Biomaterial Scaffolds for Tissue Engineering: From Design Principles to Clinical Applications
This article provides a comprehensive overview of the latest advancements in biomaterial scaffolds for tissue engineering, tailored for researchers, scientists, and drug development professionals.
Biomaterial Scaffolds for Tissue Engineering: From Design Principles to Clinical Applications
Abstract
This article provides a comprehensive overview of the latest advancements in biomaterial scaffolds for tissue engineering, tailored for researchers, scientists, and drug development professionals. It explores the foundational design principles of ideal scaffolds, including biocompatibility, mechanical properties, and bioactivity. The review delves into methodological innovations across material classes and fabrication techniques like 3D bioprinting, examines key challenges and optimization strategies for immune response and mechanical performance, and discusses the role of AI and high-throughput technologies in validation and comparative analysis. By synthesizing current research and future directions, this article serves as a strategic resource for advancing regenerative medicine from the laboratory to the clinic.
Blueprint for Regeneration: Core Principles of an Ideal Biomaterial Scaffold
In the field of tissue engineering, biomaterial scaffolds serve as temporary three-dimensional (3D) structures that mimic the native extracellular matrix (ECM), providing mechanical support and biochemical cues that guide cellular behavior for tissue regeneration [1]. For these scaffolds to function successfully in a clinical setting, they must fulfill two foundational requirements: biocompatibility—the ability to perform with an appropriate host response without triggering deleterious effects—and biodegradability—the capacity to break down into non-toxic byproducts at a rate that matches new tissue formation [1] [2]. These intertwined properties are non-negotiable for the safe and effective integration of implants within the human body. Without them, scaffolds risk provoking severe immune responses, chronic inflammation, or mechanical failure, ultimately leading to device rejection and therapeutic failure. This whitepaper provides an in-depth technical examination of the principles, assessment methodologies, and material innovations defining these critical attributes, serving as a guide for researchers and drug development professionals working at the forefront of regenerative medicine.
Defining the Core Principles
Biocompatibility: Beyond Inertness
Modern interpretations of biocompatibility have evolved from the historical concept of material inertness. Today, it is understood as an active, favorable response where the material interacts with the host's biological system in a way that supports the intended function—be it promoting cell adhesion, proliferation, differentiation, or integration with surrounding native tissue [2]. A key metric of biocompatibility is the foreign body response (FBR), an immune-mediated reaction that begins with protein adsorption onto the implant surface, followed by acute and chronic inflammation, and potentially culminating in fibrosis and scar tissue formation [2]. Ideal biomaterials actively modulate this response to minimize FBR, thereby promoting integration and regeneration [2].
Biodegradability: Engineering Transience
Biodegradability refers to the controlled, predictable breakdown of a scaffold material into metabolic byproducts that the body can safely resorb or excrete. This process can occur through hydrolytic degradation (cleavage of chemical bonds by water) or enzymatic degradation (cleavage by specific enzymes present in bodily fluids) [1]. The degradation kinetics must be carefully tailored to the specific clinical application; the scaffold must maintain structural integrity long enough to support the developing tissue but subsequently degrade to avoid impeding further growth or creating long-term complications [1]. The degradation profile is thus not merely a property of disappearance but a critical design parameter that governs the success of the regeneration timeline.
Quantitative Assessment of Scaffold Properties
The evaluation of next-generation scaffolds yields critical quantitative data on their performance. The table below summarizes key findings from recent studies on composite and natural material-based scaffolds.
Table 1: Quantitative Performance Metrics of Representative Biomaterial Scaffolds
| Scaffold Material | Key Measured Property | Initial Value | Value After 8 Weeks | Experimental Model | Reference |
|---|---|---|---|---|---|
| BNC-CS-AG-GT Hydrogel | Compressive Strength | ~68 MPa | ~25 MPa | In vitro SBF + Lysozyme | [1] |
| BNC-CS-AG-GT Hydrogel | Weight / Mass Loss | 0% (Baseline) | 54% reduction | In vitro SBF + Lysozyme | [1] |
| Ulva sp. Seaweed Cellulose | Thickness | 2.00 ± 0.06 mm | Remained Consistent | In vivo Rat Subcutaneous | [2] |
| Cladophora sp. Seaweed Cellulose | Thickness | 1.70 ± 0.05 mm | Remained Consistent | In vivo Rat Subcutaneous | [2] |
These quantitative metrics are essential for researchers to model and predict scaffold behavior. The steady decline in compressive strength and mass of the BNC-CS-AG-GT hydrogel indicates a controlled degradation profile suitable for applications like bone tissue engineering where gradual load transfer to new tissue is desired [1]. Conversely, the structural stability of the seaweed cellulose scaffolds over an eight-week period suggests their utility in applications requiring longer-term mechanical support [2].
Essential Research Reagents and Materials
The following toolkit outlines critical reagents and materials used in the featured studies for fabricating and evaluating scaffold biocompatibility and biodegradation.
Table 2: The Scientist's Toolkit: Key Reagents and Materials for Scaffold Evaluation
| Reagent / Material | Function & Role in Evaluation | Example from Literature |
|---|---|---|
| Simulated Body Fluid (SBF) | Mimics the ionic composition of human blood plasma for in vitro degradation studies. | Used to study hydrolytic degradation of BNC-CS-AG-GT hydrogels [1]. |
| Lysozyme | An enzyme present in human bodily fluids (e.g., tears, saliva) that enzymatically degrades specific polymers like Chitosan. | Added to SBF to simulate enzymatic, body-fluid-driven degradation [1]. |
| AlamarBlue Assay | A cell viability indicator that uses a redox reaction to measure cell proliferation and cytotoxicity. | Confirmed the non-toxicity of seaweed cellulose (SC) scaffolds in vitro [2]. |
| CaCl₂ (Calcium Chloride) | A cross-linking agent used to form stable, ionic-bridged hydrogel networks with polymers like Alginate. | Used to cross-link BNC-CS-AG-GT scaffolds post-fabrication [1]. |
| Matrigel | A tumor-derived extracellular matrix commonly used for organoid culture, but poses xenogeneic risks. | Discussed as a suboptimal control in liver organoid research, to be replaced by defined biomaterials [3]. |
Standardized Experimental Protocols
To ensure reproducibility and accurate comparison of data across studies, adherence to standardized experimental protocols is paramount. The following sections detail common methodologies for assessing biodegradation and biocompatibility.
In Vitro Biodegradation Protocol
This protocol assesses the degradation profile of scaffolds in a controlled, simulated physiological environment [1].
- Step 1: Scaffold Preparation. Fabricate scaffolds into standardized dimensions (e.g., 5mm diameter cylinders using a biopsy punch). Sterilize the scaffolds, typically via autoclaving at 121°C for 15 minutes [1].
- Step 2: SBF and Lysozyme Preparation. Prepare SBF solution with ions at physiological concentrations (NaCl, NaHCO₃, KCl, CaCl₂, etc.). Supplement the SBF with a defined concentration of lysozyme (e.g., consistent with levels found in human serum) to model enzymatic activity [1].
- Step 3: Incubation and Sampling. Immerse pre-weighed scaffolds in the SBF-lysozyme solution and incubate at 37°C under gentle agitation to simulate body temperature and fluid movement. The study duration should be relevant to the intended application (e.g., up to 8 weeks). Sample the solution at regular intervals [1].
- Step 4: Analysis.
- Mass Loss: At each time point, remove scaffolds, rinse, dry thoroughly, and weigh. Calculate percentage weight loss relative to the initial mass [1].
- Mechanical Properties: Measure compressive strength using a universal testing machine to track the loss of mechanical integrity over time [1].
- Solution Analysis: Analyze the incubation medium for soluble degradation products using assays like HPLC for sugar content and Bradford assay for protein content [1].
In Vitro Biocompatibility and Cytotoxicity Protocol (MC3T3-E1 Cell Line)
This protocol evaluates scaffold toxicity and its ability to support cell growth and function, using the osteoblastic MC3T3-E1 cell line as an example [1].
- Step 1: Scaffold Sterilization and Pre-conditioning. Sterilize scaffolds (e.g., via ethanol immersion or UV irradiation) and equilibrate in cell culture medium.
- Step 2: Cell Seeding. Seed cells directly onto the surface of the scaffolds at a defined density. A control group is typically cultured on standard tissue culture plastic.
- Step 3: Cell Culture. Cultivate the cell-scaffold constructs in an appropriate osteogenic medium, changing the medium regularly. The culture period can extend several weeks to monitor long-term effects.
- Step 4: End-Point Analysis.
- Cell Viability/Cytotoxicity: Use assays like AlamarBlue to quantify metabolic activity as a proxy for cell viability and proliferation [2].
- Cell Differentiation: Measure specific differentiation markers. For osteogenesis, Alkaline Phosphatase (ALP) activity is a key early marker [1].
- Cell Morphology and Adhesion: Use techniques like scanning electron microscopy (SEM) to visualize cell attachment and morphology on the scaffold surface.
- Mineralization: Assess matrix mineralization, a late-stage marker of osteogenic differentiation, using stains like Alizarin Red S [1].
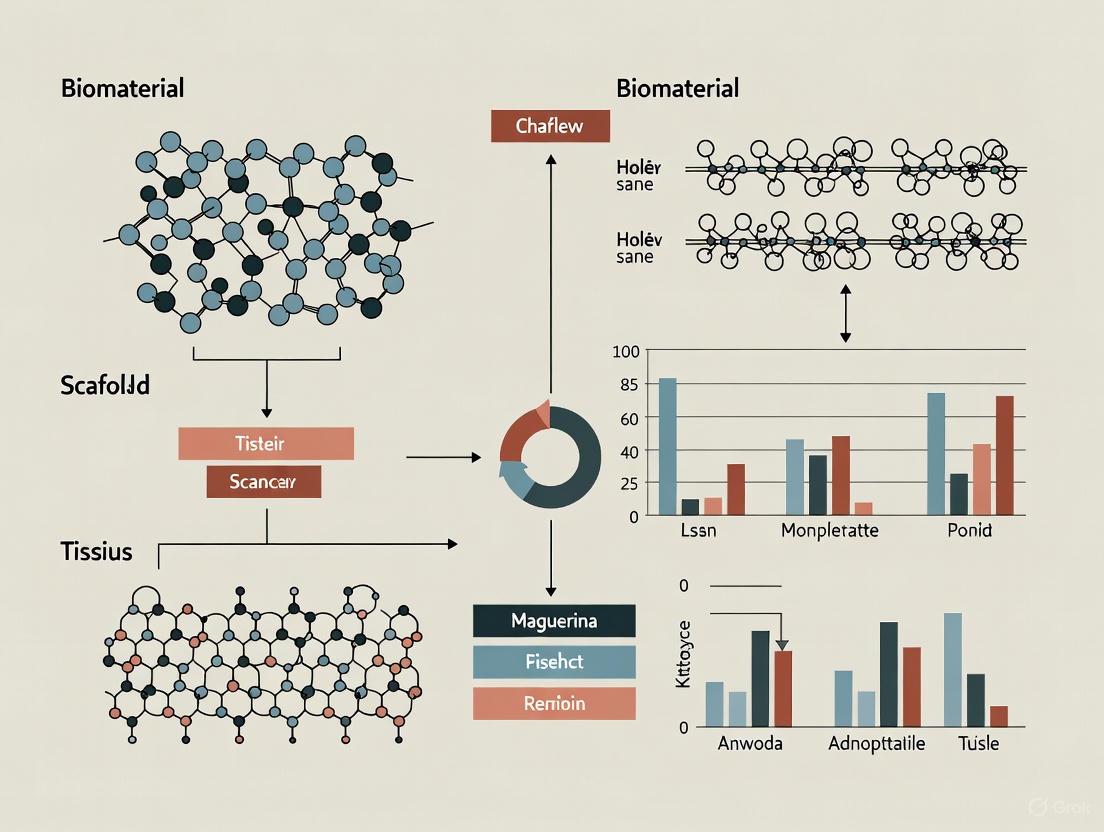
The experimental workflow for these assessments is visualized below.
Material Innovations and Case Studies
Composite Hydrogels: BNC-CS-AG-GT
Bacterial Nanocellulose (BNC) possesses excellent mechanical strength but suffers from limited innate biodegradability in the human body. To overcome this, a composite hydrogel integrating BNC with Chitosan (CS), Alginate (AG), and Gelatin (GT) was developed [1]. In this design:
- BNC provides the nanofibrillar structural reinforcement.
- CS enhances biodegradability (via lysozyme degradation) and introduces antibacterial properties.
- AG enables ionic cross-linking with Ca²⁺ for hydrogel stability.
- GT improves cell adhesion through its RGD peptide sequences [1].
This multi-material approach successfully created a scaffold with a compressive strength of ~68 MPa, which degraded gradually in SBF with lysozyme, losing 54% of its mass over 8 weeks while supporting osteoblast adhesion, proliferation, and differentiation without cytotoxicity [1].
Seaweed-Derived Cellulose Scaffolds
Seaweed cellulose (SC) presents a sustainable and lignin-free alternative to plant-derived cellulose, simplifying extraction [2]. Studies comparing SC from Ulva sp. (porous architecture) and Cladophora sp. (fibrous architecture) revealed how scaffold microstructure dictates the in vivo host response in a rat subcutaneous implantation model [2]:
- Ulva sp. (Porous): Promoted compartmentalized healing with distributed vascularized connective tissue.
- Cladophora sp. (Fibrous): Supported stratified tissue organization with aligned collagen deposition.
Both scaffolds showed minimal FBR, successful integration, and progressive vascularization over eight weeks, highlighting that biocompatibility is not only a chemical but also a structural property [2].
The distinct host responses elicited by different scaffold architectures are summarized below.
Biocompatibility and biodegradability are not standalone properties but are deeply interconnected, forming the non-negotiable foundation for the safe and successful integration of biomaterial scaffolds. As the field progresses, future work will focus on developing "smarter" biomaterials with precisely tunable degradation rates and bioactive surfaces that can actively direct cellular processes. The shift towards sustainable sources, such as seaweed-derived cellulose, further highlights the growing importance of eco-design in biomedical materials [2]. The ongoing challenge is to seamlessly integrate these advanced materials into complex, functional tissues, a goal that demands continued collaboration across materials science, cell biology, and clinical medicine.
In the field of tissue engineering and regenerative medicine (TERM), the ultimate goal is to develop biological substitutes that restore, maintain, or improve tissue function. Central to this endeavor is the design of biomaterial scaffolds that faithfully replicate the native tissue environment. The term "biomimicry" was first described by Otto Schmitt in 1957 and has since evolved to encompass various strategies for imitating nature's solutions [4]. In TERM, successful biomimicry requires a multifaceted approach that addresses three critical aspects: mechanical properties (matching tissue stiffness and strength), morphological properties (recreating architectural features), and biological properties (recreating the biochemical microenvironment) [4]. This technical guide focuses specifically on the mechanical and structural dimensions of biomimicry, examining how scaffolds can be engineered to withstand physiological loads while providing appropriate architectural cues that direct cellular behavior and tissue formation.
The consequences of failing to mimic native mechanical and structural properties can be severe. Mechanical mismatches between implants and native tissues often lead to graft failure, stress shielding, and improper mechanotransduction, where cells receive incorrect mechanical cues that steer them toward undesirable fates [4]. Similarly, inadequate structural design can inhibit cell infiltration, vascularization, and nutrient waste exchange, ultimately compromising tissue integration and regeneration. As such, a deep understanding of native tissue biomechanics and architecture provides the essential foundation for designing effective tissue engineering scaffolds.
Native Tissue Biomechanics: A Quantitative Framework for Biomimicry
Native tissues exhibit remarkable diversity in their mechanical properties, spanning several orders of magnitude in stiffness and strength. These properties are precisely tuned to withstand the specific physiological loads each tissue experiences daily. Table 1 summarizes the mechanical properties of key human tissues, providing critical target values for scaffold design.
Table 1: Mechanical Properties of Native Human Tissues
| Tissue Type | Elastic/Young's Modulus | Ultimate Tensile Strength | Key Mechanical Characteristics |
|---|---|---|---|
| Cortical Bone | 19.3 GPa [4] | 50-150 MPa (highly variable) | High stiffness, compressive strength |
| Hyaline Cartilage | 0.2-0.8 MPa [5] | 4-40 MPa (region-dependent) | Compressive resilience, low friction |
| Meniscus | 0.182 MPa (bovine, compressive) [6] | Varies by direction | Anisotropic, tension-resistant |
| Skin | 0.1-16 kPa [4] | 5-30 MPa | Highly elastic, viscoelastic |
| Bladder | Variable | N/A | Dynamic, elastic |
These mechanical properties are not arbitrary; they play crucial roles in tissue development, homeostasis, and function. For example, the meniscus exhibits anisotropic mechanical behavior due to its specialized collagen architecture, with the equilibrium modulus significantly higher in the circumferential direction than in the radial direction [6]. This anisotropy enables the meniscus to effectively convert compressive tibiofemoral forces into tensile hoop stresses, which are efficiently managed by the circumferentially aligned collagen fibers. Similarly, bone's exceptional stiffness enables weight-bearing capabilities, while skin's elasticity allows for stretching and recovery. These structure-function relationships must guide the design of tissue-engineered constructs.
Experimental Methodologies for Characterizing Mechanical and Structural Properties
Rigorous characterization of both native tissues and engineered scaffolds is essential for effective biomimicry. The following experimental protocols provide standardized methodologies for assessing key mechanical and structural parameters.
Mechanical Testing Protocols
Uniaxial Tensile Testing:
- Purpose: To determine elastic modulus, ultimate tensile strength, and strain-to-failure of scaffold materials.
- Sample Preparation: Prepare rectangular specimens (e.g., 30mm × 10mm × thickness) according to ASTM D638. Hydrate samples in physiological solution for 24 hours prior to testing.
- Protocol: Mount samples in mechanical testing system with pneumatic or manual grips. Apply pre-load of 0.01N to ensure proper alignment. Conduct test at strain rate of 1% per minute until failure. Record force and displacement data at 100Hz sampling rate.
- Data Analysis: Calculate engineering stress (force/initial cross-sectional area) and engineering strain (change in length/original length). Determine elastic modulus from the linear region of the stress-strain curve (typically 0-10% strain).
Unconfined Compression Testing:
- Purpose: To evaluate compressive modulus and stress relaxation behavior, particularly for cartilaginous tissues.
- Sample Preparation: Prepare cylindrical specimens (e.g., 5mm diameter × 2mm height). Maintain hydration throughout preparation and testing.
- Protocol: Place sample between impermeable platens. Apply 5% strain at rate of 0.5% per second, then hold for 30 minutes to reach equilibrium. Record force data throughout.
- Data Analysis: Calculate equilibrium modulus from equilibrium stress divided by applied strain. Calculate stress relaxation percentage as (peak stress - equilibrium stress)/peak stress × 100%.
Structural Characterization Techniques
Scanning Electron Microscopy (SEM) for Pore Architecture:
- Purpose: To visualize and quantify scaffold porosity, pore size, and interconnectivity.
- Sample Preparation: Dehydrate scaffolds through graded ethanol series (50%, 70%, 90%, 100%), critical point dry, and sputter-coat with gold/palladium.
- Protocol: Image samples at multiple magnifications (50X-5000X) under appropriate accelerating voltage (5-15kV). Capture images from at least three different regions per sample.
- Data Analysis: Use image analysis software (e.g., ImageJ) to measure pore size distribution, strut thickness, and porosity percentage. Calculate interconnectivity by analyzing pore throat sizes.
Histological Analysis for Tissue Integration:
- Purpose: To assess cell distribution, extracellular matrix production, and tissue-scaffold integration.
- Sample Preparation: Fix constructs in 4% paraformaldehyde for 24 hours, dehydrate, and embed in paraffin. Section at 5-10μm thickness.
- Protocol: Deparaffinize and rehydrate sections. Perform staining (H&E for cell distribution, Safranin-O for proteoglycans, Masson's Trichrome for collagen). Image using brightfield microscopy.
- Data Analysis: Use established scoring systems (e.g., International Cartilage Repair Society grading system) for semi-quantitative assessment [5]. For quantitative analysis, measure staining intensity, cell number per area, and tissue infiltration depth.
Table 2: Advanced Characterization Techniques for Scaffold Evaluation
| Technique | Primary Application | Key Parameters Measured | Considerations |
|---|---|---|---|
| Micro-Computed Tomography (μCT) | 3D pore architecture | Porosity, pore size distribution, interconnectivity, scaffold degradation | Requires density contrast; may need staining for polymer scaffolds |
| Atomic Force Microscopy (AFM) | Nanoscale mechanical properties | Local stiffness, surface roughness, adhesion properties | Time-consuming; provides high spatial resolution |
| Confocal Microscopy | 3D cell distribution and viability | Cell infiltration, spatial organization, viability in thick constructs | Requires fluorescent labeling; limited penetration depth |
| Finite Element Analysis (FEA) | Computational modeling of mechanical behavior | Stress/strain distributions, prediction of failure points | Dependent on accurate material properties and boundary conditions |
Engineering Strategies for Mechanical and Structural Biomimicry
Material Selection and Composite Design
The choice of base material fundamentally influences scaffold mechanical properties. Synthetic polymers like poly(ε-caprolactone) [PCL] offer tunable degradation rates and high initial strength, making them suitable for load-bearing applications [4]. For example, PCL reinforced with Zein and gum Arabic in electrospun meshes achieved tensile strengths up to 2.9 MPa, appropriate for skin regeneration [4]. Natural polymers like collagen and elastin provide inherent bioactivity but often require reinforcement to achieve adequate mechanical properties. Janke et al. demonstrated that adding poly(L-lactide-co-ɛ-caprolactone) [PLCL] to collagen type I scaffolds increased ultimate tensile strength from 1.8 ± 0.8 kPa to 160 ± 20 kPa, achieving the J-shaped stress-strain curve characteristic of many native soft tissues [4].
Composite materials have emerged as particularly promising strategies for reconciling the often-conflicting demands of mechanical strength and bioactivity. For instance, hydroxyapatite (HA)/chitosan nanocomposites combine the osteoconductivity of HA with the processability of chitosan, creating scaffolds with enhanced compressive strength for bone tissue engineering [7]. Similarly, incorporating reduced graphene oxide (rGO) into polymer matrices can significantly improve electrical conductivity while maintaining mechanical integrity, which is crucial for engineering electrically responsive tissues like cardiac muscle [4].
Porosity Design and Architectural Control
Porosity represents a critical design parameter that simultaneously influences both mechanical and biological performance. An optimal pore architecture must balance sufficient porosity for cell infiltration and nutrient diffusion (typically >80% for many tissues) with preserved mechanical integrity [8]. Table 3 summarizes target pore sizes for various tissue engineering applications.
Table 3: Target Pore Sizes for Tissue-Specific Scaffold Design
| Tissue Type | Optimal Pore Size Range | Primary Rationale |
|---|---|---|
| Bone | 200-350 μm [7] | Facilitates vascularization and osteoconduction |
| Cartilage | 100-200 μm | Supports chondrocyte migration and ECM production |
| Skin | 50-150 μm | Promotes fibroblast infiltration and keratinocyte migration |
| Nerve | 10-100 μm | Guides axonal extension and Schwann cell migration |
| Vascular | 50-200 μm (with hierarchical design) | Enables endothelialization and mechanical compliance |
Advanced manufacturing technologies now enable unprecedented control over pore architecture. 3D bioprinting allows for precise spatial patterning of multiple materials and cells, creating scaffolds with region-specific mechanical properties that mimic tissue interfaces like the osteochondral junction [8]. Freeze-drying (lyophilization) techniques can produce highly interconnected porous networks by controlling ice crystal formation during freezing; lower temperatures typically yield denser, more compact structures with smaller pores, while higher temperatures create larger, more open architectures [7]. Electrospinning generates nanofibrous scaffolds that closely mimic the native extracellular matrix's fibrous architecture, with fiber alignment providing contact guidance for cell orientation and tissue organization [6].
Convergence Strategies for Complex Tissue Mimicry
The most successful approaches for replicating complex tissues often combine multiple fabrication techniques. For the knee meniscus, which features circumferentially oriented collagen fibers (600nm diameter) interwoven with radial tie-fibers, convergent manufacturing strategies have shown particular promise [6]. For example, combining electrospinning to replicate the nanofibrous micro-architecture with 3D printing to create the macroscopic wedge-shaped structure enables better recapitulation of the meniscus's hierarchical organization. Similarly, decellularized ECM scaffolds preserve the native tissue's complex ultrastructure and biochemical composition while providing a biomechanically competent template for cell repopulation [6].
These convergent approaches acknowledge that tissues are not homogeneous but exhibit spatial variations in composition, architecture, and mechanical properties. The meniscus, for instance, demonstrates regional variations in proteoglycan content, with higher concentrations in the inner regions where compressive forces predominate [6]. Successfully mimicking such complexity requires designing scaffolds with graded mechanical properties and heterogeneous pore architectures that mirror this native spatial organization.
Computational Modeling in Scaffold Design
Computational approaches have become indispensable tools for optimizing scaffold design before fabrication. Finite Element Analysis (FEA) enables prediction of stress distributions throughout scaffold architectures under physiological loading conditions, identifying potential failure points and guiding structural reinforcement [8]. For example, FEA can model how different pore geometries (e.g., hexagonal vs. rectangular) influence stress concentration factors in bone scaffolds, enabling data-driven design decisions.
Modern modeling approaches also incorporate fluid-structure interactions to simulate nutrient transport and waste removal through porous networks, predicting regions potentially limited by diffusion constraints. These computational models can be coupled with cell behavior algorithms that predict how mechanical cues (substrate stiffness, fluid shear stress) influence cell migration, proliferation, and differentiation, creating comprehensive in silico testing platforms for scaffold optimization [8].
The following diagram illustrates the integrated computational-experimental workflow for scaffold design and validation:
Scaffold Design Workflow: This diagram illustrates the iterative process of designing and validating tissue engineering scaffolds, integrating computational modeling with experimental validation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the methodologies described in this guide requires specific reagents and equipment. The following table catalogues essential research tools for developing and characterizing biomimetic scaffolds.
Table 4: Essential Research Reagents and Materials for Scaffold Development
| Category/Item | Specific Examples | Primary Function/Application |
|---|---|---|
| Base Polymers | Poly(ε-caprolactone) [PCL], Polylactic acid [PLA], Gelatin methacryloyl [GelMA], Collagen type I | Scaffold matrix material providing structural integrity and biocompatibility |
| Crosslinkers | 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide [EDAC], Genipin, Methacrylic anhydride | Enhance mechanical properties through chemical bonding of polymer chains |
| Bioactive Additives | Hydroxyapatite [HA], Bone morphogenetic protein-2 [BMP-2], RGD peptide, Reduced graphene oxide [rGO] | Enhance osteoconduction, specific differentiation, cell adhesion, or electrical conductivity |
| Characterization Reagents | Safranin-O, Hematoxylin & Eosin, Alcian blue, Alizarin red | Histological staining for proteoglycans, cell nuclei, glycosaminoglycans, and mineralization |
| Fabrication Equipment | 3D bioprinter, Electrospinning apparatus, Freeze-dryer | Scaffold fabrication with controlled architecture and porosity |
Mimicking the mechanical and structural properties of native tissue remains a fundamental challenge in tissue engineering, but continued advances in materials science, manufacturing technologies, and characterization methodologies are steadily closing the gap. The emerging paradigm recognizes that successful biomimicry requires integrated approaches that simultaneously address mechanical, structural, and biological cues in a spatially coordinated manner.
Future progress will likely be driven by several key developments. Stimuli-responsive biomaterials that dynamically alter their mechanical properties in response to physiological cues or external triggers could better mimic the adaptive nature of living tissues. Multi-material bioprinting technologies with increasingly fine resolution will enable more faithful replication of tissue interfaces and spatial heterogeneity. Advanced characterization techniques, particularly in vivo monitoring methods, will provide richer understanding of how scaffolds perform under physiological conditions. Finally, machine learning algorithms are poised to revolutionize scaffold design by identifying non-intuitive structure-property relationships and optimizing complex, multi-parameter design spaces [8].
As these technologies mature, the field moves closer to the ultimate goal of creating tissue-engineered constructs that seamlessly integrate with native tissues, providing functional restoration that persists for the long term. By maintaining a rigorous focus on mimicking both the mechanical and structural properties of native tissues, researchers can develop increasingly sophisticated solutions to the challenging problems of tissue loss and organ failure.
The field of tissue engineering has undergone a profound transformation, evolving from the development of passive, structural scaffolds to the engineering of sophisticated "smart" platforms that actively and precisely interface with biological systems to orchestrate therapeutic outcomes [9]. This evolution represents a fundamental paradigm shift, fueled by convergence of breakthroughs in materials science, immunology, and bioengineering. Where first-generation biomaterials were designed primarily for structural support with minimal biological interaction, contemporary approaches embrace bioactive and stimuli-responsive systems capable of dynamic biological regulation. This transition acknowledges the immune system not as an adversary to be evaded, but as a powerful biological system that can be rationally programmed and harnessed for therapeutic benefit, particularly through strategic manipulation of macrophage polarization and other immune mechanisms [9].
The "intelligence" ascribed to smart biomaterials is fundamentally rooted in their engineered capacity to sense specific alterations in their surrounding environment and respond to these changes in a predetermined, functional manner [9]. These advanced systems are transforming the landscape of tissue engineering by effectively addressing various regenerative clinical challenges across cardiology, orthopedics, and neural tissue regeneration [10]. By combining the advantageous properties of metals, polymers, and ceramics, hybrid scaffolds surpass limitations associated with single-material constructs, enabling advanced applications in biomimetics, wound healing, targeted drug delivery, and even tumor therapy [10]. This technical guide explores the fundamental principles, design considerations, and methodological approaches for incorporating bioactivity and smart functionality into biomaterial scaffolds for tissue engineering applications.
Classification and Evolution of Biomaterial Scaffolds
The classification of biomaterials reflects an increasing level of sophistication in their interaction with biological systems, essentially mirroring an evolution in their biomimetic capabilities [9]. This progression highlights a journey from static implants to dynamic, self-adaptive platforms, with each category representing distinct characteristics and functionalities.
Table 1: Classification Levels of Biomaterial Scaffolds
| Classification | Key Characteristics | Primary Functions | Representative Examples |
|---|---|---|---|
| Inert Materials | Minimal biological interaction; designed primarily for structural support | Mechanical support; space occupation | Titanium alloys; inert ceramics; certain polymers [9] |
| Active Materials (Bioactive) | Elicit defined biological response at material-tissue interface | Release of pre-loaded bioactive agents; surface-mediated cellular interactions | Drug-eluting stents; antibiotic-loaded bone cements; hydroxyapatite coatings [9] |
| Responsive Materials | Sense and respond to specific environmental stimuli (pH, temperature, enzymes) | On-demand drug release; structural transformation in response to pathological cues | pH-sensitive hydrogels; temperature-responsive polymers like PNIPAM; enzyme-degradable matrices [9] |
| Autonomous Materials | Bi-directional responsiveness; sense, respond, and adapt based on feedback | Create adaptive, interactive systems that mimic homeostatic feedback loops | Materials that receive cellular feedback and remodel accordingly; 4D printed structures [9] |
The trajectory from inert to autonomous systems embodies the conceptual pivot in biomaterial design. While inert materials often trigger a foreign body response culminating in fibrous capsule formation, advanced smart materials aim to actively modulate this response, engaging with immune components like macrophages to skillfully guide their behavior toward pro-regenerative, anti-inflammatory phenotypes [9]. This strategic manipulation creates local microenvironments conducive to constructive tissue repair and functional restoration, rather than destructive inflammation or scarring.
Critical Design Parameters for Smart Scaffolds
Architectural and Biomechanical Considerations
The architectural design of scaffolds represents a critical determinant of their biological performance and integration with host tissues. Several key parameters must be optimized during the design process:
Porosity and Pore Size: Porosity significantly influences cell migration, nutrient diffusion, and vascularization. Optimal pore sizes vary by tissue type: typically 100-350μm for bone regeneration, 20-150μm for skin regeneration, and smaller dimensions for neural applications [10]. Interconnected pore networks are essential for uniform cell distribution and tissue formation.
Biomechanical Compatibility: Scaffolds must match the mechanical properties of native tissues to avoid stress shielding or mechanical failure. Critical parameters include compressive modulus (bone: 0.1-20 GPa; cartilage: 0.1-1 MPa), tensile strength, and fatigue resistance. Hybrid scaffolds combining metals, polymers, and ceramics offer enhanced mechanical integrity over single-material constructs [10].
Degradation Kinetics: The degradation rate should synchronize with tissue regeneration pace. Materials can be engineered with specific hydrolysis rates, enzymatic sensitivity, or responsive cleavage mechanisms. Monitoring includes mass loss over time (typically weeks to months) and molecular weight reduction [10].
Bioactivity and Signaling Incorporation
Bioactivity in scaffolds extends beyond basic structural support to encompass deliberate interactions with biological systems:
Chemical Bioactivity: Surface functionalization with specific peptide sequences (e.g., RGD for cell adhesion) or mineral components (e.g., hydroxyapatite for osteoconduction) enhances cellular interactions and tissue-specific differentiation.
Physical Bioactivity: Topographical features at micro- and nano-scales (grooves, pits, fibers) influence cell morphology, alignment, and gene expression through contact guidance mechanisms [10].
Biological Signaling: Controlled delivery of growth factors (BMP-2 for bone, VEGF for vasculature, NGF for nerves) at physiological concentrations (typically ng to μg per mg scaffold) directs cellular processes and tissue maturation.
Stimuli-Responsive Mechanisms in Smart Scaffolds
Stimuli-responsive biomaterials represent a cornerstone of smart functionality, enabling precise spatiotemporal control over scaffold behavior and therapeutic delivery. These systems exploit specific environmental triggers to initiate predetermined responses.
