Immunomodulatory Biomaterials: Mastering Host Interactions for Regenerative Medicine and Advanced Drug Delivery
This article provides a comprehensive analysis of the dynamic interplay between biomaterials and the host immune system, a critical determinant for the success of medical implants, tissue engineering, and drug...
Immunomodulatory Biomaterials: Mastering Host Interactions for Regenerative Medicine and Advanced Drug Delivery
Abstract
This article provides a comprehensive analysis of the dynamic interplay between biomaterials and the host immune system, a critical determinant for the success of medical implants, tissue engineering, and drug delivery systems. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational immunology, advanced material design strategies, and state-of-the-art analytical techniques. We explore the evolution from bioinert to bioactive and smart immunomodulatory materials, detailing how physical, chemical, and biological properties can be engineered to steer immune responses toward pro-regenerative outcomes. The content further addresses critical challenges in biocompatibility and clinical translation, evaluates current in vitro and in vivo validation methodologies, and compares the performance of natural and synthetic biomaterials. This resource aims to equip experts with the knowledge to design next-generation biomaterials that proactively harness the immune system for improved therapeutic efficacy.
The Immune System Meets Biomaterials: Decoding the Foreign Body Response and Foundational Interactions
The Foreign Body Response: A Sequential Biological Process
The implantation of a biomaterial initiates a complex and sequential host reaction known as the Foreign Body Response (FBR). This process begins with surgical injury and can culminate in the isolation of the implant within a dense fibrous capsule, which often compromises the device's functionality [1] [2]. The FBR is an inevitable host reaction marked by a cascade of inflammatory and fibrotic processes, governed by a dynamic network of molecular signaling pathways, cellular mechanosensing, and intercellular communication [1].
The sequence of events unfolds as follows:
- Surgical Injury and Acute Inflammation: Implantation causes local tissue damage and rupture of blood vessels, leading to blood-material interactions and the formation of a provisional matrix containing fibrin and inflammatory mediators. This matrix facilitates the recruitment of innate immune cells, primarily neutrophils, which characterize the initial acute inflammatory phase [2].
- Chronic Inflammation and Monocyte/Macrophage Involvement: If the acute inflammation does not resolve, or due to the persistent presence of the foreign material, the response transitions to a chronic phase. This stage is dominated by monocytes and macrophages. Macrophages attempt to phagocytose the material, and upon failing, may fuse to form foreign body giant cells (FBGCs) on the implant surface [2].
- Fibrosis and Encapsulation: The prolonged inflammatory milieu stimulates the activation and proliferation of fibroblasts. These cells deposit dense layers of collagen and extracellular matrix, forming a avascular fibrous capsule that walls off the implant from the surrounding tissue [1] [2]. This encapsulation can lead to functional failure of devices such as sensors, drug-delivery systems, and implants [3].
Table 1: Key Cellular Players in the Foreign Body Response.
| Cell Type | Role in FBR | Key Outputs |
|---|---|---|
| Neutrophils | First responders; initiate acute inflammation; release reactive oxygen species (ROS) and enzymes. | Cytokines, proteases, DAMPs. |
| Macrophages | Central regulators of inflammation and fibrosis; attempt phagocytosis; form FBGCs. | Pro-inflammatory (TNF-α, IL-6) & pro-fibrotic cytokines; growth factors. |
| Fibroblasts | Effector cells of fibrosis; produce and remodel extracellular matrix (ECM). | Collagen, fibronectin; fibrous capsule. |
| Foreign Body Giant Cells (FBGCs) | Formed from macrophage fusion; persist on material surface. | Sustained inflammatory signals; enzymes. |
Quantitative Analysis of FBR Severity and Biomaterial Performance
The severity of the FBR and the performance of novel biomaterials are quantified using specific histological, molecular, and functional metrics. These parameters allow for the direct comparison between different materials and the evaluation of new anti-FBR strategies.
Table 2: Quantitative Metrics for Assessing the Foreign Body Response In Vivo.
| Assessment Method | Quantitative Parameters | Interpretation and Significance |
|---|---|---|
| Histological Staining (e.g., H&E, Masson's Trichrome) | Fibrous capsule thickness (μm); Cellular density and composition. | Thinner capsule indicates better biocompatibility; identifies inflammatory cell infiltration. |
| Immunohistochemistry (IHC) | Expression levels of markers (e.g., CCR-7, TNF-α, IL-6, IL-10). | Quantifies pro- vs. anti-inflammatory responses at the implant-tissue interface. |
| Proteome Profiler Antibody Array | Relative concentration of multiple cytokines/chemokines from peri-implant tissue. | Provides a systemic view of the immune and inflammatory status. |
| Functional Device Testing | Device longevity (days); Signal fidelity; Drug delivery efficacy. | Measures the ultimate clinical impact of the FBR on implant performance. |
Recent research on a novel immunocompatible elastomer platform, termed EVADE, provides a benchmark for high-performance, anti-fibrotic materials. In a subcutaneous implantation model in C57BL/6 mice, EVADE (H90 formulation) demonstrated a significantly reduced fibrotic capsule thickness of 10–40 μm after one month, compared to 45–135 μm for medical-grade PDMS controls [3]. This superior performance was maintained long-term, with negligible inflammation and capsule formation observed after one year in mice and two months in non-human primate models [3]. Proteomic analysis revealed that EVADE implants significantly reduced the expression of the pro-inflammatory alarmins S100A8/A9 at the implant site, suggesting a key molecular target for mitigating fibrosis [3].
Detailed Experimental Protocol for Subcutaneous Implantation and FBR Evaluation
This protocol details a standard methodology for evaluating the host response to biomaterials in a rodent subcutaneous implantation model, synthesizing established practices from the field [2] [3].
Materials and Pre-implantation Preparation
- Biomaterials: Fabricate test materials (e.g., polymer discs of EVADE, PDMS) to standardized dimensions (e.g., 5 mm diameter, 1 mm thickness). Adjust material modulus to be comparable between groups if necessary [3].
- Animals: C57BL/6 mice (or other appropriate strain), 8-12 weeks old.
- Sterilization: Sterilize all materials and surgical instruments using ethylene oxide gas or autoclaving (where material properties allow).
- Anesthesia: Prepare a ketamine/xylazine mixture (e.g., 100 mg/kg ketamine and 10 mg/kg xylazine) for intraperitoneal injection.
Surgical Implantation Procedure
- Anesthetize the mouse and confirm the depth of anesthesia by the absence of a pedal reflex.
- Shave the dorsal fur and disinfect the surgical site with alternating scrubs of betadine and 70% ethanol.
- Using aseptic technique, make a single midline incision of approximately 1 cm in the dorsal skin.
- Create subcutaneous pockets by blunt dissection laterally from the incision. Each mouse can accommodate multiple implants (e.g., one per quadrant), with each pocket sized to fit the implant without excessive tension.
- Insert one sterile material disc into each subcutaneous pocket. Include sham-operated controls (incision without implant) if required by the experimental design.
- Close the incision with surgical wound clips or sutures.
- Monitor the animals until fully recovered from anesthesia and provide post-operative analgesia as approved by the institutional animal care and use committee.
Post-implantation Analysis and Tissue Harvest
- Duration: Plan endpoints based on the biological phase of interest: acute inflammation (e.g., 3-7 days), chronic inflammation and early fibrosis (e.g., 2-4 weeks), or long-term encapsulation (e.g., 1-3 months, or longer) [3].
- Euthanasia and Harvest: At the designated time point, euthanize animals according to approved protocols. Carefully excise the implant with the surrounding tissue envelope intact.
- Sample Processing:
- For histology: Fix the entire tissue-implant construct in 10% neutral buffered formalin for 24-48 hours. After fixation, carefully remove the implant to avoid damaging the tissue cavity before processing the tissue for paraffin embedding. Section tissues to 5 μm thickness.
- For protein/mRNA analysis: Dissect the tissue adjacent to the implant (a defined peri-implant area) and snap-freeze in liquid nitrogen. Store at -80°C until analysis.
Key Outcome Measures and Analytical Techniques
- Histological Evaluation: Stain sections with Hematoxylin and Eosin (H&E) for general morphology and cellular infiltration, and Masson's Trichrome for collagen deposition and fibrous capsule visualization [3]. Quantify fibrous capsule thickness from multiple, standardized locations around the implant using image analysis software.
- Immunohistochemistry (IHC): Perform IHC for specific cell markers (e.g., CCR-7 for M1 macrophages, CD206 for M2 macrophages) and inflammatory mediators (e.g., TNF-α, IL-6, S100A8/A9) [3]. Use semi-quantitative or quantitative (e.g., image analysis) scoring systems.
- Protein-Level Analysis: Use Proteome Profiler Antibody Arrays to simultaneously measure the relative levels of multiple cytokines and chemokines from homogenized peri-implant tissue lysates, following the manufacturer's protocol [3].
Molecular Signaling in the Foreign Body Response
The progression of the FBR is directed by a complex interplay of molecular signals. Key pathways involve the initial recruitment of immune cells via cytokines and chemokines, the activation of macrophages into pro-inflammatory (M1) or pro-healing (M2) phenotypes, and the subsequent activation of fibroblasts leading to fibrosis [1] [2]. Recent mechanistic studies highlight the role of specific proteins, such as the S100A8/A9 heterodimer, as critical alarmins that drive the inflammatory and fibrotic cascade. Inhibition or knockout of S100A8/A9 has been shown to substantially attenuate fibrosis in mouse models, identifying it as a promising therapeutic target [3].
The Scientist's Toolkit: Essential Reagents and Materials for FBR Research
Table 3: Key Research Reagent Solutions for Foreign Body Response Studies.
| Reagent / Material | Function and Application in FBR Research |
|---|---|
| EVADE Elastomers | A novel platform of immunocompatible elastomers (e.g., H90) used as a test material demonstrating long-term suppression of inflammation and capsule formation in vivo [3]. |
| Medical-Grade PDMS | A widely used reference/control elastomer known to elicit a standard FBR, enabling comparative assessment of new materials [3]. |
| Proteome Profiler Antibody Arrays | Membrane-based arrays used to simultaneously detect and semi-quantify multiple inflammation-related cytokines and chemokines from tissue lysates surrounding the implant [3]. |
| S100A8/A9 Inhibitors | Specific antibodies or pharmacological agents used to block the function of the S100A8/A9 alarmin complex, allowing for mechanistic studies of fibrosis [3]. |
| Cytokine-specific Antibodies | Essential reagents for immunohistochemistry (IHC) and ELISA to localize and quantify key inflammatory markers (e.g., TNF-α, IL-6, CCR-7, IL-10) in tissue sections [3]. |
| Masson's Trichrome Stain | A standard three-color staining protocol used on paraffin-embedded tissue sections to distinguish collagen (blue/green) from muscle (red) and cell nuclei (black), critical for quantifying fibrous capsule formation [3]. |
This technical guide provides an in-depth analysis of the central roles played by macrophages, neutrophils, dendritic cells, and lymphocytes in the context of biomaterial host interactions and immune responses. The successful integration of biomaterials and the subsequent tissue regeneration process are fundamentally governed by a carefully orchestrated immune response. Understanding these cellular mechanisms is paramount for researchers and drug development professionals aiming to design next-generation immunomodulatory biomaterials and therapeutic strategies. This whitepaper synthesizes current research to detail the specific functions, signaling pathways, and experimental approaches relevant to characterizing these key immune players, with a particular emphasis on their temporal coordination following biomaterial implantation.
Macrophages: The Orchestrators of Immune Response and Tissue Repair
M1/M2 Polarization and Functional Phenotypes
Macrophages are versatile innate immune cells essential for maintaining tissue homeostasis, providing host defense, and orchestrating tissue repair. They exhibit remarkable phenotypic plasticity, dynamically polarizing in response to local microenvironmental cues [4]. The classical framework describes polarization into two main phenotypes: the pro-inflammatory M1 and the anti-inflammatory or pro-regenerative M2 macrophages [5] [6].
M1 Macrophages (Classical Activation): Induced by microbial components like lipopolysaccharide (LPS) and Th1 cytokines such as interferon-gamma (IFN-γ), M1 macrophages drive pro-inflammatory responses [5] [4]. Key signaling pathways involve JAK-STAT1 activation downstream of the IFN-γ receptor, and MyD88/TRIF signaling downstream of TLR4 engagement, leading to the activation of transcription factors like NF-κB and IRF3 [4]. This results in the high production of inflammatory cytokines (e.g., TNF-α, IL-6, IL-12), generation of reactive oxygen and nitrogen species, and strong antimicrobial activity [5] [6]. They are characterized by surface markers like CD80, CD86, and high expression of MHC class II molecules [6].
M2 Macrophages (Alternative Activation): Polarized by Th2 cytokines including IL-4 and IL-13, M2 macrophages are associated with immune regulation, wound healing, and tissue regeneration [5] [4]. The IL-4Rα receptor signaling activates JAK-STAT6, along with transcription factors IRF4 and PPARγ [4]. This phenotype upregulates surface markers like the mannose receptor (CD206) and CD163, and produces anti-inflammatory factors (e.g., IL-10, TGF-β) and enzymes like Arginase-1 (Arg-1) which promote matrix deposition and repair [5] [6]. The M2 phenotype can be further subdivided into M2a, M2b, M2c, and M2d based on specific inducers and functions, with M2a being primarily linked to anti-inflammatory responses and bone regeneration [5].
caption: Table 1: Key Characteristics of M1 and M2 Macrophage Polarization
| Feature | M1 (Pro-inflammatory) | M2 (Anti-inflammatory/Pro-regenerative) |
|---|---|---|
| Primary Inducers | LPS, IFN-γ, GM-CSF [5] [4] | IL-4, IL-13, IL-10, Glucocorticoids [5] [4] |
| Key Signaling Pathways | TLR/MyD88/TRIF, JAK-STAT1, NF-κB, IRF3 [4] | IL-4R/JAK-STAT6, IRF4, PPARγ [4] |
| Characteristic Markers | CD80, CD86, MHC-II, iNOS [5] [6] | CD206, CD163, Arg-1, FIZZ1 [5] [6] |
| Major Secretory Products | TNF-α, IL-6, IL-12, IL-1β, ROS/NOS [5] [4] | IL-10, TGF-β, CCL17, CCL22, VEGF [5] [6] |
| Primary Functions | Pathogen clearance, pro-inflammatory response, antimicrobial activity [6] | Tissue repair, angiogenesis, immune regulation, matrix remodeling [5] |
The Role of Macrophages in Biomaterial Integration and Bone Regeneration
The temporal sequence of macrophage polarization is critical for successful biomaterial integration and bone regeneration. Following injury or implantation, an initial M1-dominated response is beneficial for pathogen clearance and initiation of the healing process [5]. Subsequently, a timely transition to an M2-dominated phenotype facilitates tissue repair, angiogenesis, and osteogenesis [5]. Biomaterials can be engineered with specific physical and chemical properties to actively guide this polarization. Key biomaterial properties that influence macrophage behavior include:
- Stiffness: Substrate elasticity can direct macrophage polarization [5].
- Topography and Pore Architecture: Surface geometry and scaffold microstructure provide physical cues [5].
- Hydrophilicity and Chemical Composition: Surface chemistry and the release of bioactive ions (e.g., from metals) can modulate the immune response [5] [7].
An imbalance, such as a prolonged M1 response or premature M2 polarization, can lead to chronic inflammation, fibrous encapsulation of the implant, or failed integration [5]. Therefore, designing biomaterials that encourage a dynamic shift from M1 to M2 is a key strategy in bone tissue engineering [5] [7].
Neutrophils: The First Responders
Recruitment and Core Antibacterial Functions
Neutrophils are the most abundant leukocytes in human blood and are the first immune cells recruited to sites of injury, infection, or biomaterial implantation [8] [9]. Their recruitment involves a well-defined sequence of steps: rolling, adhesion, crawling, and transmigration out of blood vessels, guided by chemokine gradients like IL-8 [8]. Upon arrival, they deploy several potent mechanisms to eliminate pathogens and clear debris [8]:
- Phagocytosis: Direct engulfment and destruction of bacteria within phagolysosomes using oxidative (e.g., Hypochlorous acid generated via Myeloperoxidase (MPO)) and non-oxidative (e.g., lysozyme, defensins) mechanisms [8].
- Degranulation: Release of pre-formed antimicrobial proteins and enzymes from cytoplasmic granules into the extracellular space [8].
- Neutrophil Extracellular Traps (NETs): A unique cell death process (NETosis) where neutrophils extrude a web of DNA decorated with histones and granule proteins (e.g., NE, MPO) to trap and neutralize pathogens [8]. NETs can be formed via NADPH oxidase (NOX)-dependent or NOX-independent pathways [8].
- Oxidative Burst: Rapid production of large quantities of reactive oxygen species (ROS) via the NADPH oxidase complex for microbial killing [8].
Neutrophils as Instructive Cells for Tissue Repair
Beyond their antibacterial role, neutrophils are critical instructors of the subsequent immune response to biomaterials. They secrete cytokines and chemokines that recruit and influence the polarization of other immune cells, particularly monocytes and macrophages [10] [9]. Their lifespan and mode of death are crucial for determining the healing outcome. Apoptotic neutrophil death followed by efferocytosis (clearance by macrophages) is a key signal that prompts macrophages to switch from a pro-inflammatory M1 to a pro-healing M2 phenotype, thereby resolving inflammation [9]. Conversely, persistent neutrophil activation or excessive NETosis can lead to chronic inflammation, tissue damage, and fibrous encapsulation of biomaterials, preventing integration [8] [9]. Recent studies show that neutrophil response is influenced by biomaterial properties such as polymer origin (natural vs. synthetic), stiffness, and surface charge [10].
Dendritic Cells: Bridging Innate and Adaptive Immunity
Subsets, Development, and Core Functions
Dendritic cells (DCs) are professional antigen-presenting cells (APCs) that form a critical bridge between the innate and adaptive immune systems [11]. They originate from bone marrow hematopoietic stem cells under the regulation of cytokines like Flt3L and key transcription factors (e.g., IRF8, PU.1) [11]. The main DC subsets include:
- Classical DCs (cDC1 and cDC2): Specialized in antigen capture and presentation. cDC1s are critical for cross-presenting antigens to CD8+ T cells, while cDC2s primarily activate CD4+ T cells [11].
- Plasmacytoid DCs (pDCs): Specialized in secreting vast amounts of Type I Interferons (IFN-α/β) in response to viral infections [11].
- Monocyte-derived DCs (moDCs): Differentiated from monocytes during inflammation [11].
- Langerhans Cells: Tissue-resident DCs in the epidermis [11].
The core functions of DCs involve antigen capture in peripheral tissues, followed by migration to secondary lymphoid organs. During migration, they undergo maturation, upregulating MHC and co-stimulatory molecules (CD80, CD86). In the lymph nodes, they present processed antigens to naïve T cells, thereby activating and polarizing antigen-specific T cell responses (e.g., Th1, Th2, Th17) [11]. DCs are also indispensable for inducing immune tolerance to self-antigens [11].
DCs in Biomaterial and Therapeutic Contexts
In the context of biomaterials, DCs can be targeted to steer immune responses toward either tolerance (for implant acceptance) or immunity (for vaccine development). DC-based therapies, such as cancer vaccines, have been explored, with the first FDA-approved DC vaccine (Sipuleucel-T) for prostate cancer [11] [12]. Biomaterial scaffolds are being used to enhance DC-based therapies by providing a 3D environment for cell delivery, controlling the release of antigens and adjuvants, and recruiting host DCs to the implantation site [12].
Lymphocytes: The Adaptive Immune Specificity
Lymphocytes, including T cells and B cells, provide antigen-specific, long-lasting adaptive immunity. Their role in the response to biomaterials is complex and shaped by the initial innate immune response.
- T Cells: Activated by DCs, T cells can exert both beneficial and detrimental effects on tissue regeneration. Cytotoxic CD8+ T cells can clear infected cells, while CD4+ Helper T cells (e.g., Th1, Th2) release cytokines that can influence macrophage polarization and osteoblast/osteoclast activity [5]. Regulatory T cells (Tregs) are crucial for suppressing excessive inflammation and promoting tolerance [7]. The success of Chimeric Antigen Receptor (CAR) T cell therapies in oncology highlights the potential of engineered lymphocyte therapies [12].
- B Cells: Primarily responsible for producing antigen-specific antibodies. Their role in the direct response to biomaterials is less characterized but contributes to the overall humoral immune response.
The interaction between biomaterials and lymphocytes is often indirect, mediated by innate immune cells like DCs and macrophages. An uncontrolled adaptive response can lead to implant rejection, while a regulated response can support healing.
Experimental Protocols and Methodologies
Protocol 1: In Vitro Assessment of Macrophage Polarization
Objective: To evaluate the immunomodulatory effect of a biomaterial surface on macrophage polarization.
Materials:
- Cells: Primary human or murine monocytes (e.g., from bone marrow or peripheral blood) or a macrophage cell line (e.g., RAW 264.7).
- Culture Reagents: Macrophage Colony-Stimulating Factor (M-CSF) for differentiation, polarization cytokines (e.g., LPS + IFN-γ for M1; IL-4 for M2), cell culture media.
- Test Material: Biomaterial scaffolds or flat substrates placed in culture wells.
- Analysis Tools: Antibodies for flow cytometry (anti-CD80, CD86, CD206, MHC-II), ELISA kits for cytokines (TNF-α, IL-12, IL-10, TGF-β), reagents for RNA extraction and qPCR (for iNOS, Arg-1, etc.).
Methodology:
- Monocyte Isolation and Differentiation: Isolate monocytes and seed them onto the test biomaterial and control surfaces (e.g., tissue culture plastic). Differentiate monocytes into naïve (M0) macrophages using M-CSF (50 ng/mL) for 5-7 days [5].
- Polarization Stimulation: Stimulate the differentiated macrophages with M1 polarizing agents (e.g., 100 ng/mL LPS + 20 ng/mL IFN-γ) or M2 polarizing agents (e.g., 20 ng/mL IL-4) for 24-48 hours. A material-only group without polarizing cytokines is essential to assess the material's intrinsic effect.
- Cell Harvest and Analysis:
- Flow Cytometry: Harvest cells and stain for M1 (CD80, CD86) and M2 (CD206) surface markers. Analyze using a flow cytometer to determine the percentage of positively stained cells [6].
- Gene Expression Analysis (qRT-PCR): Lyse cells to extract RNA. Perform reverse transcription and qPCR for M1-associated genes (iNOS, IL-12) and M2-associated genes (Arg-1, Ym1). Normalize data to a housekeeping gene (e.g., GAPDH) and use the 2^(-ΔΔCt) method for analysis [5].
- Cytokine Secretion (ELISA): Collect cell culture supernatants. Use specific ELISA kits to quantify the secretion of M1 (TNF-α, IL-12) and M2 (IL-10) cytokines according to the manufacturer's instructions.
Protocol 2: In Vitro Functional Profiling of Neutrophil Response to Biomaterials
Objective: To characterize key neutrophil functions (activation, NETosis, phagocytosis) when cultured on different biomaterials.
Materials:
- Cells: Freshly isolated human neutrophils from peripheral blood.
- Culture Reagents: Histopaque density gradient media, HBSS buffer, fluorescent probes (e.g., SYTOX Green for extracellular DNA, CM-H2DCFDA for ROS).
- Test Material: Biopolymer substrates of varying composition and stiffness.
- Analysis Tools: Fluorescent microscope, plate reader, MPO activity assay kit.
Methodology:
- Neutrophil Isolation: Isolate neutrophils from fresh human blood using density gradient centrifugation (e.g., with Histopaque) [10].
- Culture on Biomaterials: Seed purified neutrophils onto the test biomaterials and control surfaces. Culture for a defined period (e.g., 4-6 hours).
- Functional Assays:
- NETosis Assay: Stain cultures with a cell-impermeable DNA dye (e.g., SYTOX Green). Quantify fluorescence, which indicates extracellular DNA release, using a plate reader or image the fibrous NET structures using fluorescence microscopy [8] [10].
- Reactive Oxygen Species (ROS) Production: Load cells with a ROS-sensitive fluorescent dye (e.g., CM-H2DCFDA) before seeding. Measure fluorescence intensity over time as an indicator of oxidative burst [8] [10].
- Phagocytosis Assay: Incubate neutrophils with fluorescently labeled particles (e.g., pHrodo E. coli bioparticles). Measure internalized fluorescence after quenching extracellular signal [8].
- Cell Survival/Death Assay: Use a viability dye (e.g., Propidium Iodide) and an apoptosis marker (e.g., Annexin V) to distinguish between apoptotic and necrotic neutrophils via flow cytometry [10].
caption: Table 2: Key Parameters for Profiling Neutrophil-Biomaterial Interactions In Vitro
| Parameter Measured | Experimental Assay | Key Reagents/Tools | Interpretation of Results |
|---|---|---|---|
| NET Formation | Fluorescence-based NETosis assay [8] [10] | SYTOX Green, Anti-citrullinated Histone H3 (CitH3) Antibody | High fluorescence/extensive fibrous structures indicate strong neutrophil activation and NET release. |
| ROS Production | Oxidative burst assay [8] [10] | CM-H2DCFDA, Dihydrorhodamine 123 | Increased fluorescence intensity indicates elevated ROS generation, a key bactericidal mechanism. |
| Cell Viability & Death Mode | Annexin V/PI staining & flow cytometry [10] | Annexin V-FITC, Propidium Iodide (PI) | High Annexin V+/PI- (apoptosis) is desirable for resolution; High PI+ (necrosis) can promote inflammation. |
| Cytokine/Chemokine Release | Multiplex ELISA of culture supernatant [10] | Multiplex cytokine array (e.g., for IL-8, TNF-α) | Identifies the secretory profile, indicating the pro-inflammatory or regulatory role of neutrophils. |
| Phagocytic Capacity | Phagocytosis of fluorescent bioparticles [8] | pHrodo Green E. coli BioParticles | A decrease in fluorescence over time (after quenching) indicates efficient particle internalization. |
Signaling Pathways and Cellular Crosstalk
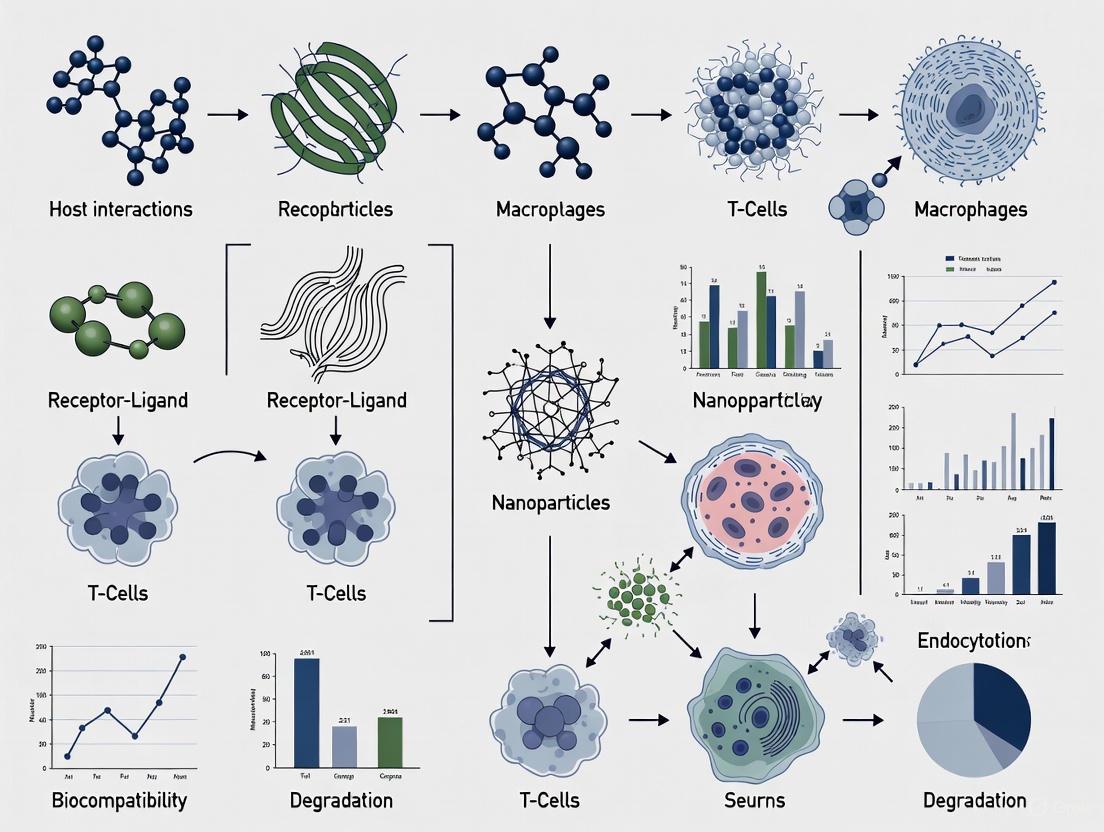
The following diagrams illustrate the core signaling pathways and the sequential crosstalk between immune cells in response to biomaterials.
caption: Figure 1: Signaling pathways driving macrophage M1 and M2 polarization.
caption: Figure 2: Sequential crosstalk and orchestration between key immune cells following biomaterial implantation.
The Scientist's Toolkit: Essential Research Reagents
caption: Table 3: Key Research Reagent Solutions for Immune Cell Studies
| Reagent / Tool | Primary Function in Research | Specific Application Example |
|---|---|---|
| Recombinant Cytokines (e.g., M-CSF, IFN-γ, IL-4, IL-13) | Direct polarization and differentiation of immune cells in vitro. | Differentiating monocytes to macrophages (M-CSF); polarizing macrophages to M1 (IFN-γ + LPS) or M2 (IL-4) [5] [4]. |
| Fluorescent Conjugated Antibodies (for Flow Cytometry) | Identification and phenotyping of cell populations via surface and intracellular markers. | Staining for M1 markers (CD80, CD86) and M2 markers (CD206) on macrophages; identifying DC subsets (CD11c, CD141, CD1c) [5] [11]. |
| ELISA Kits | Quantification of specific protein secretion (cytokines, chemokines) in cell culture supernatants. | Measuring TNF-α or IL-12 (M1) and IL-10 or TGF-β (M2) to assess macrophage polarization [5]. |
| SYTOX Green / Anti-CitH3 Antibody | Detection and quantification of Neutrophil Extracellular Traps (NETs). | Staining extracellular DNA and citrullinated histones to visualize and quantify NETosis in response to biomaterials [8]. |
| Flt3 Ligand (Flt3L) | Expansion and differentiation of classical DC (cDC) precursors in vitro and in vivo. | Generating large numbers of DCs from bone marrow cultures for functional studies or therapeutic applications [11]. |
| pHrodo BioParticles | Measurement of phagocytic activity. | Neutrophils or macrophages ingest these particles, which fluoresce brightly in the acidic phagolysosome, allowing phagocytosis quantification [8]. |
The interaction between biomaterials and the biological environment is a critical determinant of their success or failure in medical applications. Upon implantation or injection, the surface of any biomaterial is immediately coated by a dynamic layer of adsorbed biomolecules, predominantly proteins, forming what is known as the "protein corona" [13] [14]. This corona represents the primary interface between the synthetic material and the host's biological systems, effectively creating a new biological identity that overwrites the material's original synthetic properties [15] [13]. The composition and behavior of this protein layer fundamentally dictate subsequent immune recognition, inflammatory responses, and ultimately, therapeutic efficacy [16] [15].
The formation of the protein corona is not a passive process but rather a dynamic exchange of biomolecules that evolves as the material transitions through different biological compartments [13]. This review synthesizes current understanding of how the protein corona mediates immune recognition, with particular emphasis on the physicochemical determinants of corona composition, subsequent immune signaling pathways activated, and advanced computational approaches for predicting these interactions. Within the broader context of biomaterial-host interactions, understanding and controlling corona formation represents a paradigm shift from designing bioinert materials to actively engineering bioactive interfaces that direct favorable immune responses [16].
The Fundamental Nature of the Protein Corona
Structural Organization and Dynamics
The protein corona is structurally organized into two distinct layers with different stability and exchange kinetics. The hard corona consists of proteins with high binding affinity that are directly adsorbed to the nanoparticle surface through electrostatic and hydrophobic interactions [13]. This layer remains stable for extended periods and maintains its integrity even in dynamic biological environments. Surrounding this core is the soft corona, comprising proteins with weaker binding affinity that undergo continuous exchange with the surrounding biological milieu [13]. This dynamic outer layer fluctuates rapidly in response to changes in the biological environment, making its characterization methodologically challenging.
The corona formation follows a temporal evolution where small, highly mobile proteins like albumin initially adsorb to the surface but are gradually displaced by proteins with higher binding affinities—a phenomenon known as the Vroman effect [13]. This process reaches equilibrium typically within 30-60 minutes for many nanomaterial systems, though the exact kinetics depend on material properties and biological conditions [13].
Key Factors Influencing Corona Composition
Multiple factors determine the precise composition of the protein corona, creating a complex "personalized" profile that varies based on both material properties and biological context [15].
Table 1: Factors Influencing Protein Corona Composition
| Factor Category | Specific Parameters | Impact on Corona Composition |
|---|---|---|
| Nanoparticle Properties | Size, Shape, Surface chemistry, Hydrophobicity/hydrophilicity, Surface charge (ζ-potential), Material composition | Smaller particles have higher curvature affecting protein binding; hydrophobic surfaces promote more protein unfolding; surface charge determines electrostatic interactions |
| Biological Environment | Protein source (species), Protein concentration, Biological fluid composition (plasma, BALF, etc.), Disease state, Temperature, pH | Disease states alter plasma composition; protein concentration affects binding kinetics; different biological fluids contain distinct protein profiles |
| Temporal Factors | Incubation time, Administration route, Temporal disease progression | Corona evolves over time through Vroman effect; disease progression dynamically alters available proteins |
The physicochemical properties of the nanoparticle surface profoundly influence corona formation. Surface hydrophobicity drives protein adsorption through hydrophobic interactions, often resulting in protein unfolding and denaturation [13]. Hydrophobic nanoparticles typically adsorb approximately twice as much protein as hydrophilic counterparts and form more stable coronas with reduced dynamic exchange [13]. Surface charge, represented by ζ-potential, determines electrostatic interactions with charged protein domains, with highly positive or negative surfaces attracting oppositely charged proteins [17].
The biological context introduces significant variability in corona composition. Recent research demonstrates that disease states dynamically alter plasma biomolecule profiles, which in turn dramatically affects corona composition and subsequent immune responses [15]. For instance, in murine models of LPS-induced endotoxemia, the corona formed at different time points post-inflammatory challenge (3hr vs 8hr) exhibited distinct protein fingerprints and elicited dramatically different macrophage responses [15].
Quantitative Analysis of Corona-Mediated Immune Responses
Immune Cell Responses to Corona-Coated Materials
The protein corona directly influences immune recognition by presenting specific surface epitopes and ligands to immune cells. The table below summarizes key findings from recent studies investigating immune responses to protein corona-coated biomaterials.
Table 2: Immune Cell Responses to Corona-Coated Biomaterials
| Immune Cell Type | Material | Key Corona-Mediated Effects | Experimental Model |
|---|---|---|---|
| Macrophages | Titanium with hydrophilic surface | ↓ Pro-inflammatory cytokines (IL-1β, IL-6, TNF); ↑ Anti-inflammatory cytokines (IL-4, IL-10); ↑ M2 phenotype | In vitro (C57BL/6J mice) [16] |
| Macrophages | PLGA NPs with inflammatory plasma corona | ↑ Co-stimulatory molecules (CD80: 1.43-fold, CD86: 2.30-fold); ↑ PD-L1 (14.61-fold); ↑ Pro-inflammatory cytokines (TNFα, IL-6, CXCL1) | In vitro (bone marrow-derived macrophages) [15] |
| Macrophages | Nanoengineered surfaces (70 nm topography) | Reduced inflammatory response; Alterations in adsorbed protein composition (↓ clusterin, ↑ ApoB and IgG gamma) | In vitro (macrophages) [18] |
| Neutrophils | Hydrophilic Titanium | ↓ Cytokine release; ↓ NET formation | In vitro (C57BL/6J mice) [16] |
| Neutrophils | Hydrophobic PTFE | ↑ NET formation; ↑ ROS generation; ↑ Histone citrullination | In vitro (Human PBMC) [16] |
Key Corona Proteins and Their Immune Implications
Machine learning analysis of extensive protein corona databases has identified specific proteins whose adsorption consistently correlates with distinct immune responses and biodistribution patterns.
Table 3: Key Corona Proteins and Their Immunological Significance
| Protein | Immune/Biological Function | Impact on Nanoparticle Fate |
|---|---|---|
| Apolipoprotein E (APOE) | Lipoprotein mediating cellular uptake via LDL receptor pathways | Enhances targeting to brain and liver; associated with receptor-mediated uptake [17] |
| Apolipoprotein B-100 (APOB-100) | Principal lipoprotein in LDL particles | Promotes liver targeting via LDL receptor pathways [17] |
| Complement C3 (C3) | Central component of complement system | Opsonization; promotes immune recognition and clearance; enhances uptake by monocytes [17] |
| Clusterin (CLUS/ApoJ) | Dysopsonin, chaperone protein | Reduces nonspecific cell uptake; may impart "stealth" properties [17] |
| Immunoglobulins (IgG) | Antibody-mediated opsonization | Enhances phagocytic clearance via Fc receptor recognition [18] |
| Albumin | Most abundant serum protein | Can impart stealth properties at high coverage; initial corona component [13] |
Meta-analysis of 817 nanoparticle formulations revealed that silica, polystyrene, and lipid-based nanoparticles smaller than 100 nm with moderately negative to neutral ζ-potentials preferentially bind APOE and APOB-100, which are linked to receptor-mediated uptake and enhanced delivery efficiency [17]. In contrast, metal and metal-oxide nanoparticles with highly negative surface charge enrich complement component C3, indicating greater likelihood of immune recognition and clearance [17].
Molecular Mechanisms and Signaling Pathways
The protein corona influences immune responses through specific receptor-mediated signaling pathways. Integrated multi-omics approaches have identified Toll-like receptor 4 (TLR4) signaling as a central pathway activated by specific corona compositions.
Diagram 1: TLR4/MyD88/NF-κB Signaling Pathway in Corona-Mediated Immune Activation
Pharmacological inhibition and genetic knockout studies have validated that specific nanoparticle coronas mediate immune activation through the TLR4/MyD88/NF-κB signaling axis [15]. Coronas enriched with damage-associated molecular patterns (DAMPs) or pathogen-associated molecular patterns (PAMPs) from inflammatory environments can directly activate pattern recognition receptors on immune cells, initiating a cascade that leads to NF-κB translocation and pro-inflammatory gene expression.
