment parameters, environmental controls, and acceptance criteria [54]. The DHR then provides the objective evidence that each batch was made following these exact specifications and passed all defined quality checks [79] [81].
3. A supplier changed a raw material slightly. What documentation is affected? This change can have a cascading effect and must be handled through a formal change control process.
- DHF: Requires an impact assessment. You may need to re-verify or re-validate that the device still meets all design inputs and user needs. This could involve repeating biocompatibility or mechanical tests [80].
- DMR: Must be updated to reflect the new raw material specification and any resulting changes to the manufacturing process [79].
- Risk Management File: Must be updated to include an assessment of any new potential risks introduced by the material change [54].
4. What is the future of DHF, DMR, and DHR with new regulations? The FDA is aligning its Quality System Regulation (QSR) with the international standard ISO 13485:2016, effective February 2, 2026. The new rule, called Quality Management System Regulation (QMSR), eliminates the specific terms DHF, DMR, and DHR [79] [81]. However, the documentation requirements remain substantively the same. The records will be consolidated under the term "Medical Device File" (MDF) [81]. The logical sequence and intent of demonstrating a controlled design and manufacturing process will not change.
Experimental Protocol: Validating a Biomaterial's Critical Property
This protocol outlines a general methodology for generating the verification data required for the DHF, specifically for validating a key biomaterial property.
Title: In Vitro Validation of Biomaterial Degradation Rate
1. Scope This protocol describes a procedure to determine the in vitro degradation profile of [Material Name], a biodegradable polymer intended for use as a tissue engineering scaffold.
2. Experimental Workflow The testing process follows a defined sequence to ensure reliable and documentable results.
3. Materials and Reagents Key research reagents and their functions in this experiment are listed below.
| Item | Function/Justification |
|---|---|
| Phosphate Buffered Saline (PBS) | Simulates the ionic strength and pH of the physiological environment [25]. |
| Simulated Body Fluid (SBF) | A more complex solution that mimics human blood plasma for bioactive material testing [25]. |
| Analytical Balance (±0.1 mg) | Precisely measures sample mass loss over time. |
| Gel Permeation Chromatography (GPC) | Determines changes in the polymer's molecular weight, indicating chain scission and degradation [25]. |
| Scanning Electron Microscope (SEM) | Characterizes surface morphology changes, such as cracking or pore formation, due to degradation [25]. |
4. Methodology
- Sample Preparation: Prepare sterile material samples (e.g., 10mm x 10mm x 2mm discs) with a known initial dry mass (Mâ‚€) and molecular weight profile.
- Immersion and Incubation: Immerse each sample in a controlled volume of pre-warmed PBS (pH 7.4) at 37°C. Maintain constant agitation to simulate fluid flow.
- Sample Withdrawal and Analysis: In triplicate, withdraw samples at predetermined time points.
- Rinse and Dry: Rinse with deionized water and dry to a constant mass.
- Mass Measurement: Measure dry mass (Mₜ). Calculate mass loss:
[(M₀ - Mₜ) / M₀] * 100%. - Molecular Weight Analysis: Use GPC to determine the remaining molecular weight of the polymer.
- Morphological Analysis: Use SEM to image the surface of degraded samples.
5. Documentation for DHF This experiment generates a Design Verification Report, which becomes part of the DHF. The report must include:
- A reference to the specific design input being verified (e.g., "The scaffold shall degrade by approximately 50% in mass over 8 weeks in vitro.").
- The approved protocol.
- The complete raw data.
- Statistical analysis of the results.
- A conclusion stating whether the results pass/fail the pre-defined acceptance criteria, thus verifying the design input [79] [80].
Comparative Analysis of Testing Outcomes Across Material Classes
Standardized Testing Protocols by Material Class
The biological evaluation of medical devices has evolved from a one-size-fits-all testing approach to a more nuanced, risk-based framework that prioritizes patient safety [4]. The following section outlines the standardized testing protocols and expected outcomes for major biomaterial classes, based on ISO 10993-1 requirements.
Table 1: Standardized Testing Protocols and Expected Outcomes by Material Class
| Material Class | Key Standardized Tests | Expected Performance Range | Common Failure Modes |
|---|---|---|---|
| Metallic Biomaterials | Cytotoxicity, Sensitization, Irritation, Systemic Toxicity, Implantation Effects, Hemocompatibility [4] | High tensile strength, corrosion resistance, no significant ion release [82] | Corrosion, metal ion leaching, fatigue failure, allergic responses [49] |
| Polymeric Biomaterials | Cytotoxicity, Sensitization, Irritation, Systemic Toxicity, Genotoxicity, Hemocompatibility [4] | Biocompatibility, specified flexibility, no significant leachables [82] [83] | Leaching of additives (e.g., DEHP), polymer degradation, swelling, creep [4] [49] |
| Ceramic Biomaterials | Cytotoxicity, Sensitization, Irritation, Implantation Effects [4] | High wear resistance, bioactivity, osseointegration potential [82] | Brittle fracture, low impact resistance, slow degradation [82] |
| Natural Biomaterials | Cytotoxicity, Sensitization, Irritation, Systemic Toxicity, Hemocompatibility [4] | High biocompatibility, controlled biodegradability, support for tissue remodeling [83] | Rapid/uncontrolled degradation, immunogenic response, batch-to-batch variability [83] |
Troubleshooting Guides & FAQs
This section addresses common experimental challenges and procedural questions faced by researchers during biomaterial testing, framed within the context of standardization challenges.
