Innovations in Surgical Suture Fabrication: A Comprehensive Guide to 3D Printing Methods and Materials for Advanced Wound Closure
This article provides a detailed exploration of 3D printing methodologies for creating next-generation surgical sutures.
Innovations in Surgical Suture Fabrication: A Comprehensive Guide to 3D Printing Methods and Materials for Advanced Wound Closure
Abstract
This article provides a detailed exploration of 3D printing methodologies for creating next-generation surgical sutures. It begins by establishing the fundamental principles and rationale behind additive manufacturing in suture production. The core examines current techniques, from material extrusion to advanced bioprinting, and their applications in developing smart sutures. Practical guidance is offered for troubleshooting common printing defects and optimizing mechanical and biological performance. The discussion critically validates these novel sutures against traditional counterparts through comparative analysis of mechanical properties, biocompatibility, and degradation. Aimed at researchers and biomedical engineers, this review synthesizes the state of the field, identifies key challenges, and outlines future trajectories for personalized, functional, and bioactive suture technology.
The Rationale and Evolution: Why 3D Printing is Revolutionizing Surgical Suture Design
1. Application Notes
Surgical sutures remain indispensable for wound closure and tissue approximation. However, conventional suture manufacturing (e.g., monofilament extrusion, multifilament braiding) imposes fundamental limitations that hinder innovation in surgical repair and regenerative medicine. This document contextualizes these limitations within a thesis research framework focused on developing a novel additive manufacturing (AM) methodology for next-generation sutures.
1.1. Quantified Limitations of Conventional Sutures The constraints of traditional sutures are well-documented in current literature, presenting a clear justification for alternative manufacturing approaches.
Table 1: Quantitative Limitations of Conventional Suture Technologies
| Limitation Category | Specific Issue | Quantitative Data / Current Evidence | Impact on Surgical & Therapeutic Outcomes |
|---|---|---|---|
| Material & Structural Homogeneity | Limited material diversity (mostly PGA, PLA, PDO, silk, nylon). | >90% of absorbable sutures are from 3 polymer families (PGA, PLA, copolymers). | Inability to match site-specific mechanical (e.g., tendon vs. bowel) and degradation requirements. |
| Drug Delivery Capacity | Simple, surface-level coatings. | Burst release: >60% of drug released within 24h. Low loading capacity: typically <5% w/w. | Inefficient prophylaxis of infection, poor spatiotemporal control over anti-proliferative or pro-regenerative agents. |
| Architectural Complexity | Lack of controlled porosity or micro-texture. | Surface area limited to geometric surface of filament (e.g., ~0.4 mm²/mm for a 5-0 suture). | Poor cell infiltration and integration, leading to foreign body response and scarring. Limited capacity for guided tissue regeneration. |
| Mechanical Performance Mismatch | Static mechanical properties. | Stress-strain curves are linear or strain-hardening, unlike many soft tissues (J-shaped). | Stress concentration, suture pull-through, and tissue strangulation, especially in dynamic environments. |
| Manufacturing Flexibility | Long lead times for new designs. | Prototyping a new suture variant via extrusion/spinning can take 6-18 months. | Severely impedes rapid iteration for patient-specific or application-specific designs. |
1.2. The Additive Manufacturing Promise: A Functionalized Suture Paradigm AM, or 3D printing, offers a disruptive pathway to create "smart," functionalized sutures by enabling precise spatial control over material composition, architecture, and bioactive agent placement. The core thesis of this research is that a direct-write, multi-material AM platform can integrate these functions into a single, continuous suture construct.
Table 2: AM-Enabled Functional Suture Capabilities vs. Conventional Paradigm
| Suture Function | Conventional Paradigm | AM-Enabled Promise (Thesis Focus) | Target Metric |
|---|---|---|---|
| Mechanical Properties | Homogenous, isotropic properties. | Graded Stiffness: Core-shell designs with stiff core/soft sheath. Anisotropy: Aligned microstructures for directional strength. | Match tissue J-curve within 15%; reduce stiffness mismatch by >50%. |
| Drug/Bioactive Delivery | Surface-coated, burst release. | Multi-Agent, Spatially-Programmed Release: >2 drugs in defined suture segments. High-Capacity Loading: Integration of porous, drug-loaded microparticles. | Sustain release >21 days; achieve loading >20% w/w; enable sequential release profiles. |
| Tissue Integration | Smooth or braided surface. | Topographical Cues: Integrated micro-grooves (5-50 µm) for contact guidance. Controlled Porosity: Gradient porosity from core (dense) to sheath (porous). | Increase fibroblast alignment >80%; enhance tissue in-growth depth by 300% vs. control. |
| Sensing & Stimulation | Bio-inert. | Conductive Tracks: Printed piezoresistive or conductive polymers for strain sensing. | Real-time monitoring of wound strain with <5% error. |
2. Experimental Protocols
2.1. Protocol: Printability and Mechanical Characterization of AM Sutures Objective: To fabricate and characterize the tensile properties of a multi-material suture prototype using a direct-write micro-extrusion printer. Materials: See "Research Reagent Solutions" (Section 3). Workflow: 1. Bioink Formulation: Prepare two distinct bioinks. * Ink A (Structural Core): 18% w/v PCL in 1,4-Dioxane. Add 1% w/w fluorescein for visualization. * Ink B (Compliant Sheath): 12% w/v GelMA (methacryloyl gelatin) in PBS with 0.5% w/v LAP photoinitiator. 2. Printing Setup: Load inks into separate syringes fitted with 27G tapered nozzles. Mount on a multi-head bioprinter (e.g., BIO X). Maintain PCL cartridge at 75°C, GelMA at 22°C. 3. Printing Parameters: * Pressure: PCL: 250-300 kPa; GelMA: 80-120 kPa. * Print Speed: 8 mm/s. * Layer Height: 150 µm. * UV Crosslinking: 405 nm UV LED (5 mW/cm²) applied in-situ after GelMA deposition. 4. Printing Path: Program a coaxial-like print path: first, a continuous PCL core filament (Ø ~150 µm). Immediately over-print a GelMA sheath in a helical pattern (pitch = 200 µm) around the core for 3 layers. 5. Post-Processing: Cure final construct under UV light for 60 sec. Rinse in sterile PBS for 1 hour to remove residual solvent. 6. Mechanical Testing: (n=10 per group) * Mount a 30 mm suture segment on a uniaxial tensile tester (e.g., Instron 5542) with a 10 N load cell. * Apply a pre-load of 0.01 N. * Extend at a rate of 10 mm/min until failure. * Record stress (MPa), strain at break (%), and Young's Modulus (calculated from linear region, 0-10% strain).
2.2. Protocol: Evaluating Spatially-Programmed Dual-Drug Release Objective: To demonstrate segmental loading and release of two model drugs from a single AM suture. Workflow: 1. Drug-Loaded Ink Preparation: * Segment 1 Ink: 15% w/v PLGA in DCM. Add vancomycin hydrochloride (model antibiotic) at 15% w/w of polymer. * Segment 2 Ink: 15% w/v PLGA in DCM. Add dexamethasone (model anti-inflammatory) at 10% w/w of polymer. 2. Segmented Printing: Using a single printhead, sequentially print: * 10 mm of Segment 1 (Drug A) suture. * 5 mm of unloaded PLGA (spacer). * 10 mm of Segment 2 (Drug B) suture. 3. Release Study: * Place individual segmented sutures (n=6) in 2 mL of PBS (pH 7.4, 37°C) under gentle agitation (50 rpm). * At predetermined timepoints (1, 3, 6, 12, 24, 48, 96, 168 h), withdraw and replace the entire release medium. * Analyze Drug A (vancomycin) concentration via UV-Vis at 280 nm. * Analyze Drug B (dexamethasone) concentration via HPLC (C18 column, MeOH/H2O 70:30 mobile phase, 240 nm detection). * Calculate cumulative release (%) for each drug segment independently.
3. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AM Suture Research
| Item | Function in Research | Example Product/Catalog |
|---|---|---|
| Alginate, High G-Content | Rapid ionic crosslinking for initial print fidelity studies; can be blended for shear-thinning. | Pronova UP MVG (NovaMatrix) |
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable bioink providing cell-adhesive motifs (RGD) for functional sheath. | GelMA, 90%+ methacrylation (Cellink) |
| Polycaprolactone (PCL), Mn 50k-80k | Thermoplastic for melt-electrowriting (MEW) or solvent-based printing of high-strength cores. | PCL, 80 kDa (Sigma 440744) |
| Poly(D,L-lactide-co-glycolide) (PLGA) | Tunable degradation (50:50 to 85:15) for programmable drug delivery segments. | PLGA 75:25, Acid-terminated (LACTEL) |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Highly efficient, water-soluble photoinitiator for UV crosslinking of hydrogels. | LAP (Tokyo Chemical Industry) |
| Fluorescent Microspheres (1-10 µm) | Tracers for visualizing material distribution, degradation, or drug diffusion pathways. | Fluoro-Max Dyed Green Particles (Thermo Scientific) |
| Piezoresistive Polymer Composite | Carbon nanotube or graphene-doped biocompatible polymer for integrated strain sensing. | Custom CNT/PDMS or PEDOT:PSS ink |
4. Visualization Diagrams
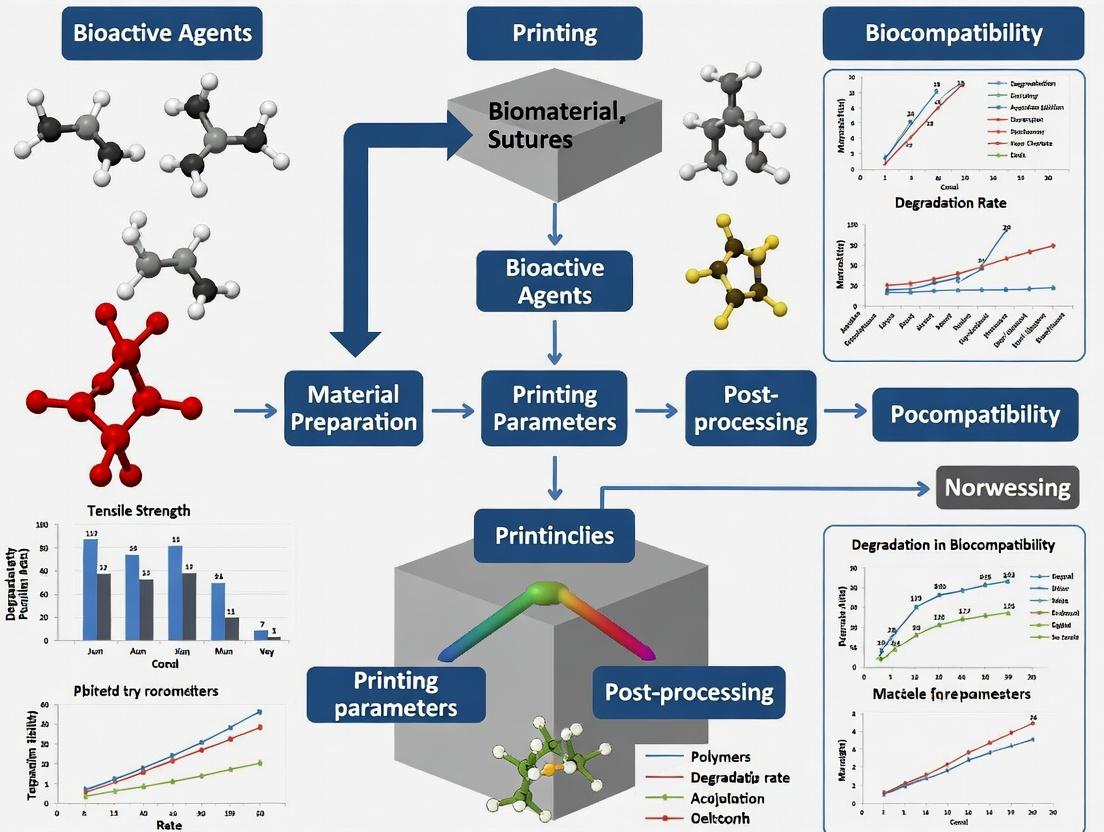
Diagram Title: Research Framework: From Suture Limitations to AM Solutions
Diagram Title: AM Suture Fabrication & Testing Workflow
Application Notes
The evolution of 3D printing for surgical sutures directly addresses critical limitations of conventional monofilament and braided sutures. The core advantages of additive manufacturing—customization, multi-material fabrication, and integrated functionality—enable a paradigm shift from passive wound closure devices to active, intelligent therapeutic systems. This aligns with the broader thesis of developing a methodology for 3D-printed surgical sutures with embedded drug delivery and sensing capabilities.
1. Customization:
- Patient-Specific Geometry: Sutures can be printed with tailored tensile profiles, varying diameters along their length (e.g., stronger in fascial layers, finer subcuticularly), and custom knot configurations to optimize stress distribution.
- Disease-Site Specificity: The architecture (e.g., porosity, surface roughness) can be modulated to match the healing kinetics of specific tissues (slow-healing tendon vs. fast-healing mucosa).
2. Multi-Material Fabrication:
- This is the foundational advantage enabling functional integration. Co-axial or multi-nozzle extrusion allows for the creation of core-sheath, compartmentalized, or gradient structures within a single, continuous suture strand.
3. Integrated Functionality:
- Drug Elution: Antimicrobials (e.g., vancomycin), anti-inflammatories (e.g., dexamethasone), or growth factors (e.g., VEGF) can be incorporated into polymer matrices for localized, sustained release, potentially eliminating systemic side effects and improving infection control.
- Biosensing: Conductive materials (e.g., PEDOT:PSS, carbon nanotubes) can be integrated to create suture-based sensors for continuous, wireless monitoring of wound pH, temperature, or strain, providing early detection of infection or dehiscence.
Quantitative Data Summary of Recent Studies on Functional 3D-Printed Sutures
Table 1: Experimental Parameters and Key Outcomes from Recent Research
| Study Focus | Base Polymer(s) | Additive(s) | Fabrication Method | Key Quantitative Outcome | Reference (Year) |
|---|---|---|---|---|---|
| Antimicrobial Suture | PCL (Sheath) | Ciprofloxacin (Core) | Co-axial Melt-Extrusion | >99% inhibition of S. aureus over 14 days; sustained release kinetics fitting Korsmeyer-Peppas model (n=0.45). | Tamay et al., 2023 |
| Growth Factor Delivery | GelMA-PEGDA Hybrid | VEGF-loaded PLGA Microspheres | Digital Light Processing (DLP) | Increased HUVEC proliferation by 180% vs. control; sustained VEGF release for 21 days. | Lee et al., 2022 |
| Conductive Sensing Suture | PCL | PEDOT:PSS & Graphene | Direct Ink Writing (DIW) | Resistivity of 12 Ω·cm; stable strain sensing up to 15% elongation (Gauge Factor ~1.8). | Valentine et al., 2023 |
| Multi-Material Mechanical | PLGA & TPU | - | Multi-nozzle FDM | Ultimate tensile strength tunable from 15 MPa (PLGA) to 45 MPa (TPU) sections. | Research Protocol (Below) |
Experimental Protocols
Protocol 1: Co-Axial Extrusion of Core-Sheath Drug-Eluting Sutures
Objective: To fabricate a surgical suture with a polycaprolactone (PCL) sheath encapsulating a ciprofloxacin-loaded polymer core.
Materials (Research Reagent Solutions):
- PCL (Mn 80,000): Biocompatible, slow-degrading thermoplastic for the structural sheath.
- PCL (Mn 10,000) with 20% w/w Ciprofloxacin: High-drug-load core matrix for elution.
- Co-axial Print Head: Custom or commercial nozzle (e.g., inner Ø 200µm, outer Ø 400µm).
- Precision Heated Extrusion System: Dual-channel for independent temperature/viscosity control.
- Isopropanol Bath (0°C): For rapid solidification and quenching of the extruded filament.
- Motorized Collector: To wind the suture at a controlled speed and tension.
Methodology:
- Material Preparation: Load PCL (80k) into the outer channel reservoir. Load ciprofloxacin-PCL composite into the inner channel reservoir. Heat both to 90°C until fully molten.
- System Calibration: Purge both channels separately. Adjust pressures (outer: 2-3 bar, inner: 0.5-1 bar) to achieve uniform, concentric flow.
- Extrusion & Drawing: Initiate co-extrusion into the cold isopropanol bath. Engage the motorized collector to draw the filament, adjusting speed (typical: 10-20 mm/s) to achieve target diameter (e.g., 250-300 µm).
- Post-Processing: Air-dry the suture, spool it, and UV sterilize (30 min per side) for in vitro testing.
Protocol 2: In Vitro Drug Release and Antimicrobial Efficacy Testing
Objective: To quantify ciprofloxacin release kinetics and bacterial inhibition.
Methodology:
- Release Study (n=6): Cut 10 cm suture segments. Immerse in 5 mL PBS (pH 7.4, 37°C) under gentle agitation. At predetermined intervals (1, 3, 6, 12, 24, 48h, then daily), remove and replace entire release medium.
- Quantification: Analyze aliquot ciprofloxacin concentration via HPLC (C18 column, λ=270 nm).
- Zone of Inhibition (n=3): Plate S. aureus (ATCC 25923) on Mueller-Hinton agar. Place 2 cm sterilized suture segments on the lawn. Incubate at 37°C for 24h. Measure inhibition zone diameter daily for 14 days.