The diagram illustrates how corona components (such as LPS or LPS-binding proteins enriched in inflammatory conditions) engage TLR4 receptors, triggering downstream signaling through the MyD88 adaptor protein, resulting in IKK complex activation, NF-κB nuclear translocation, and ultimately production of pro-inflammatory cytokines and immune activation.
Experimental Methodologies for Corona Research
Standard Protocol for Protein Corona Isolation and Characterization
The following workflow represents a standardized approach for protein corona isolation and characterization, synthesized from multiple methodological approaches [15] [13] [18].
Diagram 2: Protein Corona Isolation and Characterization Workflow
Step 1: Nanoparticle Formulation and Characterization
- Synthesize nanoparticles with defined physicochemical properties (size, charge, hydrophobicity)
- Common systems include PLGA, titanium, silica, and lipid-based nanoparticles [15] [17]
- Characterize baseline properties using DLS (size, PDI), ζ-potential measurements (surface charge), and TEM (morphology) [13]
Step 2: Biological Fluid Incubation
- Incubate nanoparticles with relevant biological fluid (human plasma, serum, BALF)
- Standard conditions: 37°C with gentle agitation for 30-60 minutes [13]
- Protein concentration typically 50-100% of physiological concentration [17]
- Consider disease-specific biofluids for personalized corona profiling [15]
Step 3: Corona Isolation
- Separate corona-coated nanoparticles from unbound proteins via centrifugation
- Alternative methods: magnetic separation, size-exclusion chromatography [13]
- Centrifugation parameters: typically 14,000-20,000 × g for 15-30 minutes [15]
Step 4: Washing and Corona Stabilization
- Carefully wash pellet with mild buffer (e.g., PBS) to remove loosely associated proteins
- Repeat centrifugation 2-3 times to isolate hard corona [13]
- Note: Washing may remove components of the soft corona [13]
Step 5: Corona Characterization
- SDS-PAGE: Qualitative protein fingerprinting [15]
- LC-MS/MS: Quantitative proteomic analysis [17]
- DLS: Hydrodynamic size and aggregation state [15]
- Additional techniques: ITC, FTIR, circular dichroism for structural information [13] [14]
Step 6: Biological Response Assessment
- Incubate corona-coated nanoparticles with immune cells (e.g., macrophages)
- Assess cellular association/uptake via flow cytometry [15]
- Measure cytokine secretion via multiplex ELISA [15]
- Evaluate surface marker expression (CD80, CD86, PD-L1) via flow cytometry [15]
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Protein Corona Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Nanoparticle Systems | PLGA, Titanium, Silica, Gold, Lipid NPs | Model substrates for corona formation studies; PLGA particularly common due to FDA approval [15] |
| Biological Fluids | Human plasma, Fetal Bovine Serum, BALF | Source of proteins for corona formation; human plasma most relevant for clinical translation [17] |
| Characterization Instruments | DLS, SDS-PAGE, LC-MS/MS, Flow Cytometry | Quantify corona size, composition, and biological effects [15] [13] |
| Cell Culture Models | Bone marrow-derived macrophages, THP-1, RAW 264.7 | Assess immune responses to corona-coated materials [16] [15] |
| Cytokine Analysis | Multiplex ELISA, Luminex arrays | Quantify immune activation through cytokine secretion profiles [15] |
Advanced Prediction and Engineering Approaches
Machine Learning for Corona Composition Prediction
Machine learning (ML) approaches have emerged as powerful tools for predicting protein corona composition based on nanoparticle properties, addressing the methodological challenges and time-consuming nature of experimental characterization [17] [14]. The creation of the Protein Corona Database (PC-DB) with 817 unique nanoparticle formulations and quantitative profiles for 2497 proteins has enabled the development of predictive models with high accuracy (ROC-AUC > 0.85) [17].
Feature importance analysis from these models identifies NP size, ζ-potential, and incubation time as the most influential predictors of protein adsorption [17]. Commonly employed algorithms include LightGBM and XGBoost, which can handle the complex, non-linear relationships between nanoparticle properties and corona composition [17] [14]. These models reveal that silica, polystyrene, and lipid-based nanoparticles smaller than 100 nm with moderately negative to neutral ζ-potentials preferentially bind APOE and APOB-100, while metal and metal-oxide nanoparticles with highly negative surface charge enrich complement component C3 [17].
Strategic Corona Engineering for Immunomodulation
The growing understanding of corona formation has enabled strategic engineering approaches to manipulate corona composition for desired immune outcomes:
Surface Property Modulation: Precisely engineered nanotopography can selectively alter protein adsorption patterns. Surfaces with 70 nm topography demonstrated reduced clusterin adsorption while increasing ApoB and IgG gamma binding, resulting in attenuated inflammatory responses [18].
Pre-adsorption Strategies: Intentional pre-formation of coronas with specific proteins (e.g., apolipoproteins for brain targeting) can steer biological interactions toward desired outcomes [17] [14].
Personalized Corona Design: Accounting for disease-specific plasma compositions enables designing nanoparticles that maintain intended functionality in specific patient populations [15] [14].
Stealth Corona Engineering: Enriching coronas with dysopsonins like clusterin can reduce immune recognition and extend circulation half-life [17].
The protein corona represents a critical transformation point where synthetic materials acquire biological identity, fundamentally directing subsequent immune recognition and responses. The physicochemical properties of biomaterials—including size, surface chemistry, charge, and topography—determine corona composition, which in turn activates specific immune signaling pathways and cellular responses. Strategic engineering of these material properties enables rational design of coronas that steer immune responses toward desired outcomes, whether for enhanced integration, targeted delivery, or controlled immunomodulation.
The emerging capabilities in machine learning prediction of corona composition, combined with advanced multi-omics characterization approaches, are accelerating our ability to design biomaterials with predictable biological fates. This knowledge is particularly crucial within the context of personalized medicine, where disease-specific corona variations significantly impact therapeutic efficacy. Future research directions include the development of dynamic corona models that account for temporal evolution in disease states, standardized characterization methodologies across laboratories, and clinical translation of corona engineering strategies for improved medical outcomes.
The host immune response is a critical determinant of the long-term success of medical implants. While acute inflammation is a protective and necessary biological process for initiating tissue repair, its dysregulation into a state of chronic inflammation frequently leads to implant failure through mechanisms such as foreign body reaction, fibrosis, and inadequate osseointegration [19] [20]. This whitepaper delineates the temporal dynamics of acute versus chronic inflammation within the context of biomaterial host interactions, framing this continuum as the central paradigm for understanding and improving implant outcomes. A profound understanding of these processes is foundational to the development of next-generation, immuno-informed biomaterials that can proactively modulate the host response to favor integration and longevity [7] [21].
The failure of a biomaterial to integrate is not merely a passive rejection but often a consequence of active, sustained immune signaling. Chronic inflammation is increasingly recognized as a "silent epidemic" and a common pathway in numerous disease states, a concept that extends directly to the persistence of inflammation around biomedical implants [19]. This document provides a detailed analysis of the immunological mechanisms, quantitative biomarkers, and advanced material science strategies that define the transition from beneficial acute inflammation to pathological chronic inflammation at the implant-tissue interface. It is intended to equip researchers and drug development professionals with the experimental frameworks and conceptual tools needed to navigate this complex biological landscape.
The Immunological Basis of Inflammation in Tissue Repair
Phases of Normal Healing
Tissue repair following implantation is a dynamic process orchestrated primarily by the immune system, unfolding in overlapping phases: hemostasis, inflammation, proliferation, and remodeling [7] [22]. The inflammatory phase is initiated immediately after injury and implantation, characterized by the recruitment of innate immune cells such as neutrophils and macrophages to the wound site [22]. These cells clear cellular debris and pathogens and set the stage for subsequent repair. The successful resolution of this acute inflammatory phase and the transition to proliferation is paramount for healing.
Macrophage Polarization: A Key Regulatory Axis
Macrophages demonstrate remarkable functional plasticity, and their phenotypic polarization is a crucial event in inflammation and repair [23]. The classical dichotomy outlines:
- M1 Macrophages (Pro-inflammatory): Stimulated by factors like IFN-γ or LPS, these cells express high levels of iNOS, TNF-α, IL-6, and IL-12. They are essential for initial pathogen clearance and debridement but can exacerbate tissue damage if their activity is prolonged [23] [24].
- M2 Macrophages (Pro-reparative): Activated by IL-4 or IL-13, these cells express markers like CD206 and Arg-1, and secrete anti-inflammatory cytokines (e.g., IL-10) and growth factors (e.g., TGF-β, PDGF) that promote angiogenesis, matrix deposition, and tissue remodeling [23] [24].
It is critical to note that this M1/M2 dichotomy is a simplification; in vivo, macrophages exist along a spectrum of functional states [23]. The timely transition from a predominantly M1 to a predominantly M2 phenotype is a hallmark of successful healing and implant integration. Conversely, a persistent M1 state is a characteristic feature of chronic inflammation and implant failure [24] [22].
Table 1: Key Characteristics of Macrophage Phenotypes in Implant Integration
| Feature | M1 (Pro-inflammatory) | M2 (Pro-reparative) |
|---|---|---|
| Activating Stimuli | IFN-γ, LPS, TNF-α | IL-4, IL-13, IL-10, Immune Complexes |
| Key Surface Markers | CD80, CD86, MHC-II | CD206, CD163 |
| Secreted Factors | TNF-α, IL-1β, IL-6, IL-12, ROS | IL-10, TGF-β, VEGF, PDGF, Arg-1 |
| Primary Functions | Pathogen clearance, debridement, pro-inflammation | Inflammation resolution, angiogenesis, matrix remodeling |
| Effect on Implants | Linked to chronic inflammation & fibrosis | Promotes integration & tissue repair |
Acute vs. Chronic Inflammation: A Temporal and Functional Dichotomy
Acute Inflammation: A Controlled, Protective Response
Acute inflammation is the body's immediate, short-term defensive response to tissue injury caused by implantation. It is characterized by the classic signs of redness, swelling, heat, pain, and loss of function [19]. This phase is typically self-limiting and resolves within days to weeks as the threat is eliminated and repair processes commence. The role of acute inflammation in implant healing is protective and constructive; it is essential for clearing debris, preventing infection, and initiating the signaling cascades that lead to tissue regeneration [19] [22].
Chronic Inflammation: A Dysregulated, Pathological State
Chronic inflammation, in contrast, is a low-grade, persistent inflammatory response that can last for months or years. Unlike its acute counterpart, it is systemic and often "silent," lacking the obvious cardinal signs [19]. In the context of implants, chronic inflammation is frequently driven by a persistent foreign body reaction to the biomaterial itself. This state is characterized by a sustained influx of mononuclear cells (lymphocytes, macrophages), ongoing tissue destruction, and simultaneous attempts at healing that lead to fibrosis and encapsulation of the implant [19] [20]. The failure to resolve acute inflammation, due to factors such as persistent immune activation, microbial biofilm, or excessive tissue damage, is a primary driver of this transition.
Table 2: Contrasting Features of Acute and Chronic Inflammation in Implant Biology
| Characteristic | Acute Inflammation | Chronic Inflammation |
|---|---|---|
| Onset & Duration | Immediate, short-term (days-weeks) | Delayed, long-term (months-years) |
| Cardinal Signs | Present (redness, swelling, heat, pain) | Often absent or subclinical |
| Primary Immune Cells | Neutrophils, M1 Macrophages | Macrophages, Lymphocytes, Plasma Cells |
| Tissue Outcomes | Tissue repair and regeneration | Tissue destruction, fibrosis, necrosis |
| Role in Implant Success | Essential for initiating integration | Primary cause of failure (loosening, fibrosis) |
| Biomarkers | Rapid, transient rise in CRP, cfDNA | Sustained, low-level elevation of CRP, NLR, PLR |
Quantitative Biomarkers and Clinical Evidence
Monitoring the inflammatory response is crucial for predicting implant outcomes. Clinical studies leverage various biomarkers to assess systemic and local inflammation.
Evidence from Cochlear and Dental Implants
A recent retrospective cohort study on sequential cochlear implantation provides compelling evidence for immunological memory influencing contralateral implant outcomes. The study found that the second implanted ear exhibited significantly higher and more rapidly increasing electrode impedances, consistent with a more robust immune response, suggesting the first implant "primed" the immune system [25]. Linear mixed models confirmed statistically significant effects of implant sequence and time on delta impedance (p < 0.0001), with the most pronounced differences in the basal and apical electrode groups [25].
In dental implantology, a study investigated preoperative inflammatory biomarkers as predictors of early failure in systemically healthy patients. While the neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and C-reactive protein (CRP) showed limited predictive value, the Systemic Immune-Inflammation Index (SII) demonstrated statistically significant discrimination for impaired osseointegration (p=0.015) [26]. This highlights the potential of composite biomarkers in risk stratification.
Kinetics of Key Biomarkers
The kinetic profiles of biomarkers provide a temporal window into the inflammatory state:
- Cell-free DNA (cfDNA): Released rapidly from damaged cells, cfDNA peaks within minutes to hours of an acute injury, making it an excellent early marker of cellular stress [27].
- C-reactive Protein (CRP): This classic acute-phase protein exhibits delayed kinetics, with levels beginning to rise after a delay of up to 24 hours and potentially peaking around 48 hours post-injury [27].
Table 3: Kinetic Profiles and Utility of Inflammation Biomarkers
| Biomarker | Origin / Stimulus | Kinetic Profile | Utility in Implant Monitoring |
|---|---|---|---|
| C-reactive Protein (CRP) | Liver; cytokine stimulation (e.g., IL-6) | Rises after ~24h, peaks at ~48h | Indicator of prolonged inflammation; useful for monitoring post-surgical burden. |
| Cell-free DNA (cfDNA) | Apoptotic or necrotic cells | Rises within minutes, peaks immediately post-injury | Promising for early detection of significant cellular damage during implantation. |
| Neutrophil-to-Lymphocyte Ratio (NLR) | Complete Blood Count (CBC) | Dynamic, reflects systemic inflammatory state | Pre-operative elevated levels may suggest a subclinical pro-inflammatory state. |
| Systemic Immune-Inflammation Index (SII) | CBC-derived (Platelets × Neutrophils/Lymphocytes) | Composite measure of inflammatory status | Shown to be a significant predictor of early dental implant failure [26]. |
Experimental Models and Methodologies
Protocol: Retrospective Analysis of Clinical Impedance Data
This methodology, used to investigate immunological memory in cochlear implants, can be adapted for studying other chronic inflammatory responses to implants [25].
- Cohort Selection: Apply strict inclusion/exclusion criteria. For example, in the cited study, patients with bilateral sequential implants from the same manufacturer and similar array types were selected, while those with explantation events or confounding medical conditions were excluded. A final cohort of 79 patients was established [25].
- Data Extraction: Collect longitudinal patient data from clinical databases. Key data points include patient demographics, implantation dates, and serial impedance measurements for all electrodes.
- Data Processing:
- Define a baseline measurement (e.g., the visit immediately following initial activation).
- Calculate delta impedance (change from baseline) for each electrode over time.
- Remove data from deactivated electrodes to avoid confounding.
- Statistical Analysis:
- Use paired t-tests to compare average absolute impedance between first and second implants at specific time points (e.g., 12 months).
- Employ linear mixed models to analyze the effects of fixed factors (implant sequence, time, electrode group) and random effects (individual patient trajectories).
- Perform post-hoc analyses on estimated marginal means and slopes to pinpoint significant differences.
Protocol: In Vivo Evaluation of a Smart Implant Coating
This protocol details the evaluation of an inflammation-responsive, multifunctional peptide coating (DOPA-P1@P2) on titanium implants, a prime example of immuno-informed biomaterial design [24].
- Surface Functionalization:
- Synthesize a mussel-inspired peptide ((DOPA)4-OEG5-DBCO) and the functional peptides P1 (N3-K15-PVGLIG-K23) and P2 (N3-Y5-PVGLIG-K23) via solid-phase peptide synthesis.
- Purify peptides using High-Performance Liquid Chromatography (HPLC) and verify molecular masses with Electrospray Ionization Mass Spectrometry (ESI-MS).
- Modify titanium implants by first coating with the mussel-inspired peptide, then grafting P1 and P2 via bioorthogonal click chemistry between DBCO and azide (-N3) groups [24].
- In Vivo Implantation and Analysis:
- Use a rodent model (e.g., rat or rabbit) for bone implantation into critical-sized defect sites.
- Experimental Groups: Include a control group (unmodified TiO₂) and the test group (DOPA-P1@P2 coated implants).
- Outcome Measures:
- Biomechanical Testing: At sacrifice, perform a push-out test to measure the maximal force required for implant displacement.
- Micro-Computed Tomography (μCT): Quantify bone volume fraction (BV/TV) and bone-to-implant contact (BIC) around the implant.
- Histological and Immunohistochemical Analysis: Process explanted tissue to assess tissue morphology, inflammation, and cellular composition. Use specific antibodies to identify M1 (e.g., iNOS) and M2 (e.g., CD206) macrophages.
- Data Interpretation: The DOPA-P1@P2 coating demonstrated a 161% increase in push-out force, a 207% increase in bone volume, and a 1409% increase in BIC compared to control, validating its success via sequential immune modulation and osteogenesis [24].
Diagram 1: Macrophage-Driven Pathways to Implant Success vs Failure
Advanced Strategies: Immuno-Informed Biomaterials
The emerging field of immuno-informed biomaterials seeks to design implants that actively direct the host immune response toward a regenerative outcome rather than a hostile one [7] [21]. Key strategies include:
- Surface Topography Modification: Engineering surface micro- and nano-topography to directly influence immune cell behavior. For instance, reducing the surface roughness of silicone mammary implants to 4 μm was shown to improve immune response and reduce capsular fibrosis [21].
- Bioactive Functionalization: Coating implants with peptides or cytokines that promote a pro-regenerative environment. The DOPA-P1@P2 coating is a sophisticated example, using an MMP-cleavable sequence (PVGLIG) to sequentially release an anti-inflammatory peptide (K23) first, followed by angiogenic (K15) and osteogenic (Y5) peptides [24].
- Mechanotransduction Modulation: Designing biomaterials with mechanical properties (e.g., stiffness) that favorably influence macrophage polarization through mechanosensitive pathways involving integrins and focal adhesion kinase (FAK) [23].
Diagram 2: Sequential Action of a Smart Inflammation-Responsive Coating
The Scientist's Toolkit: Key Research Reagents and Models
Table 4: Essential Tools for Investigating Inflammation in Implant Models
| Tool / Reagent | Function / Purpose | Specific Examples / Targets |
|---|---|---|
| Polarization Inducers | To polarize macrophages to specific phenotypes in vitro for functional assays. | LPS + IFN-γ (for M1); IL-4 or IL-13 (for M2) [23]. |
| MMP-Cleavable Peptides | To create "smart" coatings that release bioactive factors in response to inflammatory enzymes. | PVGLIG sequence (cleaved by MMP-2/9) [24]. |
| Anti-inflammatory Peptides | To bias the local immune microenvironment toward a reparative state upon implantation. | K23 peptide (KAFAKLAARLYRKALARQLGVAA) [24]. |
| Angiogenic & Osteogenic Peptides | To promote vascularization and bone formation in the proliferation phase of healing. | K15 (VEGF-mimetic), Y5 (OGP-derived) [24]. |
| Flow Cytometry Antibodies | To identify and quantify immune cell populations and their activation states from explanted tissue. | CD80/86 (M1), CD206/163 (M2), Ly6C (monocyte subsets) [23]. |
| Rodent Implantation Model | A standard in vivo model for evaluating the host response and osseointegration of novel implants. | Critical-sized bone defect model in rat or rabbit femur/tibia [24]. |
| Linear Mixed Models | A powerful statistical framework for analyzing longitudinal data from implant studies (e.g., impedance, imaging). | Accounts for fixed effects (implant type, time) and random effects (individual variation) [25]. |
The dichotomy between acute and chronic inflammation represents the fundamental axis upon which implant success pivots. The temporal dynamics of the immune response, particularly the critical phenotype switch in macrophages, dictate whether the outcome is functional integration or fibrotic failure. The growing body of evidence, from clinical retrospective studies to advanced material science, underscores that passive biocompatibility is no longer sufficient. The future of regenerative medicine and implantology lies in the proactive design of immuno-informed biomaterials that can actively guide the inflammatory response through its natural, reparative sequence [7] [21]. By leveraging quantitative biomarkers, sophisticated experimental models, and a deep understanding of immunology, researchers and drug developers can pioneer a new generation of implants that not replace tissue but truly integrate and heal with the body.
The interaction between biomaterials and the host immune system is a critical determinant of clinical success. This whitepaper provides a comparative analysis of the innate immunogenic profiles of natural and synthetic biomaterials. It explores the distinct mechanisms through which these materials interact with immune cells, details key experimental methodologies for profiling these responses, and visualizes the underlying signaling pathways. The objective is to furnish researchers and drug development professionals with a structured technical guide to inform the rational selection and design of biomaterials for applications in regenerative medicine, drug delivery, and tissue engineering.
Upon implantation, all biomaterials initiate a complex sequence of immune responses, a process known as the host response. The innate immune system is the first to react, with outcomes ranging from constructive remodeling and integration to chronic inflammation and fibrotic encapsulation [28]. The immunogenic profile of a biomaterial—its inherent capacity to stimulate immune activation—is not a binary property but a spectrum heavily influenced by its origin and physicochemical characteristics.
The paradigm in biomaterials science has evolved from designing inert materials that passively avoid immune detection to developing active, "smart" systems that dynamically modulate immune responses [29] [30]. This shift acknowledges the immune system not as an adversary but as a powerful therapeutic target. Understanding the fundamental differences in how natural and synthetic polymers engage with innate immune pathways is, therefore, foundational to advancing the field of immuno-informed biomaterial design.
Comparative Immunogenic Profiles
The following tables summarize the key immunological characteristics, mechanisms, and properties of natural and synthetic biomaterials.
Table 1: Immune Activation Mechanisms and Key Characteristics
| Feature | Natural Biomaterials | Synthetic Biomaterials |
|---|---|---|
| General Immunogenicity | Often considered low, but can elicit specific immune recognition [31]. | Variable; can be engineered for low immunogenicity, but some exhibit intrinsic immunostimulatory properties [32]. |
| Primary Immune Activation Pathways | Engagement of specific receptors (e.g., Integrins, DDR, OSCAR) [31]. | Activation of pattern recognition receptors (e.g., TLRs, inflammasomes) [32]. |
| Typical Macrophage Response | Often promotes a transition to pro-remodeling (M2-like) phenotypes [28]. | Can drive a pro-inflammatory (M1-like) response; highly tunable via engineering [29]. |
| Role of Adaptive Immunity | Can condition antigen-presenting cells to bias T-cell responses towards Th2 and Treg lineages [28]. | Generally lower adaptive involvement unless specifically engineered as vaccine carriers [32]. |
| Key Advantages | Biocompatible, bioactive, biodegradable, structurally biomimetic [31] [33]. | Reproducible, tunable mechanical & degradation properties, scalable manufacturing [34] [33]. |
| Key Limitations | Batch-to-batch variability, potential for immunogenicity from residual cellular components [28]. | Lack of innate bioactivity; degradation byproducts can cause acidic microenvironments and inflammation [34]. |
Table 2: Physicochemical Properties and Degradation Profiles
| Property | Natural Biomaterials | Synthetic Biomaterials |
|---|---|---|
| Common Examples | Collagen, Chitosan, Hyaluronic Acid, Fibrin, Alginate [31] [33]. | PLGA, PLA, PCL, PBAEs, Polyethylene Glycol (PEG) [34] [32]. |
| Degradation Mechanism | Primarily enzymatic (e.g., matrix metalloproteinases, lysozymes) [34]. | Primarily hydrolytic (cleavage of ester bonds) [34]. |
| Degradation Byproducts | Natural amino acids, sugars (generally well-tolerated) [33]. | Acidic monomers (e.g., lactic acid, glycolic acid) that may provoke inflammation [34]. |
| Mechanical Properties | Often limited mechanical strength; may require cross-linking or blending [34]. | Highly tunable mechanical strength and elasticity [34]. |
| Influence of Form | Immunogenicity can be affected by fibrillar vs. monomeric structure (e.g., in collagen) [31]. | Immunogenicity is highly form-dependent (e.g., particulate forms are more immunogenic than soluble polymers) [32]. |
Experimental Protocols for Profiling Immunogenicity
A critical step in biomaterial evaluation is the systematic assessment of their immunogenic potential. The following is a detailed protocol for evaluating the intrinsic immunogenicity of synthetic polymer particles, a common experimental approach in the field.
Detailed Protocol: Evaluating Intrinsic Immunostimulatory Properties of Polymeric Particles
This methodology is adapted from studies on degradable poly(beta-amino esters) (PBAEs) and can be generalized for other synthetic polymers [32].
1. Objective: To determine the intrinsic capacity of polymer particles to activate dendritic cells (DCs) and enhance T-cell proliferation in vitro.
2. Materials and Reagents:
- Polymers of Interest: e.g., PBAEs, PLGA, or other synthetic polymers.
- Cell Culture Media: RPMI-1640 supplemented with fetal bovine serum (FBS).
- Immune Cells: Bone marrow-derived dendritic cells (BMDCs) from mouse models and CD4+ T cells isolated via negative selection kits.
- Activation Reagents: Toll-like receptor agonists (e.g., LPS, Poly(I:C)).
- Assay Kits: ELISA kits for cytokines (e.g., IL-1β, IL-6, TNF-α) and CFSE for T-cell proliferation tracking.
- Characterization Equipment: Dynamic Light Scattering (DLS) for particle size and zeta potential, Gel Permeation Chromatography (GPC) for molecular weight.
3. Experimental Workflow:
Diagram 1: Immunogenicity Assay Workflow
4. Step-by-Step Procedure:
- Step 1: Polymer Synthesis and Particle Fabrication. Synthesize polymers via established methods (e.g., Michael-type addition for PBAEs). Characterize the initial molecular weight using GPC. Form particles via electrostatic condensation or emulsion methods. Characterize particle size, polydispersity index (PDI), and zeta potential using DLS [32].
- Step 2: In Vitro Degradation. Incubate particles in buffers mimicking physiological (pH 7.4) and inflammatory (pH 5.0) conditions at 37°C. Withdraw samples at predetermined time points (e.g., 0, 6, 24, 72 hours). Lyophilize and analyze the molecular weight of degraded polymer fragments via GPC to track degradation kinetics [32].
- Step 3: Dendritic Cell Activation Assay. Isplicate and culture BMDCs. Seed DCs in plates and treat with:
- Negative control: Media only.
- Positive control: TLR agonist (e.g., LPS).
- Experimental groups: Particles fabricated from polymers at different degradation stages (varying MW). After 18-24 hours, collect supernatant for cytokine analysis (ELISA) and harvest cells for analysis of surface activation markers (CD40, CD80, CD86) via flow cytometry [32].
- Step 4: T-cell Proliferation Co-culture. Isolate CD4+ T cells from spleens of transgenic mice (e.g., 2D2 mice) and label with CFSE. Co-culture these T cells with the particle-treated BMDCs. After 3-5 days, analyze T-cell proliferation by measuring CFSE dilution using flow cytometry [32].
5. Data Analysis:
- Correlate DC activation (cytokine levels, marker expression) and T-cell proliferation with polymer properties (MW, particle size, charge).
- A key finding to assess is whether high molecular weight particles elicit a stronger immunostimulatory effect, which wanes with degradation, as demonstrated with PBAEs [32].
Key Signaling Pathways in Biomaterial-Immune Interactions
The innate immune response to biomaterials is mediated by specific receptor-ligand interactions. The pathways differ significantly between natural and synthetic materials.
Natural Biomaterial Pathway: Collagen-Integrin Signaling
Collagen, a predominant natural polymer, interacts with immune and stromal cells primarily through integrin receptors, initiating a pro-regenerative signaling cascade [31].
Diagram 2: Collagen-Integrin Signaling
Synthetic Biomaterial Pathway: Particulate-Induced Inflammasome Activation
Synthetic polymer particles, similar to pathogens, are often recognized by the innate immune system as danger signals, leading to activation of inflammasomes and pro-inflammatory cytokine production [32].
Diagram 3: Particulate-Induced Inflammasome Activation
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for conducting experiments in biomaterial immunogenicity.
Table 3: Key Research Reagents for Biomaterial-Immune Profiling
| Reagent / Material | Function / Application | Specific Example |
|---|---|---|
| Poly(beta-amino esters) (PBAEs) | Model degradable, cationic synthetic polymer for studying the impact of molecular weight and form on intrinsic immunogenicity [32]. | Polymers synthesized from monomers like 1,4-butanediol diacrylate and 4,4′-trimethylenedipiperidine [32]. |
| Poly(lactic-co-glycolic acid) (PLGA) | A widely used, FDA-approved synthetic polymer known to exhibit intrinsic immunostimulatory properties; a benchmark material [32]. | Commercial PLGA resins with various lactide:glycolide ratios and molecular weights. |
| Toll-like Receptor (TLR) Agonists | Positive controls for activating immune cells in vitro to benchmark biomaterial-induced immunostimulation [32]. | Lipopolysaccharide (LPS, TLR4 agonist) or Poly(I:C) (TLR3 agonist). |
| Fluorescent Antibody Conjugates | Critical for flow cytometry analysis of immune cell surface markers to determine activation and polarization states [32]. | Antibodies against CD40, CD80, CD86 for DCs; CD206, CD64 for macrophages. |
| CFSE (Carboxyfluorescein succinimidyl ester) | A cell proliferation dye used to track and quantify T-cell division in co-culture assays with biomaterial-treated antigen-presenting cells [32]. | Used to label T cells before co-culture; proliferation is measured as dye dilution via flow cytometry. |
| Decellularized ECM Bioscaffolds | Representative natural biomaterials used to study pro-remodeling immune responses; quality is dependent on source tissue and decellularization method [28]. | ECM scaffolds derived from porcine small intestine submucosa (SIS), urinary bladder, or dermis. |
The innate immunogenic profiles of natural and synthetic biomaterials are distinct, rooted in their fundamental compositions and interactions with the host. Natural biomaterials tend to engage specific receptor-mediated pathways that can promote constructive remodeling, whereas synthetic biomaterials often trigger pattern-recognition receptors, leading to inflammation, though this is highly tunable. The future of the field lies in the rational design of "smart" hybrid materials that combine the bioactivity of natural polymers with the engineerability of synthetic systems. By leveraging detailed experimental profiling and a deep understanding of immune signaling pathways, researchers can now design biomaterials that do not just evade the immune system, but actively orchestrate it to achieve desired therapeutic outcomes.
Engineering Immunomodulation: Strategic Design of Smart and Bioactive Biomaterials
The field of biomaterials science has undergone a profound transformation, evolving from the development of passive constructs intended primarily for structural support to the engineering of sophisticated "smart" platforms [30] [29]. These advanced biomaterials are meticulously designed to actively and precisely interface with the host's biological systems, particularly the immune system, to orchestrate desired therapeutic outcomes [30]. This evolution represents a paradigm shift, fueled by the convergence of breakthroughs in materials science, immunology, and bioengineering. The traditional goal of achieving "bio-inertness"—a state of passive coexistence—has been replaced by the ambition of active "immunomodulation" [29]. This conceptual pivot acknowledges the immune system not as an adversary to be evaded, but as a powerful biological system that can be rationally programmed and harnessed for therapeutic benefit [29] [35]. The capacity to intelligently interact with and guide cellular and tissue responses positions smart biomaterials at the forefront of regenerative medicine and advanced therapeutics, offering transformative strategies for disease intervention and tissue repair [30].
The Classification Spectrum: From Inert to Autonomous Biomaterials
The classification of biomaterials reflects an increasing level of sophistication in their interaction with biological systems, essentially mirroring an evolution in their biomimetic capabilities [30] [29]. This progression highlights a journey from static implants to dynamic, self-adaptive platforms.
Table 1: Classification of Biomaterials Based on Biological Interaction and "Smartness"
| Classification | Core Functionality | Key Characteristics | Representative Examples |
|---|---|---|---|
| Inert Materials | Passive structural support; occupy space | Designed for minimal biological interaction; often trigger Foreign Body Reaction (FBR) and fibrous encapsulation | Certain titanium alloys, inert ceramics, inert polymers [30] [29] |
| Active Materials (Bioactive) | Elicit a defined biological response at interface | Release pre-loaded bioactive agents (drugs, growth factors) or possess inherent surface bioactivity | Drug-eluting stents, antibiotic-loaded bone cements, hydroxyapatite coatings [30] [29] |
| Responsive Materials | Sense and respond to specific environmental stimuli | Dynamic change in properties or payload release triggered by pH, temperature, enzymes, etc. | pH-sensitive hydrogels, temperature-responsive polymers (PNIPAM), enzyme-degradable matrices [30] [29] |
| Autonomous Materials | Sense, respond, and adapt based on feedback; mimic homeostatic loops | Bi-directional responsiveness; capable of receiving cellular feedback and remodeling accordingly | Engineered systems that adjust drug release based on real-time inflammatory marker levels [30] |
Decoding the Host Immune Response to Biomaterials
The interaction between an implanted biomaterial and the host immune system is a critical determinant of its ultimate clinical success [29]. An inappropriate or unresolved immune response can precipitate a cascade of adverse events, including chronic inflammation, the formation of a dense fibrous capsule that isolates the implant, and ultimately, implant failure and compromised tissue healing [29] [36]. This host response, known as the Foreign Body Response (FBR), is a sequential biological reaction [36] [35].
Phases of the Foreign Body Response (FBR)
- Protein Adsorption: Within seconds to minutes, host plasma proteins (e.g., albumin, fibrinogen, fibronectin) adsorb onto the biomaterial surface, forming a provisional matrix. The composition of this protein layer is influenced by the biomaterial's surface properties and dictates subsequent cell interactions [36] [35].
- Acute Inflammation: Granulocytes, particularly neutrophils, infiltrate the site. They attempt to phagocytose the material and release reactive oxygen species (ROS) and enzymes. Neutrophils also release chemokines like CXCL8 and CCL2 to recruit monocytes [36] [35].
- Chronic Inflammation: Monocytes differentiate into macrophages on the material surface. These cells undergo "frustrated phagocytosis" when unable to engulf large implants, leading to increased release of cytokines and chemokines. Macrophages can fuse to form Foreign Body Giant Cells (FBGCs), a hallmark of chronic FBR [36] [35].
- Fibrosis: Triggered by pro-fibrotic signals like TGF-β from macrophages and other cells, fibroblasts and endothelial cells deposit collagen, forming a dense, avascular fibrous capsule that walls off the implant [36].
Macrophage Polarination: A Key Immunomodulatory Target
Macrophages are highly plastic cells central to the FBR and regenerative outcomes [36] [7]. They can polarize into different functional phenotypes in response to environmental cues:
- M1 Phenotype (Pro-inflammatory): Induced by factors like interferon-γ (IFN-γ) or lipopolysaccharide (LPS). M1 macrophages secrete pro-inflammatory cytokines (e.g., IL-1β, TNF-α, IL-6), produce high levels of ROS, and contribute to tissue destruction and chronic inflammation [36] [7].
- M2 Phenotype (Anti-inflammatory/Pro-regenerative): Induced by cytokines like IL-4 or IL-13. M2 macrophages secrete anti-inflammatory cytokines (e.g., IL-10), promote tissue repair, angiogenesis, and matrix remodeling. A timely transition from M1 to M2 is associated with successful integration and regeneration [36] [7] [37].
Diagram 1: Macrophage Polarization Pathways and Functional Outcomes. The balance between M1 and M2 phenotypes is a primary target for immunomodulatory biomaterials, which seek to promote the M2 pro-regenerative pathway [36] [7] [37].
Design Principles and Experimental Methodologies for Immunomodulatory Biomaterials
The design of immunomodulatory biomaterials involves precise engineering of physical, chemical, and biological properties to dictate favorable interactions with the immune system.
Physical and Chemical Property Modulation
Biomaterial properties such as surface topography, stiffness, and wettability are powerful tools for directing immune cell fate [36] [35].
Table 2: Key Biomaterial Properties and Their Immunomodulatory Effects
| Property | Experimental Tuning Methods | Observed Immunomodulatory Effect | Key References |
|---|---|---|---|
| Stiffness | Varying cross-linking density in hydrogels; blending polymers of different elastic moduli | Softer substrates tend to promote M2 macrophage polarization; stiffer substrates can promote M1 and fibrosis. | [36] |
| Surface Topography | Lithography to create micro/nano-patterns (pillars, grooves); electrospinning to control fiber diameter | Specific micro-patterns can reduce FBGC formation; nanofibrous structures can mimic native ECM. | [36] [35] |
| Wettability (Hydrophilicity) | Surface plasma treatment; chemical grafting with hydrophilic (e.g., PEG) or hydrophobic polymers | Moderately hydrophilic surfaces often reduce non-specific protein adsorption and attenuate inflammatory response. | [36] |
| Chemical Composition | Using natural polymers (e.g., chitosan, HA) vs. synthetic (e.g., PLA, PGA); incorporating bioactive ions (e.g., Sr²⁺, Mg²⁺) | Chitosan and Hyaluronic Acid can promote M2 polarization; Mg²⁺ ions reduce pro-inflammatory responses and promote osteogenesis. | [31] [7] |
Integrating Bioactive Cargo and Stimuli-Responsivity
A core strategy for active biomaterials is the controlled delivery of immunomodulatory factors or the incorporation of sensorial capabilities.
- Cytokine and Growth Factor Delivery: Biomaterials can be loaded with anti-inflammatory (e.g., IL-4, IL-10) or pro-regenerative (e.g., TGF-β) factors. The key is spatiotemporally controlled release to match the healing phases [30] [7].
- Stimuli-Responsive Systems: "Smart" biomaterials sense and respond to pathological cues [30] [29]:
- pH-Responsive: Utilize polymers with ionizable groups or pH-labile bonds (e.g., hydrazones, acetals) that degrade in acidic environments like chronic wounds or tumors.
- Enzyme-Responsive: Incorporate peptide cross-linkers or polymer backbones that are cleaved by enzymes overexpressed at the implant site (e.g., Matrix Metalloproteinases - MMPs).
- Temperature-Responsive: Use polymers like poly(N-isopropylacrylamide) - PNIPAM, which undergo sol-gel transition at body temperature, enabling injectable depot formation.
