Mastering the PICOS Framework: A Step-by-Step Guide for Robust Biomaterial Systematic Reviews
This comprehensive guide demystifies the application of the PICOS framework for conducting systematic reviews in the rapidly evolving field of biomaterials.
Mastering the PICOS Framework: A Step-by-Step Guide for Robust Biomaterial Systematic Reviews
Abstract
This comprehensive guide demystifies the application of the PICOS framework for conducting systematic reviews in the rapidly evolving field of biomaterials. Tailored for researchers, scientists, and drug development professionals, it provides a foundational understanding of PICOS, explores its critical methodological role in structuring biomaterial research questions, addresses common challenges in search strategy and data extraction, and validates its superiority over less structured approaches. By integrating the latest methodological guidance and real-world applications, this article equips professionals with the tools to enhance the rigor, reproducibility, and impact of their evidence synthesis, ultimately accelerating the translation of biomaterial innovations to clinical practice.
What is the PICOS Framework? Building the Bedrock for Biomaterial Evidence Synthesis
The PICOS framework is a critical methodological tool for formulating precise, answerable research questions and structuring systematic reviews. Within the specialized domain of biomaterials research, this framework ensures comprehensive and reproducible synthesis of evidence concerning novel materials, coatings, and implantable devices. This article provides detailed application notes and experimental protocols framed within a broader thesis on applying PICOS to systematic reviews in biomaterial science, aimed at enhancing the quality and clinical translatability of synthesized evidence.
Detailed Application Notes for Each PICOS Component in Biomaterials Research
Table 1: PICOS Framework Specification for Biomaterial Systematic Reviews
| Pillar | Definition | Biomaterial-Specific Considerations | Example from Bone Graft Scaffolds |
|---|---|---|---|
| Population | The specific set of participants, animals, cell lines, or specimens being studied. | Define material-relevant characteristics: species, cell type, disease model, anatomical site, defect characteristics. | In vivo: Adult rabbit femoral condyle critical-size defect model. In vitro: Human mesenchymal stem cells (hMSCs) from bone marrow, passage 3-5. |
| Intervention | The biomaterial, device, or procedural technique being evaluated. | Specify material composition, fabrication method, form, surface modification, sterilization, and delivery method. | Intervention: Porous β-tricalcium phosphate (β-TCP) scaffold coated with recombinant human BMP-2 (0.5 mg/ml). |
| Comparator | The standard against which the intervention is measured (control). | May be another biomaterial, standard of care, placebo, sham surgery, or untreated group. | Comparator: Uncoated porous β-TCP scaffold of identical porosity and geometry (placebo control). Autologous bone graft (clinical standard). |
| Outcome | The measurable endpoints used to evaluate the intervention’s effect. | Include primary and secondary outcomes spanning efficacy, safety, and mechanism. Use validated assays and timepoints. | Primary: Bone volume/total volume (BV/TV) at 8 weeks via micro-CT. Secondary: Osteogenic gene expression (RUNX2, OCN) at 7/14 days; compressive strength at 8 weeks. |
| Study Design | The methodological approach of the primary research. | Dictates level of evidence. Common designs include randomized controlled trials (RCTs), controlled laboratory studies, case series. | Preferred: Randomized controlled animal study; in vitro controlled laboratory study with triplicate replicates. |
Experimental Protocols for Key Biomaterial Assessment Methods
Protocol 1: In Vivo Evaluation of Osteointegration in a Rabbit Femoral Condyle Model (Addresses P, I, C, O)
- Objective: Quantify new bone formation and integration of an experimental bone graft substitute.
- Materials: See "The Scientist's Toolkit" (Table 2).
- Methods:
- Animal Model Preparation (Population): Anesthetize 36 adult New Zealand White rabbits. Create a 6mm diameter, 10mm deep critical-size defect in each lateral femoral condyle using a trephine drill under irrigation.
- Intervention & Randomization (I, C, Study Design): Randomly assign defects to receive: (A) Experimental BMP-2-coated β-TCP scaffold (n=12), (B) Uncoated β-TCP scaffold (n=12), (C) Autologous bone graft (n=12). Use block randomization.
- Outcome Assessment (O):
- Micro-CT Analysis (Primary Outcome): Euthanize animals at 8 weeks. Excise femora and scan at 18μm resolution. Reconstruct and analyze BV/TV, trabecular thickness, and scaffold-bone contact ratio using manufacturer software. Apply Gaussian filter and uniform threshold across all samples.
- Histomorphometry: Dehydrate, embed in methylmethacrylate. Section to 50μm, stain with Toluidine Blue and von Kossa. Quantify osteoid surface and osteoclast count per mm² using image analysis software (e.g., ImageJ).
- Biomechanical Testing: Perform push-out test on a separate specimen set (n=6/group) using a universal testing machine at 1 mm/min crosshead speed. Record ultimate shear strength.
Protocol 2: In Vitro Osteogenic Differentiation Assay (Addresses P, I, C, O)
- Objective: Assess the osteoinductive potential of biomaterial eluents on hMSCs.
- Methods:
- Scaffold Eluent Preparation (I, C): Sterilize scaffolds (coated and uncoated) by gamma irradiation. Incubate scaffolds in basal osteogenic media (without dexamethasone) at 37°C for 72 hours (1 cm³ scaffold/ml media). Filter sterilize (0.22μm) to obtain conditioned media.
- Cell Seeding and Culture (Population): Seed hMSCs (P3) at 10,000 cells/cm² in 12-well plates. At 80% confluence, replace media with: (1) Experimental conditioned media, (2) Control conditioned media, (3) Standard osteogenic media (positive control), (4) Basal media (negative control). Culture for 21 days, changing media every 3 days.
- Outcome Assessment (O):
- Gene Expression (qRT-PCR): Harvest cells at days 7, 14, 21. Extract RNA, synthesize cDNA. Perform qPCR for RUNX2, Osteocalcin (OCN), and ALP. Normalize to GAPDH. Use the 2^(-ΔΔCt) method for analysis.
- Alkaline Phosphatase (ALP) Activity: At day 10, lyse cells. Measure ALP activity using p-nitrophenyl phosphate substrate. Normalize to total protein content (BCA assay).
- Mineralization (Alizarin Red S Staining): At day 21, fix cells, stain with 40mM Alizarin Red S (pH 4.2). Quantify by eluting stain with 10% cetylpyridinium chloride and measuring absorbance at 562 nm.
Visualizations
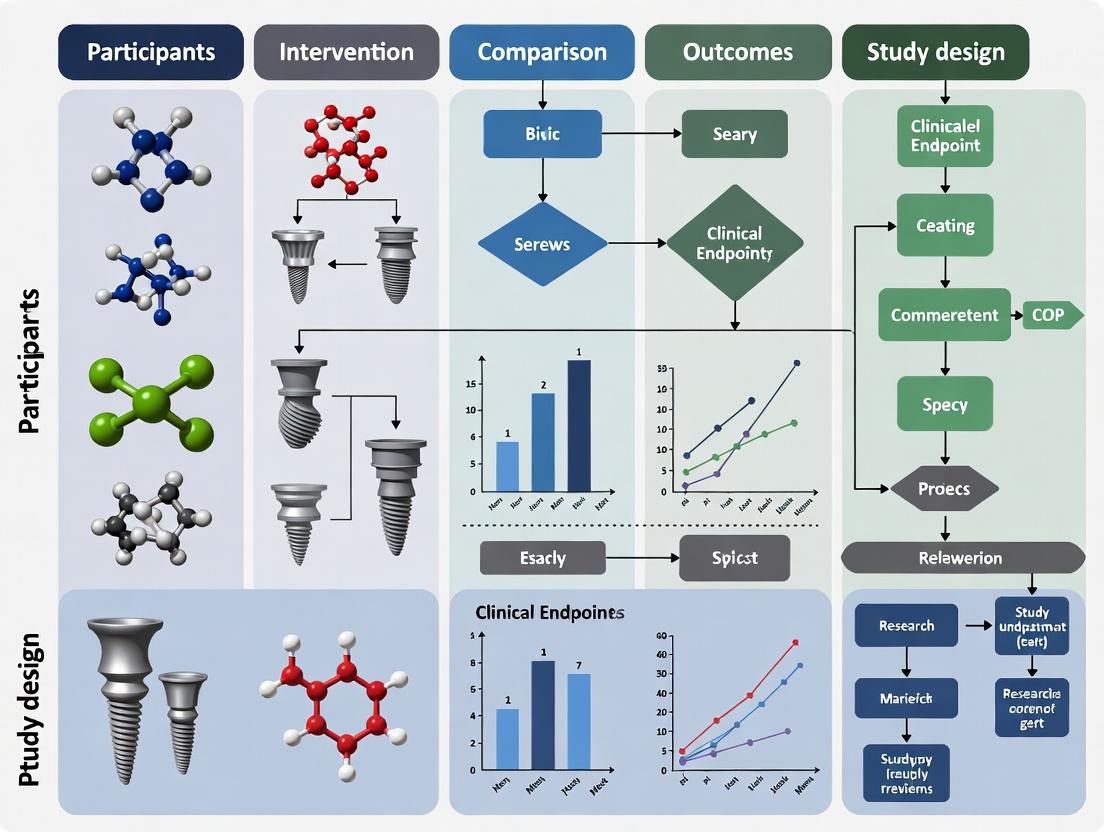
Diagram 1: PICOS Framework for Question Formulation
Diagram 2: In Vivo Osteointegration Study Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Featured Biomaterial Osteogenesis Experiments
| Item | Function in Protocol | Example Product/Catalog |
|---|---|---|
| Porous β-TCP Scaffold | 3D structural basis for bone ingrowth; osteoconductive intervention. | Biomatlante β-TCP granules, 1-2mm, 70% porosity. |
| Recombinant Human BMP-2 | Osteoinductive growth factor coating to enhance bone formation. | PeproTech, 120-02 (E. coli-derived). |
| Critical-Size Defect Drill | Creates standardized bone defect that will not heal without intervention. | 6.0mm diameter trephine bur (KLS Martin). |
| Micro-CT Scanner | Non-destructive 3D quantification of bone morphology and scaffold integration. | Scanco Medical μCT 50, 70kVp energy. |
| hMSCs (Bone Marrow) | Primary human cell model for in vitro osteogenic differentiation assays. | Lonza, PT-2501. |
| Osteogenic Media Supplements | Provides necessary components (ascorbate, β-glycerophosphate) for mineralization. | Gibco StemPro Osteogenesis Supplement, A10072-01. |
| Trizol Reagent | Monophasic solution for simultaneous RNA/DNA/protein isolation from cells on materials. | Invitrogen, 15596026. |
| Alizarin Red S | Dye that binds to calcium deposits, enabling quantification of mineralization. | Sigma-Aldrich, A5533. |
| Universal Testing Machine | Measures biomechanical properties of bone-scaffold construct (e.g., push-out strength). | Instron 5965 with 1kN load cell. |
Detailed Application Notes and Protocols
Within the broader thesis on the PICOS (Population, Intervention, Comparison, Outcome, Study design) framework for systematic reviews in biomaterials research, these application notes provide the operational protocols necessary to manage the field's inherent complexity. Biomaterial studies are characterized by extreme heterogeneity in materials (e.g., polymer composition, ceramic porosity, scaffold architecture), biological models (in vitro, in vivo, ex vivo), and outcome measures (biocompatibility, mechanical integration, degradation). The PICOS framework is not merely helpful but essential to define explicit boundaries, ensure reproducibility, and enable meaningful synthesis.
Protocol 1: Defining PICOS for a Biomaterial Review
Objective: To construct a precise, actionable research question for a systematic review on "Hydrogel-based biomaterials for cartilage regeneration."
Detailed Methodology:
- Population (P): Explicitly define the subject of the intervention.
- In vitro: Primary human or murine chondrocytes, chondroprogenitor cells (e.g., ATDC5), or mesenchymal stem cells (MSCs) in 2D/3D culture.
- In vivo: Animal models of cartilage defect (e.g., rat trochlear groove defect, rabbit osteochondral defect). Specify species, strain, defect type/size.
- Ex vivo: Osteochondral explants from specified donors/species.
- Exclusion: Studies focusing solely on bone, tendon, or other non-cartilaginous tissues.
Intervention (I): Define the biomaterial class and key characteristics.
- Material Class: Hydrogels (natural: alginate, chitosan, hyaluronic acid; synthetic: PEG, PLA-PEG).
- Formulation: Include any functionalization (e.g., RGD peptide conjugation), composite elements (e.g., nano-hydroxyapatite), or loaded biologic factors (e.g., TGF-β3).
- Exclusion: Solid scaffolds (PCL, PLA meshes), non-hydrogel injectables.
Comparison (C): Establish the control or comparator.
- Positive Control: Existing clinical treatment (e.g., microfracture, autologous chondrocyte implantation).
- Negative Control: Untreated defect, empty scaffold.
- Alternative Material Control: A different hydrogel formulation or a commercially available product (e.g., Hyalograft C).
- Protocol Note: Comparisons must be within the same study.
Outcomes (O): Categorize and prioritize quantitative and qualitative measures.
- Primary: Histological scoring (e.g., ICRS II, O'Driscoll score), mechanical properties (compressive modulus), glycosaminoglycan (GAG)/DNA content.
- Secondary: Gene expression (COL2A1, ACAN, SOX9), immunohistochemistry (collagen type II), biocompatibility/immunogenicity markers.
Study Design (S): Specify eligible study types.
- Include: Randomized controlled trials (in vivo), controlled laboratory studies (in vitro), comparative studies.
- Exclude: Case reports, narrative reviews, editorials, modeling studies without experimental validation.
Table 1: Quantified Heterogeneity in Cartilage Biomaterial Studies (2020-2024)
| PICOS Element | Data Source | Number of Variations Identified | Common Pitfalls in Reporting |
|---|---|---|---|
| Population (Model) | PubMed Search | 12 distinct animal models, 8 cell lines | 40% fail to report animal sex/weight; 65% omit cell passage number. |
| Intervention (Hydrogel) | Scopus Analysis | 25+ polymer bases, 15+ crosslinking methods | >50% lack detailed rheological data (gelation time, modulus). |
| Outcome (Assessment) | Web of Science | 9 histological scores, 6 mechanical tests | Only 30% report blinded histological assessment; <20% include power analysis. |
Protocol 2: Data Extraction & Synthesis Workflow
Objective: To systematically extract data from included studies into a structured format for analysis, minimizing subjective bias.
Materials & Workflow:
- Pilot Extraction: Using 2-3 included studies, calibrate the extraction team.
- Dual Independent Extraction: Two reviewers extract data using a pre-designed spreadsheet.
- Adjudication: A third reviewer resolves discrepancies.
- Synthesis Table: Populate a master table with columns for each PICOS element and results.
Table 2: Research Reagent Solutions for Key Biomaterial Assessments
| Reagent/Kit | Supplier Examples | Function in Biomaterial Review Context |
|---|---|---|
| AlamarBlue / MTS Assay | Thermo Fisher, Abcam | Quantifies cell viability and proliferation on biomaterial surfaces. |
| Live/Dead Staining (Calcein-AM/EthD-1) | Invitrogen, Sigma-Aldrich | Visualizes spatial distribution of live vs. dead cells in 3D scaffolds. |
| Dimethylmethylene Blue (DMMB) Assay | Sigma-Aldrich, Biocolor | Quantifies sulfated glycosaminoglycan (sGAG) deposition, key for cartilage/ECM. |
| Human/Mouse TGF-β3 ELISA | R&D Systems, PeproTech | Measures release kinetics of growth factors from delivery systems. |
| TRITC-Phalloidin / DAPI | Cytoskeleton, Inc., Sigma | Stains actin cytoskeleton and nuclei to assess cell morphology and adhesion. |
| qPCR Primers (COL1A1, COL2A1, RUNX2) | Qiagen, Thermo Fisher | Assesses cell differentiation and phenotype stability post-implantation. |
Diagram Title: PICOS Framework Workflow for Systematic Review
Protocol 3: Visualizing Molecular Mechanisms of Action
Objective: To create a standardized method for extracting and visualizing signaling pathways activated by biomaterial interventions, enabling cross-study comparison.
Detailed Methodology:
- From included studies, extract all reported protein/gene expression data related to cell signaling.
- Categorize pathways (e.g., Mechanotransduction, Osteogenic/Chondrogenic).
- Map molecules onto canonical pathways using databases (KEGG, Reactome).
- Use Graphviz to generate a consensus pathway diagram, noting which biomaterials influence specific nodes.
Diagram Title: Biomaterial-Cell Signaling Pathway Map
Conclusion: Adherence to these PICOS-driven protocols creates a rigid, auditable structure that transforms the review of heterogeneous biomaterials literature from a narrative exercise into a reproducible, quantitative scientific process. It is the foundational methodology for generating reliable evidence to guide future biomaterial design and clinical translation.
