Advanced Drug-Eluting Stent Coatings: Techniques, Applications, and Future Directions
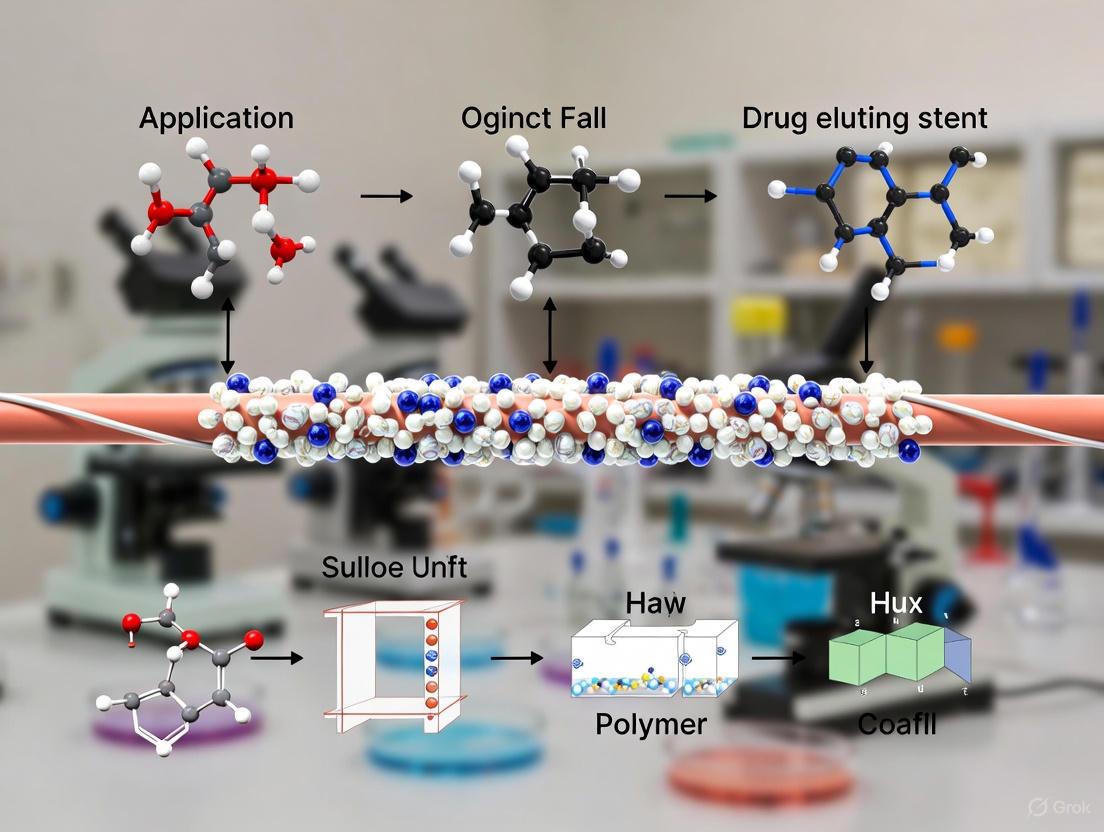
This comprehensive review explores the evolving landscape of drug-eluting stent (DES) coatings and application techniques, addressing critical needs for researchers and development professionals.
Advanced Drug-Eluting Stent Coatings: Techniques, Applications, and Future Directions
Abstract
This comprehensive review explores the evolving landscape of drug-eluting stent (DES) coatings and application techniques, addressing critical needs for researchers and development professionals. The article systematically examines foundational principles of DES technology, detailing coating materials, drug mechanisms, and stent platform requirements. It analyzes current methodological approaches including coating application techniques, polymer-based and polymer-free systems, and advanced drug delivery mechanisms. The content further addresses troubleshooting and optimization strategies for challenges like stent thrombosis and restenosis, incorporating computational modeling and material innovations. Finally, it validates approaches through clinical outcomes analysis and comparative assessment of different DES generations, providing a thorough evidence base for technology development and clinical application.
The Evolution of Drug-Eluting Stents: From Concept to Modern Coatings
The development of the first-generation drug-eluting stent (DES) marked a revolutionary advancement in interventional cardiology, fundamentally changing the treatment paradigm for coronary artery disease (CAD). Before its advent, percutaneous coronary intervention (PCI) was limited by the significant challenge of in-stent restenosis (ISR), a process of re-narrowing of the treated artery [1]. Bare-metal stents (BMS), introduced in the mid-1980s, represented an improvement over plain old balloon angioplasty (POBA) by effectively addressing acute vessel closure and elastic recoil [2] [1]. However, the metallic scaffold provoked a healing response characterized by neointimal hyperplasia—an excessive proliferation of smooth muscle cells—which led to ISR rates of 15-30% [1]. This pathological process created a critical need for innovative solutions that could inhibit this hyperproliferative response while maintaining vessel patency, thereby setting the stage for the groundbreaking development of first-generation DES.
The Evolution of Stent Technology: From BMS to First-Generation DES
The Bare-Metal Stent Era
Bare-metal stents were constructed from stainless steel and provided radial strength to mechanically scaffold coronary arteries open after angioplasty [1]. By preventing vessel recoil and negative remodeling, they represented a significant step forward from POBA. Nonetheless, their deployment caused injury to the vessel wall, triggering a cascade of inflammatory and proliferative responses that resulted in excessive tissue growth through the stent struts [1]. This neointimal hyperplasia necessitated repeat revascularization procedures in a substantial proportion of patients, with studies reporting restenosis rates of 15-35% [2]. This limitation highlighted the insufficiency of a purely mechanical approach and underscored the need for a biological solution to modulate the healing response.
The Conceptual Leap: Local Drug Delivery
The fundamental innovation behind the first-generation DES was the concept of localized anti-proliferative drug delivery to the vessel wall [1]. Researchers hypothesized that by coating stents with pharmaceutical agents that could inhibit smooth muscle cell proliferation, they could disrupt the pathway responsible for neointimal hyperplasia while minimizing systemic side effects. This required a sophisticated combination of three components: a metallic platform, an anti-proliferative drug, and a polymer coating to control drug release [1]. The polymer served as a drug reservoir, allowing for controlled elution kinetics that could provide therapeutic drug levels during the critical period of healing after stent implantation.
Table 1: Key Components of First-Generation Drug-Eluting Stents
| Component | Description | Examples in First-Generation DES |
|---|---|---|
| Metallic Platform | Base stent structure providing radial strength | Stainless steel (>100 μm strut thickness) [1] |
| Polymer Coating | Drug carrier vehicle controlling release kinetics | Non-degradable synthetic polymers (e.g., polyethylene-co-vinyl acetate, poly-n-butyl methacrylate) [1] |
| Anti-Proliferative Drug | Pharmaceutical agent inhibiting neointimal hyperplasia | Sirolimus, Paclitaxel [1] |
Mechanism of Action: Cytostatic vs. Cytotoxic Approaches
First-generation DES utilized two distinct classes of anti-proliferative agents with different mechanisms of action:
Sirolimus (and its analogues) functioned as cytostatic agents by inhibiting the mammalian target of rapamycin (mTOR), a key regulatory kinase in the cell cycle. This blockade prevented cell cycle progression from the G1 to S phase, thereby suppressing smooth muscle cell proliferation and migration without causing cell death [1].
Paclitaxel operated as a cytotoxic agent by stabilizing cellular microtubules, thereby disrupting normal microtubule dynamics during cell division. This mechanism caused M-phase arrest in the cell cycle, ultimately leading to cell death [2] [1].
The diagram below illustrates the signaling pathways and mechanisms of action for these two primary drugs used in first-generation DES:
Clinical Evidence and Outcomes
The introduction of first-generation DES demonstrated remarkable success in addressing the limitation of restenosis that plagued BMS. Clinical trials consistently showed that DES significantly reduced restenosis to less than 10%, a substantial improvement over the 15-30% rates observed with BMS [1]. This reduction in anatomical restenosis translated into meaningful clinical benefits, with a pronounced decrease in target lesion revascularization (TLR) procedures [1]. The ability to maintain vessel patency with fewer repeat interventions established DES as the new standard of care in percutaneous coronary intervention.
However, longer-term follow-up revealed an unanticipated concern: very late stent thrombosis (VLST), occurring more than one year after implantation [3]. This serious complication was attributed to delayed endothelialization and polymer-induced inflammation, as the permanent polymer coatings in first-generation DES sometimes provoked hypersensitivity reactions that impaired the normal healing process [1]. Histopathological studies indicated that these polymer coatings contributed to delayed vascular healing, which was associated with the increased risk of VLST [1].
Table 2: Comparative Clinical Outcomes of BMS vs. First-Generation DES
| Outcome Measure | Bare-Metal Stents (BMS) | First-Generation DES | Clinical Significance |
|---|---|---|---|
| In-Stent Restenosis | 15-30% [1] | <10% [1] | Dramatic reduction in re-narrowing |
| Target Lesion Revascularization | Higher rates [1] | Significantly reduced [1] | Fewer repeat procedures |
| Stent Thrombosis (Early) | Comparable | Comparable | Similar early safety profile |
| Very Late Stent Thrombosis | Lower incidence | Increased risk [1] | New safety concern with DES |
| Need for Dual Antiplatelet Therapy | Shorter duration | Prolonged duration required | Impact on bleeding risk |
A 14-year follow-up study provided intriguing long-term perspectives on this technological evolution. While DES demonstrated significantly lower major adverse cardiovascular and cerebrovascular events (MACCE) at 1-year follow-up compared to BMS (3 vs. 10 events, p=0.04), this benefit narrowed over time, with event rates becoming similar at 5, 10, and 14 years [4]. This long-term data suggests that while first-generation DES excelled at addressing the short- to medium-term challenge of restenosis, their advantage over BMS diminished in the very long term.
Experimental Protocols for DES Evaluation
In Vitro Drug Release Kinetics Profiling
Objective: To quantify and characterize the release kinetics of anti-proliferative drugs from stent coatings under simulated physiological conditions.
Methodology:
- Stent Preparation: Place individual DES units (n=6 per group) into separate vessels containing phosphate-buffered saline (PBS) with 0.5% Tween 20 at pH 7.4, maintained at 37°C [1].
- Sampling Protocol: Withdraw and replace release medium at predetermined time points (1, 4, 8, 24, 48, 72 hours, then weekly for 90 days).
- Drug Quantification: Analyze samples using high-performance liquid chromatography (HPLC) with UV detection to determine cumulative drug release.
- Kinetic Modeling: Fit release data to mathematical models (Higuchi, Korsmeyer-Peppas) to characterize release mechanisms.
Data Analysis: Calculate cumulative drug release profiles and determine burst release percentage (first 24 hours) versus sustained release phase.
Histomorphometric Analysis of Vessel Healing
Objective: To quantitatively assess neointimal suppression and vascular healing responses in pre-clinical models.
Methodology:
- Animal Implantation: Deploy test and control stents in appropriate animal models (porcine coronary model is standard).
- Tissue Harvest: Collect stented arterial segments at predetermined endpoints (28, 90, and 180 days).
- Processing and Sectioning: Fix vessels in formalin, embed in methylmethacrylate resin, and section using rotary microtome.
- Staining and Analysis: Perform hematoxylin and eosin (H&E) and elastic van Gieson (EVG) staining; analyze using digital morphometry.
Key Parameters:
- Neointimal Area: (Internal elastic lamina area - luminal area)
- Neointimal Thickness: Measured at each strut location
- Inflammation Score: 0-3 scale based on inflammatory cells around struts
- Endothelialization Score: Percentage of luminal surface covered by endothelium
The experimental workflow for evaluating stent performance integrates both in vitro and in vivo assessments, as visualized below:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for DES Coating and Application Research
| Reagent/Material | Function in DES Research | Application Notes |
|---|---|---|
| Sirolimus (Rapamycin) | mTOR inhibitor; cytostatic anti-proliferative [1] | Requires specific solvent systems for coating; sensitive to degradation |
| Paclitaxel | Microtubule stabilizer; cytotoxic anti-proliferative [2] [1] | Different mechanism than sirolimus; challenges with controlled release |
| Polymer Matrices (PEVA, PBMA) | Drug reservoir controlling release kinetics [1] | Early non-degradable polymers associated with late inflammation |
| Stainless Steel Platforms | Stent backbone providing radial strength [1] | Thicker struts (>100μm) compared to later generations |
| Chromatography Solvents (HPLC grade) | Drug quantification in release kinetics studies | Essential for accurate measurement of drug elution profiles |
| Cell Culture Media | Biocompatibility testing with endothelial/smooth muscle cells | Assess cytotoxicity and cellular responses to elution products |
| Histology Stains (H&E, EVG) | Tissue response evaluation in pre-clinical models | Critical for quantifying neointimal formation and inflammation |
| Thalidomide-O-C8-COOH | Thalidomide-O-C8-COOH, MF:C22H26N2O7, MW:430.5 g/mol | Chemical Reagent |
| Fmoc-Gly-Gly-Phe-OtBu | Fmoc-Gly-Gly-Phe-OtBu, MF:C32H35N3O6, MW:557.6 g/mol | Chemical Reagent |
The development of first-generation drug-eluting stents represented a paradigm shift in interventional cardiology, successfully addressing the formidable challenge of restenosis that had limited bare-metal stents. By combining mechanical scaffolding with controlled biological modulation through local drug delivery, first-generation DES achieved remarkable reductions in target lesion revascularization, establishing a new standard of care [1]. However, the emergence of very late stent thrombosis related to polymer biocompatibility issues highlighted the delicate balance between efficacy and safety in vascular implant technology [1].
These historical milestones and their limitations directly informed subsequent technological evolution, driving the development of second-generation DES with improved alloys, more biocompatible polymers, and alternative anti-proliferative agents [3] [1]. The first-generation DES story exemplifies how a transformative medical technology must continuously evolve based on long-term clinical evidence, balancing innovation with thoughtful consideration of unintended consequences to optimize patient outcomes in coronary artery disease management.
Drug-eluting stents (DES) represent a cornerstone technology in the treatment of coronary and peripheral artery disease, achieving their therapeutic effect through the sophisticated integration of three core components: a stent platform, one or more pharmacological agents, and a coating system that controls drug release [5] [6]. The careful selection and engineering of these components are critical for balancing the efficacy of preventing in-stent restenosis (ISR) with the safety profile of the implanted device [7]. The evolution from first-generation DES, which were plagued by issues of polymer-induced inflammation and late stent thrombosis, has led to advanced coating technologies including biodegradable polymers, polymer-free designs, and novel drug delivery mechanisms [3] [5]. This document provides a detailed technical overview of these key coating components and outlines standardized experimental protocols for their evaluation, serving as a practical resource for researchers and development professionals in the field.
Key Coating Components: Composition and Function
The performance of a DES is governed by the interplay between its metallic platform, the antiproliferative drug, and the polymer matrix that controls drug release. The following sections and tables detail the characteristics and options for each component.
Stent Platforms
The stent platform provides the mechanical scaffold to maintain vessel patency. The base material and structural design directly influence deliverability, radial strength, and long-term safety.
Table 1: Key Stent Platform Materials and Properties
| Material | Key Properties | Advantages | Limitations/Considerations |
|---|---|---|---|
| Cobalt-Chromium (CoCr) [3] | High radial strength, good radio-opacity | Allows for thinner strut designs (<70 µm), improved deliverability [3] | Permanent metallic implant |
| Platinum-Chromium (PtCr) [3] | Enhanced radial strength, high radio-opacity | Superior visibility under fluoroscopy | Permanent metallic implant |
| Nitinol (Nickel-Titanium) [6] | Superelasticity, shape-memory, excellent flexibility | Ideal for peripheral arteries with movement (e.g., femoropopliteal) [6] | Potential nickel toxicity concerns; requires stable oxide layer for biocompatibility [6] |
| Magnesium Alloys [3] [5] | Biocorrodible, degradable | Potential for complete resorption, restoring vasomotion [3] | Radial strength and degradation kinetics must be carefully controlled [5] |
Pharmacological Agents
The drugs eluted from DES are primarily cytostatic agents that inhibit smooth muscle cell (SMC) proliferation to prevent neointimal hyperplasia and ISR.
Table 2: Common Drugs Used in Drug-Eluting Stents
| Drug | Drug Class | Mechanism of Action | Release Kinetics & Notes |
|---|---|---|---|
| Sirolimus (and analogues like Everolimus, Zotarolimus) [3] [6] | Limus family (mTOR inhibitors) | Arrests the cell cycle in the G1 phase for both SMCs and endothelial cells [6] | Hydrophobic; requires polymer for sustained release. Efficacy depends on precise release kinetics [8]. |
| Paclitaxel [6] | Taxane | Stabilizes microtubules, inhibiting cell migration and division and inducing apoptosis [6] | Highly lipophilic; can be used on polymer-free platforms or with polymers. |
| 5-Fluorouracil (5FU) [9] | Antimetabolite | Inhibits thymidylate synthase, disrupting DNA and RNA synthesis. | Primarily investigated for drug-eluting stents in gastrointestinal cancers [9]. |
Polymer Coating Systems
Polymer coatings serve as a drug reservoir and control the release kinetics of the active agent. The trend is moving towards more biocompatible and biodegradable options to mitigate long-term risks.
Table 3: Types of Polymer Coatings for DES
| Polymer Type | Examples | Key Characteristics | Clinical Context |
|---|---|---|---|
| Durable (Permanent) Polymer | PBMA, PVDF-HFP, SIBS [5] [8] | Remains on stent permanently after drug elution. | Earlier generations linked to chronic inflammation and late stent thrombosis [8]. Newer, more biocompatible versions (e.g., fluoropolymers) are widely used [5]. |
| Biodegradable (Bioresorbable) Polymer | PLGA, PCL, Poly(l-lactic acid) (PLLA) [3] [5] | Degrades over time (months), releasing drug and then disappearing. | Eliminates long-term polymer presence, potentially improving safety. Degradation rate must match drug release profile [3] [10]. |
| Polymer-Free | Microporous stents, nanoporous surfaces, reservoir-coated stents [3] [10] | Eliminates polymer entirely, using stent surface to hold and release drug. | Aims to avoid polymer-related adverse events entirely. Performance can be comparable to BP-DES in some studies [10]. |
| Advanced & Specialized Polymers | Biomimetic polymers, Gradient-release polymers, Polyurethane-silicone (PUS) elastomers [3] [9] | Designed to mimic ECM, provide variable drug release, or offer tailored elution profiles. | Represent next-generation innovations to further optimize healing and efficacy, including for non-vascular applications [3] [9]. |
Experimental Protocols for Coating Development and Evaluation
This section provides detailed methodologies for key experiments in the development and characterization of DES coatings.
Protocol: In Vitro Drug Release Kinetics
Objective: To quantify the rate and profile of drug release from a coated stent under simulated physiological conditions [6].
Workflow Overview:
Materials:
- Coated Stent Sample: Test DES unit.
- Dissolution Apparatus: USP Apparatus 4 (flow-through cell) or 7 (reciprocating holder) are recommended for stents [6].
- Dissolution Medium: Phosphate-buffered saline (PBS, pH 7.4) or a suitable medium that maintains sink conditions.
- Analytical Instrument: High-Performance Liquid Chromatography (HPLC) system with UV-Vis or MS detector.
- Supporting Equipment: Heated water bath or jacket (37°C), sampling syringes with filters, volumetric flasks.
Procedure:
- Setup: Fill the dissolution vessel with a precise volume of pre-warmed (37°C) medium. Assemble the apparatus according to the manufacturer's instructions.
- Stent Immersion: Place the coated stent into the vessel, ensuring it is fully immersed and freely moving, or fixed in a holder as per the apparatus design.
- Agitation: Start the agitation system (e.g., rotating paddle at 50-75 rpm) to ensure uniform hydrodynamics. Maintain temperature at 37°C throughout.
- Sampling: At predetermined time points (e.g., 1 h, 6 h, 24 h, 3 d, 7 d, 14 d, 30 d), withdraw a known aliquot (e.g., 1-2 mL) of the release medium. Replace with an equal volume of fresh, pre-warmed medium to maintain constant volume and sink conditions. Filter the sample through a 0.45 µm membrane filter.
- Analysis: Analyze the drug concentration in each sample using a validated HPLC-UV method. Calculate the cumulative amount of drug released at each time point.
- Data Processing: Plot the cumulative drug released (%) versus time to generate the release profile. Model the data using relevant kinetic models (e.g., Higuchi, Korsmeyer-Peppas) to understand the release mechanism.
Protocol: Coating Integrity and Morphology Analysis
Objective: To visually and quantitatively assess the surface morphology, uniformity, thickness, and potential defects of the coating before and after simulated use (e.g., expansion).
Materials:
- Microscopy: Scanning Electron Microscope (SEM).
- Sample Preparation: Sputter coater for applying a thin conductive layer (e.g., gold) for SEM.
- Stent Samples: Un-expanded coated stent, and stent expanded in a mock artery (e.g., silicone tube) to nominal pressure.
Procedure:
- Sample Preparation: Carefully cut a representative section (e.g., 2-3 struts) from both the un-expanded and expanded stent.
- Mounting: Mount the stent segments on an SEM stub using conductive carbon tape to ensure electrical contact.
- Sputter Coating: Place the mounted samples in a sputter coater and apply a thin (5-10 nm) layer of gold/palladium to make the surface conductive.
- SEM Imaging: Transfer samples to the SEM chamber. Image the coating surface at various magnifications (e.g., 50x to 10,000x) to examine uniformity, texture, and the presence of cracks, webbing, or delamination. Obtain cross-sectional images to measure coating thickness.
- Image Analysis: Use image analysis software to measure coating thickness at multiple points and document any defects. Compare pre- and post-expansion images to assess durability.
Protocol: Biocompatibility and Hemocompatibility Assessment
Objective: To evaluate the potential for polymer coatings to induce thrombosis (blood clotting) and inflammatory responses.
Workflow Overview:
Materials:
- Test Samples: Coated stent segments or polymer-coated surfaces. Sterilize samples prior to testing.
- Biological Reagents: Fresh human platelet-rich plasma (PRP), whole blood, endothelial cell line (e.g., HUVEC), smooth muscle cell line (VSMC).
- Assay Kits: Lactate Dehydrogenase (LDH) assay kit, MTT/XTT cell viability kit, ELISA kits for inflammatory markers (e.g., TNF-α, IL-6).
Procedure (Key Assays):
- Platelet Adhesion Test: Incubate coated samples with PRP for a set time (e.g., 60 min). Gently rinse to remove non-adherent platelets. Fix and dehydrate the samples. Quantify adhesion via SEM imaging or using an LDH assay to measure platelet number.
- Hemolysis Assay: Incubate coated samples with diluted whole blood. After incubation, centrifuge and measure the hemoglobin released in the supernatant spectrophotometrically. Calculate the hemolysis ratio against controls.
- Cell Viability (Cytotoxicity): Prepare an extract of the coating by incubating it in cell culture medium. Culture relevant cells (HUVECs, VSMCs) and expose them to the extract. After 24-72 hours, measure cell viability using an MTT assay, which measures mitochondrial activity.
- In Vivo Evaluation (Animal Model): Implant the test DES and a control DES (e.g., a commercially approved device) in the coronary arteries of a porcine model. After a pre-determined period (e.g., 28-90 days), perform histopathological analysis of the stented segments to score endothelialization, inflammation, and fibrin deposition [6].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for DES Coating Research
| Category / Item | Specific Examples | Primary Function in R&D |
|---|---|---|
| Polymer Coating Materials | Poly(lactic-co-glycolic acid) (PLGA), Poly(n-butyl methacrylate) (PBMA), Poly(vinylidene fluoride-co-hexafluoropropylene) (PVDF-HFP) [5] [8] | Form the drug reservoir and control release kinetics; basis for biocompatibility testing. |
| Active Pharmaceutical Ingredients (APIs) | Sirolimus, Everolimus, Zotarolimus, Paclitaxel [3] [6] | The therapeutic agent to be eluted; used for developing and validating drug loading and release methods. |
| Analytical Standards | USP Sirolimus RS, USP Paclitaxel RS | Certified reference standards for accurate quantification of drug content and release in analytical methods (HPLC). |
| Cell Lines for Cytocompatibility | Human Umbilical Vein Endothelial Cells (HUVECs), Vascular Smooth Muscle Cells (VSMCs) [6] | In vitro models to assess coating cytotoxicity and its specific effects on vascular cell types. |
| Animal Models for In Vivo Testing | Porcine (swine) coronary model [6] | The standard pre-clinical model for evaluating stent safety, efficacy, and vascular healing responses. |
| Characterization Equipment | Scanning Electron Microscope (SEM), High-Performance Liquid Chromatography (HPLC) system | Essential for analyzing coating morphology, integrity, and drug quantification. |
| (S,R,S)-AHPC-C10-NH2 dihydrochloride | (S,R,S)-AHPC-C10-NH2 dihydrochloride, MF:C33H53Cl2N5O4S, MW:686.8 g/mol | Chemical Reagent |
| Isamoltane hemifumarate | Isamoltane hemifumarate, CAS:55050-95-8; 874882-92-5, MF:C36H48N4O8, MW:664.8 | Chemical Reagent |
Anti-Proliferative Agents and Their Pharmacokinetics
Anti-proliferative agents are pharmaceuticals designed to inhibit abnormal cellular proliferation, a process central to pathologies such as in-stent restenosis (ISR) following percutaneous coronary intervention (PCI) and cancer. In drug-eluting stents (DES) and drug-coated balloons (DCB), these agents are delivered locally to the vessel wall to suppress neointimal hyperplasia, which is the excessive growth of smooth muscle cells that leads to re-narrowing of the artery [2] [11]. The efficacy of these devices depends on a complex interplay between the pharmacological properties of the active drug, the vehicle or polymer used for delivery, the release kinetics, and the specific biological environment. This document details the primary anti-proliferative agents used in vascular devices, their pharmacokinetics, and associated experimental protocols, providing a framework for researchers developing next-generation coatings and application techniques.
Anti-Proliferative Drug Classes and Mechanisms of Action
The two dominant classes of anti-proliferative drugs used in vascular devices are the taxanes (e.g., paclitaxel) and the limus family (sirolimus and its analogs, such as everolimus and zotarolimus). Their mechanisms of action, while both anti-proliferative, target distinct cellular pathways as shown in the diagram below and summarized in the subsequent table.
Table 1: Comparison of Key Anti-Proliferative Agents in Vascular Devices
| Drug (Class) | Molecular Target | Cell Cycle Arrest | Primary Effect | Key Pharmacokinetic Challenge |
|---|---|---|---|---|
| Paclitaxel (Taxane) [2] [6] | β-tubulin | M-phase | Stabilizes microtubules, inhibiting cell division and migration | Highly lipophilic; requires excipients (e.g., shellac, BTHC) for arterial retention and transfer [2] |
| Sirolimus/Everolimus (Limus) [2] [12] | mTORC1 (via FKBP12) | G1-phase | Inhibits cell cycle progression and reduces inflammation | Poorer arterial wall penetration and shorter duration of action compared to paclitaxel [2] |
Pharmacokinetics and Drug Delivery from Stents and Balloons
The pharmacokinetic profile—encompassing drug release, tissue absorption, distribution, and retention—is a critical determinant of the safety and efficacy of DES and DCB.
Drug-Eluting Stents (DES)
DES technology has evolved through generations to optimize pharmacokinetics and biocompatibility. First-generation DES used durable polymers to elute drugs, which were associated with chronic inflammation and very late stent thrombosis due to the persistent presence of the polymer after drug elution [13] [14]. Second-generation DES featured more biocompatible durable polymers and improved stent platforms [14]. The current third-generation focuses on biodegradable polymers and polymer-free approaches, where the polymer carrier degrades and is resorbed after completing its drug-delivery function, thereby eliminating a nidus for long-term inflammation [13]. A novel advancement is the use of a crystalline drug form applied directly to the stent surface, which aims to provide a more controlled and sustained elution profile, reducing the initial "drug dumping" and local toxicity associated with polymer-based systems [14].
Drug-Coated Balloons (DCB)
DCBs offer a "leave nothing behind" alternative, delivering anti-proliferative drugs via a balloon catheter during brief inflation (typically 30-60 seconds). The key to their success is the rapid and effective transfer of the drug to the arterial wall. This is facilitated by hydrophilic matrix excipients (e.g., iopromide, urea) that enhance drug solubility and adherence to the vascular wall [2]. Paclitaxel is the predominant agent used in DCBs due to its high lipophilicity and rapid cellular uptake, which enable durable tissue effects from a single, short exposure [2]. While sirolimus-coated balloons face challenges due to the drug's poorer penetration and shorter tissue residence time, newer formulations using nanocarrier technology (e.g., MagicTouch SCB) are being developed to overcome these limitations [2].
Experimental Protocols for Coating Characterization and Performance
Robust and standardized experimental protocols are essential for the development and regulatory approval of novel DES and DCB coatings.
In Vitro Drug Release Kinetics
This protocol characterizes the drug release profile from a coated device under simulated physiological conditions.
- Objective: To quantify the rate and extent of drug release from a DES or DCB over time.
- Materials:
- Coated stent or balloon sample
- Phosphate-buffered saline (PBS) with 0.05% w/v Tween 80 (or another suitable surfactant) as the release medium, maintained at 37±0.5°C [6]
- USP Apparatus 4 (flow-through cell) or Apparatus 7 (sample immersion) may be used
- High-Performance Liquid Chromatography (HPLC) system with a validated method for drug quantification
- Method:
- Immerse the device in a known volume of release medium under continuous, gentle agitation.
- At predetermined time points (e.g., 1 hr, 6 hr, 1, 3, 7, 14, 21, 28 days), withdraw and replace the entire release medium to maintain sink conditions.
- Analyze the collected samples using HPLC to determine the cumulative amount of drug released.
- Plot the cumulative drug release (%) versus time to generate the release profile.
- Data Analysis: Model the release data using kinetic models (e.g., zero-order, first-order, Higuchi) to understand the release mechanism. Accelerated release conditions (e.g., elevated temperature) may be developed and validated to predict long-term release profiles for quality control purposes [6].
Coating Uniformity and Surface Characterization
This protocol ensures the quality and consistency of the drug-polymer coating.
- Objective: To assess the thickness, uniformity, and surface morphology of the coating on the stent struts or balloon surface.
- Materials:
- Coated stent or balloon
- Scanning Electron Microscope (SEM)
- Atomic Force Microscope (AFM)
- Optical Profilometer
- Method:
- SEM Imaging: Sparrow et al. (2022) describe sputter-coating the sample with a thin layer of gold/palladium to prevent charging. Image multiple struts or balloon sections at various magnifications (e.g., 50X to 10,000X) to visualize coating cracks, webbing, or delamination [6].
- Surface Roughness (AFM): Scan a defined area (e.g., 10 µm x 10 µm) on the coating surface using AFM in tapping mode. Calculate the average surface roughness (Ra) and root mean square roughness (Rq).
- Coating Thickness (Optical Profilometry): Use a profilometer to scan across the edge of a coated region. Measure the step height between the coated and uncoated substrate at multiple locations (n≥9) to determine average thickness and uniformity.
- Acceptance Criteria: Coating should be continuous, without significant cracking or delamination. Thickness measurements should fall within a specified range with low variability (e.g., ±10%).
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Materials for Anti-Proliferative Coating Research
| Item | Function/Application | Examples |
|---|---|---|
| Active Pharmaceutical Ingredient (API) | The anti-proliferative agent that inhibits neointimal hyperplasia. | Paclitaxel, Sirolimus (and analogs: Everolimus, Zotarolimus) [2] [11] |
| Polymer Carrier | Controls the release rate of the API from the device. Can be durable or biodegradable. | Poly(lactic-co-glycolic acid) (PLGA), Poly(n-butyl methacrylate) (PBMA), Polysulfone [13] [6] |
| Excipient (for DCBs) | Hydrophilic matrix that facilitates drug transfer from the balloon to the arterial wall. | Iopromide, Shellac, Acetyl tributyl citrate (ATBC), Urea [2] |
| Sterilization Agent | Ensures device sterility without compromising coating integrity or drug activity. | Ethylene Oxide (EtO) [6] |
| Tubulin Polymerization Assay Kit | In vitro tool to verify the mechanistic activity of paclitaxel or similar agents. | Commercial kits measuring microtubule formation kinetics. |
| Cell-Based Proliferation Assay | To test the biological efficacy of eluted drugs. | SRB assay, MTT assay using human vascular smooth muscle cells (SMCs) [15] |
| 3-GlcA-28-AraRhaxyl-medicagenate | 3-GlcA-28-AraRhaxyl-medicagenate, CAS:128192-15-4, MF:C52H80O24, MW:1089.2 g/mol | Chemical Reagent |
| N-Boc-piperazine-C3-COOH | N-Boc-piperazine-C3-COOH, CAS:959053-53-3, MF:C14H24N2O5, MW:300.355 | Chemical Reagent |
The effective application of anti-proliferative agents in DES and DCB is a cornerstone of modern interventional cardiology. The continuous refinement of these technologies—through the development of novel drugs, advanced polymer systems, and polymer-free approaches—aims to optimize pharmacokinetics for maximal therapeutic benefit and long-term safety. The experimental protocols and research tools outlined herein provide a foundational framework for scientists and engineers engaged in the critical work of developing the next generation of vascular devices. A deep understanding of drug mechanisms and pharmacokinetics, coupled with rigorous characterization methodologies, is essential for driving innovation in this field.
In the development of drug-eluting stents (DES), the interplay between structural design parameters and coating application techniques is critical for achieving optimal clinical performance. Stents must provide adequate mechanical support to maintain vessel patency while facilitating controlled drug delivery to prevent restenosis. The core mechanical properties—strut thickness, flexibility, and radial strength—are deeply interconnected and significantly influence the stent's interaction with the vascular environment, the effectiveness of the drug-eluting coating, and long-term patient outcomes [16] [17]. This document outlines key design parameters, experimental characterization methods, and their implications for DES coating and application research.