Diagram 2: Core Workflow for Evaluating Immunomodulatory Biomaterials. This pipeline integrates in vitro and in vivo analyses, culminating in advanced techniques like single-cell RNA sequencing (scRNA-seq) to deconvolute the immune microenvironment at high resolution [36].
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents for Immunomodulatory Biomaterial Development
| Reagent/Material Category | Specific Examples | Primary Function in Research |
|---|---|---|
| Natural Polymers | Chitosan, Hyaluronic Acid (HA), Alginate, Collagen, Decellularized ECM | Provide bioactive, often inherently immunomodulatory scaffolds with high biocompatibility and biodegradability [31] [7]. |
| Synthetic Polymers | Poly(lactic acid) (PLA), Poly(glycolic acid) (PGA), Polycaprolactone (PCL), Polyethylene Glycol (PEG) | Offer tunable mechanical properties, degradation rates, and a "blank slate" for functionalization with minimal batch-to-batch variation [31] [7]. |
| Cross-linkers & Functionalizers | Glutaraldehyde, Genipin, NHS-PEG-Maleimide, Succinic Anhydride | Modify material properties (e.g., stiffness, degradation) and enable covalent attachment of bioactive peptides (e.g., RGD) or cytokines [30]. |
| Polarization Cytokines | Recombinant IFN-γ, LPS (for M1); Recombinant IL-4, IL-13 (for M2) | Used in in vitro assays to polarize macrophages and test the biomaterial's ability to promote or maintain a desired phenotype [36] [7]. |
| Immunostaining Antibodies | Anti-CD86, Anti-iNOS (M1 markers); Anti-CD206, Anti-Arginase-1 (M2 markers); Anti-CD68 (pan-macrophage) | Critical for identifying and quantifying macrophage phenotypes in cell culture and on explanted tissue sections via immunofluorescence/ IHC [36] [35]. |
Signaling Pathways in Biomaterial-Immune Cell Interactions
The interaction between immune cells and biomaterials is mediated by specific receptor-ligand engagements that activate intracellular signaling cascades, ultimately determining cell behavior and fate.
Integrin-Mediated Signaling
Cell adhesion to the protein-coated biomaterial surface is primarily mediated by integrins, which transmit signals both inward (outside-in signaling) and outward (inside-out signaling) [31] [35]. The binding of collagen or other ECM proteins to integrins (e.g., α2β1) initiates the recruitment and activation of focal adhesion kinase (FAK) and Src family kinases (SFK) [31]. This leads to the activation of major downstream pathways including:
- PI3K/Akt Pathway: Promotes cell survival and proliferation.
- MAPK Pathways: Including ERK, JNK, and p38, which regulate cell growth, differentiation, and stress responses [31].
Discoidin Domain Receptor (DDR) Pathways
DDR1 and DDR2 are receptor tyrosine kinases that bind to native collagen without requiring integrin activation [31]. Their activation influences cell spreading, migration, adhesion, and proliferation through the modulation of various chemical mediators, providing an alternative pathway for cell-matrix communication [31].
Pattern Recognition Receptor (PRR) Signaling
Immune cells recognize biomaterials and adsorbed proteins via PRRs, such as Toll-like Receptors (TLRs), which typically sense Damage-Associated Molecular Patterns (DAMPs) released from injured tissue [36] [35]. TLR activation triggers signaling cascades (often involving the adapter protein MyD88) that lead to the activation of NF-κB and MAPK pathways. This results in the transcription and secretion of pro-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6), initiating and amplifying the inflammatory response [36] [35].
Diagram 3: Key Signaling Pathways in Biomaterial-Immune Cell Interactions. Integrin, DDR, and TLR signaling converge on major pathways like PI3K/Akt, MAPK, and NF-κB to dictate cell survival, migration, and inflammatory responses [31] [36] [35].
The paradigm shift from bioinert to active immunomodulatory biomaterials marks a new era in regenerative medicine and therapeutic intervention. By consciously designing materials that engage with and guide the host immune system, researchers can create microenvironments conducive to healing and integration, rather than rejection and encapsulation [30] [29] [7]. The future of this field points towards even greater precision and personalization, integrating optogenetic control, artificial intelligence-driven design, and synergistic multimodal therapies [30] [7]. As the molecular understanding of biomaterial-host interactions deepens, particularly with the aid of high-resolution technologies like single-cell RNA sequencing [36], the next generation of biomaterials will increasingly function as dynamic, autonomous partners in the intricate process of tissue repair and regeneration.
The field of bone tissue engineering is undergoing a paradigm shift, moving from a passive, biocompatible approach to an active, immuno-instructive one. While biochemical signaling has historically dominated regenerative strategies, emerging evidence highlights that physical cues from biomaterials—such as topography, stiffness, and porosity—can profoundly influence immune cell behavior, particularly macrophage polarization [38] [5]. This recognition situates biomaterials not merely as structural scaffolds but as active participants in orchestrating the immune response to achieve better regenerative outcomes. The host immune response, long considered a barrier to implant integration, is now recognized as a critical determinant of success in bone regeneration [39]. Macrophages, as central orchestrators of inflammation and tissue repair, dynamically shift their functional phenotypes in response to signals from their microenvironment. The rational design of biomaterials that can direct these phenotypic shifts through their physical properties represents a frontier in the development of next-generation osteo-immunomodulatory biomaterials [38] [5]. This whitepaper provides a comprehensive technical guide on engineering these physical properties to harness the immune system for enhanced bone regeneration, framed within the broader context of biomaterial-host interactions.
Macrophage Polarization: The Central Mechanism in Bone Regeneration
Phenotypic Plasticity and Functional Roles
Macrophages are versatile immune cells ubiquitous across all tissues, where they play key roles in development, homeostasis, immune defense, and regeneration [5]. Their functional plasticity allows them to adopt a spectrum of activation states, most broadly categorized as the pro-inflammatory M1 phenotype and the anti-inflammatory, pro-regenerative M2 phenotype [5]. This polarization is highly responsive to local environmental cues; M1 polarization is typically driven by stimuli like lipopolysaccharides (LPS) and interferon-gamma (IFN-γ), while M2 polarization is induced by cytokines including interleukin-4 (IL-4) and IL-10 [5].
Following bone injury, a carefully orchestrated temporal sequence of macrophage activity unfolds. Initially, a high M1/M2 ratio is essential for pathogen clearance and debridement of the injury site. This state subsequently transitions to an M2-dominant profile that facilitates osteoblast recruitment, matrix deposition, and bone regeneration [5]. Critically, this phenotypic balance is dynamic. Macrophages demonstrate significant polarization plasticity, capable of reversibly switching between phenotypes in response to evolving microenvironmental signals [5]. For instance, M2 macrophages can be re-polarized to an M1 state upon exposure to pro-inflammatory cytokines like TNF-α [5].
Significance in Bone Healing
The central role of macrophages in bone repair is underscored by in vitro evidence demonstrating that co-culture of macrophages with osteoblasts significantly enhances osteogenic gene expression and matrix mineralization [5]. However, an improper or mistimed polarization state can be detrimental. Prematurely polarized M2 macrophages may produce excessive fibrotic cytokines, leading to fibrous capsule formation around implants and compromising integration [5]. Therefore, the ability of biomaterials to guide the appropriate macrophage phenotype at each healing phase is critical for successful regeneration.
Engineering Immunomodulation through Physical Cues
Surface Topography
Surface topography refers to the physical patterns and features at the material-cell interface, spanning from the nano- to microscale. It is a potent modulator of macrophage adhesion, morphology, and polarization.
- Cellular Mechanosensing: Cells perceive topographic features through a process called mechanotransduction. Surface patterns are sensed through integrin-mediated adhesion, leading to cytoskeletal reorganization and activation of downstream signaling pathways such as Rho-associated protein kinase (ROCK) and Yes-associated protein (YAP)/Transcriptional coactivator with PDZ-binding motif (TAZ) [5]. These pathways ultimately converge on nuclear transcription factors that dictate polarization fate.
- Design Parameters and Immunomodulatory Effects: The specific dimensions of topographic features are critical in determining the immune response. Research on silicone mammary implants (SMIs) has demonstrated that reducing surface roughness to approximately 4 μm can improve the immune response, enhance wound healing, and reduce fibrotic capsule formation [39]. Similarly, surface nanocavitation of titanium has been shown to modulate macrophage activity, though the precise optimal dimensions are material-dependent [38].
Table 1: Topography Parameters and Their Effects on Macrophage Polarization
| Feature Type | Typical Dimensions | Macrophage Response | Key Signaling Pathways |
|---|---|---|---|
| Micropits | 1 - 10 μm | Elongated cell morphology; favors M2 polarization | ROCK, FAK |
| Nanogratings | 100 - 500 nm depth/width | Induces M2 marker expression (CD206) | YAP/TAZ |
| Surface Roughness | ~4 μm (e.g., on silicone implants) | Reduced inflammation and fibrosis | Not Specified |
| Nanocavitation | Nano-scale (on titanium) | Modulated inflammatory activity | Not Specified |
Substrate Stiffness
Substrate stiffness, the elastic modulus of a biomaterial, provides critical mechanical cues that guide macrophage fate and function.
- Mechanotransduction Pathways: Macrophages sense substrate stiffness via adhesion complexes and actin-myosin contractility. On stiffer substrates, increased cytoskeletal tension promotes nuclear translocation of mechanosensitive transcription factors, which can drive pro-inflammatory gene expression [5]. Softer substrates, which more closely mimic the elasticity of healthy native tissues, typically promote an M2-like phenotype.
- Stiffness Ranges and Phenotypic Outcomes: The ideal stiffness for promoting a regenerative response often falls within a range that mimics the target tissue. While the exact optimal values for bone are an active area of research, studies suggest that softer substrates (in the low kilopascal range) generally favor M2 polarization, while stiffer substrates (exceeding tens of kilopascals) promote the M1 phenotype [5]. This stiffness-dependent polarization creates a feedback loop, as M1 macrophages can further stiffen the extracellular matrix (ECM) through the production of cross-linking enzymes, thereby perpetuating inflammation [5].
Table 2: Macrophage Responses to Substrate Stiffness
| Stiffness Range | Macrophage Phenotype | Cytokine Secretion Profile | Downstream Effects on Bone |
|---|---|---|---|
| Soft (0.1 - 1 kPa) | M2-like | Anti-inflammatory (e.g., IL-10, TGF-β) | Promotes osteogenesis; minimizes fibrosis |
| Intermediate (1 - 20 kPa) | Mixed or M2-like | Context-dependent | Can support vascularization and remodeling |
| Stiff (>20 kPa) | M1-like | Pro-inflammatory (e.g., TNF-α, IL-1β, IL-6) | May impede mineralization; promotes chronic inflammation |
Porosity and Pore Architecture
The three-dimensional structural organization of a scaffold, particularly its porosity and pore architecture, governs macrophage infiltration, cell-cell interactions, and the formation of nutrient and oxygen gradients, all of which influence polarization.
- Influence on the Microenvironment: Pore architecture directly affects mass transport and cell packing density. In dense 3D models like tumor spheroids, cell density can reach extreme levels of up to 6 × 10⁷ cells/cm³, creating tortuous diffusion pathways that retard molecular penetration and establish chemical gradients (e.g., oxygen, pH) [40]. These gradients can polarize macrophages toward a pro-inflammatory state, similar to what is observed in the core of solid tumors.
- Design for Immunomodulation: A well-interconnected porous network with pore sizes typically recommended in the 100-400 μm range is considered beneficial for bone ingrowth. From an immunomodulatory perspective, this architecture facilitates macrophage infiltration and prevents the formation of hypoxic cores that drive inflammation [38] [5]. Furthermore, the degradation profile of the scaffold must be considered, as the byproducts of degradation and the changing mechanical environment over time can continuously influence the macrophage response [5].
Table 3: Pore Architecture Parameters and Their Immunological Implications
| Architectural Parameter | Optimal Range for Bone | Impact on Macrophage Behavior | Consequence for Regeneration |
|---|---|---|---|
| Porosity | >70-80% | Enables macrophage infiltration and M2 polarization | Supports vascularization and new bone formation |
| Pore Size | 100 - 400 μm | Influences macrophage fusion and spatial organization | Directs tissue ingrowth pattern; avoids hypoxic pockets |
| Pore Interconnectivity | High (>95%) | Prevents necrotic core formation; allows even cytokine distribution | Ensures uniform tissue regeneration throughout scaffold |
| Degradation Rate | Matches tissue growth rate | Prevents prolonged foreign body response; avoids acidic byproduct buildup | Maintains a pro-healing microenvironment over time |
Experimental Protocols for Evaluating Physical Cue Immunomodulation
Protocol 1: Evaluating Macrophage Polarization on 2D Biomaterial Surfaces
This protocol details the methodology for assessing how surface topography and stiffness on 2D substrates influence macrophage phenotype.
- Substrate Fabrication: Fabricate biomaterial substrates with controlled topography (e.g., using photolithography or etching) or stiffness (e.g., using polyacrylamide hydrogels of varying crosslink density). Characterize surfaces using Atomic Force Microscopy (AFM) for roughness and stiffness, and Scanning Electron Microscopy (SEM) for topography.
- Cell Seeding and Culture: Isolate primary human monocyte-derived macrophages (e.g., from PBMCs using M-CSF differentiation) or use a murine macrophage cell line (e.g., RAW 264.7). Seed cells at a standardized density (e.g., 50,000 cells/cm²) onto the substrates. Maintain in standard culture conditions (37°C, 5% CO₂).
- Stimulation and Conditioning: To establish a baseline polarization state, stimulate cells on different substrates with:
- M1 stimuli: LPS (100 ng/mL) + IFN-γ (20 ng/mL) for 24 hours.
- M2 stimuli: IL-4 (20 ng/mL) for 24 hours. Include an unstimulated (M0) control.
- Endpoint Analysis:
- Gene Expression: Harvest cells for qRT-PCR analysis of M1 markers (iNOS, CD80, CD86) and M2 markers (CD206, ARG1, CD163).
- Protein Secretion: Collect conditioned media and analyze cytokine profiles using ELISA (e.g., TNF-α, IL-1β for M1; IL-10, TGF-β for M2).
- Immunofluorescence: Fix and stain cells for surface markers (e.g., CD86 for M1, CD206 for M2) and cytoskeletal components (e.g., F-actin with phalloidin) to correlate morphology with phenotype.
- Data Interpretation: Compare the relative expression of M1 and M2 markers across substrates with different physical properties. A successful immunomodulatory surface will promote an M2-skewed profile under pro-healing conditions or mitigate M1 polarization under inflammatory conditions.
Protocol 2: 3D Scaffold Culture in a Spheroid Model
This protocol utilizes 3D tumor spheroid models, which present formidable penetration barriers, to evaluate the penetration and efficacy of immunomodulatory compounds released from or within scaffolds [40].
- Scaffold Preparation and Compound Loading: Fabricate 3D porous scaffolds (e.g., via electrospinning, 3D printing) with defined architecture. Load with an immunomodulatory natural product (e.g., Curcumin) or a control. Characterize the release profile in PBS.
- Spheroid Formation: Generate tumor spheroids using a relevant cell line (e.g., MC3T3-E1 for bone) in ultra-low attachment 96-well plates. Allow spheroids to mature for 72-96 hours until they reach 400-600 μm in diameter, developing characteristic gradients (e.g., hypoxic core with <0.2% O₂, acidic core with pH ~6.5-6.8) [40].
- Treatment Setup:
- Direct Treatment: Incubate spheroids with the free compound in solution.
- Scaffold-Mediated Treatment: Co-culture spheroids with the compound-loaded scaffold, either in direct contact or in a transwell system.
- Penetration and Efficacy Analysis:
- Imaging and Penetration Depth: Use confocal microscopy to track the penetration of a fluorescently labeled compound. Quantify the fluorescence intensity from the spheroid periphery to the core.
- Viability and Phenotype Assessment: After 48-72 hours of treatment, assess spheroid viability using a live/dead assay. Dissociate spheroids and analyze infiltrating immune cells (e.g., macrophages) for polarization markers via flow cytometry.
- Barrier Assessment: The dense ECM of spheroids (e.g., 33-fold increased fibronectin) and high cell density (6 × 10⁷ cells/cm³) create a stringent test for drug delivery [40]. Effective formulations must overcome these barriers to modulate the phenotype of immune cells, which often remain in the peripheral 30-50 μm of the spheroid [40].
Visualization of Signaling Pathways and Experimental Workflows
Macrophage Mechanosensing and Polarization Pathways
Diagram 1: Macrophage mechanosensing and polarization pathways.
3D Spheroid Drug Penetration and Activity Workflow
Diagram 2: 3D spheroid drug penetration and activity workflow.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for Investigating Physical Immunomodulation
| Reagent/Material | Function/Application | Example Use-Case |
|---|---|---|
| Polyacrylamide Hydrogels | Tunable-stiffness 2D substrates for mechanobiology studies. | Fabricating culture surfaces with defined elastic moduli (e.g., 1-50 kPa) to test stiffness effects on macrophage polarization. |
| Polydimethylsiloxane (PDMS) | Polymer for fabricating micro-patterned surfaces with precise topography. | Creating micro-grooves or pillars to study the effect of surface patterning on macrophage morphology and phenotype. |
| Titanium with Nanocavitation | Model metallic biomaterial with modified nano-topography. | Studying the immunomodulatory potential of nano-scale surface features on macrophage activity [38]. |
| Electrospun Nanofibrous Mats | 3D scaffolds mimicking the native ECM, with tunable fiber diameter and porosity. | Creating 3D environments to study the combined effects of topography and porosity on macrophage infiltration and polarization. |
| Polarizing Cytokines (LPS, IFN-γ, IL-4) | Biochemical stimuli to drive macrophages toward M1 or M2 phenotypes. | Used as positive controls in conjunction with physical cues to assess their combined or antagonistic effects on polarization. |
| Fluorescent Antibody Panels | Cell surface and intracellular staining for polarization markers. | Flow cytometry and immunofluorescence analysis of M1 (CD80, CD86, iNOS) and M2 (CD206, CD163, ARG1) markers. |
| 3D Tumor Spheroid Kits | Ready-to-use platforms for forming uniform multicellular spheroids. | Modeling the dense, gradient-rich tissue environment to test drug penetration and activity from immunomodulatory scaffolds [40]. |
The deliberate engineering of physical biomaterial cues—topography, stiffness, and porosity—represents a powerful and sophisticated strategy for directing the host immune response toward regenerative outcomes. By understanding the mechanobiological principles that govern macrophage polarization, researchers and clinicians can design "immuno-informed" biomaterials that actively participate in the healing process [39]. The future of this field lies in the development of dynamic and smart materials capable of adapting their physical properties in response to the evolving healing microenvironment. This progress, guided by robust experimental protocols and a deep understanding of immune cell-material interactions, holds the promise of achieving truly predictive and personalized bone regeneration therapies.
The implantation of any biomaterial into the human body elicits a complex sequence of biological responses, commencing with an inflammatory phase that is critical for determining the ultimate success or failure of the medical device [2]. This initial inflammatory response, while essential for tissue repair, can progress to chronic inflammation and foreign body reaction (FBR), culminating in fibrous encapsulation and implant failure [41]. The interface between host tissues and the biomaterial surface serves as the primary battleground where these interactions unfold, governed by the physicochemical properties of the implant itself [41].
Within this context, sophisticated surface engineering and controlled release technologies have emerged as transformative approaches for modulating host-implant interactions. These strategies aim to steer inflammatory responses toward favorable outcomes by employing precisely engineered surface chemistries, topographies, and release kinetics of therapeutic agents [41]. The evolution from passively biocompatible "immune-evasive" materials to actively "immune-interactive" systems represents a paradigm shift in biomaterial design [41]. This technical guide comprehensively examines the current state of surface functionalization and controlled release strategies for anti-inflammatory agents, framing these approaches within the broader thesis of biomaterial-host interactions and immune response research.
Surface Functionalization Strategies
Surface functionalization encompasses a suite of techniques designed to modify the outermost layer of biomaterials to dictate specific biological responses. These strategies can be broadly categorized into physical, chemical, and biological approaches, each offering distinct mechanisms for controlling host-implant interactions.
Physical Surface Modifications
Physical modifications alter surface topography and energy without necessarily changing surface chemistry, significantly influencing protein adsorption and subsequent cellular responses.
- Surface Topography Engineering: Creating micro- and nano-scale features on biomaterial surfaces directly influences cell adhesion, migration, and differentiation. For instance, introducing parallel gratings with widths ranging from 250 nm to 2 µm affects macrophage polarization, steering them toward pro-healing (M2) phenotypes [41]. Nanoscale roughness (approximately 68 nm) on implant surfaces has demonstrated appreciable decreases in pro-inflammatory cytokine expression and osteoclast activity compared to smoother or microscale rough surfaces [41].
- Techniques for Physical Modifications:
- Mechanical Methods: Grinding, machining, and blasting.
- Micro/Nanopatterning: Photolithography, electron beam lithography, soft-lithography, and colloidal lithography to create ordered topographical patterns.
- Phase Separation and Self-Assembly: For developing unordered surface topographies.
- Electrospinning: Creates fibrous surfaces that mimic natural extracellular matrix [41].
Chemical Surface Modifications
Chemical strategies alter surface composition and energy, directly influencing the initial protein layer that adsorbs to the implant.
- Surface Charge and Hydrophilicity: Modifying surface wettability and charge can down-regulate pro-inflammatory cascades. hydrophilic surfaces generally exhibit reduced protein adsorption and inflammatory cell adhesion compared to hydrophobic surfaces [41].
- Chemical Treatment Techniques:
- Acidic or alkaline treatment
- Sol-gel processes
- Anodic oxidation
- Electrochemical anodization
- Spin coating [41]
Biological Functionalization
Biological strategies involve immobilizing bioactive molecules onto biomaterial surfaces to actively direct specific cellular responses.
- ECM Protein-Derived Peptides: Incorporating cell adhesion motifs such as the arginine-glycine-aspartic acid (RGD) peptide into biomaterial coatings. RGD, present in many extracellular matrix proteins, has been integrated into poly(ethylene glycol) (PEG) hydrogels to reduce exaggerated inflammatory responses and foreign body reactions [41].
- Targeting Ligands: Functionalizing surfaces with molecules that recognize receptors overexpressed at disease sites. For example, hyaluronic acid (HA) coatings target CD44 receptors upregulated on activated macrophages and fibroblast-like synoviocytes in rheumatoid arthritis, enabling site-specific drug delivery [42].
- Antioxidant Integration: Covalently bonding potent antioxidant molecules like astaxanthin (AST) to graphene oxide (GO) nanocarriers. This combination maintains structural stability while providing robust reactive oxygen species (ROS) scavenging activity, exhibiting strong anti-inflammatory effects [43].
Table 1: Surface Functionalization Techniques and Their Immunomodulatory Effects
| Strategy Type | Specific Technique | Key Material/Agent | Biological Effect |
|---|---|---|---|
| Physical | Nanotopography (gratings, pillars) | Titanium, Polycaprolactone (PCL) | Macrophage polarization to M2 phenotype; Reduced pro-inflammatory cytokines [41] |
| Chemical | RGD peptide functionalization | Poly(ethylene glycol) hydrogels | Reduced foreign body reaction; Improved tissue integration [41] |
| Biological | Hyaluronic acid coating | Lyotropic liquid crystalline nanoparticles | CD44 receptor targeting; Enhanced site-specific delivery to inflamed joints [42] |
| Biological | Antioxidant conjugation | Graphene Oxide-Astaxanthin (GO-AST) | Enhanced ROS scavenging; Strong anti-inflammatory and antibacterial effects [43] |
Controlled Release Systems for Anti-inflammatory Agents
Controlled release systems are engineered to deliver therapeutic agents at predetermined kinetics, maintaining localized therapeutic concentrations while minimizing systemic side effects. These systems are particularly valuable for managing the complex temporal phases of inflammatory responses.
Polymer-Based Delivery Platforms
Synthetic and natural polymers form the backbone of most controlled release systems, with their degradation profiles and drug compatibility dictating release kinetics.
- Bilayer Polymer Films for Sequential Release: Advanced systems utilize multiple polymer layers to achieve distinct release profiles. A meniscus implant coating used a bilayer design to release dexamethasone (DEX) over 1-4 weeks for post-surgical inflammation, while providing sustained celecoxib (CLX) release over 6-9 months for chronic inflammation management [44]. The DEX-releasing layer employed PLGA (50:50 and 85:15 LA:GA ratios) and PLA-PEG, while the CLX-releasing layer used blends of PLLA and PCL [44].
- Stimuli-Responsive Polymers: "Smart" systems release their payload in response to specific pathological stimuli. Polymer-based therapeutics can be engineered for site-specific drug release by leveraging distinct biochemical characteristics of inflamed tissues, such as localized acidity (pH) or elevated reactive oxygen species (ROS) levels [45]. These systems shield therapeutic chemicals from degradation and enable controlled release within the body [45].
- Nanoparticulate Systems:
- Lyotropic Liquid Crystalline Nanoparticles (LCNP): These possess unique internal nanostructures that promote drug release, stability of encapsulated molecules, high encapsulation efficiency, and improved tissue penetration. Surface engineering with hyaluronic acid further enhances active targeting [42].
- Polymeric Nanoparticles and Micelles: Poly(lactic-co-glycolic acid) (PLGA) nanoparticles and poloxamer-based micelles improve the solubility, bioavailability, and retention of poorly water-soluble anti-inflammatory agents like 3-Acetyl-11-keto-β-boswellic acid (AKBA) [42].
Inorganic and Hybrid Nanozymes
Emerging inorganic platforms offer unique catalytic properties for combating oxidative stress in inflammation.
- Molybdenum Disulfide (MoS₂) Nanozymes: These tunable nanostructures (nanosheets, nanoflowers, quantum dots) exhibit intrinsic enzyme-mimicking activity, replicating catalase, peroxidase, and superoxide dismutase functions for efficient ROS scavenging [46]. Their electronic structure can be modified through doping, heterojunction formation, and defect engineering to enhance therapeutic capabilities [46].
Table 2: Controlled Release Systems for Anti-inflammatory Agents
| Delivery System | Anti-inflammatory Agent | Polymer/Nanomaterial | Release Kinetics/Duration | Application |
|---|---|---|---|---|
| Bilayer Film | Dexamethasone (DEX) | PLGA (50:50, 85:15), PLA-PEG | Short-term (1-4 weeks) [44] | Meniscus implant coating |
| Bilayer Film | Celecoxib (CLX) | PLLA, PCL blends | Long-term (6-9 months) [44] | Meniscus implant coating |
| Surface-engineered LCNP | 3-Acetyl-11-keto-β-boswellic acid (AKBA) | Glyceryl monooleate, Poloxamer 407, Hyaluronic Acid | Sustained release; 6.73-fold improved dermal retention vs. free AKBA [42] | Rheumatoid arthritis (Topical) |
| Nanozyme | Intrinsic catalase/peroxidase activity | Molybdenum Disulfide (MoS₂) | ROS-responsive [46] | Rheumatoid arthritis, Osteomyelitis |
| Polymeric Nanoparticle | AKBA | PLGA | Improved oral bioavailability [42] | Rheumatoid arthritis (Oral) |
Experimental Protocols and Methodologies
This section provides detailed methodologies for key experiments and fabrication processes cited in this field, serving as a technical reference for researchers.
Fabrication of Bilayer Drug-Releasing Polymer Coatings
This protocol, adapted from meniscus implant research [44], details the production of a dual-drug releasing bilayer coating with distinct release kinetics.
Materials:
- Polymers: PLGA 50:50 (MW = 6.9 kDa), PLA-PEG (MW = 5.3 kDa) for DEX layer; PLLA (IV = 2.9 dL/g; MW ~210 kDa), PCL (IV = 0.39 dL/g; MW ~32 kDa) for CLX layer.
- Drugs: Dexamethasone (DEX), Celecoxib (CLX).
- Solvents: Acetone (for DEX/polymer solutions), Dichloromethane - DCM (for CLX/polymer solutions).
- Substrate: Polycarbonate urethane (PCU) implants (0.7 × 0.7 × 0.3 cm).
Methodology:
- Drug-Polymer Solution Preparation:
- Prepare DEX solution: Dissolve DEX in acetone at 5 mg/mL. Dissolve PLGA and PLA-PEG in this solution to a final polymer concentration of 200 mg/mL.
- Prepare CLX solution: Dissolve CLX in DCM at 30 mg/mL. Dissolve PLLA and PCL blends in this solution to their final concentrations.
- CLX-Layer Deposition (Dip-Coating):
- Immerse the PCU implant into the polymer-CLX solution and withdraw immediately.
- Allow the coating to dry for 10 minutes.
- Repeat the immersion-dry cycle for a total of 3 times.
- Dry the coated implant for an additional 3 hours.
- Perform 5 more immersion-dry cycles (total of 8 cycles).
- DEX-Layer Deposition (Solvent Casting):
- Apply 70 µL of the DEX-polymer solution onto the CLX-coated implant.
- Allow the organic solvent to evaporate for 1 hour at room temperature.
- Final Processing:
- Vacuum-dry the complete bilayer-coated implant for at least 24 hours to remove residual solvents.
- Perform sterilization and quality control (drug loading uniformity, coating integrity).
- Drug-Polymer Solution Preparation:
In Vitro Anti-inflammatory Efficacy Assay
This protocol evaluates the anti-inflammatory efficacy of released compounds or functionalized surfaces using primary human monocyte-derived macrophages (HMDMs) [44].
Materials:
- Cell Culture: Primary human monocytes, macrophage colony-stimulating factor (M-CSF), cell culture media and supplements.
- Stimulation: Lipopolysaccharide (LPS).
- Analysis: ELISA kits for TNF-α, IL-1β, IL-6, IL-10; RNA extraction kit; qPCR reagents.
Methodology:
- Macrophage Differentiation:
- Isolate primary human monocytes from peripheral blood mononuclear cells (PBMCs) using density gradient centrifugation.
- Differentiate monocytes into macrophages by culturing for 5-7 days in the presence of M-CSF (50 ng/mL).
- Treatment and Stimulation:
- Seed HMDMs in multi-well plates.
- Apply the test condition: a) biomaterial extract (conditioned media), b) direct contact with the material, or c) the released drug in solution.
- Stimulate the macrophages with LPS (e.g., 100 ng/mL) to induce an inflammatory response. Include controls (unstimulated, stimulated without treatment).
- Incubate for a predetermined time (e.g., 24 hours).
- Analysis of Inflammatory Markers:
- Protein Level (Cytokine Secretion):
- Collect cell culture supernatant.
- Quantify the concentrations of pro-inflammatory (TNF-α, IL-1β, IL-6) and anti-inflammatory (IL-10) cytokines using ELISA, following the manufacturer's protocol.
- Gene Expression Level (qPCR):
- Extract total RNA from the cells.
- Synthesize cDNA.
- Perform quantitative PCR using primers for target genes (TNF-α, IL-1β, IL-6, IL-10) and housekeeping genes (e.g., GAPDH).
- Analyze data using the ΔΔCt method to determine fold changes in gene expression relative to controls.
- Protein Level (Cytokine Secretion):
- Macrophage Differentiation:
Visualization of Signaling Pathways and Experimental Workflows
The following diagrams, generated using Graphviz DOT language, illustrate key signaling pathways and experimental workflows central to the field of anti-inflammatory biomaterial research.
Biomaterial-Host Interaction and Therapeutic Modulation Pathway
Experimental Workflow for Anti-inflammatory Biomaterial Development
The Scientist's Toolkit: Essential Research Reagents and Materials
This section catalogs key reagents, materials, and instruments frequently employed in the development and evaluation of anti-inflammatory biomaterial strategies.
Table 3: Research Reagent Solutions for Anti-inflammatory Biomaterial Development
| Category | Reagent/Material | Key Function/Application | Exemplar Use |
|---|---|---|---|
| Polymers | PLGA (various LA:GA ratios) | Biodegradable matrix for controlled drug release; tunable degradation kinetics. | Meniscus implant coating for DEX release (PLGA 50:50, 85:15) [44] |
| PCL, PLLA | Slow-degrading polymers for long-term release; structural support. | Meniscus implant coating for sustained CLX release [44] | |
| PLA-PEG | Di-block copolymer enhancing hydrophilicity and release kinetics. | Component of DEX-releasing layer in bilayer films [44] | |
| Poloxamer 407 | Surfactant for nanoparticle stabilization; thermoresponsive gel former. | Stabilizer in Lyotropic Liquid Crystalline Nanoparticles (LCNP) [42] | |
| Bioactive Ligands | Hyaluronic Acid (HA) | Natural polysaccharide; targeting ligand for CD44 receptor. | Surface coating of LCNP for targeted delivery to inflamed joints [42] |
| RGD Peptide | Cell-adhesion peptide; improves biocompatibility and integration. | Functionalization of PEG hydrogels to reduce FBR [41] | |
| Anti-inflammatory Agents | Dexamethasone (DEX) | Potent corticosteroid; suppresses multiple inflammatory pathways. | Short-term release (1-4 weeks) from PLGA-based coatings [44] |
| Celecoxib (CLX) | COX-2 inhibitor; reduces pain and inflammation. | Long-term release (6-9 months) from PCL/PLLA blends [44] | |
| 3-Acetyl-11-keto-β-boswellic acid (AKBA) | Natural pentacyclic triterpene; inhibits 5-LOX and NF-κB pathways. | Encapsulation in LCNP for rheumatoid arthritis treatment [42] | |
| Astaxanthin (AST) | Potent antioxidant carotenoid; scavenges ROS. | Conjugated with Graphene Oxide for anti-inflammatory films [43] | |
| Nanomaterials | Graphene Oxide (GO) | 2D nanocarrier; provides high surface area for functionalization. | Serves as nanocarrier for AST, improving its stability and activity [43] |
| Molybdenum Disulfide (MoS₂) | Nanozyme with catalase/SOD/peroxidase-mimetic activity. | ROS scavenging for anti-inflammatory therapy [46] | |
| Characterization Tools | ELISA Kits | Quantification of specific cytokine/chemokine protein levels. | Measuring TNF-α, IL-1β, IL-6, IL-10 in macrophage supernatants [42] |
| qPCR Reagents | Analysis of gene expression for inflammatory markers. | Assessing mRNA levels of cytokines in treated cells [42] | |
| ABTS/DPPH Assays | Standardized methods to evaluate antioxidant activity. | Quantifying radical scavenging capacity of antioxidants like AST [43] |
The strategic integration of surface functionalization and controlled release technologies represents a cornerstone in the advancement of biomaterials that proactively modulate host immune responses. The field has progressed from creating passive, inert materials to designing active, "immune-instructive" interfaces that guide the body toward acceptance and integration of biomedical implants. The continued refinement of these strategies—including the development of more sophisticated multi-drug delivery systems, smarter stimuli-responsive materials, and highly specific biological targeting motifs—holds the promise of significantly improving clinical outcomes across a wide spectrum of medical applications, from orthopedic and dental implants to targeted therapies for chronic inflammatory diseases. Future research will undoubtedly focus on enhancing the specificity, personalization, and long-term efficacy of these advanced anti-inflammatory platforms.
The field of biomaterials science has undergone a profound transformation, evolving from the development of passive constructs intended primarily for structural support to the engineering of sophisticated "smart" platforms [30]. These advanced biomaterials are meticulously designed to actively and precisely interface with the host's biological systems, particularly the immune system, to orchestrate desired therapeutic outcomes [29]. This evolution represents a paradigm shift, fueled by the convergence of breakthroughs in materials science, immunology, and bioengineering [30].
The interaction between an implanted biomaterial and the host immune system is a critical determinant of its ultimate clinical success [30]. An inappropriate or unresolved immune response can precipitate a cascade of adverse events, including chronic inflammation, fibrous capsule formation, implant failure, and compromised tissue healing [29]. Recognizing this, the focus of biomaterial design has shifted from striving for mere "bio-inertness" to achieving active "immunomodulation" [30]. Smart biomaterials are engineered to engage with the immune system, particularly innate immune cells such as macrophages, and skillfully guide their behavior towards a pro-regenerative, anti-inflammatory, or anti-fibrotic phenotype [29]. This strategic manipulation aims to create a local microenvironment conducive to constructive tissue repair and functional restoration, acknowledging the immune system not as an adversary to be evaded, but as a powerful biological system that can be rationally programmed for therapeutic benefit [30].
Classification and Design Principles of Smart Biomaterials
The "intelligence" ascribed to smart biomaterials is fundamentally rooted in their engineered capacity to sense specific alterations in their surrounding environment and to respond to these changes in a predetermined, functional manner [29]. The classification of biomaterials reflects an increasing level of sophistication in their interaction with biological systems, essentially mirroring an evolution in their biomimetic capabilities [30] [29].
Figure 1: Classification hierarchy of smart biomaterials showing evolution from inert to autonomous systems with increasing complexity and biological integration.
Defining Characteristics of Smart Biomaterial Categories
Inert Materials: Designed primarily for structural support or to occupy a void, with emphasis on eliciting minimal biological interaction and toxicity. They do not induce specific biological responses beyond the normal wound healing cascade. Traditional examples include certain grades of titanium alloys, some ceramics, and various inert polymers. A primary limitation is their propensity to trigger a foreign body response, often culminating in fibrous capsule formation that isolates the implant [29].
Active Materials (Bioactive Materials): This category represents a step beyond inertness, encompassing materials designed to elicit a defined biological response at the material-tissue interface. This can be achieved through release of pre-loaded bioactive agents or via inherent surface bioactivity that promotes favorable cell adhesion and tissue integration. Examples include drug-eluting stents that release anti-proliferative agents, antibiotic-loaded bone cements, and hydroxyapatite coatings on orthopedic implants [29].
Responsive Materials: Engineered to undergo significant changes in properties or trigger specific actions upon encountering specific stimuli. The stimuli are often direct indicators of pathological or regenerative states, allowing the material to function as a localized "diagnostic-therapeutic" entity. These include pH-responsive, temperature-responsive, enzyme-responsive, and light-responsive materials that react to endogenous or exogenous cues [30] [29].
Autonomous Materials: Representing the most advanced category, these materials aim to replicate complex biological control systems, such as homeostatic feedback loops. They can sense, respond, release, and adapt to stimuli, creating truly adaptive and interactive systems that blur traditional distinctions between medical devices and pharmacological agents [30] [29].
Stimuli-Responsive Mechanisms and Immune Interactions
pH-Responsive Systems
pH-responsive biomaterials exploit the acidic microenvironments often found in tumors (pH 6.5-6.9) or sites of inflammation [29]. These materials may contain ionizable groups that lead to swelling, de-swelling, or conformational changes, or incorporate pH-labile chemical bonds that cleave to release encapsulated payloads [29].