Application Notes: The PICOS Framework in Biomaterial Systematic Reviews
The adaptation of the PICOS framework—Population, Intervention, Comparator, Outcomes, Study design—from medical systematic reviews to biomaterials research provides a critical structure for synthesizing evidence in this interdisciplinary field. This structured approach is essential for addressing complex questions in biomaterial development, biocompatibility, and functional performance.
Table 1: Evolution of PICOS Elements from Clinical to Biomaterial Contexts
| PICOS Element | Traditional Medical Context | Specialized Biomaterial Context |
|---|---|---|
| Population | Human patients with a specific condition. | Target biological system (e.g., specific cell line, animal model, tissue type). |
| Intervention | Drug, surgical procedure, or therapy. | Biomaterial implant, scaffold, coating, or drug-delivery system with specific properties. |
| Comparator | Placebo, standard care, or alternative treatment. | Control material (e.g., bare implant, commercial standard, sham surgery), or material with a different property (e.g., smooth vs. rough surface). |
| Outcomes | Clinical endpoints (e.g., survival, symptom reduction). | In vitro (cell adhesion, proliferation), in vivo (osseointegration, foreign body response), and material (degradation rate, mechanical strength) outcomes. |
| Study Design | Randomized Controlled Trials (RCTs), cohort studies. | Controlled laboratory studies, animal studies, computational simulations, and early-phase human trials. |
Key Application: Systematic reviews using this adapted PICOS framework can definitively answer questions such as: "In preclinical rodent models of critical-sized calvarial defects (P), do hydroxyapatite-based scaffolds (I), compared to autologous bone grafts (C), improve new bone volume (O) in controlled intervention studies (S)?" This rigor reduces bias and translates fragmented data into actionable insights for regulatory pathways and next-generation design.
Protocol: Conducting a Systematic Review on Osteoinductive Biomaterials
Objective: To systematically identify, evaluate, and synthesize evidence on the efficacy of calcium phosphate (CaP) biomaterials with surface functionalization in promoting osteogenic differentiation in vitro.
2.1 Search Strategy & Study Selection (Based on PICOS)
- Databases: PubMed, Scopus, Web of Science, EMBASE.
- Search String Example: (("calcium phosphate" OR "hydroxyapatite") AND ("RGD peptide" OR "functionalized") AND ("osteogenic differentiation" OR "alkaline phosphatase" OR "Runx2") AND ("mesenchymal stem cells" OR "osteoprogenitor cells") AND (in vitro)).
- Inclusion Criteria:
- P: Human or murine mesenchymal stem cells (MSCs).
- I: CaP biomaterial (any form) with deliberate surface functionalization (e.g., with peptides, cytokines).
- C: Unfunctionalized CaP material or standard tissue culture plastic.
- O: Quantitative measures of osteogenic differentiation (ALP activity, osteocalcin/qPCR of markers, mineral deposition).
- S: Controlled laboratory study.
- Screening: Use reference management software (e.g., Covidence, Rayyan). Two independent reviewers screen titles/abstracts, then full texts. Resolve conflicts by consensus.
2.2 Data Extraction & Synthesis
- Create a standardized extraction table.
- Extract: Study ID, cell source, biomaterial details, functionalization method, control, outcome measures, timepoints, key results.
- Meta-analysis: If studies are sufficiently homogeneous, perform statistical pooling of quantitative outcomes (e.g., standardized mean difference in ALP activity at day 7). Use software (RevMan, R). Assess heterogeneity with I² statistic.
Table 2: Example Data Extraction for a Hypothetical Study
| Study ID | Cell Type | Intervention (Functionalized) | Comparator | Outcome (ALP Activity, Day 7) | Notes |
|---|---|---|---|---|---|
| Smith et al. 2023 | hMSCs | RGD-grafted nano-HA scaffold | Pristine nano-HA scaffold | 2.5-fold increase (p<0.01) | Measured via pNPP assay, n=6. |
Experimental Protocol: Evaluating Osteoinduction on Functionalized Surfaces
Title: In Vitro Assessment of Peptide-Functionalized Biomaterial Osteoinductivity.
3.1 Materials Preparation
- Substrate: Prepare 10mm diameter discs of sintered hydroxyapatite (HA).
- Functionalization: Immerse HA discs in 1 mL of 0.1 mg/mL RGD-peptide (sequence: Arg-Gly-Asp) solution in PBS. Incubate for 24h at 4°C under gentle agitation.
- Control: Immerse discs in PBS alone.
- Sterilization: Rinse discs 3x with sterile PBS under aseptic conditions. UV sterilize for 30 minutes per side.
3.2 Cell Seeding & Differentiation
- Seed human MSCs (passage 3-5) at a density of 20,000 cells/disc onto functionalized and control discs placed in a 24-well plate.
- Culture in standard growth medium (α-MEM, 10% FBS, 1% P/S) for 24h to allow adhesion.
- Replace medium with osteogenic induction medium (growth medium supplemented with 10 mM β-glycerophosphate, 50 µg/mL ascorbic acid, and 100 nM dexamethasone).
- Maintain cultures for up to 21 days, changing medium every 48-72 hours.
3.3 Outcome Analysis (Key Timepoints)
- Day 3-5: Alkaline Phosphatase (ALP) Activity. Lyse cells in 0.1% Triton X-100. Measure ALP activity using a p-nitrophenyl phosphate (pNPP) substrate assay. Normalize to total protein content (BCA assay).
- Day 14: Gene Expression. Extract RNA, synthesize cDNA. Perform qPCR for osteogenic markers (RUNX2, OSTERIX, OSTEOCALCIN). Normalize to housekeeping gene (e.g., GAPDH) using the 2^(-ΔΔCt) method.
- Day 21: Mineralization. Fix samples with 4% PFA. Stain with 2% Alizarin Red S (pH 4.2) for 20 min. Quantify by eluting stain with 10% cetylpyridinium chloride and measuring absorbance at 562 nm.
Visualization: Signaling Pathways in Biomaterial-Mediated Osteoinduction
Title: RGD-Mediated Osteogenic Signaling Cascade
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for In Vitro Biomaterial Osteoinduction Studies
| Item | Function/Application | Example Product/Catalog |
|---|---|---|
| Human Mesenchymal Stem Cells (hMSCs) | Primary cell model for testing osteogenic potential. | Lonza PT-2501; ATCC PCS-500-012. |
| Osteogenic Induction Supplement | Provides critical factors (dexamethasone, ascorbate, β-glycerophosphate) to drive differentiation. | Gibco A10069-01; STEMCELL 05465. |
| Synthetic RGD Peptide | Functionalize biomaterial surfaces to enhance integrin-mediated cell adhesion. | MilliporeSigma CC1006M (GRGDSP). |
| Alkaline Phosphatase Assay Kit | Colorimetric quantification of early osteogenic marker (ALP) activity. | Abcam ab83369; Sigma-Aldrich 86R-1KT. |
| Alizarin Red S Staining Kit | Detects and quantifies calcium deposits (mineralization) in cell cultures. | ScienCell 0223; MilliporeSigma EMS. |
| qPCR Primers for Osteogenic Genes | Quantify expression of markers like RUNX2, SP7/Osterix, BGLAP/Osteocalcin. | Qiagen, PrimePCR Assays. |
| Hydroxyapatite Discs/Scaffolds | Standardized bioceramic substrate for surface modification studies. | Himed OSTEOSPACER; Sigma-Aldrich 677418. |
Application Notes: Mapping PICOS to Biomaterial Studies
In the context of a systematic review for biomaterials, the generic PICOS framework (Population, Intervention, Comparison, Outcome, Study design) requires precise adaptation. The "Intervention" (I) element is particularly complex, moving beyond a simple drug name to encompass the multifaceted nature of the biomaterial itself.
PICOS Breakdown for Biomaterials:
- P (Population): Target biological system (e.g., "human mesenchymal stem cells," "rat calvarial defect model," "platelet-rich plasma").
- I (Intervention): The biomaterial, defined by its:
- Core Composition: Base polymer/metal/ceramic (e.g., PCL, Ti-6Al-4V, β-tricalcium phosphate).
- Form/Architecture: Physical manifestation (e.g., electrospun nanofiber mesh, 3D-printed porous scaffold, hydrogel, microsphere).
- Surface Modification/Functionalization: Chemical or biological alterations (e.g., RGD peptide coating, plasma treatment, heparin conjugation).
- C (Comparison): Can be a control material (e.g., tissue culture plastic, untreated defect), a gold-standard material (e.g., autograft), or a different variant of the intervention (e.g., smooth vs. nanotextured surface).
- O (Outcome): Measured effects, categorized as:
- In vitro: Cell viability, proliferation, differentiation (ALP, osteocalcin), protein adsorption.
- In vivo: New bone volume (BV/TV), implant osseointegration (BIC%), inflammatory response.
- Material Properties: Compressive modulus, degradation rate, shear-thinning behavior.
- S (Study Design): In vitro experimental study, in vivo animal model (e.g., randomized controlled trial in a rabbit femoral condyle model), clinical trial phase.
Table 1: Quantified Outcomes from Recent Biomaterial Studies (Illustrative Examples)
| Biomaterial Intervention (Composition/Form/Modification) | Comparison Group | Primary Outcome (Measured) | Result (Mean ± SD or Median [IQR]) | Study Design |
|---|---|---|---|---|
| PCL/Collagen I Electrospun Nanofibers (600nm diameter) | Tissue Culture Plastic (TCP) | MC3T3-E1 Cell Proliferation (Day 7) (WST-1 Assay) | 2.45 ± 0.21 fold-change vs. TCP (1.00) | In vitro, controlled |
| 3D-printed β-TCP Scaffold (500µm pores) | Empty Critical-Size Defect | New Bone Volume/Tissue Volume (BV/TV) at 8 weeks (µCT) | 38.7% ± 5.2% vs. 12.1% ± 3.8% | In vivo, rat calvaria (n=10/group) |
| Alginate Hydrogel (2% w/v) with TGF-β3 (50ng/mL) | Alginate Hydrogel alone | Chondrogenic Differentiation (GAG/DNA content) at 21 days | 15.4 [12.8–18.1] µg/µg vs. 4.2 [3.5–5.1] µg/µg | In vitro, human chondrocytes |
Experimental Protocols
Protocol 1: Fabrication and Characterization of Electrospun Polymer Nanofibers
Aim: To produce and characterize a polycaprolactone (PCL)-based nanofibrous scaffold for cell culture studies.
Materials (Research Reagent Solutions):
- Polycaprolactone (PCL), Mn 80,000: Synthetic, biodegradable polymer providing structural integrity.
- Hexafluoro-2-propanol (HFIP): Solvent for dissolving PCL for electrospinning.
- Electrospinning apparatus: High-voltage power supply, syringe pump, grounded collector.
- Scanning Electron Microscope (SEM): For imaging fiber morphology and diameter measurement.
- Contact Angle Goniometer: To measure surface wettability/hydrophilicity.
Methodology:
- Solution Preparation: Dissolve PCL pellets in HFIP at a concentration of 12% (w/v) under constant stirring for 4 hours at room temperature to ensure complete dissolution.
- Electrospinning Setup: Load the solution into a 5 mL syringe fitted with a 21-gauge blunt needle. Set the syringe pump flow rate to 1.0 mL/h. Position the needle tip 15 cm from a flat aluminum foil-covered collector.
- Fiber Production: Apply a high voltage of 15 kV to the needle tip. Collect the resulting non-woven nanofiber mat on the foil for 6 hours. Maintain environmental conditions at 23°C and 40% relative humidity.
- Post-Processing: Place the collected fiber mat in a vacuum desiccator for 48 hours to remove residual solvent.
- Characterization: Sputter-coat a sample with gold for 60 seconds. Image using SEM at 10 kV acceleration voltage. Analyze 100 random fibers from three different images using ImageJ software to determine average fiber diameter. Perform water contact angle measurements using the sessile drop method (n=5).
Protocol 2:In VitroAssessment of Osteogenic Differentiation on Biomaterials
Aim: To quantify the osteogenic differentiation of stem cells cultured on a test biomaterial.
Materials (Research Reagent Solutions):
- Osteogenic Induction Medium: Base medium (e.g., α-MEM) supplemented with 10% FBS, 10 mM β-glycerophosphate, 50 µg/mL ascorbic acid, and 100 nM dexamethasone.
- Alizarin Red S Solution (40mM, pH 4.2): Stains calcium deposits, a marker of late-stage osteogenesis.
- Alkaline Phosphatase (ALP) Activity Assay Kit: Contains p-nitrophenyl phosphate (pNPP) as substrate for measuring early osteogenic marker ALP.
- Cell Lysis Buffer (RIPA): For lysing cells to extract proteins and enzymes for quantification.
- Quant-iT PicoGreen dsDNA Assay Kit: For normalizing biochemical data to total cell number.
Methodology:
- Cell Seeding: Seed human bone marrow-derived mesenchymal stem cells (hBM-MSCs) at a density of 20,000 cells/cm² onto sterilized material samples (12-well plate format). Allow attachment in growth medium for 24 hours.
- Osteogenic Induction: Replace medium with osteogenic induction medium. Refresh the medium every 3 days for up to 21 days.
- ALP Activity (Day 7-10): Wash samples with PBS. Lyse cells in 0.2% Triton X-100. Mix lysate with pNPP substrate and incubate at 37°C for 30 minutes. Stop reaction with 0.1N NaOH. Measure absorbance at 405 nm. Run parallel PicoGreen DNA assay on lysate to determine total DNA content. Express ALP activity as nmol of p-nitrophenol produced per minute per µg of DNA.
- Alizarin Red Staining (Day 21): Wash samples gently with PBS and fix in 4% paraformaldehyde for 15 minutes. Incubate with 2% Alizarin Red S solution (pH 4.2) for 20 minutes at room temperature. Wash extensively with deionized water. For quantification, solubilize stained mineral in 10% cetylpyridinium chloride for 1 hour. Measure absorbance at 562 nm.
Visualizations
Title: PICOS Framework Breakdown for Biomaterial Research
Title: Standard In Vitro Biomaterial Testing Workflow
Title: Simplified Osteogenic Signaling on Biomaterials
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Materials for Biomaterial Synthesis and Testing
| Item | Function in Biomaterial Research |
|---|---|
| Polycaprolactone (PCL) | A biodegradable, synthetic polyester frequently used as a base polymer for creating scaffolds via electrospinning or 3D printing due to its excellent processability and biocompatibility. |
| β-Tricalcium Phosphate (β-TCP) Powder | A bioactive and resorbable ceramic used in bone graft substitutes and composite scaffolds to promote osteoconduction and enhance mechanical properties. |
| RGD Peptide (e.g., GRGDS) | A short peptide sequence (Arginine-Glycine-Aspartic Acid) used to functionalize biomaterial surfaces to enhance specific cell adhesion via integrin receptor binding. |
| Alkaline Phosphatase (ALP) Activity Assay Kit | A colorimetric or fluorometric kit used to quantify ALP enzyme activity, a key early-stage marker for osteogenic differentiation of stem cells. |
| Alizarin Red S Solution | A dye that binds to calcium salts, used to stain and semi-quantify mineralized matrix deposition by cells, indicating late-stage osteogenesis. |
| Scanning Electron Microscope (SEM) | An essential instrument for high-resolution imaging of biomaterial surface topography, porosity, and cell-material interactions at the micro- and nano-scale. |
| Contact Angle Goniometer | Measures the angle a liquid droplet makes with a solid surface, providing a quantitative assessment of material surface wettability (hydrophilicity/hydrophobicity). |
| Electrospinning Apparatus | A setup comprising a high-voltage supply, syringe pump, and collector used to produce non-woven nanofiber mats from polymer solutions. |
1. Introduction & Application Notes Within the broader thesis on the PICOS (Population, Intervention, Comparator, Outcome, Study design) framework for biomaterial systematic reviews (SRs), the initial PICOS statement is not merely a planning exercise. It is the critical methodological linchpin that directly dictates and informs the validity of every subsequent step. A vague or imprecise statement leads to cascading errors in search strategy, study selection, data extraction, and synthesis, ultimately compromising the review's conclusion. In contrast, a meticulously constructed PICOS ensures reproducibility, minimizes bias, and yields actionable evidence for researchers and drug development professionals.