Troubleshooting Guide: Common Experimental Issues
Problem: Inconsistent Cytotoxicity Results Between Batches
Potential Cause 1: Material Variability
Potential Cause 2: Test Execution Variability
- Investigation Step: Review laboratory procedures. Manual pipetting can introduce higher variability compared to automated Liquid Handling Stations (LHS), which offer higher accuracy and reproducibility [84].
- Solution: Implement automated protocols where possible and ensure consistent technician training.
Problem: Unexpected Inflammatory Response in Implantation Studies
Potential Cause 1: Surface Contamination
- Investigation Step: Review sterilization and packaging validation records. The process must be validated to ensure effective sterilization without degrading the material’s properties [54].
- Solution: Revalidate sterilization cycles and aseptic handling procedures.
Potential Cause 2: Particulate Release
- Investigation Step: Characterize material for particulate generation under simulated use conditions. Regulators are increasing focus on particulate release [49].
- Solution: Modify manufacturing or post-processing steps to minimize particulate generation.
Problem: Failed Genotoxicity Assessment Despite Negative Cytotoxicity
- Potential Cause: Leachable Compounds
- Investigation Step: Conduct a detailed extractables and leachables study, even if cytotoxicity is negative. Some compounds may not cause immediate cell death but can damage DNA [4].
- Solution: Use chemical characterization data to identify and remove the source of the genotoxic leachable.
Investigation Path for Inflammatory Response
Frequently Asked Questions (FAQs)
Q1: How do the 2025 updates to ISO 10993-1 impact the way we categorize device contact duration?
- A: The 2025 standard introduces more precise definitions. The term "transitory" is no longer used, while "very brief contact" (less than a minute) remains. Crucially, the concept of "total exposure period" is key for devices with multiple contacts. A "contact day" is any day with tissue contact, regardless of length. Multiple exposures can quickly shift a device from "limited" to "prolonged" duration, requiring a more extensive biological evaluation [8].
Q2: Our device is intended for single-use, short-term application. Why are regulators requesting long-term toxicity data?
- A: This can be due to two key factors introduced in the updated risk-based framework:
- Reasonably Foreseeable Misuse: The standard now requires considering misuse, such as using a device longer than intended, which can result in a longer duration of exposure [8].
- Bioaccumulation: If a chemical constituent known to bioaccumulate is present, the contact duration may be considered long-term unless otherwise justified by a thorough risk assessment [8].
Q3: What is the role of chemical characterization in the biological evaluation plan?
- A: Chemical characterization (ISO 10993-18) is now a foundational step that should be conducted before biological testing. It involves a thorough analysis of the chemical composition, including extractables and leachables. This data is critical for a toxicological risk assessment and can help justify the selection (or waiver) of specific biological tests, moving away from a checklist mentality to a science-driven evaluation [4].
Q4: How can we justify grouping devices into a "family" for biocompatibility testing?
- A: To claim a device family, you must provide strong justification demonstrating that the devices have sufficiently similar manufacturing processes, materials of construction, and intended uses. This requires robust evidence, often including material characterization data, to show that the biological safety risks are comparable across the family. This approach can reduce redundant testing [4].
Experimental Protocols & Workflows
This section provides detailed methodologies for key experiments cited in the comparative analysis, with a focus on standardized protocols.
Protocol 1: Multiplexed Toxicity Screening for Biomaterials
Scope: This standardized, automated protocol allows for the concurrent analysis of viability, cytotoxicity, and apoptosis in a single assay, suitable for low- to medium-throughput laboratories [84].
Multiplexed Toxicity Screening Workflow
Key Materials:
- Robotic Liquid Handling Station (LHS): For superior accuracy and reproducibility in pipetting and dispensing compared to manual methods [84].
- Multiplexed Assay Kits: Commercial kits allowing simultaneous measurement of multiple endpoints (e.g., viability, cytotoxicity, apoptosis).
- Validated Reference Materials: Both positive and negative control materials to validate each assay run.
Protocol 2: Chemical Characterization for Toxicological Risk Assessment (ISO 10993-18)
Scope: A workflow for identifying and quantifying extractables and leachables from biomaterials to provide data for a toxicological risk assessment, a required step before biological testing [4].
Chemical Characterization and Risk Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Biomaterial Toxicity Testing
| Item | Function | Application Notes |
|---|---|---|
| Automated Liquid Handling Station (LHS) | Automates pipetting and dispensing for higher accuracy and reproducibility in assay setup [84]. | Critical for standardizing multiplexed assays; reduces human error in low-to-medium throughput labs. |
| Multiplexed Assay Kits | Allows simultaneous measurement of multiple toxicity endpoints (viability, cytotoxicity, apoptosis) from a single sample [84]. | Conserves valuable test material and increases data density per experiment. |
| Reference Control Materials | Provides known positive and negative responses to validate the performance of each test system. | Essential for demonstrating assay validity and for troubleshooting unexpected results. |
| Cell Lines for Cytotoxicity | Standardized in vitro models (e.g., L-929 fibroblasts per ISO 10993-5) to assess the basic biocompatibility of materials. | Well-characterized lines provide a consistent and reproducible baseline for comparison. |
| Analytical Grade Solvents | Used for preparing material extracts for chemical characterization and leachables studies. | Purity is critical to avoid introducing interfering contaminants during extraction. |
Statistical Methods and Data Interpretation for Regulatory Submission
The path to successful regulatory submission is fraught with challenges, many of which stem from a lack of standardization in data collection, analysis, and presentation. In the context of biomaterial testing protocols, inconsistent methodologies can create significant roadblocks. A recent review highlighted the fragmented research landscape concerning the analysis of foreign body giant cells (FBGCs), which are crucial in the body's response to implanted biomaterials. This review found significant variability in critical aspects such as cell origin and type, culture media, fusion-inducing factors, and seeding density, complicating cross-study comparisons and hindering reproducibility [37].