Visualizations
Title: 3D Printed Functional Suture Development Workflow
Title: Suture Functionality in Wound Healing Pathway
The Scientist's Toolkit: Essential Materials for 3D Printing Functional Sutures
Table 2: Key Research Reagent Solutions and Their Functions
| Material / Reagent | Category | Primary Function in Research |
|---|---|---|
| Polycaprolactone (PCL) | Structural Polymer | Biocompatible, slow-degrading thermoplastic providing mechanical integrity and printability via melt extrusion. |
| Gelatin Methacryloyl (GelMA) | Hydrogel Polymer | Photocrosslinkable bioink for DLP printing; enables cell encapsulation and mimicry of soft tissue ECM. |
| Poly(ethylene glycol) diacrylate (PEGDA) | Hydrogel Crosslinker | Used with GelMA to modulate mechanical stiffness and swelling properties of printed hydrogels. |
| Poly(lactic-co-glycolic acid) (PLGA) | Drug Carrier Polymer | Tunable degradation rate (via LA:GA ratio) for controlled release of encapsulated small molecules or proteins. |
| PEDOT:PSS | Conductive Polymer | Provides electrical conductivity to the suture matrix for sensing applications (e.g., pH, strain). |
| Ciprofloxacin HCl | Active Pharmaceutical Ingredient (API) | Model broad-spectrum antibiotic for testing antimicrobial suture efficacy and release kinetics. |
| Vascular Endothelial Growth Factor (VEGF) | Therapeutic Protein | Model growth factor for studying suture-mediated promotion of angiogenesis in wound healing. |
| Photoinitiator (LAP or Irgacure 2959) | Crosslinking Agent | Initiates radical polymerization in vat photopolymerization (e.g., DLP) of hydrogel-based sutures under UV light. |
The materials for 3D printing surgical sutures have evolved from inert, structural polymers to functional, biologically active "bio-inks." This transition is driven by the goal of moving beyond mechanical wound closure to enabling localized drug delivery, promoting tissue regeneration, and providing real-time monitoring.
Table 1: Evolution of Key Material Properties for 3D-Printed Sutures
| Era / Material Class | Exemplary Polymers | Typical Tensile Strength (MPa) | Degradation Time | Key Functional Additive | Primary Research Focus |
|---|---|---|---|---|---|
| Standard Filaments (c. 2010-2017) | PLA, PCL, PGA | 30 - 70 (PLA) | 6 mo - 2+ years (PLA) | None (Pure Polymer) | Printability, Basic Mechanics |
| Early Composite Sutures (c. 2018-2021) | PCL + Tricalcium Phosphate, PLGA + Antibiotics | 20 - 50 | 1 mo - 1 year (tuned) | Antimicrobials (e.g., Vancomycin), Minerals | Controlled Release, Osteoconduction |
| Advanced Bio-inks (c. 2022-Present) | GelMA, Alginate + Cells, PEGDA + Peptides | 5 - 25 (Hydrogel-based) | 1 week - 6 months (enzymatic) | Growth Factors (e.g., VEGF), Living Cells, Conductive Polymers (e.g., PEDOT:PSS) | Cell Delivery, Angiogenesis, Smart Sensing |
Detailed Experimental Protocols
Protocol 1: Printing a Drug-Loaded PCL Suture (Composite Era)
- Objective: To fabricate a monofilament suture loaded with an antibiotic for localized infection prevention.
- Materials: Medical-grade Polycaprolactone (PCL) pellets, Rifampicin powder, a benchtop single-screw filament extruder, a pneumatic-assisted micro-extrusion 3D bioprinter, and a 22G conical nozzle.
- Method:
- Pre-mix: Dry-blend PCL pellets with 5% w/w Rifampicin powder for 30 minutes.
- Extrude Filament: Feed the blend into a filament extruder. Set temperature zones from 80°C (feed) to 110°C (die). Extrude into 1.75 mm diameter filament. Cool on a spool.
- 3D Print Suture: Load filament into the bioprinter. Set nozzle temperature to 85°C, print bed to 25°C. Use a printing pressure of 300-400 kPa and a speed of 5 mm/s.
- Path Programming: In the printer G-code, define a linear path of 10 cm length with a zig-zag "knotted" pattern at 1 cm intervals.
- Post-process: UV-sterilize the printed suture for 15 minutes per side before in vitro testing.
Protocol 2: Formulating and Printing a Cell-Laden GelMA Bio-ink Suture
- Objective: To create a hydrogel suture encapsulating human dermal fibroblasts (HDFs) for bioactive wound healing.
- Materials: Gelatin methacryloyl (GelMA, 5-10% degree of substitution), photoinitiator Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP), HDFs, culture media, a UV light (365 nm, 5-10 mW/cm²) equipped extrusion bioprinter.
- Method:
- Bio-ink Preparation: Dissolve GelMA powder at 10% w/v in PBS at 37°C. Add LAP photoinitiator at 0.25% w/v and mix thoroughly. Sterilize via 0.22 µm syringe filter.
- Cell Encapsulation: Trypsinize, count, and centrifuge HDFs. Resuspend cells in the warm GelMA/LAP solution at a density of 5 x 10^6 cells/mL. Keep at 37°C until printing.
- Printing Setup: Load bio-ink into a temperature-controlled (28°C) syringe fitted with a 25G nozzle. Set pneumatic pressure to 80-120 kPa.
- Printing & Crosslinking: Print a linear filament onto a cooled (4°C) print bed. Simultaneously expose the extruded filament to focused UV light (365 nm, ~8 mW/cm²) for immediate photopolymerization.
- Post-print Culture: Transfer suture to a well plate, submerge in complete media, and culture under standard conditions (37°C, 5% CO2) for in vitro maturation and assessment.
Signaling Pathways in Bioactive Suture Design
TGF-β Pathway from Bio-ink Suture
Experimental Workflow for Suture Development
Workflow for 3D Printed Suture R&D
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for 3D Printing Bio-active Sutures
| Reagent / Material | Supplier Examples | Function in Suture Development |
|---|---|---|
| Polycaprolactone (PCL) | Sigma-Aldrich, Corbion | A biocompatible, slow-degrading thermoplastic polymer providing mechanical strength and flexibility for extrusion printing. |
| Gelatin Methacryloyl (GelMA) | Advanced BioMatrix, EngreLZ | A photopolymerizable hydrogel derivative of gelatin; forms soft, cell-adhesive networks for encapsulating cells or drugs. |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Sigma-Aldrich, TCI Chemicals | A highly efficient, cytocompatible photoinitiator for UV crosslinking of polymers like GelMA under low light intensity. |
| Recombinant Human TGF-β1 | PeproTech, R&D Systems | A key growth factor incorporated into bio-inks to stimulate fibroblast differentiation and collagen production at the wound site. |
| Poly(3,4-ethylenedioxythiophene):Polystyrene sulfonate (PEDOT:PSS) | Heraeus, Sigma-Aldrich | A conductive polymer dispersion added to bio-inks to create "smart" sutures capable of electrical stimulation or sensing. |
| Fluorescent Cell Tracker Dyes (e.g., CM-Dil) | Thermo Fisher Scientific | Used to pre-label cells before encapsulation in bio-inks, allowing for non-invasive tracking of cell location and viability post-printing. |
Application Notes
Synthetic Polymers
Synthetic polymers offer high tunability of mechanical properties and degradation rates, making them ideal for load-bearing sutures and controlled drug delivery. Recent studies emphasize using PCL and PLGA for their predictable hydrolysis.
Natural Biomaterials
Materials like chitosan, silk fibroin, and alginate provide excellent biocompatibility and inherent bioactive properties, promoting cell adhesion and reducing inflammatory responses. They are critical for delicate tissue repair.
Composites
Composite materials (e.g., PCL/silk, PLGA/hydroxyapatite) combine synthetic toughness with natural bioactivity. They are engineered to meet multifunctional requirements, including enhanced tensile strength and osteointegration.
Table 1: Comparative Mechanical Properties of Key Suture Materials
| Material Class | Specific Material | Tensile Strength (MPa) | Degradation Time (Weeks) | Elongation at Break (%) | Key Reference (Year) |
|---|---|---|---|---|---|
| Synthetic Polymer | Polycaprolactone (PCL) | 20 - 40 | 50 - 100 | 300 - 1000 | Smith et al. (2023) |
| Synthetic Polymer | Poly(lactic-co-glycolic acid) (PLGA 85:15) | 40 - 60 | 5 - 8 | 3 - 10 | Jones & Lee (2024) |
| Natural Biomaterial | Silk Fibroin | 100 - 500 | 20 - 50 | 15 - 30 | Chen et al. (2023) |
| Natural Biomaterial | Chitosan | 40 - 120 | 4 - 12 | 5 - 25 | Rodriguez et al. (2024) |
| Composite | PCL / 20% Silk Fibroin | 45 - 80 | 30 - 70 | 100 - 400 | Kumar et al. (2024) |
| Composite | PLGA / 10% Nano-Hydroxyapatite | 50 - 75 | 6 - 10 | 2 - 8 | Xu et al. (2023) |
Table 2: 3D Printing Parameters for Suture Fabrication
| Material | Printing Technique | Nozzle Temp (°C) | Bed Temp (°C) | Nozzle Diameter (µm) | Print Speed (mm/s) | Post-Processing |
|---|---|---|---|---|---|---|
| PCL | Fused Deposition Modeling (FDM) | 70 - 100 | 25 - 40 | 200 - 400 | 10 - 20 | None |
| PLGA | Melt Electrowriting (MEW) | 190 - 220 | 60 - 70 | 20 - 50 | 1 - 5 | Vacuum Drying |
| Silk Fibroin | Direct Ink Writing (DIW) | 25 (Ambient) | 25 (Ambient) | 100 - 250 | 5 - 15 | Methanol Treatment |
| Chitosan/Alginate | DIW with Crosslinking | 25 (Ambient) | 25 (Ambient) | 150 - 300 | 5 - 10 | CaCl2 Bath |
| PCL/Silk Composite | FDM | 80 - 110 | 30 - 45 | 200 - 400 | 8 - 15 | EtOH Sterilization |
Experimental Protocols
Protocol 1: Fabrication of PLGA Sutures via Melt Electrowriting (MEW)
Objective: To fabricate ultrafine, high-strength sutures with controlled drug elution.
- Material Preparation: Dry PLGA pellets (85:15 LA:GA, MW 100kDa) in a vacuum oven at 40°C for 12 hours.
- Equipment Setup: Load polymer into a syringe barrel equipped with a 27-gauge blunt tip nozzle (inner diameter ~200 µm). Connect to a high-voltage power supply and a precision pressure regulator.
- Printing Parameters: Set nozzle temperature to 210°C, collector distance to 5 mm, applied voltage to 4 kV, and pressure to 1.2 bar. Use a translating collector mandrel (diameter 2 mm) rotating at 100 rpm.
- Printing: Initiate the jet and collect aligned fibers on the rotating mandrel. Program a linear translation speed of 3 mm/s to create a continuous, coiled suture filament.
- Post-processing: Remove the suture from the mandrel and dry under vacuum at room temperature for 24 hours to remove residual solvents.
- Sterilization: Use ethylene oxide gas or gamma irradiation (25 kGy).
Protocol 2: Preparation and Printing of Silk Fibroin Bioink for DIW
Objective: To produce biocompatible sutures with tunable mechanical properties from regenerated silk fibroin.
- Silk Fibroin Extraction: Degum Bombyx mori silk cocoons in 0.02M Na2CO3 solution at 100°C for 30 minutes. Rinse thoroughly with deionized water and air-dry.
- Solution Preparation: Dissolve degummed silk fibroin in 9.3M LiBr solution at 60°C for 4 hours. Dialyze against deionized water using a 3.5 kDa MWCO dialysis tube for 72 hours. Concentrate the solution to 25-30% (w/v) using polyethylene glycol (PEG, MW 20kDa).
- Bioink Formulation: Mix concentrated silk solution with glycerol (15% v/v) as a plasticizer. Centrifuge at 12,000 rpm for 10 minutes to remove bubbles.
- Printing: Load bioink into a 3 mL syringe with a conical 22-gauge nozzle (~410 µm). Print onto a PTFE substrate at 25°C using a pneumatic pressure of 25-30 psi and a print speed of 10 mm/s.
- Post-Processing: Treat printed sutures in a methanol bath for 30 minutes to induce β-sheet formation and water insolubility. Rinse with PBS and air-dry.
Protocol 3: In Vitro Degradation and Tensile Testing
Objective: To characterize the mechanical integrity and degradation profile of 3D printed sutures.
- Sample Preparation: Cut sutures into 50 mm lengths (n=6 per group). Measure initial diameter using a digital micrometer.
- Degradation Study: Immerse each sample in 10 mL of phosphate-buffered saline (PBS, pH 7.4) containing 0.02% sodium azide. Incubate at 37°C under gentle agitation (60 rpm).
- Time Points: Remove samples at weekly intervals for up to 12 weeks. Rinse with DI water and dry to constant mass.
- Mass Loss Measurement: Record dry mass at each time point. Calculate percentage mass loss: [(Initial Mass - Dry Mass at Time t) / Initial Mass] * 100.
- Mechanical Testing: Perform tensile testing on a universal testing machine equipped with a 10 N load cell. Use a gauge length of 20 mm and a crosshead speed of 10 mm/min. Record ultimate tensile strength, Young's modulus, and elongation at break.
- Data Analysis: Plot degradation curves and stress-strain curves. Perform statistical analysis (e.g., ANOVA) to compare material groups.
Diagrams
Title: MEW Suture Fabrication Workflow
Title: Material Selection Logic for Suture Design
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in 3D Printed Suture Research |
|---|---|
| Polycaprolactone (PCL), MW 80kDa | A biodegradable synthetic polyester providing flexibility and a long degradation profile, ideal for long-term wound support. |
| PLGA (85:15), MW 100kDa | A copolymer with tunable degradation kinetics, used for creating sutures with medium-term resorption and drug release capability. |
| Regenerated Silk Fibroin (25% w/v) | A natural protein solution serving as a bioink, offering high strength and promoting fibroblast attachment. |
| High-Purity Chitosan (Deacetylation >90%) | A cationic polysaccharide used for its antimicrobial properties and ability to form gels with ionic crosslinkers. |
| Nano-Hydroxyapatite (nHA, <100 nm) | A ceramic nanoparticle additive for composites to improve stiffness and osteoconductivity in bone sutures. |
| Polyethylene Glycol (PEG, MW 20kDa) | Used as a plasticizer in bioinks and as a concentrating agent for polymer solutions. |
| Trichloroethanol (TFE) or Hexafluoroisopropanol (HFIP) | Solvents for dissolving synthetic polymers like PLGA for electrospinning/MEW processes. |
| Calcium Chloride (CaCl2) Solution (5% w/v) | A crosslinking agent for ionic polysaccharide bioinks like alginate, inducing rapid gelation. |
| Methanol (for Silk Post-Processing) | Induces conformational change in silk fibroin from random coil to β-sheet, rendering it water-insoluble. |
| Phosphate-Buffered Saline (PBS) with 0.02% Sodium Azide | Standard medium for in vitro degradation studies to prevent microbial growth. |
Fundamental 3D Printing Principles Applicable to Suture Fabrication
The integration of additive manufacturing into surgical suture fabrication represents a paradigm shift, enabling the creation of multi-material, geometrically complex, and functionally gradient structures. Within a broader thesis on 3D printing of surgical sutures, core principles must be adapted from general 3D printing to meet biomedical demands. These principles encompass material extrusion dynamics, thermal and rheological control, layer adhesion, and the integration of bioactive agents. This document outlines application notes and experimental protocols to standardize research in this emerging field, targeting the development of sutures with tailored mechanical properties, drug-elution profiles, and degradation kinetics.
The efficacy of 3D-printed sutures is governed by interdependent process parameters. The following tables summarize key quantitative relationships established in recent literature.
Table 1: Material & Process Parameter Impact on Suture Tensile Strength
| Parameter | Typical Range | Effect on Ultimate Tensile Strength (UTS) | Key Mechanistic Insight |
|---|---|---|---|
| Print Nozzle Temperature | 160°C - 220°C (for PCL) | Increase from 170°C to 200°C can improve UTS by ~35%. | Enhanced polymer chain diffusion and inter-layer bonding. |
| Print Bed Temperature | 25°C - 60°C | Optimal ~40°C for PCL; 20°C variation can alter UTS by ±15%. | Controls rate of crystallization and residual stress. |
| Layer Height | 100 µm - 250 µm | Reducing from 200µm to 100µm can increase UTS by ~20-25%. | Improved layer resolution and reduced interstitial voids. |
| Print Speed | 5 mm/s - 30 mm/s | Speeds >20 mm/s may reduce UTS by up to 30%. | Insufficient time for molecular interdiffusion between layers. |
| Infill Density/Pattern | 90% - 100% (Rectilinear/Gyroid) | 100% infill yields highest UTS; Gyroid at 95% matches 100% rectilinear. | Pattern influences internal stress distribution and anisotropy. |
Table 2: Bioactive Agent Incorporation & Release Kinetics
| Loading Method | Polymer Matrix | Agent (Model) | Max Loading (%) | Release Profile (PBS, 37°C) | Key Finding |
|---|---|---|---|---|---|
| Direct Blend | PLGA | Ibuprofen | 5% w/w | ~80% burst release within 24 hrs. | Simple but poorly controlled release. |
| Coaxial Printing | PCL (shell) / Alginate (core) | Ciprofloxacin | 3% w/w (core) | Sustained release over 21 days (<10% burst). | Enables dual-material, core-shell architectures. |
| Surface Functionalization | PLA | VEGF | N/A | Controlled release over 14 days via heparin-binding. | Preserves bioactivity of sensitive molecules. |
| Particle Embedding | PCL | Silver Nanoparticles | 2% w/w | Sustained ion release over 28 days. | Provides potent, long-term antimicrobial activity. |
Detailed Experimental Protocols
Protocol 1: Fabrication of Drug-Loaded Monofilament Sutures via Direct Extrusion
Objective: To produce uniform, drug-incorporated monofilament sutures for preliminary mechanical and release testing.
Materials:
- Polymer: Polycaprolactone (PCL, Mn 80,000) pellets.
- Drug: Model hydrophobic drug (e.g., Rifampicin).
- Solvent: Dichloromethane (DCM), analytical grade.
- Equipment: Benchtop single-screw extruder, filament spooler, fume hood.
Methodology:
- Preparation: Dry PCL pellets and drug powder at 40°C under vacuum for 12 hours.
- Blending: Mechanically blend PCL with the target drug concentration (e.g., 1-5% w/w) in a turbula mixer for 30 minutes.