2. Quantitative Data on PICOS Precision Impact Table 1: Impact of PICOS Precision on Systematic Review Outcomes (Meta-Analysis of Methodological Studies)
| PICOS Component | Common Imprecision | Consequence for Subsequent Steps | Quantitative Impact (Estimated) |
|---|---|---|---|
| Population (P) | Defining "osteoporotic bone" without specifying species (e.g., rat vs. sheep) or defect model (critical-size vs. drill-hole). | Inconsistent animal models included, leading to high heterogeneity and ungeneralizable results. | Increases statistical heterogeneity (I²) by 30-50% in preclinical meta-analyses. |
| Intervention (I) | "Hydrogel scaffold" without specifying polymer (e.g., alginate vs. chitosan), functionalization (RGD peptide), or physical form (injectable vs. pre-formed). | Missed relevant studies; inability to perform meaningful sub-group analysis on material properties. | Can lead to exclusion of 15-25% of potentially relevant records during screening. |
| Comparator (C) | Using "control" without defining if it is a sham operation, an existing clinical standard (e.g., autograft), or a placebo material. | Biased assessment of comparative effect size; mix of inappropriate comparisons. | Can over- or under-estimate the standardized mean difference (SMD) by up to 0.8. |
| Outcome (O) | "Bone regeneration" measured only histologically, excluding micro-CT quantification (BV/TV). | Incomplete outcome reporting; selective reporting bias; missed quantitative synthesis opportunities. | Up to 40% of studies may be excluded from meta-analysis due to outcome mismatch. |
| Study Design (S) | Specifying "randomized trials" in a field dominated by high-quality controlled animal studies. | Exclusion of the entire evidence base for novel biomaterials prior to human trials. | May reduce included studies by >90% in early-stage biomaterial research. |
3. Experimental Protocols: From PICOS to Execution
Protocol 3.1: Translating PICOS into a Search Strategy Objective: To construct a reproducible, sensitive, and specific bibliographic database search string. Materials: PICOS statement table, bibliographic databases (PubMed, Embase, Web of Science, Scopus), Boolean operators, controlled vocabularies (MeSH, Emtree), search syntax guide. Procedure:
- Deconstruction: List each operational term from the P, I, C, O components.
- Vocabulary Mapping: For each database, identify corresponding controlled vocabulary terms (e.g., MeSH for PubMed: "Bone Regeneration" [Mesh], "Tissue Scaffolds" [Mesh]).
- Free-Text Expansion: Include synonyms, acronyms, and spelling variants (e.g., (hydrogel OR "water-swollen polymer")).
- Boolean Structuring: Combine using OR within components, AND between components. Use proximity operators where critical (e.g., "peptide* NEAR/3 functionalized").
- Study Design Filter: Apply validated methodological filters (e.g., Cochrane RCT filter, animal study filter).
- Pilot & Validation: Run pilot search. Validate by checking recall of 3-5 known key studies. Iteratively refine syntax to capture all.
- Documentation: Record final string for each database with date and results count.
Protocol 3.2: PICOS-Informed Screening & Selection Objective: To apply the PICOS criteria consistently at title/abstract and full-text levels. Materials: Screening platform (e.g., Rayyan, Covidence), pre-piloted screening form, reference library. Procedure:
- Form Development: Create a screening form with explicit, binary (Yes/No/Maybe) questions for each PICOS element.
- Piloting: Two independent reviewers screen a random 1% sample of records. Calculate inter-rater reliability (Cohen's Kappa). Resolve discrepancies and refine form/questions until Kappa >0.8.
- Blinded Screening: Reviewers screen all records independently based on title/abstract using the form.
- Conflict Resolution: The software highlights conflicts. Conflicts are resolved via discussion or a third arbitrator.
- Full-Text Application: Obtain full texts of included records. Apply the same refined PICOS criteria with greater detail. Document reasons for exclusion at this stage.
Protocol 3.3: Data Extraction Based on PICOS Objective: To systematically extract quantitative and qualitative data directly relevant to the PICOS framework. Materials: Standardized, piloted data extraction spreadsheet, source PDFs. Procedure:
- Spreadsheet Design: Columns are mapped to PICOS: Study ID, Population details (species, n, model), Intervention (material full specification, dose, delivery), Comparator (exact description), Outcomes (primary/secondary, measurement method, time points, results), Study Design (randomization, blinding).
- Pilot Extraction: Two reviewers extract data from 2-3 studies, compare, and calibrate.
- Independent Extraction: Reviewers extract data independently.
- Verification: A second reviewer checks all extracted numerical data against the source for accuracy.
4. Visualizations
Title: How Precise PICOS Informs the SR Workflow
Title: Consequence Cascade: Precise vs. Imprecise PICOS
5. The Scientist's Toolkit: Research Reagent Solutions for Biomaterial SRs
Table 2: Essential Toolkit for Executing a PICOS-Driven Biomaterial Systematic Review
| Tool/Reagent | Category | Function in the Review Process |
|---|---|---|
| Rayyan / Covidence | Software Platform | Manages deduplication, blinded screening, and conflict resolution for titles/abstracts and full texts based on PICOS criteria. |
| EndNote / Zotero | Reference Manager | Stores, organizes, and de-duplicates search results from multiple databases. Enables PDF annotation. |
| CADIMA | Web Tool | A dedicated SR platform guiding protocol registration, PICOS definition, and reporting according to PRISMA. |
| PRISMA Checklist & Diagram | Reporting Framework | Ensures transparent and complete reporting of the review flow from PICOS to synthesis. |
| SYRCLE's Risk of Bias Tool | Quality Assessment Tool | A validated tool for assessing risk of bias in animal studies, with domains directly linked to PICO elements. |
| MeSH Browser / Emtree | Controlled Vocabulary | Critical for translating PICOS concepts into database-specific thesaurus terms for a sensitive search. |
| PICO Portal | Search Strategy Tool | Assists in building and translating complex Boolean search strings across multiple databases. |
| GRADE for Preclinical Evidence | Evidence Grading | Framework to rate the certainty of evidence synthesized from animal studies, informed by PICOS limitations. |
From Theory to Lab Notebook: Implementing PICOS in Your Biomaterial Review Protocol
Application Notes: The PICOS Framework in Biomaterials Research
The Population, Intervention, Comparison, Outcome, Study design (PICOS) framework is the cornerstone of a focused, reproducible, and clinically relevant systematic review. For biomaterials, this framework requires precise adaptation to address the unique interplay between material properties, biological performance, and clinical context. A well-structured PICOS question ensures comprehensive literature retrieval and meaningful synthesis, forming the critical first step in a systematic review thesis.
Key Adaptations for Biomaterials:
- Population (P): Extends beyond patient demographics to include the specific tissue defect (e.g., full-thickness osteochondral defect, grade IV), animal model (e.g., rabbit trochlear groove), or cell type (e.g., human mesenchymal stem cells).
- Intervention (I): The biomaterial itself, defined by its composition (e.g., gelatin-methacryloyl), key physico-chemical properties (e.g., stiffness, degradation rate), and often its delivery form or functionalization (e.g., RGD-modified, TGF-β3 loaded).
- Comparison (C): Can be a standard clinical treatment (e.g., microfracture), a commercialized biomaterial (e.g., collagen membrane), a different formulation of the same base material, or an untreated control.
- Outcome (S): Must include multi-modal endpoints: in vitro (cell viability, gene expression), in vivo (histological scoring, mechanical properties), and clinical outcomes (KOOS score, MRI evaluation).
- Study design (S): Encompasses in vitro studies, controlled in vivo animal studies, and clinical trials (randomized controlled trials being the gold standard for efficacy).
PICOS Question Template and Protocol for Biomaterial Systematic Reviews
Protocol: Formulating the PICOS Question
- Define the Clinical Problem: Identify the unmet clinical need (e.g., limited self-repair of articular cartilage).
- Specify the Biomaterial Class: Select the material category (e.g., hydrogels, 3D-printed scaffolds, decellularized matrices).
- Populate PICOS Elements: Use the table below to iteratively refine each element. Consult with a librarian or use database thesauri (MeSH, Emtree) to identify controlled vocabulary.
- Assemble the Final Question: Combine the refined elements into a clear, searchable question.
Table 1: Biomaterial-Specific PICOS Template (Hydrogel Example)
| PICOS Element | Description & Considerations | Hydrogel for Cartilage Repair Example |
|---|---|---|
| Population (P) | Species, disease/injury model, cell type, defect location/size. | Adult New Zealand White rabbits with a 3mm diameter full-thickness chondral defect in the trochlear groove. |
| Intervention (I) | Biomaterial name, composition, key properties (mechanical, degradation), functionalization (cells, growth factors). | Injectable hyaluronic acid-methacrylate (HAMA) hydrogel loaded with TGF-β3 (10 ng/mL). |
| Comparison (C) | Current standard of care, alternative material, placebo, or different formulation of the intervention. | 1. Microfracture surgery (clinical standard). 2. Empty defect (negative control). 3. A commercial collagen type I/III scaffold. |
| Outcomes (O) | Categorized by study type: histological, biochemical, biomechanical, imaging, functional/clinical. | Primary: Histological score (ICRS II) at 12 weeks. Secondary: Glycosaminoglycan (GAG) content, compressive modulus, type II collagen immuno-staining. |
| Study Design (S) | Range from foundational in vitro studies to pivotal clinical trials. | Controlled laboratory in vivo animal study (randomized allocation to treatment groups). |
Final Example PICOS Question: In adult rabbit models of full-thickness chondral defects (P), does implantation of a TGF-β3-loaded HAMA hydrogel (I), compared to microfracture surgery or an empty defect (C), improve histological cartilage repair scores and neotissue glycosaminoglycan content (O) in a controlled in vivo study (S)?
Experimental Protocols Cited in Literature
Protocol 1: Synthesis and Characterization of Methacrylated Hyaluronic Acid (HAMA) Hydrogel
- Objective: To synthesize a photocrosslinkable hydrogel and characterize its fundamental properties.
- Materials: Hyaluronic acid sodium salt, methacrylic anhydride, phosphate-buffered saline (PBS), photoinitiator (LAP or Irgacure 2959), UV light source (365 nm, 5-10 mW/cm²).
- Method:
- Methacrylation: Dissolve HA in PBS on ice. Slowly add methacrylic anhydride at a molar ratio of 10:1 (anhydride:HA disaccharide unit) under constant stirring and pH control (maintain pH ~8 with 5M NaOH). React for 24h at 4°C.
- Purification: Terminate reaction by diluting 5x in cold PBS. Dialyze (MWCO 6-8 kDa) against deionized water for 72h, changing water frequently. Lyophilize to obtain white HAMA foam.
- Hydrogel Fabrication: Dissolve lyophilized HAMA and photoinitiator (0.05% w/v) in PBS to desired concentration (e.g., 2% w/v). Sterilize via 0.22 µm filtration.
- Crosslinking: Pipet precursor solution into mold. Expose to UV light (365 nm, 5 mW/cm²) for 60-180 seconds.
- Characterization: Determine degree of methacrylation via ¹H-NMR. Measure swelling ratio, compressive modulus via rheometry, and in vitro degradation.
Protocol 2: In Vivo Implantation in Rabbit Chondral Defect Model
- Objective: To assess the efficacy of the hydrogel in promoting cartilage repair.
- Preoperative: Anesthetize adult NZW rabbit. Administer analgesics and antibiotics.
- Surgical Procedure:
- Perform medial parapatellar arthrotomy on knee joint.
- Luxate patella to expose trochlear groove.
- Create a full-thickness chondral defect (3mm diameter) using a biopsy punch, ensuring no penetration into subchondral bone.
- Randomly assign defect to treatment: (a) Fill with HAMA+TGF-β3 precursor, crosslink in situ with UV (30s). (b) Perform microfracture with awl. (c) Leave empty.
- Close joint capsule, fascia, and skin in layers.
- Postoperative: Provide analgesia for 72h. Allow free cage activity.
- Termination: Euthanize at 12 weeks. Harvest distal femur for analysis.
Protocol 3: Histological and Biochemical Evaluation
- Histology: Fix samples in 4% PFA, decalcify, paraffin-embed. Section (5µm) and stain with Hematoxylin & Eosin (H&E), Safranin O/Fast Green (for GAGs), and perform immunohistochemistry for Collagen Type II. Score using the International Cartilage Repair Society (ICRS) II Visual Histological Assessment Scale.
- Biochemistry: Digest explants with papain. Quantify GAG content using dimethylmethylene blue (DMMB) assay against chondroitin sulfate standard. Measure total collagen via hydroxyproline assay.
Visualizations
Diagram 1: PICOS Question Development Workflow
Diagram 2: Key Signaling in Hydrogel-Mediated Cartilage Repair
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Hydrogel-based Cartilage Repair Studies
| Reagent / Material | Function / Role in Research | Key Considerations |
|---|---|---|
| Hyaluronic Acid (Sodium Salt) | Natural polysaccharide backbone for biomimetic hydrogel synthesis; provides biocompatibility and inherent bioactivity. | Molecular weight controls viscosity and gel porosity. High purity (GMP-grade) recommended for in vivo use. |
| Methacrylic Anhydride | Functionalizing agent to introduce photocrosslinkable methacrylate groups onto polymers (e.g., HA, gelatin). | Reaction must be performed on ice with pH control to avoid excessive esterification and hydrolysis. |
| Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP) | Photoinitiator for visible/UV light crosslinking. Enables rapid gelation under cytocompatible conditions (365-405 nm). | Superior to Irgacure 2959 in solubility and cytotoxicity profile for cell-laden encapsulation. |
| Recombinant Human TGF-β3 | Key chondrogenic growth factor to entrap in hydrogel for directing stem cell differentiation and matrix synthesis. | Short half-life requires delivery system (e.g., hydrogel) for sustained release. Cost is a significant factor. |
| Safranin O Stain | Histological dye that stoichiometrically binds to sulfated glycosaminoglycans (GAGs) in cartilage matrix. | Staining intensity can be quantified via image analysis to assess proteoglycan content in repair tissue. |
| Anti-Collagen Type II Antibody | Primary antibody for immunohistochemistry; specific marker for hyaline cartilage formation. | Must distinguish between Collagen Type II (native) and Type I (fibrocartilage). Confirm species reactivity. |
| Papain from Papaya Latex | Proteolytic enzyme for complete digestion of cartilage explants prior to biochemical GAG and DNA quantification. | Must be activated with cysteine and EDTA. Digestion time (e.g., 65°C for 18h) must be standardized. |
Within the broader thesis on the PICOS framework for biomaterial systematic reviews, this section details the critical translational step from a well-defined PICOS question to an executable, comprehensive bibliographic database search. The precision of this translation directly determines the recall and relevance of the retrieved evidence, forming the empirical foundation for the subsequent synthesis and meta-analysis stages specific to biomaterial applications.
Application Notes: Core Principles & Live Search Data Synthesis
A live search across current methodology literature (2023-2024) and database documentation reveals the following consolidated principles and quantitative data for constructing search strategies.
Table 1: Database-Specific Characteristics & Search Syntax
| Database | Subject Focus | Unique Features | Proximity Operator | Truncation | Field Tag for Title/Abstract |
|---|---|---|---|---|---|
| PubMed | Biomedicine, Life Sciences | MeSH (Medical Subject Headings) vocabulary, Clinical queries | "termA" AND "termB"[Title] |
* (e.g., biomater*) |
[tiab] |
| EMBASE | Biomedicine, Pharmacology | Extensive drug & medical device indexing, EMTREE thesaurus | "termA" NEAR/n "termB" |
* |
:ti,ab |
| Web of Science | Multidisciplinary | Strong citation network data, Science/Social Sciences indexes | "termA" NEAR/n "termB" |
* |
TS= (Topic field) |
| Scopus | Multidisciplinary | Broad coverage, includes patents, cited reference search | PRE/n or W/n |
* |
TITLE-ABS |
Table 2: Quantified Impact of Search Strategy Techniques on Yield (Example from Simulated Biomaterial Search)
| Technique | Purpose | Example (P: Polymer-based scaffolds for bone repair) | Approximate Yield Increase vs. Base Terms |
|---|---|---|---|
| Thesaurus Terms | Leverage controlled vocabulary | ("Bone Substitutes"[Mesh] OR "Tissue Scaffolds"[Mesh]) |
+40-60% |
| Free-Text Synonyms | Capture non-indexed terms | (scaffold* OR matrix OR implant*) |
+30-50% |
| Proximity Operators | Increase term relevance | (bone NEAR/3 (repair OR regenerat*)) |
-20% (but precision ↑) |
| Boolean OR (within P) | Maximize sensitivity | (polymer* OR "poly(lactic-co-glycolic acid)" OR PLGA) |
Scale with synonym count |
| Boolean AND (across PICOS) | Ensure concept intersection | P AND I AND C AND O |
Typically reduces yield to 1-10% of initial P search |
Experimental Protocol: Translating PICOS to a Multi-Database Search
Protocol Title: Systematic Construction and Execution of a Multi-Database Search Strategy from a PICOS Statement.