Core Stent Design Parameters and Quantitative Data
Strut Thickness
Strut thickness is a primary determinant of stent performance, influencing both biological responses and deliverability. The trend in new-generation DES is toward thinner struts to improve hemodynamics and reduce thrombogenic risk [17].
Table 1: Impact of Strut Thickness on Stent Performance
| Strut Thickness (μm) | Stent Type/Platform | Key Performance Findings | Reference |
|---|---|---|---|
| 60-64 | Orsiro SES (≤3 mm dia.), MiStent SES | Lower thrombogenicity; faster endothelialization; reduced restenosis | [17] |
| 74-81 | Synergy EES (Pt-Cr) | Improved flexibility, trackability, and reduced side branch occlusion risk | [17] |
| 80 | Ultimaster SES (Co-Cr) | Open-cell design with biodegradable polymer on abluminal side | [17] |
| 132-140 | Early-generation DES (Cypher, Taxus) | 1.5-fold more thrombogenic than 81 μm struts in preclinical models | [17] |
| 150 | Novel L-PBF 316L Stainless Steel Stent | Target wall thickness for metallic stents balancing strength and hemodynamics | [18] |
Preclinical evidence demonstrates that thicker struts (132-140 µm) are approximately 1.5-fold more thrombogenic than thinner struts (81 µm) in ex vivo flow loops [17]. Furthermore, in a porcine model, thick-strut stents accumulated more thrombus and fibrin deposition at three days post-implantation. A pivotal clinical trial (ISAR-STEREO) showed that using thin-strut (50 µm) bare-metal stents instead of thick-strut (140 µm) counterparts significantly reduced binary restenosis at six months (15% vs. 25.8%) and target vessel revascularization (8.6% vs. 13.8%) [17].
Flexibility and Radial Strength
Flexibility is crucial for deliverability through tortuous anatomy, while radial strength is essential for resisting vascular recoil and maintaining vessel patency. These parameters are significantly influenced by stent design, including the configuration of connectors (links) and support rings.
Table 2: Stent Mechanical Performance Characteristics
| Stent Design / Parameter | Radial Strength | Flexibility / Axial Shortening | Reference |
|---|---|---|---|
| Novel Variable-Thickness (VT) Polymer Stent | 10% improvement vs. constant-thickness (CT) stent | Not quantified, but design aims to enhance flexibility | [19] |
| L-PBF 316L M-Type Stent (Metal) | 840 mN/mm | Axial shortening rate of 5.56% | [18] |
| L-PBF 316L M-Type Stent (Metal) | Radial recoil rate of 1.37% | --- | [18] |
| Connector (Bridge) Design | Secondary influence on radial strength | Primary determinant of stent flexibility | [19] |
| Support Ring Architecture & Strut Configuration | Primary determinant of radial strength | Governs axial shortening and flexibility | [18] |
Finite Element Analysis (FEA) and experimental studies show that connecting elements (bridges) have the most significant effect on stent flexibility [19]. Meanwhile, the radial-support rings are the primary load-bearing elements governing radial strength [18]. Innovative designs, such as the double-period unequal-height support rings interconnected by M-shaped struts, aim to optimize the distribution of radial force and control axial shortening during expansion [18].
Experimental Protocols for Mechanical Characterization
Protocol for Radial Strength and Stiffness Testing
Radial force testing is a critical assessment for stent design validation and regulatory submission, measuring a stent's ability to withstand external compressive forces.
- Objective: To measure the radial stiffness, chronic outward force (for self-expanding stents), and radial resistive force of a vascular stent as a function of diameter.
- Equipment: RX550/650 radial force tester (Machine Solutions Inc.) or equivalent system with a segmented head (e.g., 12 segments) for uniform compression. The system must be capable of precise control and recording of diameter and force [20].
- Environmental Control: Set the test temperature to 37°C using the chamber's temperature control system to simulate physiological conditions [20].
- Sample Preparation: Randomly select test samples. Measure and record the free (unconstrained) outer diameter and length of each stent sample using a micrometric gauging machine before and after testing [20].
- Test Profiles (Select as appropriate) [20] [21]:
- Compression Only: For balloon-expandable and self-expanding stents. The head compresses the stent from its initial diameter to a smaller target diameter at a defined speed.
- Expansion Only: Primarily for self-expanding stents. The stent is deployed or compressed to a small diameter, then the head diameter is gradually increased at a set speed to the final target diameter.
- Compression/Expansion Cycles: Multiple cycles are performed to assess the hysteresis behavior of self-expanding stents.
- Customized Profiles: Diameter variation according to a user-defined profile (e.g., specific time-diameter file).
- Data Acquisition: Record the radial force versus diameter throughout the loading and/or unloading profile [20].
- Data Analysis: Report the radial force versus diameter curve. The radial strength is often reported as the maximum compressive force per unit length (e.g., in mN/mm) sustained by the stent. For comparative analysis, the force value may be normalized by the measured stent length [20] [18].
- Regulatory Compliance: This test method supports submissions per FDA guidance and international standards such as ASTM F3067 (Guide for Radial Loading of Vascular Stents) and ISO 25539-2 (Cardiovascular implants — Endovascular devices — Part 2: Vascular stents) [20] [21] [22].
Protocol for Three-Point Bending Flexibility Test
The three-point bending test assesses stent flexibility, which correlates to its deliverability through curved vasculature.
- Objective: To quantify the bending stiffness of a stent by measuring the force-deflection relationship during bending.
- Equipment: A universal testing machine equipped with a three-point bending fixture. The fixture has two fixed lower supports and one movable upper loading pin.
- Sample Preparation: The stent sample is placed across the two lower supports.
- Test Procedure: The upper loading pin is displaced downward at a constant rate, applying a force at the mid-span of the stent until a target deflection is reached. The force and deflection are recorded simultaneously [19].
- Data Analysis: The force-deflection curve is plotted. The slope of the linear (elastic) portion of this curve is used to calculate the bending stiffness. A validated Finite Element Model (FEM) can be correlated with experimental data to analyze strain distribution, particularly in the plastic deformation range [19].
- Application in Design: This method is used to evaluate how different connector designs impact overall stent flexibility. Research has shown that optimizing design can reduce bending forces and improve conformability to vessel walls [19].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Stent Design and Coating Research
| Material / Solution | Function in Research | Relevance to DES Development | |
|---|---|---|---|
| Poly(L-lactic acid) (PLLA) Resin | Base material for fabricating polymeric stent scaffolds via 3D printing (e.g., LCD). | Biodegradable polymer used in stents (e.g., Orsiro SES) and as a drug-carrying matrix. | [19] [17] |
| Cobalt-Chromium (Co-Cr) & Platinum-Chromium (Pt-Cr) Alloys | High-strength metal platforms for stent scaffolding. | Enable thinner strut designs without sacrificing radial strength; common in new-generation DES. | [17] [23] |
| 316L Stainless Steel Powder | Feedstock for Laser Powder Bed Fusion (L-PBF) additive manufacturing of stents. | Allows monolithic fabrication of complex, patient-specific stent designs. | [18] |
| Poly(DL-lactic acid)/Polycaprolactone (PLGA-PCL) Blend | Biodegradable polymer coating for controlled drug release. | Used as an abluminal coating on stents (e.g., Ultimaster SES) to elute anti-proliferative drugs. | [17] |
| Sirolimus, Everolimus, Paclitaxel | Pharmaceutical agents (anti-proliferative) loaded into polymer coatings. | Inhibits smooth muscle cell proliferation to prevent in-stent restenosis; core of DES function. | [16] [17] [23] |
| Electropolishing Solutions | Electrolytic solutions for post-fabrication surface finishing. | Critical for reducing surface roughness of metal stents (e.g., L-PBF printed), improving biocompatibility and potentially coating uniformity. | [18] |
| Glycodeoxycholic acid monohydrate | Glycodeoxycholic acid monohydrate, MF:C26H45NO6, MW:467.6 g/mol | Chemical Reagent | |
| THP-PEG4-Pyrrolidine(N-Me)-CH2OH | THP-PEG4-Pyrrolidine(N-Me)-CH2OH, MF:C19H37NO7, MW:391.5 g/mol | Chemical Reagent |
Implications for Drug-Eluting Stent Coating and Application
The structural design parameters directly impact the constraints and opportunities for drug coating application. Thinner struts present a smaller surface area for drug deposition, requiring highly uniform and efficient coating techniques like ultrasonic spraying or dip-coating to ensure consistent drug dosage [17] [23]. The choice of polymer is critical; while durable polymers provide a stable platform, they can provoke inflammatory responses. Conversely, biodegradable polymers (e.g., PLLA, PLGA) degrade after fulfilling their drug-release function, potentially improving long-term safety by leaving behind a bare metal stent [17]. Advanced coating strategies, such as the asymmetric or gradient coating on the abluminal side only, maximize drug delivery to the vessel wall while minimizing drug loss to the bloodstream [17] [23]. Furthermore, the mechanical integrity of the coating must withstand stent crimping and expansion without cracking or delaminating, a challenge that is exacerbated in more flexible stent designs with complex deformations [19] [17].
The efficacy of drug-eluting stents (DES) is fundamentally governed by the complex, multi-layered structure of the arterial wall, which acts as the primary environment for drug transport following deployment. Cardiovascular diseases, particularly atherosclerosis, remain a leading cause of death globally, and DES have revolutionized treatment by drastically reducing the rate of in-stent restenosis (ISR) compared to bare-metal stents [7] [3]. The primary challenge in DES design lies in achieving sufficient drug delivery to the target tissues to inhibit restenosis while minimizing safety risks, a balance heavily influenced by the dynamic drug transport processes within the arterial wall [7] [24]. This Application Note details the structural components of the arterial wall, the computational and experimental methodologies used to model drug transport within it, and the key parameters that determine the safety and efficacy of drug delivery from DES.
Structural Environment of Drug Transport
The arterial wall is not a homogeneous medium but a structured, multi-layered tissue. Each layer presents a unique set of physical and biological barriers that dictate drug kinetics.
- The Endothelium and Subendothelial Intima (SES): The endothelium forms the innermost lining of the artery. During stent implantation, this layer is typically denuded, removing a significant physical barrier. The underlying subendothelial intima is a porous layer that, in atherosclerotic arteries, can contain migrated smooth muscle cells (SMCs) that become binding sites for anti-proliferative drugs [24].
- The Internal Elastic Lamina (IEL): This membrane, rich in elastin, separates the intima from the media. It acts as a selective barrier, with its fenestrations influencing the rate and distribution of drug molecules passing into the media [24].
- The Media: The medial layer is the primary target for DES-delivered drugs, as it contains the SMCs whose proliferation leads to restenosis. This layer is modeled as a porous medium where drug transport occurs via diffusion and convection, with the added complexity of reversible binding to cellular components [25] [24].
- The Adventitia: The outermost layer, consisting of connective tissue, is often modeled as a boundary condition that can act as a "sink" for drugs, influencing the overall concentration profile within the arterial wall [24].
Quantitative Framework for Drug Transport Modeling
Computational models integrate the physics of drug release from the stent coating with drug transport and binding in the arterial wall. The tables below summarize key parameters and governing equations from established models.
Table 1: Key Parameters in DES Drug Transport Models [25] [24]
| Parameter | Symbol | Typical Values / Range | Description |
|---|---|---|---|
| Strut Dimension | a |
100 - 140 µm | Size of the stent strut. |
| Coating Thickness | δ |
5 - 50 µm | Thickness of the drug-polymer coating. |
| Arterial Wall Thickness | Lx |
~200 µm | Thickness of the arterial wall layer. |
| Coating Drug Diffusivity | D1 |
0.01 - 1 µm²/s | Diffusivity of the drug within the polymer coating. |
| Vascular Drug Diffusivity | D2 |
0.1 - 10 µm²/s | Diffusivity of the drug within the arterial wall tissue. |
| Initial Drug Concentration | C0 |
~10â»âµ M | Initial drug load in the stent coating. |
| Association Rate Constant | ka |
10â´ Mâ»Â¹sâ»Â¹ | Rate constant for drug binding to tissue. |
| Dissociation Rate Constant | kd |
0.01 sâ»Â¹ | Rate constant for drug unbinding from tissue. |
| Binding Site Concentration | S0 |
~10â»âµ M | Concentration of available drug binding sites. |
Table 2: Governing Equations for Drug Transport in a Multi-Layered Artery [25] [24]
| Domain | Primary Transport Mechanism | Governing Equation / Principle |
|---|---|---|
| Stent Coating | Diffusion | Fickian diffusion: ∂c/∂t = ∇ · (D₠∇c) |
| Arterial Lumen | Convection & Diffusion | Navier-Stokes equations (flow) + Advection-Diffusion equation (drug transport). |
| Subendothelial Intima (SES) | Convection, Diffusion & Reaction | ∂c_se/∂t + u · ∇c_se = D_se ∇²c_se - k_a c_se (b_max,se - b) + k_d b |
| Media | Convection, Diffusion & Reaction | ∂c_m/∂t + u · ∇c_m = D_m ∇²c_m - k_a c_m (b_max - b) + k_d b∂b/∂t = k_a c_m (b_max - b) - k_d b (Binding kinetics) |
The following diagram illustrates the integrated process of drug release from a stent strut and its subsequent transport through the multi-layered arterial wall, incorporating the key mechanisms described in the tables above.
Experimental Protocols for Model Validation
Protocol: Computational Simulation of Arterial Drug Distribution
This protocol outlines the steps for using a finite volume method to simulate drug distribution from a single stent strut in a coronary artery cross-section, based on established computational studies [25].
I. Model Geometry Definition
- Create a 2D geometric model representing a rectangular section of the arterial wall adjacent to a single stent strut.
- Define the strut dimensions (e.g., 140 µm), coating thickness (e.g., 5-50 µm), and depth of strut embedment into the arterial wall (
Lp). - Set the overall arterial wall thickness (
Lxto ~200 µm) and the inter-strut distance (Ly, e.g., 1000 µm for an 8-strut stent in a 3-mm artery) [25].
II. Parameter Initialization
- Input the physicochemical parameters for the drug and arterial environment as listed in Table 1. This includes:
- Initial drug concentration in the coating (
Câ‚€). - Drug diffusivities in the coating (
Dâ‚) and arterial wall (Dâ‚‚). Note that the vascular diffusivity can be isotropic or anisotropic (e.g., higher circumferential diffusivityDâ‚‚ythan transmural diffusivityDâ‚‚x) [25]. - Binding kinetic parameters (
kâ‚,k_d,Sâ‚€).
- Initial drug concentration in the coating (
III. Numerical Solution
- Discretize the computational domain using a mesh with sufficient resolution near the strut to capture high concentration gradients.
- Apply boundary conditions: a symmetry condition at the tissue boundaries between struts, a perfect sink condition at the adventitial boundary, and a no-flux condition at the luminal boundary in the denuded area.
- Solve the coupled system of partial differential equations (from Table 2) for drug diffusion in the coating and drug convection-diffusion-reaction in the arterial wall using a finite volume solver until a steady-state or time-dependent solution is achieved.
IV. Data Analysis
- Extract spatiotemporal data for free and bound drug concentrations throughout the arterial wall domain.
- Calculate metrics such as the spatial-average drug level in the media and the drug content (DC) parameter, which is linked to safety [7].
- Visualize the results as contour plots of drug distribution at specific time points (e.g., 1, 7, 30 days) to identify regions of potential therapeutic efficacy or toxicity.
Protocol: Evaluating Safety and Efficacy via a Multiscale Framework
This protocol describes a more advanced framework that couples continuum-based drug transport with an agent-based model (ABM) of vascular remodeling to comprehensively assess DES performance [7].
I. Framework Setup
- Establish a multiscale computational framework with two core modules:
- A Continuum-based Drug Transport Model: Simulates drug release from the DES and its subsequent transport in the arterial wall, as described in Section 4.1.
- An Agent-Based Model (ABM) of Vascular Remodeling: Models the behavior of individual Vascular Smooth Muscle Cell (VSMC) agents in response to drug concentrations and inflammatory signals.
II. Model Coupling and Input
- Link the models so that the local free drug concentration calculated by the continuum model serves as an input to the ABM, influencing VSMC agent behaviors like proliferation and apoptosis.
- Define the inflammatory input to the ABM to be non-uniform, reflecting that VSMC agents closer to the stent strut experience stronger inflammation [7].
- Incorporate the effect of VSMC agent age on mitosis into the ABM to improve biological fidelity [7].
III. Simulation Execution
- Run coupled simulations for a defined period (e.g., 50 days post-implantation).
- Compare simulations of a novel DES design (e.g., a dual-layer coating DES) against a conventional DES.
IV. Performance Quantification
- Quantify Efficacy: Measure the degree of inhibition of neointimal hyperplasia (tissue re-growth) in the ABM.
- Quantify Safety: Calculate the drug content (DC) parameter from the continuum model, where a lower DC indicates greater safety [7].
- An optimal DES design demonstrates a significant advantage in safety (lower DC) with only a slight reduction in efficacy.
The Scientist's Toolkit: Research Reagent Solutions
The table below catalogs essential materials and computational tools used in the development and analysis of drug transport environments for DES.
Table 3: Essential Research Tools for DES Drug Transport Studies
| Research Reagent / Tool | Function / Explanation |
|---|---|
| Sirolimus (Rapamycin) | An immunosuppressive and anti-proliferative drug that inhibits mTOR, used in DES to suppress smooth muscle cell proliferation and restenosis [26]. |
| Paclitaxel | A cytotoxic anti-proliferative drug that stabilizes microtubules, preventing cell division. Also used in DES and drug-eluting balloons [24]. |
| Bio-durable Polymers | Non-degradable polymer coatings (e.g., on early-generation DES) that provide a controlled matrix for drug release over time [25]. |
| Bioresorbable Polymers | Temporary polymer coatings that degrade after completing their drug delivery function, eliminating long-term polymer presence in the artery [3]. |
| Finite Volume Method Solver | A computational fluid dynamics (CFD) technique used to numerically solve the partial differential equations governing drug transport in complex arterial geometries [25]. |
| Agent-Based Modeling (ABM) Platform | A computational modeling paradigm used to simulate the actions and interactions of individual cells (e.g., VSMCs) to assess their collective behavior on tissue remodeling [7]. |
| Dual-Layer Coating | An advanced DES coating design featuring an internal and external drug-polymer layer, which can modulate the drug release profile to mitigate burst release and improve safety [7]. |
| Anisotropic Diffusivity Parameters | A set of distinct diffusion coefficients for different directions within the arterial wall (e.g., circumferential vs. transmural), which more accurately model tissue transport and lead to more uniform drug distribution [25]. |
| Saponin C, from Liriope muscari | Saponin C, from Liriope muscari, MF:C44H70O17, MW:871.0 g/mol |
| Hexamethylbenzene-d18 | Hexamethylbenzene-d18, CAS:4342-40-9, MF:C12H18, MW:162.27 g/mol |
The multi-layered arterial wall presents a highly dynamic and structured environment that determines the fate of drugs released from eluting stents. A deep understanding of the interplay between stent-based release kinetics (influenced by coating technology and drug load) and the tissue-based transport barriers (dictated by diffusion, convection, and binding kinetics) is paramount for optimizing DES design. Computational models that integrate these factors are indispensable tools for in-silico prediction and optimization, helping to narrow down design parameters before costly and time-consuming experimental trials. The ongoing innovation in DES technology, including dual-layer coatings, bioresorbable scaffolds, and sophisticated computational frameworks, continues to advance the central goal of achieving local therapeutic efficacy while ensuring systemic safety.
The evolution of Drug-Eluting Stents (DES) represents one of the most significant advancements in interventional cardiology, fundamentally transforming the management of coronary artery disease. DES technology has progressed through distinct generations, each addressing limitations of its predecessors while introducing novel therapeutic concepts. This progression has shifted the treatment paradigm from merely providing mechanical scaffolding to actively modulating the biological process of vessel healing [3]. The journey from first to fourth-generation DES reflects continuous innovation in scaffold materials, polymer biocompatibility, drug delivery kinetics, and therapeutic agents, culminating in today's sophisticated platforms that offer unprecedented safety and efficacy profiles. Understanding this evolutionary pathway is essential for researchers and drug development professionals working to advance coronary stent technology and improve patient outcomes.
Historical Development and Generational Classification
The Pre-DES Era: Bare-Metal Stents
The foundation for DES was laid with the introduction of bare-metal stents (BMS) in 1986, which represented a significant improvement over plain balloon angioplasty by preventing vessel recoil and negative remodeling [27]. While effective initially, BMS were plagued by high rates of in-stent restenosis (approximately 30%) due to neointimal hyperplasia - a response to vascular injury from stent deployment characterized by migration and proliferation of vascular smooth muscle cells [27]. This limitation prompted the development of more advanced solutions that could actively modulate the healing process.
First-Generation DES: Proof of Concept with Limitations
First-generation DES emerged in the early 2000s, introducing the revolutionary concept of local drug delivery to inhibit neointimal hyperplasia [27]. These stents featured stainless steel scaffolds coated with either sirolimus (a rapamycin analog) or paclitaxel, released via durable polymers to suppress smooth muscle cell proliferation [3]. The pioneering RAVEL, SIRIUS, and TAXUS trials established the efficacy of these platforms in significantly reducing restenosis rates compared to BMS [27].
However, first-generation DES revealed significant safety concerns, particularly regarding late (>30 days) and very late (>12 months) stent thrombosis, attributed to delayed endothelialization caused by the persistent presence of durable polymers and the anti-proliferative drugs themselves [27]. Additionally, the thick struts (approximately 140 micrometers) and limited flexibility of these early designs posed deliverability challenges in complex anatomy [27].
Table 1: First-Generation Drug-Eluting Stents
| Characteristic | Sirolimus-Eluting Stent (SES) | Paclitaxel-Eluting Stent (PES) |
|---|---|---|
| Scaffold Material | Stainless steel | Stainless steel |
| Strut Thickness | ~140 μm | ~140 μm |
| Therapeutic Agent | Sirolimus | Paclitaxel |
| Mechanism of Action | Binds FKBP12, inhibits mTOR, arrests cell cycle in G1 phase [27] | Inhibits microtubule disassembly, arrests cell cycle in G0-G1 and G2-M phases [27] |
| Key Clinical Trials | RAVEL, SIRIUS [27] | TAXUS [27] |
| Primary Limitation | Late stent thrombosis, delayed endothelialization | Clinical inferiority to SES in restenosis rate [27] |
Second-Generation DES: Enhanced Safety and Deliverability
Second-generation DES, introduced around 2006, addressed many limitations of their predecessors through systematic improvements in scaffold design and polymer technology [28] [3]. These stents transitioned from stainless steel to cobalt-chromium or platinum-chromium alloys, enabling thinner struts (approximately 70-90 micrometers), improved flexibility, and enhanced deliverability without compromising radial strength [27]. The ENDEAVOR and SPIRIT trials established the clinical profiles of these new platforms [27].
The therapeutic agents also evolved, with everolimus and zotarolimus (both sirolimus derivatives) replacing the original drugs, offering more favorable pharmacokinetic profiles [27]. Additionally, more biocompatible polymers were introduced to reduce inflammatory responses and promote healthier vessel healing. These collective advancements resulted in significantly improved safety profiles, particularly regarding very late stent thrombosis, while maintaining efficacy in reducing restenosis [3].
Table 2: Second-Generation Drug-Eluting Stents
| Characteristic | Everolimus-Eluting Stent (EES) | Zotarolimus-Eluting Stent (ZES) |
|---|---|---|
| Scaffold Material | Cobalt-chromium | Cobalt-chromium |
| Strut Thickness | ~80 μm | ~90 μm |
| Therapeutic Agent | Everolimus | Zotarolimus |
| Mechanism of Action | Sirolimus derivative, inhibits mTOR pathway | Sirolimus derivative, inhibits mTOR pathway |
| Key Clinical Trials | SPIRIT [27] | ENDEAVOR [27] |
| Advancements | Improved safety profile, thinner struts, more biocompatible polymers | Enhanced deliverability, reduced inflammation |
Third-Generation DES: Biodegradable Polymers
Third-generation DES introduced biodegradable polymers that provided temporary drug delivery during the critical period of neointimal hyperplasia (typically 3-6 months) before completely resorbing, thereby eliminating the long-term presence of foreign material in the vessel wall [3]. This approach aimed to combine the early restenosis prevention of DES with the long-term safety profile of BMS by allowing complete endothelialization once the polymer had degraded.
The evolution continued with platform refinements including thinner strut designs and optimized drug release kinetics. Initial setbacks with early bioresorbable scaffolds led to improvements in mechanical properties and resorption profiles, paving the way for next-generation technologies [3].
Fourth-Generation DES: Polymer-Free and Bioresorbable Platforms
As of 2025, fourth-generation DES technologies have emerged, characterized by polymer-free designs, advanced bioresorbable scaffolds, and nanotechnology-enhanced drug delivery systems [3]. These innovations aim to further improve long-term outcomes by promoting natural vessel healing, restoring vasomotion, and eliminating permanent metallic implants entirely.
Advanced bioresorbable vascular scaffolds (BVS) now feature hybrid metal-polymer compositions, ultra-thin struts (<70 μm), and accelerated resorption profiles (12-18 months) [3]. Polymer-free technologies utilize nanoporous surfaces or micro-reservoirs for controlled drug elution without permanent polymer presence. Additionally, multi-drug elution platforms that combine antiproliferative, anti-inflammatory, and pro-healing agents in temporally coordinated sequences represent the cutting edge of DES technology [3].
Quantitative Clinical Outcomes Across Generations
The progressive evolution of DES technology has translated into measurable improvements in clinical outcomes, as demonstrated by numerous randomized controlled trials and registry analyses. The following tables summarize key performance metrics across generations.
Table 3: Comparative Clinical Outcomes of First vs. Second-Generation DES
| Outcome Measure | First-Generation DES | Second-Generation DES | Pooled Effect Size (OR with 95% CI) | P-value |
|---|---|---|---|---|
| All-Cause Mortality | Increased risk | Reduced risk | OR: 1.23 (95% CI: 1.05-1.45) [28] | 0.0120 |
| Myocardial Infarction | Increased risk | Reduced risk | OR: 1.48 (95% CI: 1.22-1.80) [28] | <0.0001 |
| Target Lesion Revascularization | Increased risk | Reduced risk | OR: 1.47 (95% CI: 1.24-1.74) [28] | <0.0001 |
| Cardiac Death | Similar risk | Similar risk | Not significant [28] | - |
| Major Adverse Cardiovascular Events | Similar risk | Similar risk | Not significant [28] | - |
Table 4: Contemporary DES Performance Metrics (2025)
| Performance Metric | Fourth-Generation DES | Third-Generation DES | Second-Generation DES |
|---|---|---|---|
| Target Lesion Failure (1 year) | <3% [3] | ~4-5% | ~5-6% |
| Very Late Stent Thrombosis (/year) | <0.1% [3] | ~0.2-0.3% | ~0.3-0.5% |
| Strut Thickness | 60-70 μm [3] | 70-80 μm | 80-100 μm |
| Polymer Presence | Polymer-free or fully bioresorbable [3] | Biodegradable (3-6 months) | Durable or biodegradable |
Experimental Protocols for DES Evaluation
Pre-Clinical Assessment Protocol
Objective: To evaluate the safety and efficacy of novel DES platforms in controlled animal models before human trials.
Methodology:
- Stent Implantation: Deploy test and control DES in healthy or atherosclerotic porcine coronary arteries (n=30-40 stents per group)
- Histopathological Analysis:
- Euthanize animals at 28, 90, and 180 days post-implantation
- Process arteries for plastic embedding and sectioning
- Perform hematoxylin-eosin and elastic trichrome staining
- Quantify neointimal area, inflammation score, endothelialization percentage, and fibrin deposition
- Drug Kinetics Assessment:
- Measure tissue drug concentrations at multiple time points using LC-MS/MS
- Determine arterial wall drug distribution via autoradiography or MALDI imaging
- Statistical Analysis: Compare continuous variables using ANOVA with post-hoc testing, categorical variables with chi-square test (significance at p<0.05)
Clinical Evaluation Protocol for New DES Platforms
Objective: To demonstrate clinical non-inferiority and superiority of next-generation DES compared to contemporary standards.
Study Design: Prospective, multicenter, randomized controlled trial with blinded endpoint adjudication.
Population: Patients with symptomatic coronary artery disease requiring percutaneous intervention (n=2000-5000).
Intervention:
- Experimental: Novel DES platform (e.g., polymer-free nano-coated)
- Control: Current standard-of-care DES
Primary Endpoint: Target lesion failure at 12 months (composite of cardiac death, target vessel myocardial infarction, clinically-driven target lesion revascularization).
Secondary Endpoints:
- Device success
- Procedure success
- Individual components of primary endpoint
- Stent thrombosis (ARC definite/probable)
- Patient-oriented composite endpoint (all death, all MI, all revascularization)
Follow-up Protocol: Clinical assessment at 1, 6, and 12 months, then annually to 5 years; angiographic follow-up in subset at 13 months; intravascular imaging in subset at 13 months.
Statistical Considerations:
- Power calculation based on non-inferiority margin of 3.5% for primary endpoint
- Intention-to-treat analysis
- Pre-specified subgroup analyses for complex lesions
Signaling Pathways and Biological Mechanisms
The efficacy of DES depends on precisely modulating complex biological pathways involved in vascular healing. The following diagram illustrates key signaling pathways targeted by DES therapeutic agents.
DES Technology Selection Algorithm
Choosing the appropriate DES generation and platform requires consideration of multiple clinical, anatomical, and patient-specific factors. The following workflow provides a systematic approach to DES selection.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 5: Essential Research Reagents for DES Development
| Research Reagent | Function/Application | Technical Specifications |
|---|---|---|
| Cobalt-Chromium Alloy | Scaffold material for 2nd-4th generation DES | MP35N or L605 composition, radial strength >150 kPa, strut thickness 60-90 μm [27] |
| Poly(L-lactic-co-glycolic acid) PLGA | Biodegradable polymer for drug elution | Varying lactide:glycolide ratios (50:50 to 85:15), molecular weight 10-100 kDa, degradation time 30-180 days [3] |
| Everolimus | Anti-proliferative therapeutic agent | Chemical formula C₅₃H₈₃NOâ‚â‚„, molecular weight 958.2 g/mol, solubility in ethanol ~50 mg/mL, working concentration 100 μg/cm² stent surface area [27] |
| Fluorescently-labeled Anti-CD31 Antibody | Endothelialization assessment | Host: mouse monoclonal, clone JC70A, working dilution 1:100-1:500, excitation/emission ~494/519 nm (FITC conjugate) |
| Masson's Trichrome Stain | Histological evaluation of vessel healing | Differentiates collagen (blue), muscle/cytoplasm (red), and nuclei (dark brown); quantifies neointimal area and fibrin deposition |
| PDGF-BB Recombinant Protein | In vitro smooth muscle cell proliferation assay | Source: E. coli, molecular weight ~25 kDa, working concentration 10-50 ng/mL, induces SMC migration and proliferation |
| HUVEC (Human Umbilical Vein Endothelial Cells) | Endothelialization and biocompatibility testing | Culture medium: ECM-2 with growth supplements, passage 3-6, seeding density 10,000 cells/cm² for migration assays |
| LC-MS/MS System | Drug release kinetics and tissue concentration | Column: C18 reverse phase (2.1 × 50 mm, 1.8 μm), mobile phase: methanol/water with 0.1% formic acid, LLOQ ~0.1 ng/mL for rapamycin analogs |
| 2-Picenecarboxylic acid | 2-Picenecarboxylic acid, CAS:118172-80-8, MF:C28H36O5, MW:452.6 g/mol | Chemical Reagent |
| 10-Methylhexadecanoic acid | 10-Methylhexadecanoic acid, CAS:17001-26-2, MF:C17H34O2, MW:270.5 g/mol | Chemical Reagent |
Future Directions and Emerging Technologies
The evolution of DES technology continues with several promising innovations currently in advanced stages of development. Genetically engineered endothelial progenitor cell capture stents incorporate antibodies or aptamers that selectively capture circulating endothelial progenitor cells, dramatically accelerating endothelialization and vessel healing [3]. Smart stents with integrated miniaturized sensors can monitor local flow dynamics, inflammatory markers, and endothelial function in real-time, providing unprecedented insights into vessel healing and enabling early detection of complications [3].
Three-dimensional printed personalized stents represent another frontier, with customized designs tailored to individual patient anatomy potentially manufactured in the catheterization laboratory during the procedure itself [3]. Additionally, dual-drug eluting stents carrying combinations of antiproliferative and anti-thrombotic agents with time-controlled release profiles are being developed to target the different timing of bio-response to stent implantation [27]. Gene-eluting stents that deliver plasmid DNA to express therapeutic proteins such as VEGF directly within the vessel wall are also under investigation to support healthy endothelialization [27].
These emerging technologies, combined with personalized medicine approaches based on genetic profiling and lesion-specific characteristics, promise to further refine the field of coronary intervention and improve outcomes for the millions of patients worldwide affected by coronary artery disease.
DES Coating Techniques and Advanced Application Methodologies
The application of uniform, consistent coatings is a critical step in the manufacturing of drug-eluting stents (DES), directly influencing drug delivery kinetics, safety, and therapeutic efficacy [6]. Coating techniques must ensure precise control over thickness, uniformity, and integrity to facilitate controlled drug elution and maintain biocompatibility within the vascular environment [6]. This document provides detailed application notes and experimental protocols for three central coating methods—dip-coating, spray-coating, and immersion techniques—within the specific context of DES development for researchers and scientists.
The selection of a coating method impacts critical quality attributes. Table 1 provides a comparative overview of these techniques.