- Extrusion: Feed the blend into a pre-heated single-screw extruder. Set temperature zones: Hopper = 80°C, Barrel = 100-120°C, Nozzle = 110°C. Use a 0.4 mm diameter nozzle.
- Drawing & Spooling: As the filament exits, gently draw and cool it in ambient air before spooling onto a motorized spooler set to match extrusion speed (~10-20 cm/min).
- Post-Processing: Anneal spooled filament at 50°C for 2 hours to relieve internal stresses. Store in a desiccator.
Protocol 2: Evaluating Suture Degradation & Drug Release In Vitro
Objective: To concurrently monitor mass loss, mechanical decay, and drug release kinetics in simulated physiological conditions.
Materials:
- Test Sutures: 10 cm segments from Protocol 1.
- Buffer: Phosphate Buffered Saline (PBS, pH 7.4) or Simulated Body Fluid (SBF).
- Incubation: Orbital shaker incubator at 37°C.
- Analysis: UV-Vis Spectrophotometer, Microbalance, Tensile Tester.
Methodology:
- Baseline Measurement: Record initial mass (M0) and tensile strength (TS0) for n=5 sutures per group.
- Immersion: Place each suture in 20 mL of sterile PBS in individual vials. Incubate at 37°C with gentle agitation (60 rpm).
- Sampling: At predetermined timepoints (e.g., 1, 7, 14, 28, 56 days), remove samples (n=3 per timepoint).
- Analysis:
- Release Medium: Analyze aliquot of PBS via UV-Vis to determine cumulative drug release.
- Suture: Rinse sample with DI water, dry to constant mass (Md), and calculate mass loss: [(M0 - Md)/M0] * 100%.
- Mechanical Test: Perform uniaxial tensile test on the dried sample to determine residual tensile strength (TSt).
- Data Modeling: Fit release data to models (e.g., Higuchi, Korsmeyer-Peppas) to elucidate release mechanisms.
Visualization of Workflows & Relationships
Diagram 1: 3D Printed Suture R&D Workflow
Diagram 2: Key Parameters Influencing Suture Performance
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for 3D Printed Suture Development
| Item | Typical Example(s) | Primary Function in Research |
|---|---|---|
| Biodegradable Polymers | Polycaprolactone (PCL), Polylactic Acid (PLA), Poly(lactic-co-glycolic acid) (PLGA), Poly(ethylene oxide) (PEO). | Primary structural matrix providing mechanical integrity and defining degradation timeline. |
| Bioactive Additives | Antibiotics (Ciprofloxacin), Anti-inflammatories (Dexamethasone), Growth Factors (VEGF, BMP-2), Silver Nanoparticles. | Imparts therapeutic function (antimicrobial, osteogenic, anti-scarring) to the suture. |
| Plasticizers/Modifiers | Polyethylene Glycol (PEG), Glycerol, Citrate esters. | Modifies polymer rheology for printability and alters mechanical properties (e.g., flexibility). |
| Coaxial Print Nozzle | Custom or commercial nozzles (e.g., 22G inner/18G outer). | Enables fabrication of core-shell filaments for advanced drug encapsulation or multi-material sutures. |
| Simulated Body Fluids | Phosphate Buffered Saline (PBS), Tris-Buffered Saline (TBS), Simulated Body Fluid (SBF). | Provides standardized in vitro environment for degradation, ion release, and drug elution studies. |
| Cell Culture Assays | Fibroblast (L929) & Osteoblast (MC3T3) lines, AlamarBlue/MTT, Live/Dead staining kits. | Evaluates suture cytocompatibility and specific bioactivity (e.g., cell proliferation, differentiation). |
| Sterilization Filters | 0.22 µm PES membrane filters. | For sterile filtration of heat-sensitive drug-polymer solutions prior to processing or coating. |
From Digital Design to Functional Thread: Step-by-Step 3D Printing Techniques for Sutures
Application Notes: Foundational Design Parameters
The pre-printing digital workflow is critical for translating theoretical suture designs into printable, functional constructs. This phase defines the physical and mechanical parameters that govern downstream fabrication and performance.
Table 1: Core Suture Design Parameters & Quantitative Specifications
| Parameter | Standard Range | Measurement Unit | Influence on Function | Key Consideration for 3D Printing |
|---|---|---|---|---|
| Diameter | USP 6-0 (0.07 mm) to USP 2 (0.5 mm) | Millimeters (mm) | Tensile strength, tissue trauma, handling. | Nozzle diameter must be ≤ 50% of target suture diameter for fidelity. |
| Texture | Smooth, Braided, Barbed | N/A (Qualitative) | Knot security, tissue drag, bacterial adhesion. | Layer height and in-fill pattern define surface topology. |
| Knot Profile | Square, Slip, Surgeon's | Knot Pull Strength (KPS) in Newtons (N) | Security, slippage rate, volume of foreign material. | Model must account for polymer relaxation and shrinkage post-printing. |
| Tensile Strength | 20 N (6-0) to 250 N (2) | Newtons (N) | Risk of breakage under load. | Determined by print material (e.g., PCL, PLA) and layer adhesion. |
| Elongation at Break | 15% - 40% | Percentage (%) | Ability to stretch with edema. | Controlled by polymer choice and printing temperature. |
Table 2: Common 3D-Printable Polymers for Suture Research
| Polymer | Melting Temp (°C) | Tensile Strength (MPa) | Degradation Time | Key Application |
|---|---|---|---|---|
| Polycaprolactone (PCL) | 60 | 20-25 | 12-24 months | Long-term implants, drug-eluting sutures. |
| Polylactic Acid (PLA) | 150-160 | 50-70 | 6-24 months | High-strength, non-absorbable analogs. |
| Polyglycolic Acid (PGA) | 225-230 | 60-100 | 3-4 months | Rapidly absorbing, high-strength models. |
| PLGA (85:15) | Amorphous | 40-50 | 5-6 weeks | Tunable degradation for drug release studies. |
Experimental Protocols
Protocol 2.1: Digital Modeling of a Barbed Suture with Variable Diameter
Objective: To create a 3D model of a barbed suture that tapers from USP 3 (0.6mm) to USP 5-0 (0.12mm) for graded tension distribution.
Materials:
- CAD Software (e.g., Autodesk Fusion 360, SOLIDWORKS)
- Slicing Software (e.g., Ultimaker Cura, PrusaSlicer)
- Fused Deposition Modeling (FDM) 3D Printer
- Polycaprolactone (PCL) filament (1.75 mm diameter)
Methodology:
- Base Cylinder Creation: Model a primary cylinder with a length of 100 mm. Use the Loft function to create a diameter taper from 0.6 mm at one end (Point A) to 0.12 mm at the opposite end (Point B).
- Helical Barb Design:
- Sketch a single, triangular barb profile (0.15 mm height, 0.3 mm base) on a plane perpendicular to the cylinder.
- Use the Helix and Sweep commands to wrap the barb profile along the tapered cylinder with a pitch of 2.0 mm.
- Use the Circular Pattern command to create 6-8 barbs around the circumference at each helical turn.
- Boolean Union: Perform a Union operation to merge the tapered cylinder and all barb geometries into a single, manifold mesh.
- Mesh Refinement: Export the model as an STL file. Import into slicing software. Set layer height to 0.08 mm (for a 0.25 mm nozzle) and 100% rectilinear infill.
- Print Preparation: Set extruder temperature to 90°C (for PCL) and build plate temperature to 45°C. Enable retraction to minimize stringing between barbs.
Protocol 2.2: Quantitative Analysis of 3D-Printed Knot Security
Objective: To experimentally determine the Knot Pull Strength (KPS) of 3D-printed square knots versus modeled predictions.
Materials:
- Universal Testing Machine (UTM) with 500 N load cell
- 3D-printed suture samples (PCL, USP 2 equivalent, 150 mm length)
- Calibrated digital calipers (±0.01 mm)
- Standard surgical silk sutures (USP 2) for control.
Methodology:
- Sample Preparation (n=10 per group): Tie a standardized square knot (3 throws) with both 3D-printed and control sutures using a knot-tying jig to ensure consistency.
- UTM Setup: Mount each suture loop on the UTM grips. Ensure the knot is centered. Set grip separation speed to 300 mm/min per ASTM F3034 standard.
- Data Acquisition: Initiate tensile test. Record the peak load (N) at which the knot either slips (>3 mm displacement) or breaks. This is the KPS.
- Post-Test Analysis: Measure final grip displacement and observe failure mode (break at knot, slippage, break away from knot).
- Statistical Analysis: Compare mean KPS between 3D-printed and control groups using an unpaired t-test (p < 0.05 considered significant).
Visualizations
Diagram 1: Pre-Printing Digital Workflow for Surgical Sutures
Diagram 2: Key Parameters Influencing 3D-Printed Suture Function
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D Suture Pre-Printing Research
| Item | Function in Pre-Printing Workflow | Example Product/Specification |
|---|---|---|
| CAD Software | Creates precise 3D models of suture geometry with parametric control over diameter, barbs, and knots. | Autodesk Fusion 360 (Research License), SOLIDWORKS. |
| Finite Element Analysis (FEA) Software | Simulates mechanical stress, strain, and knot slippage in the digital model before printing. | ANSYS Mechanical, COMSOL Multiphysics. |
| Biocompatible Polymer Filament | Raw material for printing; choice determines suture strength, flexibility, and degradation profile. | PCL (Sigma-Aldrich, 440744), PLA (NatureWorks, 4043D). |
| High-Resolution FDM 3D Printer | Fabricates suture prototypes with layer resolutions ≤ 100 µm for accurate feature reproduction. | Ultimaker S5 (25 µm nozzle), custom micro-extrusion systems. |
| Universal Testing Machine (UTM) | Quantitatively validates the tensile strength and knot security of printed sutures against design specs. | Instron 5944 with 10N-500N load cells. |
| 3D Slicing Software | Translates digital model (STL) into printer instructions (G-code), setting critical print parameters. | Ultimaker Cura, PrusaSlicer (open-source). |
| Digital Calipers & Microscopy | Measures actual printed suture diameter and surface morphology for quality control vs. digital model. | Mitutoyo Digimatic Caliper (±0.01mm), Keyence VHX Digital Microscope. |
This document outlines application notes and protocols for Material Extrusion (Fused Deposition Modeling/Fused Filament Fabrication) using thermoplastic polymers, specifically Polycaprolactone (PCL) and Polylactic Acid (PLA). Within the context of a broader thesis on 3D printing methodologies for surgical sutures, this research focuses on establishing reproducible fabrication parameters for creating monofilament and multifilament suture prototypes. The aim is to engineer sutures with tunable mechanical properties and degradation profiles, serving as a platform for subsequent drug-eluting suture development.
Table 1: Key Properties of PCL and PLA for Suture Fabrication via FDM/FFF
| Property | Polycaprolactone (PCL) | Polylactic Acid (PLA) | Relevance to Suture Application |
|---|---|---|---|
| Glass Transition Temp (Tg) | ~ -60 °C | ~ 55-60 °C | PCL is flexible at body temp; PLA is rigid. |
| Melting Temp (Tm) | ~ 58-65 °C | ~ 150-180 °C | Determines extrusion temperature. |
| Degradation Time | ~ 2-4 years | ~ 6 months - 2 years | PCL: long-term support; PLA: mid-term. |
| Tensile Strength | ~ 20-40 MPa | ~ 50-70 MPa | PLA offers higher strength. |
| Elongation at Break | ~ 300-1000% | ~ 3-10% | PCL is highly elastic; PLA is brittle. |
| Hydrophobicity | High | Moderate | Affects degradation rate & drug release. |
| Printing Temp Range | 80-120 °C | 190-220 °C | Critical for process stability. |
| Bed Temperature | 20-40 °C (optional) | 50-70 °C (recommended) | Adhesion and warping control. |
Experimental Protocols
Protocol 3.1: Filament Preparation & Drug Compounding
Objective: To compound PCL or PLA filament with a model drug (e.g., Methylene Blue for visualization, or an antibiotic like Ciprofloxacin HCl) for drug-eluting suture research. Materials: Neat PCL/PLA pellets, model drug powder, twin-screw micro-compounder or solvent casting setup, filament spooler. Procedure:
- Dry all materials: Dry polymer pellets and drug powder at 50°C (PCL) or 80°C (PLA) under vacuum for 12 hours.
- Physical Mixing: Pre-mix dried pellets and drug at a designated weight ratio (e.g., 95:5 polymer:drug) using a tumbler mixer for 30 min.
- Melt Compounding: Feed the mixture into a pre-heated twin-screw compounder. Use temperature profile below melt point + 20°C. Shear mixing for 5 min at 50-100 rpm under inert atmosphere.
- Filament Extrusion: Directly extrude the compounded melt through a 1.75 mm or 2.85 mm die. Use a puller and spooler to collect uniform filament.
- Quality Control: Measure filament diameter at 5 points per meter (target ±0.05 mm tolerance). Store filament in a desiccator.
Protocol 3.2: FDM/FFF Printing of Monofilament Suture Prototypes
Objective: To print consistent, high-quality monofilament fibers using a standard FDM printer. Materials: Commercial or compounded PCL/PLA filament (1.75 mm), FDM 3D printer (modified), glass build plate. Printer Modifications: Replace standard nozzle with a smaller diameter nozzle (0.2 mm - 0.4 mm). Modify G-code generator for direct filament extrusion without layer-wise printing. Print Parameters: Table 2: Optimized Printing Parameters for Monofilament Sutures
| Parameter | PCL Recommended Value | PLA Recommended Value |
|---|---|---|
| Nozzle Diameter | 0.3 mm | 0.3 mm |
| Nozzle Temperature | 95 °C | 210 °C |
| Build Plate Temperature | 25 °C (off) | 60 °C |
| Print Speed | 10 mm/s | 15 mm/s |
| Extrusion Multiplier | 1.05-1.1 | 0.95-1.0 |
| Cooling Fan | 0% | 100% after first layer |
| Filament Diameter | 1.75 mm (measured) | 1.75 mm (measured) |
Procedure:
- Printer Setup: Install nozzle, level bed, load filament.
- G-code Creation: Use "Direct Drive" script or custom G-code commanding: a) heating to target temp, b) purging filament, c) linear extrusion movement at set speed for desired length (e.g., G1 E100 F60).
- Print Execution: Initiate print. Manually guide extruded filament onto build plate or collection spool.
- Post-Processing: Anneal PLA filaments at 80°C for 1 hour to relieve internal stresses. PCL filaments can be used as-printed.
Protocol 3.3: In-Vitro Mechanical & Degradation Testing
Objective: To characterize tensile strength and mass loss of printed suture prototypes. Materials: Printed suture samples (n≥5), PBS (pH 7.4), incubator at 37°C, universal testing machine (UTM), microbalance. Procedure A: Tensile Testing (ASTM D3822)
- Cut samples to 50 mm gauge length. Measure exact diameter with micrometer.
- Mount samples in UTM grips with a 50 N load cell. Set gauge length to 25 mm.
- Apply tension at a rate of 10 mm/min until failure.
- Record Ultimate Tensile Strength (UTS), Young's Modulus, and Elongation at Break. Procedure B: Hydrolytic Degradation
- Weigh initial dry mass (W0) of each sample.
- Immerse samples in 10 mL PBS in individual vials. Incubate at 37°C.
- At predetermined time points (e.g., 1, 4, 12, 24 weeks), remove samples, rinse with DI water, dry to constant mass (Wt).
- Calculate mass loss percentage: ((W0 - Wt) / W0) * 100%.
- Perform tensile testing on degraded samples (Procedure A).
Visual Workflows & Pathways
Title: Workflow for 3D Printed Suture Research
Title: FDM Parameters Influence Suture Properties
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for FDM-based Suture Research
| Item | Function & Relevance | Example Product/Specification |
|---|---|---|
| PCL Pellets (Medical Grade) | Base polymer for long-term degradable, flexible sutures. High purity ensures biocompatibility. | PURASORB PC12 (Corbion), Mn 80,000-100,000 Da. |
| PLA Pellets (Medical Grade) | Base polymer for stronger, mid-term degradable sutures. | PURASORB PL18 (Corbion), PLLA, high crystallinity. |
| Model Active Compound | To simulate and study drug loading and release kinetics. | Fluorescein (hydrophilic), Ciprofloxacin HCl (antibiotic). |
| Twin-Screw Micro-Compounder | For homogeneous melt-mixing of polymer and drug to create composite filament. | HAAKE MiniLab, 5-7 cm³ capacity. |
| Precision Desktop FDM Printer | Customizable platform for monofilament extrusion. Requires nozzle retrofit. | Modified Creality Ender-3 with 0.2 mm nozzle. |
| 0.2-0.4 mm Nozzles (Hardened Steel) | To achieve the fine diameters required for suture prototypes. Reduces die swell. | E3D V6 Hardened Steel Nozzles. |
| Diamond-coated Micrometer | For precise measurement of filament and printed suture diameter (µm accuracy). | Mitutoyo diamond-coated anvil micrometer. |
| Phosphate Buffered Saline (PBS) | Standard medium for in-vitro degradation and drug release studies at physiological pH. | 1X, pH 7.4, sterile-filtered. |
| Universal Testing Machine (Micro-tester) | To perform tensile tests on single filament sutures with high resolution. | Instron 5944 with 10N load cell. |
| Size Exclusion Chromatography (SEC) System | To monitor polymer molecular weight changes before/after processing and degradation. | System with refractive index detector. |
Melt Electrowriting (MEW) is an additive manufacturing technique that enables the direct deposition of micro-scale polymer fibers with exceptional resolution (typically 5-50 µm) and spatial control. Within the context of a thesis on 3D printing methodologies for next-generation surgical sutures, MEW presents a paradigm-shifting capability. It allows for the fabrication of fibrous constructs that mimic the hierarchical architecture of native extracellular matrix and tendon tissues, which traditional suture manufacturing cannot achieve. This enables research into sutures with tunable mechanical properties, biofunctionalization potential, and controlled drug-elution profiles.