Table 2: Stimuli-Responsive Mechanisms in Smart Biomaterials
| Stimulus Type | Response Mechanism | Applications | Key Material Systems |
|---|---|---|---|
| pH-Responsive | Ionizable groups protonate/deprotonate; pH-labile bonds cleave | Drug delivery in acidic tumor microenvironments (pH 6.5-6.9) or inflammatory sites | Polymers with carboxylic, amine groups; hydrazone, acetal, orthoester linkages [9] |
| Temperature-Responsive | Polymer chains undergo conformational changes at LCST/UCST | Injectable depot systems; thermally-activated drug release | Poly(N-isopropylacrylamide) (PNIPAM); Pluronics; chitosan/glycerophosphate [9] |
| Enzyme-Responsive | Specific enzyme recognition and cleavage of substrate motifs | Targeted drug release in disease sites with elevated enzyme expression (MMPs in cancer, chronic wounds) | Peptide-crosslinked hydrogels; hyaluronic acid-based systems [9] |
| Magnetic-Responsive | Particle alignment or heat generation under alternating magnetic fields | Remote-controlled drug release; hyperthermia therapy | Superparamagnetic Fe₃O₄ nanoparticles; paramagnetic MnOx composites [9] |
The development of multi-stimuli responsive systems represents a growing frontier in smart biomaterials. For instance, Chen et al. developed a triple-functional stimulus-responsive nanosystem based on superparamagnetic Fe₃O₄ and paramagnetic MnOx nanoparticles co-integrated onto exfoliated graphene oxide nanosheets using a novel double redox strategy [9]. This system achieved high drug loading capacity and pH-responsive drug release performance, demonstrating the potential of combinatorial approaches.
Diagram 1: Stimuli-Responsive Mechanism Workflow in Smart Biomaterials
Advanced Fabrication Technologies: 3D and 4D Bioprinting
The fabrication of complex, functional scaffolds has been revolutionized by additive manufacturing technologies. Three-dimensional (3D) bioprinting advances have enabled the creation of in vitro models for drug testing and therapeutic efficiency evaluation with unprecedented physiological relevance [10]. Key technological approaches include:
Extrusion-Based Bioprinting: Utilizes pneumatic or mechanical dispensing systems to deposit bioinks in layer-by-layer fashion. Optimal parameters include printing pressures (15-80 kPa), nozzle diameters (100-400μm), and printing speeds (5-20 mm/s) tailored to material viscosity and cell viability requirements.
Stereolithography (SLA): Employs UV light to photopolymerize liquid resins in precise patterns. Achieves high resolution (25-100μm) using photoinitiators (Irgacure 2959, LAP) at concentrations of 0.1-1.0% w/v with exposure times of 5-30 seconds per layer.
Digital Light Processing (DLP): Projects entire layers simultaneously for faster printing speeds. Utilizes similar photochemistry to SLA but with reduced printing times, though with potential trade-offs in resolution.
The emergence of 4D printing introduces the critical dimension of time, creating dynamic structures that evolve post-fabrication [10]. This is achieved primarily through shape memory polymers (SMPs) that can be programmed to undergo predictable morphological changes in response to specific stimuli. The 4D printing process involves: (1) Creating a 3D structure from SMPs or other responsive materials; (2) Programming the temporary shape through mechanical deformation above transition temperature; (3) Fixing the temporary shape by cooling below transition temperature; (4) Triggering shape recovery through application of stimulus (heat, light, solvent). This capability allows scaffolds to mimic the complex and dynamic properties of living tissues, responding to various physiological cues with precision timing [10].
Experimental Protocols for Smart Scaffold Evaluation
Protocol for Synthesis of pH-Responsive Hybrid Scaffold
This protocol describes the synthesis and characterization of a pH-responsive hybrid scaffold system for controlled drug delivery in wound healing applications, adapted from methodologies analyzed in the SMART Protocols guidelines [11].
Materials and Reagents:
- Alginate (high G-content, Sigma-Aldrich, Catalog #W201502)
- Gelatin Type A (300 Bloom, Sigma-Aldrich, Catalog #G2500)
- Chlorogenic acid (Sigma-Aldrich, Catalog #C3878)
- 1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC, Thermo Fisher, Catalog #PG82079)
- N-Hydroxysuccinimide (NHS, Thermo Fisher, Catalog #24510)
- Calcium chloride dihydrate (CaCl₂·2H₂O, Sigma-Aldrich, Catalog #C7902)
- Phosphate Buffered Saline (PBS, pH 7.4, Thermo Fisher, Catalog #BP24384)
- MES buffer (0.1 M, pH 6.0, Thermo Fisher, Catalog #BP30068)
- Deionized water (18.2 MΩ·cm resistivity)
Equipment:
- Syringe pump (Cole-Parmer, Model #78-0100C)
- Freeze dryer (VirTis, Model #GenesisSQ)
- UV-Vis Spectrophotometer (Shimadzu, Model #UV-2600)
- Scanning Electron Microscope (Hitachi, Model #SU3900)
- Mechanical tester (Instron, Model #5943)
Procedure:
Polymer Functionalization:
- Prepare 2% w/v alginate solution in MES buffer (0.1 M, pH 6.0)
- Dissolve chlorogenic acid (CA) in DMSO at 50 mg/mL
- Add EDC (20 mM final concentration) and NHS (10 mM final concentration) to alginate solution
- Add CA solution at 1:0.1 alginate:CA molar ratio
- React for 12 hours at room temperature with continuous stirring (200 rpm)
- Dialyze against deionized water for 48 hours (MWCO 12-14 kDa)
- Lyophilize for 72 hours to obtain CA-functionalized alginate
Scaffold Fabrication:
- Prepare 3% w/v solution of CA-alginate and 5% w/v gelatin in PBS at 60°C
- Mix polymers at 1:1 volume ratio with model drug (e.g., vancomycin at 2 mg/mL)
- Transfer to syringe and maintain at 37°C
- Extrude solution into CaCl₂ crosslinking bath (2% w/v) using syringe pump at 5 mL/h
- Maintain scaffolds in crosslinking solution for 24 hours at 4°C
- Rinse with PBS and store at 4°C until use
Characterization:
- Morphological Analysis: Image by SEM at 10 kV acceleration voltage after gold sputtering. Measure pore size using ImageJ software (n=50 measurements).
- Swelling Studies: Weigh dry scaffolds (Wd), incubate in PBS at pH 7.4 and 5.5 at 37°C. Remove at time points, blot excess liquid, weigh (Ww). Calculate swelling ratio as (Ww - Wd)/Wd.
- Drug Release: Place scaffolds in release medium (PBS, pH 7.4 or 5.5) at 37°C with shaking (50 rpm). Withdraw aliquots at predetermined times, analyze by HPLC or UV-Vis. Replace with fresh medium to maintain sink conditions.
Troubleshooting:
- Poor Crosslinking: Ensure CaCl₂ solution is freshly prepared. Increase crosslinking time to 36 hours.
- Irregular Pores: Optimize extrusion rate (3-7 mL/h range) and nozzle diameter (200-400μm).
- Incomplete Drug Release: Verify drug solubility and consider adding surfactants (0.1% Tween-80) to release medium.
Protocol for Evaluating Macrophage Polarization Response
This protocol assesses the immunomodulatory potential of smart scaffolds through macrophage polarization studies, critical for evaluating pro-regenerative microenvironment formation [9].
Materials and Reagents:
- RAW 264.7 macrophage cell line (ATCC, Catalog #TIB-71)
- DMEM culture medium (Thermo Fisher, Catalog #11995065)
- Fetal Bovine Serum (FBS, Thermo Fisher, Catalog #26140079)
- Penicillin-Streptomycin (Thermo Fisher, Catalog #15140122)
- Lipopolysaccharide (LPS, Sigma-Aldrich, Catalog #L4391)
- IL-4 (PeproTech, Catalog #214-14)
- IL-10 (PeproTech, Catalog #210-10)
- IFN-γ (PeproTech, Catalog #315-05)
- Antibodies for flow cytometry: CD86-FITC, CD206-PE, iNOS-APC
- RNA extraction kit (Qiagen, Catalog #74104)
- cDNA synthesis kit (Thermo Fisher, Catalog #4368813)
- qPCR reagents (Thermo Fisher, Catalog #4309155)
Procedure:
Scaffold Sterilization and Conditioning:
- Sterilize scaffolds (5mm diameter × 2mm thickness) in 70% ethanol for 30 minutes
- UV irradiate both sides for 15 minutes each
- Pre-condition in complete DMEM for 24 hours at 37°C
Cell Seeding and Culture:
- Seed RAW 264.7 cells at 1×10⁵ cells/scaffold in 48-well plates
- Allow attachment for 6 hours, then add fresh medium
- For polarization studies, after 24 hours, add:
- M1 polarization: LPS (100 ng/mL) + IFN-γ (20 ng/mL)
- M2 polarization: IL-4 (20 ng/mL) + IL-10 (20 ng/mL)
- Culture for 48 hours with treatments
Flow Cytometry Analysis:
- Harvest cells using gentle scraping
- Wash with PBS and stain with surface antibodies (CD86, CD206) for 30 minutes at 4°C
- For intracellular staining (iNOS), fix and permeabilize cells prior to antibody incubation
- Analyze using flow cytometer, collect 10,000 events per sample
- Calculate polarization ratios as (M2 markers)/(M1 markers)
Gene Expression Analysis:
- Extract total RNA using commercial kit
- Synthesize cDNA using 1μg RNA template
- Perform qPCR with primers for M1 markers (TNF-α, IL-1β, iNOS) and M2 markers (Arg-1, IL-10, TGF-β)
- Calculate relative expression using 2^(-ΔΔCt) method with GAPDH as reference
Statistical Analysis:
- Perform experiments in triplicate with three independent replicates (n=9)
- Analyze data using one-way ANOVA with Tukey's post-hoc test
- Consider p<0.05 statistically significant
- Report data as mean ± standard deviation
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and evaluation of smart biomaterial scaffolds requires specialized reagents and materials with specific functional attributes. The following table catalogs essential components for research in this field.
Table 3: Research Reagent Solutions for Smart Biomaterial Development
| Reagent/Material | Function and Utility | Key Characteristics | Example Applications |
|---|---|---|---|
| Stimuli-Responsive Polymers | Provide sensing and response capabilities to environmental cues | Defined transition temperatures; specific cleavage sites; tunable sensitivity | PNIPAM (temperature); poly(β-amino esters) (pH); MMP-cleavable peptides (enzyme) [9] |
| Crosslinking Agents | Enable controlled scaffold formation and mechanical properties | Controlled reactivity; biocompatible byproducts; selective functionality | EDC/NHS (carboxyl-amine); genipin (natural alternative); glutaraldehyde (high efficiency) [11] |
| Bioactive Signaling Molecules | Direct cellular responses and tissue regeneration | Specific receptor binding; appropriate half-life; controlled release kinetics | Growth factors (BMP-2, VEGF, TGF-β); cytokines (IL-4, IL-10); chemokines [9] |
| Characterization Standards | Enable quantitative assessment of scaffold properties | Certified reference materials; standardized protocols; traceable values | GPC standards (molecular weight); NIST reference materials (mechanical properties) [11] |
| Cell Culture Assays | Evaluate biological responses to scaffold materials | Reproducible; quantitative; physiologically relevant | Macrophage polarization kits; metabolic activity assays (MTT, AlamarBlue); differentiation markers [9] |
Signaling Pathways in Smart Scaffold-Tissue Interactions
Smart biomaterials interact with biological systems through specific signaling pathways that ultimately dictate therapeutic outcomes. Understanding these pathways is essential for rational biomaterial design.
Diagram 2: Signaling Pathways in Smart Scaffold-Mediated Tissue Regeneration
The interaction between smart scaffolds and immune cells, particularly macrophages, creates a critical signaling network that determines regeneration success. Scaffold properties (physical cues, controlled drug release, surface topography, mechanical properties) directly influence macrophage polarization toward either pro-inflammatory M1 or pro-regenerative M2 phenotypes [9]. These phenotypes then activate specific signaling pathways: M1 macrophages typically activate NF-κB pathway promoting inflammation, while M2 macrophages preferentially activate STAT and TGF-β/Smad pathways associated with tissue repair [9]. The ultimate balance of these signaling cascades determines functional outcomes including angiogenesis, matrix deposition, and tissue remodeling.
The incorporation of bioactivity and smart functionality represents the frontier of biomaterial scaffold development, transforming passive frameworks into dynamic, regenerative environments. Advances in smart hybrid scaffolds are already revolutionizing approaches to drug delivery, wound healing, and tumor therapy, while 3D bioprinting technologies are producing increasingly sophisticated in vitro models for drug testing and therapeutic evaluation [10]. The strategic integration of stimuli-responsive mechanisms through 4D printing and shape memory polymers enables scaffolds to mimic the complex and dynamic properties of living tissues, responding to various physiological cues with unprecedented precision [10].
Future developments in this field point toward several transformative directions. Precision immune engineering will leverage increasingly sophisticated biomaterial systems to orchestrate specific immune responses tailored to individual patient needs and specific tissue contexts [9]. The integration of artificial intelligence-driven design approaches will accelerate the rational development of next-generation scaffolds, optimizing complex parameter combinations that would be impractical to explore through traditional experimental approaches alone [9]. Additionally, the convergence of biomaterial science with emerging technologies such as optogenetic control and multimodal therapeutic strategies will further blur the distinctions between medical devices and pharmacological interventions, creating truly integrated diagnostic-therapeutic systems.
As the field progresses, addressing challenges in biosafety, scalable manufacturing, and regulatory approval will be essential for successful clinical translation [9]. However, the continued evolution of smart biomaterials promises to pioneer new paradigms in precision immune engineering, offering transformative strategies for regenerative medicine and disease intervention that fundamentally exceed the capabilities of passive framework approaches.
The extracellular matrix (ECM) represents a highly sophisticated biological framework that transcends its conventional role as a passive structural scaffold [12]. Comprising a dynamic network of proteins, glycosaminoglycans, and signaling molecules, the ECM actively orchestrates fundamental cellular processes—including adhesion, migration, proliferation, and differentiation—through integrated biomechanical and biochemical cues [12]. This regulatory capacity arises from its tissue-specific composition and architecture, making it indispensable for physiological homeostasis and a critical blueprint for biomaterial design in regenerative medicine [12]. The rising global burden of chronic wounds, degenerative diseases, and organ failure has intensified the demand for advanced therapeutic strategies that address the limitations of conventional treatments [12]. While current biomaterials often fail to recapitulate the ECM's dynamic reciprocity with cells—leading to suboptimal outcomes such as fibrosis or functional deficits—recent innovations have yielded ECM-inspired platforms with enhanced biomimicry [12].
Central to the ECM's therapeutic relevance is its dual role in tissue repair: as a structural scaffold and a signaling hub. Following injury, it directs hemostasis, inflammation, proliferation, and remodeling by spatially coordinating cellular responses [12]. Key components like fibronectin and collagen engage integrin receptors, activating downstream pathways to drive migration while sequestered growth factors (e.g., TGF-β, PDGF) are released to modulate proliferation [12]. This synchronized regulation of adhesion, motility, and cell cycle progression creates an optimized microenvironment for regeneration [12]. Despite these advances, critical translational challenges persist. Gaps remain in understanding how engineered ECM analogs influence regenerative outcomes, particularly in mimicking dynamic remodeling [12]. Immune responses, mechanical mismatches, and inadequate vascularization further complicate clinical implementation [12]. This review systematically examines ECM biology and its biomaterial applications, analyzing: (i) structure-function relationships governing cell fate; (ii) molecular signaling mechanisms; (iii) comparative advantages of biomaterial classes; and (iv) strategies to overcome immunological, manufacturing, and regulatory barriers.
Fundamental ECM Biology and Composition
The ECM is a highly dynamic, three-dimensional network that provides not only structural support for tissues but also biochemical and mechanical cues essential for cellular function [13]. Composed of macromolecules such as collagens, glycosaminoglycans, elastin, and proteoglycans, the ECM regulates fundamental biological processes, including cell adhesion, migration, differentiation, and signal transduction [13]. The composition and mechanical properties of ECM show significant differences across tissue types, anatomical regions, and pathological states [13].
Table 1: Key ECM Components and Their Functions in Tissue Regeneration
| ECM Component | Primary Function | Role in Regeneration |
|---|---|---|
| Collagens (especially types I, II, III, IV, VI) | Provide tensile strength and structural integrity [13] | Type III to I transition enhances tissue strength; Type IV is crucial for basement membrane function [12] [14] |
| Elastin | Allows tissues to resume shape after stretching [13] | Provides resilience and stretch capacity to regenerating tissues [13] |
| Fibronectin | Mediates cell adhesion and migration [13] [14] | Forms provisional matrix after injury; regulates cell adhesion, differentiation, and communication [12] [14] |
| Laminin | Major component of basement membranes [14] | Promotes cell adhesion, differentiation, and angiogenesis; binds to integrins and other ECM components [14] |
| Proteoglycans/GAGs | Maintain structural properties and facilitate cell signaling [13] | Regulate water retention, growth factor binding, and cell signaling processes [13] |
The mechanical properties of the ECM—including stiffness, viscoelasticity, pore size, porosity, topology, and geometry—serve as key regulators of cellular behavior via mechanotransduction pathways [13]. Changes in ECM mechanics are frequently observed in pathological conditions, including cancer, fibrosis, and cardiovascular diseases, where dysregulated ECM remodeling promotes disease progression [13]. The aberrant stiffening of the ECM, for instance, enhances tumor invasion and fibrosis progression by altering cellular mechano-signaling [13].
Table 2: ECM Mechanical Properties Across Tissues and Pathological States
| Tissue/State | Stiffness/Mechanical Properties | Biological Significance |
|---|---|---|
| Brain Tissue | <2 kPa [13] | Soft environment suitable for neuronal function |
| Bone Tissue | 40–55 MPa [13] | Rigid structure providing mechanical support |
| Normal Breast Tissue | 0.167±0.031 kPa [13] | Physiological stiffness maintaining tissue homeostasis |
| Breast Cancer Tumor | 4.04±0.9 kPa [13] | Increased stiffness promoting malignancy and invasion |
| Pulmonary Fibrosis | 16.52 ± 2.25 kPa (5–10x increase) [13] | Progressive hardening driving disease progression |
Integrin-Mediated Signaling in Tissue Repair and Regeneration
Core Mechanisms of Integrin Signaling
Integrins serve as fundamental mediators of bidirectional communication between cells and their ECM microenvironment, playing indispensable roles in tissue repair and regeneration [12]. These transmembrane receptors, composed of α and β subunits, recognize specific ECM components including collagen, fibronectin, and laminin, thereby orchestrating essential cellular processes such as adhesion, migration, proliferation, and survival [12]. The dynamic interplay between integrins and their ECM ligands forms the molecular foundation for tissue regeneration, with distinct subunit combinations conferring specificity to these critical interactions [12].
The activation of integrin signaling initiates with ECM ligand binding, which induces conformational changes that promote receptor clustering and the assembly of focal adhesion complexes [12]. These specialized structures serve as mechanical and biochemical signaling hubs, recruiting adaptor proteins including talin, vinculin, and paxillin to bridge the connection between integrins and the actin cytoskeleton [12]. The formation of focal adhesions triggers the activation of multiple downstream signaling pathways that collectively coordinate the cellular response to tissue injury [12].
Central to this signaling network is the focal adhesion kinase (FAK) pathway, which, upon activation at Tyr397, recruits Src family kinases to regulate cytoskeletal dynamics and promote cell migration [12]. Parallel MAPK/ERK pathway activation regulates gene expression for proliferation and differentiation, while the PI3K/Akt pathway promotes cell survival in stressful, injured tissue microenvironments [12]. These interconnected pathways function synergistically to ensure appropriate cellular responses during the repair process [12].
Integrin Signaling in Mesenchymal Stem Cell Differentiation
The role of integrin signaling is particularly crucial in mesenchymal stem cell (MSC) differentiation, which is fundamental to tissue engineering strategies [15]. MSCs are multipotent stem cells with the ability to differentiate into various cell types, including adipocytes, chondrocytes, and osteoblasts [15]. The interaction of cell-ECM is mediated by integrins, which regulate cell adhesion, migration, and signaling, all of which are essential for tissue development and regeneration [15].
The activation of downstream pathways by integrin varies significantly across different MSC lineages [15]. In adipocytes, the interaction of ECM and integrin regulates adipogenesis through the activation of the Wnt/β-catenin pathway and inhibition of focal adhesion kinase (FAK) activity [15]. These activations reduce the expression of adipogenic markers such as AP2, AdipoQ, and CEBPα [15]. In chondrocytes, integrin receives signals from inflammation and produces inflammatory mediators (IL-1β and TNF-α) and matrix-degrading enzymes (MMP-3 and MMP-13), while the activation of MAPK-ERK is driven by Src, leading to chondrogenesis [15]. In osteoblasts, the activation of integrin induces both Wnt/β-catenin and FAK/ERK pathways activation, which in turn promote mineralization and osteogenic differentiation, respectively [15].
Dynamic ECM Remodeling in Wound Healing
ECM remodeling is a dynamic, tightly regulated process essential for wound healing, involving degradation of the provisional matrix and deposition of new ECM components critical for tissue restoration [12]. Shortly after injury, a fibrin-rich provisional matrix forms, offering structural support and enabling cellular infiltration that initiates repair [12]. This matrix also modulates the inflammatory response by recruiting fibroblasts and endothelial cells [12].
Matrix metalloproteinases (MMPs) become pivotal during the remodeling phase by degrading the provisional matrix and facilitating fibroblast migration and ECM synthesis [12]. MMPs ensure a balanced transition from matrix degradation to new ECM formation, which is essential for effective healing [12]. A hallmark of this phase is the replacement of type III collagen with type I collagen, enhancing tissue tensile strength and restoring structural integrity [12]. Moreover, remodeling involves upregulation of matricellular proteins like fibronectin and tenascin-C, which modulate cell-ECM interactions and influence cell behavior, including adhesion, migration, and differentiation [12].
Precise regulation of ECM turnover is crucial; dysregulation can lead to pathological scarring, such as hypertrophic scars or keloids [12]. Overall, ECM remodeling supports both early repair and later tissue normalization through coordinated synthesis and degradation [12]. The dynamic process of ECM remodeling during wound healing highlights its key phases and components, illustrating the transition from provisional matrix formation to collagen maturation and tissue restoration [12].
ECM-Inspired Biomaterials for Tissue Engineering
Design Principles and Material Classes
ECM-inspired biomaterials have emerged as a significant advancement in the field of tissue engineering, presenting promising approaches for the repair and regeneration of damaged tissues [12]. These biomaterials are engineered to replicate both the structural and biochemical characteristics of the natural ECM, providing an optimal environment conducive to cellular activities critical for healing [12]. The inherent properties of the ECM are being investigated in efforts to develop scaffolds that promote cell attachment and proliferation while also enhancing the intricate processes of tissue repair and remodeling [12].
The design principles underlying ECM-inspired biomaterials focus on recapitulating key aspects of native ECM, including:
- Structural mimicry: Replicating the three-dimensional architecture of natural ECM [12]
- Biochemical signaling: Incorporating bioactive molecules that regulate cellular behavior [12]
- Mechanical compatibility: Matching tissue-specific mechanical properties [12]
- Dynamic remodeling: Enabling controlled degradation and neotissue formation [12]
Table 3: Classes of ECM-Inspired Biomaterials and Their Applications
| Biomaterial Class | Key Examples | Advantages | Clinical Applications |
|---|---|---|---|
| ECM-based Scaffolds | Decellularized tissues, ECM hydrogels [12] [16] | Preserves native ECM composition and bioactivity [12] | Dermal regeneration, musculoskeletal repair [12] |
| Natural Biomaterials | Collagen, hyaluronic acid, fibrin [12] | Innate biocompatibility and bioactivity [12] | Wound healing, cartilage regeneration [12] |
| Synthetic Polymers | PLGA, PEG, PCL [12] | Tunable mechanical properties and degradation [12] | Bone tissue engineering, drug delivery [12] |
| Bioceramics | Hydroxyapatite, β-tricalcium phosphate [12] | Excellent osteoconductivity and mechanical strength [12] | Bone defect repair, dental applications [12] |
| Composite Materials | Polymer-ceramic blends, nano-reinforced composites [12] | Combines advantages of multiple material classes [12] | Osteochondral regeneration, vascular grafts [12] |
Advanced Fabrication Technologies
Innovations in decellularization, biofunctionalization, and advanced manufacturing are discussed as promising avenues to enhance biomimicry and therapeutic efficacy [12]. Furthermore, clinically approved ECM-derived products and the need for standardized protocols to bridge translational gaps are explored [12]. Key fabrication technologies include:
- 3D Bioprinting: Enables precise replication of the ECM's hierarchical architecture through layer-by-layer deposition of bioinks containing cells and biomaterials [12]
- Electrospinning: Creates nanofibrous scaffolds that mimic the fibrous structure of natural ECM [12] [17]
- Decellularization: Preserves the complex composition and ultrastructure of native ECM while removing cellular components [12] [16]
- Biofunctionalization: Enhances scaffolds with peptides, glycosaminoglycan mimetics, and nanostructured coatings [12]
Immune Response to ECM Bioscaffolds
The immune response to an implanted biomaterial is initiated by the inflammation caused by surgery itself [16]. The disruption of blood vessels, basement membranes, and tissues, in general, triggers coagulation cascade events, which result in the accumulation of platelets and leukocytes [16]. The contact of blood with the implanted biomaterial enables the adsorption of proteins such as albumin, immunoglobulins, and fibrinogen, which modulate the platelets' activation and coagulation events, therefore influencing the progression of the healing [16].
Unlike synthetic implants, which are often associated with chronic inflammation or fibrotic encapsulation, ECM bioscaffolds interact dynamically with host cells, promoting constructive tissue remodeling [16]. This effect is largely attributed to the preservation of structural and biochemical cues—such as degradation products and matrix-bound nanovesicles (MBV) [16]. These cues influence immune cell behavior and support the transition from inflammation to resolution and functional tissue regeneration [16]. However, the immunomodulatory properties of ECM bioscaffolds are dependent on the source tissue and, critically, on the methods used for decellularization [16]. Inadequate removal of cellular components or the presence of residual chemicals can shift the host response towards a pro-inflammatory, non-constructive phenotype, ultimately compromising therapeutic outcomes [16].
After the inflammatory response onset, innate immune cells interact with the implanted material through transmembrane receptors called integrins that activate metabolic pathways in response to mechanical and biochemical stimuli [16]. These metabolic pathways include cascade factors such as NF-κB, MAPK, TGF-β, JAK/STAT, PI3K/Akt/mTOR, and control the release of cytokines and growth factors that communicate and amplify the immune response at the local level [16].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Key Research Reagent Solutions
Table 4: Essential Research Reagents for ECM and Integrin Signaling Studies
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Integrin Ligands | RGD peptides, collagen-mimetic peptides, laminin-derived peptides [12] [14] | Biomaterial functionalization | Promote specific integrin binding and cell adhesion [12] |
| ECM Component Antibodies | Anti-collagen I, III, IV; anti-fibronectin; anti-laminin antibodies [14] | Immunohistochemistry, ELISA, Western blot | Detection and quantification of ECM proteins [14] |
| MMP Inhibitors/Assays | GM6001, MMP-2/9 inhibitor I, fluorescent MMP substrates [12] | Study of ECM remodeling | Modulation and measurement of protease activity [12] |
| Decellularization Reagents | SDS, Triton X-100, sodium deoxycholate, nucleases [12] [16] | Tissue decellularization | Removal of cellular content while preserving ECM structure [12] [16] |
| Mechanosensing Probes | YAP/TAZ antibodies, FRET-based tension sensors [13] | Mechanotransduction studies | Visualization of mechanical signaling pathways [13] |
Experimental Protocols for Critical Assessments
Protocol 1: Assessment of ECM Scaffold Immunomodulatory Properties
- Scaffold Preparation: Decellularize tissue using perfusion with 0.1% SDS followed by 1% Triton X-100, with nuclease treatment (50 U/mL DNase and RNase in PBS) for 3 hours at 37°C [16]
- Immune Cell Isolation: Isolate human peripheral blood mononuclear cells (PBMCs) using density gradient centrifugation [16]
- Co-culture Setup: Seed PBMCs on ECM scaffolds at density of 1×10^6 cells/cm² in RPMI-1640 medium with 10% FBS [16]
- Phenotype Analysis: After 72 hours, analyze macrophage polarization markers (CD86 for M1, CD206 for M2) using flow cytometry [16]
- Cytokine Profiling: Quantify cytokine secretion (IL-1β, IL-6, TNF-α for pro-inflammatory; IL-10, TGF-β for pro-remodeling) using multiplex ELISA [16]
Protocol 2: Evaluation of Integrin-Mediated MSC Differentiation
- Biomaterial Fabrication: Prepare RGD-functionalized hydrogels at varying stiffness (1-50 kPa) to mimic different tissue microenvironments [15]
- MSC Culture and Seeding: Culture human MSCs in growth medium and seed at passage 3-5 on functionalized surfaces at 10,000 cells/cm² [15]
- Osteogenic Differentiation: For osteogenesis, use medium supplemented with 10 mM β-glycerophosphate, 50 μM ascorbate-2-phosphate, and 100 nM dexamethasone for 21 days [15]
- Adipogenic Differentiation: For adipogenesis, use medium with 1 μM dexamethasone, 0.5 mM IBMX, 10 μg/mL insulin, and 200 μM indomethacin for 14 days [15]
- Analysis: Quantify differentiation using Alizarin Red S staining (mineralization) for osteogenesis or Oil Red O staining (lipid accumulation) for adipogenesis [15]
The ECM represents a pivotal system that intricately influences cell behavior, tissue repair, and regeneration through a multitude of signaling pathways and interactions [14]. This review has underscored the importance of various matrix proteins, including collagens, fibronectin, laminin, and others, in mediating these processes [14]. The unique properties of each of these proteins enable them to play critical roles in wound healing, cell adhesion, differentiation, and communication [14].
By integrating emerging research with clinical perspectives, this review provides a roadmap for developing next-generation ECM-inspired biomaterials that address unmet needs in regenerative medicine, emphasizing interdisciplinary collaboration to optimize safety, functionality, and patient outcomes [12]. Future research directions should focus on:
- Advanced Biomimicry: Developing materials that better replicate the dynamic nature of ECM remodeling [12]
- Immunomodulation Strategies: Harnessing the immune-modulating properties of ECM for enhanced tissue integration [16]
- Personalized Approaches: Creating patient-specific scaffolds based on individual ECM profiles [13]
- Advanced Manufacturing: Utilizing 3D bioprinting and other technologies for complex tissue constructs [12]
- Standardization and Regulation: Establishing standardized protocols and regulatory frameworks for clinical translation [12]
The continued exploration of ECM biology and integrin signaling mechanisms will undoubtedly yield new insights and innovative solutions for tissue engineering and regenerative medicine applications. As our understanding of these complex systems deepens, so too will our ability to create increasingly sophisticated biomaterials that truly learn from nature's design principles.
Building Functional Tissues: Material Innovations and Fabrication Technologies
Natural polymers represent a cornerstone of modern tissue engineering, providing biomimetic scaffolds that closely resemble the native extracellular matrix (ECM). Among these, collagen, hyaluronic acid, chitosan, and silk fibroin have emerged as particularly promising materials due to their exceptional biocompatibility, tunable properties, and diverse biological functions. This technical guide provides an in-depth analysis of these four key natural polymers, focusing on their structural characteristics, biological mechanisms, and experimental applications in tissue engineering. By synthesizing current research findings and methodologies, this whitepaper aims to equip researchers and drug development professionals with the practical knowledge necessary to leverage these biomaterials for advanced therapeutic strategies. The content is framed within the broader context of biomaterial scaffold development, emphasizing the critical role of natural polymers in creating functional tissue constructs that support cell adhesion, proliferation, differentiation, and ultimately, tissue regeneration.
Polymer Profiles and Properties
Table 1: Fundamental Characteristics of Key Natural Polymers
| Polymer | Chemical Structure | Primary Sources | Key Properties | Degradation Mechanism |
|---|---|---|---|---|
| Collagen | Triple helix of polypeptide chains with [Gly-X-Y]ₙ repeats | Mammalian tissues (skin, tendon), marine organisms [18] | Excellent biocompatibility, low immunogenicity, biodegradability, hemostatic properties, mechanical strength [18] | Enzymatic degradation by matrix metalloproteinases (MMPs) [18] |
| Hyaluronic Acid (HA) | Linear polysaccharide composed of D-glucuronic acid and N-acetyl-D-glucosamine [19] | Bacterial fermentation, rooster combs, vertebrate connective tissues [19] | Biocompatible, biodegradable, viscoelastic, CD44 receptor recognition, molecular weight-dependent bioactivity [19] [20] | Hyaluronidase-mediated degradation [19] |
| Chitosan | Linear polysaccharide of (β1→4) linked 2-amino-2-deoxy-d-glucose and N-acetyl-2-amino-2-deoxy-d-glucose [21] | Crustacean shells, insect cuticles, fungal cell walls [21] | Biocompatible, biodegradable, antimicrobial, hemostatic, pH-sensitive solubility [21] [22] | Enzymatic degradation by lysozyme and bacterial enzymes in colon [21] |
| Silk Fibroin (SF) | Protein with crystalline β-sheet domains surrounded by less organized regions [23] | Silkworms (Bombyx mori), spiders [22] | Excellent mechanical properties, biocompatible, biodegradable, versatile processability, tunable degradation [23] [22] | Proteolytic degradation; rate controlled by β-sheet content [23] |
Table 2: Mechanical and Functional Performance Metrics
| Polymer | Tensile Strength | Elongation at Break | Compressive Strength | Key Functional Advantages | Common Modifications |
|---|---|---|---|---|---|
| Collagen | Variable (source-dependent) | High elasticity in native forms | Enhanced in composite scaffolds [18] | Reconstructs ECM microenvironment, promotes cell adhesion, migration, proliferation, differentiation [18] | Cross-linking (EDC/NHS), polymer composite formation [24] |
| Hyaluronic Acid | Low (native form) | High (native form) | Low (native form) | Angiogenic potential, inflammation modulation, antibacterial, antioxidant functions [19] | Methacrylation, acrylation, norbornene, thiolation for cross-linking [20] |
| Chitosan | Moderate | Moderate to high | Moderate | Antimicrobial, mucoadhesive, hemostatic, can be functionalized via amino groups [21] [25] | Acylation, quaternization, carboxymethylation, thiolation [21] |
| Silk Fibroin | High (0.5-1.2 GPa) | High (10-30%) | Enhanced through β-sheet formation [23] | Superior mechanical strength, supports mesenchymal stem cell adhesion, proliferation, and differentiation [23] | Cross-linking, blending with other polymers, β-sheet content control [23] |
Cellular Interactions and Signaling Mechanisms
Collagen-Cell Interactions
Collagen regulates cellular behavior through specific receptor-mediated interactions. Integrins (α1β1, α2β1, α10β1, α11β1) and discoidin domain receptors (DDRs) serve as primary collagen receptors, recognizing specific triple-helical sequences within the collagen structure [18]. The GxOGEx' motif facilitates integrin binding, while DDR1 interacts with collagen types I, II, III, and IV, and DDR2 primarily binds collagen types I and III with high affinity for the GVMGFO motif [18]. These interactions trigger intracellular signaling cascades that direct fundamental cellular processes.