Table 1: Comparison of Coating Application Methods for Drug-Eluting Stents
| Parameter | Dip-Coating | Spray-Coating | Immersion Techniques |
|---|---|---|---|
| Primary Mechanism | Submersion and withdrawal of stent into coating solution [6] | Atomization of coating solution directed onto stent surface [6] [29] | Prolonged submersion to saturate or functionalize the surface |
| Coating Uniformity | Challenging to ensure uniformity; prone to edge effects [6] | High uniformity achievable; industry-feasible for layer-by-layer coating [6] [29] | Varies with substrate and solution properties |
| Process Control | Dependent on withdrawal speed and viscosity [30] | High control via programmable parameters (spray rate, pattern, nozzle distance) [29] | Dependent on immersion time and concentration |
| Scalability | Suitable for R&D and small batches [29] | Highly scalable for industrial production with high productivity [6] | Easily scalable for batch processing |
| Key Challenges | Ensuring uniformity, avoiding sagging, managing solvent evaporation [6] | Managing overspray, nozzle clogging, ensuring consistent droplet size [6] | Controlling drug leaching back into solution, achieving precise thickness |
Dip-Coating Methodology
Dip-coating involves the controlled submersion and withdrawal of a stent from a coating solution reservoir. The coating thickness is primarily governed by the withdrawal speed and the viscosity of the coating solution [30].
Experimental Protocol: Dip-Coating of a Polymeric Drug Solution
Objective: To apply a uniform primer layer of a biodegradable polymer (e.g., PLGA) onto a nitinol stent platform.
Materials:
- Stent Substrate: Cleaned, bare nitinol stent.
- Coating Solution: Poly(D,L-lactide-co-glycolide) (PLGA) dissolved in a suitable organic solvent (e.g., acetone, dimethyl sulfoxide) to a target concentration (e.g., 1-5% w/v).
- Equipment: Precision dip-coater apparatus (automated or semi-automated), solvent-resistant container, fume hood, drying oven.
Procedure:
- Stent Preparation: Plasma clean the nitinol stent to increase surface energy and promote coating adhesion.
- Solution Preparation: Dissolve the PLGA polymer in the solvent under constant stirring until a clear, homogeneous solution is achieved.
- Coating Process:
- Secure the stent vertically in the dip-coater holder.
- Program the dip-coater with the following parameters:
- Immersion speed: 5 mm/s
- Dwell time in solution: 30 seconds
- Withdrawal speed: 1 mm/s (optimize based on desired thickness)
- Initiate the coating cycle to submerge the stent completely, hold, and withdraw.
- Drying & Curing:
- Immediately transfer the coated stent to a drying oven.
- Cure at a controlled temperature (e.g., 40-50°C) for 1-2 hours to evaporate the solvent.
- Quality Assessment: Determine coating mass gravimetrically and inspect for defects using scanning electron microscopy (SEM).
Workflow Visualization
The following diagram illustrates the sequential steps involved in a standardized dip-coating process.
Spray-Coating Methodology
Spray-coating employs atomization to deposit a fine mist of coating solution onto the stent surface. It is the most widely used technique in industrial-scale DES manufacturing due to its precision and layer-by-layer capability [6] [29].
Experimental Protocol: Spray-Coating of a Drug-Polymer Matrix
Objective: To apply a uniform layer of a drug-polymer matrix (e.g., Sirolimus in PLGA) onto a primed stent surface.
Materials:
- Stent Substrate: Primer-coated nitinol stent mounted on a rotating mandrel.
- Coating Solution: Homogeneous dispersion of crystalline Sirolimus in PLGA solution [31].
- Equipment: Ultrasonic spray coater with precision nozzle, XYZ motion stage, rotary fixture, fume hood, drying oven.
Procedure:
- System Setup:
- Mount the stent securely on a rotating mandrel within the spray chamber.
- Set the nozzle-to-stent distance (e.g., 10-30 mm).
- Calibrate the spray parameters using a blank substrate.
- Coating Process:
- Program the spray coater with optimized parameters:
- Nozzle type: Ultrasonic or air-assisted
- Liquid flow rate: 0.1 - 0.5 mL/min
- Atomization pressure (if applicable): 5-15 psi
- Mandrel rotation speed: 100-500 rpm
- Nozzle traverse speed: 1-10 mm/s
- Number of passes: 10-100 (to achieve target drug dose)
- Initiate the spray cycle, ensuring even coverage over the entire stent surface.
- Program the spray coater with optimized parameters:
- Drying Between Layers: Apply mild drying (e.g., 40°C air flow) between passes to prevent washing off previous layers.
- Final Curing: After the final pass, cure the stent in an oven at a specified temperature and time to form a stable coating.
- Quality Assessment: Measure coating thickness per strut via SEM and perform HPLC to quantify drug content and uniformity.
Workflow Visualization
The following diagram outlines the core operational loop of a spray-coating system.
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful coating development relies on a suite of specialized materials. Table 2 details key reagents and their functions in DES coating formulation and application.
Table 2: Essential Research Reagents for Stent Coating R&D
| Reagent/Material | Function/Description | Example in DES Context |
|---|---|---|
| Biodegradable Polymers | Acts as a drug-carrying matrix; controls drug release rate; degrades in vivo to improve long-term biocompatibility [6] [31]. | Poly(lactide-co-glycolic acid) (PLGA) [31]. |
| Cytostatic Drugs | The active pharmaceutical ingredient that inhibits smooth muscle cell proliferation to prevent in-stent restenosis [6]. | Sirolimus (arrests cell cycle) or Paclitaxel (disrupts microtubules) [6]. |
| Organic Solvents | Dissolves or disperses the polymer and drug to create a coatable solution; evaporates during drying. | Acetone, Dichloromethane, Dimethyl Sulfoxide. |
| Primer Solutions | Enhances adhesion between the metallic stent surface and the drug-polymer coating, improving durability [30]. | A thin, adhesive polymer layer (e.g., Parylene). |
| Stent Platform | The underlying scaffold that provides mechanical support to the artery. | Cobalt-Chromium alloy or Nitinol (NiTi) for flexibility [6]. |
| Methyl 15-methylheptadecanoate | Methyl 15-methylheptadecanoate, CAS:54833-55-5, MF:C19H38O2, MW:298.5 g/mol | Chemical Reagent |
| 21-Methyldocosanoic acid | 21-Methyldocosanoic acid, CAS:59708-74-6, MF:C23H46O2, MW:354.6 g/mol | Chemical Reagent |
Critical Coating Challenges and Evaluation Parameters
Regardless of the application method, coated stents must be rigorously evaluated against key performance parameters, as outlined in Table 3.
Table 3: Key Evaluation Parameters for Coated Stents
| Evaluation Parameter | Description | Standard Analytical Methods |
|---|---|---|
| Coating Uniformity | Consistency of coating thickness and distribution across the stent strut geometry. | Scanning Electron Microscopy (SEM), Optical Coherence Tomography [6]. |
| Drug Release Kinetics | Profile of drug elution over time in a physiological environment; target is sustained release over weeks [6]. | In vitro release testing using USP apparatus in phosphate buffer at 37°C [6]. |
| Coating Integrity | Resistance to cracking, peeling, or delamination during stent crimping and expansion. | SEM analysis post-deployment in simulated use conditions [6] [31]. |
| Drug Stability | Integrity of the active pharmaceutical ingredient during processing and storage. | HPLC-MS/MS to quantify parent drug and degradants [31]. |
| Sterilization Stability | Coating integrity and drug efficacy post-sterilization (e.g., via Ethylene Oxide) [6]. | In vitro release testing and functional assays post-sterilization. |
Drug-eluting stents (DES) represent the standard of care in percutaneous coronary intervention (PCI), primarily due to their ability to reduce the incidence of in-stent restenosis (ISR) through the localized delivery of antiproliferative agents [10] [3]. The polymer coating on the stent platform is a critical component, functioning as a drug reservoir and controlling the release kinetics of the therapeutic agent. Historically, first-generation DES utilized durable polymers (DPs), which remain permanently on the stent surface after drug elution is complete. While effective, these polymers have been associated with persistent inflammation and delayed vessel healing, contributing to risks such as late stent thrombosis (ST) [10] [6].
To mitigate these long-term risks, biodegradable polymer (BP) platforms were developed. These polymers provide controlled drug release and then fully resorb over a defined period, leaving behind a bare stent scaffold. This approach aims to eliminate the long-term inflammatory stimulus of a permanent polymer, thereby potentially enhancing vascular healing and reducing very late adverse events [10] [3]. This document provides a detailed comparison of these two polymer platforms and outlines essential experimental protocols for their evaluation within a research context.
Comparative Analysis: Biodegradable vs. Durable Polymers
The choice between biodegradable and durable polymer systems involves a careful trade-off between initial performance and long-term safety. The following table summarizes the core characteristics of each platform.
Table 1: Fundamental Characteristics of Polymer Platforms
| Feature | Biodegradable Polymers (BP) | Durable Polymers (DP) |
|---|---|---|
| Definition | Polymers designed to break down into biologically acceptable compounds upon completion of drug release [3]. | Non-erodible polymers that remain permanently on the stent strut after drug elution [6]. |
| Primary Rationale | Eliminate long-term polymer presence to reduce chronic inflammation and allow vessel healing, potentially reducing very late ST [10] [3]. | Proven technology with established, predictable drug release profiles for effective suppression of neointimal hyperplasia [6]. |
| Key Advantages | • Reduced long-term inflammatory response [10]• Potential for restored vasomortality• Eliminates risk of polymer-induced late complications | • Extensive long-term clinical data• Highly stable and predictable coating integrity• Simpler regulatory pathway for established polymers |
| Inherent Challenges | • Transient inflammatory response during degradation [6]• Critical dependency on degradation kinetics matching healing process• Potential for acidic by-products upon hydrolysis | • Risk of chronic inflammation and hypersensitivity [10] [6]• Potential for late stent malapposition• Permanent implant with no bioresorption |
| Common Materials | Polylactic-co-glycolic acid (PLGA), Polylactic acid (PLA), Polyhydroxyalkanoates (PHA) [32]. | Polyethylene-co-vinyl acetate (PEVA), Poly-n-butyl methacrylate (PBMA), Polyurethane (PU), Polysiloxanes [6] [9]. |
Clinical evidence comparing these platforms is evolving. A 2025 meta-analysis of randomized controlled trials (RCTs) found that at 12 and 24 months, polymer-free DES and thin-strut biodegradable polymer DES demonstrated comparable clinical performance for endpoints including target lesion revascularization (TLR), myocardial infarction (MI), and stent thrombosis [10]. This suggests that modern BP-DES have achieved parity with advanced PF-DES in the medium term. The study also highlighted device-specific effects, noting a significant reduction in cardiac death with the BioFreedom polymer-free stent, which underscores that outcomes can be influenced by specific stent design and drug combination, not just the polymer category itself [10].
Table 2: Clinical and Market Outlook (2025-2030)
| Parameter | Biodegradable Polymer DES | Durable Polymer DES & Related Markets |
|---|---|---|
| Clinical Performance (12-month) | Comparable to PF-DES for TLR, MI, and ST [10]. | Mature technology; performance is drug and patient-specific. |
| Market Growth Driver | Focus on long-term safety and vascular healing [3] [33]. | Innovation in drug combinations and polymer biocompatibility [3]. |
| Global Polymer Market Context | The broader biodegradable polymer market is projected to grow from USD 9.3 Billion (2024) to USD 27.0 Billion by 2030 (CAGR 19.4%) [34]. | -- |
| DES-Specific Market Forecast | The biodegradable coated DES market is poised for significant expansion, potentially reaching an estimated 8.2 million units by 2033 [33]. | -- |
Experimental Protocols for Polymer Coating Evaluation
Robust and standardized experimental protocols are essential for the development and regulatory approval of new polymer-coated DES. The following sections outline key methodologies.
Protocol: In Vitro Drug Release Kinetics
1. Objective: To characterize the drug release profile of a coated stent under simulated physiological conditions, and to establish an accelerated release model for quality control.
2. Materials:
- Coated stent samples
- Phosphate Buffered Saline (PBS), pH 7.4, with optional 0.02% w/v sodium azide (as preservative)
- USP Apparatus 4 (Flow-Through Cell) or Apparatus 2 (Paddle)
- Controlled temperature water bath or incubator (37°C ± 0.5°C)
- High-Performance Liquid Chromatography (HPLC) system with validated analytical method
3. Methodology:
- Real-Time Release Study:
- Immerse individual stents in a known volume of release medium (e.g., 50 mL) in a sealed container.
- Incubate at 37°C under gentle agitation.
- At predetermined time points (e.g., 1, 4, 8, 24 hours, then weekly up to 90-180 days), withdraw and replace the entire release medium to maintain sink conditions.
- Analyze the drug concentration in the withdrawn samples using HPLC.
- Plot cumulative drug release (%) versus time to generate the release profile [6].
- Accelerated Release Study:
- To predict long-term release behavior in a shorter timeframe, conditions may be modified (e.g., elevated temperature, altered pH, or addition of organic solvents).
- A correlation between accelerated and real-time release profiles must be established and validated [6].
4. Data Analysis:
- Determine key release parameters: burst release (%), daily release rate, and time for 50%, 80%, and 95% cumulative release.
- Fit release data to kinetic models (e.g., zero-order, first-order, Higuchi) to understand the release mechanism.
The workflow for designing and analyzing a drug release study is outlined below.
Protocol: Coating Integrity and Surface Characterization
1. Objective: To assess the uniformity, thickness, and physical state of the drug-polymer coating before and after simulated use and sterilization.
2. Materials:
- Coated stent samples (pre- and post-expansion)
- Scanning Electron Microscope (SEM)
- Atomic Force Microscope (AFM)
- Optical Coherence Tomography (OCT) system or Thin-Film Laser Profilometer
- Fourier Transform Infrared (FTIR) Spectrometer
3. Methodology:
- Surface Morphology (SEM):
- Mount stents on SEM stubs and sputter-coat with a conductive layer (e.g., gold) if non-conductive.
- Image the stent surface at various magnifications (e.g., 50x to 10,000x) to evaluate coating uniformity, presence of cracks, webbing, or delamination [6].
- Coating Thickness (OCT/Profilometer):
- Use OCT cross-sectional imaging or a laser profilometer to perform multiple point measurements along the stent struts.
- Calculate the average coating thickness and standard deviation to ensure it conforms to design specifications [6].
- Drug-Polymer Interaction (FTIR):
- Perform FTIR spectroscopy in attenuated total reflectance (ATR) mode on the coated stent.
- Compare the spectrum of the drug-polymer coating to that of the pure drug and pure polymer.
- Identify any shifts, disappearance, or appearance of peaks to determine if the drug remains in its crystalline form or is dispersed amorphously within the polymer matrix [9].
4. Data Analysis:
- Report qualitative SEM observations with representative images.
- Quantify coating thickness and surface roughness (Ra) from profilometry data.
- Interpret FTIR spectra to confirm drug stability and compatibility with the polymer.
The Scientist's Toolkit: Key Research Reagents & Materials
Successful development and testing of polymer-coated stents require a suite of specialized materials and analytical tools.
Table 3: Essential Research Reagents and Materials
| Category / Item | Function / Explanation | Examples / Notes |
|---|---|---|
| Polymer Substrates | Forms the drug-eluting matrix; controls release kinetics and influences biocompatibility. | Biodegradable: PLGA, PLA, PHA [32]. Durable: PEVA, PBMA, Polysiloxanes [9]. |
| Active Agents | Pharmacological agent to inhibit neointimal hyperplasia and restenosis. | Sirolimus, Everolimus, Paclitaxel, Zotarolimus [3] [6]. |
| Coating Solvents | Dissolves polymer and drug for uniform coating application via spray or dip-coating. | Tetrahydrofuran (THF), Dimethylformamide (DMF), Chloroform. Must have appropriate volatility and solubility. |
| Analytical Standards | Certified reference materials for quantifying drug content and degradation products. | USP-grade reference standards for the active drug (e.g., Sirolimus) and potential impurities. |
| Characterization Tools | Instruments for critical quality attribute analysis. | HPLC: Drug quantification and release kinetics [6]. SEM: Coating morphology and integrity [6]. FTIR: Drug-polymer compatibility and stability [9]. |
| 2-Nitrophenanthraquinone | 2-Nitrophenanthraquinone, CAS:604-95-5, MF:C14H7NO4, MW:253.21 g/mol | Chemical Reagent |
| Tert-butyl 11-aminoundecanoate | Tert-butyl 11-aminoundecanoate, CAS:220851-29-6, MF:C15H31NO2, MW:257.41 g/mol | Chemical Reagent |
The biological response to a coated stent involves a complex signaling pathway, which is simplified in the following diagram.
The evolution of drug-eluting stents (DES) has been driven by the need to overcome the limitations of permanent polymer coatings, which have been associated with chronic inflammation, delayed arterial healing, and late stent thrombosis [8]. Polymer-free technologies represent a significant innovation by eliminating the polymeric carrier while maintaining controlled drug delivery through advanced physical architectures. Two principal platforms have emerged: microporous surfaces and reservoir/channel systems. Microporous technology utilizes a high-surface-area metallic surface with nanoscale to microscale pores to adsorb and retain pharmaceutical agents [35]. Reservoir systems incorporate precisely engineered cavities or channels within the stent struts themselves, which can be loaded with drug formulations without surface coatings [36]. These platforms enable direct tissue contact with the bare metal surface while providing controlled drug elution kinetics, potentially offering superior vascular healing profiles compared to conventional polymer-based DES [37].
Table 1: Comparison of Polymer-Free DES Technologies
| Technology Feature | Microporous Surface Technology | Reservoir/Channel Systems |
|---|---|---|
| Drug Carrier Mechanism | Adsorption onto porous surface; probucol often used as excipient [37] | Physical encapsulation within machined reservoirs [36] |
| Surface Architecture | Microporous (pores 2-50 nm) and macroporous (pores >50 nm) structures [35] | Rhombic-shaped or groove-based channels laser-etched into struts [36] |
| Representative Devices | Yukon Choice PC, Cre8, Axxion [38] | NEVO (Cordis), Firehawk (MicroPort), Janus (Sorin) [36] |
| Drug Loading Method | Simple mixing, solvent evaporation, or vacuum processes [35] | Precision filling of reservoirs with drug-polymer mixes [36] |
| Strut Thickness | 87-96 μm (stainless steel) or 68-79 μm (cobalt chromium) [37] | Varies by design; can maintain thin strut profiles [36] |
| Potential Advantages | Enhanced endothelialization; reduced inflammation [37] | Programmable multi-drug delivery; no surface coating [36] |
Table 2: Quantitative Preclinical Performance Data of Polymer-Free DES
| DES Platform | Neointimal Area (mm²) at 90 days | Percentage Diameter Stenosis (%) | Endothelialization at 14 days | Inflammation Score (0-3) |
|---|---|---|---|---|
| CC-EEPFS (Test Device) | 2.1 ± 0.4 | 22 ± 5 | Near-complete (≥95%) [37] | 0.5 ± 0.2 |
| SS-SEPBS (Polymer Control) | 3.0 ± 0.5 | 35 ± 7 | Limited coverage [37] | 1.5 ± 0.4 |
| SS-SEPFS (Polymer-Free) | 2.4 ± 0.3 | 26 ± 6 | Significant improvement over polymer [37] | 0.8 ± 0.3 |
Microporous Surface Technology: Application Notes
Technology Principle and Design Rationale
Microporous surface technology leverages the fundamental principles of adsorption and capillary action to retain and elute pharmaceutical agents from stent surfaces. The technology utilizes a network of interconnected pores with varying dimensions classified as micropores (width <2 nm), mesopores (2-50 nm), and macropores (>50 nm) [35]. This hierarchical pore structure creates an exceptionally high surface area for drug adsorption while enabling controlled release kinetics through diffusion from the water-filled channels. The absence of synthetic polymers eliminates the risk of polymer-induced hypersensitivity reactions and chronic inflammation, addressing a key limitation of first-generation DES [8]. Microporous surfaces can be engineered on various stent alloys including stainless steel and cobalt-chromium through specialized surface treatment processes that create controlled roughness and porosity at the micron and sub-micron scale.
Experimental Protocol: Preclinical Evaluation of Microporous DES
Objective: To assess the safety and efficacy of microporous polymer-free DES in a porcine model of coronary stenting, with focus on vascular healing, endothelialization, and neointimal suppression.
Materials and Equipment:
- Test microporous polymer-free DES (e.g., CoCr-everolimus with probucol matrix)
- Control stents (polymer-based DES and bare metal stents)
- Juvenile domestic farm pigs (3 months old, 25-35 kg)
- Quantitative Coronary Angiography (QCA) system
- Scanning Electron Microscope
- Histopathology supplies (MMA resin, microtome, H&E, VVG stains)
Procedure:
- Stent Implantation:
- Pre-medicate animals with clopidogrel (75 mg) and aspirin (100 mg) 48 hours pre-procedure
- Induce general anesthesia with ketamine (20 mg/kg, i.m.) and xylazine (2 mg/kg, i.m.)
- Maintain anesthesia with isoflurane (1-2 vol%) in oxygen/air mixture
- Administer heparin (5000 IU i.a.) and aspirin (250 mg i.a.) before catheterization
- Implant stents in LAD, LCx, and RCA with 1.1:1 overstretch ratio
- Document vessel patency post-procedure via angiography
Tissue Harvest and Processing:
- Euthanize animals at predetermined endpoints (14, 28, 90 days)
- Pressure-fix coronary arteries with 10% buffered formalin at 100 mm Hg
- Excise stented segments with proximal and distal native vessel margins
- Embed tissue in methyl methacrylate (MMA) resin
- Section using laser microtome at 10 μm thickness
Endpoint Assessment:
- Angiographic Analysis (QCA): Measure late lumen loss as MLDpost-procedure - MLDfollow-up
- Histopathology: Grade injury, inflammation, and fibrin deposition using established scoring systems
- Morphometry: Quantify lumen area, internal elastic lamina (IEL) area, and neointimal area
- SEM Evaluation: Assess endothelial coverage percentage at 14-day timepoint
Data Analysis: Calculate percentage stenosis as [1 - (Lumen Area/IEL Area)] × 100. Compare neointimal area, inflammation scores, and endothelialization between test and control devices using appropriate statistical methods (ANOVA with post-hoc testing). A sample size of n=10 per group provides 80% power to detect 30% difference in neointimal area with α=0.05.
Reservoir/Channel Systems: Application Notes
Technology Principle and Design Rationale
Reservoir or channel stent systems represent a paradigm shift in DES technology by incorporating dedicated drug reservoirs within the stent struts rather than relying on surface coatings. These systems feature laser-machined cavities, grooves, or channels that function as discrete drug depots [36]. The rhombic-shaped reservoir design has demonstrated particular promise, offering multiple advantages including significantly increased drug capacity (multiple times conventional DES) and enhanced fatigue resistance with a safety factor up to 50% higher than conventional DES [36]. This geometry optimizes stress distribution around the reservoir edges, mitigating the potential for strut fatigue failure in peripheral arteries subjected to complex biomechanical forces. The reservoir approach enables sophisticated drug delivery paradigms including programmable multi-drug release kinetics and site-specific therapy targeting.
Experimental Protocol: In Vitro Drug Release Testing
Objective: To characterize the drug release profile from reservoir-based DES under accelerated and real-time conditions.
Materials and Equipment:
- Reservoir DES test samples (n=6 per group)
- USP Apparatus 4 (flow-through cell) or Apparatus 7 (reciprocating holder)
- Phosphate buffered saline (PBS, pH 7.4) with 0.05% Tween 80
- High-performance liquid chromatography (HPLC) system with validated assay
- Controlled temperature water bath (37±0.5°C)
- Sampling apparatus and vials
Procedure:
- Apparatus Setup:
- Fill dissolution vessels with 250 mL release medium (PBS + Tween 80)
- Maintain temperature at 37±0.5°C with continuous stirring (50 rpm)
- For reservoir stents, consider using USP Apparatus 7 to simulate vessel wall contact
Sample Placement:
- Mount stents in suitable holders ensuring complete immersion
- Position to ensure uniform fluid flow across all reservoir surfaces
- Include appropriate sink conditions throughout testing
Sampling Schedule:
- Collect samples at 1, 2, 4, 8, 24, 48, 72, 96, 120, 168, 336, 504, and 672 hours
- Withdraw 1 mL aliquots and replace with fresh pre-warmed medium
- Filter samples through 0.45 μm membrane before analysis
Drug Quantification:
- Analyze samples using validated HPLC method
- Calculate cumulative drug release percentage at each time point
- Plot release profile (cumulative % released vs. time)
Accelerated Release Testing:
- Conduct parallel testing at elevated temperature (45°C) with increased agitation
- Establish correlation between accelerated and real-time release profiles
- Use accelerated method for quality control and stability testing
Data Analysis: Fit release data to appropriate mathematical models (zero-order, first-order, Higuchi, Korsmeyer-Peppas) to understand release mechanisms. Determine key release parameters including initial burst release percentage, daily release rate, and time for 50% and 80% drug release (T50, T80).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Polymer-Free DES Research
| Category/Item | Function/Application | Representative Examples |
|---|---|---|
| Stent Platforms | Structural scaffold for drug delivery | Cobalt-chromium (CoCr) alloys, Stainless steel (316L), Nitinol (NiTi) [36] [37] |
| Anti-Restenotic Drugs | Inhibit neointimal hyperplasia | Sirolimus, Everolimus, Zotarolimus (cytostatic); Paclitaxel (cytotoxic) [36] [6] |
| Excipients/Matrices | Modulate drug release kinetics | Probucol (hydrophobic excipient) [37] |
| Porous Carriers | High surface area for drug adsorption | Mesoporous silica, Ethylene vinyl acetate, Polypropylene foam powder [35] |
| Coating Solvents | Drug loading and formulation | Acetone, Ethanol, Dichloromethane (for solvent evaporation processes) [35] |
| In Vitro Release Media | Simulate physiological conditions | PBS (pH 7.4) with 0.05% Tween 80 [6] |
| Sterilization Methods | Terminal sterilization of finished devices | Ethylene oxide (EtO) sterilization [6] |
| Analytical Instruments | Drug release quantification and characterization | HPLC (drug quantification), SEM (surface morphology), QCA (angiographic analysis) [37] [6] |
| Fmoc-NH-PEG12-CH2COOH | Fmoc-NH-PEG12-CH2COOH|PEG Linker|CAS 2291257-76-4 | |
| Cholesteryl 10-undecenoate | Cholesteryl 10-undecenoate, CAS:30948-01-7, MF:C38H64O2, MW:552.9 g/mol | Chemical Reagent |
Clinical and Regulatory Considerations
The translation of polymer-free DES technologies from preclinical development to clinical application requires rigorous evaluation of safety and efficacy. Recent randomized controlled trials have demonstrated that polymer-free DES exhibit non-inferiority compared to contemporary polymer-based DES for clinical endpoints including target lesion failure [39]. At 9-month follow-up, freedom from target lesion failure was 95.8% for polymer-free sirolimus- and probucol-eluting stents versus 97.3% for durable polymer everolimus-eluting stents, meeting non-inferiority criteria [39]. However, a comprehensive meta-analysis of 10 randomized trials revealed nuanced outcomes, with polymer-free DES showing benefits in reducing long-term late lumen loss and all-cause mortality, but no superiority in reducing myocardial infarction, target lesion revascularization, or late stent thrombosis [38]. Notably, certain polymer-free platforms have demonstrated an increased risk of early stent thrombosis within 30 days compared to biodegradable polymer DES (1.0% vs 0.3%; HR 3.72) [40], highlighting the importance of optimal antithrombotic regimens.
Regulatory assessment of polymer-free DES follows stringent requirements for Class D medical devices, with expectations for comprehensive non-clinical testing including sterility validation, stability studies, and demonstration of equivalent or superior performance to predicate devices [6]. Stability testing should follow ICH guidelines, with particular attention to drug content uniformity, coating integrity, and mechanical performance over the proposed shelf life. Establishing in vitro-in vivo correlation (IVIVC) is particularly valuable for supporting product changes and quality control, potentially reducing the need for extensive clinical studies [6].
Application Notes: Nanoporous Materials in Drug-Eluting Stents
Rationale for Nanoporous Architectures in Stent Coatings
The integration of nanoporous structures onto drug-eluting stents (DES) represents a paradigm shift in local intravascular drug delivery. These architectures function as highly efficient reservoirs for therapeutic agents, offering significant advantages over conventional polymer coatings. Their unique properties include an extensive surface area-to-volume ratio, which can exceed 1000 m² gâ»Â¹ for materials like mesoporous silica nanoparticles, enabling high drug loading capacity [41] [42]. Furthermore, the tunable pore size, typically within the 1-100 nm range, allows for precise control over drug release kinetics, while surface functionalization facilitates targeted delivery and enhanced biocompatibility [42]. The primary goal is to mitigate in-stent restenosis (ISR)—a re-narrowing of the artery that occurs in a significant proportion of angioplasty procedures—by providing sustained, controlled release of antiproliferative drugs directly to the vessel wall [6] [43].
Key Nanoporous Coating Technologies and Performance
Table 1: Comparison of Nanoporous Material Platforms for Stent Coatings
| Material Platform | Key Characteristics | Drug Release Mechanism | Targeted Application in DES |
|---|---|---|---|
| Mesoporous Silica Nanoparticles (MSNs) [41] [42] | High surface area (>1000 m²/g); tunable pore size (2-50 nm); surface easily functionalized. | Diffusion-controlled release; can be gated with stimuli-responsive caps. | Delivery of sirolimus, everolimus; targeted delivery via folic acid/antibody modification. |
| Nanoporous Alumina Membranes (NPAIMs) [44] | Inorganic, highly ordered nanochannels; robust mechanical stability. | Sustained release via molecular diffusion through pores over periods up to 28 days. | Investigated for controlled release of memantine; potential for other neurovascular therapeutics. |
| Sol-Gel Derived Oxides (e.g., Titania, Zirconia) [42] | Biocompatible; formed via low-temperature sol-gel process; hybrid organic-inorganic compositions possible. | Degradation-controlled or diffusion-controlled release, depending on matrix density. | Biostable coatings for enhanced biocompatibility and drug elution. |
| Polymer-Based Nanoporous Matrices (e.g., PLGA, PVP) [3] [43] | Biodegradable (e.g., PLGA) or non-degradable (e.g., PVP); can be engineered into reservoirs or monoliths. | Drug release via polymer degradation, erosion, or diffusion. Prevents burst release in matrix systems [43]. | Mainstay in current DES; used in matrix or reservoir systems for sirolimus, paclitaxel, etc. |
Quantitative Landscape and Clinical Impact
The controlled-release drug delivery market, a segment in which advanced DES are key players, is projected to grow from USD 66.93 billion in 2025 to USD 105.74 billion by 2030, reflecting a compound annual growth rate (CAGR) of 9.58% [45]. This growth is steered by the escalating burden of chronic diseases like coronary artery disease and the demonstrated clinical efficacy of advanced DES. Fourth-generation DES and bioresorbable vascular scaffolds (BVS) featuring nanoporous technologies have demonstrated remarkable clinical outcomes, including target lesion failure rates below 3% at one year and very late stent thrombosis rates declining to unprecedented lows (< 0.1% per year) [3].
Experimental Protocols
Protocol 1: Synthesis and Functionalization of Nanoporous Silica Coatings via Sol-Gel Method
Application: Creating a uniform, drug-loaded mesoporous silica coating on a nitinol stent substrate for controlled release of sirolimus.
Principle: The sol-gel method allows for the precise synthesis of nanoporous metal oxides at low temperatures, preserving the stability of the therapeutic drug [42]. The process involves the transition of a colloidal solution (sol) into a solid, porous network (gel) through hydrolysis and condensation reactions.
Materials:
- Stent substrate: Nitinol stent (bare metal or pre-coated with an adhesion layer).
- Silica precursor: Tetraethyl orthosilicate (TEOS).
- Structure-directing agent: Cetyltrimethylammonium bromide (CTAB).
- Solvent: Anhydrous ethanol and deionized water.
- Catalyst: Hydrochloric acid (HCl, 0.1M) or ammonium hydroxide (NHâ‚„OH, 25%).
- Therapeutic agent: Sirolimus.
- Functionalization agent: (3-Aminopropyl)triethoxysilane (APTES) and Polyethylene glycol (PEG)-succinimidyl ester.
Procedure:
- Sol Preparation: Dissolve 1.0 g of CTAB in a mixture of 50 mL ethanol and 10 mL deionized water. Stir vigorously at 35°C until fully dissolved.
- Precursor Addition: Slowly add 5 mL of TEOS dropwise to the stirring CTAB solution. Continue stirring for 2 hours to allow for partial hydrolysis and condensation.
- Drug Loading (One-Pot Method): Add 200 mg of sirolimus to the evolving sol. Stir for an additional 1 hour to allow for incorporation into the developing silica network.
- Dip-Coating: Immerse the clean nitinol stent into the prepared sol. Withdraw at a controlled, slow rate (e.g., 2 mm/s) to ensure a uniform coating layer.
- Aging and Drying: Allow the coated stent to age in a sealed container at room temperature for 24 hours to complete gelation. Subsequently, dry it in an oven at 60°C for 12 hours.
- Template Removal (Calcination): Place the dried stent in a furnace and heat to 350°C (below the drug degradation temperature) for 4 hours to remove the CTAB template, creating the mesoporous structure.
- Surface Functionalization:
- React the drug-loaded, porous stent with a 2% v/v solution of APTES in toluene for 4 hours to create amine-terminated surfaces.
- Rinse with toluene and ethanol.
- Submerge the stent in a 1 mg/mL solution of PEG-succinimidyl ester in PBS (pH 7.4) for 12 hours to conjugate PEG, enhancing biocompatibility and reducing immune detection [41] [42].
- Characterization: Characterize the coating using Scanning Electron Microscopy (SEM) for surface morphology, Atomic Force Microscopy (AFM) for surface roughness, and Fourier-Transform Infrared Spectroscopy (FTIR) to confirm chemical functionalization [44].
Protocol 2: In Vitro Drug Release Kinetics and Degradation Profiling
Application: Evaluating the release profile of sirolimus from a nanoporous-coated stent under simulated physiological conditions.
