Advanced Degradable Suture Materials and Implantation: A Comprehensive Guide for Biomedical Research
This article provides a comprehensive analysis of degradable suture materials and their implantation methods, tailored for researchers, scientists, and drug development professionals.
Advanced Degradable Suture Materials and Implantation: A Comprehensive Guide for Biomedical Research
Abstract
This article provides a comprehensive analysis of degradable suture materials and their implantation methods, tailored for researchers, scientists, and drug development professionals. It explores the foundational science behind material chemistry, from established polymers to emerging biomaterials like albumin composites and biodegradable metals. The scope extends to methodological considerations for implantation, critical troubleshooting of mechanical integrity and biocompatibility, and a rigorous comparative validation of material properties. By synthesizing current research and performance data, this review serves as a strategic resource for guiding the development and application of next-generation sutures in tissue engineering and clinical practice.
The Material Science of Degradation: From Polymer Chemistry to Novel Biomaterials
Surgical sutures are medical devices essential for approximating tissues and facilitating the wound-healing process. Within the context of degradable biomaterials research, they are fundamentally classified based on their interaction with the biological environment over time. Absorbable sutures are those that lose their tensile strength within 60 days and are subsequently broken down and metabolized by the body, with little to no trace remaining [1] [2]. In contrast, Non-absorbable sutures are defined by their ability to retain most of their initial tensile strength for longer than 2-3 months, and they typically remain encapsulated in tissue or require manual removal [1] [3].
This classification is not merely temporal but is rooted in the material's composition and its degradation mechanism. Absorbable sutures, constructed from natural or synthetic polymers, are engineered to undergo hydrolytic degradation or proteolytic enzymatic degradation at a rate commensurate with tissue healing [4] [1]. Non-absorbable sutures, made from biostable materials, provide permanent structural support, making them indispensable in high-tension anatomical regions or for securing prosthetic implants [1] [3]. The following sections will delineate the key characteristics, quantitative properties, and experimental protocols central to the research and development of these critical biomaterials.
Key Characteristics and Comparative Analysis
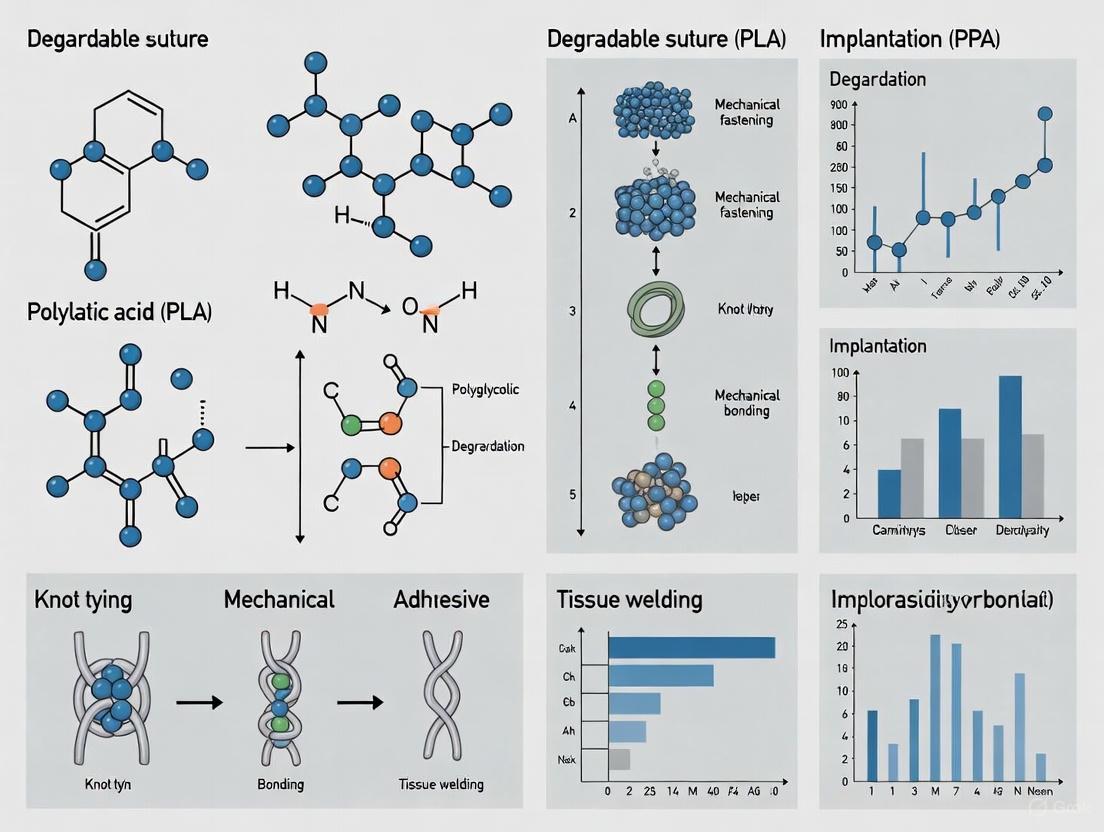
The selection of a suture material for a specific clinical or research application is guided by a detailed understanding of its physicochemical and mechanical properties. The following diagram illustrates the primary classification logic and key degradation pathways for suture materials, providing a framework for their study.
Material Composition and Degradation Profiles
The core distinction between absorbable and non-absorbable sutures lies in their material composition, which directly dictates their degradation profile and biological interaction.
Absorbable Sutures: These materials are designed with a finite lifespan in vivo. Natural variants, such as surgical gut (catgut), are degraded by proteolytic enzymes and subsequently phagocytosed by macrophages [4]. Synthetic absorbables, including polyglycolic acid (PGA), polylactide (PLA), poly-p-dioxanone (PDS), and copolymers like polyglactin 910 (Vicryl), degrade primarily through hydrolysis of their ester bonds [4] [1]. The degradation kinetics are influenced by the polymer's crystallinity, molecular weight, and the local biological environment (e.g., pH, enzyme levels) [4]. A critical performance metric is the "strength retention half-life," which varies significantly between suture groups, as detailed in Table 1.
Non-Absorbable Sutures: These materials are engineered for biostability. They encompass natural fibers like silk and cotton, and synthetic polymers such as polypropylene (Prolene), polyamide (nylon), polyester, and polyvinylidene fluoride (PVDF) [1] [2] [3]. They do not undergo significant degradation; instead, they elicit a foreign body reaction that typically results in the suture becoming encapsulated by fibrous tissue [3]. Their resistance to hydrolysis ensures long-term mechanical support, a necessity in procedures like hernia repair, cardiovascular surgery, and the securing of orthopedic hardware [1] [3].
Quantitative Mechanical and Physical Properties
The functional performance of a suture is quantifiable through a set of standardized mechanical properties. Recent comparative studies of commonly used materials provide critical data for evidence-based selection.
Table 1: Comparative Properties of Representative Suture Materials
| Suture Material | Type & Classification | Tensile Strength (Relative) | Key Degradation / Strength Retention Timeline | Primary Tissue Reaction |
|---|---|---|---|---|
| Vicryl (Polyglactin 910) | Synthetic, Absorbable, Multifilament | Highest [5] | ~50% strength loss in 14-21 days; total absorption in 60-90 days [4] [1] | Moderate tissue reactivity [5] |
| Monocryl (Polyglecaprone 25) | Synthetic, Absorbable, Monofilament | Not Specified | Classified as a medium-term absorbable [4] | Lower reaction vs. multifilament [6] |
| PDS (Polydioxanone) | Synthetic, Absorbable, Monofilament | Not Specified | ~50% strength loss in 28-35 days; total absorption in 180-210 days [4] [1] | Minimal [1] |
| SafilQuick+ (PGA) | Synthetic, Absorbable, Braided | Not Specified | Loses strength significantly in 9-12 days; total absorption ~42 days [4] | Not Specified |
| Silk | Natural, Non-Absorbable, Multifilament | Lowest of compared materials [5] | Retains strength >2-3 months; undergoes slow proteolysis [1] [7] | Significant tissue reactivity [5] |
| Polypropylene (Prolene) | Synthetic, Non-Absorbable, Monofilament | Intermediate (Lower than VICRYL) [5] | Retains tensile strength for >2 years [5] [1] | Minimal tissue reaction [5] |
| Nylon | Synthetic, Non-Absorbable, Monofilament | High | Tensile strength decreases 15-25% per year in vivo [1] | Low tissue reactivity [1] |
Further physical properties are critical for handling and performance. Suture size, denoted by the U.S. Pharmacopeia (USP) system ranging from 12-0 (smallest) to 10 (largest), directly influences tensile strength and tissue drag [5]. The physical configuration—monofilament versus multifilament (braided or twisted)—also presents a trade-off: monofilaments exhibit lower tissue reactivity and reduced risk of infection, while multifilaments generally offer superior knot security and handling [5] [2]. Research indicates that multifilament constructions (e.g., VICRYL, silk) can score higher in tenacity, toughness, and knot tensile strength compared to monofilaments like polypropylene [5].
Experimental Protocols for Suture Evaluation
Robust and standardized experimental methodologies are paramount for characterizing suture materials in a research and development setting. The protocols below are adapted from current literature and international standards.
Protocol 1: Tensile Strength and Elongation at Break
Objective: To determine the ultimate tensile strength and elongation of suture materials under a controlled, uniaxial load, simulating the mechanical stresses encountered in vivo.
Materials & Reagents:
- Universal Testing Machine (UTM) equipped with a calibrated load cell (e.g., 100 N capacity)
- Standardized suture samples (e.g., 20-30 cm lengths)
- Micrometer for precise diameter measurement
- Environmental chamber (optional, for conditioned testing)
Methodology:
- Sample Preparation: Cut a minimum of six specimens per suture type to a standardized length. Measure and record the diameter of each specimen at three points along its length using a micrometer [5] [2].
- UTM Setup: Mount the specimen in the UTM grips, ensuring it is aligned axially. Set the gauge length (distance between grips) to a standardized distance, typically 10 mm [2].
- Testing Parameters: Program the UTM to apply a tensile load at a constant crosshead speed of 50 mm/min until failure [2].
- Data Collection: The UTM software will generate a force-elongation curve. Record the Breaking Force (N) and the Elongation at Break (%).
- Data Analysis: Calculate the mean and standard deviation for each suture group. Statistical analysis (e.g., one-way ANOVA with post-hoc Tukey test) should be performed to identify significant differences between materials (p < 0.05) [5] [2].
Protocol 2: In Vitro Hydrolytic Degradation and Strength Retention
Objective: To simulate the in vivo absorption process and quantify the loss of mechanical strength over time, a critical parameter for absorbable sutures.
Materials & Reagents:
- Phosphate Buffered Saline (PBS) or Ringer's Solution (8.6 g/L NaCl, 0.3 g/L KCl, 0.33 g/L CaCl₂·2H₂O) [4]
- Temperature-controlled incubator or water bath (set to 37°C ± 1°C)
- Sealed containers for solution immersion
- Universal Testing Machine (as in Protocol 1)
Methodology:
- Baseline Testing: Perform tensile strength testing on a representative set of fresh suture samples (Group T=0) as per Protocol 1.
- Solution Immersion: Place the remaining test samples in individual containers filled with a sufficient volume of pre-warmed PBS or Ringer's solution to fully submerge them. Seal the containers to prevent evaporation and place them in the incubator at 37°C [4].
- Sampling Interval: Remove a cohort of samples (e.g., n=6-8) at predetermined time intervals relevant to the suture's expected absorption profile (e.g., days 1, 3, 7, 14, 21, 28) [4].