DDR1 binding to collagen activates the MAPK/ERK pathway, regulating immune cell migration, monocyte-to-macrophage differentiation, and secretion of chemotactic factors that enhance macrophage migration [18]. DDR2 activation primarily regulates MMP expression to mediate cell migration, inducing MMP-8 expression to degrade collagen networks and release chemotactic peptides that induce neutrophil chemotactic migration in 3D matrices [18]. Additionally, increased DDR2 expression enhances endogenous collagen synthesis, creating a positive feedback loop that promotes fibroblast proliferation and ECM remodeling through MMP-2 expression [18].
Beyond receptor-mediated signaling, collagen matrices provide physical guidance cues through haptotaxis (migration along adhesion gradients), durotaxis (migration along stiffness gradients), and contact guidance (migration along topological features) [18]. These mechanisms collectively enable collagen to orchestrate complex tissue regeneration processes by directing cell positioning, differentiation, and tissue assembly.
Hyaluronic Acid Molecular Weight-Specific Effects
Hyaluronic acid exhibits dichotomous biological effects directly correlated with its molecular weight. High molecular weight HA (>500 kDa) demonstrates immunosuppressive and anti-inflammatory properties, while low molecular weight HA (<500 kDa) promotes pro-inflammatory phenotypes [20]. This size-dependent bioactivity significantly influences its application in tissue engineering, where specific inflammatory responses may be desirable or detrimental depending on the regeneration context.
HA interacts with cells primarily through CD44 and RHAMM (Receptor for Hyaluronan-Mediated Motility) receptors [19]. CD44, widely expressed on fibroblasts, blood cells, and cancer cells, regulates cell adhesion, migration, and proliferation. RHAMM promotes cell movement and focal adhesion turnover during migration and in response to cytokines [19]. These receptor interactions enable HA to directly influence cellular behavior and tissue organization.
The degradation products of HA further modulate biological responses. Oligosaccharides generated through hyaluronidase activity affect wound healing, angiogenesis, and immune reactions [19]. This degradation creates a dynamic feedback system where HA fragments can either promote or resolve inflammatory processes depending on their size, concentration, and temporal presentation during the healing cascade.
Experimental Methodologies and Protocols
Preparation of Carp Collagen Scaffolds for Guided Bone Regeneration
Objective: To fabricate and modify carp collagen membranes with controlled degradation properties for guided bone regeneration applications, ensuring structural integrity for a minimum critical period of 4 weeks to facilitate initial bone formation [24].
Materials and Reagents:
- European carp (Cyprinus carpio) skin
- Deionized water
- N-ethyl-N'-(3-dimethylaminopropyl)carbodiimide (EDC)
- N-hydroxysuccinimide (NHS)
- 95% ethanol solution
- 0.1 M Na₂HPO₄
- Purasorb polymers (l-lactide, ε-caprolactone, d,l-lactide, glycolide)
Procedure:
- Collagen Isolation: Isolate collagen from carp skin using established procedures [24].
- Dispersion Preparation: Create a 4 wt% aqueous collagen dispersion by swelling collagen in deionized water. Homogenize at 10,000 rpm for 10 minutes and allow to stand at 20°C for 60 minutes. Perform final homogenization at 6,500 rpm for 10 minutes [24].
- Lyophilization: Transfer the resulting dispersion to containers (10 × 10 × 2 cm), freeze at -70°C for 5 hours, and lyophilize using a BenchTop 4KZL lyophilizer [24].
- Cross-linking: Prepare a 95 wt% ethanol solution containing EDC and NHS at a 4:1 ratio (wt/wt). Immerse collagen membranes for 24 hours for cross-linking [24].
- Washing: Wash membranes sequentially with 0.1 M Na₂HPO₄ (2 × 30 minutes) and deionized water (30 minutes) [24].
- Final Processing: Freeze washed membranes at -30°C and lyophilize [24].
- Polymer Modification (Optional): For enhanced mechanical properties, impregnate the upper layer of selected membranes with biodegradable polymers including:
- Copolymer of poly-l-lactide and PCL (70:30 ratio)
- Copolymer of PCL and PGA (50:50 ratio)
- Copolymer of d,l-lactide and glycolide (50:50 ratio) [24]
Evaluation Methods:
- Micro-MRI: Utilize micro-MRI as a noninvasive approach to monitor in vivo degradation of collagen membranes up to scaffold disintegration [24].
- Histological Analysis: Assess local tissue response, inflammatory reaction, and residual membrane integrity through complementary histological techniques [24].
Fabrication of Silk Fibroin/Chitosan-Hyaluronic Acid Composite Scaffolds
Objective: To develop composite SF/CS-HA scaffolds that enhance cell proliferation compared to pure silk fibroin scaffolds for tissue engineering applications [26].
Materials and Reagents:
- Silk fibroin protein (SF)
- Chitosan (CS)
- Hyaluronic acid (HA)
- Human dermal fibroblasts (HDF)
- Cell culture media and reagents
- MTT assay reagents
- Confocal microscopy materials
Procedure:
- Scaffold Fabrication: Fabricate SF/CS-HA microparticles to produce composite scaffolds [26].
- Characterization: Confirm co-existence of SF and CS-HA in composite microparticles using zeta potential measurements and ATR-FTIR spectroscopy [26].
- Cell Seeding and Culture: Seed human dermal fibroblasts (HDF) onto scaffolds and culture for 7 days [26].
- Cell Proliferation Assessment:
- Metabolic Analysis: Monitor daily glucose consumption and lactate formation as metabolic parameters of HDF grown in different scaffolds [26].
Expected Results:
- HDF should proliferate effectively and migrate into SF/CS-HA scaffolds to depths of approximately 160 μm [26].
- SF/CS-HA scaffolds should demonstrate significantly higher cell density compared to pure SF scaffolds [26].
- MTT assay should reveal that growth rates of HDF in SF/CS-HA scaffolds significantly exceed those in SF and SF/CS scaffolds (p < 0.01) [26].
- Metabolic parameters (glucose consumption, lactate formation) of HDF in SF/CS-HA and SF/CS scaffolds should be significantly higher than in SF scaffolds (p < 0.01) for most culture days [26].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Natural Polymer Scaffold Development
| Reagent/Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Cross-linking Agents | EDC, NHS, genipin [24] | Enhance mechanical properties and control degradation rates of collagen and chitosan scaffolds | EDC/NHS ratio of 4:1 (wt/wt) effectively cross-linked carp collagen membranes [24] |
| Polymer Modifiers | l-lactide, ε-caprolactone, d,l-lactide, glycolide [24] | Modify degradation kinetics and mechanical strength of base polymers | d,l-lactide and glycolide (50:50 ratio) extended collagen membrane integrity [24] |
| Functionalization Chemistry | Methacrylate, acrylate, norbornene, thiol groups [20] | Enable chemical modification and cross-linking of hyaluronic acid | Methacrylated HA allows photopolymerization; degree of substitution controls hydrogel properties [20] |
| Cell Adhesion Promoters | RGD peptides, collagen-derived peptides [18] | Enhance cell-scaffold integration and signaling | RGD sequence incorporation improves cell adhesion to silk fibroin [18] |
| Characterization Tools | Micro-MRI, ATR-FTIR, zeta potential [24] [26] | Analyze scaffold structure, composition, and degradation | Micro-MRI enables noninvasive in vivo degradation monitoring [24] |
| Degradation Enzymes | Matrix metalloproteinases (MMPs), hyaluronidases [18] [19] | Study scaffold degradation patterns and rates | MMP overexpression in chronic wounds delays healing by disrupting basement membrane [18] |
The strategic application of natural polymers in tissue engineering continues to evolve, with collagen, hyaluronic acid, chitosan, and silk fibroin each offering unique advantages for specific tissue regeneration contexts. The future development of these biomaterials lies in creating increasingly sophisticated composite systems that leverage the complementary properties of multiple polymers. As evidenced by the enhanced cell proliferation in SF/CS-HA composites compared to single polymer scaffolds [26], these synergistic approaches can overcome limitations of individual materials.
Advanced fabrication technologies enabling precise spatial control over scaffold architecture and composition will further enhance the biomimetic potential of natural polymer-based systems. The incorporation of bioresponsive elements that dynamically interact with the cellular environment represents another promising direction. For instance, HA-based hydrogels with tunable properties responsive to environmental cues [20] offer exciting possibilities for creating smart scaffolds that adapt to changing physiological conditions during the regeneration process.
As research progresses, standardization of natural polymer extraction, characterization, and modification protocols will be crucial for clinical translation. Addressing challenges related to batch-to-batch variability, sterilization methods, and scalable production will ensure the consistent performance required for therapeutic applications. With continued innovation in material design and processing techniques, natural polymers are poised to remain at the forefront of tissue engineering strategies, enabling increasingly functional and predictable tissue regeneration outcomes.
Advances in Synthetic and Composite Polymers for Tunable Properties
The field of tissue engineering has witnessed a transformative shift with the development of advanced synthetic and composite polymers, which offer unprecedented control over material properties for regenerative medicine. These materials serve as the foundation for three-dimensional scaffolds that mimic the native extracellular matrix (ECM), providing structural support and biological cues for cell attachment, proliferation, and differentiation [27]. The convergence of smart biodegradable polymers and sophisticated fabrication technologies has enabled the creation of scaffolds with tunable mechanical properties, controlled degradation profiles, and enhanced bioactivity [28]. This technical guide examines recent advances in polymer design, fabrication methodologies, and functionalization strategies that allow researchers to precisely engineer material characteristics for specific tissue engineering applications, particularly in bone regeneration.
The evolution from first-generation bio-inert scaffolds to contemporary bioactive systems represents a paradigm shift in biomaterial science. Modern scaffold design emphasizes multifunctional performance through the strategic combination of natural and synthetic polymers, incorporation of bioactive ceramics, and application of nanotechnology [29]. These composites provide not only structural templates but also dynamic microenvironments that actively guide tissue regeneration through controlled degradation and the release of biological factors [30]. Furthermore, the emergence of stimuli-responsive polymers has introduced a new dimension to scaffold functionality, enabling materials that adapt their properties in response to physiological cues such as pH, temperature, or enzymatic activity [28].
Material Systems and Their Properties
Synthetic Biodegradable Polymers
Synthetic polymers offer significant advantages in tissue engineering due to their reproducible production, tunable mechanical properties, and controllable degradation kinetics. The most widely used synthetic biodegradable polymers belong to the aliphatic polyester family, which degrade through hydrolysis of ester bonds in their backbones [31].
Poly(lactic acid) (PLA), poly(glycolic acid) (PGA), and their copolymers (PLGA) are among the few FDA-approved synthetic polymers for certain clinical applications. PGA is highly crystalline and degrades rapidly, losing mechanical integrity within 2-4 weeks, while PLA is more hydrophobic and requires months to years for complete degradation [31]. The degradation rate of PLGA can be precisely tuned by adjusting the lactide to glycolide ratio, achieving intermediate degradation profiles between its constituent homopolymers.
Poly(ε-caprolactone) (PCL) degrades at a much slower rate than PLA or PGA, making it suitable for long-term implants and drug delivery systems. Its semi-crystalline nature with a low glass transition temperature (-60°C) keeps it in a rubbery state under physiological conditions, providing favorable material permeability [31].
Poly(glycerol sebacate) (PGS) is an elastomeric polymer synthesized from glycerol and sebacic acid, both of which are biocompatible metabolites. PGS exhibits thermoset elastomeric properties and can be tuned to achieve specific mechanical properties and degradation rates by controlling curing parameters and the degree of acrylation [31]. Its elastomeric nature makes it particularly suitable for soft tissue engineering applications.
Recent innovations in polymer chemistry have enabled unprecedented control over material properties. For instance, resorbable elastomer-like materials with controlled cis:trans double bond ratios in their backbones allow independent tuning of mechanical properties and degradation rates—a significant advancement over traditional approaches where these properties are intrinsically linked [32].
Composite and Functional Polymer Systems
The limitations of single-component polymer systems have driven the development of composite materials that combine the advantages of multiple constituents. These composites typically integrate synthetic polymers with natural polymers or inorganic components to enhance bioactivity and mechanical performance.
Natural-synthetic polymer blends, such as PCL-gelatin composites, leverage the mechanical stability of synthetic polymers with the improved cellular affinity of natural polymers. Gelatin, derived from collagen hydrolysis, contains RGD sequences that facilitate cell attachment and proliferation, while PCL provides structural integrity and extends the degradation timeline [27].
Ceramic-polymer composites incorporate bioactive inorganic materials like hydroxyapatite (HAp), tricalcium phosphate (TCP), or bioactive glass into polymer matrices. These composites significantly enhance osteoconductivity and mechanical strength, making them ideal for bone tissue engineering. The incorporation of nano-hydroxyapatite (nHA) into a nanofibrous polymer matrix creates a composite that closely mimics the composition and structure of natural bone [27] [29].
Conductive polymer composites represent another frontier in functional biomaterials. Materials such as polyaniline, polypyrrole, and polythiophene provide electrical conductivity that can support the regeneration of electrically responsive tissues like cardiac muscle, nerve, and bone [33]. These polymers feature conjugated backbones with alternating single and double bonds that enable electron delocalization, resulting in electrical conductivity that can be enhanced through doping processes [33].
Table 1: Properties of Key Synthetic Biodegradable Polymers
| Polymer | Degradation Time | Elastic Modulus | Key Characteristics | Primary Applications |
|---|---|---|---|---|
| PGA | 2-4 weeks | High crystallinity | Rapid degradation, good tensile strength | Sutures, simple scaffolds |
| PLA | Months to years | 1-3 GPa | Slow degradation, hydrophobic | Bone fixation, long-term scaffolds |
| PLGA | Tunable: weeks to months | 1-2 GPa | Degradation rate depends on LA:GA ratio | Drug delivery, various scaffolds |
| PCL | >1 year | 0.2-0.4 GPa | Slow degradation, rubbery state | Long-term implants, drug delivery |
| PGS | ~6 weeks in vivo | 0.002-1.5 MPa | Elastomeric, surface erosion | Soft tissue engineering |
Fabrication Techniques for Polymeric Scaffolds
The fabrication methodology significantly influences the architectural and mechanical properties of tissue engineering scaffolds. Conventional techniques such as solvent casting/particle leaching, freeze-drying, thermal induced phase separation (TIPS), and gas foaming enable the creation of porous structures but offer limited control over pore geometry and distribution [34].
Electrospinning has emerged as a versatile technique for producing fibrous scaffolds with fiber diameters ranging from micrometers to nanometers. These scaffolds mimic the fibrous structure of the native ECM, providing high surface area for cell attachment. The composition, alignment, and functionalization of electrospun fibers can be precisely controlled to direct cellular responses [28] [34].
Additive manufacturing (AM) technologies, including stereolithography (SLA), fused deposition modeling (FDM), selective laser sintering (SLS), and 3D bioprinting, have revolutionized scaffold fabrication by enabling precise control over internal architecture and pore network design [28] [34]. These techniques allow the creation of scaffolds with complex, patient-specific geometries and functionally graded structures. For bone tissue engineering, AM facilitates the fabrication of scaffolds with mechanical properties tailored to match those of native bone, reducing stress shielding effects [29].
Triply periodic minimal surfaces (TPMS) have gained attention as superior scaffold designs due to their high surface-area-to-volume ratio, enhanced permeability, and reduced stress concentration compared to conventional lattice structures [35]. The mathematical definition of TPMS geometries enables precise control over pore size and distribution, facilitating the creation of functionally graded structures that mimic the natural transition between different tissue types, such as the osteochondral interface [35].
Table 2: Scaffold Fabrication Techniques and Their Characteristics
| Fabrication Method | Resolution | Porosity Control | Advantages | Limitations |
|---|---|---|---|---|
| Solvent casting/particle leaching | 10-500 μm | Moderate (~90%) | Simple, inexpensive | Limited thickness, solvent residues |
| Freeze-drying | 1-200 μm | High (>90%) | High porosity, interconnected pores | Random pore structure, fragile |
| Gas foaming | 50-500 μm | High (>85%) | No organic solvents | Mostly closed pores |
| Electrospinning | 0.1-10 μm | Moderate-high (70-90%) | ECM-like structure, high surface area | Limited thickness, small pore size |
| 3D Printing/FDM | 100-500 μm | Good (60-80%) | Good structural control, mechanical strength | Limited resolution, thermal stress |
| Stereolithography | 10-100 μm | Excellent (60-90%) | High resolution, complex geometries | Limited materials, UV sensitivity |
Degradation Behavior and Control Strategies
Degradation Mechanisms
The degradation behavior of polymeric scaffolds significantly influences their performance in tissue engineering applications. Two primary erosion mechanisms govern scaffold degradation: surface erosion and bulk degradation [35] [36].
In surface erosion, the hydrolytic reaction occurs faster than water diffusion into the material, resulting in a thinning of scaffold features from the outside inward without a reduction in molecular weight in the bulk material. This mechanism is typically observed in polyanhydrides and polyorthoesters and leads to a relatively linear loss of mass over time while largely maintaining mechanical integrity until late stages of degradation [36].
In bulk degradation, water penetrates the material faster than hydrolysis occurs, resulting in a relatively uniform reduction of molecular weight throughout the scaffold. Polyesters like PLA, PGA, and PCL typically degrade through this mechanism. A phenomenon known as autocatalysis can occur in bulk-degrading polymers when acidic degradation products accelerate the hydrolysis reaction, leading to faster degradation in the interior of the scaffold than at the surface [36].
The degradation mechanism has profound implications for scaffold performance. Surface erosion generally provides more predictable degradation profiles and better maintenance of mechanical properties during the initial stages of implantation. In contrast, bulk degradation with autocatalysis can lead to sudden mechanical failure, which may be undesirable in load-bearing applications [36].
Controlling Degradation Behavior
Several strategies have been developed to control the degradation behavior of polymeric scaffolds:
Chemical composition control through copolymerization represents a fundamental approach for tuning degradation rates. For example, adjusting the ratio of lactide to glycolide in PLGA copolymers enables precise control over degradation timelines from weeks to months [31]. Similarly, incorporating succinate-based monomer units into elastomer backbones allows degradation rate adjustment while maintaining mechanical properties through independent control of double bond stereochemistry [32].
Architectural design significantly influences degradation behavior. Scaffold porosity and pore interconnectivity affect fluid penetration and, consequently, degradation kinetics. Lower porosity scaffolds with limited interconnectivity may experience accelerated internal degradation due to acid autocatalysis, as degradation products are trapped within the structure [35]. TPMS-based architectures with their high permeability can mitigate this effect by facilitating the removal of acidic degradation products [35].
Composite formulation can modify degradation profiles. Incorporating ceramic nanoparticles like hydroxyapatite or bioactive glass into polymer matrices can buffer acidic degradation products, reducing autocatalytic effects and creating a more neutral microenvironment conducive to bone formation [29].
Table 3: Degradation Mechanisms and Their Implications
| Degradation Mechanism | Typical Polymers | Mass Loss Profile | Mechanical Integrity | Clinical Implications |
|---|---|---|---|---|
| Surface erosion | Polyanhydrides, polyorthoesters | Linear decrease over time | Maintained until late stages | Predictable resorption timeline |
| Bulk degradation (without autocatalysis) | PCL, low-thickness PLA | Slow initial, then rapid loss | Gradual decrease | Suitable for long-term support |
| Bulk degradation (with autocatalysis) | PLGA, thick PLA sections | Lag phase then rapid loss | Sudden failure possible | Risk of premature mechanical failure |
Experimental Protocols for Polymer Characterization
Degradation Kinetics Assessment
Objective: To quantitatively evaluate the degradation profile of polymeric scaffolds under simulated physiological conditions.
Materials:
- Polymer scaffolds (5 mm diameter × 2 mm thickness)
- Phosphate buffered saline (PBS), pH 7.4
- Sodium azide (0.02% w/v)
- Incubation oven maintained at 37°C
- Analytical balance (accuracy ±0.01 mg)
- Vacuum desiccator
- Molecular weight characterization system (GPC/SEC)
Methodology:
- Pre-weigh dry scaffolds (W₀) after 24 hours in a vacuum desiccator
- Immerse samples in PBS with sodium azide (5 mL per sample) to prevent microbial growth
- Incubate at 37°C with gentle agitation (60 rpm)
- At predetermined time points (e.g., 1, 2, 4, 8, 12 weeks): a. Remove samples from solution and rinse with deionized water b. Blot gently and dry to constant weight in a vacuum desiccator c. Record dry weight (Wₜ) d. Calculate mass loss percentage: [(W₀ - Wₜ)/W₀] × 100
- Parallel samples should be used for molecular weight analysis via gel permeation chromatography (GPC)
- Monitor pH changes of the degradation medium throughout the study
- Characterize morphological changes via scanning electron microscopy (SEM)
Data Analysis: Plot mass retention (%) and molecular weight retention (%) versus time to determine degradation kinetics. Fit data to appropriate mathematical models (zero-order, first-order, or Hopfenberg models) to quantify degradation rates [35] [36].
Mechanical Property Evaluation During Degradation
Objective: To assess changes in mechanical properties of polymeric scaffolds throughout the degradation process.
Materials:
- Universal mechanical testing system
- Load cells appropriate for expected force range (typically 10N-1kN)
- Environmental chamber for temperature control (optional)
- PBS solution at 37°C
- Calibrated calipers or non-contact measurement system
Methodology:
- Prepare scaffold samples according to standardized dimensions (e.g., 10×10×5 mm for compression testing)
- For wet condition testing, hydrate samples in PBS for 24 hours at 37°C prior to testing
- Conduct baseline mechanical testing on fresh samples: a. Compression testing: Apply load until 50% strain or fracture at constant crosshead speed (typically 1 mm/min) b. Calculate compressive modulus from the linear region of the stress-strain curve (usually 0-10% strain)
- For degradation time course: a. Maintain parallel samples in PBS at 37°C b. At predetermined intervals, remove samples and perform mechanical testing as above c. Measure sample dimensions before each test to calculate accurate engineering stress
- For composite materials, perform cyclic loading tests to evaluate recovery and viscoelastic properties
Data Analysis: Plot mechanical properties (modulus, ultimate strength, strain at failure) versus degradation time. Correlate mechanical property changes with mass loss and molecular weight data to establish structure-property relationships [35] [32].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Advanced Polymer Scaffold Development
| Reagent/Material | Function/Application | Key Characteristics |
|---|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) | Versatile synthetic polymer scaffold base | Tunable degradation (weeks-months), FDA-approved for certain applications |
| Nano-hydroxyapatite (nHA) | Bioactive ceramic reinforcement | Enhances osteoconductivity, improves compressive strength |
| Gelatin | Natural polymer component | Contains RGD sequences for cell adhesion, modifies degradation rate |
| Polypyrrole | Conductive polymer component | Provides electrical conductivity (∼10³ S/cm), supports neural/cardiac tissue |
| Succinate-based monomers | Degradation control modifiers | Enable independent control of mechanics and degradation in elastomers |
| Triply Periodic Minimal Surface (TPMS) designs | Advanced scaffold architectures | High surface-area-to-volume ratio, reduced stress concentration |
| Bioactive glass (45S5) | Osteoconductive additive | Forms bond with bone tissue, releases therapeutic ions |
| Halloysite nanotubes (HNT) | Nanocomposite reinforcement | Improves mechanical properties, drug delivery vehicle |
The advancement of synthetic and composite polymers with tunable properties represents a cornerstone of modern tissue engineering strategies. Through sophisticated material design, researchers can now create scaffolds that not only provide structural support but also actively participate in the regenerative process through controlled degradation, release of bioactive factors, and delivery of physical cues. The independent control of mechanical properties and degradation behavior demonstrated in recent elastomer systems marks a significant milestone in biomaterial development [32].
Future directions in the field point toward increasingly smart material systems that respond dynamically to physiological cues and provide temporal control over multiple functions. The integration of conductive polymers for electrically responsive tissues [33], the development of four-dimensional printing techniques that enable post-fabrication morphological changes, and the creation of immunomodulatory scaffolds that actively coordinate the inflammatory response represent exciting frontiers. As these technologies mature, the clinical translation of tunable polymeric scaffolds will continue to expand, offering new solutions for tissue regeneration and personalized medicine.
The global burden of tissue loss and organ damage drives an urgent need for advanced regenerative medicine strategies. Tissue engineering aims to create biological substitutes to restore, maintain, or improve tissue function, with three-dimensional scaffolds serving as fundamental components that mimic the native extracellular matrix (ECM) [37]. These temporary frameworks provide structural support and biochemical cues that guide cellular adhesion, proliferation, and differentiation. Among the various fabrication technologies available, 3D bioprinting, electrospinning, and freeze-drying have emerged as particularly powerful techniques for creating sophisticated scaffold architectures. Each method offers unique advantages for specific tissue engineering applications, with 3D bioprinting providing unprecedented geometric control, electrospinning enabling nanofibrous ECM mimicry, and freeze-drying preserving bioactive components while creating porous matrices [38] [39] [40]. This technical guide examines these cutting-edge fabrication methods, their underlying principles, current applications, and experimental protocols within the context of biomaterial scaffold development for tissue engineering.
3D Bioprinting
3D bioprinting is an additive manufacturing technique that fabricates complex three-dimensional tissue constructs through layer-by-layer deposition of bioinks containing living cells and biocompatible materials [38] [41]. Unlike conventional 3D printing focused on structural properties, bioprinting emphasizes biological functionality and compatibility. The process typically involves three stages: preprocessing (digital design creation), processing (actual printing), and postprocessing (tissue maturation) [42]. Key advantages include high customization capability, precision control over internal architecture, and the ability to create patient-specific constructs with heterogeneous cell distributions.
The technology's effectiveness heavily depends on porosity parameters, which directly influence critical mechanical and biological properties including nutrient diffusion, cell adhesion, waste removal, and structural integrity [38]. Porosity characteristics such as pore size, geometry, distribution, and interconnectivity significantly affect cellular behavior and must be carefully optimized for specific tissue applications.
Experimental Protocol: Extrusion Bioprinting
Materials and Equipment:
- 3D bioprinter with temperature-controlled extrusion system
- Sterile cell culture facilities
- Bioink components (hydrogel precursor, cells, growth factors)
- CAD software for scaffold design
- Curing system (UV crosslinking station or ionic crosslinking bath)
Methodology:
- Bioink Preparation:
- Prepare hydrogel precursor solution (e.g., gelatin methacryloyl, alginate, hyaluronic acid)
- Mix with cells at appropriate density (typically 1-10×10^6 cells/mL)
- Maintain bioink at optimal temperature to balance viscosity and cell viability
Scaffold Design:
- Create digital model using CAD software with desired pore architecture
- Slice model into sequential 2D layers for printing path generation
- Set printing parameters (pressure, speed, nozzle height) based on material properties
Printing Process:
- Load bioink into sterile printing cartridges
- Set build plate temperature to facilitate adhesion and crosslinking
- Execute printing with layer-by-layer deposition
- Apply crosslinking during or immediately after deposition (UV exposure, ionic crosslinking)
Post-processing:
- Transfer constructs to cell culture media
- Maintain in appropriate culture conditions (bioreactor recommended)
- Monitor cell viability and tissue maturation over time
A recent innovation from MIT researchers addresses a significant limitation in conventional bioprinting through the integration of real-time process control. Their system incorporates a modular monitoring technique using a digital microscope that captures high-resolution images during printing and rapidly compares them to the intended design through an AI-based image analysis pipeline. This approach enables rapid identification of defects such as over- or under-deposition of bioink, facilitating optimization of printing parameters across different materials [41].
Technical Specifications
Table 1: 3D Bioprinting Techniques and Characteristics
| Technique | Principle | Resolution | Materials | Advantages | Limitations |
|---|---|---|---|---|---|
| Extrusion-Based | Mechanical or pneumatic extrusion through nozzle | 50-500 μm | High-viscosity hydrogels, cell spheroids | High cell density, structural integrity | Shear stress on cells |
| SLA/DLP | UV light crosslinks photosensitive polymers | 10-100 μm | PEGDA, GelMA | High resolution, smooth surfaces | Limited materials, UV potential cytotoxicity |
| Inkjet | Thermal or acoustic droplet ejection | 50-300 μm | Low-viscosity bioinks | High speed, low cost | Limited structural strength |
| Laser-Assisted | Laser energy transfers cells from ribbon | 10-100 μm | High cell density suspensions | High resolution, high viability | Complex setup, low speed |
Table 2: Bioink Formulations for Tissue-Specific Applications
| Tissue Type | Base Material | Cell Type | Additive Factors | Crosslinking Method | Target Porosity |
|---|---|---|---|---|---|
| Bone | Alginate-GelMA composite | Mesenchymal stem cells | BMP-2, β-tricalcium phosphate | Ionic + UV crosslinking | 70-90%, >200μm pores |
| Cartilage | Hyaluronic acid-GelMA | Chondrocytes | TGF-β3 | UV crosslinking | 80-90%, 150-250μm |
| Skin | Collagen-fibrin | Keratinocytes, fibroblasts | VEGF, EGF | Enzymatic (thrombin) | 85-95%, 100-300μm |
| Nerve | RGD-alginate | Neural stem cells | NGF, GDNF | Ionic (CaCl₂) | 90-95%, oriented channels |
Electrospinning
Electrospinning is a versatile technique for fabricating micro- and nanoscale fibrous scaffolds that closely mimic the structural characteristics of the native extracellular matrix [39]. The process utilizes high-voltage electrostatic forces to draw polymer solutions or melts into continuous fibers with diameters ranging from tens of nanometers to several micrometers [43]. These fibers create scaffolds with high surface area-to-volume ratios, tunable morphology, and interconnected porosity that facilitate cell adhesion, proliferation, and nutrient diffusion.
The electrospinning apparatus consists of four main components: a high-voltage power supply, a solution storage unit with ejection device (typically a syringe pump with metallic needle), and a collection device [39]. During the process, application of high voltage (typically 5-30 kV) creates a Taylor cone at the needle tip, from which a charged polymer jet is ejected toward the grounded collector. The jet undergoes bending instability and rapid stretching during its trajectory, resulting in substantial fiber thinning before deposition on the collector.
Experimental Protocol: Solution Electrospinning
Materials and Equipment:
- High-voltage power supply (0-30 kV)
- Syringe pump with precise flow rate control
- Collector assembly (static or rotating mandrel)
- Polymer solutions in appropriate solvents
- Fume hood for safe solvent evaporation
Methodology:
- Polymer Solution Preparation:
- Dissolve polymer in suitable solvent at optimized concentration (typically 5-20% w/v)
- Stir continuously until complete dissolution and homogeneous solution achieved
- Allow solution to degas to remove air bubbles that may disrupt fiber formation
Equipment Setup:
- Load solution into syringe and attach to pump system
- Connect high-voltage source to needle tip
- Set collector distance (typically 10-20 cm)
- Adjust collector type based on desired fiber alignment (static for random, rotating for aligned)
Parameter Optimization:
- Apply voltage gradually until stable Taylor cone forms
- Optimize flow rate (0.5-3 mL/h) to maintain continuous jet without dripping
- Control environmental conditions (temperature 20-25°C, humidity 30-50%)
Scaffold Collection:
- Collect fibers for predetermined time based on desired thickness
- Remove scaffold from collector carefully to maintain structure
- Post-process if needed (crosslinking, sterilization)
Critical Parameters: Solution properties (viscosity, conductivity, surface tension), process variables (voltage, flow rate, collection distance), and environmental conditions (temperature, humidity) significantly influence fiber morphology and diameter [44]. Specific collector configurations including static flat plates, rotating drums, and patterned collectors enable control over fiber alignment and scaffold architecture.
Technical Specifications
Table 3: Electrospinning Parameters and Their Effects on Fiber Properties
| Parameter Category | Specific Parameter | Effect on Fiber Morphology | Optimal Range |
|---|---|---|---|
| Solution Properties | Concentration | Higher concentration increases fiber diameter, prevents bead formation | 5-20% w/v |
| Solvent volatility | Controls fiber drying rate, surface morphology | Medium evaporation rate | |
| Conductivity | Higher conductivity reduces fiber diameter | Adjust with salts | |
| Process Parameters | Voltage | Higher voltage reduces fiber diameter, but too high causes instability | 10-20 kV |
| Flow rate | Higher rate increases diameter, may cause defects | 0.5-3 mL/h | |
| Collection distance | Shorter distance reduces drying time | 10-20 cm | |
| Environmental | Humidity | Affects solvent evaporation, fiber morphology | 30-50% |
| Temperature | Higher temperature reduces solution viscosity | 20-25°C |
Table 4: Electrospinning Applications in Soft Tissue Engineering
| Tissue Type | Polymer System | Fiber Architecture | Functionalization | Key Outcomes |
|---|---|---|---|---|
| Skin | PCL/gelatin blend | Random multilayered | Silver nanoparticles for antimicrobial effect | Enhanced re-epithelialization, reduced infection |
| Nerve | PLLA/PCL | Aligned conduit | NGF-loaded nanoparticles | Directed neurite extension, Schwann cell migration |
| Blood Vessel | PU/silk fibroin | Tubular with controlled porosity | Heparin for anticoagulation | Patency >4 weeks, endothelialization |
| Muscle | PLGA/collagen | Aligned nanofibers | IGF-1 sustained release | Myoblast alignment, contractile function |
Freeze-Drying
Freeze-drying (lyophilization) is a dehydration technique that preserves the structural and functional integrity of sensitive biological materials by removing water under low temperature and pressure conditions [40] [45]. The process involves three primary stages: freezing the material, primary drying (sublimation of ice crystals under vacuum), and secondary drying (removal of unfrozen water by desorption) [45]. In tissue engineering, freeze-drying creates highly porous scaffolds with interconnected networks that facilitate nutrient diffusion and cell infiltration.
The technique is particularly valuable for preserving protein drugs, vaccines, and sensitive biologics, with approximately 50% of biopharmaceuticals on the market being lyophilized formulations [45]. For scaffold fabrication, freeze-drying enables control over pore architecture by manipulating freezing parameters, crystal growth direction, and solution composition.
