Biomaterials in Controlled Drug Delivery: From Smart Carriers to Clinical Translation
This article provides a comprehensive analysis of the transformative role of biomaterials in controlled drug delivery systems, tailored for researchers, scientists, and drug development professionals.
Biomaterials in Controlled Drug Delivery: From Smart Carriers to Clinical Translation
Abstract
This article provides a comprehensive analysis of the transformative role of biomaterials in controlled drug delivery systems, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of material-tissue interactions and the classification of natural, synthetic, and bio-inspired systems. The scope extends to advanced methodologies including stimuli-responsive hydrogels, nanoparticle targeting, and 3D-bioprinted scaffolds for applications in oncology, regenerative medicine, and beyond. The review critically addresses key challenges in biocompatibility, scalability, and immune response, while evaluating optimization strategies through high-throughput screening and AI-driven design. Finally, it offers a comparative assessment of clinical translation pathways, regulatory hurdles, and the efficacy of various biomaterial platforms, synthesizing current trends to forecast future directions in personalized and intelligent therapeutics.
The Foundation of Biomaterial-Driven Drug Delivery: Principles, Materials, and Mechanisms
Defining Biomaterials and Their Evolution in Controlled Release
Biomaterials are substances engineered to interact with biological systems for a medical purpose, ranging from treating or diagnosing diseases to replacing or repairing tissue functions [1]. In the context of controlled drug delivery, these materials serve as the foundational platform for encapsulating, stabilizing, and releasing therapeutic agents in a predetermined manner [2]. Their versatility and adaptability have revolutionized therapeutic outcomes by significantly enhancing drug bioavailability while minimizing adverse effects, thereby addressing the critical limitations of conventional drug delivery systems [1] [3]. The evolution of biomaterials has transitioned from simple, inert carriers to sophisticated, intelligently designed systems capable of responding to dynamic physiological cues, marking a paradigm shift in modern pharmacotherapy.
The core objective of using biomaterials in controlled release is to extend, confine, and target the active pharmaceutical ingredient (API) within the diseased tissue, thereby protecting it from premature degradation and ensuring a protected interaction with the biological environment [3]. This is particularly crucial for potent drugs requiring low dosages, substances susceptible to degradation in the gastrointestinal tract, or compounds with undesirable organoleptic properties [3]. By carefully selecting and engineering excipients and biomaterials, formulators can overcome these challenges, achieving precise control over release kinetics and site-specific targeting that was previously unattainable with conventional dosage forms like tablets and capsules [1] [3].
Historical Evolution and Generational Shift
The development of ophthalmic biomaterials provides a clear framework for understanding the broader evolution of biomaterials in controlled release, characterized by a structured transition from passive to highly adaptive systems [4]. This progression reflects the convergence of materials science, biomedical engineering, and pathophysiology, with each generation overcoming specific clinical and technological limitations.
Table 1: Generational Evolution of Biomaterials in Controlled Drug Delivery
| Generation | Core Characteristics | Key Material Examples | Advantages | Limitations | Representative Applications |
|---|---|---|---|---|---|
| 1st: Inert Biomaterials | Chemically/mechanically stable; biologically inert; passive structural support [4] | PMMA, PDMS, PVA, Titanium [4] | Excellent biocompatibility and durability; long-term safety [4] | Lack of bioactivity; no therapeutic interaction; low oxygen permeability [4] | Intraocular Lenses (IOLs), Vitreous Substitutes, Contact Lenses [4] |
| 2nd: Bioactive Biomaterials | Biodegradable; surface reactive; promote tissue integration; controlled drug release [4] | PLGA, PLA, PCL, Chitosan, Hydroxyapatite (Hap), Collagen [4] | Promotes cell adhesion & tissue regeneration; tunable degradation rates [4] | Mechanical weakness; pre-programmed release without real-time adaptability [4] | Biodegradable implants, drug-loaded microspheres (e.g., Ozurdex), regenerative scaffolds [4] |
| 3rd: Actively Interactive Smart Biomaterials | Stimuli-responsive; dynamic, on-demand release capability [4] | PNIPAM, Pluronic F127, PEG-PLGA, ZIF-8 [4] | Spatiotemporally targeted drug delivery; improved therapeutic precision [4] | Complex fabrication; mainly open-loop control; potential biosafety concerns [4] | Temperature-sensitive gels, ROS-scavenging nanocarriers, photothermal materials [4] |
| 4th: Closed-Loop & Autonomous Systems (Emerging) | Integration of sensing, computation, and actuation; mimicry of biological feedback [4] | Zwitterionic hydrogels, conductive nanomaterials, iPSC-GelMA hybrids [4] | Real-time monitoring and adaptive control; personalized & autonomous therapeutic response [4] | Power/miniaturization challenges; significant ethical, data, and regulatory barriers [4] | Smart contact lenses for IOP monitoring, autonomous implants for neurostimulation [4] |
This four-stage model illustrates the functional trajectory from basic structural replacements to intelligently adaptive, cell-instructive platforms. The field is currently advancing through the third generation and into the fourth, leveraging innovations in materials science, microfabrication, and bioelectronics to create systems capable of autonomous, real-time control [4].
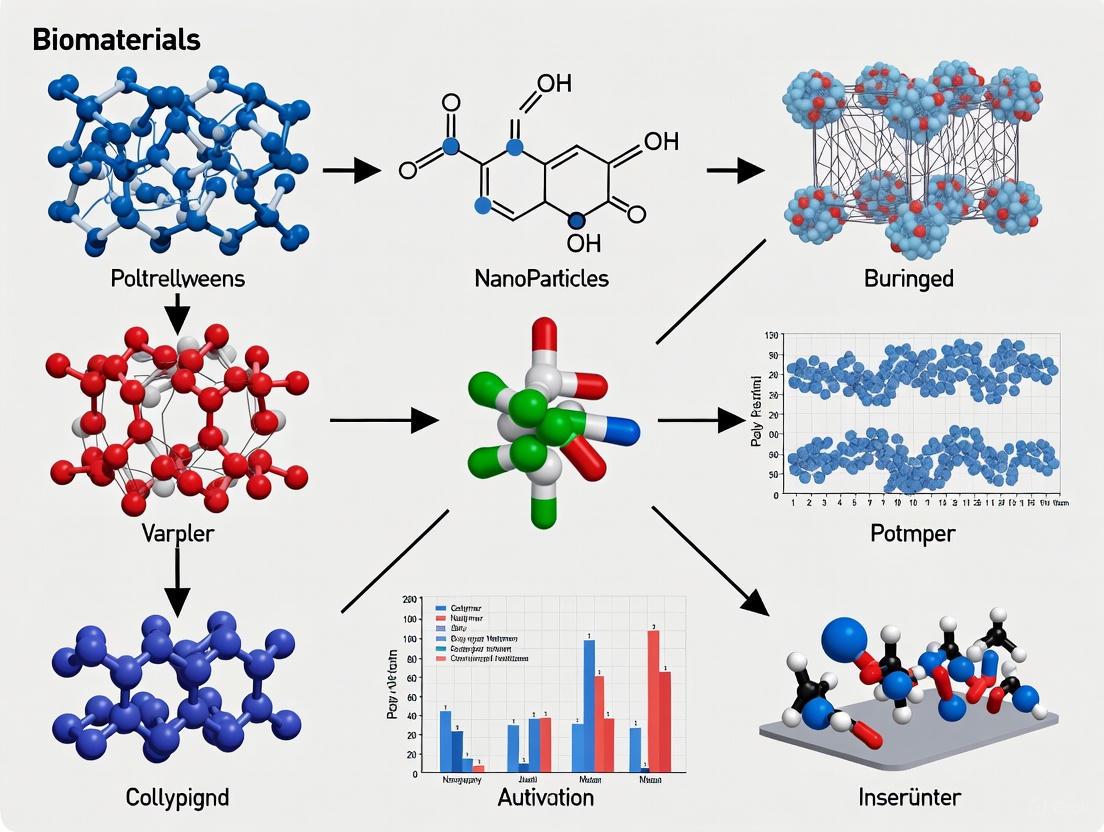
Figure 1: Generational Roadmap of Biomaterials. The evolution progresses from passive, inert systems to bioactive, then stimuli-responsive, and finally towards autonomous, closed-loop platforms [4].
Advanced Biomaterial Systems and Controlled Release Mechanisms
Classification and Material Design
Contemporary biomaterials for controlled release are categorized based on their origin and properties into biobased, biodegradable, and biocompatible materials [1]. Their design must carefully consider parameters such as particle size, with nanoparticles preferred for enhanced bioavailability and targeted delivery, and high surface area, which directly influences drug-loading capacity and interactions with biological components [1]. Advanced rational design focuses on creating versatile and biocompatible polymeric nanoparticles that can protect biologics from degradation, target their delivery, and increase their in vivo half-lives [5]. Key platforms include layer-by-layer nanoparticles, dendrimers, nanogels, self-assembled nanoparticles, and nanocomplexes [5].
Key Release Mechanisms and System Architectures
Controlled drug release is achieved through various fundamental mechanisms, including diffusion, chemical reactions, dissolution, and osmosis, often used in combination [6]. Material-driven strategies have evolved to exploit these mechanisms in sophisticated ways:
- Structurally Engineered Systems: These include bilayer architectures, layer-by-layer assembly techniques, and porous matrix designs that provide structural control over the release profile [7].
- Stimuli-Responsive Mechanisms: These "smart" systems release their payload in response to specific physicochemical triggers in the microenvironment [7] [8]. These triggers include:
- Physical Condition Modulation: Changes in temperature or mechanical force.
- Swelling/Degradation Behavior: Water uptake or material erosion.
- Dynamic Chemical Bond Engineering: Cleavage of bonds by enzymes or pH shifts.
- Crosslinking Network Optimization: Changes in mesh size and porosity.
- Nanotechnology-Enabled Delivery: Polymeric nanoparticles, liposomes, and lipid nanoparticles are engineered with surface modifications to improve gene delivery efficiency and reduce immune responses [8]. For instance, polymer-based nanocarriers like polyethyleneimine (PEI) utilize the "proton sponge" effect to enhance endosomal escape, while liposomes benefit from high biocompatibility and surface functionalization for targeted delivery [8].
Table 2: Advanced Biomaterial Platforms for Controlled Release
| Platform | Key Components | Release Mechanism | Application Examples |
|---|---|---|---|
| Intelligent Hydrogels | Chitosan, PVA-CMC, Dragon's blood resin, Sage extract [8] | Swelling/degradation; response to pH, temperature, or enzymatic activity [8] | Fast-gelling hydrogel for periodontal regeneration; anti-inflammatory wound dressing [8] |
| Branched Peptide-Based Materials | Dendritic peptide structures, natural polymers [9] | Self-assembly; controlled degradation due to slower degradation rates and greater stiffness [9] | Drug delivery systems, wound healing scaffolds, tissue engineering constructs [9] |
| Electrospun Nanofibers | Various biodegradable polymers (e.g., PLGA, PLA) [8] | Diffusion; high surface area and tunable porosity facilitate localized delivery [8] | Diabetic wound healing scaffolds, serving as localized drug delivery systems and structural supports [8] |
| Polymeric Nanoparticles | PLGA, PLA, PEG-PLGA, PEI [8] [5] | Diffusion; degradation; "proton sponge" effect for endosomal escape [8] [5] | Delivery of biologics; cancer therapy; oocyte cryopreservation (PLGA-RES nanocomposite) [8] [5] |
| Motile Microrobots | Hydrogel matrix, magnetic components [8] | Magnetically propelled penetration; sustained release from hydrogel matrix [8] | Co-delivery of drugs for osteosarcoma treatment under external magnetic field guidance [8] |
Experimental Analysis and Computational Modeling
Computational Workflow for Release Kinetics
Understanding and predicting drug release from porous polymeric biomaterials is fundamental to rational design. A leading computational methodology integrates mass transfer simulation with artificial intelligence (AI) to create highly accurate predictive models [10]. The workflow begins with the numerical simulation of diffusional mass transfer, described by Fick's second law, which includes a reaction term:
$$\frac{\partial C}{\partial t} + \nabla \cdot \left(-D\nabla C\right)=R$$
where C is the drug concentration (mol/m³), t is time (s), D is the drug diffusivity (m²/s), and R is the chemical reaction term [10]. Solving this equation for a specific geometry (e.g., a cylindrical fibrin matrix) generates a comprehensive dataset of concentration (C) values at different spatial coordinates (r, z), typically comprising over 15,000 data points [10].
Figure 2: Computational Workflow for Drug Release Modeling. This integrated approach combines physics-based simulation with machine learning to predict drug concentration distributions [10].
Machine Learning Model Performance
In a critical study evaluating three regression models—Kernel Ridge Regression (KRR), Gaussian Process Regression (GPR), and Gradient Boosting (GB)—the GB model, optimized with the Firefly Optimization (FFA) algorithm, demonstrated superior performance. It achieved an exceptional R² score of 0.9977, indicating near-perfect alignment with the simulation data, along with the lowest Mean Squared Error (MSE) and Root Mean Squared Error (RMSE) [10]. This highlights the power of ensemble ML methods in modeling complex spatial datasets for drug release prediction.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and testing of advanced biomaterials for controlled release rely on a specific toolkit of reagents, materials, and methodologies.
Table 3: Key Research Reagent Solutions for Biomaterial-Based Drug Delivery
| Reagent/Material | Function in Research | Specific Example & Rationale |
|---|---|---|
| Biodegradable Polymers (PLGA, PLA, PCL) | Form the matrix of nanoparticles, microspheres, and scaffolds; control release kinetics via degradation rate [4] [1]. | PLGA microspheres used in Ozurdex; provide sustained release of dexamethasone over several weeks [4]. |
| Stimuli-Responsive Polymers (PNIPAM, Pluronic F127) | Enable "smart," on-demand drug release in response to temperature, pH, or enzyme triggers [4]. | PNIPAM used in temperature-sensitive hydrogels that gel at body temperature for injectable depot formation [4]. |
| Natural Polymers & Peptides (Chitosan, Branched Peptides, Collagen) | Enhance biocompatibility and provide biomimetic properties; can self-assemble into structured scaffolds [8] [9]. | Branched peptides offer slower degradation, greater stiffness, and modularity for designing tissue engineering constructs [9]. |
| Crosslinking Agents | Stabilize hydrogel networks and control mesh size, directly influencing diffusion-based release rates and mechanical strength [7]. | Genipin is used as a natural crosslinker for chitosan hydrogels, modulating its swelling and release profile. |
| Bioactive Glass & Ceramics (Hydroxyapatite, 4555 Bioglass) | Used in composite materials for bone-related applications; offer osteoconductivity and tunable dissolution rates [2]. | Hydroxyapatite (Hap) is used in orbital implants (e.g., Bio-Eye) for its bioactive integration with bone [4]. |
| Computational Modeling Software | Predicts drug release profiles and optimizes biomaterial design in silico, reducing experimental trial and error [10]. | Used to implement Gradient Boosting models with Firefly Optimization for predicting concentration distributions from porous carriers [10]. |
The evolution of biomaterials from inert structural components to intelligently interactive systems has fundamentally transformed the landscape of controlled drug delivery. This journey, delineated by the four-generation roadmap, showcases a clear trajectory toward greater integration with biological processes, culminating in the emerging paradigm of closed-loop, autonomous therapeutic systems [4]. The ongoing integration of AI and machine learning, both in the computational design of materials and the optimization of release kinetics, is poised to further accelerate this evolution [8] [10].
Future research will focus on bridging the gap between laboratory innovation and clinical application. Key frontiers include the development of AI-assisted material design to optimize biomaterial properties for specific therapeutic needs, and a deeper investigation of the interactions between biomaterials and the immune system to ensure long-term safety and efficacy [8]. Furthermore, the expansion of innovative platforms like microrobots and nanofibers into diverse disease contexts will advance their role in personalized medicine [8]. As the field progresses, addressing the challenges of manufacturing complexity, potential toxicity, and comprehensive regulatory frameworks will be essential for translating these groundbreaking biomaterial-based controlled release systems into mainstream clinical practice, ultimately enabling treatments that are precisely tailored to individual patient needs [1].
The development of advanced drug delivery systems (DDSs) represents a paradigm shift in managing complex chronic conditions, including cancer, neurological disorders, and inflammatory diseases. Biomaterials serve as the foundational cornerstone of these systems, engineered to enhance therapeutic efficacy, improve patient compliance, and minimize side effects through precise spatial and temporal control of drug release [11]. Among the diverse array of biomaterials, three key classes have emerged as particularly significant: synthetic polymers like poly(lactic-co-glycolic acid) (PLGA) and polyethylene glycol (PEG), natural polymers such as chitosan and collagen, and specialized medical ceramics. These materials enable formulators to overcome fundamental biological barriers, including the reticuloendothelial system (RES) clearance, the blood-brain barrier (BBB), and the complex tumor microenvironment [12] [13]. This technical guide provides an in-depth analysis of these core material classes, detailing their properties, fabrication methodologies, and mechanisms of action within the context of modern controlled drug delivery research.
Synthetic Polymers
PLGA (Poly(lactic-co-glycolic acid))
PLGA is a FDA-approved, biodegradable, and biocompatible copolymer widely utilized in drug delivery systems. Its degradation occurs through hydrolysis of ester linkages into lactic acid and glycolic acid, which are metabolized via the Krebs cycle and excreted as carbon dioxide and water [11]. The properties of PLGA, such as degradation rate and drug release kinetics, can be finely tuned by adjusting its molecular weight, lactide to glycolide ratio, and end-group chemistry [11].
- Applications: PLGA-based nanoparticles and microspheres are extensively used for the controlled delivery of small-molecule drugs, proteins, peptides, antibiotics, and antiviral agents. They enhance drug stability, aqueous solubility, and bioavailability while enabling sustained release profiles from weeks to months [11]. Applications span cancer therapy, pain management, and long-acting injectables, with commercial examples including Lupron Depot and Risperdal Consta [11].
- Key Formulation Parameters: The critical quality attributes of PLGA formulations include particle size, size distribution, porosity, and drug loading capacity, all of which significantly influence in vitro and in vivo performance [11] [14]. Factors such as a higher molecular weight, a higher lactide ratio, and acid end caps contribute to lower hydrophilicity and a slower degradation rate [11].
PEG (Polyethylene glycol) and PEGylation
PEG is a hydrophilic, non-ionic synthetic polymer extensively used to modify the surface of drug carriers, such as PLGA nanoparticles, in a process known as PEGylation. This process forms a steric "stealth" corona around the nanoparticle, reducing opsonization and recognition by the immune system [12]. The primary outcome is a significantly extended systemic circulation time, which increases the likelihood of the drug carrier reaching its target site, a crucial advantage in targeted therapies like cancer treatment [12]. Furthermore, PEGylation provides a versatile platform for the subsequent conjugation of targeting ligands (e.g., antibodies, peptides) while maintaining the nanoparticle's stealth properties [12].
Natural Polymers
Chitosan
Chitosan is a natural cationic polysaccharide derived from the deacetylation of chitin, sourced from crustacean shells, fungi, and other biological materials [15] [16]. Its key attributes include excellent biocompatibility, biodegradability, inherent antibacterial activity, and mucoadhesive properties [15]. However, its application can be limited by poor water solubility, rapid in vivo depolymerization, and insufficient mechanical strength, which can be mitigated through chemical modification or blending with other polymers like collagen [15].
- Applications in Drug Delivery: Chitosan's positive charge enables strong interaction with negatively charged lipids and proteins, making it ideal for gene delivery, protein/peptide delivery, and mucosal drug delivery systems [15] [13]. Its composite with collagen is particularly promising for wound healing and tissue engineering due to synergistic hemostatic, antibacterial, and tissue regeneration activities [15].
- Modifications: Derivatives such as carboxymethyl chitosan, quaternized chitosan, and sulfated chitosan have been developed to enhance solubility, biological activity, and functional versatility for specialized drug delivery applications [15].
Collagen
Collagen, the primary fibrous protein in the extracellular matrix of animals, is characterized by a unique triple-helical structure and a primary sequence of repeating Gly-Xaa-Yaa triplets [16]. Marine-derived collagen, sourced from fish skins and scales or jellyfish, is gaining traction as an alternative to terrestrial sources due to its lower immunogenicity, excellent biocompatibility, and superior scaffold-forming properties that facilitate cellular adhesion and proliferation [16].
- Applications in Drug Delivery and Beyond: Collagen's role extends to tissue engineering scaffolds, wound dressings, and as a carrier for controlled drug release [15] [13]. In composites with chitosan, it enhances mechanical strength and positively affects cell proliferation, creating an ideal environment for tissue repair and regeneration [15].
- Formats: Collagen can be processed into various forms, including nanoparticles, nanofibers, hydrogels, films, and sponges, to suit different delivery needs [15].
Ceramics
Medical ceramics are inorganic, non-metallic materials engineered for use within the human body. They are broadly categorized into bioinert and biocompatible ceramics.
- Bioinert ceramics, such as alumina and zirconia, are characterized by high wear resistance, corrosion resistance, and mechanical strength. They do not interact with surrounding tissues and are primarily used in load-bearing dental and orthopedic implants [17] [18].
- Biocompatible ceramics, including hydroxyapatite and bioactive glasses, actively interact with biological tissues. They are osteoconductive (supporting bone growth along their surface) and can undergo osseointegration, making them suitable for bone grafts and coatings on metal implants [17] [18].
A prominent application in drug delivery involves mesoporous silica nanoparticles and other bioactive ceramics. These materials can be engineered as implantable devices for targeted drug delivery, offering low toxicity, adjustable sizes, and the capability for controlled release [18]. Their surfaces can be functionalized with specific ligands to achieve active targeting, and their porous structure allows for high drug loading [17]. Emerging applications include their use in cancer treatment, diagnostics, and hybrid therapeutic systems [18].
Quantitative Data Comparison
The following tables summarize key properties and application parameters for the discussed biomaterial classes.
Table 1: Comparative Properties of Key Biomaterial Classes for Drug Delivery
| Material Class | Representative Materials | Key Properties | Degradation Timeline | Primary Drug Delivery Advantages |
|---|---|---|---|---|
| Synthetic Polymers | PLGA, PEG | Tunable degradation, biocompatible, excellent processability | Weeks to months [11] | Controlled release kinetics, "stealth" properties (PEG), high drug loading [12] [11] |
| Natural Polymers | Chitosan, Collagen | Inherent bioactivity, biocompatible, biodegradable | Days to weeks [15] | Mucoadhesion (chitosan), innate cell interaction, hemostatic [15] [16] |
| Ceramics | Hydroxyapatite, Zirconia, Bioactive Glass | High compressive strength, wear-resistant, osteoconductive | Non-degradable to years (resorbable) [17] | Osseointegration, high stability, targeted delivery to bone [17] [18] |
Table 2: Influence of PLGA Properties on Drug Release Performance [11] [14]
| PLGA Property | Impact on Degradation & Drug Release | Typical Range/Options |
|---|---|---|
| Lactide:Glycolide Ratio | Higher lactide content slows degradation. 50:50 degrades faster than 75:25 [11]. | 50:50, 65:35, 75:25, 85:15 |
| Molecular Weight | Higher molecular weight extends degradation duration [11]. | 10 kDa to >100 kDa |
| End Group | Acid end group (COOH) leads to faster degradation than ester-capped (alkyl) [11]. | Carboxylate (acid) or Ester (capped) |
| Crystallinity | More crystalline regions slow down water penetration and degradation [14]. | Amorphous to semi-crystalline |
Experimental Protocols
Protocol: Preparation of PEGylated PLGA Nanoparticles via Emulsion Solvent Evaporation
This is a standard method for synthesizing drug-loaded PEGylated PLGA nanoparticles, as detailed in recent literature [12].
1. Reagent Setup:
- Organic Phase: Dissolve 50 mg of PLGA polymer and 5 mg of the drug (e.g., a chemotherapeutic agent) in 5 mL of a volatile organic solvent (e.g., dichloromethane, DCM).
- Aqueous Phase: Prepare a 1-2% (w/v) aqueous solution of a stabilizer such as polyvinyl alcohol (PVA).
- PEG Solution: Have a solution of PEG-terminated phospholipid (e.g., DSPE-PEG) or PEG polymer ready for post-formation surface coating.
2. Primary Emulsion Formation:
- The organic phase is added to the aqueous PVA solution (typical volume ratio 1:5 to 1:10 organic:aqueous).
- The mixture is immediately emulsified using a high-speed homogenizer (e.g., 10,000-15,000 rpm for 2-5 minutes) or via probe sonication (e.g., 50-100 W for 1-2 minutes in an ice bath) to form a crude oil-in-water (o/w) emulsion.
3. Emulsion Refinement:
- The coarse emulsion is further processed using a high-pressure homogenizer or subjected to extended sonication to reduce the droplet size and achieve a narrow size distribution.
4. Solvent Evaporation:
- The fine emulsion is stirred continuously at room temperature for several hours (typically 3-6 hours) to allow the organic solvent to evaporate, solidifying the nanoparticles.
- Alternatively, pressure can be reduced to accelerate solvent removal.
5. PEGylation and Purification:
- The PEG solution is added to the nanoparticle suspension and stirred to allow the PEG chains to adsorb or anchor onto the PLGA surface, forming the protective corona [12].
- The nanoparticles are collected by ultracentrifugation (e.g., 20,000-30,000 rpm for 30 minutes at 4°C) and washed 2-3 times with distilled water or Milli-Q water to remove excess PVA, unencapsulated drug, and free PEG.
6. Characterization:
- Size and Zeta Potential: The mean particle size, polydispersity index (PDI), and surface charge (zeta potential) are determined using dynamic light scattering (DLS) [12].
- Drug Loading and Encapsulation Efficiency: The drug content is quantified using a validated HPLC or UV-Vis method after dissolving the nanoparticles in a suitable solvent.
Protocol: Fabrication of Chitosan-Collagen Composite Nanoparticles
This protocol outlines the preparation of composite nanoparticles leveraging the synergistic effects of chitosan and collagen [15].
1. Solution Preparation:
- Chitosan Solution: Dissolve medium molecular weight chitosan in a 1% (v/v) acetic acid solution to obtain a 0.5-1 mg/mL concentration. Filter the solution to remove any undissolved particles.
- Collagen Solution: Dissolve type I collagen (from bovine or marine source) in a weak acid solution (e.g., 0.1M acetic acid) or as per manufacturer's instructions to a similar concentration.
2. Composite Formation:
- Under constant magnetic stirring, add the collagen solution dropwise to the chitosan solution. The positive charge of chitosan facilitates a strong electrostatic interaction with the negatively charged residues of collagen, leading to the self-assembly of composite nanoparticles [15].
- Alternatively, the two solutions can be mixed and then subjected to ionic gelation by adding a cross-linker like tripolyphosphate (TPP).
3. Cross-linking:
- To improve the stability of the nanoparticles, a cross-linking agent such as EDC/NHS can be added to the suspension to form covalent amide bonds between the amine groups of chitosan and carboxyl groups of collagen [15].
4. Purification:
- The nanoparticle suspension is dialyzed against distilled water for 24 hours to remove excess acid and cross-linkers, or purified via repeated centrifugation and resuspension cycles.
5. Characterization:
- Similar to the PLGA protocol, the composite nanoparticles are characterized for size, zeta potential, and morphology (e.g., using SEM or TEM).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Biomaterial Fabrication
| Reagent/Material | Function/Application | Example Use-Case |
|---|---|---|
| PLGA Resins | Biodegradable polymer matrix for drug encapsulation. | Forming the core of nanoparticles for sustained release [11]. |
| DSPE-PEG | Amphiphilic polymer for PEGylation and stealth coating. | Conjugating to PLGA surface to reduce immune clearance [12]. |
| Chitosan (Various Mw) | Natural cationic polymer for gene/drug delivery and composites. | Forming ionic complexes with DNA or creating composite scaffolds with collagen [15]. |
| Type I Collagen | Natural protein for bioactive scaffolds and composites. | Providing a biomimetic matrix in wound healing dressings [15] [16]. |
| EDC/NHS Crosslinker | Activating carboxyl groups for covalent conjugation to amines. | Anchoring targeting ligands to nanoparticles or crosslinking collagen-chitosan hydrogels [12] [15]. |
| Polyvinyl Alcohol | Surfactant and stabilizer in emulsion formulations. | Preventing coalescence of droplets during PLGA nanoparticle formation [12]. |
| Hydroxyapatite Powder | Bioceramic for bone tissue engineering and drug delivery. | Fabricating osteoconductive scaffolds or coatings for orthopedic implants [18]. |
Visual Workflows and Logical Relationships
The following diagrams illustrate the strategic selection of biomaterials and the experimental workflow for nanoparticle synthesis.
Diagram 1: Biomaterial Selection Strategy
Diagram 2: Nanoparticle Synthesis Workflow
Within the broader thesis on the role of biomaterials in controlled drug delivery systems, understanding the fundamental release mechanisms is paramount. These mechanisms—diffusion, degradation, and stimuli-response—dictate the spatiotemporal control of therapeutic agent release, thereby directly influencing the efficacy and safety of treatments for complex diseases [7] [19]. The evolution from simple passive coverage to advanced, multifunctional dressing systems underscores the critical need for material-driven drug release strategies that can be precisely engineered [7]. This whitepaper provides an in-depth technical examination of these core release mechanisms, framing them within the context of contemporary biomaterial innovations such as intelligent responsive hydrogels, nanoparticle-hydrogel hybrids, and enzyme-triggered systems [8] [20] [21]. By synthesizing recent advancements and detailed methodologies, this guide aims to equip researchers and drug development professionals with the knowledge to design next-generation drug delivery platforms.
Core Release Mechanisms in Biomaterials
The controlled release of bioactive agents from biomaterials is governed by three primary mechanisms, which can operate in isolation or in concert. These mechanisms are the foundation for achieving tailored release profiles that meet specific therapeutic needs.
Diffusion-Controlled Release
Diffusion-controlled release is driven by the concentration gradient of the drug between the carrier matrix and the external environment. The drug's path through the biomaterial's structure is the critical rate-determining step. This mechanism is dominant in reservoir systems (where a drug core is surrounded by a polymeric membrane) and matrix systems (where the drug is dispersed throughout a polymer network) [19]. The porosity, swelling behavior, and structural architecture of the biomaterial—such as in bilayer or layer-by-layer assemblies—exert precise control over the diffusion pathway [7]. In nanoparticle-hydrogel hybrids, molecular interactions (electrostatic forces, hydrogen bonding) significantly influence the diffusion rate and the initial burst release [21].
Degradation-Controlled Release
Degradation-controlled release occurs as the biomaterial matrix undergoes chemical breakdown, typically through hydrolysis or enzymatic cleavage, which liberates the encapsulated drug. The rate of drug release is thus directly coupled to the rate of polymer chain scission [19]. Common biodegradable polymers include poly(lactic-co-glycolic acid) (PLGA), polylactic acid (PLA), and polyglycolic acid (PGA), which break down into non-toxic byproducts [19]. Engineers can tailor drug release profiles by manipulating the polymer's chemical composition, crystallinity, and molecular weight to achieve a desired degradation rate, ranging from days to months. This mechanism is fundamental to applications where the biomaterial serves a temporary purpose, such as in bioresorbable stents or tissue engineering scaffolds [19].
Stimuli-Responsive Release
Stimuli-responsive, or "smart," release mechanisms enable on-demand drug delivery in response to specific internal (endogenous) or external (exogenous) triggers. This provides a high level of spatial and temporal precision, minimizing off-target effects [8] [22].
Endogenous Stimuli: These are pathological abnormalities in the disease microenvironment. Systems can be engineered to respond to:
- pH: The slightly acidic pH of tumor microenvironments or the pH gradient in cellular compartments (endosomes/lysosomes) can trigger drug release [22] [23].
- Enzymes: Overexpressed enzymes (e.g., matrix metalloproteinases) at disease sites can cleave specific peptide sequences or chemical bonds incorporated into the biomaterial, leading to a highly specific release [20].
- Redox Potential: The significant difference in glutathione concentration between the intracellular and extracellular spaces can degrade materials containing disulfide bonds [22].
Exogenous Stimuli: These are externally applied physical triggers that allow for precise, remote-controlled release:
- Light: Near-infrared (NIR) light can be used with photothermal agents like MXene to generate heat, causing a structural change in the carrier and subsequent drug release [22].
- Magnetic Fields: Magnetic nanoparticles embedded in a hydrogel can be activated by an alternating magnetic field to generate heat, facilitating drug release [21].
- Ultrasound: Ultrasound waves can induce cavitation or thermal effects that disrupt the structure of nanocarriers, releasing their payload [22] [23].
Table 1: Comparison of Fundamental Release Mechanisms
| Mechanism | Key Principle | Trigger/Driver | Common Biomaterials | Release Kinetics Profile |
|---|---|---|---|---|
| Diffusion | Molecular motion down a concentration gradient | Concentration gradient | Alginate, Chitosan, PVA hydrogels, Layer-by-layer assemblies [7] [21] | Often first-order (Fickian); can exhibit initial burst release |
| Degradation | Erosion of the carrier matrix | Hydrolytic or enzymatic cleavage of polymer chains | PLGA, PLA, PGA, Chitosan [8] [19] | Often zero-order (constant release) possible; dependent on degradation rate |
| Stimuli-Response | Material transformation upon stimulus | pH, enzymes, redox, light, temperature, magnetic field [22] | Peptide-based systems, MXenes, PVA-CMC hydrogels, smart polymers [20] [24] [22] | Pulsatile or on-demand; highly tunable based on stimulus sensitivity |
Advanced Hybrid Systems and Combined Mechanisms
In advanced drug delivery systems, these fundamental mechanisms are rarely isolated. Hybrid systems are designed to leverage multiple mechanisms sequentially or synergistically to overcome complex biological barriers and meet dynamic therapeutic demands [21]. A prominent example is the nanoparticle-hydrogel hybrid material, which combines the high drug-loading capacity and targeted potential of nanoparticles with the biocompatibility and sustained-release properties of hydrogel matrices [21].
In such systems, the release profile is a complex interplay of mechanisms: initial diffusion from the hydrogel matrix, followed by the release of drugs encapsulated in nanoparticles, which may itself be controlled by diffusion, degradation, or a stimulus. For instance, a drug-loaded polymeric NP within a hydrogel may first be released from the hydrogel via diffusion, and once at the target site, the NP may release its payload in response to a local pH change or enzyme [21]. This multi-stage release allows for sophisticated control, such as sustained release of one therapeutic agent while providing on-demand release of another [8]. The design of these composites requires a deep understanding of the molecular interactions between the drug, nanoparticle, and hydrogel network to predict and optimize the overall release behavior [21].
Diagram 1: Hybrid system release pathways.
Experimental Protocols for Characterizing Release Mechanisms
Robust experimental characterization is essential to validate and quantify drug release mechanisms. Below are detailed methodologies for key experiments.
Protocol: In Vitro Drug Release Kinetics under Physiological and Stimuli-Responsive Conditions
Objective: To quantify the drug release profile from a biomaterial system under sink conditions and to evaluate the impact of specific stimuli (e.g., pH, enzyme, light) on the release kinetics [24] [22].
Materials:
- Test articles: Drug-loaded biomaterial (e.g., hydrogel, nanoparticles, hybrid composite)
- Release medium: Phosphate Buffered Saline (PBS), pH 7.4; and modified media for stimuli tests (e.g., acetate buffer for pH 5.5, or medium with specific enzyme)
- Dialysis bags or membrane-less methods in vials
- Thermostated water bath or shaker incubator (37°C)
- UV-Vis spectrophotometer, HPLC, or other analytical instrument for drug quantification
Procedure:
- Sample Preparation: Precisely weigh a known amount of drug-loaded biomaterial (e.g., 100 mg of hydrogel) and place it into a dialysis bag (MWCO selected to retain the carrier but allow free drug passage). Seal the bag securely.
- Initial Setup: Immerse the dialysis bag in a large volume (e.g., 50-100x the sample volume) of pre-warmed (37°C) release medium (PBS, pH 7.4) to maintain sink conditions. Place the vessel in a shaker incubator at a constant, low agitation speed (e.g., 50 rpm).
- Sampling: At predetermined time intervals (e.g., 0.5, 1, 2, 4, 8, 12, 24, 48, 72 hours...), withdraw a fixed aliquot (e.g., 1 mL) from the external release medium. Immediately replace with an equal volume of fresh, pre-warmed medium to maintain constant volume and sink conditions.
- Analysis: Quantify the drug concentration in each withdrawn sample using a pre-validated analytical method (e.g., HPLC-UV, fluorescence spectroscopy). Construct a calibration curve with known drug concentrations for accurate quantification.
- Stimuli-Responsive Triggering: For stimuli tests, after a baseline period (e.g., 4 hours), replace the entire medium with a trigger-specific medium (e.g., low pH buffer, enzyme solution). For external triggers like NIR light, expose the sample to a laser (e.g., 808 nm, 1.5 W/cm²) for a set duration (e.g., 5 minutes) at specific time points, then continue sampling as before.
- Data Processing: Calculate the cumulative drug release (%) at each time point. Plot cumulative release (%) versus time to generate the release profile. Fit the data to mathematical models (e.g., Zero-order, First-order, Higuchi, Korsmeyer-Peppas) to infer the dominant release mechanism.
Protocol: Evaluating Biomaterial Degradation and Its Correlation to Drug Release
Objective: To monitor the mass loss and morphological changes of a biodegradable biomaterial over time and correlate this degradation profile with the observed drug release profile [19].
Materials:
- Pre-weighed samples of the drug-loaded biodegradable polymer (e.g., PLGA microspheres, chitosan scaffold)
- Degradation medium (e.g., PBS, pH 7.4, with or without 0.1 mg/mL lipase or other relevant enzymes)
- Analytical balance (precision ±0.01 mg)
- Scanning Electron Microscope (SEM)
- Gel Permeation Chromatography (GPC) system
Procedure:
- Baseline Measurement: Precisely weigh (W₀) and photograph each sample. For a subset of samples, characterize initial molecular weight (Mₙ₀) via GPC and initial morphology via SEM.
- Incubation: Immerse each sample in a vial containing degradation medium and incubate at 37°C under gentle agitation.
- Monitoring: At predetermined time points (e.g., weekly), remove samples in triplicate from the incubation medium.
- Mass Loss: Rinse the samples with deionized water, lyophilize, and accurately weigh the dry mass (Wₜ). Calculate the remaining mass percentage: (Wₜ / W₀) * 100%.
- Molecular Weight Change: Analyze the molecular weight (Mₙₜ) of the dried polymer using GPC.
- Morphological Analysis: Image the samples using SEM to observe surface erosion, pore formation, and cracks.
- Correlation: Plot the degradation profile (remaining mass % and Mₙ decrease over time) alongside the drug release profile from Protocol 4.1. A strong correlation between polymer mass loss/molecular weight decrease and cumulative drug release indicates a degradation-controlled mechanism.
Table 2: Research Reagent Solutions for Key Experiments
| Reagent / Material | Function / Role in Experiment | Key Characteristics & Considerations |
|---|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable polymer for degradation-controlled release studies [8] [19]. | Varying lactide:glycolide ratios and molecular weights allow tuning of degradation rates from weeks to months. |
| Chitosan | A natural, biocompatible polymer for forming pH-sensitive hydrogels and nanoparticles [8]. | Positively charged at low pH, enabling swelling and drug release in acidic environments like tumors. |
| MXene (Ti₃C₂Tₓ) | A 2D nanomaterial acting as a photothermal agent for exogenous stimuli-response [22]. | High NIR photothermal conversion efficiency; enables light-triggered drug release from composite systems. |
| Polyethyleneimine (PEI) | A cationic polymer used for its "proton sponge" effect to enhance endosomal escape [8]. | Facilitates release from degradation in acidic cellular compartments (endosomes). |
| Enzyme (e.g., MMP-2) | A biological trigger to study enzyme-responsive drug release [20]. | Must be specific to the cleavable peptide sequence (e.g., GPLG↓V) engineered into the biomaterial. |
| Dialysis Membrane | A semi-permeable barrier for conducting in vitro release studies under sink conditions. | Molecular Weight Cut-Off (MWCO) must be selected to retain the biomaterial carrier but allow free drug diffusion. |
Visualization of Stimuli-Responsive Pathways
Stimuli-responsive systems rely on specific chemical or physical pathways to trigger drug release. The following diagram illustrates the sequence of events for endogenous and exogenous triggers.