- Post-Immersion Testing: Gently rinse the retrieved samples with deionized water and pat dry. Immediately subject them to tensile testing as described in Protocol 1.
- Data Analysis: Calculate the percentage of original tensile strength retained at each time point: (Strength at Time T / Baseline Strength) x 100%. Plot the strength retention profile over time to model the degradation kinetics [4].
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers embarking on the evaluation of suture materials, the following table catalogues essential tools and their specific functions in a experimental workflow.
Table 2: Key Research Reagent Solutions for Suture Characterization
| Research Tool / Reagent | Primary Function in Suture Research |
|---|---|
| Universal Testing Machine (UTM) | The cornerstone instrument for quantifying key mechanical properties including tensile strength, elongation at break, and modulus [5] [2]. |
| Ringer's Solution / PBS | Isotonic solutions used in in vitro degradation studies to simulate the biological environment and initiate hydrolytic degradation of absorbable sutures [4]. |
| Scanning Electron Microscope (SEM) | Used for high-resolution imaging of suture surface morphology, degradation patterns, and structural integrity before and after testing [2]. |
| Micrometer / Digital Caliper | Provides precise measurement of suture diameter, a critical variable that correlates with tensile strength and is required for standardized reporting [5]. |
| Cell Viability Assays (e.g., MTT) | In vitro biocompatibility tests to assess the cytotoxicity of suture materials or their degradation byproducts on cultured cell lines [2]. |
| Temperature-Controlled Incubator | Maintains a constant 37°C environment for degradation studies, accelerating hydrolysis and mimicking physiological temperature [4]. |
| Prudomestin | Prudomestin | High-Purity Research Compound |
| (+)-Intermedine | (+)-Intermedine, CAS:146-68-9, MF:C19H13IN5O2.Cl, MW:505.7 g/mol |
The rational selection between absorbable and non-absorbable sutures is a critical decision point in both clinical practice and biomaterials research, hinging on a deep understanding of their defining characteristics. Absorbable sutures offer the key advantage of autonomous degradation, eliminating the need for removal and reducing long-term foreign body presence, but require precise matching of their strength retention profile to the tissue's healing timeline. Non-absorbable sutures provide dependable, long-term mechanical support but may necessitate a secondary removal procedure or remain as a permanent implant.
The future of suture technology, as indicated by market and research trends, is moving toward "smart" functionalities. The biodegradable smart suture market is projected to grow significantly, driven by innovations such as sutures capable of controlled drug delivery and responsiveness to environmental changes like pH or temperature [8]. Furthermore, ongoing research into novel polymers, such as poly-4-hydroxybutyrate (P4HB), and the refinement of copolymer compositions promise next-generation sutures with enhanced biocompatibility and precisely engineered degradation rates [1] [9]. This evolution underscores the importance of the fundamental characterization protocols outlined herein, which provide the essential toolkit for developing and evaluating the advanced suture materials of tomorrow.
Surgical sutures are fundamental medical devices designed to approximate tissue and secure wound closure until the healing process provides sufficient strength. The ideal suture material balances multiple properties: high tensile strength, excellent handling and knot security, minimal tissue reactivity, predictable degradation, and sterility [10] [11]. Sutures are broadly classified as either natural (derived from biological sources like animal intestines or silk worm filaments) or synthetic (manufactured through chemical polymerization) [12]. A critical distinction lies in their fate within the body: absorbable sutures are designed to degrade and lose tensile strength within weeks to months, while non-absorbable sutures maintain their strength for longer than 2-3 months [13] [1]. The selection of a specific suture material is a critical surgical decision that directly influences wound healing, infection risk, and cosmetic outcome [12].
This review provides a detailed comparison of six key materials—catgut, silk, polyglycolide (PGA), polylactide (PLA), polydioxanone (PDO), and poly-4-hydroxybutyrate (P4HB)—framed within ongoing research on degradable biomaterials. We present standardized experimental data and protocols to support preclinical evaluation and material selection for research and drug development applications.
Material Properties and Performance Data
Quantitative Comparison of Suture Materials
Table 1: Fundamental Properties of Suture Materials
| Material | Classification | Absorption Time (Days) | Tensile Strength Retention | Primary Degradation Mechanism | Tissue Reaction |
|---|---|---|---|---|---|
| Catgut | Natural, Absorbable | 60-70 [13] | Lost by 60 days [13] | Proteolytic enzymatic degradation [1] | Moderate to Severe [14] |
| Silk | Natural, Non-Absorbable | N/A (Non-absorbable) [1] | Retains strength >2 months [1] | Not applicable; encapsulation in tissue | Moderate [5] |
| PGA | Synthetic, Absorbable | 60-90 [13] | ~50% at 2-3 weeks [15] | Hydrolysis [13] | Minimal [13] |
| PLA | Synthetic, Absorbable | 180+ [13] | Prolonged (>6 months) [15] | Hydrolysis [13] | Minimal [13] |
| PDO | Synthetic, Absorbable | 180+ [13] | ~70% at 4 weeks, ~50% at 6 weeks [13] | Hydrolysis [13] | Minimal [13] |
| P4HB | Synthetic, Absorbable | 365-540 [15] | ~65% at 12 weeks [14] | Hydrolysis & surface erosion [15] | Minimal [14] |
Table 2: Experimental Mechanical and Functional Performance
| Material | Structure | Key Functional Advantages | Key Functional Limitations | Common Trade Names |
|---|---|---|---|---|
| Catgut | Monofilament or Twisted [13] | Rapid absorption, proven history | High tissue reactivity, unpredictable absorption [14] | Chromic Catgut [14] |
| Silk | Braided Multifilament [5] | Excellent handling & knot security [5] | High capillarity, infection risk, moderate reactivity [5] | Silk, Virgin Silk [13] |
| PGA | Braided Multifilament [13] | High initial strength, predictable absorption [13] | Stiff, can saw through tissue [13] | Dexon [13] |
| PLA | Various [13] | Long-term strength retention [15] | Slow degradation, acidification upon hydrolysis [15] | Orthodek [13] |
| PDO | Monofilament [13] | Flexibility, good knot strength [13] | Slow absorption, potential for late inflammation [13] | PDS, PDS II [13] |
| P4HB | Monofilament [15] | High elasticity, biocompatible degradation product [15] | Higher cost, specialized production [15] | TephaFlex [13] [15] |
Analysis of Comparative Data
The data reveals a clear evolutionary pathway from natural to advanced synthetic materials. Natural materials like catgut and silk, while historically important, are characterized by significant biological reactivity and unpredictable degradation profiles [14] [5]. In contrast, synthetic materials (PGA, PLA, PDO, P4HB) offer superior control over mechanical properties and absorption kinetics, leading to minimized tissue reaction [13]. The global absorbable sutures market, valued at USD 3 billion in 2024, is dominated by synthetic materials, which hold a 71.4% market share due to these advantages [16].
PGA and PLA, among the first-generation synthetic absorbables, degrade via hydrolysis of their ester bonds, producing predictable strength loss profiles [13]. PDO offers a good balance of flexibility and strength retention, making it suitable for tissues requiring extended support [13]. P4HB represents a significant advancement; it is a bacterial-derived polyester that is FDA-approved and exhibits exceptional elasticity, with degradation products that are natural human metabolites [15]. Its degradation profile, spanning 12-18 months for complete resorption, makes it ideal for applications like soft tissue repair where long-term, gentle support is needed [15].
Experimental Protocols for Suture Evaluation
Protocol 1: In Vitro Degradation and Strength Retention
Objective: To quantitatively assess the mass loss, molecular weight change, and tensile strength retention of absorbable suture materials under simulated physiological conditions.
Reagents and Equipment:
- Phosphate Buffered Saline (PBS), pH 7.4: Simulates physiological pH.
- Lipase Solution (e.g., from Pseudomonas cepacia): Models enzymatic degradation for certain polymers [14].
- Incubator: Maintained at 37°C.
- Tensile Testing Machine: Equipped with a small-load cell (e.g., 50 N capacity).
- Gel Permeation Chromatography (GPC): For monitoring changes in molecular weight.
Methodology:
- Sample Preparation: Cut suture samples to standardized lengths (e.g., 20 cm). Record initial mass and diameter. For braided sutures, ensure consistent pre-tensioning during measurement.
- Immersion Study: Aseptically place samples in sterile containers with PBS or lipase solution. Maintain a consistent buffer-to-suture mass ratio (e.g., 20:1). Incubate at 37°C [14].
- Time-Point Sampling: Remove samples in triplicate at predetermined intervals (e.g., 1, 2, 4, 8, 12 weeks).
- Analysis:
- Mass Loss: Rinse retrieved samples with deionized water, dry to constant weight in a vacuum desiccator, and calculate percentage mass loss.
- Molecular Weight: Dissolve dried suture fragments in appropriate solvent (e.g., Hexafluoroisopropanol for PDO, P4HB) and analyze via GPC to determine Mn and Mw [14].
- Tensile Strength: Perform uniaxial tensile tests on wet samples according to ASTM F2548. Clamp a gauge length of suture and pull at a constant crosshead speed (e.g., 50 mm/min) until failure. Record peak load and calculate tensile strength [5].
Data Interpretation: Plot strength retention and molecular weight against time. Materials like PGA will show a rapid decline, whereas PDO, PLA, and P4HB will demonstrate more extended strength retention profiles [14] [13].
Protocol 2: In Vivo Biocompatibility and Tissue Response
Objective: To evaluate the local tissue reaction, foreign body response, and in vivo degradation kinetics of suture materials in a live animal model.
Reagents and Equipment:
- Animal Model: Female Sprague-Dawley rats (200-250 g).
- Suture Implantation Device: Trocar or large-bore needle.
- Histology Supplies: Formalin fixative, paraffin embedding station, microtome, Hematoxylin & Eosin (H&E) stain, stain for macrophages (e.g., CD68 immunohistochemistry).
Methodology:
- Implantation: Anesthetize rats according to approved IACUC protocol. Make a small skin incision and implant pre-sterilized suture segments (e.g., 2 cm long) into the tergal muscle mass or subcutaneous tissue using a trocar. Implant negative control materials (e.g., USP polyethylene) concurrently [14].
- Explanation: Euthanize animals and explant the suture and surrounding tissue block at designated time points (e.g., 1, 4, 12, 26 weeks).
- Histopathological Analysis:
- Fix tissue blocks in 10% neutral buffered formalin for 48 hours.
- Process, embed in paraffin, and section to 5 µm thickness.
- Stain sections with H&E and analyze under light microscopy for inflammatory cell infiltration (neutrophils, lymphocytes, macrophages), fibrosis, and capsule formation.
- Score the foreign body reaction semi-quantitatively on a standardized scale (e.g., 0-4) for parameters like inflammation and fibrosis [14].
Data Interpretation: Compare the inflammatory scores and degradation progress of test materials against controls and each other. Catgut typically incurs a more pronounced and persistent cellular response, while advanced synthetics like P4HB show markedly milder reactions [14].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Suture Material Research
| Reagent / Material | Function in Research | Application Example |
|---|---|---|
| Polyglactin 910 (Vicryl) | Model braided synthetic absorbable suture | Positive control for in vitro hydrolysis and strength retention studies [5] [12]. |
| Polydioxanone (PDS) | Model monofilament, slow-absorbing suture | Benchmark for evaluating long-term (≥6 months) tissue response and strength loss [13]. |
| Lipase Enzyme (P. cepacia) | Catalyst for accelerated in vitro polymer degradation | Simulating enzymatic degradation of aliphatic polyesters like P4HB in buffer solutions [14]. |
| Phosphate Buffered Saline (PBS) | Simulates physiological pH environment | Standard medium for in vitro hydrolysis studies under controlled, non-enzymatic conditions [14]. |
| Triclosan-coated Sutures (Vicryl Plus) | Antimicrobial suture model | Studying efficacy in reducing bacterial biofilm formation and surgical site infections (SSI) [12]. |
| 1-Bromoadamantane | 1-Bromoadamantane (1-Adamantyl Bromide) >99.0% | |
| 5-Methylindole | 5-Methylindole, CAS:614-96-0, MF:C9H9N, MW:131.17 g/mol | Chemical Reagent |
Research Workflow and Material Selection Pathways
The following diagram illustrates the logical decision-making process for selecting and evaluating suture materials in a research context, integrating the key concepts and protocols discussed.