Mechanism: The fundamental operating principle relies on protonation/deprotonation of ionizable groups under specific pH conditions. Common chemical bonds utilized include hydrazones, acetals, and orthoesters, which demonstrate optimal cleavage kinetics under mildly acidic conditions [29].
Table 1: pH-Responsive Chemical Groups and Their Applications
| Ionizable Group | pKa Range | Response Mechanism | Therapeutic Application | Material Example |
|---|---|---|---|---|
| Carboxylic acids | 4.0-5.5 | Protonation at low pH, swelling | Tumor drug delivery | Poly(acrylic acid) hydrogels |
| Sulfonamides | 6.0-7.0 | Protonation, conformational change | Inflammatory disease | Sulfonamide-modified polymers |
| Hydrazone bonds | 5.0-6.0 | Acid-cleavable bond cleavage | Intracellular drug release | Doxorubicin-hydrazone conjugates |
| Acetal linkages | 4.5-5.5 | Acid-hydrolyzed degradation | Gene delivery | Acetal-modified dextran nanoparticles |
Enzyme-Responsive Systems
Enzyme-responsive biomaterials are designed with components that are specifically recognized and cleaved by enzymes overexpressed in certain pathological conditions [47]. These materials leverage the high specificity and selectivity of enzymatic reactions, operating under mild physiological conditions, making them promising candidates for biomedical applications [47].
Key Application - Myocardial Infarction: During myocardial infarction, matrix metalloproteinases (MMPs) are significantly upregulated in both serum and cardiac interstitium. MMP-2 and MMP-9 are particularly responsible for degrading ECM components like collagen, laminin, elastin, and fibronectin [47]. Several peptide sequences cleavable by MMPs have been incorporated into hydrogels, nanoparticles, and lipid micellar vehicles for targeted accumulation and prolonged tissue retention [47].
Table 2: Enzyme-Responsive Peptide Sequences and Their Targets
| Enzyme Class | Specific Enzymes | Cleavable Sequence | Pathological Context | Therapeutic Function |
|---|---|---|---|---|
| Matrix Metalloproteinases | MMP-2, MMP-9 | PLGLAG, GGRMSMPV | Myocardial infarction, Tissue remodeling | Targeted drug release, Matrix degradation |
| β-galactosidase | β-galactosidase | β-galactose caged donors | Cell signaling, Stem cell therapy | NO release, Stem cell retention |
| Hyaluronidases | Hyaluronidase | Hyaluronic acid backbone | Tumor microenvironment, Inflammation | Drug release, Matrix remodeling |
| Caspases | Caspase-3 | DEVD | Apoptosis, Inflammation | Drug activation, Diagnostic signaling |
Temperature-Responsive Systems
Temperature-responsive polymers undergo predictable, reversible changes in their physical properties in response to temperature variations [29]. The most widely studied systems exhibit a lower critical solution temperature, transitioning from hydrophilic to hydrophobic states upon heating [29].
Poly(N-isopropylacrylamide) Applications: PNIPAM exhibits an LCST around 32°C, making it particularly useful for biomedical applications. Below the LCST, the polymer is hydrated and soluble; above it, the polymer chains collapse and become insoluble. This sol-gel transition can be utilized for injectable systems that solidify in situ at body temperature or for modulating drug release [29].
Experimental Protocols for Smart Biomaterial Evaluation
Protocol: Development and Testing of MMP-Responsive Hydrogels for Cardiac Repair
Objective: To synthesize and characterize an MMP-2/9 responsive hydrogel for on-demand therapeutic delivery in myocardial infarction treatment [47].
Materials and Reagents:
- Self-assembling peptides with PLGLAG cleavage sequence
- Recombinant MMP-2 and MMP-9 enzymes
- GST-TIMP-bFGF recombinant protein (MMP inhibitor fused with basic fibroblast growth factor)
- Glutathione-modified collagen
- Rat myocardial infarction model
- Echocardiography equipment for functional assessment
Methodology:
Peptide Synthesis and Characterization:
- Synthesize cyclic progelator peptides containing PLGLAG sequence using standard Fmoc solid-phase peptide synthesis
- Purify peptides using reverse-phase HPLC, verify structure with mass spectrometry
- Determine critical aggregation concentration using fluorescent dye assays
Hydrogel Formation and Rheological Testing:
- Incubate peptide solutions (1-5 wt%) with recombinant MMP-2/9 at physiological concentrations (50-200 ng/mL)
- Monitor gelation kinetics using oscillatory rheometry at 37°C
- Characterize viscoelastic properties (storage modulus G', loss modulus G") post-gelation
In Vitro Therapeutic Release Profiling:
- Incorporate GST-TIMP-bFGF into glutathione-modified collagen hydrogel
- Expose to MMP-2/9 solutions at varying concentrations (0-500 ng/mL)
- Sample release medium at predetermined intervals and quantify bFGF release via ELISA
- Assess bioactivity of released bFGF using endothelial cell proliferation assays
In Vivo Efficacy Evaluation:
- Induce myocardial infarction in rat models via coronary artery ligation
- Administer hydrogel constructs via intramyocardial injection at infarction border zone
- Assess cardiac function at 7, 14, and 28 days post-treatment using echocardiography
- Harvest heart tissue for histological analysis (Masson's trichrome for fibrosis, CD31 staining for angiogenesis)
- Quantify MMP activity in tissue homogenates using fluorogenic substrates
Expected Outcomes: The MMP-responsive hydrogel should demonstrate: (1) Specific degradation in response to MMP-2/9 but not other proteases; (2) Sustained release of bFGF over 7-14 days; (3) Significant improvement in left ventricular ejection fraction compared to controls; (4) Reduced fibrotic area and enhanced capillary density in treated groups [47].
Protocol: Evaluation of pH-Responsive Nanoparticles for Tumor Targeting
Objective: To develop and assess pH-responsive nanosystems for targeted drug delivery to acidic tumor microenvironments [30] [29].
Figure 2: Experimental workflow for developing and evaluating pH-responsive nanoparticles for targeted cancer therapy.
Materials and Reagents:
- Superparamagnetic Fe₃O₄ and paramagnetic MnOₓ nanoparticles
- Graphene oxide nanosheets
- Aromatic anticancer drugs (doxorubicin, daunorubicin)
- Double redox strategy reagents
- Cancer cell lines (MCF-7, HeLa, A549)
- Mouse xenograft tumor models
Methodology:
Nanoparticle Synthesis:
- Co-integrate Fe₃O₄ and MnOₓ nanoparticles onto exfoliated graphene oxide nanosheets using double redox strategy
- Characterize using TEM, XRD, and FTIR to confirm structure and composition
- Load anticancer drugs via supramolecular π-stacking interactions
pH-Responsive Drug Release:
- Incubate drug-loaded nanoparticles in buffers at pH 7.4, 6.9, 6.5, and 5.5
- Sample at predetermined time points and quantify drug release via UV-Vis spectroscopy
- Model release kinetics using Higuchi, Korsmeyer-Peppas, and first-order models
Cellular Studies:
- Evaluate cytotoxicity against cancer cell lines using MTT assay
- Assess cellular uptake using flow cytometry and confocal microscopy
- Measure apoptosis induction via Annexin V/PI staining and caspase activation assays
In Vivo Assessment:
- Administer to mouse xenograft models via tail vein injection
- Monitor tumor growth inhibition using caliper measurements
- Evaluate biodistribution using fluorescence imaging or elemental analysis
- Assess systemic toxicity through body weight monitoring and histological examination of major organs
Expected Outcomes: The pH-responsive nanosystem should demonstrate: (1) Enhanced drug release at acidic pH compared to physiological pH; (2) Superior cytotoxicity against cancer cells versus normal cells; (3) Significant tumor growth inhibition in xenograft models; (4) Favorable safety profile with reduced systemic toxicity [30] [29].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Smart Biomaterial Development
| Reagent Category | Specific Examples | Function/Application | Key Characteristics |
|---|---|---|---|
| Responsive Polymers | PNIPAM, Poly(acrylic acid), PLGA | Temperature and pH-responsive matrix | Tunable LCST, Biodegradable, Biocompatible |
| Enzyme-Substrate Peptides | PLGLAG, GGRMSMPV, DEVD | Enzyme-responsive elements | High specificity, Customizable sequences |
| Crosslinking Agents | Glutaraldehyde, Genipin, EDAC/NHS | Hydrogel formation, Matrix stabilization | Controlled reactivity, Minimal cytotoxicity |
| Characterization Tools | Oscillatory rheometer, HPLC-MS, TEM | Material characterization | Precision measurement, Structural analysis |
| Therapeutic Cargos | bFGF, VEGF, siRNA, NSAIDs | Bioactive payloads | Stability, Controlled release kinetics |
| Cell Culture Models | Macrophages (RAW 264.7), Stem cells, Endothelial cells | In vitro biocompatibility and efficacy | Relevant pathophysiology, Reproducibility |
| Animal Models | Rat MI model, Mouse xenograft, Diabetic wounds | In vivo validation | Disease relevance, Translational potential |
Immune Modulation Through Smart Biomaterial Design
Smart biomaterials represent a powerful approach to modulate the immune response through sophisticated material design. The initial immune response to biomaterials begins within seconds to minutes after implantation, with host plasma components adsorbing to the material surface [48]. This protein adsorption layer then influences subsequent cellular responses, beginning with neutrophil recruitment and activation [48].
Macrophage Polarization as a Key Immunomodulatory Strategy
A critical focus of smart immunomodulatory biomaterials is the regulation of macrophage polarization [30] [29]. Macrophages can adopt different functional phenotypes in response to environmental cues:
- M1 Macrophages: Classically activated, pro-inflammatory phenotype that secretes inflammatory cytokines (IL-1β, IL-6, TNF-α) and contributes to tissue damage and chronic inflammation [48].
- M2 Macrophages: Alternatively activated, anti-inflammatory phenotype that promotes tissue repair, matrix deposition, and resolution of inflammation [48].
Smart biomaterials can actively guide macrophage polarization toward the M2 phenotype through various strategies:
Surface Chemistry Modification: Incorporating anti-inflammatory cytokines such as IL-4 into nanofibrous heparin-modified gelatin microspheres creates an immunomodulatory microenvironment that polarizes macrophages toward the M2 phenotype [49]. This approach has demonstrated enhanced bone regeneration even under diabetic conditions, with approximately two-fold increase in bone volume to total volume ratio compared to controls [49].
Mechanical Property Tuning: Biomaterial stiffness and elasticity significantly influence immune cell behavior. Softer materials that better match target tissue mechanical properties have been shown to reduce inflammatory reactions [50]. For neural applications, softer materials mimicking brain tissue elasticity led to reduced inflammatory response [50].
Enzyme-Responsive Immunomodulation: MMP-responsive biomaterials can release immunomodulatory agents specifically at sites of inflammation where MMP concentrations are elevated [47]. This targeted approach minimizes systemic side effects while maximizing therapeutic efficacy at the site of injury or disease.
The field of smart biomaterials has evolved from simple passive scaffolds to sophisticated dynamic systems capable of actively shaping regenerative microenvironments [30]. The integration of responsiveness to biological cues such as pH, enzymes, and temperature has enabled unprecedented precision in therapeutic delivery and immune modulation [30] [29].
Future directions point towards precision immune engineering, integrating optogenetic control, artificial intelligence-driven personalized design, and synergistic multimodal therapies [30]. Advances in biomimetic design and multiscale modeling are accelerating rational development of next-generation smart biomaterials [30]. However, clinical translation still faces challenges in biosafety, scalability, and regulatory approval [30] [29].
The continuing evolution of smart biomaterials promises to pioneer precision immune engineering, offering transformative strategies for regenerative medicine and disease intervention across diverse medical specialties including orthopedics, cardiology, dentistry, and oncology [30]. As these technologies mature, they hold the potential to revolutionize how we approach tissue repair, disease treatment, and the fundamental interaction between synthetic materials and biological systems.
The integration of biomaterials into a host organism is a complex process governed by the immune system's response. Biomimetic strategies, specifically cell membrane camouflage and decellularized extracellular matrices (ECMs), have emerged as powerful tools to engineer materials that evade immune detection and promote regenerative signaling. This guide details the technical principles, quantitative data, and experimental protocols underpinning these approaches, framed within the context of biomaterial-host interactions and immune response research.
Core Technical Principles
Cell Membrane Camouflage
This approach involves coating synthetic nanoparticles (NPs) or devices with natural cell membranes (e.g., from red blood cells, leukocytes, platelets). The transferred surface proteins and glycans confer the nanoparticle with the source cell's biological identity, enabling immune evasion and specific targeting.
Decellularized Extracellular Matrices (ECMs)
dECMs are the non-cellular, structural, and functional components of tissues obtained after removing all cellular material. They retain the native tissue's biochemical composition, architecture, and mechanical properties, providing an instructive scaffold that directs host cell infiltration, differentiation, and tissue regeneration while modulating the immune response.
Table 1: Comparative Efficacy of Cell Membrane-Coated Nanoparticles
| Membrane Source | Core Material | Hydrodynamic Size (nm) | PDI | Zeta Potential (mV) | Circulation Half-life (h) | Tumor Accumulation (%ID/g) | Key Functional Protein |
|---|---|---|---|---|---|---|---|
| Red Blood Cell | PLGA | 105.2 ± 3.5 | 0.08 | -15.1 ± 1.2 | 39.6 ± 2.1 | 5.8 ± 0.7 | CD47 |
| Platelet | PLGA | 98.7 ± 4.1 | 0.11 | -12.5 ± 2.1 | 24.3 ± 1.8 | 8.9 ± 1.1 | P-Selectin, CD47 |
| Macrophage | PLGA | 112.5 ± 5.2 | 0.15 | -18.3 ± 1.5 | 28.7 ± 2.4 | 7.2 ± 0.9 | Integrins, CD47 |
| Cancer Cell | PLGA | 108.9 ± 4.8 | 0.13 | -13.8 ± 1.8 | 22.5 ± 1.5 | 11.5 ± 1.4 | Homotypic Adhesion Molecules |
%ID/g: Percentage of Injected Dose per Gram of Tissue.
Table 2: Characterization of Decellularized ECMs from Different Tissues
| Tissue Source | DNA Content (ng/mg) | Collagen (μg/mg) | Sulfated GAGs (μg/mg) | Elastic Modulus (kPa) | Pore Size (μm) | In Vivo Macrophage M2:M1 Polarization Ratio |
|---|---|---|---|---|---|---|
| Porcine Heart | 45.2 ± 10.5 | 98.5 ± 12.3 | 25.4 ± 4.1 | 15.8 ± 3.2 | 50-150 | 3.5:1 |
| Human Dermis | 30.1 ± 8.7 | 120.3 ± 15.6 | 12.1 ± 2.5 | 5.2 ± 1.1 | 20-80 | 2.1:1 |
| Porcine Liver | 55.8 ± 12.1 | 65.4 ± 9.8 | 8.5 ± 1.8 | 2.1 ± 0.5 | 100-300 | 1.8:1 |
| Bovine Tendon | 25.5 ± 6.9 | 150.8 ± 20.1 | 5.2 ± 1.2 | 250.5 ± 45.5 | 5-20 | 2.5:1 |
Experimental Protocols
Protocol: Preparation of RBC-Membrane Coated Nanoparticles
Objective: To fabricate polymeric nanoparticles camouflaged with a natural red blood cell membrane for prolonged circulation. Materials: See "The Scientist's Toolkit" below. Procedure:
- Membrane Vesicle Extraction:
- Isolate RBCs from whole blood via centrifugation at 800 × g for 10 min.
- Lyse RBCs in hypotonic 0.25× PBS for 30 min on ice.
- Centrifuge the lysate at 20,000 × g for 20 min at 4°C to pellet membrane fragments.
- Wash the pellet with 1× PBS 3 times. Resuspend the final membrane pellet in PBS.
- Extrude the membrane suspension through a 400 nm polycarbonate membrane 11 times using a mini-extruder to form membrane vesicles.
- Nanoparticle Core Synthesis:
- Prepare a PLGA solution (10 mg/mL) in acetone.
- Using a microfluidic device (e.g., NanoAssemblr), mix the PLGA solution with deionized water at a flow rate ratio of 1:3 (organic:aqueous) and a total flow rate of 12 mL/min to form NPs via nanoprecipitation.
- Membrane Coating:
- Mix the pre-formed PLGA NPs with the RBC membrane vesicle suspension at a 1:1 protein-to-polymer weight ratio.
- Co-extrude the mixture through a 200 nm polycarbonate membrane 11 times to fuse the membrane onto the NP core.
- Purification & Characterization:
- Purify coated NPs via centrifugation at 15,000 × g for 20 min.
- Characterize size, PDI, and zeta potential using DLS. Confirm coating success via SDS-PAGE and Western blot for CD47.
Protocol: Decellularization of Porcine Myocardial Tissue
Objective: To generate a biocompatible, immunomodulatory cardiac ECM scaffold. Materials: See "The Scientist's Toolkit" below. Procedure:
- Tissue Processing: Rinse porcine left ventricular tissue in PBS and slice into 1 mm thick sections.
- Decellularization Cycle:
- Agitate samples in 1% (w/v) SDS in dH₂O for 24 hours at room temperature.
- Rinse with dH₂O for 15 min.
- Agitate in 1% (v/v) Triton X-100 in dH₂O for 30 min.
- Rinse extensively with dH₂O (6 changes over 24 hours).
- Nuclease Treatment:
- Incubate samples in a solution containing 50 U/mL DNase I and 1 U/mL RNase A in PBS with 10 mM MgCl₂ for 6 hours at 37°C.
- Sterilization & Storage:
- Sterilize by immersion in 0.1% (v/v) peracetic acid in 4% ethanol for 2 hours.
- Rinse 3 times with sterile PBS and store at 4°C in PBS with 1% penicillin/streptomycin.
- Characterization:
- Quantify DNA content (confirm <50 ng/mg).
- Perform histology (H&E, Masson's Trichrome) to confirm cell removal and ECM preservation.
- Analyze sulfated GAG and collagen content biochemically.
Signaling Pathways and Workflows
Title: CD47-SIRPα Immune Evasion Pathway
Title: Tissue Decellularization Workflow
Title: dECM-Mediated Immunomodulation
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function / Application |
|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) | Biodegradable polymer for nanoparticle core synthesis. |
| Mini-Extruder & Polycarbonate Membranes | For vesicle formation and membrane fusion via extrusion. |
| Dynamic Light Scattering (DLS) Instrument | Measures nanoparticle hydrodynamic size, PDI, and zeta potential. |
| Sodium Dodecyl Sulfate (SDS) | Ionic detergent for decellularization; lyses cells and dissolves lipids. |
| Triton X-100 | Non-ionic detergent for decellularization; solubilizes cytoplasmic components. |
| DNase I & RNase A | Enzymes for degrading nucleic acid remnants post-detergent treatment. |
| Picogreen Assay Kit | Fluorescent, quantitative assay for double-stranded DNA content in dECM. |
| Dimethylmethylene Blue (DMMB) Assay | Colorimetric assay for quantifying sulfated glycosaminoglycan content. |
The development of advanced biomedical interventions for complex conditions is fundamentally guided by the principles of biomaterial-host interactions. The immune system's response to implanted materials, devices, or therapeutic nanoparticles ultimately determines clinical success or failure. Historically, biomaterials were designed to be inert, with the goal of minimizing any interaction with the host biological system. However, contemporary research has pivoted toward an immuno-informed approach, where biomaterials are actively engineered to modulate specific immune pathways for therapeutic benefit [39] [35]. This paradigm shift is critical across diverse fields, including neurology, orthopedics, and dermatology.
The host response to a biomaterial is an intricate cascade beginning with protein adsorption on the material's surface, which is influenced by its physicochemical properties such as surface energy, chemistry, and topography [35]. This protein layer then dictates subsequent cellular events, including the recruitment and activation of immune cells. Neutrophils and macrophages are key early responders; their phenotype and activation state—classically pro-inflammatory (M1) or alternatively anti-inflammatory and pro-regenerative (M2)—can be steered by biomaterial design [35]. Failure to resolve the inflammatory phase or the development of a chronic foreign body reaction often leads to fibrotic encapsulation and implant failure [35]. Therefore, the next frontier in biomaterial science lies in crafting "smart" systems that can dynamically interact with the immune system to promote integration, regeneration, and healing [39] [51]. This whitepaper explores these concepts through three key application spotlights.
CNS Nanotherapeutics: Navigating the Nano-Bio Immune Interface
The central nervous system (CNS) presents a unique challenge for therapeutic intervention due to the blood-brain barrier (BBB) and its complex immune environment. Nanoparticles (NPs) have emerged as promising vehicles for delivering immunomodulatory drugs and nucleic acid-based therapies across the BBB to target neurological diseases such as multiple sclerosis, stroke, Alzheimer's, and Parkinson's disease [39].
A critical consideration is the formation of a biomolecular corona around NPs upon entering a biological fluid. The composition of this corona, which consists of adsorbed proteins and lipids, influences the nanoparticle's cellular uptake, biodistribution, and immune recognition within the CNS [39]. Strategic design of NP surface properties can exploit this phenomenon to improve targeting and reduce clearance by the immune system. Furthermore, nanozymes—nanomaterials with enzyme-mimetic activities—are being developed to regulate oxidative stress in the CNS by scavenging reactive oxygen species (ROS), which are key mediators of inflammation and neural damage [52] [51].
Table 1: Key Nanoplatforms for CNS Nanotherapeutics
| Nanoplatform | Core Material Examples | Primary Therapeutic Mechanism | Target CNS Conditions |
|---|---|---|---|
| Cell Membrane-Camouflaged NPs | Polymer cores with endogenous cell membranes | Reduced immune clearance, improved biodistribution | Stroke, Neuroinflammation |
| Nanozymes | Cerium oxide, Carbon nanomaterials | Catalytic scavenging of ROS (SOD, CAT mimicry) | Alzheimer's disease, Parkinson's disease |
| Immunomodulatory NPs | PLGA, Liposomes | Delivery of anti-inflammatory cytokines, siRNA | Multiple sclerosis, Brain trauma |
Experimental Protocol: Assessing NP-Mediated Immune Modulation in Microglia
Objective: To evaluate the effect of antioxidant nanozymes on the polarization of microglial cells from a pro-inflammatory M1 to an anti-inflammatory M2 phenotype in vitro.
Methodology:
- Cell Culture: Immortalized murine microglial cell line (e.g., BV-2) is cultured and stimulated with Lipopolysaccharide (LPS) (100 ng/mL) for 24 hours to induce a pro-inflammatory M1 state.
- Nanozyme Treatment: LPS-activated microglia are treated with a range of concentrations (e.g., 10-100 µg/mL) of catalytic nanozymes (e.g., CeO₂ NPs) for 48 hours. A control group receives vehicle only.
- Flow Cytometry Analysis: Cells are harvested and stained with fluorescently labeled antibodies against classic M1 (e.g., CD86) and M2 (e.g., CD206) surface markers. The shift in the cell population from CD86⁺ to CD206⁺ is quantified.
- Cytokine Profiling: Cell culture supernatants are analyzed using ELISA to measure the levels of pro-inflammatory cytokines (TNF-α, IL-6) and anti-inflammatory cytokines (IL-10, TGF-β).
- ROS Measurement: Intracellular ROS levels are measured using a fluorescent probe (e.g., DCFH-DA) via fluorescence microscopy or plate reader.
Diagram 1: Workflow for microglial immunomodulation assay.
Guided Bone Regeneration (GBR): Orchestrating Macrophage-Driven Healing
GBR is a surgical procedure used to reconstruct alveolar bone defects, often in preparation for dental implants. The success of GBR is highly dependent on the host's immune response to the implanted biomaterial membrane and bone graft. Macrophages play a pivotal role in this process, directing the balance between successful osteogenesis (bone formation) and undesirable fibrous encapsulation [39] [35].
The temporal shift in macrophage polarization from M1 to M2 is now recognized as a crucial event for positive outcomes. M1 macrophages dominate the initial inflammatory phase, secreting factors like IL-1β and TNF-α, which are necessary for initiating healing but can be detrimental if sustained. The transition to M2 macrophages promotes tissue remodeling and angiogenesis through the release of anti-inflammatory cytokines (e.g., IL-10) and growth factors [35]. Consequently, next-generation GBR membranes are being engineered with specific surface topographies and biochemical cues to actively recruit macrophages and favor their polarization toward the pro-regenerative M2 phenotype [39]. The surface properties of the biomaterial, including roughness and chemistry, are key design parameters that modulate the initial protein adsorption and subsequent immune cell response [39] [35].
Table 2: Quantitative GBR Healing Assessment using the MAPS Index
| MAPS Domain | Parameter | Score 1 (Compromised) | Score 2 (Questionable) | Score 3 (Normal) | Score 4 (Optimal) |
|---|---|---|---|---|---|
| BioMechanical | Wound Edge Approximation | Open full-thickness margin | Open, not full-thickness | Edge-to-edge, visible line | Merged, no line |
| Aesthetic/Anatomical | Tissue Quantity | Major discrepancy | Moderate discrepancy | Minor discrepancy | No discrepancy |
| Pathophysiologic | Signs of Infection | Spontaneous suppuration | Exudate on light palpation | Slight exudate on compression | No exudate |
| Pathophysiologic | Tissue Perfusion | Entire flap necrosis | Partial necrosis (critical site) | Necrosis (non-critical site) | No necrosis |
| Subject-related | Discomfort | Severe | Moderate | Slight | Absent |
Experimental Protocol: Evaluating Macrophage-Biomaterial InteractionIn Vitro
Objective: To test the immunomodulatory capacity of a novel GBR membrane by analyzing macrophage adhesion, morphology, and phenotypic expression.
Methodology:
- Material Preparation: Sterilize test GBR membranes (e.g., with varied surface microtopography) and place them in 24-well culture plates.
- Macrophage Culture: Human monocyte cell line (THP-1) is differentiated into macrophages using Phorbol 12-myristate 13-acetate (PMA) (e.g., 100 nM for 48 hours).
- Seeding and Culture: Differentiated macrophages are seeded onto the test membranes and cultured for up to 5 days.
- Cell Morphology and Adhesion: Cells are fixed, permeabilized, and stained for F-actin (e.g., Phalloidin) and nuclei (DAPI). Adhesion and cell spreading are visualized using confocal laser scanning microscopy. Analysis of foreign body giant cell (FBGC) formation is performed.
- Gene Expression Analysis: RNA is extracted from macrophages on the membranes. Quantitative PCR (qPCR) is performed to assess the relative expression of M1 markers (e.g., iNOS, TNF-α) and M2 markers (e.g., ARG1, CD206).
- Cytokine Secretion: Multiplex ELISA is used to quantify the secretion of M1 (TNF-α, IL-6) and M2 (IL-10, TGF-β) associated cytokines in the culture supernatant.
Diagram 2: GBR immune response pathway driven by macrophage polarization.
Advanced Wound Healing: Intelligent Systems for Microvascular Repair
Chronic wounds, such as diabetic foot ulcers (DFUs), represent a failure of the normal healing process, often due to underlying microvascular dysfunction, persistent inflammation, and bacterial infection [53] [52]. Acellular approaches, particularly those leveraging exosomes and stimuli-responsive nanozymes, are emerging as powerful strategies to overcome these challenges.
Exosomes, which are nanoscale extracellular vesicles derived from stem or mature cells, act as natural carriers of pro-angiogenic cargo (e.g., VEGF, FGF2, miR-126). They promote microvascular regenerative vascularization and wound repair by activating key signaling pathways such as Wnt/β-catenin, Notch, and PI3K/Akt [53]. Their acellular nature eliminates risks associated with cell-based therapies, such as immune rejection [53].
Conversely, nanozymes are synthetic nanomaterials engineered with enzyme-mimetic activities to dynamically regulate the wound microenvironment [52]. They can be designed to be responsive to specific wound conditions like pH, redox imbalance (H₂O₂, GSH), or ATP levels [52] [51]. For example, a nanozyme with catalase (CAT)-like activity can decompose excess H₂O₂ at the wound site to alleviate oxidative stress and inflammation, while one with peroxidase (POD)-like activity can produce bactericidal ROS in response to bacterial metabolites [52]. This spatiotemporal control allows for precise intervention at different healing stages.
Table 3: Key Pro-Angiogenic Cargos in Exosome Therapies
| Cargo Type | Specific Molecule | Primary Signaling Pathway | Documented Effect in Wound Healing |
|---|---|---|---|
| Growth Factor | Vascular Endothelial Growth Factor (VEGF) | PI3K/Akt | Promotes endothelial cell proliferation and new blood vessel formation [53] |
| Growth Factor | Fibroblast Growth Factor 2 (FGF2) | Notch | Stimulates angiogenesis and fibroblast proliferation [53] |
| microRNA | miR-126 | Notch, PI3K/Akt | Enhances angiogenic signaling and vascular integrity [53] |
Experimental Protocol: Testing a pH-Responsive Nanozyme in a Diabetic Wound Model
Objective: To assess the antibacterial and pro-healing efficacy of a pH-responsive antimicrobial nanozyme in a murine diabetic wound model.
Methodography:
- Animal Model: Induce diabetes in C57BL/6 mice (e.g., with streptozotocin). After confirming hyperglycemia, create full-thickness excisional wounds on the dorsum.
- Bacterial Infection: Infect wounds with a defined inoculum of Staphylococcus aureus (e.g., 1x10⁸ CFU).
- Treatment Groups:
- Group 1: Untreated control.
- Group 2: Treated with a standard topical gel.
- Group 3: Treated with nanozyme-incorporated gel.
- Treatment Regimen: Apply treatments topically every other day until wound closure.
- Monitoring and Analysis:
- Wound Closure: Document wound area reduction through daily digital photography and planimetric analysis.
- Bacterial Load: On day 7, harvest wound tissue, homogenize, and perform serial dilution plating on agar plates to quantify bacterial burden (CFU/g tissue).
- Histological Analysis: On final day, harvest healed wound tissue for H&E staining to assess epithelial gap and granulation tissue thickness, and for immunohistochemistry (CD31 staining) to quantify microvessel density.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Biomaterial-Immune Research
| Category / Item | Function / Application | Example Use-Case |
|---|---|---|
| THP-1 Human Monocyte Cell Line | Differentiate into macrophages for in vitro immunomodulation studies. | Testing macrophage polarization on novel GBR membranes [39]. |
| LPS (Lipopolysaccharide) | Potent stimulator of pro-inflammatory M1 macrophage polarization. | Creating a controlled inflammatory environment in cell cultures [35]. |
| Recombinant Cytokines (e.g., IL-4, IL-13) | Induce alternative M2 macrophage polarization. | Used as a positive control for inducing an anti-inflammatory phenotype [35]. |
| Fluorescent Antibodies (CD86, CD206) | Cell surface markers for identifying M1 and M2 phenotypes via flow cytometry. | Quantifying the macrophage polarization state in response to biomaterials [35]. |
| Exosome Isolation Kits (e.g., from UC) | Isolate and purify exosomes from stem cell-conditioned media. | Sourcing acellular pro-angiogenic nanotherapeutics for wound healing studies [53]. |
| Nanozymes (e.g., CeO₂, V₂O₅) | Catalytic nanomaterials that mimic enzymes like SOD and CAT. | Scavenging ROS in models of chronic wounds or neuroinflammation [52] [51]. |
| Cytokine ELISA Kits | Quantify protein levels of specific cytokines (e.g., TNF-α, IL-10) in supernatants. | Measuring the inflammatory secretome of immune cells exposed to biomaterials. |
| CBCT (Cone-Beam Computed Tomography) | High-resolution 3D imaging for quantifying bone regeneration. | Evaluating horizontal bone gain in GBR procedures [54]. |
Navigating Biocompatibility Challenges: Strategies to Mitigate Rejection and Optimize Performance
The clinical success of implantable medical devices (IMDs) is fundamentally constrained by a predictable yet complex set of biological responses to foreign materials. Despite advances in biomaterial science, the host immune system often recognizes these implants as foreign, initiating a cascade of events that can lead to device failure [55]. The core of this problem lies in the fundamental principles of biomaterial-host interactions, which are characterized by a series of immune-mediated processes [56]. Understanding these processes is critical for developing next-generation implants with improved longevity and functionality.
This technical guide examines the principal failure modes of chronic inflammation, fibrous encapsulation, and implant loosening within the broader context of biomaterial host interactions and immune response research. These interrelated phenomena represent the most significant biological barriers to long-term implant success, contributing substantially to the estimated $10 billion annual cost to healthcare systems from implant failure [55]. By synthesizing current understanding of the cellular and molecular mechanisms driving these failure modes, this document provides researchers and drug development professionals with a foundational framework for developing innovative solutions.
The Fundamental Biological Processes
The Foreign Body Response (FBR) Cascade
Implantation of any medical device triggers a sterile immune response known as the foreign body response (FBR), a precisely orchestrated sequence of events that begins within minutes of implantation and can continue for years [55] [57]. The FBR consists of multiple overlapping phases: protein adsorption, acute inflammation, chronic inflammation, foreign body giant cell formation, and fibrous encapsulation [55] [58].
Table 1: Phases of the Foreign Body Response (FBR)
| Phase | Timeframe | Key Cells Involved | Major Molecular Mediators |
|---|---|---|---|
| Protein Adsorption | Immediate (seconds to minutes) | Plasma proteins | Fibrinogen, albumin, complement proteins, immunoglobulins [55] [58] |
| Acute Inflammation | 2-7 days post-implantation | Neutrophils, monocytes | Reactive oxygen species, proteinases, pro-inflammatory cytokines [55] [58] |
| Chronic Inflammation | ~1-3 weeks | Macrophages, lymphocytes | IL-1β, IL-6, TNF-α, MCP-1 [55] [58] |
| Foreign Body Giant Cell Formation | Weeks to months | Macrophages, FBGCs | IL-4, IL-13, adhesion molecules [55] |
| Fibrous Encapsulation | Weeks to permanent | Fibroblasts, myofibroblasts | Collagen, α-SMA, TGF-β [55] [57] |
The initial event following implantation is the rapid adsorption of blood plasma proteins onto the biomaterial surface, forming a provisional matrix that determines subsequent cellular responses [55] [58]. The composition of this protein layer is influenced by material properties including surface chemistry, topography, and wettability [55]. Notably, adsorbed fibrinogen appears particularly pro-inflammatory and promotes downstream immune activation [59] [55].
The acute inflammatory phase is characterized by massive neutrophil infiltration to the implantation site, typically lasting approximately one week [55] [58]. Neutrophils attempt to phagocytose the foreign material and secrete reactive oxygen species (ROS), proteinases, and cytokines that cause local tissue damage and further recruit immune cells [55] [58]. When the acute response fails to resolve the foreign body, the response progresses to chronic inflammation, dominated by monocyte-derived macrophages [55].
Key Signaling Pathways in Chronic Inflammation
The transition from acute to chronic inflammation represents a critical juncture in the FBR. Macrophages are the central arbiters of this phase, attempting to eliminate the implant through phagocytosis while secreting pro-inflammatory cytokines and chemokines [55]. The activation state of macrophages evolves during this process, with initial dominance of the pro-inflammatory M1 phenotype gradually shifting toward a mix of M1 and M2 (anti-inflammatory, pro-healing) phenotypes in a well-regulated response [55]. However, in the presence of non-phagocytosable biomaterials, this resolution is often delayed, maintaining a chronic inflammatory state [55].
The transcription factor NF-κB serves as a master regulator of the chronic inflammatory response to biomaterials [58] [60]. Numerous stimuli, including wear particles and cytokines, activate the IKK complex, which phosphorylates IκB proteins, leading to their degradation and subsequent nuclear translocation of NF-κB dimers (primarily p50/p65) [58] [60]. This triggers the expression of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6), chemokines (MCP-1), and enzymes (COX-2) that perpetuate the inflammatory response and contribute to tissue destruction [58] [60].
Figure 1: NF-κB Signaling Pathway in Chronic Inflammation and Osteolysis. This core pathway is activated by wear particles and cytokines, leading to pro-inflammatory gene expression that drives chronic inflammation and bone destruction [58] [60].
In the specific context of orthopedic implants, wear particles generated from bearing surfaces are particularly potent activators of this inflammatory cascade [61] [58] [60]. The physical, material, topographic, and chemical properties of these particles determine their biological activity [58] [60]. For example, polyethylene wear rates exceeding 0.15 mm/year significantly enhance the risk of aseptic loosening, while rates below 0.05 mm/year are associated with better implant stability [58].
Specific Failure Modes
Fibrous Encapsulation
Fibrous encapsulation represents the terminal phase of the FBR and a major failure mode for many IMDs [55] [57]. This process begins with the activation of fibroblasts via chemokines and cytokines secreted by pro-inflammatory macrophages [55]. Weak focal adhesion of fibroblasts on material surfaces triggers their differentiation into myofibroblasts, characterized by α-smooth muscle actin (α-SMA) expression in intracytoplasmic stress fibers and secretion of collagen [55]. Ultimately, these cells create a dense, avascular collagen fiber network that isolates the device from surrounding tissues [55].
The clinical consequences of fibrous encapsulation are device-specific but universally detrimental. For biosensors, lack of vascularization reduces blood supply, limiting oxygen and analyte diffusion [55]. In drug delivery systems, the fibrous capsule obstructs therapeutic diffusion, rendering the treatment ineffective [55]. For breast implants, excessive fibrosis manifests as capsular contracture, with failure rates approaching 30% [55].
Table 2: Device-Specific Consequences of Fibrous Encapsulation
| Implant Category | FBR-Related Issues | Clinical Consequences |
|---|---|---|
| Cardiovascular Implants | Granulomatous reaction, fibrosis-related replacement complications, thrombosis [55] | Device malfunction, need for revision surgery |
| Neural Implants | Microelectrode array recording failures, giant cell formation [55] | Loss of signal fidelity, device failure |
| Ocular Implants | Anterior and posterior capsule opacification, fibrous proliferation [55] | Visual impairment, need for additional interventions |
| Breast Implants | Capsular contracture, granuloma formation [55] | Pain, deformity, need for explantation |
| Drug Delivery Systems | Fibrosis and isolation of the implant [55] | Reduced drug efficacy, treatment failure |
| Biosensors | Fibrous encapsulation, lack of vascularization [55] | Impaired analyte sensing, inaccurate readings |
Implant Loosening
Implant loosening represents a particularly devastating failure mode in load-bearing applications, primarily affecting orthopedic implants [61] [58] [62]. This process is classically categorized as either aseptic or septic loosening, with aseptic loosening accounting for the majority of failures [61]. Despite the nomenclature "aseptic," recent evidence suggests that subclinical biofilms may be overlooked in many cases diagnosed as aseptic loosening [61].