These standardization challenges directly impact regulatory success. An analysis of FDA submissions revealed that 32% of submissions had critical data conformance issues, preventing them from even entering the official review process. Furthermore, only 50% of new drug applications are approved on their first submission, with a median delay of 435 days to approval following an unsuccessful first attempt [85]. This underscores the critical need for robust statistical methods and standardized data interpretation practices from the earliest research stages.
Troubleshooting Guides
Data Conformance and Quality Issues
Problem: Submission rejected at the gateway due to data standards non-compliance.
- Solution: Implement CDISC compliance checks throughout the data collection process, not just before submission. Ensure all datasets (SDTM, ADaM) and supporting documentation (define.xml, cSDRG, aCRG, ADRG) are validated against the current FDA Data Standards Catalog [85].
- Preventive Measure: Engage biostatisticians and statistical programmers with specific regulatory submission experience early in the study design phase to architect the data collection structure for eventual CDISC compliance [86].
Problem: Inconsistent results across endpoints, sites, or studies.
- Solution: Perform a Data Quality Oversight (DQO) analysis using specialized software to detect spurious data patterns. Statistically review the impact of anomalies and missing data on the results to pre-empt regulatory reviewer comments [85].
- Preventive Measure: Establish a standardized statistical analysis plan (SAP) before study initiation and ensure consistent application across all sites and analyses.
Statistical Interpretation and Efficacy Challenges
Problem: Uncertainties related to dose selection.
- Solution: Re-analyze dosing justification evidence. Review the distribution of responses across different dose groups and ensure the selected dose is supported by a clear risk-benefit profile [85].
- Preventive Measure: Implement adaptive trial designs or robust Phase II studies that adequately characterize the dose-response relationship before pivotal trials.
Problem: Choice of study endpoints that fail to adequately reflect a clinically meaningful effect.
- Solution: Conduct a comprehensive review of existing regulatory guidance and relevant literature on endpoint selection before finalizing the study protocol. Ensure endpoints are validated and recognized by regulatory bodies for the specific disease context [85].
- Preventive Measure: Consult with regulatory agencies through formal meetings (e.g., FDA Type B meetings) to gain alignment on endpoint selection before initiating pivotal studies.
Frequently Asked Questions (FAQs)
Q1: What are the most common statistical reasons for first-time submission failures? The efficacy-related reasons for failed first-time submissions include poor efficacy compared to standard of care, uncertainties in dose selection, choice of endpoints that fail to reflect a clinically meaningful effect, inconsistent results across different endpoints, and study conduct issues due to missing data and/or data integrity problems [85].
Q2: How can we pre-empt potential regulatory questions about our statistical analysis? Perform a thorough statistical review of submission data that mirrors the regulatory reviewer's likely approach. This includes reviewing the distribution and balance of study populations across studies and sites, analyzing the consistency of efficacy analyses across different regions and timepoints, and examining the appropriateness of endpoints [85]. Having a strong sponsor statistician who can clearly explain issues and concerns is also invaluable [86].
Q3: What role does early biostatistician involvement play in submission success? Early interaction with a skilled biostatistician significantly impacts successful outcomes. Biostatisticians facilitate clearer communication with regulatory bodies, help avoid unnecessary delays due to unsatisfactory submissions, and increase the likelihood of first-time approval. They can also shorten the time from final data to integrated analysis [86].
Q4: How is AI expected to impact biomarker analysis and regulatory strategies by 2025? By 2025, AI and machine learning are expected to revolutionize biomarker analysis through more sophisticated predictive models that forecast disease progression and treatment responses. AI will also facilitate automated interpretation of complex datasets, significantly reducing time for biomarker discovery and validation. This will support more personalized treatment plans and potentially influence clinical trial designs [24].
Q5: Why is standardization particularly challenging in biomaterials research, and how does this affect regulatory submissions? Biomaterials research faces specific standardization challenges, such as the significant variability in methods used to study critical phenomena like foreign body giant cell formation. Inconsistencies in cell origin, culture conditions, and read-outs hamper reproducibility and cross-study comparisons, making it difficult to build a compelling evidence base for regulatory approval [37].