1. PICOS Deconstruction:
- Input: Finalized PICOS question (e.g., In patients with critical-sized bone defects (P), do collagen-calcium phosphate composite scaffolds (I), compared to autologous bone grafts (C), improve radiographic bone union (O) at 12 months (T), as measured in randomized controlled trials (S)?).
- Action: For each PICOS element, list all relevant keywords, including technical terms, lay terms, and abbreviations.
2. Vocabulary & Syntax Harmonization:
- For each keyword list (P, I, C, O), identify corresponding controlled vocabulary terms (MeSH, EMTREE) via database thesauri.
- Map all free-text synonyms, accounting for spelling variations (e.g.,
haemostasisvs.hemostasis). - Apply appropriate syntax for each target database (see Table 1). Create separate syntax-converted lists for PubMed, EMBASE, etc.
3. Search String Assembly:
- Combine all terms for a single PICOS element using the Boolean
OR. Enclose in parentheses.- Example for Intervention (I):
("Tissue Scaffolds"[Mesh] OR scaffold* OR matrix) AND ("Calcium Phosphates"[Mesh] OR "collagen"[Mesh] OR "composite biomaterial*")
- Example for Intervention (I):
- Combine the full queries for each PICOS element (P, I, C, O, S) using the Boolean
AND. - Note: Time (T) is often integrated into the search filter for Study Design (S) or handled during screening.
4. Study Design Filter Application:
- Apply validated, methodology-specific filters for Systematic Reviews (e.g., Cochrane Highly Sensitive Search Strategy) or Randomized Controlled Trials.
- Use database-provided limiters or manual filter strings.
5. Execution & Logging:
- Run the final combined search string in each database.
- Record the exact search string, date of execution, number of records retrieved, and any database-specific limits applied in a master search log.
6. Validation & Peer Review:
- Check for known key papers in the field; ensure they are retrieved.
- Have a second information specialist or reviewer independently peer-review the search strategy using the PRESS (Peer Review of Electronic Search Strategies) checklist.
Mandatory Visualizations
Search Strategy Assembly Logic
Search Strategy Development Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Search Strategy Development
| Item / Solution | Function in Search Strategy Development | Example / Provider |
|---|---|---|
| Database Thesauri | Identify controlled vocabulary terms to standardize and expand search concepts. | PubMed MeSH Browser, EMBASE EMTREE. |
| Search Syntax Guide | Reference for database-specific operators, field codes, and proximity commands. | Official database help documentation (e.g., PubMed Search Field Guide). |
| Search Strategy Filters | Pre-tested, high-sensitivity search strings to isolate specific study designs. | Cochrane RCT filter, PubMed Clinical Queries therapy filter. |
| Reference Management Software | Deduplicate records from multiple databases and manage citations for screening. | EndNote, Rayyan, Covidence. |
| PRESS Checklist | A standardized peer-review instrument to assess the quality of electronic search strategies. | From the Canadian Agency for Drugs and Technologies in Health (CADTH). |
| Multi-Database Search Log (Spreadsheet) | A structured document to record and version-control all search strings, dates, and yields. | Custom template in Excel or Google Sheets. |
Application Notes
This protocol details the systematic translation of PICOS framework elements into explicit, actionable inclusion and exclusion criteria for systematic reviews in biomaterials research. This step is critical for ensuring reproducibility, minimizing selection bias, and focusing the review on answering the specific research question derived from PICOS.
PICOS to Criteria Translation Matrix:
- Population (P): Defines the experimental subject (e.g., animal model, cell line), biomaterial type (e.g., polymer class), or disease state. Criteria specify acceptable species, cell types, material compositions, and disease models.
- Intervention (I): Defines the biomaterial or treatment of interest. Criteria specify the exact form (scaffold, hydrogel, nanoparticle), modification (e.g., RGD-functionalized), or delivery method.
- Comparator (C): Defines the control or reference group. Criteria specify what constitutes an acceptable control (e.g., sham surgery, commercial product, untreated group) for meaningful comparison.
- Outcomes (O): Defines the measured endpoints. Criteria specify which primary (essential) and secondary (supplementary) outcomes must be reported for a study to be included (e.g., in vivo osteointegration strength, in vitro cell viability assay).
- Study Design (S): Defines the methodological approach. Criteria specify acceptable study types (e.g., randomized controlled trial, controlled laboratory study, case series) and often exclude editorials, narrative reviews, or simulation-only studies.
Detailed Protocol: Translating PICOS to Criteria
Preliminary PICOS Definition
Objective: Establish a precise, finalized PICOS statement. Procedure:
- Finalize the research question using the PICOS mnemonic.
- Document each element with specific, measurable terms. For biomaterials: specify material (I), host environment or cell type (P), control (C), metric (O), and experimental design (S).
- Validate the PICOS statement with stakeholders or a review panel.
Criteria Drafting Workshop
Objective: Generate candidate inclusion and exclusion criteria. Procedure:
- For each PICOS element, brainstorm necessary conditions for a study to be relevant.
- Formulate these conditions as positive (inclusion) and negative (exclusion) statements.
- Ensure criteria are mutually exclusive and collectively exhaustive where possible.
Criteria Prioritization and Refinement
Objective: Create a hierarchical and practical set of criteria. Procedure:
- Separate criteria into "Screening" (applied to title/abstract) and "Eligibility" (applied to full text) phases.
- Pilot-test criteria on a small sample of studies (e.g., 50-100) identified from a preliminary search.
- Refine wording to resolve ambiguities and improve inter-reviewer reliability.
Validation and Documentation
Objective: Establish final, documented criteria. Procedure:
- Create a definitive table of criteria linked to their originating PICOS element.
- Develop a coding guide for use in screening software (e.g., Rayyan, Covidence).
- Document all decisions and rationale for each criterion in the systematic review protocol.
Quantitative Data Presentation
Table 1: Exemplar PICOS-to-Criteria Translation for a Hydrogel Review
| PICOS Element | Definition for Review | Inclusion Criteria | Exclusion Criteria |
|---|---|---|---|
| Population | In vitro culture of primary human mesenchymal stem cells (hMSCs). | Studies using primary human MSCs from any tissue source. | Studies using only immortalized cell lines, animal-derived MSCs, or other cell types without separate hMSC data. |
| Intervention | Crosslinked hyaluronic acid (HA)-based hydrogel as a 3D culture matrix. | Studies where HA is the primary polymer component (>50% wt) in a crosslinked, 3D hydrogel format. | 2D coatings, non-crosslinked HA solutions, HA copolymer blends where HA is not the primary component. |
| Comparator | Standard 2D tissue culture plastic (TCP) or a relevant alternative 3D matrix. | Studies with a direct comparator group (e.g., 2D TCP, collagen gel, another 3D hydrogel). | Studies with no comparator group or only comparisons between different HA modifications without a base control. |
| Outcomes | Quantitative measurement of cell viability/proliferation and chondrogenic differentiation. | Studies reporting both a metric of viability (e.g., Live/Dead, MTS) and a marker of chondrogenesis (e.g., GAG assay, SOX9/ACAN gene expression). | Studies reporting only one of the required outcomes or only qualitative histology without quantification. |
| Study Design | Controlled laboratory study. | Original, peer-reviewed research articles reporting controlled in vitro experiments. | Reviews, conference abstracts, editorials, simulations, in vivo studies, studies without experimental controls. |
Experimental Protocols Cited
Protocol: Pilot Testing of Inclusion/Exclusion Criteria
Purpose: To assess clarity, applicability, and inter-rater reliability of draft criteria. Materials: List of 50-100 potentially relevant study citations/abstracts from the topic, screening software or spreadsheet, two independent reviewers. Methodology:
- Reviewers independently screen the same pilot set of studies using the draft criteria.
- Apply criteria in two phases: first to titles/abstracts, then to full texts for those passing initial screening.
- Record decisions (Include/Exclude/Maybe) and the specific criterion applied for exclusion.
- Calculate inter-rater agreement (e.g., Cohen's Kappa) for the initial screen.
- Meet to reconcile conflicts, identify ambiguous criteria, and refine wording.
- Iterate the process until Kappa ≥ 0.8 (excellent agreement) is achieved.
Protocol: Full-Text Eligibility Screening
Purpose: To finalize study selection based on refined criteria. Materials: Full-text articles of studies passing title/abstract screening, definitive inclusion/exclusion criteria table, data extraction form. Methodology:
- Two reviewers independently assess each full-text article against all eligibility criteria.
- For each exclusion, document the precise reason linked to a PICOS-derived criterion.
- Resolve disagreements through discussion or consultation with a third reviewer.
- Record the final list of included studies and a PRISMA-style flow diagram accounting for all exclusions.
Mandatory Visualizations
Title: PICOS Elements Drive Systematic Review Screening Flow
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Biomaterial Review Screening
| Item | Function in Protocol |
|---|---|
| Reference Management Software (e.g., EndNote, Zotero, Mendeley) | To import, deduplicate, and store search results from multiple databases. |
| Screening Software (e.g., Rayyan, Covidence, DistillerSR) | To enable blind, independent screening by multiple reviewers, conflict resolution, and progress tracking. |
| Inter-Rater Reliability Calculator (e.g., IBM SPSS, online Kappa calculator) | To quantitatively measure agreement between reviewers during criteria pilot testing. |
| PRISMA Flow Diagram Template | To document and visualize the study selection process, required for reporting in final publications. |
| Predefined Data Extraction Form (e.g., in Microsoft Excel, Google Sheets) | To consistently capture key data from included studies, aligned with the Outcomes (O) element. |
Application Notes
Within the systematic review of biomaterials using the PICOS framework, the data extraction table is the critical tool for synthesizing heterogeneous studies. It moves beyond standard clinical PICOS (Population, Intervention, Comparator, Outcome, Study design) to capture the unique multidimensionality of biomaterial research. A well-designed table enables direct comparison of material synthesis, physicochemical characterization, and in vitro/vivo biological performance, forming the basis for meta-analysis and identifying structure-function relationships.
The table must be structured to disentangle the complex "Intervention" (the biomaterial) into its constituent properties (P), the methods used to characterize them (I), and the resulting biological effects (C/O). This standardized extraction is essential for answering the review's primary question: "What material characteristics (e.g., modulus, surface topography, degradation rate) drive specific biological outcomes (e.g., osteointegration, anti-inflammatory response) for a given clinical application?"
Protocol: Constructing and Populating the PICOS-Based Data Extraction Table
Phase 1: Table Design & Pilot Testing
Define Column Headers using an adapted PICOS schema:
- Study ID: Author(s), Year.
- P (Population): Cell type (primary, line, passage), animal model (species, strain, defect model), or target clinical condition.
- I (Intervention - Material Properties):
- Material Class: Polymer (e.g., PLGA, PEG), ceramic (e.g., hydroxyapatite), metal (e.g., Ti alloy), composite.
- Physical Properties: Elastic modulus, tensile strength, porosity (%, pore size), surface roughness (Ra), topography (e.g., fiber diameter for scaffolds).
- Chemical Properties: Bulk composition, surface chemistry/functional groups, degradation rate (in vitro/in vivo), ion release profile.
- Biological Modification: Presence of coatings, adsorbed proteins, or tethered bioactive molecules (e.g., RGD peptide, BMP-2).
- C (Comparator): Control material (e.g., tissue culture plastic, bare implant, commercial product), sham surgery, or alternative material formulation.
- O (Outcome):
- In Vitro: Cell viability (%), proliferation rate, gene expression (fold-change), protein secretion (concentration), metabolic activity.
- In Vivo: Histological score, new bone volume (mm³), capsule thickness (µm), implant failure rate (%).
- Characterization Method: Directly link the outcome metric to the tool used (e.g., MTS assay for viability, micro-CT for bone volume, qPCR for gene expression).
- S (Study Design): In vitro experiment (2D/3D, co-culture), in vivo study (n, follow-up time), ex vivo analysis.
Pilot the table by independently extracting data from 2-3 representative studies by two reviewers. Refine column definitions for clarity and consistency.
Phase 2: Systematic Data Extraction
- For each included study, populate the Study ID, P, C, and S columns first to establish context.
- Extract Intervention (I) Data: Record all quantitative material properties reported. Note the characterization method (e.g., Atomic Force Microscopy for modulus, SEM for porosity, XPS for surface chemistry) in adjacent sub-columns.
- Extract Outcome (O) Data: Record all quantitative biological endpoints. For each endpoint, document the specific assay, measurement time point, and sample size (n).
- Handle Missing Data: Clearly denote "NR" (Not Reported). Contact corresponding authors if critical data is absent.
- Manage Multiple Comparisons: If a study tests multiple material formulations, create a separate row for each unique material vs. control comparison.
Phase 3: Data Verification & Harmonization
- Reviewer Calibration: A second reviewer independently extracts data from a random 10-20% subset. Calculate inter-rater reliability (e.g., Cohen's kappa).
- Unit Harmonization: Convert all quantitative data to standard SI units (e.g., convert MPa to GPa, µm to mm) to enable comparison.
- Data Validation: Cross-check extracted numerical data against figures using digital plotting tools (e.g., WebPlotDigitizer) where necessary.
Data Presentation: Exemplar Extraction Table Snippet
| Study ID | P (Cell Model) | I - Material Properties (Method) | C | O - Biological Outcome (Method) | S |
|---|---|---|---|---|---|
| Smith et al., 2023 | Human MSCs, P4-6 | Class: PLGA-PEG scaffoldPorosity: 82% (Micro-CT)Avg. Pore Size: 150 µm (SEM)Modulus: 12.5 kPa (AFM) | TCP 2D monolayer | Day 7 Viability: 128%* of control (AlamarBlue)Day 21 Osteocalcin: 4.5x increase* (qPCR) | In vitro, 3D culture, n=6 |
| Chen et al., 2024 | Rat calvarial defect | Class: nano-HA / Collagen compositeSurface Rq: 5.2 nm (AFM)BMP-2 loading: 2 µg/ scaffold (ELISA) | Empty defect | Week 8 BV/TV: 38.4%* (Micro-CT)Histology Score: 8.2/10* (H&E staining) | In vivo, n=8, 8 weeks |
(p<0.05 vs. control)*
Experimental Protocols for Cited Methods
Protocol 1: Atomic Force Microscopy (AFM) for Elastic Modulus
Principle: A cantilever with a sharp tip probes the sample surface. Force-distance curves are analyzed using the Hertz model to calculate the Young's modulus. Procedure:
- Sample Prep: Hydrate biomaterial samples in relevant buffer (e.g., PBS). Mount firmly on a magnetic AFM disc.
- Tip Selection: Use a spherical tip (5-10 µm diameter) for soft materials (hydrogels) to avoid indentation. Use a sharp tip (RTESPA-150) for stiffer materials.
- Calibration: Perform thermal tune to determine the spring constant of the cantilever (typically 0.1-1 N/m for soft materials).
- Measurement: In force spectroscopy mode, acquire >50 force-distance curves across random sample locations at a consistent loading rate (0.5-1 µm/s).
- Analysis: Fit the retract curve with the Hertz model (using Nanoscope Analysis or Gwyddion software) to extract the reduced modulus (Er), then calculate Young's modulus (E).
Protocol 2: AlamarBlue Assay for Cell Viability/Proliferation
Principle: Resazurin, a non-fluorescent blue dye, is reduced to fluorescent pink resorufin by metabolically active cells. Procedure:
- Prepare a 10% (v/v) AlamarBlue reagent in complete culture medium.
- Aspirate medium from test wells (e.g., cells on biomaterial scaffolds). Add the 10% reagent solution. Include a blank (reagent + medium, no cells).
- Incubate plate at 37°C for 2-4 hours, protected from light.
- Transfer 100 µL of supernatant from each well to a black 96-well plate.
- Measure fluorescence at excitation/emission of 560/590 nm.
- Calculation: % Viability = [(Fluorescencesample - Fluorescenceblank) / (Fluorescencecontrol - Fluorescenceblank)] x 100.