Diagram 2: Stimuli-responsive drug release pathways.
The strategic manipulation of diffusion, degradation, and stimuli-response mechanisms is the cornerstone of advanced controlled drug delivery. As biomaterials science progresses, the integration of these mechanisms into sophisticated, multi-functional systems is becoming the standard for addressing complex therapeutic challenges. Future directions point towards the increased use of AI-assisted biomaterial design to optimize these release properties, a deeper investigation into biomaterial-immune system interactions, and the expansion of innovative platforms like microrobots and hybrid composites into diverse disease contexts [8] [25]. By mastering these fundamental release mechanisms and their interplay, researchers can continue to push the boundaries of personalized medicine, developing safer, more effective treatments that dynamically respond to the needs of the patient.
The Extracellular Matrix (ECM) as a Blueprint for Biomaterial Design
The Extracellular Matrix (ECM) is a highly complex, hierarchically organized microenvironment comprised of natural polymers, growth factors, and signaling molecules that collectively provide a structurally supportive network filled with biomolecule cues regulating cell behavior [26]. Far from being a passive structural element, the ECM actively orchestrates fundamental cellular processes—including adhesion, migration, proliferation, and differentiation—through integrated biomechanical and biochemical cues [27]. This regulatory capacity arises from its tissue-specific composition and architecture, making it indispensable for physiological homeostasis and a critical blueprint for biomaterial design in regenerative medicine and controlled drug delivery [27]. The composition of the ECM varies significantly across different tissue types and developmental stages, with its main components including collagens, elastin, laminin, fibronectin, proteoglycans, and glycosaminoglycans (GAGs) [28]. Furthermore, the ECM serves as a dynamic reservoir for various growth factors, including fibroblast growth factor (FGF), vascular endothelial growth factor (VEGF), and transforming growth factor (TGF-β), which are released in a tightly regulated manner to guide tissue development and repair processes [28]. The rising global burden of chronic diseases and organ failure has intensified the demand for advanced therapeutic strategies that address the limitations of conventional treatments, positioning ECM-inspired biomaterials as promising platforms for enhancing controlled drug delivery systems [27].
Decellularized ECM (dECM) as a Fundamental Biomaterial Platform
The Decellularization Process and Its Impact on ECM Properties
Decellularization represents a cornerstone technique in ECM-based biomaterial design, focused on removing cellular components from native tissues while preserving the intrinsic ECM structure and composition [28]. The fundamental objective is to eliminate immunogenic cellular materials—including DNA and cell membranes—that could trigger adverse host responses, while retaining the complex architecture and bioactive molecules that constitute the functional ECM [26] [28]. This process produces decellularized ECM (dECM) that can be sourced from allogeneic or xenogeneic tissues and subsequently fabricated into various biomaterial formats, including membranes, hydrogels, bio-inks, and porous structures for applications in biomaterial implants, disease models, and drug screening platforms [26].
Decellularization methodologies can be broadly classified into three main categories, each with distinct mechanisms and effects on ECM properties [28]:
- Chemical Methods: Utilize surfactants (ionic, non-ionic, zwitterionic), acids, and alkaline solutions to solubilize cell membranes and disrupt DNA-protein interactions.
- Enzymatic Methods: Employ nucleases (e.g., DNase, RNase) and proteases (e.g., trypsin) to degrade nucleic acids and protein components.
- Physical Methods: Apply freezing-thawing, mechanical pressure, and perfusion to mechanically disrupt cells and facilitate their removal.
The efficacy of decellularization and the preservation of key ECM components are quantitatively assessed through specific benchmarks, as detailed in Table 1 [28] [29].
Table 1: Key Quantitative Benchmarks for Effective Tissue Decellularization
| Parameter | Target Value | Analytical Methods | Functional Significance |
|---|---|---|---|
| DNA Content | <50 ng per mg of dry tissue weight | DNA quantification assays | Reduces immunogenic potential and inflammatory responses |
| Collagen Retention | No significant decrease compared to native tissue | Hydroxyproline assay, SDS-PAGE | Maintains structural integrity and mechanical strength |
| Glycosaminoglycan (GAG) Content | No significant decrease compared to native tissue | DMMB assay, Alcian blue staining | Preserves growth factor binding capacity and hydration |
| Scaffold Porosity | ~75% (tissue-dependent) | SEM analysis, mercury porosimetry | Facilitates cell infiltration, vascularization, and nutrient diffusion |
| Pore Size | ~123 μm (for skeletal muscle scaffolds) | SEM analysis | Enables cell migration and tissue integration |
The successful decellularization of skeletal muscle tissue, for instance, demonstrates a dramatic reduction in DNA content from 1865 ± 398.3 ng/mg in native tissue to 15.11 ± 8.13 ng/mg in decellularized tissue, while effectively preserving collagen (41.01 ± 7.17 μg/mg vs 55.33 ± 10.14 μg/mg in native tissue) and GAG content (49.30 ± 2.45 ng/mg vs 54.08 ± 2.94 ng/mg in native tissue) [29]. These parameters are critical for maintaining the bioactivity and mechanical functionality of the resulting dECM scaffolds for drug delivery applications.
dECM as a Versatile Drug Delivery Carrier
Decellularized ECM biomaterials offer immense potential as versatile drug delivery systems, with various encapsulation, bulk absorption, and conjugation techniques demonstrating success in achieving controlled and localized release of therapeutic agents [26]. From growth factors to small molecules, dECM-based materials can deliver targeted bioactive signals while mimicking the native tissue environment, thus enhancing regenerative outcomes [26]. The inherent presence of GAGs in dECM, particularly heparan sulfate, provides natural binding sites for numerous growth factors through electrostatic interactions, enabling their protection, retention, and sustained release at the target site [28] [29]. This intrinsic property has been strategically enhanced through the immobilization of heparin—a structural analog of heparan sulfate—onto dECM scaffolds to create high-affinity binding platforms for therapeutic growth factors [29].
Table 2: Growth Factor Release Profiles from Heparinized dECM Scaffolds
| Growth Factor | Initial Concentration in PRP | Release Duration (DSMS-HP) | Cumulative Release Percentage | Therapeutic Application |
|---|---|---|---|---|
| PDGF-BB | 16998.7 ± 1073.3 pg/mL | 4 days | 56.13 ± 2.91% | Angiogenesis, cell proliferation |
| FGF2 | 68.33 ± 28.18 pg/mL | 4 days | 72.22 ± 9.58% | Tissue repair, morphogenesis |
| VEGF | 1207.47 ± 292.166 pg/mL | 4 days | 67.78 ± 14.66% | Blood vessel formation |
As illustrated in Table 2, heparinized dECM scaffolds (DSMS-HP) demonstrate significantly prolonged release kinetics compared to non-heparinized controls (DSMS-P), with growth factors being released over approximately 4 days versus 1-2 days for the control group [29]. This sustained release profile is particularly valuable for therapeutic applications requiring prolonged growth factor exposure to effectively promote processes such as angiogenesis, cell proliferation, and tissue regeneration [29].
Experimental Protocols for dECM-Based Drug Delivery Systems
Protocol: Fabrication of Heparinized dECM Scaffolds for Growth Factor Delivery
This protocol details the methodology for creating affinity-based drug delivery systems using heparin-functionalized dECM, enabling controlled, prolonged release of growth factors from platelet-rich plasma (PRP) for enhanced skeletal muscle regeneration [29].
Materials and Reagents:
- Native skeletal muscle tissue (allogeneic or xenogeneic source)
- Ionic and non-ionic detergents (e.g., SDS, Triton X-100)
- DNase and RNase solutions
- N-hydroxysuccinimide (NHS) and 1-ethyl-3-(3-dimethylaminopropyl)-carbodiimide (EDC)
- Heparin sodium salt
- Platelet-rich plasma (PRP)
- Phosphate-buffered saline (PBS)
- Cryostat or freeze-drying system
Procedure:
- Tissue Decellularization:
- Rinse native skeletal muscle tissue thoroughly in distilled water to remove residual blood components.
- Immerse tissue in 1% (w/v) SDS solution for 24-48 hours with continuous agitation.
- Treat with 1% (v/v) Triton X-100 for 6 hours to remove residual cellular membranes and lipids.
- Incubate in DNase/RNase solution (50 U/mL in PBS) for 3 hours at 37°C to degrade nucleic acids.
- Wash extensively with distilled water for 72 hours to remove all detergent residues.
Scaffold Fabrication:
- Mince the decellularized tissue into small fragments and digest using an acidic pepsin solution to create a pre-gel solution.
- Neutralize the digest with NaOH and reconstitute in PBS to the desired concentration.
- Crosslink the dECM solution using EDC/NHS chemistry (5:2 molar ratio) at 4°C for 6 hours.
- Pour the crosslinked solution into molds and freeze at -80°C for 2 hours, followed by lyophilization for 48 hours to create porous scaffolds.
Heparin Functionalization:
- Prepare heparin solution (10 mg/mL in MES buffer, pH 5.5).
- Activate heparin carboxyl groups using EDC/NHS (5:2 molar ratio) for 30 minutes at room temperature.
- Incubate dECM scaffolds in the activated heparin solution for 24 hours at 4°C with gentle agitation.
- Wash extensively with PBS to remove unbound heparin.
PRP Loading:
- Immerse heparinized scaffolds in PRP solution for 2 hours at room temperature.
- Remove excess solution and rinse gently with PBS to remove surface-adsorbed proteins.
Quality Control Assessments:
- Verify decellularization efficiency through DNA quantification (<50 ng/mg dry tissue).
- Confirm collagen and GAG retention using hydroxyproline and DMMB assays, respectively.
- Assess scaffold microstructure and porosity using scanning electron microscopy.
- Validate heparin binding through toluidine blue staining.
Protocol: Functional Assessment of dECM Drug Delivery Systems
In Vitro Release Kinetics Study:
- Prepare dECM scaffolds (n=5 per group): DSMS (control), DSMS-H (heparinized), DSMS-P (PRP-loaded), DSMS-HP (heparinized and PRP-loaded).
- Immerse each scaffold in 1 mL of PBS (pH 7.4) and incubate at 37°C with gentle agitation.
- Collect 100 μL of release medium at predetermined time points (1, 2, 4, 8, 24, 48, 72, 96 hours).
- Replace with fresh PBS after each collection to maintain sink conditions.
- Quantify growth factor (PDGF-BB, FGF2, VEGF) concentrations in collected samples using enzyme-linked immunosorbent assays (ELISA).
- Calculate cumulative release percentages and generate release kinetics profiles.
In Vivo Efficacy Assessment in Volumetric Muscle Loss (VML) Model:
- Surgical Procedure:
- Anesthetize adult male mice (8-10 weeks old) using isoflurane inhalation.
- Create a critical-sized defect (approximately 4×4×2 mm) in the tibialis anterior muscle.
- Implant experimental scaffolds (DSMS, DSMS-H, DSMS-P, DSMS-HP) into the defect site.
- Suture the overlying fascia and skin layers separately.
- Post-operative Analysis:
- Euthanize animals at 2, 4, and 8 weeks post-implantation (n=6 per time point).
- Harvest implanted muscles and process for histological analysis (H&E, Masson's trichrome staining).
- Assess angiogenesis through CD31 immunohistochemistry.
- Evaluate myogenic regeneration using desmin and myosin heavy chain immunostaining.
- Quantify host cell migration into the scaffold by measuring cellular density at the implant interface.
ECM-Mimetic Biomaterials for Advanced Drug Delivery
Engineering Synthetic ECM Analogues
While dECM platforms provide exceptional bioactivity, synthetic ECM-mimetic hydrogels have been developed to overcome limitations related to batch-to-batch variability, mechanical tunability, and clinical translation potential [30]. These engineered systems are designed to replicate key features of the native ECM while offering improved reproducibility, defined composition, and tunable physical properties [30]. The polymer backbone of these synthetic hydrogels is typically engineered to reproduce the structural and biochemical features of the ECM, often through the incorporation of key matrix components or bioactive motifs such as hyaluronic acid, collagen, or RGD peptides within the hydrogel network [30].
The integration of nanomaterials into hydrogels represents a significant advancement in this field, substantially expanding their mechanical and functional properties [30]. Nanomaterials such as carbon nanotubes, gold nanoparticles, graphene, magnetic nanocomposites, and ceramic nanofillers have been incorporated into hydrogels to enhance their performance through improved mechanical strength, increased electrical conductivity, and enhanced responsiveness to stimuli [30]. These functionalities can be broadly grouped into electromagnetic responsiveness (exemplified by conductive or magnetically aligned systems), mechanical reinforcement (which enhances toughness and stretchability), and stimuli-responsiveness (which enables spatiotemporal control over cell behaviors such as migration and differentiation) [30].
Integrin-Mediated Signaling in Biomaterial Design
Integrins serve as fundamental mediators of bidirectional communication between cells and their ECM microenvironment, playing indispensable roles in tissue repair and regeneration [27]. These transmembrane receptors, composed of α and β subunits, recognize specific ECM components including collagen, fibronectin, and laminin, thereby orchestrating essential cellular processes such as adhesion, migration, proliferation, and survival [27]. The activation of integrin signaling initiates with ECM ligand binding, which induces conformational changes that promote receptor clustering and the assembly of focal adhesion complexes [27]. These specialized structures serve as mechanical and biochemical signaling hubs, recruiting adaptor proteins including talin, vinculin, and paxillin to bridge the connection between integrins and the actin cytoskeleton [27].
The following diagram illustrates the key molecular events in integrin-mediated signaling, which can be strategically leveraged in biomaterial design to enhance regenerative outcomes:
Integrin-Mediated Signaling Pathway
Central to this signaling network is the focal adhesion kinase (FAK) pathway, which, upon activation at Tyr397, recruits Src family kinases to regulate cytoskeletal dynamics and promote cell migration [27]. Parallel MAPK/ERK pathway activation regulates gene expression for proliferation and differentiation, while the PI3K/Akt pathway promotes cell survival in stressful, injured tissue microenvironments [27]. These interconnected pathways function synergistically to ensure appropriate cellular responses during the repair process [27]. The mechanical properties of the ECM exert a profound influence on integrin signaling dynamics, with substrate stiffness, topography, and ligand density collectively modulating the spatial organization and activation state of integrin clusters [27]. This mechanosensitive regulation of integrin function has inspired innovative biomaterial design strategies aimed at recapitulating key aspects of native ECM signaling, particularly through engineered matrices incorporating RGD peptide sequences that demonstrate enhanced capacity to promote cell adhesion and migration through selective engagement of αvβ3 and α5β1 integrins [27].
Experimental Workflow for dECM-Based Drug Delivery System
The following diagram outlines the comprehensive experimental workflow for developing dECM-based drug delivery systems, from tissue processing through functional assessment:
dECM Drug Delivery System Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for dECM-Based Drug Delivery Research
| Reagent/Chemical | Function | Specific Application Example |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Ionic surfactant for cell membrane disruption and DNA removal | Efficient cellular component removal during tissue decellularization [28] |
| Triton X-100 | Non-ionic surfactant for lipid dissolution | Removal of residual cellular membranes after initial decellularization [28] |
| DNase/RNase Solutions | Enzymatic degradation of nucleic acids | Elimination of immunogenic DNA/RNA fragments from decellularized tissues [28] |
| EDC/NHS Crosslinker | Zero-length crosslinking for scaffold stabilization | Enhancing mechanical properties of dECM scaffolds and conjugating bioactive molecules [29] |
| Heparin Sodium Salt | Glycosaminoglycan analog for growth factor binding | Creating affinity-based delivery systems for sustained growth factor release [29] |
| Platelet-Rich Plasma (PRP) | Natural source of multiple growth factors | Therapeutic cargo for enhanced tissue regeneration [29] |
| Toluidine Blue | Metachromatic dye for heparin detection | Qualitative assessment of heparin conjugation to dECM scaffolds [29] |
The extracellular matrix serves as an unparalleled blueprint for biomaterial design, providing both structural templates and sophisticated signaling platforms that can be engineered for controlled drug delivery applications [26] [27]. Decellularized ECM platforms offer the distinct advantage of preserving tissue-specific biochemical and architectural cues that are difficult to replicate synthetically, while strategic modifications such as heparin functionalization significantly enhance their capacity for sustained therapeutic delivery [26] [29]. The integration of nanomaterials into ECM-mimetic systems further expands their functionality, enabling enhanced mechanical properties, stimuli-responsiveness, and dynamic control over drug release profiles [30].
Despite these promising advances, challenges remain in standardization, scalability, and immune response modulation [28] [27]. Future directions in ECM-based biomaterial design are directed towards improving ECM-mimetic platforms through the development of more sophisticated biofabrication techniques, including 3D bioprinting with dECM-based bio-inks, and the creation of intelligent, responsive systems that can dynamically adapt to the changing microenvironment during tissue regeneration [26] [28]. By continuing to draw inspiration from the native ECM while leveraging advances in materials science and engineering, researchers can develop increasingly sophisticated biomaterial-based drug delivery systems that bridge the gap between structural mimicry and active biological control, ultimately enabling more effective therapeutic outcomes in regenerative medicine [27].
The interdisciplinary field of biomaterials for controlled drug delivery represents a critical convergence of material science, pharmaceutical technology, and regenerative medicine, driving revolutionary approaches to therapeutic interventions. Over the past two decades, this domain has evolved from simple passive drug carriers to sophisticated systems capable of dynamic biological interaction and spatiotemporal control over drug release. The growing emphasis on precision medicine and targeted therapies has further accelerated innovation in biomaterial-based delivery platforms, making them indispensable in addressing complex disease states. This bibliometric analysis provides a comprehensive, data-driven overview of the scientific landscape from 2005 to 2024, mapping the evolution, current state, and emerging frontiers in biomaterial-driven regenerative drug delivery research. By systematically examining publication trends, geographical contributions, institutional partnerships, and thematic shifts, this review serves as an invaluable navigational tool for researchers, funding agencies, and policy makers seeking to understand the knowledge architecture of this rapidly advancing field and identify promising trajectories for future investigation [31].
The analysis encompasses global research output from January 2005 to December 2024, with data extracted from the Science Citation Index Expanded (Web of Science Core Collection). This systematic approach enables robust quantification of the field's development through metrics including publication volume, citation impact, geographical distribution, institutional productivity, and keyword evolution. The findings presented herein not only document the remarkable expansion of biomaterials research in drug delivery but also highlight the synergistic integration of once-disparate disciplines including nanotechnology, tissue engineering, and digital health, collectively pushing the boundaries of what is therapeutically possible [31].
Quantitative Analysis of Research Growth
Global Publication Output and Impact
The period from 2005 to 2024 witnessed exponential growth in research output focused on biomaterial-driven drug delivery systems. According to the bibliometric data, a total of 885 scholarly publications were recorded globally on this topic during this twenty-year span. The annual publication count first exceeded 50 in 2017 and surpassed 100 in 2024, reaching its peak at 116 publications in 2023. This trajectory demonstrates a maximum annual growth rate of 32.4%, particularly accelerating in the most recent decade, indicating the field's rapidly increasing importance and research activity [31].
Citation analysis further substantiates the field's growing impact, with publications receiving an average of 9.41 citations per year. The highest impact year was 2010, with an impressive 16.71 citations per publication annually. This pattern suggests that while publication volume has increased dramatically in recent years, the foundational works from the earlier period continue to exert substantial influence, providing theoretical and methodological frameworks that subsequent research has built upon. The sharp increase in publications post-2020 suggests that the COVID-19 pandemic substantially accelerated research activity in this field, potentially due to increased recognition of the importance of advanced delivery systems for novel therapeutics [31].
Table 1: Annual Publication Trends in Biomaterials for Drug Delivery (2005-2024)
| Year Range | Total Publications | Key Milestones | Average Citations/Publication/Year |
|---|---|---|---|
| 2005-2009 | <100 | Foundational period | 12.35 |
| 2010-2014 | ~150 | Accelerated growth | 16.71 (peak in 2010) |
| 2015-2019 | ~300 | Exceeded 50 publications annually | 10.22 |
| 2020-2024 | ~400+ | Exceeded 100 publications annually (2024) | 8.75 |
Geographical Distribution and Collaboration Networks
Research in biomaterials for drug delivery has become a truly global endeavor, with 77 countries/regions contributing to the scientific output. The United States leads in research volume with 259 publications, representing 29.3% of the total output, followed by China with 175 publications (19.8%), and India with 76 publications (8.6%) [31]. When measuring research impact through H-index metrics, the United States maintains dominance (H-index = 78), with China (H-index = 51) and Iran (H-index = 30) completing the top tier [31].
Network analysis has identified the United States and China as central nodes in global research collaboration, with Germany, the United Kingdom, France, India, Italy, South Korea, and Australia comprising additional key contributors. The collaboration network exhibits extensive globalization patterns, featuring three principal knowledge exchange hubs: North America, Europe, and East Asia. This tripartite structure underscores the intercontinental nature of contemporary scientific cooperation and highlights how geographical diversity has strengthened the field's development through cross-pollination of ideas and methodologies [31].
Table 2: Leading Countries in Biomaterials for Drug Delivery Research (2005-2024)
| Rank | Country | Article Counts | Percentage of Total | H-index |
|---|---|---|---|---|
| 1 | United States | 259 | 29.27% | 78 |
| 2 | China | 175 | 19.77% | 51 |
| 3 | India | 76 | 8.59% | 27 |
| 4 | Iran | 67 | 7.57% | 30 |
| 5 | Italy | 60 | 6.78% | 25 |
| 6 | England | 51 | 5.76% | 24 |
| 7 | Germany | 47 | 5.31% | 22 |
| 8 | South Korea | 45 | 5.09% | 21 |
| 9 | Australia | 43 | 4.86% | 20 |
| 10 | Spain | 40 | 4.52% | 18 |
Leading Institutions and Institutional Networks
The global research landscape encompasses over 1,300 participating institutions, with Harvard University and the University of California System emerging as the most productive institutions (26 publications each), followed closely by the Chinese Academy of Sciences (24 publications) and Universidade do Minho (20 publications) [31]. Bibliometric analysis reveals distinct dimensions of scientific influence, with collaborative network mapping identifying three predominant knowledge hubs centered around the Chinese Academy of Sciences, Zhejiang University, and the National University of Singapore [31].
Citation network analysis demonstrates dense interconnection patterns among high-output institutions, suggesting reciprocal citation behaviors that reinforce their disciplinary leadership. Temporal network visualization tracks the progressive expansion of research contributions, with China, the USA, and European nations driving biomaterial-focused advances in regenerative drug delivery systems. These visualizations confirm two critical trends: the formation of self-reinforcing academic ecosystems among top-tier institutions, and the increasing globalization of interdisciplinary research in advanced therapeutic development [31].
Evolution of Research Foci and Emerging Trends
Journal Distribution and Research Areas
The analysis encompassed 324 journals contributing to global research dissemination in biomaterials for drug delivery. ACTA Biomaterialia and Biomaterials emerged as the predominant sources in this domain, with the remaining high-yield journals primarily concentrating on biomaterial engineering, molecular sciences, and pharmaceutical delivery systems [31]. Application of Bradford's law of scattering facilitated the stratification of journals into three distinct zones, identifying 19 core dissemination channels that accounted for the majority of impactful publications [31].
Analysis of research categories using VOSviewer revealed that the dominant research domains include Materials Science, Engineering, Chemistry, Polymer Science, and Science Technology Other Topics. These focal areas underscore the primary directions of current research and point to promising avenues for future advancements in the field. The persistent strength of polymer science reflects the continuous innovation in polymeric architectures for drug encapsulation and controlled release, while the growing presence of "Science Technology Other Topics" indicates the field's expanding boundaries into emerging interdisciplinary areas [31].
Table 3: Core Journals in Biomaterials for Drug Delivery Research
| Rank | Journal | Article Counts | Primary Focus |
|---|---|---|---|
| 1 | Acta Biomaterialia | 33 | Biomaterial engineering and characterization |
| 2 | Biomaterials | 31 | Fundamental biomaterial research |
| 3 | Polymers | 23 | Polymer-based delivery systems |
| 4 | International Journal of Molecular Sciences | 19 | Molecular mechanisms and interactions |
| 5 | Advanced Healthcare Materials | 18 | Translational material applications |
Keyword Evolution and Conceptual Shifts
Keyword analysis over the twenty-year period reveals a significant conceptual evolution in the field. Early research (2005-2010) was dominated by fundamental material concepts such as "biocompatibility," "scaffolds," "hydrogels," and "controlled release." The middle period (2011-2018) showed a shift toward functional sophistication with emerging terms including "targeted drug delivery," "nanoparticles," "stimuli-responsive," and "tissue engineering." The most recent period (2019-2024) demonstrates a focus on precision and personalization, with keywords such as "precision medicine," "organ-on-a-chip," "3D bioprinting," "CRISPR delivery," and "AI-assisted design" gaining prominence [8] [31] [32].
This conceptual trajectory illustrates the field's journey from developing basic biocompatible materials to creating intelligent, responsive systems capable of complex biological interactions. The emerging frontiers highlight the growing integration of digital technologies, computational approaches, and personalized strategies that collectively represent the next evolutionary phase in biomaterial-based drug delivery [8].
Emerging Research Trends and Methodological Innovations
Intelligent Responsive Biomaterials
Stimuli-responsive biomaterials represent one of the most dynamic research frontiers, with materials engineered to react to specific physiological cues or external triggers. Recent innovations include enzyme-responsive biomaterials programmed to undergo structural or functional changes when exposed to specific enzymes associated with disease states [20]. These systems enable precise control over drug release kinetics, particularly beneficial for pathological environments characterized by unique enzymatic signatures, such as tumor microenvironments or inflamed tissues [20].
Thermoresponsive hydrogels represent another advanced category, with systems like chitosan-based fast-gelling hydrogels at body temperature proving particularly useful for irregularly shaped tissue defects [8]. These materials allow controlled release of encapsulated drugs while forming a microenvironment beneficial for tissue regeneration, demonstrating the dual functionality that characterizes next-generation biomaterials. The high porosity of these hydrogels enhances cell penetration and nutrient exchange, making them excellent local delivery platforms for periodontal regeneration and other specialized applications [8].
Diagram 1: Stimuli-Responsive Biomaterial Mechanisms. This diagram illustrates the diverse triggers and therapeutic outcomes of intelligent responsive biomaterials in drug delivery.
Nanotechnology-Enabled Delivery Platforms
Nanotechnology has revolutionized drug delivery by enabling unprecedented precision at cellular and molecular levels. Recent innovations include non-viral vectors such as polymers, liposomes, and lipid nanoparticles, which are engineered with surface modifications to improve gene delivery efficiency and reduce immune responses [8]. Polymer-based nanocarriers like polyethyleneimine (PEI) utilize the "proton sponge" effect to enhance endosomal escape, while liposomes benefit from high biocompatibility and surface functionalization for targeted delivery in cardiovascular diseases and other conditions [8].
Poly(Lactic-co-Glycolic Acid)-Resveratrol (PLGA-RES) nanocomposites represent another significant advancement, combining PLGA's biodegradability with the potent antioxidant properties of RES. This innovative approach helps combat oxidative stress during cryopreservation cycles, demonstrating significantly higher oocyte viability and maturation, thus overcoming a major challenge in reproductive medicine [8]. These engineered nanoscale biomaterials showcase the potential to protect against physicochemical damage at the cellular level under severe environmental conditions, expanding applications beyond traditional drug delivery into cellular preservation and regenerative medicine [8].
Advanced Delivery Systems for Complex Diseases
Innovative delivery systems with multiple functions have become key platforms for confronting complex diseases. A notable example includes motile hydrogel microrobots for osteosarcoma treatment via magnetically propelled methods [8]. Under an external magnetic field, these microrobots penetrate tumor sites to co-deliver therapeutic agents, with the hydrogel matrix providing sustained drug release favorable for higher drug retention at the target site. Preclinical studies have shown excellent antitumor activity in both 2D and 3D tumor models without significant toxicity to healthy tissues [8].
Electrospun nanofiber scaffolds represent another advanced platform for promoting diabetic wound healing, leveraging their high surface area, tunable porosity, and biocompatibility to serve as effective localized drug delivery systems and structural supports [8]. By incorporating various therapeutic agents, these scaffolds modulate inflammation and facilitate granulation tissue formation, addressing the impaired healing processes characteristic of diabetic pathophysiology. Similarly, exosome-based therapies have emerged as promising candidates for treating orthopedic degenerative diseases, facilitating cartilage and bone repair by delivering bioactive substances such as proteins and nucleic acids [8].
Table 4: Research Reagent Solutions for Biomaterial Drug Delivery Systems
| Category | Specific Materials | Function/Application | Key Characteristics |
|---|---|---|---|
| Natural Polymers | Chitosan, Hyaluronic Acid | Thermoresponsive hydrogels, scaffolding | Biocompatibility, enzymatic degradation |
| Synthetic Polymers | PLGA, PVA-CMC, PEG | Nanoparticles, micelles, hydrogels | Controlled biodegradation, tunable properties |
| Lipid-Based Systems | Liposomes, Lipid Nanoparticles | mRNA/vaccine delivery, targeted therapy | Self-assembly, biomimetic properties |
| Inorganic Nanoparticles | Bioactive glass, Mesoporous silica, Calcium phosphate | Bone regeneration, controlled release | Mechanical strength, osseointegration |
| Stimuli-Responsive Materials | Rotaxanes, pH-sensitive polymers | Targeted drug release, smart delivery | Environmental responsiveness |
| Hybrid/Composite Materials | Polymer-ceramic composites, Hydrogel-ceramic blends | Multifunctional delivery systems | Combined mechanical/biological properties |
Micro Robotics and Digital Integration
Micro robotics represents a frontier innovation in drug delivery, utilizing tiny, soft robots that can navigate narrow spaces within the human body to dispense medicines with unprecedented precision. Recent developments include grain-sized soft robots controlled using magnetic fields that can transport up to four different drugs and release them in reprogrammable orders and doses [33]. These systems have demonstrated movement speeds of 0.30 mm to 16.5 mm per second in different body areas, with controlled movements continuing for up to 8 hours, offering remarkable potential for targeted combination therapy [33].
The integration of digital health technologies is simultaneously transforming smart drug delivery systems, improving precision, accessibility, and patient adherence. Innovations include the use of artificial intelligence in drug delivery, real-time health monitoring, and Internet of Things connectivity, enabling devices to revolutionize chronic disease management [34]. The market is witnessing growing emphasis on tailored therapies that focus on individual patient needs, with developers creating smart drug delivery systems that provide customized dosages based on specific patient characteristics, such as genetic markers or real-time health data [34]. This shift toward digitalization is driving innovation in smart drug delivery systems, potentially improving treatment outcomes and patient compliance across multiple therapeutic areas.
Diagram 2: Biomaterial Development and Evaluation Workflow. This diagram outlines the comprehensive methodology for developing and testing advanced biomaterials for drug delivery applications.
Future Perspectives and Concluding Remarks
The bibliometric analysis of the past two decades reveals a field in rapid transition, moving from simple drug carrier systems to sophisticated bio-responsive platforms capable of dynamic interaction with biological environments. Future research trajectories are likely to focus increasingly on personalization, with biomaterials designed to respond to individual patient pathophysiology rather than generic disease categories. The integration of artificial intelligence and machine learning in biomaterial design represents another promising frontier, enabling rapid optimization of material properties for specific therapeutic needs and accelerating the development timeline for new delivery systems [8].
Despite remarkable progress, significant challenges remain in scalability, safety, and regulatory translation. Current data indicates that fewer than 10% of preclinical biomaterial-based delivery systems progress to Phase III trials, highlighting the translational gap between laboratory innovation and clinical implementation [31]. Addressing this discrepancy will require enhanced collaboration between academic researchers, clinical practitioners, regulatory bodies, and industry partners to ensure that promising platforms successfully navigate the path from benchtop to bedside. Furthermore, investigating interactions between biomaterials and the immune system is critical to ensuring safety and efficacy, particularly as systems become more complex and biologically active [8].
The expanding application of innovative platforms like microrobots, nanofibers, and exosome-based delivery to diverse disease contexts will further advance their role in personalized medicine. As treatment paradigms shift toward more individualized, mechanism-based interventions, biomaterial-driven drug delivery is poised to become a foundational enabler of next-generation medicine – driving growth at the nexus of technology, biology, and patient-centered care [35]. The remarkable progress documented in this bibliometric analysis suggests that the coming decade will witness even more transformative advances as these convergent technologies mature and find their place in clinical practice.
Advanced Fabrication and Application of Biomaterial Systems in Therapeutics
The evolution of biomaterials for controlled drug delivery has been fundamentally transformed by the advent of nanocarrier engineering. These sophisticated systems, typically ranging from 1 to 1000 nanometers, are designed to overcome the limitations of conventional drug formulations, such as poor bioavailability, non-specific biodistribution, and suboptimal therapeutic indices [3]. By leveraging engineered materials at the nanoscale, these carriers protect therapeutic agents, facilitate targeted delivery to disease sites, and provide controlled release kinetics, thereby enhancing efficacy while minimizing off-target effects [36] [3].
The significance of nanocarriers extends beyond simple drug encapsulation. Their design incorporates principles of biomaterial science, pharmaceutics, and molecular biology to create systems that interact intelligently with biological environments. The clinical success of several nanocarrier-based formulations, including liposomal doxorubicin (Doxil) and polymeric nanoparticles, has validated their potential and spurred further innovation in the field [37]. This technical guide provides a comprehensive examination of three pivotal nanocarrier platforms—liposomes, polymeric nanoparticles, and dendrimers—within the broader context of biomaterial science for controlled drug delivery research.
Nanocarrier Platforms: Composition, Structure, and Functional Attributes
Liposomes
Structural Composition and Formation: Liposomes are spherical vesicles consisting of one or more concentric phospholipid bilayers enclosing aqueous compartments. This amphiphilic structure enables the encapsulation of both hydrophilic drugs (within the aqueous core) and hydrophobic drugs (within the lipid bilayers) [37]. They are typically classified based on their size and lamellarity: Small Unilamellar Vesicles (SUVs, 20-100 nm), Large Unilamellar Vesicles (LUVs, 100-1000 nm), and Multilamellar Vesicles (MLVs, >500 nm) [37].
Formation Mechanisms: Liposome preparation commonly employs thin-film hydration, ethanol injection, or detergent removal methods. The lipid film hydration technique involves dissolving lipids in an organic solvent, evaporating to form a thin film, hydrating with an aqueous buffer, and downsizing through extrusion or sonication. Active loading techniques, utilizing pH gradients or ion exchange, enable high-efficiency encapsulation of certain therapeutics [37].
Functionalization Strategies:
- Stealth Liposomes: Surface-grafted polyethylene glycol (PEG) creates a hydrophilic layer that reduces opsonization and phagocytic clearance, significantly extending circulation half-life [36] [37].
- Ligand-Targeted Liposomes: Antibodies, peptides, or small molecules conjugated to the surface enable active targeting to specific cell types or receptors [36].
- Stimuli-Responsive Liposomes: Designed with lipid compositions sensitive to environmental triggers (pH, temperature, enzymes) for controlled drug release at target sites [37].
Polymeric Nanoparticles
Material Composition and Synthesis: Polymeric nanoparticles are solid colloidal particles typically fabricated from biodegradable or biocompatible polymers. The most extensively studied include poly(lactic-co-glycolic acid) (PLGA), polylactic acid (PLA), polycaprolactone (PCL), and chitosan [3] [38]. These materials offer tunable degradation rates, mechanical properties, and drug release profiles.
Fabrication Techniques:
- Single/Double Emulsion-Solvent Evaporation: Particularly suitable for encapsulating hydrophilic/hydrophobic drugs, respectively.
- Nanoprecipitation: Involves controlled addition of a polymer solution into a non-solvent, inducing nanoparticle formation.
- Ionic Gelation: Used for chitosan-based systems, where cross-linking occurs via tripolyphosphate (TPP) ions [38].
Functional Capabilities: Polymeric nanoparticles provide exceptional versatility in surface modification, drug loading capacity, and controlled release kinetics. Their surfaces can be functionalized with targeting ligands, and their polymer composition can be engineered for stimuli-responsive behavior [3].
Dendrimers
Structural Characteristics: Dendrimers are highly branched, monodisperse, synthetic macromolecules with a symmetrical architecture radiating from a central core. Their precise nanoscale structure, defined by generations (G0, G1, G2, etc.), results in a globular shape with numerous surface functional groups [39].
Drug Loading Strategies:
- Covalent Conjugation: Drug molecules are chemically attached to surface groups.
- Host-Guest Complexation: Utilizing interior cavities for hydrophobic drug encapsulation.
- Electrostatic Interaction: Particularly for nucleic acid delivery [39].
Surface Engineering: The high density of surface functional groups enables multivalent ligand conjugation for targeted delivery. Dendrimers have shown significant promise for HIV treatment, with their ability to interact with viral envelopes and inhibit replication [39].
Table 1: Comparative Analysis of Nanocarrier Platforms
| Characteristic | Liposomes | Polymeric Nanoparticles | Dendrimers |
|---|---|---|---|
| Typical Size Range | 50-400 nm | 50-300 nm | 2-10 nm (core diameter) |
| Drug Loading Capacity | High for both hydrophilic & hydrophobic drugs | Moderate to high, depends on drug-polymer affinity | Moderate, primarily surface conjugation |
| Encapsulation Efficiency | 30-70% (passive); >90% (active loading) | 30-80% | Varies by generation and functionalization |
| Release Kinetics | Burst release followed by sustained release (days-weeks) | Typically biphasic: initial burst then sustained (weeks-months) | Dependent on conjugation chemistry and degradation |
| Scalability & Manufacturing | Established but challenges with batch-to-batch consistency | Scalable with emulsion methods; reproducibility challenges | Controlled synthesis but complex purification |
| Regulatory Status | Multiple FDA-approved products | Several FDA-approved products (e.g., PLGA-based) | Mostly in preclinical/clinical development |
Table 2: Biomaterial Composition and Functional Properties
| Nanocarrier Type | Common Materials | Key Functional Properties | Clinical Applications |
|---|---|---|---|
| Liposomes | Phosphatidylcholine, Cholesterol, PEG-lipids | Extended circulation, Passive targeting via EPR, Fusion with cell membranes | Cancer therapy (Doxil), Antifungals (AmBisome), Vaccines |
| Polymeric Nanoparticles | PLGA, PLA, Chitosan, Poly(ε-caprolactone) | Biodegradability, Controlled release, Surface functionalization | Cancer therapy, Protein delivery, Sustained release formulations |
| Dendrimers | PAMAM, PPI, Poly(L-lysine) | Monodispersity, Multivalent surface, Precise architecture | Drug/gene delivery, Antimicrobial applications, Diagnostic imaging |
Advanced Methodologies in Nanocarrier Evaluation
SCP-Nano: Single-Cell Resolution Biodistribution Analysis
Experimental Protocol: The Single Cell Precision Nanocarrier Identification (SCP-Nano) pipeline represents a breakthrough in evaluating nanocarrier biodistribution at single-cell resolution across entire organisms [40].