Essential Data Tables for Regulatory Submissions
Quantitative Analysis of Submission Outcomes
Table: Analysis of FDA New Drug Application Outcomes (2000-2012) [86] [85]
| Outcome Metric | Percentage/Number | Impact |
|---|---|---|
| Approved on First Submission | 50% | Most efficient path to market |
| Ultimately Approved After Resubmission | 73% | Additional resources required |
| Median Delay After First Unsuccessful Submission | 435 days | Significant commercial and patient impact |
| Submissions with Critical Data Conformance Issues | 32% | Prevents official review start |
Table: Efficacy-Related Reasons for First-Time Submission Failures [85]
| Reason for Failure | Description | Potential Preventive Action |
|---|---|---|
| Poor Efficacy | Compared to standard of care | Better preclinical models and Phase II dose-finding |
| Dose Selection Uncertainties | Inadequate justification for chosen dose | Comprehensive dose-response studies |
| Endpoint Issues | Fails to reflect clinically meaningful effect | Early regulatory consultation on endpoint selection |
| Inconsistent Results | Across different endpoints or sites | Robust statistical analysis plan and centralized monitoring |
| Study Conduct Problems | Missing data and data integrity issues | Improved site training and data management |
Standardized Experimental Workflows
Data Conformance Verification Pathway
Statistical Analysis Planning Process
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Standardized Biomaterial Testing
| Research Reagent/Instrument | Function in Biomaterial Testing |
|---|---|
| Mach-1 Mechanical Tester | Multiaxial mechanical testing (compression, tension, shear, friction) of tissues and biomaterials; can automatically map mechanical properties of curved samples in 3D [87] |
| Bio AFMs | Atomic force microscopy for quantitative live-cell mechanical property mapping and high-resolution molecular and cellular imaging [87] |
| Calcium Phosphate Biomaterials | Bone graft substitute materials manufactured under ISO 13485:2016 certified Quality Management Systems for consistent quality [87] |
| RESOMER Bioresorbable Polymers | Bioresorbable polymers for medical devices that degrade predictably in the body [87] |
| CellScale Biomaterials Test Systems | Specialized test systems for biomaterials testing with temperature-controlled media baths and image capture/analysis software [87] |
| Color Contrast Analyser | Software tool to measure color contrast between foreground and background to ensure accessibility in data presentation [88] |
| CluePoints Software | FDA-endorsed software for Data Quality Oversight, using machine learning to detect spurious data patterns within and across studies [85] |
Post-Market Surveillance and Real-World Performance Validation
Troubleshooting Common PMS Challenges
Problem: Inconsistent Data from Multiple Real-World Sources Your surveillance system is collecting data from electronic health records (EHRs), patient registries, and claims databases, but the information is inconsistent and cannot be easily integrated or compared.
- Root Cause: Different data sources often use non-standardized terminologies, formats, and collection protocols. This heterogeneity is a fundamental challenge in biomaterial testing standardization [89].
- Solution:
- Implement Data Standards: Adopt established biomedical terminology standards, such as those from CEN TC 251 and ISO TC 215, which provide categorial structures to increase interoperability between systems [90].
- Utilize NLP and AI: Deploy Natural Language Processing (NLP) to transform unstructured text from clinical notes and reports into structured, analyzable data [91].
- Create a Data Governance Plan: Develop a standardized data collection plan that defines specific data points, formats, and quality checks across all sources [92].
Problem: Inability to Detect Subtle Safety Signals Despite collecting a large volume of adverse event reports, your statistical methods are failing to identify potential safety signals early enough.
- Root Cause: Traditional spontaneous reporting systems can be subject to underreporting and reporting bias. Rare or long-term adverse events may be missed without sophisticated analysis [91] [89].
- Solution:
- Leverage Advanced Analytics: Implement machine learning (ML) algorithms designed for early signal detection. These can analyze complex datasets to identify subtle patterns and associations that traditional methods might miss [91] [24].
- Expand Data Scope: Incorporate data from wearable devices and patient-reported outcomes (PROs) to gain a more continuous and patient-centric view of device performance [91] [89].
- Apply Target Trial Emulation: Use this methodology to apply the rigorous design principles of a randomized clinical trial to observational real-world data, helping to draw more valid causal inferences about device performance [89].
Problem: Failure to Meet Evolving Regulatory Standards for Reporting Your organization struggles to keep pace with updated regulatory requirements for post-market surveillance (PMS) reporting, such as the FDA's Section 522 studies or the EU MDR's Periodic Safety Update Reports (PSURs).
- Root Cause: Global regulatory expectations are continuously strengthening, and requirements can vary by region [91] [93] [92].
- Solution:
- Establish Regulatory Intelligence: Designate a team to maintain current awareness of updates from the FDA, EMA, and other relevant authorities [91].
- Develop a Proactive PMS Plan: Create a comprehensive plan that is commensurate with your device's risk profile. This should outline data collection methods, analysis plans, and reporting schedules [93] [92].
- Integrate with Quality Systems: Ensure your PMS activities are seamlessly integrated with your Quality Management System (QMS) and Corrective and Preventive Action (CAPA) processes to promptly address any identified issues [93] [92].
Frequently Asked Questions (FAQs)
What are the primary regulatory requirements for post-market surveillance of medical devices? Regulatory requirements vary by region but share common core components. In the United States, the FDA mandates requirements under 21 CFR Part 822 for post-market surveillance plans, 21 CFR Part 803 for Medical Device Reporting (MDR) of adverse events, and 21 CFR Part 806 for reporting corrections and removals [93] [92]. For certain higher-risk devices, Section 522 of the FD&C Act gives the FDA authority to order specific post-market studies [93]. In the European Union, the Medical Device Regulation (MDR) requires manufacturers to have a PMS system and produce Post-Market Surveillance Reports (PMSRs) or Periodic Safety Update Reports (PSURs) [92].