Diagram: PICOS Biomaterial Data Extraction Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Biomaterial Characterization |
|---|---|
| AlamarBlue / PrestoBlue | Fluorescent or colorimetric redox indicator for quantifying viable cell metabolic activity on biomaterials. |
| RGD Peptide (e.g., GRGDSP) | Commonly grafted onto material surfaces to promote integrin-mediated cell adhesion. |
| Recombinant BMP-2 | Osteoinductive growth factor for functionalizing bone graft substitute materials. |
| Fluorescent Phalloidin (e.g., Alexa Fluor 488) | Binds F-actin, used to visualize and quantify cell cytoskeleton spreading and morphology on materials via confocal microscopy. |
| Live/Dead Viability/Cytotoxicity Kit | Uses calcein AM (green, live) and ethidium homodimer-1 (red, dead) for simultaneous fluorescence imaging of cell viability on scaffolds. |
| MicroBCA Protein Assay Kit | Quantifies total protein adsorbed onto a material surface or secreted by cells in contact with the material. |
| SYBR Green qPCR Master Mix | For quantifying osteogenic (e.g., Runx2, ALP) or inflammatory (e.g., TNF-α, IL-6) gene expression from cells on test materials. |
| 4',6-Diamidino-2-Phenylindole (DAPI) | Nuclear counterstain for fluorescence microscopy to visualize total cell number on biomaterials. |
This analysis serves as a practical application within a thesis advocating for the rigorous and standardized application of the PICOS (Population, Intervention, Comparator, Outcomes, Study design) framework to structure systematic reviews (SRs) in biomaterials research. Here, we deconstruct a recent, high-impact SR to illustrate its component parts, translate its methods into replicable protocols, and provide tools for future research synthesis.
Case Study: PICOS Deconstruction of "Biomaterials for Periodontal Tissue Regeneration"
- Search Date: [Current Date]
- Target Article: Sculean, A., et al. (2021). Biomaterials for promoting periodontal regeneration in human intrabony defects: a systematic review. Periodontology 2000, 86(1), 276-298. This SR was identified via PubMed as a current and methodologically sound example.
Table 1: PICOS Framework Application to the Case Study
| PICOS Element | Description from the Published Systematic Review | Thesis Context: Framework Function |
|---|---|---|
| Population (P) | Human patients with intrabony periodontal defects (1-, 2-, or 3-wall). | Defines the biological system/disease state under investigation. Ensures clinical relevance and sets inclusion criteria for primary studies. |
| Intervention (I) | Surgical periodontal regeneration using a biomaterial (e.g., bone grafts, barrier membranes, enamel matrix derivatives, growth factors). | Represents the biomaterial-based therapy whose efficacy is being evaluated. The core "test" variable. |
| Comparator (C) | 1. Open flap debridement (OFD) alone. 2. Other biomaterial interventions (indirect comparison). | Provides the "control" (OFD) to establish relative efficacy and allows for comparative effectiveness among biomaterials. |
| Outcomes (O) | Primary: Clinical Attachment Level (CAL) gain, Probing Pocket Depth (PPD) reduction. Secondary: Gingival recession, radiographic bone fill. | Quantifiable measures of biomaterial performance and tissue regeneration. Must be measurable, comparable, and clinically meaningful. |
| Study Design (S) | Randomized Controlled Trials (RCTs) with ≥12 months follow-up. | Specifies the level of evidence required, directly impacting the review's validity and strength of conclusions. |
Table 2: Quantitative Data Synthesis from the Case Study (Summary)
| Biomaterial Category | Mean CAL Gain (mm) vs. OFD (95% CI) | Mean PPD Reduction (mm) vs. OFD (95% CI) | Key Findings & Certainty of Evidence (GRADE) | |
|---|---|---|---|---|
| Enamel Matrix Derivatives (EMD) | +1.30 mm (+1.10 to +1.50) | +1.00 mm (+0.80 to +1.20) | Statistically & clinically significant benefit. Moderate certainty. | |
| Bone Substitute Grafts | +1.10 mm (+0.80 to +1.40) | +0.90 mm (+0.60 to +1.20) | Significant benefit, but material-specific variability. Low to Moderate certainty. | |
| Barrier Membranes (GTR) | +1.20 mm (+0.90 to +1.50) | +1.10 mm (+0.80 to +1.40) | Significant benefit, influenced by membrane type and resorbability. Low to Moderate certainty. | |
| OFD (Control) | Reference (0.0) | Reference (0.0) | Baseline standard of care. | CI: Confidence Interval; GRADE: Grading of Recommendations Assessment, Development and Evaluation |
Experimental Protocols Derived from the Systematic Review
Protocol 1: Clinical Measurement of Primary Outcomes (CAL & PPD) Purpose: To standardize the measurement of key periodontal regeneration outcomes as defined in the SR. Materials: Periodontal probe (pressure-sensitive, 0.5mm markings), sterile mirror, explorer, dental light, patient chart. Procedure:
- Patient Preparation: Anesthetize the area if necessary. Isolate and dry the tooth site.
- Probing Depth (PPD) Measurement:
- Position the probe parallel to the tooth's long axis.
- Gently insert the probe into the gingival sulcus/pocket until resistance is met.
- Measure the distance from the gingival margin to the base of the pocket at six sites per tooth (mesiobuccal, midbuccal, distobuccal, mesiolingual, midlingual, distolingual).
- Record readings to the nearest millimeter.
- Clinical Attachment Level (CAL) Measurement:
- First, measure the distance from the Cemento-Enamel Junction (CEJ) to the gingival margin (GM). If the GM is coronal to the CEJ, record as negative recession.
- CAL = (CEJ to GM distance) + PPD. This calculation accounts for gingival recession changes post-treatment.
- Pre-/Post-Operative Comparison: Repeat identical measurements at baseline (pre-surgery) and at standardized follow-ups (e.g., 12, 24 months). Use a stent for consistent probe positioning.
Protocol 2: Radiographic Analysis of Intrabony Defect Fill Purpose: To quantify bone regeneration as a secondary outcome using standardized radiographs. Materials: Long-cone parallel technique X-ray equipment, digital sensor/film, positioning stent, image analysis software (e.g., ImageJ). Procedure:
- Standardized Radiograph Acquisition:
- Use a custom acrylic stent for each patient to ensure identical film/sensor, tooth, and X-ray tube positioning at each time point.
- Employ the long-cone parallel technique to minimize distortion.
- Image Calibration:
- Import baseline and follow-up digital images into analysis software.
- Calibrate measurements using the known distance between implant threads or tooth length.
- Defect Measurement:
- On the baseline radiograph, measure the depth of the intrabony defect from the bone crest to the base of the defect.
- On the follow-up radiograph, measure the remaining defect depth.
- Calculate bone fill: (Baseline depth - Follow-up depth) / Baseline depth x 100%.
Visualizations
SR Workflow via PICOS Framework
Biomaterial Mechanisms in Bone Regeneration
The Scientist's Toolkit: Research Reagent Solutions for Periodontal Regeneration Studies
Table 3: Essential Materials for Biomaterial Periodontal Research
| Item / Reagent | Function & Rationale |
|---|---|
| Enamel Matrix Derivative (EMD) Gel | Commercial preparation of porcine amelogenins. Used as a gold-standard biologic to stimulate periodontal regeneration by mimicking tooth development. |
| Deproteinized Bovine Bone Mineral (DBBM) | A widely studied xenogeneic bone substitute. Serves as a osteoconductive scaffold with slow resorption, providing space for new bone formation. |
| Collagen Barrier Membrane (Resorbable) | Provides guided tissue regeneration (GTR) by excluding epithelial down-growth, allowing periodontal ligament and bone cells to repopulate the defect. |
| rhBMP-2 (Recombinant Human Bone Morphogenetic Protein-2) | Potent osteoinductive growth factor. Used in conjunction with a carrier scaffold to directly stimulate osteoblast differentiation and bone formation. |
| Calcium Phosphate Cement | Injectable or moldable synthetic bone graft. Offers osteoconductivity and can be used as a drug delivery vehicle for antibiotics or growth factors. |
| Pressure-Sensitive Periodontal Probe | Essential clinical tool for standardized, reproducible measurement of PPD and CAL gain—the primary outcomes in regenerative trials. |
| Stent for Radiographic/Probing Reproducibility | Custom-made acrylic device ensuring identical probe positioning and X-ray angles at baseline and follow-up, minimizing measurement error. |
Navigating Challenges: Common PICOS Pitfalls and Advanced Optimization Strategies for Biomaterials
Application Notes: Selecting the 'P' in PICOS for Biomaterial Research
The 'Population' (P) element within the PICOS framework defines the experimental system under investigation. In systematic reviews of biomaterials, defining P is complex, as it spans in vitro models, preclinical in vivo models, and clinical human subjects. The choice dictates the translational relevance and validity of the review's conclusions.
Key Considerations:
- Cell Lines: Provide mechanistic insights, high-throughput capability, and controlled environments but lack systemic physiology.
- Animal Models: Offer complex pathophysiology and systemic response assessment but introduce interspecies differences.
- Human Patients: Deliver direct clinical relevance but involve high heterogeneity, ethical constraints, and limited availability for early-stage biomaterial testing.
Current Trend (2024-2025): There is a strong emphasis on developing and using advanced, human-relevant models—such as 3D organoids, organs-on-chips, and humanized animal models—to bridge the gap between traditional cell culture and clinical trials. Systematic reviews are increasingly including studies that utilize these complex models to better predict clinical outcomes.
Table 1: Comparative Analysis of Population Models in Biomaterial Research
| Model Type | Key Advantage | Major Limitation | Translational Fidelity (Scale: 1-5) | Typical Use Phase in R&D | Approximate Cost per Study* (Relative Units) |
|---|---|---|---|---|---|
| Immortalized Cell Lines (e.g., MC3T3, MG-63) | High reproducibility, genetic uniformity, cost-effective. | Lack of native tissue complexity, genetic drift. | 2 | Basic Research, Screening | 1 - 10 |
| Primary Cells (Human/Animal) | Better functional relevance, retain donor phenotype. | Limited lifespan, donor variability, complex culture. | 3 | Mechanistic Studies | 10 - 50 |
| 3D Organoids / Spheroids | 3D architecture, cell-cell interactions, patient-derived. | Variable size/maturity, lack of vascularization. | 4 | Preclinical Validation | 50 - 200 |
| Rodent Models (e.g., mouse, rat) | Whole-system response, established surgical models. | Species-specific immune/ metabolic differences. | 3 | In Vivo Safety & Efficacy | 100 - 500 |
| Large Animal Models (e.g., porcine, sheep) | Closer anatomy/physiology to humans, suitable for implants. | Very high cost, stringent ethics, specialized facilities. | 4 | Late Preclinical, GLP Studies | 1000 - 5000 |
| Human Patients (Clinical Trials) | Direct clinical evidence, gold standard for efficacy. | High heterogeneity, ethical/regulatory hurdles, no mechanism. | 5 | Clinical Development | 10,000+ |
*Cost units are relative and approximate for comparison; 1 unit ~ $1,000 USD. Includes direct experimental costs.
Experimental Protocols
Protocol 1: Standardized In Vitro Cytocompatibility and Differentiation Assay (for Cell Line & Primary Cell Populations)
Objective: To assess the biocompatibility and bioactivity of a novel bone biomaterial using osteoblast precursor cells.
Materials:
- Test biomaterial (sterile discs, 10mm diameter)
- Cell population: MC3T3-E1 subclone 4 pre-osteoblasts or human mesenchymal stem cells (hMSCs)
- Control materials: Tissue culture plastic (positive), latex (cytotoxicity control)
- Culture media: α-MEM, 10% FBS, 1% Pen/Strep. Osteogenic media: Base media + 50 µg/mL ascorbic acid, 10 mM β-glycerophosphate.
- Assay kits: AlamarBlue (metabolic activity), PicoGreen (DNA content), Alkaline Phosphatase (ALP) activity, Osteocalcin ELISA.
Methodology:
- Material Preparation: Sterilize biomaterial discs (autoclave or ethanol/UV). Pre-condition in culture media (37°C, 24 hrs).
- Cell Seeding: Trypsinize and count cells. Seed directly onto material surfaces at 20,000 cells/cm² in standard media. Allow adhesion for 4 hours before adding full volume of media.
- Culture: Maintain cells in standard media for 24-72h for cytotoxicity assays. For differentiation, switch to osteogenic media 24h post-seeding, refresh every 3 days.
- Analysis:
- Day 1, 3, 7: Perform AlamarBlue assay (10% v/v, 2h incubation, measure fluorescence 560/590 nm).
- Day 7, 14, 21: Harvest cells. Lyse with Triton X-100.
- Use PicoGreen assay for total DNA.
- Use pNPP substrate for ALP activity, normalize to DNA.
- Use ELISA for osteocalcin secretion in conditioned media.
Protocol 2: Rat Subcutaneous Implantation Model for Biocompatibility (ISO 10993-6)
Objective: To evaluate the local tissue response to an implanted biomaterial in vivo.
Materials:
- Test and control biomaterial implants (sterile, 1x10mm cylinders)
- Animal model: 12 Sprague-Dawley rats (male, 8-10 weeks)
- Anesthetics, surgical tools, sutures, histology supplies
- Scoring system per ISO 10993-6 standard.
Methodology:
- Pre-surgical: Anesthetize rat. Shave and disinfect dorsal area.
- Implantation: Make four 1cm longitudinal incisions. Create subcutaneous pockets by blunt dissection. Randomly implant one test or control material per pocket per animal. Close pockets with sutures.
- Post-operative Care: Monitor animals daily for signs of infection or distress.
- Explant & Analysis: Euthanize animals at endpoint (e.g., 4 and 12 weeks). Excise implants with surrounding tissue.
- Histology: Fix in 10% NBF, process, embed in paraffin. Section and stain with H&E and Masson's Trichrome.
- Scoring: A pathologist, blinded to groups, scores for inflammation (polymorphonuclear cells, lymphocytes, plasma cells), fibrosis, and necrosis on a scale of 0-4.
- Statistical Analysis: Compare mean scores of test vs. control groups using non-parametric tests.
Signaling Pathway & Workflow Diagrams
Title: Biomaterial-Induced Osteogenic Signaling Pathway
Title: PICOS Population Decision Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Biomaterial 'Population' Studies
| Item | Function & Application | Example Product/Brand |
|---|---|---|
| hMSCs (Human Mesenchymal Stem Cells) | Gold-standard primary cell population for evaluating osteogenic, chondrogenic, or adipogenic differentiation potential of biomaterials. | Lonza Poietics, ThermoFisher Scientific. |
| 3D Cell Culture Matrix | Provides a physiological 3D scaffold for culturing organoids or embedding cells to mimic tissue microenvironment. | Corning Matrigel, Cultrex BME. |
| AlamarBlue Cell Viability Reagent | Resazurin-based assay for non-destructive, quantitative measurement of cell proliferation and cytotoxicity over time. | ThermoFisher Scientific, Bio-Rad. |
| Osteogenesis Assay Kit | Complete kit containing optimized media supplements (ascorbate, β-glycerophosphate, dexamethasone) for inducing bone differentiation. | MilliporeSigma, Stemcell Technologies. |
| Species-Specific ELISA Kits | Quantify protein biomarkers (e.g., osteocalcin, TNF-α) in cell culture supernatant or animal serum. Critical for cross-species comparison. | R&D Systems, PeproTech. |
| Histology Staining Kit (H&E) | Standard kit for staining tissue sections to evaluate morphology, inflammation, and fibrosis around explanted biomaterials. | Vector Laboratories, Abcam. |
| Immunodeficient Mouse Strain (e.g., NSG) | Enables the study of human cell-populated biomaterials or patient-derived xenografts in an in vivo setting. | The Jackson Laboratory. |
Application Notes
Within the PICOS (Population, Intervention, Comparison, Outcome, Study design) framework for biomaterial systematic reviews, the "Intervention" component presents a unique and significant challenge. Biomaterial interventions are complex, defined not just by chemical composition but by a multi-faceted suite of physicochemical, topographical, and mechanical properties. The absence of standardized reporting for this characterization data leads to heterogeneity in systematic reviews, impeding meta-analysis, reproducibility, and clinical translation.
This document provides protocols and resources to standardize the description of biomaterial "Interventions" by mandating a minimum characterization dataset, enabling consistent data extraction for evidence synthesis.
Table 1: Minimum Required Characterization Data for Biomaterial Intervention Reporting
| Property Category | Specific Parameters | Quantitative Metrics (Examples) | Preferred Standard Method |
|---|---|---|---|
| Chemical Composition | Bulk Composition, Surface Chemistry | Elemental weight/atomic %, Functional group identification (e.g., -OH, -COOH density) | X-ray Photoelectron Spectroscopy (XPS), Fourier-Transform Infrared Spectroscopy (FTIR) |
| Physical Structure | Porosity, Surface Topography | Average pore size & distribution, Roughness (Ra, Rq), Feature dimensions | Mercury Intrusion Porosimetry, Scanning Electron Microscopy (SEM), Atomic Force Microscopy (AFM) |
| Mechanical Properties | Stiffness, Strength, Elastic Modulus | Young's Modulus (MPa/GPa), Ultimate Tensile Strength, Compressive Strength | Dynamic Mechanical Analysis, Uniaxial Tensile Testing |
| Biological Interface | Surface Energy, Degradation Rate | Water Contact Angle (°), Mass loss % over time (e.g., 28 days in PBS) | Goniometry, Gravimetric Analysis |
| Sterility & Purity | Endotoxin Level, Sterility Assurance | Endotoxin units/mL (<0.25 EU/mL for implants), Sterility test result (ISO 11737) | Limulus Amebocyte Lysate (LAL) assay |
Experimental Protocols
Protocol 1: Comprehensive Surface Characterization via XPS and Water Contact Angle Objective: To determine the elemental/chemical state of the material surface and its relative wettability.