Principle: This protocol uses an accelerated release model to predict long-term (e.g., 28-day) drug release behavior in a shorter experimental timeframe, facilitating formulation development and quality control [6].
Materials:
- Test Article: Nanoporous silica-coated DES (from Protocol 1).
- Release Medium: Phosphate Buffered Saline (PBS, pH 7.4) with 0.5% w/w sodium dodecyl sulfate (SDS) to maintain sink conditions.
- Apparatus: USP Apparatus 4 (Flow-Through Cell) or custom-designed stent holder in a sealed vial incubator.
- Analytical Instrument: High-Performance Liquid Chromatography (HPLC) system with a C18 column and UV detector.
Procedure:
- Sample Preparation: Precisely measure the weight of the coated stent. Place the stent in a sealed vial containing 50 mL of pre-warmed (37°C) release medium.
- Incubation: Place the vials in an incubator shaker maintained at 37°C and agitate at 60 rpm.
- Sampling: At predetermined time intervals (e.g., 1, 4, 8, and 24 hours; then daily for 28 days), withdraw 1 mL of the release medium.
- Replenishment: Immediately replace the withdrawn volume with 1 mL of fresh, pre-warmed release medium to maintain a constant volume.
- Sample Analysis: Filter the withdrawn samples through a 0.45 μm membrane filter. Analyze the sirolimus concentration using the validated HPLC method.
- Data Analysis: Calculate the cumulative drug release and plot it against time. Fit the data to kinetic models (e.g., Higuchi, Korsmeyer-Peppas) to determine the underlying release mechanism.
- Coating Integrity Check: After the study period, retrieve the stent, rinse gently with water, dry, and analyze via SEM to observe any morphological changes or coating degradation.
Diagram 1: In vitro drug release kinetics workflow.
Protocol 3: Computational Modeling of Coating-Drug Interactions
Application: Using Density Functional Theory (DFT) to predict and optimize the interaction between a nanoporous alumina (α-Al₂O₃) coating, polymer modifiers, and an antiproliferative drug.
Principle: Molecular modeling provides insights into the chemical, physical, and biological properties of coating systems before synthesis, saving time and resources. It can calculate key parameters like Total Dipole Moment (TDM) and band gap energy, which correlate with coating stability and biological activity [44].
Materials:
- Software: GAUSSIAN 09 or similar computational chemistry software.
- Model Molecules: Digital models of α-Al₂O₃, polymers (e.g., PVDF, PVP), metal-organic frameworks (e.g., Zn-MOF), and the drug (e.g., Sirolimus).
Procedure:
- Model Building: Construct three-dimensional molecular models of the alumina substrate, coating polymers, and the drug molecule.
- Geometry Optimization: Perform initial geometry optimization of all individual molecules and their complexes to find the most stable configuration.
- DFT Calculation: Run DFT calculations at the B3LYP/LANL2DZ level of theory to study the interaction between the alumina substrate and the coating polymers, and subsequently between the functionalized substrate and the drug molecule.
- Parameter Calculation: Calculate key quantum chemical parameters from the results, including:
- Total Dipole Moment (TDM): Indicates the polarity of the system, influencing solubility and interaction with biological membranes.
- Band Gap Energy: The energy difference between the HOMO and LUMO; a lower band gap often suggests higher chemical reactivity and biological activity.
- Molecular Electrostatic Potential (MESP): Maps the charge distribution, predicting sites for electrophilic and nucleophilic attack [44].
- Validation: Correlate computational findings with experimental data from FTIR and XRD to validate the models.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Developing Nanoporous Stent Coatings
| Reagent/Material | Function/Application | Example Use-Case |
|---|---|---|
| Poly(Lactic-co-Glycolic Acid) (PLGA) [3] [43] | Biodegradable polymer for matrix/reservoir coatings. Degrades into lactic and glycolic acid, providing controlled drug release. | Used in bioresorbable polymer coatings for everolimus-eluting stents (e.g., Esprit BTK). |
| Polyvinylpyrrolidone (PVP) [44] [43] | Non-ionic, non-toxic polymer acting as a pore-former and hydrophilic modifier. Reduces biofouling and improves biocompatibility. | Component of hydrophilic coatings to reduce friction and control drug release; used in functionalizing NPAIMs. |
| Polyethylene Glycol (PEG) [41] [42] [43] | Polymer used for "PEGylation" of nanoparticle surfaces. Reduces immune recognition (stealth effect), prolongs circulation time, and enhances stability. | Conjugated to the surface of mesoporous silica nanoparticles to minimize opsonization and improve safety profile. |
| Lipid Nanoparticles (LNPs) [45] [46] | Advanced carrier system for nucleic acids and hydrophobic drugs. Composed of ionizable lipids, phospholipids, cholesterol, and PEG-lipids. | Emerging platform for delivering siRNA or mRNA to modulate vascular healing responses post-stenting. |
| Silica Nanoparticles (MSNs) [41] [42] | Inorganic, high-surface-area nanoporous carrier. Tunable pore size allows for high drug loading and controlled release. | Folic acid-modified MSNs can be used for targeted delivery of chemotherapeutics; explored for stent coatings. |
| Sirolimus (Rapamycin) & Everolimus [3] [26] | Antiproliferative drugs. Inhibit mTOR pathway, arresting smooth muscle cell cycle in G1 phase to prevent restenosis. | Primary therapeutic agents in the majority of modern limus-eluting stents and balloons. |
| Anodized Aluminum Oxide (AAO) [44] | Template with highly ordered, parallel nanopores. Used to create structured nanoporous membranes for fundamental release studies. | Serves as a model nanoporous membrane for studying diffusion kinetics of drugs like memantine in neural applications. |
| Ald-Ph-PEG12-TFP ester | Ald-Ph-PEG12-TFP ester, CAS:2055105-36-5, MF:C41H59F4NO16, MW:897.9 g/mol | Chemical Reagent |
| 3',5'-Dimethoxybiphenyl-3-ol | 3',5'-Dimethoxybiphenyl-3-ol, CAS:868666-20-0, MF:C14H14O3, MW:230.26 g/mol | Chemical Reagent |
Diagram 2: Drug action on restenosis pathway.
This document provides detailed application notes and experimental protocols for the evaluation of novel material approaches in drug-eluting stents (DES), specifically focusing on biomimetic polymers and bioresorbable scaffolds (BRS). These technologies represent the forefront of research aimed at overcoming the limitations of previous stent generations, such as permanent polymer-induced inflammation, delayed endothelial healing, and late stent thrombosis [3] [47]. The content is structured to provide translational scientists and development professionals with a framework for the in vitro and pre-clinical assessment of these advanced materials, including standardized methodologies and key analytical endpoints.
The following tables summarize the core characteristics, advantages, and challenges associated with these novel material classes, providing a structured comparison for research and development planning.
Table 1: Overview of Novel Stent Material Approaches
| Material Class | Core Function | Key Advantages | Primary Challenges |
|---|---|---|---|
| Biomimetic Polymers | Mimic the extracellular matrix to promote natural vascular healing while eluting drugs. | Promotes endothelial cell attachment; Reduces inflammatory response; Improves hemocompatibility. | Scalability of manufacturing; Long-term stability of biological motifs; Batch-to-batch reproducibility. |
| Bioresorbable Scaffolds (BRS) | Provide temporary vessel support and drug delivery, then fully resorb. | Restores vasomotion; Eliminates permanent implant risk; Reduces very late stent thrombosis. | Balancing radial strength with degradation profile; Managing early thrombotic risk; Thicker struts can limit deliverability. |
Table 2: Quantitative Performance of Select Material Systems
| Material System | Drug Release Profile | Key Preclinical/Clinical Findings | Degradation/Resorption Timeline |
|---|---|---|---|
| Poly-L-lactic Acid (PLLA) BRS [48] | Sustained release of Everolimus over months. | 5-year registry data shows MACE rates influenced by lesion complexity; No long-term difference in stent thrombosis vs. on-label use [48]. | Complete resorption typically in 24-36 months. |
| Polymer-Free Hybrid DES [37] | Probucol matrix for controlled Everolimus release. | Significantly lower neointimal growth at 90 days in porcine model; Near-complete endothelialization at 14 days [37]. | Not applicable (polymer-free). |
| Polyurethane-Silicone (PUS) Elastomer [9] | Controlled release of 5-FU; profile varies significantly with stent platform (12d to 150d). | Post-sterilization drug stability maintained; Comparable in vitro cytotoxicity to free drug against carcinoma cells [9]. | Biodurable (non-erodible). |
Experimental Protocols for Preclinical Assessment
Protocol: In Vitro Drug Release Kinetics
Objective: To quantify and model the drug release profile from a coated stent or scaffold under simulated physiological conditions.
Materials:
- Coated stent or scaffold specimen
- Phosphate Buffered Saline (PBS), pH 7.4, or other biorelevant dissolution media (e.g., with surfactants)
- Incubation shaker or USP Apparatus 4 (flow-through cell)
- HPLC system with validated analytical method
Methodology:
- Sample Immersion: Immerse the stent in a fixed volume of release medium (e.g., 50 mL PBS) and maintain at 37°C under gentle agitation.
- Sampling: At predetermined time points (e.g., 1h, 6h, 24h, 3d, 7d, 14d, 30d), withdraw and replace the entire release medium or an aliquot.
- Analysis: Quantify the drug concentration in the sampled medium using HPLC.
- Data Modeling: Plot cumulative drug release (%) versus time. Fit data to kinetic models (e.g., zero-order, first-order, Higuchi) to understand release mechanisms.
Technical Notes: The underlying stent structure (e.g., braided vs. woven) can significantly impact release kinetics, as observed with 5-fluorouracil release plateauing at 12 days for colonic stents versus a gradual release over 150 days for oesophageal stents [9]. Accelerated release conditions (e.g., elevated temperature, altered pH) may be developed to predict long-term release profiles for quality control purposes [6].
Protocol: In Vivo Porcine Model of Coronary Stenting
Objective: To evaluate the vascular healing response, efficacy, and safety of a novel stent/scaffold in a controlled pre-clinical model.
Materials:
- Juvenile domestic farm pigs (castrated males, ~3 months old)
- Test and control stent/scaffold systems
- Dual antiplatelet therapy (e.g., Clopidogrel, Aspirin)
- Standard interventional equipment (angiography suite, guide catheters, etc.)
- Histopathology processing supplies (MMA resin, H&E, VVG stain)
Methodology:
- Pre-Procedure: Administer a loading dose of antiplatelet drugs (e.g., Clopidogrel 75 mg, Aspirin 100 mg) at least two days prior to stenting [37].
- Stent Implantation: Under general anesthesia and angiographic guidance, implant stents in coronary arteries (LAD, LCx, RCA) with a target overstretch ratio of 1.1:1 relative to the reference vessel diameter [37].
- Follow-up and Endpoint Analysis:
- 14-Day Endpoint (Re-endothelialization): Use Scanning Electron Microscopy (SEM) on pressure-fixed, bisected vessels to quantify the percentage of strut coverage by endothelial cells [37].
- 28-/90-Day Endpoints (Efficacy & Safety): Perform quantitative coronary angiography (QCA) to measure late lumen loss. Process vessels for histomorphometry to measure neointimal area, % stenosis, and score for inflammation and fibrin deposition [37].
Technical Notes: The porcine model is the standard for coronary stent evaluation. Pathologists must be blinded to the treatment groups until after raw data collection is complete. The GABI-R registry highlights the importance of testing devices in complex, "off-label" scenarios (e.g., bifurcations, tortuous lesions) which are associated with higher early event rates [48].
Technology Workflow and Signaling Pathways
The following diagram illustrates the integrated research and development workflow for novel stent materials, from design to pre-clinical validation.
Diagram 1: Integrated R&D Workflow for Novel Stent Materials. This workflow outlines the critical stages from material synthesis to pre-clinical validation, highlighting key characterization and evaluation parameters at each stage [9] [6] [37].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for DES Coating Research
| Reagent / Material | Function / Role in Research | Example Application |
|---|---|---|
| Polyurethane-Silicone (PUS) Elastomer [9] | A biodurable, flexible polymer matrix for hydrophilic drug encapsulation. | Used as a basecoat reservoir for 5-fluorouracil in gastrointestinal stents [9]. |
| Poly(ethylene-co-vinyl acetate) (PEVA) [9] | A diffusion-regulating topcoat to control drug release rate from an underlying reservoir. | Applied as a topcoat over a PUS-5FU basecoat to achieve sustained release over 150 days [9]. |
| Poly-L-lactic Acid (PLLA) [48] | A biodegradable polymer forming the scaffold structure and controlling drug release. | Used as the backbone for bioresorbable vascular scaffolds (e.g., ABSORB BVS) eluting Everolimus [48]. |
| Probucol [37] | A non-polymeric excipient used to create a polymer-free drug matrix for controlled release. | Serves as a carrier for Everolimus in a polymer-free DES, demonstrating improved vascular healing in pre-clinical models [37]. |
| Exosome-Mimetic Nanovesicles (EMNVs) [47] | Biologically inspired vesicles for targeted delivery of therapeutic cargo (e.g., microRNA). | Coated on stents to promote endothelial regeneration and modulate inflammation; a next-generation approach in preclinical development [47]. |
| Tetramethylammonium acetate hydrate | Tetramethylammonium acetate hydrate, CAS:1266615-86-4, MF:C6H17NO3, MW:151.20 | Chemical Reagent |
| Fmoc-N-amido-PEG3-azide | Fmoc-N-amido-PEG3-azide, CAS:1172605-58-1, MF:C23H28N4O5, MW:440.5 g/mol | Chemical Reagent |
Technical and Regulatory Considerations
- Sterilization: Terminal sterilization is a critical step. Ethylene oxide (EtO) is commonly used, but regulatory scrutiny on emissions requires careful management. Gamma radiation is an alternative, and research shows certain 5-FU polymer coatings remain stable after gamma sterilization [9] [6].
- Stability Testing: While specific regulatory guidance for DES stability is evolving, it is recommended to follow ICH Q1 guidelines. Studies must assess the impact of storage on drug potency, polymer integrity, coating morphology, and mechanical performance of the stent [6].
- Coating Process Challenges: Achieving a uniform, defect-free coating is paramount. Techniques like spray coating are industry-preferred for productivity. Key challenges include controlling thickness, avoiding webbing between stent struts, and ensuring adequate adhesion during stent expansion [6].
The development of biomimetic polymers and bioresorbable scaffolds is paving the way for a new generation of stents that actively promote healing and ultimately disappear, thereby mitigating long-term complications. The protocols and data presented herein provide a foundational framework for the systematic and standardized evaluation of these promising technologies. Future directions will involve the clinical translation of advanced concepts, including biologically active EMNV coatings [47], smart stents with sensing capabilities [3], and personalized approaches leveraging 3D printing [49].
Advanced drug-eluting stents (DES) have evolved from single-agent delivery to sophisticated multi-drug elution platforms that release combinations of therapeutic agents in a temporally coordinated manner to optimize vessel healing [3]. These systems represent a paradigm shift in interventional cardiology, moving beyond the singular focus on inhibiting smooth muscle cell proliferation to embrace a more holistic approach that addresses the multiple biological pathways involved in the vascular response to stent implantation.
The core innovation lies in the precise engineering of release kinetics to deliver different drugs during specific phases of the healing process. This sequential targeting aligns therapeutic intervention with the natural chronology of vascular pathophysiology: initially combating early inflammatory responses, followed by sustained release to prevent late neointimal proliferation, while simultaneously promoting endothelial recovery [3]. The development of these platforms requires interdisciplinary integration of biomaterial science, pharmaceutical kinetics, and vascular biology to create systems that can navigate the complex biological environment following percutaneous coronary intervention (PCI).
Current Technology Landscape
Advanced Platform Architectures
Contemporary multi-drug elution platforms employ several sophisticated architectural strategies to achieve coordinated drug release:
Gradient-release polymer systems provide variable drug release rates tailored to the temporal needs of the healing vessel wall [3]. These systems utilize polymer matrices with engineered diffusion properties or layered constructions that release higher initial drug concentrations to address the acute inflammatory phase, followed by sustained release profiles to manage the proliferative phase of healing.
Biomimetic polymers represent another innovative approach, where the polymer structure mimics the natural extracellular matrix to promote endothelial cell attachment and proliferation while simultaneously delivering antiproliferative agents to smooth muscle cells [3]. This architecture achieves the delicate balance between inhibiting restenosis and promoting re-endothelialization, addressing a fundamental challenge in stent design.
Nanoporous surface technologies create microscopic reservoirs within the stent surface, enabling polymer-free drug delivery with precisely controlled elution kinetics [3]. These platforms can be engineered to house multiple drugs in separate reservoirs with distinct release profiles, eliminating concerns about polymer-induced chronic inflammation while offering exceptional control over release timing.
Table 1: Multi-Drug Elution Platform Architectures and Characteristics
| Platform Architecture | Mechanism of Action | Therapeutic Advantages | Technical Challenges |
|---|---|---|---|
| Gradient-release polymers | Variable drug release rates via engineered diffusion | Matches drug delivery to healing chronology | Complex manufacturing and quality control |
| Biomimetic polymers | Mimics extracellular matrix for cell attachment | Promotes endothelialization while inhibiting SMC proliferation | Balancing competing biological responses |
| Nanoporous surfaces | Polymer-free micro-reservoirs with controlled elution | Eliminates polymer inflammation concerns | Drug loading capacity limitations |
| Bioresorbable scaffolds | Temporary mechanical support with drug elution | Eliminates permanent implant, restores vasomotion | Maintaining radial strength during resorption |
Therapeutic Agent Combinations
The strategic selection of drug combinations targets complementary pathological processes:
Antiproliferative + Anti-inflammatory Agents: This combination addresses both the excessive smooth muscle cell proliferation that leads to restenosis and the underlying inflammatory drivers that potentiate this process [3] [50]. The anti-inflammatory component moderates the initial injury response, while antiproliferative agents prevent the subsequent hyperplastic reaction.
Antiproliferative + Pro-healing Agents: This approach inhibits pathological restructuring while actively promoting endothelial recovery [3]. The pro-healing component accelerates the formation of a functional endothelial layer, which provides natural protection against restenosis and thrombosis, potentially reducing the duration of required dual antiplatelet therapy.
Multi-specific Bioactive Cocktails: Emerging platforms incorporate three or more agents that target distinct pathways—inflammation, proliferation, and impaired healing—simultaneously [3]. These sophisticated systems represent the cutting edge of multi-drug elution technology, requiring exceptionally precise control over release kinetics and drug compatibility.
Quantitative Release Kinetics and Modeling
Experimental Release Profiles
Characterizing multi-drug release kinetics requires sophisticated analytical methodologies that can discriminate between multiple agents simultaneously. High-performance liquid chromatography (HPLC) with gradient protocols and multiple wavelength detection enables precise quantification of individual drug concentrations in complex mixtures [51]. For example, researchers have successfully monitored four different drugs—metronidazole, ketoprofen, doxycycline, and simvastatin—released from multilayered association polymer systems using mobile phase gradients and specific UV detection wavelengths [51].
The translation from in vitro to in vivo release profiles presents significant challenges. Comparative studies have demonstrated that while sequential release of multiple drugs can be maintained following implantation, release rates often differ substantially between controlled laboratory conditions and physiological environments [51]. Specifically, drugs may initially release more quickly in vivo due to enzymatic activity and cellular interactions, then subsequently release more slowly as the tissue response creates additional diffusion barriers.
Table 2: Mathematical Models for Analyzing Multi-Drug Release Kinetics
| Model Name | Model Type | Governing Equation | Application in Multi-Drug Systems |
|---|---|---|---|
| Higuchi Model | Physical (Diffusion-based) | ( Q = k_H \cdot \sqrt{t} ) | Analysis of individual drug release from monolithic systems |
| Korsmeyer-Peppas | Semi-empirical | ( \frac{Mt}{M\infty} = k \cdot t^n ) | Mechanism determination (diffusion, erosion) for each drug |
| Hopfenberg Model | Physical (Erosion-based) | ( \frac{Mt}{M\infty} = 1 - \left(1 - k \cdot t\right)^n ) | Systems with significant erosion components |
| Weibull Function | Empirical | ( \frac{Mt}{M\infty} = 1 - \exp\left(-a \cdot t^b\right) ) | Comparison of release profiles between different drugs |
Mathematical Modeling Approaches
Mathematical models are indispensable tools for designing and optimizing multi-drug elution systems, enabling researchers to predict release behavior and decipher the underlying physical mechanisms [52]. These models range from physically-based approaches that describe specific release mechanisms (diffusion, erosion, swelling) to empirical models that provide robust fitting of experimental data without mechanistic assumptions.
For complex multi-drug systems, model superposition is often employed, where the release profile of each drug is described by an appropriate individual model, and interactions between drugs are accounted for through coupling terms [52]. This approach allows researchers to simulate scenarios such as competitive diffusion or carrier material modifications induced by one drug that affect the release of another.
The selection of an appropriate model depends critically on the carrier geometry, material properties, and the dominant release mechanisms [52]. No universal model exists that can accurately predict all multi-drug release scenarios, necessitating careful mechanistic analysis for each new system design.
Experimental Protocols
In Vitro Release Kinetics Assessment
Objective: To quantitatively characterize the coordinated release profiles of multiple therapeutic agents from advanced stent platforms under simulated physiological conditions.
Materials:
- Coated stent samples (multiple replicates, typically n≥6)
- Phosphate-buffered saline (PBS), pH 7.4 ± 0.1, with 0.02% sodium azide
- Temperature-controlled shaking incubator (37°C ± 0.5°C)
- HPLC system with:
- Kinetix C18 column or equivalent
- Diode array detector (190-400 nm)
- Gradient pump system
- Drug standards (≥98% purity) for calibration
- Membrane filters (0.45 μm)
Procedure:
- Sample Preparation: Accurately measure and record the dimensions and coating weight of each stent sample. Place individual stents in sterile containers with precise volume of release medium (typically 5-10 mL).
Release Study Setup: Incubate samples at 37°C with gentle horizontal shaking (60-70 rpm). Maintain sink conditions throughout the study.
Sampling Protocol: At predetermined time intervals (1, 4, 8, 24 hours initially, then less frequently), completely withdraw and replace the release medium.
Sample Analysis:
- Filter withdrawn samples through 0.45 μm membrane
- Analyze using validated HPLC methods with wavelength switching:
- Metronidazole: 318 nm detection with gradient elution (100% 0.1% TFA to 70:30 0.1% TFA:ACN over 3 min)
- Doxycycline: 350 nm detection with same gradient
- Ketoprofen: 260 nm detection with isocratic elution (60% ACN, 40% 0.1% TFA)
- Simvastatin: 240 nm detection with isocratic elution (70% ACN, 30% 0.1% TFA) [51]
Data Processing: Calculate cumulative drug release using standard curves and normalize to total drug content.
Quality Control: Include system suitability tests with each analysis batch. Assess precision (RSD <2%), accuracy (85-115%), and specificity for each analyte.
In Vivo Translation Validation
Objective: To evaluate the correlation between in vitro release profiles and in vivo performance of multi-drug eluting systems.
Animal Model: Male Sprague-Dawley rats (6-8 weeks) are commonly used for initial in vivo assessments [51].
Surgical Implantation:
- Anesthetize animals and perform aseptic surgical preparation.
- Make transverse incision between ears and gently elevate periosteum to expose calvaria.
- Implant multi-drug devices with drug-releasing side facing bone surface.
- Sutured close incision and monitor recovery.
Device Retrieval and Analysis:
- Euthanize animals at predetermined time points (e.g., 1, 3, 6, 9, 12, 18 days).
- Carefully explant devices, removing adherent tissue without disturbing drug layers.
- Cross-section devices for morphological analysis of remaining structure.
- Measure residual mass and thickness of remaining carrier layers.
- Completely dissolve remaining device in PBS, filter, and analyze drug content by HPLC.
- Construct in vivo release profiles by measuring drugs remaining in retrieved devices.
Data Correlation: Compare in vivo and in vitro release profiles to establish predictive relationships. Note that sequential release patterns observed in vitro are generally maintained in vivo, though absolute rates often differ [51].
Research Reagent Solutions
Table 3: Essential Research Reagents for Multi-Drug Elution Studies
| Reagent/Category | Specific Examples | Research Function | Technical Considerations |
|---|---|---|---|
| Biocompatible Polymers | PLGA, PCL, PDLLA-PCL, cellulose acetate phthalate-Pluronic F127 | Form drug carrier matrix; control release kinetics | Degradation rate, drug compatibility, processing requirements |
| Therapeutic Agents | Sirolimus, everolimus, zotarolimus, paclitaxel, anti-inflammatories | Biological activity; inhibition of restenosis and promotion of healing | Solubility, stability, therapeutic window, compatibility |
| Analytical Standards | Drug reference standards (≥98% purity), deuterated internal standards | HPLC/LC-MS quantification; method validation | Storage conditions, stability, purity verification |
| Cell Culture Models | hBMECs, hBVPs, hASTROs, VSMCs | Biocompatibility assessment; cellular uptake studies | Passage number, culture conditions, phenotypic validation |
| Nanoparticle Systems | PLGA NPs, albumin-based NPs (BSA, HSA), nanolipid carriers | Targeted delivery; enhanced cellular uptake | Size distribution, surface charge, drug loading efficiency |
Pathway Visualization and Experimental Workflows
Diagram 1: Multi-Drug Elution Platform Development Workflow. This flowchart outlines the comprehensive development pathway from initial design through in vitro characterization to in vivo validation and optimization.
Multi-drug elution platforms represent a transformative advancement in stent technology, moving beyond single-mechanism approaches to address the complex, multifactorial process of vascular healing following stent implantation. The coordinated release of multiple therapeutic agents—timed to match the chronological progression of the healing response—offers unprecedented opportunities to improve clinical outcomes by simultaneously inhibiting pathological processes while promoting physiological recovery.
Future developments in this field will likely focus on increasingly sophisticated personalized approaches, where stent platforms are tailored to individual patient characteristics such as diabetes status, inflammatory biomarkers, and genetic profiles [3]. Additionally, the integration of sensing technologies within stent platforms could enable real-time monitoring of vascular healing, creating responsive systems that adapt therapeutic delivery based on actual tissue response rather than predetermined release profiles [3].
As these advanced platforms progress through preclinical development toward clinical application, rigorous assessment of drug interactions, long-term safety, and manufacturing reproducibility will be essential. The successful translation of multi-drug elution platforms promises to usher in a new era of precision interventional cardiology, fundamentally enhancing the management of coronary artery disease.
Addressing DES Challenges: Thrombosis, Restenosis and Coating Optimization
Stent thrombosis (ST) remains one of the most devastating complications following percutaneous coronary intervention (PCI), characterized by the sudden occlusion of a stented coronary artery due to thrombus formation [53]. Despite advancements in drug-eluting stent (DES) technology and optimized pharmacotherapy, ST continues to be associated with substantial morbidity and mortality [54] [55]. Contemporary registry data indicate that definite or probable ST occurs in approximately 0.5% of PCI cases, with a 30-day mortality rate approaching 25% and long-term mortality risk exceeding 30% at 10 years [54] [55]. The clinical consequences typically include myocardial infarction, emergent revascularization, and heightened cardiovascular risk, necessitating timely recognition and intervention [54].
The pathogenesis of ST is multifactorial, involving complex interactions between patient-specific factors, procedural characteristics, lesion morphology, and stent-related technological aspects [54] [53]. This application note provides a comprehensive framework for researchers and drug development professionals, detailing the mechanisms, risk stratification, experimental methodologies, and mitigation strategies for stent thrombosis within the broader context of drug-eluting stent coating and application techniques research.
Pathophysiological Mechanisms and Risk Factor Classification
Stent thrombosis represents a critical failure of the vascular healing process following stent implantation. The pathophysiology involves the triad of endothelial injury, altered blood flow, and hypercoagulability, often referred to as Virchow's triad in the context of vascular devices [53].
Temporal Classification and Prevalence
The Academic Research Consortium classifies ST based on timing post-implantation [56]:
Table 1: Temporal Classification of Stent Thrombosis
| Classification | Timeframe | Prevalence | Primary Mechanisms |
|---|---|---|---|
| Acute | 0-24 hours | 0.5-4% | Procedural factors; platelet activation |
| Subacute | 24 hours to 30 days | 5.3-15% | Delayed endothelialization; inadequate antiplatelet therapy |
| Late | 31 days to 1 year | 6-28.6% | Delayed healing; persistent inflammation |
| Very Late | >1 year | 35.4-75% | Hypersensitivity reactions; neoatherosclerosis; malapposition |
Data from multiple registries show variability in ST prevalence based on timing, with subacute and very late ST being most frequently observed [54] [55]. The PRESTIGE registry, utilizing optical coherence tomography (OCT), found the prevalence of acute/subacute, late, and very late ST to be 6.1%, 28.6%, and 71.4%, respectively [54].
Comprehensive Risk Factor Stratification
Risk factors for ST span patient characteristics, procedural variables, lesion complexity, and stent technology factors [54] [55] [53].
Table 2: Comprehensive Risk Factors for Stent Thrombosis
| Risk Category | Specific Factors | Risk Magnitude/Association |
|---|---|---|
| Patient Factors | Advanced age, female sex, smoking, diabetes, chronic kidney disease, obesity, premature antiplatelet discontinuation | 2-fold increase with obesity; 45% case fatality rate with antiplatelet discontinuation |
| Procedural Factors | Stent under-expansion, malapposition, edge dissections, residual thrombus, longer stent length | Stent length >30-36mm associated with increased risk |
| Lesion Characteristics | Bifurcation lesions, calcified lesions, chronic total occlusions, in-stent restenosis, small vessel diameter <2.5mm | Bifurcation lesions associated with 1.5-2× increased risk |
| Stent Technology | Polymer biocompatibility, strut thickness, drug type, coating integrity, hypersensitivity reactions | First-generation DES associated with higher late ST rates |
Experimental Protocols for Thrombogenicity Assessment
Intravascular Imaging Protocol for Mechanism Elucidation
Intravascular ultrasound (IVUS) and optical coherence tomography (OCT) provide critical insights into ST mechanisms and should be employed according to standardized protocols [56].
Protocol: Multimodal Intravascular Assessment of Stent Thrombosis
Pre-procedural Setup
- Administer intracoronary nitroglycerin (100-200μg) to minimize vasospasm
- Calibrate imaging systems according to manufacturer specifications
- Prepare automated pullback device with standardized speed (0.5mm/s for OCT; 1.0mm/s for IVUS)
Image Acquisition
- Position imaging catheter distal to the stent segment (>5mm beyond distal edge)
- Initiate automated pullback through the entire stent length and 5-10mm proximal and distal reference segments
- Record continuous imaging with particular attention to:
- Stent-vessel wall apposition (distance between strut and vessel wall >200μm indicates malapposition)
- Stent expansion (minimum stent area <5.0mm² or <90% of reference lumen area indicates under-expansion)
- Thrombus identification (echolucent masses in IVUS; high-attenuation, irregular masses in OCT)
Quantitative Analysis
- Measure minimum and maximum stent diameters
- Calculate symmetry index (minimum diameter/maximum diameter)
- Assess reference vessel dimensions at proximal and distal edges
- Document presence of tissue prolapse, dissections, or uncovered struts
Qualitative Assessment
- Characterize thrombus morphology (white/red based on OCT signal intensity)
- Evaluate neointimal coverage (heterogeneous vs. homogeneous patterns)
- Identify signs of neoatherosclerosis (lipid-laden neointima, calcification, thin-cap fibroatheroma)
This protocol was utilized in a case study of recurrent subacute ST, where IVUS examination revealed 81.3% stenosis within the stent, with low-intensity echoes suggestive of thrombus distinct from the homogeneous hypoechoic appearance of neointimal hyperplasia [56].
In Vitro Drug Release Kinetics Assessment
Understanding drug release profiles from DES is critical for predicting clinical performance and potential thrombotic risk [6].
Protocol: Accelerated and Real-Time Drug Release Testing
Apparatus Setup
- USP Apparatus 7 (reciprocating holder) with specially designed stent holders
- Dissolution vessels maintained at 37°C ± 0.5°C
- Phosphate buffered saline (PBS, pH 7.4) with 0.05% polysorbate 80 as dissolution medium
- Sampling points: 1, 3, 6, 24, 48, 72 hours, then weekly until 90 days
Accelerated Release Conditions
- Elevated temperature (45°C) with appropriate stability validation
- Agitation rate: 30 dips per minute
- Medium: PBS with 20% ethanol or alternative hydro-organic solvent
- Sampling points: 1, 2, 4, 8, 12, 24, 48, 72 hours
Analytical Methodology
- High-performance liquid chromatography (HPLC) with UV detection
- Validation for specificity, linearity, accuracy, and precision
- Calculation of cumulative drug release and release kinetics (Higuchi, Korsmeyer-Peppas models)
Coating Integrity Assessment
- Scanning electron microscopy (SEM) pre- and post-release testing
- Assessment of coating defects, cracking, delamination
- Energy-dispersive X-ray spectroscopy (EDS) for elemental analysis
This methodology allows researchers to establish in vitro-in vivo correlation (IVIVC), which is essential for using in vitro release data as a surrogate for in vivo behavior and reducing clinical studies needed for product development [6].
Technological Mitigation Strategies
Advanced Stent Coating Technologies
Next-generation DES platforms incorporate sophisticated coating technologies to reduce thrombogenicity while maintaining anti-restenotic efficacy [3] [43].
Polymer-Based Coating Systems:
- Bioresorbable polymers with programmable degradation: Unlike earlier biodegradable polymers, these advanced materials can be programmed to degrade at specific rates based on individual patient characteristics and lesion complexity [3].
- Biomimetic polymers: These polymers mimic the extracellular matrix, promoting endothelial cell attachment and proliferation while simultaneously delivering antiproliferative agents [3].
- Nanoporous surface technologies: These create microscopic reservoirs within the stent surface, allowing for polymer-free drug delivery with precisely controlled elution kinetics [3].
Drug Delivery Mechanisms:
- Gradient-release polymers: These sophisticated systems provide variable drug release rates tailored to the temporal needs of the healing vessel wall [3].