The pathogenesis of aseptic loosening centers on the generation of wear particles from articulating surfaces [61] [58] [62]. These particles activate macrophages through pattern recognition receptors including Toll-like receptors (TLRs), leading to NF-κB activation and subsequent expression of pro-inflammatory cytokines [58] [60]. Crucially, these inflammatory mediators stimulate osteoclast differentiation and activation via the RANK/RANKL pathway while simultaneously inhibiting osteoblast function [58]. The resulting imbalance in bone remodeling favors net bone resorption at the implant-bone interface, leading to progressive osteolysis and eventual mechanical loosening of the implant [61] [58].
The physical characteristics of wear particles significantly influence their biological activity. Metallic wear particles from cobalt-chrome metal-on-metal hip replacements are much smaller than polymeric particles but present in much greater numbers [58]. While modern highly cross-linked polyethylene has reduced wear rates, particle generation remains inevitable over the long functional life expectancies now demanded of orthopedic implants [58] [62].
Experimental Methodologies for Investigation
In Vivo Implantation Models
Animal models, particularly mouse models, have been essential for advancing our understanding of FBR mechanisms and testing potential therapeutic interventions [55] [62]. The subcutaneous implantation model in mice or rats represents the standard for initial biocompatibility assessment due to its technical simplicity and minimal invasiveness [57]. However, researchers must carefully consider species-specific immune differences and the anatomical relevance of the implantation site when interpreting results.
Detailed Protocol: Subcutaneous Implantation in Mice
- Material Preparation: Sterilize test materials (typically 5-15 mm diameter discs or 10 mg rolled cylinders) by UV irradiation for 30 minutes per side [57].
- Animal Preparation: Anesthetize mice (typically C57BL/6 or BALB/c strains, 8-12 weeks old) using approved anesthetic protocols.
- Surgical Procedure: Make a 1-1.5 cm dorsal midline incision. Create subcutaneous pockets by blunt dissection on each side of the incision. Insert one material specimen per pocket, ensuring no contact with the incision line.
- Closure: Close the incision with surgical staples or sutures.
- Study Duration & Analysis: Euthanize animals at predetermined timepoints (e.g., 3, 7, 14, 21, 28 days). Explant specimens with surrounding tissue for:
- Histological analysis (H&E staining for general morphology, Masson's Trichrome for collagen deposition)
- Immunohistochemistry (macrophage markers: F4/80, CD68; myofibroblast marker: α-SMA)
- RNA extraction and gene expression analysis of inflammatory markers (TNF-α, IL-1β, IL-6, MCP-1)
- Quantification of fibrous capsule thickness from histological sections [55] [57].
While subcutaneous implantation provides valuable screening data, orthopedic implant loosening requires specialized models that incorporate mechanical loading and bone integration assessment. These typically involve implantation into femurs or tibiae of larger animals (rabbits, dogs, sheep) or specialized mouse models [62].
In Vitro Macrophage-Biomaterial Interaction Studies
In vitro systems provide controlled environments for mechanistic studies of specific cell-material interactions, with macrophages being the primary focus in FBR research.
Detailed Protocol: Macrophage Polarization in Response to Wear Particles
- Cell Culture: Use primary human monocyte-derived macrophages or murine macrophage cell lines (RAW 264.7). Differentiate primary monocytes for 7 days with M-CSF (50 ng/mL).
- Particle Preparation: Prepare wear particles (e.g., polyethylene, titanium, PMMA) in sizes ranging from 0.1-10 μm. Sterilize by gamma irradiation or ethanol washing. Opsonize in culture medium with 10% FBS for 30 minutes at 37°C.
- Stimulation: Seed macrophages at 5×10^5 cells/mL in appropriate plates. Add particles at clinically relevant concentrations (typically 10-100 particles per cell).
- Analysis:
- Gene Expression: After 6-24 hours, extract RNA and analyze pro-inflammatory (M1: iNOS, TNF-α, IL-1β) and anti-inflammatory (M2: Arg-1, IL-10) markers by qRT-PCR.
- Protein Secretion: After 24-48 hours, collect supernatants for cytokine analysis (TNF-α, IL-1β, IL-6, MCP-1) by ELISA.
- Cell Morphology: Assess actin cytoskeleton organization and cell spreading by phalloidin staining.
- NF-κB Activation: Monitor nuclear translocation of p65 subunit by immunofluorescence or measure IκB degradation by Western blot [58] [60].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating Implant Failure Modes
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Biomaterial Polymers | Poly(lactic-co-glycolic acid) (PLGA), Polycaprolactone (PCL), Polytetrafluoroethylene (PTFE), Poly(2-hydroxyethyl methacrylate) (pHEMA) [55] [57] | Fabrication of test substrates and drug delivery systems | Model implant materials with tunable properties for studying material-immune cell interactions |
| Wear Particles | Ultra-high molecular weight polyethylene (UHMWPE), Titanium, Cobalt-chrome, Polymethylmethacrylate (PMMA) [61] [58] [60] | In vitro and in vivo stimulation of inflammatory responses | Activate macrophages and model particle-induced osteolysis and inflammation |
| Macrophage Polarization Markers | CD68 (pan-macrophage), iNOS (M1), CD206 (M2), F4/80 (mouse macrophages) [55] [58] | Immunohistochemistry, flow cytometry | Identify and quantify macrophage phenotypes in peri-implant tissues |
| Cytokine Analysis | ELISA kits for TNF-α, IL-1β, IL-6, MCP-1 [55] [58] | Quantification of inflammatory mediators in tissue homogenates or cell culture supernatants | Measure the intensity of inflammatory responses |
| Fibrosis Markers | Anti-α-SMA antibody, Masson's Trichrome stain, Sirius Red stain [55] [57] | Histological assessment of fibrous encapsulation | Identify myofibroblasts and quantify collagen deposition |
| NF-κB Pathway Components | Anti-p65 antibody, Phospho-IκBα antibody, IKK inhibitors (e.g., BMS-345541) [58] [60] | Mechanistic studies of inflammatory signaling | Investigate core signaling pathways in chronic inflammation |
Emerging Research and Strategic Interventions
Current research focuses on disrupting the FBR cascade at multiple points, with particular interest in immunomodulatory approaches that steer the host response toward tolerance rather than confrontation. Biomaterial surface properties—including topography, chemistry, and mechanical stiffness—are recognized as critical determinants of protein adsorption and subsequent immune activation [55]. Microscale and nanoscale surface patterning can significantly reduce macrophage adhesion and FBGC formation compared to smooth surfaces [55].
Novel biomaterial strategies include the incorporation of immunomodulatory agents that alter the local immune microenvironment. For instance, incorporating metabolic inhibitors into polylactide polymers has been shown to shift immune cells toward pro-regenerative phenotypes by altering glycolytic pathways [63]. Similarly, creating localized immunosuppressive environments around implants using nanofibers functionalized with immune checkpoint molecules shows promise for protecting implants from immune attack [63].
Targeting specific cellular drivers of fibrosis represents another promising approach. Recent research has identified skeletal stem cells expressing the leptin receptor as crucial for generating and maintaining fibrotic tissue around titanium implants [63]. Selective targeting of these cells significantly reduces peri-implant fibrosis in animal models, suggesting potential therapeutic applications [63].
The timing of therapeutic intervention is also gaining recognition as a critical factor. While most research has focused on preventing the initiation of FBR, emerging strategies address the maintenance phase of established fibrosis, potentially offering treatments for patients with already-failing implants [58] [60].
Chronic inflammation, fibrous encapsulation, and implant loosening represent interconnected failure modes rooted in the fundamental immune recognition of biomaterials as foreign. The foreign body response follows a predictable sequence of events, from initial protein adsorption to eventual fibrous encapsulation, with wear particle-induced inflammation driving periprosthetic osteolysis in orthopedic applications. The transcription factor NF-κB serves as a master regulator of these processes, integrating multiple inflammatory signals into a coordinated gene expression program that perpetuates chronic inflammation and bone destruction.
Substantial challenges remain in translating mechanistic understanding into clinical applications. These include the complexity of human immune responses compared to animal models, potential off-target effects of immunomodulatory therapies, and the long-term safety of innovative biomaterials. However, current research directions focusing on immunomodulatory biomaterials, selective targeting of fibrotic cells, and manipulation of the local implant microenvironment offer promising avenues for overcoming these limitations. By deepening our understanding of the intricate interplay between biomaterials and the immune system at molecular, cellular, and tissue levels, researchers can design advanced implants that better integrate with host tissues and function effectively throughout a patient's lifetime.
Macrophage polarization represents a critical frontier in biomaterial host interactions and immune response research, governing outcomes in tissue regeneration, cancer, and chronic disease. The M1 to M2 phenotypic transition is not merely a cellular identity switch but a fundamental reprogramming of immune signaling, metabolic pathways, and secretory profiles that determines whether tissues progress toward inflammation or repair. This whitepaper synthesizes current scientific understanding of macrophage polarization mechanisms, providing researchers and drug development professionals with quantitative data, experimental protocols, and strategic frameworks for manipulating this dynamic process. Within the context of biomaterial design, we examine how physical cues, biochemical signaling, and advanced therapeutic interventions can be engineered to direct macrophage phenotypes toward pro-regenerative states, thereby unlocking new possibilities for immune-informed regenerative medicine and overcoming the limitations of conventional approaches that fail to resolve chronic inflammation.
Macrophages, central players in innate immunity, exhibit remarkable plasticity that allows them to adopt diverse functional phenotypes in response to microenvironmental signals. The classic dichotomy describes pro-inflammatory M1 macrophages and pro-regenerative M2 macrophages, though this spectrum is now understood to encompass multiple intermediate and specialized subsets [64]. The M1 phenotype, activated by stimuli such as interferon-gamma (IFN-γ) and lipopolysaccharide (LPS), is characterized by high production of inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6, IL-12), reactive oxygen and nitrogen species, and potent antimicrobial activity [4] [65]. In contrast, the M2 phenotype, induced by interleukins (IL-4, IL-10, IL-13), produces anti-inflammatory cytokines (IL-10, TGF-β), growth factors, and promotes tissue repair, angiogenesis, and immunoregulation [5] [4]. Successful tissue regeneration following injury requires a carefully timed transition from an initial M1-dominated inflammatory phase to a subsequent M2-dominated reparative phase [66] [5]. Disruption of this transition perpetuates a chronic inflammatory state that impairs healing and drives pathology in conditions such as chronic wounds, fibrotic disorders, and failed biomaterial integration [66] [64]. Therefore, strategic control of macrophage polarization represents a powerful therapeutic approach in regenerative medicine and biomaterial science.
Molecular Mechanisms of Phenotypic Switching
Core Signaling Pathways
The molecular control of macrophage polarization involves a complex interplay of multiple signaling pathways, transcription factors, and epigenetic regulators. The table below summarizes the principal pathways and their roles in M1/M2 polarization.
Table 1: Key Signaling Pathways in Macrophage Polarization
| Pathway | M1-Polarizing Role | M2-Polarizing Role | Key Molecular Players |
|---|---|---|---|
| JAK-STAT | STAT1 activation by IFN-γ/LPS drives M1 genes [4] [65] | STAT6 activation by IL-4/IL-13 drives M2 genes [67] [4] | JAK1/2, STAT1, STAT6, IRF4, SOCS proteins |
| NF-κB | Canonical pathway activation by TLR ligands (e.g., LPS) promotes pro-inflammatory cytokine production [65] | Non-canonical pathway and certain regulators can support M2; generally inhibited in M2 [65] | p65/p50 subunits, IKK complex, IκB |
| PI3K/AKT | Generally suppressed; promotes M2 polarization [67] [65] | Activation promotes M2 polarization; regulates metabolism and gene expression [67] [65] | PI3K, AKT, mTOR, PTEN |
| MAPK | p38 and JNK activation promotes M1 inflammatory responses [65] | ERK activation often associated with M2 polarization [65] | p38, JNK, ERK, MAPK kinases |
| Inflammasome | NLRP3 activation drives caspase-1 cleavage and IL-1β/IL-18 maturation in M1 [65] | Generally suppressed; IL-1β is a pro-inflammatory cytokine | NLRP3, ASC, Caspase-1 |
| cGAS-STING | Cytosolic DNA sensing drives type I interferon and pro-inflammatory responses in M1 [65] | Role in M2 is less defined; can contribute to resolution in certain contexts [65] | cGAS, STING, TBK1, IRF3 |
The following diagram illustrates the core signaling pathways involved in macrophage polarization, integrating the key stimuli and intracellular signaling events that drive M1 and M2 phenotypes.
Metabolic Reprogramming
Macrophage polarization is intrinsically linked to cellular metabolism, a process known as metabolic reprogramming. M1 macrophages primarily rely on glycolysis for rapid energy production, even under aerobic conditions, a phenomenon known as the Warburg effect [67] [68]. This glycolytic shift is stabilized by the transcription factor HIF-1α (hypoxia-inducible factor 1-alpha) and supports the production of intermediates for inflammatory gene expression and nitric oxide synthesis [68]. In contrast, M2 macrophages predominantly utilize oxidative phosphorylation (OXPHOS) and fatty acid oxidation (FAO) to generate ATP, supporting their long-term tissue repair functions [67] [65]. Key metabolic checkpoints include:
- Arg1 (Arginase-1): Expressed in M2 macrophages, diverts arginine away from iNOS (Inducible Nitric Oxide Synthase)-mediated NO production in M1 macrophages and toward polyamine and proline synthesis, which support cell proliferation and collagen deposition [67] [4].
- ATP Citrate Lyase (ACLY): Links glycolysis to fatty acid synthesis in M1 macrophages, supporting membrane biogenesis and inflammatory signaling [65].
- Succinate: Accumulates in M1 macrophages, stabilizing HIF-1α and promoting IL-1β production [65].
Targeting these metabolic pathways presents a promising strategy for modulating macrophage phenotype. For instance, the drug Metformin inhibits OXPHOS, thereby favoring a glycolytic M1 state, whereas Etomoxir inhibits FAO, disrupting the metabolic program of M2 macrophages [68].
Research has identified multiple strategic axes to promote the M1-to-M2 transition. The table below synthesizes quantitative and mechanistic data on the most promising approaches.
Table 2: Comparative Analysis of M2-Polarizing Strategies
| Strategy Category | Specific Agent/Intervention | Reported Efficacy/Outcome | Key Mechanisms of Action |
|---|---|---|---|
| Cytokine & Signaling Therapy | IL-4 / IL-13 | Induces M2a phenotype; enhances tissue repair in bone and wound models [5] [64] | Activation of STAT6 and IRF4 transcription factors [4] [65] |
| IL-10 | Induces M2c phenotype; promotes resolution of inflammation [64] | Activation of STAT3 and suppression of pro-inflammatory signaling [4] | |
| Small Molecule Inhibitors | JAK/STAT Inhibitors | Shifts balance from M1; potential in autoimmune disease [65] | Blocks IFN-γ/STAT1 signaling axis [65] |
| PI3Kγ Inhibitors | Reprogrammed TAMs to M1, inhibited tumor growth in vivo [65] | Inhibits AKT activation, disrupting M2-associated signaling [65] | |
| Biomaterial-Driven Cues | Stiffness (1–20 kPa) | Optimal soft substrates (∼10 kPa) promote M2 markers (CD206) [5] | Modulation of actin cytoskeleton and mechanosensitive transcription factors (e.g., YAP/TAZ) [5] |
| Surface Topography | Micropatterns (2–5 μm grooves) reduce CD86, increase CD206 [5] | Alters cell morphology and integrin clustering [5] | |
| Nanoparticle Delivery | TLR Agonist NPs | Ferumoxytol + TLR3 agonist promoted M1 in tumors [68] | Targeted delivery of polarization signals to specific tissues/cells [68] |
| siRNA-Loaded NPs | Knockdown of IRF5/STAT1 promoted M2 shift in vitro [68] | Silencing key M1-polarizing transcription factors [68] |
Experimental Protocols for Polarization Studies
Robust in vitro and in vivo models are essential for validating macrophage polarization strategies. The following protocols provide a standardized framework for researchers.
In Vitro Polarization and Assessment of Human Macrophages
This protocol details the generation of monocyte-derived macrophages and their subsequent polarization, a cornerstone assay in the field [4] [64].
Key Research Reagent Solutions: Table 3: Essential Reagents for Macrophage Polarization Experiments
| Reagent / Material | Function / Purpose | Example |
|---|---|---|
| Recombinant Human M-CSF | Differentiates monocytes into M0 macrophages | 20–50 ng/mL for 5–7 days [5] |
| Polarizing Cytokines | Directs macrophages toward M1 or M2 phenotypes | IFN-γ (20–50 ng/mL) + LPS (10–100 ng/mL) for M1; IL-4 (20–50 ng/mL) for M2 [5] [64] |
| Flow Cytometry Antibodies | Surface marker quantification for phenotyping | Anti-human CD86 (M1), CD80 (M1), CD206 (M2), CD163 (M2) [5] [64] |
| qPCR Primers | Gene expression analysis of polarization markers | TNF-α, IL-1β, IL-6, iNOS (M1); Arg1, FIZZ1, Ym1, IL-10 (M2) [5] [4] |
| ELISA Kits | Quantification of secreted cytokines in supernatant | TNF-α, IL-12 (M1); IL-10, TGF-β (M2) [64] |
Step-by-Step Workflow:
- Monocyte Isolation: Isolate human peripheral blood mononuclear cells (PBMCs) from buffy coats or leukapheresis samples using density gradient centrifugation (e.g., Ficoll-Paque). Isolate CD14+ monocytes from PBMCs using positive selection magnetic-activated cell sorting (MACS) or adherence to plastic.
- M0 Macrophage Differentiation: Culture the purified CD14+ monocytes in RPMI-1640 or DMEM complete medium supplemented with 10% FBS, 1% Penicillin/Streptomycin, and 50 ng/mL recombinant human M-CSF for 6 days. Replenish medium and M-CSF on day 3 or 4.
- Phenotypic Polarization: On day 6, detach the differentiated M0 macrophages and seed them for experiments.
- For M1 polarization: Treat cells with 50 ng/mL IFN-γ for 24 hours, followed by a refresh of medium containing both 50 ng/mL IFN-γ and 10 ng/mL LPS for an additional 24 hours.
- For M2 polarization: Treat cells with 20–50 ng/mL recombinant human IL-4 for 48 hours.
- Phenotype Validation (24–48 hours post-polarization):
- Flow Cytometry: Harvest and stain cells with fluorochrome-conjugated antibodies against M1 surface markers (CD80, CD86) and M2 markers (CD206, CD163). Analyze using flow cytometry.
- Gene Expression (qRT-PCR): Extract total RNA and synthesize cDNA. Perform qPCR for M1-associated genes (TNF-α, IL-1β, iNOS) and M2-associated genes (Arg1, CD206, IL-10). Normalize data to a housekeeping gene (e.g., GAPDH, β-actin) and analyze using the 2^–ΔΔCt method.
- Cytokine Secretion (ELISA): Collect cell culture supernatants. Measure the concentration of secreted M1 (TNF-α, IL-12) and M2 (IL-10, TGF-β) cytokines using commercial ELISA kits according to manufacturer instructions.
The experimental workflow for in vitro polarization and analysis is visualized below.
In Vivo Assessment in a Mouse Bone Defect Model
To evaluate polarization strategies in a complex physiological environment, a rodent bone defect model integrated with biomaterial scaffolds is highly relevant [66] [5].
Procedure:
- Animal Model Establishment: Anesthetize 10–12 week-old C57BL/6 mice. Create a critical-sized calvarial defect (e.g., 3–4 mm diameter) using a trephine drill under sterile conditions.
- Implantation: Implant the test biomaterial scaffold (e.g., an immunomodulatory hydrogel) into the defect. Include control groups (empty defect, scaffold-only).
- Tissue Harvest and Analysis: Euthanize animals at predetermined time points (e.g., 3, 7, 14 days). Excise the defect site with surrounding tissue.
- Immunofluorescence Staining: Fix and section the harvested tissue. Perform co-staining for M1 macrophages (e.g., iNOS+ or CD86+) and M2 macrophages (e.g., CD206+ or Arg1+). Use DAPI for nuclei. Quantify the M1/M2 ratio using fluorescence microscopy and image analysis software.
- RNA Extraction and Transcriptomic Analysis: Homogenize a portion of the harvested tissue. Extract total RNA for qRT-PCR analysis of polarization markers or for bulk RNA-seq to obtain a global transcriptomic profile of the immune response.
Biomaterial Strategies for Immunomodulation
Biomaterials are not passive implants; they are active participants in directing the host immune response. The physical and chemical properties of biomaterials can be engineered to favor M2 polarization and improve regenerative outcomes [5] [69].
Table 4: Biomaterial Properties as Levers for Macrophage Polarization
| Biomaterial Property | Pro-M2 Design Principle | Impact on Macrophage Phenotype & Healing |
|---|---|---|
| Stiffness | Mimic stiffness of target native tissue (e.g., ~10 kPa for soft tissues) [5] | Softer substrates reduce M1 markers (iNOS) and promote M2 markers (Arg1) via mechanotransduction [5] |
| Surface Topography | Integrate micro- and nano-scale grooves or pits [5] | Alters macrophage adhesion and morphology, leading to reduced pro-inflammatory cytokine secretion [5] |
| Chemical Functionality | Present anti-inflammatory cytokines (IL-4, IL-10) or specific peptides [66] | Sustained, localized delivery of M2-polarizing signals directly at the implant-tissue interface [66] [69] |
| Biodegradation Rate | Tune to match tissue ingrowth rate; non-cytotoxic degradation products [69] | Slow, controlled degradation minimizes persistent foreign body response and chronic M1 activation [69] |
The following diagram conceptualizes the dynamic interplay between biomaterial properties and the temporal progression of the immune response leading to tissue regeneration.
The strategic reprogramming of macrophages from a pro-inflammatory M1 to a pro-regenerative M2 phenotype represents a paradigm shift in managing the host response to biomaterials and treating inflammatory diseases. The toolkit for achieving this shift is expanding, encompassing sophisticated biomaterial design, targeted pharmacological agents, and metabolic interventions. However, significant challenges and opportunities remain. The field must move beyond the simplistic M1/M2 dichotomy to embrace the continuous spectrum of macrophage activation states, aided by single-cell transcriptomics and spatial profiling technologies [67] [65]. Future biomaterials will likely incorporate spatiotemporally controlled release of multiple immunomodulatory factors to guide, rather than force, the natural healing cascade. The clinical translation of these strategies will depend on robust, scalable manufacturing and a deep understanding of patient-specific immune variability. As research continues to unravel the intricate dialogue between macrophages and their microenvironment, the goal of achieving predictable, scar-free regeneration through precise immunomodulation moves increasingly within reach.
A critical challenge in pharmaceutical and biomaterial research is the frequent failure of standard in vitro tests to accurately predict in vivo performance and outcomes. This disconnect presents a major hurdle in product development, leading to costly late-stage failures and delays in bringing new therapies to market. For biomaterials, the host immune response is a particularly complex variable that is difficult to capture in a laboratory setting. Biomaterials implanted in the body are often recognized as foreign, triggering an immune response that typically involves the activation of innate immunity and the initiation of an inflammatory response, which can persist as chronic inflammation and cause implant failure [50]. This article provides an in-depth technical guide to advanced methodologies and strategic approaches designed to bridge this critical gap, with a specific focus on the interplay between biomaterials and the immune system.
Understanding the Roots of Poor Correlation
Physiological and Formulation Complexities
The divergence between in vitro and in vivo results stems from several inherent limitations. Traditional in vitro systems often operate in isolation, unable to replicate the dynamic, multi-factorial environment of a living organism.
- Physiological Variability: In vitro models struggle to mimic human physiological variability, including differences in gastrointestinal fluids, motility, and metabolic enzymes, which complicates the extrapolation of preclinical data to human outcomes [70].
- Dynamic Immune Responses: For biomaterials, the immune response is a key determinant of success. The process involves an initial acute inflammatory response that can transition to a chronic state, leading to fibrous tissue encapsulation and implant failure. This complex sequence, orchestrated by immune cells like macrophages, neutrophils, and T cells, is not captured in simple in vitro systems [50] [7].
- Complex Formulation Dynamics: Lipid-based formulations (LBFs), used to enhance the bioavailability of poorly water-soluble drugs, undergo complex processes like digestion, micelle formation, and dynamic solubilization in the gastrointestinal tract. Standard dissolution tests fail to account for these dynamic processes, leading to poor predictive power [70].
Case Studies Highlighting Correlation Failures
Several studies underscore these challenges. Research on the drug fenofibrate demonstrated that in vitro dispersion data failed to distinguish between the performance of different LBFs in fasted versus fed states in animal models, and no correlation could be established [70]. Similarly, a review of the pH-stat lipolysis model found that it correlated well with in vivo data for only half of the drugs studied [70]. For the drug cinnarizine, researchers observed precipitation during in vitro lipolysis that was not reflected in the in vivo performance, allowing only for a qualitative (Level D) correlation [70].
Advanced Methodologies for Enhanced Prediction
To overcome these limitations, the field has moved towards more sophisticated, biorelevant tools and integrated models.
AdvancedIn VitroTools
Moving beyond simple dissolution apparatuses (e.g., USP) is critical for complex formulations like LBFs and for predicting host responses to biomaterials.
Table 1: Advanced In Vitro Tools for Improved Biorelevance
| Tool/Assay | Key Application | Functional Principle | Advantages over Standard Tests |
|---|---|---|---|
| Lipolysis Assays | Lipid-based Formulations (LBFs) | Mimics the enzymatic digestion of lipids in the GI tract by incorporating digestive enzymes and bile salts [70]. | Captures dynamic solubilization and precipitation processes critical to LBF performance. |
| Combined Dissolution-Permeation Systems | Absorption Prediction | Integrates a dissolution compartment with a permeability barrier (e.g., Caco-2 cell monolayers) [70]. | Simultaneously assesses drug release and absorption, accounting for permeation limitations. |
| Immunomodulatory Biomaterial Testing | Biomaterial-Host Integration | Utilizes cell culture models (e.g., macrophages) to assess inflammatory response to material surfaces [7] [50]. | Predicts the in vivo foreign body response and potential for fibrosis or integration. |
Incorporating Immunomodulation in Biomaterial Design
A key strategy for improving the in vivo success of biomaterials is the engineering of immunomodulatory properties directly into the material. The immune system, particularly macrophages, plays a pivotal role in tissue healing and regeneration. Macrophages can transition between pro-inflammatory (M1) and anti-inflammatory (M2) phenotypes, and an imbalance can lead to chronic inflammation or fibrosis [7]. Advanced biomaterials are now designed to actively modulate this response through several strategies:
- Surface Physical Modifications: Altering surface topography, roughness, and patterning at the micro- and nano-scale can significantly influence immune cell adhesion and activation. For example, reducing the surface roughness of silicone mammary implants to 4 μm was shown to improve immune response and reduce fibrosis [21] [50].
- Bioactive Functionalization: Biomaterials can be functionalized with anti-inflammatory cytokines (e.g., IL-4, IL-10) or other agents to promote a shift from M1 to M2 macrophage phenotypes, fostering a regenerative environment instead of a hostile one [7] [50].
- Mechanical Property Tuning: The stiffness and elasticity of a biomaterial can direct immune cell behavior. Softer materials that match the mechanical properties of the target tissue (e.g., brain) have been shown to reduce inflammatory reactions [50].
IntegratedIn SilicoModeling Platforms
Computational models provide a powerful means to integrate complex data and improve prediction.
- Physiologically Based Pharmacokinetic (PBPK) Modeling: PBPK models simulate drug absorption, distribution, metabolism, and excretion by incorporating physiological parameters (e.g., organ perfusion rates, tissue composition) [71]. When combined with in vitro data, they can predict human pharmacokinetics, reducing reliance on animal studies.
- Artificial Intelligence (AI) and Machine Learning (ML): AI/ML platforms can predict key drug properties and pharmacokinetic parameters directly from molecular structure, as demonstrated by an integrated AI-PBPK platform that successfully forecasted human pharmacokinetic curves and tissue distribution [72]. In biomaterials, ML can analyze complex datasets to predict the immunomodulatory properties of polymers, accelerating the design of safer implants [7].
A Strategic Framework for Robust In Vitro-In Vivo Correlation (IVIVC)
Establishing a predictive IVIVC is a formalized process endorsed by regulatory bodies. The following workflow outlines a comprehensive, integrated approach.
Experimental Protocols for Key Assays
Protocol for In Vitro Lipolysis Assay
This protocol is critical for evaluating lipid-based formulations (LBFs) [70].
- Simulated Intestinal Media Preparation: Prepare a biorelevant medium containing Tris buffer (pH 7.5), sodium taurodeoxycholate (bile salt), and phosphatidylcholine (lecithin) to simulate fed or fasted state conditions.
- Temperature Control: Maintain the digestion vessel at 37°C with constant stirring.
- Initiation of Digestion: Add pancreatic extract (containing lipase, colipase, and other enzymes) to the medium to start the lipid digestion process.
- pH-Stat Titration: Use a pH-stat apparatus to automatically titrate sodium hydroxide (NaOH) into the vessel, maintaining a constant pH of 7.5. The volume of NaOH consumed is directly proportional to the extent of fatty acid liberation from digestion.
- Sampling: At predetermined time points, collect samples from the vessel. Immediately treat samples with a lipase inhibitor (e.g., 4-bromophenyl boronic acid) to halt further digestion.
- Sample Analysis: Centrifuge samples to separate different phases (aqueous, oily, pellet). Analyze the drug concentration in each phase using HPLC-UV to track drug distribution and potential precipitation throughout the digestion process.
Protocol for Assessing Macrophage Polarization on Biomaterials
This protocol evaluates the immunomodulatory potential of a biomaterial [7] [50].
- Cell Culture: Culture a monocyte/macrophage cell line (e.g., RAW 264.7) or primary human monocyte-derived macrophages.
- Material Sterilization and Seeding: Sterilize the biomaterial sample (e.g., a disc, scaffold) via ethanol, UV, or gamma irradiation. Seed macrophages onto the material's surface at a defined density.
- Stimulation and Co-culture: Stimulate cells with interferon-gamma (IFN-γ) and lipopolysaccharide (LPS) to induce a pro-inflammatory (M1) state. Co-culture the stimulated cells with the test biomaterial for 24-72 hours.
- Analysis of Phenotype:
- Gene Expression (qRT-PCR): Analyze RNA for M1 markers (e.g., iNOS, TNF-α, IL-6) and M2 markers (e.g., ARG1, CD206, IL-10).
- Surface Markers (Flow Cytometry): Stain cells for M1 (e.g., CD86) and M2 (e.g., CD206) surface proteins.
- Cytokine Secretion (ELISA): Measure the secretion of M1-associated (TNF-α, IL-6) and M2-associated (IL-10, TGF-β) cytokines in the culture supernatant.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Research Reagents for Advanced Correlation Studies
| Reagent / Material | Function / Application | Technical Notes |
|---|---|---|
| Pancreatic Lipase Extract | Key enzyme for in vitro lipolysis assays simulating GI digestion [70]. | Use from porcine or recombinant sources; activity must be standardized. |
| Sodium Taurodeoxycholate | A primary bile salt used to create biorelevant simulated intestinal fluids [70]. | Critical for forming micelles and solubilizing lipolytic products. |
| Caco-2 Cell Line | Human colon adenocarcinoma cells; form polarized monolayers for integrated dissolution/permeation studies [70]. | The gold standard for predicting human intestinal permeability. |
| Polarization Cytokines (IFN-γ, IL-4) | Used to polarize macrophages to pro-inflammatory (M1, using IFN-γ) or anti-inflammatory (M2, using IL-4) states for biomaterial testing [7]. | Essential for establishing baseline immune responses in in vitro models. |
| Anti-inflammatory Cytokines (e.g., IL-10) | Bioactive molecules that can be incorporated into biomaterials to induce a pro-regenerative immune environment [50]. | Enables active immunomodulation from the material surface. |
| siRNA/miRNA Sequences | Genetic tools to precisely target and silence specific genes or pathways involved in the inflammatory response to biomaterials [50]. | Allows for highly specific immunomodulation strategies. |
The Critical Role of IVIVC Levels and Regulatory Strategy
Formal IVIVC is a predictive mathematical model relating an in vitro property (e.g., dissolution rate) to an in vivo response (e.g., plasma drug concentration). The U.S. Food and Drug Administration (FDA) recognizes multiple levels of correlation, with varying predictive power and regulatory utility [70] [71].
Table 3: Levels of In Vitro-In Vivo Correlation (IVIVC)
| Level | Definition | Predictive Value | Regulatory Acceptance |
|---|---|---|---|
| Level A | A point-to-point correlation between in vitro dissolution and the in vivo absorption rate [71]. | High – predicts the full plasma concentration-time profile. | Most preferred by regulators; can support biowaivers for post-approval changes [71]. |
| Level B | Uses statistical moment analysis to compare the mean in vitro dissolution time to the mean in vivo residence or absorption time [70] [71]. | Moderate – does not reflect the actual shape of the in vivo profile. | Less robust; generally not sufficient for waiving bioequivalence studies [71]. |
| Level C | Relates a single dissolution time point (e.g., t~50%~) to a single pharmacokinetic parameter (e.g., AUC or C~max~) [70] [71]. | Low – does not predict the full profile. | Least rigorous; useful for early development but insufficient for biowaivers [71]. |
A validated Level A IVIVC is a powerful regulatory asset. It can be used to set clinically relevant dissolution specifications and to obtain a biowaiver, allowing sponsors to forego additional in vivo bioequivalence studies for certain formulation and manufacturing changes [71]. This significantly reduces development time and cost.
Overcoming the hurdle of poor in vitro-in vivo correlation requires a paradigm shift from simplistic testing to a holistic, integrated approach. By employing biorelevant in vitro tools that capture complex physiological processes like lipid digestion and immune activation, and by leveraging the power of computational models like PBPK and AI, researchers can significantly improve the predictive power of their development pipelines. For biomaterials, explicitly designing for a favorable immune response—by engineering surface, mechanical, and bioactive properties—is no longer a futuristic concept but a necessary strategy to ensure in vivo success. As these advanced methodologies continue to evolve and become more accessible, they promise to de-risk development, accelerate the delivery of innovative drugs and medical devices to patients, and usher in a new era of precision medicine.
Tailoring Biomaterials for Aging Immune Systems ('Inflammaging') and Inter-individual Variation
The success of biomedical implants, tissue-engineered constructs, and drug delivery systems is fundamentally governed by their interaction with the host immune system. The aging global population presents a unique challenge, as biomaterials must increasingly function within the context of immunosenescence and inflammaging—the age-related chronic, low-grade inflammation. This altered immune landscape significantly impacts host-biomaterial integration, repair processes, and long-term therapeutic outcomes. This whitepaper delineates the key age-related shifts in immune function, details their consequences for biomaterial performance, and synthesizes a strategic framework for the design and evaluation of next-generation biomaterials tailored for aging populations. By embracing an immunologically informed approach that accounts for inter-individual variation, the field can overcome a major barrier to the clinical translation and efficacy of biomaterial-based therapies for the elderly.
The host response to biomaterials is a dynamic cascade involving innate and adaptive immunity. The traditional paradigm of biomaterial design has often sought to be passively "inert." However, contemporary understanding recognizes that all materials actively interact with the immune system, and the goal is to orchestrate a desired immunomodulatory response rather than suppress all activity [73] [74]. This paradigm is complicated by aging, which induces profound, systemic changes in immune function.
Aging is characterized by a state of chronic, low-grade inflammation, termed "inflammaging," coupled with a progressive decline in immune efficacy known as immunosenescence [75]. These changes are not merely quantitative but qualitative, affecting the very nature of how immune cells recognize, respond to, and resolve challenges. For biomaterials, this can manifest as a delayed, dysregulated foreign body response (FBR), impaired tissue integration, and a heightened propensity for fibrosis and chronic inflammation [76]. Furthermore, the immune system's high degree of plasticity means that inter-individual variation—driven by genetics, past infections, diet, and environment—can lead to vastly different outcomes for the same implanted material [77] [78]. Therefore, tailoring biomaterials for the aging immune system is not a niche consideration but a central challenge in ensuring the broad success of regenerative medicine and medical devices.
The Aging Immune System: Key Shifts and Impact on Biomaterial Integration
Understanding the specific alterations in the aged immune microenvironment is the first step in designing compatible biomaterials. These changes occur at multiple levels, from systemic signaling to cellular dysfunction.
Systemic Inflammaging and Cellular Senescence
A hallmark of aging is the accumulation of senescent cells, which secrete a complex mixture of pro-inflammatory cytokines, chemokines, and growth factors known as the Senescence-Associated Secretory Phenotype (SASP) [75]. The SASP includes factors like IL-1β, IL-6, and TNF-α, which perpetuate a chronic inflammatory milieu. This environment can pre-condition the host to respond more aggressively to an implant, skewing the critical balance between pro- and anti-inflammatory signals needed for constructive remodeling. Moreover, the aging immune system becomes less efficient at clearing these senescent cells, creating a vicious cycle of inflammation and dysfunction [75].
Dysregulation of Key Immune Cells
The functionality of nearly all immune cells is altered with age, directly impacting the phases of the FBR. The table below summarizes the key age-related changes in critical immune cell types.
Table 1: Age-Related Dysregulation of Key Immune Cells in the Foreign Body Response
| Immune Cell | Key Age-Related Changes | Impact on Biomaterial Integration & Tissue Repair |
|---|---|---|
| Macrophages | - Dysregulated polarization; impaired transition from pro-inflammatory M1 to pro-healing M2 phenotype [76].- Reduced phagocytic and autophagic capacity [75].- Increased baseline secretion of pro-inflammatory SASP factors (e.g., TNF-α, IL-6) [75]. | - Prolonged inflammatory phase, hindering integration.- Failure to clear cellular debris, leading to chronic inflammation.- Promotion of fibrosis over functional tissue regeneration. |
| T-cells | - Immunosenescence: Decline in naive T-cell population and diversity [75].- Shift in CD4+ T-helper subsets; increased TH17 activity linked to fibrosis [77].- Increased biophysical stiffness, impairing migratory ability [76]. | - Weakened adaptive immune surveillance, increasing infection risk.- Contributes to persistent inflammation and fibrotic encapsulation of implants.- Reduced homing to injury sites, impairing coordination of repair. |
| Neutrophils | - Decreased phagocytic capacity, chemotaxis, and pathogen clearance [75].- Abnormal release of Neutrophil Extracellular Traps (NETs) [75]. | - Inefficient clearance of initial injury site, compromising subsequent healing phases.- Can contribute to collateral tissue damage and persistent inflammation. |
| Hematopoietic Stem Cells (HSCs) | - Myeloid Bias: Increased differentiation into myeloid cells (e.g., neutrophils, macrophages) over lymphoid cells (e.g., T-cells, B-cells) [75]. | - Alters the entire immune cell supply chain, contributing to a pro-inflammatory baseline and reducing adaptive immune capacity from the outset. |
The following diagram illustrates the vicious cycle of inflammaging and its impact on the host's ability to respond to a biomaterial implant.