Biodegradation is a critical process in biomedical engineering, particularly for the development of advanced degradable suture materials and implants. These materials are designed to perform their therapeutic function and then safely break down within the body, eliminating the need for secondary removal surgeries and reducing long-term complications [17]. The degradation process in biological environments occurs through three primary, often interconnected, mechanisms: hydrolysis, enzymatic degradation, and cellular phagocytosis. Understanding these mechanisms at a fundamental level enables researchers to design materials with tailored degradation profiles that match tissue healing timelines, thereby optimizing clinical outcomes [17] [18]. This document provides a detailed overview of these mechanisms, supported by experimental protocols and data analysis tools, specifically framed within research on next-generation suture materials.
Mechanism 1: Hydrolysis
Principle and Key Factors
Hydrolysis is a chemical process where polymer chains are cleaved through the reaction with water molecules. This mechanism is particularly dominant in synthetic biodegradable polymers used in sutures, such as polyglycolic acid (PGA), polylactic acid (PLA), and polydioxanone (PDS) [19] [18]. The process occurs without direct cellular involvement and is influenced by both the intrinsic properties of the polymer and the external environment.
The rate of hydrolytic degradation is governed by several key factors [20]:
- Chemical Structure: Polymers with hydrolytically labile bonds in their backbone, such as esters, carbonates, and amides, degrade more rapidly.
- Hydrophobicity/ Hydrophilicity Balance: Hydrophilic polymers tend to absorb more water, accelerating the hydrolysis process. Computational LogP(SA)â»Â¹ values can predict this behavior, with negative values indicating higher water affinity and potentially faster degradation [20].
- Glass Transition Temperature (Tg): Polymers with a lower Tg have more chain mobility, which can facilitate water penetration and increase degradation rates.
- Crystallinity: The amorphous regions of a polymer are more accessible to water and degrade faster than the crystalline regions.
Experimental Protocol: Monitoring Hydrolytic DegradationIn Vitro
Objective: To quantify the hydrolytic degradation rate of a novel albumin-based suture material under simulated physiological conditions [19].
Materials:
- Phosphate Buffered Saline (PBS): pH 7.4, to simulate physiological pH.
- Suture Samples: Pre-cut to standardized lengths (e.g., 2 cm) and weights.
- Incubation Vessels: Hermetic containers to prevent evaporation.
- Analytical Balance: Precision of ±0.01 mg.
- Gel Permeation Chromatography (GPC) System: For monitoring changes in molecular weight.
- Scanning Electron Microscope (SEM): For examining surface erosion.
Procedure:
- Baseline Characterization: Weigh each suture sample (W₀) and characterize initial molecular weight (Mₙ₀, Mᵂ₀) via GPC.
- Immersion: Immerse samples in PBS maintained at 37°C in an incubator. Use a high surface-to-volume ratio of PBS to sample to ensure sink conditions.
- Sampling: At predetermined time points (e.g., 1, 2, 4, 8, 12 weeks), retrieve triplicate samples from the PBS.
- Mass Loss Analysis: Rinse retrieved samples with deionized water, dry to constant weight in a vacuum desiccator, and record the dry weight (Wₜ).
- Molecular Weight Analysis: Analyze the dried samples using GPC to determine the remaining molecular weight (Mₙₜ, Mᵂₜ).
- Morphological Analysis: Examine the surface morphology of the dried samples using SEM to identify cracking, pitting, or surface erosion features.
Data Analysis:
- Mass Loss (%) = [(W₀ - Wₜ) / W₀] × 100
- Molecular Weight Retention (%) = (Mₙₜ / Mₙ₀) × 100
- Fit the mass loss and molecular weight data to kinetic models (e.g., first-order) to determine the degradation rate constant.
Table 1: Key Properties Influencing Hydrolytic Degradation Rates of Suture Polymers
| Polymer | Labile Bond | Typical Tg (°C) | Crystallinity | Relative Degradation Rate |
|---|---|---|---|---|
| Polyglycolic Acid (PGA) | Ester | 35-40 | High | Fast [20] |
| Polylactic Acid (PLA) | Ester | 55-60 | Medium | Slow [20] |
| Polycaprolactone (PCL) | Ester | (-60) - (-65) | Low | Medium [20] |
| Polydioxanone (PDS) | Ester, Ether | ~ -10 | Medium | Medium |
Figure 1: Mechanism and Key Influencing Factors of Hydrolytic Degradation.
Mechanism 2: Enzymatic Degradation
Principle and Key Factors
Enzymatic degradation involves the specific cleavage of polymer chains by biologically active enzymes, such as proteases, esterases, and lipases [20] [21]. This mechanism is often more specific and faster than hydrolysis alone and is a key degradation route for natural polymer-based sutures like catgut, silk, and albumin [19]. Enzymes act as biological catalysts, lowering the activation energy required for bond scission.
The efficiency of enzymatic degradation depends on:
- Enzyme-Substrate Specificity: The enzyme must recognize and bind to specific chemical structures on the polymer.
- Surface Accessibility: Enzymes are too large to penetrate dense polymer matrices, so degradation is primarily a surface-erosion process.
- Environmental Conditions: Local pH and temperature can dramatically affect enzyme activity.
- Presence of Inhibitors or Activators: Other molecules in the biological milieu can modulate enzyme function.
Experimental Protocol: Evaluating Enzymatic Degradation Kinetics
Objective: To determine the degradation profile of a silk fibroin suture in the presence of a protease enzyme solution [17] [18].
Materials:
- Enzyme Solution: Protease from Streptomyces griseus (e.g., 1 U/mL) in Tris-HCl buffer (pH 7.8).
- Inactivated Enzyme Control: Enzyme solution boiled for 10 minutes to denature the enzyme.
- Suture Samples: Pre-weighed and characterized.
- Orbital Shaker: For constant, gentle agitation.
- UV-Vis Spectrophotometer: For analyzing protein release (e.g., absorbance at 280 nm).
Procedure:
- Solution Preparation: Prepare the active and inactivated enzyme solutions.
- Immersion: Immerse triplicate suture samples in both the active and control solutions. Maintain at 37°C with constant agitation.
- Sampling: At regular intervals, withdraw a small aliquot (e.g., 1 mL) from the supernatant and replace with fresh buffer or enzyme solution to maintain volume and activity.
- Analysis of Soluble Products:
- Measure the absorbance of the supernatant at 280 nm to quantify the release of soluble protein fragments.
- Alternatively, use the BCA or Bradford assay for more precise protein quantification.
- Sample Retrieval: At major time points, retrieve entire suture samples for mass loss, GPC, and SEM analysis, as described in the hydrolysis protocol.
Data Analysis:
- Plot the concentration of soluble degradation products vs. time.
- Model the degradation kinetics using the Michaelis-Menten equation to determine Vₘâ‚â‚“ (maximum degradation rate) and Kₘ (Michaelis constant).
- The Haldane-Andrews model can be applied if high substrate concentrations (e.g., high suture mass) inhibit the enzyme [21].
Table 2: Common Enzymes in Biodegradation of Suture Materials
| Enzyme Class | Target Polymer/Bond | Relevant Suture Material |
|---|---|---|
| Proteases | Peptide bonds | Albumin, Collagen, Silk [19] |
| Esterases | Ester bonds | PGA, PLA, PCL [20] |
| Lipases | Ester bonds (in lipids) | Polyurethanes, PCL [20] |
| Collagenases | Collagen triple helix | Catgut |
Mechanism 3: Cellular Phagocytosis
Principle and Key Factors
Cellular phagocytosis is an active, energy-dependent process where specialized immune cells, primarily macrophages, engulf and internalize small particles or fragments of degraded material [22]. This process is crucial for the final clearance of degradation products and is intimately linked to the inflammatory and tissue-repair response [17]. When an implant degrades via hydrolysis or enzymes to micro- and nano-scale fragments, phagocytes can clear these fragments.
The process is highly regulated by "eat-me" signals [22]:
- Phosphatidylserine (PS) Exposure: In apoptotic cells, PS is externalized to the outer leaflet of the membrane, acting as a primary "eat-me" signal for phagocytes.
- Receptor Recognition: Phagocytes express receptors (e.g., TAM family receptors MerTK and Axl, Tim-4) that bind to these signals.
- Cytoskeletal Rearrangement: Upon binding, the phagocyte's actin cytoskeleton reorganizes to extend pseudopods and engulf the target.
- Formation of Phagolysosome: The internalized material is trafficked to lysosomes, where it is degraded by potent acidic hydrolases [23].
Experimental Protocol: Assessing Macrophage-Mediated Phagocytosis of Suture Fragments
Objective: To visualize and quantify the uptake of fluorescently-labeled suture fragments by macrophages in vitro.
Materials:
- Macrophage Cell Line: e.g., RAW 264.7 or primary bone marrow-derived macrophages (BMDMs).
- Fluorescent Suture Fragments: Micronized suture material labeled with a stable fluorophore (e.g., FITC).
- Cell Culture Facilities: Including COâ‚‚ incubator and sterile hood.
- Confocal Microscope: For high-resolution imaging.
- Flow Cytometer: For quantitative analysis.
- Inhibitors: e.g., Cytochalasin D (actin polymerization inhibitor) as a negative control.
Procedure:
- Fragment Preparation: Generate and sterilize micron-sized fragments of the suture material. Label with a non-toxic fluorescent dye.
- Cell Seeding: Seed macrophages into multi-well plates (containing coverslips for microscopy) and allow to adhere overnight.
- Treatment: Incubate cells with fluorescent suture fragments at a predetermined particle-to-cell ratio. Include wells with cytochalasin D pre-treatment to confirm phagocytosis is energy-dependent.
- Incubation: Incubate for 2-6 hours.
- Analysis:
- Confocal Microscopy: Fix cells, stain actin cytoskeleton (e.g., with phalloidin) and nuclei (DAPI). Image to visualize internalized fragments.
- Flow Cytometry: Trypsinize and collect cells. Analyze the fluorescence intensity of the cell population, which corresponds to fragment uptake.
Data Analysis:
- Quantify the percentage of fluorescent-positive cells via flow cytometry.
- Determine the mean fluorescence intensity, which indicates the average phagocytic load per cell.
- From microscopy images, count the number of particles per cell.