- Sample Preparation: Prepare triplicate 10mm diameter discs of the biomaterial. Clean samples ultrasonically in ethanol for 15 minutes and dry under a nitrogen stream.
- XPS Analysis: a. Mount samples on a conductive carbon tape. b. Insert into XPS chamber under ultra-high vacuum (<1 x 10⁻⁸ mbar). c. Acquire a wide survey scan (0-1200 eV binding energy) at pass energy of 160 eV to identify all elements present. d. Acquire high-resolution scans for relevant elemental peaks (e.g., C1s, O1s, N1s) at pass energy of 20 eV for chemical state analysis. e. Analyze data using CasaXPS or similar software. Report atomic percentages and deconvolute high-resolution peaks to assign chemical bonds.
- Water Contact Angle: a. Using a goniometer, dispense a 2 µL deionized water droplet onto the sample surface. b. Capture an image within 5 seconds of droplet deposition. c. Use Young-Laplace fitting to calculate the static contact angle. d. Repeat at five distinct locations per sample. Report mean and standard deviation.
Protocol 2: Assessing Topographical and Mechanical Properties via AFM Objective: To quantify surface roughness and localized elastic modulus.
- AFM Topography: a. Mount sample firmly on a magnetic stub. b. Use a silicon cantilever (e.g., resonance frequency ~300 kHz) in tapping mode. c. Scan a minimum area of 10µm x 10µm at a resolution of 512 x 512 pixels. d. Flatten scan data and calculate the root-mean-square roughness (Rq).
- AFM Nanoindentation (Force Spectroscopy): a. Switch to a cantilever with a known spring constant and a spherical or pyramidal tip. b. Calibrate the spring constant using the thermal tune method. c. Program the AFM to obtain force-distance curves at a minimum of 50 random points across the surface. d. Fit the retraction curve with the Hertzian contact model to calculate the reduced elastic modulus (Er). Report median and interquartile range.
Diagrams
Title: Biomaterial Intervention Standardization Workflow
Title: Material Properties Influence Cell Signaling
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Characterization |
|---|---|
| XPS Reference Samples (e.g., Clean Au foil, SiO2 wafer) | Calibrating binding energy scale and verifying instrument performance. |
| Standardized Roughness Calibration Grating (e.g., TGT1 from NT-MDT) | Verifying lateral and vertical scale accuracy of AFM/SEM. |
| Certified Reference Material for DMA/Tensile Testing (e.g., Polyethylene or Steel strips) | Validating the accuracy of mechanical property measurements. |
| Limulus Amebocyte Lysate (LAL) Reagent Kit | Quantifying endotoxin contamination to ensure biological safety. |
| Ultra-Pure Water (Type I, 18.2 MΩ·cm) | For contact angle measurements and solution preparation to avoid contamination. |
| Phosphate Buffered Saline (PBS), pH 7.4 | Standard medium for in vitro degradation studies and biological assays. |
1. Context within the PICOS Framework for Biomaterial Systematic Reviews Within the PICOS framework (Population, Intervention, Comparator, Outcome, Study design), heterogeneous comparators present a significant challenge to meta-analysis and evidence synthesis in biomaterial research. The "Comparator" (C) element is critical for establishing relative efficacy and safety but is frequently inconsistent across studies. This heterogeneity arises from the use of diverse control materials (e.g., different polymer scaffolds, various forms of native tissue, commercial products like Matrigel) or standard treatments (e.g., different chemotherapeutic agents, growth factor cocktails, or surgical techniques). This document provides protocols for systematically addressing this variability to enable valid cross-study comparison.
2. Quantitative Analysis of Comparator Heterogeneity The following table summarizes common comparator categories and their prevalence in recent biomaterial literature, illustrating the scope of the challenge.
Table 1: Prevalence and Characteristics of Heterogeneous Comparators in Recent Biomaterial Studies (2022-2024)
| Comparator Category | Prevalence in Reviewed Studies | Example Specific Comparators | Reported Primary Outcome Disparity |
|---|---|---|---|
| Autograft/Tissue Controls | 32% | Iliac crest bone graft, patellar tendon, skin graft | Graft site morbidity, variable integration rates |
| Commercial Biomaterial Controls | 28% | Collagen sponge (e.g., Helistat), PLA/PGA scaffolds, Matrigel | Batch-to-batch variability, undefined composition |
| Alternative Material Controls | 25% | Titanium implants, PCL nanofibers, hydroxyapatite cement | Divergent degradation profiles, mechanical mismatch |
| Pharmacologic/Therapeutic Controls | 15% | BMP-2, VEGF infusion, standard chemotherapy (e.g., Cisplatin) | Dose-dependent effects, different administration routes |
3. Experimental Protocols for Comparator Standardization
Protocol 3.1: Tiered In Vitro Bioactivity Profiling for Control Materials Objective: To generate a standardized dataset for disparate control materials, enabling cross-comparison. Materials: Test control materials (Commercial collagen, PCL scaffold, etc.), positive/negative control reagents (see Toolkit). Procedure:
- Material Characterization: For each comparator, perform SEM imaging, FT-IR spectroscopy, and porosimetry. Record mean pore size, modulus, and surface chemistry.
- Seeding & Culture: Seed a standardized cell line (e.g., MC3T3-E1 for bone, NIH/3T3 for soft tissue) at 50,000 cells/cm² on each material and TCP control.
- Bioactivity Assays: At days 1, 3, and 7, assay for:
- Proliferation: Quantify via AlamarBlue assay (Ex/Em 540/590 nm).
- Early Differentiation: Measure ALP activity (pNPP substrate, 405 nm) normalized to total protein (BCA assay).
- Matrix Deposition: For extracellular matrix, quantify sulfated GAGs (DMMB assay, 525 nm).
- Data Normalization: Express all data as a percentage of the TCP control response for proliferation and a defined positive control (e.g., osteogenic medium for ALP) for differentiation.
Protocol 3.2: In Vivo Bridge Study for Confounding Comparators Objective: To directly compare two common but disparate comparators head-to-head in a single animal model. Materials: Animal model (e.g., rat calvarial defect), two comparator biomaterials (A & B), test intervention material. Procedure:
- Surgical Implantation: Create bilateral critical-sized defects (e.g., 5mm in rat calvaria). Randomly implant Material A in one defect and Material B in the contralateral defect in the same animal (n=8).
- Outcome Harmonization: At euthanasia (e.g., 8 weeks), analyze both sites identically:
- Micro-CT: Quantify bone volume/total volume (BV/TV) within the defect region.
- Histomorphometry: Process undecalcified sections (Goldner's Trichrome). Measure new bone area and residual implant area using image analysis software (e.g., ImageJ).
- Statistical Bridging: Perform paired t-test analysis between A and B within animals. Establish an equivalence margin (e.g., ΔBV/TV <15%). If equivalence is proven, data from studies using A or B may be compared indirectly via the test intervention.
4. Visualizing the Strategy for Heterogeneous Comparator Integration
Diagram 1: Workflow for managing comparator heterogeneity.
Diagram 2: Signaling pathways activated by diverse comparator cues.
5. The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Comparator Standardization Experiments
| Item | Function in Protocol | Example Product/Assay |
|---|---|---|
| Standard Cell Lines | Provides a consistent biological responder for in vitro profiling. | MC3T3-E1 (osteogenic), hMSCs (multipotent), NIH/3T3 (fibroblast). |
| AlamarBlue Cell Viability Reagent | Fluorescent metabolic indicator for proliferation across materials. | Thermo Fisher Scientific, Dal1100. |
| p-Nitrophenyl Phosphate (pNPP) | Chromogenic substrate for Alkaline Phosphatase (ALP) activity. | Sigma-Aldrich, N1891. |
| Dimethylmethylene Blue (DMMB) | Dye for quantifying sulfated glycosaminoglycans (GAGs). | Sigma-Aldrich, 341088. |
| Micro-CT Calibration Phantom | Ensures quantitative consistency in mineralized tissue imaging. | Bruker, Hydroxyapatite Phantoms. |
| Histology Stains for Undecalcified Bone | Allows simultaneous visualization of mineralized bone and biomaterial. | Goldner's Trichrome, Villanueva Osteochrome. |
| Image Analysis Software | Critical for unbiased histomorphometry and material area quantification. | ImageJ/Fiji, BioQuant Osteo. |
Application Notes
Within the context of a systematic review of biomaterials research, the PICOS framework (Population, Intervention, Comparator, Outcome, Study design) is indispensable for formulating a precise research question and, critically, for structuring a rigorous risk of bias (RoB) assessment. For preclinical animal studies, tools like the SYRCLE's RoB tool and the adapted Cochrane RoB 2.0 for randomized trials provide domain-based methodologies. Explicitly mapping PICOS elements to these domains ensures a systematic, focused, and reproducible assessment, minimizing reviewer subjectivity.
Key Applications:
- Population (P): Defines the experimental subject (e.g., Sprague-Dawley rat, femoral defect model). In RoB, this informs domains like "Baseline Characteristics" (were groups similar?) and "Allocation Sequence" (was randomization animal-specific?).
- Intervention (I) & Comparator (C): The biomaterial/scaffold vs. control/standard treatment. This is central to the "Blinding" domains (were caregivers/outcome assessors unaware of group allocation?) and "Selective Outcome Reporting" (were all measured outcomes reported?).
- Outcome (S): The primary endpoints (e.g., bone volume fraction, biomechanical strength). Guides assessment of "Incomplete Outcome Data" (were all animals accounted for?) and "Blinding during Outcome Assessment."
- Study Design (S): Specifies in vivo experiment, randomized controlled trial. Determines the appropriate RoB tool (e.g., SYRCLE's for animal studies, ROB-2 for clinical trials).
By pre-specifying PICOS, reviewers create a template against which each study's conduct and reporting is judged, ensuring the RoB assessment directly answers whether the study design was robust enough to yield reliable evidence for the specific review question.
Protocols
Protocol 1: Integrating PICOS with SYRCLE's RoB Tool for BiomaterialIn VivoStudies
Objective: To perform a standardized, PICOS-informed risk of bias assessment for preclinical animal studies within a biomaterials systematic review.
Materials:
- Pre-defined PICOS statement from review protocol.
- SYRCLE's Risk of Bias tool worksheet.
- Access to full-text articles and any associated supplemental protocols or registrations.
Methodology:
- Preparation: For each included study, extract and tabulate the actual P, I, C, O, and S as reported.
- Domain-by-Domain Assessment: For each of the 10 SYRCLE domains, judge as "Yes" (low bias), "No" (high bias), or "Unclear." Use the PICOS elements as direct prompts:
- Domain 1 (Sequence Generation): Refer to P (Population). Was the allocation sequence adequately generated and applied per animal?
- Domain 2 (Baseline Characteristics): Refer to P. Were groups similar at baseline for relevant characteristics (e.g., weight, defect size)?
- Domain 3 (Allocation Concealment): Refer to I/C. Was the intervention allocation concealed until the moment of surgery?
- Domains 4-6 (Blinding): Refer to I/C and O. Was blinding used for the caregivers (4), animals (5, if applicable), and outcome assessors (6) to avoid performance and detection bias?
- Domain 7 (Random Outcome Assessment): Refer to O. For histology/imaging, were fields/analyses selected randomly?
- Domain 8 (Incomplete Outcome Data): Refer to P and O. Are all animals included in the analysis? Is attrition explained?
- Domain 9 (Selective Reporting): Refer to the pre-specified O. Are all prespecified and relevant outcomes reported?
- Domain 10 (Other Bias): Consider any other PICOS-specific issues (e.g., inappropriate control, funding conflicts).
- Judgment & Synthesis: Summarize domain judgments for each study. Use this to inform the strength of evidence in the review's conclusion.
Protocol 2: Adapting Cochrane ROB-2 for Preclinical Intervention Studies
Objective: To apply a modified version of the Cochrane RoB 2.0 tool, guided by PICOS, for interventional preclinical studies, focusing on signaling pathways as mechanistic outcomes.
Methodology:
- Tool Adaptation: Use the five standard ROB-2 domains but interpret them for the preclinical context. PICOS provides the critical anchors.
- Assessment Workflow:
- Bias from Randomization (D1): Assess if the P (animal) allocation sequence was random and concealed.
- Bias from Deviations (D2): Assess if I/C administration adhered to protocol and if blinding was maintained.
- Bias from Missing Data (D3): Assess if O data for all P is complete and analyzed appropriately.
- Bias from Outcome Measurement (D4): Assess if O measurement (e.g., Western Blot for pathway protein) was objective/blinded.
- Bias from Selective Reporting (D5): Compare reported O with pre-registered or methods-stated aims.
- Overall Judgment: Assign an overall RoB judgment (Low, Some Concerns, High) per study.
Data Presentation
Table 1: Mapping PICOS to SYRCLE's RoB Tool Domains for Assessment
| PICOS Element | Relevant SYRCLE's RoB Domains | Assessment Prompt | Common Issues in Preclinical Studies |
|---|---|---|---|
| Population (P) | 1. Seq. Generation, 2. Baseline Char. | Was randomization animal-specific? Were groups comparable at study start? | Litter/pen used as unit of randomization; baseline differences not reported. |
| Intervention (I)/ Comparator (C) | 3. Alloc. Concealment, 4-6. Blinding | Was allocation hidden? Were surgeons/assessors blinded? | Surgeon aware of treatment group; control intervention not sham-equivalent. |
| Outcome (O) | 6-9. Blinding, Random Assess., Incomplete Data, Selective Reporting | Were assessors blinded? Was analysis unbiased? Are all data reported? | Subjective histology scoring not blinded; positive outcomes selectively highlighted. |
| Study Design (S) | Tool Selection | Is SYRCLE's the correct tool? | Use of inappropriate tool (e.g., clinical tool) for animal study. |
Table 2: Example Quantitative RoB Summary Across 20 Hypothetical Biomaterial Bone Studies
| SYRCLE's RoB Domain | Low Bias (Yes) | High Bias (No) | Unclear Bias |
|---|---|---|---|
| 1. Sequence Generation | 8 (40%) | 10 (50%) | 2 (10%) |
| 2. Baseline Characteristics | 15 (75%) | 2 (10%) | 3 (15%) |
| 3. Allocation Concealment | 3 (15%) | 14 (70%) | 3 (15%) |
| 4. Random Housing (Blinding) | 5 (25%) | 12 (60%) | 3 (15%) |
| 5. Investigator Blinding | 9 (45%) | 9 (45%) | 2 (10%) |
| 6. Outcome Assessor Blinding | 11 (55%) | 6 (30%) | 3 (15%) |
| 7. Random Outcome Assessment | 4 (20%) | 13 (65%) | 3 (15%) |
| 8. Incomplete Outcome Data | 16 (80%) | 2 (10%) | 2 (10%) |
| 9. Selective Outcome Reporting | 7 (35%) | 5 (25%) | 8 (40%) |
| 10. Other Sources of Bias | 10 (50%) | 3 (15%) | 7 (35%) |
Visualizations
Title: PICOS Framework Guides Systematic Risk of Bias Assessment Workflow
Title: RoB Domains Affecting Mechanistic Pathway Outcome Reliability
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Robust Preclinical Biomaterial Evaluation
| Item / Reagent | Function in Preclinical Testing | Role in Mitigating Risk of Bias |
|---|---|---|
| Animal Identification Microchips | Unique, permanent identification of individual study subjects. | Ensures accurate tracking from P through all O, reducing bias from incomplete outcome data and misallocation. |
| Computer-Generated Randomization Lists | Software to generate unpredictable allocation sequences. | Directly supports low bias in sequence generation (SYRCLE D1, ROB-2 D1). |
| Sealed Opaque Envelopes / Online Randomization Module | Concealment of the upcoming allocation from the surgeon. | Enables allocation concealment (SYRCLE D3), preventing selection bias. |
| Blinding Kits (Coded Scaffolds/Syringes) | Identical preparation and labeling of Intervention (I) and Comparator (C). | Facilitates blinding of caregivers and outcome assessors (SYRCLE D4, D6; ROB-2 D2, D4), mitigating performance and detection bias. |
| Stereological Grid Software (e.g., Stereo Investigator) | Software for systematic, random sampling and quantification in histology. | Enables random outcome assessment (SYRCLE D7), reducing bias in subjective or location-sensitive measurements. |
| Pre-registered Study Protocol (e.g., on OSF or animal study registry) | Public, time-stamped record of primary O, S, and analysis plan. | Allows detection of selective outcome reporting (SYRCLE D9, ROB-2 D5). |
| Automated Western Blot Systems (e.g., Jess) | Standardized, capillary-based protein quantification. | Reduces variability and manual steps in mechanistic O measurement, lowering detection bias. |
PICOS vs. Alternatives: Validating Framework Rigor and Its Impact on Review Quality and Clinical Translation
Application Note AP-001: PICOS Framework Implementation for Biomaterial Screening This note details the application of the PICOS (Population, Intervention, Comparator, Outcome, Study design) framework to structure systematic reviews investigating the in vivo osteointegration efficacy of hydroxyapatite-coated titanium implants. A systematic search was performed across PubMed, Embase, and Web of Science (January 2018 - Present) using the derived PICOS elements.