What is the difference between real-world data (RWD) and real-world evidence (RWE)? Real-world data (RWD) is the raw data relating to patient health status and/or the delivery of healthcare routinely collected from a variety of sources [89]. These sources include electronic health records (EHRs), claims and billing data, patient registries, and data from wearable devices [91] [89]. Real-world evidence (RWE) is the clinical evidence about the usage and potential benefits or risks of a medical product derived from the analysis of RWD [89]. In essence, RWD is the input, and RWE is the processed, meaningful output used for regulatory and clinical decision-making [91].
How can artificial intelligence (AI) improve our post-market surveillance system? AI and machine learning (ML) can revolutionize PMS by enhancing signal detection, automating processes, and enabling predictive analytics. Key applications include [91] [24]:
- Machine Learning for Signal Detection: ML algorithms can analyze complex, multi-source datasets to identify potential safety signals earlier and with greater accuracy than traditional methods.
- Natural Language Processing (NLP): This technology can extract valuable information from unstructured data sources, such as physician's notes in EHRs or social media, converting it into analyzable data.
- Predictive Analytics: AI models can forecast potential safety issues based on historical patterns and emerging data trends, allowing for proactive risk mitigation.
Our device is an implant. What specific PMS obligations should we anticipate? Implantable devices intended for more than one year typically trigger specific regulatory obligations. In the U.S., the FDA can require a Section 522 post-market surveillance study for such devices [93] [92]. You should anticipate the need for a study plan that includes [93]:
- Longitudinal Follow-up: Tracking device performance and patient outcomes over an extended period.
- Detailed Clinical Data: Collecting specific data on safety endpoints (e.g., infection rates, failure modes) and effectiveness.
- Systematic Methodology: Implementing a scientifically valid study design, such as a patient registry or post-market clinical follow-up (PMCF) study, to collect robust real-world evidence on long-term safety and performance.
Experimental Protocols for Key PMS Activities
Protocol: Designing a Section 522 Post-Market Surveillance Study This protocol outlines the steps for designing a study under the FDA's Section 522 authority, which is often required for class II or class III devices that are implantable, life-sustaining, or pose a significant risk [93].
Objective: To address specific public health questions related to the device's safety and effectiveness in a real-world population.
Methodology:
- Study Background: Develop a comprehensive background section including device description, regulatory history, and the rationale for the study.
- Define Objectives: Clearly state the primary and secondary study objectives. Example: "The primary objective is to quantify the rate of device-related thrombosis at 2 years post-implantation."
- Study Design: Choose an appropriate observational design, such as a prospective, multi-center cohort study or the establishment of a device registry.
- Patient Population: Define explicit inclusion and exclusion criteria for subject enrollment, mirroring the intended use population.
- Data Collection:
- Variables: Specify the data to be collected (e.g., patient demographics, procedure details, adverse events, patient-reported outcomes).
- Timepoints: Define the schedule for follow-up assessments (e.g., 30 days, 6 months, 1 year, annually thereafter).
- Source Documents: Utilize EHRs, claims data, and direct patient surveys to collect information.
- Statistical Analysis Plan: Pre-define the statistical methods for analyzing the data, including success criteria and how missing data will be handled.
- Reporting: Plan for interim and final study reports to be submitted to the FDA as per the agreed schedule [93].
Workflow: Signal Management Process This workflow details the logical process for managing potential safety signals identified from post-market data.
Protocol: Implementing a Patient Registry for Long-Term Performance Validation Patient registries are a key method for gathering longitudinal real-world data on device performance [91] [89].
Objective: To systematically collect clinical data to evaluate the long-term safety, effectiveness, and quality of life impact of a biomaterial-based medical device.
Methodology:
- Registry Design: Establish a prospective, observational, multi-center registry.
- Site Selection: Identify and recruit clinical investigation sites that represent diverse care settings and patient populations.
- Standardized Data Collection:
- Case Report Forms (eCRFs): Develop electronic case report forms to ensure consistent data entry across all sites.
- Common Data Elements (CDEs): Implement standardized definitions for all key variables to overcome biomaterial testing protocol challenges and ensure data interoperability [90].
- Patient-Reported Outcomes (PROs): Integrate validated questionnaires to capture the patient's perspective on symptoms, function, and quality of life.
- Quality Assurance: Implement a monitoring plan to verify data accuracy and completeness against source documents.
- Data Analysis: Perform periodic analyses to assess cumulative incidence of adverse events, device survival rates, and predictors of clinical outcomes.