Figure 2: Cellular Phagocytosis Pathway for Suture Fragment Clearance.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Biodegradation Research
| Item | Function/Application | Example Use Case |
|---|---|---|
| Polymer Samples | Base material for suture development and degradation testing. | Human Serum Albumin (HSA) for novel composite sutures [19]. |
| Protease Enzyme | Catalyzes enzymatic degradation of protein-based sutures. | Testing degradation kinetics of silk fibroin sutures [17]. |
| Phosphate Buffered Saline (PBS) | Provides a simulated physiological environment for hydrolysis studies. | In vitro immersion studies for mass loss and molecular weight change [19]. |
| RAW 264.7 Cell Line | A murine macrophage cell line for phagocytosis assays. | Quantifying cellular uptake of fluorescent suture fragments. |
| Cytochalasin D | Inhibitor of actin polymerization; negative control for phagocytosis. | Confirming that particle uptake is an energy-dependent process. |
| Gel Permeation Chromatography (GPC) | Analyzes changes in polymer molecular weight distribution over time. | Tracking the chain scission and erosion of synthetic polymers like PLA [20]. |
| Scanning Electron Microscope (SEM) | Visualizes surface morphology and erosion patterns of degrading materials. | Identifying pitting, cracking, or surface roughening on sutures after in vitro testing [19]. |
| Jatrophane 3 | Jatrophane 3, CAS:210108-87-5, MF:C43H53NO14 | Chemical Reagent |
| (+)-Isoajmaline | (+)-Isoajmaline|Research Chemical|RUO | High-purity (+)-Isoajmaline for research applications. This product is For Research Use Only (RUO) and is not intended for diagnostic or personal use. |
The field of regenerative medicine is increasingly focused on the development of advanced biomaterials that provide temporary mechanical support and actively promote tissue healing without requiring surgical removal. Among these, degradable suture materials represent a critical area of innovation, balancing the requirements of mechanical integrity, biocompatibility, and controlled degradation. Traditional polymeric sutures, while widely used, face limitations including suboptimal tissue integration, potential cytotoxicity, and mechanical mismatch with native tissues. This has spurred research into three promising material categories: albumin-based composites, biodegradable metals (magnesium, iron, and zinc alloys), and graphene-enhanced sutures. These advanced materials offer unique advantages for tissue engineering applications, from enhanced biocompatibility and bioactive functionality to superior mechanical properties that can be tailored to specific clinical needs. This article provides a comprehensive overview of the current state of these emerging biomaterials, with detailed experimental protocols and performance data to guide research and development efforts.
Material Classes and Performance Characteristics
Albumin-Based Composite Sutures
Human serum albumin (HSA) has emerged as a promising base material for biodegradable sutures due to its excellent biocompatibility, natural origin, and biodegradability. Research demonstrates that albumin-based sutures can be fabricated using extrusion methodology to create filaments with tunable mechanical properties suitable for various medical applications [24].
Table 1: Mechanical Properties of Albumin-Based Composite Sutures
| Material Composition | Tensile Strength (MPa) | Elongation at Break (%) | Key Characteristics | Potential Applications |
|---|---|---|---|---|
| Filament Suture (FS) from HSA | 1.3 - 9.616 | 11.5 - 146.64 | Biocompatible, biodegradable, tunable mechanical properties | Soft tissue repair, 3D printing of medical devices (plates, nails) |
| HSA with gelatin additives | Data not specified | Data not specified | Enhanced cell adhesion, improved handling characteristics | Wound closure, tissue engineering scaffolds |
The mechanical versatility of albumin-based sutures is evident from the broad range of tensile strengths and elongation percentages achievable through modifications in processing parameters and additive incorporation. These sutures can be further enhanced with biodegradable organic modifiers to improve their mechanical performance and biological interactions [24]. The fundamental advantage of albumin lies in its status as a natural blood component, which minimizes immune reactions and supports natural healing processes.
Biodegradable Metal Sutures and Fasteners
Biodegradable metals represent a revolutionary approach to temporary implantable devices, combining the mechanical strength of metals with the resorbability of biodegradable materials. The three primary metal systems under investigation are magnesium (Mg), zinc (Zn), and iron (Fe) based alloys.
Table 2: Comparison of Biodegradable Metals for Surgical Applications
| Metal Type | Elastic Modulus (GPa) | Tensile Strength (MPa) | Degradation Rate | Key Advantages | Key Challenges |
|---|---|---|---|---|---|
| Magnesium Alloys (e.g., ZK60) | 41-45 [25] | 65-100 [25] | Fast (can be too rapid) | Promotes bone formation, excellent biocompatibility, similar modulus to bone | Hydrogen gas evolution, alkalization, rapid corrosion [25] |
| Zinc Alloys (e.g., Zn-Cu-Mn-Ti) | 90-110 [26] | 75-160 [26] | Intermediate (ideal for many applications) | Good biocompatibility, nutrient element, no gas evolution | Lower strength and plasticity in pure form [26] |
| Iron Alloys | 180-210 [26] | 50-1450 [26] | Slow (may be too slow) | High strength, familiar processing techniques | Very slow degradation, potential inflammation from corrosion products [26] |
Recent advances in magnesium alloys include the development of fluoridized ZK60 suture anchors for rotator cuff repair, which demonstrated superior osseointegration and new bone formation compared to titanium anchors in goat models [27]. Similarly, zinc alloys have shown remarkable progress with novel compositions like Zn-1.0Cu-0.2Mn-0.1Ti exhibiting excellent mechanical properties for surgical staples, with corrosion rates of approximately 0.02 mm/year in Hank's balanced salt solution and 0.12 mm/year in fed-state simulated intestinal fluid [28]. The varying degradation rates depending on physiological environment make these materials particularly suitable for site-specific applications.
Graphene-Enhanced Sutures
The integration of carbon-based nanomaterials with traditional suture materials has opened new frontiers in bioactive wound closure devices. Research demonstrates that coating resorbable poly(glycolide-co-lactide) (PGLA) sutures with bioactive glass nanopowders (BGNs) and graphene oxide (GO) imparts significant bioactivity and enhances wound healing properties [29].
These composite coatings create stable, homogeneous surfaces on sutures that promote fibroblast attachment, migration, and proliferation. Additionally, they stimulate the secretion of angiogenic growth factors that accelerate wound healing. The GO component enhances the electrical conductivity and mechanical strength of the coatings, while the BGNs contribute bioactive ions that support cellular functions [29]. The combination results in sutures that not only provide physical support but actively modulate the wound environment to facilitate regeneration.
Experimental Protocols
Protocol 1: Fabrication and Characterization of Albumin-Based Sutures
Materials Required:
- Human serum albumin (HSA) or bovine serum albumin (BSA)
- Gelatin powder (additive material)
- Extrusion equipment with temperature control
- Tensile testing machine
- Scanning Electron Microscope (SEM)
- Thermogravimetric analyzer (TGA)
Procedure:
- Material Preparation: Prepare HSA solution according to manufacturer specifications. For composite formulations, add gelatin powder at concentrations ranging from 0.5–50 μg/mL [24].
- Extrusion Process: Utilize sub-critical water technology and extrusion methodology to form filament sutures (FS). Optimize temperature and pressure parameters to achieve desired filament diameter [24].
- Mechanical Testing: Evaluate tensile strength and elongation at break using standardized tensile testing protocols. Target values should range from 1.3 to 9.616 MPa for tensile strength and 11.5% to 146.64% for elongation at break [24].
- Morphological Analysis: Characterize surface morphology and cross-sectional structure using SEM imaging.
- Thermal Analysis: Determine thermal stability using TGA with a temperature ramp from ambient to 600°C.
Quality Control:
- Ensure consistent filament diameter throughout the length
- Verify absence of surface defects or irregularities
- Confirm reproducible mechanical properties across batches
Protocol 2: Preparation and Evaluation of Magnesium Alloy Suture Anchors
Materials Required:
- ZK60 magnesium alloy (Mg-6.0Zn-0.5Zr)
- 42% hydrofluoric acid
- Titanium anchors (control)
- CNC machining equipment
- Ultrasonic cleaner
- Orbital shaker
- Computed tomography (CT) imaging system
Procedure:
- Anchor Fabrication: Machine ZK60 alloy into anchors with diameter of 5 mm and length of 15 mm using CNC machining [27].
- Surface Treatment: Clean anchors ultrasonically in ethanol and deionized water for 5 minutes each.
- Fluoride Coating: Immerse anchors in 42% hydrofluoric acid at room temperature with shaking at 70 rpm for 24 hours to create MgFâ‚‚ coating [27].
- Post-treatment Cleaning: Ultrasonically clean coated anchors in ethanol and deionized water for 5 minutes each.
- Sterilization: Sterilize anchors with 75% ethanol prior to implantation.
- In Vivo Evaluation: Implant anchors in animal model (e.g., goat rotator cuff) and evaluate at 4, 8, and 12 weeks using CT imaging and histological analysis [27].
Assessment Parameters:
- New bone formation quantification
- Osseointegration quality
- Tendon healing assessment
- Local tissue response
Protocol 3: Application of Graphene Oxide/Bioglass Coatings on Sutures
Materials Required:
- PGLA sutures (90:10%)
- Bioactive glass nanopowders (BGNs)
- Graphene oxide (GO) solution
- Vacuum sol deposition apparatus
- Fourier-transform infrared spectroscopy (FTIR) equipment
- Cell culture facilities (L929 fibroblast cells)
Procedure:
- Coating Preparation: Synthesize GO-doped melt-derived BGNs via sol-gel process [29].
- Surface Coating: Apply BGNs and BGNs/GO coatings to resorbable PGLA sutures using optimized vacuum sol deposition method [29].
- Characterization: Analyze chemical structure using FTIR spectroscopy in the range of 400–4000 cmâ»Â¹.
- Morphological Examination: Examine surface morphology and coating homogeneity using field emission scanning electron microscopy with elemental analysis.
- In Vitro Bioactivity: Evaluate bioactivity through immersion in simulated body fluid and monitoring of hydroxyapatite formation.
- Cellular Response: Assess fibroblast attachment, migration, and proliferation using L929 cell line.
Quality Metrics:
- Coating stability and homogeneity
- Enhanced fibroblast attachment and proliferation
- Accelerated angiogenic growth factor secretion
- Improved wound healing in in vivo models
Signaling Pathways and Biological Mechanisms
The bioactive materials described herein promote healing through modulation of critical cellular signaling pathways. Understanding these mechanisms is essential for optimizing material design and predicting clinical performance.
Magnesium ions released during degradation stimulate bone formation and improve osseointegration, as demonstrated in fluoridized ZK60 suture anchors that showed superior new bone formation compared to titanium controls [27]. Zinc alloys with nutrient elements (such as strontium) trigger signaling pathways that promote both angiogenesis and osteogenesis, creating a favorable environment for bone regeneration [26]. Bioactive glass coatings contribute ions that enhance cell adhesion and migration while stimulating angiogenic factors, particularly important for soft tissue repair [29].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Degradable Suture Development
| Reagent/Material | Function/Application | Specifications/Notes |
|---|---|---|
| Human Serum Albumin (HSA) | Base material for albumin-based sutures | Use first grade purity; source from reputable suppliers (e.g., Wako Pure Chemical Industries) [24] |
| ZK60 Magnesium Alloy | Biodegradable metal for suture anchors | Composition: Mg-6.0Zn-0.5Zr; requires MgFâ‚‚ coating for corrosion resistance [27] |
| Zn-Based Alloys | Biodegradable staples and sutures | Optimal compositions: Zn-1.0Cu-0.2Mn-0.1Ti, Zn-1.0Mn-0.1Ti, Zn-1.0Cu-0.1Ti [28] |
| Graphene Oxide (GO) | Coating component for enhanced bioactivity | Enhances electrical conductivity, mechanical strength, and bioactivity [29] |
| Bioactive Glass Nanopowders (BGNs) | Coating component for tissue integration | Promotes fibroblast attachment and proliferation; enhances wound healing [29] |
| Hydrofluoric Acid | Surface treatment for Mg alloys | 42% concentration for MgFâ‚‚ coating formation; requires careful handling [27] |
| Cyprodenate | Cyprodenate, CAS:15585-86-1, MF:C13H25NO2, MW:227.34 g/mol | Chemical Reagent |
| Csf1R-IN-13 | Csf1R-IN-13, MF:C21H20N4O3, MW:376.4 g/mol | Chemical Reagent |
The development of advanced degradable suture materials represents a multidisciplinary frontier in regenerative medicine. Albumin-based composites offer exceptional biocompatibility and tunable mechanical properties. Biodegradable metals, particularly magnesium and zinc alloys, provide superior strength and osseointegration capabilities for load-bearing applications. Graphene-enhanced sutures introduce bioactive functionality that actively promotes healing through cellular interactions. Each material class presents unique advantages and challenges that must be carefully considered for specific clinical applications. The protocols and data presented herein provide a foundation for further research and development in this rapidly evolving field, with the ultimate goal of creating next-generation surgical materials that enhance healing outcomes while eliminating the need for secondary removal procedures.