Strategic Framework for Designing Age-Tailored Biomaterials
Moving from understanding the problem to implementing solutions, the design of biomaterials must evolve to actively modulate the aged immune microenvironment. The following strategies are at the forefront of this effort.
Material-Driven Immunomodulation
The intrinsic properties of a biomaterial can be engineered to guide a favorable immune response.
- Surface Properties and Topography: Surface chemistry, charge, and micro-/nano-topography can directly influence protein adsorption and immune cell adhesion. For instance, controlling macrophage polarization towards the pro-regenerative M2 phenotype can be achieved by modifying surface roughness or presenting specific biochemical cues [74] [79].
- Mechanical Properties: The stiffness of the biomaterial should be matched to the target tissue, as mechanical cues are sensed by immune cells via mechanotransduction pathways. Aged tissues often have altered extracellular matrix (ECM) compliance, and mismatched stiffness can exacerbate the FBR [76].
- Controlled Release of Immunomodulators: Biomaterials can be designed as delivery systems for agents that actively resolve inflammation. This includes the release of anti-inflammatory cytokines (e.g., IL-4, IL-10), pro-resolving lipid mediators (e.g., Resolvins, Protectins), or drugs that target senescent cells (senolytics) [73] [74] [76].
Advanced Engineering Platforms
- Smart and Adaptive Systems: "Smart" biomaterials that change their properties in response to local environmental cues (e.g., pH, enzyme activity) are ideal for the dynamic aged microenvironment. For example, a material could release an anti-inflammatory factor specifically in response to elevated reactive oxygen species (ROS) levels [74].
- Artificial Antigen Presenting Cells (aAPCs): Engineered aAPCs are an innovative platform to directly combat T-cell immunosenescence. These biomimetic particles, with specific biophysical properties, have been shown to induce robust and sustained T memory stem cell responses even in aged mice, revitalizing adaptive immunity [76].
Table 2: Key Design Parameters for Age-Tailored Immunomodulatory Biomaterials
| Design Parameter | Target | Desired Outcome in Aging Host |
|---|---|---|
| Controlled Porosity (e.g., 30-40 μm for angiogenesis) | Macrophage polarization, vascularization | Enhanced M2 polarization, improved nutrient/waste exchange, and integration [78]. |
| Tuned Stiffness | Mechanosensing, Fibrosis | Matching native tissue mechanics to avoid excessive fibroblast activation and fibrotic encapsulation. |
| Anti-inflammatory Cytokine Release (e.g., IL-4, IL-10) | Macrophage & T-cell phenotype | Shift from chronic M1/TH17 inflammation to pro-healing M2/Treg response [77] [74]. |
| Pro-Resolving Mediator Release (e.g., Resolvin D1) | Inflammation Resolution | Active cessation of inflammatory response, promoting a healing environment [73]. |
| Senomorphic/Senolytic Delivery | Senescent Cell Burden | Reduction of local and systemic SASP, breaking the cycle of inflammaging [75]. |
The strategic application of these design principles is aimed at redirecting the dysregulated foreign body response in aged individuals towards a more constructive and regenerative outcome, as summarized below.
The Scientist's Toolkit: Experimental Protocols and Reagents
Translating the above strategies into practice requires robust experimental methodologies. Below is a protocol for evaluating the immune response to a biomaterial in the context of aging, followed by a table of essential research reagents.
Detailed Experimental Protocol: Evaluating Age-Dependent Foreign Body Response In Vivo
Objective: To assess the host immune response and tissue integration of a novel biomaterial in young versus aged murine models.
Materials:
- Test Biomaterial: Hydrogel, scaffold, or film of interest.
- Animal Models: Young adult (2-3 month old) and aged (18-24 month old) mice, preferably C57BL/6 strain.
- Surgical tools, suture, anesthesia, and analgesic agents.
- Tissue processing equipment for histology and flow cytometry.
Methodology:
- Implantation: Under aseptic conditions and approved IACUC protocol, implant the biomaterial subcutaneously or in the target tissue (e.g., abdominal wall, bone defect) in both young and aged mouse cohorts. Include a sham surgery group as a control.
- Endpoint Analysis: Euthanize animals at multiple time points (e.g., 3, 7, 14, 28 days) to capture acute and chronic phases of the FBR.
- Histology & Immunohistochemistry: Harvest and fix the implant with surrounding tissue.
- Process, embed in paraffin, and section.
- Perform H&E staining to assess general tissue architecture and cellular infiltration.
- Perform Masson's Trichrome staining to quantify collagen deposition and fibrosis.
- Perform IHC/IF staining for key immune markers:
- Macrophages: F4/80 (pan-macrophage), iNOS (M1), CD206 (M2).
- T-cells: CD3, CD4, CD8.
- Cellular Senescence: p16INK4a, p21.
- Flow Cytometry: Harvest the implant and process into a single-cell suspension.
- Stain cells with fluorescently labeled antibodies for:
- Myeloid Lineage: CD11b, Ly6G (neutrophils), Ly6C (monocytes), F4/80, MHC-II, CD206.
- Lymphoid Lineage: CD3, CD4, CD8, CD19 (B-cells), FoxP3 (Tregs).
- Analyze on a flow cytometer to quantify and phenotype infiltrating immune cells. Compare the ratios (e.g., M1/M2, CD8+/Treg) between young and aged groups.
- Stain cells with fluorescently labeled antibodies for:
- Gene Expression Analysis (qRT-PCR): Isolve RNA from the implant tissue.
- Analyze the expression of pro-inflammatory (e.g., Il1b, Il6, Tnf, Nos2) and pro-resolving/fibrotic genes (e.g., Arg1, Tgfb1, Col1a1).
- Histology & Immunohistochemistry: Harvest and fix the implant with surrounding tissue.
Data Interpretation: A successful age-tailored biomaterial should show reduced prolonged M1 markers, lower expression of SASP and fibrotic genes, and a more organized tissue structure in the aged group compared to a control material.
Essential Research Reagent Solutions
Table 3: Key Reagents for Investigating Biomaterial-Immune Interactions in Aging
| Research Reagent / Tool | Function / Target | Application in the Field |
|---|---|---|
| Anti-mouse F4/80 Antibody | Pan-macrophage marker | Identifying and quantifying total macrophage infiltration into the biomaterial in histology and flow cytometry [76]. |
| Anti-mouse iNOS & CD206 Antibodies | M1 (pro-inflammatory) and M2 (pro-healing) macrophage markers, respectively | Phenotyping macrophage polarization states in response to the biomaterial to assess immunomodulatory efficacy [77] [76]. |
| Anti-mouse CD3, CD4, CD8 Antibodies | T-lymphocyte markers | Profiling adaptive immune cell recruitment and activation (Cytotoxic T-cells, T-helper cells) [77] [76]. |
| p16INK4a Antibody | Key cyclin-dependent kinase inhibitor and senescence marker | Detecting and quantifying cellular senescence in the peri-implant tissue via IHC/IF [75]. |
| Recombinant IL-4 & IL-10 Cytokines | Anti-inflammatory cytokines | Loading into biomaterials to actively drive macrophage polarization towards an M2 phenotype and promote a tolerogenic immune response [74] [79]. |
| Senolytic Drugs (e.g., Dasatinib + Quercetin) | Induce apoptosis in senescent cells | Co-delivery with biomaterials to reduce the local burden of senescent cells and their pro-inflammatory SASP, potentially improving integration [75]. |
| Luminex / Cytokine Bead Array | Multiplexed protein quantification | Simultaneously measuring a panel of pro- and anti-inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α, IL-10) in homogenized implant tissue or serum to assess systemic and local inflammation. |
The intersection of biomaterials science, immunology, and gerontology is a critical frontier for the future of regenerative medicine. The evidence is clear that a "one-size-fits-all" approach to biomaterial design is inadequate, particularly for the physiologically distinct aging population. Success hinges on deliberately engineering immunomodulatory biomaterials (IMBs) that can navigate the complex, pro-inflammatory, and dysfunctional landscape of the aged immune system.
Future progress will depend on several key developments:
- Embracing Complexity: Moving beyond simplistic M1/M2 dichotomies to understand the full spectrum of immune cell plasticity in aging using high-dimensional techniques like single-cell RNA sequencing [78].
- Personalized Biomaterial Solutions: Leveraging computational models and AI to predict individual immune responses and design personalized material formulations based on a patient's immune history and biological age [78].
- Advanced Pre-clinical Models: Developing more sophisticated in vitro models that incorporate aged immune cells and senescent ECM, and using aged animal models as a standard for testing, not an afterthought [56] [76].
By systematically integrating these principles, researchers can pioneer a new generation of biomaterials that are not merely compatible with aging biology but are actively designed to harness and redirect it, thereby unlocking robust tissue repair and improved quality of life for the elderly.
Combating Biofilm Formation on Implants as a Failure of Immune-Biomaterial Interaction
The integration of biomaterials into the human body represents a cornerstone of modern medicine, enabling revolutionary advances in replacing damaged tissues and restoring physiological function. However, the persistent threat of implant-associated infection (IAI) undermines the therapeutic success of these interventions, representing a critical failure point in the host-biomaterial interface. Medical device-associated infections account for a substantial proportion of hospital-acquired infections, with biofilms identified as the underlying cause in 60-80% of microbial infections [80] [81]. These infections occur when opportunistic pathogens colonize implant surfaces, forming structured microbial communities encased in a protective extracellular polymeric substance (EPS) that shields them from both antimicrobial agents and host immune defenses [82] [81]. The complex interplay between the biomaterial, bacterial pathogens, and host immune system creates a perfect storm that allows biofilms to persist and thrive despite extensive therapeutic interventions.
The fundamental challenge lies in the triangular interaction between implant surfaces, microbial colonization strategies, and compromised host immunity at the implantation site. Biomaterials, whether metallic or polymeric, inadvertently create an immunocompromised zone at their interface with host tissues, reducing the efficacy of immune cells and creating a locus minoris resistentiae susceptible to bacterial colonization [83] [81]. Bacteria rapidly adhere to virtually all biomaterial surfaces, initiating a complex developmental pathway toward mature biofilms that exhibit dramatically increased resistance to antibiotics—up to 1000-fold greater than their planktonic counterparts [82]. This review examines the mechanistic basis of biofilm formation on implants as a failure of immune-biomaterial interaction and explores innovative strategies to combat this persistent clinical challenge through immunomodulatory approaches.
Pathogenesis: The Biofilm-Immune-Biomaterial Interface
Biofilm Development on Implant Surfaces
Bacterial colonization of biomaterials follows a meticulously orchestrated sequence of events that transforms free-floating planktonic cells into resilient, surface-associated communities. The process initiates with reversible attachment mediated by non-specific physical forces including van der Waals interactions, hydrophobic effects, and electrostatic forces [84]. This transient association becomes permanent through microbial surface components recognizing adhesive matrix molecules (MSCRAMMs) that facilitate firm anchorage to protein-conditioned biomaterials [81].
Following initial attachment, intracellular signaling pathways activate the production of cyclic dimeric guanosine monophosphate (c-di-GMP), triggering a phenotypic switch from motile to sessile lifestyle. This transition involves downregulation of flagellar motility and upregulation of surface adhesins, pili, and fimbriae that strengthen attachment to the surface and neighboring cells [84]. As microcolonies form, bacteria commence copious production of EPS—a highly hydrated matrix of polysaccharides, proteins, extracellular DNA, and lipids that provides structural integrity and protection [82] [84].
The final stages of biofilm development involve maturation into complex three-dimensional structures with nutrient gradients, water channels, and metabolic specialization, followed by active dispersal of planktonic cells to seed new colonization sites [84]. This highly organized developmental pathway enables bacterial communities to persist in hostile environments, including the human body with its sophisticated immune defenses.
Immune Evasion Mechanisms of Biofilms
Biofilms employ sophisticated strategies to circumvent host immune responses, creating protected niches where bacteria can persist despite robust immunological surveillance. The EPS matrix acts as a physical barrier that limits penetration of antimicrobial peptides, antibodies, and complement proteins while simultaneously impeding phagocyte migration and activation [82] [84]. Beyond physical protection, biofilms actively modulate immune cell function through multiple mechanisms:
- Macrophage polarization manipulation: Biofilms disrupt the normal M1/M2 phenotypic transition, reducing the killing efficiency of macrophages and promoting chronic infection states [83].
- Phagocytic blockade: The EPS matrix creates a steric hindrance that prevents effective phagocytosis, while biofilm-associated antigens may fail to elicit effective opsonizing antibodies [81].
- Neutrophil dysfunction: Biofilms can trigger excessive neutrophil activation leading to tissue damage from reactive oxygen species (ROS) and enzyme release, while simultaneously resisting actual bacterial killing [83].
- Immune exhaustion: Persistent biofilm antigens lead to chronic inflammation and eventual T-cell exhaustion, reducing adaptive immune effectiveness [84].
Biofilms further enhance their resilience through metabolic heterogeneity, with gradients of nutrients and oxygen creating distinct metabolic zones containing dormant "persister" cells that exhibit exceptional tolerance to antibiotics and immune effectors [82] [84]. This multicellular organization, coupled with cell-to-cell communication via quorum sensing, allows biofilms to function as coordinated microbial tissues capable withstanding host defense mechanisms.
Biomaterial Properties Influencing Biofilm Formation and Immune Response
The physicochemical characteristics of implant materials significantly impact both bacterial adhesion and subsequent immune responses, creating variable susceptibility to biofilm establishment across different biomaterials. The surface topography, chemistry, and wettability directly influence protein adsorption and cellular interactions that determine biofilm susceptibility and immune cell activity [56] [31].
Table 1: Biomaterial Properties Impacting Biofilm Formation and Immune Response
| Biomaterial Class | Examples | Biofilm Susceptibility | Immune Response |
|---|---|---|---|
| Metallic Materials | Stainless steel, Titanium alloys, Cobalt-chromium alloys | Moderate to high; corrosion increases risk | Metal ion release can cause inflammation; may impair immune cell function |
| Polymers | PTFE, Polyethylene, Silicone | High for porous materials | Particle debris triggers inflammation; can reduce phagocytic ability |
| Natural Biomaterials | Collagen, Chitosan, Hyaluronic acid | Variable based on processing | Generally more compatible; can be engineered for immunomodulation |
| Ceramics/Bioactive Glass | Hydroxyapatite, Bioglass | Lower susceptibility | Typically favorable; can support immune function |
The foreign body reaction itself creates an immunocompromised microenvironment around implants, characterized by the formation of a fibroinflammatory zone that impairs immune cell function [81]. Upon implantation, proteins immediately adsorb to the biomaterial surface, creating a conditioning film that influences subsequent bacterial and host cell interactions [81]. Macrophages encountering implants often undergo frustrated phagocytosis, releasing pro-inflammatory cytokines and ROS that cause local tissue damage without effectively clearing pathogens [83]. Eventually, macrophages fuse to form foreign body giant cells (FBGCs) that secrete additional inflammatory mediators and contribute to the formation of a dense fibrous capsule, further isolating the implant from immune surveillance and creating a protected niche for bacterial persistence [83].
Quantitative Assessment of Biofilm Dynamics
Advanced analytical techniques have enabled precise quantification of biofilm formation dynamics, providing critical insights into the interplay between bacterial communities, biomaterials, and immune responses. Digital holographic tomography (DHT) has emerged as a powerful label-free, non-destructive method for characterizing biofilm formation directly on material surfaces, enabling three-dimensional reconstruction of refractive index (RI) distributions to quantify biomass, cellular density, and viability [85].
Table 2: Quantitative Parameters of Biofilm Formation on Contact Lens Materials Measured by Digital Holographic Tomography
| Parameter | Staphylococcus epidermidis | Pseudomonas aeruginosa | Significance |
|---|---|---|---|
| Single Cell RI Range | Higher RI values | Lower RI values | Reflects species-specific cellular density and composition |
| RI Change During Cell Division | Increase during process | Increase during process | Indicates density changes during replication |
| RI Decrease During Cell Death | 9.161 × 10−3 RIU | 4.933 × 10−3 RIU | Marker for cell viability and antimicrobial efficacy |
| Biofilm Architecture | Species-dependent structures | Species-dependent structures | Influences antibiotic penetration and immune evasion |
DHT measurements have revealed that the refractive index serves as a sensitive marker for cellular viability, with characteristic decreases observed during cell death processes [85]. During cell division, RI values increase as cells elongate and cytoplasmic contents reorganize, while dying cells exhibit initial size expansion with concomitant RI decrease followed by eventual reduction in both size and RI as cell wall integrity is lost [85]. These quantitative relationships enable researchers to monitor biofilm development and treatment responses without disturbing the native biofilm structure, providing advantages over conventional methods like crystal violet staining or colony forming unit (CFU) counting that require biofilm disruption [85] [80].
The material-specific variations in biofilm formation dynamics have been quantitatively demonstrated across different biomaterials. Studies on soft contact lens materials revealed significant species- and time-dependent differences in biofilm RI and volume between hydrogel and silicone hydrogel materials, highlighting how biomaterial composition influences colonization dynamics [85]. Such quantitative assessments are essential for developing evidence-based strategies to combat biofilm formation through biomaterial engineering.
Experimental Models and Methodologies for Biofilm Research
Standard Quantitative Assessment Methods
Robust assessment of biofilm formation and treatment efficacy requires standardized methodologies that generate reproducible, quantitative data across research laboratories. The table below summarizes core techniques employed in biofilm research, each offering distinct advantages and limitations for specific applications.
Table 3: Standard Methodologies for Biofilm Quantification and Characterization
| Method | Principle | Applications | Advantages | Limitations |
|---|---|---|---|---|
| Colony Forming Unit (CFU) Counting | Viable cell enumeration through serial dilution and plating | Determination of viable bacterial numbers in biofilms | Direct measure of cell viability; no specialized equipment needed | Time-consuming; cannot detect non-culturable cells; biofilm disruption required |
| Crystal Violet Staining | Dye binding to biomass components | Total biofilm biomass quantification | High-throughput capability; inexpensive; simple protocol | Does not distinguish live/dead cells; potential for false positives |
| ATP Bioluminescence | Measurement of ATP from metabolically active cells | Assessment of viable biomass | Rapid results; high sensitivity | Affected by environmental conditions; does not provide cell counts |
| Digital Holographic Tomography (DHT) | 3D refractive index reconstruction | Label-free, non-destructive biofilm characterization on surfaces | Quantitative, non-destructive; provides structural and viability data | Specialized equipment required; complex data analysis |
| Confocal Scanning Laser Microscopy (CSLM) | Optical sectioning with fluorescent probes | 3D biofilm architecture and composition | High-resolution visualization; live/dead differentiation | Requires fluorescent labeling; limited penetration depth |
Protocol for Biofilm Assessment Using CFU Counting
The CFU counting method remains a gold standard for quantifying viable bacteria within biofilms, despite its limitations. The following detailed protocol ensures accurate and reproducible results:
- Biofilm Growth: Grow biofilms on biomaterial substrates in appropriate culture media under conditions mimicking the intended application environment (e.g., physiological temperature, shear stress) for specified durations.
- Biofilm Harvesting: Carefully remove planktonic cells by washing with sterile saline or buffer. Homogenize the biofilm using mechanical methods (scraping, vortexing with beads) or sonication to disperse bacterial aggregates into single-cell suspensions.
- Serial Dilution: Perform 10-fold serial dilutions of the homogenized biofilm suspension in sterile dilution buffer across multiple tubes (typically 10⁻¹ to 10⁻⁶).
- Plating: Aseptically plate 100μL aliquots from appropriate dilutions onto nutrient agar plates, using sterile spreaders to ensure even distribution.
- Incubation: Incubate plates at optimal growth temperature for 24-72 hours until colonies are visually distinguishable.
- Enumeration: Count colonies on plates containing 30-300 colonies for statistical validity. Calculate original concentration using the formula: CFU/mL = (number of colonies × dilution factor) / volume plated.
For low-biomass biofilms, a culture expansion step may be incorporated prior to dilution and plating, where harvested biofilms are suspended in liquid medium and incubated with shaking for a standardized duration to amplify cell numbers while maintaining experimental comparability through normalization to controls [80].
Advanced Imaging and Analysis Protocols
Advanced imaging techniques provide complementary spatial and structural information about biofilm organization:
Confocal Scanning Laser Microscopy Protocol:
- Staining: Apply fluorescent dyes such as SYTO 9 for live cells, propidium iodide for dead cells, and concanavalin A conjugated with fluorescent tags for EPS matrix components.
- Image Acquisition: Collect Z-stack images at predetermined intervals (typically 0.5-1μm) through the biofilm thickness using appropriate laser wavelengths and emission filters.
- 3D Reconstruction: Use specialized software (e.g., IMARIS, COMSTAT) to reconstruct three-dimensional architecture and quantify biovolume, thickness, surface area, and spatial distribution of different components.
Digital Holographic Tomography Protocol [85]:
- Sample Preparation: Grow biofilms directly on transparent biomaterials suitable for optical interrogation.
- Hologram Acquisition: Capture multiple holographic images with varying illumination angles using a laser source and digital camera.
- Refractive Index Tomography: Reconstruct 3D RI distributions using inverse scattering algorithms and specialized software.
- Quantitative Analysis: Extract parameters including total biofilm volume, average RI, spatial RI variations, and temporal changes corresponding to viability shifts.
Immunomodulatory Strategies to Combat Biofilm Infections
Biomaterial-Based Immunomodulation
Novel biomaterial engineering approaches focus on actively modulating host immune responses to enhance natural defenses against biofilm formation. These strategies recognize that restoring proper host-protective immunity is essential for combating established biofilms and preventing new colonization.
Metal ion-releasing coatings represent a promising approach that combines direct antibacterial effects with immunomodulatory functions. Copper (Cu)-incorporated coatings have demonstrated ability to promote M1 macrophage polarization, enhancing pro-inflammatory cytokine production (TNF-α, IL-6) while suppressing anti-inflammatory signals (IL-4, IL-10) [83] [86]. This polarization enhances phagocytic activity and intracellular bacterial killing, addressing the limitation of conventional antibiotics against internalized pathogens. Cobalt (Co)-doped titanium dioxide coatings similarly promote M1 polarization while simultaneously disrupting bacterial proton transfer mechanisms, providing dual action against planktonic and biofilm-associated bacteria [86].
Stimuli-responsive polymeric coatings offer dynamic control over immune modulation in response to infection biomarkers. Photothermally responsive systems incorporating bismuth nanoparticles within hyaluronic acid/gelatin hydrogels enable near-infrared triggered hyperthermia for biofilm disruption while simultaneously scavenging excessive ROS to mitigate inflammation-mediated tissue damage [86]. These smart materials create anti-adhesive surfaces under normal conditions while activating on-demand therapeutic responses upon detection of biofilm formation.
Cytokine-eluting biomaterials represent another innovative approach, with surfaces engineered to release interleukin cytokines that direct local immune responses toward effective biofilm clearance. These strategies require precise control over cytokine release kinetics to achieve therapeutic benefits without triggering excessive inflammation [86].
Schematic Representation of Immunomodulatory Strategies
The following diagram illustrates key immunomodulatory approaches to combat biofilm formation on implants:
Pathway Engineering for Enhanced Immune Recognition
Engineering immune recognition pathways represents a sophisticated approach to combat biofilm evasion mechanisms. Biomaterials can be functionalized with pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs) that enhance immune detection of biofilm-forming bacteria. Surfaces modified with toll-like receptor (TLR) agonists such as synthetic lipopeptides or CpG oligonucleotides trigger controlled inflammatory responses that activate macrophages and neutrophils before biofilms become established [31] [86].
The integrin receptor pathway represents another promising target for biomaterial engineering. Collagen-based biomaterials functionalized with specific peptide sequences (e.g., Gly-Pro-Hyp tripeptide) enhance integrin-mediated activation of focal adhesion kinase (FAK) and subsequent signaling through PI3K-Akt and MAPK pathways, promoting effective immune cell adhesion and activation at the implant interface [31]. Similarly, modulation of discoidin domain receptors (DDR1 and DDR2) on immune cells through collagen-functionalized biomaterials influences cell spreading, migration, and proliferation, potentially enhancing immune surveillance at vulnerable implantation sites [31].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table compiles key reagents, materials, and methodologies essential for investigating biofilm-immune-biomaterial interactions, providing researchers with a curated toolkit for experimental design.
Table 4: Essential Research Toolkit for Biofilm-Immune-Biomaterial Investigations
| Category | Specific Reagents/Materials | Research Application | Key Considerations |
|---|---|---|---|
| Biomaterial Substrates | Titanium alloys, Medical-grade polymers (PTFE, PEEK), Hydrogels, Decellularized ECM | Testing biofilm formation on clinically relevant materials | Consider surface energy, roughness, and protein adsorption characteristics |
| Bacterial Strains | Staphylococcus epidermidis, Staphylococcus aureus, Pseudomonas aeruginosa | Representative species for orthopedic and device-related infections | Select appropriate ATCC strains with characterized biofilm-forming capabilities |
| Immune Cell Models | RAW 264.7 (murine macrophages), THP-1 (human monocytes), Primary neutrophils | In vitro immunomodulation assessment | Primary cells show more physiological responses but have limited expansion capability |
| Assessment Reagents | Crystal violet, SYTO 9/propidium iodide, ATP bioluminescence kits, ELISA cytokine panels | Biofilm quantification and immune response characterization | Validate multiple methods for comprehensive assessment |
| Immunomodulatory Agents | Metal ions (Cu²⁺, Co²⁺), Cytokines (IL-4, IL-10, TNF-α), TLR agonists | Testing immune-enhanced anti-biofilm strategies | Optimize concentration to avoid excessive inflammation |
| Advanced Imaging Tools | Confocal microscopy with 3D reconstruction software, Digital holographic tomography systems | Spatial analysis of biofilm-immune cell interactions | Label-free methods avoid potential staining artifacts |
The persistent challenge of biofilm formation on medical implants represents a critical failure at the interface of biomaterials science and immunology. The traditional paradigm focused exclusively on direct bactericidal approaches has proven inadequate against the resilient, community-based defense strategies of biofilms. The emerging recognition that biofilms actively manipulate host immune responses has catalyzed a paradigm shift toward immunomodulatory strategies that enhance natural clearance mechanisms while preventing pathological inflammation.
Future advances in combating biofilm infections will likely emerge from multidisciplinary approaches that integrate materials science, immunology, microbiology, and systems biology. Promising directions include the development of smart biomaterials with feedback-controlled therapeutic release based on real-time detection of biofilm biomarkers, and personalized implant strategies that account for individual variations in immune responses. The growing understanding of the human microbiome and its interactions with medical devices may further reveal opportunities for probiotic-based approaches that exploit ecological competition to prevent pathogen colonization.
As antimicrobial resistance continues to escalate, immunomodulatory biomaterials represent a promising alternative pathway to address the persistent challenge of implant-associated infections. By strategically engineering the immune-biomaterial interface to favor host-protective responses while mitigating collateral tissue damage, researchers can develop next-generation implants that resist biofilm formation through biological integration rather than mere physical exclusion. This approach ultimately acknowledges that the most effective defense against biofilm infections may lie in optimizing the natural capabilities of the human immune system rather than attempting to replace them.
Assessing Efficacy: Advanced Analytical Techniques and Comparative Biomaterial Performance
The clinical success of biomaterials used in grafting, medical devices, and tissue engineering is profoundly limited by immune-mediated rejection, underscoring the critical importance of comprehensive in vitro immune response assessment during development. Despite a global medical device market estimated at $400 billion, clinical uptake of biomaterials remains poor, with high failure rates often attributed to adverse immune reactions [87]. For instance, the RESTORE collagen implant for rotator cuff repair was recalled after severe inflammatory reactions necessitated reoperation and removal in 4 of 19 initial clinical cases [87]. Similarly, off-label use of the InFUSE bone scaffold in cervical fusion resulted in life-threatening complications, including severe dysphagia, respiratory failure, and mortality due to immune-mediated soft tissue swelling [87]. These clinical failures highlight a significant gap in current preclinical testing paradigms, which often fail to adequately predict host immune responses.
Traditional in vitro testing protocols for biomaterials primarily follow International Organisation for Standardisation (ISO) guidelines focused on general cytotoxicity, with tissue-specific assessments often limited to cytocompatibility evaluations using metabolic assays and imaging [87]. However, a recent European multicentre analysis revealed surprisingly poor correlation between these standard in vitro tests and in vivo outcomes for bone regeneration, indicating that current methods are insufficient for predicting clinical acceptance [87]. Given that immune rejection represents a common endpoint for biomaterial failure, incorporating sophisticated immunogenic evaluation into development pipelines is essential for improving clinical translation, reducing animal testing, and enhancing patient safety [87] [39].
This technical guide provides comprehensive methodologies for assessing immune responses to biomaterials through viability, maturation, and activation assays, framed within the context of biomaterial-host interactions. By employing these predictive in vitro screening approaches, researchers can better identify potentially problematic materials earlier in development, optimize biomaterial design for improved immune compatibility, and ultimately enhance the safety profile of devices reaching clinical application.
The Immune Response to Biomaterials: Foundation for Assay Development
The Foreign Body Response Cascade
The foreign body response to implanted biomaterials follows a coordinated sequence of immune activation that begins immediately upon implantation. This cascade initiates with protein adsorption, where host plasma proteins adhere to the biomaterial surface, creating a provisional matrix that activates inflammatory pathways [87]. The subsequent acute inflammation phase, lasting from minutes to days, is characterized by infiltration of polymorphonuclear leukocytes, predominantly neutrophils, with contributions from eosinophils and basophils [87]. These cells attempt to clear surgical debris and activate host defense mechanisms.
Following the acute phase, chronic inflammation ensues, defined by the presence of mononuclear leukocytes including monocytes, macrophages, and lymphocytes [87]. Macrophages play a particularly central role in this phase, releasing enzymes crucial for tissue reorganization and angiogenesis, phagocytosing debris, and secreting cytokines and growth factors that recruit and stimulate other cell types including fibroblasts and mesenchymal stem cells [87]. This chronic inflammatory phase transitions into the resolution of healing or, in the case of incompatible materials, persistent inflammation that can lead to rejection.
Key Immune Cell Players
Different immune cell populations contribute distinct functions throughout the foreign body response, making them relevant targets for in vitro assessment:
- Macrophages exist in a spectrum of activation states, broadly categorized as pro-inflammatory M1 (classically activated) and anti-inflammatory M2 (alternatively activated) phenotypes, with M2 further subdivided into M2a (allergic responses), M2b (immune regulation), and M2c (wound healing) [87]. The balance between these phenotypes significantly influences biomaterial integration versus rejection.
- Lymphocytes including T cells and B cells contribute to the acquired immune response, with specific subpopulations such as T helper cells (Th1, Th2), cytotoxic T cells, and regulatory T cells modulating inflammatory pathways and antibody production [88].
- Dendritic cells and Natural Killer (NK) cells provide additional links between innate and adaptive immunity, serving as important indicators of immunogenic potential [87] [89].
- Peripheral Blood Mononuclear Cells (PBMCs) provide a heterogeneous population of primary immune cells (monocytes, lymphocytes) for comprehensive screening [87] [88].
Table 1: Key Immune Cell Types in Biomaterial Response and Their Functions
| Cell Type | Subpopulations | Primary Functions in FBR | Relevance to Biomaterials |
|---|---|---|---|
| Macrophages | M1, M2a, M2b, M2c | Phagocytosis, cytokine secretion, tissue remodeling | Primary effector cells; polarization predicts outcome |
| T Lymphocytes | CD4+ (Th1, Th2, Treg), CD8+ | Immune regulation, cytotoxicity, cytokine production | Drive adaptive immune response; indicate antigenicity |
| B Lymphocytes | Plasma cells, memory B cells | Antibody production, antigen presentation | Humoral response; minimal assessment in literature |
| Dendritic Cells | Conventional, plasmacytoid | Antigen presentation, T cell priming | Bridge innate/adaptive immunity |
| Natural Killer Cells | Various cytotoxic subsets | Direct cytotoxicity, cytokine secretion | Early innate response against biomaterials |
Viability Assays: Assessing Immune Cell Cytotoxicity
Methodological Approaches
Viability assays determine immune cell cytotoxicity in response to biomaterials, providing an initial assessment of biocompatibility. These assays measure whether materials induce cell death or, conversely, promote excessive activation and proliferation, both of which can indicate undesirable interactions [87].
Visualization Methods enable direct observation of immune cell morphology and attachment to biomaterial surfaces:
- Protocol: Seed immune cells (e.g., PBMCs, macrophages) onto biomaterial substrates in appropriate culture conditions. After incubation (typically 24-72 hours), stain cells using calcein-AM (for live cells) and ethidium homodimer (for dead cells) according to manufacturer instructions. Alternatively, use actin (e.g., phalloidin) and nuclei (e.g., DAPI) staining to visualize cytoskeletal organization and cell distribution.
- Imaging: Analyze using fluorescence or confocal microscopy to assess cell number, morphology, and distribution across the material surface.
- Data Interpretation: Quantitative image analysis software can calculate cell viability percentages and cell density. Note that increased immune cell viability may indicate activation rather than biocompatibility [87].
Metabolic Assays provide quantitative measures of cell viability and proliferation:
- alamarBlue Assay Protocol: Seed cells on biomaterials in culture medium. Add alamarBlue reagent (typically 10% of total volume) and incubate for 1-4 hours protected from light. Measure fluorescence (excitation 530-570 nm, emission 580-620 nm) or absorbance (570 nm with 600 nm reference). Calculate percentage reduction compared to negative and positive controls.
- Glucose-6-Phosphate Dehydrogenase (G6PD) Assay: Based on release of G6PD from damaged cells. Incubate cell-biomaterial cultures with glucose-6-phosphate, NADP+, and tetrazolium dye. Measure formazan production spectrophotometrically.
- Considerations: Metabolic assays may be influenced by material color, porosity, and degradation products that interfere with detection. Include material-only controls to account for background signal [87].
Technical Considerations and Limitations
While viability assays provide valuable initial screening data, they offer limited insight into functional immune responses when used in isolation. The table below summarizes key viability assessment methods with their applications and limitations:
Table 2: Immune Cell Viability Assessment Methods for Biomaterial Testing
| Method | Principle | Key Outputs | Advantages | Limitations |
|---|---|---|---|---|
| Live/Dead Staining | Membrane integrity discrimination | Cell viability %, morphology | Direct visualization, simple | Semi-quantitative, endpoint assay |
| Metabolic Assays (alamarBlue, MTT, WST) | Cellular reductase activity | Metabolic activity, proliferation | Quantitative, high-throughput | Indirect measure, interference possible |
| Enzyme Release (LDH, G6PD) | Membrane damage detection | Cytotoxicity percentage | Quantitative, direct damage measure | Cannot distinguish activation states |
| Flow Cytometry (Annexin V/PI) | Apoptosis/necrosis discrimination | Early/late apoptosis, necrosis | Quantitative, mechanistic insight | Requires single-cell suspension |
Maturation Assays: Evaluating Immune Cell Differentiation
Surface Marker Analysis
Maturation assays evaluate immune cell differentiation in response to biomaterials by measuring changes in surface marker expression that indicate specific activation states. These assays are particularly valuable for characterizing macrophage polarization, which strongly influences biomaterial integration versus rejection [87].
Flow Cytometry Protocols provide quantitative analysis of surface marker expression across cell populations:
- Cell Preparation: Culture primary immune cells (e.g., monocytes, macrophages, PBMCs) with biomaterial extracts or directly on material surfaces for specified durations (typically 24-72 hours). Include appropriate controls (negative, positive polarization stimuli).
- Staining Procedure: Harvest cells, wash with FACS buffer (PBS + 2% FBS), and incubate with fluorochrome-conjugated antibodies against target surface markers (see Table 3 for key markers) for 30 minutes at 4°C protected from light.
- Data Acquisition and Analysis: Analyze using flow cytometry, collecting sufficient events for statistical power (typically ≥10,000 cells per sample). Use fluorescence minus one (FMO) controls for gating. Express results as percentage of positive cells and/or mean fluorescence intensity (MFI) [87].
Immunohistochemistry and Immunofluorescence enable spatial localization of cell maturation states on biomaterial surfaces:
- Protocol: Fix cells on biomaterials with 4% paraformaldehyde, permeabilize with 0.1% Triton X-100 (for intracellular markers), and block with appropriate serum. Incubate with primary antibodies against target markers overnight at 4°C, followed by species-appropriate fluorescent secondary antibodies.
- Imaging and Analysis: Capture images using confocal or fluorescence microscopy. Quantify using image analysis software to determine marker expression patterns and cell distribution [87].
Key Maturation Markers and Interpretation
The functional state of immune cells, particularly macrophages, can be determined by characteristic surface marker profiles that indicate pro-inflammatory (rejection-associated) versus anti-inflammatory (integration-associated) responses:
Table 3: Key Immune Cell Maturation Markers for Biomaterial Assessment
| Cell Type | Pro-inflammatory Markers | Anti-inflammatory Markers | Polarization Stimuli |
|---|---|---|---|
| Macrophages | CD86, CCR7, CD80, MHC-II | CD163, CD206, CD209, CD36 | M1: IFN-γ + LPS; M2: IL-4 |
| Dendritic Cells | CD80, CD86, CD83, CCR7 | CD206, CD163 | Maturation: LPS, TNF-α |
| T Lymphocytes | CD69 (activation), CD25 (activation) | CD73, CD39 (Treg) | TCR stimulation + cytokines |
| Monocytes | CD14, CD16, CD64 | CD163, CD206 | Differentiation: M-CSF, GM-CSF |
Data Interpretation: A favorable immune response to biomaterials typically demonstrates bias toward anti-inflammatory maturation states. For example, Fearing and Van Dyke (2014) used CD86 (pro-inflammatory) and CD206 (anti-inflammatory) staining to show that keratin biomaterials promoted a favorable M2 macrophage polarization [87]. Similar approaches can be applied to other immune cell types, with results contextualized within the expected healing timeline, as early pro-inflammatory responses often precede later anti-inflammatory phases in normal wound healing.