- Targeted drug delivery systems: Utilizing antibody-conjugated nanoparticles, these systems selectively deliver antiproliferative agents to proliferating smooth muscle cells while sparing endothelial cells [3].
- Multi-drug elution platforms: These advanced systems release combinations of antiproliferative, anti-inflammatory, and pro-healing agents in a temporally coordinated manner [3].
Alternative Technologies: Drug-Eluting Balloons
Drug-eluting balloons (DEBs) represent a metal-free alternative for treating in-stent restenosis, potentially reducing thrombotic risk associated with multiple stent layers [26].
The SELUTION4ISR Trial demonstrated that a sirolimus-eluting balloon performed similarly to standard care (new DES implantation or plain balloon angioplasty) with target lesion failure rates of 16.2% versus 13.5% at one year, a difference that was not statistically significant [26]. This technology is particularly valuable for patients who already have multiple stent layers, where adding more metal may increase risk or complicate future procedures.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Stent Thrombosis Investigation
| Reagent/Material | Function/Application | Technical Specifications |
|---|---|---|
| Polymer Coating Materials | Drug encapsulation and controlled release | PVP, PEG, PLGA, PCL; biocompatible and biodegradable formulations |
| Antiproliferative Drugs | Inhibition of smooth muscle cell proliferation | Sirolimus, everolimus, zotarolimus, paclitaxel; typically 1-10μg/mm stent length |
| Platelet Reactivity Assays | Assessment of antiplatelet therapy efficacy | VerifyNow, VASP phosphorylation, light transmission aggregometry |
| Intravascular Imaging Catheters | In vivo assessment of stent deployment and healing | OCT (10-15μm axial resolution), IVUS (100-150μm axial resolution) |
| Endothelial Cell Cultures | In vitro assessment of endothelialization capacity | Human coronary artery endothelial cells (HCAECs); flow chamber systems |
| Thrombogenicity Assays | In vitro assessment of thrombus formation | Chandler loop system, hemodynamic shearing devices |
| Sterilization Systems | Terminal sterilization of coated devices | Ethylene oxide (EtO) sterilization; validated cycles for polymer-coated devices |
Stent thrombosis remains a complex, multifactorial complication of PCI with significant clinical implications. Understanding the mechanisms—from patient-specific factors to stent technology limitations—provides a framework for developing targeted mitigation strategies. Contemporary approaches focus on enhancing stent coating biocompatibility, optimizing drug release kinetics, and utilizing intravascular imaging for procedural guidance.
Future research directions include genetically engineered endothelial progenitor cell capture stents, smart stents with sensing capabilities, and 3D-printed personalized stents tailored to individual patient anatomy [3]. Additionally, the development of sophisticated in vitro testing models that better recapitulate in vivo conditions will be crucial for advancing the field and improving patient outcomes.
For researchers and drug development professionals, a comprehensive approach integrating material science, pharmaceutical technology, and clinical insight is essential for developing next-generation solutions to the challenge of stent thrombosis.
In-stent restenosis (ISR), the re-narrowing of a stented coronary artery segment, remains a significant challenge in interventional cardiology despite advancements in stent technology. It is the most common cause of stent failure after percutaneous coronary intervention (PCI), accounting for 5-10% of all PCI procedures in contemporary practice [57]. While the introduction of drug-eluting stents (DES) has reduced the first-year incidence of ISR from 20-30% in the bare-metal stent era to 5-10%, this complication continues to drive repeat revascularization procedures and can present as acute myocardial infarction in approximately 25% of cases [58] [59].
ISR represents a complex pathological process influenced by patient-specific biological factors, lesion characteristics, and procedural elements. Understanding the multifaceted mechanisms underlying ISR is crucial for developing advanced coating technologies that can mitigate this complication. This application note provides a comprehensive analysis of ISR pathophysiology and details cutting-edge coating solutions and evaluation protocols for researchers and drug development professionals working in cardiovascular device innovation.
Biological Mechanisms of In-Stent Restenosis
Pathophysiological Classification
In-stent restenosis manifests through distinct pathological processes that have important implications for treatment strategy and prognosis. The current classification integrates angiographic morphology, tissue composition characteristics, and imaging biomarkers to guide clinical decision-making [58] [59].
Table 1: Classification Systems for In-Stent Restenosis
| Classification Basis | Type | Definition and Features | Clinical Implications |
|---|---|---|---|
| Angiographic Classification | Type I: Focal | Stenosis confined within stent or margins (length ≤10 mm) | Best prognosis; drug-coated balloon efficacy >90% |
| Type II: Diffuse | Stenosis extending beyond focal margins but confined within stent (length >10 mm) | Requires intravascular imaging assessment; DCB or new stent implantation | |
| Type III: Proliferative | Diffuse stenosis extending beyond stent borders (length >10 mm) | High restenosis risk; often requires atherectomy + new stent | |
| Type IV: Total Occlusion | 100% stent occlusion | Worst prognosis; requires mechanical recanalization or bypass surgery | |
| Histopathological Classification | Neointimal Hyperplasia | Dominant smooth muscle cell proliferation with low lipid content | Responsive to antiproliferative agents (e.g., paclitaxel) |
| Neoatherosclerosis | Foam cell/cholesterol crystal accumulation with thin-cap or calcification | High late thrombosis risk; requires intensive lipid-lowering + anti-inflammatory therapy | |
| Intravascular Imaging Classification | Calcified Pattern | Calcium arc >180° on OCT or calcium thickness >0.5 mm on IVUS | Requires plaque modification (atherectomy/shockwave balloon) |
| Stent Underexpansion | Minimal stent area (MSA) <4.5 mm² or expansion ratio <80% | Post-dilation optimization critical | |
| Stent Fracture | Discontinuity of stent struts on IVUS/OCT | Requires bioresorbable scaffold or surgical intervention |
The mechanisms of ISR differ significantly between bare-metal stents and drug-eluting stents. While neointimal hyperplasia dominates in BMS-ISR, DES-ISR more frequently involves neoatherosclerosis—an accelerated form of atherosclerosis characterized by lipid-laden foamy macrophage accumulation within the neointima, potentially with necrotic core formation and/or calcification [57]. The time course also varies, with BMS-ISR typically peaking within the first 6 months post-implantation, while DES-ISR incidence continues to increase steadily for several years [57].
Key Biological Processes
Neointimal Hyperplasia
Neointimal hyperplasia represents the core pathophysiological mechanism of ISR, characterized by the accumulation of smooth muscle cells and extracellular matrix in the intimal layer [58]. This process initiates with endothelial injury during stent implantation, triggering a cascade of biological responses including platelet activation, inflammatory cell recruitment, and release of growth factors and cytokines that stimulate smooth muscle cell migration from the tunica media to the intima [6].
The complex interplay between cytokines, growth factors, and cellular elements creates a self-perpetuating cycle of vascular inflammation and remodeling. Key mediators include platelet-derived growth factor (PDGF), transforming growth factor beta (TGFβ), insulin-like growth factor (IGF), fibroblast growth factor (FGF), vascular endothelial growth factor (VEGF), thrombin, angiotensin II (ATII), interleukin-1 (IL1), IL-6, IL-8, TNF-α, interferon gamma (INFγ), and monocyte chemoattractant protein-1 (MCP-1) [6].
Diagram 1: Neointimal Hyperplasia Pathway (100 chars)
Neoatherosclerosis
Neoatherosclerosis represents a distinct pathological entity characterized by accelerated atheroma formation within the stented segment. Histologically, it features accumulation of lipid-rich foamy macrophages within the neointima, with or without necrotic core formation and/or calcification [58] [57]. Unlike native coronary atherosclerosis which develops over decades, neoatherosclerosis can manifest months to years after PCI [58].
The pathogenesis involves stent-induced vascular injury and endothelial dysfunction, leading to inflammatory cell activation, increased thrombogenicity, and reduced β-lipoprotein efflux followed by lipoprotein accumulation within the neointima. Immature endothelial cells with increased permeability further promote monocyte migration, while underlying native atherosclerotic plaques may contribute to the pathogenesis [58].
Patient-Related Risk Factors
Several patient-specific factors significantly influence ISR risk through effects on the vascular biological response:
Diabetes Mellitus: Diabetes represents an important independent risk factor for ISR. The hyperglycemic environment promotes coronary artery smooth muscle cell proliferation and migration, while endothelial dysfunction accelerates atherosclerosis [58] [59]. A recent large-scale Swedish cohort study demonstrated that poor glycemic control (HbA1c ≥10.1%) increases stent failure risk by 33% compared to patients with HbA1c of 6.1-7.0% [58]. Diabetes also modulates inflammatory cytokine expression, with upregulation of pro-inflammatory factors (IL-6, TNF-α) that exacerbate vascular wall inflammation and promote restenosis [58].
Chronic Kidney Disease (CKD): The incidence of ISR in CKD patients is significantly elevated compared to individuals with normal renal function, attributed to systemic inflammatory responses and vascular calcification associated with CKD [58] [59]. A retrospective Chinese study identified CHAâ‚‚DSâ‚‚-VASc score, fibrinogen levels, and neutrophil-to-lymphocyte ratio as independent predictors of ISR in CKD patients, with combined predictive power reaching an AUC of 0.797 [58].
Smoking: Tobacco use activates oxidative stress and inflammatory responses, inducing a pro-inflammatory microenvironment in the arterial intima with significantly increased inflammatory mediator levels. These changes accelerate neointimal hyperplasia while promoting platelet activation and fibrin deposition, increasing thrombosis tendency and impairing vessel repair capacity [58] [59].
Genetic Factors and Drug Tolerance: Some patients exhibit high on-treatment platelet reactivity after antiplatelet therapy, reducing clinical efficacy and increasing ISR risk. This phenomenon relates to genetic factors, particularly polymorphisms of the P2Y12 receptor gene, which limit postoperative antiplatelet treatment options and may increase ISR risk by affecting platelet inhibition effectiveness [58] [59].
Advanced Coating Solutions for ISR Mitigation
Evolution of Drug-Eluting Stent Coatings
Stent coating technology has evolved significantly through multiple generations to address the competing challenges of preventing restenosis while minimizing adverse effects:
First-generation DES: Utilized non-degradable synthetic polymers (e.g., SIBS for paclitaxel delivery) with sirolimus or paclitaxel as antiproliferative agents. While effective at reducing restenosis, these stents raised concerns about late stent thrombosis associated with delayed endothelialization and polymer-induced hypersensitivity reactions [3] [6].
Second-generation DES: Incorporated more biocompatible polymers and alternative antiproliferative agents (everolimus, zotarolimus), leading to enhanced safety profiles and reduced very late stent thrombosis rates [3].
Third-generation DES: Featured biodegradable polymer DES that provided antiproliferative benefits during the critical period of neointimal hyperplasia while eliminating long-term polymer presence once their function was complete [3].
Fourth-generation technologies: Characterized by polymer-free designs, bioresorbable scaffolds, and nanotechnology-enhanced drug delivery systems that promote natural vessel healing, restore vasomotion, and eliminate permanent metallic implants [3] [60].
Table 2: Advanced Coating Technologies in Drug-Eluting Stents
| Technology Platform | Key Features | Advantages | Representative Examples |
|---|---|---|---|
| Advanced Polymer Technologies | Gradient-release polymers with variable drug release rates | Tailored elution kinetics matching temporal healing needs | Biolinx polymer (Endeavor Resolute) [3] [61] |
| Bioresorbable polymers with programmable degradation | Elimination of long-term polymer presence; reduced inflammation | Poly(L-lactide) based polymers [3] | |
| Biomimetic polymers mimicking extracellular matrix | Promotion of endothelial cell attachment and proliferation | Phosphorylcholine-based coatings [3] [61] | |
| Novel Drug Delivery Mechanisms | Nanoporous surface technologies | Polymer-free drug delivery with controlled elution kinetics | Micell Technologies [3] [6] |
| Targeted drug delivery systems | Selective delivery to proliferating smooth muscle cells | Antibody-conjugated nanoparticles [3] | |
| Multi-drug elution platforms | Coordinated release of antiproliferative, anti-inflammatory, and pro-healing agents | Combination therapy stents [3] | |
| Bioresorbable Vascular Scaffolds | Hybrid metal-polymer scaffolds | Combined mechanical strength with complete resorption | Next-generation BVS [3] |
| Thin-strut BVS (<70 μm) | Reduced flow disturbances and inflammatory responses | Ultra-thin strut designs [3] | |
| Accelerated resorption profiles (12-18 months) | Reduced window of vulnerability for device-related complications | Improved resorption kinetics [3] |
Coating Composition and Characterization
Coating Materials
DES coatings typically consist of three key components: the active pharmaceutical ingredient, a polymeric carrier (or alternative drug reservoir), and the metallic stent platform [9]. The coating composition must balance multiple requirements including drug loading capacity, controlled release kinetics, and biocompatibility.
Polymer Systems:
- Durable Polymers: Early DES utilized non-degradable synthetic polymers such as styrene-b-isobutylene-b-styrene (SIBS) for Taxus Liberté, phosphorylcholine for Endeavor Sprint, and fluoropolymer for Xience V [61]. While effective for drug delivery, these persistent polymers can provoke hypersensitivity reactions, local tissue inflammation, late-stage thrombosis, and delayed vascular healing [6].
Biodegradable Polymers: Materials such as poly(L-lactide) degrade into non-toxic products after completing their drug delivery function, eliminating long-term foreign body response. These include MiStent SES (Micell Technologies), Supralimus and Supraflex (Sahajanand Medical Technologies) [6].
Biomimetic Polymers: Newer systems mimic the extracellular matrix to promote endothelial cell attachment and proliferation while delivering antiproliferative agents to smooth muscle cells, achieving the delicate balance between inhibiting restenosis and promoting endothelialization [3].
Active Pharmaceutical Ingredients:
- Antiproliferative Agents: Sirolimus and its analogs (everolimus, zotarolimus) arrest smooth muscle and endothelial cells in the G0/G1 phase of the cell cycle without causing apoptosis. Paclitaxel operates through a different mechanism, blocking the microtubular system and inducing apoptosis at low concentrations [6].
- Combination Therapies: Emerging approaches utilize multi-drug elution platforms that release combinations of antiproliferative, anti-inflammatory, and pro-healing agents in a temporally coordinated manner to optimize vessel healing [3].
Coating Application Techniques
Stent coating methodologies significantly impact product performance and consistency:
Dip Coating: Involves immersing the stent in a coating solution followed by controlled withdrawal and drying. This method was used in research settings for gastrointestinal stents with polyurethane-silicone elastomer and 5-fluorouracil [9].
Spray Coating: The most widely used industrial technique, involving atomization of coating solution onto the stent surface. This allows precise control over coating thickness and distribution [6].
Electrophoretic Deposition: Utilizes electrical fields to deposit coating materials, potentially offering improved uniformity and adherence [6].
Key coating challenges include ensuring uniformity and consistency, adequate adhesion to prevent delamination during stent expansion, and maintaining stability during sterilization and storage [6]. Scanning electron microscopy studies have revealed that different DES types exhibit significant variations in post-expansion coating irregularities, with specific patterns characteristic of each stent design [61].
Experimental Protocols for Coating Development and Evaluation
Coating Fabrication and Characterization Protocol
Objective: To fabricate and characterize polymer-based drug-eluting stent coatings with controlled drug release properties.
Materials:
- Stent platforms (bare metal or biodegradable)
- Polymer matrix (e.g., polyurethane-silicone elastomer, biodegradable polyester)
- Active pharmaceutical ingredient (e.g., sirolimus, everolimus, paclitaxel)
- Solvent system (tetrahydrofuran, dimethylacetamide)
- Coating apparatus (spray or dip coating system)
- Analytical instruments (HPLC, SEM, FTIR)
Procedure:
- Coating Solution Preparation: Dissolve polymer and drug in appropriate solvent system at predetermined ratio (typically 5-15% w/w solid content) with continuous stirring until complete dissolution [9].
Stent Coating Application:
- Spray Coating: Mount stent on mandrel and apply coating solution using automated spray system with controlled nozzle distance, spray rate, and stent rotation speed. Maintain consistent temperature and humidity conditions [6].
- Dip Coating: Immerse stent in coating solution using controlled withdrawal rate (typically 1-5 mm/s) to achieve uniform coating deposition. Repeat for multiple layers with intermediate drying [9].
Drying and Curing: Transfer coated stents to controlled environment (temperature: 25-40°C, relative humidity: 30-50%) for solvent evaporation. For certain polymers, apply thermal curing according to manufacturer specifications [9].
Coating Characterization:
- Thickness Measurement: Use scanning electron microscopy to measure coating thickness at multiple stent strut locations [61].
- Surface Morphology: Analyze coating surface using SEM at various magnifications (50-500x) to identify irregularities, cracks, or defects [61].
- Drug Content Uniformity: Assess drug distribution using FTIR photoacoustic spectroscopy or HPLC analysis of stent segments [9].
- Adhesion Testing: Evaluate coating adhesion using tape tests or mechanical expansion simulating implantation [6].
Diagram 2: Stent Coating Fabrication Workflow (100 chars)
In Vitro Drug Release Assessment Protocol
Objective: To evaluate drug release kinetics from DES under simulated physiological conditions.
Materials:
- Coated stent samples
- Release medium (phosphate buffered saline with 0.05% w/v sodium azide, pH 7.4)
- Surfactant (Tween 20 or 80 for sink condition maintenance)
- USP Apparatus 4 (flow-through cell) or Apparatus 7 (reciprocating holder)
- HPLC system with validated analytical method
- Temperature-controlled shaking water bath
Procedure:
- Apparatus Selection: Select appropriate dissolution apparatus based on stent design and testing requirements. USP Apparatus 7 (reciprocating holder) is often preferred for stent evaluation [6].
Media Preparation: Prepare release medium using PBS (pH 7.4) with addition of 0.05% w/v sodium azide to prevent microbial growth. For hydrophobic drugs, add surfactant (0.1-0.5% Tween 20 or 80) to maintain sink conditions [6].
Sample Immersion: Place individual stent samples in vessels containing predetermined volume of release medium (typically 10-50 mL depending on stent size and drug content) [6].
Incubation Conditions: Maintain system at 37±0.5°C with continuous agitation (reciprocation rate 30 dips per minute for Apparatus 7) [6].
Sampling Timepoints: Withdraw and replace medium at predetermined intervals: 1, 2, 4, 8, 24 hours; then daily for 7 days; then weekly up to 90-180 days [6].
Drug Quantification: Analyze samples using validated HPLC method with UV detection. Calculate cumulative drug release and plot release profile [6].
Release Kinetics Modeling: Fit release data to mathematical models (zero-order, first-order, Higuchi, Korsmeyer-Peppas) to elucidate release mechanisms [6].
Accelerated Release Testing: For quality control purposes, develop accelerated method using elevated temperature (50°C) or altered medium composition to predict long-term release behavior within reduced timeframe (2-4 weeks) [6].
Coating Integrity Evaluation Protocol
Objective: To assess coating durability and integrity following stent expansion and simulated implantation.
Materials:
- Expanded stent samples
- Scanning electron microscope
- Light microscope with digital imaging
- Sterile water bath at 37°C
- Balloon angioplasty system
Procedure:
- Stent Expansion: Expand coated stents in sterile water bath at 37°C using balloon inflation to nominal pressure (typically 14 atm). Use clinical-grade balloon catheters of appropriate size [61].
Sample Preparation: Dry expanded stents under laminar airflow at room temperature. Mount samples on SEM stubs without conductive coating to preserve native coating morphology [61].
SEM Imaging: Examine stent surfaces using scanning electron microscopy at multiple magnifications (50-500x). Use low-voltage protocols (1 keV) to minimize coating damage [61].
Irregularity Classification: Systematically classify coating irregularities according to established categories [61]:
- Reduced thickness: Bare metal aspects, thinning, cracks
- Increased thickness: Auricle-shaped excess, ridge-like excess, small round structures
- Inhomogeneous distribution: Granular appearance, crater irregularities
- Displacement: Wrinkles, flattened coating, webbing, detached fragments
Quantitative Analysis: Measure incidence and dimensions of irregularities across multiple imaging fields (minimum 360 images per stent type). Calculate frequency of each irregularity type per standardized image field [61].
Statistical Comparison: Compare irregularity patterns between different stent types using appropriate statistical tests (Kruskal-Wallis with Mann-Whitney post-hoc and Bonferroni correction) [61].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for DES Coating Development
| Category | Specific Reagents/Materials | Function/Application | Key Considerations |
|---|---|---|---|
| Polymer Systems | Polyurethane-silicone elastomer (ChronoSil) | Drug reservoir matrix for controlled release | Flexibility, drug compatibility, mechanical stability [9] |
| Poly(ethylene-co-vinyl acetate) (PEVA) | Diffusion-regulating topcoat | Control of drug release kinetics [9] | |
| Polylactic acid (PLA) and copolymers | Biodegradable polymer matrix | Degradation rate matching to drug release profile [6] | |
| Styrene-b-isobutylene-b-styrene (SIBS) | Non-degradable polymer for paclitaxel delivery | Durability, compatibility with lipophilic drugs [61] | |
| Active Pharmaceutical Ingredients | Sirolimus and analogs (everolimus, zotarolimus) | mTOR inhibitors for smooth muscle cell proliferation arrest | G0/G1 cell cycle arrest, therapeutic window [6] |
| Paclitaxel | Microtubule stabilizer for apoptosis induction | Cytotoxic at low concentrations, mechanism differentiation [6] | |
| 5-Fluorouracil (5FU) | Antimetabolite for gastrointestinal applications | Hydrophilic drug challenge, burst release control [9] | |
| Characterization Tools | Scanning Electron Microscopy (SEM) | Coating morphology and integrity assessment | Low-voltage protocols to prevent coating damage [61] |
| High-Performance Liquid Chromatography (HPLC) | Drug content and release kinetics quantification | Method validation for specific drug-polymer combination [6] | |
| Fourier Transform Infrared (FTIR) Spectroscopy | Chemical composition and drug distribution analysis | Photoacoustic mode for direct stent analysis [9] | |
| Testing Equipment | USP Apparatus 7 (Reciprocating Holder) | In vitro drug release evaluation | Physiological motion simulation [6] |
| Balloon Angioplasty System | Stent expansion under physiological conditions | Clinical relevance of expansion parameters [61] | |
| Environmental Control Chamber | Stability testing under ICH guidelines | Real-time and accelerated condition assessment [6] |
Future Directions and Emerging Technologies
The field of DES coating technology continues to evolve with several promising innovations emerging:
Biosensor Integration: Next-generation stents incorporating miniaturized sensors for real-time monitoring of endothelial healing, inflammatory activity, restenosis development, and local drug concentrations. These systems enable early detection of complications and timely intervention [60].
Personalized Drug Delivery: Advanced biomaterials with biosensors and adjustable polymer coatings that release specific drug amounts based on individual patient profiles, comorbidities, and genetic variabilities [60].
Genetically Engineered Stents: Stents incorporating antibodies or aptamers that selectively capture circulating endothelial progenitor cells, accelerating endothelialization and vessel healing [3].
4D-Printed Personalized Stents: Customized stent designs tailored to individual patient anatomy, potentially manufactured in the catheterization laboratory during the procedure [3].
Nanotechnology-Enhanced Coatings: Nano and micro-scale carrier systems with biodegradable polymers and cytostatic drugs offering improved intracellular uptake and prolonged tissue drug residency [6].
These innovations represent the cutting edge of stent coating technology and offer promising avenues for addressing the persistent challenge of in-stent restenosis through more sophisticated, personalized approaches to vascular intervention.
Drug-eluting stents (DES) represent a cornerstone in the treatment of coronary artery disease, significantly reducing rates of in-stent restenosis (ISR) by locally delivering anti-proliferative agents to the vessel wall. The clinical efficacy of a DES is fundamentally governed by the complex interplay between drug transport and release kinetics. Computational modeling has emerged as a powerful, cost-effective tool to simulate these processes, enabling researchers to optimize stent design and drug formulation before embarking on extensive preclinical testing. By creating virtual replicas of stented arteries, these models can predict drug distribution and retention within the arterial wall, providing critical insights that accelerate the development of next-generation DES [3] [12]. This document outlines standardized computational approaches and protocols for modeling drug transport and release, framed within a broader thesis on advancing DES coating and application techniques.
Computational Approaches to Drug Transport
The transport of drug from the stent strut into and through the arterial wall is a multiphysics problem involving diffusion, convection, and binding reactions. A two-species pharmacokinetic model is often employed to accurately capture this dynamics, distinguishing between the unbound (free) and bound drug phases [62].
Two-Species Pharmacokinetic Model
This model conceptualizes drug transport as two interdependent processes:
- Unbound Drug Transport: Governed by an unsteady convection-diffusion-reaction process. The unbound drug moves through the porous arterial wall via diffusion and is carried along by the flow of interstitial fluid (ISF).
- Drug Binding: Modeled as an unsteady reaction process where unbound drug molecules reversibly bind to specific receptors on cellular components within the vessel wall.
The governing equations for a two-dimensional axisymmetric model are summarized in the table below [62].
Table 1: Governing Equations for a Two-Species Drug Transport Model
| Component | Governing Equation | Key Parameters |
|---|---|---|
| Interstitial Fluid Flow | Brinkman equation for flow in a porous medium | Arterial wall permeability, Viscosity of ISF |
| Unbound Drug Transport | (\frac{\partial Cu}{\partial t} = \nabla \cdot (D \nabla Cu) - \nabla \cdot (\vec{v} Cu) - k{on} Cu + k{off} C_b) | (Cu): Unbound drug concentration, (D): Diffusion coefficient, (\vec{v}): ISF velocity vector, (k{on}): Binding-on rate constant, (k_{off}): Binding-off rate constant |
| Bound Drug Formation | (\frac{\partial Cb}{\partial t} = k{on} Cu - k{off} C_b) | (C_b): Bound drug concentration |
Key Physicochemical Parameters
Computational models are highly sensitive to input parameters. The following table details critical parameters and their impact on simulated drug distribution.
Table 2: Key Parameters Influencing Drug Transport and Retention [62]
| Parameter | Description | Impact on Drug Distribution & Retention |
|---|---|---|
| Peclet Number (Pe) | Ratio of convective transport rate to diffusive transport rate. | Higher Pe values enhance drug penetration depth but can reduce near-strut retention due to advective washout. |
| Equilibrium Association Constant ((k_{eq})) | Ratio of (k{on}) to (k{off}), representing binding affinity. | A higher (k_{eq}) promotes greater drug retention in the tissue by increasing the fraction of bound drug. |
| Binding-on Constant ((\psi)) | Dimensionless parameter representing the binding reaction rate. | Increasing (\psi) leads to a faster transition of drug from the unbound to the bound state, enhancing local retention. |
The diagram below illustrates the pathways and interactions described by this two-species model.
Modeling Drug Release Kinetics
The rate at which a drug is released from the stent coating sets the initial condition for the entire transport process. While early models used simplified boundary conditions, modern simulations incorporate more realistic, time-dependent release kinetics.
Time-Decaying Release Kinetics
A common approach is to model the drug release from the stent strut surface as a time-decaying function, rather than a constant concentration (Dirichlet boundary condition). This more accurately reflects the finite drug payload in the polymer coating and its gradual depletion over time [62]. The release profile can be tuned to match experimental elution data for specific drug-polymer combinations, such as the sustained release profiles required for sirolimus and its analogs [63].
The Role of Coating Technology
The design of the stent coating itself is a primary determinant of release kinetics. Advanced polymer technologies enable precise control over drug elution:
- Bioresorbable Polymers: These polymers degrade over a programmed period (e.g., 6-12 months), releasing the drug and then dissolving to eliminate the long-term presence of a foreign body [3] [63].
- Gradient-Release Polymers: Sophisticated systems provide variable drug release rates, with higher initial concentrations to combat early inflammation followed by sustained release to prevent late neointimal proliferation [3].
- Polymer-Free Systems: Utilizing nanoporous stent surfaces or other micro-reservoirs, these systems allow for polymer-free drug delivery with precisely controlled elution kinetics [3].
Application Notes & Experimental Protocols
Protocol: Setting Up a Two-Species Drug Delivery Simulation
This protocol provides a step-by-step methodology for implementing a computational model of drug transport from a half-embedded stent strut, based on established research [62].
1. Model Geometry Definition:
- Create a 2D axisymmetric computational domain representing a segment of the arterial wall.
- Model three equi-spaced, half-embedded stent struts with a diameter (δ) of 0.1 mm and an inter-strut distance of 0.3 mm to represent a typical stent pattern.
- Define the lumen-wall interface and the outer media/adventitia boundary.
2. Physics Setup:
- Fluid Flow: Activate the Brinkman Equations interface to model the flow of interstitial fluid (ISF) in the porous arterial wall. Set the dynamic viscosity of ISF to 0.72 cP and the Darcy permeability (K) to 2.0x10â»Â¹â¸ m².
- Drug Transport: Use a Transport of Diluted Species interface.
- For the unbound drug, set the diffusion coefficient (D) to 7.5x10â»Â¹Â¹ m²/s. Use the velocity field from the Brinkman solution as the convective term. Add a reaction term defined as
-k_on * C_u + k_off * C_b. - Add a second dependent variable for the bound drug. Do not assign convection or diffusion. Define its reaction term as
+k_on * C_u - k_off * C_b. - Set the initial values for both
C_uandC_bto zero.
- For the unbound drug, set the diffusion coefficient (D) to 7.5x10â»Â¹Â¹ m²/s. Use the velocity field from the Brinkman solution as the convective term. Add a reaction term defined as
3. Boundary Conditions:
- Drug Release: On the surfaces of the stent struts, apply a Time-Decaying Flux boundary condition for the unbound drug (e.g.,
Flux = C0 * exp(-beta * t)), whereC0is the initial concentration andbetais the release rate constant. - Lumen-Wall Interface: Set this boundary to a convective flux condition for the unbound drug.
- Outer Boundary: Apply a zero-concentration condition for the unbound drug to simulate a perfect sink.
4. Meshing and Grid Independence:
- Use a physics-controlled mesh, ensuring heavy refinement around the stent struts where concentration gradients are steepest.
- Perform a grid independence study by running simulations with successively finer mesh sizes (e.g., coarse, baseline, fine). The solution is considered grid-independent when the concentration profiles for different meshes nearly overlap. A baseline grid of
3201 x 81nodes has been validated for this purpose [62].
5. Solver Configuration and Analysis:
- Use a time-dependent solver with a suitable time-stepping method (e.g., BDF). The total simulation time should reflect the drug release period (e.g., 30-60 days).
- After solving, extract and plot spatial concentration profiles of bound and unbound drug at different time points.
- Conduct a sensitivity analysis by varying key dimensionless parameters (Pe, (k_{eq}), (\psi)) to quantify their influence on drug retention and distribution.
Advanced Multiscale and Hemodynamic Coupling
For a more comprehensive analysis, the drug transport model can be coupled with other physical phenomena. A quasi-steady approach is recommended to efficiently handle the disparate time scales involved [12].
Workflow for Coupled Hemodynamic-Growth Model:
- Solve Hemodynamics: Compute the blood flow field in the stented artery using Computational Fluid Dynamics (CFD), resolving Wall Shear Stress (WSS).
- Map WSS to Growth Model: Use the computed WSS to inform the rate of re-endothelialization and neointimal hyperplasia in an arterial growth model.
- Solve Drug Transport & Growth: In a homogenized time step, solve for drug transport (as in Protocol 4.1) and the consequent tissue growth, which modifies the geometry of the arterial domain.
- Update Geometry & Loop: Update the computational mesh for the fluid and solid domains based on the growth. Return to step 1, using the new geometry for the next hemodynamic simulation.
This multiscale, multiphysics framework allows for the prediction of how stent design, drug elution, and resultant hemodynamics collectively modulate long-term restenosis progression [12].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools and Physical Components for DES Research
| Item / Solution | Function / Role in DES Research |
|---|---|
| Finite Element Analysis (FEA) Software | Platform for implementing multiphysics models (e.g., COMSOL Multiphysics). Used to solve coupled systems of PDEs for fluid dynamics and drug transport. |
| Computational Fluid Dynamics (CFD) Solver | To simulate blood flow in stented arteries and compute hemodynamic parameters like Wall Shear Stress, which influences restenosis. |
| Two-Species Pharmacokinetic Model | A computational framework that distinguishes between unbound and bound drug to more accurately predict drug retention and efficacy in the arterial wall. |
| Bioresorbable Polymer (e.g., PLGA) | A coating material that degrades at a programmed rate after implant, releasing the drug and then dissolving to avoid long-term polymer presence. |
| Sirolimus (and analogs) | The primary anti-proliferative drug used in DES. It inhibits the mammalian target of rapamycin (mTOR), arresting the cell cycle and reducing neointimal hyperplasia. |
| Optical Coherence Tomography (OCT) | High-resolution imaging modality used to obtain patient-specific coronary artery geometries for constructing realistic computational models. |
| Machine Learning (ML) Algorithms | Used to accelerate the optimization of DES parameters by predicting complex property relationships and identifying optimal formulations from large datasets. |
Within the broader research on drug-eluting stent (DES) coatings and application techniques, understanding polymer-related complications is paramount for developing next-generation devices. While polymers are indispensable as drug reservoirs in DES, controlling the release of antiproliferative agents, their persistent presence or degradation can provoke local inflammatory and hypersensitivity responses [64] [65]. These reactions are key drivers of adverse clinical outcomes, including in-stent restenosis (ISR) and late stent thrombosis (LST) [64]. This document details the core mechanisms, provides quantitative data on inflammatory biomarkers, outlines standardized experimental protocols for assessing biocompatibility, and visualizes the pathophysiological pathways involved.
Pathophysiological Mechanisms and Quantitative Biomarker Profiles
Polymer-induced complications arise from two primary, interconnected pathways: the classical inflammatory response and delayed-type hypersensitivity. Table 1 summarizes the key inflammatory biomarkers elevated in these responses, based on clinical and experimental data.