The structural design of a suture—specifically, whether it is constructed as a monofilament or multifilament thread—is a fundamental determinant of its in vivo performance and degradation behavior. These structural categories present distinct trade-offs in mechanical properties, tissue reactivity, and functional longevity, making the choice critical for specific clinical and research applications [30] [31]. Within the context of degradable biomaterials, this selection directly influences the wound healing process and the success of a medical device implantation.
Monofilament sutures consist of a single, homogeneous filament of material, while multifilament (or braided) sutures are composed of multiple finer filaments twisted or braided together [30] [31]. This fundamental physical difference dictates a suture's interaction with both the host tissue and the biological environment, guiding researchers in selecting the appropriate model for simulating implantation scenarios. Understanding these performance trade-offs is essential for designing rigorous experimental protocols and accurately interpreting in vitro and in vivo data.
Structural Characteristics and Performance Trade-offs
Monofilament Sutures: Features and Performance Profile
Monofilament sutures, fashioned from a single strand of material, are characterized by their smooth, uniform surface. This structural simplicity confers several key advantages in a research and clinical context.
- Low Tissue Drag and Trauma: Their smooth surface allows for effortless passage through tissue, minimizing drag and associated trauma [30]. This is a critical property for experiments involving delicate tissues or for simulating minimally invasive procedures.
- Reduced Infection Risk and Capillarity: The absence of inter-filament spaces eliminates the wicking effect known as capillarity, thereby preventing the migration of fluids and bacteria along the suture line [30] [31]. This makes them the preferred model for studies involving contaminated or infection-prone wound environments.
- Low Tissue Reactivity: Composed of inert synthetic polymers and presenting a minimal surface area, monofilaments typically elicit a lower inflammatory response compared to multifilament structures [30]. This is a key consideration for experiments where minimizing the host immune response is a variable.
However, the monofilament design also presents significant trade-offs:
- Handling and Knot Security: These sutures are often stiffer and possess high "memory," a tendency to return to their packaged coiled state, which can complicate handling and knot tying [30] [31]. Their smooth surface also results in lower friction, often requiring additional knot throws to ensure knot security [31].
- Mechanical Properties: While strong, some monofilament types may be more susceptible to nicking or fracturing if crushed with surgical instruments, a factor that must be controlled for in mechanical testing protocols [31].
Multifilament/Braided Sutures: Features and Performance Profile
Multifilament sutures, comprising several filaments woven or twisted together, offer a contrasting set of properties derived from their complex, multi-stranded architecture.
- Superior Handling and Knot Security: The braided structure provides exceptional pliability, making them easy for surgeons to handle and manipulate [30]. The increased surface friction grants excellent knot security, with knots holding firmly with fewer throws [30] [31].
- High Tensile Strength: The collective strength of multiple fine filaments often results in a higher tensile strength-to-diameter ratio compared to monofilaments [5]. This is a critical parameter for experiments requiring high mechanical integrity in the initial phases of healing.
- Flexibility and Pliability: Their inherent flexibility makes them well-suited for applications requiring the suture to conform to delicate or complex anatomical structures [30].
The primary disadvantages of multifilament sutures are directly linked to their structure:
- Capillarity and Infection Risk: The interstitial spaces between filaments can act as micro-conduits, drawing in fluids and bacteria through capillary action [30] [31]. This structure can harbor microorganisms, potentially leading to persistent infection, which limits their use in contaminated wound models [30] [32].
- Increased Tissue Reactivity and Drag: The larger, more textured surface area can cause increased friction ("tissue drag") during passage and may provoke a greater foreign body reaction [30] [31]. Natural multifilament sutures, like silk, are known for causing significant inflammation [31].
Table 1: Performance Trade-offs between Monofilament and Multifilament Sutures
| Performance Characteristic | Monofilament Sutures | Multifilament/Braided Sutures |
|---|---|---|
| Tissue Drag | Low [30] | High [30] |
| Knot Security | Lower (requires more throws) [30] [31] | Higher (secure with fewer throws) [30] [31] |
| Handling & Pliability | Stiffer, higher memory [30] [31] | Softer, more pliable [30] [31] |
| Risk of Infection/Capillarity | Low [30] [31] | High [30] [31] |
| Tissue Reactivity | Low [30] | Moderate to High [30] [31] |
| Tensile Strength (for diameter) | Generally high | Very high [5] |
Table 2: Common Suture Materials and Their Structural Classification
| Suture Material | Example Brand Names | Filament Type | Absorbability |
|---|---|---|---|
| Polyglactin 910 | Vicryl [5] | Multifilament | Synthetic Absorbable [31] |
| Poliglecaprone 25 | Monocryl [30] | Monofilament | Synthetic Absorbable [31] |
| Polydioxanone | PDS II [30] [33] | Monofilament | Synthetic Absorbable [31] |
| Polyglycolic Acid | Dexon [32] | Multifilament | Synthetic Absorbable |
| Silk | - [5] | Multifilament | Natural, Non-absorbable [31] |
| Polypropylene | Prolene [30] | Monofilament | Synthetic Non-absorbable [31] |
| Nylon | Ethilon [31] | Monofilament | Synthetic Non-absorbable [31] |
Experimental Protocols for Evaluating Suture Performance
Protocol 1: In Vitro Degradation and Strength Retention Kinetics
Objective: To quantitatively assess the degradation profile and mechanical integrity of absorbable sutures under simulated physiological conditions over time.
Background: The degradation of synthetic absorbable sutures occurs primarily via hydrolysis, where water molecules cleave the polymer's ester bonds [4]. The rate of this process is influenced by the suture's material composition, structure, and environmental factors such as pH and enzyme presence [4] [34]. Monitoring the loss of tensile strength provides a critical metric for predicting functional performance in vivo.
Materials (Research Reagent Solutions):
- Test Sutures: Absorbable monofilament (e.g., PDS II, Monocryl) and multifilament (e.g., Vicryl) sutures, USP size 3-0 [4] [33].
- Buffered Solutions: Phosphate-Buffered Saline (PBS, pH 7.4) to simulate physiological conditions. Acidic (pH ~5.6) and alkaline (pH ~8.8) buffers to simulate pathological or specific tissue environments [34] [33].
- Incubation System: Thermostatic water bath or incubator maintained at 37°C [4] [33].
- Mechanical Tester: Universal Testing Machine (e.g., Instron) equipped with a calibrated load cell [4] [34].
- Specimen Preparation:
- Prepare multiple suture loops for each test condition and time point (n=6-8 recommended for statistical power) [4] [33].
- Create loops by tying one surgical knot followed by four simple square knots using a standardized mandrel (e.g., a 10-mL syringe) to ensure consistent loop size [33].
- All procedures should be performed aseptically to prevent microbial contamination.
Methodology:
- Baseline Measurement (Day 0): Measure the initial tensile strength of non-immersed suture loops to establish a baseline [33].
- Immersion Study: Immerse prepared suture loops in the different buffered solutions. Ensure samples are fully submerged and incubated at 37°C [4] [33].
- Time-Point Sampling: Remove samples from incubation at predetermined intervals (e.g., Days 7, 14, 21, 28) for mechanical testing [4] [33].
- Tensile Strength Testing:
- Mount each loop on the Universal Testing Machine.
- Apply a pre-load (e.g., 1 N) to remove slack.
- Pull the loop at a constant crosshead speed (e.g., 60 mm/min) until failure [33].
- Record the maximum load at break (N).
- Data Analysis:
- Calculate the percentage of original tensile strength retained at each time point:
(Strength at Time T / Baseline Strength) * 100. - Perform statistical analysis (e.g., ANOVA followed by post-hoc tests like Tukey HSD) to compare degradation profiles between suture types and across pH conditions [4] [5].
- Calculate the percentage of original tensile strength retained at each time point:
Figure 1: Workflow for in vitro degradation and strength retention testing of sutures.
Protocol 2: Impact of Dynamic Environmental pH on Suture Integrity
Objective: To evaluate the effect of fluctuating pH, simulating an oral or digestive environment, on the tensile strength of absorbable sutures.
Background: Sutures placed in the oral cavity or gastrointestinal tract are exposed to significant and rapid pH shifts due to food and beverage consumption [34]. This protocol simulates these conditions to provide a more clinically relevant assessment of suture performance in these challenging environments.
Materials (Research Reagent Solutions):
- Test Sutures: Monofilament (e.g., PGCL) and multifilament (e.g., PGLA) absorbable sutures [34].
- Test Beverages/Solutions: Artificially synthesized tea, coffee, and cola solutions, along with artificial saliva as a control [34].
- Thermal Cycling Device: To simulate oral temperature fluctuations (e.g., between 5°C and 55°C) [34].
- Artificial Saliva: Standardized solution mimicking the ionic composition of human saliva.
- Universal Testing Machine: As in Protocol 1.
Methodology:
- Specimen Preparation: Prepare suture specimens as described in Protocol 1.
- Cyclic Exposure:
- Expose suture specimens to test beverages five times per day for 5 minutes per exposure.
- Between exposures, store specimens in artificial saliva at 37°C.
- Subject all specimens to thermal cycling (e.g., 40 cycles per day between 5°C and 55°C) to simulate intra-oral temperature changes [34].
- Time-Point Testing: Perform tensile strength testing on the Universal Testing Machine at defined intervals (e.g., Days 0, 3, 7, and 14) [34].
- Data Analysis: Analyze the maximum tensile strength at break across groups and time points to identify significant decreases in strength attributable to the beverage type and pH environment.
Quantitative Data and Analysis
Recent studies provide quantitative insights into the mechanical and degradation behaviors of different suture structures. The following tables consolidate key findings from the literature.