Activation Assays: Profiling Functional Immune Responses
Cytokine and Chemokine Analysis
Activation assays measure functional immune responses through soluble mediator release, providing insight into the inflammatory environment induced by biomaterials. These analyses represent the most extensively studied aspect of in vitro immunogenicity due to their direct relevance to functional outcomes [87].
ELISA-Based Protocols offer specific, quantitative measurement of individual cytokines:
- Procedure: Collect conditioned media from immune cell-biomaterial cultures at appropriate timepoints (e.g., 6, 24, 48, 72 hours). Centrifuge to remove cells and debris. Store at -80°C until analysis.
- Assay Execution: Follow manufacturer instructions for specific cytokine ELISA kits. Typically involves coating plates with capture antibody, blocking, adding samples and standards, detecting with biotinylated detection antibody, streptavidin-HRP, and TMB substrate. Measure absorbance and calculate concentrations from standard curves.
- Key Analytes: Include pro-inflammatory cytokines (IL-1β, IL-6, TNF-α, IL-12), anti-inflammatory cytokines (IL-10, IL-1ra, TGF-β), and chemokines (IL-8, MCP-1, MIP-1α) that recruit specific immune cell populations [87].
Multiplex Immunoassays enable high-throughput analysis of multiple analytes simultaneously:
- Luminex/xMAP Technology: Use magnetic or polystyrene beads conjugated with capture antibodies for multiple targets. Incubate with samples, then detection antibodies, and analyze using flow-based instrumentation.
- Advantages: Conserve sample volume, measure dozens of analytes simultaneously, broader dynamic range than traditional ELISA.
- Considerations: Require specialized equipment, potential cross-reactivity between analytes, higher cost per sample [87].
Gene Expression Analysis
Gene expression profiling provides early detection of immune activation and insight into underlying signaling pathways, often preceding protein secretion.
qPCR Protocols for quantitative assessment of immune-related gene expression:
- RNA Extraction: Homogenize cells exposed to biomaterials using appropriate RNA isolation methods. Assess RNA quality and quantity using spectrophotometry or microfluidics.
- cDNA Synthesis: Reverse transcribe 0.5-1μg RNA using reverse transcriptase with random hexamers or oligo-dT primers.
- qPCR Analysis: Prepare reactions with gene-specific primers, cDNA template, and SYBR Green or TaqMan chemistry. Run on real-time PCR instrument using appropriate cycling conditions. Normalize to housekeeping genes (GAPDH, β-actin, HPRT) and calculate fold-change using ΔΔCt method [87].
RNA Sequencing provides comprehensive, unbiased profiling of immune activation:
- Protocol: Extract high-quality RNA (RIN > 8) from immune cells exposed to biomaterials. Prepare libraries using poly-A selection or rRNA depletion. Sequence on appropriate platform (Illumina, etc.).
- Bioinformatic Analysis: Process data through quality control, alignment, quantification, and differential expression analysis. Use pathway analysis tools (GSEA, IPA) to identify enriched immune pathways [88] [89].
- Application: As demonstrated in a 2024 study, RNA sequencing can reveal differential expression of immune-related genes and signaling pathways (e.g., FGFR4, Rap1 pathway) in response to biomaterials or immunomodulatory agents [88].
Signaling Pathway Activity Profiling
Recent advances enable quantitative assessment of signal transduction pathway activity in immune cells, providing functional insight into immune activation states:
STAP-STP Technology simultaneously measures multiple signaling pathways using transcriptomic data:
- Principle: Bayesian network-based computational models calculate pathway activity from mRNA levels of high-evidence direct target genes for each pathway [89].
- Pathways Measured: PI3K-FOXO, MAPK, NFκB, TGFβ, Notch, JAK-STAT1/2, JAK-STAT3, estrogen receptor (ER), and androgen receptor (AR) pathways [89].
- Output: Pathway Activity Score (PAS) on log2odds scale that quantitatively reflects pathway activity [89].
- Application: Each immune cell type demonstrates characteristic Signal Transduction Pathway Activity Profiles (SAPs) in resting and activated states, enabling quantitative assessment of biomaterial effects on immune cell functional state [89].
The following diagram illustrates the key signaling pathways involved in immune cell activation and their interconnections:
Advanced Model Systems: From 2D to 3D and Co-culture Approaches
Advanced In Vitro Models
Traditional 2D monoculture systems provide limited physiological relevance, driving development of advanced models that better recapitulate in vivo immune responses:
PBMC-Based Models utilize primary human immune cells for clinically relevant screening:
- Isolation Protocol: Collect peripheral blood from healthy donors in heparinized tubes. Dilute blood 1:1 with PBS. Carefully layer over Ficoll-Paque density gradient medium. Centrifuge at 400-500 × g for 30-40 minutes at room temperature with brake off. Collect PBMC layer at interface, wash twice with PBS, and resuspend in appropriate culture medium [88].
- Cryopreservation: Freeze PBMCs in freezing medium (90% FBS, 10% DMSO) using controlled-rate freezing. Store in liquid nitrogen vapor phase for long-term preservation [88].
- Application: Culture PBMCs with biomaterial extracts or on material surfaces. Assess responses using aforementioned viability, maturation, and activation assays.
3D Co-culture Models incorporate multiple cell types to simulate tissue-level interactions:
- Immune Cell-Stromal Cell Co-cultures: Seed immune cells (PBMCs, macrophages) with relevant stromal cells (fibroblasts, mesenchymal stem cells) in 3D scaffolds or hydrogels. Assess bidirectional signaling and paracrine effects.
- Transwell Systems: Culture immune cells and tissue-specific cells in separate compartments sharing soluble mediators. Useful for studying recruitment and cross-talk.
- Organ-on-a-Chip Platforms: Microfluidic systems that simulate tissue-tissue interfaces and mechanical cues. For example, Calu-3 lung epithelial cells with PBMCs in a 3D model have been used to assess immunogenic factors [88].
Integrated Workflow for Comprehensive Assessment
A comprehensive immune response assessment integrates multiple assay types in a logical workflow that progresses from simple screening to mechanistic investigation:
The Researcher's Toolkit: Essential Reagents and Materials
Successful implementation of in vitro immune response assessment requires specific reagents, cell models, and technical resources. The following table summarizes key components of the immune assessment toolkit:
Table 4: Essential Research Reagent Solutions for Immune Response Assessment
| Category | Specific Items | Function/Application | Examples/Specifications |
|---|---|---|---|
| Cell Models | Primary human PBMCs | Physiologically relevant screening | Isolated from healthy donors, multiple donors recommended |
| THP-1 monocyte cell line | Standardized macrophage model | PMA differentiation to macrophages | |
| Primary macrophages | Tissue-relevant assessment | Monocyte-derived, peritoneal, splenic | |
| HDMB, Jurkat, NK-92 | Specific lymphocyte responses | Various immortalized lines | |
| Assessment Reagents | Flow cytometry antibodies | Surface marker analysis | CD86, CCR7, CD163, CD206, CD markers |
| ELISA kits | Cytokine quantification | IL-1β, IL-6, TNF-α, IL-10, TGF-β | |
| qPCR reagents | Gene expression analysis | Immune-related primers, SYBR Green | |
| Metabolic assay kits | Viability assessment | alamarBlue, MTT, WST-8 | |
| Culture Supplements | Polarization cytokines | Direction of cell differentiation | IFN-γ + LPS (M1), IL-4 (M2) |
| Differentiation factors | Cell maturation | M-CSF (macrophages) | |
| Serum alternatives | Defined culture conditions | Reduce batch-to-batch variability | |
| Technical Resources | Flow cytometer | Multiparameter cell analysis | ≥8 colors recommended |
| ELISA plate reader | Absorbance measurement | With shaking and temperature control | |
| qPCR instrument | Gene expression quantification | 96-well or 384-well format | |
| Microscopy systems | Cell imaging | Fluorescence, confocal capabilities |
Comprehensive in vitro immune response assessment through integrated viability, maturation, and activation assays provides critical predictive data for biomaterial development and safety evaluation. By employing these methodologies early in the development pipeline, researchers can identify potentially immunogenic materials before advancing to costly animal studies and clinical trials, simultaneously reducing ethical concerns and improving clinical success rates [87].
The future of biomaterial immune compatibility assessment lies in developing increasingly sophisticated models that better recapitulate human physiology, including patient-specific immune cells, complex 3D microenvironments, and multi-tissue interfaces [88] [39]. Additionally, advanced analytical approaches such as signaling pathway activity profiling and multi-omics integration will provide deeper mechanistic insight into immune-material interactions [89]. By embracing these comprehensive assessment strategies, the field can progress toward truly immune-informed biomaterial design that maximizes therapeutic success while minimizing adverse reactions.
Single-cell RNA sequencing (scRNA-seq) has emerged as a transformative technology for dissecting the cellular heterogeneity and functional dynamics of immune microenvironments, particularly in the context of biomaterial-host interactions. This technical guide provides an in-depth examination of scRNA-seq methodologies, analytical frameworks, and applications for deconvoluting complex immune cell populations and their communication networks. We detail experimental protocols from sample preparation to computational analysis, emphasizing how this high-resolution approach reveals cellular diversity, stromal-immune interactions, and spatial niches that drive immune responses. The integration of scRNA-seq with spatial transcriptomics and trajectory inference algorithms further enables the reconstruction of cellular dynamics in response to biomaterial implantation. This whitepaper serves as a comprehensive resource for researchers and drug development professionals seeking to leverage single-cell technologies to advance understanding of immune microenvironment regulation and therapeutic targeting.
The immune microenvironment represents a highly dynamic and heterogeneous ecosystem composed of diverse cell types including various immune cell populations, stromal cells, and potentially foreign materials or biomaterials. Traditional bulk RNA sequencing approaches average gene expression across thousands of cells, obscuring critical cell-to-cell variations and rare but functionally important immune cell subpopulations [90]. Single-cell RNA sequencing (scRNA-seq) overcomes this limitation by enabling high-resolution profiling of gene expression at the individual cell level, making it particularly suited for characterizing the complex cellular landscape of immune environments [91].
In the specific context of biomaterial-host interactions, scRNA-seq provides unprecedented insights into how immune cells respond to implanted materials, differentiate into specialized subsets, and coordinate inflammatory and regenerative processes. The technology has revealed remarkable heterogeneity within immune cell populations that was previously unappreciated, including distinct macrophage activation states, T cell differentiation trajectories, and rare dendritic cell subsets that play pivotal roles in determining biomaterial integration versus rejection [92]. By capturing transcriptomic profiles of individual cells, researchers can identify novel immune cell subtypes, trace lineage relationships, and characterize transitional states that emerge during immune responses to biomaterials.
The analytical power of scRNA-seq is further enhanced through integration with complementary spatial transcriptomics approaches, which preserve the architectural context of immune cells within tissues [90]. This combination is particularly valuable for understanding how spatial organization influences immune function in biomaterial settings, revealing localized niches of immune activation and cell-cell communication networks that drive host responses. This technical guide will explore the methodologies, applications, and analytical frameworks for harnessing scRNA-seq to deconvolve immune microenvironments in biomaterial and therapeutic contexts.
Technological Foundations and Methodological Approaches
Core Principles of Single-Cell RNA Sequencing
Single-cell RNA sequencing technologies enable comprehensive transcriptomic profiling of individual cells through a multi-step process that begins with tissue dissociation and single-cell isolation, followed by cell lysis, reverse transcription, cDNA amplification, library preparation, and high-throughput sequencing [91]. Unlike bulk RNA-seq which measures average gene expression across cell populations, scRNA-seq captures the transcriptional heterogeneity within seemingly homogeneous cell populations, revealing distinct cell states, rare cell types, and continuous transitional processes that are critical for understanding immune responses [91].
The key technological advantage of scRNA-seq lies in its ability to resolve cellular diversity without prior knowledge of cell-type-specific markers, making it particularly powerful for discovering novel immune cell subsets and characterizing their functional states in response to biomaterials. Current scRNA-seq platforms employ various strategies for single-cell capture, including droplet-based systems (e.g., 10X Genomics), microwell plates (e.g., SMART-Seq), and combinatorial indexing approaches (e.g., sci-RNA-seq) [92]. Each method offers different trade-offs between throughput, sensitivity, and cost, requiring researchers to select appropriate platforms based on their specific research questions about immune microenvironments.
Essential Experimental Workflow
The standard workflow for scRNA-seq analysis of immune microenvironments involves multiple critical steps that must be carefully optimized to ensure data quality and biological relevance:
Sample Preparation and Cell Isolation: Fresh tissue samples containing the immune microenvironment of interest are dissociated into single-cell suspensions using enzymatic and mechanical methods optimized to preserve RNA integrity and maintain cell viability. For immune cells, which can be particularly sensitive to dissociation stress, protocol optimization is essential to minimize artifactual stress responses [92].
Quality Control and Cell Viability Assessment: The single-cell suspension is evaluated for viability, concentration, and potential debris using automated cell counters or flow cytometry. High viability (>90%) is typically required to ensure successful capture of viable single cells and minimize background RNA from dead cells.
Single-Cell Partitioning and Barcoding: Cells are partitioned into individual reactions using microfluidic devices or droplet-based systems where each cell is combined with a uniquely barcoded bead. These barcodes enable subsequent computational attribution of sequenced reads to their cell of origin [91].
Reverse Transcription and cDNA Amplification: Within each partition, cells are lysed and mRNA transcripts are reverse-transcribed into cDNA with incorporation of cell barcodes and unique molecular identifiers (UMIs) to correct for amplification biases and enable digital quantitation of transcript abundance [92].
Library Preparation and Sequencing: The barcoded cDNA is pooled, amplified, and prepared for sequencing using standard next-generation sequencing library protocols. Sequencing depth typically targets 20,000-100,000 reads per cell to adequately capture the transcriptional diversity of immune cells [92].
Table 1: Key Quality Control Metrics in scRNA-seq Experiments
| Quality Parameter | Target Value | Purpose |
|---|---|---|
| Cell Viability | >90% | Minimizes ambient RNA from dead cells |
| Median Genes per Cell | 1,000-3,000 | Ensures sufficient transcript capture |
| Mitochondrial RNA % | <20% | Excludes stressed/dying cells |
| Sequencing Saturation | >70% | Indicates comprehensive transcript capture |
| Median UMI Counts per Cell | 5,000-30,000 | Reflects adequate sequencing depth |
- Bioinformatic Processing and Quality Control: Raw sequencing data is demultiplexed, aligned to a reference genome, and processed through quality control filters. Cells with low unique gene counts, high mitochondrial content (indicating apoptosis or stress), or outlier UMI distributions are removed from subsequent analysis [92]. In a typical high-quality experiment, approximately 80% of initially captured cells pass these quality filters, with median gene counts around 1,800-2,500 genes per cell and median UMI counts of 5,000-30,000 per cell [92].
Research Reagent Solutions for scRNA-seq
Table 2: Essential Research Reagents for scRNA-seq of Immune Microenvironments
| Reagent/Category | Function | Examples |
|---|---|---|
| Tissue Dissociation Kits | Gentle enzymatic degradation of extracellular matrix | Multi-tissue dissociation kits with collagenase, dispase |
| Cell Viability Stains | Discrimination of live/dead cells | Propidium iodide, DAPI, 7-AAD |
| Single-Cell Partitioning Reagents | Microfluidic emulsion generation | 10X Genomics Single Cell reagents, Drop-seq kits |
| Reverse Transcription Master Mix | cDNA synthesis with template switching | SMARTScribe Reverse Transcriptase |
| PCR Amplification Kits | Whole transcriptome amplification | KAPA HiFi HotStart ReadyMix |
| Library Preparation Kits | Sequencing library construction | Illumina Nextera XT |
| Cell Surface Protein Labels | Multiplexed protein detection with transcriptome | CITE-seq antibodies, TotalSeq reagents |
| Cell Hashing Reagents | Sample multiplexing and doublet detection | MULTI-seq lipid-modified oligos |
Analytical Frameworks for Immune Microenvironment Deconvolution
Computational Pipelines and Cell Type Identification
The analysis of scRNA-seq data from immune microenvironments requires specialized computational approaches to transform raw sequencing data into biological insights. The standard analytical workflow begins with quality control, normalization, and batch correction using tools such as Seurat or Scanpy [92]. Following preprocessing, dimensionality reduction techniques including principal component analysis (PCA) and uniform manifold approximation and projection (UMAP) are applied to visualize cellular relationships in two-dimensional space.
Cell type identification represents a critical step in deconvolving immune microenvironments and typically involves both unsupervised clustering and reference-based annotation approaches. Unsupervised clustering algorithms (e.g., Louvain, Leiden) group cells based on transcriptional similarity, after which cluster identity is determined by evaluating expression of canonical marker genes for known immune cell types (e.g., CD3E for T cells, CD19 for B cells, FCGR3A for NK cells, CD14 for monocytes) [90]. Reference-based approaches leverage previously annotated single-cell atlases to automatically transfer labels to new datasets, improving consistency across studies.
For immune microenvironments in particular, special attention must be paid to transitional states and activation subtypes that may not align neatly with discrete cell type categories. Tools such as SingleR and scType have been developed specifically for fine-grained immune cell classification, leveraging comprehensive immune reference profiles to distinguish closely related subsets such as memory T cell populations, macrophage polarization states, and dendritic cell subtypes [92].
Trajectory Inference and Cellular Dynamics
Trajectory inference algorithms represent a powerful analytical framework for reconstructing dynamic processes within immune microenvironments, such as immune cell differentiation, activation, or response to biomaterials over time. These methods order cells along pseudotemporal trajectories based on transcriptional similarity, inferring the underlying sequence of state transitions without requiring time-series sampling [93].
The Genes2Genes (G2G) framework represents a recent advancement in trajectory analysis, employing a Bayesian information-theoretic dynamic programming approach to align single-cell trajectories between different conditions (e.g., different biomaterials, disease states, or time points) [93]. Unlike earlier methods such as dynamic time warping (DTW) that assume all time points must match between reference and query trajectories, G2G jointly handles both matches and mismatches, enabling identification of divergent transcriptional programs and unobserved cell states between conditions.
In the context of biomaterial-immune interactions, trajectory alignment can reveal how in vitro differentiation systems diverge from in vivo development, guiding the optimization of biomaterial design to recapitulate desired immune responses [93]. For example, G2G analysis has identified missing TNF signaling components in in vitro-derived T cells compared to their in vivo counterparts, pinpointing specific pathways that could be targeted to improve biomaterial compatibility [93].
Cell-Cell Communication Analysis
Understanding how immune cells communicate with each other and with stromal or tissue-resident cells represents a crucial aspect of deconvolving immune microenvironments. Computational methods such as CellChat and NicheNet leverage curated databases of ligand-receptor interactions to infer cell-cell communication networks from scRNA-seq data [92]. These tools identify significantly overexpressed ligand-receptor pairs between cell populations and model the probability of communication events based on expression patterns.
In giant cell tumor of bone (GCTB) research, CellChat analysis revealed that the SPP1 signaling pathway functions as a positive feedback loop between cancer-associated fibroblasts and macrophages, illustrating how scRNA-seq can uncover critical communication axes in complex microenvironments [92]. Similar approaches applied to biomaterial-immune interactions can identify key signaling pathways that drive favorable (e.g., regenerative) versus unfavorable (e.g., fibrotic) responses, informing the rational design of immunomodulatory biomaterials.
Table 3: Key Analytical Tools for scRNA-seq Data from Immune Microenvironments
| Tool Category | Representative Tools | Application in Immune Analysis |
|---|---|---|
| Quality Control | FastQC, CellRanger | Sequencing quality assessment, read alignment |
| Normalization & Batch Correction | sctransform, Harmony | Technical artifact removal, data integration |
| Dimensionality Reduction | UMAP, t-SNE, PCA | Visualization of cellular relationships |
| Clustering | Leiden, Louvain | Identification of cell populations and subtypes |
| Differential Expression | MAST, DESingle2, Wilcoxon test | Marker gene identification, condition-specific changes |
| Trajectory Inference | Monocle3, Slingshot, Genes2Genes | Reconstruction of differentiation paths and dynamics |
| Cell-Cell Communication | CellChat, NicheNet, ICELLNET | Inference of signaling networks between cell types |
Integration with Spatial Transcriptomics and Multi-omics Approaches
Complementary Spatial Context
A significant limitation of conventional scRNA-seq is the loss of spatial information during tissue dissociation, which is particularly critical for understanding immune microenvironments where cellular localization and neighborhood relationships directly influence function [90]. Spatial transcriptomics (ST) technologies address this limitation by mapping gene expression within intact tissue sections, preserving the architectural context of immune cells [90]. These approaches can be broadly categorized into image-based methods (e.g., MERFISH, seqFISH) that use sequential fluorescence in situ hybridization to detect RNA molecules, and barcode-based methods (e.g., 10X Visium, Slide-seq) that capture RNA onto spatially indexed oligonucleotide arrays [90].
The integration of scRNA-seq with spatial transcriptomics creates a powerful synergistic framework for immune microenvironment analysis. While scRNA-seq provides comprehensive characterization of cellular diversity and transcriptional states, ST maps these populations back to their native tissue contexts, revealing spatially organized niches such as immune cell aggregates, barrier structures, and gradient patterns of immune activation [90]. Computational integration methods including deconvolution approaches and multimodal intersection analysis (MIA) enable the mapping of scRNA-seq-defined cell types onto spatial coordinates, bridging cellular identity with localization [90].
In pancreatic ductal adenocarcinoma, MIA integration of scRNA-seq and ST data revealed that stress-associated cancer cells specifically colocalize with inflammatory fibroblasts that produce interleukin-6 (IL-6), uncovering a spatially organized tumor-stroma crosstalk mechanism [90]. Similar approaches applied to biomaterial interfaces could reveal how immune cells organize around implant surfaces and identify localized signaling hotspots that dictate overall host response.
Multi-omics Extensions
Beyond transcriptomics, the single-cell toolbox has expanded to include multi-omics approaches that simultaneously profile multiple molecular layers from the same cells. Technologies such as CITE-seq (Cellular Indexing of Transcriptomes and Epitopes by Sequencing) enable coupled measurement of RNA expression and surface protein abundance, providing particularly valuable information for immune cell characterization where protein markers are well-established and often critical for defining functional subsets [90]. Similarly, scATAC-seq (single-cell Assay for Transposase-Accessible Chromatin with sequencing) profiles chromatin accessibility, revealing the regulatory landscape that governs immune cell identity and function.
The integration of these multi-omics modalities with scRNA-seq creates a more comprehensive view of immune cell states in response to biomaterials. For example, paired RNA and protein measurement can identify discordances between transcriptional and translational regulation, while combined gene expression and chromatin accessibility profiling can distinguish immediate transcriptional responses from stable cell fate decisions. These insights are particularly valuable for understanding the progression from acute inflammatory responses to chronic adaptation at biomaterial interfaces.
Applications in Biomaterial Host Interactions and Immune Response Research
Characterizing Host Responses to Biomaterials
The application of scRNA-seq to biomaterial host interactions has revolutionized our understanding of how immune systems perceive and respond to implanted materials. By profiling the entire immune landscape rather than predetermined cell subsets, scRNA-seq enables unbiased discovery of novel response patterns and cellular participants in the foreign body reaction. Studies applying these approaches have revealed unexpected heterogeneity in macrophage responses to biomaterials, identifying distinct functional subsets beyond the classical M1/M2 dichotomy that play specific roles in material integration versus encapsulation [90].
In the context of bone regeneration biomaterials, scRNA-seq analysis of healing interfaces has identified specific macrophage and dendritic cell subsets that correlate with successful osteogenesis, suggesting potential immunomodulatory targets to enhance bone regeneration [92]. Similarly, analysis of synthetic graft interfaces has revealed coordinated responses between innate and adaptive immune cells that determine long-term material fate, challenging the historical focus on macrophages alone in foreign body responses.
Identifying Therapeutic Targets and Biomarkers
The high-resolution cellular and molecular insights provided by scRNA-seq facilitate the identification of novel therapeutic targets to modulate immune responses to biomaterials. By comparing successful versus failing implants at single-cell resolution, researchers can identify specific cell populations, signaling pathways, and regulatory networks that associate with favorable outcomes, providing a rational basis for targeted intervention strategies [92].
In giant cell tumor of bone research, scRNA-seq analysis identified the SPP1 signaling pathway as a critical communication axis between cancer-associated fibroblasts and macrophages, revealing a potential therapeutic target for disrupting this tumor-promoting interaction [92]. Similar approaches applied to biomaterial fibrosis could identify targetable pathways that drive collagen deposition and material encapsulation, enabling the development of next-generation biomaterials that actively steer immune responses toward regenerative rather than fibrotic outcomes.
Beyond therapeutic targets, scRNA-seq signatures can also serve as sensitive biomarkers for predicting and monitoring host responses to biomaterials. Specific immune cell abundance ratios, activation states, or transcriptional modules identified through scRNA-seq analysis may provide early indicators of impending material failure or successful integration, enabling clinical monitoring and personalized intervention strategies.
Single-cell RNA sequencing has fundamentally transformed our ability to deconvolve complex immune microenvironments, providing unprecedented resolution into cellular heterogeneity, dynamic processes, and communication networks that underlie host responses to biomaterials. The analytical frameworks and methodologies detailed in this technical guide empower researchers to move beyond population-level averaging and uncover the precise cellular and molecular mechanisms that determine the success or failure of biomedical implants and regenerative therapies.
As single-cell technologies continue to evolve, several emerging trends promise to further enhance their utility in biomaterial and immune response research. Spatial multi-omics approaches that simultaneously profile gene expression, protein localization, and chromatin accessibility in intact tissues will provide increasingly comprehensive views of immune responses in their native architectural context [90]. Computational methods for trajectory alignment and comparison, such as the Genes2Genes framework, will enable more precise characterization of how in vitro models diverge from in vivo biology, guiding the refinement of preclinical testing systems [93]. Meanwhile, ongoing efforts to reduce costs and simplify workflows will broaden accessibility of these powerful technologies across the biomaterials research community.
The integration of scRNA-seq-derived insights with biomaterial design represents a promising frontier for creating next-generation implants that actively steer immune responses toward therapeutic outcomes. By identifying the key cellular players and molecular pathways that distinguish regenerative from fibrotic responses, researchers can increasingly employ rational design principles to develop immunomodulatory materials that harness rather than fight the immune system. As these approaches mature, scRNA-seq will continue to serve as an essential tool for understanding and engineering the immune microenvironment in the context of biomaterial host interactions.
Advanced proteomic technologies now enable researchers to decipher the complex molecular cascades that determine the success of biomaterial-based therapies. This technical guide details how comparative proteomic analysis identifies key temporal pathways governing regenerative versus fibrotic healing outcomes. By characterizing host responses to diverse biomaterials across inflammatory, proliferative, and resolution phases, researchers can pinpoint specific immune activation patterns, extracellular matrix organization processes, and tissue development pathways that predict therapeutic success. This whitepaper provides experimental methodologies for proteomic profiling, data visualization techniques, and analytical frameworks essential for researchers and drug development professionals working at the intersection of biomaterial design and immune-informed therapeutic strategies.
The host immune response to implanted biomaterials represents a critical determinant of therapeutic success in tissue engineering and regenerative medicine. While biomaterials are deployed clinically to enhance wound closure rates and quality of healed tissue, their precise mechanisms of action remain incompletely understood. Proteomic profiling has emerged as a powerful methodology for characterizing the dynamic molecular events that unfold at the biomaterial-host interface. This approach enables researchers to move beyond descriptive phenomenology toward mechanistic understanding of how material properties influence downstream healing trajectories.
Within the context of biomaterial host interactions, proteomic analysis reveals how immune cell recruitment and polarization patterns direct tissue regeneration toward either functional restoration or fibrotic scarring. The wound healing cascade is characterized by the steady progression of distinct yet overlapping stages—inflammation, proliferation, and resolution—each characterized by specific protein signatures and pathway activations. By applying comparative proteomic approaches to different biomaterial formulations, researchers can identify the key temporal pathways that differentiate regenerative outcomes from fibrotic ones, ultimately informing the rational design of next-generation immunomodulatory materials.
Experimental Design for Comparative Proteomic Analysis
Biomaterial Selection and Study Timeline
Rigorous experimental design begins with selecting biomaterials that elicit distinct healing responses. A foundational approach utilizes three material types: a clinically employed collagen hydrogel (control), a fibrosis-suppressing synthetic material, and an adaptive immunity-activating biomaterial [94]. This selection enables direct comparison of protein expression patterns associated with different healing outcomes.
The study timeline must encompass critical phases of wound healing, with sample collection at timepoints representing inflammatory (days 1-3), proliferative (days 4-7), and resolution (days 8-14) phases [94]. This temporal design captures the dynamic evolution of protein signatures rather than single timepoint snapshots, enabling researchers to identify both instantaneous responses and cascading pathway activations.
Table 1: Key Biomaterial Classes for Comparative Proteomic Studies
| Biomaterial Class | Key Characteristics | Expected Healing Outcome | Proteomic Sampling Points |
|---|---|---|---|
| Collagen Hydrogel | Clinically used reference material | Standard wound closure with mixed outcomes | Days 1, 3, 7, 14 |
| Fibrosis-Suppressing Material | Modified surface properties or composition | Reduced scar formation, improved tissue architecture | Days 1, 3, 7, 14, 21 |
| Adaptive Immunity-Activating Material | Engineered to engage T-cell responses | Enhanced regeneration through immune activation | Days 1, 2, 5, 10, 21 |
Sample Preparation and Protein Quantification
Proper sample preparation is critical for obtaining meaningful proteomic data. Tissue samples surrounding the biomaterial implant should be harvested with precise spatial demarcation (e.g., 0-2mm from material interface). Protein extraction should utilize appropriate lysis buffers compatible with subsequent mass spectrometry analysis, typically containing urea, thiourea, or commercial detergent-based formulations. Protein quantification should be performed using methods compatible with detergent-containing samples, such as bicinchoninic acid (BCA) assay, with normalization across all samples prior to processing.
For comprehensive proteome coverage, a combination of enzymatic digests (typically trypsin) and fractionation techniques (strong cation exchange chromatography, high pH reversed-phase separation) is recommended. These methods reduce sample complexity and enhance protein identification rates. Recent advances in sample preparation include tandem mass tag (TMT) labeling for multiplexed quantitative comparisons across multiple conditions and timepoints within a single MS run, thereby reducing technical variability [95].
Proteomic Workflow and Data Acquisition
The analytical workflow for proteomic profiling of biomaterial-mediated healing involves coordinated sample processing, instrumental analysis, and bioinformatic processing. The following diagram illustrates the integrated workflow:
Mass Spectrometry-Based Proteomic Analysis
Liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) represents the cornerstone technology for large-scale protein identification and quantification. High-resolution mass spectrometers such as Orbitrap instruments provide the analytical performance necessary to resolve complex protein mixtures from wound tissue samples. Data-dependent acquisition (DDA) methods remain widely used for discovery proteomics, while data-independent acquisition (DIA) approaches offer enhanced reproducibility and quantitative precision.
For biomarker discovery and pathway analysis, studies should aim to quantify a minimum of 5000 proteins across the experimental groups to ensure sufficient coverage of relevant biological pathways [94]. Analytical replicates (minimum n=3 per condition) are essential for statistical robustness, with quality control measures including correlation analysis between replicates and monitoring of missing data patterns. Advanced quantitative approaches such as isobaric labeling (TMT, iTRAQ) enable multiplexed analysis of up to 16 samples simultaneously, reducing instrumental run time and technical variability [95].
Data Processing and Protein Identification
Raw mass spectrometry data requires specialized computational processing for protein identification and quantification. Search engines such as MaxQuant, Proteome Discoverer, or OpenMS match experimental spectra to theoretical spectra derived from protein sequence databases. Search parameters should account for specific digestion enzymes, potential modifications (e.g., carbamidomethylation as fixed modification, oxidation as variable modification), and mass tolerances appropriate to the instrument used.
Following database searching, results must be processed to ensure data quality. This includes filtering based on false discovery rates (typically ≤1% at both peptide and protein levels), requiring a minimum number of unique peptides per protein identification, and assessing quantitative data completeness across sample groups. Normalization strategies such as median centering or quantile normalization correct for systematic technical variation, while imputation methods carefully address missing values without introducing bias.
Bioinformatic Analysis of Proteomic Data
Pathway and Gene Ontology Analysis
Bioinformatic analysis transforms protein lists into biological insights through pathway enrichment and gene ontology (GO) analysis. Statistical approaches such as overrepresentation analysis or gene set enrichment analysis (GSEA) identify biological processes, molecular functions, and cellular compartments that are significantly altered in response to different biomaterials. As demonstrated in comparative studies, this analysis reveals how distinct biomaterials enrich specific GO terms throughout healing phases—from immune-related pathways in collagen hydrogels to epidermis development pathways in fibrosis-suppressing materials [94].
Temporal analysis of pathway activation provides particularly valuable insights. For example, adaptive immunity-activating biomaterials show early enrichment of broad immunity and inflammation GO terms, followed later by keratinization, muscle system, and lipid oxidation pathways [94]. These temporal patterns highlight the dynamic immune reprogramming capabilities of advanced biomaterials and their influence on the transition from inflammatory to regenerative phases.
Table 2: Key Pathways Differentially Activated by Biomaterial Type
| Healing Phase | Collagen Hydrogel | Fibrosis-Suppressing Material | Adaptive Immunity-Activating Material |
|---|---|---|---|
| Inflammation (Early) | Immune cell activation, Acute inflammatory response | Reduced pro-inflammatory signaling | Broad immunity, T-cell activation, Antigen presentation |
| Proliferation (Mid) | Continued immune enrichment, ECM organization | Epidermis development, Collagen synthesis, Collagen fibril organization | Metabolic reprogramming, Oxidative processes |
| Resolution (Late) | Incomplete resolution, Mixed ECM deposition | Organized ECM assembly, Reduced fibrotic markers | Keratinization, Muscle system processes, Lipid oxidation |
Data Visualization for Proteomics
Effective data visualization is essential for interpreting complex proteomic datasets and communicating findings. The R software environment with Bioconductor packages provides specialized tools for proteomics data visualization [95]. Key visualization approaches include:
- MA plots for quality control and assessment of differential protein expression, displaying the relationship between log2 fold-change and average expression intensity between experimental conditions [95]
- Volcano plots for visualizing the relationship between statistical significance (p-value) and magnitude of change (fold-change)
- Heatmaps with hierarchical clustering to reveal patterns in protein expression across multiple conditions and timepoints
- Protein-protein interaction networks to identify functional modules and hubs in the molecular response
The following diagram illustrates the primary bioinformatic workflow for pathway identification from raw proteomic data:
Advanced visualization techniques implemented in R and Bioconductor, such as those in the RforProteomics package, enable researchers to create publication-quality figures that effectively communicate complex data relationships [95]. The grammar of graphics implementation in ggplot2 facilitates layered construction of sophisticated visualizations with precise control over aesthetic attributes.
Key Pathways Governing Regenerative Outcomes
Proteomic analyses consistently identify several critical pathway categories that differentiate regenerative from fibrotic responses to biomaterial implantation.
Immune Modulation Pathways
The immune response to biomaterials represents a decisive factor in healing outcomes. Proteomic studies reveal that materials promoting regeneration typically modulate innate immune activation toward anti-inflammatory, pro-regenerative phenotypes while simultaneously engaging specific adaptive immunity components [39]. Specifically, regenerative biomaterials promote M2-like macrophage polarization, regulatory T-cell recruitment, and resolution of neutrophilic inflammation. In contrast, fibrotic responses are characterized by persistent M1-like macrophage signatures, excessive neutrophil extracellular trap formation, and Th17-driven inflammation.
Materials engineered to activate adaptive immunity demonstrate particularly interesting immune profiles, with early enrichment of antigen presentation pathways followed by coordinated T-cell and B-cell responses that appear to support tissue regeneration rather than rejection [96]. This challenges the traditional paradigm that adaptive immune activation universally undermines biomaterial integration and suggests instead that specific immune engagement can be harnessed for therapeutic benefit.
Extracellular Matrix Organization Pathways
The composition, structure, and mechanical properties of newly deposited extracellular matrix (ECM) fundamentally influence functional tissue restoration. Proteomic analyses reveal that regenerative outcomes are associated with balanced collagen synthesis (particularly types I and III in appropriate ratios), efficient collagen fibril organization, and elevated elastin deposition [94]. In contrast, fibrotic responses show dysregulated collagen crosslinking, excessive collagen deposition, and reduced elastin content.
Materials that suppress fibrosis consistently upregulate pathways involved in ECM degradation and remodeling, including matrix metalloproteinases (MMPs 2, 9, 14) and their tissue inhibitors (TIMPs) in balanced ratios. This proteolytic activity facilitates constructive tissue remodeling rather than scar formation. Additionally, regenerative materials enrich pathways associated with matrisome proteins such as fibronectin, fibrillins, and matricellular proteins that orchestrate cell-ECM interactions supporting functional tissue restoration.
Metabolic Reprogramming Pathways
Emerging evidence from proteomic studies indicates that successful tissue regeneration requires specific metabolic reprogramming at the implant site. Regenerative biomaterials activate oxidative metabolic pathways including fatty acid oxidation, mitochondrial biogenesis, and electron transport chain components [94]. This metabolic signature supports the energy-intensive process of tissue regeneration and appears linked to anti-inflammatory immune phenotypes.