Data Presentation
Table: Comparison of Common Real-World Data Sources in PMS
| Data Source | Key Strengths | Key Limitations | Best Use in PMS |
|---|---|---|---|
| Spontaneous Reporting Systems (e.g., FAERS, MAUDE [94]) | Early signal detection for rare events, global coverage [91]. | Underreporting, reporting bias, cannot determine incidence [91] [89]. | Initial detection of unexpected adverse events. |
| Electronic Health Records (EHRs) | Rich clinical detail, large patient populations, real-world context [91] [89]. | Data quality variability, unstructured data, privacy concerns [91] [89]. | Studying clinical effectiveness, outcomes in specific sub-populations. |
| Claims Data | Large population coverage, long-term follow-up, useful for health economics [91] [89]. | Limited clinical detail, coding inaccuracies, administrative purpose [91] [89]. | Tracking utilization, hospitalizations, and large-scale safety studies. |
| Patient Registries | Longitudinal follow-up, detailed data on specific diseases/devices [91] [89]. | Potential for selection bias, resource-intensive, may lack generalizability [91] [89]. | Long-term safety and performance of implants. |
| Patient-Reported Outcomes (PROs) & Digital Health Technologies | Direct patient perspective, continuous monitoring, real-time data [91] [89]. | Subjective measures, data validation challenges, technology barriers [91] [89]. | Understanding patient experience and real-world device performance. |
Table: Essential Research Reagent Solutions for Biomaterial Testing
| Reagent / Material | Function in PMS Context |
|---|---|
| Biomarker Analysis Kits (e.g., for genomics, proteomics) | Enable the development of companion diagnostics and monitoring of host response to implants via multi-omics approaches [24]. |
| Liquid Biopsy Assays | Provide a non-invasive method for real-time monitoring of disease progression or treatment response in patients with devices, such as in oncology [24]. |
| Single-Cell Analysis Platforms | Allow for deep characterization of the cellular response to biomaterials, providing insights into the tissue microenvironment and identifying rare cell populations [24]. |
| Standardized Reference Materials | Critical for calibrating equipment and ensuring the reproducibility and comparability of biomarker test results across different laboratories, addressing core standardization challenges [90]. |
| AI-Powered Data Analysis Software | Facilitates the automated interpretation of complex datasets from multi-omics and other sources, accelerating biomarker discovery and signal detection [24]. |
Logical Workflows
Workflow: Integrated Post-Market Surveillance System This diagram shows the logical flow of a comprehensive PMS system, from planning to continuous improvement.
Workflow: Post-Market Data Analysis and Decision Pathway This chart outlines the pathway for analyzing collected data and making evidence-based decisions.
Conclusion
The standardization of biomaterial testing protocols remains a dynamic challenge, caught between the rigorous requirements of regulatory frameworks and the rapid innovation in materials science. Successfully navigating this landscape requires a multidisciplinary approach that respects foundational standards while embracing methodological innovations. The future points toward more predictive, human-relevant testing models that leverage computational approaches, advanced biomimetic systems, and non-destructive techniques. As the field evolves toward personalized medicine and complex tissue-engineered products, the development of adaptable, science-based standards that can accommodate material complexity without compromising safety will be paramount. Researchers and regulators must collaborate to create a more integrated testing paradigm that accelerates translation while ensuring the highest levels of patient safety, ultimately bridging the gap between standardized assessment and transformative biomedical innovation.
References
- 1. Navigating Biocompatibility: An Introduction to ISO 10993 ... [https://medinstitute.com/blog/navigating-biocompatibility-an-introduction-to-iso-10993-series-of-standards/]
- 2. Use of International Standard ISO 10993-1, "Biological ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/use-international-standard-iso-10993-1-biological-evaluation-medical-devices-part-1-evaluation-and]
- 3. Biocompatibility FAQ [https://clin-r.com/biocompatibility-faq/]
- 4. Understanding the Key Updates to ISO 10993-1 [https://www.mddionline.com/testing/the-crucial-role-of-biological-evaluation-in-medical-device-safety-key-updates-to-the-international-organization-for-standardization-iso-10993-1]
- 5. The “Big Three†in biocompatibility testing of medical devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC10800850/]
- 6. A Practical Guide to ISO 10993-5: Cytotoxicity [https://www.mddionline.com/testing/a-practical-guide-to-iso-10993-5-cytotoxicity]
- 7. Challenges of Demonstrating Biological Equivalence [https://medinstitute.com/blog/challenges-of-demonstrating-biological-equivalence-per-iso-10993-18-and-eu-mdr/]
- 8. ISO 10993-1:2025 Updates —Top 10 Biological Evaluation ... [https://namsa.com/resources/blog/iso-10993-12025top-10-biological-evaluation-essentials-in-the-update/]
- 9. The Most Pressing Questions About ISO 10993-1 [https://www.mddionline.com/testing/nelson-labs-tackles-most-pressing-questions-about-iso-10993-1]
- 10. Biocompatibility FAQ [https://namsa.com/resources/audio/biocompatibility-faq/]
- 11. ASTM International - Wikipedia [https://en.wikipedia.org/wiki/ASTM_International]