Table 3: Strength Retention Profile of Selected Absorbable Sutures Over Time In Vitro [4] [33]
| Suture Name | Structure | Material | ~50% Strength Retention | Complete Absorption |
|---|---|---|---|---|
| SafilQuick+ | Multifilament | Polyglycolic Acid | 9-12 days [4] | ~42 days [4] |
| Monosyn Quick | Monofilament | Glyconate | 9-12 days [4] | 56 days [4] |
| Vicryl (Polysorb) | Multifilament | Polyglactin 910 | 50% at 3 weeks [33] | 56-70 days [33] |
| PDS II | Monofilament | Polydioxanone | 60% at 6 weeks [33] | 180-210 days [33] |
| Maxon | Monofilament | Polyglyconate | 50% at 4 weeks [33] | 180 days [33] |
Table 4: Tensile Strength Comparison of Suture Materials (Baseline, USP 3-0)
| Suture Material | Structure | Reported Maximum Tensile Load (Mean ± SD) | Source / Context |
|---|---|---|---|
| VICRYL | Multifilament | Highest among tested (Silk, VICRYL, PP) [5] | Scientific Reports, 2025 |
| Polypropylene | Monofilament | Intermediate between VICRYL and Silk [5] | Scientific Reports, 2025 |
| Silk | Multifilament | Lowest among tested (Silk, VICRYL, PP) [5] | Scientific Reports, 2025 |
| Polysorb | Multifilament | 70.54 ± 7.42 N [33] | J Vet Med Sci, 2025 |
| Vicryl | Multifilament | 49.31 ± 4 N [33] | J Vet Med Sci, 2025 |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 5: Key Reagents and Equipment for Suture Performance Research
| Item Name | Function/Application | Example / Specification |
|---|---|---|
| Universal Testing Machine | Measures tensile strength, elongation, and break load of suture materials. | Instron Testing System [34] |
| Thermal Cycling Device | Simulates in vivo temperature fluctuations, particularly for oral environment studies. | 5°C to 55°C cycling [34] |
| Phosphate-Buffered Saline (PBS) | A standard isotonic solution for simulating physiological pH (7.4) in immersion studies. | pH 7.4 [33] |
| Ringer's Solution | A balanced salt solution with electrolytes, used for seasoning sutures to simulate body fluid exposure. | Sodium, Potassium, Calcium Chlorides [4] |
| Artificial Saliva | Mimics the chemical composition of human saliva for intra-oral suture studies. | Standardized ionic recipe [34] |
| Acidic & Alkaline Buffers | Simulate pathological conditions or specific tissue environments (e.g., infected wounds, urinary tract). | pH 5.6 (Acidic), pH 8.8 (Alkaline) [33] |
| HbF inducer-1 | HbF Inducer-1|Fetal Hemoglobin Activator|RUO | |
| Ascleposide E | Ascleposide E, MF:C19H32O8, MW:388.5 g/mol | Chemical Reagent |
The choice between monofilament and multifilament suture designs remains a balance of competing performance priorities. Monofilaments offer lower tissue reactivity and infection risk but can be challenging to handle. Multifilaments provide superior strength and ease of use but may potentiate infection and inflammation [30] [31]. For researchers, the decision must be guided by the specific biological and mechanical requirements of the experimental model, whether it prioritizes minimal immune response (favoring monofilaments) or requires superior initial strength and handling (favoring multifilaments).
Future research is directed toward developing advanced "smart" sutures that integrate functionalities like drug delivery and environmental responsiveness [17] [8]. Furthermore, standardizing robust in vitro test protocols that accurately predict in vivo performance, particularly under dynamic physiological conditions, is a critical ongoing challenge. A deep understanding of the fundamental trade-offs between suture structures, as outlined in these application notes, provides the essential foundation for this future innovation.
Figure 2: Decision pathway for selecting suture structure based on performance trade-offs. Green arrows indicate positive drivers, red arrows indicate negative trade-offs.
Strategic Selection and Advanced Implantation Techniques for Optimal Wound Closure
Suture selection is a critical determinant of surgical success, balancing the material's mechanical properties with the biological environment of the healing tissue. For researchers and drug development professionals working on next-generation degradable biomaterials, understanding the precise relationship between a suture's absorption profile, its tensile strength retention (TSR), and specific clinical requirements provides the foundation for intelligent material design [18]. The evolution from simple wound closure devices toward multifunctional, "smart" suture platforms underscores the need for a systematic framework that matches material capabilities to clinical applications [18] [8].
This guide provides a quantitative approach to suture selection grounded in material science principles, with structured experimental protocols for evaluating novel suture formulations. By establishing clear correlations between polymer composition, degradation kinetics, and mechanical performance requirements across tissue types, researchers can accelerate the development of optimized surgical materials that actively promote healing while minimizing complications.
Suture Material Properties and Quantitative Comparisons
Fundamental Suture Classification and Characteristics
Suture materials are fundamentally categorized by their degradation mechanism and timeline:
- Absorbable sutures: Undergo predictable degradation in the body through hydrolysis or enzymatic processes, eliminating the need for removal [35] [5]. Their utility depends on maintaining sufficient strength during the critical healing phase before absorption.
- Non-absorbable sutures: Remain at the implantation site unless removed, providing permanent structural support [35]. These materials typically elicit minimal tissue reaction but require removal in superficial applications.
Material construction further differentiates suture performance:
- Monofilament sutures: Comprise a single strand, offering smooth tissue passage and reduced infection risk but challenging handling characteristics [35] [36].
- Multifilament/Braided sutures: consist of multiple woven strands, providing superior knot security and handling but potentially increased capillarity and infection risk [35] [36].
Quantitative Analysis of Absorbable Suture Properties
Table 1: Tensile Strength Retention and Absorption Profiles of Common Absorbable Sutures
| Suture Material | 50% TSR Timeframe (Days) | Complete Absorption (Days) | Key Clinical Applications |
|---|---|---|---|
| Polyglactin 910 (Vicryl) | 14-21 [37] | 56-70 [37] | General soft tissue approximation, subcutaneous closures [35] |
| Poliglecaprone 25 (Monocryl) | 7-14 [37] | 90-120 [35] [37] | Subcuticular skin closures, pediatric procedures [35] |
| Polydioxanone (PDS) | 28-42 [37] [38] | 180 [35] [37] [38] | Slow-healing tissues, fascial closures [35] |
| Polyglycolic Acid (Dexon) | 10-14 [38] | 60-90 [35] [38] | General soft tissue approximation [35] |
| Surgical Gut (Plain) | 7-10 [37] | 70-90 [37] | Mucosal tissues, superficial lacerations [35] |
| Surgical Gut (Chromic) | 10-21 [37] | 90 [37] | Mucosal tissues, episiotomy repair [35] |
Table 2: Mechanical Properties of Non-Absorbable Sutures
| Suture Material | Construction | Tensile Strength Profile | Key Clinical Applications |
|---|---|---|---|
| Polypropylene (Prolene) | Monofilament | Minimal degradation over time [35] | Vascular anastomoses, hernia repair [35] |
| Nylon (Ethilon) | Monofilament | Gradual degradation (15-20% per year) [35] | Skin closures, microsurgery [35] |
| Polyester (Ethibond) | Braided | Permanent [35] | Cardiovascular procedures, tendon repair [35] |
| Silk | Braided | Gradual degradation over 1-2 years [35] [37] | Ligatures, oral surgery [35] |
| Surgical Steel | Monofilament | Permanent [35] | Orthopedic procedures, sternum closure [35] |
Material-Tissue Matching Framework
The following diagram illustrates the decision-making process for matching suture properties to tissue healing requirements:
Experimental Protocols for Suture Evaluation
Protocol 1: In Vitro Tensile Strength and Degradation Testing
Purpose: To quantitatively evaluate the tensile strength retention and absorption profile of novel absorbable suture materials under simulated physiological conditions.
Materials and Equipment:
- Universal testing machine (e.g., Instron) with environmental chamber [37]
- pH-controlled phosphate buffered solution (PBS, pH 7.4) at 37°C
- Suture samples (minimum n=10 per time point)
- Analytical balance (±0.1 mg precision)
- Sterile surgical gloves and instruments
Procedure:
- Baseline Measurement: Condition samples in PBS for 24 hours at 37°C. Measure initial diameter and perform baseline tensile testing (5 mm/min crosshead speed) until failure [5] [37].
- Accelerated Degradation: Immerse pre-weighed suture samples in PBS at 37°C with continuous agitation. Maintain sterile conditions throughout.
- Time-point Sampling: Retrieve samples at predetermined intervals (e.g., days 1, 3, 7, 14, 21, 28, 42) for analysis.
- Strength Testing: At each interval, measure tensile strength (straight-pull and knot-pull configurations) and calculate percentage TSR relative to baseline [37].
- Mass Loss Analysis: Rinse retrieved samples, dry to constant weight, and calculate percentage mass loss.
- Morphological Assessment: Examine suture surface and cross-section using scanning electron microscopy (SEM) to characterize degradation patterns.
Data Analysis:
- Plot TSR (%) versus time to generate degradation profiles
- Calculate absorption half-life and time to complete loss of mechanical integrity
- Compare experimental data against clinical requirements in Table 1
Protocol 2: Knot Security and Handling Characteristics Assessment
Purpose: To evaluate the practical surgical performance of suture materials, focusing on knot configuration and security.
Materials and Equipment:
- Universal testing machine with custom suture grips
- Microsurgical instruments (needle holders, forceps)
- Experienced surgeon evaluators (minimum n=3)
- Standardized evaluation scoring system
Procedure:
- Knot Configuration: Create standardized surgeon's knots and square knots according to established surgical protocols [36].
- Knot Security Testing: Mount knotted sutures in testing machine and apply tensile load (10 mm/min) until failure. Record failure mode (knot slippage vs. suture breakage).
- Handling Evaluation: Qualified surgeons perform standardized wound closure simulations, rating materials on:
- Pliability and memory
- Knot tie-down performance
- Tissue drag and passage
- Overall ease of use (5-point Likert scale)
- Statistical Analysis: Perform ANOVA with post-hoc Tukey testing (p<0.05) to identify significant differences between materials [5].
Protocol 3: In Vivo Biocompatibility and Functional Assessment
Purpose: To evaluate tissue response and functional performance of novel suture materials in a living system.
Materials and Equipment:
- Approved animal model (typically rat or rabbit)
- Histopathology equipment and stains (H&E, Masson's Trichrome)
- Immunohistochemistry capabilities (IL-10, TNF-α markers) [18]
- Sterile surgical facility and protocols
Procedure:
- Implantation: Insert test and control sutures subcutaneously or in target tissue according to approved ethical protocols.
- Time-point Analysis: Euthanize animals at predetermined intervals (1, 2, 4, 8, 12 weeks) for tissue collection.
- Histopathological Evaluation:
- Assess inflammatory cell infiltration (0-4 scale)
- Quantify foreign body giant cells and fibrosis
- Measure capsule thickness around suture material [39]
- Functional Assessment: Evaluate wound healing progression, scar formation, and tissue integration.
- Molecular Analysis: Perform cytokine profiling to characterize inflammatory response [18].
Advanced Suture Technologies and Research Applications
Emerging Suture Functionalization Strategies
Advanced suture technologies now incorporate multifunctional capabilities that extend beyond mechanical approximation:
- Antibacterial sutures: Coating or impregnation with antimicrobial agents (nanosilver, chlorhexidine, chitosan) to prevent surgical site infections [18] [40]. Recent approaches achieve 93.58% antibacterial effect against common pathogens like S. aureus and E. coli [18].
- Drug-eluting sutures: Controlled release systems for antibiotics, anti-inflammatories, or growth factors to modulate the healing microenvironment [18]. These systems can reduce inflammatory cytokines (IL-10, TNF-α) and promote angiogenesis [18].
- Smart responsive sutures: Materials designed to respond to environmental changes (pH, temperature) or provide electrical stimulation to accelerate wound healing [18] [8].
- Bio-inspired materials: Novel formulations using bacterial cellulose-chitosan composites that mimic natural structures, achieving knot-pull tensile strength of 23.3±0.6 N while promoting tissue regeneration [40].