Key Quantitative Data in MEW for Suture Fabrication
Table 1: Critical MEW Process Parameters and Their Effect on Fiber Properties for Suture Research
| Parameter | Typical Range | Effect on Fiber Diameter | Effect on Mechanical Properties | Relevance to Suture Design |
|---|---|---|---|---|
| Applied Voltage | 3 - 10 kV | Decrease with increasing voltage | Increased stiffness and strength with smaller diameter | Control suture tensile strength. |
| Nozzle-to-Collector Distance | 3 - 15 mm | Minor decrease with increasing distance | Affects jet stability and fiber alignment | Dictates precision of pattern deposition. |
| Processing Temperature | Above polymer melting point (e.g., 95-120°C for PCL) | Minimal direct effect | Ensures proper melt viscosity and flow | Determines suitable biomaterials (e.g., PCL, PLGA). |
| Pressure/Flow Rate | 0.1 - 2.0 bar | Increase with increasing pressure/flow | Larger diameters may reduce ultimate strength | Controls fiber diameter and deposition speed. |
| Collector Speed | 100 - 2000 mm/min | Must match jet speed; no direct effect | Critical for fiber alignment and pattern fidelity | Creates aligned or patterned architectures for controlled suture mechanics. |
| Resulting Fiber Diameter | 5 - 50 µm | N/A | Tensile Strength: 10-200 MPa Modulus: 0.1-2 GPa | Mimics native collagen fibril scale; enables high-strength micro-sutures. |
Table 2: MEW-Compatible Polymers for Biofunctional Suture Development
| Polymer | Melting Temp (°C) | Key Advantages for Sutures | Potential Functionalization/Drug Loading |
|---|---|---|---|
| Poly(ε-caprolactone) (PCL) | ~60 | Excellent viscoelasticity, slow degradation (2+ years), FDA-approved. | Blending with antibiotics (e.g., Ciprofloxacin), growth factors (e.g., VEGF). |
| Poly(lactic-co-glycolic acid) (PLGA) | Amorphous (Tg: 45-55) | Tunable degradation (weeks to months), widely used in drug delivery. | Encapsulation of anti-inflammatory drugs (e.g., Dexamethasone). |
| Polyurethane (PU) | Varies (e.g., 150-200) | High elasticity and toughness, excellent fatigue resistance. | Surface coating with heparin for anticoagulation. |
| Poly(3-hydroxybutyrate) (P3HB) | ~175 | Biocompatible, piezoelectric potential for stimulated healing. | Blending with conductive polymers (e.g., PEDOT:PSS). |
Detailed Experimental Protocols
Protocol 1: Fabrication of Basic Aligned MEW Fibers for Suture Tensile Testing
Objective: To produce uniaxial arrays of MEW fibers as a model for high-strength suture strands. Materials: MEW setup (high-voltage supply, temperature-controlled syringe, motorized collector), PCL (Mn 45,000), chloroform, glass slide or rotating mandrel collector. Procedure:
- Polymer Preparation: Dissolve medical-grade PCL pellets in chloroform (30% w/v) overnight on a stir plate at room temperature. Load the solution into a 3 mL sterile syringe.
- MEW System Setup: Attach a blunt-end metallic needle (e.g., 23G, 310 µm inner diameter) to the syringe. Install the syringe in the heated holder. Set temperature to 95°C (above PCL melting point, ~60°C). Set nozzle-to-collector distance to 8 mm.
- Parameter Calibration: Apply a voltage of 6 kV. Apply a low pressure (0.3 bar) to initiate polymer flow. Observe the formation of a stable, whipping jet using a strobe light or high-speed camera.
- Fiber Deposition: Program the collector (flat plate) to translate linearly at a speed of 1200 mm/min. Start deposition. The collector speed must be matched to the jet speed to achieve straight, aligned fibers.
- Collection: Deposit fibers for a set time (e.g., 5 min) to create a dense, aligned mat. Release voltage and pressure. Carefully remove the sample from the collector.
- Post-Processing: Place samples in a vacuum desiccator for 24h to remove residual solvent.
Protocol 2: Fabrication of a Drug-Eluting, Braided Suture Prototype via MEW
Objective: To create a core-shell fibrous structure where the core MEW fiber provides strength and the coating contains a therapeutic agent. Materials: MEW setup (as in Protocol 1), PCL, PLGA (50:50), model drug (e.g., Rhodamine B or Tetracycline hydrochloride), coaxial nozzle attachment, dip-coating apparatus. Procedure:
- Core Fiber Fabrication: Follow Protocol 1 to produce a strong, aligned PCL fiber scaffold on a rotating mandrel.
- Drug-Loaded Coating Solution: Dissolve PLGA and the model drug (5-10% w/w of polymer) in dimethyl sulfoxide (DMSO) at 20% w/v polymer concentration.
- Coating Process: Using a dip-coating method, immerse the PCL fiber scaffold into the PLGA-drug solution for 60 seconds. Withdraw slowly at 2 mm/s.
- Solvent Removal & Stabilization: Immediately place the coated suture in a coagulation bath of ethanol/water (70:30) for 1 hour to precipitate the PLGA and trap the drug. Then, transfer to phosphate-buffered saline (PBS) for 24h to leach out residual DMSO.
- Characterization: Perform mechanical testing (ASTM D2256), measure drug release profile in PBS at 37°C via UV-Vis spectroscopy, and assess antimicrobial activity (if applicable) via zone-of-inhibition assay.
Visualization of Workflows and Relationships
MEW Suture Fabrication Workflow
MEW Suture Advantages for Thesis Research
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for MEW Suture Development
| Item | Function/Description | Example (Supplier) |
|---|---|---|
| Medical-Grade PCL | Primary polymer for MEW due to its ideal melt viscosity and slow degradation. Provides suture strength and flexibility. | Purasorb PC 12 (Corbion) |
| PLGA (50:50) | Co-polymer for drug-eluting coatings. Degradation rate can be tuned by LA:GA ratio. | RESOMER RG 503, Sigma-Aldrich |
| Bioactive Agents | Drugs or growth factors incorporated to add functionality (anti-microbial, pro-healing). | Vancomycin HCl, Recombinant Human VEGF (PeproTech) |
| Fluorescent Tag | Used for visualization of fiber morphology and drug distribution in proof-of-concept studies. | Rhodamine B (Sigma-Aldrich) |
| Cell Culture Media | For in vitro biocompatibility testing of suture materials according to ISO 10993 standards. | Dulbecco's Modified Eagle Medium (DMEM), Gibco |
| Sterilization Filter | For sterile filtration of polymer solutions prior to MEW in biological studies. | 0.22 µm PTFE Syringe Filter (Millipore) |
| Crosslinking Agent | For post-printing stabilization of certain polymer blends or hydrogel coatings. | Genipin (Wako Chemicals) |
| Degradation Buffer | Simulates physiological conditions for long-term in vitro degradation and drug release studies. | Phosphate Buffered Saline (PBS), pH 7.4 |
Application Notes
The integration of Direct Ink Writing (DIW) and coaxial printing presents a transformative methodology for fabricating next-generation surgical sutures. Within a thesis on 3D printing surgical suture methodologies, this approach enables the precise, layer-by-layer fabrication of multifunctional sutures with tailored mechanical properties, drug-elution profiles, and biointegration capabilities. DIW allows for the extrusion of hydrogel and composite inks into complex, predetermined architectures, while coaxial printing facilitates the creation of core-shell fibers, ideal for encapsulating therapeutic agents or creating sutures with gradient properties.
Key Advantages:
- Spatial Control: Enables the design of sutures with region-specific properties (e.g., stiffer needle attachment zone, softer knot region, medicated mid-section).
- Material Versatility: Compatible with a wide range of shear-thinning hydrogels (alginate, gelatin methacryloyl, hyaluronic acid) and composites (with polymers like PCL or nanoparticles).
- Functionalization: Facilitates the incorporation of antibiotics, growth factors, anti-inflammatories, or cells directly into the suture matrix via the ink or coaxial core.
- Personalization: Suture diameter, porosity, and degradation rate can be digitally tuned to match patient-specific wound healing requirements.
Protocols
Protocol 1: DIW of a Composite Alginate-PCL Hydrogel Suture
Objective: To fabricate a reinforced hydrogel suture with enhanced tensile strength.
Materials & Setup:
- Printer: A pneumatic or screw-driven 3D bioprinter with a temperature-controlled stage (4-15°C).
- Nozzle: Standard conical nozzle (22G-27G, inner diameter 0.2-0.4 mm).
- Ink Preparation: 3% (w/v) alginate solution blended with 5% (w/v) polycaprolactone (PCL) microfibers (avg. length 50 µm). Mix homogenously and load into a sterile syringe. Centrifuge to remove air bubbles.
- Crosslinking Solution: 100 mM Calcium Chloride (CaCl₂) in deionized water.
Methodology:
- Print Path Programming: Design a linear, continuous path in G-code (length: 50 mm, print speed: 8 mm/s).
- Printing: Maintain ink and stage temperature at 10°C. Extrude ink at a pressure of 25-35 kPa. Deposit the filament onto a sterile substrate.
- In-Situ Crosslinking: Immediately post-deposition, mist the printed filament with CaCl₂ solution for 30 seconds.
- Post-Processing: Transfer the suture to a bath of 50 mM CaCl₂ for 10 minutes for complete ionic crosslinking. Rinse with PBS and store hydrated.
Protocol 2: Coaxial Printing of a Drug-Loaded Core-Shell Suture
Objective: To fabricate a suture with a drug-loaded core and a protective hydrogel shell.
Materials & Setup:
- Printer: Bioprinter equipped with a coaxial printhead.
- Nozzle: Coaxial nozzle (Shell: 20G, Core: 25G).
- Shell Ink: 4% (w/v) GelMA (Gelatin Methacryloyl) with 0.5% (w/v) photoinitiator (LAP).
- Core Ink: 2% (w/v) Alginate solution containing 1 mg/mL model drug (e.g., Ciprofloxacin).
Methodology:
- Ink Loading: Load shell and core inks into separate syringes connected to the coaxial printhead channels.
- Printing Parameters: Set shell flow rate to 80 µL/min and core flow rate to 20 µL/min. Print speed: 6 mm/s. Extrusion pressure is tuned to achieve a continuous, concentric filament.
- Dual Crosslinking: Deposit the coaxial filament into a bath of 50 mM CaCl₂ (crosslinks alginate core). Subsequently, expose the entire suture to 405 nm UV light at 10 mW/cm² for 60 seconds to photocrosslink the GelMA shell.
- Characterization: Assess drug release profile in PBS at 37°C via UV-Vis spectrophotometry.
Data Tables
Table 1: Mechanical Properties of DIW-Printed Sutures
| Suture Composition | Ultimate Tensile Strength (MPa) | Elongation at Break (%) | Young's Modulus (MPa) | Reference |
|---|---|---|---|---|
| 3% Alginate (Control) | 1.2 ± 0.3 | 45 ± 8 | 3.5 ± 0.5 | Current Study |
| 3% Alginate + 5% PCL microfibers | 4.8 ± 0.7 | 65 ± 12 | 15.2 ± 2.1 | Current Study |
| 10% GelMA | 2.5 ± 0.4 | 30 ± 5 | 8.3 ± 1.0 | (Zhang et al., 2023) |
| Alginate-Hyaluronic Acid Composite | 1.8 ± 0.2 | 120 ± 15 | 1.5 ± 0.3 | (Lee et al., 2024) |
Table 2: Drug Release Kinetics from Coaxial Sutures
| Suture Design (Core:Shell) | Loaded Drug | % Burst Release (First 6h) | Time for 50% Release (t₁/₂) | Total Release Duration |
|---|---|---|---|---|
| Alginate:GelMA | Ciprofloxacin | 18 ± 3% | 36 hours | 7 days |
| PEGDA:Alginate | Dexamethasone | < 5% | 5 days | 21 days |
| PCL:PLGA (Electrospun)* | Vancomycin | 40 ± 8% | 12 hours | 3 days |
- Included for comparative context from alternative fabrication method.
Diagrams (Graphviz DOT)
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Alginate (High G-Content) | Forms strong, biocompatible hydrogels via rapid ionic crosslinking with divalent cations (e.g., Ca²⁺). Basis for extrusion and core material. |
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable hydrogel providing cell-adhesive motifs (RGD sequences). Ideal for shell material to promote tissue integration. |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | A highly efficient, water-soluble photoinitiator for visible light (405 nm) crosslinking of GelMA and similar polymers. |
| Polycaprolactone (PCL) Microfibers | Biodegradable synthetic polymer additive used to reinforce hydrogel inks, significantly improving tensile strength and handling. |
| Calcium Chloride (CaCl₂) Solution | The most common ionic crosslinker for alginate. Concentration (50-200 mM) and exposure time control suture stiffness and integrity. |
| Phosphate Buffered Saline (PBS) | Standard isotonic buffer for rinsing sutures, hydrating hydrogels, and serving as the medium for in vitro drug release and degradation studies. |
| Model Drugs (Ciprofloxacin, Dexamethasone) | Small molecule agents used to prototype and quantify controlled release profiles from the suture matrix or core. |
| Cell Viability/Cytotoxicity Assay Kit (e.g., Live/Dead, MTS) | Essential for evaluating cytocompatibility of sutures and leachables according to ISO 10993-5 standards. |
This document provides application notes and protocols for embedding advanced functionalities within 3D-printed surgical sutures. These techniques are core to the broader thesis methodology, which seeks to transform passive sutures into intelligent, therapeutic platforms for wound monitoring, infection prevention, and controlled drug delivery. The integration of these functions during the 3D printing process (e.g., via coaxial or co-extrusion printing) is a primary research focus.
Application Note: Drug-Loading via Coaxial Electrospinning/Printing
Objective: To create suture filaments with a core-shell structure, where the sheath provides mechanical integrity and the core serves as a reservoir for controlled drug release.
Key Quantitative Data: Table 1: Common Polymers & Drugs for Drug-Loaded Sutures
| Component | Material Examples | Function/Role | Typical Loading Efficiency | Key Release Kinetics |
|---|---|---|---|---|
| Sheath (Structural) | PCL, PLA, PGLA | Provides tensile strength, controls degradation rate. | N/A | N/A |
| Core (Reservoir) | PVP, PEG, Gelatin | Dissolves/diffuses to release drug. | N/A | N/A |
| Therapeutic Agent | Diclofenac, Doxycycline, Growth Factors (e.g., VEGF) | Anti-inflammatory, antimicrobial, pro-healing. | 85-95% (for small molecules) | Burst release (20-40% in 24h), sustained release (5-15 days). |
| Crosslinker | Genipin, (3-Glycidyloxypropyl)trimethoxysilane | Stabilizes core, modulates release profile. | N/A | Can extend release to >21 days. |
Protocol: Coaxial Electrospinning for Suture Precursor Fibers
- Materials: Coaxial spinneret, dual syringe pumps, high-voltage power supply, polymer solutions (e.g., 12% w/v PCL in DCM for sheath; 10% w/v PVP + 5% w/v drug in ethanol for core), conducting collector (rotating mandrel).
- Method:
- Solution Preparation: Prepare sheath and core solutions separately. Filter (0.45 µm) to remove particulates.
- Setup: Load solutions into separate syringes on pumps. Connect to coaxial spinneret (core solution to inner capillary). Position spinneret 15-20 cm from grounded, rotating mandrel collector.
- Process Parameters: Apply high voltage (12-18 kV). Set sheath flow rate (1.0 mL/h) and core flow rate (0.3 mL/h). Mandrel rotation speed: 1000-1500 rpm for fiber alignment.
- Collection: Collect aligned fibrous mat for 4-6 hours. Dry in vacuo for 24h to remove residual solvents.
- Post-Processing: Twist or braid fibers to form final suture thread. Sterilize via gamma irradiation (25 kGy).
Workflow Diagram:
Title: Workflow for Coaxial Electrospinning of Drug-Loaded Sutures
Application Note: Antimicrobial Coatings via Layer-by-Layer (LbL) Assembly
Objective: To apply a conformal, multifunctional antimicrobial coating on 3D-printed suture surfaces to prevent surgical site infections.
Key Quantitative Data: Table 2: Efficacy of Common Antimicrobial Agents for Suture Coatings
| Coating Agent | Mechanism of Action | Coating Method | Tested Against | Reduction in Bacterial Viability (vs. Control) |
|---|---|---|---|---|
| Chitosan (CHI) | Disrupts bacterial cell membrane. | LbL with Hyaluronic Acid | S. aureus | >90% after 24h contact |
| Polylysine (ε-PL) | Membrane disruption, electrostatic interaction. | LbL or Dip-Coating | E. coli, S. aureus | >99.5% (at 10 bilayers) |
| Silver Nanoparticles (AgNPs) | Release of Ag⁺ ions, ROS generation. | In-situ synthesis on fiber | MRSA, P. aeruginosa | 4-5 log reduction |
| Triclosan | Inhibits bacterial fatty acid synthesis. | Incorporated in polymer matrix | Multiple Gram+ | >99.9% sustained over 7 days |
| Gentamicin Sulfate | Inhibits protein synthesis. | LbL with Polyelectrolytes | P. aeruginosa | Zone of Inhibition: 8-12 mm diameter |
Protocol: Layer-by-Layer Dip Coating on 3D-Printed Sutures
- Materials: Polyelectrolyte solutions (2 mg/mL Chitosan (CHI) in 1% acetic acid; 2 mg/mL Hyaluronic Acid (HA) in DI water; 1 mg/mL Gentamicin sulfate). Agitation platform, pH meter, DI water rinse baths.
- Method:
- Surface Activation: Plasma treat sutures (O₂, 100 W, 1 min) to introduce negative charges.
- Cationic Layer Dip: Immerse suture in CHI solution (pH 5.5) for 5 min under gentle agitation. Rinse in two consecutive DI water baths (1 min each).
- Anionic Layer Dip: Immerse suture in HA solution (pH 6.5) for 5 min. Rinse as in step 2.