Workflow Steps:
- Nanocarrier Administration: Fluorescently labeled nanocarriers are administered to mice via relevant routes (intravenous, intramuscular, intranasal) at clinical doses (as low as 0.0005 mg kg⁻¹).
- Tissue Clearing: Optimized DISCO clearing protocol: Perfuse and fix mice, then clear tissues using a refined DISCO method (eliminating urea and sodium azide, reducing dichloromethane incubation) to preserve fluorescence.
- Light-Sheet Microscopy: Image entire cleared mouse bodies at approximately 1-2 µm lateral and 6 µm axial resolution.
- Deep Learning Analysis: Process imaging data using a 3D U-Net architecture with six encoding and five decoding layers (leaky ReLU activation) to detect and quantify targeted cells.
- Spatial Proteomics: Correlate nanocarrier distribution with tissue proteomic changes to understand functional impacts [40].
Key Applications: SCP-Nano has revealed route-dependent tissue tropism, with intramuscularly injected lipid nanoparticles (LNPs) reaching heart tissue and causing proteome changes suggesting immune activation. The method generalizes to various nanocarriers, including liposomes, polyplexes, and viral vectors [40].
Characterization Techniques for Nanocarrier Performance
Physicochemical Characterization:
- Size and Surface Charge: Dynamic Light Scattering (DLS) for hydrodynamic diameter; Laser Doppler Electrophoresis for zeta potential.
- Morphology: Transmission Electron Microscopy (TEM) and Atomic Force Microscopy (AFM) for structural analysis.
- Drug Loading and Encapsulation Efficiency: HPLC/UV-Vis spectroscopy after separation of unencapsulated drug.
In Vitro Release Kinetics:
- Dialyzer Method: Nanocarriers placed in dialysis membrane suspended in release medium; samples taken at predetermined intervals and analyzed for drug content.
- Sink Conditions Maintenance: Ensure release medium volume ≥5-10 times that required for drug saturation.
Cellular Uptake Mechanisms:
- Flow Cytometry: Quantitative analysis of cell-associated fluorescence from labeled nanocarriers.
- Confocal Microscopy: Spatial visualization of internalization and intracellular trafficking using specific organelle markers.
Research Reagent Solutions: Essential Materials for Nanocarrier Development
Table 3: Key Research Reagents for Nanocarrier Engineering
| Reagent Category | Specific Examples | Function in Nanocarrier Development |
|---|---|---|
| Lipid Components | DOPC, DSPC, Cholesterol, PEG-DSPE | Form lipid bilayers, modify membrane fluidity, provide stealth properties |
| Biodegradable Polymers | PLGA, PLA, Chitosan, Polycaprolactone | Form nanoparticle matrix, control degradation and release kinetics |
| Dendrimer Cores | PAMAM, PPI, Poly(L-lysine) | Provide scaffold for branched architecture and drug conjugation |
| Fluorescent Tags | Alexa Fluor dyes (647, 750), DiD, DiI | Enable tracking of nanocarriers in vitro and in vivo |
| Targeting Ligands | Folate, Transferrin, RGD peptides, Antibodies | Mediate specific binding to cellular receptors |
| Crosslinkers | Glutaraldehyde, EDC/NHS, SMCC | Facilitate conjugation of ligands to nanocarrier surfaces |
| Stabilizers & Cryoprotectants | Sucrose, Trehalose, Mannitol | Prevent aggregation during storage and freeze-drying |
Visualization of Nanocarrier Analysis Workflows
SCP-Nano Biodistribution Analysis Pipeline
Diagram 1: SCP-Nano analysis workflow for whole-body nanocarrier distribution at single-cell resolution.
Rational Design Framework for Targeted Nanocarriers
Diagram 2: Rational design framework for developing optimized nanocarrier systems.
Current Challenges and Future Perspectives
Translational Challenges
Despite significant advancements, nanocarrier engineering faces several translational hurdles:
Manufacturing and Scalability: Reproducible, cost-effective manufacturing at commercial scale remains challenging. Liposomal dispersions are particularly susceptible to stability issues, including degradation, drug leakage, and aggregation during storage [37]. Batch-to-batch consistency is difficult to maintain during scale-up from laboratory to industrial production.
Targeting Efficiency: While passive targeting via the Enhanced Permeability and Retention (EPR) effect is well-established, active targeting strategies often face biological barriers, including non-specific uptake by the reticuloendothelial system (RES) and inadequate penetration into target tissues [3] [37].
Biological Barriers: Overcoming sequential biological barriers—including systemic circulation, endothelial barriers, cellular membranes, and intracellular trafficking—requires sophisticated design strategies that remain incompletely realized [38].
Emerging Trends and Future Directions
Stimuli-Responsive Systems: Next-generation nanocarriers are incorporating triggers responsive to pathological conditions (pH, redox potential, enzyme overexpression) for spatially and temporally controlled drug release [37].
Integration with AI and Automation: Artificial intelligence is being leveraged to optimize nanocarrier formulations, predict in vivo performance, and analyze complex biodistribution data [40] [41]. Automated synthesis platforms enable high-throughput screening of nanocarrier compositions.
Hybrid and Multifunctional Systems: Combining elements of different nanocarrier platforms (e.g., lipid-polymer hybrids) creates systems with synergistic advantages. Theranostic nanocarriers integrating therapeutic and diagnostic capabilities represent another frontier [37].
Personalized Nanomedicine: Advances in biomarker identification and nanocarrier engineering are paving the way for patient-specific formulations tailored to individual disease characteristics and genetic profiles [41].
As nanocarrier engineering continues to evolve, the integration of biomaterial science with biological insights will enable increasingly sophisticated drug delivery systems that maximize therapeutic efficacy while minimizing adverse effects. The continued translation of these technologies from laboratory to clinic holds tremendous potential for addressing unmet medical needs across diverse disease areas.
The field of controlled drug delivery is undergoing a transformative shift with the development of stimuli-responsive "smart" biomaterials. These dynamic systems are engineered to respond to specific biological cues or external triggers, enabling precise spatiotemporal control over therapeutic release. This precision enhances drug efficacy at the target site while minimizing off-target effects and systemic toxicity, thereby addressing a fundamental challenge in modern pharmacotherapy [8] [42]. These advanced biomaterials are designed to interact with biological environments in a purposeful manner, moving beyond traditional passive delivery to actively participate in the therapeutic process [42].
Framed within the broader thesis on the role of biomaterials in controlled drug delivery, these systems represent a paradigm shift from inert carriers to interactive platforms. They can be engineered to respond to endogenous stimuli—such as pH variations, temperature fluctuations, or enzyme activity—that are inherent to pathological sites. Alternatively, they can be activated by exogenous stimuli—including light, magnetic fields, or ultrasound—applied from outside the body [43] [44]. This review provides an in-depth technical examination of three key endogenous stimulus mechanisms—pH, temperature, and enzymatic activation—focusing on their design principles, material foundations, responsive behaviors, and experimental evaluation for biomedical applications.
pH-Responsive Drug Delivery Systems
Mechanism and Design Principles
pH-responsive systems exploit the pH gradients that exist in both physiological and pathological contexts. The acidic tumor microenvironment (pH ~6.5-6.8), the progressively acidic compartments of the endocytic pathway (early endosomes, pH ~6.0-6.5; late endosomes, pH ~5.0-6.0; lysosomes, pH ~4.5-5.0), and inflamed or infected tissues (e.g., periodontal pockets) provide distinct pH landmarks for triggered drug release [45] [44] [46]. These systems are primarily engineered using polymers bearing ionizable functional groups that undergo protonation or deprotonation in response to local pH changes.
The two primary mechanisms underpinning pH-responsive behavior are:
- Protonation/Deprotonation: Polymers with weakly basic groups (e.g., tertiary amines, pyridine) accept protons in acidic environments, leading to increased hydrophilicity, electrostatic repulsion, and often swelling of the polymeric matrix. Conversely, polymers with weakly acidic groups (e.g., carboxylic acids, sulfonamides) donate protons in basic environments, becoming negatively charged [47] [46].
- Acid-Labile Bond Cleavage: The incorporation of chemical bonds that are stable at neutral pH but hydrolyze in acidic conditions—such as hydrazone, acetal, ketal, and cis-aconityl bonds—allows for the pH-triggered disintegration of the nanocarrier or the release of a conjugated drug [45].
Key Biomaterials and Formulations
A wide array of pH-responsive biomaterials has been developed, each with distinct characteristics and applications.
Table 1: Key Polymers and Mechanisms in pH-Responsive Drug Delivery
| Polymer/Category | Ionizable Group/Bond | pH-Switch | Response Mechanism | Typical Application |
|---|---|---|---|---|
| Poly(acrylic acid) (PAA) | Carboxylic acid | High pH (>5.5) | Deprotonation → Swelling | Intestinal drug delivery [47] |
| Chitosan (CS) | Primary amine | Low pH (<6.5) | Protonation → Swelling/Solubility increase | Colon-targeted delivery, wound healing [44] [47] |
| Poly(L-histidine) | Imidazole group | Low pH (<7.0) | Protonation → Hydrophilic shift/Micelle disruption | Tumor-targeted therapy [45] |
| Hydrazone-bonded systems | Hydrazone bond | Low pH (<6.0) | Acid hydrolysis → Drug conjugate cleavage | Targeted anticancer drug delivery [45] |
| Poly(β-amino ester) | Tertiary amine | Low pH (<6.5) | Protonation → Polymer backbone degradation/DNA release | Gene delivery [46] |
These materials are formulated into diverse delivery platforms, including polymeric nanoparticles, liposomes, micelles, nanogels, and hydrogels [45] [44] [46]. For instance, a doxorubicin-loaded hydrogel fabricated from O-allyl chitosan (OAL) and four-arm PEG-SH demonstrated higher drug release at pH 6.8 compared to more acidic environments, making it suitable for targeted cancer therapy [47].
Experimental Protocol: Evaluating pH-Responsive Drug Release
Objective: To characterize the in vitro drug release profile of a pH-responsive nanoparticle formulation (e.g., polymeric NPs or liposomes) under simulated physiological (pH 7.4) and pathological (e.g., pH 6.5 or 5.0) conditions.
Materials:
- Test Formulation: pH-responsive nanoparticles loaded with a model drug (e.g., Doxorubicin).
- Control Formulation: Non-pH-responsive nanoparticles (e.g., prepared without ionizable groups).
- Release Media: Phosphate-buffered saline (PBS) adjusted to target pH values (e.g., 7.4, 6.5, 5.0) with 0.02% w/v sodium azide to prevent microbial growth.
- Dialysis Membranes (appropriate molecular weight cutoff) or Float-A-Lyzer G2 devices.
- Spectrophotometer, Fluorometer, or HPLC system for quantifying drug concentration.
Methodology:
- Preparation: Place an aliquot of the nanoparticle suspension (equivalent to a known drug amount, e.g., 1 mg) into a dialysis device.
- Incubation: Immerse the dialysis device in a large volume (e.g., 50-100x the sample volume) of pre-warmed release media (37°C) under gentle agitation to maintain sink conditions.
- Sampling: At predetermined time intervals, withdraw a known volume (e.g., 1 mL) from the external release medium and replace it with an equal volume of fresh, pre-warmed medium to maintain constant volume.
- Analysis: Quantify the drug concentration in the sampled medium using a pre-validated analytical method (e.g., HPLC with UV/fluorescence detection).
- Data Processing: Calculate the cumulative percentage of drug released at each time point for each pH condition. Plot the mean release profiles (n=3) for comparison.
Expected Outcome: The pH-responsive formulation should demonstrate a significantly faster and more complete release of the drug in acidic media (pH 6.5 and 5.0) compared to the neutral pH 7.4, while the control formulation should show similar, slow release profiles across all pH conditions.
Diagram 1: pH-Responsive drug release experimental workflow.
Temperature-Responsive Drug Delivery Systems
Mechanism and Design Principles
Temperature-responsive, or thermosensitive, systems leverage the slight temperature elevation often found in inflamed tissues or tumors, or the transition from ambient to body temperature for in situ gelation. Their behavior is governed by a critical solution temperature, which can be either a Lower Critical Solution Temperature (LCST) or an Upper Critical Solution Temperature (UCST) [43].
- LCST Systems: These are the most prevalent for biomedical applications. Below the LCST, the polymer chains are hydrated and expanded, resulting in a soluble state. Upon heating above the LCST, the polymer undergoes a phase transition to a collapsed, hydrophobic, and insoluble state. This transition is driven by a entropy gain from the release of water molecules, which overcomes the favorable enthalpy of polymer-water hydrogen bonding [43].
- UCST Systems: These behave in the opposite manner, being insoluble below the UCST and soluble above it. They are less common in biomedicine due to their typically higher transition temperatures [43].
Key Biomaterials and Formulations
Thermosensitive hydrogels are a major class of temperature-responsive systems, prized for their injectability and ability to form depots in situ.
Table 2: Key Polymers and Properties in Temperature-Responsive Drug Delivery
| Polymer/System | Critical Temperature | Mechanism of Gelation/Response | Application Example |
|---|---|---|---|
| Poly(N-isopropylacrylamide) (PNIPAm) | LCST ~32°C | Dehydration of isopropyl groups & collapse of polymer chains above LCST. | Injectable depot for sustained drug release [43] |
| Pluronic F127 (PEO-PPO-PEO) | Critical Gelation Temperature ~20-30°C | Micellization of PPO blocks & intermicellar packing into a gel network. | Topical drug delivery, cell encapsulation [43] |
| Chitosan/β-Glycerophosphate (CS/β-GP) | Gelation at ~37°C | Thermodynamic disruption of CS-β-GP H-bonding → hydrophobic interactions. | Minimally invasive implantation, periodontal regeneration [43] [8] |
| Methylcellulose (MC) | LCST ~40-50°C | Heating disrupts H-bonds with water, enabling hydrophobic cross-linking via methoxy groups. | Pharmaceutical formulations [43] |
| PLGA-PEG-PLGA Triblock Copolymer | Sol-gel transition ~30-37°C | Dehydration of PEG segment → micelle aggregation & 3D network formation. | Long-acting protein delivery [43] |
These polymers can be formulated as free-flowing sols at room temperature, allowing for easy injection. Upon contact with the body, they rapidly transition into semi-solid gel depots that provide localized and sustained release of encapsulated therapeutics, such as stem cells, drugs, or bioactive molecules [43] [8].
Experimental Protocol: Characterizing Thermo-Gelation Properties
Objective: To determine the gelation temperature and time of a thermosensitive polymer solution (e.g., Chitosan/β-GP or PLGA-PEG-PLGA) and evaluate its drug release kinetics.
Materials:
- Polymer Solution: Sterile, purified thermosensitive polymer in buffer.
- Thermostatic Water Bath or Rheometer with temperature control.
- Inverted Tube Test Vials.
- Model Drug (e.g., a fluorescent dye or a low-MW API).
- Analytical instrument for drug quantification (e.g., spectrophotometer).
Methodology (Inverted Tube Test):
- Preparation: Aliquot 1 mL of the polymer solution into several small glass vials. For drug release studies, pre-load the solution with a known concentration of the model drug.
- Temperature Ramp: Place the vials in a water bath at a low starting temperature (e.g., 4°C). Gradually increase the bath temperature in small increments (e.g., 1-2°C).
- Gelation Point Determination: At each temperature step, tilt the vial to 90°. The gelation temperature (Tgel) is defined as the temperature at which the meniscus no longer moves within 30 seconds. This is a subjective but widely used test.
- Rheological Confirmation (Advanced): Using a rheometer, perform a temperature sweep while monitoring the storage (G') and loss (G'') moduli. Tgel is identified as the temperature where G' surpasses G'', indicating a transition from a liquid-like to a solid-like state.
- Drug Release from Gel Depot: Once Tgel is identified, form a gel depot in a release medium (PBS, 37°C) using the pre-loaded solution. Sample the release medium at intervals and quantify the released drug as described in Section 2.3.
Expected Outcome: The polymer solution will remain liquid below Tgel and form a stable gel above it. The drug release from the gel depot will typically follow a sustained, diffusion-controlled profile over an extended period.
Diagram 2: LCST polymer phase transition mechanism.
Enzyme-Responsive Drug Delivery Systems
Mechanism and Design Principles
Enzyme-responsive biomaterials are engineered to undergo specific, catalytic changes in the presence of disease-associated enzymes that are overexpressed at the target site. This provides a high degree of specificity, as the response is contingent on the unique enzymatic "fingerprint" of the pathology [20]. Common enzymatic triggers include matrix metalloproteinases (MMPs), phospholipases, glycosidases, and proteases (e.g., cathepsins, caspases) that are upregulated in cancer, inflammation, and other pathological conditions [20].
The design strategies involve:
- Enzyme-Specific Cleavable Linkers: Incorporating short peptide sequences, sugar units, or specific chemical bonds that are recognized and cleaved by the target enzyme into the backbone or cross-links of a polymer or between the drug and its carrier.
- Structural Transformation: Cleavage events can lead to the dissolution of a hydrogel, the disassembly of a nanoparticle, a charge reversal on a surface, or the activation of a prodrug, thereby releasing the therapeutic payload [20].
Key Biomaterials and Applications
These systems are highly versatile and can be tailored for specific diseases based on the enzyme profile. For instance, MMP-responsive hydrogels are used for tumor-targeting, as MMPs are overexpressed in the tumor microenvironment and facilitate metastasis [20]. Similarly, gingipain-responsive hydrogels have been developed for periodontitis treatment, releasing antibiotics specifically upon exposure to proteases produced by Porphyromonas gingivalis [44]. Another example involves caspase-3 responsive systems that can amplify apoptosis in cancer cells.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Developing Stimuli-Responsive Systems
| Reagent / Material | Function / Role | Example Use Case |
|---|---|---|
| Chitosan (CS) | Natural cationic polymer for pH-responsive matrices and thermogels (with β-GP). | pH-dependent swelling for colon delivery; in situ gelation for periodontal defects [43] [47]. |
| Poly(N-isopropylacrylamide) (PNIPAm) | Synthetic polymer with LCST near physiological temperature. | Gold standard for creating thermosensitive hydrogels and cell culture substrates [43]. |
| Pluronic F127 | Triblock copolymer (PEO-PPO-PEO) for thermogelling systems. | Forming injectable depots for sustained drug release and as a bioink [43]. |
| Poly(lactic-co-glycolic acid) (PLGA) | Biodegradable, biocompatible polyester for nanoparticle and microparticle fabrication. | pH/enzyme-sensitive NPs when functionalized; controlled release carrier [44] [42]. |
| Doxorubicin HCl | Model chemotherapeutic drug; fluorescent properties aid in tracking. | A benchmark drug for evaluating release kinetics from pH- or enzyme-responsive carriers in cancer models [45] [47]. |
| N,N'-Methylenebis(acrylamide) (MBAA) | Crosslinker for vinyl polymers, creates network structure in hydrogels. | Tuning the mesh size and mechanical strength of responsive hydrogels [47]. |
| Matrix Metalloproteinase (MMP) Substrate Peptide | Enzyme-cleavable crosslinker (e.g., GPLGVRG). | Designing enzyme-responsive hydrogels that degrade in the tumor microenvironment [20]. |
| Sodium β-Glycerophosphate (β-GP) | Polyol salt used to impart thermosensitivity to chitosan solutions. | Preparing injectable CS/β-GP hydrogels that gel at body temperature [43]. |
Stimuli-responsive 'smart' biomaterials represent a cornerstone of next-generation drug delivery systems. By harnessing pathological cues like local acidity, temperature shifts, and enzyme activity, they achieve unprecedented precision in therapeutic targeting. This in-depth technical guide has detailed the core mechanisms, key materials, and experimental approaches underpinning pH-, temperature-, and enzyme-activated release systems.
The future of this field lies in the convergence of these technologies to create multi-responsive systems that can react to complex biological scenarios, thereby enhancing specificity and efficacy [45] [46]. Furthermore, the integration of artificial intelligence and machine learning is poised to accelerate the discovery and optimization of novel smart biomaterials, moving beyond traditional trial-and-error approaches [42]. As these systems mature through rigorous preclinical validation and address challenges related to scalability, reproducibility, and regulatory approval, they hold the definitive potential to usher in a new era of personalized, effective, and safe therapeutics.
The efficacy of conventional chemotherapeutic agents is often hampered by their lack of specificity, leading to systemic toxicity and damage to healthy tissues [48] [49]. Within the broader thesis on the role of biomaterials in controlled drug delivery systems, targeting strategies are paramount for directing therapeutic agents to the site of disease. Biomaterials, engineered as nanoparticles or scaffolds, provide the foundational platform upon which these strategies are built [50] [51]. They can be structurally designed to control drug release kinetics, improve bioavailability, and interface effectively with biological systems [52]. The two principal paradigms for achieving site-specific delivery are passive targeting, which leverages the unique pathophysiological characteristics of diseased tissues, and active targeting, which employs biological ligands for receptor-mediated uptake [48] [53]. This whitepaper provides an in-depth technical analysis of both mechanisms, detailing their principles, methodologies, and experimental protocols, framed within the context of advanced biomaterials research.
Passive Targeting: The Enhanced Permeability and Retention (EPR) Effect
Core Principles and Pathophysiological Basis
The EPR effect, first described by Maeda and Matsumura in 1986, is a cornerstone phenomenon in cancer nanomedicine [48] [54]. It describes the selective accumulation of macromolecules and nanoparticles in solid tumors due to the distinctive features of the tumor vasculature and microenvironment [55].
The mechanism is underpinned by two key pathophysiological processes:
- Enhanced Permeability: Tumor blood vessels, formed through rapid and chaotic angiogenesis, are highly abnormal. They exhibit discontinuous endothelium, a lack of smooth muscle, and poor pericyte coverage, creating fenestrations ("gaps") between endothelial cells ranging from 200 to 2000 nm in size [48] [54]. This compromised vascular architecture allows nanoparticles to extravasate from the bloodstream into the tumor interstitium far more readily than in normal tissues, where endothelial junctions are tight (typically <10 nm) [48].
- Enhanced Retention: Tumors frequently exhibit impaired or absent lymphatic drainage. While normal tissues efficiently clear interstitial fluid and macromolecules via the lymphatic system, this function is deficient in tumors. Consequently, nanoparticles that have extravasated are not effectively removed and are retained within the tumor tissue for prolonged periods [48] [55].
The EPR effect is not a static condition but a dynamic process influenced by various vascular mediators, including vascular endothelial growth factor (VEGF), bradykinin, nitric oxide (NO), and prostaglandins, which further enhance vascular permeability [55] [54]. The tumor microenvironment (TME), characterized by hypoxia, acidosis, and elevated interstitial fluid pressure (IFP), also plays a critical and often complicating role in the efficiency of the EPR effect [48] [55].
Experimental Protocol: Evaluating the EPR Effect In Vivo
Objective: To quantify the accumulation of a model nanocarrier in a subcutaneous tumor mouse model via the EPR effect.
Materials:
- Nanoparticles: Fluorescently labeled (e.g., DiR, Cy5.5) PEGylated liposomes (~100 nm diameter) [48] [55].
- Animal Model: Immunodeficient mice (e.g., nude or SCID) bearing subcutaneous human tumor xenografts (e.g., MDA-MB-231 breast carcinoma) [54].
- Imaging System: In vivo fluorescence imaging system (IVIS) or similar.
Methodology:
- Nanoparticle Administration: Inject fluorescently labeled liposomes intravenously via the tail vein (typical dose: 5 mg/kg phospholipid in 100-200 µL PBS) [56].
- In Vivo Imaging: At predetermined time points post-injection (e.g., 1, 4, 24, 48 hours), anesthetize mice and image them using the IVIS system to monitor the real-time biodistribution and tumor accumulation of the fluorescence signal.
- Ex Vivo Analysis: At the endpoint (e.g., 48 hours), euthanize the mice. Excise the tumor and major organs (liver, spleen, kidneys, heart, lungs). Image the organs ex vivo to quantitatively compare the fluorescence intensity, which correlates with nanoparticle accumulation.
- Data Quantification: Calculate the tumor-to-background ratio or the percentage of injected dose per gram of tissue (%ID/g) from the ex vivo fluorescence data [56].
Technical Considerations:
- Controls: Include a group injected with free fluorescent dye to demonstrate that accumulation is specific to the nanocarrier's size and properties.
- EPR Heterogeneity: The extent of the EPR effect is highly variable between tumor types, models, and individual animals. Using early-stage tumors (100-500 mm³) is recommended for a more pronounced and homogeneous EPR effect [54].
Strategies to Overcome Heterogeneity and Enhance the EPR Effect
A significant challenge in clinical translation is the heterogeneity of the EPR effect. Several pharmacological and physical strategies have been developed to augment it, as detailed in the table below.
Table 1: Strategies to Enhance the EPR Effect for Improved Drug Delivery
| Strategy Category | Specific Intervention | Mechanism of Action | Key Findings & Experimental Evidence |
|---|---|---|---|
| Pharmacological: Vasomodulation | Angiotensin II (AT II) [54] | Induces hypertension, increasing tumor blood flow and perfusion. | Preclinical studies show up to 2-fold increase in nanoparticle accumulation in tumors. |
| Pharmacological: Vasomodulation | Nitroglycerin (NO donor) [54] | Relaxes vascular smooth muscle, improving blood flow and permeability. | Clinical and preclinical evidence of enhanced delivery of nanomedicines. |
| Pharmacological: Vascular Normalization | Anti-VEGF/VEGFR agents (e.g., DC101 antibody) [54] | "Prunes" immature vessels and normalizes the remaining vasculature, reducing IFP and improving perfusion. | In breast tumor models, led to a 3-fold increase in accumulation of 12 nm Abraxane particles [54]. |
| Pharmacological: Stroma Modulation | Enzyme inhibitors (e.g., Losartan) [48] | Targets the dense extracellular matrix (ECM) in desmoplastic tumors (e.g., pancreatic cancer) to reduce barrier function. | Increases nanoparticle penetration and diffusion throughout the tumor. |
| Physical Methods | Mild Hyperthermia [48] | Applies localized heat (∼40-42°C) to increase blood flow and vascular permeability. | Can enhance extravasation of nanocarriers by dilating tumor blood vessels. |
| Physical Methods | Radiation Therapy [48] | Can increase vascular permeability in a dose-dependent manner. | Used to locally enhance the EPR effect at the tumor site. |
| Physical Methods | Sonoporation (Ultrasound) [48] | Utilizes microbubbles and ultrasound to temporarily disrupt endothelial junctions. | Creates transient openings for enhanced nanoparticle extravasation. |
The following diagram illustrates the core principles of the EPR effect and the strategies used to enhance it.
Diagram 1: The EPR effect and enhancement strategies. The EPR effect arises from leaky tumor vasculature and defective lymphatic drainage. Enhancement strategies target these features.
Active Targeting: Ligand-Receptor Interactions
Core Principles and Ligand Classes
Active targeting involves the surface functionalization of nanocarriers with biological ligands that specifically bind to receptors overexpressed on target cells, such as cancer cells or endothelial cells of tumor vasculature [49] [53]. This strategy serves two primary functions:
- Increased Cellular Uptake: Facilitates receptor-mediated endocytosis of the nanocarrier, enhancing internalization and intracellular drug delivery [53].
- Improved Specificity: Reduces off-target effects by concentrating the therapeutic payload on cells bearing the target receptor [49].
A wide variety of targeting ligands have been explored, each with distinct advantages and limitations. The selection of a ligand is a critical design parameter that depends on the application, target receptor, and required physicochemical properties of the final formulation.
Table 2: Classes of Targeting Ligands for Active Drug Delivery
| Ligand Class | Key Characteristics | Example Ligand & Target Receptor | Advantages | Disadvantages |
|---|---|---|---|---|
| Antibodies | Full-length immunoglobulins (e.g., Cetuximab) [53] | EGFR | High specificity and affinity. | Large size limits conjugation density; high cost; potential immunogenicity. |
| Engineered Proteins | Small, engineered protein domains (e.g., Affibodies) [53] | HER2 | Small size allows high density conjugation; high affinity and specificity. | Requires protein engineering expertise. |
| Peptides | Short amino acid sequences (e.g., RGD peptide) [56] [53] | αvβ3 Integrin | Small size, low cost, ease of conjugation, good stability. | Can have lower affinity than antibodies. |
| Aptamers | Short, single-stranded DNA or RNA oligonucleotides [49] | Various (e.g., PSMA) | High specificity, small size, chemical synthesis, good reproducibility. | Metabolic instability, potential for nuclease degradation. |
| Small Molecules | Low molecular weight compounds (e.g., Folic Acid) [49] | Folate Receptor (FR) | Small size, chemical simplicity, biocompatibility, low cost, non-immunogenic. | Limited targeting scope, limited load capacity. |
| Polysaccharides | Natural polymers (e.g., Hyaluronic Acid) [53] | CD44 | Can serve as both carrier and targeting moiety; biodegradable. | Structural complexity; targeting and affinity variation. |
Experimental Protocol: Conjugating Folic Acid to PLGA Nanoparticles
Objective: To synthesize and characterize folic acid-conjugated PLGA nanoparticles for targeted delivery to folate receptor-positive cancer cells.
Materials:
- Polymers: PLGA (50:50, acid-terminated), PLGA-PEG-NH₂ (block copolymer), Folic Acid.
- Coupling Reagents: N-Hydroxysuccinimide (NHS), N-(3-Dimethylaminopropyl)-N'-ethylcarbodiimide (EDC).
- Solvents: Dimethylformamide (DMF), Dichloromethane (DCM), Acetone.
Synthesis Methodology:
- Activation of Folic Acid: Dissolve folic acid (1 mmol) and a 2.5-fold molar excess of both EDC and NHS in anhydrous DMF. Stir the reaction mixture for 4 hours at room temperature in the dark to form the NHS-ester of folic acid [49].
- Conjugation to Polymer: Add the activated folic acid solution dropwise to a solution of PLGA-PEG-NH₂ (1 mmol NH₂ groups) in DMF. Allow the conjugation reaction to proceed for 12-24 hours under constant stirring in the dark.
- Purification & Precipitation: Purify the resulting FA-PLGA-PEG copolymer by dialysis against DMF for 24 hours to remove unreacted molecules, followed by dialysis against deionized water. Lyophilize the final product.
- Nanoparticle Formulation: Prepare nanoparticles using a single or double emulsion-solvent evaporation method.
- Drug Loading: Dissolve the FA-PLGA-PEG copolymer, plain PLGA, and a hydrophobic drug (e.g., Paclitaxel) in DCM.
- Emulsification: Emulsify the organic phase in an aqueous polyvinyl alcohol (PVA) solution using a probe sonicator to form a primary water-in-oil emulsion (W/O). This is then emulsified into a larger volume of PVA solution to form a double (W/O/W) emulsion.
- Solvent Evaporation: Stir the final emulsion overnight to evaporate the organic solvent and harden the nanoparticles.
- Collection: Collect the nanoparticles by ultracentrifugation, wash with water to remove PVA, and resuspend in buffer or lyophilize for storage [49] [56].
Characterization:
- Size and Zeta Potential: Determine hydrodynamic diameter and surface charge using Dynamic Light Scattering (DLS).
- Ligand Confirmation: Confirm the presence of surface folic acid using Fourier-Transform Infrared Spectroscopy (FTIR) or X-ray Photoelectron Spectroscopy (XPS).
- Cellular Uptake: Evaluate targeting efficiency by incubating nanoparticles with FR-positive (e.g., KB cells) and FR-negative cells. Use flow cytometry or confocal microscopy to quantify internalization, demonstrating superior uptake in FR-positive cells [49].
Comparative Analysis of Targeting Strategies
The choice between passive and active targeting, or their combination, is a fundamental decision in drug delivery system design. The following table provides a direct comparison.
Table 3: Comparative Analysis of Passive vs. Active Targeting Strategies
| Parameter | Passive Targeting (EPR) | Active Targeting (Ligand-Mediated) |
|---|---|---|
| Mechanism | Physicochemical & pathophysiological (size, vascular leakiness, poor drainage). | Biological (specific ligand-receptor binding). |
| Primary Goal | Selective accumulation in the tumor interstitium. | Enhanced cellular internalization and increased tumor cell specificity. |
| Key Factors | Nanoparticle size (40-400 nm), shape, surface charge, and PEGylation for long circulation [48] [55]. | Ligand specificity, receptor density, binding affinity, and ligand density on nanoparticle surface. |
| Tumor Accumulation (Typical %ID/g) | Generally low; a meta-analysis showed a median of ~0.7% of the injected dose (ID) reaches the tumor [48]. | Can significantly enhance cellular uptake, but does not always dramatically increase the total tumor accumulation compared to passive targeting alone [48] [56]. |
| Advantages | Relatively simple nanocarrier design; proven clinical success (Doxil, Abraxane) [48]. | Potential for higher intracellular drug concentration; ability to target specific cell populations (e.g., cancer stem cells); can target disseminated and metastatic sites where EPR is weak [48] [53]. |
| Limitations/Challenges | High heterogeneity between tumors and patients; inadequate tumor accumulation; inability to distinguish between tumor and healthy endothelial cells [48] [54]. | Complex design and manufacturing; potential for immunogenicity; cost; receptor saturation and downregulation; may compromise nanoparticle stealth if PEGylation is insufficient [48] [49]. |
The workflow for developing a dual-passive and active targeted nanocarrier is summarized below.
Diagram 2: Development workflow for a targeted nanocarrier. The process involves fabricating a core nanoparticle, optimizing its properties for passive targeting, conjugating ligands for active targeting, and subsequent validation.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs key materials and reagents essential for research in targeted drug delivery, as featured in the cited studies and experimental protocols.
Table 4: Essential Research Reagents for Targeted Drug Delivery Systems
| Reagent/Material | Function/Application | Specific Examples from Literature |
|---|---|---|
| Biodegradable Polymers | Form the core matrix of nanoparticles; control drug release kinetics. | PLGA [56], PEG [48] [55], PLGA-PEG block copolymer [50], Hyaluronic Acid (HA) [53]. |
| Lipids | Primary components of liposomal nanocarriers. | Phospholipids, cholesterol (used in Doxil) [48]. |
| Targeting Ligands | Confer specificity for active targeting. | Folic Acid [49], RGD Peptide [56], Cetuximab (anti-EGFR antibody) [53], HER2-specific Affibody [53]. |
| Coupling Agents | Facilitate covalent conjugation of ligands to nanocarriers. | EDC, NHS (for carbodiimide chemistry) [49]. |
| Cross-linkers | Used in biomaterial scaffold fabrication and some nanoparticle systems. | Maleimide-functionalized PEG (PEG-MAL) for thiol-based conjugation [50]. |
| Imaging Agents | Enable tracking of nanocarrier biodistribution and accumulation. | Fluorescent dyes (DiR, Cy5.5), Superparamagnetic Iron Oxides (SPIO) for MRI [56]. |
| Advanced Nanomaterials | Provide high surface area, stimuli-responsiveness, and multifunctionality. | Biodegradable Graphene Nanocomposites (BGNs) [52], Gold Nanoparticles (AuNPs) [55]. |
Within the paradigm of biomaterials for controlled drug delivery, passive and active targeting strategies are not mutually exclusive but are highly complementary. The EPR effect provides the foundational mechanism for achieving initial, broad accumulation of nanocarriers within the tumor tissue. Subsequently, active targeting ligands function to precisely enhance cellular uptake and specificity at the target site [48]. The future of the field lies in the rational design of "smart" biomaterials that integrate both strategies while also incorporating elements to overcome biological barriers, such as matrix-digesting enzymes or stimuli-responsive drug release mechanisms [48] [52]. Furthermore, the use of companion imaging diagnostics (theranostics) to pre-select patients based on EPR competence is a critical step toward personalized nanomedicine and improved clinical translation [56] [54]. The experimental protocols and data summarized in this technical guide provide a framework for researchers to design, synthesize, and evaluate the next generation of targeted drug delivery systems.
Cancer Nanomedicine: Targeted Therapies and Intelligent Delivery Systems
Advanced Nanocarrier Platforms
Table 1: Biomaterial Platforms in Cancer Nanomedicine
| Platform | Key Material Composition | Therapeutic Payload | Targeting Mechanism | Application |
|---|---|---|---|---|
| Self-assembled Protein Nanoparticles [57] | Cytotoxic proteins | Self-delivered cytotoxic proteins | Targeting CXCR4+ metastatic cancers | Metastatic cancer therapy |
| Polymeric Nanocarriers [58] | PEGylated PLGA, cyclodextrin-based polymers | Chemotherapeutic agents | Passive & active tumor targeting (ligand functionalization) | Liver cancer therapy |
| Stimuli-Responsive Hydrogels [8] [59] | Chitosan, PVA-CMC, composite polymers | Drugs, immunotherapeutic agents | Response to tumor microenvironment (pH, temperature) | Localized & sustained drug delivery |
| Graphene Nanocomposites [52] | Biodegradable graphene oxide (GO), reduced GO (rGO) | Aromatic drug molecules via π-π stacking | High drug loading; spatiotemporally controlled release | Combination therapy & imaging |
Experimental Protocol: Microfluidic Fabrication of Polymeric Nanocarriers
Objective: To synthesize polymeric nanocarriers with controlled size, surface chemistry, and payload distribution for targeted liver cancer therapy [58].
Materials and Methods:
- Polymer Solution: Prepare PLGA-PEG copolymer solution in organic solvent (e.g., acetonitrile) at 10 mg/mL concentration.
- Aqueous Phase: Prepare surfactant solution (e.g., 1% PVA) in deionized water.
- Drug Loading: Dissolve chemotherapeutic agent (e.g., Doxorubicin) in polymer solution at 5% w/w ratio.
- Microfluidic Setup: Utilize a droplet-based microfluidic chip with precisely controlled flow rates.
- Fabrication: Introduce organic and aqueous phases into the microfluidic device at optimized flow rate ratios (typically 1:5 organic-to-aqueous phase).
- Collection & Purification: Collect nanoparticle suspension and centrifuge at 15,000 rpm for 30 minutes.
- Characterization: Analyze particle size distribution (dynamic light scattering), surface charge (zeta potential), and drug encapsulation efficiency (HPLC).
Diagram 1: Microfluidic nanocarrier synthesis workflow for liver cancer therapy.
The Scientist's Toolkit: Cancer Nanomedicine
Table 2: Essential Research Reagents for Cancer Nanomedicine
| Reagent/Material | Function | Example Application |
|---|---|---|
| PEGylated PLGA | Biodegradable polymer core for drug encapsulation; PEG enhances circulation time [58]. | Liver cancer nanocarriers |
| Targeting Ligands | Surface functionalization for active targeting (e.g., peptides, antibodies) [58]. | CXCR4+ cancer targeting [57] |
| Stimuli-Responsive Polymers | Enable drug release in response to tumor microenvironment (pH, enzymes) [8]. | Intelligent hydrogel systems |
| Graphene Oxide (GO) | High surface area for drug loading via π-π stacking; composite reinforcement [52]. | Multifunctional nanocomposites |
Cardiovascular Implants: Engineered Drug-Eluting Systems
Active Implantable Drug Delivery Systems (AIDDS)
Active Implantable Drug Delivery Systems (AIDDSs) represent a specialized class of devices that actively regulate therapeutic agent release through internal actuation or control mechanisms [60]. These systems integrate drug reservoirs, actuation units, control electronics, and communication interfaces to achieve programmable dosing.