Research Reagent Solutions for Suture Development
Table 3: Essential Research Materials for Advanced Suture Development
| Reagent/Material | Function | Research Applications |
|---|---|---|
| Polyglycolic Acid (PGA) | Synthetic polymer base | Primary material for absorbable sutures with rapid absorption [38] [9] |
| Polydioxanone (PDS) | Synthetic polymer base | Long-term absorbable sutures for slow-healing tissues [38] [9] |
| Chitosan | Natural polymer additive | Enhances antibacterial properties and flexibility [18] [40] |
| Nanoparticles (Ag, TiOâ‚‚) | Functional additives | Provide sustained antimicrobial activity [18] |
| Hyaluronic Acid | Coating material | Improves biocompatibility and antibacterial capabilities [36] |
| Chlorhexidine | Antimicrobial agent | Surgical site infection prevention in coated sutures [18] |
| Bacterial Cellulose | Base material | Bio-derived suture substrate with high purity and biocompatibility [40] |
The systematic matching of suture properties to clinical requirements represents a critical advancement in surgical materials science. By aligning quantitative metrics of tensile strength retention and absorption profiles with specific tissue healing timelines, researchers can design next-generation sutures that optimize patient outcomes. The experimental frameworks provided herein establish standardized methodologies for evaluating novel materials, while emerging technologies in antibacterial functionality, drug delivery, and smart responsiveness point toward future developments in active wound management. As the biodegradable suture market continues to expand—projected to reach $909.9 million by 2034—these principles will guide the innovation of specialized solutions tailored to specific surgical applications and patient populations [9].
Suture classification and sizing are fundamental to ensuring predictable performance, facilitating clear communication between researchers and clinicians, and maintaining quality control in the development of new degradable materials. The United States Pharmacopeia (USP) system provides a standardized framework for categorizing sutures based on diameter, a critical physical property directly linked to tensile strength [41] [42]. For research focused on degradable suture materials, a precise understanding of these standards is indispensable for accurately reporting material specifications, comparing experimental results, and designing pre-clinical studies that can be translated to clinical practice. This document outlines the key principles of suture classification and sizing, with a focus on applications within materials science research for implantable, degradable devices.
Suture Sizing Systems
USP System and Metric Measurements
The USP system classifies sutures using a numerical scale where diameter decreases as the number of zeros increases [41] [43]. This system provides a standardized nomenclature that is universally recognized. The corresponding metric sizes offer a direct measurement of the suture's diameter in millimeters, which is essential for precise engineering and material property calculations [42] [44].
Table 1: USP Suture Sizes and Metric Equivalents
| USP Designation | Synthetic Absorbable Diameter Range (mm) | Non-Absorbable Diameter Range (mm) | Typified Research and Clinical Applications |
|---|---|---|---|
| 11-0 | - | 0.01 | Microsurgery, ophthalmology [43] |
| 10-0 | 0.02–0.029 | 0.02–0.029 | Microvascular, nerve repair [45] |
| 9-0 | 0.03–0.039 | 0.03–0.039 | Microsurgery [43] |
| 8-0 | 0.04–0.049 | 0.04–0.049 | Small vessel repair, grafting [43] |
| 7-0 | 0.05–0.069 | 0.05–0.069 | Vessel repair, fine facial suturing [43] |
| 6-0 | 0.07–0.099 | 0.07–0.099 | Facial skin closure, tendon repair [43] |
| 5-0 | 0.10–0.149 | 0.10–0.149 | Vessel repair, skin closure (limbs, face) [43] |
| 4-0 | 0.15–0.199 | 0.15–0.199 | Closure of fascia, muscle [43] |
| 3-0 | 0.20–0.249 | 0.20–0.249 | Closure of thick skin, fascia [43] |
| 2-0 | 0.30–0.339 | 0.30–0.339 | Fascia, drain stitches [43] |
| 0 | 0.35–0.399 | 0.35–0.399 | Fascia closure [43] |
| 1 | 0.40–0.499 | 0.40–0.499 | Large tendon repairs, thick fascial closures [43] |
| 2 | 0.50–0.599 | 0.50–0.599 | Large tendon repairs, orthopaedic surgery [43] |
| 3 | 0.60–0.699 | 0.60–0.699 | - |
| 4 | 0.60–0.699 | 0.60–0.699 | - |
Key Suture Classification Criteria
Beyond diameter, sutures are characterized by several other critical parameters that influence their in vivo performance and experimental outcomes.
- Absorbability: Absorbable sutures are degraded in tissue within 60 days, losing tensile strength as they are broken down, making them ideal for internal tissues and temporary support [41] [46] [44]. Non-absorbable sutures maintain their tensile strength for longer than 60 days and are used for long-term support or structures that heal slowly [41] [46].
- Filament Structure: Monofilament sutures consist of a single strand, offering low tissue drag and a reduced risk of harboring bacteria, but can be prone to crushing and have higher memory, which can compromise knot security [41] [46]. Multifilament sutures (braided or twisted) provide superior handling, pliability, and knot security but have a higher tendency for bacterial colonization and increased tissue drag [41] [46].
- Material Origin: Natural sutures (e.g., silk, catgut) are derived from organic sources and typically provoke a greater inflammatory response [41] [44]. Synthetic sutures (e.g., polyglactin 910, poliglecaprone 25, polydioxanone) offer more predictable degradation profiles and lower immunogenicity [41] [18].
Table 2: Common Suture Materials and Their Properties
| Material (Brand Name Examples) | Absorbability | Filament Structure | Key Properties and Degradation Profile | Research Applications |
|---|---|---|---|---|
| Polyglactin 910 (Vicryl) | Absorbable | Multifilament/Braided | Retains 50% strength at 21 days; fully absorbed in 56-70 days [44]. Moderate tissue reaction. | Subcutaneous closure, in vitro degradation studies [41] [44]. |
| Poliglecaprone 25 (Monocryl) | Absorbable | Monofilament | Loses 50% strength in ~1 week; complete absorption by 120 days [41]. Minimal tissue reaction. | Intradermal closure models, studies requiring minimal inflammation [41]. |
| Polydioxanone (PDS) | Absorbable | Monofilament | Long-term support; retains strength for 4-6 months [41]. Complete absorption can take up to 6 months [46]. | Fascia, tendon repair models; long-term degradation studies [41] [46]. |
| Chromic Gut | Absorbable | Multifilament | Natural material; treated to delay absorption. Loses strength in 21-28 days [44]. Higher tissue reactivity. | Mucosal or rapid-healing tissue models (e.g., oral surgery) [44]. |
| Nylon (Ethilon) | Non-Absorbable | Monofilament | Gradual loss of tensile strength over years [44]. Very low tissue reactivity but high memory. | As a control in degradation studies; skin closure in long-term animal models [41] [44]. |
| Polypropylene (Prolene) | Non-Absorbable | Monofilament | Inert, maintains strength indefinitely [41]. | Vascular anastomosis models, infected wound studies [41] [44]. |
| Silk | Non-Absorbable* | Multifilament | Excellent handling but high tissue reactivity; loses strength over about a year [41]. | Securing drains/implants in research; historical control [41] [44]. |
*Note: Silk is often classified as non-absorbable but undergoes proteolytic degradation over time.
Experimental Protocols for Suture Characterization
Protocol: In Vitro Tensile Strength and Degradation Profiling
Objective: To quantitatively monitor the loss of tensile strength and mass of degradable suture materials under simulated physiological conditions over time.
Materials:
- Test Sutures: Degradable suture materials (e.g., Vicryl, Monocryl, PDS) in a specified USP size (e.g., 3-0).
- Control Sutures: Non-absorbable sutures (e.g., Polypropylene) of the same size.
- Buffered Solution: Phosphate-Buffered Saline (PBS), pH 7.4, with optional addition of 20 µg/mL sodium azide to prevent microbial growth.
- Incubation Environment: Water bath or incubator maintained at 37°C ± 1°C.
- Tensile Testing Equipment: Universal testing machine (e.g., Instron) with calibrated load cells.
- Analytical Balance: Precision of at least 0.1 mg.
Methodology:
- Sample Preparation: Cut suture samples to a standardized length (e.g., 15 cm). Record initial mass (Wâ‚€) for each sample using the analytical balance.
- Baseline Tensile Strength: Perform tensile testing on a set of samples (n≥5) at time zero. Clamp the suture ends and apply a constant extension rate (e.g., 50 mm/min) until failure. Record the peak force (F) in Newtons (N).
- In Vitro Incubation: Place individual suture samples in separate containers with a sufficient volume of PBS (e.g., 10 mL per sample) to ensure complete immersion. Incubate at 37°C.
- Time-Point Sampling: At predetermined intervals (e.g., 1, 2, 3, 4, 8, 12, 16 weeks), remove a cohort of samples (n≥5) from incubation.
- Gently rinse samples with deionized water and dry to a constant mass in a desiccator.
- Record the dry mass (Wₜ) for each sample.
- Post-Incubation Tensile Testing: Perform tensile testing on the retrieved samples as described in step 2.
- Data Analysis:
- Tensile Strength Retention: Calculate the percentage of initial tensile strength retained at each time point:
(Fₜ / F₀) × 100%. - Mass Loss: Calculate the percentage of mass remaining:
(Wₜ / W₀) × 100%. - Plot strength retention and mass loss over time to generate degradation profiles.
- Tensile Strength Retention: Calculate the percentage of initial tensile strength retained at each time point:
Protocol: Assessing Antibacterial Efficacy of Coated Sutures
Objective: To evaluate the ability of sutures with antibacterial coatings to inhibit bacterial colonization in a standardized in vitro assay.
Materials:
- Test Sutures: Antibacterial-coated sutures (e.g., Triclosan-coated Vicryl Plus) and uncoated control sutures of the same type and size.
- Bacterial Strains: Relevant American Type Culture Collection (ATCC) strains, such as Staphylococcus aureus (ATCC 25923) and Escherichia coli (ATCC 25922).
- Culture Media: Tryptic Soy Broth (TSB) and Tryptic Soy Agar (TSA).
- Equipment: Biosafety cabinet, shaking incubator, spectrophotometer, sterile containers.
Methodology:
- Suture Preparation: Aseptically cut sutures into 1 cm segments.
- Bacterial Inoculum Preparation: Grow bacterial strains overnight in TSB. Dilute the culture in fresh medium to a standard optical density (e.g., 0.1 at 600 nm), corresponding to approximately 1-5 x 10⸠CFU/mL.
- Inoculation and Incubation: Place individual suture segments in wells of a 24-well plate containing 2 mL of the bacterial inoculum. Incubate at 37°C with shaking for a defined period (e.g., 6, 24, or 48 hours).
- Bacterial Quantification (Post-incubation):
- Retrieve suture segments and rinse gently in PBS to remove non-adherent bacteria.
- Transfer each segment to a tube containing 1 mL of PBS and vortex vigorously for 2 minutes to dislodge adherent bacteria.
- Perform serial dilutions of the PBS suspension and plate on TSA plates.
- Count colony-forming units (CFU) after overnight incubation at 37°C.
- Data Analysis: Report results as CFU per suture segment. Compare the mean bacterial counts for the antibacterial-coated sutures against the uncoated controls. A statistically significant reduction (e.g., p < 0.05 using a t-test) in CFU for the test group indicates efficacy.