Experimental Protocol: Scaffold Fabrication by Freeze-Drying
Materials and Equipment:
- Freeze-dryer with temperature and vacuum control
- Polymer solutions or hydrogel precursors
- Mold containers for shaping scaffolds
- Cryoprotectants (sugars, polymers)
Methodology:
- Solution Preparation:
- Prepare polymer solution at desired concentration
- Incorporate bioactive agents if needed (growth factors, drugs)
- Add porogens or control ice crystal formation agents
Freezing Stage:
- Pour solution into molds of desired shape
- Apply controlled freezing protocol (direction, rate)
- Typical freezing rates: 1-5°C/min to -40°C to -80°C
- Annealing step may be included to optimize ice crystal size
Primary Drying (Sublimation):
- Transfer frozen samples to freeze-dryer pre-cooled to shelf temperature
- Apply vacuum (typically 0.01-0.1 mbar)
- Maintain shelf temperature below but close to collapse temperature
- Duration: 24-72 hours depending on sample thickness
Secondary Drying (Desorption):
- Gradually increase shelf temperature to remove bound water
- Typical conditions: 20-25°C for 4-10 hours
- Target residual moisture: <1% for optimal stability
Post-processing:
- Store in moisture-proof containers under inert gas
- Sterilize by gamma irradiation or ethylene oxide
Critical Considerations: The glass transition temperature (Tg') of the formulation determines the maximum product temperature during primary drying without structural collapse. Cryoprotectants including trehalose, sucrose, and dextran are often incorporated to stabilize bioactive components and control pore architecture [45].
Comparative Analysis and Future Directions
Technology Integration and Hybrid Approaches
Each fabrication technique offers distinct advantages that can be leveraged through combinatorial approaches. Integrating electrospinning with 3D printing creates scaffolds with hierarchical structures—nanofibrous surfaces on macro-scale architectures [43]. Similarly, freeze-dried microspheres can be incorporated into bioinks for enhanced drug delivery capabilities within 3D printed constructs.
Emerging research focuses on 4D bioprinting, which adds the dimension of time to create dynamic structures that change shape or functionality in response to environmental stimuli [42]. These advanced fabrication approaches represent the future of tissue engineering, enabling increasingly complex tissue mimics that better replicate native physiology.
Technical Comparison
Table 5: Comparative Analysis of Scaffold Fabrication Techniques
| Parameter | 3D Bioprinting | Electrospinning | Freeze-Drying |
|---|---|---|---|
| Resolution | 50-500 μm | 100 nm-5 μm | 20-300 μm |
| Porosity | Controlled architecture, 70-95% | High porosity (>80%), interconnected | Very high (90-98%), isotropic |
| Scalability | Moderate, patient-specific | High for flat constructs, limited for 3D | Excellent for batch production |
| Cell Encapsulation | Direct incorporation possible | Limited to surface seeding | Post-seeding required |
| Mechanical Properties | Tunable, structure-dependent | Anisotropic, high surface area | Isotropic, typically weak |
| Biomolecule Incorporation | Direct printing or post-loading | Surface adsorption or blend incorporation | Direct incorporation with stability |
Research Reagent Solutions
Table 6: Essential Materials for Scaffold Fabrication
| Material Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Natural Polymers | Collagen, gelatin, chitosan, alginate, hyaluronic acid | ECM mimicry, cell adhesion | Excellent biocompatibility, limited mechanical strength |
| Synthetic Polymers | PLGA, PCL, PEG, PLA | Structural integrity, tunable degradation | Predictable properties, modifiable chemistry |
| Crosslinkers | Genipin, glutaraldehyde, methacrylation, EDC/NHS | Enhance stability, control mechanical properties | Cytotoxicity considerations crucial |
| Bioactive Factors | BMP-2, VEGF, TGF-β, NGF | Direct cell behavior, enhance regeneration | Controlled release kinetics important |
| Conductive Additives | Polypyrrole, carbon nanotubes, graphene | Enhance electrophysiological functionality | Particularly for neural/cardiac tissue |
Workflow Visualization
Scaffold Fabrication Workflow Decision Pathway
The diagram illustrates the integrated workflow for scaffold fabrication using the three featured techniques, highlighting both the common pathway and method-specific processes from design to final application.
3D bioprinting, electrospinning, and freeze-drying represent complementary fabrication technologies that collectively address the diverse requirements of tissue engineering scaffolds. 3D bioprinting excels in creating complex, patient-specific geometries with controlled porosity and direct cell encapsulation. Electrospinning produces nanofibrous scaffolds that closely mimic native ECM structure, particularly valuable for soft tissue applications. Freeze-drying creates highly porous matrices ideal for preserving bioactive molecules and supporting cell infiltration. The optimal selection and combination of these techniques, guided by comprehensive characterization and understanding of structure-function relationships, will drive future advances in regenerative medicine. As these technologies continue to evolve with improvements in resolution, bioactivity, and scalability, they promise to overcome current limitations in tissue engineering and enable the fabrication of increasingly functional tissue constructs for clinical applications.
Bionic scaffolds represent a paradigm shift in regenerative medicine, offering sophisticated three-dimensional architectures that mimic the native extracellular matrix (ECM) to guide tissue regeneration. For cartilage and bone tissues, which possess limited self-repair capabilities, these scaffolds provide not only structural support but also biological cues that direct cellular behavior and tissue formation. The global tissue engineering and regeneration market, valued at $4.8 billion in 2024, is projected to reach $9.8 billion by 2030, growing at a compound annual growth rate (CAGR) of 12.8%, reflecting the significant scientific and commercial interest in this field [46]. This growth is fueled by an aging population, rising chronic disease prevalence, and innovations in biomaterials and fabrication technologies. This technical review examines the fundamental design principles, material options, and experimental methodologies driving advancements in bionic scaffolds for musculoskeletal tissue engineering, providing researchers with a comprehensive reference for scaffold design and evaluation.
Core Design Principles for Ideal Bionic Scaffolds
Essential Characteristics of Effective Scaffolds
The design of bionic scaffolds for cartilage and bone regeneration must balance multiple, often competing, requirements to successfully replicate native tissue function. The core characteristics of ideal scaffolds are summarized in the table below.
Table 1: Key Characteristics of Ideal Bionic Scaffolds for Cartilage and Bone Tissue Engineering
| Characteristic | Technical Specifications | Functional Significance |
|---|---|---|
| Biocompatibility | Non-toxic, non-immunogenic interactions with host tissue [47] | Prevents adverse immune reactions and supports cell viability and integration |
| Biodegradability | Controlled degradation rate matching tissue regeneration pace; non-toxic byproducts [47] | Provides temporary support while gradually transferring load to neotissue |
| Mechanical Properties | Compressive modulus: 0.02-1.16 MPa (superficial cartilage) to 6.44-7.75 MPa (deep cartilage) [47] | Withstands physiological loads while providing appropriate mechanical cues for cell differentiation |
| Structural Properties | Porosity >90%, pore size 100-400 μm, interconnected pore network [47] | Facilitates cell migration, nutrient diffusion, and vascularization |
| Bioactivity | Capacity to deliver growth factors, cells, or drugs [47] | Enhances regeneration through controlled release of therapeutic agents |
Scaffold Design Logic and Implementation Strategy
The following diagram illustrates the systematic approach to designing bionic scaffolds that meet the requirements outlined in Table 1.
Diagram 1: Systematic Workflow for Bionic Scaffold Design. This flowchart outlines the logical progression from initial tissue analysis to clinical application, highlighting how core design parameters inform material and fabrication choices.
Material Platforms for Bionic Scaffolds
Natural Polymer-Based Scaffolds
Natural polymers derived from ECM components offer inherent biocompatibility and biological recognition sites that support cell adhesion and function.
Table 2: Natural Polymer-Based Scaffolds for Cartilage and Bone Regeneration
| Material | Key Advantages | Limitations | Recent Applications |
|---|---|---|---|
| Collagen | Excellent biocompatibility; natural component of ECM; promotes cell adhesion [47] | Poor mechanical strength; rapid degradation | Type I collagen-HA hydrogel for hyaline cartilage regeneration [47] |
| Hyaluronic Acid (HA) | Natural cartilage component; enhances lubrication; supports chondrogenesis [47] | Rapid resorption; weak mechanical properties | HA-transglutaminase hydrogel combined with collagen in ovine model [47] |
| Gelatin | Low immunogenicity; derived from collagen; cost-effective [47] | Poor mechanical properties; requires crosslinking | Pullulan-gelatin cryogel with upregulated glycosaminoglycan production [47] |
| Silk Fibroin | Strong mechanical properties; slow degradation; maintains chondrocyte phenotype [47] | Complex processing; potential immunogenicity | Better chondrocyte phenotype maintenance vs. collagen-based materials [47] |
| Chitosan | Antibacterial properties; biocompatible; molds into various geometries [47] | Variable mechanical properties based on source | Clinical use for patellofemoral osteochondral lesions with microfractures [47] |
Synthetic and Composite Scaffolds
Synthetic polymers offer precise control over mechanical properties, degradation rates, and scaffold architecture, while composite materials combine the advantages of multiple material systems.
Polycaprolactone (PCL)-Based Systems: PCL is an FDA-approved synthetic polymer with excellent biocompatibility and tunable degradation kinetics. A recent study demonstrated a PCL/collagen type I composite scaffold fabricated using low-temperature deposition manufacturing (LDM) 3D printing technology that created a ring and radial fiber structure double-bionic of the natural meniscus [48]. This composite approach compensated for PCL's lack of biofunctional groups while overcoming collagen's mechanical limitations, resulting in a scaffold that promoted meniscus fibrochondrocyte proliferation and increased secretion of collagen and glycosaminoglycan [48].
Electroactive Biomaterials: Innovative electrically conductive scaffolds have shown promise for tissue regeneration. Researchers have developed electroactive, biodegradable scaffolds that integrate electrically conductive components to support bladder tissue regeneration, demonstrating the potential of electroactive materials for various tissue engineering applications [49]. These materials provide ionic conductivity similar to native tissues, which may enhance cell signaling and tissue integration.
Fiber Parameter Control: Synthetic scaffolds allow precise control over fiber diameter, alignment, and porosity, which significantly influences cellular responses. Cells typically exhibit rounded morphology on nanofibers, randomly oriented fibers, and low-porosity scaffolds, while displaying elongated, spindle-shaped morphology on microfibers, aligned fibers, and high-porosity scaffolds [50]. These morphological differences directly impact cell differentiation and tissue formation.
Quantitative Analysis of Scaffold Performance
Experimental Results from Recent Studies
Recent preclinical studies have generated quantitative data on the performance of various bionic scaffolds, providing insights into structure-function relationships.
Table 3: Quantitative Performance Metrics of Bionic Scaffolds in Preclinical Studies
| Scaffold Type | Experimental Model | Key Performance Metrics | Results |
|---|---|---|---|
| PCL/COL I (80/20 ratio) | Rabbit meniscus defect model [48] | - Compressive modulus- Cell proliferation- ECM secretion | Promoted meniscus regeneration; increased collagen and GAG production; recruited stem cells |
| Type I collagen-HA hydrogel | Cartilage defect model [47] | - Hyaline cartilage formation- Integration with native tissue- Mechanical properties | Regenerated hyaline cartilage without additional cellular components |
| Silk fibroin-based scaffold | Chondrocyte culture study [47] | - Chondrocyte phenotype maintenance- Collagen II production- Mechanical strength | Better maintenance of chondrocyte phenotype compared to collagen-based materials |
| Freeze-dried scaffolds | Bone tissue engineering [7] | - Compressive strength- Porosity- Cell attachment | Superior compressive strength and high porosity facilitating effective cell attachment |
Methodology for Scaffold Fabrication and Evaluation
Low-Temperature Deposition Manufacturing (LDM) for PCL/COL I Scaffolds
Materials Preparation:
- Prepare PCL/COL I solutions with varying mass ratios (e.g., 60%PCL/40%COL I, 80%PCL/20%COL I, 90%PCL/10%COL I) by dissolving PCL particles and COL I in a mixture of hexafluoroisopropanol (HFIP) and 1,4-dioxane [48].
- Total mass maintained at 2g with solvent ratios adjusted accordingly (e.g., 2ml HFIP:8ml 1,4-dioxane for 60%PCL/40%COL I) [48].
Scaffold Fabrication:
- Obtain meniscus geometry from Micro-CT scans of New Zealand white rabbit meniscus.
- Process and optimize scan data into ring-shaped radial wedge-shaped meniscus scaffold model using UG software.
- Import model data in STL format to 3D bioprinter equipped with LDM technology.
- Print scaffold in controlled cooling chamber to maintain low temperatures during composite solution deposition [48].
Characterization Methods:
- Morphological Analysis: Freeze-dry scaffold, sputter-coat with gold, and observe microstructure using scanning electron microscopy (e.g., Hitachi S-4800) [48].
- FTIR Analysis: Perform Fourier-transform infrared spectroscopy on freeze-dried samples to analyze chemical composition and interactions between components [48].
- Mechanical Testing: Evaluate compressive and tensile properties using mechanical testing systems to ensure match with native tissue requirements.
- Biological Assessment: Culture meniscus fibrochondrocytes on scaffolds and assess cell proliferation, viability, and ECM production (collagen and GAG quantification) [48].
Freeze-Drying Method for Porous Scaffold Fabrication
Process Parameters:
- Lower freeze-drying temperatures produce denser, more compact scaffold structures due to slower ice crystal formation [7].
- Interconnected porous architectures critical for nutrient diffusion and cell infiltration are achieved through controlled freezing and sublimation cycles [7].
Resulting Scaffold Properties:
- Superior compressive strength appropriate for bone tissue engineering
- High porosity with interconnected pores facilitating cell attachment and proliferation [7]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for Bionic Scaffold Development
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Polycaprolactone (PCL) | Synthetic polymer for scaffold framework; provides mechanical strength and controlled degradation [48] | FDA-approved PCL particles for LDM 3D printing [48] |
| Collagen Type I | Natural ECM component; enhances cell adhesion and biocompatibility [48] | Combined with PCL in composite scaffolds [48] |
| Hyaluronic Acid (HA) | Mimics native cartilage environment; supports chondrogenesis [47] | HA-transglutaminase hydrogels for cartilage defects [47] |
| Hexafluoroisopropanol (HFIP) | Solvent for polymer dissolution in scaffold fabrication [48] | Used in mixture with 1,4-dioxane for PCL/COL I solutions [48] |
| Silk Fibroin | Natural polymer with strong mechanical properties; supports chondrocyte phenotype [47] | Silk-based scaffolds for cartilage regeneration [47] |
| Gelatin | Collagen-derived material with low immunogenicity; requires crosslinking for stability [47] | Pullulan-gelatin cryogels for cartilage-specific ECM production [47] |
| Chitosan | Biocompatible, antibacterial natural polymer; moldable into various geometries [47] | Clinical scaffolds for osteochondral lesions [47] |
Experimental Workflow for Scaffold Validation
The comprehensive evaluation of bionic scaffolds requires a systematic approach from material characterization to functional assessment, as illustrated in the following experimental workflow.
Diagram 2: Comprehensive Experimental Workflow for Scaffold Validation. This flowchart illustrates the key stages in evaluating bionic scaffolds, from initial material characterization to final data analysis, highlighting essential assessment methods at each stage.
Bionic scaffolds represent a promising solution for the significant clinical challenge of cartilage and bone regeneration. The optimal scaffold design requires careful balancing of biocompatibility, mechanical properties, structural characteristics, and bioactivity. Current research demonstrates that composite approaches, combining natural polymers like collagen with synthetic polymers like PCL, often yield superior results by leveraging the advantages of each material type. Advanced fabrication technologies such as LDM 3D printing enable precise control over scaffold architecture, creating structures that closely mimic native tissue organization. As the field progresses, emerging technologies including electroactive biomaterials and smart scaffolds with controlled release capabilities offer exciting opportunities for enhanced tissue regeneration. The continued translation of these technologies from laboratory research to clinical applications holds significant potential for addressing unmet needs in musculoskeletal tissue repair.
The global demand for tissue and organ transplantation significantly outstrips supply, with solid organ transplants covering less than 10% of the global need [51]. Tissue engineering, which utilizes scaffolds to support cell growth and form new tissues, presents a promising solution to this crisis. Traditionally, these scaffolds have been derived from synthetic materials or animal tissues, but these sources face challenges related to cost, biocompatibility, environmental impact, and ethical concerns [52] [51]. In response, research has increasingly turned to sustainable, natural sources, with seaweed emerging as a leading candidate for the next generation of tissue engineering scaffolds [53] [2] [54].
Seaweeds, or macroalgae, are abundant, fast-growing marine organisms that require no arable land, freshwater, or fertilizers to cultivate [2] [54]. Their natural architecture, which includes porous and fibrous networks, closely mimics the human extracellular matrix (ECM) [53] [2]. Furthermore, seaweed-derived polymers such as cellulose, ulvan, and fucoidan exhibit excellent biocompatibility, biodegradability, and bioactivity [2] [54] [55]. This whitepaper provides a technical overview of seaweed-based scaffolds, detailing their sources, properties, fabrication protocols, and performance in preclinical models, framed within the broader context of sustainable biomaterial research for tissue engineering.
Seaweeds are classified into three main groups—red (Rhodophyta), green (Chlorophyta), and brown (Phaeophyta)—each with distinct biochemical profiles that influence their suitability for scaffolding.
Red seaweed, such as Devaleraea mollis (Pacific dulse), has been successfully decellularized to create scaffolds that support the growth of human cardiac muscle cells. Its innate framework provides an excellent anchor for growing cells and tissues [53] [56] [57].
Green seaweed, particularly species of the genus Ulva (sea lettuce), is a promising source of ulvan, a sulfated polysaccharide composed of rhamnose and glucuronic acid residues. Ulvan possesses immunomodulatory, antimicrobial, and anticoagulant properties, making it a versatile candidate for biomaterial design [54]. Ulva also contains substantial amounts of cellulose, hemicellulose, and starch [54].
Brown seaweed, such as Padina sp., contains fucoidan, a sulfated, water-soluble polysaccharide known for its antioxidant, anti-inflammatory, and osteo-inductive properties. Fucoidan's high sulfate content creates a negatively charged surface that attracts water, promoting successful cell adhesion and migration [55].
Table 1: Key Seaweed Species and Their Bioactive Components for Tissue Engineering
| Seaweed Type | Example Species | Key Structural Components | Relevant Bioactivities |
|---|---|---|---|
| Red Seaweed | Devaleraea mollis (Pacific dulse) | Cellulose, Glycosides, Polysaccharides | Excellent biocompatibility with human cardiomyocytes [53] [56] |
| Green Seaweed | Ulva sp. (Sea Lettuce) | Ulvan, Cellulose, Hemicellulose | Immunomodulatory, Antimicrobial, Anticoagulant [54] |
| Brown Seaweed | Padina sp. | Fucoidan, Alginate, Cellulose | Antioxidant, Anti-inflammatory, Osteo-inductive [55] |
A critical advantage of seaweed cellulose over terrestrial plant cellulose is its lack of lignin, which makes extraction less energy-intensive and more cost-effective [2]. Furthermore, the structural diversity of seaweed cellulose—ranging from the porous architecture of Ulva to the fibrous matrix of Cladophora—allows for the tailoring of scaffolds to specific tissue engineering applications [2].
Structural and Functional Properties of Seaweed Scaffolds
The microarchitecture of a scaffold is a critical determinant of its function, as it influences cell migration, nutrient diffusion, and tissue organization. Research on scaffolds derived from green macroalgae Ulva sp. and Cladophora sp. highlights this structure-function relationship.
- Ulva sp. Scaffolds: Feature a comb-like porous structure with an average pore size of 20.2 ± 4 µm. This architecture facilitates multidirectional cell growth and efficient nutrient diffusion, supporting rapid cell proliferation [2].
- Cladophora sp. Scaffolds: Exhibit a dense fibrous matrix composed of fibers ranging from 5 µm to over 80 µm, overlaid with nanoscale microfibrils (55–400 nm). This structure promotes unidirectional cell alignment and stratified tissue organization [2].
These distinct morphologies directly influence cellular behavior. In vitro studies show that the porous Ulva scaffolds support rapid, multidirectional fibroblast proliferation, reaching saturation by week three. In contrast, the fibrous Cladophora scaffolds promote elongated cell growth along the fiber axes with consistent, linear proliferation over time [2].
Table 2: Quantitative In Vivo Biocompatibility Data for Seaweed Cellulose (SC) Scaffolds (8-Week Study in Rat Model) [2]*
| Parameter | Ulva sp. (Porous Scaffold) | Cladophora sp. (Fibrous Scaffold) |
|---|---|---|
| Initial Inflammatory Response (Week 1) | Milder; polymorphonuclear-hemorrhage interspersed in necrotic site [2] | More pronounced; PMNN clusters at the implant's necrotic center [2] |
| Inflammation Resolution | Gradual reduction of PMNNs; smaller necrotic cavities persisted to week 8 [2] | Faster resolution; necrotic center diminished by week 4; no PMNNs by week 8 [2] |
| Foreign Body Reaction (FBR) | Gradual increase in FBGCs by week 4, followed by a steady reduction [2] | Earlier FBR resolution; transformation of macrophages into FBGCs at the implant-tissue interface [2] |
| Tissue Healing Dynamics | Promoted compartmentalized healing with distributed vascularized connective tissue [2] | Supported stratified tissue organization with aligned collagen deposition [2] |
| Structural Integrity | Maintained original dimensions (Ø=8mm, thickness=2mm) through 8 weeks [2] | Maintained original dimensions (Ø=8mm, thickness=1.7mm) through 8 weeks [2] |
Detailed Experimental Protocols
Decellularization of Red Seaweed (Pacific Dulse)
A protocol for decellularizing Pacific dulse (Devaleraea mollis) was optimized to preserve its natural honeycombed architecture while removing cellular material [53] [56].
Key Steps:
- Cleaning and Drying: Native dulse samples are thoroughly cleaned and dried [53].
- Hydrophilicity Treatment: Samples are treated with Sodium Dodecyl Sulfate (SDS) to remove hydrophobic barriers and allow water to penetrate the structure. Concentrations of 10%, 12%, and 15% SDS were found to be most effective for preserving structural integrity [53] [56].
- Cell Removal: The scaffolds are washed with Triton X-100 (2%), a common laboratory detergent, to wash away all cellular material [53] [56].
- Decolorization: Treatment with a low concentration of bleach (Sodium Hypochlorite, NaClO, 0.2%) removes red pigment [53] [56].
- Characterization: The resulting scaffolds are characterized using light microscopy, scanning electron microscopy (SEM), Fourier-transform infrared spectroscopy (FTIR), and Raman spectroscopy to confirm decellularization and structural preservation [56].
Decellularization of Brown Seaweed (Padina sp.)
A different protocol has been established for the decellularization of brown seaweed for bone tissue engineering applications [55].
Key Steps:
- Pigment and Protein Removal: Seaweed biomass is boiled in acetone at 60°C for 60 minutes, repeated four times, to remove chlorophyll and proteins [55].
- Polysaccharide Removal: The residual biomass is boiled in acetate buffer (pH 4.5) at 60°C for 5 hours to remove simpler polysaccharides [55].
- Neutralization and Alkylation: The bleached seaweed is neutralized with distilled water and then alkylated in 0.5M Sodium Hydroxide (NaOH) at 60°C for 4-6 hours to remove excess lipids [55].
- Acid Treatment and Final Processing: Samples are pH-neutralized, acidified in Hydrochloric Acid (HCl) to remove excessive polysaccharides, rinsed, and finally freeze-dried for storage [55].
Diagram 1: Decellularization workflow for red seaweed (Pacific dulse).
In Vivo Biocompatibility Testing
The in vivo performance of seaweed-derived scaffolds is typically evaluated using subcutaneous implantation models to assess integration, immune response, and healing dynamics [2].
Key Steps:
- Implant Preparation: Sterilized seaweed cellulose implants (e.g., 8 mm diameter) are prepared from porous (Ulva sp.) and fibrous (Cladophora sp.) sources [2].
- Animal Model: Implants are subcutaneously implanted in animal models (e.g., Sprague-Dawley rats) [2].
- Tissue Collection and Analysis: Explanted sites are collected at predetermined time points (e.g., 1, 4, and 8 weeks) for histopathological analysis [2].
- Hematoxylin & Eosin (H&E) Staining: Assesses inflammation and general tissue morphology [2].
- Masson's Trichrome Staining: Evaluates collagen deposition, indicating tissue maturation and repair [2].
- Immunohistochemical Staining (e.g., anti-CD31): Visualizes vascularization within the implant site, a critical marker for successful integration [2].
Diagram 2: Key steps for in vivo biocompatibility testing.
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents for Seaweed Scaffold Development
| Reagent/Material | Function in Scaffold Preparation | Example Usage |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Surfactant; removes hydrophobic barriers, facilitating decellularization [53] [56] | Treatment of Pacific dulse at 10-15% concentration [56] |
| Triton X-100 | Non-ionic detergent; washes away cellular material [53] [56] | Used at 2% concentration following SDS treatment [53] |
| Sodium Hypochlorite (NaClO) | Oxidizing agent; removes pigments from the seaweed matrix [53] [56] | Used at 0.2% concentration for decolorization [56] |
| Acetate Buffer | Acidic buffer; removes simpler polysaccharides during decellularization [55] | Used at pH 4.5, 60°C for brown seaweed (Padina sp.) [55] |
| Sodium Hydroxide (NaOH) | Strong base; used for alkylation to remove excessive lipids [55] | Used at 0.5M concentration for brown seaweed processing [55] |
| Hydrochloric Acid (HCl) | Strong acid; removes excessive polysaccharides [55] | Final acidification step in brown seaweed protocol [55] |
Seaweed-derived scaffolds represent a paradigm shift in biomaterial design, offering a powerful combination of clinical efficacy and environmental sustainability. Their innate architectures closely mimic the human extracellular matrix, guiding specific tissue responses from cardiac muscle cells to bone-forming osteoblasts. The renewable nature of seaweed, which requires no arable land or freshwater, underscores its potential as a cornerstone for the future of green, cost-effective biomedical solutions [53] [2] [54]. While challenges in standardization and mechanical tailoring remain, the convergence of marine biology, materials science, and regenerative medicine is paving the way for a new era of eco-friendly tissue engineering that addresses both critical healthcare needs and pressing environmental concerns.
Navigating Complex Challenges: Immune Response, Durability, and Clinical Translation
The field of tissue engineering has undergone a paradigm shift, moving from the design of passive, inert biomaterial scaffolds to the development of active, immunomodulatory platforms that dynamically interact with the host immune system [58]. The success of any implanted biomaterial is fundamentally governed by the host response it elicits, a process orchestrated largely by macrophages [59] [60]. These innate immune cells exhibit remarkable functional plasticity, enabling them to adopt a spectrum of activation states in response to local environmental cues [59]. Traditionally, this spectrum is simplified into pro-inflammatory (M1) and anti-inflammatory/pro-regenerative (M2) phenotypes [61]. A timely transition from a pro-inflammatory M1-dominated phase to a pro-regenerative M2-dominated phase is critical for successful tissue integration and regeneration [62] [60].
Within the context of a broader thesis on biomaterial scaffolds for tissue engineering, this review posits that rational biomaterial design must prioritize the active modulation of macrophage polarization. This approach moves beyond merely evading the immune system towards deliberately harnessing it to create a pro-regenerative microenvironment. The following sections will detail the molecular mechanisms of macrophage polarization, the specific biomaterial properties that influence it, and the advanced strategies employed by next-generation "smart" biomaterials. Furthermore, this guide provides a practical toolkit for researchers, including standardized experimental protocols and a curated list of research reagents, to facilitate the translation of these concepts into laboratory practice.
Macrophage Polarization: Mechanisms and Significance in Tissue Regeneration
The Spectrum of Macrophage Phenotypes
Macrophages are not terminally differentiated cells but exist in a state of functional plasticity, allowing them to dynamically shift their phenotype in response to changing signals within the microenvironment [59]. The classical M1 phenotype is induced by stimuli such as interferon-gamma (IFN-γ) and bacterial lipopolysaccharide (LPS). These macrophages are characterized by high expression of pro-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6, IL-12), the production of reactive oxygen species (ROS), and inducible nitric oxide synthase (iNOS) [59] [61]. Their primary role is host defense against pathogens and debris clearance in the initial phases of wound healing [62].
In contrast, the M2 phenotype is induced by cytokines such as IL-4, IL-10, and IL-13 [59]. M2 macrophages are associated with tissue repair and regeneration, producing anti-inflammatory cytokines like IL-10 and TGF-β, as well as growth factors (e.g., VEGF, PDGF, BMP-2) that promote angiogenesis, matrix deposition, and resolution of inflammation [62] [60]. It is important to note that the M2 classification encompasses several subtypes (M2a, M2b, M2c, M2d), each with distinct functions in immunoregulation, matrix remodeling, and angiogenesis [59].
The following diagram illustrates the key signaling pathways and biomarkers associated with M1 and M2 macrophage polarization.
The Critical Role of Macrophage Dynamics in Bone Regeneration
The process of bone healing provides a clear example of the importance of temporal macrophage dynamics. Following a fracture, an initial pro-inflammatory phase is characterized by the dominance of M1 macrophages [59] [62]. This phase is essential for clearing debris and initiating the healing cascade. Subsequently, a transition to an M2-dominated phase is required to resolve inflammation and support osteogenesis and angiogenesis through the secretion of factors like TGF-β and BMP-2 [62]. A failure in this M1-to-M2 transition is associated with impaired healing and chronic inflammation, as often seen in conditions like osteomyelitis [62]. Therefore, biomaterial strategies that can actively promote this phenotypic switch are highly desirable for bone tissue engineering applications.
Biomaterial Design Parameters for Modulating Macrophage Polarization
The physical and chemical properties of biomaterials provide a powerful toolkit for directing macrophage polarization. These properties are not passive features but act as active instructional cues that are sensed by immune cells.
Physical Cues
Surface Topography and Pore Architecture: The physical microstructure of a scaffold, including its surface texture and pore size, significantly influences macrophage morphology and phenotype. Studies using 3D scaffolds fabricated via two-photon polymerization have demonstrated that pore size can finely tune the macrophage response. Large pores (e.g., 50×50×20 μm³) have been shown to upregulate the M2 marker Arg1, while smaller pores (e.g., 15×15×15 μm³) promote a more M1-like state, marked by increased iNOS expression [63]. This highlights the potential of tailoring scaffold architecture to induce desired immune responses.
Stiffness: The mechanical stiffness of a substrate is a critical determinant of macrophage polarization. Macrophages cultured on softer substrates (mimicking the elasticity of healthy, soft tissues) tend to polarize towards an M2 phenotype. In contrast, stiffer substrates promote a pro-inflammatory M1 state, characterized by increased expression of genes like iNOS and TNF-α [64]. For bone regeneration, matching the scaffold stiffness to that of native bone may help in reducing adverse immune reactions.
Table 1: Impact of Biomaterial Physical Properties on Macrophage Polarization
| Property | Pro-Inflammatory (M1) Cue | Pro-Regenerative (M2) Cue | Proposed Mechanism |
|---|---|---|---|
| Stiffness | High stiffness (rigid polyacrylamide gels) [64] | Low stiffness (soft, compliant substrates) [64] | Activation of mechanosensitive pathways (e.g., NF-κB) |
| Topography/Porosity | Small pore sizes (15×15×15 μm³) [63] | Large pore sizes (50×50×20 μm³) [63] | Altered cytoskeletal organization and nuclear shape |
| Surface Roughness | Micron-scale sharp features | Nano-scale smooth or grooved textures | Focal adhesion complexity and inflammatory signaling |
Chemical and Biological Cues
Surface Chemistry and Hydrophilicity: The chemical composition of a biomaterial's surface dictates protein adsorption, which in turn influences how macrophages perceive the implant. Hydrophilic surfaces generally promote M2 polarization and improve tissue integration, whereas hydrophobic surfaces often trigger an M1 response and foreign body reaction [59] [60]. Incorporating specific biological signals, such as the RGD peptide sequence, can also enhance M2 polarization by facilitating integrin-mediated adhesion [60].
Bioactive Molecule Delivery: A primary strategy for immunomodulation is the controlled release of bioactive molecules from the biomaterial scaffold. The sustained delivery of M2-promoting cytokines such as IL-4 or IL-10 has been successfully used to steer macrophages towards a pro-regenerative phenotype [64] [62]. Furthermore, the molecular weight of natural polymers can influence the response; for instance, high molecular weight hyaluronic acid promotes an anti-inflammatory state, while its shorter fragments are inflammatory [64].
Table 2: Biomaterial Chemical Strategies for Immunomodulation
| Strategy | Specific Example | Effect on Macrophages | Key References |
|---|---|---|---|
| Cytokine Delivery | Controlled release of IL-4, IL-10, or IL-13 | Promotes M2 polarization; drives tissue repair | [64] [62] |
| Surface Functionalization | Grafting of RGD peptides or anti-inflammatory molecules | Enhances M2 marker expression (CD206) | [60] |
| Molecular Weight Control | Use of high molecular weight Hyaluronic Acid | Induces anti-inflammatory gene expression | [64] |
| Mitochondrial Targeting | Delivery of therapeutics to macrophage mitochondria | Modulates metabolic state to influence polarization | [65] |
Advanced Smart Biomaterials and Hydrogel Systems
The next frontier in biomaterial science involves the development of "smart" or responsive systems that can dynamically interact with the biological microenvironment.
Classification of Biomaterial Smartness
The evolution of biomaterials can be categorized by their level of interactivity, ranging from inert to autonomous systems [58] [9]. The following diagram outlines this progression.
Stimuli-Responsive and Immunomodulatory Hydrogels
Hydrogels have emerged as particularly promising platforms, especially for treating complex scenarios like infected bone defects (osteomyelitis) [62]. These water-swollen polymer networks can be engineered to be stimuli-responsive, releasing their payload or changing properties in response to specific pathological triggers:
- pH-Responsiveness: Releasing antibiotics or immunomodulators in the acidic microenvironment of a bacterial infection or inflammatory site [58] [9].
- Enzyme-Responsiveness: Degrading in the presence of matrix metalloproteinases (MMPs) that are overexpressed in chronic wounds, thereby delivering factors precisely where needed [58].
These advanced hydrogels function as multifunctional therapeutic systems that not only control infection through localized antibiotic delivery but also actively resolve the associated detrimental inflammation by driving the macrophage phenotype switch from M1 to M2, thereby creating a pro-regenerative milieu conducive to bone healing [62].
The Scientist's Toolkit: Research Reagent Solutions
To empirically investigate macrophage-biomaterial interactions, a standardized set of tools and assays is required. The following table catalogs key research reagents and their applications in this field.