Table 1: Key Inflammatory Biomarkers in Polymer-Related Complications
| Biomarker Category | Specific Biomarker | Role in Pathophysiology | Associated Stent/Polymer Type | Clinical/Experimental Evidence |
|---|---|---|---|---|
| Pro-inflammatory Cytokines | IL-6 | Orchestrates acute phase response; stimulates hepatic CRP production [66]. | PMMA bone cement [66]. | Post-op levels significantly higher in cemented vs. uncemented THA (p=0.001) [66]. |
| TNF-α | Potent pro-inflammatory cytokine; activates endothelial cells [66]. | PMMA bone cement [66]. | Post-op levels significantly higher in cemented vs. uncemented THA (p<0.001) [66]. | |
| Acute Phase Reactants | C-Reactive Protein (CRP) | Nonspecific marker of inflammation; independent predictor of MACE and restenosis [64]. | Durable polymer DES [64]. | Plasma levels significantly increased in patients with restenosis [64]. |
| Erythrocyte Sedimentation Rate (ESR) | Reflects systemic changes in plasma proteins post-surgery [66]. | PMMA bone cement [66]. | Post-op levels significantly higher in cemented vs. uncemented THA (p=0.002) [66]. | |
| Allergic Response Mediators | Histamine | Released by mast cells; increases vascular permeability [66] [64]. | PMMA bone cement [66]. | Post-op levels significantly higher in cemented vs. uncemented THA (p<0.001) [66]. |
| Eosinophils & Mast Cells | Effector cells in allergic inflammation; secrete growth factors and proteases [64]. | Metal alloys (e.g., Nickel, Cobalt-Chromium) [64]. | Infiltration found at sites of restenosis; associated with metal hypersensitivity [64]. | |
| Cell Adhesion Molecules | ICAM-1 | Mediates leukocyte adhesion and transendothelial migration [64]. | Metal ions (e.g., Nickel) [64]. | Expression upregulated by nickel salts, facilitating leukocyte recruitment [64]. |
The following diagram illustrates the interconnected cellular and molecular pathways triggered by stent polymer materials, leading to inflammation and restenosis.
Diagram Title: Pathways of Polymer-Induced Inflammation and Restenosis
Experimental Protocols for Assessing Polymer Biocompatibility
Protocol: In Vitro Profiling of Polymer-Induced Immune Activation
This protocol outlines a method for evaluating the inflammatory potential of polymer coatings or their leachates using human peripheral blood mononuclear cells (PBMCs), simulating the initial immune response post-stent implantation [50].
1. Reagent Preparation:
- Test Polymer Coating: Apply the polymer coating to sterile glass coverslips or the bottom of a culture-grade well. Ensure uniform thickness and sterilize via gamma irradiation or ethylene oxide treatment, following established standards [9].
- Culture Medium: Use RPMI-1640 medium supplemented with 10% heat-inactivated fetal bovine serum (FBS), 1% L-glutamine, and 1% penicillin-streptomycin.
- Positive Control: Prepare Lipopolysaccharide (LPS) at 1 µg/mL in culture medium.
- Negative Control: Use culture medium only.
2. PBMC Isolation and Seeding:
- Isolate PBMCs from healthy human donor blood using density gradient centrifugation (e.g., Ficoll-Paque).
- Wash the PBMC pellet twice with phosphate-buffered saline (PBS) and resuspend in culture medium.
- Seed PBMCs onto the polymer-coated surfaces, positive control wells, and negative control wells at a density of 1 x 10^6 cells/mL.
- Incubate the cells at 37°C in a 5% CO₂ atmosphere for 24, 48, and 72 hours.
3. Sample Collection and Analysis:
- Supernatant Collection: At each time point, collect the culture supernatant by centrifugation. Aliquot and store at -80°C for subsequent analysis.
- Cytokine Profiling: Quantify the levels of key pro-inflammatory cytokines (e.g., IL-6, TNF-α, IL-1β) and chemokines (e.g., MCP-1) in the supernatant using enzyme-linked immunosorbent assay (ELISA) kits, following manufacturer instructions [50].
- Cell Viability Assay: Perform an MTT or XTT assay on the remaining cells to assess polymer cytotoxicity, following standard protocols.
4. Data Interpretation:
- Compare cytokine levels from polymer-coated samples against negative and positive controls.
- A statistically significant increase in specific cytokines indicates the polymer's potential to activate immune pathways.
Protocol: In Vivo Histological Evaluation of Vascular Inflammation and Hypersensitivity
This protocol describes the histological processing and analysis of stented arterial segments from animal models to evaluate the vascular healing response, inflammation, and signs of hypersensitivity.
1. Animal Model and Stent Implantation:
- Perform stent implantation (polymer-coated vs. control) into the target artery (e.g., porcine coronary artery, rabbit iliac artery) according to approved animal care and use protocols.
2. Tissue Harvesting and Processing:
- At the predetermined endpoint (e.g., 28, 90, and 180 days), euthanize the animal and perfuse the vasculature with saline followed by 10% neutral buffered formalin under physiological pressure.
- Carefully dissect the stented arterial segment and immerse it in formalin for fixation for a minimum of 48 hours.
3. Tissue Processing and Sectioning:
- Process the fixed stented segment through a graded series of alcohols and xylene, followed by infiltration and embedding in polymethylmethacrylate (PMMA) resin to support the metal stent struts.
- Once polymerized, use a precision saw (e.g., Isomet) to cut the block, and then grind and polish to obtain 30-50 µm thick sections. Alternatively, for polymer stents without metal, paraffin embedding and microtomy can be used.
4. Staining and Histomorphometric Analysis:
- Stain sections with Hematoxylin and Eosin (H&E) for general morphology and cell nuclei visualization.
- Perform specific stains as required:
- Verhoeff-Van Gieson (VVG) stain: To visualize internal and external elastic laminae for measuring neointimal area.
- Immunohistochemistry (IHC): Use primary antibodies against specific cell types and markers:
- CD68: To identify macrophages.
- CD3: To identify T-lymphocytes, key in hypersensitivity.
- Tryptase/Chymase: To identify mast cells, effectors in allergic inflammation [64].
- Analysis: Use image analysis software to perform histomorphometry. Key parameters include:
- Inflammation Score: A semi-quantitative score (e.g., 0-3) based on the density of inflammatory cells around struts.
- Fibrin Deposition: Assess the degree of fibrin deposition, indicating delayed healing.
- Neointimal Thickness/Area: Measure the thickness and cross-sectional area of the neointima.
- Endothelialization Score: Assess the percentage of the luminal surface covered by endothelium.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents for Investigating Polymer-Related Inflammation
| Item | Function/Application in Research | Example Use Case |
|---|---|---|
| Human PBMCs | Primary immune cells for in vitro testing of polymer biocompatibility and cytokine release profiles [50]. | Profiling inflammatory protein signatures released upon contact with polymer eluates [50]. |
| ELISA Kits (IL-6, TNF-α, etc.) | Quantifying specific inflammatory cytokines in cell culture supernatants or serum/plasma from animal models. | Measuring IL-6 and TNF-α levels in PBMC supernatant to gauge polymer-induced inflammation [66] [50]. |
| CD68, CD3 Antibodies | IHC markers for identifying macrophages and T-lymphocytes, respectively, in tissue sections [64]. | Staining stented arterial sections to characterize the type and extent of cellular infiltrate [64]. |
| Mast Cell Tryptase Antibody | IHC marker for detecting mast cell infiltration, a hallmark of hypersensitivity reactions [64]. | Investigating suspected metal or polymer hypersensitivity in explained stents or animal tissues [64]. |
| Poly(lactide-co-glycolide) (PLGA) | A common biodegradable polymer used as a benchmark for comparing new polymer coatings [67] [43]. | Served as a control biodegradable polymer in studies comparing vascular healing and inflammation [43]. |
| Cobalt-Chromium (CoCr) Alloy Platform | A standard metallic stent platform; its interaction with polymers and ion release can be studied [64] [65]. | Used as the base platform for testing novel polymer coatings and assessing synergistic effects on inflammation [64]. |
The performance of a Drug-Eluting Stent (DES) is fundamentally governed by the release kinetics of its therapeutic agent. Optimal release kinetics must balance two critical, and often competing, objectives: efficacious inhibition of neointimal hyperplasia (tissue re-growth) and promotion of rapid vascular healing to ensure long-term safety. An initial burst release is often necessary to combat acute inflammatory responses and smooth muscle cell proliferation immediately following stent implantation, while a sustained, controlled release is required to prevent late-stage restenosis. However, the prolonged presence of both the drug and the polymer carrier has been linked to delayed endothelialization and late stent thrombosis, a serious safety concern [3] [8]. Therefore, the core challenge in DES design is engineering a drug release profile that delivers a therapeutically effective dose within a specific temporal window, using materials and methods that minimize adverse biological responses. This document provides detailed application notes and experimental protocols to guide researchers in systematically optimizing these critical release kinetics.
Key Factors Influencing Drug Release Kinetics
The drug release profile from a DES is a complex function of multiple interdependent variables. Understanding and controlling these factors is essential for rational design. The most critical factors are summarized in the table below.
Table 1: Key Factors Influencing Drug Release Kinetics from DES
| Factor Category | Specific Parameter | Impact on Release Kinetics | Safety & Efficacy Consideration |
|---|---|---|---|
| Polymer System | Biodegradable vs. Non-biodegradable | Determines if release is dominated by diffusion (non-degradable) or a combination of diffusion and polymer erosion (degradable) [3]. | Biodegradable polymers eliminate long-term polymer presence, reducing risk of late inflammation and thrombosis [3] [8]. |
| Polymer Composition & Hydrophilicity | Affects drug-polymer interaction, diffusion rate, and water penetration. Hydrophilic polymers can increase initial burst release. | Biomimetic polymers can promote endothelial cell attachment, improving safety profile [3]. | |
| Polymer Layer Thickness & Uniformity | Thicker layers can prolong release; non-uniformity causes inconsistent local drug dosing [6]. | Defects in coating can lead to dose dumping or incomplete treatment, risking restenosis [9]. | |
| Drug Properties | Drug Solubility (Hydrophilicity/Lipophilicity) | Hydrophilic drugs (e.g., 5-FU) tend to diffuse faster, leading to higher burst release [9]. | A high burst of cytotoxic drugs may impair initial endothelial healing. |
| Molecular Weight & Size | Larger molecules diffuse more slowly through the polymer matrix. | Impacts the required drug loading to achieve therapeutic concentration. | |
| Stent Platform & Coating Design | Drug Loading & Drug-Polymer Ratio | Higher loading can prolong release duration but may increase burst release if not properly controlled [68]. | Must exceed Minimum Inhibitory Concentration (MIC) but stay below toxic thresholds [68]. |
| Coating Architecture (e.g., reservoir matrix, multilayer) | Multilayer coatings (e.g., basecoat + diffusion-regulating topcoat) offer superior control over release rate [9]. | Allows for sophisticated release profiles (e.g., fast-slow) to match biological healing stages. | |
| Use of Nano/Micro-carriers | Nanoporous surfaces or micro-reservoirs enable polymer-free drug delivery with precise elution kinetics [3] [6]. | Reduces polymer-related adverse effects and can enable targeted delivery. |
Experimental Protocols for Release Kinetics Optimization
Protocol: Evidence-Based Design-of-Experiments (DoE) for Formulation Optimization
This protocol leverages historical data to minimize initial experimental runs, providing a high-throughput method for identifying critical factor interactions [68].
1. Systematic Literature Review & Data Extraction:
- Objective: Identify eligible datasets for a meta-analysis.
- Procedure:
- Conduct a literature search using relevant keywords (e.g., "PLGA," "sirolimus," "drug-eluting stent," "release kinetics").
- From eligible publications, extract data on independent variables (e.g., polymer MW, LA:GA ratio, drug-polymer ratio) and the dependent variable (cumulative drug release over time).
- Use software like GetData Graph Digitizer to extract numerical data from published release curves.
- Normalize all release data to cumulative percentage to ensure comparability.
2. Interaction and Correlation Analysis:
- Objective: Quantitatively assess how factors influence each other and the release response.
- Procedure:
- Input the extracted data into DoE software (e.g., Design-Expert, JMP).
- Perform statistical analysis to calculate interaction effects and Pearson correlation coefficients between factors.
- Generate scatter plots and line graphs to visualize these relationships. Synergistic or antagonistic effects between factors will be identified at this stage.
3. Regression Modeling and ANOVA:
- Objective: Develop a mathematical model that predicts release kinetics based on factor inputs.
- Procedure:
- Test various regression models (linear, quadratic, cubic) suggested by the software.
- Use Analysis of Variance (ANOVA) to assess the significance of the model and each factor. A high F-value and a low p-value (typically < 0.05) indicate a significant factor.
- Evaluate the model's goodness-of-fit using the R² value and the insignificance of the lack-of-fit test.
4. Numerical and Graphical Optimization:
- Objective: Identify the optimal factor settings to achieve a target release profile.
- Procedure:
- Define optimization criteria based on the therapeutic window. For example: "Maximize release at 24 hours > MIC" and "Maximize sustained release over 30 days".
- Use the software's optimization function to generate desirability plots and identify the design space that meets all criteria.
- The final output is a set of optimized formulation parameters predicted to yield the ideal release profile.
The following diagram illustrates this evidence-based DoE workflow.
Protocol: In Vitro Drug Release Testing Under Physiological Conditions
1. Dissolution Media Preparation:
- Objective: Mimic the physiological environment at the implantation site.
- Procedure:
- Use a phosphate-buffered saline (PBS) solution at pH 7.4 and maintain a temperature of 37±0.5°C.
- For improved in vitro-in vivo correlation (IVIVC), consider adding surfactants (e.g., 0.1% Tween 80) to simulate protein interactions or enzymes to model biodegradation.
2. Sample Immersion and Agitation:
- Objective: Ensure consistent hydrodynamic conditions.
- Procedure:
- Place the coated stent or a representative coated coupon into a vessel containing a known volume of dissolution media.
- Use a shaking incubator or a USP Apparatus 4 (flow-through cell) to provide gentle, controlled agitation.
3. Sampling and Analytical Quantification:
- Objective: Accurately measure the amount of drug released over time.
- Procedure:
- At predetermined time points (e.g., 1h, 6h, 24h, 3d, 7d, 30d), withdraw a specific volume of the release medium.
- Immediately replace with an equal volume of fresh, pre-warmed media to maintain sink conditions.
- Analyze the drug concentration in the sampled media using a validated analytical method, typically High-Performance Liquid Chromatography (HPLC) with UV detection.
- Calculate the cumulative drug release percentage and plot the release profile over time.
4. Accelerated Release Testing:
- Objective: Obtain release profile data more quickly for quality control purposes.
- Procedure:
- Establish accelerated conditions (e.g., higher temperature, different pH) that have been correlated with real-time release data.
- This is critical for product development and stability testing, as real-time release studies can last 6-12 months [6].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagent Solutions for DES Coating and Release Studies
| Category | Item | Function & Application Note |
|---|---|---|
| Polymer Matrix | Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable polymer; release kinetics can be tuned by adjusting its MW and LA:GA ratio [68]. |
| Poly(ethylene-co-vinyl acetate) (PEVA) / Poly(n-butyl methacrylate) (PBMA) | Non-biodegradable polymers used in diffusion-controlled release systems, often as a topcoat to regulate drug release [9] [8]. | |
| Polyurethane-Silicone (PUS) Elastomer | Provides flexibility and high drug loading capacity; suitable as a basecoat reservoir [9]. | |
| Therapeutic Agents | Sirolimus (and analogs: Everolimus, Zotarolimus) | Limus-family drugs inhibit mTOR, arresting smooth muscle cell proliferation in the G1 phase [3] [26]. |
| Paclitaxel | Stabilizes microtubules, preventing cell division and migration; can induce apoptosis [6]. | |
| Coating Solvents | Dimethylacetamide (DMAc), Tetrahydrofuran (THF), Chloroform | Common solvents for dissolving polymers and drugs for dip-coating or spray-coating processes. Purity is critical for coating uniformity. |
| Analytical Tools | HPLC-UV/Vis System | The gold standard for quantifying drug concentration in release media during in vitro testing. |
| FTIR-PA Spectrometry | Used to characterize coating uniformity, drug distribution, and crystallinity within the polymer matrix [9]. |
Advanced Optimization and Analysis Workflow
Integrating the protocols and tools above into a cohesive workflow is key to efficient DES development. The following diagram maps the path from initial formulation to final performance validation, highlighting the role of advanced modeling techniques like Model-Informed Drug Development (MIDD) and Quantitative Systems Pharmacology (QSP). These computational approaches can simulate drug release, pharmacokinetics/pharmacodynamics (PK/PD), and patient responses, drastically reducing development time and cost by prioritizing the most promising formulations for experimental testing [69] [70].
Drug-eluting stents (DES) represent a cornerstone of modern interventional cardiology, significantly reducing restenosis rates compared to their bare-metal predecessors. The core principle of DES technology involves the localized delivery of antiproliferative agents to inhibit neointimal hyperplasia, a process of smooth muscle cell migration and proliferation that leads to vessel re-occlusion. However, first-generation DES, while effective at reducing restenosis, introduced new challenges, including late and very late stent thrombosis, largely attributed to delayed endothelial healing and inflammatory responses to the permanent polymer coatings [27] [8]. These complications have driven intensive research into next-generation materials designed to enhance biocompatibility and improve long-term clinical outcomes. This document outlines the current landscape of material innovations in DES, providing a detailed analysis of advanced polymers, stent platforms, and the experimental protocols used to evaluate their safety and efficacy, framed within the broader context of developing the ideal drug-eluting implant.
Current State of Material Innovations
The evolution of DES has progressed through generations, from permanent polymer coatings to the current focus on bioactive and fully bioresorbable systems. The following tables summarize key quantitative data on advanced polymer technologies and stent platform innovations.
Table 1: Advanced Polymer Coating Technologies for Drug-Eluting Stents
| Polymer Technology | Key Characteristics | Impact on Biocompatibility | Clinical/Preclinical Outcomes |
|---|---|---|---|
| Bioresorbable Polymers [3] [31] | Poly(lactide-co-glycolic acid) (PLGA); degrades into water and COâ‚‚. | Eliminates long-term polymer presence, reducing chronic inflammation and late thrombosis. | Coating absorption within 90 days; significantly reduced neointimal thickness and inflammation in porcine models [31]. |
| Biomimetic Polymers [3] | Mimics the extracellular matrix; promotes endothelial cell attachment. | Achieves balance between inhibiting restenosis and promoting re-endothelialization. | Preclinical stage; shows promise in accelerating vessel healing. |
| Gradient-Release Polymers [3] | Provides variable drug release rates tailored to temporal healing needs. | Higher initial dose to combat early inflammation, followed by sustained release. | Target lesion failure rates below 3% at one year in clinical studies. |
| Nanoporous Surface Technologies [3] | Creates microscopic reservoirs for polymer-free drug delivery. | Eliminates polymer-related inflammatory responses entirely. | Preclinical and early clinical evaluation. |
| Zwitterionic Hydrogels [71] | Highly hydrophilic; resists protein adsorption and platelet adhesion. | Superior hemocompatibility; reduces thrombogenicity. | In vitro studies show high stability and anticoagulant efficacy. |
Table 2: Innovative Stent Platform Materials and Designs
| Stent Platform | Material Composition | Advantages | Associated Complications & Status |
|---|---|---|---|
| Cobalt-Chromium (2nd Gen) [27] | Co-Cr alloy (e.g., MP35N, L605). | High radial strength, thin struts (~70 µm), improved flexibility. | Lower risk for target vessel revascularization vs. stainless steel; current clinical standard. |
| Platinum-Chromium [27] | Pt-Cr alloy. | Excellent radial strength, flexibility, conformability, and visibility. | Used in contemporary DES platforms. |
| Bioresorbable Metallic Scaffolds [72] | Magnesium (Mg) alloys (e.g., WE43). | "Intervention without implantation"; complete degradability. | Challenges: Paradox of delaying degradation vs. promoting healing; under investigation. |
| Bioresorbable Polymeric Scaffolds [27] | Poly-(L-lactic acid) (PLLA), tyrosine-derived polymers. | Restores vasomotion; avoids permanent caging. | Risk of scaffold fracture; requires robust mechanical design. |
| Thin-Strut Stents [27] [8] | Various alloys (Co-Cr, Pt-Cr). | Reduced flow disturbances, less vessel injury, lower thrombogenicity. | 1.5-fold less thrombogenic than thick-strutted DES [8]; superior in ISAR-STEREO trial [27]. |
Experimental Protocols for Evaluating New Stent Coatings
Rigorous preclinical testing is essential for validating the safety and performance of novel stent materials. The following protocol details a standard methodology for coating fabrication, in vitro drug release kinetics, and biocompatibility assessment, adaptable for various coating formulations.
Protocol: Coating Fabrication and In Vitro Evaluation of a Bioresorbable Polymer-based DES
1. Objective: To fabricate a sirolimus-eluting stent with a bioresorbable PLGA coating and characterize its drug release profile and biological efficacy in vitro.
2. Materials:
- Stent Platform: Cobalt-chromium bare metal stent (e.g., GENIUS Magic).
- Polymer: Poly(D,L-lactide-co-glycolide) (PLGA) (e.g., 50:50 molar ratio).
- Therapeutic Agent: Sirolimus (Rapamycin).
- Solvent: Reagent-grade acetone.
- Coating Apparatus: Ultrasonic spray coater or dip-coater.
- Release Medium: Phosphate Buffered Saline (PBS), pH 7.4, with 0.5% w/w Tween 80 to maintain sink conditions.
- Cell Culture: Human Coronary Artery Smooth Muscle Cells (HCASMCs), cell culture media.
3. Methodology:
A. Coating Fabrication via Electrostatic Deposition [31]: 1. Preparation: Precisely weigh sirolimus and PLGA polymer to achieve a target drug-to-polymer ratio (e.g., 1:1 to 1:3). 2. Formulation: Dissolve the drug-polymer mixture in a suitable solvent (e.g., acetone) to create a homogeneous coating solution. 3. Coating: Utilize a dry-powder electrostatic coating process. Briefly, the coating material is charged and applied to the grounded stent platform. This ensures a uniform, crystalline coating without the use of solvents that can degrade the drug. 4. Curing: Allow the coated stents to dry and cure under controlled temperature and humidity to ensure coating stability.
B. Coating Characterization: 1. Surface Morphology: Image the coated stents using Scanning Electron Microscopy (SEM) at various magnifications (e.g., 35x to 5000x) to assess coating uniformity, thickness, and the presence of cracks or defects. 2. Drug Stability: Perform High-Performance Liquid Chromatography with tandem mass spectrometry (HPLC-MS/MS) to quantify the amount of sirolimus and its primary degradants on the stent before and after incubation in serum-supplemented media at 37°C for 14 days.
C. In Vitro Drug Release Kinetics [8]: 1. Setup: Place individual coated stents (n=3-6) in tubes containing a known volume of release medium (PBS + Tween 80). Maintain the system at 37°C under gentle agitation. 2. Sampling: At predetermined time points (e.g., 1, 3, 7, 14, 21, 28 days), withdraw the entire release medium and replace it with fresh pre-warmed medium to maintain sink conditions. 3. Analysis: Quantify the amount of sirolimus in the collected samples using a validated HPLC-UV or HPLC-MS/MS method. 4. Data Modeling: Plot the cumulative drug released over time and fit the data to kinetic models (e.g., Higuchi, Korsmeyer-Peppas) to understand the release mechanism.
D. In Vitro Biological Efficacy (Cytotoxicity Assay): 1. Conditioned Media Preparation: Incubate sterile stents (coated and uncoated control) in cell culture media for 24-48 hours to create "conditioned media." 2. Cell Seeding: Plate HCASMCs in 96-well plates at a standardized density and allow to adhere overnight. 3. Treatment: Replace the standard media with the conditioned media from the stents. 4. Viability Assessment: After 72 hours of exposure, assess cell viability using a colorimetric assay like MTT or WST-1. A significant reduction in viability in the sirolimus-eluting stent group compared to the bare metal stent control confirms the anti-proliferative efficacy of the released drug.
4. Data Interpretation:
- A well-formulated coating will show a smooth, uniform surface under SEM.
- The drug release profile should demonstrate sustained release over 3-4 weeks, with a minimal initial burst, to match the timeline of VSMC proliferation [8].
- HCASMC viability should be significantly inhibited (>70% reduction) by the conditioned media from the drug-eluting stent, confirming the bioactivity of the released sirolimus.
Diagram 1: Stent Coating and In Vitro Evaluation Workflow
The Scientist's Toolkit: Key Research Reagents and Materials
Successful development and testing of next-generation DES coatings require a suite of specialized materials and analytical tools. The following table details essential components for a research laboratory in this field.
Table 3: Essential Research Reagents and Materials for DES Development
| Item | Function/Description | Example Use Case |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) [31] [8] | A bioresorbable polymer that degrades by hydrolysis into lactic and glycolic acid. Serves as a drug-carrying matrix. | Used in absorbable coatings; matches drug release with coating erosion [31]. |
| Sirolimus (Rapamycin) & Analogs [27] | mTOR inhibitor; arrests vascular smooth muscle cell cycle in G1 phase. The primary antiproliferative drug class. | Loaded onto stents to inhibit neointimal hyperplasia and restenosis. |
| Poly(ethylene-co-vinyl acetate) (PEVA) [9] [8] | A non-biodegradable polymer used as a diffusion-regulating membrane to control drug release kinetics. | Applied as a topcoat over a drug-loaded basecoat to achieve sustained release profiles [9]. |
| Cobalt-Chromium Bare Metal Stent [27] [31] | A high-strength, thin-strut alloy stent platform serving as the scaffold for coating applications. | The underlying platform for many 2nd and 3rd generation DES; provides excellent deliverability. |
| Human Coronary Artery Smooth Muscle Cells (HCASMCs) | Primary cell line used for in vitro efficacy testing of antiproliferative agents released from DES. | Treated with stent-conditioned media in MTT assays to verify drug bioactivity. |
| Scanning Electron Microscope (SEM) [9] [31] | Instrument for high-resolution imaging of stent coating surface morphology, uniformity, and defects. | Critical for Quality Control; identifies cracks, delamination, or non-uniform drug distribution. |
| HPLC-MS/MS System [31] | Analytical instrument for quantifying drug content, profiling release kinetics, and detecting degradants. | Used for drug stability testing under simulated use conditions and in release studies. |
Advanced Testing: In Vivo and Ex Vivo Models
Preclinical in vivo models are indispensable for evaluating the comprehensive biological response to a new DES, beyond what is possible with in vitro systems.
Protocol: In Vivo Evaluation in a Porcine Coronary Artery Model
1. Objective: To assess the safety, efficacy, and vascular healing response of a novel DES in a clinically relevant animal model.
2. Materials:
- Animal Model: Healthy Yucatan mini-swine.
- Stents: Novel DES, control Bare Metal Stent (BMS), and a clinically approved DES.
- Antiplatelet Therapy: Aspirin and Clopidogrel (or similar), administered pre- and post-operatively.
- Analysis Tools: Histopathology equipment, SEM, HPLC-MS/MS for tissue drug levels.
3. Methodology [31]:
A. Stent Implantation: 1. Pre-medication: Administer dual antiplatelet therapy for several days prior to surgery. 2. Procedure: Under general anesthesia, deploy stents in porcine coronary arteries using standard percutaneous techniques. Aim for a balloon-to-artery ratio of approximately 1.1:1 to 1.15:1 to induce a standardized injury. Include overlapping stent configurations to test performance in complex scenarios. 3. Post-operative care: Continue dual antiplatelet therapy until termination.
B. Endpoint Analysis: 1. Termination Time Points: Euthanize animals at pre-defined time points (e.g., 3, 30, 90 days) to capture early, mid, and late healing responses. 2. Perfusion Fixation: Perfuse the heart in situ with buffered formalin at physiological pressure to preserve vessel morphology.
C. Histopathology and Histomorphometry: 1. Processing: Embed the stented arterial segments in resin and section them. 2. Staining: Stain sections with Hematoxylin and Eosin (H&E) and Verhoeff's tissue elastin stain. 3. Blinded Scoring: A pathologist, blinded to the treatment groups, scores each stent strut for: - Injury Score: Measures vessel wall injury caused by the stent strut. - Inflammation Score: Quantifies the inflammatory response around each strut. 4. Morphometric Analysis: Using computer-assisted image analysis, measure: - Lumen Area - Neointimal Area - % Area Stenosis = (Neointimal Area / Lumen Area) * 100
D. Pharmacokinetic Analysis: 1. Tissue Harvest: At various time points (e.g., 1, 7, 28, 90 days), harvest stented arteries without fixation. 2. Drug Extraction: Homogenize the tissue and extract sirolimus. 3. Quantification: Use HPLC-MS/MS to determine the arterial tissue concentration of the drug over time, generating a pharmacokinetic profile.
4. Data Interpretation:
- A superior DES will show significantly lower % area stenosis and neointimal thickness compared to BMS controls at 28-30 days.
- Lower inflammation scores indicate better biocompatibility of the polymer coating.
- The pharmacokinetic profile should show sustained drug levels in the arterial wall for several weeks, aligning with the period of highest risk for restenosis.
Diagram 2: In Vivo Stent Evaluation Workflow
The relentless pursuit of enhanced biocompatibility in drug-eluting stents has driven a material science revolution in interventional cardiology. The shift from inert, permanent polymers to bioactive, bioresorbable, and biomimetic coatings represents a paradigm aimed at resolving the critical paradox of inhibiting restenosis while promoting rapid and healthy endothelial healing. As detailed in these application notes, the path to clinical translation is underpinned by rigorous, standardized experimental protocols that scrutinize material properties, drug release kinetics, and biological performance from the laboratory bench to advanced in vivo models. The ongoing integration of nanotechnology, personalized medicine approaches based on genetic profiling, and the development of "smart" stents with sensing capabilities [3] promise to further refine this field. By systematically applying the principles and methods outlined herein, researchers and drug development professionals can continue to innovate, contributing to the next generation of DES that offer improved safety profiles and long-term outcomes for patients worldwide.
Clinical Validation and Comparative Analysis of DES Technologies
The evaluation of drug-eluting stents (DES) relies on a standardized set of clinical outcome metrics that provide critical insights into their safety and efficacy. Target lesion revascularization (TLR), major adverse cardiovascular events (MACE), stent thrombosis (ST), and mortality rates represent the cornerstone endpoints in contemporary interventional cardiology research and clinical practice [73]. These metrics are particularly crucial when investigating novel stent coating technologies and application techniques, as they directly reflect clinical performance and patient outcomes. The evolution from bare-metal stents (BMS) to modern DES has dramatically improved these clinical metrics, though specific challenges remain in optimizing coating polymers, drug release kinetics, and biocompatibility [3] [8]. This document provides a comprehensive framework for assessing these critical outcome measures within the context of drug-eluting stent coating research.
Quantitative Clinical Outcome Metrics
Comparative Clinical Outcomes Between Stent Types
Table 1: Comparative Clinical Outcomes of DES vs. BMS from Contemporary Evidence
| Outcome Metric | DES Performance | BMS Performance | Follow-up Period | References |
|---|---|---|---|---|
| Target Lesion Revascularization (TLR) | 1% - 3% | ~8% | 1-3 years | [73] [74] [75] |
| MACE (Composite Endpoint) | 7% - 16.7% | ~14% | 1-3 years | [73] [74] [75] |
| All-Cause Mortality | 2% - 3% | ~3% | 1 year | [74] |
| Stent Thrombosis (Overall) | <0.5% - 2.9% | 1.2% | Up to 5 years | [76] [54] [8] |
| Very Late Stent Thrombosis | <0.1% per year (4th Gen DES) | N/A | Beyond 1 year | [3] |
| Target Lesion Failure (TLF) | 10.4% (Short DES) - 16.7% (Long DES) | N/A | 3 years | [75] |
Impact of Stent Length on Clinical Outcomes
Table 2: Impact of Second-Generation Drug-Eluting Stent (DES2) Length on 3-Year Outcomes [75]
| Outcome Metric | Short Stent Group (<20mm) | Long Stent Group (≥30mm) | Statistical Significance |
|---|---|---|---|
| Target Lesion Failure (TLF) | 10.4% | 16.7% | p=0.01 |
| All-Cause Death | 10.1% | 12.6% | p=0.30 |
| Cardiovascular Death | 4.7% | 7.1% | p=0.20 |
| Any Myocardial Infarction | 3.6% | 5.3% | p=0.30 |
| Target Lesion Revascularization | 3.6% | 6.9% | p=0.06 |
| Definite Stent Thrombosis | 0.4% | 1.6% | p=0.15 |
Experimental Protocols for Outcome Assessment
Protocol for Assessing Stent Thrombosis
Objective: To systematically evaluate and classify stent thrombosis events according to Academic Research Consortium (ARC) criteria.
Methodology:
- Event Classification: Classify all suspected stent thrombosis events according to ARC criteria:
Temporal Classification: Categorize timing of stent thrombosis:
- Acute: Within 24 hours of implantation
- Subacute: 24 hours to 30 days
- Late: 31 days to 1 year
- Very Late: Beyond 1 year [54]
Risk Factor Documentation: Record patient, lesion, and procedural characteristics:
- Patient Factors: Age, gender, smoking status, diabetes, renal function, DAPT adherence
- Lesion Characteristics: Bifurcations, calcification, chronic total occlusions, in-stent restenosis
- Procedural Factors: Stent under-expansion, malapposition, edge dissections [54]
Imaging Assessment: Utilize intravascular imaging (OCT/IVUS) to assess:
- Stent expansion and apposition
- Tissue coverage and healing patterns
- Presence of uncovered struts or malapposition [54]
Protocol for MACE and TLR Assessment
Objective: To standardize the evaluation of Major Adverse Cardiovascular Events and Target Lesion Revascularization in clinical studies.