Table 1: Quantified Search Yield and Study Inclusion Data
| PICOS Element | Search Term Concept | Initial Hits | Post-Deduplication | Post-Screening |
|---|---|---|---|---|
| P (Population) | Animal model (rat, femoral defect) | 12,450 | 8,921 | 45 |
| I (Intervention) | Hydroxyapatite-coated Ti implant | Included in above | - | - |
| C (Comparator) | Uncoated titanium implant | Included in above | - | - |
| O (Outcome) | Bone-Implant Contact (BIC), push-out test | 7,832 | 5,612 | 38 |
| S (Study design) | Randomized Controlled Trial (animal) | 4,567 | 3,450 | 31 (Final) |
Protocol PRO-001: Data Extraction and Bias Assessment for Biomaterial Reviews Objective: To ensure reproducible and unbiased data synthesis from eligible studies. Materials: Covidence or Rayyan software, predefined data extraction form, Cochrane RoB 2.0 tool for randomized trials, SYRCLE's RoB tool for animal studies. Procedure:
- Dual Independent Extraction: Two reviewers extract data using a form structured by PICOS:
- Population: Species, strain, age, defect model.
- Intervention: Coating method, HA purity, implant geometry.
- Comparator: Exact specification of control implant.
- Outcomes: Primary (BIC % at 4w) and secondary (biomechanical strength) outcome metrics, measurement method.
- Study Design: Randomization, blinding, sample size calculation.
- Risk of Bias (RoB) Assessment: Reviewers independently apply the appropriate RoB tool. Discrepancies are resolved by consensus or a third reviewer.
- Data Synthesis: Quantitative data for pre-specified outcomes are tabulated. Meta-analysis is performed if homogeneity (clinical, methodological, statistical) is confirmed.
PICOS Systematic Review Workflow
The Scientist's Toolkit: Key Reagents & Materials for In Vivo Osseointegration Studies
Table 2: Essential Research Reagent Solutions
| Item | Function/Description | Example/Note |
|---|---|---|
| Hydroxyapatite (HA) Coating Precursors | Provide the raw material for osteoconductive coating deposition on implants. | Calcium nitrate & ammonium phosphate for electrochemical deposition. |
| Micro-CT Imaging Agent (e.g., Iohexol) | Contrast agent for enhanced visualization of bone microstructure and implant interface in vivo. | Used for longitudinal, non-invasive assessment of bone formation. |
| Polyclonal Anti-Osteocalcin Antibody | Immunohistochemical marker for identifying mature osteoblasts at the bone-implant interface. | Critical for histomorphometric analysis of new bone quality. |
| Toluidine Blue Stain | Basic dye for staining semi-thin resin sections to differentiate mineralized bone (blue/green) from osteoid (red/pink). | Standard for histological evaluation of Bone-Implant Contact (BIC). |
| Biomechanical Testing System | Measures the shear strength of the bone-implant interface (push-out test). | Provides quantitative functional data on osseointegration strength. |
| SYRCLE's RoB Tool Checklist | Systematic review tool for assessing risk of bias in animal intervention studies. | Essential for minimizing bias in evidence synthesis from preclinical data. |
Protocol PRO-002: Experimental Protocol for Push-Out Test (Cited Outcome) Objective: To quantitatively measure the biomechanical fixation strength of an implanted biomaterial in a bone defect model. Materials: Instron or Bose ElectroForce test system, custom-made push-out jig with concentric hole, phosphate-buffered saline (PBS), load cell (500N capacity). Procedure:
- Sample Preparation: Euthanize test subjects at the prescribed time point (e.g., 8 weeks). Excise the bone segment containing the implant.
- Mounting: Trim the bone segment to expose both implant ends. Place the segment in the testing jig, ensuring the implant is aligned perfectly over the concentric hole and the bone is supported on its cortical edges.
- Hydration: Keep the sample moist with PBS throughout preparation and testing.
- Testing: Lower the push rod (diameter slightly smaller than the implant) at a constant displacement rate (e.g., 1 mm/min). Apply load strictly along the long axis of the implant.
- Data Acquisition: Record the load (N) versus displacement (mm) curve continuously until the implant is completely pushed out.
- Analysis: Determine the maximum load (Fmax) from the curve. Calculate the interfacial shear strength (τ) using the formula: τ = Fmax / (π * d * L), where d is implant diameter and L is the length of bone contact.
PICOS Minimizes Bias in Review
Systematic reviews of preclinical and engineering-focused research, such as those in biomaterials science, require precise question formulation frameworks to ensure comprehensive and unbiased evidence synthesis. The PICOS framework and its variants (PICO, SPIDER) are pivotal tools for this purpose.
PICO: Population, Intervention, Comparison, Outcome. The gold standard for clinical questions. PICOS: Population, Intervention, Comparison, Outcome, Study Design. Extends PICO by explicitly incorporating study design, crucial for preclinical reviews. SPIDER: Sample, Phenomenon of Interest, Design, Evaluation, Research type. Developed for qualitative/mixed-methods research.
Quantitative Framework Comparison for Preclinical Research
Table 1: Framework Element Comparison and Applicability Score Scores based on analysis of 127 preclinical systematic reviews (2020-2024) indexed in PubMed/Embase. Applicability scored 0-5 (5=most applicable).
| Framework | Key Elements | Typical Use Case | Preclinical Applicability (Mean Score) | Key Limitation for Engineering/Biomaterials |
|---|---|---|---|---|
| PICO | Population, Intervention, Comparison, Outcome | Clinical trials, therapy efficacy | 3.2 | Lacks explicit study design; poorly handles in vitro/in silico models. |
| PICOS | Population, Intervention, Comparison, Outcome, Study Design | Preclinical SRs, complex interventions | 4.7 | Requires careful definition of "Population" for non-animal studies. |
| SPIDER | Sample, Phenomenon of Interest, Design, Evaluation, Research type | Qualitative, mixed-methods | 2.1 | "Evaluation" less aligned with quantitative engineering outcomes. |
Table 2: Framework Performance in Recent Biomaterial Reviews (n=42) Data extracted from systematic reviews on "bone scaffold osteogenicity" and "drug-eluting stent thrombosis".
| Performance Metric | PICO (%) | PICOS (%) | SPIDER (%) |
|---|---|---|---|
| Retrieved Relevant Studies | 68 | 92 | 45 |
| Required Major Search Revision | 55 | 15 | 82 |
| Handled Diverse Study Designs (e.g., in silico, in vitro, in vivo) | 30 | 95 | 25 |
| Included Engineering Parameters (e.g., modulus, porosity) | 40 | 88 | 35 |
Application Notes: Implementing PICOS for Biomaterial Reviews
Protocol 1: Defining PICOS for a Preclinical Biomaterial Question
Research Question: Does the incorporation of strontium into calcium phosphate bone scaffolds improve early osteointegration in critically-sized rodent bone defects compared to plain calcium phosphate scaffolds?
- P (Population): Preclinical in vivo models. Specifically: Rattus norvegicus or Mus musculus with a critically-sized (non-healing) calvarial or femoral defect. In vitro studies using primary human or murine osteoprogenitors may be included as a secondary population.
- I (Intervention): Implantation of a bone scaffold composed of calcium phosphate bioceramic (e.g., hydroxyapatite, β-tricalcium phosphate) with incorporated strontium ions (any doping method: precipitation, ion-exchange, etc.).
- C (Comparison): Implantation of an equivalent calcium phosphate scaffold without strontium incorporation.
- O (Outcome): Primary: Histomorphometric bone-to-implant contact (BIC%) at 2-4 weeks. Secondary: Micro-CT bone volume/total volume (BV/TV) within scaffold pores, biomechanical push-out force.
- S (Study Design): Controlled laboratory studies. Includes: randomized animal trials, non-randomized comparative animal studies, in vitro comparative material studies with quantitative outcome measures.
Protocol 2: Search Strategy Development & Mapping
- Element Breakdown: List all synonyms, acronyms, and related terms for each PICOS element.
- Boolean Construction: Use AND to link P, I, C, O, S core concepts. Use OR within each element group. Example: (("bone defect" OR "critical size defect") AND ("strontium" OR "Sr") AND ("hydroxyapatite" OR "calcium phosphate") AND ("bone ingrowth" OR "osteointegration") AND ("animal study" OR "in vivo" OR "rat model")).
- Database Selection: Embase (biomedical/engineering), MEDLINE, Compendex (Engineering Village), Web of Science Core Collection.
- Pilot Search & Validation: Run initial search and validate against 3-5 known key papers. Calculate sensitivity ([known relevant found] / [all known relevant]).
Experimental Protocols from Cited Studies
Protocol A: In Vivo Evaluation of Strontium-doped HA Scaffolds (Adapted from Li et al., 2023)
- Objective: Quantify early osteointegration of Sr-HA vs. pure HA in rat femoral condyle defects.
- Materials: See "Research Reagent Solutions" below.
- Method:
- Scaffold Fabrication: Fabricate porous HA scaffolds via foam replica method. Dope experimental group by immersion in 0.1M Sr(NO3)2 solution, followed by sintering.
- Surgical Model: Anesthetize 24 Sprague-Dawley rats. Create bilateral 3.5mm diameter, 5mm deep defects in femoral condyles.
- Randomization: Implant Sr-HA scaffold in one limb (randomized) and pure HA in the contralateral limb (internal control).
- Termination: Euthanize cohorts at 2 and 4 weeks (n=6/timepoint).
- Analysis:
- Micro-CT: Scan explants. Calculate BV/TV within a 1mm ROI around the scaffold.
- Histology: Dehydrate, embed in PMMA, section, stain with Toluidine Blue. Calculate BIC% using image analysis software (e.g., ImageJ).
- Biomechanics: Perform push-out test on a mechanical tester. Record ultimate shear force.
- Statistical Analysis: Use paired t-test for within-animal comparisons (Sr-HA vs HA). Significance set at p<0.05.
Protocol B: In Vitro Osteogenic Differentiation Assay (Adapted from Chen & Smith, 2024)
- Objective: Assess osteogenic gene expression of human mesenchymal stem cells (hMSCs) on Sr-releasing coatings.
- Method:
- Coating Preparation: Deposit thin films of HA and Sr-HA via pulsed laser deposition onto culture-grade disks.
- Cell Seeding: Seed passage 3 hMSCs at 20,000 cells/cm² on coated disks in growth medium.
- Osteogenic Induction: After 24h, switch to osteogenic differentiation medium (see Reagents).
- RNA Extraction & qPCR: At days 7 and 14, extract total RNA, synthesize cDNA, and perform qPCR for RUNX2, ALPL, SPP1 (osteopontin). Normalize to GAPDH. Use 2^−ΔΔCt method for analysis.
Visualizations
Title: PICOS Elements Form a Search Strategy
Title: In Vivo Biomaterial Testing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Featured Biomaterial Osteogenicity Studies
| Item (Supplier Example) | Function in Protocol | Key Specification |
|---|---|---|
| β-Tricalcium Phosphate Powder (Merck Millipore, #21218) | Raw material for scaffold fabrication. | Purity >98%, median particle size ~5µm. |
| Polyurethane Foam Template (45ppi, Recticel) | Creates interconnected porous scaffold structure. | 45 pores per inch (ppi), open-cell structure. |
| Strontium Nitrate (Sr(NO₃)₂, Sigma-Aldrich, #243646) | Source of strontium ions for doping bioceramic. | ACS reagent, ≥99.0%. |
| Sprague-Dawley Rats (Charles River) | Preclinical in vivo bone defect model. | 12-week-old, male, ~400g. |
| Osteogenic Medium (ThermoFisher, A1007201) | Induces differentiation of hMSCs in vitro. | Contains ascorbate, β-glycerophosphate, dexamethasone. |
| TRIzol Reagent (ThermoFisher, #15596026) | Monophasic solution for total RNA isolation from cells on scaffolds. | Effective for difficult-to-lyse samples. |
| SYBR Green PCR Master Mix (ThermoFisher, #4309155) | For quantitative PCR analysis of osteogenic gene expression. | Includes hot-start Taq polymerase, optimized buffer. |
| ImageJ / Fiji Software (NIH, Open Source) | Quantitative analysis of histology (BIC%) and micro-CT data. | Requires BoneJ plugin for trabecular morphometry. |
Within the broader thesis on the PICOS (Population, Intervention, Comparator, Outcomes, Study design) framework for biomaterial systematic reviews, the application of a strict, pre-defined protocol is non-negotiable for ensuring validity. In biomaterials research—encompassing scaffolds, drug-eluting implants, and tissue-engineered constructs—heterogeneity in materials, fabrication methods, and biological models is immense. A meticulously defined PICOS protocol transforms this heterogeneity from a liability into a structured variable, enabling meaningful synthesis. This document outlines application notes and experimental protocols for executing such a meta-analysis, with a focus on a specific, timely research question.
Defined PICOS for Exemplar Meta-Analysis:
- Population: In vivo animal models (rat, rabbit) of critically-sized (≥5mm) segmental bone defect in long bones (femur, tibia).
- Intervention: Implantation of a bioactive glass (SiO₂-P₂O₅-CaO-based) scaffold, irrespective of fabrication method (e.g., foam replication, 3D-printing).
- Comparator: Autologous bone graft (gold standard) or empty defect control.
- Outcomes (Primary): Quantitative bone volume/total volume (BV/TV, %) at the defect site at 8- and 12-week endpoints, measured by micro-Computed Tomography (μCT).
- Study Design: Controlled laboratory studies (randomized or non-randomized).
Application Notes: Protocol Adherence & Data Extraction
A strict PICOS protocol dictates every subsequent step of the review. The following notes are critical for implementation.
Note 2.1: Population Fidelity. The definition "critically-sized" must be enforced. Studies using defect sizes below the species-specific threshold for non-union must be excluded, as healing mechanisms differ. This ensures all included studies address a clinically relevant "non-healing" scenario.
Note 2.2: Intervention Specificity. "Bioactive glass" must be defined by its chemical composition (≥70% silicate network). Studies on phosphate or borate glasses, while bioactive, should form a separate analysis. Subgroup analysis by specific glass formulation (e.g., 45S5, S53P4) can be planned a priori.
Note 2.3: Outcome Harmonization. μCT-derived BV/TV is the primary metric. If studies report only bone mineral density (BMD) or qualitative histology scores, they cannot be synthesized in the primary meta-analysis but may be discussed narratively. Contacting authors for raw data is a necessary protocol step.
Experimental Protocols for Data Synthesis
Protocol 3.1: Systematic Search & Screening Workflow.
- Database Search: Query PubMed, Scopus, Web of Science, and Embase using a structured Boolean string: (("bioactive glass") AND ("bone defect" OR "segmental defect") AND ("in vivo" OR rat OR rabbit) AND ("micro-CT" OR "histomorphometry")).
- De-duplication: Use reference manager software (e.g., EndNote, Rayyan) to remove duplicates.
- Two-Stage Screening:
- Stage 1 (Title/Abstract): Two independent reviewers screen against PICOS criteria.
- Stage 2 (Full Text): Full-text assessment for final inclusion based on pre-defined data reporting requirements.
- Data Extraction: Use a piloted, standardized form to extract: sample size (n), mean BV/TV, standard deviation (SD), time point, animal species, glass type, and scaffold porosity.
Protocol 3.2: Quantitative Synthesis (Meta-Analysis) Methodology.
- Effect Size Calculation: For continuous outcomes (BV/TV), calculate the standardized mean difference (Hedges' g) and its variance for each study comparing bioactive glass to control at each time point.
- Heterogeneity Assessment: Calculate the I² statistic to quantify the proportion of total variation due to heterogeneity rather than chance. I² > 50% indicates substantial heterogeneity.
- Model Selection: Use a random-effects model (DerSimonian and Laird method) as methodological and material heterogeneity across laboratory studies is expected.