Table 3: Essential Research Reagents for Studying Macrophage-Biomaterial Interactions
| Reagent / Tool Category | Specific Examples | Primary Function in Research |
|---|---|---|
| Polarizing Cytokines | IFN-γ, LPS (for M1); IL-4, IL-10, IL-13 (for M2) | To generate reference M1 and M2 macrophage populations in vitro for comparison with biomaterial-conditioned cells. |
| Flow Cytometry Antibodies | Anti-CD80, CD86, MHC-II (M1); Anti-CD206, CD163, CD209 (M2) | To quantify the expression of canonical surface markers and define the polarization state of macrophages. |
| Gene Expression Assays | Primers/probes for iNOS, TNF-α, IL-1β (M1); Arg1, Ym1, FIZZ1 (M2) | To assess transcriptional changes in polarization markers using qRT-PCR. |
| Cytokine Detection | ELISA or Multiplex Assays for TNF-α, IL-12, IL-6 (M1); TGF-β, IL-10 (M2) | To measure the functional secretory profile of macrophages. |
| Engineered Scaffolds | 3D scaffolds with tunable pore size (Two-Photon Polymerization); Hydrogels with variable stiffness | To systematically study the impact of specific physical properties on macrophage behavior. |
| Mitochondrial Probes | MitoTrackers, JC-1, TMRM | To assess mitochondrial membrane potential and function, linked to metabolic polarization states [65]. |
Detailed Experimental Protocol: Evaluating Macrophage Response to 3D Scaffolds
This protocol provides a methodology for assessing the immunomodulatory capacity of 3D biomaterial scaffolds in vitro, using macrophage polarization as a key readout.
Scaffold Preparation and Sterilization
- Fabrication: Fabricate scaffolds using an appropriate method (e.g., two-photon polymerization for precise 3D architectures [63], or electrospinning for fibrous scaffolds).
- Sterilization: Sterilize scaffolds using methods compatible with the material (e.g., ethanol immersion, UV irradiation, or ethylene oxide gas).
- Pre-conditioning: Immerse the sterile scaffolds in cell culture medium (e.g., RPMI-1640 with 10% FBS) for 24 hours at 37°C to allow for protein adsorption and stabilize the material.
Macrophage Culture and Seeding
- Cell Line: Use a human (THP-1) or murine (RAW 264.7) macrophage cell line. Differentiate THP-1 monocytes into macrophages by treating with 100 ng/mL Phorbol 12-myristate 13-acetate (PMA) for 48 hours.
- Seeding: Seed macrophages onto the pre-conditioned scaffolds and tissue culture plastic (TCP) controls at a density of 1-5 x 10^5 cells per scaffold, depending on scaffold volume and porosity.
- Culture Period: Maintain cultures for a pre-defined period (e.g., 1, 3, and 7 days) to capture both early and late responses.
Sample Collection and Analysis
- Gene Expression (qRT-PCR): At each time point, lyse cells directly on the scaffold to extract RNA. Analyze the expression of key M1 (iNOS, TNF-α, IL-1β) and M2 (Arg1, CD206, Ym1) markers. Normalize data to housekeeping genes (GAPDH, β-actin) and report as fold-change relative to control.
- Protein Secretion (Cytokine ELISA): Collect conditioned media from the cultures. Quantify the secretion of M1 (TNF-α, IL-6) and M2 (IL-10, TGF-β) cytokines using commercially available ELISA kits.
- Cell Phenotype (Flow Cytometry): Carefully dissociate cells from the scaffolds using enzymatic or mechanical methods. Stain the cells with fluorescently conjugated antibodies against M1 (CD80, CD86) and M2 (CD206, CD163) surface markers. Analyze using flow cytometry.
- Cell Morphology (Immunofluorescence): Fix cells on scaffolds and stain for F-actin (e.g., with phalloidin) and nuclei (DAPI). Use confocal microscopy to visualize and quantify cell morphology, cytoskeletal organization, and infiltration into the scaffold [63].
Data Interpretation
A successful pro-regenerative scaffold will demonstrate a shift in macrophage response over time, characterized by an initial, controlled M1 response at day 1, followed by a significant increase in M2 markers and a decrease in M1 markers by days 3 and 7, relative to control surfaces that may sustain an M1 profile.
The strategic management of the host immune response through biomaterial design is no longer a supplementary consideration but a central tenet of effective tissue engineering. By manipulating physical, chemical, and biological properties, scaffolds can be engineered to actively guide macrophage polarization from a pro-inflammatory to a pro-regenerative state, thereby creating a microenvironment conducive to healing and integration.
Future directions in the field point towards increasing sophistication, including the development of autonomous biomaterials capable of closed-loop feedback [58], the integration of artificial intelligence for personalized scaffold design [60], and a deeper exploration of metabolic regulation (e.g., via mitochondria-targeting [65]) to control immune cell function. The translation of these advanced immunomodulatory strategies from the laboratory to the clinic holds the promise of significantly improving the outcomes of regenerative medicine therapies for bone and other tissues.
In the field of tissue engineering, biomaterial scaffolds serve as temporary three-dimensional frameworks that support cell attachment, proliferation, and differentiation, ultimately leading to the formation of new functional tissues. The success of these scaffolds hinges on two critical and often competing properties: mechanical strength and biodegradation rate. The mechanical properties must withstand in vivo forces and maintain structural integrity, while the degradation profile must synchronize with the pace of new tissue formation to ensure a seamless transition from scaffold to native tissue [66] [67].
Achieving an optimal balance between these properties presents a significant challenge for researchers and clinicians. If a scaffold degrades too quickly, it risks losing mechanical integrity prematurely, potentially leading to structural failure before the new tissue can bear loads. Conversely, if degradation is too slow, the scaffold may persist too long, potentially impeding tissue regeneration or causing chronic inflammatory responses [66] [68]. This technical guide explores the fundamental principles, material strategies, and experimental methodologies essential for optimizing this critical interplay, with a focus on applications in bone, cartilage, and soft tissue engineering.
Fundamental Principles and Key Challenges
The Role of Scaffold Mechanics in Tissue Regeneration
The mechanical properties of a scaffold are not merely passive requirements for handling and implantation; they actively influence cellular behavior and tissue development through mechanotransduction pathways. Mesenchymal stromal cells (MSCs), for instance, demonstrate lineage commitment influenced by substrate stiffness. Research indicates that MSCs cultured on stiffer substrates (elastic moduli of 25–40 kPa) commit to osteogenic lineages, while softer matrices (approximately 1 kPa) promote chondrogenic differentiation, with increased expression of collagen-Ⅱ [69]. Signaling molecules such as RhoA/ROCK/myosin II, YAP/TAZ, TGF-β, and Wnt/β-catenin are involved in this stiffness-regulated differentiation [69]. Therefore, matching the scaffold's mechanical properties to the target tissue is crucial for guiding correct tissue regeneration.
Table 1: Mechanical Properties of Native Human Tissues for Benchmarking
| Tissue Type | Tensile Strength (MPa) | Compressive Strength (MPa) | Young's Modulus | Key Components |
|---|---|---|---|---|
| Cortical Bone | 50-150 | 130-230 | 7-30 GPa | Hydroxyapatite, Collagen I |
| Cancellous Bone | 10-100 | 2-12 | 0.02-0.5 GPa | Hydroxyapatite, Collagen I |
| Articular Cartilage | 10-40 | - | 0.5-25 MPa (Compressive Modulus) | Collagen II, Proteoglycans |
| Soft Tissues (e.g., skin, blood vessels) | 5-20 | - | 0.1-500 MPa | Collagen, Elastin |
Understanding Biodegradation Kinetics
Biodegradation is the biological catalytic process that breaks down complex macromolecules into smaller, less complex molecular structures (by-products) [68]. The degradation mechanism can occur through bulk erosion (where degradation happens throughout the material) or surface erosion (where degradation proceeds from the surface inward). Key mechanisms include:
- Hydrolysis: Cleavage of chemical bonds (e.g., ester, ether, amide, anhydride) by water [66] [68].
- Enzymatic Degradation: Specific enzymes target and break particular chemical bonds [68].
The ideal scaffold should maintain mechanical integrity during the initial phases of healing (typically 4-12 weeks for bone) and then gradually degrade, transferring load to the newly formed tissue. This prevents issues like "stress-shielding," where the scaffold bears most of the load, hindering proper tissue maturation and leading to poor integration or failure [66] [67].
Primary Challenges in Balancing Properties
- Mismatched Degradation and Tissue Growth Rates: Rapid degradation can outpace tissue formation, while slow degradation can physically impede tissue growth and remodeling [66] [52].
- Inflammatory Response to Degradation By-products: Some materials, like certain polyesters (e.g., PLA, PGA), produce acidic by-products upon degradation that can lower the local pH, potentially causing localized inflammation or tissue necrosis [66] [52].
- Loss of Mechanical Function During Degradation: The decline in mechanical properties (e.g., strength, modulus) must be predictable and should ideally mirror the increase in mechanical competence of the newly formed tissue [66] [68].
- Species-Specific Variability in Preclinical Models: Differences in healing rates and immune responses between animal models (e.g., sheep, pigs, goats) and humans make direct translation of degradation profiles challenging [66].
Material Systems and Their Properties
The choice of biomaterial forms the foundation for tuning mechanical and degradation properties. Materials can be broadly categorized into synthetic polymers, natural polymers, metals, and ceramics, each with distinct advantages and limitations.
Table 2: Comparison of Key Biomaterial Classes for Scaffolds
| Material Class | Examples | Typical Tensile/Compressive Strength | Degradation Time | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| Synthetic Polymers | PLA, PGA, PCL, PLGA [66] [70] | Varies widely; PCL/PLCL blend: ~147 kPa - 434 kPa [70] | Months to years (tunable) [70] [52] | Tailorable mechanical properties and degradation rates; consistent quality [66] [71] | Acidic degradation byproducts; limited bioactivity; potential inflammation [66] [52] |
| Natural Polymers | Collagen, Chitosan, Alginate, Starch [52] | Generally lower strength (e.g., soft hydrogels) [52] | Days to months [52] | Excellent biocompatibility; inherent bioactivity; cellular recognition sites [52] | Low mechanical strength; batch-to-batch variability; rapid degradation [52] |
| Biodegradable Metals | Mg alloys, Fe-Mn alloys [66] [72] | Fe-35%Mn TPMS scaffold: High strength [72] | Months to years [66] | High mechanical strength (bone-like); osteogenic potential (Mg) [66] [72] | Rapid degradation & gas formation (Mg); corrosion control challenges [66] |
| Bio-ceramics & Composites | Hydroxyapatite (HA), β-Tricalcium Phosphate [66] [73] | High compressive strength, but brittle [66] | Very slow (years) [66] | Excellent osteoconductivity; bioinert or bioactive [66] [73] | Brittleness; low tensile strength; difficult processing [66] |
Composite Material Strategies
To overcome individual material limitations, composite strategies have been developed:
- Polymer-Ceramic Composites: Combining PLA with hydroxyapatite (HA) enhances the osteoconductivity and compressive modulus of the polymer while providing a more controlled degradation profile compared to pure ceramics [66] [73]. The HA particles act as a buffer against acidic degradation products, mitigating local pH drops [66].
- Polymer-Polymer Blends and Hybrids: Blending polymers like PCL and PLCL allows for the adjustment of degradation rates and mechanical performance. For instance, a PCL/PLCL blend (1:3 ratio) was developed to tailor degradation time and improve rebound properties for soft tissue engineering [70].
- Natural-Synthetic Hybrids: Combining natural polymers like chitosan or alginate with synthetic polymers like PEG or PLA can improve the mechanical robustness of natural polymers while maintaining good bioactivity [69] [52].
Strategies for Optimizing the Balance
Material Design and Selection
The molecular structure of the polymer backbone directly influences its degradation rate. For polyesters, the following general trends are observed:
- Crystallinity: More crystalline regions (e.g., in PCL) are less accessible to water, leading to slower degradation compared to amorphous regions (e.g., in PLA) [66] [70].
- Hydrophilicity/Hydrophobicity: Hydrophobic polymers degrade more slowly than hydrophilic ones.
- Copolymer Composition and Ratio: Using copolymers like PLGA allows precise tuning of degradation rates by varying the ratio of its lactic and glycolic acid components [66].
Advanced Fabrication and Post-Processing Techniques
Additive Manufacturing (3D Printing) 3D printing enables the creation of scaffolds with complex, patient-specific geometries and controlled internal architectures, such as pore size, shape, and connectivity [66] [73]. This control directly impacts both mechanical properties and degradation. For example, Triply Periodic Minimal Surface (TPMS) designs (e.g., gyroid, diamond, Schwarz primitive) in Fe-Mn scaffolds have shown how geometry influences both mechanical strength and corrosion (degradation) behavior [72].
Post-Processing Treatments
- Pre-Heat Treatment: Applying pre-heat treatment to PCL/PLCL blend solutions before the Thermally Induced Phase Separation (TIPS) process has been shown to significantly improve mechanical strength (tensile strength, elastic modulus, and strain) by altering the microstructure, such as increasing strut size [70].
- Crosslinking: Chemical or physical crosslinking of natural polymers like collagen, alginate, or chitosan can enhance their mechanical strength and slow down their degradation rate [52].
Bioactive Modifications
- Surface Coatings: Applying bioactive coatings, such as calcium phosphate on magnesium alloys, can create a barrier that initially slows down the corrosion rate, allowing the implant to maintain mechanical integrity longer while promoting bone integration [66].
- Incorporation of Bioactive Molecules: Embedding growth factors (e.g., Bone Morphogenetic Proteins - BMPs) into scaffolds can enhance tissue regeneration, effectively compensating for any temporary mechanical deficits during the degradation process by accelerating functional tissue formation [66] [73].
Experimental Protocols for Evaluation
Rigorous in vitro and in vivo evaluation is essential to characterize and validate the performance of engineered scaffolds.
In Vitro Degradation Assessment
The following protocol, aligned with ASTM F1635-11 guidelines, outlines a standard method for assessing scaffold degradation in simulated physiological conditions [68].
Objective: To quantitatively evaluate the mass loss, morphological changes, and mechanical property decay of a scaffold over time in simulated body fluid (SBF).
Materials and Reagents:
- Phosphate Buffered Saline (PBS): pH 7.4, as a standard degradation medium.
- Tris-Buffer with Enzymes: For enzymatic degradation studies (e.g., with collagenase for collagen-based scaffolds, lipase for polyesters).
- Specimen Scaffolds: Sterilized, pre-weighed and characterized scaffolds (n≥5 per time point).
- Incubation Environment: Shaking water bath or orbital incubator maintained at 37°C.
Procedure:
- Pre-degradation Characterization (Day 0):
- Record the initial dry mass (W₀) using a high-precision balance (≥0.1 mg accuracy).
- Measure initial mechanical properties (e.g., compressive/tensile modulus and strength).
- Image the scaffold microstructure using Scanning Electron Microscopy (SEM).
- Analyze chemical composition via Fourier Transform Infrared Spectroscopy (FTIR) or other techniques.
Immersion and Incubation:
- Immerse each scaffold in a sufficient volume of pre-warmed degradation medium (e.g., PBS) to ensure sink conditions (typical volume-to-mass ratio > 50:1).
- Place samples in an incubator at 37°C.
Sampling and Analysis at Predefined Time Points:
- At each time point (e.g., 1, 7, 14, 28, 56 days), remove samples from the incubation medium (n≥3).
- Rinsing and Drying: Rinse retrieved samples with deionized water and dry to a constant weight in a vacuum desiccator.
- Gravimetric Analysis: Weigh the dried samples (Wₜ). Calculate the mass loss percentage:
Mass Loss (%) = [(W₀ - Wₜ) / W₀] × 100. - pH Monitoring: Record the pH of the degradation medium at each change.
- Mechanical Testing: Perform mechanical tests on the wet or rehydrated samples to determine the retention of properties.
- Morphological Analysis: Examine the scaffold surface and cross-section using SEM to observe pore structure, surface erosion, crack formation, etc.
- Chemical Analysis: Use FTIR, Gel Permeation Chromatography (GPC) for molecular weight changes, or HPLC to identify and quantify degradation by-products.
In Vivo Evaluation in Large Animal Models
Large animal models (e.g., sheep, pigs, goats) are critical for bridging the gap between lab research and human clinical applications due to their anatomical and physiological similarities to humans [66].
Protocol Outline for Orthopedic Implant Evaluation in a Sheep Model:
- Scaffold Implantation: Create a critical-sized bone defect (e.g., in the femoral condyle or tibia) and implant the test scaffold, with a positive control (autograft) and a negative control (empty defect or commercial product), following approved ethical guidelines.
- Post-Op Monitoring: Monitor animals for weight-bearing, signs of infection, or inflammation.
- Longitudinal Analysis: Use micro-Computed Tomography (μCT) at 4, 8, and 12 weeks to non-destructively monitor bone ingrowth and scaffold degradation in 3D.
- Terminal Analysis (at 12 weeks):
- Mechanical Testing: Perform a push-out test or a 3-point bending test on the explanted bone-scaffold construct to assess interfacial strength and integration.
- Histology: Process explanted tissues, section them, and stain (e.g., with H&E, Masson's Trichrome, Toluidine Blue). This allows for qualitative and semi-quantitative assessment of:
- New bone formation and its integration with the scaffold.
- The extent of scaffold degradation.
- Cellular response (osteoblasts, osteoclasts, inflammatory cells).
- Statistical Analysis: Compare results between test and control groups using appropriate statistical tests (e.g., ANOVA with post-hoc tests) to determine significance.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Materials and Reagents for Scaffold Research
| Item | Function/Application | Key Considerations |
|---|---|---|
| Polycaprolactone (PCL) | Synthetic polymer for scaffolds; provides long degradation time and good elasticity [70]. | Often blended with other polymers (e.g., PLCL) to adjust degradation profile [70]. |
| Polylactic Acid (PLA) | A common, FDA-approved synthetic polymer with tunable mechanical properties [66]. | Degradation produces acidic by-products; can be copolymerized with GA to form PLGA [66]. |
| Hydroxyapatite (HA) | Calcium phosphate ceramic; used as a powder or coating to enhance osteoconductivity in composites [66] [73]. | Improves compressive strength and buffers acidic degradation by-products of polymers [66]. |
| Mg-based Alloys | Biodegradable metals for load-bearing applications (e.g., orthopedic screws) [66]. | Prone to rapid degradation and hydrogen gas formation; requires alloying/surface treatment [66]. |
| Chitosan | Natural polymer derived from chitin; used in hydrogels and scaffolds for its biocompatibility and hemostatic properties [52]. | Mechanical properties are often enhanced through crosslinking or composite formation [52]. |
| Hyaluronic Acid (HA) | Natural polysaccharide; used in hydrogels for cartilage regeneration and as a lubricant [69]. | Often chemically modified (e.g., methacrylated) to improve mechanical strength [69]. |
| Bone Morphogenetic Protein-2 (BMP-2) | A growth factor incorporated into scaffolds to actively induce osteogenic differentiation and bone formation [66]. | Requires controlled release systems; high doses can have side effects. |
| Crosslinking Agents (e.g., Genipin, Glutaraldehyde) | Used to crosslink natural polymers like collagen or gelatin to improve mechanical strength and slow degradation [52]. | Biocompatibility of the crosslinker and its by-products must be evaluated. |
The field of biomaterial scaffolds is rapidly advancing with the integration of emerging technologies. Smart implants embedded with biosensors are being developed to provide real-time, non-invasive monitoring of parameters like strain, pH, and temperature, offering direct insight into the scaffold's performance and the healing process in vivo [66]. 4D printing, where 3D-printed structures can change their shape or properties over time in response to specific stimuli (e.g., pH, temperature), presents a revolutionary approach for creating dynamic scaffolds that can better adapt to the healing environment [74]. Furthermore, the use of gene-activated bioinks is exploring the incorporation of genetic material into scaffolds to direct cellular behavior more precisely from within, offering a powerful tool for enhancing tissue regeneration [73].
In conclusion, optimizing the interplay between mechanical strength and biodegradation is a complex, multi-faceted challenge central to the success of tissue engineering scaffolds. A successful strategy requires an integrated approach combining rational material design, advanced fabrication technologies, and thorough biological evaluation. By leveraging composite material systems, patient-specific designs enabled by 3D printing, and bioactive functionalization, researchers can create sophisticated scaffolds that provide temporally and spatially appropriate mechanical support while harmoniously degrading in concert with new tissue growth. This balance is not a fixed target but a dynamic process that, when mastered, paves the way for the next generation of regenerative medicine therapies.
Overcoming Vascularization Hurdles to Support Large Tissue Constructs
The quest to engineer large, functional tissues is a cornerstone of regenerative medicine, yet a persistent and significant challenge remains: the creation of integrated, hierarchical vascular networks capable of supporting cell survival post-implantation. Without a robust blood supply to deliver oxygen and nutrients, cells within thick tissue constructs (>1-2 mm³) face rapid necrosis, leading to implant failure [75] [76]. This vascularization hurdle is the critical bottleneck limiting the clinical translation of engineered tissues for the repair of significant defects. Within the context of biomaterial scaffolds for tissue engineering, overcoming this barrier requires a multi-faceted strategy that mimics the body's own complex mechanical and biological environments. This guide details the current mechanical, structural, and biological strategies—from the optimization of scaffold properties and the integration of patterned channels to the spatiotemporal delivery of growth factors—that are being leveraged to pre-vascularize tissue constructs and ensure their rapid anastomosis with the host vasculature upon implantation [75] [77].
Core Challenges in Tissue Vascularization
The primary obstacle in engineering large tissues is the diffusion limit of oxygen and nutrients, which is approximately 100-200 µm [76]. This makes the central, core regions of larger constructs vulnerable to cell death. Furthermore, the body's natural angiogenic response from host vessels is relatively slow, progressing at a rate of only ~5 µm/hour, which is insufficient to rescue a large implant from ischemia [75]. An ideal engineered vascular network must therefore meet several stringent criteria: it must be dense enough for no cell to be more than 20 µm from a blood vessel, hierarchically structured from large vessels to capillaries, mature and stable to prevent leakage, and capable of rapid surgical integration with the host's circulatory system [75] [78]. Tumor angiogenesis research reveals that dysfunctional, leaky vasculature can exacerbate hypoxia and interstitial pressure, underscoring the need for engineered vessels to be functionally normalized [79].
Mechanical and Scaffold-Based Strategies
Mechanical cues from the scaffold microenvironment play a fundamental role in guiding vasculogenesis and angiogenesis. Cells sense and respond to physical properties such as stiffness, topography, and spatial structure through a process called mechanotransduction, activating biochemical pathways that influence cell adhesion, proliferation, migration, and ultimately, vascular network formation [75].
Optimization of Scaffold Physical Properties
The physical properties of a scaffold are critical determinants of its success in supporting vascularization.
- Stiffness: Substrate stiffness profoundly affects endothelial cell (EC) function. Within a physiologically relevant range, a higher stiffness promotes EC adhesion, proliferation, and capillary-like tube formation. However, excessively stiff substrates can disrupt cell-cell junctions, impede collective migration, and promote inflammatory responses, highlighting the need for a balanced approach [75] [78].
- Surface Topography and Anisotropy: Introducing micro-grooves, aligned nanofibers, or other anisotropic structures into the scaffold provides contact guidance, directing the migration of ECs and the alignment of the resulting vascular networks. This controlled alignment is crucial for promoting better integration with the host's often-anisotropic blood vessels [75] [80].
- Pore Structure: An interconnected, hierarchical pore structure is beneficial for both the in vitro formation of vascular networks and the subsequent ingrowth of host blood vessels post-implantation. The pores must be large and interconnected enough to allow for cell infiltration, vessel ingrowth, and nutrient diffusion [75].
Table 1: Scaffold Physical Properties and Their Influence on Vascularization
| Scaffold Property | Target Range/Type | Impact on Vascularization |
|---|---|---|
| Stiffness | Physiologically tuned (e.g., 1-50 kPa for soft tissues) | Promotes EC adhesion, proliferation, and tube formation; excessive stiffness disrupts junctions [75]. |
| Surface Roughness/Anisotropy | Aligned fibers, micro-grooves | Provides contact guidance for EC migration and vascular network alignment [75]. |
| Pore Structure | Interconnected, hierarchical | Facilitates host vessel ingrowth and nutrient diffusion; supports self-assembly of vascular networks [75]. |
| Fractal Dimension/Lacunarity | Tunable via processing (e.g., heat treatment) | Measures microarchitecture complexity; influences cell adhesion and tissue integration [81]. |
Incorporation of Pre-Formed Channels and Microfabrication
A highly effective strategy to overcome diffusion limits is the incorporation of hollow, perfusable channels within scaffolds that serve as a template for rapid blood perfusion. These channels can be created using various advanced fabrication techniques.
- 3D Printing: Technologies like 3D bioprinting allow for the direct fabrication of customizable channel networks within hydrogel or polymer scaffolds. A 2025 study combined 3D printing with phase separation to create polycaprolactone (PCL) tubes that enhanced nutrient perfusion and supported the self-assembly of robust microvascular networks in cardiac tissues [82].
- Micropatterning and Layer-by-Layer Stacking: Photolithography can be used to create precise two-dimensional patterns (e.g., hexagonal structures) in hydrogels like Gelatin Methacryloyl (GelMA). These patterned layers can be stacked to form thick, large-scale constructs. Computational fluid dynamics modeling is often used to optimize the design of these structures to maximize transport diffusivity [77].
- Decellularized Natural Templates: Plant-based scaffolds, such as decellularized leatherleaf viburnum leaves, offer a naturally derived, sustainable vascular architecture. These cellulose-based scaffolds can be engineered into small-diameter vascular grafts. Mild alkaline heat treatment (30-35°C) has been shown to improve their biocompatibility and endothelial cell seeding efficiency without compromising mechanical integrity, achieving burst pressures ≥820 mmHg [81].
Table 2: Fabrication Techniques for Pre-Formed Channel Networks
| Fabrication Technique | Key Material Example | Key Outcome/Performance |
|---|---|---|
| 3D Printing & Phase Separation | Polycaprolactone (PCL) | Enabled formation of biomimetic vascular tubes supporting microvascular networks and enhancing cardiomyocyte function [82]. |
| Micropatterning & Stacking | Gelatin Methacryloyl (GelMA) | Created hexagonal-patterned, multi-layered hydrogels that supported rapid vascularization in diabetic mice [77]. |
| Decellularized Plant Scaffolds | Leatherleaf viburnum cellulose | Produced small-diameter grafts with suture retention strength and burst pressure suitable for implantation [81]. |
The following workflow diagram illustrates the typical process for creating and validating a vascularized tissue construct using micropatterning techniques.
Biological and Biochemical Signaling Strategies
Beyond physical structure, the biochemical environment is paramount for inducing stable and mature vascular networks. This involves the delivery of specific cells, growth factors, and genes.
Prevascularization often relies on co-culture systems that mimic the natural cellular interactions during blood vessel formation.
- Endothelial Lineage Cells: These are the primary building blocks of blood vessels. Common sources include Human Umbilical Vein Endothelial Cells (HUVECs) and, to overcome proliferation limitations, endothelial cells derived from human induced pluripotent stem cells (hiPSCs) [75].
- Supporting Cells: The stability and maturation of new vessels depend on pericytes and smooth muscle cells. These supporting cells are typically recruited by ECs in a co-culture system and secrete essential growth factors that stabilize the nascent vascular networks [75] [76].
Spatiotemporal Delivery of Bioactive Molecules
The controlled delivery of growth factors is critical, as a single, bolus dose often leads to immature, leaky, and dysfunctional vessels reminiscent of tumor vasculature [76]. Advanced biomaterial systems are designed to mimic the natural temporal sequence of angiogenesis.
- Degradation-Dependent Release: Growth factors like VEGF or BMP-2 are non-covalently encapsulated within biodegradable hydrogels (e.g., modified alginate, gelatin). As the scaffold degrades due to cell-secreted enzymes like MMPs, the factors are released in a controlled manner, though an initial burst release can be a limitation [76] [83].
- Trigger-Specific Release: More sophisticated systems use covalent bonding of factors to the scaffold via enzyme-sensitive or light-sensitive linkers. For example, a VEGF-heparin complex can be bound to a scaffold with an MMP-2 cleavable linker, ensuring release is directly triggered by the cellular activity of invading ECs [76].
- Layer-by-Layer (LBL) Assembly: This technique involves building a scaffold with sequential polymer layers, each containing different biomolecules. As cells invade and degrade the matrix, they are exposed to different factors in a pre-programmed sequence, such as VEGF for initiation followed by PDGF for maturation [76].
The diagram below summarizes the key signaling pathways involved in angiogenesis that are targeted by these delivery strategies.
Experimental Protocol: Fabricating a Multi-Layered, Patterned Hydrogel Construct
The following detailed protocol is adapted from a 2022 study that successfully engineered thick, vascularized tissues in diabetic mice [77].
Step 1: Synthesis of Functionalized Gelatin (GelPhMA)
- Dissolve 2% (w/v) porcine skin gelatin in 50 mM MES buffer at 60°C for 30 min.
- Cool to 27°C and adjust pH to 6.0.
- Add tyramine, EDC, and NHS to the solution to synthesize GelPh conjugates. Subsequently, react with methacrylic anhydride to introduce methacrylate groups, creating GelPhMA.
- Confirm the degree of functionalization (e.g., ~78% for Ph and ~71% for MA) via ¹H-NMR spectroscopy.
Step 2: Photolithography for Micropatterning
- Prepare a prepolymer solution of 10% (w/v) GelPhMA with 0.5% (w/v) lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) photoinitiator.
- Pour the solution onto a silicon wafer and cover with a photomask featuring a hexagonal network design (e.g., 300 µm channel width).
- Expose to UV light (e.g., 365 nm, 5 mW/cm²) for 60 seconds to crosslink the exposed pattern.
- Wash away the uncrosslinked polymer to reveal the micropatterned hydrogel layer.
Step 3: Cell Seeding and Layer Stacking
- Seed a co-culture of Human Umbilial Vein Endothelial Cells (HUVECs) and supporting cells (e.g., fibroblasts) onto the patterned hydrogel layer at a density of 5-10 million cells/mL.
- Culture for 24-48 hours to allow cell attachment.
- To create a thick construct, repeat Steps 2 and 3 to produce additional cell-laden layers.
- Stack these layers and use a final application of GelPhMA prepolymer and UV exposure to fuse them into a single, multi-layered construct.
Step 4: In Vivo Implantation and Analysis
- Implant the multi-layered construct subcutaneously in an animal model (e.g., diabetic mouse).
- After 2-4 weeks, harvest the implant for analysis.
- Assess vascularization and perfusion via:
- Micro-CT angiography after perfusing with a radio-opaque contrast agent.
- Histological staining (e.g., H&E, CD31 for endothelial cells, α-SMA for pericytes/smooth muscle cells) to confirm vessel maturity and integration.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for Vascularization Studies
| Reagent/Material | Function/Application | Example in Use |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | A photo-crosslinkable, tunable hydrogel that supports cell encapsulation and micropatterning. | Used to create hexagonal-patterned, multi-layered constructs for subcutaneous vascularization studies [77]. |
| Polycaprolactone (PCL) | A biodegradable polyester used in 3D printing for creating mechanically robust scaffold structures and channels. | Combined with phase separation to fabricate biomimetic vascular tubes that support microvascular self-assembly [82]. |
| Vascular Endothelial Growth Factor (VEGF) | A key mitogen for endothelial cells; stimulates proliferation, migration, and vascular permeability. | Delivered via enzyme-sensitive linkers in scaffolds to promote angiogenesis in bone defect models [76] [83]. |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | A highly efficient, water-soluble photoinitiator for UV crosslinking of hydrogels. | Used at 0.5% (w/v) to crosslink GelPhMA hydrogels in photolithography processes [77]. |
| Decellularized Plant Scaffolds | Sustainable, cellulose-based scaffolds with innate microchannel structures for small-diameter vascular grafts. | Leatherleaf viburnum scaffolds treated with mild heat (30-35°C) showed improved endothelialization and burst pressure [81]. |
| Cationic Polymers (e.g., PEI, PLL) | Non-viral vectors for gene delivery; complex with DNA/RNA via electrostatic interaction for pro-angiogenic gene therapy. | Used to deliver genes like ZNF580 or VEGF to endothelial cells to enhance their pro-angiogenic behavior [84]. |
Overcoming the vascularization hurdle is not a matter of a single solution but requires the strategic integration of multiple advanced approaches. The future of supporting large tissue constructs lies in the synergistic combination of mechanically optimized scaffolds, precisely fabricated perfusable architectures, and the spatiotemporally controlled delivery of biological cues. By continuing to refine biomaterials that actively participate in and guide the vascularization process—through dynamic mechanical conditioning in bioreactors, advanced 3D bioprinting, and intelligent growth factor delivery systems—researchers are poised to bridge the gap between laboratory-scale constructs and clinically viable, functional engineered tissues. This progress will ultimately unlock the full potential of regenerative medicine for treating a wide array of human diseases and injuries.
Addressing Immunogenicity and Ensuring Long-Term Scaffold Durability and Safety
The clinical success of biomaterial scaffolds in tissue engineering is fundamentally governed by their interactions with the host immune system and their degradation behavior in physiological environments. An inappropriate immune response can trigger chronic inflammation, fibrous encapsulation, and ultimately implant failure, while uncontrolled degradation can lead to premature loss of mechanical integrity or toxic byproduct accumulation [85]. The field has consequently evolved from developing passive, bioinert materials to designing advanced "smart" scaffolds that actively modulate immune responses and exhibit precisely tuned degradation profiles [9]. This whitepaper provides a technical guide to the principles and methodologies for addressing immunogenicity and ensuring the long-term durability and safety of biomaterial scaffolds, framed within the context of current research and emerging trends.
Understanding and Modulating the Immune Response to Scaffolds
The Foreign Body Reaction and Its Consequences
Upon implantation, biomaterials initiate a complex immune response, beginning with an acute phase involving protein adsorption and neutrophil recruitment, which can transition to a chronic state dominated by macrophages [85]. A key outcome is the Foreign Body Reaction (FBR), a persistent inflammatory condition that often results in the formation of a fibrous capsule around the implant, isolating it from surrounding tissues and severely compromising its function [85] [9]. This is particularly detrimental in applications like glucose sensors, where fibrous encapsulation impedes analyte diffusion, and in bone implants, where chronic inflammation can activate osteoclasts, leading to bone resorption and implant loosening [85].
Strategic Immunomodulation for Pro-Regenerative Outcomes
Modern strategies aim not to eliminate the immune response but to guide it toward a pro-regenerative outcome. Central to this is the polarization of macrophages from a pro-inflammatory (M1) phenotype to an anti-inflammatory, pro-healing (M2) phenotype [85] [9]. This shift is crucial for effective tissue integration and healing. The following diagram illustrates the strategic pathways for scaffold-driven immunomodulation to achieve this goal.