Table 3: Engineering Features of Active Implantable Drug Delivery Systems
| System Component | Technical Specifications | Functional Requirements |
|---|---|---|
| Actuation Mechanism | Electrothermal, electrochemical, piezoelectric | On-demand drug release capability |
| Power Source | Biodegradable batteries, wireless transfer | Long-term operation (months to years) |
| Drug Reservoir | Nano-porous membranes, refillable containers | Stable drug storage, protection from degradation |
| Control System | Microcontrollers, closed-loop sensors | Programmable dosing, physiological feedback |
Experimental Protocol: Implantable Reservoir System Testing
Objective: To evaluate the in vitro release kinetics and biocompatibility of an active implantable drug delivery system for cardiovascular applications [60].
Materials and Methods:
- Device Fabrication: Manufacture implantable reservoir (1-5 mL capacity) with nano-porous silicon membrane (pore size: 5-10 nm).
- Drug Loading: Fill reservoir with anticoagulant (e.g., Heparin) or anti-proliferative drug solution at physiological concentration.
- Release Testing: Immerse device in simulated body fluid (pH 7.4) at 37°C with constant agitation.
- Sampling & Analysis: Collect aliquots at predetermined intervals (1, 4, 8, 24 hours, then daily) for 30 days.
- Analytical Method: Use HPLC-MS to quantify drug concentration in release medium.
- Kinetic Modeling: Apply zero-order, first-order, and Higuchi models to release data.
- Biocompatibility Assessment: Perform ISO 10993-5 cytotoxicity testing using human endothelial cell lines.
Diagram 2: AIDDS component interaction for controlled cardiovascular drug release.
Tissue Engineering Scaffolds: Integrated Regeneration and Delivery
Biomaterial Scaffolds with Controlled Biofactor Delivery
Tissue engineering scaffolds have evolved from passive structural supports to active systems that provide spatiotemporal control over bioactive factor delivery [61] [62]. These advanced scaffolds are particularly crucial for cartilage regeneration, where controlled presentation of growth factors is essential for directing stem cell differentiation and tissue maturation [62] [63].
Table 4: Biomaterial Scaffolds for Controlled Drug Delivery in Tissue Engineering
| Scaffold Type | Material Composition | Bioactive Agents | Release Mechanism | Target Application |
|---|---|---|---|---|
| Natural Polymer-Based | Collagen, Hyaluronic Acid, Chitosan, Silk Fibroin [63] | TGF-β, BMP-2, IGF-1 | Diffusion, degradation-controlled release [62] | Cartilage regeneration |
| Synthetic Hydrogels | PVA, PLGA, thermosensitive polymers [8] | Growth factors, antibiotics | Swelling, environmentally responsive release | Periodontal, bone repair |
| Bionic Composite Scaffolds | Silk fibroin, gelatin-hydroxyapatite [63] | Drugs, cytokines | Surface topography-mediated release | Immunomodulation |
| Graphene Nanocomposites | GO-Chitosan, rGO-Gelatin [52] | Small molecules, peptides | Stimuli-responsive (pH, NIR) | Neural, bone tissue engineering |
The Scientist's Toolkit: Tissue Engineering Scaffolds
Table 5: Essential Research Reagents for Tissue Engineering Scaffolds
| Reagent/Material | Function | Application Example |
|---|---|---|
| Type I/II Collagen | Natural ECM component providing cell adhesion sites [63]. | Collagen-HA hydrogel for hyaline cartilage [63] |
| Silk Fibroin | High mechanical strength, slow degradation, maintains chondrocyte phenotype [63]. | Load-bearing cartilage scaffolds |
| Chitosan | Biocompatible, biodegradable, antibacterial properties [63]. | Clinical cartilage repair scaffolds |
| Graphene Oxide (GO) | Mechanical reinforcement, electrical conductivity, drug adsorption [52]. | Neural tissue engineering |
Experimental Protocol: Development of Drug-Activated Scaffolds
Objective: To fabricate and characterize a biomimetic scaffold with controlled spatiotemporal release of multiple growth factors for cartilage tissue engineering [61] [62].
Materials and Methods:
- Polymer Solution Preparation: Dissolve chitosan (2% w/v) in acetic acid (1% v/v) and mix with graphene oxide (0.5% w/v) suspension.
- Growth Factor Incorporation: Add TGF-β3 (10 ng/mL) and BMP-2 (50 ng/mL) to polymer solution using dual-compartment syringe.
- Scaffold Fabrication: Employ 3D bioprinting at 20°C with 150 μm nozzle diameter, 15 mm/s printing speed.
- Cross-linking: Immerse scaffolds in tripolyphosphate solution (2% w/v) for 30 minutes.
- Release Kinetics: Incubate scaffolds in PBS (pH 7.4) at 37°C with constant shaking.
- Bioactivity Assessment: Seed human mesenchymal stem cells (hMSCs) at 10,000 cells/scaffold and culture in chondrogenic medium.
- Analysis: Evaluate cell viability (Live/Dead assay), chondrogenic differentiation (GAG/DNA content), and gene expression (SOX9, COL2A1).
Diagram 3: Workflow for developing drug-activated scaffolds in cartilage tissue engineering.
The field of controlled drug delivery is undergoing a paradigm shift, moving from simple systemic administration to sophisticated targeted therapies that enhance therapeutic efficacy while minimizing side effects. This transformation is being driven by the convergence of three innovative platforms: 3D bioprinting, electrospinning, and organ-on-a-chip (OoC) technologies. Within the context of biomaterials research, these platforms enable unprecedented control over the spatiotemporal release of active pharmaceutical compounds, creating new possibilities for therapeutic and regenerative medicine [64] [65].
Biomaterials serve as the foundational element that unites these technologies, providing the structural and chemical basis for controlled release systems. Advances in polymers, hydrogels, nanomaterials, and biocomposites are addressing critical challenges in drug stability, controlled release kinetics, and site-specific targeting [2]. The emergence of stimuli-responsive biomaterials, triggered by pH, temperature, or enzymes, further enhances therapeutic efficacy and adaptability for personalized treatment approaches [7] [2]. This technical guide explores the integration of these advanced platforms, providing detailed methodologies, comparative analysis, and future directions for researchers and drug development professionals working at the intersection of biomaterials and controlled drug delivery.
Technology-Specific Analysis
3D Bioprinting for Drug Delivery
2.1.1 Fundamental Principles and Applications Three-dimensional bioprinting is transforming the delivery of active pharmaceutical compounds by enabling patient-specific solutions that enhance treatment efficacy and safety. This technology allows for the fabrication of complex delivery systems containing drugs, cells, and various biomolecules with controlled and sustained release profiles [64]. By leveraging bioinks with tunable properties, 3D bioprinting enables localized drug administration, reducing systemic side effects while improving bioavailability [64]. The technology particularly excels in creating structures that mimic native tissue architecture, making it invaluable for both therapeutic applications and in vitro testing platforms.
A significant advancement in this field is in situ 3D bioprinting, which facilitates the direct deposition of therapeutic agents at the site of injury or disease. This approach enhances precision medicine and supports tissue regeneration by providing spatially controlled drug release exactly where needed [64]. The integration of biocompatible bioinks with nanomedicines minimizes toxicity, enhances drug retention, reduces adverse effects, and enables personalized treatments, significantly improving therapeutic outcomes and pharmacokinetics [64].
2.1.2 Current Challenges and Limitations Despite these advancements, challenges remain in obtaining ideal biomaterial properties, post-printing modifications, printability, and biodegradability, all critical for clinical translation [64]. The resolution of bioprinted structures, vascularization of constructs, and long-term stability of incorporated bioactive agents represent additional hurdles that must be addressed to fully realize the potential of this technology in clinical settings.
Table 1: Key Parameters in 3D Bioprinting for Drug Delivery
| Parameter Category | Specific Parameters | Impact on Drug Delivery |
|---|---|---|
| Bioink Properties | Viscosity, gelation kinetics, biocompatibility, functional groups | Determines drug loading capacity, release kinetics, and cell viability |
| Structural Design | Porosity, pore size, geometric complexity, internal architecture | Influences drug diffusion rates and tissue integration |
| Printing Parameters | Nozzle diameter, printing speed, pressure, resolution | Afforts precision of drug placement and structural integrity |
| Post-processing | Crosslinking method, sterilization, maturation time | Modifies release profile and mechanical stability |
Electrospinning Technology
2.2.1 Technical Fundamentals Electrospinning has emerged as a highly effective technique for fabricating micro- and nanofibers characterized by high porosity, large surface area, and structural mimicry of the extracellular matrix (ECM) [66]. The equipment for electrospinning typically comprises four main components: a high-voltage power supply, a collection device, a solution storage unit, and an ejection device [66]. During the fabrication process, a high-voltage power supply (ranging from several thousand to tens of thousands of volts) establishes a voltage differential between the solution and the collection device, enabling the solution to overcome its surface tension and form a Taylor cone [66].
Electrospinning technology can be categorized into two primary types based on the polymer state: melt electrospinning and solution electrospinning [66]. Melt electrospinning offers the advantage of avoiding toxic solvents and enables large-scale production, though it typically produces thicker fibers compared to solution electrospinning [66]. Solution electrospinning involves mixing organic solvents and raw materials in precise proportions to form a solution, which is then sprayed as a jet under high voltage, ultimately yielding nanofibers [66].
2.2.2 Factors Influencing Fiber Morphology and Drug Release Numerous factors influence the electrospinning process, broadly categorized into: (1) solution properties (concentration, solvent properties, viscosity, conductivity), (2) process parameters (voltage level, collection distance, feed rate, nozzle diameter), and (3) environmental conditions (temperature, humidity, airflow) [66]. The selection of collector type also plays a critical role in determining fiber morphology and alignment characteristics, with static flat plate collectors producing randomly oriented nonwoven fiber mats, while rotating drum collectors enable the fabrication of aligned fiber architectures [66].
Table 2: Electrospinning Parameters and Their Effects on Fiber Properties
| Parameter Category | Key Variables | Influence on Fiber Characteristics |
|---|---|---|
| Solution Properties | Polymer concentration, viscosity, conductivity, surface tension | Determines fiber diameter, morphology, and bead formation |
| Process Parameters | Applied voltage, feed rate, collection distance, needle diameter | Affects jet stability, fiber alignment, and deposition pattern |
| Environmental Factors | Temperature, humidity, atmospheric composition | Influences solvent evaporation rate and fiber solidification |
| Collector Configuration | Static vs. rotating, geometry, material | Controls fiber orientation, packing density, and mat structure |
Electrospun nanofibers have emerged as an appealing vehicle for drug delivery owing to their remarkable drug-loading efficiency and adaptability in enabling drug administration through multiple delivery routes [67]. The essence of drug delivery via electrospun fibers relies on the interactive synergy between drug and carrier, with synthetic/natural and hydrophilic/hydrophobic polymer combinations serving as superior drug carriers in regulating release patterns compared to individual polymer-carriers [67].
Organ-on-a-Chip Systems
2.3.1 Design Principles and Microfabrication Organ-on-a-chip (OoC) devices simulate human organs within a microenvironment, potentially surpassing traditional preclinical methods and paving the way for innovative treatments [68]. These microphysiological systems are microscale models of human organs and tissues that reproduce their 3D properties and offer greater precision than conventional methods [68]. Microfluidics enables the creation of anatomical structures and specific organ conditions, while advances in microfabrication allow the miniaturization and integration of components such as pumps and valves [68].
When developing OoC devices, it is crucial to consider both physical and biological factors to simulate realistic physiological and pathological conditions [68]. This includes biocompatibility, analysis of mechanical stresses and deformations, cell types, growth factors, cytokines, and drug risks [68]. Microfabrication plays a critical role in creating models that accurately reflect the unique characteristics of different tissues, such as size, shape, cell density, and fluid flow patterns, ensuring consistency with in vivo conditions [68].
2.3.2 Materials and Scaffolding Strategies The materials used in OoC construction significantly influence their functionality and biological relevance. Polydimethylsiloxane (PDMS) remains widely used due to its biocompatibility, optical transparency, and ease of fabrication [69]. However, alternative materials such as polycarbonate, polyurethane, poly-methyl-methacrylate (PMMA), and cellulose are gaining traction for specific applications [69].
The use of biocompatible coatings and materials is essential for OoC engineering. Extracellular matrix (ECM) components are commonly used as coatings due to their effects on cell orientation, protein expression, differentiation, and adhesion [69]. Among the most frequently used coatings are collagen, fibronectin, and Matrigel, selected according to the specific cell type and intended OoC application [69]. Coating techniques include self-assembled monolayers (SAMs), dip coating, spin coating, microcontact printing, and 3D bioprinting, each offering distinct advantages and drawbacks [69].
Integrated Workflows and Experimental Protocols
Technology Integration Strategies
The true potential of these platforms emerges through their integration, creating synergistic systems that overcome individual limitations. The convergence of 3D bioprinting, electrospinning, and OoC technologies enables the development of highly sophisticated models for drug testing and disease modeling.
3.1.1 Integrated Fabrication Workflow The integration workflow begins with cell sourcing, where pluripotent stem cells or adult stem cells are isolated and differentiated [70]. These cells are used to develop organoids that capture key aspects of native tissue architecture and function [71]. Parallel processes of electrospinning and bioink formulation create the scaffold materials and cellular components that are subsequently integrated into OoC devices through 3D bioprinting and microfabrication techniques [66] [69]. The final integrated platform undergoes functional validation before application in drug testing and development.
Detailed Methodologies
3.2.1 Protocol for Fabricating Drug-Loaded Electrospun Fibers
Materials Required:
- Polymer(s): PLGA, PCL, chitosan, or polymer blends
- Solvent: Hexafluoro-2-isopropanol (HFIP), chloroform, DMSO (based on polymer selection)
- Active pharmaceutical ingredient (API)
- Electrospinning apparatus with high-voltage power supply
- Syringe pump with controlled flow rate capability
- Collector mandrel (static or rotating)
Step-by-Step Procedure:
- Prepare polymer solution by dissolving the selected polymer(s) in appropriate solvent at concentrations typically ranging from 5-20% w/v, depending on polymer molecular weight and desired fiber morphology.
- Add the API to the polymer solution at the desired loading concentration (typically 1-10% w/w relative to polymer) and ensure complete dissolution/dispersion.
- Transfer the drug-polymer solution to a syringe equipped with a metallic needle (gauge 18-25).
- Set the electrospinning parameters: applied voltage (10-25 kV), flow rate (0.5-3 mL/h), and tip-to-collector distance (10-20 cm).
- For aligned fibers, use a rotating mandrel collector with rotational speed between 1000-5000 rpm.
- Conduct the electrospinning process in a controlled environment (temperature: 22±2°C, humidity: 40±5%).
- Collect fibers for predetermined time periods (typically 2-12 hours) to achieve desired mat thickness.
- Vacuum-dry the collected fibers for 24 hours to remove residual solvents.
Quality Control Assessment:
- Characterize fiber morphology using scanning electron microscopy (SEM)
- Determine API distribution within fibers using confocal microscopy or HPLC
- Evaluate mechanical properties through tensile testing
- Assess drug release kinetics using Franz diffusion cells or similar apparatus
3.2.2 Protocol for 3D Bioprinting of Drug-Releasing Tissue Constructs
Materials Required:
- Bioink components: Alginate, gelatin methacryloyl (GelMA), hyaluronic acid, decellularized ECM
- Crosslinking agents: Calcium chloride, photoinitiators (LAP or Irgacure 2959)
- Cells: Primary cells or cell lines relevant to target tissue
- API or drug-loaded nanoparticles
- 3D bioprinter with temperature-controlled printheads
- UV light source for photocurring (if using photopolymerizable bioinks)
Step-by-Step Procedure:
- Prepare bioink by mixing polymer components with cells at a density of 1-10×10^6 cells/mL and API or drug-loaded nanoparticles.
- Load bioink into printing cartridges and maintain at appropriate temperature (typically 4-37°C depending on bioink properties).
- Design the 3D structure using CAD software, incorporating internal channels for nutrient transport if needed.
- Set printing parameters: pressure (10-80 kPa), printing speed (5-20 mm/s), nozzle diameter (100-400 μm), and layer height (50-300 μm).
- Print constructs layer-by-layer onto substrates maintained at physiological temperature.
- Apply crosslinking strategies after each layer or upon completion of printing:
- For ionic crosslinking: Mist with calcium chloride solution
- For photocurring: Expose to UV light (365 nm, 5-15 mW/cm²) for 30-120 seconds
- Transfer constructs to culture media and maintain in bioreactors if necessary for maturation.
Post-Printing Validation:
- Assess cell viability using live/dead staining
- Evaluate structural fidelity through micro-CT or similar imaging
- Measure mechanical properties via compression testing
- Quantify drug release kinetics over time
3.2.3 Protocol for Integrating Bioprinted Constructs into OoC Platforms
Materials Required:
- OoC device (commercial or custom-fabricated)
- Peristaltic or pneumatic pumps for fluid circulation
- Tubing and connectors
- Culture media reservoirs
- Bioprinted constructs or cells for direct printing into OoC
- ECM coatings (collagen, fibronectin, Matrigel)
Step-by-Step Procedure:
- If using prefabricated constructs, secure them within the OoC device chambers using biocompatible adhesives or mechanical anchoring.
- For direct bioprinting into OoC devices, modify bioink viscosity and printing parameters to accommodate microfluidic constraints.
- Functionalize OoC chamber surfaces with appropriate ECM coatings using techniques such as:
- Spin coating: Apply ECM solution and rotate at 1000-3000 rpm for 30-60 seconds
- Microcontact printing: Stamp patterned ECM using PDMS stamps
- Dip coating: Immerse device in ECM solution and slowly withdraw
- Connect OoC device to fluidic circulation system, ensuring sterile connections.
- Establish flow rates appropriate for the specific organ model (typically 10-500 μL/h).
- Implement operational protocols:
- For barrier function assessment: Measure transepithelial/transendothelial electrical resistance (TEER)
- For metabolism studies: Collect effluent for analysis of metabolic markers
- For drug testing: Introduce compounds through appropriate inlets and monitor responses
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of integrated 3D bioprinting, electrospinning, and OoC platforms requires specific materials and reagents carefully selected for their biocompatibility and functional properties.
Table 3: Essential Research Reagents and Materials for Integrated Platform Development
| Category | Specific Materials | Key Functions | Application Notes |
|---|---|---|---|
| Structural Polymers | PLGA, PCL, alginate, GelMA, chitosan, collagen, silk fibroin | Provide structural integrity, mimic ECM, control drug release | Selection based on degradation rate, mechanical properties, and biocompatibility |
| OoC Device Materials | PDMS, PMMA, polycarbonate, polyurethane, cellulose | Form microfluidic channels, chambers, and membranes | Balance optical clarity, gas permeability, and drug absorption characteristics |
| Bioactive Coatings | Collagen I/IV, fibronectin, laminin, Matrigel, RGD peptides | Enhance cell adhesion, differentiation, and tissue-specific function | Application via spin coating, dip coating, or microcontact printing |
| Crosslinking Agents | Calcium chloride, genipin, glutaraldehyde, LAP, Irgacure 2959 | Stabilize printed structures, control mechanical properties | Consider cytotoxicity and crosslinking kinetics |
| Cell Sources | Primary cells, iPSCs, adult stem cells, organoids | Recreate tissue-specific functions and responses | Maintain phenotype and functionality throughout fabrication process |
| Analytical Tools | TEER electrodes, metabolic assays, immunofluorescence markers, HPLC | Assess barrier function, viability, expression, and drug release | Implement real-time monitoring where possible |
Quantitative Data Analysis and Comparison
To facilitate informed decision-making in platform selection and design, we present key quantitative parameters across the three technologies.
Table 4: Performance Metrics of Integrated Drug Delivery Platforms
| Performance Metric | 3D Bioprinting | Electrospinning | OoC Integration |
|---|---|---|---|
| Spatial Resolution | 50-300 μm | 0.1-10 μm | 10-100 μm (channel features) |
| Drug Loading Capacity | 0.1-10% w/w | 1-30% w/w | Varies with integration method |
| Release Duration | Days to weeks | Hours to months | Days to weeks (with perfusion) |
| Fabrication Speed | 1-100 mm³/h | 0.1-10 mL/h | Varies with complexity |
| Cell Viability Post-Fabrication | 70-95% | N/A (unless cell-electrospinning) | 85-98% |
| Barrier Function (TEER values) | Tissue-dependent | N/A | Physiologically relevant levels |
| Scalability | Moderate | High | Low to moderate |
| Regulatory Compliance Path | Evolving framework | Established for some formats | Emerging standards |
The integration of 3D bioprinting, electrospinning, and organ-on-a-chip technologies represents a transformative approach in controlled drug delivery research. These platforms, united through advanced biomaterials, enable the creation of sophisticated models that closely mimic human physiology and pathology. The synergistic combination of these technologies addresses individual limitations while amplifying their respective strengths—3D bioprinting provides architectural precision, electrospinning offers superior biomimicry of ECM, and OoC platforms introduce physiological relevance through microfluidics and mechanical cues.
Future developments in this field will likely focus on several key areas: (1) enhancing the biocompatibility and functionality of biomaterials through novel polymer synthesis and modification strategies; (2) improving the scalability and reproducibility of fabrication processes to enable clinical translation; (3) developing standardized validation protocols for regulatory approval; and (4) incorporating intelligent sensing and monitoring capabilities for real-time assessment of drug responses [64] [68] [66]. As these technologies continue to converge and evolve, they hold tremendous promise for advancing personalized medicine, reducing reliance on animal testing, and accelerating the development of safer, more effective therapeutic agents.
The ongoing integration of these platforms is poised to redefine the landscape of drug development and regenerative medicine, ultimately leading to more predictive models of human physiology and more effective targeted therapies for a wide range of diseases and conditions.
Overcoming Translational Hurdles: Biocompatibility, Scalability, and Intelligent Design
The development of advanced drug delivery systems (DDS) represents a cornerstone of modern therapeutic strategies, enabling targeted treatment, reduced systemic toxicity, and improved patient compliance. Biomaterials serve as the fundamental building blocks for these systems, providing structural support, controlled release kinetics, and bioactive signaling. However, the clinical translation of biomaterial-based DDS faces three interconnected critical challenges: immunogenicity, the unwanted immune response to implanted materials; mechanical mismatch, the disparity between material properties and native tissue; and burst release, the rapid, uncontrolled initial release of therapeutic agents. These challenges collectively determine the safety, efficacy, and functional longevity of drug delivery platforms. This whitepaper provides a comprehensive technical analysis of these hurdles, grounded in the context of biomaterials' role in controlled drug delivery systems research, and presents evidence-based strategies to overcome them, supported by quantitative data, experimental protocols, and visualization tools for research scientists and drug development professionals.
Immunogenicity: Mastering the Host Immune Response
Immunological Mechanisms and Biomaterial Interactions
Upon implantation, biomaterials trigger a complex sequence of immune responses known as the foreign body reaction (FBR). This process initiates with protein adsorption onto the material surface within seconds of implantation, forming a provisional protein matrix that determines subsequent immune cell interactions [72] [73]. Innate immune cells, particularly neutrophils and monocytes, are recruited to the implantation site, where monocytes differentiate into macrophages. These macrophages attempt to phagocytose the material, a process that culminates in the fusion of macrophages into foreign body giant cells (FBGCs) when the material is too large for phagocytosis [73] [74].
The polarization state of macrophages serves as a critical determinant of biomaterial integration and performance. The pro-inflammatory M1 phenotype, induced by interferon-γ (IFN-γ) or lipopolysaccharide (LPS), secretes inflammatory cytokines including TNF-α, IL-1β, and IL-6, which promote chronic inflammation, tissue damage, and fibrosis. In contrast, the anti-inflammatory M2 phenotype, induced by IL-4 and IL-13, secretes IL-10, TGF-β, and vascular endothelial growth factor (VEGF), which facilitate tissue repair, regeneration, and vascularization [72] [73]. The dynamic balance between these phenotypes directly influences the outcome of biomaterial integration, where sustained M1 activation leads to fibrous encapsulation and implant failure, while M2 polarization supports functional tissue integration.
Table 1: Key Immune Cell Types and Their Roles in Biomaterial Response
| Immune Cell | Primary Function in FBR | Key Secreted Factors | Impact on Biomaterial Integration |
|---|---|---|---|
| Neutrophils | Initial inflammatory response; release of reactive oxygen species (ROS) and enzymes | MMPs, ROS, IL-8 | ECM degradation; amplification of inflammation |
| M1 Macrophages | Pathogen clearance; pro-inflammatory response | TNF-α, IL-1β, IL-6, ROS | Chronic inflammation; fibrosis; implant failure |
| M2 Macrophages | Tissue repair; inflammation resolution | IL-10, TGF-β, VEGF, PDGF | Angiogenesis; tissue integration; constructive remodeling |
| T Lymphocytes | Adaptive immune regulation; cytokine signaling | IFN-γ (Th1), IL-4 (Th2), IL-17 (Th17) | Modulation of macrophage polarization; chronic inflammation |
| Foreign Body Giant Cells (FBGCs) | Attempted phagocytosis of large implants | ROS, enzymes, pro-inflammatory cytokines | Peri-implant fibrosis; barrier formation; isolation of implant |
Strategic Biomaterial Design to Mitigate Immunogenicity
Advanced biomaterial engineering offers multiple strategies to modulate immune responses toward favorable outcomes. Surface modification techniques, including the immobilization of anti-inflammatory molecules such as IL-4 or IL-10, can directly steer macrophage polarization toward the M2 phenotype [73]. The incorporation of immune checkpoint molecules (e.g., PD-L1) on nanofibers has demonstrated efficacy in creating localized immunosuppressive environments, protecting implants from immune attack in autoimmune disease models [74]. Biomaterial chemistry also profoundly influences immune activation; for instance, zwitterionic polymers exhibit superior resistance to protein fouling, thereby reducing initial immune recognition and activation [74].
The strategic selection of biomaterial composition can inherently direct immune responses. Natural polymers like chitosan and hyaluronic acid generally elicit milder inflammatory responses compared to synthetic polymers, though chemical modifications can alter their immunogenicity [73]. Decellularized extracellular matrix (ECM) scaffolds retain native tissue-specific biochemical and structural cues that promote constructive remodeling while minimizing immune activation [75]. Additionally, the release of specific bioactive ions from biodegradable metals, such as magnesium (Mg²⁺) and strontium (Sr²⁺), creates a regenerative immune microenvironment; Mg²⁺ ions reduce inflammation and promote osteogenesis in bone healing applications [76].
Experimental Protocol: In Vitro Macrophage Polarization Assay
Purpose: To evaluate the immunomodulatory capacity of biomaterial surfaces on macrophage polarization.
Materials:
- RAW 264.7 murine macrophage cell line or primary bone marrow-derived macrophages (BMDMs)
- Test biomaterial films or 3D scaffolds (1 cm diameter)
- Cell culture media: DMEM supplemented with 10% FBS, 1% penicillin-streptomycin
- Polarizing agents: LPS (100 ng/mL) and IFN-γ (20 ng/mL) for M1 polarization; IL-4 (20 ng/mL) for M2 polarization
- Antibodies for flow cytometry: anti-CD86-FITC (M1 marker), anti-CD206-PE (M2 marker)
- RNA isolation kit and qPCR reagents for gene expression analysis (iNOS, ARG1, TNF-α, IL-10)
- ELISA kits for cytokine detection (TNF-α, IL-1β, IL-10, TGF-β)
Methodology:
- Cell Seeding: Seed macrophages at 5×10⁵ cells/well on biomaterial surfaces in 24-well plates. Allow attachment for 6 hours.
- Polarization Induction: Treat cells with M1 (LPS + IFN-γ) or M2 (IL-4) polarizing agents for 24-48 hours.
- Flow Cytometry Analysis: Harvest cells, stain with CD86 and CD206 antibodies, and analyze using flow cytometry to determine M1/M2 population ratios.
- Gene Expression Profiling: Extract total RNA, synthesize cDNA, and perform qPCR for M1 (iNOS, TNF-α) and M2 (ARG1, IL-10) marker genes.
- Cytokine Secretion Analysis: Collect conditioned media and quantify secreted cytokine levels using ELISA.
- Statistical Analysis: Perform one-way ANOVA with post-hoc Tukey test (n≥5, p<0.05 considered significant).
Diagram Title: Macrophage Polarization Pathways in Foreign Body Response
Mechanical Mismatch: Achieving Biomechanical Compatibility
Consequences of Mechanical Disparity
Mechanical mismatch between implants and native tissue creates biomechanical incompatibility that leads to several pathological outcomes. The stress shielding phenomenon occurs when a stiff implant bears the majority of mechanical load, effectively shielding the surrounding bone from normal stress patterns, resulting in bone resorption, implant loosening, and eventual failure [75]. This mechanical mismatch also generates abnormal stress concentrations at the tissue-implant interface, inducing chronic inflammation, fibrotic encapsulation, and impaired tissue integration. Furthermore, mechanical properties directly influence cellular responses through mechanotransduction pathways; excessive stiffness can promote fibroblast-to-myofibroblast differentiation, driving excessive ECM deposition and fibrosis [75] [76].
The elastic modulus of common biomaterials varies significantly: medical-grade titanium (110 GPa) and cobalt-chromium alloys (230 GPa) substantially exceed the modulus of cortical bone (5-30 GPa), creating substantial stress shielding effects. In contrast, magnesium alloys (41-45 GPa) provide a closer match to bone mechanical properties, reducing stress shielding effects while maintaining sufficient load-bearing capacity [76].
Biomaterial Strategies for Mechanical Compatibility
Material selection forms the first line of defense against mechanical mismatch. Magnesium alloys have emerged as promising candidates for bone fixation devices due to their bone-like modulus (41-45 GPa) and biodegradability [76]. Advanced Mg-Sr-Mn alloys demonstrate yield strength of 205 MPa and ultimate tensile strength of 242 MPa, exceeding the minimum clinical benchmarks for orthopedic applications while maintaining favorable degradation profiles [76].
Structural engineering approaches, including controlled porosity architectures and composite materials, enable fine-tuning of effective mechanical properties. Porous titanium structures created through additive manufacturing can reduce effective modulus while maintaining strength, better matching the graded mechanical properties of native tissue [75]. Similarly, polymer-ceramic composites (e.g., PLGA-hydroxyapatite) can be engineered to mimic the anisotropic mechanical behavior of bone and cartilage.
Dynamic and responsive materials represent the cutting edge of mechanical compatibility. Shape memory polymers and alloys, self-healing hydrogels, and stress-responsive biomaterials can adapt their mechanical properties in response to changing physiological loads and tissue remodeling, maintaining long-term mechanical harmony throughout the healing process [75].
Table 2: Mechanical Properties of Native Tissues and Biomaterials
| Material/Tissue | Elastic Modulus (GPa) | Tensile Strength (MPa) | Key Advantages/Limitations |
|---|---|---|---|
| Cortical Bone | 5-30 | 50-150 | Natural benchmark; anisotropic |
| Cartilage | 0.001-0.01 | 10-40 | Viscoelastic; low load-bearing |
| Magnesium Alloys (Mg-Sr-Mn) | 41-45 | 242 (UTS) | Biodegradable; bone-like modulus; stress reduction |
| Titanium (Ti-6Al-4V) | 110 | 860-900 | High strength; excessive stiffness causes stress shielding |
| Cobalt-Chromium Alloys | 230 | 600-1795 | Wear resistance; high stiffness causes significant stress shielding |
| PLGA (85:15) | 2-4 | 40-60 | Tunable degradation; moderate strength |
| Porous Titanium (50% porosity) | 15-20 | 100-200 | Reduced modulus; enhanced tissue integration |
Experimental Protocol: In Vivo Assessment of Mechanical Integration
Purpose: To evaluate the biomechanical integration of biomaterials with host tissue in a bone defect model.
Materials:
- Animal model: Sprague-Dawley rats (12-16 weeks, n=8/group)
- Test implants: Cylindrical implants (2mm diameter × 4mm length) of test material vs. control
- * Surgical equipment:* Drill press, trephine burr (2.5mm), sterile surgical instruments
- Micro-CT scanner for bone-implant contact analysis
- Mechanical testing system with custom fixture for push-out test
- Histology supplies: Tissue processor, embedding medium, microtome, staining solutions (H&E, Masson's Trichrome)
Methodology:
- Surgical Procedure: Create bilateral critical-sized defects in femoral condyles using trephine burr. Press-fit implants into defects. Close surgical site in layers.
- Post-operative Monitoring: Administer analgesics for 48 hours. Monitor weight bearing and wound healing daily.
- Sample Harvesting: Euthanize animals at 4, 8, and 12 weeks post-implantation. Dissect femurs and remove soft tissue.
- Micro-CT Analysis: Scan samples at 10μm resolution. Quantify bone volume/total volume (BV/TV) ratio and bone-implant contact (BIC) percentage within 500μm peri-implant region.
- Biomechanical Push-out Test: Position samples in custom fixture with 1.8mm diameter support. Apply compressive load at 1mm/min crosshead speed until implant failure or displacement. Record maximum shear strength.
- Histomorphometric Analysis: Process undecalcified sections (50μm) with staining. Quantify fibrous tissue thickness at bone-implant interface using image analysis software.
- Statistical Analysis: Two-way ANOVA with post-hoc Bonferroni test (p<0.05 significant).
Diagram Title: Mechanical Mismatch Impact on Tissue Integration
Burst Release: Controlling Drug Release Kinetics
Mechanisms and Impact of Burst Release
Burst release refers to the rapid, often uncontrolled initial release of a significant fraction of the encapsulated drug within the first hours to days following implantation. This phenomenon primarily results from surface-associated drug that readily diffuses out of the carrier matrix upon contact with the biological environment. Additional contributing factors include high initial concentration gradients, pore connectivity in porous materials, and swelling-induced expulsion in hydrogel systems [7] [77] [78].
The clinical consequences of burst release are substantial. A rapid drug dump can lead to local cytotoxicity, particularly with high-potency therapeutic agents, causing tissue damage and impairing healing. Simultaneously, it produces systemic exposure with potential off-target effects, defeating the purpose of localized delivery. Perhaps most critically, burst release depletes the drug reservoir, resulting in subtherapeutic concentrations at later time points when continued treatment is most needed, potentially leading to treatment failure and necessitating reintervention [77] [78].
Engineering Solutions for Controlled Release
Polymer-based delivery systems, particularly those utilizing PLGA (poly(lactic-co-glycolic acid)), offer highly tunable release kinetics through control over polymer parameters. The lactide:glycolide (LA:GA) ratio directly governs degradation rate, with 50:50 PLGA degrading over 2-3 months, while 75:25 PLGA requires 4-6 months for complete degradation [77]. Molecular weight significantly influences release duration, with higher molecular weight polymers (>100 kDa) providing extended release profiles compared to low molecular weight variants (10-20 kDa) [77]. End-group chemistry further modulates release; acid-terminated PLGA degrades more rapidly via autocatalytic hydrolysis compared to ester-capped equivalents [77].
Structural engineering approaches effectively mitigate burst release. Multilayer systems with drug-free outer layers act as diffusion barriers, delaying initial release. Core-shell architectures with rate-controlling membranes provide zero-order release kinetics, while porous structures with optimized tortuosity create diffusion pathways that moderate initial release [7] [78].
Stimuli-responsive systems represent an advanced strategy for precise temporal control. These "smart" biomaterials release therapeutic payloads in response to specific physiological triggers, including pH changes (acidic tumor microenvironments), enzyme activity (MMP overexpression in diseased tissues), temperature variations, or external stimuli such as light or magnetic fields [7] [8].
Experimental Protocol: Optimization of PLGA-Based Delivery Systems
Purpose: To systematically optimize PLGA-based microparticles for controlled drug release using an evidence-based Design of Experiments (DoE) approach.
Materials:
- Polymers: PLGA with varying LA:GA ratios (50:50, 65:35, 75:25, 85:15) and molecular weights (10-120 kDa)
- Drug: Vancomycin hydrochloride as model antibiotic
- Solvents: Dichloromethane (DCM), ethyl acetate
- Stabilizers: Polyvinyl alcohol (PVA, 1-5% w/v)
- Equipment: Homogenizer, sonicator, freeze dryer, HPLC system with C18 column
- Software: Design-Expert for experimental design and optimization
Methodology:
- Experimental Design: Implement a central composite design with four critical factors: LA:GA ratio (50:50 to 85:15), molecular weight (15-100 kDa), polymer-to-drug ratio (2:1 to 10:1), and particle size (5-50 μm).
- Double Emulsion Fabrication: (W1/O/W2) method: Dissolve drug in inner aqueous phase (W1). Emulsify with polymer in organic phase (O) using probe sonication. Add primary emulsion to outer aqueous phase (W2) containing PVA. Homogenize at 5000 rpm for 2 minutes.
- Solvent Evaporation: Stir emulsion for 4 hours at room temperature to evaporate organic solvent.
- Particle Collection: Centrifuge at 10,000 × g for 10 minutes. Wash three times with distilled water. Lyophilize for 48 hours.
- Characterization: Determine particle size by laser diffraction. Analyze surface morphology by SEM. Measure drug loading by HPLC after dissolution in DMSO.
- In Vitro Release Study: Incubate particles (n=5) in PBS (pH 7.4) at 37°C with gentle shaking. Collect samples at predetermined time points (1, 3, 6, 12, 24, 48, 72 hours, then weekly). Analyze drug concentration by HPLC.
- Release Kinetics Modeling: Fit release data to zero-order, first-order, Higuchi, and Korsmeyer-Peppas models to identify release mechanisms.
- Data Analysis: Use response surface methodology to model factor interactions and identify optimal factor combinations that minimize burst release while maintaining therapeutic levels.
Table 3: PLGA Formulation Parameters and Their Impact on Release Kinetics
| Formulation Parameter | Impact on Burst Release | Effect on Release Duration | Optimization Strategy |
|---|---|---|---|
| LA:GA Ratio | Higher GA increases initial burst | Higher LA content extends release duration | Balance based on therapeutic window (e.g., 75:25 for 4-6 month release) |
| Molecular Weight (Mw) | Lower Mw increases burst release | Higher Mw (>100 kDa) extends release to 3-6 months | Select Mw based on required release duration |
| Polymer:Drug Ratio | Lower ratio increases burst release | Higher ratio extends release but reduces loading | Optimize for therapeutic dose (typically 5:1 to 10:1) |
| Particle Size | Smaller particles (<10μm) increase burst | Larger particles (>50μm) extend release but limit injection | Size distribution 10-50μm for balance |
| Porosity | High porosity increases burst release | Low porosity extends release but may cause lag phase | Controlled porosity (10-30%) via excipient addition |
| Encapsulation Method | Double emulsion reduces burst vs. single emulsion | Complex coacervation provides most linear release | W1/O/W2 for hydrophilic drugs; O/W for hydrophobic |
Integrated Design Approaches: The Scientist's Toolkit
Research Reagent Solutions for Advanced Biomaterial Development
Table 4: Essential Research Reagents for Biomaterial-Drug Delivery Systems
| Reagent/Category | Function | Application Examples | Key Considerations |
|---|---|---|---|
| PLGA Polymers | Biodegradable carrier matrix | Controlled release microspheres, implants | LA:GA ratio, Mw, end-group chemistry determine degradation rate |
| RGD Peptide | Integrin-binding ligand | Surface functionalization for cell adhesion | Concentration, spatial presentation critical for signaling efficacy |
| Mg-Sr-Mn Alloys | Metallic biomaterial with osteoconductive properties | Bone fixation devices, orthopedic implants | Sr²⁺ promotes osteogenesis; Mn enhances corrosion resistance |
| Chitosan | Natural polymer with inherent antimicrobial activity | Hydrogels, wound dressings, mucoadhesive systems | Degree of deacetylation affects biodegradation and properties |
| Hyaluronic Acid | ECM component with CD44 receptor targeting | Viscoelastic injections, hydrogel crosslinking | Molecular weight influences residence time and immunogenicity |
| Porous Silicon | Biodegradable material with high drug loading capacity | Multistage delivery systems, immunotherapy | Pore size and surface chemistry control loading and release |
| Stimuli-Responsive Linkers | Enable triggered release in specific microenvironments | Enzyme-cleavable (MMP-sensitive), pH-sensitive peptides | Specificity, cleavage kinetics must match pathological signals |
Advanced Characterization Techniques
Comprehensive characterization of biomaterial-drug systems requires multidisciplinary approaches. In vitro release testing should simulate physiological conditions with sink conditions maintained throughout the study period. Accelerated release studies at elevated temperatures can provide preliminary data but must be correlated with real-time release profiles. Material characterization includes surface analysis (SEM, AFM), porosity measurement (mercury porosimetry, BET), thermal analysis (DSC, TGA), and mechanical testing (tensile, compression, shear).