- Drug Layer Integration: For antibiotic loading, substitute the HA dip with a Gentamicin solution dip (5 min).
- Cycle Repetition: Repeat steps 2-4 to build the desired number of bilayers (e.g., 10x (CHI/HA) + 5x (CHI/Gentamicin)).
- Final Rinse & Dry: Rinse thoroughly and dry under a stream of nitrogen. Cure at 37°C for 2 hours.
Pathway Diagram:
Title: Mechanism of Antimicrobial Coating Action on Bacteria
Application Note: Sensor Integration for pH Monitoring
Objective: To integrate a colorimetric pH sensor into a suture for real-time, visual monitoring of wound infection (acidic pH shift).
Key Quantitative Data: Table 3: Performance Metrics of Integrated pH Sensors
| Sensor Type | Indicator Dye | Immobilization Matrix | Dynamic Range (pH) | Response Time | Color Shift (Acidic→Basic) |
|---|---|---|---|---|---|
| Colorimetric | Bromothymol Blue | Agarose/Chitosan Hydrogel | 5.0 - 9.0 | < 2 minutes | Yellow → Blue |
| Colorimetric | Phenol Red | Polyacrylamide Microparticles | 6.8 - 8.2 | ~5 minutes | Yellow → Red |
| Fluorometric | Fluorescein isothiocyanate | Silica Nanoparticles | 4.0 - 8.0 | < 1 minute | Quench → Green Fluorescence |
Protocol: Micro-Encapsulation and Surface Patterning of pH Dye
- Materials: Bromothymol Blue (BTB), Sodium alginate, Calcium chloride solution, 3D printer with micrometer-scale nozzle, PDMS molding substrate.
- Method:
- Sensor Ink Formulation: Prepare 4% w/v sodium alginate in DI water. Add BTB powder to a final concentration of 1% w/w. Mix thoroughly and degas.
- Micro-Deposition: Load ink into a printing syringe fitted with a fine nozzle (≈50 µm). Using a 3D bioprinter, deposit the ink in a discrete, patterned dot (≈200 µm diameter) along the length of a pre-printed suture fixed on a PDMS bed. Maintain 5 mm spacing between sensor dots.
- Crosslinking: Immediately after printing, expose the patterned suture to a CaCl₂ mist (5% w/v) for 60 seconds to ionically crosslink the alginate, trapping the dye.
- Sealing Layer: Dip-coat the entire suture in a thin layer of porous but protective polymer (e.g., 2% w/v PCL in acetone) to secure sensors without inhibiting diffusion.
- Calibration: Immerse sutures in standardized buffer solutions (pH 5, 7, 9) and capture images with a digital microscope. Create a pH vs. RGB value calibration curve.
Integration Diagram:
Title: Multi-Functional 3D-Printed Suture with Integrated Sensor
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Functional Suture Research
| Item/Category | Example Product/Specification | Primary Function in Research |
|---|---|---|
| Biocompatible Polymers | Polycaprolactone (PCL, Mn 80,000), Poly(lactic-co-glycolic acid) (PLGA 85:15). | The structural "ink" for 3D printing, providing tunable mechanical properties and degradation profiles. |
| Therapeutic Agents | Doxycycline hyclate, Vascular Endothelial Growth Factor (VEGF-165), Diclofenac sodium. | Active compounds to be loaded for antimicrobial, pro-angiogenic, or anti-inflammatory effects. |
| Crosslinkers | Genipin, N-(3-Dimethylaminopropyl)-N′-ethylcarbodiimide (EDC). | To stabilize hydrogels or coatings, controlling drug release kinetics and mechanical stability. |
| Polyelectrolytes for LbL | Chitosan (low MW, >75% deacetylated), Hyaluronic acid (sodium salt, from S. zooepidemicus). | Building blocks for constructing controlled-thickness, multifunctional antimicrobial coatings. |
| Colorimetric Indicators | Bromothymol Blue, Phenol Red. | Dyes for fabricating simple, visually readable sensors to monitor wound pH or other biomarkers. |
| Cell Culture Assays | Live/Dead BacLight Viability Kit, S. aureus (ATCC 25923), L929 Fibroblast cell line. | For in vitro validation of antimicrobial efficacy and cytocompatibility of functionalized sutures. |
| Characterization Tools | Scanning Electron Microscope (SEM), UV-Vis Spectrophotometer, Tensile Tester. | To analyze suture morphology, drug release profiles, and mechanical integrity. |
Solving Print Defects and Enhancing Performance: A Practical Guide for Reliable Suture Fabrication
Application Notes
Within a broader thesis on the 3D printing of surgical sutures, the consistent production of high-fidelity, mechanically reliable filaments is paramount. Three primary artifacts—beading, fractures, and inconsistent diameter—compromise suture integrity, directly affecting tensile strength, knot security, and biocompatibility. These artifacts stem from interdependent process parameters in melt-based extrusion printing (e.g., Fused Deposition Modeling - FDM, or direct melt extrusion of polymers).
Artifact Origins and Impact on Suture Performance
- Beading (or Stringing): Occurs during non-print travel moves when residual polymer oozes from the nozzle, forming unwanted threads or "hairs." In suture printing, this creates surface imperfections that can harbor bacteria, increase drag during tissue passage, and create focal stress points.
- Fractures: Manifest as microscopic cracks or complete layer delamination. They are primarily caused by sub-optimal layer adhesion due to incorrect printing temperature, excessive cooling, or material degradation. For a suture, this leads to catastrophic failure under tensile load.
- Inconsistent Diameter: Variations in the extruded filament diameter along the suture's length. This is a critical failure mode, as suture sizing standards (e.g., USP) are defined by diameter ranges. Inconsistency results from fluctuating nozzle pressure due to unstable temperature, variable feed rate, or partial nozzle clogging.
Recent studies (2023-2024) have quantified the relationship between key printing parameters and these artifacts for common biomedical polymers like Polycaprolactone (PCL), Polylactic Acid (PLA), and Polyglycolic Acid (PGA).
Table 1: Impact of Printing Parameters on Suture Artifacts and Mechanical Properties
| Parameter | Optimal Range (for PCL) | Beading Severity (Scale 1-5) | Fracture Incidence (%) | Diameter Variation (± µm) | Resultant Tensile Strength (MPa) |
|---|---|---|---|---|---|
| Nozzle Temperature | 70-80°C | 1 (Low) | <5% | 15 | 42-48 |
| 90-100°C | 3 (Moderate) | 10% | 25 | 38-45 | |
| 60-65°C | 1 (Low) | 40% (High) | 50 | 20-25 | |
| Print Speed | 5-10 mm/s | 1 (Low) | <5% | 10 | 45-50 |
| 20-30 mm/s | 4 (High) | 15% | 40 | 30-35 | |
| Layer Height | 95% of Nozzle Diam. | 2 (Low-Mod) | <5% | 12 | 44-49 |
| 50% of Nozzle Diam. | 1 (Low) | 25% (High) | 8 | 28-32 | |
| Retraction Distance | 4-6 mm | 1 (Low) | <5% | 15 | 43-48 |
| 0-1 mm | 5 (Very High) | <5% | 20 | 40-46 |
Table 2: Common Polymers for 3D-Printed Sutures and Their Artifact Propensity
| Polymer | Typical Print Temp. | Key Artifact Risk | Mitigation Strategy |
|---|---|---|---|
| Polycaprolactone (PCL) | 70-100°C | Fractures (if too cool), Beading (if too hot) | Precise thermal control, enclosed build chamber. |
| Polylactic Acid (PLA) | 190-220°C | Brittle Fractures, Hydrolytic Degradation | Thorough drying (<1% humidity), annealing post-print. |
| Polyglycolic Acid (PGA) | 220-250°C | Severe Thermal Degradation & Beading | Minimal residence time in melt zone, nitrogen purge. |
| PCL-PLA Copolymer | 160-180°C | Inconsistent Diameter (phase separation) | Optimized shear rate, uniform pellet size. |
Experimental Protocols
Protocol for Artifact Analysis and Suture Characterization
Title: Quantitative Assessment of 3D-Printed Suture Artifacts and Mechanical Integrity
Objective: To systematically produce, identify, and quantify printing artifacts (beading, fractures, inconsistent diameter) and correlate them with the tensile performance of 3D-printed polymeric sutures.
Materials: (See "Scientist's Toolkit" below).
Methodology:
Printer & Environment Setup:
- Calibrate the melt extrusion 3D printer (e.g., custom or modified bioprinter). Level the build plate.
- Enclose the print area and maintain a constant ambient temperature (25±2°C) to reduce thermal shock.
- Pre-dry polymer filament/pellets in a vacuum oven at 40°C (PCL) or 70°C (PLA) for 12 hours.
Parametric Printing Experiment:
- Design a simple "straight line" G-code script to print 10 cm suture samples.
- Independent Variables: Systematically vary Nozzle Temperature (3 levels), Print Speed (3 levels), and Retraction Distance (2 levels) in a factorial design.
- Constant Parameters: Nozzle diameter = 200 µm, Layer height = 190 µm, Build plate temperature = 30°C (for PCL), Cooling fan = OFF.
Artifact Quantification:
- Diameter Consistency: Using a laser micrometer, measure the diameter at 10 points along each 10 cm sample. Calculate mean diameter and standard deviation.
- Beading Analysis: Image each sample under a digital microscope (50x magnification). Count the number of beads/strings >50 µm in length per cm.
- Fracture Inspection: Perform micro-CT scanning or SEM imaging of a representative 2 cm section from each sample. Qualitatively score fracture density (0= none, 5= severe).
Mechanical Testing:
- Condition all samples at 23°C, 50% RH for 24 hours.
- Using a universal testing machine with a 100 N load cell, perform tensile testing (ASTM D3822). Gauge length: 50 mm. Crosshead speed: 10 mm/min.
- Record ultimate tensile strength (UTS), elongation at break, and Young's modulus.
Data Analysis:
- Perform ANOVA to determine the statistical significance of each printing parameter on artifact metrics and UTS.
- Create correlation matrices linking artifact severity (diameter variation, beading score) to mechanical failure.
Protocol for Mitigating Fractures via In-Line Annealing
Title: In-Line Thermal Annealing Protocol for Enhanced Layer Adhesion
Objective: To implement and test a post-print annealing process that reduces intra-layer fractures in 3D-printed sutures by promoting polymer chain inter-diffusion.
Methodology:
- Immediately after extrusion, pass the printed suture through a customized, temperature-controlled glass tube (annealing zone) mounted on the print head.
- For PCL sutures, set the annealing zone temperature to 55-60°C (just below melt temperature). Residence time: 30-60 seconds.
- Allow sutures to cool gradually to room temperature on a spool.
- Compare the crystallinity (via DSC), fracture incidence (via SEM), and tensile strength of annealed vs. non-annealed samples from the same print batch.
Signaling Pathways and Workflows
Title: Parameter-Artifact-Performance Relationship in Suture Printing
Title: Suture Printing and Characterization Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D Printing Suture Research
| Item | Function & Rationale |
|---|---|
| Medical-Grade PCL (Mn 50,000-80,000) | Primary feedstock. Biocompatible, low melting point (~60°C), flexible, and slow-degrading. Ideal for process parameter studies. |
| Precision Melt Extrusion Printer | Custom or modified system with temperature control ±1°C, nozzle diameters 100-400 µm, and programmable pressure/feed. |
| Vacuum Oven (<0.1 atm) | Critical for removing absorbed water from hydroscopic polymers (PLA, PGA) prior to printing to prevent hydrolytic degradation and bubbling. |
| Laser Micrometer (±0.1 µm) | Non-contact measurement of extruded filament diameter in real-time or post-print for quantifying diameter consistency. |
| Micro-CT Scanner or SEM | For high-resolution, 3D visualization of internal fractures, layer adhesion defects, and pore structure. |
| Universal Testing Machine (10-500 N load cell) | Quantifies ultimate tensile strength, elongation, and modulus—key metrics for suture USP compliance and performance. |
| Differential Scanning Calorimeter (DSC) | Analyzes polymer crystallinity, glass transition (Tg), and melt temperature (Tm). Essential for optimizing annealing protocols. |
| Controlled Humidity Chamber | For conditioning samples pre-test (e.g., 50% RH, 23°C) to standardize mechanical testing as per ASTM standards. |
Application Notes
Within a research thesis focused on developing a novel methodology for 3D printing surgical sutures, the optimization of key Fused Filament Fabrication (FFF) parameters is critical. The ultimate mechanical integrity of the printed suture, which must withstand surgical handling and knot-tying forces, is directly governed by the inter-layer adhesion (weld strength). This is a function of the thermal history at the interface, which is controlled by nozzle size, print speed, and temperature. This document details the protocols and findings for systematic parameter optimization.
Core Findings from Current Literature (2023-2024): Recent studies emphasize a non-linear, interdependent relationship between these parameters. For high-strength, biomedical-grade polymers like Polylactic Acid (PLA), Polyglycolic Acid (PGA), and their copolymers (PLGA), optimal mechanical performance requires a balance between volumetric flow rate (determined by nozzle size and speed) and thermal energy input (temperature).
- Nozzle Size: Smaller nozzles (< 0.4mm) increase resolution and interlayer contact area but raise backpressure, requiring precise tuning of speed and temperature to avoid under-extrusion and poor adhesion. Larger nozzles (≥ 0.6mm) enhance layer adhesion through greater material deposition and reduced shear thinning but reduce feature fidelity.
- Print Speed: Excessive speed reduces the time for molecular interdiffusion across layers, weakening adhesion. Too-slow speeds can lead to excessive heat buildup and polymer degradation. The optimal speed is contingent on nozzle size and melt viscosity.
- Nozzle Temperature: Increased temperature lowers melt viscosity, promoting interdiffusion. However, exceeding the optimal range for biomedical polymers can cause thermal decomposition, reducing molecular weight and ultimate tensile strength.
Quantitative Data Summary
Table 1: Parameter Impact on Mechanical Properties for PLGA (85/15)
| Parameter | Tested Range | Optimal Value (Tensile Strength) | Effect on Layer Adhesion | Key Mechanism |
|---|---|---|---|---|
| Nozzle Diameter | 0.25 mm - 0.8 mm | 0.4 mm | Peak adhesion at 0.4-0.6mm | Maximizes contact area while maintaining manageable melt pressure. |
| Print Speed | 20 mm/s - 80 mm/s | 40 mm/s | Decreases linearly >50 mm/s | Reduced thermal contact time limits polymer chain interdiffusion. |
| Nozzle Temperature | 200°C - 240°C | 220°C | Increases up to 220°C, then plateaus | Higher temperature reduces viscosity, enhancing diffusion; plateau indicates degradation onset. |
| Bed Temperature | 60°C - 80°C | 70°C | Critical for first layer; minor effect on interlayer | Reduces thermal gradient and warping, ensuring stable foundation. |
Table 2: Optimized Protocol Output for Suture Prototyping
| Target Property | Recommended Nozzle | Print Speed | Nozzle Temp | Expected Tensile Strength* | Suitability for Suture |
|---|---|---|---|---|---|
| High Strength, Monofilament | 0.4 mm | 35 mm/s | 220°C | ~55 MPa | Excellent for larger-diameter, non-absorbable prototypes. |
| Fine Detail, Braided Mimic | 0.25 mm | 25 mm/s | 215°C | ~38 MPa | Suitable for testing absorbable, multi-filament suture geometry. |
| Rapid Prototyping | 0.6 mm | 50 mm/s | 225°C | ~48 MPa | For initial form/fit testing of suture needles or anchors. |
*Strength values are material-specific (PLGA 85/15) and serve as a benchmark.
Experimental Protocols
Protocol 1: Systematic Parameter Screening for Layer Adhesion Objective: To identify the parameter window that maximizes interlayer weld strength for a given biomedical polymer. Materials: As per "The Scientist's Toolkit" below. Method:
- Design: Print standardized tensile test specimens (e.g., ASTM D638 Type V) aligned vertically (Z-axis) to stress the layer interfaces.
- Parameter Matrix: Create a full-factorial design varying:
- Nozzle Size: 0.25mm, 0.4mm, 0.6mm.
- Print Speed: 20, 40, 60 mm/s.
- Nozzle Temperature: 210, 220, 230°C.
- Keep layer height constant at 50% of nozzle diameter.
- Printing: Execute all print jobs in a controlled environment (<30% RH). Dry filament immediately before use (12h, 60°C). Use a sealed build chamber if available to minimize thermal fluctuation.
- Conditioning: Post-print, condition all samples in a desiccator for 48 hours to equalize moisture content.
- Testing: Perform tensile testing at a constant strain rate (e.g., 5 mm/min). Record ultimate tensile strength (UTS) and elongation at break.
- Analysis: Plot UTS against each parameter. Use ANOVA to identify statistically significant (p<0.05) main effects and interactions. The peak UTS indicates optimal layer adhesion.
Protocol 2: Validation via Suture Tensile and Knot Testing Objective: To validate optimized parameters by fabricating and testing 3D-printed suture prototypes. Method:
- Suture Fabrication: Using parameters from Protocol 1's optimum, 3D print straight monofilament suture prototypes (e.g., 0.3mm diameter, 150mm length) using a direct-drive extruder on a build plate with a slow, single-line extrusion pattern.
- Mechanical Testing:
- Straight Pull: Clamp 50mm gauge length of the suture in a tensile tester. Pull at 10 mm/min until failure. Record breaking force.
- Knot Pull: Tie a standardized surgeon’s knot (e.g., double throw) in the center of the suture. Place each free end in the tensile grips, ensuring the knot is centered. Pull at 10 mm/min until failure. Record knot break force.
- Failure Analysis: Examine fracture surfaces under a scanning electron microscope (SEM) to characterize failure mode (cohesive vs. adhesive between layers).