In contrast, fibrotic environments display enhanced glycolytic metabolism and pentose phosphate pathway activation, mirroring the metabolic profile of pro-inflammatory immune cells. The ability of biomaterials to influence this metabolic switch represents a crucial determinant of healing outcomes, with materials promoting oxidative metabolism associated with superior functional recovery and reduced scar formation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful proteomic profiling of biomaterial-mediated healing requires specialized reagents and analytical tools. The following table details essential resources for conducting these studies:
Table 3: Essential Research Reagents and Materials for Proteomic Profiling of Biomaterial-Mediated Healing
| Category | Specific Reagents/Materials | Function/Application | Technical Notes |
|---|---|---|---|
| Biomaterial Models | Collagen hydrogels, MAP scaffolds, Silicone implants with controlled surface topography [94] [39] | Provide standardized platforms for comparing host responses | Surface microtopography (e.g., 4μm roughness) significantly influences immune response and fibrosis [39] |
| Protein Separation | Trypsin/Lys-C mixture for digestion, TMTpro 16-plex kits, High-pH reversed-phase fractionation columns | Enable comprehensive protein identification and multiplexed quantification | TMT multiplexing reduces technical variability; 16-plex allows extensive experimental designs [95] |
| Mass Spectrometry | LC-MS/MS systems (Orbitrap platforms), C18 capillary columns, Nanoflow LC systems | Provide high-resolution protein separation and identification | Data-independent acquisition (DIA) methods enhance quantitative reproducibility [95] |
| Data Analysis Software | MaxQuant, Proteome Discoverer, R/Bioconductor packages (RforProteomics, MSnbase) [95] | Process raw MS data, perform statistical analysis, and visualize results | MSnbase provides specialized data containers for quantitative proteomics data [95] |
| Pathway Analysis Tools | Gene ontology databases, KEGG/Reactome pathway resources, STRING database, Cytoscape | Identify biologically relevant patterns in protein expression data | Overrepresentation analysis and GSEA provide complementary insights [94] |
| Validation Reagents | Antibodies for key pathway proteins (HSP60, collagen subtypes, macrophage markers), ELISA kits, Immunohistochemistry reagents | Confirm proteomic findings through orthogonal methods | Spatial validation (e.g., immunohistochemistry) confirms protein localization [39] |
Proteomic profiling provides an unparalleled window into the molecular mechanisms through which biomaterials direct healing toward regenerative versus fibrotic outcomes. By employing the experimental designs, analytical workflows, and bioinformatic approaches outlined in this technical guide, researchers can systematically decipher how material properties influence immune responses, extracellular matrix dynamics, and metabolic pathways throughout the healing cascade. These insights are accelerating the development of precision biomaterials that actively orchestrate regenerative processes through controlled manipulation of host responses, ultimately improving therapeutic outcomes across diverse clinical applications.
This whitepaper provides a comparative evaluation of three prominent classes of biomaterials—silicone implants, ceramics, and natural polymer scaffolds—within the context of biomaterial-host interactions and immune response. Through systematic analysis of mechanical properties, biodegradation behavior, and immunomodulatory effects, we identify material-specific strengths and limitations. Silicone implants offer permanent structural support but trigger foreign body reactions and fibrous encapsulation. Ceramics excel in osseointegration but exhibit limited degradation control, while natural polymers provide superior biocompatibility and bioactive signaling but require mechanical enhancement. This analysis underscores that the host immune response is a pivotal determinant of clinical performance, necessitating material selection based on specific anatomical and immunological requirements.
Biomaterials are engineered to interact with biological systems for a therapeutic purpose, such as replacing, supporting, or enhancing damaged tissues or organs [2] [97]. The clinical success of any implanted biomaterial is fundamentally governed by the host's biological response, a complex interplay involving inflammation, wound healing, foreign body reactions, and fibrous encapsulation [2] [56]. These responses are influenced by the material's physicochemical and biological properties, including its composition, texture, and surface characteristics [2].
This review focuses on a comparative analysis of three distinct biomaterial categories:
- Silicone Implants: Predominantly used as permanent, non-degradable devices for cosmetic and reconstructive surgery (e.g., breast implants) [98].
- Ceramics: Primarily used in hard tissue repair due to their excellent osteoconductivity and mechanical strength, often as biodegradable scaffolds in bone tissue engineering [99] [100].
- Natural Polymer Scaffolds: Derived from biological sources, these biodegradable materials mimic the native extracellular matrix (ECM) and are applied in both soft and hard tissue regeneration [101] [102] [79].
Framed within a broader thesis on biomaterial-host interactions, this paper evaluates these materials based on their performance, the methodologies for their testing, and their specific interplay with the host immune system. A critical understanding of these interactions is essential for developing safer and more effective biomaterial-based therapies [56].
Material Classifications and Applications
Silicone Implants are typically composed of a silicone elastomer shell filled with either silicone gel or saline solution. They are designed as permanent devices for breast augmentation and reconstruction [98]. Their history has been marked by safety concerns, leading to significant regulatory evolution and postmarket surveillance [98].
Ceramic-Based Biomaterials include calcium phosphates (e.g., hydroxyapatite, tricalcium phosphate), bioactive glasses, and glass-ceramics [99] [100]. Traditionally used for bone and dental defects, their application is expanding into soft-tissue engineering. They serve as porous, three-dimensional scaffolds that provide a temporary mechanical environment conducive to new tissue growth [99].
Natural Polymer Scaffolds are derived from proteins (e.g., collagen, silk fibroin, gelatin) or polysaccharides (e.g., chitosan, alginate, hyaluronic acid) [101] [102] [79]. These materials are bioresorbable and are exploited in regenerative medicine for their innate bioactivity and ability to mimic the native ECM, supporting cell adhesion, proliferation, and differentiation [102].
Comparative Performance Data
The following tables summarize key performance metrics for the three biomaterial classes, highlighting their distinct characteristics.
Table 1: Comparative Mechanical Properties and Biodegradability
| Material Class | Typical Mechanical Properties | Degradation Profile | Key Structural Features |
|---|---|---|---|
| Silicone Implants | Permanent, elastic, non-degradable [98] | Non-biodegradable; subject to rupture and wear [98] | Solid shell with smooth or textured surface [98] |
| Ceramics | High compressive strength, brittle [99] [100] | Slow to non-degradable (HA) to bioresorbable (β-TCP) [99] | Porous structure; pore size 300-700 μm ideal for bone ingrowth [100] |
| Natural Polymers | Low mechanical strength, flexible [102] [103] | Biodegradable; rate varies from days to months [102] [79] | Hydrogels, fibrous mats, porous scaffolds; highly tunable [102] |
Table 2: Host Biological Response and Common Complications
| Material Class | Biocompatibility & Immune Response | Most Common Complications | Tissue Integration |
|---|---|---|---|
| Silicone Implants | Biocompatible but triggers foreign body reaction; fibrous capsule formation [98] [2] | Capsular contracture, rupture, seroma, infection, BIA-ALCL [98] | Limited; often separated from tissue by fibrous capsule |
| Ceramics | Highly biocompatible; bioactive (direct bonding to bone) [99] [100] | Brittle fracture, slow/variable degradation rates, poor vascularization in large scaffolds [99] [100] | Excellent osteointegration; promotes direct bone bonding and cell infiltration [100] |
| Natural Polymers | High biocompatibility; can modulate immune response (e.g., promote M2 macrophages) [2] [79] | Rapid degradation, low mechanical strength, potential immunogenicity depending on source [102] [103] | Superior; promotes excellent cell adhesion and tissue in-growth [102] |
Experimental Methodologies for Evaluation
Standardized experimental protocols are crucial for the comparative evaluation of biomaterials. The following section outlines key methodologies cited in the literature.
In Vitro Biocompatibility and Immune Profiling (ISO 10993)
The ISO 10993 standard provides a foundational framework for assessing biomaterial biocompatibility [56]. A typical protocol involves:
- Material Preparation: Sterilize biomaterial samples (e.g., silicone disc, ceramic scaffold, polymer hydrogel) and condition them in cell culture medium.
- Immune Cell Culture: Isolate primary human macrophages or use macrophage cell lines (e.g., THP-1).
- Exposure and Co-culture: Seed immune cells directly onto material samples or treat them with material extracts. Include positive (Lipopolysaccharide, LPS) and negative (culture medium) controls.
- Endpoint Analysis:
- Cytotoxicity: Measure cell viability using MTT or AlamarBlue assays.
- Immune Phenotyping: Use flow cytometry to analyze surface markers for macrophage polarization (e.g., CD86 for M1, CD206 for M2) [2].
- Cytokine Secretion: Quantify pro-inflammatory (e.g., TNF-α, IL-6) and anti-inflammatory (e.g., IL-10) cytokines in the supernatant via ELISA [2].
- Cell Morphology: Visualize cell adhesion and spreading using scanning electron microscopy (SEM) or fluorescence microscopy.
This methodology directly assesses the initial immune response, predicting the material's potential to cause inflammation or foster a pro-regenerative environment [56].
In Vivo Evaluation of Scaffolds for Bone Regeneration
Large animal models are critical for preclinical evaluation of scaffolds, particularly for bone regeneration, as they closely mimic human physiological conditions [100]. A standard protocol is as follows:
- Animal Model and Defect Creation: Utilize a large animal model (e.g., sheep, minipig). Create critical-sized segmental bone defects (e.g., >2 cm in the mandible) to ensure the defect will not heal spontaneously [100].
- Implantation: Implant the test scaffolds (ceramic or natural polymer-based) into the defect site. Compare against empty defects (negative control) and autografts (positive control).
- Post-Op Monitoring: Monitor animals for a predetermined period (e.g., 12-24 weeks).
- Endpoint Analysis:
- Radiological Analysis: Perform computed tomography (CT) scans at multiple time points to quantify new bone formation and scaffold degradation in 3D.
- Histological Analysis: After euthanasia, explant the defect site. Process bone samples for histology (e.g., H&E staining, Masson's Trichrome). Analyze for tissue in-growth, vascularization, and inflammation.
- Biomechanical Testing: Perform mechanical testing (e.g., compression, torsion) on explanted bones to assess the restoration of mechanical function.
This comprehensive protocol allows for the evaluation of scaffold performance in a biologically relevant environment, assessing integration, regeneration, and functional recovery [100].
Analysis of Host Immune and Biological Responses
The host immune response is a critical determinant of implant success or failure. Each class of biomaterial interacts with the immune system in distinct ways.
Signaling Pathways in Biomaterial-Host Interactions
The introduction of a biomaterial initiates a cascade of biological events, beginning with protein adsorption and the activation of specific immune cells and signaling pathways.
Immune Signaling Pathways: This diagram illustrates the distinct immune signaling pathways triggered by different biomaterial classes, leading to varied clinical outcomes.
Silicone Implants predominantly trigger the foreign body reaction pathway. This begins with protein adsorption, followed by the recruitment and activation of macrophages. The persistent presence of the non-degradable material can lead to macrophage fusion, forming foreign body giant cells and culminating in fibrous encapsulation (capsular contracture), which is the most common complication [98] [2]. This pathway is often associated with a chronic inflammatory response.
Natural Polymers, such as collagen, interact with host cells via specific receptor-mediated pathways. Collagen binds to integrin and discoidin domain receptors (DDR) on cell surfaces, activating intracellular signaling cascades like MAPK and PI3K/Akt [79]. These signals can promote a shift in macrophage polarization towards the pro-healing M2 phenotype, which is associated with the secretion of anti-inflammatory cytokines and growth factors that support tissue regeneration and integration, rather than fibrosis [2] [79].
Ceramics exert their biological effects largely through their surface chemistry and ionic dissolution products. As bioactive glasses degrade, they release ions such as calcium, silicate, and phosphate. These ions have been shown to stimulate osteogenesis by promoting osteoblast proliferation and differentiation and can also induce angiogenesis, which is crucial for supplying nutrients to regenerating bone [99].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and materials essential for conducting research in biomaterial-host interactions.
Table 3: Essential Research Reagents for Biomaterial-Immune Response Studies
| Reagent / Material | Function & Application | Experimental Context |
|---|---|---|
| THP-1 Cell Line | Human monocyte cell line; can be differentiated into macrophages for standardized in vitro immunogenicity testing [2]. | In vitro immune profiling (Protocol 3.1) |
| ELISA Kits (e.g., TNF-α, IL-6, IL-10) | Quantify secretion of specific cytokines to determine pro- vs. anti-inflammatory immune response to a biomaterial [2]. | In vitro immune profiling & in vivo serum/tissue analysis |
| Flow Cytometry Antibodies (CD86, CD206) | Identify and characterize macrophage surface markers to distinguish between pro-inflammatory M1 (CD86) and pro-healing M2 (CD206) phenotypes [2]. | In vitro & ex vivo immune cell phenotyping |
| Critical-sized Bone Defect Model | A standardized animal model (e.g., in sheep mandible) to evaluate the efficacy of scaffolds in regenerating bone that cannot heal spontaneously [100]. | In vivo evaluation of bone scaffolds (Protocol 3.2) |
| Micro-CT Scanner | Non-destructive, 3D quantification of new bone formation, scaffold degradation, and bone morphology within a defect site [100]. | In vivo longitudinal monitoring & endpoint analysis |
| Decellularized Tissue Matrix | Provides a natural, biomimetic scaffold that retains the native ECM architecture and bioactive cues, used as a positive control for tissue integration studies [2] [102]. | In vitro & in vivo scaffold performance comparison |
This comparative analysis demonstrates that the ideal biomaterial does not exist; rather, material selection is a strategic decision based on the specific clinical application and desired interaction with the host immune system. Silicone implants serve as permanent prosthetics but are plagued by long-term foreign body reactions. Ceramics are unparalleled for bone regeneration under load-bearing conditions due to their osteoconductivity and strength, but their brittle nature and degradation kinetics need refinement. Natural polymer scaffolds offer the highest level of bioactivity and promote favorable immunomodulation for tissue integration and regeneration, though their mechanical weakness limits their use in load-bearing applications.
Future research should focus on the development of composite and "bio-inspired" materials that combine the mechanical advantages of synthetics with the bioactivity of natural polymers [97] [103]. Furthermore, a paradigm shift towards designing "immunomodulatory" biomaterials that actively promote a pro-regenerative immune response, rather than merely passively avoiding a negative one, is critical [79] [56]. Standardizing evaluation protocols, as outlined in this review, will be essential to accurately compare new biomaterials and accelerate their translation from the laboratory to the clinic.
The journey of a medical innovation from a laboratory concept ("bench") to clinical application ("bedside") represents one of the most challenging yet critical processes in biomedical science. This translation pathway is particularly complex for biomaterials, where success depends not only on therapeutic efficacy but also on harmonious integration with the host biological environment, especially the immune system. Within the broader context of biomaterial-host interactions and immune response research, understanding the factors that determine successful clinical translation becomes paramount for advancing regenerative medicine and therapeutic interventions.
The biomaterial translation landscape is characterized by significant attrition rates. In diagnostic colorectal cancer biomarkers, for instance, a staggering 2,910 biomarkers were identified in the literature, yet only four achieved clinical adoption—a translation rate of just 0.14% [104]. Similarly, despite promising preclinical findings, many biomaterial-based therapeutic approaches fail to navigate the complex pathway to commercial clinical use. This high failure rate underscores the critical importance of analyzing both successful and unsuccessful translation journeys to identify key determinants of clinical success.
This technical guide examines the bench-to-bedside translation process through the dual lenses of clinical outcomes and lessons from marketed products, with particular emphasis on how biomaterial-host interactions, especially immune responses, influence translation success. By synthesizing evidence from diverse case studies and clinical trials, we aim to provide researchers, scientists, and drug development professionals with actionable insights to optimize their translation strategies within the framework of biomaterial-immune system interactions.
Biomaterial-Host Interactions: The Immune Interface
Fundamental Immune Mechanisms in Biomaterial Integration
The host immune response represents a critical determinant of biomaterial success or failure. Upon implantation, biomaterials immediately interact with biological systems, triggering a cascade of events collectively known as the foreign body response [39]. This response begins with protein adsorption onto the material surface, followed by immune cell recognition and activation. The nature of this immune dialogue directly dictates clinical outcomes, influencing both safety profiles and functional efficacy.
Macrophages play a pivotal role in determining biomaterial fate through their remarkable plasticity. These cells can polarize into various phenotypes, primarily categorized as pro-inflammatory M1 macrophages or anti-inflammatory, tissue-reparative M2 macrophages [105] [39]. Successful biomaterials strategically guide this polarization toward the M2 phenotype, fostering a regenerative microenvironment rather than a chronic inflammatory state. Surface properties of biomaterials—including topography, chemistry, and energy—directly influence macrophage polarization and subsequent immune responses [39]. For instance, reducing silicone mammary implant surface roughness to approximately 4μm has demonstrated improved immune response, wound healing, and reduced fibrosis in clinical observations [39].
Advanced Immunomodulatory Biomaterial Strategies
Recent advances in biomaterial science have focused on actively steering immune responses toward therapeutic outcomes through several sophisticated approaches:
Surface Modification Techniques: Biomaterial surfaces are engineered with specific chemical patterns or biofunctional motifs to minimize adverse immune recognition while promoting beneficial host integration [39].
Integration of Immunomodulatory Agents: Biomaterials are designed as delivery vehicles for immune-modulating compounds such as anti-inflammatory cytokines (e.g., IL-10, TGF-β) that create a local tolerogenic environment [105] [39].
Biomimetic Strategies: Utilizing natural biomaterials or creating synthetic materials that mimic natural extracellular matrix components to evade immune detection [39].
Cell Membrane-Camouflaged Nanoparticles: Employing natural cell membranes to cloak biomaterials, effectively disguising them from immune surveillance [39].
The following diagram illustrates the key immune pathways and cellular interactions at the biomaterial-host interface:
Diagram Title: Biomaterial-Host Immune Interface Pathways
Quantitative Analysis of Translation Outcomes
Translation Rates Across Biomedical Domains
The translation pathway from discovery to clinical application is characterized by significant attrition across multiple biomedical domains. The following table summarizes translation rates and timelines for different therapeutic categories:
Table 1: Translation Metrics Across Biomedical Innovation Categories
| Therapeutic Category | Translation Rate | Typical Timeline | Key Bottlenecks |
|---|---|---|---|
| Diagnostic CRC Biomarkers | 0.14% (4/2,910) [104] | 10+ years | Clinical validation, regulatory approval |
| MSC-based Therapies | ~15% (estimated) [105] | 7-12 years | Manufacturing, potency variability |
| Exosome Therapeutics | 0% (No FDA approval yet) [106] | N/A | Standardization, characterization |
| Biomaterial Medical Devices | ~5-10% (estimated) [107] [108] | 5-10 years | Biocompatibility, immune response |
| Small Molecule Drugs | ~10% (estimated) [109] | 10-15 years | Efficacy, safety |
Publication Patterns as Predictors of Translation Success
Analysis of diagnostic colorectal cancer biomarkers reveals distinct publication patterns between stalled and successfully translated biomarkers. Successful biomarkers demonstrate significantly higher publication frequency and journal impact factors compared to their stalled counterparts [104]. Specifically:
- 84.3% of stalled biomarkers had only a single publication, indicating limited validation and scientific consensus [104]
- Successful biomarkers averaged >20 publications prior to clinical adoption
- The highest journal impact factor for successful biomarkers was significantly greater than for stalled biomarkers (p<0.05) [104]
These quantitative patterns suggest that rigorous validation across multiple studies and in high-impact journals correlates with increased translation potential, likely reflecting more robust evidence generation and scientific consensus.
Case Studies: Lessons from Marketed Products
Mesenchymal Stem Cell (MSC) Therapeutics: Clinical Efficacy and Mechanisms
MSC-based therapies represent a promising frontier in regenerative medicine, with several products successfully navigating the translation pathway. The therapeutic effects of MSCs are mediated through multiple mechanisms, with recent research emphasizing paracrine signaling and mitochondrial transfer as primary mechanisms rather than direct engraftment and differentiation [105].
Table 2: Clinically Translated MSC Therapies and Outcomes
| Product/Condition | Mechanism of Action | Clinical Trial Evidence | Outcomes |
|---|---|---|---|
| Remestemcel-L (GVHD) | Immunomodulation via PGE2, IDO, PD-L1 secretion [105] | Phase III trial [105] | 70.4% response rate at day 28 [105] |
| UC-MSCs (COVID-19 ARDS) | Mitochondrial transfer to alveolar epithelial cells, anti-inflammatory effects [105] | REMEDY trial [105] | Reduced mortality, improved oxygenation [105] |
| MSC Therapy (Myocardial Ischemia) | Mitochondrial transfer to cardiomyocytes, paracrine factor secretion [105] | PARACCT trial [105] | Reduced scar formation, improved ejection fraction [105] |
Recent advances have uncovered mitochondrial transfer as a novel therapeutic mechanism where MSCs donate mitochondria to injured cells through tunneling nanotubes, restoring cellular bioenergetics in conditions such as acute respiratory distress syndrome (ARDS) and myocardial ischemia [105]. In ARDS models, MSC-mediated mitochondrial transfer to alveolar epithelial cells resulted in increased ATP generation, decreased oxidative stress, and improved survival outcomes [105].
Biomaterial Medical Devices: Surface-Immune Interactions
The development of drug-eluting stents provides compelling insights into how biomaterial-host immune interactions can determine clinical success. The case of AlchiMedics' electro-grafted (eG) polymer technology illustrates the critical importance of understanding and optimizing the immune response to biomaterials [108].
Originally developed as a covalent bonding strategy to prevent polymer delamination, the eG technology demonstrated unexpected superior healing performance in animal models, with 95% strut coverage at 14 days compared to 70% at 28 days for the benchmark product [108]. This enhanced healing was attributed to the technology's ability to promote endothelialization while minimizing inflammatory responses—a crucial factor in addressing the issue of late stent thrombosis [108].
The translation journey of this technology highlights several critical lessons:
- Value Proposition Evolution: The initial mechanical bonding value was supplemented by the biological healing advantage, which ultimately proved more significant clinically [108]
- Partner Selection: Collaboration with appropriate regional partners (Beijing Sun Technology/SINOMED) facilitated market access despite challenges with major players [108]
- Persistence in Evidence Generation: Continuous clinical evidence generation, including optical coherence tomography studies demonstrating superior endothelial coverage in humans, secured regulatory approvals across multiple jurisdictions [108]
This case exemplifies how a deep understanding of biomaterial-immune cell interactions—specifically, the competition between endothelial cells and smooth muscle cells—can transform a technology's clinical value proposition and ultimate translation success [108].
Exosome-Based Diagnostics: Navigating Regulatory Pathways
Exosome technologies represent an emerging frontier in diagnostic and therapeutic applications, with two exosome-based diagnostics having received FDA Fast Track Approval [106]:
ExoDx Prostate IntelliScore (EPI) Test: A urine-based test that avoids invasive prostate biopsies, evaluated in two clinical trials with 1,022 patients and used in more than 30,000 patients since launch [106]
Guardant360 CDx: A blood-based test for tumor mutation profiling in solid tumors, used by more than 7,000 oncologists with over 150,000 tests performed [106]
The successful translation of these exosome-based diagnostics demonstrates the importance of addressing clear clinical needs (non-invasive alternatives to biopsies) and generating substantial clinical evidence across large patient populations. The global exosome market is anticipated to grow to over $1 billion by 2030, with a compound annual growth rate of 10.5% [106].
Experimental Methodologies for Assessing Biomaterial-Immune Interactions
Standardized Protocols for Immune Compatibility Assessment
Robust assessment of biomaterial-immune interactions requires standardized methodologies that predict clinical performance. The following experimental workflow provides a comprehensive approach for evaluating biomaterial compatibility:
Diagram Title: Biomaterial Immune Testing Workflow
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents for Biomaterial-Immune Interaction Studies
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Surface Characterization Tools | SEM, FTIR, TGA, AFM [39] [108] | Biomaterial physical characterization | Quantify surface topography, chemistry, and mechanical properties |
| Immune Cell Assays | Macrophage polarization assays, cytokine profiling (ELISA, multiplex arrays) [105] [39] | In vitro immune compatibility | Assess inflammatory potential and immunomodulatory properties |
| Animal Models | Rodent foreign body model, rabbit iliac artery stent model [108] | Preclinical safety and efficacy | Evaluate host responses in physiologically relevant environments |
| Biomaterial Formulations | Electro-grafted polymers, biodegradable scaffolds (PLGA), natural polymers (silk, cellulose acetate) [39] [108] | Biomaterial screening and optimization | Provide platforms with tunable immune properties |
| Analytical Platforms | Flow cytometry, OCT, RNA sequencing [105] [108] | Mechanism of action studies | Elucidate cellular and molecular responses to biomaterials |
Advanced Translation Strategies and Future Directions
Innovative Approaches to Enhance Translation Success
The increasing complexity of biomaterial-host interactions demands sophisticated translation strategies. Several innovative approaches show promise for enhancing translation success:
AI-Driven Platforms: Artificial intelligence and machine learning are being utilized to personalize therapies, optimize cell selection, and predict patient-specific responses to biomaterials [105] [109].
Master Protocol Trials: Basket, umbrella, and platform trials enable more efficient evaluation of multiple therapies or biomarkers simultaneously, accelerating evidence generation [109].
Digital Endpoints: Advanced wearable technologies and digital biomarkers provide continuous, real-world data on patient responses and functional outcomes [109].
3D Bioprinting and Scalable Manufacturing: Advanced manufacturing technologies ensure more consistent and precise biomaterial fabrication, addressing potency variability issues [105].
Regulatory and Commercialization Considerations
Successful translation requires meticulous attention to regulatory pathways and commercialization strategies from the earliest stages of development. Key considerations include:
Early Regulatory Engagement: Integrating regulatory strategy from the beginning, with a clear understanding of whether the product will be classified as a medical device, combination product, or drug/biological product [107] [108].
Robust Quality Management: Implementing a comprehensive quality management system to regulate research, development, and manufacturing processes [107].
Clinical Trial Design: Conducting trials with appropriate indications, inclusion criteria, control groups, and endpoints that align with regulatory expectations [107] [104].
Post-Market Surveillance: Developing strategies for ongoing safety and effectiveness monitoring after regulatory approval and commercialization [107].
The integration of these strategic elements—from mechanistic insights to robust quality control and regulatory frameworks—is essential to successfully translating biomaterial innovations from bench to bedside and ensuring their reliable application in clinical practice [105] [107].
The translation of biomaterials from laboratory concepts to clinically viable products remains a formidable challenge, with success heavily dependent on understanding and optimizing host interactions, particularly immune responses. Through analysis of clinical outcomes and lessons from marketed products, several key principles emerge: the critical importance of immune compatibility, the value of multidisciplinary approaches spanning basic science to regulatory strategy, and the necessity of persistent evidence generation across the translation continuum.
As the field advances, emerging technologies in AI, advanced manufacturing, and digital health offer promising avenues to accelerate translation and enhance success rates. However, these technological advances must be coupled with a deepened understanding of fundamental biomaterial-host interactions to truly realize the potential of next-generation biomaterials in clinical practice. By applying the insights and methodologies outlined in this technical guide, researchers and developers can strategically navigate the complex translation pathway to deliver safe, effective biomaterial-based solutions that address unmet clinical needs.
Conclusion
The field of biomaterials has irrevocably shifted from passively avoiding immune responses to actively directing them, positioning immunomodulation as the cornerstone of next-generation medical implants and regenerative strategies. The synthesis of knowledge across foundational immunology, advanced material design, and robust validation techniques is paramount for clinical success. Future progress hinges on the development of personalized, autonomous biomaterials that can dynamically adapt to the host microenvironment in real-time. Leveraging artificial intelligence for material design, integrating multi-omics data for patient-specific solutions, and establishing more predictive in vitro immunological models will be critical. This evolution toward precision immune engineering promises to unlock unprecedented outcomes in tissue regeneration, drug delivery, and the treatment of chronic diseases, ultimately improving patient quality of life and expanding the horizons of modern medicine.
References
- 1. Molecular Signaling in Biomaterial-induced Foreign Body ... [https://pubmed.ncbi.nlm.nih.gov/40981767/]
- 2. Biological responses to biomaterials: a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12068782/]
- 3. Immunocompatible elastomer with increased resistance to ... [https://www.nature.com/articles/s41467-024-52023-z]
- 4. Macrophages in immunoregulation and therapeutics [https://www.nature.com/articles/s41392-023-01452-1]
- 5. Physical cues in biomaterials modulate macrophage ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1640560/full]
- 6. Macrophage M1/M2 polarization [https://www.sciencedirect.com/science/article/abs/pii/S0014299920301825]
- 7. Advanced biomaterials in immune modulation: The future ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325008099]
- 8. Bioscaffold materials resist infection and promote bone defect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12571867/]
- 9. Immunomodulation and cellular response to biomaterials [https://pubs.rsc.org/en/content/articlelanding/2019/mh/c9mh00291j]
- 10. TOWARDS UNDERSTANDING HOW NEUTROPHIL ... [https://boneandjoint.org.uk/Article/10.1302/1358-992X.2024.1.117]
- 11. Dendritic Cells: Origin, Classification, Development, Biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587171/]
- 12. Biomaterial scaffolds for therapeutic immune cell ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925006947]
- 13. The Protein Corona Paradox: Challenges in Achieving True ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12108862/]
- 14. A review on protein corona formation on nanoparticles and ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325009317]
- 15. Inflammatory disease progression shapes nanoparticle ... [https://www.nature.com/articles/s41467-025-56210-4]
- 16. Control of innate immune response by biomaterial surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8497396/]
- 17. Meta-Analysis and Machine Learning Prediction of Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593346/]
- 18. Manipulation of Serum Protein Adsorption by ... [https://acs.figshare.com/collections/Manipulation_of_Serum_Protein_Adsorption_by_Nanoengineered_Biomaterials_Influences_Subsequent_Immune_Responses/7426640]
- 19. Could chronic inflammation be the medical paradigm shift ... [https://aeon.co/essays/could-chronic-inflammation-be-the-medical-paradigm-shift-of-our-age]
- 20. Inflammation: The Cause of All Diseases [https://www.mdpi.com/2073-4409/13/22/1906]
- 21. Editorial: Biomimetics and immuno-informed biomaterials [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1595675/full]
- 22. Immunomodulatory Mechanisms of Chronic Wound Healing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538007/]
- 23. Macrophages as Multifaceted Orchestrators of Tissue Repair [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255350/]
- 24. Peptide-based inflammation-responsive implant coating ... [https://www.nature.com/articles/s41467-025-58444-8]
- 25. Electrode impedance dynamics in sequential cochlear implant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605110/]
- 26. Can Preoperative Blood Inflammatory Biomarkers Predict ... [https://www.mdpi.com/2306-5354/12/11/1208]
- 27. Battle of the Biomarkers of Systemic Inflammation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12024891/]
- 28. Immune Response to Extracellular Matrix Bioscaffolds [https://www.mdpi.com/2673-8449/5/3/28]
- 29. Smart biomaterials: as active immune modulators to shape pro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12558899/]
- 30. Smart biomaterials: as active immune modulators to shape ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1669399/full]
- 31. exploring the interplay between natural biomaterials and host ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10627157/]
- 32. Intrinsic immunogenicity of rapidly-degradable polymers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4754144/]
- 33. Natural and Synthetic Polymers for Biomedical ... [https://www.mdpi.com/2073-4360/16/8/1159]
- 34. Advanced Biocompatible and Biodegradable Polymers [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611034/]
- 35. Biomaterials: Foreign Bodies or Tuners for the Immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6386828/]
- 36. Immunomodulatory Biomaterials and Emerging Analytical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9852373/]
- 37. Research Progress on Biomaterials with Immunomodulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12412535/]
- 38. Physical cues in biomaterials modulate macrophage ... [https://pubmed.ncbi.nlm.nih.gov/40771725/]
- 39. Editorial: Biomimetics and immuno-informed biomaterials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12176579/]
- 40. Formulation Strategies for Immunomodulatory Natural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567283/]
- 41. Modulation of immune-inflammatory responses through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8554547/]
- 42. Surface-engineered hyaluronic acid-coated lyotropic liquid ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03846-5]
- 43. Surface-mediated high antioxidant and anti-inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9258176/]
- 44. Controlled co-delivery of anti-inflammatory drugs from ... [https://link.springer.com/article/10.1007/s13346-025-01942-5]
- 45. Innovative polymer-based therapeutics targeting ... [https://pubmed.ncbi.nlm.nih.gov/41083766/]
- 46. Next-generation anti-inflammatory platforms: Engineering ... [https://www.sciencedirect.com/science/article/pii/S2589234725001198]
- 47. Enzyme-responsive biomaterials for biomedical applications [https://www.nature.com/articles/s43246-025-00983-0]
- 48. Biomaterials: Foreign Bodies or Tuners for the Immune ... [https://www.mdpi.com/1422-0067/20/3/636]
- 49. Advanced smart biomaterials and constructs for hard tissue ... [https://www.nature.com/articles/s41413-018-0032-9]
- 50. Engineering the Immune Response to Biomaterials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12097135/]
- 51. Advanced Nanomedicines for Treating Refractory ... [https://link.springer.com/article/10.1007/s40820-025-01829-7]
- 52. Advanced wound healing with Stimuli-Responsive nanozymes [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03558-w]
- 53. Exosomes: the future of acellular nanotherapeutics in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12443856/]
- 54. Prognosis recovery score of apical surgery Guided Bone ... [https://www.sciencedirect.com/science/article/pii/S2405844024090649]
- 55. Advanced strategies to thwart foreign body response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9472022/]
- 56. Interplay between biomaterials and the immune system [https://www.sciencedirect.com/science/article/pii/S1742706122007255]
- 57. Effect of tissue microenvironment on fibrous capsule ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8135119/]
- 58. Chronic inflammation in biomaterial induced periprosthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3849197/]
- 59. Inflammatory responses to biomaterials [https://pubmed.ncbi.nlm.nih.gov/7726145/]
- 60. Chronic inflammation in biomaterial-induced periprosthetic ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706113004947]
- 61. Aseptic and septic prosthetic joint loosening: Impact of ... [https://pubmed.ncbi.nlm.nih.gov/34564034/]
- 62. aseptic implant loosening--the contribution and future ... [https://pubmed.ncbi.nlm.nih.gov/24827940/]
- 63. Overcoming immune hurdles to implant longevity [https://www.nature.com/articles/s41551-024-01276-6]
- 64. Mechanisms and Therapeutic Strategies of Macrophage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077540/]
- 65. Macrophage polarization in cancer and beyond: from ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525003386]
- 66. From macrophage polarization to clinical translation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504304/]
- 67. Advances in the regulation of macrophage polarization by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12328869/]
- 68. Reprogram to heal: Macrophage phenotypes as living ... [https://www.sciencedirect.com/science/article/abs/pii/S0024320525002358]
- 69. Biomaterial Strategies of Macrophage Behaviour in Bone ... [https://link.springer.com/article/10.1007/s40883-025-00443-8]
- 70. Improving In Vitro–In Vivo Correlation (IVIVC) for Lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567226/]
- 71. CMC Perspectives of In Vitro / In Vivo Correlation (IVIVC) ... [https://premier-research.com/perspectives/cmc-perspectives-of-in-vitro-in-vivo-correlation-ivivc-in-drug-development/]
- 72. An Integrated AI-PBPK Platform for Predicting Drug In Vivo ... [https://pubmed.ncbi.nlm.nih.gov/40418625/]
- 73. The inflammasome in host response to biomaterials [https://www.sciencedirect.com/science/article/abs/pii/S1742706118305853]
- 74. Interactions Between Immunomodulatory Biomaterials and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.820940/full]
- 75. Inflammation and aging: signaling pathways and ... [https://www.nature.com/articles/s41392-023-01502-8]
- 76. The Interplay of Biomaterials, Immunology, and Aging [https://www.sciqst.com/The%20Interplay%20of%20Biomaterials,%20Immunology,%20and%20Aging:%20Innovations%20and%20Challenges%20in%20Therapeutic%20Interventions]
- 77. The Immune System and Its Contribution to Variability in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7891216/]
- 78. Rethinking immunity in bioengineering [https://www.nature.com/articles/s44222-025-00336-z]
- 79. Material matters: exploring the interplay between natural ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1269960/full]
- 80. Quantitative and Qualitative Assessment Methods for Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6133255/]
- 81. Implant infections: adhesion, biofilm and formation evasion immune [https://www.nature.com/articles/s41579-018-0019-y?error=cookies_not_supported&code=29f63432-6cea-4440-9166-d3b9da8f95cd]
- 82. Bacterial Biofilm on Formation and Approaches to Its... Biomaterials [https://pubmed.ncbi.nlm.nih.gov/37511440/]
- 83. Immunomodulatory biomaterials for implant-associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9721013/]
- 84. by the host microbiota: a protective shield against... Biofilm formation [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02348-0]
- 85. Quantifying the Dynamics of Bacterial Biofilm Formation on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10932241/]
- 86. Engineering immunomodulatory biomaterials to combat ... [https://www.frontiersin.org/journals/biomaterials-science/articles/10.3389/fbiom.2023.1336842/full]
- 87. The Role of In Vitro Immune Response Assessment for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6787714/]
- 88. Development of an in vitro method to assess the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408726/]
- 89. Quantitative characterization of immune cells by measuring ... [https://www.nature.com/articles/s41598-024-75666-w]
- 90. Single-cell and spatial transcriptomics integration [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528096/]
- 91. Advancements in single-cell RNA sequencing and spatial ... [https://www.frontierspartnerships.org/journals/acta-biochimica-polonica/articles/10.3389/abp.2025.13922/full]
- 92. Single-cell RNA sequencing reveals key signaling pathways ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009258/]
- 93. Gene-level alignment of single-cell trajectories [https://www.nature.com/articles/s41592-024-02378-4]
- 94. Comparative proteomic analysis of skin wound healing ... [https://pubmed.ncbi.nlm.nih.gov/40939262/]
- 95. Visualization of proteomics data using R and Bioconductor [https://pmc.ncbi.nlm.nih.gov/articles/PMC4510819/]
- 96. Adaptive immunity of materials: Implications for tissue ... [https://www.sciencedirect.com/science/article/pii/S2452199X24003104]
- 97. Implanted cardiovascular polymers: Natural, synthetic and ... [https://www.sciencedirect.com/science/article/abs/pii/S0079670008000543]
- 98. Safety and Performance of Postmarketing Breast Implants [https://pmc.ncbi.nlm.nih.gov/articles/PMC12194552/]
- 99. Bioceramics and Scaffolds: A Winning Combination for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4681769/]
- 100. How Does Ceramic-Based Scaffold Microarchitecture ... [https://www.mdpi.com/2076-3417/15/12/6899]
- 101. A Comparative Review of Natural and Synthetic Biopolymer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8037451/]
- 102. A Review of Recent Advances in Natural Polymer-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145843/]
- 103. Advanced polymeric scaffolds for bone tissue regeneration [https://www.explorationpub.com/Journals/ebmx/Article/101340]
- 104. Assessing the translation of diagnostic colorectal cancer ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1598697/full]
- 105. From bench to bedside: translating mesenchymal stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344367/]
- 106. From Bench to Bedside: The Global Market for Exosome ... [https://bioinformant.com/from-bench-to-bedside-the-global-market-for-exosome-therapeutics/]
- 107. Translation of biomaterials from bench to clinic - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8965774/]
- 108. Journey of medical device development from the bench to ... [https://www.explorationpub.com/Journals/ebmx/Article/10134]
- 109. The next generation of evidence-based medicine [https://www.nature.com/articles/s41591-022-02160-z]