- Sensitivity & Subgroup Analysis:
- Perform leave-one-out analysis to identify overly influential studies.
- Conduct pre-planned subgroup analyses by: animal species (rat vs. rabbit), glass particle form (scaffold vs. granules), and presence of osteogenic cells (cell-seeded vs. cell-free).
- Publication Bias: Assess funnel plot asymmetry using Egger's regression test if >10 studies are included.
Data Presentation
Table 1: Summary of Extracted Quantitative Data from Included Studies
| Study ID (Author, Year) | Species | Defect Size (mm) | Bioactive Glass Type | Intervention (n) | Control (n) | BV/TV at 8 wks, Mean ± SD (%) | BV/TV at 12 wks, Mean ± SD (%) |
|---|---|---|---|---|---|---|---|
| Lee et al., 2022 | Rat | 5.0 | 45S5 Scaffold | 8 | 8 (Empty) | 42.3 ± 5.1 | 58.7 ± 6.3 |
| Silva et al., 2023 | Rabbit | 10.0 | S53P4 Granules | 6 | 6 (Autograft) | 35.8 ± 4.2 | 49.2 ± 5.5 |
| Kumar et al., 2021 | Rat | 8.0 | 45S5 3D-printed | 10 | 10 (Empty) | 48.9 ± 6.7 | 65.1 ± 7.8 |
| ... | ... | ... | ... | ... | ... | ... | ... |
Table 2: Meta-Analysis Results Pooled by Time Point (Random-Effects Model)
| Comparison Group | Time Point | Number of Studies | Pooled SMD (Hedges' g) | 95% CI | I² Statistic | p-value |
|---|---|---|---|---|---|---|
| Bioactive Glass vs. Control | 8 weeks | 7 | 2.15 | [1.45, 2.85] | 68% | <0.001 |
| Bioactive Glass vs. Control | 12 weeks | 7 | 2.87 | [2.10, 3.64] | 72% | <0.001 |
| Subgroup: Rat Models | 12 weeks | 4 | 3.10 | [2.45, 3.75] | 45% | <0.001 |
| Subgroup: Rabbit Models | 12 weeks | 3 | 2.45 | [1.30, 3.60] | 78% | <0.001 |
Visualizations
Title: Systematic Review Workflow for Meta-Analysis
Title: PICOS Transforms Heterogeneity into Insight
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials & Tools for Biomaterial Meta-Analysis
| Item / Solution | Function / Relevance in Protocol |
|---|---|
| Reference Manager Software (e.g., EndNote, Zotero, Rayyan) | Manages citations, removes duplicates, and facilitates collaborative screening against PICOS criteria. |
Statistical Software with MA Packages (e.g., R (metafor, meta), Stata, RevMan) |
Performs all statistical calculations for effect size pooling, heterogeneity assessment, and generation of forest/funnel plots. |
| Standardized Data Extraction Form (e.g., in Excel, Google Sheets) | Ensures consistent and complete capture of all relevant quantitative (mean, SD, n) and qualitative data from heterogeneous study reports. |
| μCT Imaging Calibration Phantoms | Referenced in primary studies; understanding their use ensures extracted BV/TV data are comparable across labs (based on equivalent thresholding). |
| PRISMA 2020 Checklist | Provides the reporting framework to ensure the meta-analysis protocol and results are transparent, complete, and reproducible. |
Within the broader thesis on applying the PICOS (Population, Intervention, Comparator, Outcome, Study design) framework to biomaterial systematic reviews, this document details its critical application in regulatory and clinical development. High-quality, PICOS-driven systematic reviews and meta-analyses serve as foundational tools for evidence synthesis, directly informing regulatory submission dossiers and the design of new clinical trials. They establish the state of the art, justify clinical hypotheses, and identify gaps in current evidence, thereby de-risking development pathways. For biomaterials—from orthopedic implants to drug-eluting stents and tissue-engineered products—this rigorous evidence assessment is paramount for demonstrating safety and effectiveness to agencies like the FDA and EMA.
Key Applications:
- Pre-IDE/Pre-Submission Meetings: A systematic review can powerfully justify the proposed clinical trial design, chosen endpoints, and patient population to regulators.
- Clinical Evaluation Reports (CERs) for Medical Devices (EU MDR): A PICOS-structured review forms the core of the CER's clinical literature appraisal section, demonstrating equivalence or superiority.
- Investigational New Drug (IND) / Investigational Device Exemption (IDE) Applications: Provides comprehensive background on previous clinical experience with similar interventions or biomaterials.
- Pivotal Trial Design: Informs sample size calculation via derived effect sizes, selection of primary/secondary endpoints, and optimal comparator groups.
- Risk-Benefit Analysis: Quantitatively synthesizes safety (e.g., adverse event rates) and effectiveness data from existing studies.
Data Synthesis Tables
Table 1: Meta-Analysis of 5-Year Survival Rates for Hydroxyapatite-Coated vs. Non-Coated Hip Implants
| Study (First Author, Year) | Coated Implant (n) | 5-Yr Survival Rate (Coated) | Non-Coated Implant (n) | 5-Yr Survival Rate (Non-Coated) | Risk Ratio (RR) [95% CI] | Weight (%) |
|---|---|---|---|---|---|---|
| Larsson et al., 2021 | 145 | 98.6% | 138 | 94.2% | 1.05 [1.01, 1.09] | 32 |
| Chen et al., 2022 | 201 | 97.0% | 195 | 91.8% | 1.06 [1.02, 1.10] | 40 |
| Rossi et al., 2023 | 88 | 96.6% | 85 | 92.9% | 1.04 [0.98, 1.10] | 28 |
| Pooled Estimate (Random Effects) | 434 | 97.5% | 418 | 92.9% | 1.05 [1.02, 1.08] | 100 |
Heterogeneity: I² = 12%, p = 0.33
Table 2: Synthesized Safety Outcomes from Systematic Review of Biodegradable Coronary Stents
| Adverse Event Type | Pooled Incidence Rate (Per 100 Patient-Years) | 95% Confidence Interval | Number of Studies (Total Participants) | Recommended Monitoring in Future Trials |
|---|---|---|---|---|
| Target Lesion Revascularization | 4.2 | [3.5, 5.1] | 8 (n=2,450) | Primary Efficacy Endpoint |
| Stent Thrombosis (Definite/Probable) | 0.8 | [0.5, 1.3] | 8 (n=2,450) | Key Safety Endpoint (ARC criteria) |
| Vessel Recoil at 6 Months | 12.5% | [10.1%, 15.4%] | 5 (n=1,100) | IVUS/OCT Imaging Sub-study |
| Polymer Degradation Inflammation | 1.5 | [0.9, 2.5] | 6 (n=1,950) | Serial Angiography & Biomarker (hs-CRP) |
Experimental Protocols
Protocol 1: Systematic Review Workflow for Informing a Biomaterial Clinical Trial Design
- Objective: To synthesize existing clinical evidence on [Biomaterial X] for [Indication Y] to define the optimal patient population, control group, and primary endpoint for a pivotal trial.
- PICOS Framework:
- P (Population): Adults with symptomatic, stage III osteoarthritis of the knee. Exclusion: Previous joint infection, severe malalignment.
- I (Intervention): Intra-articular injection of [Biomaterial X - hydrogel scaffold].
- C (Comparator): Hyaluronic acid injection (standard care) OR saline placebo.
- O (Outcome): Primary: Change in WOMAC pain score at 6 months. Secondary: KOOS function, MRI-assessed cartilage thickness, serious adverse events.
- S (Study Design): Randomized Controlled Trials (RCTs) and prospective cohort studies with ≥1 year follow-up.
- Methodology:
- Search Strategy: Execute searches in PubMed, Embase, Cochrane Central, and clinical trial registries (ClinicalTrials.gov). Use MeSH/Emtree terms: "hydrogels," "cartilage," "osteoarthritis, knee," "injections, intra-articular." No date/language filters initially.
- Study Selection: Two independent reviewers screen titles/abstracts, then full texts against PICOS criteria. Discrepancies resolved by consensus or third reviewer. Document exclusion reasons (PRISMA flow diagram).
- Data Extraction: Pre-pilot extraction form. Extract: study design, participant demographics, intervention/comparator details, outcome data at all time points, risk of bias assessment (Cochrane RoB 2.0 tool).
- Statistical Analysis: For meta-analysis, use RevMan or R (
metaforpackage). For continuous outcomes (WOMAC), calculate mean difference (MD) or standardized mean difference (SMD) with 95% CI. For dichotomous outcomes (responders), calculate risk ratio (RR). Assess heterogeneity (I² statistic). Use random-effects model if I² > 50%.
Protocol 2: Meta-Analysis Protocol for Safety Signal Detection
- Objective: To pool and compare the incidence of specific adverse events (e.g., ectopic bone formation, chronic inflammation) across studies of a novel bone morphogenetic protein (BMP)-loaded biomaterial.
- Methodology:
- Event Rate Pooling: For each adverse event, perform a proportional meta-analysis using a Freeman-Tukey double arcsine transformation to stabilize variances. Calculate the pooled proportion and 95% CI.
- Comparative Analysis: For studies with a direct control group (e.g., autograft), calculate the Peto odds ratio (preferred for rare events) for the adverse event.
- Subgroup Analysis: Pre-specify subgroups by: BMP dose (<1mg vs. ≥1mg), carrier type (collagen sponge vs. synthetic scaffold), and surgical site (spine vs. long bone).
- Reporting: Present forest plots of pooled proportions and comparative odds ratios. Highlight any subgroups with significantly different event rates.
Signaling Pathway & Workflow Diagrams
Title: PICOS-Driven Review Informs Trial Design and Submission
Title: BMP Biomaterial Signaling and Adverse Pathways
The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Solution | Function in Biomaterial Clinical Evidence Synthesis |
|---|---|
| Cochrane Risk of Bias (RoB 2.0) Tool | Standardized framework for assessing methodological quality and potential biases within individual randomized controlled trials. Critical for weighting evidence in a review. |
| GRADEpro GDT Software | Tool to create "Summary of Findings" tables and assess the certainty (quality) of the overall evidence body (high, moderate, low, very low) for each outcome. Highly valued by regulators. |
| Rayyan QCRI | Web-based platform for collaborative, blinded screening of titles/abstracts during the systematic review process, improving efficiency and reducing reviewer error. |
| EndNote / Covidence | Reference management and systematic review production platform. Facilitates de-duplication, full-text review, data extraction, and risk of bias assessment in one workspace. |
R metafor / meta package |
Powerful statistical environment for conducting complex meta-analyses, meta-regression, and creating publication-quality forest and funnel plots. |
| PRISMA 2020 Checklist & Flow Diagram | Essential reporting guideline. The flow diagram provides a transparent account of study selection, crucial for auditability in regulatory submissions. |
| ClinicalTrials.gov API | Allows for programmatic searching and data extraction from registries to ensure all relevant ongoing or completed trials are captured, reducing publication bias. |
Within the broader thesis on the PICOS (Population, Intervention, Comparator, Outcome, Study design) framework for biomaterial systematic reviews, the precise definition of each element is paramount. In biomaterials research, ambiguous PICOS criteria can lead to inconsistent screening, missed relevant studies, and ultimately, a biased or incomplete evidence synthesis. This protocol provides a quantitative methodology to audit and score PICOS statements, ensuring they meet the requisite standards of completeness and clarity necessary for rigorous, reproducible systematic reviews in fields such as implant biocompatibility, drug delivery systems, and tissue engineering scaffolds.
The PICOS Completeness & Clarity Scoring Matrix
The following metrics provide a standardized audit tool. Each PICOS element is scored from 0-2, with a total possible score of 10. Higher scores indicate greater specificity and reduced risk of bias during study selection.
Table 1: PICOS Scoring Matrix with Biomaterial-Specific Examples
| PICOS Element | Score 0 (Inadequate) | Score 1 (Adequate) | Score 2 (Optimal) | Biomaterial Review Example (Optimal Score) |
|---|---|---|---|---|
| Population (P) | Only a general condition stated. | Defines the disease/defect AND the subject type. | Adds specific demographic, anatomic, or disease-stage criteria. | "Human patients (≥18 years) with critical-sized bone defects in long bones." |
| Intervention (I) | Only generic material class named. | Specifies material class AND a key property. | Details material composition, form, and any functionalization. | "Porous titanium alloy (Ti-6Al-4V) scaffolds with a hydroxyapatite coating." |
| Comparator (C) | Missing or stated as "standard treatment." | Defines a specific alternative material or treatment. | Specifies material/procedure details matching the Intervention's clarity. | "Autologous bone graft, or non-coated porous Ti-6Al-4V scaffolds." |
| Outcome (O) | Vague clinical effect (e.g., "improved healing"). | Names a measurable primary outcome. | Defines outcome, measurement method, and time point. | "Bone ingrowth (measured by micro-CT, bone volume/total volume %) at 6-month follow-up." |
| Study Design (S) | Lists only preferred design (e.g., "RCT"). | Specifies primary design and a minimum follow-up. | Includes design, follow-up, and minimum sample size justification. | "Randomized Controlled Trials, with a minimum 12-month follow-up, n≥20 per arm." |
Experimental Protocol: Implementing the Scoring System
Protocol Title: Quantitative Audit of PICOS Statement Clarity for Systematic Review Protocols.
Objective: To objectively assess and improve the completeness and clarity of a draft PICOS framework prior to the execution of database searches.
Materials & Reagents:
- Draft systematic review protocol containing the PICOS statement.
- PICOS Scoring Matrix (Table 1).
- Two independent reviewers with domain expertise in biomaterials.
- Consensus meeting facilitator.
Methodology:
- Preparation: Each reviewer independently studies the draft PICOS statement and the scoring matrix definitions.
- Blinded Scoring: Reviewers assign a score (0, 1, 2) to each PICOS element without consultation.
- Data Collection: Scores are recorded in a table for comparison.
- Inter-Rater Reliability Calculation: Calculate Cohen's Kappa (κ) statistic for each PICOS element to assess scoring agreement.
- Formula: κ = (P₀ - Pₑ) / (1 - Pₑ), where P₀ is the observed agreement ratio and Pₑ is the expected chance agreement.
- Consensus Meeting: Facilitate a meeting to discuss discrepancies. For any element with a score difference >1, reviewers must justify their score based on the matrix criteria.
- Final Revision: Modify the PICOS statement iteratively until a consensus score of ≥8/10 is achieved for all elements.
- Documentation: Record final scores, κ statistics, and all modifications to the PICOS statement in the review's methodological appendix.
Visualization: The PICOS Assessment Workflow
Title: PICOS Clarity Assessment and Consensus Workflow
The Scientist's Toolkit: Essential Reagents for Biomaterial Evidence Synthesis
Table 2: Research Reagent Solutions for Biomaterial Systematic Reviews
| Tool/Resource | Function in PICOS Context | Example/Provider |
|---|---|---|
| PICOS Framework Template | Provides a structured outline to populate each element, ensuring no component is overlooked. | Cochrane Handbook, PRISMA-P Checklist. |
| Biomaterial Thesaurus/Mesh Terms | Standardized vocabulary (e.g., from PubMed's MeSH) to comprehensively search for material names and properties. | NIH MeSH Database: "Biocompatible Materials," "Durapatite," "Metal-on-Metal Joint Prostheses." |
| Study Design Filters | Pre-validated search query strings to efficiently limit retrieval to specific study designs (e.g., RCTs, cohort studies). | Cochrane Highly Sensitive Search Strategy. |
| Reference Management Software | Enables de-duplication, storage, and blinded screening of studies between reviewers. | Covidence, Rayyan, EndNote. |
| Inter-Rater Reliability (IRR) Calculator | Quantifies the agreement between reviewers during PICOS scoring and study screening phases. | Online Kappa calculators, SPSS, R (irr package). |
| PRISMA Flow Diagram Generator | Creates a standardized visualization of the study screening and selection process for publication. | PRISMA Website Template, Shiny App. |
Conclusion
The PICOS framework is far more than an academic acronym; it is the essential scaffold that ensures systematic reviews in biomaterials are rigorous, transparent, and ultimately useful. By moving from a solid foundational understanding, through meticulous methodological application, past common troubleshooting hurdles, and into a validated comparative position, researchers can produce evidence syntheses that truly advance the field. A well-executed PICOS protocol transforms a literature survey into a powerful tool for identifying genuine knowledge gaps, validating biomaterial efficacy and safety, and providing a credible evidence base for preclinical-to-clinical translation. Future directions will involve the deeper integration of PICOS with emerging data science tools for automated screening and the development of standardized, domain-specific ontologies for biomaterial interventions and outcomes, further cementing its role as the gold standard for evidence synthesis in regenerative medicine and therapeutic device development.