- 12. Medical Device Standards and Implant Standards [https://www.astm.org/Standards/medical-device-and-implant-standards.html]
- 13. ASTM International [https://www.engineeringtoolbox.com/astm-d_29.html]
- 14. Standards & Publications - Products & Services [https://store.astm.org/products-services/standards-and-publications/standards/bos-standards.html?volume=13&year=2025]
- 15. Material testing standards according to EN, ISO and ASTM - Barrus [https://barrus-testing.com/solutions/material-testing-standards/]
- 16. Subcommittee F04.42 on Biomaterials and Biomolecules ... [https://www.astm.org/membership-participation/technical-committees/committee-f04/subcommittee-f04/jurisdiction-f0442]
- 17. Regulatory Guidelines For Biocompatibility Safety Testing [https://www.mddionline.com/regulatory-quality/regulatory-guidelines-for-biocompatibility-safety-testing]
- 18. FDA Issues Draft Guidance for Medical Device Biocompatibility [https://www.exponent.com/article/fda-issues-draft-guidance-medical-device-biocompatibility]
- 19. Biocompatibility Assessment Resource Center [https://www.fda.gov/medical-devices/premarket-submissions-selecting-and-preparing-correct-submission/biocompatibility-assessment-resource-center]
- 20. Newly Added Guidance Documents [https://www.fda.gov/drugs/guidances-drugs/newly-added-guidance-documents]
- 21. A Recent Timeline of U.S. Actions to Reduce and Replace ... [https://emulatebio.com/alternatives-to-animal-testing-in-drug-development/]
- 22. Alternatives to Animal Testing [https://www.niehs.nih.gov/health/topics/science/sya-iccvam]
- 23. FDA Announces Plan to Phase Out Animal Testing ... [https://www.fda.gov/news-events/press-announcements/fda-announces-plan-phase-out-animal-testing-requirement-monoclonal-antibodies-and-other-drugs]
- 24. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 25. Advanced testing and biocompatibility strategies for sustainable... [https://biotechsustainablematerials.biomedcentral.com/articles/10.1186/s44316-024-00018-7]
- 26. 2025 Nanomaterial SDS Requirements: Practical Guide [https://www.sdscopilot.com/blog/Nanomaterials]
- 27. Computational optimization of 3D printed bone scaffolds ... [https://www.nature.com/articles/s41598-025-15122-5]
- 28. Advances in 3D-Printed scaffolds for bone defect repair [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1707406/full]
- 29. Biocompatibility Evaluation Endpoints by Contact Duration ... [https://www.fda.gov/medical-devices/biocompatibility-assessment-resource-center/biocompatibility-evaluation-endpoints-contact-duration-periods]
- 30. Biocompatibility Test - an overview [https://www.sciencedirect.com/topics/engineering/biocompatibility-test]
- 31. Basics of Biocompatibility: Information Needed for ... [https://www.fda.gov/medical-devices/biocompatibility-assessment-resource-center/basics-biocompatibility-information-needed-assessment-fda]
- 32. Future challenges in the in vitro and in vivo evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4817327/]
- 33. Biocompatibility Test Methods [https://pacificbiolabs.com/biocompatibility-test-methods/]
- 34. Medical Device Biocompatibility Testing and ISO 10993 ... [https://namsa.com/services/testing/biocompatibility-testing/]
- 35. Biocompatibility Testing for Medical Devices 101 [https://www.greenlight.guru/blog/medical-device-biocompatibility]
- 36. National Deviations to IEC 60601-1 [https://www.mddionline.com/testing/national-deviations-to-iec-60601-1]
- 37. Evaluating different methodologies to induce in vitro ... [https://pubmed.ncbi.nlm.nih.gov/39826854/]
- 38. Surface Characterization [https://www.anton-paar.com/us-en/surface-characterization/?srsltid=AfmBOoqjnhinmOYeh9gddpXKyJio9PZE7_cLyO7aPB08ogqxBooOdnLV]
- 39. Mechanical Testing [https://www.nanoscience.com/techniques/mechanical-testing/]
- 40. The Three Challenges in Biomedical QC Testing [https://www.medicaldesignbriefs.com/component/content/article/40429-the-three-challenges-in-biomedical-qc-testing]
- 41. Imaging challenges in biomaterials and tissue engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC3799904/]
- 42. Protocols & Troubleshooting Guides [https://www.rndsystems.com/resources/protocols-troubleshooting-guides]
- 43. Challenges With the Development of Biomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6554598/]
- 44. A Challenge for Engineering Biomimetic Microvascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9252339/]
- 45. The Art of Engineering Biomimetic Cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8325697/]
- 46. Application of biomimetic approaches in the treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538068/]
- 47. A review of biomaterial degradation assessment ... [https://www.nature.com/articles/s41529-024-00487-1]
- 48. The Most Common Issues Affecting Biocompatibility Tests [https://www.rqmplus.com/blog/the-most-common-issues-affecting-biocompatibility-tests]
- 49. Biocompatibility Challenges in New Material Selection for ... [https://www.lexim.ai/post/biocompatibility-challenges-in-new-material-selection-for-medical-devices]
- 50. Recent advances in 3D printing of biodegradable metals for ... [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-023-00371-7]
- 51. Biomaterials as Implants in the Orthopedic Field for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10303232/]
- 52. Biodegradable Polymers in Biomedical Applications [https://www.mdpi.com/1422-0067/24/23/16952]