Biological characterization encompasses sterility testing, endotoxin detection, cytotoxicity assessment (ISO 10993-5), and hemocompatibility evaluation. For immunomodulatory materials, specific assays including macrophage polarization studies, cytokine profiling, and lymphocyte activation tests provide critical safety and efficacy data. In vivo evaluation should include not only efficacy models but also comprehensive biocompatibility assessment, including histopathological evaluation of implant sites and distant organs to identify potential systemic effects.
The convergence of biomaterial science, immunology, and drug delivery has created unprecedented opportunities to overcome the traditional challenges of immunogenicity, mechanical mismatch, and burst release. The next generation of biomaterial-based drug delivery systems will leverage advanced manufacturing technologies including 3D bioprinting for patient-specific architectures and microfluidic fabrication for highly uniform particles. Intelligent responsive systems that adapt to changing physiological conditions will provide unprecedented control over drug release profiles. Multi-modal approaches that combine structural design, material selection, and bioactive functionalization will address the interconnected nature of these challenges, creating truly integrated solutions.
Furthermore, the adoption of computational modeling and artificial intelligence in biomaterial design will accelerate optimization and reduce development timelines. As our understanding of material-immune system interactions deepens, we can anticipate increasingly sophisticated immunomodulatory strategies that not only suppress unwanted immune responses but actively harness immune mechanisms for enhanced tissue repair and regeneration. By systematically addressing these fundamental challenges through integrated design approaches, biomaterial-based drug delivery systems will continue to evolve toward safer, more effective, and clinically transformative therapies.
Optimizing Biocompatibility and Reducing Foreign Body Response
The success of implantable biomaterials in controlled drug delivery systems is fundamentally governed by their biocompatibility and their ability to mitigate the host's immune response. The foreign body response (FBR) is a complex physiological reaction to implanted materials, often resulting in the formation of a fibrous capsule that can isolate the device and severely compromise its function, particularly the reliable release of therapeutics [74]. For drug delivery systems, this fibrotic barrier can impede drug diffusion, alter release kinetics, and ultimately lead to therapeutic failure. This whitepaper provides an in-depth technical guide for researchers and drug development professionals on the core mechanisms, evaluation methodologies, and advanced material strategies for optimizing biocompatibility and suppressing the FBR, thereby ensuring the efficacy and longevity of advanced drug delivery systems.
Core Mechanisms of the Foreign Body Response
A nuanced understanding of the FBR cascade is essential for developing strategies to counteract it. The response unfolds in a sequential manner, initiating the moment a material is introduced to the biological environment.
The Signaling Pathways Driving the FBR
Recent research has elucidated the critical role of specific signaling pathways in initiating the FBR. A key finding is the central involvement of Toll-like receptors (TLRs) 2 and 4 in recognizing adsorbed proteins as damage-associated molecular patterns (DAMPs) [79]. The following diagram illustrates this pivotal signaling cascade and the primary cellular response.
Figure 1: The core signaling pathway of the foreign body response, highlighting the critical role of TLR2/TLR4 activation by adsorbed proteins (DAMPs) in driving the response toward fibrosis.
The FBR begins with the rapid, non-specific adsorption of host proteins onto the material's surface [79]. These adsorbed proteins can undergo conformational changes, causing them to be recognized by the immune system as DAMPs. Innate immune cells, particularly macrophages, then adhere to the protein-coated surface. This study identified that macrophages, not neutrophils, are the primary cells responding to surface-adsorbed plasma via TLR2 and/or TLR4, and that the deletion of both receptors was required to significantly inhibit activation across all tested materials [79]. In vivo, simultaneous deletion of TLR2 and TLR4 nearly abrogated the FBR and eliminated material-dependent differences in a subcutaneous implant model, establishing them as critical therapeutic targets [79].
Following this activation, macrophages release pro-inflammatory cytokines, sustaining a state of chronic inflammation at the implant site. If unresolved, this process leads to the activation of fibroblasts and the excessive deposition of collagen and other extracellular matrix components, forming a dense, avascular fibrous capsule around the implant [74]. This capsule acts as a physical barrier, hindering the diffusion of drugs from an implanted delivery system and isolating the device from the surrounding tissue.
Quantitative Evaluation of Biocompatibility and FBR
Robust and standardized evaluation is critical for assessing the biocompatibility of new materials and the effectiveness of FBR-mitigation strategies. The international standard ISO 10993-1:2025 provides a framework for the biological evaluation of medical devices within a risk management structure, emphasizing the identification of biological hazards, hazardous situations, and potential harms [80].
Standardized Histopathological Scoring
According to DIN EN ISO 10993-6, a key standard for implantation effects, histological evaluation involves a semi-quantitative assessment of cellular and tissue reactions [81]. The scoring, typically on a scale from 0 to 4, assesses various cell types and tissue changes to calculate a total irritation score, which classifies the material's biocompatibility.
Table 1: Histopathological Scoring Criteria Based on DIN EN ISO 10993-6 [81].
| Cell Type / Tissue Change | Scoring Scale (0-4) | Description of Frequency/Severity |
|---|---|---|
| Polymorphonuclear Cells | 0 = None, 1 = Rare, 2 = Mild, 3 = Moderate, 4 = Severe | Presence of neutrophils indicating acute inflammation. |
| Lymphocytes | 0 = None, 1 = Rare, 2 = Mild, 3 = Moderate, 4 = Severe | Presence indicating chronic inflammation. |
| Plasma Cells | 0 = None, 1 = Rare, 2 = Mild, 3 = Moderate, 4 = Severe | Presence often associated with immune recognition. |
| Macrophages | 0 = None, 1 = Rare, 2 = Mild, 3 = Moderate, 4 = Severe | Phagocytic activity and foreign body giant cell formation. |
| Multinucleated Giant Cells | 0 = None, 1 = Rare, 2 = Mild, 3 = Moderate, 4 = Severe | Characteristic of the foreign body response. |
| Necrosis | 0 = None, 1 = Rare, 2 = Mild, 3 = Moderate, 4 = Severe | Tissue death surrounding the implant. |
| Fibrosis | 0 = None, 1 = Rare, 2 = Mild, 3 = Moderate, 4 = Severe | Deposition of fibrous connective tissue (capsule). |
| Neovascularization | 0 = None, 1 = Rare, 2 = Mild, 3 = Moderate, 4 = Severe | Formation of new blood vessels. |
Site-Specific In Vivo Implantation Models
The choice of implantation model significantly impacts the observed tissue response, a critical consideration for validating drug delivery systems for specific anatomical sites. A 2025 comparative study of subcutaneous and calvarial (bone) implantation in rats revealed stark differences in host response to the same bone substitute material [81].
Table 2: Comparative Host Response in Different Implantation Models (Adapted from [81]).
| Parameter | Subcutaneous Implant Model | Calvarial Implant Model |
|---|---|---|
| Primary Cell Types | Macrophages and multinucleated giant cells | Macrophages and multinucleated giant cells |
| Inflammatory Reaction | Stronger, with higher polymorphonuclear cell and lymphocyte counts at day 10 | Milder inflammatory reaction |
| Plasma Cell Infiltration | Moderate, observed until day 30 | Not observed |
| Neovascularization | Low levels | Significantly increased, reflecting bone-specific regeneration |
| Material Degradation & Phagocytosis | Significantly greater at day 60 | Slower degradation |
| Long-term Outcome | Consistently elevated irritancy scores & fibrosis | Increased fibrosis at day 60, coupled with bone regeneration |
This data underscores the importance of selecting a biologically relevant implantation model that reflects the intended clinical application of the drug delivery device.
Advanced Material Strategies to Mitigate FBR
Innovations in biomaterial design focus on actively modulating the host immune response rather than passively accepting it. The following experimental workflow outlines a comprehensive approach to developing and validating advanced biomaterials with reduced FBR.
Figure 2: Integrated experimental workflow for developing FBR-mitigating biomaterials, from material synthesis to functional drug delivery validation.
Strategic Approaches and Experimental Protocols
Strategy A: Targeting Initial Protein Recognition
- Protocol for TLR Inhibition: Based on the findings that co-inhibition of TLR2 and TLR4 significantly reduces the FBR [79], researchers can incorporate small-molecule inhibitors or neutralizing antibodies for these receptors into the biomaterial matrix. In vitro, this involves pre-treating macrophages with inhibitors or fabricating material surfaces with immobilized inhibitors and challenging them with adsorbed plasma proteins. Activation is measured via cytokine (e.g., TNF-α, IL-6) ELISA. In vivo, this strategy can be tested using a subcutaneous implant model in TLR2/4 knockout mice or wild-type mice with local, sustained delivery of inhibitors from the implant. Explants are harvested at 10, 30, and 60 days for histological scoring according to Table 1 [81].
Strategy B: Engineering Material Properties
- Protocol for Zwitterionic Coatings: The use of zwitterionic materials, which possess mixed positive and negative charges, can dramatically reduce non-specific protein adsorption. A 2024 study demonstrated an injectable, biodegradable zwitterionic gel that extended the functional longevity of insulin infusion catheters in diabetic minipigs from 2 days to 13 days by reducing pro-inflammatory markers [74]. In vitro protein adsorption can be quantified using techniques like Quartz Crystal Microbalance (QCM) or SDS-PAGE of eluted proteins. In vivo efficacy is validated in relevant animal models with frequent histological analysis.
Strategy C: Localized Immunomodulation
- Protocol for Metabolic Reprogramming: Instead of broad immunosuppression, strategies can locally alter the immune microenvironment. One study incorporated metabolic inhibitors into polylactide to lower glycolytic pathways in the implant microenvironment, which reduced inflammation and promoted pro-regenerative immune responses [74]. In vitro, this requires co-culture models of immune cells and material samples, with analysis of metabolic profiles (e.g., Seahorse Analyzer) and cell phenotypes (flow cytometry). In vivo evaluation involves implanting these "metabolically active" materials and analyzing the composition of infiltrating cells via immunofluorescence and transcriptomics.
The Scientist's Toolkit: Key Research Reagents and Materials
The following table details essential materials and reagents used in the featured experiments and broader research in this field.
Table 3: Key Research Reagent Solutions for FBR Studies.
| Reagent / Material | Function in Research | Specific Example / Rationale |
|---|---|---|
| TLR2 and TLR4 Inhibitors | To probe the mechanism of FBR initiation and as a potential therapeutic. | Small molecule antagonists (e.g., TAK-242 for TLR4) or neutralizing antibodies used in vitro and in local delivery systems [79]. |
| Zwitterionic Polymers | To create ultra-low-fouling surfaces that minimize protein adsorption. | Injectable zwitterionic gel used to coat catheters, preventing occlusion and inflammation [74]. |
| Immunomodulatory Drugs | For localized, sustained release to skew the immune response toward tolerance. | Immune checkpoint molecules or drugs integrated into nanofibers to create immunosuppressive niches [74]. |
| Biodegradable Polymers (e.g., PLGA, Polylactide) | Serve as the base material for implants and drug delivery systems. | Polylactide acts as a scaffold and drug carrier; its microenvironment can be metabolically altered [74]. |
| HA/β-TCP Ceramics & Collagen Scaffolds | Used as bone filler models and in composite materials for tissue engineering. | Synthetic biphasic granules in a type I collagen scaffold used to test site-specific biocompatibility [81]. |
| Metabolic Inhibitors | To reprogram the local metabolic profile of immune cells at the implant site. | Integrated into polylactide to reduce glycolysis and promote a pro-regenerative macrophage phenotype [74]. |
Overcoming the foreign body response is a critical hurdle for the next generation of implantable drug delivery systems. The field is moving beyond inert biomaterials toward "smart," actively immunomodulatory materials. By leveraging insights into core mechanisms like TLR2/4 signaling and employing rigorous, site-specific evaluations per updated ISO standards, researchers can design materials that control host interactions. The integration of advanced strategies—such as surface engineering, localized drug delivery, and metabolic reprogramming—holds the promise of creating seamlessly integrated devices that deliver therapeutics reliably over their intended lifespan, ultimately advancing the paradigm of personalized medicine.
Strategies for Enhancing Vascularization and Tissue Integration
The successful integration of engineered tissues and controlled drug delivery systems hinges on the rapid establishment of functional vascular networks. Vascularization—the formation of blood vessels—is arguably the most significant challenge in tissue engineering and regenerative medicine, as it ensures the delivery of oxygen and nutrients while removing metabolic waste [82]. Without adequate vascular supply, cells within engineered constructs experience diffusion limitations, restricting tissue development to dimensions of only 100-200 μm from the nearest capillary, far below clinically relevant sizes [82]. This limitation profoundly impacts the efficacy of drug delivery systems, where controlled release of therapeutic agents depends on viable surrounding tissue for proper function and integration.
Within the context of biomaterials for controlled drug delivery, vascularization strategies must achieve two critical objectives: (1) creating pre-vascularized networks within biomaterial constructs that can anastomose (connect) with host vasculature upon implantation, and (2) designing biomaterial systems that actively promote vascular ingrowth from host tissues through controlled release of pro-angiogenic factors [82] [83]. The emergence of advanced biomaterial platforms—including smart scaffolds, hydrogels, and microfabricated systems—has revolutionized our approach to these challenges by providing precise spatiotemporal control over biological cues.
Fundamental Vascularization Principles and Challenges
Oxygen Diffusion and Mass Transport Limitations
The core constraint driving vascularization needs stems from fundamental physical principles. Fick's law of diffusion governs oxygen transport through tissues, with oxygen consumption following Michaelis-Menten kinetics [82]. Together, these principles create a diffusion-limited environment where cells beyond the 100-200 μm threshold from blood vessels experience hypoxia, nutrient deficiency, and eventual cell death [82]. This limitation is particularly problematic for drug delivery systems, where sustained release depends on viable surrounding tissue.
Quantitative modeling of oxygen distribution requires consideration of multiple factors:
- Flow rates through the scaffold or tissue
- Diffusion coefficients within each tissue region
- Oxygen consumption rates of specific cell types
- Geometric and biological conditions of the construct
Direct measurement techniques using oxygen probes or oxygen-sensitive dyes enable validation of these models and provide critical data for optimizing vascularization strategies [82].
Key Biological Processes in Vascularization
Table 1: Fundamental Biological Processes in Vascular Formation
| Process | Mechanism | Primary Cells Involved | Role in Tissue Integration |
|---|---|---|---|
| Angiogenesis | Sprouting of new vessels from existing ones | Endothelial cells, pericytes | Establishes initial capillary networks |
| Arteriogenesis | Maturation and expansion of arterial vessels | Endothelial cells, vascular smooth muscle cells | Provides adequate blood flow capacity |
| Vasculogenesis | De novo vessel formation from progenitor cells | Endothelial progenitor cells | Creates foundational vascular networks |
| Vessel Maturation | Stabilization and specialization of vessels | Pericytes, smooth muscle cells | Ensures long-term vessel stability and function |
The vascularization process involves multiple coordinated biological mechanisms. Angiogenesis, the formation of new blood vessels from pre-existing ones, is initiated when endothelial cells respond to angiogenic stimuli such as vascular endothelial growth factor (VEGF) [83]. Vasculogenesis involves the assembly of blood vessels from endothelial progenitor cells, while arteriogenesis refers to the remodeling of existing vessels into larger, stabilized structures [83]. Successful tissue integration requires not just the initial formation of vessels, but their maturation through recruitment of pericytes and smooth muscle cells, deposition of basement membrane, and establishment of hierarchical networks capable of sustaining blood flow [84].
Biomaterial-Based Vascularization Strategies
Scaffold Design and Functionalization
Scaffold-based approaches represent one of the most extensively investigated strategies for enhancing vascularization. These biomaterials provide three-dimensional frameworks that can be engineered to present specific biochemical and biophysical cues to promote blood vessel formation.
Scaffold Functionalization with Growth Factors Growth factor delivery represents a classical approach to inducing vascularization within biomaterial scaffolds [82]. The strategic incorporation of pro-angiogenic factors mimics the natural process where these molecules associate with the extracellular matrix (ECM), which stabilizes their conformation and protects them from proteolytic degradation [82].
Table 2: Key Growth Factors in Vascularization Strategies
| Growth Factor | Primary Function | Delivery Challenges | Biomaterial Solutions |
|---|---|---|---|
| VEGF | Initiates endothelial capillary formation; increases vascular permeability | Short half-life; excessive amounts cause vascular leakage | Heparin-binding; controlled release systems; affinity-based tethering |
| bFGF | Induces proliferation of endothelial cells and smooth muscle cells | Rapid diffusion; mitogen for multiple cell types | Fusion proteins; binding domain incorporation; encapsulation |
| PDGF | Recruits smooth muscle cells to endothelial linings; promotes vessel maturation | High levels cause vessel destabilization | Dual delivery systems; microsphere encapsulation; sequential release |
| Angiopoietin-1 | Promotes endothelial cell migration; stabilizes newly formed capillaries | Overexpression induces endothelial hyperplasia | Combinatorial approaches; sustained release platforms |
Effective growth factor delivery requires sophisticated biomaterial strategies to overcome inherent limitations of protein therapeutics. Single-factor release systems have demonstrated promise but often fail to recapitulate the complex temporal sequences of natural vascular development [82]. More advanced approaches include fusion proteins composed of growth factors coupled with specific binding domains (e.g., collagen-binding or fibrin-binding domains) that enhance retention within biomaterial scaffolds [82]. Alternatively, scaffolds can be modified with heparin-binding sites or synthetic mimics that sequester heparin-binding growth factors through affinity-based interactions [85].
Material Properties and Scaffold Architecture Beyond biochemical functionalization, the physical and architectural properties of scaffolds significantly influence vascularization outcomes. Porosity and pore interconnectivity are critical for facilitating cell infiltration, nutrient diffusion, and vascular ingrowth [82]. Advanced fabrication techniques, including 3D printing, electrospinning, and sacrificial templating, enable precise control over scaffold architecture at multiple length scales [86] [27].
The mechanical properties of scaffolds, particularly stiffness, have emerged as crucial regulators of vascular cell behavior. Intermediate stiffness values (approximately 2 kPa) have been shown to support the most robust and stable vascular network formation in dextran-based hydrogels, while both softer and stiffer matrices resulted in suboptimal outcomes [85]. This stiffness-dependent vascular assembly underscores the importance of matching biomaterial mechanical properties to the target tissue environment.
Advanced Growth Factor Delivery Systems
Controlled growth factor delivery represents a cornerstone of vascularization strategies within drug delivery research. Sophisticated biomaterial systems have been developed to address the challenges of spatiotemporal control over growth factor presentation.
Dual and Sequential Delivery Systems The maturation of functional vascular networks requires the sequential action of multiple growth factors. VEGF initiates vessel formation, while PDGF and angiopoietins promote vessel stabilization and maturation [82] [84]. Biomaterial systems capable of delivering multiple factors with distinct release kinetics have demonstrated enhanced vascularization outcomes compared to single-factor approaches.
One innovative strategy involves incorporating VEGF mixed directly with polymer particles while pre-encapsulating PDGF into microspheres before scaffold formation [82]. This approach produces differential release profiles, with VEGF largely released from scaffold surfaces for rapid activity and PDGF released more slowly through bulk degradation for sustained effects [82]. Similarly, electrospun fibers and microspheres integrated into scaffolds can provide sequential release of VEGF, bFGF, and PDGF to promote vascular density and maturity [84].
Heparin-Mimetic Biomaterials Heparin, a highly sulfated glycosaminoglycan, naturally binds to a wide range of growth factors through electrostatic interactions, stabilizing them and modulating their signaling [85]. However, native heparin's potent anticoagulant activity and batch-to-batch variability limit its clinical application [85]. To address these limitations, researchers have developed synthetic heparin-mimetic biomaterials by introducing sulfate groups onto polysaccharide backbones such as dextran [85].
These heparin-mimetic hydrogels bind and immobilize growth factors, enhance angiogenic signaling, and promote both in vitro vascular network formation and in vivo tissue microvascularization to a similar extent as heparin-conjugated hydrogels, but without inducing local bleeding at implantation sites [85]. This decoupling of pro-angiogenic effects from anticoagulant activity represents a significant advancement in biomaterial design for vascularization applications.
Stimuli-Responsive Delivery Systems Smart biomaterials that respond to specific environmental cues offer sophisticated control over growth factor delivery. Enzyme-responsive systems can release factors in response to matrix metalloproteinases (MMPs) upregulated during vascular remodeling [27]. pH-responsive materials may activate in the acidic environment of ischemic tissues, while mechano-responsive systems could release factors in response to the physical forces associated with vascular development [27].
These stimuli-responsive platforms represent the cutting edge of controlled drug delivery for vascularization, potentially enabling autonomous regulation of therapeutic factor release in response to the dynamic tissue environment.
Cell-Based Vascularization Strategies
Cell-based approaches leverage the innate capacity of specific cell types to form and stabilize vascular networks, offering self-assembling, biologically relevant solutions to the vascularization challenge.
Endothelial Cell Seeding and Coculture The direct incorporation of endothelial cells (ECs) into biomaterial constructs represents a straightforward approach to pre-vascularization. When co-cultured with supporting cells such as fibroblasts or mesenchymal stem cells, ECs can spontaneously form capillary-like networks within 3D biomaterial matrices [82] [85]. The presence of supporting cells is crucial, as they provide necessary paracrine signals and ECM remodeling activities that stabilize the emerging vascular structures [85].
In one representative approach, human umbilical vein endothelial cells (HUVECs) and human dermal fibroblasts were encapsulated in 3D co-cultures within various dextran-based hydrogels [85]. Only hydrogels conjugated with heparin and impregnated with VEGF and bFGF supported robust multicellular networks featuring higher densities of longer vessels with numerous branch points and defined lumen structures after 14 days [85].
Stem Cell-Based Approaches Stem cells, particularly mesenchymal stem cells (MSCs) and induced pluripotent stem cells (iPSCs), offer powerful tools for vascularization strategies. MSCs enhance vascularization by differentiating into multiple cell types and releasing pro-angiogenic factors like VEGF, supporting endothelial proliferation and maturation [84]. iPSCs provide scalability and potential for patient-specific therapy, crucial for long-term vascular integration [84].
The integration of cell-based approaches in tissue engineering represents a promising avenue for developing vascularized constructs. Across multiple studies, the synergistic use of MSCs and ECs has emerged as a fundamental strategy to promote both angiogenesis and osteogenesis, enhancing healing in large defects [84]. Innovations in scaffold-free techniques, such as temperature-responsive cell sheets, allow for autonomous formation of functional tissue analogues that enhance vascular integration [84].
Cell Encapsulation Technologies Cell encapsulation creates a protective environment that preserves cell viability, shields cells from immunological rejection, and enables sustained release of therapeutic molecules [87]. Biomaterial-supported cell encapsulation matrices have demonstrated superior properties for enhancing biological functionality, making them highly significant for translational medicine [87].
Microfluidic systems enable single-cell encapsulation, which offers improved circulation in the bloodstream and reduces the risk of entrapment compared to multicellular aggregates [87]. These advanced encapsulation techniques allow precise control over the cellular microenvironment, potentially enhancing the therapeutic potential of cell-based vascularization approaches.
Experimental Models and Assessment Methodologies
In Vitro Vascularization Models
The development of physiologically relevant in vitro models is essential for evaluating vascularization strategies and elucidating fundamental biological mechanisms.
Microfluidic Vascular Models Microfluidic systems, often referred to as "organs-on-chips," enable the creation of sophisticated in vitro vascular models with controlled geometries and perfusion conditions [86]. These platforms typically feature endothelialized microchannels surrounded by supporting cells and ECM components, allowing researchers to replicate key aspects of the vascular microenvironment, including shear stress, basement membrane interactions, and paracrine signaling [86].
Advanced microfluidic systems now incorporate multiple cell types (endothelial cells, pericytes, smooth muscle cells) in physiologically relevant arrangements, subject to controlled mechanical forces including fluid shear stress and cyclic stretch [86]. These systems have evolved from simple, straight channel designs to complex geometries with bifurcations, curvature, and 3D architecture that better mimic in vivo vascular networks [86].
3D Angiogenesis Assays Traditional 2D cultures fail to recapitulate the three-dimensional nature of vascular network formation. 3D angiogenesis assays embed endothelial cells within natural or synthetic hydrogels, often in co-culture with supporting cell types [85]. These systems allow assessment of multiple parameters, including:
- Endothelial cell sprouting and migration
- Tube formation and lumenogenesis
- Network complexity and connectivity
- Branching patterns and network remodeling
The angiogenic sprouting assay, where encapsulated HUVEC spheroids exhibit varying degrees of sprouting and endothelial cell invasion depending on hydrogel compositions, provides a robust platform for evaluating pro-angiogenic biomaterials [85].
Vascular Assessment and Quantification Methods
Accurate quantification of vascular networks is essential for evaluating the efficacy of vascularization strategies and optimizing biomaterial design.
Imaging and Visualization Techniques Multiple imaging modalities are employed to visualize vascular structures in both laboratory and clinical settings [88]. Confocal microscopy of fluorescently labeled vessels (e.g., with lectin stains or endothelial-specific antibodies) enables high-resolution 3D reconstruction of vascular networks [88]. Perfusion studies with fluorescent dextrans or other tracer molecules assess vascular functionality and connectivity to the host circulation [85].
For in vivo assessment, intravital microscopy techniques allow longitudinal monitoring of vascular development and remodeling within implanted constructs, providing valuable insights into the dynamics of the integration process.
Machine Learning-Enhanced Vascular Quantification Traditional methods for quantifying vascular density often rely on manual tracing, which is time-consuming and subject to observer bias [88]. Recent advances in machine learning and artificial intelligence have enabled development of semi-automated tools specifically designed for vascular analysis in complex tissue environments.
The BioSegment software leverages a machine learning deep convolutional neural network (CNN) to detect and localize user-defined vascular features within images [88]. This approach enables high-throughput quantification of vascular metrics, including vessel density, length, branching points, and diameter distribution, even in challenging samples with irregular vessel morphology or background noise [88]. Such tools are particularly valuable for tissue manufacturing workflows, where engineered constructs require frequent monitoring to ensure vascular growth benchmarks are met [88].
Table 3: Quantitative Methods for Vascular Assessment
| Method | Primary Output | Throughput | Limitations | Best Applications |
|---|---|---|---|---|
| Manual Tracing | Vessel length, density | Low | Time-consuming; observer-dependent | Small datasets; validation of automated methods |
| Angiogenesis Analyzer | Network morphology; branches; junctions | Medium | Limited to clear, uniform vasculature | 2D endothelial cell assays; simple 3D models |
| BioSegment | Vessel detection; density; length | High | Requires training data | High-throughput screening; complex 3D tissues |
| Perfusion Analysis | Functional vessel density; connectivity | Medium | Requires intravascular tracer | Assessment of network functionality and integration |
Experimental Protocols for Vascularization Research
Protocol: In Vitro Vascular Network Formation in 3D Hydrogels
This protocol describes a standardized method for evaluating the capacity of biomaterial scaffolds to support the formation of endothelial cell networks in 3D culture, adapted from established methodologies [85].
Materials
- Dextran-based hydrogel system: Methacrylated dextran (Dex-MA), MMP-cleavable crosslinker, thiol-terminated RGD peptide
- Human umbilical vein endothelial cells (HUVECs)
- Human dermal fibroblasts (HDFs)
- Endothelial cell growth medium: EGM-2 basal medium with supplements
- Pro-angiogenic factors: VEGF (50 ng/mL), bFGF (50 ng/mL)
- Heparin or heparin-mimetic biomaterial (optional)
- Cell viability assay: Calcein AM/EthD-1 or similar
- Immunostaining reagents: CD31 antibody, phalloidin, DAPI
- Confocal microscopy equipment
Procedure
- Hydrogel Preparation:
- Prepare dextran-based hydrogels by reacting Dex-MA with di-thiolated MMP-cleavable crosslinkers and thiol-terminated RGD peptides via Michael-type addition reaction.
- For functionalized hydrogels, conjugate heparin or incorporate heparin-mimetic biomaterials during crosslinking.
- Adjust hydrogel stiffness to intermediate range (~2 kPa) by controlling macromer concentration and crosslinking density.
Cell Encapsulation:
- Mix HUVECs and HDFs in a 2:1 ratio at a final density of 5-10 × 10^6 cells/mL in hydrogel precursor solution.
- Add VEGF and bFGF to final concentrations of 50 ng/mL each.
- Initiate crosslinking and plate the cell-hydrogel mixture in appropriate culture vessels.
- Culture in endothelial cell growth medium for up to 14 days, with medium changes every 2-3 days.
Assessment and Analysis:
- At designated time points (e.g., days 7 and 14), assess network formation by confocal microscopy.
- Fix constructs and immunostain for CD31 (endothelial marker) and actin cytoskeleton.
- Acquire z-stack images and create maximum intensity projections for analysis.
- Quantify network parameters: vessel density, vessel length, number of branch points, and lumen formation.
Troubleshooting
- Poor network formation: Optimize cell density, growth factor concentrations, and hydrogel stiffness.
- Rapid network regression: Ensure appropriate MMP sensitivity for matrix remodeling; consider adding additional stabilizing factors.
- Incomplete imaging penetration: Use optical clearing techniques for thicker constructs.
Protocol: Machine Learning-Assisted Vascular Quantification
This protocol describes the use of BioSegment software for high-throughput quantification of vascular networks, based on established methodologies [88].
Materials
- Fluorescent or phase contrast images of vascular networks
- BioSegment software (custom platform leveraging YOLOv4 neural network)
- Image preprocessing tools: ImageJ or similar software
- Training dataset: Expert-annotated vascular images
Procedure
- Image Preparation:
- For 3D confocal images, create maximum intensity projections using ImageJ and save as PNG files.
- Apply histogram equalization to enhance contrast if images have low feature distinction.
- For phase contrast images, convert to PNG format and apply same preprocessing.
Model Training:
- Import preprocessed images into BioSegment software environment.
- Generate expert annotations using polygonal chains (polylines) to identify vascular features.
- Manually trace vessels to create training data, with tracings converted to overlapping rectangles as input regions.
- Utilize transfer learning with pre-trained weights (YOLOv4-tiny.weights trained on MS-COCO dataset).
- Partition training data into three sets (training, validation, testing) and train the neural network.
Image Analysis:
- Apply trained model to new image datasets for vascular detection and quantification.
- Export quantitative metrics: vessel density, length distribution, branching frequency.
- Validate automated measurements against manual annotations for a subset of images.
Interpretation
- Higher vessel density and increased branching typically indicate more robust vascularization.
- Compare different experimental conditions using statistical analysis of multiple replicates.
- Consider vessel morphology (diameter, continuity) in addition to quantitative metrics.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Vascularization Studies
| Category | Specific Reagents/Materials | Function/Application | Key Considerations |
|---|---|---|---|
| Biomaterials | Methacrylated dextran; PEGDA; GelMA; collagen; fibrin | 3D scaffold formation; controlled release | Tunable stiffness; degradation profile; biocompatibility |
| Pro-Angiogenic Factors | VEGF; bFGF; PDGF; Angiopoietin-1 | Stimulate endothelial cell behavior | Short half-life requires stabilization; concentration-dependent effects |
| Heparin-Based Materials | Native heparin; heparin-mimetic dextran sulfate | Growth factor stabilization; controlled release | Anticoagulant activity may cause bleeding; batch variability |
| Endothelial Cells | HUVECs; HMVECs; EPCs | Vasculature formation; network assembly | Source variability; limited expansion capacity; donor differences |
| Supporting Cells | Human dermal fibroblasts; MSCs; pericytes | Paracrine signaling; vessel stabilization | Cell ratio optimization; culture condition requirements |
| Characterization Tools CD31 antibodies; lectin stains; viability assays | Network visualization; quantification | Antibody specificity; staining penetration in 3D | |
| Analysis Software | BioSegment; Angiogenesis Analyzer; ImageJ plugins | Quantitative vascular analysis | Training requirements; parameter optimization; validation needs |
Signaling Pathways in Vascularization
The following diagrams illustrate key molecular mechanisms involved in vascular development and maturation, providing insight into potential therapeutic targets for enhancing vascularization.
Integrin Signaling Pathway: This diagram illustrates how extracellular matrix (ECM) components engage integrin receptors to activate downstream signaling pathways that regulate essential cellular processes in vascular development. Integrin binding initiates focal adhesion kinase (FAK) activation, which recruits Src family kinases and activates both MAPK/ERK and PI3K/Akt pathways, collectively coordinating cell adhesion, migration, proliferation, and survival during vascularization [27].
Hypoxia-Induced Angiogenic Signaling: This diagram shows the molecular response to hypoxic conditions that drives spontaneous vascularization. Hypoxia stabilizes hypoxia-inducible factor-1 (HIF-1), which induces VEGF expression. VEGF binding to VEGFR2 activates downstream Ras/Raf/ERK pathways, while parallel EGF signaling activates ERK5, collectively regulating endothelial cell proliferation and migration [83].
The strategic enhancement of vascularization and tissue integration represents a cornerstone challenge in the development of advanced biomaterial systems for controlled drug delivery. Current approaches span multiple complementary strategies: scaffold functionalization with growth factors, advanced delivery systems for sequential factor release, cell-based techniques utilizing endothelial and stem cells, and sophisticated in vitro models for evaluation and optimization.
Future directions in vascularization research will likely focus on several key areas:
- Personalized approaches leveraging patient-specific cells and biomarkers
- Multimodal strategies combining biochemical, physical, and cellular cues
- Dynamic, responsive systems that adapt to the changing tissue environment
- Advanced manufacturing techniques for creating hierarchical vascular architectures
- Integration with sensing technologies for real-time monitoring of integration success
As these technologies mature, they will increasingly enable the creation of biomaterial-based drug delivery systems that not only deliver therapeutic agents but actively participate in the regenerative process through guided vascular integration. This synergistic approach holds particular promise for addressing complex clinical challenges in tissue repair, regeneration, and sustained therapeutic delivery.
High-Throughput Screening and Orthogonal Experiments for Material Optimization
The development of advanced biomaterials for controlled drug delivery is a complex, multi-parameter challenge. Traditional trial-and-error approaches are insufficient for efficiently optimizing the multitude of material properties that influence drug release kinetics, biocompatibility, and therapeutic efficacy. High-Throughput Screening (HTS) has emerged as a transformative methodology that enables the rapid assessment of thousands of material combinations in a single experiment, dramatically accelerating the optimization process [89]. When integrated with orthogonal validation strategies, this approach provides a powerful framework for identifying optimal biomaterial formulations with enhanced predictive accuracy for in vivo performance.
In the specific context of drug delivery systems, HTS enables researchers to systematically investigate how variations in material composition, physical properties, and structural parameters influence drug loading capacity, release profiles, and biological interactions. The integration of orthogonal experiments is critical for confirming that identified "hit" formulations exhibit genuine functional properties rather than assay-specific artifacts [90]. This combined approach is particularly valuable for addressing the challenges of modern drug delivery, including the need for targeted release, reduced side effects, and improved therapeutic outcomes across diverse pathological conditions [7].
High-Throughput Screening Methodologies for Biomaterial Optimization
Core Principles and Technical Implementation
High-Throughput Screening (HTS) is an automated methodology that enables the rapid testing of thousands—even millions—of chemical, biological, or material samples in a highly parallelized format [91]. In the context of biomaterials for drug delivery, HTS facilitates the efficient exploration of complex parameter spaces that would be prohibitively time-consuming using conventional methods. A single HTS experiment can process over 10,000 samples per day, compared to approximately 100 samples per week with traditional laboratory techniques [91].
The fundamental workflow of HTS involves several standardized steps: (1) library preparation of material formulations or compound collections; (2) automated liquid handling using robotics to dispense minute volumes into multi-well plates (96, 384, or 1536 wells); (3) assay execution with appropriate biological or chemical tests; and (4) data analysis using statistical methods to identify active compounds or optimal formulations [91]. The reliability of HTS assays is typically quantified using the Z'-factor, with values above 0.5 generally indicating robust assay performance [91].
Quantitative HTS (qHTS) represents an advanced evolution of this approach, wherein compounds or materials are tested across a range of concentrations or parameter values rather than at a single point [92]. This methodology generates complete concentration-response curves for each tested condition, providing rich datasets that enable more accurate potency estimates and reduce false negatives that frequently occur in single-concentration screens [92]. The qHTS approach produces concentration-response curves that are classified based on quality of fit (r²), response magnitude (efficacy), and curve completeness (asymptotes) into four distinct categories: Class 1 (complete curves), Class 2 (incomplete curves), Class 3 (activity only at highest concentration), and Class 4 (inactive) [92].
Advanced HTS Platforms for Multi-Parameter Biomaterial Screening
Innovative HTS platforms have been developed specifically to address the multi-factorial nature of biomaterial optimization. The double-orthogonal gradient (DOG) screening technology represents a particularly advanced approach that enables simultaneous investigation of three critical surface parameters: stiffness (S), wettability (W), and topography (T) [89]. This platform utilizes surface gradients of these parameters orthogonally combined to create a comprehensive screening surface that incorporates every parameter combination within their tunable boundaries [89].
The DOG platform is fabricated on 20 × 20 mm polydimethylsiloxane (PDMS) substrates using multistep sequential air plasma treatments [89]. After characterization, cells are seeded and cultured on these gradient surfaces, followed by fixation, immunostaining, and automated imaging. The resulting data is visualized as heat maps and 3D representations that facilitate identification of regions of interest (ROIs) where specific cell behaviors (e.g., adhesion, spreading, vimentin expression) are optimized [89]. These ROIs are subsequently translated to homogeneous substrates for validation, enabling direct correlation of cellular responses with specific parameter combinations.
Another innovative approach integrates photo-controlled thiol-ene surface chemistry with machine learning-based label-free cell identification and statistics [93]. This system utilizes chips with orthogonal gradients of functional molecular densities to significantly increase screening throughput while maintaining biological relevance [93]. Such platforms have successfully identified specific combinatorial densities of polyethylene glycol (PEG) and REDV peptide that promote endothelial cell selectivity over smooth muscle cells, with subsequent translation to medical nickel-titanium alloy surfaces to improve endothelialization [93].
Table 1: Comparison of HTS Approaches for Biomaterial Optimization
| HTS Approach | Key Features | Throughput | Parameters Screened | Applications in Drug Delivery |
|---|---|---|---|---|
| Traditional HTS | Single-point screening; compound libraries | 10,000+ samples/day | Single parameter per assay | Initial compound library screening; hit identification |
| Quantitative HTS (qHTS) | Concentration-response curves; multiple data points per sample | ≈50-70% of traditional HTS | Potency, efficacy, toxicity | Dose-response characterization; reduced false negatives |
| Double-Orthogonal Gradient (DOG) | Simultaneous gradient screening; orthogonal parameter combination | 4 combinatorial surfaces in single experiment | Stiffness, wettability, topography | Optimizing cell-material interactions for implantable devices |
| Combinatorial Surface Chemistry | Orthogonal molecular density gradients; machine learning analysis | High-throughput cell selectivity screening | Functional molecular density & combination | Selective cell adhesion surfaces; targeted delivery systems |
Orthogonal Experiments for Hit Validation in Biomaterial Development
The Essential Role of Orthogonal Validation
In HTS campaigns for biomaterial optimization, initial "hits" – formulations showing promising properties – must be rigorously validated to distinguish genuine bioactivity from assay-specific artifacts. Orthogonal experiments are specifically designed for this purpose, employing different assay principles or readout technologies to confirm the biological activity or material properties observed in primary screens [90]. This validation strategy is particularly crucial in biomaterial science for drug delivery, where material-performance relationships must be reliably established before progressing to costly in vivo studies.