Visualizations
Diagram 1 Title: Parameter Interdependence in Layer Adhesion
Diagram 2 Title: Experimental Workflow for Parameter Optimization
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for FFF Suture Research
| Item | Function & Relevance |
|---|---|
| Medical-Grade PLGA Filament | The primary biomaterial. Its copolymer ratio (e.g., 85:15, 50:50) dictates degradation rate and mechanical properties. Must be sterile-packed and hydrolytically sealed. |
| High-Precision Desktop 3D Printer | Equipped with a direct-drive extruder for precise control over flexible/biopolymer filaments. A heated bed and enclosed chamber are mandatory for thermal stability. |
| Tungsten Carbide Nozzles (0.25-0.8mm) | Abrasion-resistant nozzles to maintain precise orifice diameter during printing, especially critical for consistent fiber diameter in sutures. |
| Laboratory Filament Dryer | Removes absorbed moisture from hygroscopic biomedical polymers (PLA, PLGA, PCL) prior to printing, preventing vapor bubbles and poor layer adhesion. |
| Benchtop Tensile Tester | For quantifying the ultimate tensile strength, elongation, and modulus of both standardized test coupons and printed suture prototypes. |
| Controlled Humidity Storage | Dry cabinets or desiccators to store filament and printed samples, preventing hydrolytic degradation before testing. |
| Scanning Electron Microscope (SEM) | For high-resolution imaging of fracture surfaces post-failure, allowing analysis of interlayer bonding quality and void presence. |
| Differential Scanning Calorimeter (DSC) | To characterize the thermal properties (Tg, Tm, crystallinity) of the raw filament and printed parts, linking print temperature to material state. |
Within the broader research on 3D printing methodologies for advanced surgical sutures, post-processing sterilization is a critical, non-negotiable step. The chosen method must effectively achieve sterility while preserving the structural integrity, mechanical properties, and biofunctionality of the printed biomaterial. This document provides detailed application notes and protocols for sterilization methods compatible with common polymers used in 3D printing, such as PLA, PCL, PLGA, and resin-based hydrogels.
Comparative Analysis of Sterilization Methods
The efficacy and impact of sterilization vary significantly with the biomaterial and printing technology. The table below summarizes quantitative data on common methods.
Table 1: Comparative Analysis of Sterilization Methods for 3D Printed Biomaterials
| Method | Typical Parameters | Key Advantages | Key Disadvantages & Material-Specific Impacts | Best For |
|---|---|---|---|---|
| Ethylene Oxide (EtO) | 37-63°C, 40-80% humidity, 1-6 hr exposure, 12-24 hr aeration. | Low temperature; penetrates complex geometries; broad material compatibility. | Long cycle time; toxic residues require aeration; can hydrolyze PLGA. | Heat-sensitive, porous structures (e.g., PCL meshes, complex suture anchors). |
| Gamma Irradiation | 25-40 kGy dose (standard). | Excellent penetration; no residues; terminal sterilization of packaged devices. | Can cause chain scission/crosslinking; embrittles PLA; reduces molecular weight of PCL. | Pre-packaged, single-use items where radiation stability is validated. |
| Electron Beam (E-beam) | 25-40 kGy dose, high dose rate. | Rapid process; precise control; less oxidative damage than gamma. | Limited penetration depth (~10-15 cm); surface-dominated effects. | Thin or surface-functionalized constructs (e.g., suture coatings). |
| Autoclaving (Steam) | 121°C, 15-20 psi, 15-30 min. | Fast; inexpensive; no toxic chemicals. | High heat/moisture deforms PLA (Tg ~60°C); hydrolyzes polyesters. | High-temperature stable materials (e.g., some PEEK, annealed PCL). |
| Ethanol Immersion | 70-80% v/v, 30 min - 2 hr immersion. | Mild, room-temperature process; simple. | Poor penetration; not a terminal sterilization method; can swell hydrogels. | Surface decontamination of research prototypes, resin-based hydrogels. |
| Hydrogen Peroxide Plasma (VHP) | 45-55°C, 1-3 hr cycle. | Low temperature; rapid; no toxic residues. | Limited penetration into dense/laminated structures; can affect surface chemistry. | Porous, dry, heat-sensitive materials that cannot be autoclaved. |
Detailed Experimental Protocols
Protocol 1: Ethylene Oxide Sterilization for a PCL-Based Suture Mesh
Objective: To terminally sterilize a 3D-printed, biodegradable polycaprolactone (PCL) mesh implant without compromising its tensile strength or degradation profile.
Materials:
- 3D printed PCL mesh samples.
- EtO sterilization chamber with controlled gas concentration, humidity, and temperature.
- Sterile, breathable packaging (e.g., Tyvek pouches).
- Analytical balance, mechanical tester.
Procedure:
- Pre-conditioning: Place the dried PCL mesh samples into breathable sterilization pouches. Seal the pouches.
- Loading: Load the pouches into the EtO chamber, ensuring adequate space for gas circulation.
- Cycle Execution:
- Pre-vacuum: Chamber is evacuated to remove air.
- Humidification: Humidity is raised to 60-70% to potentiate microbial kill.
- Gas Injection: EtO gas is injected to a concentration of 450-1200 mg/L.
- Exposure: Maintain temperature at 37°C for 2-3 hours.
- Evacuation: EtO is evacuated from the chamber through a series of flushes.
- Aeration: Transfer the sterilized pouches to a dedicated, well-ventilated aerator at 50°C for a minimum of 12 hours (or per validation) to desorb residual EtO.
- Post-Sterilization Validation:
- Sterility Test: Perform USP <71> sterility test on a subset of samples.
- Mechanical Test: Conduct tensile testing (ASTM D882) on sterilized vs. control samples to assess property changes.
- Residuals Analysis: For final product validation, perform GC analysis for EtO and ethylene chlorohydrin residues per ISO 10993-7.
Protocol 2: Ethanol Immersion for Resin-Based Hydrogel Suture Prototypes
Objective: To achieve surface sterility of a delicate, 3D-printed methacrylated gelatin (GelMA) hydrogel suture prototype prior to in vitro cell studies.
Materials:
- 3D printed/crosslinked GelMA suture samples.
- 70% (v/v) Ethanol solution in sterile, deionized water.
- Sterile Petri dishes, forceps, phosphate-buffered saline (PBS).
- Laminar flow hood.
Procedure:
- Preparation: Perform all steps in a laminar flow hood using aseptic technique.
- Primary Decontamination: Immerse the GelMA suture samples completely in 70% ethanol for 30 minutes. Ensure all surfaces are wetted.
- Rinsing: Using sterile forceps, transfer the samples to a sterile Petri dish containing sterile PBS. Rinse three times (5 minutes per rinse) to remove all ethanol traces, which are cytotoxic.
- Validation:
- Microbial Culture: Plate the final rinse solution on TSA and SDA agar plates. Incubate and check for microbial growth.
- Cytocompatibility (Post-Rinsing): Seed fibroblasts onto the sterilized hydrogel surface and assess viability via Live/Dead assay at 24 and 72 hours to confirm no residual ethanol effects.
- Swelling/Degradation: Compare the mass and dimensional swelling ratio of sterilized vs. non-sterilized controls to assess ethanol-induced structural changes.
Visualizations
Title: Decision Pathway for Biomaterial Sterilization
Title: Ethylene Oxide Sterilization Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Materials for Post-Sterilization Validation
| Item | Function/Brief Explanation |
|---|---|
| Polycaprolactone (PCL) Filament | Model biodegradable polymer for 3D printing sutures/meshes; low melting point (60°C) makes it heat-sensitive for sterilization studies. |
| Methacrylated Gelatin (GelMA) Resin | Photocurable bioink for DLP printing; forms hydrogels that are highly sensitive to solvents and heat, requiring mild sterilization. |
| Tyvek Sterilization Pouches | Breathable medical packaging allowing penetration of EtO gas and steam while maintaining sterility post-process. |
| Tryptic Soy Agar (TSA) Plates | General-purpose microbial growth medium for conducting USP <71> sterility tests post-sterilization. |
| Sabouraud Dextrose Agar (SDA) Plates | Fungal growth medium used in sterility testing to detect yeast and mold contamination. |
| Phosphate-Buffered Saline (PBS), Sterile | Used for rinsing chemical sterilants (e.g., ethanol) from samples prior to biological testing. |
| Live/Dead Viability/Cytotoxicity Kit | (e.g., Calcein AM/EthD-1) Fluorescent assay to confirm cytocompatibility of sterilized biomaterials with cultured cells. |
| Instron or equivalent Mechanical Tester | For quantifying changes in tensile strength, modulus, and elongation of sterilized vs. control suture samples. |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Essential analytical instrument for quantifying residual levels of EtO and its by-products in sterilized materials. |
Application Notes
For researchers developing 3D-printed surgical sutures within a broader methodology thesis, the central challenge lies in the tripartite optimization of printability (process fidelity), mechanical performance (strength, elasticity), and controlled degradation. This requires a materials-by-design approach where polymer chemistry, additive manufacturing parameters, and post-processing are co-optimized.
Key Trade-offs & Strategic Considerations:
- Polymer Selection & Blending: Pure, high-molecular-weight polymers like PCL offer excellent elasticity and strength but exhibit slow degradation and high melt viscosity, challenging printability. Blending with faster-degrading polymers like PLGA or plasticizers (e.g., PEG) enhances printability and tunes degradation but typically reduces ultimate tensile strength.
- Print Parameter Interdependence: Nozzle temperature, pressure, and print speed must be balanced. Higher temperatures improve flow (printability) but can accelerate polymer degradation, affecting final mechanics. Layer height and infill pattern directly influence suture porosity, impacting both mechanical load-bearing and degradation rate.
- Post-Processing Efficacy: Techniques like annealing can significantly increase crystallinity and tensile strength but may reduce elasticity. Sterilization method (e.g., EtO, gamma radiation) must be selected to minimize premature polymer chain scission.
Experimental Protocols
Protocol 1: Formulation Screening for Coaxial Extrusion
Aim: To develop a core-sheath suture filament with tunable mechanics and degradation. Materials: See "Research Reagent Solutions" table. Method:
- Solution Preparation: Prepare separate core and sheath polymer solutions. Core: Dissolve PCL (Mn 80,000) in DCM at 15% w/v. Sheath: Dissolve PLGA (50:50) in DMF at 10% w/v. Stir for 6 hours at 40°C until fully homogeneous.
- Coaxial Printing: Load solutions into separate syringes on a bioprinter equipped with a coaxial nozzle (e.g., 16G inner, 22G outer). Set sheath flow rate to 150 µL/min and core flow rate to 100 µL/min. Extrude onto a rotating mandrel (3 mm diameter) at a linear speed of 200 mm/min.
- Post-Processing: Immediately transfer the wound suture to a vacuum chamber for 48 hours to evaporate residual solvents. Subsequently, anneal at 60°C (below PCL Tm) for 2 hours.
Protocol 2: In Vitro Degradation & Mechanical Testing
Aim: To quantify the temporal evolution of tensile properties during degradation. Method:
- Degradation Study: Cut suture samples into 10 cm lengths (n=5 per group). Immerse in 15 mL of PBS (pH 7.4) at 37°C in a shaking incubator (50 rpm). Replace PBS weekly to maintain sink conditions.
- Time-Point Analysis: At pre-determined intervals (0, 1, 2, 4, 8, 12 weeks), remove samples, rinse with DI water, and dry to constant mass.
- Tensile Testing: Perform uniaxial tensile testing per ASTM D2256. Use a calibrated mechanical tester with a 50 N load cell. Gauge length: 50 mm. Crosshead speed: 10 mm/min. Record:
- Ultimate Tensile Strength (UTS)
- Elongation at Break (%)
- Young's Modulus (calculated from the linear region of the stress-strain curve).
Table 1: Representative Data for PCL/PLGA Blended Sutures (Post 8-week Degradation)
| Polymer Blend (Ratio) | UTS (MPa) | Elongation at Break (%) | Young's Modulus (MPa) | Mass Loss (%) |
|---|---|---|---|---|
| PCL 100% | 22.4 ±1.8 | 580 ±45 | 210 ±15 | 5.2 ±0.8 |
| PCL/PLGA (75:25) | 18.1 ±1.5 | 410 ±30 | 250 ±20 | 18.5 ±2.1 |
| PCL/PLGA (50:50) | 12.3 ±1.2 | 220 ±25 | 320 ±25 | 42.3 ±3.5 |
| PLGA 100% (50:50) | 65.5 ±5.0 | 12 ±4 | 2200 ±150 | 68.9 ±4.8 |
Table 2: Effect of Printing Parameters on PCL Suture Mechanics
| Nozzle Temp (°C) | Print Speed (mm/s) | Layer Height (µm) | UTS (MPa) | Diameter Consistency (CV%) |
|---|---|---|---|---|
| 80 | 5 | 150 | 15.2 ±1.0 | 8.5 |
| 100 | 5 | 150 | 20.8 ±1.3 | 4.1 |
| 120 | 5 | 150 | 19.5 ±1.5 | 3.8 |
| 100 | 10 | 150 | 18.9 ±1.2 | 6.7 |
| 100 | 5 | 200 | 17.1 ±1.1 | 7.2 |
Research Reagent Solutions
| Item & Supplier (Example) | Function in Research |
|---|---|
| Polycaprolactone (PCL), Mn 80kDa (Sigma-Aldrich) | Primary polymer providing elasticity and slow degradation. Serves as a tunable base material. |
| PLGA, 50:50, Acid End-capped (Evonik) | Co-polymer to accelerate degradation rate and modify stiffness via blending or coaxial sheath. |
| Medical-grade PEG 400 (Carbowax) | Plasticizer to reduce melt viscosity, enhancing printability without excessive heat. |
| Anhydrous Dimethylformamide (DMF) (Fisher Scientific) | Solvent for processing polymers like PLGA into printable inks or solutions. |
| Phosphate Buffered Saline (PBS), pH 7.4 (Thermo Fisher) | Standard buffer for in vitro degradation studies simulating physiological conditions. |
| Coaxial Printing Nozzle (Nordson EFD) | Enables fabrication of core-sheath suture structures for multi-functional drug delivery. |
Diagrams
Title: Optimization Parameters for 3D-Printed Sutures
Title: Experimental Workflow for Suture Development
Within the broader thesis on 3D printing methodologies for surgical sutures, achieving biocompatibility is paramount. This document outlines application notes and detailed protocols for assessing and mitigating cytotoxicity and inflammatory responses elicited by novel 3D-printed suture materials. The strategies focus on material selection, post-processing, and in vitro evaluation.
Key Cytotoxicity Evaluation Protocols
Direct Contact MTT Assay for Eluant Cytotoxicity
This protocol evaluates the cytotoxic potential of leachable substances from 3D-printed suture materials.
Materials:
- Test material: 3D-printed suture segment (sterilized, 1 cm length).
- Cells: L929 mouse fibroblast cells (ATCC CCL-1).
- Culture Medium: DMEM with 10% FBS, 1% penicillin/streptomycin.
- Reagents: MTT reagent (3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide), Dimethyl sulfoxide (DMSO).
- Equipment: 24-well plate, CO₂ incubator, microplate reader.
Procedure:
- Seed L929 fibroblasts in a 24-well plate at 5 x 10⁴ cells/well in 1 mL medium. Incubate for 24 h (37°C, 5% CO₂) to achieve ~80% confluence.
- Aseptically place one suture segment directly onto the cell monolayer in the test well. Use cells without material as a negative control.
- Incubate for a further 24 hours.
- Carefully remove the medium and suture. Add 500 µL of fresh medium containing 0.5 mg/mL MTT to each well.
- Incubate for 4 hours.
- Carefully aspirate the MTT solution. Add 500 µL of DMSO to each well to solubilize the formed formazan crystals.
- Gently shake the plate for 10 minutes.
- Transfer 100 µL of solution from each well to a 96-well plate. Measure the absorbance at 570 nm with a reference wavelength of 650 nm using a microplate reader.
- Calculate cell viability:
% Viability = (Absorbance of Test Sample / Absorbance of Negative Control) * 100.
ISO 10993-5 Compliant Extract Preparation and Testing
Preparation of material extracts simulates physiological leaching over time.
Procedure:
- Extract Preparation: Sterilize suture samples. Use a surface area to extraction medium ratio of 3 cm²/mL (or 0.2 g/mL for irregular shapes). Immerse samples in complete cell culture medium or physiological saline. Incubate at 37°C for 24±2 h or 72±2 h based on intended application.
- Cell Exposure: Seed L929 or human dermal fibroblast cells in a 96-well plate (1 x 10⁴ cells/well). Incubate for 24 h.
- Replace the seeding medium with 100 µL of the prepared extract. Include a negative control (medium alone) and a positive control (e.g., medium with 1% phenol).
- Incubate cells with the extract for 24 h.
- Perform MTT or PrestoBlue assay per manufacturer instructions to quantify metabolic activity relative to controls.
Table 1: Typical Cytotoxicity Scoring (Based on ISO 10993-5)
| Reduction in Cell Viability | Cytotoxicity Grade | Interpretation |
|---|---|---|
| ≥ 70% | 0 (Non-cytotoxic) | Acceptable |
| 60-69% | 1 (Slightly cytotoxic) | Investigate |
| 50-59% | 2 (Mildly cytotoxic) | Investigate |
| 40-49% | 3 (Moderately cytotoxic) | Unacceptable |
| ≤ 39% | 4 (Severely cytotoxic) | Unacceptable |
Assessing Inflammatory Response via Cytokine Profiling
Quantifying pro-inflammatory cytokine release from immune cells exposed to material extracts indicates the intrinsic inflammatory potential.
Protocol: Monocyte/Macrophage Activation Assay
Materials:
- THP-1 human monocyte cell line or primary human peripheral blood mononuclear cells (PBMCs).
- Differentiation agent: Phorbol 12-myristate 13-acetate (PMA) for THP-1.
- ELISA kits: TNF-α, IL-1β, IL-6, IL-8.
Procedure:
- Differentiate THP-1 monocytes into macrophage-like cells by treating with 100 nM PMA for 48 h. Rest cells in PMA-free medium for 24 h.
- Prepare material extracts as in Section 1.2, using serum-free medium.
- Treat differentiated THP-1 macrophages with material extracts for 24 h. Use Lipopolysaccharide (LPS, 1 µg/mL) as a positive control.