The strategies outlined above can be implemented through several technical approaches:
Material Composition and Bioactivity: The intrinsic chemistry of a scaffold can directly influence immune cell behavior. A seminal study demonstrated that tuning the ratio of gelatin (Gel) to chondroitin sulfate (CS) in macroporous microribbon (µRB) scaffolds directly influenced macrophage polarization and mesenchymal stem cell (MSC) crosstalk. The Gel50_CS50 formulation was identified as optimal, promoting a pro-regenerative environment that led to robust bone regeneration in a critical-sized defect model without exogenous growth factors [86]. In contrast, high CS ratios (e.g., 100% CS) increased M1 macrophage polarization, inhibiting bone formation [86].
Physical and Mechanical Properties: Immune cells are mechanosensitive. Scaffold properties such as stiffness, elasticity, and surface topography directly affect macrophage polarization [85]. Matching the mechanical properties of the target tissue is critical; for instance, softer materials mimicking brain tissue reduce inflammatory reactions [85]. Surface modifications, including nanopatterning of features like spikes and grooves, can significantly enhance biocompatibility and reduce FBR by modulating how immune cells adhere and perceive the material [85].
Delivery of Immunomodulatory Agents: Biomaterials can act as delivery vehicles for precise, localized immunomodulation. This includes the release of:
- Small molecule drugs: Non-steroidal anti-inflammatory drugs (NSAIDs) or specific inhibitors like those targeting Colony Stimulating Factor 1 Receptor (CSF1R) to alter macrophage differentiation [85].
- Biological agents: Anti-inflammatory cytokines (e.g., IL-4, IL-10) or advanced genetic tools like siRNA and miRNA to silence pro-inflammatory pathways [85].
- Cell-based therapies: Incorporation of MSCs or their products (e.g., extracellular vesicles), which naturally secrete anti-inflammatory factors and promote immune tolerance [85] [87].
Assessing and Controlling Scaffold Degradation for Long-Term Safety
Biodegradation Mechanisms and Assessment Techniques
Scaffold degradation is a critical property that must be synchronized with tissue repair. Degradation that is too fast leads to a premature loss of mechanical support, while degradation that is too slow can perpetuate chronic inflammation and fibrosis [88]. The primary mechanisms of biodegradation are hydrolysis, enzymatic cleavage, and oxidative degradation [88]. Accurate assessment is paramount, and current guidelines (e.g., ASTM F1635-11) recommend a multi-faceted approach, as no single technique provides a complete picture [68].
Table 1: Techniques for Assessing Biomaterial Scaffold Degradation
| Assessment Approach | Specific Techniques | Measured Parameters | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Physical | Gravimetric Analysis | Mass loss over time | Simple, cost-effective, quantitative | Cannot distinguish dissolution from degradation; not suitable for soluble formulations [68] |
| Scanning Electron Microscopy (SEM) | Surface morphology, porosity, cracks | Visualizes surface erosion and microstructural changes | Invasive sampling; requires solid, dry samples [68] | |
| Mechanical | Tensile/Compressive Testing | Young's modulus, tensile strength, strain at break | Directly measures functional integrity | Infer degradation but cannot confirm it [68] |
| Chemical | Size Exclusion Chromatography (SEC) | Molecular weight distribution | Tracks backbone cleavage (confirms degradation) | Higher cost; requires specialized equipment and expertise [68] |
| NMR, Mass Spectrometry | Chemical structure of degradation by-products | Identifies and quantifies degradation products | Complex data analysis [68] | |
| FTIR, XPS | Changes in chemical bonds and surface chemistry | Monitors chemical changes non-destructively | May not detect early-stage degradation [68] |
Tuning Degradation Properties for Clinical Application
Material selection and processing are key to controlling degradation. Blending polymers allows for the fine-tuning of degradation rates and mechanical properties. For example, blending poly(lactic acid) (PLA) with poly(ε-caprolactone) (PCL) creates a system where PLA provides rigidity and biodegradability, while PCL contributes flexibility and a slower degradation rate [89]. Research shows that increasing the PCL content in 3D-printed PLA/PCL scaffolds from 0% to 70% significantly reduces weight loss in phosphate-buffered saline, demonstrating a slower degradation profile [89]. Furthermore, the degradation rate of starch-based and PLGA scaffolds can be controlled by adjusting their cross-linking density or the ratio of lactic to glycolic acid monomers, respectively [88].
Experimental Protocols for Key Analyses
In Vitro Co-Culture Model for Screening Immunomodulatory Scaffolds
Purpose: To predict a scaffold's ability to modulate immune-stem cell crosstalk and its in vivo regenerative potential, surpassing the limitations of monoculture models [86].
Detailed Methodology:
- Scaffold Fabrication: Fabricate scaffolds with varying compositions (e.g., Gelatin/Chondroitin Sulfate ratios: 100/0, 50/50, 0/100) using methods like wet-spinning to create macroporous structures [86].
- Immune Cell Priming: Isolate primary macrophages (e.g., from mouse bone marrow) and prime them toward a pro-inflammatory (M1) phenotype using a cocktail of lipopolysaccharide (LPS) and interferon-gamma (IFN-γ) to mimic the acute inflammatory phase at an injury site [86].
- 3D Co-Culture Setup: Co-encapsulate the primed M1 macrophages and mesenchymal stem cells (MSCs) within the scaffold at a physiologically relevant ratio (e.g., 5:1, Mφ:MSC). Include control groups with MSC monoculture [86].
- Analysis:
- Cell Viability: Assess using a live/dead assay kit and confocal microscopy after 1-3 days of culture.
- Osteogenic Differentiation (for bone applications): Culture for 3-5 weeks. Quantify osteogenic gene expression (e.g., Runx2, Osteocalcin) via qRT-PCR at weekly intervals. At endpoint, perform Alizarin Red S (ARS) staining to quantify mineralized matrix deposition [86].
- Macrophage Phenotyping: At defined time points (e.g., day 7), analyze culture supernatants for cytokine profiles (e.g., TNF-α, IL-10 via ELISA) or perform immunostaining/flow cytometry on retrieved cells for M1 (e.g., iNOS) and M2 (e.g., CD206) markers [86].
Interpretation: A scaffold composition that promotes a shift toward M2 markers and enhances osteogenesis in the co-culture model (e.g., Gel50_CS50) is a leading candidate for in vivo testing, as it demonstrates the capacity to foster a pro-regenerative niche [86].
Comprehensive In Vitro Degradation Study
Purpose: To systematically evaluate the degradation profile of a scaffold in a simulated physiological environment.
Detailed Methodology:
- Pre-degradation Characterization: Weigh initial dry mass (Wᵢ). Characterize initial mechanical properties (e.g., compressive/tensile modulus) and chemical structure (e.g., via FTIR) [68].
- Degradation Setup: Immerse pre-weighed sterile scaffolds (n≥3) in phosphate-buffered saline (PBS, pH 7.4) or simulated body fluid, with or without enzymes (e.g., lysozyme, collagenase). Maintain at 37°C under gentle agitation. Refresh the solution periodically to maintain pH and enzyme activity [68] [89].
- Time-point Sampling:
- Gravimetric Analysis: At predetermined intervals (e.g., 1, 2, 4 weeks), remove samples from solution, rinse with deionized water, dry thoroughly to constant mass, and weigh final dry mass (W_f). Calculate percentage mass loss:
[(Wᵢ - W_f) / Wᵢ] × 100%[89]. - Mechanical Testing: Perform unconfined compression or tensile tests on wet samples from each time point to track changes in mechanical strength and modulus [68].
- Morphological Examination: Image samples using SEM to observe surface erosion, pore structure changes, and crack formation [68].
- Chemical Analysis: Use SEC to monitor changes in polymer molecular weight. Use NMR or HPLC to identify and quantify degradation products in the incubation medium [68].
- Gravimetric Analysis: At predetermined intervals (e.g., 1, 2, 4 weeks), remove samples from solution, rinse with deionized water, dry thoroughly to constant mass, and weigh final dry mass (W_f). Calculate percentage mass loss:
- pH Monitoring: Monitor the pH of the degradation medium throughout the study, as acidic byproducts (e.g., from PLA degradation) can cause local acidification and autocatalytic degradation [88].
The Scientist's Toolkit: Key Reagents and Materials
Table 2: Essential Research Reagents for Scaffold Immunogenicity and Degradation Studies
| Reagent/Material | Function/Application | Technical Notes |
|---|---|---|
| Gelatin | Denatured collagen; provides bioactive RGD sequences for cell adhesion; component of tunable immunomodulatory scaffolds [86]. | Sourced from type I collagen; cross-linkable (e.g., with methacryloyl groups) to control stability and mechanics. |
| Chondroitin Sulfate (CS) | Glycosaminoglycan (GAG); modulates immune response; key component in scaffolds for bone regeneration [86]. | Ratio to gelatin is critical; high CS content (e.g., 100%) can promote pro-inflammatory M1 macrophage polarization. |
| PLA/PCL Blends | Polymer system for tunable mechanical properties and degradation rates; feedstock for 3D printing (FFF) [89]. | PLA provides stiffness; PCL provides flexibility and slows degradation. Ratios (e.g., 70/30, 50/50) dictate final properties. |
| Macrophage Colony-Stimulating Factor (M-CSF) | Differentiates monocytes into macrophages for in vitro immunomodulation assays. | Essential for generating primary macrophages from bone marrow or blood-derived monocytes. |
| LPS / IFN-γ | Cytokines used to polarize macrophages toward a pro-inflammatory (M1) phenotype in co-culture models. | Creates an in vitro environment mimicking acute inflammation at an implant site. |
| Alizarin Red S (ARS) | Histochemical dye that binds to calcium deposits; quantifies in vitro osteogenic differentiation and mineralization. | Standard endpoint measurement for bone tissue engineering studies. |
| Size Exclusion Chromatography (SEC) | Analytical technique to monitor the change in polymer molecular weight distribution during degradation. | Considered a gold-standard chemical method to confirm degradation, as it tracks backbone cleavage [68]. |
The convergence of immunology and biomaterials science is paving the way for a new generation of scaffolds that are not merely passive supports but active participants in the healing process. Success hinges on a holistic design strategy that simultaneously addresses immunogenicity and degradation. This involves selecting and tuning material compositions—such as Gel/CS or PLA/PCL blends—to guide favorable immune-stem cell crosstalk, and employing comprehensive, multi-faceted assessment protocols to ensure scaffold degradation is synchronized with tissue regeneration. As the field advances, the integration of stimuli-responsive "smart" materials, advanced bioreactor cultures, and AI-driven design will further enhance our ability to create safe, durable, and clinically effective scaffold-based therapies.
Process Optimization with AI and Digital Twins for Enhanced Fabrication Control
The convergence of Artificial Intelligence (AI) and Digital Twin (DT) technologies is initiating a paradigm shift in the fabrication of biomaterial scaffolds for tissue engineering. This synergy is creating a new generation of technological advancement in the biomedical industry, enabling unprecedented control over manufacturing processes [90]. A Digital Twin is a virtual representation of a physical system—such as a scaffold, a bioprinter, or even a biological process—that is continuously updated with real-world data via sensors [91] [92]. When coupled with AI, these digital replicas enable data-driven experimentation, precise diagnostic support, and predictive modeling, allowing researchers to simulate and optimize fabrication parameters in a risk-free virtual environment before applying them in the physical world [91] [92].
Within the hierarchical framework of Digital Twins, three main types are particularly relevant to tissue engineering:
- Digital Twin Prototype (DTP): Developed before a physical product exists, enabling rapid virtual prototyping and testing of design concepts, materials, and predicted behaviors [91] [92].
- Digital Twin Instance (DTI): Created for an existing physical product or process, establishing a real-time bidirectional communication link that allows for continuous monitoring, validation, and updates [91] [92].
- Digital Twin Aggregation (DTA): Focuses on analyzing large-scale data from physical products to leverage intelligent capabilities for optimizing design, monitoring performance, and drawing data-driven conclusions [91] [92].
The integration of these technologies is critical for addressing the profound complexity of tissue engineering, which involves navigating a vast design space of biomaterial properties, cellular behaviors, and manufacturing parameters [90]. AI and DTs provide a powerful framework to manage this complexity, accelerating the development of scaffolds that are not only biocompatible but also functionally tailored to specific therapeutic applications.
Core AI and Digital Twin Frameworks for Fabrication Control
Implementing a closed-loop system for fabrication control requires a structured integration of data, models, and physical hardware. The following framework outlines the core components and their logical interactions, illustrating how AI and DTs create an adaptive optimization pipeline.
Key AI Models and Algorithms for Predictive Control
The AI component of this framework relies on a suite of sophisticated algorithms for predictive modeling and optimization. These models learn from both historical data and real-time inputs to predict scaffold behavior and optimize fabrication parameters.
Table 1: Key AI Models and Algorithms for Fabrication Control in Tissue Engineering
| Model/Algorithm | Description | Application in Scaffold Fabrication |
|---|---|---|
| Finite Element Analysis (FEA) | A numerical technique for simulating the deformation and mechanical properties of structures under load [90]. | Predicting stress-strain distribution within a scaffold under physiological loads to optimize architectural design and prevent failure. |
| Supervised Learning | Algorithms that learn a mapping function from input data to corresponding outputs based on labeled training data [90]. | Predicting the printability of a bio-ink based on its viscosity and composition, or forecasting cell viability from printing parameters. |
| Neural Networks (NN) / Deep Learning (DL) | Multi-layered learning models that extract complex features and relationships from raw data [90]. | Analyzing real-time imaging data during bioprinting to detect defects and power adaptive, real-time corrections. |
| Support Vector Machines (SVM) | A classification algorithm that finds the optimal hyperplane to separate data of different categories [90]. | Classifying the success or failure of a scaffold fabrication run based on a set of process parameters. |
| Random Forests | An ensemble method that uses multiple decision trees to improve predictive accuracy and control over-fitting [90]. | Identifying the most critical fabrication parameters (e.g., pressure, speed, temperature) that influence scaffold pore size and mechanical integrity. |
These AI strategies enable a shift from traditional, often empirical, optimization to a data-driven paradigm. For instance, Artificial Neural Networks (ANNs) with more than 30 variables have been used to accurately predict the outcomes of vascular tissue engineering strategies with over 94% accuracy [90]. Similarly, mechanistic computational models can create patient-specific digital twins, such as those used to model cardiovascular function in heart failure patients, providing a comprehensive representation of an individual's disease state for personalized therapeutic planning [93]. This capability is directly transferable to simulating the performance of biomaterial scaffolds within a specific biological context.
Experimental Protocols for Implementation
Translating the conceptual framework into actionable research requires robust and reproducible experimental methodologies. The following protocols detail how to establish an AI-guided digital twin system for bioprinting optimization and scaffold biocompatibility assessment.
Protocol: AI-Guided Real-Time Bioprinting Optimization
This protocol, adapted from a novel technique developed by MIT researchers, describes the setup for a modular, low-cost monitoring system that enables real-time print quality control and parameter optimization [41].
Objective: To integrate a real-time, AI-based monitoring technique for detecting defects and identifying optimal print parameters during the 3D bioprinting of tissue scaffolds.
Materials and Reagents:
- Standard 3D bioprinter (the method is printer-agnostic)
- Bio-inks of interest (e.g., cell-laden gelatin methacryloyl (GelMA), alginate)
- Modular digital microscope (cost < $500)
- Computational unit with image analysis software (e.g., Python with OpenCV, TensorFlow)
Methodology:
- System Setup: Mount the digital microscope to the print head or a fixed position to capture the print area. Ensure consistent lighting to facilitate high-resolution image capture.
- Image Acquisition: Program the system to capture high-resolution images of the fabricated tissue construct after each printed layer is completed.
- AI-Based Image Analysis: In real-time, feed the captured images to an AI-based image analysis pipeline. This pipeline should:
- Rapidly compare the captured image to the intended digital design (G-code or CAD model).
- Identify and classify common print defects, such as depositing too much or too little bio-ink, misalignment, or strand fusion.
- Defect Correction and Parameter Tuning: Use the analysis output to:
- Adaptive Correction: Implement a feedback loop to make immediate adjustments to the printing parameters (e.g., pressure, speed) for subsequent layers to correct the identified defects.
- Parameter Optimization: Systematically run test prints with varying parameters (e.g., pressure, speed, nozzle diameter) and use the monitoring system to identify the set of parameters that produces the highest fidelity to the digital design for a given bio-ink.
Validation: The success of this protocol is validated by quantifying the reduction in print defects and the improvement in inter-tissue reproducibility. Furthermore, the optimized parameters should yield scaffolds with enhanced mechanical properties and improved cell viability post-printing [41].
Protocol: Assessing the Impact of Fabrication on Scaffold Biocompatibility
This protocol outlines methods to evaluate how fabrication processes, and subsequent modifications, affect the immune compatibility and endothelialization potential of a scaffold, using plant-derived scaffolds as an exemplar [81].
Objective: To quantitatively evaluate the effects of a fabrication process (e.g., heat treatment) on the mechanical integrity and cellular response to a decellularized scaffold.
Materials and Reagents:
- Decellularized scaffolds (e.g., leatherleaf viburnum leaves)
- NaOH solution
- Endothelial Cells (ECs)
- White Blood Cells (WBCs)
- Cell culture media and reagents
- Tensile testing machine
- Burst pressure testing apparatus
- Scanning Electron Microscope (SEM)
Methodology:
- Scaffold Treatment: Subject decellularized scaffolds to the process parameter of interest. For example, perform mild alkaline heat treatment by incubating scaffolds in 5% NaOH at temperatures between 30–40°C for 15–60 minutes [81].
- Mechanical Characterization:
- Tensile Testing: Cut dog bone-shaped samples and perform uniaxial tension tests at a constant strain rate until failure. Record maximum tensile load and calculate elastic modulus.
- Burst Pressure Testing: Form scaffolds into tubular grafts, secure them to a pressure sensor, and inject water at a constant pressure until failure to measure peak burst pressure.
- Biocompatibility Assessment:
- White Blood Cell (WBC) Viability: Seed WBCs onto treated and untreated scaffolds and perform a viability assay (e.g., Live/Dead staining). Improved viability indicates reduced immunogenicity.
- Endothelial Cell (EC) Seeding: Seed ECs onto the scaffolds and evaluate seeding efficiency and the ability to form a confluent monolayer over time, which is critical for preventing thrombosis in vascular grafts.
Validation: Successful treatment is indicated by scaffolds that retain >90% of their tensile strength and achieve burst pressures ≥820 mmHg (exceeding physiological arterial pressures), while also demonstrating a significant increase in WBC viability and improved EC seeding efficiency [81].
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of AI and DT-guided fabrication control relies on a suite of essential reagents and materials. The table below catalogs key solutions used in the featured experiments and the broader field.
Table 2: Key Research Reagent Solutions for AI-Enhanced Scaffold Fabrication
| Item | Function | Application Example |
|---|---|---|
| Modular Digital Microscope | Low-cost, high-resolution imaging for real-time process monitoring during bioprinting [41]. | Capturing layer-by-layer images for AI-based defect detection in 3D bioprinting processes. |
| Decellularized Plant Scaffolds | Sustainable, biocompatible, and tunable natural platforms for vascular graft engineering [81]. | Serving as a test substrate for evaluating the effects of heat treatment on mechanical properties and biocompatibility. |
| Defined Bio-inks | Custom formulations of living cells, biocompatible materials, and growth factors for building 3D structures [41]. | Used as the primary printing material; their properties are optimized via AI and digital twin simulations. |
| AI-Based Image Analysis Pipeline | Software tool for rapidly comparing printed structures to their digital design to identify defects [41]. | The core analytical component for real-time quality control in an adaptive bioprinting system. |
| Mechanistic Computational Models | Mathematical models that simulate system behavior (e.g., cardiovascular function, scaffold mechanics) [93]. | Generating patient-specific digital twins to predict scaffold performance and optimize design pre-fabrication. |
The integration of AI and Digital Twins represents a foundational shift in the fabrication of biomaterial scaffolds, moving the field from iterative, experience-based optimization toward a predictive, data-driven engineering discipline. The frameworks and protocols detailed in this guide provide researchers with a roadmap for implementing these advanced technologies. By establishing a closed-loop system where digital models inform physical fabrication and real-time data from the physical world refines the digital counterpart, it is possible to achieve unprecedented levels of control over scaffold architecture, mechanics, and biological function. This approach not only accelerates process optimization and reduces material waste but also paves the way for the robust and scalable manufacturing of personalized, clinically effective tissue engineering products. As these technologies mature, their synergy promises to unlock new frontiers in regenerative medicine, ultimately enabling the fabrication of complex, functional tissues and organs.
From Lab to Clinic: Predictive Modeling, Preclinical Validation, and Material Performance Analysis
AI and Deep Learning Models for Predicting Biocompatibility and Scaffold Performance
The development of biomaterial scaffolds is a cornerstone of tissue engineering, a field aimed at restoring or replacing damaged biological tissues. A critical challenge in this process is predicting scaffold biocompatibility and performance before fabrication and implantation, as traditional trial-and-error methods are often time-consuming, resource-intensive, and can lead to costly failures [94]. Artificial Intelligence (AI), particularly deep learning models, is revolutionizing this domain by providing powerful tools for predictive modeling and optimization. By learning complex patterns from existing data, these models can accurately forecast how a scaffold will interact with biological systems, thereby accelerating the design of safer and more effective regenerative therapies [95] [96]. This whitepaper provides an in-depth technical guide to the core AI models and methodologies being deployed to predict biocompatibility and scaffold performance within the broader context of biomaterial scaffolds for tissue engineering applications.
Core Deep Learning Architectures for Prediction
Two primary deep learning architectures have emerged as pivotal tools for predicting scaffold performance: Artificial Neural Networks (ANNs) for structured numerical data and Convolutional Neural Networks (CNNs) for image-based analysis.
Artificial Neural Networks (ANNs) for Structured Data
ANNs are computational models inspired by the biological neural networks of the human brain. They are exceptionally well-suited for modeling the complex, non-linear relationships between scaffold design parameters and their resulting biological and mechanical properties [95] [96].
Architectural and Mathematical Foundation:
A typical ANN consists of an input layer, one or more hidden layers, and an output layer. Each layer contains interconnected nodes, or "neurons." The operation of a single neuron is mathematically represented as:
y = f(∑(i=1 to n) w_i * x_i + b)
where x_i are the input features, w_i are the corresponding weights, b is the bias term, and y is the neuron's output. The activation function f introduces non-linearity, enabling the network to model complex relationships. Common activation functions include the Rectified Linear Unit (ReLU), f(x) = max(0, x), and the Sigmoid function, f(x) = 1 / (1 + e^{-x}) [95].
The learning process involves adjusting the weights and biases to minimize a loss function. For binary classification tasks, such as predicting biocompatibility (compatible/incompatible), binary cross-entropy is often employed:
L = -1/N ∑(i=1 to N) [y_i * log(ŷ_i) + (1 - y_i) * log(1 - ŷ_i)]
where y_i is the true label, ŷ_i is the predicted probability, and N is the number of samples. Optimization algorithms like stochastic gradient descent (SGD) or Adam are used to iteratively update the parameters and reduce this loss [95].
Convolutional Neural Networks (CNNs) for Image Analysis
CNNs are a specialized class of deep neural networks designed for processing grid-like data, such as images. They are particularly valuable for analyzing microscopic images of scaffold microstructures to predict cell behavior or identify defects [95] [97].
Architectural and Mathematical Foundation:
The core component of a CNN is the convolutional layer. In this layer, small filters (or kernels) slide over the input image to perform a convolution operation, producing feature maps that highlight specific patterns like edges, textures, or pores. This operation is expressed as:
y(i,j) = ∑(m=1 to M)∑(n=1 to N) x(i+m, j+n) * w(m,n) + b
Here, x is the input matrix, w is the filter, b is the bias, and y(i,j) is the output feature map element [95].
CNNs typically stack multiple convolutional layers, interspersed with pooling layers (e.g., max pooling) to reduce spatial dimensions and increase translational invariance, and fully connected layers at the end for final classification or regression tasks. The ability of CNNs to automatically and hierarchically learn spatial features from scaffold images makes them superior to traditional image analysis techniques [95] [97].
Comparative Performance Analysis of AI Models
Direct comparative studies provide critical insights into the performance and appropriate application of different AI models. A seminal 2025 study offers a quantitative benchmark for ANN and CNN models in predicting scaffold biocompatibility [98].
Table 1: Comparative Performance of ANN and CNN Models for Biocompatibility Prediction [98]
| Model | Key Architecture/Input | Accuracy | Precision | Recall | F1-Score |
|---|---|---|---|---|---|
| ANN | 20 neurons, 100 epochs; 15 design parameters | 1.0 | 1.0 | 1.0 | 1.0 |
| CNN | Batch size of 56; scaffold images | N/A | 0.88 | 0.90 | 0.87 |
Experimental Outcome and Interpretation: In this study, the ANN model, trained on 15 key numerical design parameters (e.g., porosity, pore size, material composition), achieved perfect scores across all metrics, correctly predicting the biocompatibility of all five scaffold samples in experimental validation [98]. The CNN model, while robust, misclassified one sample when analyzing scaffold images. This demonstrates that for structured numerical data derived from design software, ANNs can outperform CNNs by efficiently modeling the complex, non-linear relationships between design parameters and biological outcomes. CNNs remain the tool of choice for tasks reliant on visual data, such as analyzing scaffold microstructure from microscopy images or predicting cell alignment [95] [98].
Experimental Protocols for AI-Driven Biocompatibility Assessment
Implementing AI models for scaffold prediction requires a methodical workflow. The following protocol, synthesizing methodologies from recent literature, details the process for developing and validating an ANN model for biocompatibility prediction.
Objective: To develop and validate an ANN model for predicting the biocompatibility of tissue scaffolds based on their design parameters.
Workflow Overview: The diagram below outlines the key stages of this experimental protocol.
Detailed Experimental Methodology
Step 1: Data Acquisition and Parameter Selection
- Input Data Generation: Utilize bioprinting or scaffold design software (e.g., PrusaSlicer) to generate a wide range of scaffold designs [98].
- Key Parameters: For each design, extract a comprehensive set of numerical parameters known to influence biocompatibility. These typically include:
- Structural Properties: Porosity (%), pore size (µm), surface area-to-volume ratio.
- Mechanical Properties: Compressive modulus (MPa), tensile strength, degradation rate.
- Material Composition: Polymer type (e.g., PCL, PLGA), ceramic content (e.g., hydroxyapatite %), crosslinking density [95] [98] [99].
- Output Data (Labels): Obtain experimental biocompatibility labels for each design through in vitro assays (e.g., cell viability > 90%, low inflammatory cytokine release) or from historical data. This creates a labeled dataset for supervised learning.
Step 2: Data Preprocessing and Standardization
- Data Cleaning: Handle missing values and remove outliers.
- Normalization: Standardize all input features to a common scale (e.g., 0 to 1) using techniques like Min-Max scaling or Z-score normalization. This prevents features with larger numerical ranges from dominating the model training [98].
- Data Splitting: Partition the dataset into three subsets:
- Training Set (~70-80%): Used to train the model.
- Validation Set (~10-15%): Used to tune hyperparameters and prevent overfitting.
- Test Set (~10-15%): Used for the final, unbiased evaluation of model performance [98].
Step 3: Model Architecture Definition and Training
- Model Selection: Choose an ANN architecture. A foundational model could consist of:
- Input Layer: Number of neurons equals the number of design parameters (e.g., 15).
- Hidden Layers: Start with 1-2 hidden layers containing 10-20 neurons each, using ReLU activation functions.
- Output Layer: A single neuron with a sigmoid activation function for binary classification (biocompatible vs. non-biocompatible) [98].
- Compilation and Training:
Step 4: Model Performance Evaluation
- Metrics: Evaluate the trained model on the held-out test set using standard metrics: Accuracy, Precision, Recall, and F1-Score [98].
- Confusion Matrix: Generate a confusion matrix to visualize true positives, false positives, true negatives, and false negatives.
Step 5: Experimental Validation
- Prototype Fabrication: Fabricate a small batch of novel scaffold designs (e.g., n=5) not included in the original training dataset.
- In Vitro/In Vivo Testing: Conduct standard biocompatibility tests (e.g., ISO 10993-5 for cytotoxicity) on these prototypes.
- Model Validation: Compare the experimental results with the model's predictions to calculate the real-world predictive accuracy and validate the model's utility [98].
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful application of AI in tissue engineering relies on a foundation of specific materials, software, and analytical tools.
Table 2: Key Research Reagent Solutions for AI-Driven Scaffold Development
| Category | Item | Specific Examples & Functions |
|---|---|---|
| Biomaterials | Synthetic Polymers | Polycaprolactone (PCL), Polylactic-co-glycolic acid (PLGA): Provide biodegradable, mechanically tunable scaffold matrices [95] [99]. |
| Ceramics & Bioactive Glass | Hydroxyapatite, Bioglass: Enhance osteoconductivity and mechanical strength in bone tissue engineering; can release therapeutic ions (Ca, Si) [99]. | |
| Conductive Polymers | Electroactive Elastomers (e.g., PEDOT:PSS blends): Support cell signaling and improve regeneration in electrically sensitive tissues (e.g., bladder, nerve) [49]. | |
| Software & Data | Design & Slicing Software | PrusaSlicer, CAD Software: Generate 3D scaffold models and extract key numerical design parameters for ANN input [98]. |
| AI/ML Frameworks | TensorFlow, PyTorch: Provide libraries for building and training custom ANN and CNN models [96]. | |
| Public Datasets | Protein Data Bank (PDB), The Cancer Imaging Archive (TCIA): Serve as resources for training AI models on protein structures or medical images [97]. | |
| Analytical Assays | Biocompatibility Assays | Cell Viability (e.g., MTS, Live/Dead staining), Cytokine Release Assays: Generate experimental data to label datasets for model training [98]. |
| Imaging & Microscopy | SEM, Confocal Microscopy: Produce high-resolution images of scaffold microstructure for CNN-based analysis [95] [94]. |
Integrated Workflow: From Data to Clinical Application
The ultimate power of AI in tissue engineering is realized when models are integrated into a seamless, iterative workflow that bridges computational design and clinical application. This process, known as the Design-Build-Test-Analyze (DBTA) cycle, is supercharged by AI, dramatically accelerating the path to viable clinical products.
AI-Augmented Workflow for Scaffold Development: The following diagram illustrates this integrated, multimodal AI workflow, highlighting how different data types and models converge to inform the design of patient-specific scaffolds.
This workflow demonstrates how multimodal AI integrates heterogeneous data sources—such as clinical imaging (CT, MRI), genomic information, and scaffold design parameters—to build a holistic predictive model [97]. ANNs process the numerical and clinical data, while CNNs analyze medical and scaffold images. The output is a patient-specific, optimized scaffold design that can be fabricated via 3D bioprinting or additive manufacturing. The results from testing these fabricated scaffolds then feed back into the AI models as new training data, creating a continuous cycle of improvement and refinement that pushes the entire field forward [97] [94]. This closed-loop system is foundational to the future of personalized regenerative medicine.
High-Throughput Screening and Single-Cell Sequencing for Robust Biomaterial Assessment
The development of advanced biomaterial scaffolds is a cornerstone of modern tissue engineering, aimed at regenerating damaged tissues and restoring biological function. The effectiveness of these scaffolds hinges on their successful integration with the host's cellular environment, a process that requires a sophisticated understanding of complex cell-biomaterial interactions [100]. Traditional methods for assessing these interactions, such as bulk transcriptomics, proteomics, and metabolomics, rely on aggregated signals from large cell populations. These conventional approaches suffer from an averaging effect that obscures critical single-cell variations, rare cell characteristics, and dynamic changes in gene expression and signaling pathways [100]. Consequently, the precise mechanisms underlying cell-biomaterial interactions remain incompletely understood, impeding the rational design of highly tailored and biocompatible materials.
The integration of High-Throughput Screening (HTS) and Single-Cell RNA Sequencing (scRNA-seq) represents a paradigm shift in biomaterial evaluation. HTS enables the rapid, parallel testing of numerous material compositions and physical cues against diverse cellular responses, generating vast, multidimensional datasets. scRNA-seq complements this by providing an unprecedented granular view of cellular heterogeneity, revealing distinct cell types, functional states, and subtle alterations induced by biomaterials at the resolution of individual cells [100]. This powerful combination allows researchers to move beyond superficial observations to deeply investigate the specific mechanisms of biological responses, facilitating the development of next-generation biomaterials with precisely engineered properties for enhanced biocompatibility, controlled immune modulation, and superior regenerative outcomes [100].
Core Concepts and Quantitative Frameworks
The Biomaterial-Mediated Cell Atlas (BCA)
A pivotal concept emerging from this technological integration is the Biomaterial-mediated Cell Atlas (BCA). The BCA extends the framework of the Human Cell Atlas (HCA) by creating a comprehensive compendium of cellular responses to various biomaterials at the single-cell level [100]. It is defined as a framework that "characterizes how biomaterials mediate cellular responses at multi-omics levels through their physical/chemical/biological cues, bridging material science and biology to advance regenerative medicine, therapeutics, and biomaterial design" [100]. The BCA plays multiple crucial roles:
- Biological Safety: It provides evidence of a biomaterial's biocompatibility by mapping local or systemic toxic effects on tissues at the cellular level [100].
- Bioactivity: It evaluates a biomaterial's capacity to interact with and positively influence surrounding tissues, such as by promoting regeneration or reducing inflammation [100].
- Immune Microenvironment: It analyzes immune reactions to foreign material, providing information on immunomodulatory properties and helping to mitigate adverse immune responses [100].
Key Scaffold Parameters for High-Throughput Screening
In the context of bone tissue engineering and other applications, key architectural parameters of scaffolds must be optimized. HTS platforms are ideally suited to systematically vary and test these parameters. The table below summarizes critical factors and their optimal ranges as identified in recent research, particularly for freeze-dried scaffolds [7].