Orthogonal validation serves multiple critical functions: (1) confirming primary screening results through independent methodological approaches; (2) identifying and eliminating false positives caused by assay interference; (3) providing additional layers of characterization for promising material formulations; and (4) building confidence in structure-activity relationships before committing to further development [90]. For biomaterials intended for controlled drug delivery, orthogonal approaches typically evaluate the same fundamental biological outcome or material property as the primary assay but employ complementary detection methods or experimental systems.
Implementing Orthogonal Assays for Drug Delivery Biomaterials
A strategic cascade of orthogonal assays should be implemented to validate HTS hits for biomaterial drug delivery systems. For primary screens utilizing fluorescence-based readouts, orthogonal validation should employ alternative detection methods such as luminescence- or absorbance-based assays [90]. Similarly, bulk-readout assays (single value per well) should be supplemented with high-content imaging and analysis that provide single-cell resolution and additional morphological data [90].
For biomaterial formulations targeting specific biological interactions, cell-based phenotypic screening should be validated using different cell models (2D vs. 3D cultures), relevant primary cells, or more physiologically relevant culture conditions [90]. Additionally, biophysical characterization techniques including surface plasmon resonance (SPR), isothermal titration calorimetry (ITC), microscale thermophoresis (MST), and thermal shift assays (TSA) provide complementary data on material-target interactions, binding affinities, and structural stability [90].
The critical importance of orthogonal validation is underscored by research demonstrating that compounds with artifact nature can produce convincing-looking dose-response curves in primary screens [90]. Without orthogonal confirmation, these false positives can misdirect research efforts and resources. This is particularly relevant for biomaterial drug delivery systems, where optimal formulations must balance multiple performance parameters including drug loading capacity, controlled release kinetics, biocompatibility, and target-specific delivery.
Table 2: Orthogonal Assay Strategies for Biomaterial Hit Validation
| Primary Screen Readout | Orthogonal Assay Options | Key Measured Parameters | Application in Drug Delivery Biomaterials |
|---|---|---|---|
| Fluorescence-based | Luminescence- or absorbance-based assays | Release kinetics; cellular uptake; targeting efficiency | Confirmation of drug release profiles; verification of cellular internalization |
| Bulk population readouts | High-content imaging; single-cell analysis | Heterogeneity of cell responses; subcellular localization | Spatial distribution of drug release; single-cell response variability |
| Biochemical binding assays | Biophysical methods (SPR, ITC, MST, TSA) | Binding affinity; thermodynamics; binding stoichiometry | Ligand-receptor interactions for targeted delivery systems |
| Simple 2D cell cultures | Complex 3D models; primary cells; co-culture systems | Penetration depth; efficacy in physiological models; cell-type specificity | Performance in tissue-mimicking environments; cell-selective targeting |
Integrated Workflows: Combining HTS and Orthogonal Methods
The most effective biomaterial optimization strategies seamlessly integrate HTS with orthogonal validation into a cohesive workflow. This integrated approach begins with primary HTS to identify initial hits, progresses through orthogonal confirmation, and culminates in advanced characterization of validated leads. The entire process is designed to maximize efficiency while ensuring the reliability of selected formulations.
Diagram: Integrated HTS and Orthogonal Validation Workflow
Counter Screens and Cellular Fitness Assessments
Beyond orthogonal assays, comprehensive hit validation requires counter screens and cellular fitness assessments to exclude artifacts and toxic formulations. Counter screens are specifically designed to identify compounds or materials that interfere with assay technology rather than genuinely modulating biological activity [90]. For biomaterial drug delivery systems, this includes testing for autofluorescence, signal quenching, singlet oxygen quenching, light scattering, and reporter enzyme modulation [90].
Cellular fitness screens are equally critical for evaluating potential toxicity or detrimental effects on cell health. These assessments utilize viability assays (e.g., CellTiter-Glo, MTT), cytotoxicity measurements (e.g., LDH release, CellTox Green), and apoptosis detection (e.g., caspase activation) [90]. Advanced morphological profiling using cell painting assays – which employ multiplexed fluorescent staining of eight cellular components – provides comprehensive evaluation of cellular states following material exposure [90]. This extensive staining coupled with machine learning analysis enables detailed assessment of material-induced cytopathology and prediction of cellular toxicity [90].
For complex biomaterial formulations such as biodegradable graphene nanocomposites (BGNs), these integrated workflows are particularly valuable. BGNs combine the exceptional physicochemical properties of graphene with the biocompatibility of biodegradable polymers, creating materials with high drug loading capacity and tunable release kinetics [52]. HTS approaches facilitate optimization of BGN composition, while orthogonal methods confirm drug delivery functionality and cellular compatibility.
Application Case Studies in Drug Delivery Systems
Gradient-Based Screening for Implantable Drug Delivery Devices
The DOG screening platform has demonstrated particular utility for optimizing surface properties of implantable drug delivery devices. In one application, this technology was used to investigate the response of human bone-marrow-derived mesenchymal stem cells (hBM-MSCs) to combinatorial surface properties [89]. The platform identified optimal combinations of stiffness, wettability, and topography that enhanced cell adhesion, spreading, and vimentin expression – critical factors for successful integration of implantable devices [89].
Following screening, regions of interest were translated to homogeneous substrates bearing the exact parameter combinations identified in the screen [89]. Cells cultured on these translated surfaces exhibited similar behaviors to those observed in the screening platform, validating the HTS approach and demonstrating its translational potential [89]. This methodology represents a significant advancement over traditional approaches that typically investigate parameters in isolation rather than assessing their combinatorial effects.
Machine Learning-Enhanced HTS for Selective Biomaterial Surfaces
An innovative paradigm combining HTS with machine learning has been developed for screening cell-selective biomaterial surfaces [93]. This approach utilizes chips with orthogonal gradients of functional molecular densities to significantly increase throughput while maintaining biological relevance [93]. Machine learning-based graph recognition enables rapid cell identification and statistics in co-culture systems, facilitating efficient screening of surface compositions that promote selective cell behaviors [93].
In a specific application, this technology identified a particular combinatorial density of polyethylene glycol (PEG) and REDV peptide that selectively promotes endothelial cell (EC) adhesion over smooth muscle cells (SMC) [93]. This optimized composition was successfully translated as a coating formula for medical nickel-titanium alloy surfaces, where it improved EC competitiveness and induced endothelialization – a critical requirement for vascular drug delivery devices [93].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for HTS and Orthogonal Biomaterial Screening
| Reagent/Material | Function in HTS/Orthogonal Screening | Specific Applications in Drug Delivery |
|---|---|---|
| Polydimethylsiloxane (PDMS) | Substrate for gradient fabrication; flexible polymer platform | DOG screening platforms; implantable device prototypes |
| Polyethylene Glycol (PEG) | Bioinert polymer; controls surface properties & protein adsorption | Stealth drug delivery systems; reducing non-specific binding |
| Functional Peptides (e.g., REDV) | Promotes specific cell adhesion; enhances biocompatibility | Targeted drug delivery; endothelialization of implants |
| Graphene Oxide (GO) | High surface area nanomaterial; drug loading carrier | Controlled release systems; composite biomaterials |
| Biodegradable Polymers (PLA, PLGA) | Temporary structural support; controlled degradation | Injectable depots; tissue engineering scaffolds |
| Photo-reactive Crosslinkers | Spatially controlled surface modification; patterning | Precision surface engineering; gradient fabrication |
Quality Control and Data Analysis in HTS
Robust quality control procedures are essential for ensuring the reliability of HTS data, particularly in quantitative HTS (qHTS) where concentration-response relationships are characterized. The CASANOVA (Cluster Analysis by Subgroups using ANOVA) method provides an automated quality control approach that identifies and filters out compounds with multiple cluster response patterns to improve potency estimation in qHTS assays [94]. This method is particularly important given that only approximately 20% of compounds with response values outside the noise band demonstrate single cluster responses across experimental replicates [94].
Systematic quality control is crucial because inconsistent response patterns can lead to highly variable potency estimates for the same compound [94]. Factors contributing to this variability include chemical supplier differences, institutional site preparation of chemical libraries, concentration-spacing, and compound purity [94]. Without proper quality control, potency estimates derived from qHTS assays may be unreliable for downstream applications such as predictive cheminformatics, in vivo activity modeling, and drug sensitivity testing [94].
Diagram: Quality Control Pipeline for qHTS Data
The integration of High-Throughput Screening with orthogonal experimental validation represents a paradigm shift in biomaterial optimization for controlled drug delivery systems. This combined approach enables comprehensive exploration of complex parameter spaces while ensuring the reliability and biological relevance of identified "hit" formulations. As the field advances, emerging technologies including artificial intelligence-driven screening design, miniaturized screening platforms, and self-driving laboratories promise to further accelerate the development of advanced drug delivery biomaterials [91].
The continued refinement of HTS technologies, particularly those enabling multi-parameter optimization like the DOG platform, will be essential for addressing the increasingly sophisticated requirements of modern drug delivery systems. Similarly, the development of more physiologically relevant orthogonal assays – including complex 3D tissue models and organ-on-a-chip systems – will enhance the predictive accuracy of screening outcomes for in vivo performance. Together, these methodologies provide a powerful framework for advancing the next generation of biomaterial-based drug delivery systems with enhanced therapeutic efficacy and reduced side effects.
The Role of AI and Machine Learning in Predictive Biomaterial Design
The field of biomaterials for controlled drug delivery is undergoing a fundamental transformation, shifting from traditional, empirical "trial-and-error" approaches to a data-driven paradigm powered by artificial intelligence (AI) and machine learning (ML) [42]. This revolution is critical for designing next-generation biomaterials that are dynamic, programmable, and capable of interacting with biological environments with high precision and purpose [42]. The integration of AI is accelerating biomaterial discovery, optimizing material properties, and advancing innovations from laboratory research to clinical application, thereby enhancing the development of safer, more personalized, and future-ready biomedical interventions [42] [95]. Within this context, predictive biomaterial design has emerged as a cornerstone for creating advanced drug delivery systems (DDSs), enabling researchers to navigate the complex parameter space of material synthesis and biological interactions with unprecedented speed and accuracy [96].
Computational Frameworks: AI/ML Algorithms in Biomaterial Science
The application of AI in biomaterial design leverages a suite of computational algorithms, each suited to specific types of problems and data structures. These algorithms can analyze vast datasets, review diverse biomaterials, plan complex experiments, and predict materials that fulfill strict specifications for a desired application [95].
Key Machine Learning Algorithms
- Random Forest (RF): An ensemble learning method that operates by constructing a multitude of decision trees. It is highly effective for classification and regression tasks and is particularly valued for its robustness and ability to handle high-dimensional data. In one study, an RF algorithm achieved the highest accuracy (88.1%), precision (90.6%), and F1 score (87.0%) in predicting the printability of biomaterial inks for 3D printing [97].
- Deep Learning (DL): Utilizes artificial neural networks with multiple layers to model complex, non-linear relationships. DL excels at tasks involving unstructured data like images and complex pattern recognition. In printability prediction, a DL model demonstrated the highest recall (87.3%), indicating a superior ability to minimize false negatives [97].
- Kernel Machine Models/Hybrid Systems: Advanced models like the Tunable Nanoparticle platform guided by AI (TuNa-AI) represent a hybrid approach designed to handle complex optimization problems. Unlike standard models, TuNa-AI can simultaneously optimize both the identity of ingredients and their mixing ratios, a critical requirement for formulating stable drug-loaded nanoparticles. This platform resulted in a 42.9% increase in successful nanoparticle formation compared to standard approaches [98].
Table 1: Key Machine Learning Algorithms and Their Applications in Biomaterial Design
| Algorithm | Primary Function | Advantages | Exemplary Application in Biomaterials |
|---|---|---|---|
| Random Forest (RF) | Classification, Regression | High accuracy, handles high-dimensional data, robust to overfitting | Predicting biomaterial ink printability for 3D printing [97] |
| Deep Learning (DL) | Pattern Recognition, Complex Modeling | Models highly non-linear relationships, excels with image/data | Generating fine-granularity printability maps for ink development [97] |
| Hybrid Kernel Machines (e.g., TuNa-AI) | Multi-parameter Optimization | Optimizes both material identity and quantity ratios | Designing and optimizing tunable nanoparticles for drug delivery [98] |
| Decision Tree (DT) | Classification, Regression | Simple, interpretable model structure | Baseline model for predicting printability of biomaterials [97] |
AI-Driven Design of Key Biomaterials for Drug Delivery
AI and ML methodologies are being deployed across various classes of biomaterials to overcome specific challenges in drug delivery, from nanoparticle formulation to the creation of smart scaffolds.
Nanoparticle Design and Optimization
The synthesis of nanomedicines involves numerous parameters, and the complexity of nano-bio interactions in vivo presents significant difficulties [96]. ML guides the rational design of nanoparticles (NPs) across multiple stages:
- Synthesis and Formulation: ML accelerates the process of identifying optimal synthesis parameters and material ratios. For instance, the TuNa-AI platform uses an automated robotic system to generate extensive datasets (e.g., 1275 distinct formulations) that train AI models to select and optimize nanoparticle recipes. This has been successfully used to improve the encapsulation of venetoclax, a leukemia drug, resulting in nanoparticles with improved solubility and enhanced efficacy in halting leukemia cell growth in vitro [98].
- Predicting Nano-Bio Interactions: ML models are developed to predict complex interactions, including NP-protein interactions (corona formation), blood circulation time, extravasation into the tumor microenvironment, tumor penetration, and cellular internalization. This comprehensive approach aims to enhance delivery efficiency and therapeutic outcomes in precision cancer nanomedicine [96].
3D Printable Biomaterial Inks
The development of biomaterial inks for 3D printing, particularly for applications like drug-eluting scaffolds, has been hampered by time-consuming empirical printability testing. ML directly addresses this bottleneck.
- Printability Prediction: ML algorithms can predict the "printability" of a biomaterial formulation—its ability to be extruded and maintain shape fidelity (SF)—based on its composition. Researchers have trained models on datasets of 210 formulations containing 16 different bioactive and smart materials. The models successfully classified printability (yes/no), guiding the ink development process and generating predictive "printability windows" [97].
- Workflow Integration: The process involves 3D printing various formulations, quantitatively assessing their SF, and using this data to train ML models. These models can then rapidly screen virtual formulations, significantly accelerating the development of new printable biomaterials for biomedical engineering [97].
Smart Hydrogels
Hydrogels are a cornerstone of biomedical applications due to their similarity to natural tissues. AI is revitalizing their design and optimization.
- Property Prediction and Multi-attribute Optimization: AI technology allows for the prediction and optimization of hydrogel composition and properties. Models can be built to automatically adjust parameters during the preparation process to achieve desired outcomes, such as tailored mechanical properties, swelling behavior, and drug release profiles [99].
- High-Throughput Screening: Combined with automated high-throughput experimentation, AI enables the rapid screening of a vast space of hydrogel formulations, moving away from slow, traditional development methods. This is particularly useful for designing environmentally responsive hydrogels (e.g., pH- or temperature-sensitive) for targeted drug delivery [99].
Experimental Protocols and Methodologies
To illustrate the practical integration of AI into biomaterial research, here are detailed methodologies for key experiments cited in this guide.
Protocol 1: AI-Driven Design of Tunable Drug-Loaded Nanoparticles
This protocol is based on the TuNa-AI platform for designing and optimizing nanoparticles (NPs) for drug delivery [98].
- Objective: To identify an optimal nanoparticle formulation that maximizes drug encapsulation efficiency and stability.
- Automated Library Generation:
- Utilize an automated liquid handling robot to systematically mix a library of excipients (e.g., lipids, polymers) with one or more therapeutic agents in a wide range of predetermined ratios.
- This generates a large dataset (e.g., 1275 distinct formulations) where each data point represents a unique recipe.
- Data Labeling and Characterization:
- For each formulated NP, characterize key performance metrics, including:
- Formation Success: A binary label (success/failure) for stable NP formation.
- Encapsulation Efficiency: The percentage of the drug successfully incorporated into the NP.
- Size and Polydispersity: Measured via dynamic light scattering (DLS).
- This creates a labeled dataset for ML training.
- For each formulated NP, characterize key performance metrics, including:
- Model Training and Optimization (TuNa-AI):
- Train a hybrid kernel machine model on the generated dataset. The model learns the complex relationships between the input parameters (excipient identity and quantitative ratios) and the output performance metrics.
- Use the trained model to predict the optimal formulation (ingredients and ratios) that maximizes the desired outcomes (e.g., formation success and encapsulation).
- Validation and Testing:
- Synthesize the AI-predicted optimal NP formulation in the lab.
- Validate the model's accuracy by testing the resulting NPs for encapsulation efficiency, stability, and in vitro therapeutic efficacy (e.g., ability to halt cancer cell growth in a leukemia model).
AI-Driven Nanoparticle Design Workflow
Protocol 2: Predicting Biomaterial Printability via Machine Learning
This protocol details the use of ML to predict the printability of biomaterial inks for 3D direct ink writing (DIW) [97].
- Objective: To train an ML model that can accurately predict if a new biomaterial formulation will be printable.
- Ink Formulation and Printing:
- Prepare a large and diverse set of biomaterial ink formulations (e.g., 210 samples) by varying polymers (e.g., Pluronic F127, polycaprolactone), solvents (aqueous/organic), and functional fillers (e.g., Laponite nanoclay, hydroxyapatite nanoparticles).
- Quantitative Printability Assessment:
- 3D print each formulation into a standardized structure (e.g., a 4-layer 0°/90° grid scaffold).
- Calculate the Shape Fidelity (SF) for each printed structure. SF is a quantitative measure of printability, often defined as the agreement between the designed (CAD) structure and the actual printed structure. Formulations are then classified as "printable" or "non-printable" based on a predefined SF threshold.
- Dataset Curation for ML:
- Construct a dataset where the input features are the ink formulation components and their concentrations, and the output label is the binary printability classification.
- Model Training and Evaluation:
- Split the dataset into training and testing sets (e.g., 70:30 ratio).
- Train multiple ML algorithms (e.g., Decision Tree, Random Forest, Deep Learning) on the training data.
- Evaluate and compare model performance using metrics like accuracy, precision, recall, and F1 score to select the best-performing model (e.g., Random Forest with 88.1% accuracy).
- Model Deployment and Prediction:
- Use the trained model to predict the printability of new, untested formulations, generating a "printability map" to guide future ink development.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials and reagents essential for conducting experiments in AI-guided predictive biomaterial design, as featured in the cited research.
Table 2: Research Reagent Solutions for AI-Guided Biomaterial Experiments
| Reagent/Material | Function in Research | Exemplary Application |
|---|---|---|
| Pluronic F127 | A thermo-gelling, biocompatible synthetic polymer used to form shear-thinning hydrogels. | Key component of hydrogel-based bioinks for 3D bioprinting and drug delivery [97]. |
| Polycaprolactone (PCL) | A biodegradable polyester providing mechanical strength; often dissolved in organic solvents for printing. | Used in polymer-based inks for creating robust bone tissue engineering scaffolds [97]. |
| Laponite (LP) Nanoclay | A bioactive viscosity enhancer and rheological modifier for ink formulations. | Added to hydrogel inks to improve printability and shape fidelity [97]. |
| Hydroxyapatite Nanoparticles (nHA) | A bioactive ceramic that mimics bone mineral, enhancing osteoconductivity. | Filler in polymer-based inks (e.g., with PCL) for bone tissue engineering scaffolds [97]. |
| Albumin | A natural protein that can self-assemble and bind therapeutic molecules. | Serves as a versatile excipient for creating nanoparticle drug formulations (e.g., Abraxane) [42] [98]. |
| Venetoclax | A model BCL-2 inhibitor chemotherapeutic drug that is difficult to encapsulate. | Used as a challenging payload to test the efficacy of AI-designed nanoparticle delivery systems [98]. |
| PEGylated Lipids | Lipids conjugated with polyethylene glycol (PEG) to create stealth coatings on nanoparticles. | Critical excipients in AI-designed liposomal formulations to reduce opsonization and prolong blood circulation time [42] [96]. |
Challenges and Future Perspectives
Despite its transformative potential, the integration of AI into predictive biomaterial design faces several hurdles. The "black box" nature of some complex ML models hinders interpretability and widespread adoption in interdisciplinary research [97]. There is also a critical need for large, high-quality, and standardized datasets to train robust models, as current data are often fragmented and inconsistent [100] [96]. Furthermore, navigating the regulatory approval pathway for AI-designed biomaterials presents a new challenge for translational medicine [42].
Future progress depends on collaborative efforts to establish public, curated biomaterial databases, develop more interpretable AI models, and create frameworks for clinical validation. By addressing these challenges, the synergy of AI and biomaterial science will fully realize its potential in creating intelligent therapeutic platforms for precision medicine, ultimately leading to more effective and personalized drug delivery systems [101] [102] [100].
Future AI-Biomaterials Research Roadmap
Bench-to-Bedside Translation: Evaluating Efficacy, Safety, and Commercial Viability
In Vitro and In Vivo Models for Assessing Therapeutic Efficacy and Safety
The journey of a new therapeutic from discovery to clinical approval is a long, expensive, and complex process, typically taking 10–15 years and requiring billions of dollars [103] [104]. A significant bottleneck in this pipeline is the unreliable prediction of human efficacy and toxicity, particularly drug-induced liver injury (DILI), which contributes significantly to the approximately 90% failure rate of drugs between Phase 1 trials and market [103]. Preclinical models—ranging from simple cell cultures to complex animal studies—serve as the essential foundation for assessing therapeutic efficacy and safety before human trials.
Within the specific context of biomaterials in controlled drug delivery, these models take on heightened importance. The integration of functional biomaterials aims to overcome major biological barriers—such as enzyme degradation and poor cellular transport—to improve drug stability, targetability, and therapeutic effectiveness [8]. Evaluating whether these advanced delivery systems (e.g., nanoparticles, hydrogels, microrobots) successfully achieve their goals without unintended consequences depends entirely on robust, predictive preclinical models. This guide provides an in-depth technical overview of the current landscape of these models, detailing their applications, limitations, methodologies, and their pivotal role in de-risking the development of biomaterial-based drug delivery systems.
The Pressing Need for Improved Models in Drug Development
The traditional drug development paradigm has heavily relied on animal testing for preclinical safety assessment. However, this approach is often time-consuming, costly, and exhibits poor correlation with human outcomes due to profound interspecies physiological differences [103]. A comprehensive review highlights the two critical missteps in animal testing: the safe tagging of a toxic drug and the toxic tagging of a beneficial drug [103]. Notably, nearly half of the 578 drugs withdrawn or discontinued post-approval in the US and Europe were due to toxicity issues uncovered in humans [103].
This predictive failure has driven regulatory modernization, exemplified by the FDA Modernization Act 2.0, which now allows for alternatives to animal testing, including advanced in vitro models and computer models, for drug and biological product applications [103] [104]. Similarly, the European Union and other countries have implemented bans on animal testing for cosmetics [103]. This regulatory shift has accelerated the development and adoption of more human-relevant systems, particularly Complex In Vitro Models (CIVMs) that incorporate three-dimensional (3D) structures, multicellular environments, and physiological cues to better mimic human organ and tissue biology [104].
Landscape of In Vitro Models
In vitro models have evolved from simple two-dimensional (2D) cultures into sophisticated systems that more accurately recapitulate the in vivo microenvironment.
Two-Dimensional (2D) Cell Cultures
Description and Applications: 2D cell cultures, where cells grow as a monolayer on a flat surface, are the most accessible and widely used in vitro model. They are affordable, easy to use, and amenable to high-throughput screening (HTS). In drug discovery, they are crucial for initial HTS, serving as disease models for efficacy assessments and early safety evaluations [103]. Cell-based assays account for nearly half of HTS efforts and provide insights into toxicity profiles, impacts on signaling pathways, and overall cellular effects [103].
Key Limitations: The primary drawback of 2D cultures is their notable disparity from in vivo conditions. They fail to replicate the tissue-specific mechanical and biochemical characteristics of target organs, including cell-cell and cell-matrix interactions, nutrient gradients, and physiologically relevant mechanical forces [104]. Furthermore, the artificial environment can lead to genotypic and phenotypic drift in cell lines over time, potentially altering drug sensitivity and response [105].
Complex In Vitro Models (CIVMs)
CIVMs are defined as systems in a 3D multi-cellular environment within a biopolymer or tissue-derived matrix. They often incorporate primary or stem cell-derived cells, immune system components, and mechanical factors like stretch or perfusion [104]. These models bridge the gap between conventional 2D cultures and in vivo models.
- Organoids: Organoids are 3D structures derived from pluripotent stem cells (PSCs), neonatal tissue stem cells, or adult stem cells (ASCs) that spontaneously self-organize into properly differentiated functional cell types, resembling their in vivo counterpart and imitating some organ functions [104]. They require specific media compositions recapitulating the in vivo stem cell niche and are typically embedded in matrices like Matrigel to support 3D growth.
- Spheroids: Simple 3D aggregates of cells that form through self-assembly. While less complex than organoids, they model some aspects of tissue microenvironments and drug penetration.
- Organ-on-a-Chip (OOC) Systems: Microfluidic devices that house living cells arranged to model organ-level physiology and pathophysiology. They can incorporate dynamic fluid flow, mechanical cues (e.g., cyclic strain), and organ-organ interactions [103]. For orally administered drugs (which constitute ~80% of best-selling drugs), combined systems like gut-liver-on-a-chip are highly valuable for evaluating drug metabolism and toxicity (DILI) [103].
- Tissue Slice Cultures: Precision-cut slices of animal or human tissue that retain the original tissue's heterogeneous cellular composition, native 3D architecture, and extracellular matrix [104] [105]. They are particularly useful for studying complex tissues like the liver or brain.
Table 1: Comparison of Major In Vitro Model Types
| Model Type | Key Characteristics | Primary Applications in Drug Delivery | Key Advantages | Major Limitations |
|---|---|---|---|---|
| 2D Cell Culture | Monolayer culture; simple setup [104] | High-throughput screening (HTS), initial efficacy/toxicity tests [103] | Low cost, high scalability, easy readouts [103] | Low physiological relevance, no tissue context [104] |
| Organoids | 3D, self-organizing, stem cell-derived [104] | Disease modeling, personalized drug screening [104] | High biological relevance, patient-specific (PDOs) [104] | Variable reproducibility, high cost, complex culture [104] |
| Spheroids | 3D cell aggregates | Penetration studies, intermediate complexity assays | Simple formation, better than 2D for some endpoints | Limited complexity and maturity |
| Organ-on-a-Chip | Microfluidic, dynamic flow, multi-cellular [103] [104] | ADME studies, DILI assessment, barrier function [103] | Incorporates physiological shear/stress, human-relevant [103] | Technically complex, low-to-medium throughput [103] |
| Tissue Slices | Ex vivo, native tissue architecture [104] [105] | Metabolism studies, toxicity in native tissue context [105] | Preserves in vivo cell heterogeneity and ECM [105] | Limited lifespan, donor variability, access to human tissue [105] |
Landscape of In Vivo Models
In vivo models remain indispensable for studying whole-body physiology, systemic drug effects, and complex interactions between organs.
Murine Models (Mice and Rats)
Description and Applications: Mice and rats are the most commonly used animal models in biomedical research. They are used to investigate the overall effects of therapeutics on the body, including pharmacokinetics, biodistribution, efficacy, and systemic toxicity [103]. Their short reproductive cycles, well-characterized genetics, and the availability of extensive historical data are significant advantages.
Advanced Murine Models:
- Genetically Engineered Mouse Models (GEMMs): These models have specific genes inserted, deleted, or modified to study their function in disease or to create human-relevant disease phenotypes.
- Xenograft Models: Human tumor cells or patient-derived tumor tissue (PDX) are implanted into immunocompromised mice to study cancer biology and evaluate oncology therapeutics [103] [105].
- Humanized Mice: These models are engrafted with human cells or tissues, most commonly components of the human immune system. This has emerged as a major tool for accurately modeling human immune responses, which is critical for immuno-oncology and vaccine development [103].
Non-Human Primates (NHPs)
Description and Applications: Due to their close phylogenetic and biochemical similarity to humans, NHPs like rhesus macaques are used for studies where rodent models are insufficient. They have been extensively used for vaccine development, orthopedic surgical techniques, and neurodegenerative diseases like Parkinson's [103]. Their immune responses are particularly similar to humans, making them reliable for researching diseases like HIV, Zika virus, and tuberculosis [103].
Critical Considerations in In Vivo Modeling for Drug Delivery
When testing biomaterial-based delivery systems (e.g., nanoparticles, liposomes), understanding the in vivo fate of the carrier itself is paramount. The carrier's journey—from administration to reaching target tissues, interacting with cells, and undergoing intracellular processing—directly impacts therapeutic success [106]. Key aspects include:
- Blood Circulation Time: Influenced by size, surface charge, and stealth coatings (e.g., PEGylation).
- Tissue Distribution and Targeting: Passive targeting via the Enhanced Permeability and Retention (EPR) effect or active targeting via surface ligands.
- Intracellular Fate: Mechanisms of cellular uptake, endosomal escape, and eventual degradation and excretion [106]. Failure to fully understand this fate can lead to clinical trial failures, as evidenced by the fact that 6 out of 13 FDA-approved nanocarriers have been discontinued, some for reasons related to safety or efficacy [106].
Table 2: Comparison of Major In Vivo Model Types
| Model Type | Key Characteristics | Primary Applications | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Murine (Rodent) Models | Short lifespan, well-characterized genetics [103] | Early efficacy, PK/PD, initial toxicity screening [103] | Low cost, high availability, genetic tools [103] | Significant physiological differences from humans [103] |
| Humanized Mouse Models | Engrafted with human cells/tissues (e.g., immune system) [103] | Immuno-oncology, infectious disease, human-specific drug target validation [103] [105] | Models human-specific responses; bridges in vitro and clinical trial [103] | Technically challenging, expensive, variable engraftment [103] |
| Patient-Derived Xenografts | Implanted with human patient tumor tissue [105] | Oncology drug testing, personalized medicine approaches [105] | Retains tumor heterogeneity and patient-specific drug responses [105] | Requires immunocompromised hosts, no human immune context [105] |
| Non-Human Primates | Close phylogenetic and biochemical similarity to humans [103] | Advanced PK/PD, toxicology, vaccine development, complex diseases [103] | High physiological and immunological similarity to humans [103] | Extremely high cost, serious ethical concerns, limited availability [103] |
Quantitative Data and Experimental Protocols
Experimental Protocol: Assessing Drug Efficacy and Toxicity in a 3D Liver Spheroid Model
This protocol is designed for evaluating the hepatotoxicity (DILI) of a drug candidate or the biocompatibility and protective effects of a biomaterial-based delivery system.
Objective: To generate 3D human liver spheroids and use them to assess compound-induced cytotoxicity and hepatotoxicity.
Materials:
- Cells: Primary human hepatocytes or hepatocyte-like cells derived from induced pluripotent stem cells (iPSCs); non-parenchymal cells (e.g., hepatic stellate cells, Kupffer cells) for co-culture.
- Matrix: Ultra-low attachment (ULA) 96-well round-bottom plates or Matrigel.
- Media: Hepatocyte culture medium (e.g., William's E Medium) supplemented with growth factors and hormones.
- Reagents: Test compound/drug-loaded biomaterial, AlamarBlue/CellTiter-Glo for viability, Albumin ELISA kit, CYP450 activity assay kit (e.g., P450-Glo), High-content imaging (HCI) system.
Methodology:
- Spheroid Formation:
- Create a single-cell suspension of hepatocytes (with or without NPCs) at a density of 1,000-5,000 cells per well in complete medium.
- Seed 100 µL of cell suspension into each well of a ULA 96-well plate.
- Centrifuge the plate at 300-500 x g for 5 minutes to aggregate cells at the well bottom.
- Incubate at 37°C, 5% CO2 for 3-5 days, allowing spheroid self-assembly. Monitor formation daily under a microscope.
Compound Treatment:
- After spheroids are fully formed (compact, spherical), carefully aspirate 50% of the medium and replace with fresh medium containing the test article.
- Test a range of concentrations of the free drug and the drug encapsulated in the biomaterial carrier. Include a vehicle control.
- Treat spheroids for a predetermined period (e.g., 48 hours to 14 days for repeated dosing), refreshing medium and compounds every 2-3 days.
Endpoint Analysis:
- Viability/Cytotoxicity: Add AlamarBlue reagent and measure fluorescence. Alternatively, use ATP-based assays (CellTiter-Glo 3D) to quantify metabolically active cells.
- Liver-Specific Function:
- Albumin Secretion: Collect conditioned media and quantify secreted human albumin using an ELISA kit. Normalize to total protein or cell number.
- Urea Production: Measure urea concentration in the conditioned media using a colorimetric assay.
- CYP450 Activity: Incubate spheroids with a luminogenic CYP substrate and measure luminescence.
- High-Content Imaging (HCI):
- Stain spheroids with fluorescent dyes for live/dead cells (e.g., Calcein-AM/Propidium Iodide), mitochondria, or nuclei.
- Image using a confocal microscope or HCI system with Z-stacking capability.
- Quantify spheroid size, morphology, and intensity of fluorescence markers to assess structural integrity and specific toxicity.
Data Interpretation: Compare the IC50 values for viability between 2D and 3D models; a significant difference often indicates the superior predictive power of the 3D system. A functional biomaterial carrier should show reduced cytotoxicity and better preservation of albumin secretion and CYP450 activity compared to the free drug, indicating protective targeting.
The Scientist's Toolkit: Essential Reagents for Advanced Model Development
Table 3: Key Research Reagent Solutions
| Reagent / Material | Function / Application | Specific Examples |
|---|---|---|
| Induced Pluripotent Stem Cells | Generate patient-specific, differentiated cells for organoids and disease modeling [103] [104] | Human iPSCs differentiated into hepatocyte-like cells, cardiomyocytes |
| Extracellular Matrix (ECM) Hydrogels | Provide a 3D scaffold that mimics the native tissue microenvironment for cell growth and signaling [104] | Matrigel, Collagen I, Fibrin, synthetic PEG-based hydrogels |
| Microfluidic Devices | Create dynamic culture environments with perfusion and mechanical forces for Organ-on-a-Chip models [103] [104] | Commercial chips (e.g., Emulate, Mimetas) or custom PDMS devices |
| Cytokines & Growth Factors | Direct stem cell differentiation and maintain tissue-specific function in 3D cultures [104] | FGF, EGF, HGF, BMP4, Wnt-3A, R-spondin, Noggin [104] |
| High-Throughput Screening Assays | Multiparameter toxicity and efficacy testing in miniaturized formats (384-/1536-well) [103] | Fluorometric/Luminescent viability assays (CellTiter-Glo), calcium flux assays |
| Biomaterial Carriers (for delivery) | Act as test articles to improve drug stability, targeting, and controlled release [106] [8] | Liposomes, PLGA nanoparticles, thermosensitive hydrogels (e.g., Chitosan-based) [8] |
Integration with Biomaterials in Drug Delivery Research
Advanced preclinical models are particularly crucial for testing the increasingly sophisticated class of functional biomaterials for drug delivery. These models provide the necessary biological complexity to evaluate if these systems perform as designed.
- Testing Intelligent Responsive Materials: Thermosensitive or pH-sensitive hydrogels are designed to release their payload in response to specific physiological triggers. For example, a chitosan-based thermosensitive hydrogel developed for periodontal regeneration can be tested in a 3D periodontal tissue model or a bone-on-a-chip platform to validate its fast-gelling property at body temperature and controlled release profile in a tissue-like environment [8].
- Evaluating Nanocarrier Targeting and Fate: The intracellular and subcellular fate of nanocarriers (liposomes, polymer nanoparticles) is a critical determinant of efficacy. Using advanced in vitro models (e.g., co-culture spheroids that mimic tumor heterogeneity) allows researchers to track whether surface-functionalized nanoparticles actively target cancer cells and successfully release their payload intracellularly, providing data beyond what simple 2D cultures can offer [106] [8].
- Validating Complex Delivery Systems: Systems like magnetically propelled hydrogel microrobots for osteosarcoma treatment require models that can mimic the physical barriers and tissue structures they will navigate. A 3D tumor spheroid or an organ-on-a-chip model with a vascular component can provide a more realistic environment to test the microrobot's penetration and drug delivery efficiency under an external magnetic field [8].
Visualizing Workflows and Relationships
The following diagrams illustrate the experimental workflow for evaluating a biomaterial-based drug delivery system and the logical relationship between model complexity and physiological relevance.
Diagram 1: Integrated Preclinical Evaluation Workflow. This flowchart outlines a sequential strategy for testing drug-biomaterial systems, from initial in vitro screens to advanced in vivo models, culminating in a data-driven decision point.
Diagram 2: Model Complexity and Relevance Spectrum. This diagram shows the continuum of preclinical models, from simple systems with low physiological relevance to complex systems with high human predictive power.
The field of preclinical modeling is undergoing a rapid transformation, moving away from traditional, poorly predictive systems toward more human-relevant, complex models. The integration of CIVMs like organoids and OOCs into the drug development pipeline, accelerated by regulatory changes, holds immense promise for improving the prediction of human efficacy and safety, particularly for biomaterial-based drug delivery systems [103] [104].
Future advancements will be driven by several key trends:
- AI and Machine Learning: The integration of AI/ML will play a pivotal role in optimizing complex culture parameters for CIVMs, analyzing the vast multiparameter data they generate, and even assisting in the design of next-generation biomaterials [103] [8].
- Multi-Organ Systems (Human-on-a-Chip): Linking individual organ chips to create interconnected systems will enable the study of complex ADME processes and systemic effects of drugs delivered via biomaterial carriers [103].
- Standardization and Validation: Widespread adoption of CIVMs depends on the standardization of protocols and rigorous validation against clinical outcomes to build confidence in their predictive value.
- Focus on the Biomaterial-Biology Interface: As biomaterials become more sophisticated, understanding their intricate interactions with biological systems—from protein corona formation to immune responses—in the context of these advanced models will be critical for successful clinical translation [106] [8].
By strategically employing a fit-for-purpose combination of these evolving in vitro and in vivo models, researchers can de-risk the development of controlled drug delivery systems, leading to more effective, safer, and more rapidly approved therapies.
The evolution of biomaterials from passive structural scaffolds to dynamic, "smart" platforms represents a paradigm shift in controlled drug delivery systems research [107]. These advanced materials are engineered to actively interface with biological systems, precisely controlling the spatiotemporal release of therapeutic agents. However, a critical challenge persists: balancing their enhanced therapeutic efficacy against potential toxicity. As biomaterials grow more complex—integrating responsiveness to stimuli like pH, enzymes, or temperature—their interactions with the immune system and biological environments become more intricate, necessitating a rigorous, comparative assessment of their safety and performance [107] [108]. This analysis is foundational to any thesis on the role of biomaterials in modern drug delivery, as it directly impacts clinical translation and therapeutic success. This review provides a structured comparison of major biomaterial platforms, detailing their efficacy-toxicity profiles, supported by standardized experimental methodologies essential for research and development.