Methodology:
- Endpoint Definitions:
- MACE: Composite of all-cause death, any myocardial infarction, and target lesion revascularization [75]
- TLR: Repeat intervention to treat luminal stenosis within 5mm of stent edges for recurrent symptoms or demonstrable ischemia [74]
- Myocardial Infarction: Defined according to the Fourth Universal Definition of MI [75]
Follow-up Schedule:
- Conduct regular follow-up at 30 days, 6 months, 1 year, and annually thereafter
- Utilize telephone follow-up, clinic visits, and database review
- Document all adverse events and medication adherence
Angiographic Assessment:
- Perform quantitative coronary angiography for suspected restenosis
- Measure binary restenosis (>50% diameter stenosis)
- Document late lumen loss and percentage diameter stenosis
Clinical Event Adjudication:
- Establish independent clinical events committee
- Blinded review of all potential endpoint events
- Apply standardized definitions across all sites
Pathophysiology and Risk Factor Relationships
Figure 1: Pathophysiology of Stent-Related Complications and MACE Components
Experimental Workflow for Stent Coating Evaluation
Figure 2: Comprehensive Workflow for Stent Coating Evaluation
The Scientist's Toolkit: Essential Research Materials
Table 3: Essential Research Reagents and Materials for DES Coating Studies
| Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Polymer Matrix Materials | Polyvinylpyrrolidone (PVP), Polyethylene glycol (PEG), Poly(lactic-co-glycolic acid) (PLGA), Polycaprolactone (PCL) [43] | Coating formulation, drug encapsulation | Controlled drug release, enhanced biocompatibility, structural support |
| Antiproliferative Drugs | Sirolimus, Everolimus, Zotarolimus, Paclitaxel [43] [26] | Bioactivity assessment | Inhibition of smooth muscle cell proliferation, reduction of neointimal hyperplasia |
| Coating Technologies | Nanoporous surfaces, Gradient-release polymers, Biomimetic polymers, Bioresorbable polymers [3] [43] | Advanced coating development | Programmable degradation, targeted drug delivery, improved endothelialization |
| Characterization Tools | Electron microscopy, HPLC, Mass spectrometry, Optical coherence tomography [54] [8] | Coating quality control | Assessment of coating uniformity, drug release kinetics, surface morphology |
| In-Vitro Test Systems | Cell culture models (VSMCs), Flow chambers, Platelet reactivity assays [8] | Biocompatibility screening | Evaluation of thrombogenicity, endothelial cell growth, inflammatory response |
| Animal Models | Porcine coronary injury model, Rabbit iliac artery model [8] | Pre-clinical safety and efficacy | Assessment of vascular healing, restenosis potential, tissue integration |
Advanced Coating Technologies and Clinical Implications
Contemporary research in drug-eluting stent coatings focuses on several innovative approaches to optimize clinical outcomes. Fourth-generation DES technologies incorporate polymer-free designs, bioresorbable vascular scaffolds (BVS), and nanotechnology-enhanced drug delivery systems [3]. These advancements aim to further reduce long-term complications by promoting natural vessel healing and restoring vasomotion.
The drug release kinetics from stent coatings are critically important, as vascular smooth muscle cells begin hyperproliferation within 24 hours after stent implantation and continue for approximately two weeks [8]. Advanced coating systems employ various mechanisms including:
- Reservoir systems where drugs are encapsulated within polymeric membranes
- Matrix systems with drugs dispersed within polymer networks
- Conjugated systems utilizing covalent drug-polymer conjugates for controlled release [43]
Recent clinical evidence demonstrates that second-generation DES consistently outperform bare-metal stents across all key metrics, with particular advantages in high-risk populations such as patients with diabetes and complex coronary anatomy [73]. The continuing evolution of stent coating technologies promises further improvements in clinical outcomes through enhanced biocompatibility and personalized approaches based on patient-specific factors and lesion characteristics.
Drug-eluting stents (DES) represent a revolutionary advancement in the management of coronary artery disease, fundamentally transforming percutaneous coronary intervention (PCI) outcomes. The progressive generational evolution of DES has focused on addressing the limitations of previous platforms, particularly concerning safety and efficacy endpoints. First-generation DES successfully reduced restenosis rates compared to bare-metal stents but revealed significant long-term safety concerns, including persistent inflammatory responses and late stent thrombosis. These limitations prompted the development of second-generation DES with more biocompatible polymers and different antiproliferative drugs. Subsequent third-generation DES have further refined these technologies with bioresorbable polymers and enhanced stent designs, aiming to optimize vascular healing while maintaining anti-restenotic efficacy [77].
The clinical performance across DES generations demonstrates a trajectory of continuous improvement. Contemporary practice has largely adopted new-generation DES, with current clinical guidelines reflecting their superior safety profile. Understanding the technological distinctions and their corresponding clinical outcomes is essential for researchers and clinicians aiming to optimize patient-specific stent selection and contribute to future device development. This document provides a structured comparison of DES generations, focusing on quantitative performance metrics, experimental methodologies for evaluation, and technical protocols relevant for research and development professionals [78] [77].
Technological Comparison Across Generations
The fundamental differences between DES generations lie in their platform alloy, polymer technology, and antiproliferative drug selection. These components collectively influence the long-term clinical performance by modulating vascular healing and drug release kinetics.
- First-Generation DES: Utilized stainless steel platforms and durable polymers such as poly(ethylene-co-vinyl acetate) (PEVA), poly(n-butyl methacrylate) (PBMA), or poly(styrene-b-isobutylene-b-styrene) (SIBS). These polymers were associated with hypersensitivity reactions, local tissue inflammation, and delayed vascular healing, contributing to late-stage thrombosis. The primary drugs were sirolimus (Cypher stent) or paclitaxel (Taxus stent) [77].
- Second-Generation DES: Featured improved cobalt-chromium or platinum-chromium alloys, providing thinner struts for better deliverability and radial strength. They introduced more biocompatible, durable polymers like poly(vinylidene fluoride-co-hexafluoropropylene) and different limus-family drugs (e.g., everolimus, zotarolimus). These changes reduced the inflammatory response and improved safety profiles [78] [77].
- Third-Generation DES: Incorporate bioresorbable polymeric coatings (e.g., polylactic acid) or polymer-free technologies. These stents aim to provide temporary drug delivery and then fully resorb, leaving a bare metal scaffold that avoids the long-term presence of inflammatory triggers. Drugs include everolimus, sirolimus, and biolimus A9. Some third-generation stents also utilize novel stent designs for enhanced flexibility [78] [77].
Table 1: Technological Components of Drug-Eluting Stent Generations
| Component | First-Generation DES | Second-Generation DES | Third-Generation DES |
|---|---|---|---|
| Stent Platform | Stainless Steel | Cobalt-Chromium or Platinum-Chromium | Cobalt-Chromium, with bioresorbable scaffolds |
| Polymer Type | Durable (e.g., PEVA, PBMA, SIBS) | Biocompatible Durable (e.g., fluorinated polymers) | Bioresorbable (e.g., Polylactic acid) or Polymer-free |
| Exemplary Drugs | Sirolimus, Paclitaxel | Everolimus, Zotarolimus | Everolimus, Sirolimus, Biolimus |
| Key Coating Challenge | Polymer-induced inflammation; late stent thrombosis | Optimizing biocompatibility; controlled drug release | Ensuring controlled drug releaseåŒæ¥ with polymer resorption |
Quantitative Clinical Performance Data
Long-term clinical studies consistently demonstrate the superior performance of new-generation DES (second and third) over first-generation devices. Key outcome measures include target lesion failure (TLF), major adverse cardiac events (MACE), and stent thrombosis (ST).
A 2021 real-world study with 3-year follow-up data compared new-generation DES in vessels of different sizes. While focusing on vessel diameter, the study utilized contemporary DES and reported outstandingly low event rates. For instance, the risk of TLF was significantly lower in the very small DES group compared to the small DES group (adjusted hazard ratio [HR] = 0.282, p = 0.040). The risks of MACEs and all-cause mortality were also significantly lower (MACE adjusted HR = 0.215, p = 0.001; all-cause mortality adjusted HR = 0.181, p = 0.005). Notably, no cases of stent thrombosis occurred in any group during the follow-up period, underscoring the enhanced safety of new-generation DES [78].
Historical comparisons with first-generation DES reveal a stark contrast. First-generation DES were associated with an annual stent thrombosis rate of 0.3–0.6%, which significantly increased patient mortality by 10–30%. The shift to more biocompatible polymers and improved stent designs in newer generations has been pivotal in mitigating these risks [77].
Table 2: Key Clinical Outcome Measures Across Generations
| Clinical Endpoint | First-Generation DES (Historical Data) | New-Generation DES (Contemporary Data, 3-Year Follow-Up) |
|---|---|---|
| Target Lesion Failure (TLF) | N/A (Established high restenosis vs. BMS) | Adjusted HR for very small vs. small vessels: 0.282 [78] |
| Major Adverse Cardiac Events (MACE) | N/A | Adjusted HR for very small vs. small vessels: 0.215 [78] |
| Stent Thrombosis (ST) | 0.3-0.6% annually [77] | 0% incidence reported in 3-year study [78] |
| All-Cause Mortality | Increased (attributed to late ST) [77] | Adjusted HR for very small vs. small vessels: 0.181 [78] |
Experimental Protocols for DES Evaluation
Robust experimental protocols are essential for evaluating DES performance in both non-clinical and clinical settings. The following methodologies are standard in the field.
In Vitro Drug Release Kinetics
Objective: To characterize the drug release profile of a DES under simulated physiological conditions. Methodology:
- Apparatus: Use a USP Apparatus 7 (reciprocating holder) or a custom-designed flow-through cell system.
- Media: Utilize phosphate-buffered saline (PBS, pH 7.4) with 0.05% w/v sodium dodecyl sulfate (SDS) to maintain sink conditions, or a medium with surfactants like Tween 80 to simulate lipid-rich environments.
- Temperature: Maintain at 37°C ± 0.5°C.
- Procedure: Immerse the DES in the release medium with continuous agitation. At predetermined time points (e.g., 1, 4, 24, 48 hours, then weekly up to 90 days), withdraw and replace the entire medium. Analyze the collected samples using a validated high-performance liquid chromatography (HPLC) or LC-MS/MS method to quantify the drug concentration.
- Data Analysis: Plot cumulative drug release (%) versus time to generate the release profile. Model the data to understand the release kinetics (e.g., biphasic release: initial burst followed by sustained release) [6].
Coating Integrity and Characterization
Objective: To assess the uniformity, adhesion, and morphology of the polymer-drug coating on the stent struts. Methodology:
- Scanning Electron Microscopy (SEM): Image the coated stent before and after expansion (using a balloon catheter in a fixture) at various magnifications. Evaluate for cracks, delamination, or webbing between struts.
- Atomic Force Microscopy (AFM): Perform to determine surface roughness and coating thickness at the nanoscale.
- Differential Scanning Calorimetry (DSC): Analyze the thermal properties of the coating (e.g., glass transition temperature, polymer crystallinity) which can affect drug release and stability.
- FTIR Spectroscopy: Confirm the chemical integrity of the polymer and drug, and identify any potential interactions between them [6].
Biological Efficacy and Safety Testing
Objective: To evaluate the biological response to the DES, including antiproliferative efficacy and biocompatibility. Methodology:
- Cell Culture Studies:
- Smooth Muscle Cell (SMC) Proliferation Assay: Treat human coronary SMCs with stent eluents or use direct contact models. Use assays like MTT or BrdU to quantify cell proliferation after 24-72 hours. Compare against control groups (bare stent, stent with polymer only).
- Endothelial Cell (EC) Migration and Viability: Assess the re-endothelialization potential by studying EC viability and migration (e.g., using a scratch assay) under the influence of stent eluents.
- Animal Implantation Model (e.g., Porcine Coronary Artery):
- As per U.S. FDA recommendations, implant the test DES, a control bare metal stent, and a commercially approved DES (positive control) in coronary arteries of healthy pigs.
- Endpoint (28-90 days): Perform histomorphometric analysis of the explanted arteries to measure key parameters: Neointimal Area, Lumen Area, and Percent Area Stenosis. Evaluate inflammation scores around the struts and endothelialization status [6].
Diagram 1: DES evaluation workflow showing in vitro, biological, and clinical stages.
Signaling Pathways of DES Drugs
The antiproliferative drugs used in DES primarily target cell cycle progression in smooth muscle cells to prevent neointimal hyperplasia. The two main classes, Limus-family drugs and paclitaxel, operate through distinct mechanisms.
Limus-family drugs (e.g., Sirolimus, Everolimus, Zotarolimus) are macrocyclic lactones. They first cross the cell membrane and bind with high affinity to the cytosolic immunophilin FK506 Binding Protein 12 (FKBP12). This drug-FKBP12 complex then directly binds to and inhibits the mammalian Target of Rapamycin (mTOR), a critical serine/threonine kinase. mTOR inhibition blocks the progression of the cell cycle from the G1 phase to the S phase by preventing the phosphorylation of key downstream substrates like p70S6 kinase and 4E-BP1, ultimately leading to cell cycle arrest and inhibition of SMC proliferation [79].
Paclitaxel, a taxane derivative, operates via a microtubule-stabilizing mechanism. It binds directly to the β-subunit of tubulin in cellular microtubules, promoting microtubule assembly and stabilizing them against depolymerization. This stabilization disrupts the normal dynamic reorganization of the microtubule network that is essential for vital interphase and mitotic cellular functions. Consequently, paclitaxel arrests cells in the G2/M phase of the cell cycle, preventing cell division and inducing apoptosis [6] [79].
Diagram 2: Key signaling pathways for Limus-family drugs and Paclitaxel.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents, materials, and instruments essential for conducting rigorous DES-related research, from basic coating development to biological evaluation.
Table 3: Essential Research Reagents and Materials for DES Development
| Item/Category | Function/Application | Specific Examples & Notes |
|---|---|---|
| Antiproliferative Drugs | Active pharmaceutical ingredient to inhibit neointimal hyperplasia. | Sirolimus, Everolimus, Zotarolimus, Paclitaxel. Require high purity and stability testing. |
| Biocompatible Polymers | Coating matrix for controlled drug delivery and enhanced biocompatibility. | Durable: Fluorinated polymers. Bioresorbable: Polylactic acid (PLA), Poly(lactic-co-glycolic acid) (PLGA). |
| HPLC / LC-MS/MS System | Quantification of drug content and in vitro release kinetics. | Systems with UV/PDA or mass spectrometry detection. Validated methods are required. |
| Scanning Electron Microscope (SEM) | High-resolution imaging of stent coating morphology, uniformity, and integrity pre-/post-expansion. | Critical for assessing coating defects like cracking or delamination. |
| Cell Lines | In vitro models for efficacy and safety testing. | Human Coronary Artery Smooth Muscle Cells (HCASMCs): For antiproliferative assessment. Human Coronary Artery Endothelial Cells (HCAECs): For re-endothelialization potential. |
| Animal Implantation Model | Preclinical in vivo assessment of safety and efficacy. | Porcine Model: Standard for coronary stent evaluation due to anatomical and physiological similarities to humans. |
| Dissolution Apparatus & Media | Simulating the physiological environment for drug release studies. | USP Apparatus 7 (reciprocating holder) or flow-through cells. Media: PBS pH 7.4, often with surfactants (Tween 80, SDS). |
Drug-eluting stents (DES) represent the standard of care in percutaneous coronary intervention (PCI), designed to mitigate the risk of in-stent restenosis (ISR) through the localized delivery of antiproliferative agents. The platform for drug delivery—specifically, the use of a polymer coating or polymer-free technologies—is a critical determinant of stent performance, influencing both drug release kinetics and long-term vessel healing. Polymer-based DES utilize a polymer coating to control the elution of the drug, while polymer-free DES aim to eliminate long-term polymer presence, thereby theoretically reducing the risks of chronic inflammation and delayed arterial healing associated with durable polymers [10] [80]. Despite technological advancements, the comparative efficacy and safety profiles of these platforms, particularly in complex patient and lesion subsets, remain a central focus of interventional cardiology research. This application note synthesizes current evidence and provides detailed experimental protocols for the preclinical and clinical evaluation of these technologies, framed within a broader thesis on stent coating and application techniques.
Current Clinical Evidence and Outcomes
Recent meta-analyses and randomized controlled trials (RCTs) have provided robust data comparing contemporary polymer-free DES (PF-DES) and biodegradable polymer DES (BP-DES). The overall consensus indicates comparable clinical performance for most endpoints, with nuanced differences emerging in specific clinical scenarios.
Table 1: Key Clinical Outcomes from Meta-Analysis of PF-DES vs. BP-DES (12-Month Follow-Up)
| Outcome | Pooled Risk Ratio (PF-DES vs. BP-DES) | 95% Confidence Interval | Heterogeneity (I²) |
|---|---|---|---|
| Target Lesion Revascularization (TLR) | 1.51 | 0.83 – 2.75 | >50% |
| Myocardial Infarction (MI) | Not Significant | Not Reported | Not Significant |
| All-Cause Death | Not Significant | Not Reported | Not Significant |
| Stent Thrombosis | Not Significant | Not Reported | Not Significant |
| Cardiac Death (BioFreedom PF-DES only) | 0.57 | 0.35 – 0.90 | Not Reported |
Source: Adapted from [10]
Table 2: Outcomes in Specific Patient Subgroups
| Subgroup | Stent Types Compared | Primary Outcome | Key Finding |
|---|---|---|---|
| Patients with Diabetes Mellitus | Polymer-free Amphilimus-eluting Stent (PF-AES) | 12-month MACE (Cardiac death, TVMI, revascularization) | No significant difference between DM and non-DM groups (adjusted HR 1.20; 95% CI 0.63–2.30) [81] [82] |
| All-Comer Patients | PF-AES vs. Biodegradable-Polymer EES | 1-year Device-Oriented Composite Endpoint | PF-AES non-inferior (8.2% vs. 7.2%; risk difference 1%) [40] |
| All-Comer Patients | PF-AES vs. Biodegradable-Polymer EES | Definite/Probable Stent Thrombosis | Higher with PF-AES (1.0% vs. 0.3%; HR 3.72, 95% CI: 1.04-13.33) [40] |
| AMI with Cardiogenic Shock | DP-DES vs. BP-DES | 12-month Target Vessel Failure | No significant difference (34.2% vs. 28.5%; adjusted HR 0.98, 95% CI: 0.77–1.27) [80] |
| Small Vessel CAD | BP-DES vs. DP-DES | 2-year Target Lesion Failure | Significant reduction with BP-DES, not sustained at 5 years [83] |
Evidence Interpretation
The data reveals that while PF-DES and BP-DES show broad comparability in efficacy endpoints like TLR, safety signals may differ. The increased risk of early stent thrombosis observed with some PF-DES platforms warrants careful consideration of antiplatelet therapy regimes [40]. Conversely, device-specific benefits, such as the significant reduction in cardiac death associated with the BioFreedom stent, highlight that technological variations within a category can profoundly impact clinical outcomes [10]. In high-risk anatomical settings like small vessel disease, BP-DES may offer mid-term advantages in composite efficacy endpoints [83].
Experimental Protocols for Preclinical Evaluation
A standardized preclinical assessment is crucial for evaluating new DES coatings and platforms. The following protocol outlines key experiments.
Protocol 1: In Vitro Drug Release and Coating Characterization
Objective: To quantify drug release kinetics and assess coating integrity and uniformity.
- Materials:
- Test DES and control DES
- USP Apparatus 4 (flow-through cell) or Apparatus 7 (reciprocating holder)
- Phosphate-buffered saline (PBS) with 0.05% Tween 80 (or similar surfactant) as release medium, maintained at 37°C
- High-Performance Liquid Chromatography (HPLC) system for drug quantification
- Scanning Electron Microscopy (SEM) for coating surface morphology
- Procedure:
- Sample Preparation: Place each stent (n=3-6) into a separate flow-through cell.
- Drug Release: Circulate the release medium at a constant flow rate (e.g., 16 mL/min). Collect eluent samples at predetermined time points (e.g., 1h, 6h, 1, 2, 3, 7, 14, 21, 28 days).
- Drug Quantification: Analyze samples via HPLC to determine drug concentration. Calculate cumulative drug release over time.
- Coating Integrity: Pre- and post-release, image stent struts using SEM to evaluate coating uniformity, surface characteristics, and presence of cracks or delamination.
- Data Analysis: Generate a drug release profile. Fit data to kinetic models (e.g., zero-order, first-order, Higuchi) to understand release mechanisms. Report mean release rates and coating morphology descriptively [6].
Protocol 2: In Vivo Assessment of Vascular Healing and Safety
Objective: To evaluate arterial healing, inflammation, and neointimal formation in a relevant animal model.
- Materials:
- Healthy porcine or rabbit model (e.g., Yorkshire pig)
- Test DES, control DES (e.g., market-leading BP-DES/DP-DES), and Bare Metal Stent (BMS)
- Optical Coherence Tomography (OCT) or Intravascular Ultrasound (IVUS)
- Histopathology equipment and stains (H&E, Elastic Van Gieson)
- Procedure:
- Stent Implantation: Implant stents in coronary or iliofemoral arteries following standard surgical and angiographic techniques. Adhere to animal welfare guidelines.
- Follow-up: Terminate animals at pre-defined endpoints (e.g., 28 days for early healing, 90 and 180 days for long-term outcomes).
- Angiographic and OCT/IVUS Analysis: Before termination, perform angiography and OCT/IVUS to assess lumen diameter, neointimal hyperplasia area, and stent apposition.
- Histopathological Analysis: Process explanted arteries for histology. Key assessments include:
- Injury Score: Quantify vessel injury based on strut penetration.
- Inflammation Score: Grade inflammatory response around each strut (0-3 scale).
- Neointimal Thickness/Area: Measure the thickness of the neointimal layer.
- Endothelialization Score: Assess the percentage of struts covered by endothelium.
- Data Analysis: Compare scores and measurements between test and control groups using appropriate statistical tests (e.g., ANOVA). Superior performance is indicated by lower inflammation and neointimal area, with complete endothelialization [80] [6].
Diagram 1: Preclinical evaluation workflow for DES. Integrated data from in vitro and in vivo studies informs the decision to advance to clinical trials.
Signaling Pathways in In-Stent Restenosis and DES Action
The efficacy of DES is mediated through the disruption of key signaling pathways that drive neointimal hyperplasia, the primary pathological process in ISR.
Diagram 2: Key signaling pathways in ISR and DES drug mechanisms. Stent injury triggers a cascade leading to Smooth Muscle Cell (SMC) proliferation. Limus drugs and paclitaxel inhibit this process via distinct pathways.
The central pathway involves:
- Vessel Injury: Stent implantation causes endothelial denudation and mechanical injury.
- Inflammatory Response: Platelet activation and fibrin deposition release chemotactic agents (IL-8, MCP-1) and cytokines (IL-1, IL-6, TNF-α) [6].
- Growth Factor Release: Cytokines stimulate the production of growth factors (PDGF, FGF, VEGF, TGFβ), which are potent mitogens for SMCs [6].
- SMC Proliferation and Migration: Signaling from these growth factors prompts SMCs to migrate from the tunica media to the intima and proliferate, forming neointimal tissue.
- DES Drug Action:
- Limus-family drugs (Sirolimus, Everolimus, Biolimus): Form a complex with FKBP-12, which binds to and inhibits the mTOR (mammalian Target of Rapamycin) pathway. This arrest SMCs and endothelial cells in the late G1 phase of the cell cycle, preventing proliferation [6].
- Paclitaxel: Binds to and stabilizes microtubules, preventing their disassembly. This disrupts cell division, intracellular transport, and migration, ultimately leading to apoptosis (programmed cell death) [6].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for DES Coating and Evaluation
| Category / Reagent | Example Products / Components | Primary Function in Research |
|---|---|---|
| Stent Platforms | Cobalt-Chromium (CoCr) alloy, Stainless Steel, Nitinol (for peripheral DES) | Provides the mechanical scaffold; base for coating. |
| Biodegradable Polymers | Poly(L-lactide) (PLLA), Poly(D,L-lactide-co-glycolide) (PLGA) | Controls drug release rate; degrades over time post-drug elution. |
| Durable Polymers | Poly(n-butyl methacrylate) (PBMA), Poly(vinylidene fluoride-co-hexafluoropropylene) (PVDF-HFP) | Provides permanent, controlled drug release matrix. |
| Antiproliferative Drugs | Sirolimus (Rapamycin), Everolimus, Zotarolimus, Biolimus A9, Paclitaxel | Inhibits smooth muscle cell proliferation to prevent restenosis. |
| Coating Solvents | Dimethylacetamide (DMAc), Tetrahydrofuran (THF), Acetone, Chloroform | Dissolves drug and polymer for spray or dip coating. |
| In Vitro Release Media | Phosphate Buffered Saline (PBS), PBS with surfactants (e.g., Tween 80) | Simulates physiological conditions for drug release testing. |
| Characterization Tools | Scanning Electron Microscopy (SEM), High-Performance Liquid Chromatography (HPLC) | Analyzes coating morphology and quantifies drug release. |
The choice between polymer-based and polymer-free DES platforms involves a nuanced trade-off. Current evidence demonstrates that both biodegradable polymer DES and polymer-free DES offer comparable and excellent efficacy in preventing target lesion revascularization [10]. However, the decision must be individualized, considering specific device characteristics, such as the potential for reduced cardiac death with the BioFreedom PF-DES [10], alongside the observed increase in early stent thrombosis with another PF-AES platform [40]. The ongoing evolution of stent technology—including the development of bioresorbable scaffolds, novel drug formulations like amphilimus, and personalized coating solutions—continues to shape this dynamic field. Future research should focus on long-term outcomes, head-to-head comparisons of specific devices, and the development of personalized approaches based on patient-specific risk factors like diabetes and high bleeding risk.
Drug-coated balloons (DCBs) have emerged as a compelling alternative to drug-eluting stents (DES) in the treatment of coronary artery disease (CAD), offering a "leave nothing behind" strategy that avoids permanent vascular scaffold implantation. [2] [84] While DES reduce restenosis by delivering antiproliferative drugs from a permanent metallic platform, they carry risks of late stent thrombosis, neoatherosclerosis, and require prolonged dual antiplatelet therapy (DAPT). [84] DCBs were initially developed for managing in-stent restenosis (ISR) but have expanded to broader indications including small vessel disease and bifurcation lesions. [2] The fundamental technological difference lies in the delivery mechanism: DCBs transfer antiproliferative drugs directly to the arterial wall during brief balloon inflation using excipients that enhance drug bioavailability, while DES provide sustained elution from a permanent implant. [2]
Two primary antiproliferative drugs dominate these technologies. Paclitaxel, used in most DCBs, inhibits the cell cycle by causing M-phase arrest through microtubule stabilization, rapidly transferring into vascular tissue due to high lipophilicity. [2] [84] Sirolimus (and its analogs), more common in DES, inhibits mTOR signaling leading to reversible cell cycle arrest at the G1/S phase, though its poorer arterial wall penetration historically limited DCB applications until novel excipients like nanocarriers improved delivery. [2] The excipient technology is crucial for DCB performance, with substances like iopromide, urea, shellac, and citrate derivatives enhancing drug adhesion, stability, and transfer to the vessel wall. [2]
Table 1: Key Antiproliferative Drug Comparative Pharmacology
| Parameter | Paclitaxel-Based DCB | Sirolimus-Based DCB | Limus-Based DES |
|---|---|---|---|
| Mechanism | Microtubule stabilization, M-phase arrest | mTOR inhibition, G1/S phase arrest | mTOR inhibition, G1/S phase arrest |
| Cellular Uptake | Rapid, high lipophilicity | Slower, requires enhanced formulations | Sustained release from polymer |
| Tissue Retention | Prolonged (>14 days) | Shorter duration | Continuous elution (weeks-months) |
| Excipient Role | Critical for initial transfer | Essential for penetration and retention | Polymer controls release kinetics |
Quantitative Outcomes and Comparative Evidence
Recent randomized controlled trials and meta-analyses have generated substantial evidence comparing DCBs and DES across various clinical scenarios. For in-stent restenosis (ISR), a mixed treatment comparison meta-analysis of 18 RCTs encompassing 3,820 patients found both DCBs and DES significantly reduced major adverse cardiovascular events (MACE) compared to plain old balloon angioplasty (POBA), with no significant difference in clinical outcomes between DCB and DES at mean 18-month follow-up. [85] The AGENT IDE trial demonstrated DCB's superiority over POBA for ISR, with significantly reduced target lesion failure (27% vs. 34%) at 2-year follow-up, leading to FDA approval of the AGENT DCB for this indication. [84]
For de novo coronary artery disease, evidence varies by lesion complexity. The REC-CAGEFREE I trial (n=2,272) failed to prove non-inferiority of DCBs to DES for non-complex lesions (device-oriented composite endpoint: DCB 6.4% vs. DES 3.4%). [2] However, in small vessel disease (SVD), the Dissolve SVD trial (n=277) established DCB non-inferiority to DES for in-segment diameter stenosis at 9 months, while the ANDROMEDA meta-analysis (n=1,475) found DCBs associated with lower MACE risk than DES at 3 years (HR 0.67, 95% CI 0.47-0.96). [2]
In acute coronary syndrome (ACS), a real-world retrospective study (n=168) found no significant MACE difference between DCB and DES at 12 months (11.9% vs. 10.9%, p=0.64), despite the DCB cohort having more complex patients with higher rates of prior PCI and myocardial infarction. [86] This suggests DCBs may be particularly valuable in ACS patients where impaired vasomotion and thrombotic risks make permanent implants less desirable.
Table 2: Key Randomized Trial Outcomes: DCB versus DES
| Trial Name | Population | N | Follow-up | Primary Endpoint | DCB Result | DES Result | Conclusion |
|---|---|---|---|---|---|---|---|
| REC-CAGEFREE I [2] | De novo non-complex CAD | 2,272 | 2 years | Device-oriented composite endpoint | 6.4% | 3.4% | Failed non-inferiority |
| Dissolve SVD [2] | De novo small vessel CAD | 277 | 9 months | In-segment diameter stenosis | 31.2% ± 2.0% | 26.1% ± 2.1% | Proven non-inferiority |
| AGENT IDE [84] | ISR | 600 | 2 years | Target lesion failure | 27% | 34% (POBA) | Superior to POBA |
| PEPCAD II [84] | ISR | 131 | 6 months | Late lumen loss | 0.17 ± 0.42 mm | 0.38 ± 0.61 mm | Superior to PES |
Real-world safety data from the FDA MAUDE database identified device-related complications with the AGENT DCB, including balloon rupture (33.55% of reports) and shaft breakage (10.32%), though many reports described off-label use in de novo lesions. [87] Injury outcomes included angina (32.84%), acute myocardial infarction (29.85%), and coronary perforation (8.95%), highlighting the importance of optimal lesion preparation and device selection. [87]
Experimental Protocols and Methodologies
Preclinical DCB Efficacy Testing Protocol
Objective: Evaluate the efficacy and safety of novel DCB formulations in porcine coronary model.
Materials:
- Juvenile domestic swine (25-30 kg)
- Test DCB devices (various drug/excipient combinations)
- Control devices (POBA, DES)
- Quantitative coronary angiography (QCA) system
- Optical coherence tomography (OCT) or intravascular ultrasound (IVUS)
- Histopathology equipment
Methodology:
- Anesthesia and Preparation: Induce anesthesia with ketamine (20 mg/kg) and xylazine (2 mg/kg), maintain with isoflurane (1.5-2.5%). Administer aspirin (325 mg) and clopidogrel (300 mg) via nasogastric tube pre-procedure.
- Arterial Access: Perform carotid or femoral artery cutdown, introduce 7F sheath. Administer heparin (100-200 IU/kg) to maintain ACT >250s.
- Vessel Injury: Under fluoroscopic guidance, introduce oversized balloon (1.1:1.0 balloon:artery ratio) to target coronary arteries, inflate to 8-10 atm for 30s to create denudation injury.
- Device Application: After 28 days, randomize injured segments to receive test DCB, control POBA, or DES following manufacturer's instructions for inflation time/pressure.
- Follow-up Assessment: At 28 days post-treatment, perform QCA, OCT/IVUS, then euthanize for histopathological analysis.
Endpoint Measurements:
- Angiographic: Late lumen loss, binary restenosis (>50% diameter stenosis)
- Histopathological: Neointimal area, inflammation score (0-3), endothelialization score (1-3)
- Morphometric: Vessel area, lumen area, neointimal thickness
This protocol directly supports the evaluation of neointimal suppression and vascular healing parameters critical for regulatory approval, as referenced in the AGENT IDE trial methodology. [84]
Clinical Angiographic Restenosis Assessment Protocol
Objective: Quantitatively compare angiographic outcomes between DCB and DES in randomized clinical trials.
Materials:
- Digital angiography system with standardized acquisition settings
- Quantitative coronary angiography (QCA) software
- Core laboratory with blinded analysts
- Standardized catheter for calibration
Methodology:
- Baseline Angiography: Acquire images in identical projections before and immediately after intervention, noting gantry angles for follow-up.
- QCA Analysis:
- Calibrate using contrast catheter or guide catheter as reference
- Define analysis segment including treated area + 5mm margins
- Automatically detect lumen contours with manual correction
- Calculate reference vessel diameter, minimum lumen diameter, percent diameter stenosis
- Follow-up Protocol: Repeat identical projections at predetermined intervals (typically 6-9 months) using identical calibration methods.