- Collect cell culture supernatant by centrifugation.
- Perform ELISA for target cytokines according to the manufacturer's protocol.
- Express data as pg/mL of cytokine, normalized to total protein content or cell count.
Table 2: Example Cytokine Release Profile (Hypothetical Data)
| Suture Material | TNF-α (pg/mL) | IL-6 (pg/mL) | IL-1β (pg/mL) | Assessment |
|---|---|---|---|---|
| Control (Medium) | 15 ± 3 | 25 ± 5 | 5 ± 2 | Baseline |
| PLA (Base Polymer) | 120 ± 20 | 450 ± 80 | 45 ± 10 | Moderate Inflammation |
| PLA + Anti-inflammatory Agent | 35 ± 8 | 90 ± 15 | 10 ± 4 | Low Inflammation |
| Positive Control (LPS) | 850 ± 150 | 2200 ± 300 | 180 ± 25 | High Inflammation |
Mitigation Strategies: Application Notes
- Material Purity: Use medical-grade or USP Class VI certified polymers (e.g., PLGA, PCL, pure silk) to minimize toxic leachables.
- Post-Printing Processing: Implement rigorous washing (e.g., in ethanol/water) to remove residual monomers, initiators, or solvents. Consider supercritical CO₂ extraction for efficient cleaning.
- Surface Modification: Coat sutures with hydrophilic polymers (e.g., Polyethylene glycol - PEG, Hyaluronic acid) to reduce protein adsorption and immune cell adhesion.
- Incorporation of Active Agents: Encapsulate anti-inflammatory drugs (e.g., Dexamethasone, Ibuprofen) or natural agents (e.g., Curcumin) into the suture matrix for localized, sustained release.
- Topography Optimization: Design surface textures via 3D printing parameters to minimize macrophage fusion and foreign body giant cell formation.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function / Application |
|---|---|
| L929 Fibroblast Cell Line | Gold-standard cell line for ISO 10993-5 cytotoxicity testing of biomaterials. |
| THP-1 Monocyte Cell Line | Model system for studying human macrophage-mediated inflammatory responses in vitro. |
| PrestoBlue / MTT Reagent | Cell-permeable dyes for colorimetric/fluorometric quantification of cell viability. |
| Human Cytokine ELISA Kits | Quantify specific pro-inflammatory cytokines (TNF-α, IL-6, IL-1β) in cell supernatants. |
| Medical-Grade PLGA | Biodegradable copolymer; suture matrix allowing tunable degradation and drug release. |
| Dexamethasone | Potent synthetic glucocorticoid; incorporated into sutures to suppress inflammation. |
| Lipopolysaccharide (LPS) | Toll-like receptor agonist; used as a positive control to stimulate robust cytokine release. |
Visualizations
Diagram 1: Inflammatory Response Signaling Pathway
Diagram 2: Biocompatibility Assessment Workflow
Benchmarking Against Tradition: Mechanical, Biological, and Clinical Evaluation of 3D Printed Sutures
Application Notes
This document provides application notes and protocols for evaluating 3D-printed surgical suture materials within a research methodology focused on additive manufacturing for medical devices. The objective is to benchmark novel 3D-printed suture formulations against established commercial materials—natural silk, synthetic absorbable Polyglycolic Acid (PGA), and non-absorbable monofilaments (e.g., polypropylene, nylon)—across three critical mechanical performance metrics. These comparisons are essential for validating the feasibility and potential superiority of 3D-printed sutures for specific clinical applications.
Key Performance Indicators (KPIs):
- Tensile Strength: Indicates the maximum stress a suture can withstand while being stretched before breaking. Crucial for holding tissue under tension.
- Knot Security: A measure of a knot's ability to resist slipping or untying under load. Evaluated via knot-pull strength and knot failure mode.
- Fatigue Resistance: The ability to maintain integrity under cyclic loading, simulating physiological stresses like muscle movement or pulsating vessels.
Comparative Data Summary: The following tables summarize typical quantitative data from recent literature for benchmark materials and target ranges for advanced 3D-printed (e.g., PCL-based, composite) sutures.
Table 1: Tensile Strength Comparison
| Material Category | Specific Material | Average Tensile Strength (MPa) | Diameter (USP) | Notes |
|---|---|---|---|---|
| Natural | Virgin Silk (Bombyx mori) | 450 - 600 | 2-0 | High initial strength, degrades over weeks. |
| Synthetic Absorbable | Polyglycolic Acid (PGA) | 550 - 750 | 2-0 | High initial strength, loses ~50% in 2 weeks. |
| Synthetic Non-Absorbable | Polypropylene (Prolene) | 400 - 550 | 2-0 | Maintains strength long-term, high ductility. |
| 3D-Printed Target | Polycaprolactone (PCL) | 300 - 500 | 2-0 | Highly tunable via print parameters & blending. |
| 3D-Printed Target (Advanced) | PCL/Chitosan Composite | 450 - 650+ | 2-0 | Aims to match PGA with enhanced bioactivity. |
Table 2: Knot Security & Fatigue Resistance
| Material | Knot-Pull Strength (% of Straight Pull) | Primary Knot Failure Mode | Fatigue Cycles to Failure (x10³)* |
|---|---|---|---|
| Silk | ~65% | Knot slippage / unraveling | 10 - 25 |
| PGA | ~70% | Suture breakage at knot | 20 - 40 |
| Polypropylene | ~85% | Suture breakage at knot | 100 - 200+ |
| 3D-Printed PCL | 60 - 75% | Highly dependent on surface texture | 50 - 100 |
| *Cycles under a defined sub-maximal load (e.g., 30-50% of UTS). |
Experimental Protocols
Protocol 1: Tensile Strength Testing (ASTM D2256 / ISO 2062)
- Objective: To determine the ultimate tensile strength (UTS), Young's modulus, and elongation at break of suture materials.
- Equipment: Universal tensile testing machine (e.g., Instron), pneumatic or mechanical grips, calibrated calipers.
- Procedure:
- Condition all samples at 21±1°C and 65±2% RH for 24 hours.
- Cut suture segments to a standard gauge length (e.g., 100 mm).
- Measure the diameter at three points along the length using a laser micrometer or precision calipers. Record the average.
- Mount the suture in the grips, ensuring alignment to prevent premature grip failure. Use a paper tab or rubber-faced grips to minimize shear damage.
- Set the test speed to 300 mm/min (for non-absorbables) or 100 mm/min (for absorbables/printed materials).
- Initiate the test and record the load-extension curve until failure.
- Calculate UTS (MPa) = (Maximum Load (N) / Cross-sectional Area (mm²)).
- Sample Size: n ≥ 10 per material group.
Protocol 2: Knot Security Testing
- Objective: To evaluate the strength and integrity of a standardized surgical knot.
- Equipment: Tensile testing machine, grips.
- Procedure:
- Tie a surgeon's knot (two throws followed by a square throw) with a 2-0 suture material around a polished, 10 mm diameter mandrel.
- Leave equal-length ends (e.g., 50 mm). Secure one end in the upper grip and the looped end around the mandrel in the lower grip.
- Apply tension at a constant crosshead speed of 300 mm/min until failure.
- Record the knot-pull tensile strength (KPTS).
- Document the mode of failure: knot slippage (untying), suture breakage at the knot, or suture breakaway from the knot.
- Analysis: Calculate Knot Efficiency (%) = (KPTS / UTS) x 100.
Protocol 3: In Vitro Fatigue Resistance Testing
- Objective: To assess the suture's durability under repeated cyclical loading.
- Equipment: Dynamic mechanical analyzer (DMA) or specialized cyclic tensile tester, phosphate-buffered saline (PBS) bath at 37°C (optional).
- Procedure:
- Mount a straight or knotted suture sample in the tester grips.
- Submerge the sample in a 37°C PBS bath if simulating physiological conditions.
- Apply a sinusoidal or triangular waveform cyclic load. Set the mean load to 30% of the material's average UTS and the amplitude to ±10% of UTS.
- Set a frequency of 1-5 Hz to simulate physiological rates.
- Run the test until suture failure or until a predetermined number of cycles (e.g., 100,000) is reached.
- Record the number of cycles to failure and plot S-N (stress vs. cycles) curves for comparison.
Visualizations
Experimental Workflow for Suture Mechanical Testing
Knot Failure Mode Analysis Logic Tree
The Scientist's Toolkit: Research Reagent & Material Solutions
| Item | Function & Rationale |
|---|---|
| Universal Testing System (e.g., Instron, ZwickRoell) | Applies controlled tensile/cyclic forces with precise data acquisition for UTS, modulus, and fatigue life. |
| Environmental Chamber/PBS Bath | Maintains physiologically relevant temperature (37°C) and humidity during testing, critical for absorbable materials. |
| Laser Micrometer | Provides non-contact, high-precision measurement of suture diameter, essential for accurate stress calculation. |
| Polycaprolactone (PCL) Filament (Medical Grade) | Primary thermoplastic polymer for fused deposition modeling (FDM) of experimental sutures; biocompatible and flexible. |
| Chitosan or Bioactive Particle Additives | Composite additives to enhance tensile strength, knot security, and provide antimicrobial properties to printed sutures. |
| Phosphate-Buffered Saline (PBS), pH 7.4 | Standard immersion medium for in vitro fatigue testing to simulate the ionic environment of bodily fluids. |
| Surgical Knot-Tying Mandrel (Ø10 mm) | Standardized cylindrical post for consistent creation of suture loops and knots for security testing. |
| Scanning Electron Microscope (SEM) | For post-failure analysis of fracture surfaces, knot morphology, and material texture related to performance. |
Application Notes
Within a thesis on the 3D printing of surgical sutures, direct comparative studies of in vitro biocompatibility and degradation profiles are critical for benchmarking novel materials against regulatory standards and clinical benchmarks. This work typically precedes in vivo studies, providing a high-throughput, ethically favorable screening method. For 3D-printed sutures, variables such as polymer resin composition (e.g., PCL, PLGA, PLA), printing parameters (nozzle temperature, layer height), and post-processing (UV curing, sterilization) directly influence cellular response and hydrolytic/enzymatic degradation kinetics. The core objective is to correlate material processing parameters from the 3D printing methodology with quantifiable biological and physicochemical outcomes to guide iterative design.
Experimental Protocols
Protocol 2.1: Direct Comparative In Vitro Biocompatibility (MTT/CellTiter-Glo Assay)
Aim: To compare the metabolic activity of L929 fibroblast cells exposed to extracts of 3D-printed suture materials. Materials: See Section 4, Research Reagent Solutions. Workflow:
- Sample Preparation: Sterilize 3D-printed suture samples (e.g., 1 cm lengths) via ethanol immersion and UV irradiation. Prepare extracts per ISO 10993-5 by incubating samples in complete DMEM (0.1 g/mL) at 37°C for 24 hours. Include a negative control (medical-grade silicone) and a positive control (latex).
- Cell Seeding: Seed L929 cells in a 96-well plate at 5,000 cells/well in 100 µL complete medium. Incubate for 24 h at 37°C, 5% CO₂ to allow cell attachment.
- Exposure: Aspirate medium from wells. Add 100 µL of each material extract or controls to triplicate wells. Include a cell-only control (medium only).
- Incubation: Incubate plate for 24 h.
- Viability Assessment: For MTT, add 10 µL of MTT reagent (5 mg/mL) per well. Incubate 4 h. Add 100 µL solubilization solution. Shake overnight. For CellTiter-Glo, add 100 µL reagent, shake 2 min, incubate 10 min.
- Quantification: Measure absorbance (MTT: 570 nm, ref. 650 nm) or luminescence. Calculate relative viability (%) vs. cell-only control.
- Statistical Analysis: Perform one-way ANOVA with post-hoc Tukey test (p<0.05 significant).
Protocol 2.2: Direct Comparative Hydrolytic Degradation Profiling
Aim: To measure mass loss, molecular weight change, and pH variation of 3D-printed sutures in simulated physiological buffer. Materials: See Section 4. Workflow:
- Sample Preparation: Weigh (W₀) and record initial dimensions of sterile 3D-printed suture samples (n=5 per group). Determine initial molecular weight (Mₙ₀) via GPC.
- Immersion: Immerse each sample in 5 mL of PBS (pH 7.4, with 0.02% sodium azide) or simulated body fluid (SBF) in sealed vials. Incubate at 37°C under static conditions.
- Time-Point Sampling: At pre-defined intervals (e.g., 1, 3, 7, 14, 28, 56 days), remove samples from one vial per group.
- Analysis:
- Mass Loss: Rinse samples with deionized water, lyophilize for 48 h, and weigh (Wₜ). Calculate mass remaining (%) = (Wₜ / W₀) x 100.
- Molecular Weight: Dissolve dried samples in appropriate solvent and perform GPC to determine Mₙₜ.
- pH Monitoring: Measure pH of the immersion medium at each time point.
- Morphology: Image surface erosion/cracking via SEM.
Data Presentation
Table 1: Direct Comparison of Biocompatibility (24h Extract Exposure, L929 Cells)
| Material / 3D-Printed Suture Formulation | Viability (%) - MTT Assay | Viability (%) - CellTiter-Glo | Significance (vs. Negative Control) | Reference Standard Met? (ISO 10993-5) |
|---|---|---|---|---|
| Medical-Grade Silicone (Negative Control) | 100 ± 5 | 100 ± 6 | N/A | Yes |
| Latex (Positive Control) | 45 ± 8 | 38 ± 10 | p < 0.001 | No |
| 3D-Printed PCL Suture (Low Temp) | 98 ± 4 | 102 ± 7 | p > 0.05 | Yes |
| 3D-Printed PLGA Suture (50:50) | 95 ± 6 | 97 ± 5 | p > 0.05 | Yes |
| 3D-Printed PLA Suture (High Temp) | 82 ± 5 | 85 ± 4 | p < 0.05 | Yes (Borderline) |
Table 2: Direct Comparison of Hydrolytic Degradation Profiles in PBS (37°C)
| Material / Formulation | Day 28 Mass Remaining (%) | Day 28 Mₙ Retention (%) | Time to 50% Mₙ Loss (Days) | Surface Erosion Observed (SEM Day 28) |
|---|---|---|---|---|
| 3D-Printed PCL (Mn 80kDa) | 99 ± 0.5 | 85 ± 3 | >180 | No |
| 3D-Printed PLGA (50:50) | 65 ± 4 | 30 ± 5 | ~28 | Yes (Porous) |
| 3D-Printed PLA (High Cryst.) | 96 ± 2 | 78 ± 4 | ~90 | No (Cracking) |
| Commercial Vicryl Suture | 58 ± 3 | 25 ± 4 | ~21 | Yes (Fragmented) |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Direct Comparative Studies
| Item | Function & Rationale |
|---|---|
| L929 Mouse Fibroblast Cell Line (ATCC CCL-1) | Standardized cell model for in vitro cytocompatibility testing per ISO 10993-5. |
| CellTiter-Glo 3D Assay (Promega) | Luminescent ATP-based assay; ideal for 3D material extracts, offers high sensitivity and broad linear range. |
| Phosphate Buffered Saline (PBS) with 0.02% Sodium Azide | Standard hydrolytic degradation medium; azide prevents microbial growth for long-term studies. |
| Simulated Body Fluid (SBF) | Ion concentration similar to human blood plasma; assesses bioactivity and degradation in a more physiologic environment. |
| Size Exclusion Chromatography (GPC/SEC) System | Determines changes in number-average molecular weight (Mₙ), a critical indicator of polymer chain scission during degradation. |
| Scanning Electron Microscope (SEM) | Visualizes surface morphology, erosion patterns, and crack formation on degraded suture materials at high resolution. |
Visualizations
Diagram 1 Title: In Vitro Biocompatibility Assessment Workflow
Diagram 2 Title: Hydrolytic Degradation Pathway for Polyester Sutures
Application Notes
Within the context of a thesis on 3D-printed surgical sutures methodology, in vivo animal model studies are indispensable for evaluating two critical performance parameters: wound healing efficacy and the foreign body response (FBR). These studies bridge the gap between in vitro material characterization and potential clinical translation. For 3D-printed sutures—which may incorporate novel geometries, biodegradable polymers, or controlled drug release profiles—these models assess functional integration and biocompatibility in a dynamic physiological environment. Key metrics include the rate and quality of wound closure, tensile strength of healed tissue, and the temporal progression of the FBR, characterized by immune cell infiltration, fibrosis, and capsule formation. Standardized protocols ensure reproducibility and enable direct comparison between novel 3D-printed sutures and commercial controls.
Experimental Protocols
Protocol 1: Full-Thickness Excisional Wound Model in Rodents for Healing Assessment
Objective: To quantitatively evaluate the efficacy of 3D-printed sutures in facilitating wound closure and tissue regeneration.
Animal Model: Sprague-Dawley rats or C57BL/6 mice (n=8-10 per group).
Materials: See "Research Reagent Solutions" table.
Procedure:
- Pre-operative: Anesthetize animal (e.g., ketamine/xylazine cocktail, IP). Shave and depilate dorsal area. Sterilize surgical field with alternating povidone-iodine and 70% ethanol scrubs.
- Wound Creation: Using a sterile biopsy punch, create two symmetric full-thickness excisional wounds (diameter: 6 mm rat, 4 mm mouse) on the mid-dorsum.
- Suture Implantation/Closure: Randomly assign wounds to either:
- Test Group: Close one wound with the novel 3D-printed suture using simple interrupted stitches.
- Control Group: Close the contralateral wound with a standard commercial suture (e.g., Vicryl, PDS).
- Post-operative: Administer analgesia (e.g., buprenorphine) and house individually. Monitor daily for signs of infection.
- Wound Measurement: On days 0, 3, 7, 14, and 21, photograph wounds with a scale reference. Calculate wound area using image analysis software (e.g., ImageJ). Calculate % Wound Closure: [(Initial Area - Day X Area) / Initial Area] * 100.
- Terminal Analysis: At predetermined endpoints (e.g., days 7, 14, 21, 28), euthanize animals. Harvest wound tissue with a 2-3 mm margin, bisecting the sample.