- 53. standardized, resource-efficient: ClicKit-Well [https://www.ikts.fraunhofer.de/en/departments/electronics_microsystems_biomedicine/bio_nanotechnology/biological_materials_analysis/cr_biomaterial_testing_2_0_clickit-well.html]
- 54. Validation and Documentation Requirements for Biomaterials [https://boydbiomedical.com/articles/validation-and-documentation-requirements-for-biomaterials]
- 55. What makes mechanical testing of BIOMATERIALS ... [https://www.cellscale.com/calebs-corner/mechanical-testing-of-biomaterials/]
- 56. Cell Lines vs. Primary Cells [https://www.stemcell.com/physiological-relevance-of-human-primary-cells-vs-cell-lines]
- 57. Primary cells vs. cell lines: Is it not time for something better? [https://www.bit.bio/blog/primary-cells-vs-cell-lines]
- 58. Primary Cell Culture Guide [https://www.atcc.org/resources/culture-guides/primary-cell-culture-guide]
- 59. Guidance for evaluating biomaterials' properties and ... [https://www.sciencedirect.com/science/article/pii/S0109564124003488]
- 60. Cell culture and maintenance protocol [https://www.abcam.com/en-us/technical-resources/protocols/cell-culture-and-maintenance-protocol]
- 61. Human Primary Cell Culture Market Size & Forecast, 2025 ... [https://www.coherentmarketinsights.com/industry-reports/human-primary-cell-culture-market]
- 62. Mapping Biomaterial Complexity by Machine Learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394815/]
- 63. Artificial Intelligence in Biomaterials: A Comprehensive ... [https://www.mdpi.com/2076-3417/14/15/6590]
- 64. Leveraging In Silico and Artificial Intelligence Models to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180087/]
- 65. Evidence-based biomaterials research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9122837/]
- 66. Challenges and Opportunities for Integrating In Silico ... [https://www.mdpi.com/2073-4441/12/12/3549]
- 67. In silico assessment of biocompatibility and toxicity [https://pmc.ncbi.nlm.nih.gov/articles/PMC11150300/]
- 68. Next-Gen Biocompatibility Testing: Innovations in Medical ... [https://ebi.bio/next-gen-biocompatibility-testing-innovations-in-medical-devices-labs/]
- 69. A review on the applications of machine learning ... [https://www.sciencedirect.com/science/article/pii/S2590183425000183]
- 70. The synergy of artificial intelligence in biomaterials ... [https://www.sciencedirect.com/science/article/pii/S305072352500001X]
- 71. Integrating ex-ante and prospective life-cycle assessment ... [https://www.sciencedirect.com/science/article/pii/S2352550923002543]
- 72. Current practices and challenges in the standardization and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5004491/]
- 73. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 74. How to be a Better Troubleshooter in Your Laboratory [https://www.goldbio.com/blogs/articles/how-to-be-a-better-troubleshooter?srsltid=AfmBOooZfMEd7nmAj3ArgtgULjs7nmhZyyrbBS9vrXwGQyoy2Hx_87pp]
- 75. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 76. ICH Guidelines for Analytical Method Validation Explained [https://amsbiopharma.com/ich-guidelines-analytical-method/]
- 77. Advancing clinical biochemistry: addressing gaps and driving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12011881/]
- 78. Biocompatible Materials for Medical Devices: A Guide ... [https://www.labmanager.com/biocompatible-materials-for-medical-devices-a-guide-for-laboratory-professionals-34339]
- 79. DHF vs. DMR vs. DHR: Differences Explained [https://www.greenlight.guru/blog/design-history-file-dhf-device-master-record-dmr-device-history-record-dhr]
- 80. DHF vs DMR vs DHR: Everything You Need to Know - Simbex [https://simbex.com/dhf-vs-dmr-vs-dhr-everything-you-need-to-know/]
- 81. Differences Between DHF, DMR, DHR, and QMSR for ... [https://www.scilife.io/blog/differences-dhr-dmr-dhr]
- 82. Global Biomaterial Testing Equipment Market Analysis ... [https://www.linkedin.com/pulse/global-biomaterial-testing-equipment-market-analysis-2025-2032-r2src]
- 83. Biomaterials Market Size to Hit USD 523.75 Billion by 2034 [https://www.precedenceresearch.com/biomaterials-market]
- 84. Standardization of automated cell-based protocols for ... [https://pubmed.ncbi.nlm.nih.gov/21518824/]
- 85. Regulatory Submission - Data Analysis & Review [https://www.quanticate.com/regulatory-submission]
- 86. Statistical Support for Regulatory Submissions [https://pharpoint.com/resources/statistical-support-regulatory-submissions-discussions/]
- 87. Resource Guide | Society for Biomaterials (SFB) [https://biomaterials.org/about-society/resource-guide]
- 88. Tips to Create an Accessible and Contrasted Color Palette [https://stephaniewalter.design/blog/tips-create-accessible-color-palette/]
- 89. Real-world data: a brief review of the methods, applications ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-022-01768-6]
- 90. Standards and biomedical terminologies: the CEN TC 251 ... [https://pubmed.ncbi.nlm.nih.gov/18487839/]
- 91. Post-Marketing Surveillance in 2025: Evolving Strategies ... [https://www.vitrana.com/post-marketing-surveillance-in-2025-evolving-strategies-for-real-world-safety-monitoring/]
- 92. Post Market Surveillance: What You Need to Know ... [https://www.nsf.org/knowledge-library/post-market-surveillance-what-you-need-to-know-to-ensure-patient-safety]
- 93. Medical Device Post-Market Surveillance: Complete FDA ... [https://www.complizen.ai/post/medical-device-post-market-surveillance-fda]
- 94. How to Report Medical Device Problems [https://www.fda.gov/medical-devices/medical-device-safety/medical-device-reporting-mdr-how-report-medical-device-problems]