Table 1: Key Biomaterial Scaffold Parameters and Their Impact on Biological Response
| Parameter | Optimal Range/Type | Biological Impact |
|---|---|---|
| Porosity | High Porosity | Facilitates effective cell attachment, proliferation, and nutrient diffusion [7]. |
| Pore Size | Interconnected Porous Architecture | Critical for cell infiltration and vascularization [7]. |
| Compressive Strength | Improved Strength | Enhances mechanical stability, making scaffolds suitable for load-bearing applications like bone tissue engineering [7]. |
| Synthesis Method | Freeze-Drying | A sustainable method that creates denser, more compact structures with slower ice crystal formation at lower temperatures [7]. |
| Material Type | Hybrid/Composite Scaffolds (Metals, Polymers, Ceramics) | Combines advantageous properties to surpass limitations of single-material constructs [10]. |
Single-Cell Sequencing vs. Bulk Analysis
The transition from bulk analysis to single-cell resolution is fundamental to the BCA. The following table contrasts these two approaches, highlighting the transformative potential of scRNA-seq in biomaterial assessment.
Table 2: Contrasting Bulk and Single-Cell Analytical Approaches in Biomaterial Science
| Feature | Bulk Analysis | Single-Cell Analysis (scRNA-seq) |
|---|---|---|
| Resolution | Tissue-level, averaged signals [100]. | Single-cell level, resolution of individual cells [100]. |
| Data Output | Averaged gene expression across a population [100]. | Gene expression profile for each individual cell [100]. |
| Insight Generated | General cellular response; masks heterogeneity [100]. | Reveals cellular heterogeneity, rare cell types, and dynamic state changes [100]. |
| Identification Capacity | Limited to major cell populations. | Identifies distinct cell types, functional pathways, and subtle implant-induced alterations [100]. |
| Primary Limitation | Averaging effect obscures critical single-cell variations [100]. | Higher cost and computational complexity; technical artifacts (e.g., drop-out events). |
Experimental Protocols for Integrated Assessment
Protocol 1: High-Throughput Screening of Scaffold Formulations
This protocol outlines the steps for creating and screening a library of biomaterial scaffolds to identify top candidates for further single-cell analysis.
Library Design and Fabrication:
- Parameter Variation: Systematically vary scaffold parameters (e.g., polymer ratios, crosslinking density, incorporation of bioactive signals like SDF-1α) [100] in a multi-well plate format.
- Fabrication Technique: Utilize automated fabrication methods such as 3D bioprinting or robotic dispensing to ensure consistency and enable complex architectures like those found in smart, 4D-printed hybrid scaffolds [10].
- Sterilization: Employ gamma irradiation or ethanol immersion for sterilization, ensuring aseptic conditions for cell culture.
Cell Seeding and Culture:
- Cell Source: Select relevant cell types (e.g., primary osteoblasts for bone, mesenchymal stem cells, or co-cultures).
- Dynamic Seeding: Use bioreactors or orbital shakers to promote uniform cell distribution across the scaffold pores.
- Culture Conditions: Maintain cultures under standard conditions (e.g., 37°C, 5% CO₂) for a predetermined period, with medium changes as per protocol.
Endpoint Staining and Multiparametric Imaging:
- Staining: Fix cells and stain for key markers:
- Viability/Cytotoxicity: Calcein-AM (live, green) / Ethidium homodimer-1 (dead, red).
- Proliferation: EdU or Ki67 immunofluorescence.
- Cell Morphology: Phalloidin (actin cytoskeleton) / DAPI (nuclei).
- Imaging: Acquire high-content images using an automated inverted fluorescence microscope across all wells.
- Staining: Fix cells and stain for key markers:
Image and Data Analysis:
- Quantification: Use image analysis software (e.g., CellProfiler, ImageJ) to quantify parameters like cell number, viability, spreading area, and colonization depth.
- Hit Selection: Normalize data to controls and apply statistical analysis (e.g., Z-score) to identify scaffold formulations that significantly outperform others in the desired outcomes.
Protocol 2: Single-Cell RNA Sequencing of Cell-Scaffold Constructs
This protocol details the process for preparing single-cell suspensions from the top-performing scaffold candidates identified in HTS for downstream sequencing.
Sample Preparation and Dissociation:
- Selection: Retrieve cell-scaffold constructs identified as "hits" from the HTS screen.
- Dissociation: Carefully wash constructs with PBS and enzymatically digest using a combination of collagenase IV and trypsin-EDTA to break down the matrix and create a single-cell suspension. The specific enzymes and incubation times must be optimized for the scaffold material.
- Quenching and Filtration: Neutralize the enzymes with a complete culture medium. Pass the cell suspension through a cell strainer (e.g., 40 µm) to remove debris and any undigested aggregates.
- Viability and Counting: Assess cell viability using trypan blue exclusion and count cells with an automated cell counter or hemocytometer. Aim for a viability of >80%.
Library Preparation and Sequencing:
- Platform Selection: Choose a droplet-based (e.g., 10x Genomics) or well-based (e.g., SMART-Seq) scRNA-seq platform based on the required cell throughput and sequencing depth.
- Barcoding and cDNA Synthesis: Load the single-cell suspension onto the chosen platform where individual cells are captured, lysed, and their mRNA is barcoded with unique molecular identifiers (UMIs) and reverse-transcribed into cDNA.
- Library Construction: Amplify the cDNA and construct sequencing libraries following the manufacturer's protocol.
- Sequencing: Sequence the libraries on a high-throughput sequencer (e.g., Illumina NovaSeq) to a sufficient depth (e.g., 50,000 reads per cell).
Bioinformatic Analysis:
- Preprocessing: Use pipelines (e.g., Cell Ranger for 10x Genomics data) to demultiplex samples, align reads to a reference genome, and generate a gene expression matrix (cells x genes).
- Quality Control: Filter out low-quality cells based on metrics like the number of genes detected per cell, total UMI counts, and mitochondrial gene percentage.
- Dimensionality Reduction and Clustering: Perform principal component analysis (PCA) and graph-based clustering (e.g., Seurat, Scanpy) to identify distinct cell subpopulations.
- Cell Type Annotation: Identify cell types by comparing the expression of known marker genes in each cluster to reference databases.
- Differential Expression and Pathway Analysis: Compare gene expression profiles between cells from different scaffold conditions to identify differentially expressed genes and enriched biological pathways using tools like GSEA.
Visualizing the Integrated Workflow and Cellular Insights
The following diagrams, created using DOT language, illustrate the core experimental workflow and the analytical power of single-cell sequencing.
HTS to scRNA-seq Workflow
Resolving Cellular Heterogeneity
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the described integrated pipeline requires a suite of specialized reagents and tools. The following table details key components of the research toolkit.
Table 3: Essential Research Reagents and Materials for Integrated Biomaterial Assessment
| Category | Item | Function and Application |
|---|---|---|
| Scaffold Fabrication | Polymers (Natural & Synthetic) | Base materials (e.g., PCL, PLGA, Alginate, Chitosan) for constructing the 3D scaffold architecture [7] [10]. |
| Bioactive Signals (e.g., SDF-1α) | Chemically immobilized into scaffolds to direct specific cellular responses like progenitor cell recruitment and angiogenesis [100]. | |
| Freeze-Dryer | Key equipment for a sustainable synthesis method that creates scaffolds with superior compressive strength and high, interconnected porosity [7]. | |
| Cell Culture & HTS | Primary Cells / Stem Cells | Biologically relevant models (e.g., osteoblasts, MSCs) for assessing cell-scaffold interactions in a physiologically meaningful context. |
| Multiplex Assay Kits | Enable simultaneous measurement of multiple endpoints (viability, cytotoxicity, apoptosis) from a single well, maximizing HTS data density. | |
| High-Content Imaging System | Automated fluorescence microscope for rapid, multiparametric image acquisition across hundreds of scaffold samples. | |
| scRNA-seq | Single-Cell Isolation Kit | Reagents for generating high-viability single-cell suspensions from often challenging 3D cell-scaffold constructs (e.g., enzymatic dissociation mixes). |
| scRNA-seq Library Prep Kit | Commercial kits (e.g., 10x Genomics) for barcoding, reverse transcription, and preparation of sequencing-ready libraries from single cells. | |
| Cell Ranger / Seurat | Standard software pipelines for processing raw sequencing data, performing quality control, and conducting initial clustering and analysis. |
The strategic integration of High-Throughput Screening and Single-Cell Sequencing marks a significant leap forward in biomaterial science. This combined approach moves beyond the limitations of traditional, population-averaged methods, enabling the deconvolution of complex cellular heterogeneity in response to material cues. By systematically screening material libraries and then deeply probing the cellular responses of top candidates at single-cell resolution, researchers can construct a quantitative Biomaterial-mediated Cell Atlas. This atlas provides unprecedented insights into biological safety, bioactivity, and immune modulation, ultimately paving the way for the data-driven and rational design of robust, effective, and clinically transformative biomaterial scaffolds for tissue engineering.
Tissue engineering represents a transformative approach in regenerative medicine, aiming to restore or replace damaged tissues and organs. At the core of this strategy lies the scaffold—a three-dimensional framework that provides structural and biochemical cues to support cell attachment, proliferation, and differentiation. The selection of appropriate scaffold materials profoundly influences the success of tissue regeneration outcomes, necessitating a thorough understanding of available options. This comprehensive analysis examines the three primary categories of scaffold materials: natural, synthetic, and hybrid systems. Within the context of biomaterial research for tissue engineering, each class presents distinct advantages and limitations concerning biocompatibility, mechanical properties, degradation kinetics, and biofunctional properties. By synthesizing current research and emerging trends, this review provides researchers and drug development professionals with a technical foundation for material selection and scaffold design, ultimately contributing to the advancement of regenerative therapies.
Material Classifications and Properties
Natural Polymer-Based Scaffolds
Natural polymers are derived from biological sources, including plants, animals, and microorganisms. Their inherent bioactivity and similarity to native extracellular matrix (ECM) components make them particularly attractive for tissue engineering applications.
Plant-derived polymers primarily include polysaccharides (e.g., cellulose, alginate, pectin, starch) and proteins (e.g., soy, zein, gluten). These materials offer significant advantages in terms of sustainability, biocompatibility, and ability to simulate the ECM environment [52]. Their inherent hydrophilicity promotes cell adhesion and proliferation, essential for tissue regeneration. However, challenges include mechanical instability and inconsistent degradation rates that must be carefully controlled to match the pace of new tissue formation [52].
Animal-derived polymers such as collagen, gelatin, hyaluronic acid, silk fibroin, and chitosan are widely utilized in scaffold fabrication. Collagen and gelatin provide excellent cell-recognition sites, while silk fibroin demonstrates good biocompatibility, slow degradation, and strong mechanical properties, making it suitable for cartilage regeneration [101]. Chitosan, formed by chitin deacetylation, offers biocompatibility, biodegradability, antibacterial properties, and can be molded into various geometries [101].
Synthetic Polymer-Based Scaffolds
Synthetic polymers offer tunable mechanical properties, predictable degradation rates, and batch-to-batch consistency, addressing some limitations of natural materials.
Common synthetic polymers include polycaprolactone (PCL), poly(lactic-co-glycolic acid) (PLGA), polyvinyl alcohol (PVA), and thermoplastic polyurethane (TPU). PCL and PLGA have been widely used in scaffold fabrication due to their tuneable mechanical properties and degradation rates [52]. TPU provides excellent elasticity and durability, ideal for enduring dynamic environments like blood vessels [102].
Despite their advantages, synthetic polymers frequently exhibit insufficient bioactivity and may provoke inflammatory responses upon degradation [52]. They also lack natural cell recognition sites, often requiring surface modification or functionalization to improve cellular interactions.
Hybrid Scaffold Systems
Hybrid scaffolds combine materials from different origins (natural-natural, natural-synthetic, or polymer-ceramic) to create systems that surpass the limitations of single-material constructs [10]. These systems strategically integrate components to achieve optimized mechanical properties, bioactivity, and degradation profiles.
Examples include silk fibroin-TPU blends for vascular grafts [102], composite hydrogel-biodegradable magnesium scaffolds for osteochondral regeneration [103], and polymer-ceramic composites for bone tissue engineering [104]. The integration of stimuli-responsive mechanisms through 4D printing and shape memory polymers further enhances their potential for advanced clinical applications [10].
Table 1: Comparative Properties of Scaffold Material Classes
| Property | Natural Polymers | Synthetic Polymers | Hybrid Systems |
|---|---|---|---|
| Biocompatibility | High (inherent bioactivity) [52] [101] | Variable (may cause inflammatory responses) [52] | Tunable (can be optimized) [10] [103] |
| Mechanical Strength | Generally low (requires reinforcement) [52] | High and tunable [52] [102] | Can be engineered for specific applications [103] [104] |
| Degradation Rate | Variable (often unpredictable) [52] | Controllable and predictable [52] | Designed to match tissue regeneration pace [10] |
| Bioactivity | High (cell recognition sites present) [52] [101] | Low (requires functionalization) [52] | Can incorporate bioactive elements [10] [105] |
| Manufacturing Reproducibility | Low (batch-to-batch variations) [52] | High (consistent properties) [52] | Moderate to high (depends on components) [10] |
| Cost Effectiveness | High (sustainable sources) [52] | Variable (depends on polymer complexity) | Moderate to high (depends on component combination) |
| Clinical Translation | Several in clinical use (e.g., chitosan scaffolds) [101] | Widely used in clinical applications | Emerging (showing promising results) [10] [103] |
Key Design Parameters for Scaffold Development
Biocompatibility and Biodegradability
Biocompatibility—the ability of a scaffold to interact with local tissue safely without apparent hazardous effects—is a fundamental requirement for all tissue engineering scaffolds [101]. Biodegradability refers to the scaffold's ability to degrade slowly and be metabolized, facilitating tissue regeneration while the scaffold gradually transfers load to the newly formed tissue [101]. Degradation products must not induce cellular toxicity or interfere with the differentiation and proliferation of stem cells or specialized cells like chondrocytes [101].
Mechanical and Structural Properties
Scaffolds must provide adequate mechanical stimuli to facilitate cell growth and differentiation while withstanding physiological loads [101]. The compressive modulus of materials should closely match that of native tissue; for articular cartilage, this ranges from 0.02–1.16 MPa in the superficial zone to 6.44–7.75 MPa in the deep zone [101].
Porosity and pore architecture critically influence nutrient flow, cell migration, proliferation, and ECM secretion [101]. Proper porosity, typically characterized by interconnected pores with appropriate size distributions, facilitates tissue integration while maintaining mechanical integrity. Excessive porosity can reduce mechanical properties and hinder cell adhesion, while insufficient porosity limits cell migration and proliferation [101].
Bioactivity and Functionalization
Beyond structural support, scaffolds can be functionalized with bioactive molecules to direct specific cellular responses. Incorporation of growth factors, cytokines, drugs, or extracellular vesicles can promote targeted tissue regeneration [101]. For example, curcumin integration into scaffolds provides anti-inflammatory, antioxidant, anti-catabolic, and chondroprotective effects, though its clinical translation is hindered by poor bioavailability that requires advanced delivery systems [105].
Surface topography, from nano-topography to complex micropatterns, represents another biofunctionalization strategy that significantly influences cell adhesion and proliferation [101].
Experimental Methodologies for Scaffold Evaluation
Scaffold Fabrication Techniques
Various fabrication techniques are employed to develop scaffolds with specific architectural features:
- Electrospinning: Creates nanofibrous mats that mimic native ECM structure, used for creating aligned fibers for vascular grafts [102] or starch-based nanofibrous mats for soft tissue engineering [52].
- Freeze-drying: Produces highly porous scaffolds through sublimation, used for creating nanocomposite scaffolds with hydroxyapatite, magnetic clay, and graphene oxide for bone tissue engineering [104].
- 3D Bioprinting: Enables precise spatial control over scaffold architecture and cell placement, allowing creation of complex structures with multiple materials and gradients [10].
- Solvent Casting/Particulate Leaching: Creates porous structures by dissolving away porogens from a polymer matrix, controlling pore size and interconnectivity [52].
DECIPHER Method for Cardiac Tissue Engineering
The DECellularized In situ Polyacrylamide Hydrogel–ECM hybRid (DECIPHER) method represents an advanced approach for creating scaffolds that independently control ligand presentation and stiffness [106]. This protocol enables investigation of age-related cardiac fibroblast activation:
- Tissue Stabilization: Native murine cardiac tissue sections (young: 1-2 months; aged: 18-24 months) are stabilized using N-methylolacrylamide, formed by prereacting acrylamide hydrogel solution with formaldehyde, which binds to amine groups of tissue proteins.
- Hydrogel Crosslinking: PA hydrogel is crosslinked with ultraviolet (UV) light while linked to methacrylated coverslips, stabilizing tissue proteins onto the PA mesh and creating an interpenetrating hybrid hydrogel.
- Decellularization: Optimized decellularization using sodium deoxycholate (SDC) and deoxyribonuclease (DNase) completely removes cellular structures while preserving >95.8% of collagen and >52.0% of sulfated glycosoaminoglycans (sGAGs).
- Mechanical Tuning: PA hydrogel compositions are optimized to mimic young (E = 11.5 ± 0.9 kPa) or aged (E = 39.6 ± 4.0 kPa) tissue stiffness, independently of the native ECM ligand presentation.
- Cell Seeding: Primary cardiac fibroblasts are seeded onto four scaffold combinations: SoftY (soft, young ECM), StiffY (stiff, young ECM), SoftA (soft, aged ECM), and StiffA (stiff, aged ECM).
This method demonstrates that young ECM ligand presentation can outweigh profibrotic stiffness cues in maintaining cardiac fibroblast quiescence, providing insights for matrix-based treatment strategies [106].
Molecular Dynamics Simulation for Protein-Scaffold Interactions
Molecular dynamics simulations provide a computational approach to predict protein adsorption and cell adhesion potential of scaffold materials before experimental validation [102]:
- System Setup: Three different compositions of Bombyx mori silk fibroin (SF) and thermoplastic polyurethane (TPU)—SF:TPU-3/7 (70% TPU), SF:TPU-1/1 (50% TPU), and SF:TPU-7/3 (30% TPU)—are modeled.
- Force Field Application: The Dreiding force field is applied to compute potential energy, considering both bonded (bond stretching, angle bending, dihedral torsion, inversion) and non-bonded (van der Waals, electrostatic, hydrogen bonding) contributions.
- Protein Interaction Simulation: Interactions between scaffold surfaces and vascular ECM proteins (fibronectin and laminin) are simulated using Material Studio software.
- Adhesion Energy Calculation: Adhesion energy is calculated based on van der Waals interactions, electrostatic forces, and hydrogen bonding quantified using the Lennard-Jones potential equation.
- Conformational Analysis: Final protein conformation after adsorption is analyzed to predict cell attachment capability.
- Experimental Validation: Simulation predictions are validated through MTT cell viability assays, cell adhesion studies, and live/dead assays using third-passage human umbilical vein endothelial cells (HUVECs).
This approach demonstrated that balanced SF and TPU content (SF:TPU-1/1) yielded the highest cell viability (94.7%), validating simulation predictions [102].
Table 2: Characterization Techniques for Scaffold Evaluation
| Characterization Category | Specific Techniques | Key Parameters Measured | Application Examples |
|---|---|---|---|
| Structural Analysis | Scanning Electron Microscopy (SEM) [104] [102] | Surface morphology, pore structure, fiber diameter | Nanocomposite scaffold imaging [104]; Cell adhesion assessment [102] |
| Architectural Analysis | Confocal Imaging [106], IHC [106] | Fiber alignment, porosity, interconnectivity | DECIPHER scaffold architecture quantification [106] |
| Mechanical Testing | Nanoindentation [106], Compression Testing [104] | Young's modulus, compressive strength, viscoelasticity | Cardiac tissue stiffness mapping [106]; Bone scaffold compression testing (12 MPa for PVA/CMC/HAp/CGF) [104] |
| Compositional Analysis | XRD, FT-IR [104], IHC [106] | Chemical composition, crystallinity, functional groups | Nanocomposite scaffold component verification [104]; ECM composition preservation [106] |
| Thermal Analysis | TGA [104] | Thermal stability, decomposition temperature | Polymer nanocomposite degradation behavior [104] |
| Biological Evaluation | MTT Assay [104] [102], Live/Dead Staining [102] | Cell viability, proliferation, cytotoxicity | HUVEC viability on SF/TPU scaffolds [102]; Osteoblast viability on nanocomposites [104] |
| Protein Interaction | Molecular Dynamics Simulation [102] | Adhesion energy, protein conformation | Fibronectin and laminin adsorption on polymer blends [102] |
Advanced Applications and Case Studies
Curcumin-Based Scaffolds for Cartilage Regeneration
Curcumin, a natural polyphenol with multi-modal therapeutic properties, has been integrated into advanced cartilage tissue engineering scaffolds to address its poor bioavailability [105]. Implementation strategies include:
- Delivery Systems: Nanoparticles, hydrogels (chitosan, gelatin methacrylate), and synthetic scaffolds (PCL, PLGA) enable targeted, sustained release of curcumin [105].
- Therapeutic Mechanisms: Curcumin suppresses NF-κB and COX-2 pathways, reduces IL-1β and TNF-α levels, scavenges ROS, inhibits MMPs, and promotes collagen type II and aggrecan synthesis [105].
- Clinical Formulations: Bioavailable formulations like Meriva (curcumin-phosphatidylcholine complex) and Theracurmin (nanoparticulate formulation) significantly improve WOMAC scores, reduce inflammatory markers (IL-6, CRP) in OA patients, and enhance joint function post-mosaicplasty [105].
Soft-Hard Hybrid Scaffold for Osteochondral Regeneration
Osteochondral injuries present a unique challenge requiring regeneration of both cartilage and subchondral bone. A novel hybrid scaffold addresses this need through [103]:
- Cartilage Layer: Bioactive hydrogel containing kartogenin (KGN) and bone marrow stromal cells (BMSCs) replicates the mechanical properties and chondrogenic potential of native hyaline cartilage.
- Bone Layer: Biodegradable magnesium (Mg) alloy scaffold with customized porous structure provides mechanical response comparable to trabecular bone, supporting regulated degradation, angiogenesis, and osteogenesis.
- Integration Strategy: The bioactive hydrogel is compressed into the pores of the Mg scaffold, creating a stable interface throughout the repair process that simultaneously promotes regeneration of both cartilage and subchondral bone through upregulation of osteogenic and chondrogenic specific genes [103].
Nanocomposite Scaffolds for Bone Tissue Engineering
Advanced nanocomposite scaffolds combine natural polymers (carboxymethyl cellulose/CMC or alginate/Alg), synthetic polymers (PVA), and functional additives for enhanced bone regeneration [104]:
- Composition: PVA/CMC or PVA/Alg polymer matrix with 10 wt.% hydroxyapatite (HAp) and 2 wt.% magnetic clay nanoparticles modified with graphene oxide (CGF).
- Fabrication: Scaffolds prepared using freeze-drying process create porous polymer matrices favorable for cell infiltration and nutrient transport.
- Properties: PVA/CMC/HAp/CGF scaffold demonstrates compressive strength of 12 MPa, porosity of 72%, swelling of 1860%, and biodegradation of 43% over 21 days—properties suitable for cancellous bone regeneration [104].
- Bioactivity: Excellent biomineralization in simulated body fluid (SBF) and favorable cell viability in MTT tests (OD: 1.483 for PVA/CMC/HAp/CGF) confirm therapeutic potential [104].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Scaffold Development and Evaluation
| Reagent/Material | Category | Function/Application | Example Use Cases |
|---|---|---|---|
| Plant-based Polymers (Cellulose, Alginate, Starch, Soy protein) [52] | Natural Material | Sustainable, biocompatible scaffold matrix with tunable properties | Bone regeneration, wound healing, drug delivery [52] |
| Silk Fibroin (B. mori) [102] | Natural Material | High tensile strength, controlled biodegradability, supports tissue integration | Vascular grafts, cartilage repair [101] [102] |
| Chitosan [101] | Natural Material | Biocompatible, biodegradable, antibacterial properties, moldable geometries | Cartilage scaffolds (clinical use with microfracture techniques) [101] |
| Thermoplastic Polyurethane (TPU) [102] | Synthetic Polymer | Excellent elasticity, durability, blood compatibility | Vascular grafts in dynamic environments [102] |
| Polycaprolactone (PCL) [52] | Synthetic Polymer | Tunable mechanical properties, controlled degradation rates | Electrospun scaffolds, hybrid systems [52] |
| Polyvinyl Alcohol (PVA) [104] | Synthetic Polymer | High mechanical strength, low toxicity, chemical stability | Nanocomposite scaffolds with CMC or Alg [104] |
| Hydroxyapatite (HAp) [104] | Ceramic Additive | Enhances biomineralization, osteoconduction, mechanical strength | Bone tissue scaffolds (10 wt.% loading) [104] |
| Magnesium (Mg) Alloy [103] | Metallic Component | Biodegradable metal with osteogenic potential, mechanical support | Osteochondral scaffold bone layer [103] |
| Graphene Oxide (GO) [104] | Nanomaterial Additive | Improves mechanical properties, antibacterial, osteoinductive | Modified clay composites in bone scaffolds [104] |
| Curcumin [105] | Bioactive Compound | Anti-inflammatory, antioxidant, chondroprotective effects | Cartilage regeneration scaffolds (requires delivery systems) [105] |
| Kartogenin (KGN) [103] | Bioactive Molecule | Chondrogenic differentiation promoter | Osteochondral scaffold cartilage layer [103] |
The field of scaffold-based tissue engineering continues to evolve with several emerging trends shaping future research directions. Smart scaffolds incorporating stimuli-responsive mechanisms through 4D printing and shape memory polymers represent a paradigm shift toward dynamic systems that mimic the complex and changing properties of living tissues [10]. These advanced materials can respond to various biological stimuli, enabling more precise control over tissue regeneration processes.
The integration of computational design tools with experimental validation accelerates scaffold development and optimization. Molecular dynamics simulations, as demonstrated for SF-TPU vascular grafts, provide powerful predictive capabilities for protein adsorption and cell adhesion potential before embarking on extensive experimental work [102]. This computational-experimental approach streamlines material selection and reduces development timelines.
Multi-material fabrication techniques enable creation of graded scaffolds that address interfacial tissue regeneration challenges, such as osteochondral defects requiring simultaneous regeneration of cartilage and bone [103]. These approaches better recapitulate the natural transitions between different tissue types, promoting functional integration.
Despite significant advances, challenges remain in achieving optimal vascularization of engineered constructs, controlling immune responses to scaffold materials, and ensuring manufacturing scalability and reproducibility for clinical translation. The development of plant-based polymers addresses sustainability concerns but requires further refinement of their mechanical properties and degradation control [52].
In conclusion, the strategic selection and combination of natural, synthetic, and hybrid materials enables design of scaffolds with tailored properties for specific tissue engineering applications. As research advances, the integration of biological knowledge with material science innovations will continue to produce increasingly sophisticated scaffolds that better mimic native tissue environments, ultimately enhancing clinical outcomes in regenerative medicine.
The development of biomaterial scaffolds for tissue engineering represents a frontier in regenerative medicine, offering potential solutions for repairing or replacing damaged tissues and organs. The efficacy of these scaffolds, however, is contingent upon rigorous and standardized evaluation through a hierarchy of biological models. Benchmarking success across in vitro systems, in vivo animal models, and emerging ex vivo platforms is critical for translating promising biomaterials from the laboratory to clinical application. This guide provides a comprehensive technical framework for evaluating regenerative efficacy, focusing on the integration of quantitative metrics, standardized protocols, and functional outcomes tailored for researchers and drug development professionals. The ultimate goal is to establish a robust predictive value between preclinical performance and clinical success for scaffold-based therapies, which is essential for gaining regulatory approval and ensuring patient safety [107] [108].
The selection of appropriate models is driven by the need to replicate the complex multi-faceted biological environment that scaffolds will encounter in the human body. No single model can fully capture this complexity; therefore, a sequential, complementary approach is necessary. In vitro models provide initial high-throughput data on biocompatibility and mechanism of action, while in vivo models offer insights into systemic integration, functional restoration, and long-term safety. Recent advancements have also emphasized the importance of disease-specific models that can simulate pathological microenvironments, such as chronic inflammation or impaired vascularization, providing a more realistic assessment of therapeutic potential [108] [47].
Foundational Principles of Biomaterial Scaffold Evaluation
The evaluation of any biomaterial scaffold is guided by a set of core principles that correspond to its intended biological performance. These principles form the basis for selecting appropriate assay endpoints across all testing models.
- Biocompatibility and Biodegradability: The scaffold must support cell adhesion, proliferation, and differentiation without eliciting a detrimental immune response. Its degradation profile should be controllable, and the degradation by-products must be non-cytotoxic and effectively cleared by the body [47]. This is a foundational assessment performed initially in vitro.
- Mechanical and Structural Properties: The scaffold must possess mechanical properties (e.g., compressive modulus, tensile strength) that are appropriate for the target tissue to provide structural support and integrity until new tissue forms. Porosity and pore interconnectivity are critical for cell infiltration, vascularization, and nutrient waste exchange [47].
- Bioactivity and Functional Efficacy: Beyond passive structural support, scaffolds are increasingly designed to be bioactive. This includes the capacity for spatiotemporally controlled delivery of growth factors, drugs, or genes to actively direct cellular processes and modulate the host immune response towards a regenerative outcome [108] [47].
Table 1: Key Properties for Scaffold Evaluation and Their Corresponding Metrics
| Property Category | Key Metrics | Relevant Testing Models |
|---|---|---|
| Biocompatibility | Cell viability, Apoptosis, Immunogenicity (cytokine secretion), Hemocompatibility | In vitro cell culture, Ex vivo whole blood assay |
| Biodegradation | Mass loss profile, Swelling behavior, By-product analysis (HPLC/MS) | In vitro simulated body fluid, In vivo implantation |
| Mechanical | Compressive/Tensile modulus, Stress-strain curve, Fatigue resistance | In vitro mechanical testers, In vivo functional recovery |
| Structural | Porosity, Pore size distribution, Surface topography (SEM) | Scanning Electron Microscopy (SEM), Micro-CT |
| Bioactivity | Growth factor release kinetics, Gene expression (qPCR), Protein synthesis (Western Blot, IHC) | In vitro cell culture, In vivo implantation and retrieval |
In Vitro Model Systems
In vitro models serve as the first line of evaluation, offering controlled, high-throughput systems for initial safety and efficacy screening.
Two-Dimensional (2D) Cell Culture
Protocol 1: Standardized Cytocompatibility and Cell Adhesion Assay
- Objective: To quantitatively assess scaffold support for cell attachment, viability, and proliferation.
- Materials: Sterile scaffold discs (e.g., 5 mm diameter, 2 mm thickness), cell line relevant to target tissue (e.g., chondrocytes for cartilage, HSCs for hematopoietic), complete cell culture medium, Live/Dead staining kit, AlamarBlue or MTS reagent, Phalloidin/DAPI staining solutions.
- Methodology:
- Pre-conditioning: Sterilize scaffolds (e.g., UV irradiation, ethanol wash) and equilibrate in culture medium for 24 hours.
- Cell Seeding: Seed cells at a density of 50,000–100,000 cells per scaffold. Use a drop-wise method to ensure uniform cell distribution and allow 2-4 hours for attachment in an incubator (37°C, 5% CO₂).
- Viability Assessment (Day 1, 3, 7): Incubate cell-scaffold constructs with Live/Dead stain (Calcein-AM for live cells, Ethidium homodimer-1 for dead cells) for 30-45 minutes. Image using confocal microscopy to visualize viable and non-viable cells in 3D.
- Proliferation Quantification (Day 1, 3, 7): Transfer constructs to a new plate with medium containing 10% AlamarBlue reagent. Incubate for 2-4 hours, then measure fluorescence (Ex/Em ~560/590 nm). Normalize readings to day 1.
- Cytoskeletal Organization (Endpoint): Fix constructs with 4% PFA, permeabilize with 0.1% Triton X-100, and stain with Phalloidin (for F-actin) and DAPI (for nuclei). Image using confocal microscopy to assess cell morphology and spreading within the scaffold architecture [47].
- Data Interpretation: A successful scaffold will show a high percentage of live cells, a significant increase in metabolic activity over time, and well-spread cytoskeletal architecture, indicating positive cell-material interactions.
Three-Dimensional (3D) and Co-Culture Systems
3D cultures more accurately mimic the natural tissue microenvironment. Co-culture systems are vital for evaluating scaffolds designed to support multiple cell types, such as in vascularized tissue constructs.
Protocol 2: Osteochondral Co-culture Model for Gradient Scaffolds
- Objective: To evaluate the efficacy of a biphasic scaffold in supporting the simultaneous differentiation of chondrogenic and osteogenic lineages.
- Materials: Biphasic scaffold (e.g., collagen-HA hydrogel top for cartilage, silicate-based ceramic bottom for bone), human Mesenchymal Stem Cells (hMSCs), chondrogenic medium (with TGF-β3), osteogenic medium (with BMP-2 and dexamethasone).
- Methodology:
- Sequential Seeding: Seed hMSCs onto the chondrogenic phase at a high density (e.g., 10x10^6 cells/mL). After 4 hours, seed hMSCs onto the osteogenic phase.
- Differential Culture: Maintain the construct in a dual-medium system or a custom osteochondral medium for 21-28 days, changing the medium every 2-3 days.
- Endpoint Analysis:
- Gene Expression: Separate the two phases and perform RNA extraction and qPCR for chondrogenic markers (e.g., COL2A1, ACAN, SOX9) and osteogenic markers (e.g., RUNX2, OSTERIX, COL1A1).
- Histology: Section the entire construct and stain with Safranin O/Fast Green (for glycosaminoglycans in cartilage) and Alizarin Red (for calcium deposits in bone) [47].
- Data Interpretation: Successful scaffold design will demonstrate spatially confined gene upregulation and matrix deposition specific to each lineage, indicating the scaffold's ability to guide region-specific tissue formation.
In Vivo Animal Models
In vivo models are indispensable for assessing systemic toxicity, immunogenicity, functional integration, and long-term stability of scaffolds in a complex physiological environment. The choice of model is dictated by the target clinical application.
Small Animal Models
Rodents (Mice and Rats) are widely used for preliminary in vivo testing due to their low cost, availability of genetic tools, and well-characterized immune systems. They are ideal for proof-of-concept studies on scaffold biocompatibility, degradation, and early-stage tissue integration.
Protocol 3: Subcutaneous Implantation for Biocompatibility and Degradation
- Objective: To evaluate the host inflammatory response and in vivo degradation profile of a novel scaffold.
- Animal Model: Immunocompetent (e.g., C57BL/6) or immunodeficient (e.g., nude mouse) for human cell-seeded scaffolds.
- Methodology:
- Implantation: Anesthetize the animal. Make a small dorsal incision and create subcutaneous pockets. Implant sterile scaffold discs (e.g., 8 mm diameter). Include a sham operation as a control.