Biomaterial Platform Classification and Key Characteristics
Biomaterials are classified by their level of biological interaction, evolving from passive bystanders to active participants in therapeutic regulation [107].
- Inert Materials: Primarily provide structural support and aim for minimal biological interaction (e.g., titanium alloys, certain ceramics). A major limitation is their potential to trigger a foreign body response (FBR), leading to fibrous capsule formation and implant failure [107].
- Active Materials (Bioactive Materials): Elicit a specific biological response, either through the release of pre-loaded bioactive agents (e.g., drug-eluting stents) or via inherent surface properties that promote tissue integration (e.g., hydroxyapatite coatings) [107].
- Responsive (Smart) Materials: Represent the forefront of biomaterial research. These systems dynamically alter their properties or release payloads in response to specific endogenous (pH, enzymes, redox state) or exogenous (light, magnetic fields) stimuli [107]. This enables precise, targeted drug delivery, transforming the biomaterial into an in situ therapeutic system [107].
The following diagram illustrates the evolutionary trajectory of biomaterials and their core interactive logic with the biological environment.
Quantitative Efficacy and Toxicity Profile Comparison
A critical evaluation of biomaterials for drug delivery requires a side-by-side comparison of their therapeutic potential against their toxicological risks. The table below summarizes the key efficacy and toxicity parameters for major biomaterial classes.
Table 1: Comparative Efficacy and Toxicity Profiles of Major Biomaterial Platforms
| Material Class | Key Subtypes & Examples | Primary Efficacy Strengths | Documented Toxicity & Biocompatibility Concerns | Dominant Applications in Drug Delivery |
|---|---|---|---|---|
| Metallic(Market Share: 37.7-40.1% [109] [110]) | Titanium/alloys, Stainless steel, Cobalt-Chromium alloys [109] [110] | Superior mechanical strength, fatigue resistance, corrosion resistance. Excellent for load-bearing implants [110]. | Ion release (e.g., Ni, Cr, Co) potential for cytotoxicity, inflammation, and allergic reactions. Risk of fibrous encapsulation due to bio-inertness [107]. | Orthopedic implants (highest application share), dental devices, cardiovascular stents [109] [110]. |
| Polymeric(Projected CAGR: 14.9% [109]) | Natural (Chitosan, Hyaluronic Acid); Synthetic (PLGA, PVA, PNIPAM) [107] [8] [111] | High versatility, tunable biodegradability, biocompatibility. Can be engineered for controlled/sustained release and stimuli-responsiveness [107] [8]. | Inconsistent degradation rates; acidic byproducts (e.g., from PLGA) can cause local pH drop and inflammation. Residual crosslinkers or monomers can be cytotoxic [111]. | Targeted drug delivery, injectable depots (thermosensitive gels), wound dressings, nanocarriers [8] [7]. |
| Ceramic | Bioglass, Hydroxyapatite, Calcium Phosphates [111] | High biocompatibility, osteoconductivity (bone-bonding ability), bioresorbability [111]. | Brittleness, poor tensile strength. Potential for particle shedding and foreign body response if resorption/proliferation rates are mismatched [111]. | Bone tissue engineering, dental repair, coatings for metallic implants to enhance integration [111]. |
| Nanoscale(Lipid, Polymeric, Inorganic) | Lipid NPs, PEI, Graphene Oxide, Mesoporous Silica [107] [8] [112] | Enhanced drug stability & bioavailability; superior tissue penetration & cellular uptake; ability for surface functionalization & active targeting [8] [112]. | Unknown long-term biodistribution & accumulation; nanoparticle-induced oxidative stress & inflammation; potential for immune activation. Specific concerns with material type (e.g., cationic polymer PEI's membrane toxicity) [8] [112]. | CNS drug delivery (crossing BBB), cancer theranostics, vaccine delivery, intracellular targeting [108] [112]. |
Standardized Experimental Protocols for Efficacy and Toxicity Assessment
Robust, standardized experimental protocols are non-negotiable for the reliable comparison of biomaterial platforms. The following section details key methodologies cited in current literature.
In Vitro Toxicity and Biocompatibility Assays
A. Lactate Dehydrogenase (LDH) Release Assay for Cytotoxicity
- Principle: Measures the integrity of the cellular membrane, a marker of cell death. Damage to the plasma membrane releases the cytosolic enzyme LDH into the cell culture supernatant [111].
- Detailed Protocol:
- Cell Seeding: Seed healthy human osteoblasts (hFOB 1.19) or other relevant cell lines at a density of 5 × 10⁴ cells/cm² in a 24-well plate and culture for 24 hours [111].
- Extract Preparation & Exposure: Immerse the biomaterial (e.g., a chitosan-bioglass composite disc) in cell culture medium (1.5 mL/well) for 24 hours at 34°C/5% CO₂ to create an extract. Replace the medium on the pre-seeded cells with 1 mL of this biomaterial extract. Incubate for 48 hours [111].
- Sample Collection & Reaction: Collect the supernatant from each well. Transfer to a 96-well plate and mix with the LDH assay reagent (containing dye and catalyst). Incubate in the dark for 30 minutes [111].
- Data Acquisition & Analysis: Measure optical density (OD) at 490 nm (signal) and 690 nm (reference). Calculate cytotoxicity percentage using the formula:
Cytotoxicity [%] = (OD_sample − OD_control) / (OD_positive_control − OD_control) × 100%where the positive control is cells treated with Triton X-100 [111].
B. WST-1 Mitochondrial Activity/Proliferation Assay
- Principle: Measures metabolic activity as a surrogate for cell viability and proliferation. The tetrazolium salt WST-1 is cleaved to formazan by mitochondrial dehydrogenases in viable cells [111].
- Detailed Protocol:
- Cell Treatment: Follow the same cell seeding and extract exposure protocol as for the LDH assay [111].
- Reagent Addition & Incubation: After the 48-hour exposure, add 40 µL of WST-1 reagent directly to each well. Incubate the plate for 2 hours at 34°C/5% CO₂ [111].
- Data Acquisition & Analysis: Transfer the media to a 96-well plate. Measure OD at 450 nm (signal) and 620 nm (reference). Calculate proliferation percentage relative to untreated control cells:
Proliferation [%] = (OD_sample / OD_control) × 100%[111].
The workflow for conducting a standardized in vitro biocompatibility assessment, from material preparation to data interpretation, is outlined below.
In Vivo Efficacy and Safety Modeling
A. Diabetic Wound Healing Model for Hydrogel Efficacy
- Principle: Evaluates the therapeutic potential of biomaterial-based dressings (e.g., enzyme-responsive hyaluronic acid microneedles) in a pathologically compromised healing environment [107].
- Detailed Protocol:
- Animal Model Induction: Induce diabetes in mice (e.g., using streptozotocin) [107].
- Wound Creation & Intervention: Create full-thickness skin wounds on the diabetic mice. Apply the test biomaterial (e.g., ZCO-HA microneedles) to the wound site. Include untreated and standard-care control groups [107].
- Efficacy Endpoints: Monitor wound closure rate over time. Perform histological analysis of healed tissue to assess collagen formation, epithelial regeneration, and macrophage polarization [107].
- Systemic Toxicity Screening: Monitor animal body weight and behavior. Collect blood samples for biochemical analysis and major organs (liver, kidney) for histopathological examination to rule out systemic toxicity [107].
B. Assessment of Immunomodulatory Efficacy
- Principle: Quantifies a smart biomaterial's ability to actively shape the immune microenvironment, particularly by driving macrophage polarization from a pro-inflammatory (M1) to a pro-regenerative (M2) phenotype [107].
- Detailed Protocol:
- Implantation: Implant the biomaterial subcutaneously or in a specific tissue defect in a rodent model [107].
- Tissue Harvest & Analysis: Harvest the peri-implant tissue at multiple time points. Analyze tissue lysates using ELISA or multiplex immunoassays to quantify the ratio of M2-associated cytokines (e.g., IL-10, TGF-β) to M1-associated cytokines (e.g., TNF-α, IL-6, IL-1β) [107] [8]. Flow cytometry and immunohistochemistry can be used to further characterize immune cell populations.
The Scientist's Toolkit: Essential Research Reagents and Materials
Success in biomaterials research hinges on the selection of appropriate reagents and materials. The following table catalogs key solutions used in the experiments cited herein.
Table 2: Essential Research Reagents and Materials for Biomaterial Drug Delivery Studies
| Reagent/Material | Function & Role in Research | Specific Example(s) & Rationale |
|---|---|---|
| hFOB 1.19 Cell Line (Human Fetal Osteoblast) | A non-cancerous, biologically relevant in vitro model for assessing biocompatibility, particularly for orthopedic and bone-contact applications [111]. | Preferred over cancer cell lines or animal cells due to closer biological similarity to healthy human osteoblasts, providing more translational toxicity data [111]. |
| Cytotoxicity Detection KitPLUS (LDH) | A standardized, colorimetric kit for quantifying cell death based on the release of lactate dehydrogenase from damaged cells [111]. | Provides a reliable and reproducible metric for membrane integrity, a direct indicator of acute cytotoxicity [111]. |
| WST-1 Cell Proliferation Reagent | A colorimetric assay kit used to measure cell metabolic activity and proliferation, serving as a positive indicator of biocompatibility [111]. | The tetrazolium salt is more stable and less toxic than MTT, allowing for longer incubation and continuous monitoring [111]. |
| Chitosan (Heppe Medical) | A natural polysaccharide serving as a base polymer for constructing biocompatible and biodegradable composite scaffolds [111]. | Known for high biocompatibility and antimicrobial properties; serves as a benchmark material for developing new composites [111]. |
| Sol-Gel Derived Bioglass (SiO₂-P₂O₅-CaO) | A bioactive ceramic filler used to enhance the osteoconductive properties and mechanical integrity of composite biomaterials [111]. | Promotes direct bonding to bone tissue and can release bioactive ions (e.g., Ca²⁺, Sr²⁺) that stimulate osteogenesis [111]. |
| Functional Peptides (Pro-regenerative, Antibacterial) | Bioactive molecules incorporated into biomaterials to provide specific, advanced functions such as stimulating cell growth or preventing infection [111]. | Covalently bound or adsorbed onto composite surfaces to actively guide tissue regeneration and improve implant success [111]. |
The comparative analysis of biomaterial platforms reveals a fundamental trade-off: enhancing functional efficacy often introduces new biocompatibility complexities. While smart, responsive materials offer unprecedented control over drug delivery, their sophisticated chemistries and dynamic interactions with the biological milieu demand more rigorous, multi-parametric toxicity screening. The future of biomaterials in drug delivery lies in the rational design of platforms that not only demonstrate high therapeutic efficacy but also possess a well-characterized and minimal toxicity profile. This will be accelerated by the integration of advanced tools like AI-driven material design and predictive modeling, ultimately enabling the safe and effective clinical translation envisioned in contemporary drug delivery research.
The integration of advanced biomaterials into drug delivery systems represents a paradigm shift in modern therapeutics, enabling unprecedented control over drug release kinetics, tissue-specific targeting, and therapeutic efficacy. This whitepaper examines the current clinical translation landscape for biomaterial-based drug delivery systems, focusing specifically on recently approved products and late-stage clinical trials. Biomaterials—engineered to interact with biological systems for therapeutic purposes—have evolved from inert carriers to active participants in disease treatment, capable of responding to specific physiological stimuli and remodeling pathological microenvironments [1]. The convergence of materials science with pharmaceutical research is producing increasingly sophisticated platforms that address fundamental challenges in drug delivery, including poor bioavailability, systemic toxicity, and patient non-compliance.
The transition from laboratory innovation to clinically viable products requires navigating complex translational pathways. Despite tremendous potential demonstrated in preclinical studies, many biomaterial-based delivery systems fail to reach clinical application due to formulation challenges, manufacturing complexities, and biological barriers [113]. This analysis provides drug development professionals with a comprehensive overview of the current state of clinical translation, highlighting successful approval pathways, ongoing late-stage trials, and the experimental methodologies driving advancement in this rapidly evolving field.
Approved Biomaterial-Based Drug Products (2025)
The year 2025 has witnessed significant regulatory milestones for novel drug products incorporating advanced biomaterial formulations. These approvals demonstrate the expanding clinical utility of biomaterials across diverse therapeutic areas, from oncology to rare diseases. The U.S. Food and Drug Administration (FDA) has approved numerous novel drugs that utilize sophisticated delivery platforms to enhance therapeutic outcomes [114].
Table 1: Selected FDA-Approved Novel Drug Products in 2025 Featuring Advanced Delivery Systems
| Drug Name | Active Ingredient | Approval Date | FDA-Approved Use | Delivery Technology |
|---|---|---|---|---|
| Hyrnuo | Sevabertinib | 11/19/2025 | Locally advanced or metastatic non-squamous NSCLC with HER2 mutations | Targeted molecular therapy |
| Redemplo | Plozasiran | 11/18/2025 | Reduce triglycerides in adults with familial chylomicronemia syndrome | RNA-targeted delivery system |
| Komzifti | Ziftomenib | 11/13/2025 | Relapsed/refractory AML with NPM1 mutation | Small molecule inhibitor |
| Lynkuet | Elinzanetant | 10/24/2025 | Moderate-to-severe vasomotor symptoms due to menopause | Oral controlled-release |
| Jascayd | Nerandomilast | 10/07/2025 | Idiopathic pulmonary fibrosis | Polymer-based formulation |
| Rhapsido | Remibrutinib | 09/30/2025 | Chronic spontaneous urticaria after antihistamine failure | BTK inhibitor delivery |
| Modeyso | Dordaviprone | 08/06/2025 | Diffuse midline glioma with H3 K27M mutation | Brain-penetrant delivery |
| Vizz | Aceclidine | 07/31/2025 | Treatment of presbyopia | Ophthalmic delivery system |
| Zegfrovy | Sunvozertinib | 07/02/2025 | NSCLC with EGFR exon 20 insertion mutations | Targeted kinase inhibitor |
| Datroway | Datopotamab deruxtecan-dlnk | 01/17/2025 | HR-positive, HER2-negative breast cancer | Antibody-drug conjugate |
These approvals highlight several key trends in biomaterial-based drug development. First, there is a pronounced emphasis on targeted therapies, particularly in oncology, where antibody-drug conjugates (ADCs) like Datroway represent sophisticated biomaterial platforms that combine targeting moieties with controlled payload release [114]. Second, the approval of drugs for rare diseases and specific genetic mutations demonstrates how biomaterials enable precise therapeutic interventions for specialized patient populations. Finally, the diversity of administration routes—from oral to injectable formulations—showcases the adaptability of biomaterial platforms across physiological systems.
The controlled release drug delivery market reflects this therapeutic expansion, with projections estimating growth from USD 58.18 billion in 2025 to USD 119.34 billion by 2032, representing a compound annual growth rate (CAGR) of 10.8% [115]. This growth is driven particularly by applications in oncology, which holds a 24.7% market share, as controlled release technologies effectively address the need to reduce systemic toxicity of chemotherapy through localized, sustained drug delivery [115].
Late-Stage Clinical Trials (2025)
The late-stage clinical trial landscape for biomaterial-based delivery systems reveals several promising platforms approaching regulatory review. These trials emphasize innovative mechanisms for controlling drug release profiles, enhancing targeting specificity, and responding to physiological stimuli. Notable late-stage studies include investigations of novel biomaterial platforms across therapeutic areas including metabolic disorders, immunology, and oncology.
Table 2: Selected Late-Stage Clinical Trials of Biomaterial-Based Delivery Systems
| Trial/Compound | Sponsor | Phase | Indication | Biomaterial Platform | Primary Endpoint |
|---|---|---|---|---|---|
| Orforglipron (Attain-1) | Eli Lilly | Phase 3 | Obesity | Oral incretin formulation | Weight reduction from baseline |
| Amlitelimab (Coast-1, Shore) | Sanofi | Phase 3 | Eczema, Asthma | OX40L-blocking antibody | Disease severity score improvement |
| Sonelokimab (Vela-1, Vela-2) | Moonlake Immunotherapeutics | Phase 3 | Hidradenitis Suppurativa | Nanobody-albumin binding | HiSCR75 response rate |
| Ivonescimab (Harmoni-2) | Akeso, Summit Therapeutics | Phase 3 | NSCLC | PD-1/VEGF bispecific antibody | Overall survival |
| Fenebrutinib (FENhance 1/2, FENtrepid) | Roche | Phase 3 | Multiple Sclerosis | Brain-penetrant BTK inhibitor | Annualized relapse rate |
The Orforglipron (Attain-1) trial represents a significant advancement in oral delivery of incretin therapies for obesity. This chemical-based oral formulation offers potential manufacturing advantages over biologic alternatives, potentially enabling broader patient access. Phase 3 results expected in late 2025 will scrutinize both efficacy and gastrointestinal side effect profiles, which have challenged earlier glucagon-like peptide-1 (GLP-1) receptor agonists [116].
In immunology, Amlitelimab represents a next-generation biomaterial approach that targets OX40L to modulate T-cell-driven inflammation across multiple conditions. The drug's potential positioning as a longer-lasting alternative to existing therapies like Dupixent depends on Phase 3 data expected in late 2025. Similarly, Sonelokimab's unique nanobody structure with albumin binding aims to provide enhanced tissue penetration and less frequent dosing in hidradenitis suppurativa, with Phase 3 results anticipated in September 2025 [116].
The Ivonescimab trial (Harmoni-2) exemplifies innovative biomaterial engineering for oncology applications, combining PD-1 and VEGF inhibition in a single bispecific antibody structure. Final overall survival analysis expected by end of 2025 will determine whether this dual-targeting approach provides meaningful clinical advantages over established immunotherapies [116].
Advanced Biomaterial Platforms in Development
Enzyme-Responsive Biomaterials
Recent advances in biomaterial engineering have produced enzyme-responsive systems that undergo precise structural and functional changes when exposed to specific enzymatic activity in disease microenvironments. These intelligent materials leverage pathological overexpression of particular enzymes to trigger drug release at targeted sites, minimizing off-target effects and enhancing therapeutic precision [20].
Experimental studies have demonstrated enzyme-responsive biomaterials programmed to react to matrix metalloproteinases (MMPs) commonly overexpressed in tumor environments, inflammatory conditions, and fibrotic diseases. Upon enzymatic activation, these systems undergo controlled degradation or conformational changes that release therapeutic payloads directly at disease sites. This approach represents a significant advancement over passive targeting mechanisms, as it leverages biological cues inherent to the pathology itself [20].
Key Experimental Protocol: Enzyme-Responsive Nanoparticle Synthesis
- Polymer Functionalization: Synthesize or source biocompatible polymer backbone (e.g., PLGA, PEG) with side chains containing enzyme-cleavable peptide sequences (e.g., GPLGIAGQ for MMP-2 cleavage).
- Drug Encapsulation: Incorporate therapeutic agent using double emulsion solvent evaporation method with 1:10 drug-to-polymer ratio.
- Cross-linking: Apply UV-induced cross-linking or chemical cross-linkers (e.g., glutaraldehyde at 0.1% v/v) to stabilize nanoparticle structure.
- Characterization: Determine particle size distribution (target 100-200nm) using dynamic light scattering, enzyme-responsive degradation via incubation with target enzyme, and drug release kinetics using Franz diffusion cells.
- In Vitro Validation: Assess cellular uptake and cytotoxicity in enzyme-positive vs. enzyme-negative cell lines to confirm targeted activation.
Extracellular Matrix (ECM)-Based Biomaterials
Decellularized extracellular matrix (ECM) scaffolds represent a distinct class of biomaterials that provide native biological signaling environments for controlled drug delivery and tissue regeneration. These materials maintain complex arrays of structural proteins and bioactive molecules that guide cellular integration and provide sustained release of therapeutic agents [117].
ECM biomaterials have demonstrated clinical success across multiple applications, including wound care, breast reconstruction, and guided tissue regeneration. Their mechanism of action involves gradual in vivo degradation that releases embedded signaling molecules which modulate the local cellular environment. This creates a feedback loop where the material's breakdown products further influence tissue repair processes [117].
Key Experimental Protocol: ECM Hydrogel Preparation for Drug Delivery
- Tissue Decellularization: Subject donor tissue (porcine small intestinal submucosa or urinary bladder matrix) to serial detergent treatments (0.1% SDS followed by 1% Triton X-100) with nuclease incubation to remove cellular material while preserving ECM composition.
- Communtation and Solubilization: Lyophilize and mill decellularized ECM to powder, then digest with 1 mg/mL pepsin in 0.1 M HCl for 48-72 hours at room temperature.
- Therapeutic Agent Incorporation: Mix drug solution with ECM digest at 4°C using gentle vortexing to achieve homogeneous distribution.
- Gelation Induction: Neutralize to physiological pH (7.4) using 0.1 M NaOH and raise ionic strength with 10× PBS to initiate self-assembly into hydrogel.
- Release Kinetics Assessment: Conduct elution studies in PBS at 37°C with periodic sampling for drug quantification via HPLC, correlating release profile with hydrogel mass loss.
Nanomaterial-Based Delivery Systems
Nanoparticle platforms continue to advance toward clinical translation, with particular progress in oncology applications where they can preferentially accumulate in tumor tissue through enhanced permeability and retention (EPR) effects. Recent innovations focus on overcoming biological barriers and enabling triggered release in response to specific disease microenvironment cues [113].
Advanced nanomaterial systems include Mn-based nanozymes that function as "metabolic surgeons" in acidic tumor microenvironments. These materials exhibit dual peroxidase/catalase activities that decompose H2O2 into hydroxyl radicals (∙OH) and oxygen (O2), simultaneously inducing ROS-mediated ablation while alleviating tumor hypoxia. The liberated Mn2+ ions further function to block PD-L1, synergizing with photothermal immunogenic cell death for comprehensive tumor suppression [118].
Experimental Methodologies and Technical Protocols
Formulation Strategies for Clinical Translation
Translating nanoparticle-based delivery systems from laboratory proof-of-concept to clinically viable products requires sophisticated formulation strategies that address stability, administration route, and manufacturing scalability. Advanced secondary delivery platforms play a crucial role in bridging this translational gap by transforming functional nanoparticles into finished drug products [113].
Table 3: Advanced Formulation Platforms for Biomaterial-Based Drug Delivery
| Formulation Platform | Administration Route | Clinical Challenge Addressed | Key Biomaterial Components |
|---|---|---|---|
| Sterile Injectables | Intravenous | Stability in circulation, controlled release | PLGA, PEG, liposomes, dendrimers |
| Hydrogels | Topical/Implantable | Sustained local delivery, tissue integration | Hyaluronic acid, chitosan, alginate, ECM hydrogels |
| Microspheres | Oral | Gastrointestinal protection, controlled release | Enteric polymers (Eudragit), pH-sensitive materials |
| Dry Powder Formulations | Pulmonary | Aerodynamic properties, deep lung deposition | Spray-dried biologics, lipid nanoparticles |
| Polymer Implants | Subcutaneous/Intracavitary | Long-term controlled release (months/years) | PCL, PLA, PGA, EVAc polymers |
Injectable depot systems represent one of the most clinically advanced biomaterial platforms, with the injectables segment holding a dominant 30.62% share of the controlled release drug delivery market [115]. These systems typically utilize biodegradable polymers like poly(lactic-co-glycolic acid) (PLGA) that undergo hydrolysis to release encapsulated therapeutics over extended periods ranging from weeks to months. The Wurster technique, a specialized air suspension coating process, holds a 25.6% market share in controlled release technologies due to its versatility in applying uniform functional coatings to tablets, pellets, and multiparticulate systems [115].
Key Experimental Protocol: Wurster Technique Coating for Controlled Release
- Equipment Setup: Configure Wurster coater with bottom-spray arrangement, ensuring appropriate partition height and nozzle positioning for optimal particle movement.
- Coating Solution Preparation: Dissolve controlled release polymer (e.g., ethyl cellulose, Eudragit) at 5-15% w/v in appropriate solvent with plasticizer (e.g., 20% triethyl citrate relative to polymer weight).
- Process Parameters: Establish key operating conditions - inlet temperature (30-45°C), atomization air pressure (1-2 bar), fluidization air volume (50-100 m³/h), and spray rate (5-15 mL/min) - optimized for specific substrate.
- Coating Application: Load drug cores (500μm-1mm) into chamber and apply coating solution until target weight gain (2-10%) is achieved for desired release profile.
- Curing: Post-treatment thermal curing (40°C for 2-24 hours) to ensure polymer film formation and stability.
- Quality Control: Assess coated particles for drug content uniformity, in vitro release performance using USP apparatus, and accelerated stability (40°C/75% RH for 3 months).
Characterization Methods for Biomaterial-Drug Systems
Comprehensive characterization of biomaterial-based delivery systems requires orthogonal analytical techniques that evaluate critical quality attributes from nanoscale to macroscopic levels. These methodologies ensure consistent performance and predict in vivo behavior.
Key Material Characterization Techniques:
- Surface Area and Porosity Analysis: Conduct N2 adsorption-desorption isotherms (BET method) to quantify surface area and pore size distribution, critical parameters influencing drug loading capacity and release kinetics.
- Thermal Analysis: Perform differential scanning calorimetry (DSC) and thermogravimetric analysis (TGA) to determine polymer crystallinity, drug-polymer interactions, and thermal stability.
- In Vitro Release Testing: Utilize USP apparatus I (baskets) or II (paddles) with sink conditions maintained, sampling at predetermined intervals for HPLC quantification of released drug.
- Degradation Profiling: Incubate materials in relevant physiological buffers (e.g., PBS, simulated gastric/intestinal fluids) with periodic assessment of mass loss, molecular weight reduction (GPC), and morphological changes (SEM).
- Mechanical Properties: Textural analysis for hydrogels (compression testing) and films (tensile testing) to ensure appropriate physical integrity for intended application.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development of biomaterial-based drug delivery systems requires specialized reagents and materials that enable precise control over material properties and drug release characteristics.
Table 4: Essential Research Reagents for Biomaterial Drug Delivery Development
| Category/Reagent | Function | Key Applications |
|---|---|---|
| Biodegradable Polymers | ||
| PLGA (Poly(lactic-co-glycolic acid)) | Controlled release matrix, tunable degradation | Injectable microparticles, implants |
| PLA (Polylactic acid) | Slower degrading structural polymer | Long-term implants, tissue scaffolds |
| PEG (Polyethylene glycol) | Stealth coating, hydrophilicity enhancement | Nanoparticle surface functionalization |
| Natural Polymers | ||
| Chitosan | Mucoadhesion, permeation enhancement | Nasal, oral, and wound delivery |
| Alginate | Ionic cross-linking, pH responsiveness | Hydrogels, microbeads |
| Hyaluronic acid | CD44 receptor targeting, viscoelasticity | Ophthalmic, intra-articular delivery |
| Functional Additives | ||
| Triethyl citrate | Plasticizer for polymer films | Coating formulations, flexible hydrogels |
| Poloxamers | Thermo-responsive gelling, stabilization | In situ gelling systems, emulsion stabilization |
| Trehalose | Cryo-/lyo-protectant | Biologic stabilization in nanoparticles |
| Characterization Tools | ||
| Fluorescent dyes (Cy5, FITC) | Tracking material fate, cellular uptake | In vitro and in vivo imaging |
| Enzyme substrates | Responsive system validation | Enzyme-responsive material testing |
| Cell viability assays (MTT, Live/Dead) | Biocompatibility assessment | Cytotoxicity screening |
Signaling Pathways in Biomaterial-Mediated Therapeutic Effects
Biomaterial-based delivery systems interact with biological systems through specific molecular pathways that determine their therapeutic effects and biocompatibility. Understanding these pathways is essential for rational design of advanced delivery platforms.
The clinical translation landscape for biomaterial-based drug delivery systems reflects a maturation of the field from simple controlled release platforms to sophisticated, biologically interactive systems. The approved products and late-stage trials of 2025 demonstrate increasing precision in targeting, greater responsiveness to pathological cues, and expanded application across therapeutic areas. As research continues to address remaining challenges in manufacturing scalability, long-term stability, and predictive in vitro-in vivo correlations, biomaterial platforms are poised to enable increasingly personalized therapeutic interventions that dynamically adapt to patient-specific disease states and treatment needs.
Navigating Regulatory Pathways and Standardization for Market Approval
The development of controlled drug delivery systems (DDS) based on functional biomaterials represents a frontier in pharmaceutical technology, enabling breakthrough treatments for complex diseases from chronic wounds to central nervous system disorders [7] [112]. These advanced therapeutic products, which combine biomaterial scaffolds, carriers, or matrices with active pharmaceutical ingredients, occupy a unique regulatory category that intersects medical devices, biologics, and drugs. The global regenerative medicine market has surpassed USD 15 billion, reflecting massive R&D investment, yet translational challenges persist with fewer than 10% of preclinical biomaterial-based delivery systems progressing to Phase III trials [31]. This high attrition rate underscores the critical importance of robust regulatory strategy throughout the development lifecycle. The fundamental regulatory challenge for biomaterial-based DDS lies in their inherent complexity – these products often combine structural, material, and biological functions that do not fit neatly into traditional regulatory categories. As the field advances toward increasingly sophisticated systems including 3D-bioprinted scaffolds, stimuli-responsive hydrogels, and multifunctional nanocarriers, regulatory frameworks must evolve to address their unique characterization requirements, manufacturing controls, and performance metrics [8] [119]. This technical guide provides a comprehensive framework for navigating these regulatory pathways, with specific emphasis on standardization approaches that can de-risk development and accelerate market approval for biomaterial-based controlled drug delivery systems.
Regulatory Framework Foundations
Investigational New Drug (IND) Application Requirements
The Investigational New Drug (IND) application serves as the primary regulatory gateway to human clinical testing in the United States and represents a critical milestone in the translation of biomaterial-based DDS from laboratory to clinic. Current Federal law requires that a drug be the subject of an approved marketing application before interstate distribution, and the IND provides the exemption that allows shipment of investigational drugs to clinical investigators across state lines [120]. For biomaterial-drug combination products, sponsors must provide comprehensive information across three core domains in their IND submission:
Animal Pharmacology and Toxicology Studies: Preclinical data must demonstrate that the biomaterial-based DDS is reasonably safe for initial human testing. This includes evaluation of drug release kinetics, biomaterial degradation profiles, and local tissue responses at implantation or administration sites. The complexity of biomaterial systems often necessitates extended-duration toxicology studies to fully characterize the safety profile of both the polymer matrix and its degradation products alongside the active pharmaceutical ingredient [120].
Manufacturing Information: Detailed information must be provided regarding the composition, manufacturer, stability, and controls used for manufacturing both the biomaterial and the final drug product. For complex biomaterial systems such as thermosensitive hydrogels, electrospun nanofibers, or 3D-printed scaffolds, this requires particularly rigorous characterization of critical quality attributes (CQAs) that impact drug release performance and biocompatibility. The FDA's Pre-IND Consultation Program offers valuable opportunity for early communication with review divisions to establish appropriate CQAs and control strategies [120].
Clinical Protocols and Investigator Information: Detailed protocols for proposed clinical studies must demonstrate that initial-phase trials will not expose subjects to unnecessary risks. For biomaterial-based DDS targeting specialized applications such as CNS drug delivery or personalized tissue regeneration, investigator qualifications and experience with both the technology platform and patient population are particularly scrutinized [112] [120].
Table 1: IND Application Types for Biomaterial-Based DDS
| IND Type | Applicable Context | Key Considerations for Biomaterial DDS |
|---|---|---|
| Investigator IND | Physician-initiated research on unapproved biomaterial DDS or new indications | Qualification of investigator in both drug delivery and biomaterial implantation techniques |
| Emergency Use IND | Emergency situations without time for standard IND submission | Limited to serious or immediately life-threatening conditions where biomaterial DDS may offer unique benefits |
| Treatment IND | Experimental biomaterial DDS showing promise for serious conditions | Available during final clinical work and FDA review; requires substantial evidence of efficacy and safety |
The IND submission triggers a 30-day review period during which the FDA assesses whether research subjects would be exposed to unreasonable risk. For novel biomaterial systems with limited human precedent, this review may raise additional questions regarding long-term material stability, drug-material interactions, and unique implantation or administration procedures that require specialized training [120].
International Regulatory Harmonization
The global research landscape for biomaterial-driven regenerative drug delivery reveals significant concentration of innovation in the United States (259 publications), China (175 publications), and India (76 publications), creating both challenges and opportunities for international regulatory harmonization [31]. This geographic distribution of research output necessitates careful planning for global development programs, with particular attention to region-specific requirements for clinical evidence generation, manufacturing quality systems, and product classification. Bibliometric analysis of the field reveals extensive globalization patterns with three principal knowledge exchange hubs: North America, Europe, and East Asia, suggesting emerging opportunities for regulatory convergence in these regions [31] [25].
Leading academic institutions including Harvard University, the University of California System, and the Chinese Academy of Sciences have emerged as key innovation centers driving biomaterial advances, often through collaborative international research networks [31]. These partnerships increasingly influence regulatory science through consensus standards development and pre-competitive sharing of characterization methodologies for complex biomaterial systems. The growing emphasis on open science principles, as reflected in the updated SPIRIT 2025 guidelines, further supports this trend toward transparent protocol content that facilitates cross-regional regulatory evaluation [121].
Biomaterial-Specific Characterization Requirements
Material Properties and Drug Release Profiling
Comprehensive characterization of biomaterial properties and their relationship to drug release kinetics represents a fundamental requirement for regulatory submission of controlled release systems. The structural and functional properties of marine-derived biomaterials including chitosan, alginate, and marine collagen make them particularly promising for drug delivery, but also introduce characterization challenges related to their natural variability, complex degradation behavior, and potential batch-to-batch inconsistencies [119]. Standardized testing methodologies must be implemented to establish robust specifications for these materials, with particular emphasis on:
- Structural characterization including molecular weight distribution, degree of deacetylation (for chitosan), and monomer sequence analysis
- Functional performance through in vitro drug release profiling under physiologically relevant conditions
- Accelerated stability studies to establish shelf-life and storage conditions for both the biomaterial and finished drug product
For intelligent responsive biomaterials such as temperature-sensitive hydrogels or pH-responsive nanoparticles, additional characterization of the trigger mechanism and response kinetics is essential. As highlighted in recent research, "Smart responsive materials for drug delivery systems include thermosensitive hydrogel systems using chitosan, erythropoietin (EPO), and FK506, developed as fast-gelling hydrogels at body temperature—a property particularly useful in irregularly shaped tissue defects" [8]. These dynamic systems require specialized testing to demonstrate reproducible performance across anticipated physiological variations in the target patient population.
Table 2: Essential Material Characterization Tests for Biomaterial-Based DDS
| Characterization Category | Key Parameters | Standard Methodologies |
|---|---|---|
| Structural Properties | Molecular weight, polydispersity, chemical modification degree, crystallinity | GPC/SEC, NMR, XRD, FTIR |
| Functional Performance | Glass transition temperature, viscosity, gelation time, swelling ratio | DSC, rheometry, in vitro gelation tests |
| Drug Release Profile | Release kinetics, mechanism (diffusion, erosion, swelling), completeness | USP dissolution apparatus, dialysis methods, continuous flow systems |
| Stability | Shelf-life, in-use stability, extractables/leachables | Accelerated stability studies, LC-MS, GC-MS |
Preclinical Proof-of-Concept and Safety Assessment
The preclinical development phase for biomaterial-based DDS requires rigorous demonstration of both proof-of-concept efficacy and comprehensive safety assessment. For complex systems combining structural scaffolds with controlled release functionality, this typically involves multiple animal models with progressive complexity, beginning with small animal models for initial screening and progressing to large animal models that more closely recapitulate human physiology and clinical use conditions. The bibliometric analysis of the field reveals that materials science, engineering, chemistry, polymer science represent the dominant research domains, highlighting the interdisciplinary nature of the required preclinical evidence [31].
Key elements of the preclinical safety assessment for biomaterial DDS include:
- Local tissue compatibility studies evaluating the response to both the initial material implantation and its degradation products over time
- Systemic toxicity assessment with particular attention to accumulation in non-target tissues and organs
- Degradation product profiling and toxicokinetic evaluation of both the polymer and plasticizers, stabilizers, or other processing additives
- Specialized safety pharmacology studies for site-specific applications (e.g., neurocompatibility for CNS delivery systems)
As noted in recent research on CNS drug delivery, "Nanomaterials emerge as potent tools in designing innovative drug delivery systems that demonstrate the potential to overcome the limitations posed by CNS tumors," highlighting the need for specialized blood-brain barrier penetration studies for these applications [112]. Similarly, for wound healing applications, "Electrospun nanofiber scaffolds demonstrate ability to modulate inflammation and facilitate granulation tissue formation," requiring comprehensive dermal safety and wound healing progression studies [8].
Clinical Development and Trial Design
SPIRIT 2025 Guidelines for Protocol Development
The updated SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) 2025 statement provides an evidence-based framework for clinical trial protocol development that addresses key methodological advances and emerging best practices in complex therapeutic areas [121]. For biomaterial-based DDS trials, several aspects of the updated guidelines warrant particular attention:
Open Science Requirements: The updated guidelines emphasize transparency through trial registration, protocol and statistical analysis plan accessibility, and data sharing commitments. For biomaterial systems, this may include sharing of material characterization data, manufacturing process details, and in vitro release methodology to facilitate scientific scrutiny and reproducibility [121].
Patient and Public Involvement: New SPIRIT 2025 items address plans for patient or public involvement in trial design, conduct, and reporting. For biomaterial DDS with specialized administration requirements (e.g., implantable systems, injectable in situ forming depots), early patient input can inform device design refinements, administration procedure development, and patient education materials [121].
Enhanced Harms Assessment: The guidelines place additional emphasis on comprehensive assessment and reporting of harms, which for biomaterial systems should include local tissue reactions, device-related adverse events, and long-term follow-up for biodegradable systems where complete degradation may extend beyond the primary study period [121].
The SPIRIT 2025 checklist consists of 34 minimum items that should be addressed in clinical trial protocols, with particular relevance to biomaterial DDS including detailed description of interventions, comparator selection rationale, and outcome assessment methods that account for both drug- and device-related endpoints [121].
Endpoint Selection and Evidence Generation
Clinical development programs for biomaterial-based DDS require carefully constructed endpoint hierarchies that capture both the drug-related therapeutic effects and device-related performance metrics. The complex nature of these combination products often necessitates composite endpoints and validated patient-reported outcome measures specifically designed to assess the unique benefits of the technology. Recent analyses of pharmaceutical requirements for drug delivery systems emphasize that "DDS must generate robust real-world data that demonstrate therapeutic performance and cost-effectiveness early in the development process to reduce uncertainty and control costs before market entry" [122].
For biomaterial DDS targeting specific clinical applications, endpoint selection should reflect the unique value proposition of the technology:
- For wound healing applications, this may include quantitative measures of healing progression, infection control, and dressing performance in addition to standard wound closure endpoints [7]
- For oncology applications utilizing targeted nanocarriers, endpoint strategies should capture both tumor response and reductions in systemic toxicity compared to conventional administration [32]
- For regenerative medicine applications, functional tissue restoration metrics may be required alongside structural assessment through imaging or histology [31]
The growing emphasis on real-world evidence and health economic outcomes in regulatory and reimbursement decisions necessitates early planning for post-market evidence generation, particularly for biomaterial systems that may demonstrate advantages in patient adherence, administration frequency reduction, or healthcare resource utilization [122].
Standardization and Quality Control Systems
Manufacturing Process Controls
The manufacturing process for biomaterial-based DDS requires rigorous control strategies to ensure consistent product quality, particularly for naturally-derived materials with inherent variability. As noted in research on marine biomaterials, "Despite their high biological potential and environmental advantages, marine biomaterials remain underexploited in the pharmaceutical field due to several factors, including raw material variability, limited standardization, and lack of regulatory harmonization" [119]. Implementation of Quality by Design (QbD) principles provides a systematic framework for identifying and controlling critical process parameters that impact product quality.