- Endpoint Calculation:
- Late lumen loss = Post-procedure MLD - Follow-up MLD
- Binary restenosis = >50% diameter stenosis at follow-up
- Target lesion revascularization driven by angiographic restenosis with symptoms/ischemia
This standardized QCA methodology underpins the angiographic outcomes reported in trials like PEPCAD II and Dissolve SVD, enabling valid cross-trial comparisons. [2] [84]
Signaling Pathways and Mechanisms
Diagram 1: Drug Mechanisms in DCB and DES Technologies
Research Reagent Solutions
Table 3: Essential Research Reagents for DCB/DES Development
| Reagent Category | Specific Examples | Research Function | Technical Notes |
|---|---|---|---|
| Antiproliferative Drugs | Paclitaxel, Sirolimus, Everolimus, Zotarolimus | Primary therapeutic agents | Paclitaxel preferred for DCB due to rapid uptake; sirolimus requires advanced formulations |
| Excipient Technologies | Iopromide, Urea, Shellac, BTHC, ATBC, Nanocarriers | Enhance drug transfer and retention | Critical for DCB performance; hydrophilic properties improve tissue penetration |
| Coating Matrices | Phosphorylcholine, Poly-lactide-co-glycolide, Polyvinylpyrrolidone | Control drug release kinetics | DES polymers require biocompatibility; DCB coatings need fracture resistance |
| In Vitro Test Systems | Human coronary smooth muscle cells, Endothelial cell cultures | Preliminary efficacy screening | Assess cytotoxicity, proliferation inhibition, migration suppression |
| Animal Models | Porcine coronary injury model, Rabbit iliac injury model | Preclinical safety/efficacy | Porcine model best predicts human vascular response |
| Analytical Methods | HPLC-MS drug quantification, Scanning electron microscopy | Coating characterization and quality control | Ensure uniform coating distribution and drug stability |
Clinical Application Protocols
DCB Application for In-Stent Restenosis
Indications: ISR of bare-metal or drug-eluting stents with >70% diameter stenosis associated with symptoms or ischemia. [84]
Contraindications:
- Flow-limiting dissections after predilatation
- Vessel diameter >4.0mm or <2.0mm
- Lesions requiring mechanical atherectomy
- Contraindication to recommended DAPT
Procedure Protocol:
- Lesion Preparation:
- Perform predilatation with non-compliant balloon (balloon:vessel ratio 0.8-1.0:1)
- Use high-pressure inflation (14-18 atm) to adequately expand underexpanded stent if present
- Assess result with OCT/IVUS if available to rule out mechanical issues
- DCB Selection:
- Choose DCB with documented efficacy for ISR (e.g., AGENT, SeQuent Please)
- Match balloon length to cover entire ISR segment + 2-3mm margins
- Select nominal diameter matching 1:1 vessel reference diameter
- DCB Delivery:
- Avoid pre-dilation balloon contact with DCB during delivery
- Inflate to nominal pressure (typically 7-8 atm) for recommended time (30-60s)
- Maintain steady inflation without "pumping"
- Post-DCB Assessment:
- Check for flow-limiting dissections (Type C-F)
- If significant dissection persists, consider bailout stenting
- Avoid post-dilatation unless necessary, then use non-compliant balloon
Medication Regimen:
- Pre-procedure: Aspirin (75-325mg), clopidogrel (600mg) or ticagrelor (180mg)
- Intra-procedure: Unfractionated heparin (70-100 IU/kg)
- Post-procedure: DAPT for 1-3 months (aspirin indefinitely)
This protocol aligns with the techniques used in the AGENT IDE and PEPCAD II trials that established DCB efficacy for ISR. [84]
DCB for De Novo Small Vessel Disease Protocol
Indications: De novo lesions in coronary vessels with reference diameter 2.0-2.75mm, length <25mm. [2]
Key Considerations:
- Optimal lesion preparation is critical
- Avoid geographic mismatch between preparation balloon and DCB
- Residual stenosis <30% after preparation suggests DCB suitability
Procedure Protocol:
- Vessel Assessment:
- Pre-procedure IVUS/OCT recommended for vessel sizing
- Reference diameter measurement using distal marker or QCA
- Lesion Preparation:
- Semi-compliant balloon predilatation (balloon:vessel 1:1)
- Moderate pressure (8-12 atm) until waist disappearance
- Assess for dissections - only Type A/B dissections acceptable for DCB alone
- DCB Application:
- Select DCB with clinical evidence in SVD (e.g., SeQuent Please, Pantera Lux)
- DCB should cover prepared segment completely
- Minimum 60s inflation time at nominal pressure
- Bailout Stenting Indications:
- Flow-limiting dissection (Type C-F)
- Significant recoil (>50%)
- Persistent residual stenosis >30%
- Slow or no-reflow phenomenon
Medication Regimen: Similar to ISR protocol with DAPT duration of 1-3 months based on bleeding risk.
This methodology reflects the approaches used in the BASKET-SMALL 2 and Dissolve SVD trials that demonstrated DCB non-inferiority to DES in SVD. [2]
DCB technology represents a paradigm shift in percutaneous coronary intervention, offering a stent-less approach that mitigates many long-term limitations of permanent implants. While DES remain superior for many de novo lesions based on current evidence, DCBs have established definitive roles in ISR and small vessel disease, with expanding applications in bifurcations, ACS, and patients with high bleeding risk. [2] [85] [86] The ongoing development of sirolimus-based DCBs and improved excipient technologies promises to enhance DCB performance, potentially expanding indications. Future research directions should focus on optimizing lesion preparation techniques, identifying patient and lesion characteristics most suitable for DCB therapy, and developing standardized protocols for complex lesion subsets. As the evidence base matures with longer-term follow-up from recent trials, DCBs are poised to play an increasingly prominent role in the interventional cardiology arsenal, particularly for clinical scenarios where avoiding permanent implants provides tangible benefits.
The efficacy of a drug-eluting stent (DES) is intrinsically linked to the performance of its polymer coating and drug delivery system. Intravascular imaging, specifically Intravascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT), has emerged as a critical in vivo methodology for the preclinical and clinical validation of these technologies. These modalities move beyond traditional angiographic assessment by providing high-resolution, cross-sectional data on stent-vessel interactions and the biological response to the implanted device [88]. For researchers and scientists developing next-generation coatings, IVUS and OCT provide indispensable quantitative metrics on stent integration, drug distribution effects, and long-term vascular healing, thereby bridging the gap between benchtop characterization and clinical outcomes [3].
This document outlines standardized application notes and experimental protocols for utilizing IVUS and OCT in the context of DES coating performance assessment, providing a framework for robust and reproducible research.
Technical Specifications and Comparative Analysis
IVUS and OCT offer complementary strengths for stent performance evaluation, governed by their underlying physical principles. IVUS utilizes high-frequency ultrasound (20-65 MHz), providing deep tissue penetration (4-8 mm) ideal for assessing vessel remodeling and stent expansion in large vessels [89] [88]. OCT employs near-infrared light (≈1310 nm wavelength) to achieve an axial resolution of 10-20 µm, approximately ten times greater than IVUS, enabling exquisite detail of the stent-tissue interface and superficial vessel layers [89] [88].
Table 1: Core Technical Specifications of IVUS and OCT [89] [88] [90]
| Parameter | IVUS | OCT |
|---|---|---|
| Energy Source | Ultrasound | Near-infrared light |
| Typical Frequency / Wavelength | 40-65 MHz | 1310 nm |
| Axial Resolution | 22-100 µm | 10-20 µm |
| Tissue Penetration | 4-8 mm | 1-3 mm |
| Blood Clearance Required | No | Yes (contrast flush) |
| Key Strength in DES Assessment | Vessel remodeling, stent expansion | Strut coverage, neointimal characterization |
The clinical evidence supporting intravascular imaging guidance for optimizing stent deployment is robust. A large network meta-analysis of 28 randomized controlled trials demonstrated that IVUS-guided percutaneous coronary intervention (PCI) significantly reduces the risk of major adverse cardiovascular events (MACE) compared to angiography-guided procedures (Risk Ratio: 0.62) [91]. This outcome is closely linked to achieving optimal stent expansion and apposition, parameters directly measurable by IVUS and OCT.
Table 2: Key Clinical Outcomes from Imaging-Guided PCI Trials [91] [90]
| Intervention | Risk Ratio for MACE vs. Angiography | Key Supported Outcomes |
|---|---|---|
| IVUS-guided PCI | 0.62 (95% CI: 0.46-0.85) [91] | Reduced cardiac mortality, target lesion revascularization, and stent thrombosis [90]. |
| OCT-guided PCI | Data varies by trial and complexity [90] | Superior stent expansion and apposition; enhanced detection of procedure-related complications [88]. |
Validation Parameters for Coating Performance
Intravascular imaging provides quantitative and qualitative metrics essential for evaluating DES coating performance and its biological sequelae.
Post-Implantation Stent Assessment
- Stent Expansion: Measured as the minimum stent area (MSA) divided by the average reference lumen area. IVUS is particularly robust for this due to its deep penetration [92] [90]. Incomplete expansion is a primary correlate of stent failure.
- Stent Apposition: The distance from the stent strut to the vessel wall. Both IVUS and OCT detect malapposition, but OCT's superior resolution allows for detection of minor malapposition not visible on IVUS [88].
Follow-up Vascular Healing Assessment
- Strut Coverage: A critical parameter for assessing the completion of endothelialization and the risk of late stent thrombosis. OCT's high resolution makes it the gold standard for measuring neointimal thickness over individual struts and classifying struts as "covered" or "uncovered" [89] [88].
- Neointimal Characterization: OCT can differentiate between homogeneous (benign) and heterogeneous (concerning) neointimal tissue, and can identify features like neoatherosclerosis within the stented segment [88]. This is crucial for understanding the long-term biological response to the polymer and drug.
Figure 1: Core Workflow for DES Coating Validation. This diagram outlines the primary stages for using intravascular imaging in a longitudinal study to assess drug-eluting stent coating performance.
Experimental Protocols
Protocol 1: IVUS for Vessel Sizing and Stent Expansion
Objective: To utilize IVUS for precise vessel measurement to guide stent selection and to quantitatively confirm optimal stent expansion post-deployment.
Methodology:
- Image Acquisition: Pre-dilate the lesion if necessary. Advance the IVUS catheter distal to the target lesion. Initiate an automatic motorized pullback at 0.5-1.0 mm/s to a point proximal to the segment of interest [92]. Administer intracoronary nitrates prior to imaging to prevent vasospasm.
- Pre-Stenting Analysis: Identify the proximal and distal reference segments, defined as the sites with the largest lumen within 10 mm of the lesion without major intervening branches [92]. Measure the Lumen Area and Vessel Area (defined by the border of the external elastic membrane) at these references. The Stent Diameter should be selected based on the median reference vessel diameter.
- Post-Stenting Analysis: Repeat the pullback through the stented segment. Measure the Minimum Stent Area (MSA). Calculate Stent Expansion as: (MSA / Average Reference Lumen Area) × 100%. An expansion of ≥80% is often targeted [90]. Systemically inspect for strut malapposition.
Protocol 2: OCT for Strut Coverage and Apposition
Objective: To employ high-resolution OCT for the detailed assessment of stent strut coverage, tissue characteristics, and precise malapposition at follow-up.
Methodology:
- Image Acquisition: Advance the OCT catheter distal to the stent. Perform a contrast flush (e.g., 8-16 mL via a power injector) to clear blood from the field. Initiate an automated pullback (18-36 mm/s) during flush acquisition [89].
- Image Analysis (Per 1-mm Cross-Section):
- Strut Apposition: Measure the distance from the strut's luminal surface to the vessel wall. A distance greater than the strut thickness + polymer coating (e.g., >70 µm for modern DES) is typically considered malapposed [88].
- Strut Coverage: A strut is classified as "covered" if a tissue layer is visible over its luminal surface. Measure the Neointimal Thickness on covered struts. The percentage of Uncovered Struts is a key safety endpoint.
- Neointimal Characterization: Qualify the tissue covering the struts as Homogeneous (uniform, high-signal), Heterogeneous (irregular, low-signal), or Layered [88].
Figure 2: OCT Strut-Level Analysis Logic. This decision tree outlines the step-by-step qualitative and quantitative assessment of individual stent struts during follow-up analysis.
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of intravascular imaging studies requires specific tools and reagents. The following table details essential items for a research cath lab.
Table 3: Essential Research Materials for Intravascular Imaging Studies
| Item | Function / Application | Considerations |
|---|---|---|
| IVUS Console & Catheter | Provides console and single-use catheter for ultrasound-based image acquisition. | Available in mechanical rotating and phased-array designs. High-definition (40-65 MHz) systems offer superior resolution [92]. |
| OCT Console & Catheter | Provides console and single-use catheter for light-based image acquisition. | Frequency-domain systems are standard. Requires blood clearance via contrast flush for operation [89]. |
| Automated Pullback Device | Standardizes catheter withdrawal speed during image acquisition. | Critical for volumetric analysis and reproducible longitudinal assessment. Speeds vary (IVUS: 0.5-10 mm/s; OCT: 18-36 mm/s) [92] [89]. |
| Intracoronary Nitroglycerin | Vasodilator administered prior to imaging. | Prevents catheter-induced vasospasm and ensures vessel dimensions are measured at maximal dilation [92]. |
| Radiopaque Contrast Media | Used for angiography and as a flush medium for OCT. | Clears blood from the vessel to enable light-based imaging. Iso-osmolar agents may be preferred for patient safety. |
| Dedicated Imaging Analysis Software | Software for quantitative measurement of lumen/stent dimensions, plaque burden, and strut-level analysis. | Enables precise, core-lab caliber measurements. Essential for calculating key endpoints like stent expansion and neointimal thickness. |
Drug-eluting stents (DES) represent a cornerstone of percutaneous coronary intervention (PCI), fundamentally revolutionizing the management of coronary artery disease by significantly reducing the need for repeat revascularizations compared to their bare-metal predecessors [27]. The long-term clinical success of these devices is intrinsically linked to their coating technologies and application techniques, which control the elution of antiproliferative drugs to prevent in-stent restenosis [8] [6]. While first-generation DES demonstrated efficacy in reducing restenosis, they raised concerns regarding late stent thrombosis attributed to delayed arterial healing and polymer-induced inflammation [8] [27]. Contemporary research focuses on optimizing coating polymers, drug release kinetics, and stent platforms to enhance long-term durability and mitigate very late complications. This document synthesizes critical long-term outcome data and provides standardized experimental protocols for evaluating next-generation DES coatings within the broader thesis research on advanced stent technologies.
Long-Term Clinical Outcomes of Contemporary DES
Table 1: Five-Year Clinical Outcomes from Network Meta-Analysis of Currently Used DES (29 RCTs, n=46,502) [93]
| DES Type | Definite/Probable Stent Thrombosis | All-Cause Mortality | Cardiac Death | Target Lesion Revascularization | Any Myocardial Infarction |
|---|---|---|---|---|---|
| Synergy | Ranked Highest (P-score: 0.85) | Ranked Highest (P-score: 0.76) | Ranked Highest (P-score: 0.87) | - | - |
| Promus | - | - | - | Ranked Highest (P-score: 0.93) | Ranked Highest (P-score: 0.86) |
| Nobori/BioMatrix | - | - | - | - | - |
| Orsiro | - | - | - | - | - |
| Xience | - | - | - | - | - |
| Resolute | - | - | - | - | - |
| Overall Network Comparison | Non-significant differences between all DES | Non-significant differences between all DES | Non-significant differences between all DES | Non-significant differences between all DES | Non-significant differences between all DES |
Note: This network meta-analysis found no statistically significant differences in direct head-to-head comparisons for all 5-year outcomes. Ranking was based on P-scores, with Synergy and Promus generally showing favorable performance across key endpoints [93].
Table 2: Five-Year Outcomes from Real-World Observational Study (RANGO Study, n=646) [94]
| Clinical Endpoint | Overall Population | Diabetic Subgroup | Small-Vessel Disease (≤2.5 mm) |
|---|---|---|---|
| Target Lesion Failure (TLF) | 8.7% | 11.1% | 10.3% |
| Patient-oriented Composite Endpoint (PoCE) | 21.8% | 29.1% | 24.1% |
| Stent Thrombosis | 1.2% | 1.0% | 0% |
Note: The RANGO study assessed the Angiolite (cobalt-chromium, sirolimus-eluting, fluoroacrylate-based polymer) stent in a high-risk real-world population, demonstrating low annualized event rates (<2%/year for TLF) and no signal of late complications [94].
Experimental Protocols for DES Coating Evaluation
Protocol: In Vitro Drug Release Kinetics
Objective: To characterize the drug release profile from a DES coating under both real-time and accelerated conditions.
Background: The release kinetics of antiproliferative drugs are critical for DES efficacy, requiring sustained elution over approximately 3 months to counteract smooth muscle cell proliferation [8] [6]. Accelerated release testing provides a predictive model for long-term performance.
Materials:
- DES test samples (n ≥ 3)
- USP Apparatus 2 (Paddle) or 4 (Flow-Through Cell)
- Suitable release medium (e.g., PBS with 0.05% w/v sodium azide, pH 7.4, ± surfactants)
- Temperature-controlled water bath or oven (37°C ± 0.5°C)
- HPLC or UV-Vis spectrophotometer for drug quantification
Methodology:
- Sample Preparation: Accurately weigh and record the initial weight of each DES sample.
- Apparatus Setup: Place individual DES samples into separate vessels containing a defined volume of release medium (e.g., 50 mL for Apparatus 2). Ensure sink conditions are maintained.
- Real-Time Conditions: Incubate samples at 37°C with gentle agitation. Withdraw aliquots of release medium at predetermined time points (e.g., 1, 4, 8, 24, 48 hours; 7, 14, 21, 28, 35, 42, 56, 84 days) and replace with fresh pre-warmed medium to maintain constant volume.
- Accelerated Conditions: To establish an IVIVC, perform parallel tests at elevated temperatures (e.g., 45°C, 50°C) or with modified medium composition (e.g., increased surfactant concentration) [6].
- Drug Quantification: Analyze withdrawn samples using a validated analytical method (HPLC preferred) to determine cumulative drug release.
- Data Analysis: Plot cumulative drug release (%) versus time. Calculate release rate constants and model the release kinetics (zero-order, first-order, Higuchi, Korsmeyer-Peppas).
Diagram: Experimental Workflow for DES Drug Release Studies
Protocol: Coating Integrity and Surface Characterization
Objective: To evaluate the physical and chemical properties of DES coatings before and after expansion and during drug release.
Background: Coating uniformity, thickness, and integrity directly influence drug release homogeneity and thrombogenicity. Thin-strut stents (≈70 μm) demonstrate superior performance compared to thick-strut designs [27].
Materials:
- Scanning Electron Microscope (SEM)
- Atomic Force Microscope (AFM)
- Optical Coherence Tomography (OCT) system
- Stent expansion fixture
- Digital micrometer or coating thickness gauge
Methodology:
- Pre-expansion Characterization:
- Image unexpanded stent struts using SEM at various magnifications (50X to 5000X) to assess coating uniformity, cracks, or defects.
- Measure coating thickness at multiple points using SEM cross-section or AFM.
- Perform surface roughness analysis via AFM.
Post-expansion Characterization:
- Expand DES to nominal pressure (e.g., 8-14 atm) in a simulated vessel environment or using a standard expansion fixture.
- Repeat SEM imaging to identify coating fractures, webbing, or delamination at bends and connectors.
- Utilize OCT to assess strut apposition and coating deformation in a lumen-mimicking environment.
Stability Testing:
- Perform real-time and accelerated aging studies per ICH Q1 guidelines [6].
- Periodically extract samples and repeat surface characterization to evaluate coating degradation, polymer crystallization, or drug crystallization.
Signaling Pathways of DES-Based Pharmacotherapy
Diagram: Molecular Mechanisms of DES Drugs in Vascular Cells
Figure 1: Key signaling pathways targeted by DES therapeutics. Sirolimus analogs and paclitaxel employ distinct mechanisms to inhibit vascular smooth muscle cell (VSMC) proliferation, the primary driver of in-stent restenosis [27] [6].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for DES Coating Research and Development
| Reagent/Material | Function/Application | Examples/Notes |
|---|---|---|
| Biodegradable Polymers | Coating matrix for controlled drug release; degrades after fulfilling function to eliminate long-term polymer presence [3] [77]. | Poly(L-lactic acid) (PLLA), Poly(lactic-co-glycolic acid) (PLGA), Poly(caprolactone) (PCL) |
| Antiproliferative Drugs | Active pharmaceutical ingredients that inhibit vascular smooth muscle cell proliferation to prevent restenosis [27] [6]. | Sirolimus, Everolimus, Zotarolimus, Novolimus, Paclitaxel |
| Coating Solvents | Dissolve polymer and drug for uniform stent coating application; removed during drying process. | Tetrahydrofuran (THF), Dimethylacetamide (DMAc), Chloroform (requires strict residue control) |
| Bioactive Coatings | Promote endothelialization while inhibiting smooth muscle cell hyperplasia; enhance biocompatibility [77]. | Heparin, Hyaluronic Acid, Anti-CD34 antibodies (for endothelial progenitor cell capture) |
| Metal Alloys | Stent scaffold providing radial strength and vascular support [27]. | Cobalt-Chromium (L605), Platinum-Chromium, Nitinol (Ni-Ti for peripheral), Magnesium (bioresorbable) |
| Characterization Standards | Reference materials for analytical method validation and quality control. | USP DOCUMENTATION, Drug and polymer reference standards, Coated stent performance standards |
Long-term studies extending to 5 years confirm the durable benefits of contemporary drug-eluting stents, with very low rates of target lesion failure and stent thrombosis, even in high-risk patient populations and complex lesions [93] [94]. The evolution of stent coatings—from permanent polymers to advanced biodegradable polymers and polymer-free technologies—has directly addressed the limitations of early DES generations, particularly the risk of very late stent thrombosis. The experimental frameworks and characterization methodologies outlined in this document provide a standardized approach for evaluating next-generation DES coatings, facilitating the development of safer, more effective devices that promote vascular healing while preventing restenosis. As DES technology continues to advance, the integration of personalized approaches based on patient-specific factors and lesion characteristics promises to further optimize long-term outcomes in coronary artery disease management.
Conclusion
The development of drug-eluting stent coatings represents a continuous evolution toward optimized therapeutic outcomes through material science, pharmacological innovation, and advanced application techniques. The field has progressed significantly from early polymer coatings to sophisticated biodegradable and polymer-free systems that address fundamental challenges of thrombosis and restenosis while promoting vascular healing. Future directions point toward personalized medicine approaches including patient-specific stent selection, genetically engineered coatings, 3D-printed personalized stents, and smart stents with sensing capabilities. The integration of computational modeling, nanotechnology, and biomimetic materials will further enhance DES performance, ultimately improving outcomes for millions of patients worldwide affected by coronary artery disease. Continued innovation in coating technologies and application methods remains essential to address persistent challenges and unlock new therapeutic possibilities in interventional cardiology.
References
- 1. Drug-Eluting Stent Use in Percutaneous Coronary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12250108/]
- 2. Drug-Coated Balloons: Recent Evidence and Upcoming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12112549/]
- 3. 2025 Guide: Drug-Eluting Coronary Stent Innovations ... [https://invamed.com/2025-guide-drug-eluting-coronary-stent-innovations-transforming-patient-outcomes/]
- 4. Natural history of coronary stents: 14 year follow-up of drug ... [https://www.sciencedirect.com/science/article/pii/S0019483223001748]
- 5. Coatings for Cardiovascular Stents—An Up-to-Date Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC10817058/]
- 6. Drug delivery, development, and technological aspects for ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X25001632]
- 7. A quantitative study of the effects of a dual layer coating ... [https://www.sciencedirect.com/science/article/abs/pii/S0021929024003828]
- 8. Coating Techniques and Release Kinetics of Drug-Eluting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6542673/]
- 9. Comparison of polymer-coated, drug-eluting self-expandable ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d4pm00312h]
- 10. Polymer-Free Versus Biodegradable Polymer Drug-Eluting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190656/]
- 11. - Drug stents eluting [https://pubmed.ncbi.nlm.nih.gov/17091802/]
- 12. A computational model of coronary arteries with in-stent ... [https://www.nature.com/articles/s41598-025-22291-w]
- 13. Evolutionary perspective of drug stents: from thick polymer to... eluting [https://cardiothoracicsurgery.biomedcentral.com/articles/10.1186/s13019-022-01812-y]
- 14. Evolution of Drug - Eluting Profile: Is a Crystalline... Stent Drug Elution [https://www.emjreviews.com/interventional-cardiology/article/evolution-of-drug-eluting-stent-drug-elution-profile-is-a-crystalline-drug-form-the-ideal-solution/]
- 15. Design, synthesis and antiproliferative activity of novel ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1528235/full]
- 16. - Drug Stents and Balloons—Materials, Structure Designs, and... Eluting [https://pmc.ncbi.nlm.nih.gov/articles/PMC7594099/]
- 17. The Impact of Thin-Strut, Biodegradable Polymer Stent ... [https://citoday.com/articles/2017-jan-feb/the-impact-of-thin-strut-biodegradable-polymer-stent-designs]
- 18. Structural Design and Mechanical Properties of Metal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593961/]
- 19. Enhancing flexibility and strength-to-weight ratio of ... [https://www.sciencedirect.com/science/article/abs/pii/S175161612300615X]
- 20. Radial Force Measurement for Cardiovascular Devices [https://vivitrolabs.com/testing-services/radial-force-measurement/]
- 21. Radial Force [https://medinstitute.com/services/medical-device-testing/radial-force/]
- 22. New Standard Test Method for Vascular Stent Radial ... [https://www.astm.org/news/press-releases/new-standard-test-method-vascular-stent-radial-stiffness-and-strength-proposed-astm-medical-devices]
- 23. - Drug Design Eluting Stent [https://www.news-medical.net/health/Drug-Eluting-Stent-Design.aspx]
- 24. Optimization of Drug Delivery by Drug-Eluting Stents [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0130182]
- 25. Modeling Intravascular Delivery from Drug-Eluting Stents ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3442148/]
- 26. New Drug-Eluting Balloon May Be as Safe and Effective as ... [https://www.mountsinai.org/about/newsroom/2025/new-drug-eluting-balloon-may-be-as-safe-and-effective-as-conventional-metal-stents-for-repeat-percutaneous-coronary-interventions]
- 27. Drug Eluting Stent Compounds - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK537349/]
- 28. Outcomes of first-generation versus second ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425509/]
- 29. Dip Coater Strategic Insights: Analysis 2025 and Forecasts ... [https://www.archivemarketresearch.com/reports/dip-coater-494313]
- 30. Functional coatings for textiles: advancements in flame ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra01429h]
- 31. Enhanced drug delivery capabilities from stents coated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4637970/]
- 32. Recent advances in biodegradable polymer blends and their ... [https://pubs.rsc.org/en/content/articlehtml/2025/gc/d5gc01294e]
- 33. Biodegradable Coated Drug-eluting Stent 2025-2033 [https://www.datainsightsmarket.com/reports/biodegradable-coated-drug-eluting-stent-228935]
- 34. Biodegradable Polymers Strategic Market Report 2024 ... [https://finance.yahoo.com/news/biodegradable-polymers-strategic-market-report-130400916.html]
- 35. Porous Carriers for Controlled/Modulated Drug Delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC2846463/]
- 36. Rhombic-Shaped Channel Stent with Enhanced Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6187719/]
- 37. Preclinical Assessment of a Novel Polymer-Free Hybrid ... [https://link.springer.com/article/10.1007/s12265-025-10680-5]
- 38. Polymer-free versus permanent polymer drug eluting stents ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5643741/]
- 39. Polymer-free sirolimus- and probucol-eluting stents versus ... [https://pubmed.ncbi.nlm.nih.gov/39909305/]
- 40. Polymer-free versus biodegradable-polymer drug-eluting stent ... [https://eurointervention.pcronline.com/article/polymer-free-versus-biodegradable-polymer-drug-eluting-stent-in-patients-undergoing-percutaneous-coronary-intervention-an-assessor-blind-non-inferiority-randomised-controlled-trial]
- 41. Nanomedicine: How nanomaterials are transforming drug ... [https://www.sciencedirect.com/science/article/pii/S2949829524000901]
- 42. Functionalized nanoporous architectures derived from sol–gel ... [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d5tb00958h?page=search]
- 43. Drug-Eluting Hydrophilic Coatings Prevent Coronary ... [https://hydromer.com/drug-eluting-hydrophilic-coatings/]
- 44. Harnessing computational and experimental strategies to ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224725006707]
- 45. controlled release drug delivery market size & share analysis [https://www.mordorintelligence.com/industry-reports/controlled-release-drug-delivery-market]
- 46. Nanoparticle Drug Delivery Systems Competitive Strategies [https://www.datainsightsmarket.com/reports/nanoparticle-drug-delivery-systems-1725740]
- 47. Bioinspired Coronary Stents: A Technological Perspective on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593828/]
- 48. 5-year data from the GABI-R® registry - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12283802/]
- 49. Cardiac Stents from Research to Clinical Applications [https://www.scientificarchives.com/article/cardiac-stents-from-research-to-clinical-applications]
- 50. Drug-eluting coronary stents mediate inflammation ... [https://www.sciencedirect.com/science/article/pii/S0014480025000413]
- 51. Comparison of Sequential Drug Release in Vitro and in Vivo [https://pmc.ncbi.nlm.nih.gov/articles/PMC4691229/]
- 52. Drug Carriers: A Review on the Most Used Mathematical ... [https://www.mdpi.com/2227-9717/10/6/1094]
- 53. Thrombotic Events after Implantation of Drug-eluting Stents [https://www.ecrjournal.com/articles/thrombotic-events-after-implantation-drug-eluting-stents?language_content_entity=en]
- 54. Stent thrombosis: a contemporary guide to definitions, risk ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1622235/full]
- 55. Stent thrombosis: a contemporary guide to definitions, risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582928/]
- 56. Recurrent subacute stent thrombosis after drug-eluting stent ... [https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-025-04658-z]
- 57. Management of in-stent restenosis [https://eurointervention.pcronline.com/article/management-of-in-stent-restenosis]
- 58. Research advances in the etiology of in-stent restenosis of ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1585102/full]
- 59. Research advances in the etiology of in-stent restenosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12313509/]
- 60. Next-generation biodegradable cardiovascular stents [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578071/]
- 61. Coating irregularities of durable polymer-based drug ... [https://eurointervention.pcronline.com/article/coating-irregularities-of-durable-polymer-based-drug-eluting-stents-as-assessed-by-scanning-electron-microscopy]
- 62. Physiological consequences of half-embedded drug ... [https://www.sciencedirect.com/science/article/abs/pii/S1350453325000530]
- 63. The Future of Drug-Eluting Stents: A Coatings Perspective [https://www.mddionline.com/materials/future-drug-eluting-stents-coatings-perspective]
- 64. Hypersensitivity and in-stent restenosis in coronary ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.1003322/full]
- 65. Drug-Eluting Stent Use in Percutaneous Coronary ... [https://www.mdpi.com/2077-0383/14/13/4643]
- 66. Systemic inflammatory response to cemented and ... [https://www.nature.com/articles/s41598-025-24695-0]
- 67. Inflammation-modulating polymeric nanoparticles: design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271758/]
- 68. A new evidence-based design-of-experiments approach ... [https://www.nature.com/articles/s41598-024-82496-3]
- 69. Advancing drug development with “Fit-for-Purpose†modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 70. Combining Mechanistic Quantitative Systems ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1685468/full]
- 71. Biocompatible Coatings for Cardiovascular & Orthopedic ... [https://www.kingsresearch.com/blog/biocompatible-coatings-cardiovascular-orthopedic]
- 72. Advances and prospects in drug-like coatings on Mg alloy ... [https://www.sciencedirect.com/science/article/pii/S2213956725003172]
- 73. Comparative Efficacy and Long-Term Outcomes of Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12286641/]
- 74. The clinical outcome of restricting drug-eluting stents to ... [https://eurointervention.pcronline.com/article/the-clinical-outcome-of-restricting-drug-eluting-stents-to-patients-at-highest-risk-of-restenosis]
- 75. Long-Term Outcomes of Patients Undergoing Implantation ... [https://opencardiovascularmedicinejournal.com/VOLUME/19/ELOCATOR/e18741924362476/FULLTEXT/]
- 76. Stent thrombosis: a contemporary guide to definitions, risk ... [https://pubmed.ncbi.nlm.nih.gov/41195125/]
- 77. Coatings for Cardiovascular Stents—An Up-to-Date Review [https://www.mdpi.com/1422-0067/25/2/1078]
- 78. Long-Term Clinical Outcomes of New-Generation Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8414071/]
- 79. Drug-Coated Balloons for Coronary Interventions: A Focused ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12352407/]
- 80. Efficacy and safety of durable versus biodegradable ... [https://www.nature.com/articles/s41598-024-56925-2]
- 81. Efficacy and safety of polymer-free amphilimus-eluting stent in ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0336017]
- 82. Efficacy and safety of polymer-free amphilimus-eluting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599944/]
- 83. A systematic review and meta-analysis [https://www.sciencedirect.com/science/article/abs/pii/S1553838925003562]
- 84. Drug-Coated Balloons for Coronary Interventions: A Focused ... [https://journal.houstonmethodist.org/articles/10.14797/mdcvj.1607]
- 85. Drug-Eluting Stent, Drug-Coated Balloon, or Plain Old ... [https://pubmed.ncbi.nlm.nih.gov/41221602/]
- 86. Comparative efficacy of drug-coated balloons versus ... [https://bjcardio.co.uk/2025/10/comparative-efficacy-of-drug-coated-balloons-versus-drug-eluting-stents-in-treating-de-novo-cad-in-acs/]
- 87. Real-World Safety and Complications of the Boston ... [https://pubmed.ncbi.nlm.nih.gov/40778487/]
- 88. Intravascular Imaging Guidance for Percutaneous ... [https://www.mdpi.com/2077-0383/14/22/7994]
- 89. The Rise of Optical Coherent Tomography in Intracoronary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12415738/]
- 90. IVUS has more robust data than OCT for PCI guidance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11384219/]
- 91. Comparison of intravascular imaging, physiological ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1604050/full]
- 92. CVIT 2025 clinical expert consensus document on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11910423/]
- 93. Longâ€Term (5â€Years) Outcomes of Current Drugâ€Eluting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336763/]
- 94. Final 5-year outcomes of the Epic02 – RANGO study: A ... [https://www.sciencedirect.com/science/article/pii/S1553838925001162]