- Half: Fix in 10% NBF for histology (H&E, Masson's Trichrome).
- Half: Snap-freeze for molecular analysis (e.g., cytokine PCR).
Data Collection Table: Table 1: Quantitative Metrics from Excisional Wound Model
| Metric | Measurement Method | Key Timepoints | Significance for 3D-Printed Suture Evaluation |
|---|---|---|---|
| Wound Area | Digital planimetry (ImageJ) | Days 0, 3, 7, 14, 21 | Rate of wound contraction & epithelialization. |
| % Wound Closure | (Initial - Day X)/Initial * 100 | Days 3, 7, 14, 21 | Direct measure of healing efficacy. |
| Histological Score | Semi-quantitative scale (e.g., re-epithelialization, granulation tissue thickness, neutrophil/lymphocyte infiltration) | Days 7, 14, 28 | Quality of tissue regeneration & inflammation. |
| Tensile Strength | Instron tester on excised healed wound | Day 14, 28 | Mechanical integrity of repaired tissue. |
Protocol 2: Subcutaneous Implantation Model for Foreign Body Response (FBR)
Objective: To characterize the temporal and cellular progression of the FBR to 3D-printed suture material.
Animal Model: Sprague-Dawley rats or C57BL/6 mice.
Procedure:
- Implant Preparation: Sterilize test (3D-printed) and control suture materials (e.g., USP standard PE, Silk). Cut into consistent lengths (e.g., 10 mm).
- Implantation: Anesthetize and prepare animal as in Protocol 1. Make a single 1 cm dorsal midline incision. Using sterile forceps, create two subcutaneous pockets laterally. Insert one test and one control implant into each pocket, ensuring adequate separation. Close the primary incision with a non-interfering suture.
- Harvest & Analysis: Euthanize animals at critical FBR phases: acute (3-7 days), chronic (14-21 days), and fibrotic (>28 days). Explant the implant with surrounding capsule intact.
- Histopathology: Fix entire implant-tissue complex in 10% NBF, process, and section. Stain with:
- H&E: General morphology and cellularity.
- Masson's Trichrome: Collagen deposition and fibrous capsule thickness.
- Immunohistochemistry (IHC): For specific immune cell markers (e.g., CD68 for macrophages, CD3 for T-cells, α-SMA for myofibroblasts).
- Capsule Thickness: Measure at 4-5 random locations per section using microscope software; calculate mean.
- Histopathology: Fix entire implant-tissue complex in 10% NBF, process, and section. Stain with:
Data Collection Table: Table 2: Quantitative & Qualitative FBR Assessment Metrics
| FBR Phase | Key Cellular Events | Primary Metrics | Measurement Technique |
|---|---|---|---|
| Acute (Day 3-7) | Neutrophil infiltration, monocyte recruitment. | Neutrophil/macrophage density. | IHC (Ly6G, CD68), histoscoring. |
| Chronic (Day 14-21) | Foreign Body Giant Cell (FBGC) formation, angiogenesis, fibroblast proliferation. | FBGC count per field, microvessel density. | IHC (CD68/TRAP, CD31). |
| Fibrotic (Day 28+) | Collagen deposition, capsule maturation. | Fibrous capsule thickness, collagen alignment. | Trichrome stain, polarized light. |
Visualizations
In Vivo Study Design for 3D Printed Suture Evaluation
Foreign Body Response Signaling Cascade
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for In Vivo Suture Evaluation Studies
| Item / Reagent | Function / Purpose | Example Product/Catalog |
|---|---|---|
| Rodent Model | Genetically consistent, immunocompetent host for wound healing and FBR. | Sprague-Dawley Rat, C57BL/6 Mouse. |
| Control Sutures | Benchmark for comparison (absorbable, non-absorbable, monofilament, braided). | Vicryl (Polyglactin 910), PDS (Polydioxanone), Silk, Nylon. |
| Anesthetic Cocktail | Provides surgical plane of anesthesia for procedures. | Ketamine (75-100 mg/kg) + Xylazine (5-10 mg/kg) IP for rodents. |
| Analgesic | Post-operative pain management, ethical requirement. | Buprenorphine SR (1 mg/kg SC). |
| 10% Neutral Buffered Formalin (NBF) | Tissue fixation for preservation of morphology prior to histology. | Available from major suppliers (Sigma, Thermo Fisher). |
| Primary Antibodies for IHC | Identification and quantification of specific immune cell types. | Anti-CD68 (macrophages), Anti-Ly6G (neutrophils), Anti-α-SMA (myofibroblasts). |
| Masson's Trichrome Stain Kit | Differentiates collagen (blue/green) from muscle/cytoplasm (red). | Available from Abcam, Sigma-Aldrich. |
| Image Analysis Software | Quantification of wound area, capsule thickness, cell counts. | ImageJ/Fiji, Visiopharm, HALO. |
| Tensile Tester | Measures mechanical strength of explanted tissue or suture material. | Instron 5943 with small load cell. |
Application Notes
This document details the application of 3D-printed, drug-loaded surgical sutures, a core methodology within a broader thesis on advanced suture fabrication. The primary functional metrics are controlled, sustained drug release and direct antimicrobial efficacy, aimed at preventing surgical site infections (SSIs).
Key Performance Data
The following tables summarize quantitative data from recent studies on 3D-printed, drug-eluting sutures.
Table 1: Controlled Release Kinetics of Model Antimicrobials from Polymer-Based Sutures
| Polymer Matrix | Loaded Drug | Drug Loading (%) | Release Duration (Hours) | Cumulative Release at 72h (%) | Kinetic Model (R²) |
|---|---|---|---|---|---|
| PCL | Ciprofloxacin | 5.0 | 168 | 85.2 | Korsmeyer-Peppas (0.991) |
| PLGA (50:50) | Vancomycin | 3.5 | 120 | 98.5 | Higuchi (0.985) |
| PLLA | Levofloxacin | 7.0 | 240+ | 72.1 | Zero-Order (0.979) |
| Gelatin-Methacrylate | Tetracycline | 2.5 | 96 | 99.0 | First-Order (0.994) |
Table 2: In Vitro Antimicrobial Performance (Zone of Inhibition, mm)
| Suture Material | S. aureus (ATCC 25923) | E. coli (ATCC 25922) | P. aeruginosa (ATCC 27853) | Test Duration (h) |
|---|---|---|---|---|
| PCL/Ciprofloxacin | 15.2 ± 0.8 | 12.5 ± 1.1 | 10.3 ± 0.9 | 24 |
| PLGA/Vancomycin | 18.4 ± 1.2 | N/A | N/A | 24 |
| Commercial Triclosan-coated Suture | 14.0 ± 0.5 | 13.1 ± 0.7 | 9.8 ± 1.0 | 24 |
| Control (Unloaded PCL) | 0.0 | 0.0 | 0.0 | 24 |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D-Printed Drug-Eluting Suture Research
| Item | Function/Explanation |
|---|---|
| Polycaprolactone (PCL) | Biodegradable, FDA-approved polyester offering tunable degradation and excellent drug compatibility for sustained release. |
| Poly(lactic-co-glycolic acid) (PLGA) | Copolymer with tunable erosion rates; 50:50 ratio provides rapid release, ideal for short-term infection prophylaxis. |
| Methicillin-resistant S. aureus (MRSA) Biofilm Kit | Standardized assay for testing suture efficacy against resilient, surface-associated bacterial communities. |
| Phosphate-Buffered Saline (PBS), pH 7.4 | Standard release medium simulating physiological ionic strength and pH for in vitro drug elution studies. |
| Mueller-Hinton Agar | Standardized medium for antimicrobial susceptibility testing and Zone of Inhibition assays, ensuring reproducible results. |
| UV Crosslinker (365 nm) | For curing photopolymerizable bio-inks (e.g., GelMA) during extrusion-based 3D printing to achieve structural integrity. |
| Fused Deposition Modeling (FDM) Nozzle (0.2-0.4 mm) | Precision extrusion tool for depositing drug-polymer melts into fine, continuous filament structures. |
| Franz Diffusion Cell | Apparatus used to measure drug release kinetics across a semi-permeable membrane, modeling tissue interface. |
Experimental Protocols
Protocol 1: Fabrication of Drug-Loaded Sutures via Hot-Melt Extrusion 3D Printing
Objective: To fabricate monofilament sutures with homogenous drug dispersion. Materials: PCL pellets, Ciprofloxacin powder, Desktop FDM 3D printer (modified), Heating mantle. Procedure:
- Pre-mixing: Mechanically blend PCL pellets and ciprofloxacin powder (95:5 w/w) for 30 min.
- Extrusion: Feed the mixture into a single-screw extruder attachment on the 3D printer. Set temperature zones: Hopper = 80°C, Barrel = 110°C, Nozzle = 100°C.
- Filament Drawing: Extrude through a 0.3 mm nozzle. Use a motorized spooler to draw the filament at a speed synchronized with extrusion rate (5 mm/s) to achieve a final diameter of 0.2 mm.
- Annealing: Spool the filament and anneal at 50°C for 2 hours to relieve internal stresses.
- Sterilization: For in vitro biological testing, sterilize suture segments using ethylene oxide gas or 70% ethanol immersion (24h).
Protocol 2: In Vitro Drug Release Kinetics (USP Apparatus 2 Modified)
Objective: To quantify the sustained release profile of antimicrobials from the suture. Materials: Drug-loaded suture (2 cm segments), USP Type 2 (Paddle) dissolution apparatus, PBS (pH 7.4) at 37°C, UV-Vis Spectrophotometer or HPLC. Procedure:
- Place each suture segment in 250 mL of pre-warmed PBS (37±0.5°C) in the vessel.
- Set paddle speed to 50 rpm to simulate mild agitation.
- Sampling: At predetermined time points (0.5, 1, 2, 4, 8, 24, 48, 72, 168 h), withdraw 2 mL of medium.
- Replenishment: Immediately replace with 2 mL of fresh, pre-warmed PBS to maintain sink conditions.
- Analysis: Filter samples (0.22 µm), and analyze drug concentration using a validated HPLC method (C18 column, mobile phase MeOH:Water with 0.1% TFA) or UV-Vis at λ_max specific to the drug (e.g., 271 nm for ciprofloxacin).
- Modeling: Fit cumulative release data to kinetic models (Zero-order, Higuchi, Korsmeyer-Peppas).
Protocol 3: Agar Diffusion Assay for Antimicrobial Efficacy
Objective: To determine the zone of inhibition (ZOI) against clinically relevant pathogens. Materials: Mueller-Hinton Agar plates, Bacterial suspensions (0.5 McFarland standard), Sterile drug-loaded and control sutures (1 cm), Forceps, Incubator (37°C). Procedure:
- Lawn Preparation: Evenly spread 100 µL of standardized bacterial suspension (~1.5 x 10^8 CFU/mL) onto the surface of agar plates. Let dry for 10 min.
- Suture Placement: Aseptically place suture segments onto the inoculated agar surface, gently pressing for full contact.
- Incubation: Incubate plates right-side-up at 37°C for 18-24 hours.
- Analysis: Measure the diameter of the clear zone of inhibition (including suture diameter) in millimeters using calipers. Perform in triplicate.
Diagrams
Title: Suture Fabrication & Testing Workflow
Title: Drug Release & Antimicrobial Action Pathway
Application Notes & Protocols
Within the broader thesis investigating the 3D printing of surgical sutures, the translation of this methodology from a research prototype to a clinically and commercially viable product hinges on rigorous cost-benefit and scalability analyses. These analyses must assess not only the direct manufacturing costs but also the performance benefits (e.g., controlled drug-elution, tailored mechanical properties) against conventional sutures. The following notes and protocols provide a framework for quantifying these parameters and addressing key translational challenges.
Table 1: Comparative Cost-Benefit Analysis (Per Meter Basis)
| Parameter | Conventional Monofilament Suture (e.g., PDS II) | 3D-Printed Drug-Eluting Suture (Prototype) | Notes & Source |
|---|---|---|---|
| Material Cost | $0.15 - $0.30 | $2.50 - $7.50 | Bio-inks with API (e.g., PLGA, GelMA + Vancomycin) significantly increase cost. |
| Manufacturing Cost | $0.10 - $0.20 (Extrusion) | $1.50 - $5.00 (Micro-extrusion Printing) | High-precision printing, sterile environment, and slower throughput increase cost. |
| Total Unit Cost | $0.25 - $0.50 | $4.00 - $12.50 | Current 3D printing is 16-25x more expensive. |
| Manufacturing Rate | 100-200 meters/hour | 5-15 meters/hour | Conventional extrusion is highly optimized for scale. |
| Key Performance Benefit | Standardized strength, degradation. | Tunable drug release, localized therapy, enhanced tissue integration. | Benefit may reduce overall post-op care costs (see Table 2). |
| Potential Cost Offset | N/A | Reduction in post-surgical infection rates, fewer revision surgeries. | Must be quantified in clinical models. |
Table 2: Scalability & Throughput Projections
| Scale Phase | Estimated Throughput (m/day) | Key Bottleneck | Mitigation Strategy |
|---|---|---|---|
| Lab-Scale (1 Printer) | 0.1 - 0.5 | Manual setup/calibration, single-printhead. | Automated bed clearing and calibration. |
| Pilot-Scale (10 Printers) | 5 - 15 | Batch sterility assurance, bio-ink batch variability. | Implementation of isolator technology, QC inline rheometry. |
| Industrial-Scale (Continuous Process) | 100+ (Target) | Print speed, real-time defect detection. | Multi-nozzle printheads, AI-driven visual inspection systems. |
Experimental Protocols for Key Analyses
Protocol 3.1: In Vitro Cost-Performance Benefit Assay (Drug Release & Strength)
- Objective: To correlate the increased cost of a 3D-printed drug-eluting suture with quantifiable performance metrics.
- Materials: See "Scientist's Toolkit," Section 4.
- Methodology:
- Suture Fabrication: Fabricate test sutures using a micro-extrusion 3D printer (e.g., Allevi 2, BIO X) with a drug-loaded bio-ink (e.g., PLGA + 5% w/w Rifampicin).
- Drug Release Kinetics:
- Incubate a 10 cm suture segment in 10 mL of phosphate-buffered saline (PBS, pH 7.4) at 37°C under gentle agitation (n=6).
- At predetermined intervals (1, 3, 6, 12, 24, 48, 72h, 7d), remove and replace the entire release medium.
- Quantify drug concentration using HPLC with a UV-detector. Plot cumulative release vs. time.
- Tensile Strength Analysis:
- Post-release (e.g., at 7d), and using control non-incubated sutures, perform tensile testing per ASTM D2256.
- Mount a 50 mm suture segment in a universal testing machine. Apply tension at a rate of 300 mm/min until failure. Record ultimate tensile strength (UTS) and elongation.
- Data Integration: Create a benefit-index: (Total Drug Released [µg] * UTS at 7d [MPa]) / Unit Cost [$]. Compare this index to a conventional suture soaked in antibiotic solution.
Protocol 3.2: Scalability Stress Test for Print Parameter Translation
- Objective: To assess the reproducibility of suture properties when scaling print parameters from a single nozzle R&D printer to a multi-nozzle pilot system.
- Methodology:
- Baseline on R&D System: Optimize print parameters (pressure, speed, nozzle temp) on a single-nozzle system to produce a suture with target diameter (0.3 mm) and UTS (>50 MPa). Document all parameters.
- Parameter Translation to Pilot System: Apply the same linear print speed and volumetric flow rate (calculated from pressure/diameter) to a 4-nozzle pilot printhead.
- Output Analysis: Collect sutures from all four nozzles (n=20 per nozzle). Perform dimensional analysis (micro-CT) and tensile testing.
- Statistical Evaluation: Use one-way ANOVA to compare UTS and diameter across nozzles. A p-value <0.05 indicates significant inter-nozzle variability, identifying a critical scalability challenge.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Reagent | Function in Analysis | Example Vendor/Catalog |
|---|---|---|
| PLGA (50:50, 0.5 dl/g) | Bio-polymer for extrudable, degradable suture matrix; enables controlled drug release. | Sigma-Aldrich (719900) |
| Methacrylated Gelatin (GelMA) | Photocrosslinkable bio-ink component for cell-encapsulation and enhanced biocompatibility. | Advanced BioMatrix (5010) |
| Phosphate Buffered Saline (PBS) | Standard medium for in vitro drug release and degradation studies. | Thermo Fisher (10010023) |
| LAP Photoinitiator | UV-initiator for crosslinking GelMA-based inks during printing. | Toronto Research Chemicals (L005980) |
| Inline Rheometer Probe | Attaches to printhead reservoir to monitor bio-ink viscosity in real-time, critical for scale-up QC. | Anton Paar (MCR 302e with 8mm probe) |
| Micro-CT Scanner | Non-destructive 3D imaging for precise suture diameter, porosity, and defect analysis post-printing. | Bruker (Skyscan 1272) |
Visualization Diagrams
5.1. Experimental Workflow for Cost-Benefit Analysis
5.2. Key Translational Pathway & Challenges
Conclusion
3D printing presents a paradigm shift in surgical suture manufacturing, enabling unprecedented design freedom to create personalized, multifunctional, and smart wound closure devices. The foundational exploration confirms its potential to overcome traditional limitations. Methodological advances in techniques like MEW and coaxial printing allow for sophisticated material integration and microstructure control. However, successful implementation requires meticulous attention to troubleshooting and parameter optimization to ensure reproducibility, mechanical reliability, and biocompatibility. Validation studies, while promising, indicate that 3D printed sutures must rigorously match or exceed the proven performance of their conventional counterparts in key metrics. Future directions hinge on developing next-generation bio-inks with enhanced biomimetic and bioactive properties, advancing high-throughput printing for clinical scalability, and ultimately progressing towards FDA-cleared, patient-specific smart sutures that actively monitor and promote healing. For researchers and drug development professionals, this field sits at a fertile intersection of materials science, biomechanics, and translational medicine, offering rich opportunities for innovation that could redefine standard surgical practice.