- Study Timeline: Explant scaffolds at predetermined time points (e.g., 1, 4, 12 weeks).
- Explant Analysis:
- Histology: Process explants for H&E staining to assess general tissue architecture and presence of immune cells (neutrophils, lymphocytes, macrophages). Use Masson's Trichrome to visualize collagen deposition.
- Immunohistochemistry (IHC): Stain for CD68 (pan-macrophage marker) and CD206 (M2 pro-regenerative macrophage marker) to characterize the immune response.
- Scaffold Degradation: Measure remaining scaffold mass and analyze morphology via SEM [47].
Large Animal Models
Porcine (Pig) models are often considered a critical step before clinical trials due to their physiological and anatomical similarities to humans, particularly in skin wound healing, cardiovascular studies, and joint size.
Protocol 4: Porcine Full-Thickness Burn Model for Skin-Regenerating Scaffolds
- Objective: To assess the efficacy of a cell-seeded scaffold in promoting wound healing and skin regeneration.
- Source: This protocol is adapted from a recent study using iMSCs seeded on Integra for burn wound healing [109].
- Methodology:
- Burn Creation and Excision: Create standardized full-thickness burns on the porcine dorsum. Perform wound excision to remove necrotic tissue.
- Scaffold Application: Seed Induced Mesenchymal Stem Cells (iMSCs) onto Integra Dermal Regeneration Template at densities of 5,000–20,000 cells/cm². Apply the acellular Integra and cell-seeded scaffolds to the excised wounds.
- In Vivo Monitoring:
- Wound Closure Rate: Capture digital images weekly and calculate the percentage reduction in wound area over time.
- Re-epithelialization: Quantify the rate and extent of new epithelial layer formation.
- Scar Assessment: Use the Vancouver Scar Scale (VSS) at the endpoint to evaluate scar quality (pliability, height, vascularity, pigmentation).
- Endpoint Histomorphometry:
- After 40 days, euthanize the animal and collect tissue samples.
- Analyze for neovascularization (IHC for CD31), collagen levels (Trichrome stain), and fibrosis markers (e.g., α-SMA) [109].
- Data Interpretation: A superior scaffold treatment will show significantly accelerated wound closure, improved re-epithelialization, higher quality of regenerated skin with mature vascular structures, and reduced fibrosis compared to acellular controls.
Table 2: Key In Vivo Models for Specific Tissue Engineering Applications
| Target Tissue | Recommended Model | Key Outcome Measures | Advantages |
|---|---|---|---|
| Skin | Porcine full-thickness burn model [109] | Wound closure rate, Re-epithelialization, Scar quality (VSS), Neovascularization | Skin anatomy and healing process closely mimics humans |
| Cartilage | Ovine model [47] | International Cartilage Repair Society (ICRS) score, Histology (Safranin O), Mechanical indentation testing | Comparable joint size and loading conditions |
| Bladder | Rodent or porcine augmentation model [49] | Urodynamics (capacity, compliance), Histology for smooth muscle and urothelium regeneration | Functional readout of organ-level performance |
| Bone | Critical-sized calvarial defect in rats or rabbits | Micro-CT (bone volume, density), Histology (H&E, Trichrome) | Highly standardized, quantifiable defect model |
| Hematopoietic System | Murine xenotransplantation model [107] | Human cell engraftment in bone marrow, Multilineage differentiation in peripheral blood | Gold standard for assessing functional HSC activity |
Data Integration and Analysis
The final step in benchmarking is the holistic integration of data from all models to build a compelling case for the scaffold's therapeutic potential.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Evaluating Regenerative Scaffolds
| Reagent / Material | Function / Application | Example in Context |
|---|---|---|
| UM171 Molecule [107] | Small molecule that enhances ex vivo expansion of hematopoietic stem cells (HSCs) by promoting self-renewal. | Used in culture protocols for umbilical cord blood HSCs to achieve therapeutic cell doses. |
| Nicotinamide (NAM) [107] | Epigenetic inhibitor that reduces reactive oxygen species (ROS) and improves mitochondrial metabolism in HSCs. | Supplemented in culture medium to maintain HSC "stemness" during expansion. |
| Soluplus Polymer [107] | A caprolactam-based polymer used as a substrate in chemically defined culture systems. | Enabled a 55-fold selective expansion of CD34+ UCB-HSCs. |
| Integra Dermal Regeneration Template [109] | A synthetic bilayer scaffold (bovine collagen + glycosaminoglycan) used as a wound coverage material. | Served as a delivery vehicle for iMSCs in a porcine burn model. |
| Electroactive Biodegradable Elastomer [49] | A conductive scaffold material that provides electrical cues without needing seeded cells. | Used for cell-free bladder tissue regeneration, restoring function in animal models. |
| Type I/II Collagen & Hyaluronic Acid (HA) Scaffolds [47] | Natural polymer-based scaffolds that mimic the native cartilage extracellular matrix (ECM). | Provide a bioactive 3D environment for chondrocyte adhesion and cartilage matrix production. |
Visualizing Workflows and Signaling Pathways
The following diagrams illustrate the core experimental workflow for scaffold evaluation and a key molecular pathway modulated by culture additives.
Diagram 1: Scaffold evaluation workflow.
Diagram 2: HSC expansion molecular pathway.
The clinical translation of biomaterial scaffolds for tissue engineering represents a rapidly advancing frontier in regenerative medicine, with millions of patients having been treated with extracellular matrix (ECM)-based scaffolds alone [110]. These products have become standard of care in applications ranging from breast reconstruction and hernia repair to chronic wound treatment [110]. Despite these successes, the path to regulatory approval remains complex, requiring careful navigation of evolving regulatory frameworks, rigorous validation protocols, and demonstration of both safety and clinical benefit. The regulatory acceptance of novel endpoints and technologies can be a "long, multifaceted and costly process" that demands strategic planning from the earliest development stages [111]. This technical guide examines the current regulatory considerations and standardization requirements for biomaterial scaffolds within the context of tissue engineering applications, providing researchers and product developers with a framework for successful clinical translation.
The U.S. Food and Drug Administration (FDA) regulates regenerative medicine products primarily through the Food, Drug, and Cosmetics Act (FD&C) and the Public Health Service Act, with human cell, tissue, and cellular and tissue-based products (HCT/Ps) falling under the Center for Biologics Evaluation and Research (CBER) [112]. The recent establishment of the Office of Therapeutic Products (OTP) within CBER in 2023 has streamlined the evaluation process for novel cell and gene therapy products, including combination products that incorporate biomaterial scaffolds [112]. As of 2025, only a limited number of cell-based tissue engineering therapies have received FDA approval, highlighting the stringent requirements for clinical translation [112]. For combination products that deliver manufactured cells with ECM or other scaffolds, compliance must be demonstrated for all individual components in addition to the final combinatory product, as specified in 21 CFR Part 4 [112].
Regulatory Framework and Approval Pathways
FDA Regulatory Structure and Product Classification
Biomaterial scaffolds for tissue engineering applications typically follow one of several regulatory pathways depending on their composition, mechanism of action, and intended use. The FDA's risk-based approach categorizes products based on their potential risk to patients, with more novel products generally facing more comprehensive approval requirements [112]. The regulatory classification of a biomaterial scaffold significantly impacts the evidentiary requirements for approval, with combination products often requiring the most extensive data packages.
Table 1: FDA Regulatory Pathways for Biomaterial Scaffolds
| Product Category | Primary Center | Key Regulatory Considerations | Examples |
|---|---|---|---|
| Biologic Scaffolds | CBER/OTP | Chemistry Manufacturing and Controls (CMC), potency, clinical benefit | ECM scaffolds for wound healing [110] |
| Medical Devices with Biologic Components | CDRH/CBER | Substantial equivalence or de novo classification, biocompatibility | Surgical mesh with biologic coating [112] |
| Combination Products | CBER (Lead) | Compliance with both device and biologic regulations, cross-center collaboration | Cell-seeded scaffolds for tissue regeneration [112] |
| HCT/Ps | CBER | Minimal manipulation, homologous use requirements | Decellularized tissues for transplantation [112] |
The classification of a product depends heavily on the "degree of novelty" and how distinct the final product is from native human tissues [112]. Products that are more distinct from native tissues or incorporate novel technologies generally face more complex approval processes, as they cannot rely on pre-existing approved technologies for substantial equivalence determinations [112].
Key Regulatory Considerations for Biomaterial Scaffolds
Several key considerations dominate the regulatory pathway for biomaterial scaffolds. First, the Context of Use (CoU) must be clearly defined, including how the scaffold will be used in clinical trials, the patient population, study design, and endpoint hierarchy [111]. The CoU directly influences the validation requirements and evidentiary burden. Second, the Concept of Interest (CoI) must represent a health experience meaningful to patients and reflect the intended treatment benefit [111]. For novel endpoints, establishing early whether they address core disease aspects and are meaningful to patients is crucial for regulatory acceptance.
The FDA's fit-for-purpose approach recognizes that the validation requirements should be appropriate for the intended use of the scaffold or endpoint [111]. The highest evidentiary bar applies to products intended as primary endpoints or to support label claims in pivotal trials [111]. For biomaterial scaffolds, this typically requires comprehensive data on:
- Biocompatibility and immunogenicity: The scaffold must demonstrate acceptable interaction with host tissues without excessive immune activation [12] [101]
- Mechanical properties: Scaffolds must provide appropriate mechanical support matching native tissue characteristics [101]
- Degradation profile: The rate of degradation should match tissue regeneration while avoiding toxic byproducts [110] [101]
- Clinical performance: Meaningful functional improvement must be demonstrated in the target population
Table 2: Key Properties and Validation Requirements for Biomaterial Scaffolds
| Property Category | Key Parameters | Standardized Testing Methods | Regulatory Thresholds |
|---|---|---|---|
| Biocompatibility | Cytotoxicity, hemocompatibility, sensitization | ISO 10993 series, MTT assay, live/dead staining | No cytotoxicity, acceptable immune response [101] |
| Mechanical Properties | Compressive modulus, tensile strength, suture retention | ASTM F2150, ASTM D638, ASTM F2458 | Match native tissue properties (e.g., 0.02-1.16 MPa for superficial cartilage) [101] |
| Degradation | Mass loss profile, byproduct analysis, mechanical integrity | Mass loss over time, HPLC for byproducts | Non-toxic byproducts, degradation rate matching tissue regeneration [110] [101] |
| Sterility | Sterility assurance, endotoxin levels, bioburden | USP <71>, bacterial endotoxin testing | Sterile, endotoxin limits based on product type [112] |
| Potency | Bioactivity, host cell infiltration, tissue formation | In vitro bioactivity assays, in vivo integration studies | Quantitative measure of therapeutic effect [112] |
Standardization of Validation Protocols
Decellularization and ECM Scaffold Standardization
Decellularization protocols for biologic scaffolds demonstrate the critical importance of standardization in tissue engineering. Current literature reveals "significant variability in in vitro culture conditions," including cell origin and type, culture media and sera, fusion-inducing factors, seeding density, and culture surfaces [113]. This variability complicates cross-study comparisons and hinders regulatory evaluation. Similar challenges exist in decellularization protocols, which "differ among species and research groups," particularly in the choice of decellularization agents [114].
Successful decellularization must balance complete cell removal with preservation of ECM integrity and bioactivity. The gold standard for decellularization validation includes:
- Quantification of DNA removal: Less than 50 ng double-stranded DNA (dsDNA) per mg ECM dry weight [110]
- Verification of ECM composition retention: Preservation of key structural and functional proteins including collagen, elastin, and glycosaminoglycans (GAGs) [110]
- Confirmation of ultrastructure maintenance: Retention of native ECM architecture via scanning electron microscopy (SEM) [114] [110]
- Demonstration of bioactivity: Support of cell adhesion, proliferation, and differentiation in vitro [12]
Standardization efforts should establish minimum reporting requirements for decellularization protocols, including specific agents, concentrations, exposure times, temperature conditions, and washing procedures. Furthermore, standardized quantitative metrics for assessing decellularization efficacy and ECM preservation are essential for regulatory evaluation and comparison across studies.
In Vitro Validation Protocols
Standardized in vitro validation provides critical data for regulatory submissions and helps establish a product's biologic activity before proceeding to costly animal studies. Key validation protocols include:
Foreign Body Response (FBR) Assessment The foreign body reaction represents a significant challenge for implanted biomaterials. Standardized protocols for in vitro assessment of FBR include:
- Foreign Body Giant Cell (FBGC) Formation Assay: Using primary human macrophages cultured with fusion-inducing factors (e.g., IL-4, IL-13) for 7-14 days, with quantification of multinucleated cells containing three or more nuclei [113]
- Macrophage Polarization Assessment: Flow cytometry analysis of M1 (pro-inflammatory) and M2 (pro-regenerative) macrophage markers following material exposure
- Cytokine Secretion Profiling: Multiplex ELISA analysis of pro-inflammatory (TNF-α, IL-1β, IL-6) and regulatory (IL-10, TGF-β) cytokines
Bioactivity and Potency Assays Potency assays representing the product's specific ability to achieve its intended effect are required for biologic licensure [112]. For biomaterial scaffolds, these may include:
- Cell Adhesion and Proliferation Assays: Quantification of specific cell types (relevant to target tissue) adhering to and proliferating on the scaffold
- Biofactor Release Kinetics: Measurement of controlled release of incorporated growth factors or other bioactive molecules
- Host Cell Recruitment: Assessment of the scaffold's ability to recruit endogenous stem cells or progenitor cells in vitro
Diagram 1: Scaffold Validation Workflow
Preclinical Animal Model Standardization
Preclinical animal studies provide critical safety and efficacy data required for regulatory approval. Standardization of these studies includes:
- Model Selection: Choosing animal models that accurately recapitulate human disease and allow assessment of the scaffold's performance under clinically relevant conditions
- Implantation Protocol Standardization: Consistent surgical techniques, control materials, and postoperative care across study groups
- Endpoint Harmonization: Establishing standardized timepoints for assessment that capture both short-term integration and long-term functional outcomes
- Histopathological Scoring Systems: Using validated, quantitative scoring systems for tissue integration, vascularization, immune response, and remodeling
For cartilage repair applications, large animal models such as ovine or caprine models have demonstrated predictive value for clinical outcomes [101]. Standardized outcome measures include histological scoring using established systems (e.g., O'Driscoll, ICRS II), mechanical property assessment, and quantitative ECM composition analysis.
Experimental Design and Methodologies
Design of Experiments (DoE) for Biomaterial Optimization
The Design of Experiments (DoE) methodology provides a structured, efficient approach for optimizing biomaterial scaffold formulations while reducing experimental burden [115]. DoE analyzes the relationship between multiple input variables (factors) and output variables (responses), allowing identification of factors with the largest influence on critical quality attributes.
For bioink development, as demonstrated in UBC's iGEM project, a typical DoE approach includes:
- Planning Phase: Identification of critical factors (e.g., sodium alginate concentration, crosslinker concentration, polymer ratio) and response variables (e.g., compressive modulus, printability, cell viability)
- Screening Phase: Using fractional factorial designs to identify the most influential factors from a larger set of potential variables
- Optimization Phase: Response surface methodology (RSM) to model the relationship between critical factors and responses, identifying optimal formulation ranges
- Verification Phase: Experimental confirmation of predicted optimal formulations [115]
Table 3: Example DoE Factors and Levels for Alginate-Based Bioink Optimization
| Factor | Low Level (-1) | Middle Level (0) | High Level (1) | Response Variables |
|---|---|---|---|---|
| Sodium Alginate | 1 wt% | 2 wt% | 3 wt% | Compressive modulus, viscosity, cell viability |
| MGS-1 | 20 wt% | 30 wt% | 40 wt% | Shape fidelity, mineralization capacity |
| CMC | 2 wt% | 3 wt% | 4 wt% | Printability, structural integrity |
| Crosslinking Time | 5 min | 10 min | 15 min | Gelation kinetics, mechanical properties |
Implementation of DoE approaches provides regulators with systematic evidence of product understanding and control, supporting quality by design (QbD) principles increasingly expected in regulatory submissions.
Advanced Analytical Methodologies
Comprehensive scaffold characterization requires advanced analytical methodologies to assess properties relevant to clinical performance:
Mechanical Characterization
- Compressive Testing: Assessment of compressive modulus and strength under physiologically relevant conditions
- Tensile Testing: Evaluation of elastic modulus, ultimate tensile strength, and elongation at break
- Dynamic Mechanical Analysis (DMA): Measurement of viscoelastic properties including storage modulus (E') and loss modulus (E") [114]
Structural Characterization
- Scanning Electron Microscopy (SEM): High-resolution imaging of scaffold microstructure and porosity
- Micro-Computed Tomography (μCT): Three-dimensional analysis of pore architecture, connectivity, and distribution
- Mercury Porosimetry: Quantitative assessment of pore size distribution and total porosity
Biological Characterization
- Immunohistochemistry/Immunofluorescence: Spatial localization of specific ECM components, cell types, and signaling molecules
- DNA Quantification: Fluorometric quantification of residual DNA following decellularization [114]
- Glycosaminoglycan (GAG) Assay: Spectrophotometric quantification of sulfated GAG content via dimethylmethylene blue (DMMB) assay
- Mass Spectrometry Proteomics: Comprehensive analysis of ECM composition and retained signaling molecules
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Biomaterial Scaffold Validation
| Reagent/Material | Function | Application Examples | Key Considerations |
|---|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Ionic detergent for cell lysis and lipid removal | Decellularization protocols [114] | Concentration and exposure time must be balanced against ECM preservation |
| Sodium Deoxycholate (SDC) | Ionic detergent for nuclear membrane disruption | Decellularization protocols [114] | Typically used in combination with other detergents |
| DNase/RNase Enzymes | Nucleic acid degradation | Removal of residual genetic material after decellularization [114] | Requires specific ionic conditions for optimal activity |
| 4′,6-diamidino-2-phenylindole (DAPI) | DNA fluorescent staining | Quantification of nuclear material in decellularized tissues [114] | Standard for visualizing residual cellular material |
| MTT Assay Reagents | Cell viability and proliferation assessment | Biocompatibility testing of scaffold extracts or direct contact [114] | Colorimetric measurement of metabolic activity |
| Collagenase Enzymes | Collagen degradation | Assessment of biodegradation profile [110] | Activity varies by collagen type and source |
| RGD Peptides | Integrin-binding ligand | Biofunctionalization of synthetic scaffolds to enhance cell adhesion [12] | Mimics native ECM cell adhesion motifs |
| IL-4/IL-13 Cytokines | Macrophage fusion induction | In vitro foreign body giant cell formation assays [113] | Essential for standardized FBGC assessment |
Signaling Pathways in Host-Scaffold Integration
Understanding the molecular mechanisms governing host-scaffold integration is essential for designing biomaterials with enhanced regenerative capacity. Integrin-mediated signaling represents a primary pathway through which cells perceive and respond to biomaterial scaffolds.
Diagram 2: Integrin-Mediated Signaling Pathway
Integrins serve as fundamental mediators of bidirectional communication between cells and their ECM microenvironment [12]. These transmembrane receptors, composed of α and β subunits, recognize specific ECM components including collagen, fibronectin, and laminin, orchestrating essential cellular processes including adhesion, migration, proliferation, and survival [12]. The activation of integrin signaling begins with ECM ligand binding, which induces conformational changes that promote receptor clustering and assembly of focal adhesion complexes [12]. These specialized structures serve as mechanical and biochemical signaling hubs, recruiting adaptor proteins including talin, vinculin, and paxillin to bridge connections between integrins and the actin cytoskeleton [12].
Central to this signaling network is the focal adhesion kinase (FAK) pathway, which, upon activation at Tyr397, recruits Src family kinases to regulate cytoskeletal dynamics and promote cell migration [12]. Parallel MAPK/ERK pathway activation regulates gene expression for proliferation and differentiation, while the PI3K/Akt pathway promotes cell survival in stressful, injured tissue microenvironments [12]. These interconnected pathways function synergistically to ensure appropriate cellular responses during the repair process, and their targeted modulation through biomaterial design represents a promising strategy for enhancing regenerative outcomes.
Successful clinical translation of biomaterial scaffolds requires integrated strategic planning encompassing regulatory, technical, and clinical considerations. Early and frequent consultation with regulatory agencies through Q-Submission programs, Pre-Submission meetings (for devices), or Type C meetings (for drugs and biologics) is essential to align development strategies with regulatory expectations [111]. These consultations provide valuable feedback on proposed validation approaches, clinical trial designs, and endpoint selection, potentially de-risking the development process.
The evolving regulatory landscape for biomaterial scaffolds continues to emphasize rigorous standardization, comprehensive characterization, and demonstration of clinical benefit. By implementing robust validation protocols, employing systematic optimization approaches like DoE, and maintaining awareness of regulatory expectations throughout development, researchers can navigate the complex path to clinical approval more efficiently. The continued advancement of standardized protocols and analytical methods will further support the translation of increasingly sophisticated biomaterial scaffolds, ultimately expanding treatment options for patients requiring tissue repair and regeneration.
Conclusion
The field of biomaterial scaffolds is advancing rapidly, moving from passive structural supports to dynamic, bioinstructive environments that actively orchestrate tissue regeneration. Success hinges on a multi-faceted approach that integrates foundational material science with advanced manufacturing and a deep understanding of host immune responses. The increasing integration of AI for predictive design and high-throughput technologies for validation is set to accelerate the development of next-generation, patient-specific scaffolds. Future progress will depend on interdisciplinary collaboration to overcome persistent challenges in vascularization, immune compatibility, and the fabrication of complex, multi-tissue interfaces, ultimately bridging the critical gap between promising laboratory results and widespread clinical application in regenerative medicine.
References
- 1. In Vitro Biodegradation and Biocompatibility of Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489643/]
- 2. Biocompatibility and structural insights of seaweed-derived ... [https://www.nature.com/articles/s41598-025-19632-0]
- 3. Current advances and prospects in biomaterials-guided ... [https://www.sciencedirect.com/science/article/pii/S2666138125000131]
- 4. A Tissue Engineering's Guide to Biomimicry - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530705/]
- 5. Modern experimental methods for assessing the ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1595116/full]
- 6. Tissue Engineering Approaches to Recapitulate the Micro [https://link.springer.com/article/10.1007/s40883-025-00411-2]
- 7. Advancements in Bone Tissue Engineering [https://pubmed.ncbi.nlm.nih.gov/39989325/]
- 8. Recent Advances in 3D Bioprinting of Porous Scaffolds for ... [https://www.mdpi.com/2079-4983/16/9/328]
- 9. Smart biomaterials: as active immune modulators to shape ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1669399/full]
- 10. Advances in smart hybrid scaffolds: A strategic approach ... [https://www.sciencedirect.com/science/article/pii/S2666138125000039]
- 11. A guideline for reporting experimental protocols in life sciences [https://pmc.ncbi.nlm.nih.gov/articles/PMC5978404/]
- 12. Biomaterials in tissue repair and regeneration: key insights ... [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2025.1565810/full]
- 13. Extracellular Matrix Signaling Cues: Biological Functions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271642/]
- 14. Structural extracellular matrix-mediated molecular ... [https://www.sciencedirect.com/science/article/abs/pii/S030090842400230X]
- 15. Integrin signaling pathways in mesenchymal stem cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04608-8]
- 16. Immune Response to Extracellular Matrix Bioscaffolds [https://www.mdpi.com/2673-8449/5/3/28]
- 17. Progress in biomaterials inspired by the extracellular matrix [https://www.sciencedirect.com/science/article/pii/S2666542524000870]
- 18. Recent Advances in the Development and Application of Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071569/]
- 19. Advances in hyaluronic acid-based biomaterials: applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534349/]
- 20. Hyaluronic acid as a versatile building block for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11903855/]
- 21. Chitosan: An overview of its properties, solubility, functional ... [https://www.sciencedirect.com/science/article/abs/pii/S0008621525000357]
- 22. A Review of Recent Advances in Natural Polymer-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145843/]
- 23. Effects of silk fibroin incorporation on the mechanical ... [https://www.sciencedirect.com/science/article/pii/S2590093525000505]
- 24. In Vivo Degradation and Local Tissue Response of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359101/]
- 25. Stability, challenges, and prospects of chitosan for the ... [https://www.sciencedirect.com/science/article/pii/S2405844024159105]
- 26. / Silk – fibroin versus chitosan scaffolds for... hyaluronic acid silk fibroin [https://link.springer.com/article/10.1007/s10856-009-3876-0]
- 27. Biocomposite Scaffolds for Tissue Engineering: Materials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11595283/]
- 28. Smart and Biodegradable Polymers in Tissue Engineering and Interventional Devices: A Brief Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300715/]
- 29. Design strategies for composite matrix and multifunctional ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2022.1051678/full]
- 30. Biopolymer-based composites for tissue engineering ... [https://www.sciencedirect.com/science/article/pii/S1359836823002044]
- 31. Synthetic biodegradable functional polymers for tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4341840/]
- 32. Concomitant control of mechanical properties and ... [https://www.nature.com/articles/s41467-020-20610-5]
- 33. Frontiers | Functionalized conductive polymer composites for tissue engineering and biomedical applications- a mini review [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1533944/full]
- 34. Various manufacturing methods and ideal properties of ... [https://www.sciencedirect.com/science/article/pii/S2772810222000113]
- 35. Effect of degradation in polymer scaffolds on mechanical ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482524004864]
- 36. The Degradation of Synthetic Polymeric Scaffolds With ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.846665/full]
- 37. Tissue engineering: Hydrogel scaffolds and mechanical ... [https://www.sciencedirect.com/science/article/abs/pii/S0001868625003021]
- 38. Recent Advances in 3D Bioprinting of Porous Scaffolds for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470888/]
- 39. Recent Progress in the Application of Electrospinning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12295322/]
- 40. Preservation of biomaterials and cells by freeze-drying [https://www.sciencedirect.com/science/article/pii/S0168365921003400]
- 41. New 3D bioprinting technique may improve production of ... [https://news.mit.edu/2025/new-3d-bioprinting-technique-may-improve-production-engineered-tissue-0917]
- 42. 3D Printing for Tissue Engineering: Printing Techniques ... [https://www.mdpi.com/2306-5354/12/9/936]
- 43. Soft tissue scaffold fabrication based on electrospinning [https://www.sciencedirect.com/science/article/abs/pii/S0001868625002714]
- 44. Influence of electrospinning parameters on the ... [https://www.sciencedirect.com/science/article/pii/S2949829525001640]
- 45. Freeze-drying Technology in Pharmaceutical and ... [https://www.pharmaexcipients.com/news/freeze-drying-pharmaceutical/]
- 46. Tissue Engineering and Regeneration Market Set to Surge ... [https://www.bccresearch.com/pressroom/hlc/tissue-engineering-and-regeneration-market-set-to-surge-at-128-cagr?srsltid=AfmBOoo6GRJMsvcX0I45hh69bm_2EWqldm61RDkUjbTgytCyWx7tNgt8]
- 47. Recent advances in bionic scaffolds for cartilage tissue ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1625550/full]
- 48. Bionic scaffolds with integrated structural components ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12478442/]
- 49. Novel 'Scaffolding' Biomaterial Improves Bladder ... [https://www.mccormick.northwestern.edu/news/articles/2025/01/novel-scaffolding-biomaterial-improves-bladder-regeneration-and-function/]
- 50. Synthetic scaffolds for musculoskeletal tissue engineering [https://www.nature.com/articles/s41536-019-0076-5]
- 51. Plant-Based Scaffolds for Tissue Engineering: A Review [https://www.mdpi.com/2073-4360/17/19/2705]
- 52. Plant-based Biodegradable and Biocompatible Polymers ... [https://www.sciencedirect.com/science/article/abs/pii/S0008621525003258]
- 53. Cost-effective and eco-friendly tissue scaffolds from seaweed [https://cen.acs.org/materials/biomaterials/Cost-effective-eco-friendly-tissue/103/web/2025/10]
- 54. Ulva Seaweed-Derived Ulvan: A Promising Marine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11857750/]
- 55. The potent osteo-inductive capacity of bioinspired brown ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11358581/]
- 56. Development and optimization of decellularized seaweed ... [https://pubmed.ncbi.nlm.nih.gov/41118230/]
- 57. Seaweed Makes for Eco-Friendly Tissue Scaffolds and ... [https://publishing.aip.org/publications/latest-content/seaweed-makes-for-eco-friendly-tissue-scaffolds-and-reduces-animal-testing/]
- 58. Smart biomaterials: as active immune modulators to shape pro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12558899/]
- 59. Physical cues in biomaterials modulate macrophage ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1640560/full]
- 60. The impact of biomaterial characteristics on macrophage ... [https://www.oaepublish.com/articles/2347-9264.2024.166]
- 61. Biomaterial Strategies of Macrophage Behaviour in Bone ... [https://link.springer.com/article/10.1007/s40883-025-00443-8]
- 62. From macrophage polarization to clinical translation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504304/]
- 63. Engineering macrophage responses through 3D scaffold ... [https://www.sciencedirect.com/science/article/pii/S2590006425008993]
- 64. Harnessing Biomaterials for Immunomodulatory-Driven Tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10272262/]
- 65. Mitochondria-Targeted Biomaterials-Regulating ... [https://pubmed.ncbi.nlm.nih.gov/39925677/]
- 66. Advancements in biodegradable implants: evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577823/]
- 67. Design, Materials, and Mechanobiology of Biodegradable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4391163/]
- 68. A review of biomaterial degradation assessment ... [https://www.nature.com/articles/s41529-024-00487-1]
- 69. Mechanical properties of biomaterials' influence on hydrogel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10154526/]
- 70. Improvement of Mechanical Strength of Tissue Engineering ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8395951/]
- 71. Biomaterials Market Size to Surge USD 526.63 Billion by ... [https://www.towardschemandmaterials.com/insights/biomaterials-market]
- 72. Optimising degradation and mechanical performance of ... [https://www.sciencedirect.com/science/article/pii/S2590183423000455]
- 73. Advances in bioink-based 3D printed scaffolds [https://pubs.rsc.org/en/content/articlelanding/2025/bm/d4bm01606h]
- 74. Development and Optimization of Resorbable Biomaterials ... [https://pubmed.ncbi.nlm.nih.gov/40548428/]
- 75. Mechanical strategies to promote vascularization for tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11441985/]
- 76. Angiogenesis in Tissue Engineering: As Nature Intended? [https://pmc.ncbi.nlm.nih.gov/articles/PMC7099606/]
- 77. A strategy to engineer vascularized tissue constructs by ... [https://www.sciencedirect.com/science/article/pii/S1742706121007443]
- 78. Vascular Tissue Engineering: Challenges and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.721843/full]
- 79. Angiogenic signaling pathways and anti ... [https://www.nature.com/articles/s41392-023-01460-1]
- 80. Mitigating challenges and expanding the future of vascular ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.1079421/full]
- 81. Improving the Biocompatibility of Plant-Derived Scaffolds for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565551/]
- 82. Biomimetic vascular scaffolds via hybrid 3D printing-phase ... [https://pubmed.ncbi.nlm.nih.gov/40690254/]
- 83. Biomaterial mediated strategies targeting vascularization for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4662653/]
- 84. Biomaterial-based vascularization strategies for enhanced ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03140-4]
- 85. Engineering the Immune Response to Biomaterials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12097135/]
- 86. Modulating immune-stem cell crosstalk enables robust ... [https://www.nature.com/articles/s41536-025-00421-2]
- 87. Editorial: Tissue engineering and regenerative medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC11949865/]
- 88. Applications and Recent Advances in 3D Bioprinting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300073/]
- 89. Tailoring the mechanical and degradation properties of 3D... [https://www.degruyterbrill.com/document/doi/10.1515/rams-2025-0098/html?lang=en&srsltid=AfmBOoobryZkJAikXouB1CFCxLnugQvnh3pN_jpBBk2wrjxdynUCm9tB]
- 90. Recent advances in artificial intelligent strategies for tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11348508/]
- 91. A Technological Review of Digital Twins and Artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294331/]
- 92. A Technological Review of Digital Twins and Artificial ... [https://www.mdpi.com/2227-9032/13/14/1763]
- 93. Identification of digital twins to guide interpretable AI for ... [https://www.nature.com/articles/s41746-025-01501-9]
- 94. Review on machine learning application in tissue ... [https://link.springer.com/article/10.1007/s10853-024-10449-2]
- 95. Comparative analysis of deep learning models for ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525006328]
- 96. Artificial Intelligence in Biomaterials: A Comprehensive ... [https://www.mdpi.com/2076-3417/14/15/6590]
- 97. Multimodal AI in Biomedicine: Pioneering the Future of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195918/]
- 98. Comparative analysis of deep learning models for ... [https://pubmed.ncbi.nlm.nih.gov/40306018/]
- 99. Next-Generation Biomaterials for Load-Bearing Tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12295659/]
- 100. Biomaterial-mediated Cell Atlas: an insight from single-cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12356410/]
- 101. Recent advances in bionic scaffolds for cartilage tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289700/]
- 102. A study on the cellular adhesion properties of a hybrid ... [https://www.nature.com/articles/s41598-025-01545-7]
- 103. A soft-hard hybrid scaffold for osteochondral regeneration ... [https://pubmed.ncbi.nlm.nih.gov/40499226/]
- 104. Fabrication of biodegradable nanocomposite scaffolds with ... [https://www.nature.com/articles/s41598-025-07270-5]
- 105. A comprehensive review of curcumin-based scaffolds in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482016/]
- 106. Hybrid hydrogel–extracellular matrix scaffolds identify ... [https://www.nature.com/articles/s41563-025-02234-6]
- 107. Culturing Potential: advances in ex vivo cell culture systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284713/]
- 108. Advances in Drug Delivery Integrated with Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030587/]
- 109. Human iPSCs-derived mesenchymal stem cells promote ... [https://www.nature.com/articles/s41536-025-00427-w]
- 110. Advances, challenges, and future directions in the clinical ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X24001698]
- 111. Regulatory considerations for successful implementation of ... [https://www.nature.com/articles/s41746-025-01513-5]
- 112. Cell manufacturing for cell-based tissue engineering [https://www.frontiersin.org/journals/chemical-engineering/articles/10.3389/fceng.2025.1637075/full]
- 113. Evaluating different methodologies to induce in vitro ... [https://pubmed.ncbi.nlm.nih.gov/39826854/]
- 114. Standardizing decellularization protocols for optimized ... [https://www.sciencedirect.com/science/article/pii/S2352320424002311]
- 115. Bioink: Model Validation - 2025 UBC iGEM Wiki [https://2025.igem.wiki/ubc-vancouver/bioprinter/bioink-model-validation]