Key elements of the control strategy for biomaterial DDS manufacturing include:
- Raw material qualification with particular attention to biologically-sourced polymers requiring detailed characterization of source, extraction methodology, and purification history
- In-process controls for critical manufacturing steps such as polymer synthesis, drug loading, and sterilization
- Release testing encompassing both standard pharmaceutical quality attributes and biomaterial-specific characteristics such as porosity, degradation rate, and mechanical properties
- Stability-indicating methods validated to detect changes in both the drug substance and biomaterial carrier over time
Advanced manufacturing technologies including 3D bioprinting, electrospinning, and microfluidic fabrication offer unprecedented control over biomaterial architecture but introduce additional validation challenges related to process reproducibility, scalability, and real-time quality verification [119].
Analytical Method Validation
The complex nature of biomaterial-based DDS necessitates comprehensive analytical method validation beyond standard drug product requirements. Methods must be developed and validated to characterize drug-material interactions, release kinetics, and material degradation behavior under physiologically relevant conditions. As highlighted in recent research on functional biomaterials, "Future perspectives in functional biomaterials aim to bridge the gap between laboratory studies and clinical applications," with analytical method robustness representing a critical translational component [8].
Specialized analytical considerations for biomaterial DDS include:
- Drug release method development that appropriately simulates the in vivo environment and accounts for sink conditions, fluid dynamics, and enzyme activity where relevant
- Characterization of material degradation through monitoring of molecular weight changes, mass loss, and degradation product formation
- Surface characterization for systems where drug release is controlled by surface erosion or diffusion through the polymer matrix
- Accelerated release methods developed with understanding of their predictive value for in vivo performance
The development of standardized methodologies through organizations such as ASTM International and ISO provides valuable tools for analytical method harmonization, though biomaterial-specific standards remain limited for many emerging technology platforms.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Biomaterial DDS Development
| Material/Reagent | Function in Development | Key Considerations |
|---|---|---|
| Chitosan | Natural polysaccharide for nanoparticle and hydrogel formation; exhibits intrinsic antibacterial and wound-healing properties | Degree of deacetylation, molecular weight, and viscosity significantly impact performance and drug release [119] |
| PLGA | Biodegradable synthetic polymer for controlled release microspheres and implants; FDA-approved with predictable degradation kinetics | Lactide:glycolide ratio, molecular weight, and end-group chemistry determine erosion rate and drug release profile [31] |
| Alginate | Marine-derived polysaccharide for hydrogel formation and wound dressings; excellent moisture retention and biocompatibility | Guluronic acid content, molecular weight, and purification method impact gelation and stability [119] |
| PVA | Synthetic polymer for hydrogel preparation and particle stabilization; excellent film-forming properties | Degree of hydrolysis, molecular weight, and residual acetate content affect physical properties [8] |
| Lipids | Formulation of lipid nanoparticles for nucleic acid and poorly soluble drug delivery; enhanced biocompatibility | Lipid composition, phase transition temperature, and surface modification enable targeting and triggered release [32] |
| Marine Collagen | Biocompatible protein for tissue engineering scaffolds and wound healing; lower immunogenicity than mammalian collagen | Source species, extraction method, and cross-linking density impact mechanical properties and degradation [119] |
Visualizing Development Workflows
Regulatory Pathway Diagram
Biomaterial DDS Regulatory Pathway
Material Characterization Workflow
Biomaterial Characterization Workflow
The successful navigation of regulatory pathways for biomaterial-based controlled drug delivery systems requires proactive planning, robust characterization, and strategic evidence generation throughout the development lifecycle. The field is characterized by rapid technological advancement, with emerging areas including AI-assisted material design, personalized manufacturing approaches, and digital integration creating both opportunities and regulatory considerations [8]. As the pharmaceutical industry increasingly prioritizes drug delivery systems that "accelerate R&D timelines, minimize development risks and costs, and maximize product value," biomaterial-based platforms are well-positioned to address these needs through enhanced therapeutic performance and patient-centric design [122].
Strategic development approaches should emphasize:
- Early regulatory engagement through Pre-IND meetings to align on characterization requirements and clinical development plans
- Investment in analytical development to establish robust correlations between material properties and in vivo performance
- Proactive standardization through participation in consensus standards development for emerging technology platforms
- Integrated safety assessment that addresses both conventional pharmaceutical safety concerns and biomaterial-specific considerations
The continuing evolution of regulatory science for complex drug-device combination products promises more streamlined pathways for biomaterial-based DDS that demonstrate well-understood safety profiles and substantial therapeutic advantages. By adopting a science-based, quality-driven development approach aligned with regulatory expectations, innovators can successfully navigate these pathways to bring transformative biomaterial-based drug delivery technologies to patients in need.
Market Analysis and Future Projections for Biomaterial-Based Therapies
The field of controlled drug delivery represents a paradigm shift in therapeutic strategies, moving from conventional bolus administration to sophisticated, spatially and temporally controlled release systems. At the heart of this revolution lie biomaterials—natural or synthetic substances engineered to interact with biological systems for medical purposes. These materials serve as the foundational platform for advanced drug delivery systems (DDS), enabling unprecedented control over drug pharmacokinetics and biodistribution [123] [2]. The global biomaterials market, valued at approximately USD 171.85 billion in 2024, is projected to surge to USD 526.63 billion by 2034, growing at a robust compound annual growth rate (CAGR) of 11.85% [123] [124]. This remarkable growth is propelled by the convergence of several critical factors: an aging global population, rising prevalence of chronic diseases, advancements in material science, and the escalating demand for personalized medicine approaches that minimize side effects and maximize therapeutic efficacy [123] [125] [126].
Within this expanding market, drug delivery applications represent a pivotal growth segment. Biomaterials overcome fundamental limitations of conventional drug administration, including poor drug solubility, rapid clearance, enzymatic degradation, and non-specific toxicity [2] [8]. By designing biomaterials with precise physical, chemical, and biological properties, researchers can create carriers that protect therapeutic agents, target them to specific tissues or cells, and release them in response to specific physiological triggers [127] [8]. This whitepaper provides a comprehensive analysis of the current market landscape, explores cutting-edge material platforms, details experimental methodologies, and projects future trajectories for biomaterial-based therapies, with a specialized focus on their transformative role in controlled drug delivery systems.
Market Landscape Analysis
The biomaterials market demonstrates vigorous growth across multiple dimensions, including revenue, volume, and technological adoption. The table below summarizes key quantitative projections that define the market's trajectory from 2024 to 2034.
Table 1: Global Biomaterials Market Quantitative Overview (2024-2034)
| Metric | 2024 Baseline | 2034 Projection | CAGR (2025-2034) | Primary Drivers |
|---|---|---|---|---|
| Market Value | USD 171.85 Billion [123] | USD 526.63 Billion [123] | 11.85% [123] | Aging population, chronic disease prevalence, demand for minimally invasive surgeries [123] [126] |
| Market Volume | 805.32 Kilo Tons [123] | 1,850.43 Kilo Tons [123] | 8.68% [123] | Growing application in medical implants and devices [123] |
| Smart Biomaterials Value | USD 14.5 Billion (2023) [125] | USD 50.5 Billion [125] | 12.3% (2024-2034) [125] | Demand for targeted/personalized medicine, investment in novel drug delivery systems [125] |
Segmentation Analysis
The market's composition reveals dominant segments and high-growth opportunities, crucial for strategic research and development focus.
Table 2: Biomaterials Market Segmentation by Material Type and Application (2024)
| Segmentation | Dominant Segment (2024) | Market Share/Size | Fastest-Growing Segment | Projected CAGR |
|---|---|---|---|---|
| By Material Type | Synthetic Biomaterials [123] [124] | 73.34% volume share [123] | Natural Biomaterials [123] [124] | 13.15% [123] |
| By Application | Orthopedic Applications [123] [126] [110] | 35% share [123] | Tissue Engineering [123] | Not Specified |
| By Technology | 3D Printing [110] | 31.4% share (2025) [110] | Not Specified | Not Specified |
Material-Type Dynamics: The dominance of synthetic biomaterials (polymers, metals, ceramics) is attributed to their superior strength, controlled degradation rates, and design flexibility, making them ideal for implants and stents [123] [124]. However, the natural biomaterials segment (e.g., collagen, chitosan, hyaluronic acid) is growing faster due to their superior biocompatibility, biodegradability, and integration with human tissues, which are highly valued in regenerative medicine and soft tissue applications [123] [124].
Application-Focus Shift: While orthopedic applications (e.g., joint replacements, bone grafts) currently lead due to an aging population and rising musculoskeletal disorders, drug delivery systems and tissue engineering are critical growth frontiers [123] [126] [110]. The expansion is fueled by technological advancements and a growing focus on regenerative solutions for complex diseases [123] [125].
Regional Market Dynamics
Geographically, the market landscape is characterized by established leadership and rapidly emerging centers of innovation.
Table 3: Regional Market Analysis and Growth Projections
| Region | Market Share (2024/2025) | Growth Outlook | Key Growth Drivers |
|---|---|---|---|
| North America | Largest share (41.21% volume in 2024) [123] | CAGR of 7.44% (volume, 2025-2034) [123] | Advanced healthcare infrastructure, significant R&D investments, strong regulatory frameworks, presence of key market players [123] [126] [110] |
| Asia Pacific | 24.5% share (2025) [110] | Fastest-growing (CAGR: 14.96%) [123] [124] | Supportive government initiatives, rising healthcare investments, expanding medical tourism, large patient population [123] [124] [110] |
| Europe | Steady growth [128] | CAGR of 7.9% (2025-2035) [128] | Strong academic research, focus on sustainable/biodegradable implants, stringent EU regulations ensuring product quality [128] |
Advanced Biomaterials for Drug Delivery
Intelligent Stimuli-Responsive Biomaterials
"Smart" or stimuli-responsive biomaterials represent the cutting edge of drug delivery technology. These dynamically functional materials adapt their properties in response to specific environmental triggers, enabling precise spatiotemporal control over drug release [125] [127] [8].
Physiological Stimuli-Responsive Systems: These systems exploit pathological variations in the body's internal environment. Common triggers include pH (e.g., acidic tumor microenvironments or inflamed tissues), enzyme concentrations (e.g., matrix metalloproteinases at disease sites), and redox potential [7] [8]. For instance, a PVA-CMC-based hydrogel embedded with natural bioactive extracts (dragon's blood resin and sage) dynamically responds to wound microenvironments, releasing anti-inflammatory and antioxidant compounds to accelerate collagen formation and epithelial regeneration [8].
Externally Triggered Systems: These systems require an external application of energy or substance for activation, offering unparalleled control for clinicians. Key modalities include:
- Temperature-Sensitive Systems: Chitosan-based hydrogels that undergo sol-gel transition at body temperature, ideal for forming depots in irregular tissue defects [8].
- Light-Responsive Systems: Water-dispersible upconversion nanoparticles activated by low-power red light for deep-tissue, non-invasive therapy [127].
- Magnetically Propelled Systems: Motile hydrogel microrobots navigated by external magnetic fields to penetrate tumor sites for localized drug delivery [8].
Nanotechnology-Driven Delivery Platforms
Nanotechnology has unlocked new possibilities for precision medicine by engineering materials at the nanoscale to overcome biological barriers [8].
Polymeric Nanoparticles and LNPs: Biodegradable polymers like PLGA are extensively used for controlled release, as demonstrated in a PLGA-Resveratrol nanocomposite for protecting oocytes during cryopreservation [8]. Lipid Nanoparticles (LNPs), crucial for mRNA vaccine delivery, are being optimized for repeated administrations by carefully engineering the structure and ratio of PEG lipids to avoid accelerated blood clearance [127].
Inorganic Nanoparticles (INPs): Platforms such as mesoporous silica nanoparticles and calcium phosphate systems offer tunable surfaces and high payload capacity for targeted delivery and immune activation in cancer immunotherapy [2] [127]. Silica-coated gold nanorods (AuNR@SiO₂) can be designed to induce precisely controlled mild hyperthermia for enhanced cancer therapy [127].
Electrospun Nanofibers: These scaffolds provide a high surface-area-to-volume ratio and tunable porosity, making them excellent localized delivery systems. They are particularly effective in applications like diabetic wound healing, where they modulate inflammation and support granulation tissue formation [8].
Next-Generation and Composite Systems
The frontier of biomaterial science involves integrating multiple functionalities and materials to create synergistic therapeutic effects.
- Multifunctional Nanocomposites: These combine different material classes to achieve enhanced mechanical, biological, and therapeutic properties. Examples include polymer-ceramic composites and hydrogel-ceramic blends designed for bone tissue regeneration and drug delivery [2].
- Supramolecular Systems: Materials like NIR-triggered supramolecular hydrogels loaded with MXene–doxorubicin complexes achieve synergistic chemo-photothermal therapy with excellent tumor localization and spatiotemporal control [127].
- Exosome-Based Therapies: Natural nanovesicles known as exosomes are emerging as promising carriers for nucleic acids and proteins in orthopedic degenerative diseases. Engineering modifications are being employed to improve their stability and targeting efficacy [8].
Experimental Protocols and Methodologies
This section details standardized experimental protocols for developing and characterizing advanced biomaterial-based drug delivery systems, providing a technical reference for researchers.
Protocol 1: Formulation and Evaluation of Thermo-Responsive Hydrogels
This protocol outlines the synthesis and characterization of an injectable, thermosensitive hydrogel for controlled drug delivery, based on the chitosan-based system described by Gu et al. [8].
Objective: To develop a fast-gelling, thermosensitive hydrogel for the sustained co-delivery of therapeutic proteins (e.g., EPO) and small molecules (e.g., FK506).
Materials:
- Polymer: Chitosan (medium molecular weight, >75% deacetylation)
- Crosslinker: Glycerophosphate disodium salt (β-GP)
- Bioactive Agents: Recombinant human EPO, FK506 (Tacrolimus)
- Solvent: Dilute hydrochloric acid (0.1M HCl)
- Cell Culture: Human periodontal ligament cells (hPDLCs)
Methodology:
- Hydrogel Preparation:
- Dissolve chitosan powder (2% w/v) in 0.1M HCl under continuous stirring at 4°C for 12 hours to obtain a clear solution.
- Slowly add a 50% (w/v) aqueous solution of β-GP dropwise to the chitosan solution under vigorous stirring on an ice bath until a final β-GP concentration of 10% (w/w) is achieved. Maintain the temperature below 10°C throughout to prevent premature gelling.
- Add EPO (1000 IU/mL) and FK506 (100 ng/mL) to the sol-state hydrogel and mix gently to ensure uniform distribution.
Gelation Time and Rheological Analysis:
- Transfer the hydrogel sol to a vial and incubate at 37°C in a water bath.
- Determine the gelation time using the test-tube inversion method (the point at which the material no longer flows upon 90° inversion within 30 seconds).
- Characterize viscoelastic properties using a rheometer with a parallel-plate geometry. Perform time-sweep experiments at 1 Hz frequency and 1% strain to monitor the evolution of storage (G') and loss (G'') moduli at 37°C.
In Vitro Drug Release Kinetics:
- Pipette 1 mL of the drug-loaded hydrogel sol into a dialysis tube (MWCO: 100 kDa). Immerse the tube in 50 mL of phosphate-buffered saline (PBS, pH 7.4) at 37°C under gentle agitation (50 rpm).
- At predetermined time points, collect 1 mL of the release medium and replace it with fresh pre-warmed PBS.
- Quantify the released EPO using an ELISA kit and FK506 using HPLC to construct release profiles.
In Vitro Biological Efficacy:
- Cell Viability and Proliferation: Culture hPDLCs on the surface of pre-formed hydrogels. Assess viability using a Live/Dead assay kit and quantify proliferation with a CCK-8 assay at 1, 3, and 7 days.
- Osteogenic Differentiation: Seed hPDLCs on hydrogels in osteogenic medium. After 14 and 21 days, quantify osteogenic markers (ALP activity, OPN, OCN expression via RT-qPCR) and perform Alizarin Red S staining to visualize calcium deposition.
Protocol 2: Development of Targeted Lipid Nanoparticles (LNPs) for mRNA Delivery
This protocol, informed by Lee et al. [127], focuses on formulating and optimizing mRNA-loaded LNPs, with emphasis on PEG lipid design to mitigate the accelerated blood clearance (ABC) phenomenon upon repeated administration.
Objective: To formulate and characterize mRNA-loaded LNPs with a PEG lipid composition that enables efficient protein expression and minimizes the ABC effect for chronic dosing.
Materials:
- Lipids: Ionizable lipid (e.g., DLin-MC3-DMA), DSPC (helper lipid), Cholesterol, PEG-lipids (e.g., DMG-PEG2000, DSG-PEG2000) at varying molar ratios (1.5-3.0%).
- mRNA: Firefly luciferase (FLuc) mRNA or target therapeutic mRNA.
- Aqueous Buffer: 10 mM citrate buffer (pH 4.0).
- Purification: Dialysis cassettes (MWCO: 20 kDa).
Methodology:
- LNP Formulation via Microfluidics:
- Prepare the organic phase: Dissolve the ionizable lipid, DSPC, cholesterol, and PEG-lipid in ethanol at a predetermined molar ratio (e.g., 50:10:38.5:1.5).
- Prepare the aqueous phase: Dilute mRNA in citrate buffer to a concentration of 0.1 mg/mL.
- Use a microfluidic device to mix the two phases at a fixed flow rate ratio (aqueous:organic = 3:1), ensuring total flow rate is optimized for nanoparticle size control.
- Immediately dilute the formed LNPs in 1X PBS (pH 7.4) to stabilize the particles.
LNP Purification and Characterization:
- Purification: Dialyze the LNP suspension against PBS for 4 hours at 4°C to remove ethanol and exchange the buffer.
- Particle Size and Zeta Potential: Determine the hydrodynamic diameter, polydispersity index (PDI), and zeta potential using dynamic light scattering (DLS).
- mRNA Encapsulation Efficiency: Use a Ribogreen assay. Measure fluorescence with and without a detergent (Triton X-100) to disrupt the LNPs. Calculate encapsulation efficiency as:
(1 - (free mRNA/total mRNA)) * 100.
In Vitro Transfection Efficiency:
- Seed HEK-293 or other relevant cells in 24-well plates.
- Transfect cells with LNPs containing FLuc mRNA at a predetermined mRNA concentration.
- After 24-48 hours, lyse cells and measure luciferase activity using a luminometer. Normalize protein concentration using a BCA assay. Report results as Relative Light Units (RLU) per mg of protein.
In Vivo Evaluation of ABC Phenomenon:
- Administer a first dose of LNPs (with different PEG-lipid structures/ratios) intravenously to Balb/c mice.
- Administer a second, identical dose 7 days later.
- Collect blood at various time points post-injection to measure pharmacokinetics and monitor for increased clearance and reduced expression of the second dose, which indicates the ABC phenomenon.
Visualization of Concepts and Workflows
Smart Biomaterial Drug Release Mechanisms
Diagram Title: Smart Biomaterial Drug Release Mechanisms
Workflow for Biomaterial-Based Therapy Development
Diagram Title: Biomaterial Therapy Development Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Successful research in biomaterial-based drug delivery relies on a suite of specialized reagents and materials. The following table details essential components and their functions in developing these advanced systems.
Table 4: Key Research Reagent Solutions for Biomaterial-Based Drug Delivery
| Reagent/Material | Function/Application | Research Context |
|---|---|---|
| Chitosan | Natural polymer for thermosensitive hydrogels; forms injectable depots that gel at body temperature. | Used in fast-gelling hydrogels for periodontal tissue regeneration and controlled drug release [8]. |
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable synthetic polymer for nanoparticles; enables sustained release of encapsulated drugs. | Used in PLGA-RES nanocomposites for oocyte cryopreservation and numerous other drug delivery applications [8]. |
| Ionizable Lipid (e.g., DLin-MC3-DMA) | Key component of LNPs for encapsulating and delivering nucleic acids (mRNA, siRNA). | Critical for the formulation of mRNA-loaded lipid nanoparticles for therapeutic protein expression [127]. |
| PEG-Lipid (e.g., DMG-PEG2000) | Provides a hydrophilic stealth layer on nanoparticles, reducing immune recognition and improving circulation time. | Structure and ratio are critical for avoiding the Accelerated Blood Clearance (ABC) phenomenon in repeated mRNA LNP administrations [127]. |
| Mesoporous Silica Nanoparticles | Inorganic nanoparticles with high surface area and tunable pores for high drug loading and controlled release. | Explored as versatile platforms for targeted drug delivery and cancer immunotherapy [2] [127]. |
| Hyaluronic Acid | Natural polysaccharide used in hydrogels and nanoparticles; bioactive and targets CD44 receptors on some cancer cells. | Used in water-dispersible upconversion nanoparticles for deep-tissue imaging and transdermal therapy [127]. |
| Polyethyleneimine (PEI) | Cationic polymer for non-viral gene delivery; facilitates endosomal escape via the "proton sponge" effect. | A key polymer-based nanocarrier reviewed for its use in gene delivery systems [8]. |
| Decellularized Extracellular Matrix (dECM) | Natural biomaterial providing tissue-specific biological cues for cell growth and tissue regeneration. | Used as a bioink component for 3D bioprinting physiologically relevant tissue models like blood-brain barriers [127]. |
The trajectory of biomaterial-based therapies points toward an era of increasingly intelligent, personalized, and integrative medical solutions. Several key trends are poised to define the next decade of research and clinical translation.
AI-Driven Material Design and Discovery: Artificial intelligence (AI) and machine learning are set to revolutionize biomaterials research by rapidly predicting material properties, optimizing synthesis parameters, and designing novel materials with tailored functionalities. Explainable AI (XAI) will be crucial for building trust and providing transparency in model predictions, accelerating the development of next-generation drug delivery systems [126] [8].
Advanced Biofabrication and 3D Bioprinting: The integration of 3D printing with biomaterials will evolve from creating structural implants to fabricating complex, living tissues. Coaxial 3D bioprinting allows for the creation of perfusable, vascularized tissue constructs, as demonstrated in blood-brain barrier models [127]. This technology will enable high-fidelity disease modeling and the development of more effective, personalized therapies.
Integration of Bioelectronics and Biomaterials: The convergence of flexible bioelectronics with biomaterials will give rise to therapeutic bioelectronic implants capable of real-time monitoring of physiological signals (e.g., metabolite levels, inflammation) and on-demand, triggered drug release, creating closed-loop systems for managing chronic diseases [125].
Focus on Immuno-Engineered Biomaterials: Understanding and controlling the interaction between biomaterials and the immune system will become paramount. Future materials will be explicitly designed to modulate immune responses—suppressing inflammation where detrimental or activating immunity for applications like cancer vaccines and immunotherapy [127] [8].
Sustainability and Green Biomaterials: The drive toward eco-friendly medical solutions will intensify. Research will focus on biomaterials derived from agricultural waste (e.g., rice husk nanosilica) and the development of fully biodegradable, biosourced composites, aligning medical innovation with global environmental sustainability goals [123] [124].
In conclusion, biomaterial-based therapies are transitioning from passive structural components to dynamic, interactive systems capable of sophisticated diagnostic and therapeutic functions. The market's robust growth reflects their expanding role in addressing unmet clinical needs. For researchers and drug development professionals, the future lies in harnessing interdisciplinary approaches—merging materials science, biology, data science, and engineering—to develop the next wave of smart, personalized, and sustainable biomaterial solutions that will redefine controlled drug delivery and regenerative medicine.
Conclusion
Biomaterials have fundamentally reshaped the landscape of controlled drug delivery, evolving from simple sustained-release platforms to sophisticated, intelligent systems capable of targeted and personalized therapy. The integration of ECM-mimetic designs, smart responsive materials, and advanced manufacturing techniques like 3D bioprinting has significantly enhanced therapeutic precision. However, the journey from laboratory innovation to clinical application necessitates overcoming persistent challenges in immunogenicity, scalable manufacturing, and rigorous regulatory validation. The future of the field is intrinsically linked to interdisciplinary collaboration, leveraging AI and high-throughput screening to accelerate the design of next-generation biomaterials. The convergence of biomaterials with gene editing, immunotherapy, and personalized medicine promises a new era of treatments that are not only more effective but also safer and tailored to individual patient needs, ultimately bridging the critical gap between innovative material science and transformative clinical impact.
References
- 1. Biomaterials for Drug Delivery and Human Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10817481/]
- 2. Special Issue : Biomaterials for Controlled Drug Delivery [https://www.mdpi.com/journal/pharmaceutics/special_issues/X05ODU0LCH]
- 3. Controlled Drug Delivery Systems: Current Status and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8512302/]
- 4. Next-generation smart ophthalmic biomaterials: From passive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607147/]
- 5. Advanced rational design of polymeric nanoparticles for ... [https://pubmed.ncbi.nlm.nih.gov/40484283/]
- 6. Drug Delivery | Society for Biomaterials (SFB) [https://biomaterials.org/node/1105/sigs-overview/drug-delivery]
- 7. Biomaterials-mediated sequential drug delivery: emerging ... [https://www.sciencedirect.com/science/article/pii/S1818087625000728]
- 8. Editorial: Functional biomaterials for drug delivery [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1550444/full]
- 9. Evolution of branched peptides as novel biomaterials [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d4tb01897d]
- 10. Computational analysis of controlled drug release from ... [https://www.nature.com/articles/s41598-024-79749-6]
- 11. Recent Applications of PLGA in Drug Delivery Systems [https://www.mdpi.com/2073-4360/16/18/2606]
- 12. PEGylated PLGA nanoparticles: unlocking advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288292/]
- 13. From Molecules to Mind: The Critical Role of Chitosan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11901451/]
- 14. The drug release of PLGA-based nanoparticles and their ... [https://www.sciencedirect.com/science/article/pii/S2405844024141965]
- 15. Chitosan-collagen composite biomaterials: Advances and ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025065882]
- 16. Marine-Derived Collagen and Chitosan: Perspectives on ... [https://www.mdpi.com/1660-3397/23/8/318]
- 17. Medical Ceramics in the Real World: 5 Uses You'll Actually ... [https://www.linkedin.com/pulse/medical-ceramics-real-world-5-uses-youll-actually-v2e4f/]
- 18. Medical Ceramics Market to Reach $29.93 Billion by 2032, ... [https://www.prnewswire.com/news-releases/medical-ceramics-market-to-reach-29-93-billion-by-2032--growing-at-a-cagr-of-6-2-from-2025--says-meticulous-research-302490633.html]
- 19. Biomaterials for Drug Delivery and Human Applications [https://www.mdpi.com/1996-1944/17/2/456]
- 20. Researchers Develop Enzyme-Responsive Biomaterials for ... [https://www.geneonline.com/researchers-develop-enzyme-responsive-biomaterials-for-targeted-drug-delivery-and-tissue-engineering-applications/]
- 21. Recent Developments in Nanoparticle‐Hydrogel Hybrid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463025/]
- 22. Stimuli-Responsive MXene Nanomaterials for Advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595973/]
- 23. Biomaterials in Drug Delivery: Advancements in Cancer ... [https://www.mdpi.com/1422-0067/25/6/3126]
- 24. Stimuli-responsive peptide-based nanodrug delivery systems ... [https://pubs.rsc.org/en/content/articlehtml/2025/cc/d5cc00950b]
- 25. Biomaterial-driven regenerative drug delivery: a vicennial ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1593985/full]
- 26. Decellularized extracellular matrix as a drug delivery carrier [https://www.sciencedirect.com/science/article/abs/pii/S0168365925002810]
- 27. Biomaterials in tissue repair and regeneration: key insights ... [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2025.1565810/full]
- 28. Design and Applications of Extracellular Matrix Scaffolds in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293650/]
- 29. Controlled delivery of PRP from decellularized extracellular ... [https://www.nature.com/articles/s41598-025-92319-8]
- 30. Extracellular-Matrix-Mimetic Hydrogels by Using ... [https://www.mdpi.com/1422-0067/26/11/4987]
- 31. Biomaterial-driven regenerative drug delivery - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12301386/]
- 32. Drug Delivery Technologies Impacting 2025 and Beyond [https://www.pharmaadvancement.com/pharma-trends/drug-delivery-technologies-impacting-2025-and-beyond/]
- 33. 5 Areas Of Drug Delivery Innovation To Watch In 2025 [https://www.drugdeliveryleader.com/doc/areas-of-drug-delivery-innovation-to-watch-in-2025-0001]
- 34. Smart Drug Delivery Systems Market Size | Forecast, 2025 ... [https://www.gminsights.com/industry-analysis/smart-drug-delivery-systems-market]
- 35. Targeted Drug Delivery Research Business Report 2025 ... [https://aijourn.com/targeted-drug-delivery-research-business-report-2025-global-market-to-reach-24-9-billion-by-2030-smart-polymers-and-external-stimuli-open-new-frontiers-in-precision-delivery-researchandmarkets-c/]
- 36. - and Polymer -based liposome in targeted nanoparticles drug delivery [https://pubmed.ncbi.nlm.nih.gov/20515826/]
- 37. Advancements in Liposomal Drug and... | Preprints.org Delivery [https://www.preprints.org/manuscript/202503.1603/v1]
- 38. Advances and Emerging Trends in Drug Delivery Systems [https://juniperpublishers.com/jpcr/JPCR.MS.ID.555802.php]
- 39. -mediated advanced Nanoparticle : a modernized... drug delivery [https://www.dovepress.com/recent-advances-in-nanoparticle-based-antiretroviral-drug-delivery-sys-peer-reviewed-fulltext-article-IJN]
- 40. Nanocarrier imaging at single-cell resolution across entire ... [https://www.nature.com/articles/s41587-024-02528-1]
- 41. Robotics, microfluidics, nanotechnology and AI in the synthesis and... [https://link.springer.com/article/10.1007/s13346-021-00929-2]
- 42. Next-Generation Biomaterials: Design Strategies, Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12529143/]
- 43. A Comprehensive Review of Thermosensitive Hydrogels [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294456/]
- 44. Advances in pH-responsive drug delivery systems for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12203708/]
- 45. Breaking barriers with pH-responsive nanocarriers [https://www.sciencedirect.com/science/article/abs/pii/S0378517325007689]
- 46. A comprehensive study on pH-sensitive nanoparticles ... [https://www.bsmiab.org/jabet/articles/178-1730094477]
- 47. pH-Responsive Hydrogels: Recent Advances in ... [https://www.mdpi.com/2073-4360/17/11/1451]
- 48. Recent Advances in Tumor Targeting via EPR Effect for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8234032/]
- 49. Different Targeting Ligands-Mediated Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10893104/]
- 50. Biomaterial-targeted precision nanoparticle delivery to the ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706122005608]
- 51. Protein-based biomaterials: Advances in structural design ... [https://pubmed.ncbi.nlm.nih.gov/41224090/]
- 52. a review of their role in controlled drug delivery and tissue ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra06280b?page=search]
- 53. Active Targeting Strategies Using Biological Ligands for ... [https://www.mdpi.com/2072-6694/11/5/640]
- 54. Approaches to Improve EPR-Based Drug Delivery for Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10051487/]
- 55. Enhancement of EPR Effect for Passive Tumor Targeting [https://www.mdpi.com/2076-3417/15/6/3189]
- 56. Comparison of active, passive and magnetic targeting to ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365914005793]
- 57. NANBIOSIS Researchers Present Advances in ... [https://www.nanbiosis.es/nanbiosis-researchers-present-advances-in-nanomedicine-at-nanomat-2025/]
- 58. Microfluidic-engineered polymeric nanocarriers for ... [https://pubmed.ncbi.nlm.nih.gov/41201532/]
- 59. Hydrogels in cancer treatment: mapping the future of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1607240/full]
- 60. Active implantable drug delivery systems: engineering factors ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00131e]
- 61. Engineering therapeutic scaffolds: integrating drug delivery ... [https://pubmed.ncbi.nlm.nih.gov/40838346/]
- 62. Control and interplay of scaffold-biomolecules interactions ... [https://pubs.rsc.org/en/content/articlelanding/2025/bm/d5bm00049a]
- 63. Recent advances in bionic scaffolds for cartilage tissue ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1625550/full]
- 64. Exploring the 3D Bioprinting Landscape in the Delivery of ... [https://pubmed.ncbi.nlm.nih.gov/40999931/]
- 65. Engineering therapeutic scaffolds: integrating drug delivery ... [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d5tb01338k]
- 66. Recent Progress in the Application of Electrospinning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12295322/]
- 67. A review of electrospun polymeric fibers as potential drug ... [https://www.sciencedirect.com/science/article/pii/S2468217925000863]
- 68. State-of-the-Art Organ-on-Chip Models and Designs for ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383757/]
- 69. Advancing Organ-on-a-Chip Systems: The Role of Scaffold ... [https://www.mdpi.com/2073-4360/17/9/1263]
- 70. Organ-on-a-Chip: A Roadmap for Translational Research in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610883/]
- 71. Organoids and organs-on-chips: Recent advances ... [https://www.sciencedirect.com/science/article/abs/pii/S2666634025000947]
- 72. Research Progress on Biomaterials with Immunomodulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12412535/]
- 73. Advanced biomaterials in immune modulation: The future ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325008099]
- 74. Overcoming immune hurdles to implant longevity [https://www.nature.com/articles/s41551-024-01276-6]
- 75. Biomaterials in tissue repair and regeneration: key insights ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394198/]
- 76. Controllable degradation behavior, mechanical properties ... [https://www.nature.com/articles/s41529-025-00658-8]
- 77. Sustained-Release Intra-Articular Drug Delivery: PLGA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566636/]
- 78. A new evidence-based design-of-experiments approach ... [https://www.nature.com/articles/s41598-024-82496-3]
- 79. The foreign body response to biomaterial implants is ... [https://pubmed.ncbi.nlm.nih.gov/40516838/]
- 80. ISO 10993-1:2025 Updates —Top 10 Biological Evaluation ... [https://namsa.com/resources/blog/iso-10993-12025top-10-biological-evaluation-essentials-in-the-update/]
- 81. Comparative Evaluation of Biocompatibility Data from the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12588249/]
- 82. Vascularization Strategies for Tissue Engineering - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2817665/]
- 83. Biomaterial-based vascularization strategies for enhanced ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03140-4]
- 84. From Bone To Blood Flow: Tissue Engineering In ... [https://orthopedicreviews.openmedicalpublishing.org/article/132223-from-bone-to-blood-flow-tissue-engineering-in-orthopedics-a-narrative-review]
- 85. Engineering a heparin-mimetic biomaterial to promote ... [https://www.nature.com/articles/s42003-025-08946-4]
- 86. Engineering in vitro vascular microsystems [https://www.nature.com/articles/s41378-025-00956-w]
- 87. Cell encapsulated biomaterials for translational medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12596701/]
- 88. Quantifying Vascular Density in Tissue Engineered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8110917/]
- 89. Double‐Orthogonal Gradient‐Based High‐Throughput ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11935256/]
- 90. Brief Guide: Experimental Strategies for High-Quality Hit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8293735/]
- 91. High-Throughput Screening (HTS): A Simple Guide ... [https://www.chemcopilot.com/blog/hts-material-discovery]
- 92. Quantitative high-throughput screening: A titration-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1518803/]
- 93. A paradigm for high-throughput screening of cell-selective ... [https://www.sciencedirect.com/science/article/pii/S2452199X23001408]
- 94. Quality Control of Quantitative High Throughput Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6520559/]
- 95. The synergy of artificial intelligence in biomaterials ... [https://www.sciencedirect.com/science/article/pii/S305072352500001X]
- 96. Machine Learning-Enhanced Nanoparticle Design for ... [https://pubmed.ncbi.nlm.nih.gov/40536233/]
- 97. Machine Learning in Predicting Printable Biomaterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10353544/]
- 98. AI Engineers Nanoparticles for Improved Drug Delivery [https://pratt.duke.edu/news/ai-engineers-nanoparticles-for-improved-drug-delivery/]
- 99. AI energized hydrogel design, optimization and application in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10924066/]
- 100. AI-guided biomaterials and biofabrication strategies for ... [https://www.sciencedirect.com/science/article/pii/S3050562325001795]
- 101. Artificial intelligence-assisted next-generation biomaterials [https://pubmed.ncbi.nlm.nih.gov/40695076/]
- 102. How artificial intelligence shapes the future of biomaterials? [https://www.sciencedirect.com/science/article/pii/S2949822824002788]
- 103. Advanced In Vitro Models for Preclinical Drug Safety [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763796/]
- 104. Complex in vitro model: A transformative model in drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10828975/]
- 105. Exploring the landscape of current in vitro and in vivo ... [https://link.springer.com/article/10.1007/s00259-025-07123-3]
- 106. In vivo Fate of Targeted Drug Delivery Carriers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11246094/]
- 107. Smart biomaterials: as active immune modulators to shape pro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12558899/]
- 108. Innovative biomaterial strategies for mitigating radiotherapy ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854525008835]
- 109. 2025 Biomaterials Global Market Overview, 2021-2030 - [https://www.globenewswire.com/news-release/2025/02/27/3033608/28124/en/2025-Biomaterials-Global-Market-Overview-2021-2030-Collaborative-Research-and-Smart-Biomaterials-Drive-Industry-Growth.html]
- 110. Biomaterials Market Trends, Share and Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/biomaterials-market]
- 111. Assessment of the Toxicity of Biocompatible Materials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8778995/]
- 112. Challenges and material innovations in drug delivery to ... [https://pubmed.ncbi.nlm.nih.gov/39985979]
- 113. Bridging the Gap: The Role of Advanced Formulation ... [https://pubmed.ncbi.nlm.nih.gov/41185748/]
- 114. Novel Drug Approvals for 2025 [https://www.fda.gov/drugs/novel-drug-approvals-fda/novel-drug-approvals-2025]
- 115. Controlled Release Drug Delivery Market Size & Trends, ... [https://www.coherentmarketinsights.com/industry-reports/controlled-release-drug-delivery-market]
- 116. 10 clinical trials to watch the rest of 2025 [https://www.biopharmadive.com/news/biotech-pharma-clinical-trials-watch-2025/736120/]
- 117. Advances, challenges, and future directions in the clinical ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X24001698]
- 118. Editorial: Pharmaceutical biomaterials [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1661817/full]
- 119. From Sea to Therapy: Marine Biomaterials for Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388878/]
- 120. Investigational New Drug (IND) Application [https://www.fda.gov/drugs/types-applications/investigational-new-drug-ind-application]
- 121. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 122. Pharma's Requirements for Drug Delivery Systems in 2025 [https://alirahealth.com/pharma-requirements-drug-delivery-system-selection/]
- 123. Biomaterials Market Size to Surge USD 526.63 Billion by ... [https://www.towardschemandmaterials.com/insights/biomaterials-market]
- 124. Biomaterials Market Size to Worth USD 526.63 Billion by ... [https://finance.yahoo.com/news/biomaterials-market-size-worth-usd-131600880.html]
- 125. Smart Biomaterials Market Forecast to 2034: Driving [https://www.globenewswire.com/news-release/2025/03/21/3047102/32656/en/Smart-Biomaterials-Market-Forecast-to-2034-Driving-Advances-in-Tissue-Engineering-Implants-and-Drug-Delivery-with-a-Projected-Valuation-of-US-50-5-Billion-TMR-Analysis.html]
- 126. Biomaterials Market Size to Hit USD 523.75 Billion by 2034 [https://www.precedenceresearch.com/biomaterials-market]
- 127. Smart Biomaterials for Delivery of Drugs and Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311304/]
- 128. Biomaterial Market Size & Growth Outlook 2023-2035 [https://www.futuremarketinsights.com/reports/biomaterials-market]