Visualization of Suture Characterization Workflows
Suture Development and Characterization Workflow
Suture R&D Workflow
Structure-Property Relationships in Degradable Sutures
Suture Property Relationships
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Suture Research
| Item | Function/Application | Research Context |
|---|---|---|
| Polydioxanone (PDS) | A slow-degrading polymer providing long-term mechanical support [41]. | Used as a benchmark control in long-term degradation studies (up to 6 months) [41] [46]. |
| Polyglactin 910 (Vicryl) | A mid-range absorbable braided suture with predictable degradation [41] [44]. | Ideal for studying the effects of braided structure on cellular ingrowth/bacterial adhesion and medium-term (2-3 month) degradation [41] [18]. |
| Triclosan-coated Sutures | Sutures with a broad-spectrum antimicrobial coating (e.g., Vicryl Plus) [46]. | Critical for research aimed at reducing surgical site infections (SSIs) and evaluating biofilm formation on implants [18]. |
| Bacterial Cellulose (BC) & Chitosan (CS) | Novel natural biomaterials for next-generation sutures [18] [40]. | BC offers high purity and biocompatibility; CS provides inherent antibacterial properties. Used in developing bio-inspired, multifunctional sutures [18] [40]. |
| Electrospinning Apparatus | A manufacturing technology for producing fibrous polymer scaffolds at micro/nano scale [18]. | Enables the fabrication of novel suture materials with high surface-area-to-volume ratios, useful for drug delivery and tailored degradation studies [18]. |
| Antiarol rutinoside | Antiarol rutinoside, MF:C21H32O13, MW:492.5 g/mol | Chemical Reagent |
| 7-Hydroxy-TSU-68 | 7-Hydroxy-TSU-68, MF:C18H18N2O4, MW:326.3 g/mol | Chemical Reagent |
The evolution of surgical sutures from simple wound closure devices to advanced, multifunctional biomedical implants represents a significant stride in medical science. Within the context of degradable suture materials, specialized coatings are not merely ancillary features but are critical determinants of clinical success. These engineered interfaces between the suture material and host tissue are designed to modulate fundamental biological responses, enhance mechanical performance, and mitigate postoperative complications. The strategic application of coatings transforms passive suture threads into active therapeutic participants that align with the healing timeline of the tissue they approximate.
The drive toward sophisticated coatings is fueled by the clinical limitations of uncoated sutures, which can provoke inflammatory reactions, exhibit suboptimal handling characteristics, and serve as niduses for microbial colonization [18]. The ideal coated suture for implantation must therefore fulfill a complex set of criteria: it must biodegrade in synchrony with tissue regeneration, release antimicrobial agents in a controlled manner to prevent infection, and provide sufficient knot security to maintain apposition without causing secondary trauma. This document delineates the core functions, quantitative performance metrics, and standardized testing protocols for these specialized coatings, providing a rigorous framework for their evaluation within research on degradable suture materials and implantation methodologies.
Core Coating Functions and Quantitative Analysis
Enhancing Biocompatibility and Tissue Response
Biocompatibility refers to the ability of a suture material to perform its intended function without eliciting any undesirable local or systemic effects in the host. Coatings significantly enhance this property by creating a physical and chemical barrier that modulates the suture-tissue interaction, thereby minimizing chronic inflammation and promoting integration.
Key Mechanisms:
- Reduction of Inflammatory Cytokines: Advanced coatings are engineered to sustainably release anti-inflammatory agents. For instance, silk sutures coated with combined-therapy drugs have demonstrated a significant reduction in key inflammatory markers, including interleukin-10 (IL-10) and tumor necrosis factor-α (TNF-α), thereby shortening the inflammation duration and promoting angiogenesis [18].
- Surface Modification for Cellular Response: Coatings can be functionalized with bioactive molecules such as peptides or growth factors to directly encourage specific cellular behaviors like attachment, proliferation, and differentiation. A prominent example is the coating of absorbable sutures with human serum albumin, which has been shown to enhance cell attachment and proliferation, making the sutures suitable for delivering cell therapy in soft tissues [19].
Table 1: Biomaterial Coatings for Enhanced Biocompatibility
| Coating Material | Base Suture | Experimental Model | Key Biocompatibility Outcome | Source |
|---|---|---|---|---|
| Drug-loaded Silk Fibroin | Silk | Sprague Dawley (SD) mice | Reduced IL-10 & TNF-α expression; promoted angiogenesis | [18] |
| Human Serum Albumin | Absorbable Suture | In vitro cell culture | Enhanced cell attachment and proliferation | [19] |
| Chitosan | Bacterial Cellulose | Not Specified | Imparted antibacterial properties and enhanced flexibility | [40] |
Optimizing Knot Security and Handling
Knot security is a critical mechanical property that prevents suture failure and wound dehiscence. Handling properties refer to the suture's pliability, ease of passage through tissue, and knot tie-down behavior. Coatings are extensively used to fine-tune these physical attributes.
Key Mechanisms:
- Reduction of Inter-filament Friction: In braided multifilament sutures like VICRYL (polyglactin 910), coatings such as polyglactin 370 and calcium stearate are applied to fill the interstices of the braid. This creates a smoother surface, reduces tissue drag, and allows for tighter, more secure knots by minimizing friction between strands [5].
- Enhanced Tensile and Knot-Pull Strength: The inherent structure of the suture, influenced by its coating, directly impacts its strength. Multifilament braided sutures generally score higher in tenacity and knot tensile strength compared to monofilaments. For example, a novel bio-inspired helical-hollow fiber made from bacterial cellulose and chitosan (BCS fiber) demonstrated a knot-pull tensile strength of 23.3 ± 0.6 N, exceeding the required standards for surgical sutures [40].
Table 2: Mechanical Performance of Coated versus Uncoated Sutures
| Suture Type & Construction | Coating | Tensile Strength | Knot Pull Strength | Handling Assessment | Source |
|---|---|---|---|---|---|
| VICRYL (Braided, Multifilament) | Polyglactin 370 & Calcium Stearate | Highest among tested materials | Highest knot toughness | Excellent | [5] |
| Polypropylene (Monofilament) | Not Specified | Lower than VICRYL | Lower than VICRYL | High plasticity, prone to creep | [5] |
| BCS Fiber (Helical-Hollow) | Chitosan integrated | High | 23.3 ± 0.6 N | Good flexibility | [40] |
Imparting Antimicrobial Properties
Surgical site infections (SSIs) represent a major postoperative complication. Antimicrobial coatings are a proactive strategy to prevent bacterial colonization and biofilm formation on the suture material itself.
Key Mechanisms:
- Contact-Based Antimicrobial Action: Coatings impregnated with agents like Triclosan provide a long-standing protective effect by disrupting bacterial cell membranes, effective for up to one month in vivo [47]. Metallic nanoparticles, such as nanosilver coated on polycaprolactone sutures, also provide potent, broad-spectrum contact-based antimicrobial activity [18].
- Sustainable Drug Release Systems: More advanced systems are designed for controlled release. For instance, sutures with a stage-controlled functional coating of curcumin@ZIF-8 (SZC) have shown excellent and sustained antibacterial efficacy against E. coli and S. aureus [18]. Similarly, silk sutures coated with titanium dioxide (TiOâ‚‚) achieved a sustainable antibacterial effect of 93.58% [18].
Table 3: Antimicrobial Coating Technologies and Their Efficacy
| Antimicrobial Agent | Coating/Delivery System | Target Microorganisms | Reported Efficacy | Source |
|---|---|---|---|---|
| Triclosan | Impregnated Coating | Broad-spectrum | Reduces SSI risk; protective for ~1 month | [47] |
| Nano Silver Particles | Biopolymer Coating | Broad-spectrum | Significant antimicrobial properties | [18] |
| Curcumin | Stage-controlled ZIF-8 (SZC) | E. coli, S. aureus | Excellent and sustained antibacterial activity | [18] |
| Titanium Dioxide (TiOâ‚‚) | Integrated Coating | Not Specified | 93.58% sustainable antibacterial effect | [18] |
Experimental Protocols for Coating Evaluation
Protocol: In Vitro Assessment of Antimicrobial Efficacy
1.0 Objective: To quantitatively evaluate the ability of an antimicrobial-coated suture to inhibit the growth of specific microorganisms in a controlled laboratory environment.
2.0 Materials:
- Test and Control Sutures: Antimicrobial-coated suture segments and identical uncoated segments.
- Microbial Strains: Standard reference strains (e.g., Staphylococcus aureus ATCC 6538, Escherichia coli ATCC 25922).
- Culture Media: Tryptic Soy Broth (TSB), Tryptic Soy Agar (TSA).
- Equipment: Sterile forceps, shaking incubator, spectrophotometer, colony counter.
3.0 Procedure:
- Sample Preparation: Aseptically cut suture segments to 1 cm lengths. Pre-wet in sterile saline if necessary to simulate in vivo conditions.
- Inoculum Preparation: Grow bacterial cultures to mid-log phase in TSB and dilute to a concentration of ~1 x 10^6 CFU/mL in fresh broth, confirmed by spectrophotometry.
- Incubation: Place individual suture segments in tubes containing 5 mL of the standardized inoculum. Incubate the tubes at 37°C under constant agitation for 18-24 hours.
- Enumeration of Viable Bacteria:
- After incubation, vortex each tube vigorously for 60 seconds to dislodge adhered bacteria.
- Perform serial decimal dilutions of the broth in sterile saline.
- Plate 100 µL of each dilution onto TSA plates in duplicate.
- Incubate plates at 37°C for 24 hours and count the resulting colonies.
- Calculation: Determine the bacterial concentration (CFU/mL) for each sample. Calculate the log reduction using the formula: Log Reduction = Logâ‚â‚€(CFU from control suture) - Logâ‚â‚€(CFU from test suture)
4.0 Data Interpretation: A log reduction of ≥2 (i.e., a 99% kill rate) relative to the uncoated control is typically considered indicative of significant antimicrobial activity [47] [18].
Protocol: Mechanical Testing of Knot Security
1.0 Objective: To determine the knot pull tensile strength of a suture, which is a critical indicator of its performance in securing a wound.
2.0 Materials:
- Suture Samples: Coated and uncoated control sutures.
- Equipment: Universal tensile testing machine (e.g., Instron) equipped with a calibrated load cell, surgical gloves.
3.0 Procedure:
- Knot Tying: Cut a 15 cm length of suture. Under consistent conditions, tie a standardized knot (e.g., a surgeon's square knot with three throws) in the center of the strand. Use a gauge to ensure the two free ends are of equal length (e.g., 2 cm each).
- Mounting: Secure the ends of the suture in the upper and lower clamps of the tensile tester, ensuring the knot is centered between the grips. The gauge length (distance between grips) should be standardized (e.g., 5 cm).
- Tensile Test: Initiate the test with a constant crosshead speed (e.g., 300 mm/min) until suture failure (breakage or knot slippage).
- Data Recording: The software will generate a force-elongation curve. Record the Knot Pull Strength, defined as the maximum force (in Newtons, N) sustained by the knot before failure.
4.0 Data Interpretation: Compare the mean knot pull strength of coated sutures against uncoated controls and established regulatory benchmarks. For example, the BCS fiber suture demonstrated a knot-pull strength of 23.3 ± 0.6 N, confirming its suitability [40]. The test also reveals the mode of failure (breakage at knot vs. slippage), informing on both material strength and knot security.
Protocol: In Vivo Biocompatibility and Degradation Analysis
1.0 Objective: To assess the local tissue response and degradation profile of a coated suture in a living organism.
2.0 Materials:
- Suture Samples: Sterile coated test sutures and control sutures.
- Animal Model: Approved species (e.g., Sprague Dawley rats, as used in [18]).
- Equipment & Reagents: Standard surgical suite, histology equipment, ELISA kits for cytokine analysis (e.g., for TNF-α, IL-10).
3.0 Procedure:
- Implantation: Following ethical approval, create subcutaneous pockets or intramuscular implant sites. Implant suture segments aseptically. Each animal can host multiple test and control samples in a randomized pattern.
- Monitoring & Explanation: Euthanize animals at predetermined timepoints (e.g., 3, 7, 28, 56 days post-implantation). Carefully excise the suture and surrounding tissue en bloc.
- Histological Processing:
- Fix tissue samples in 10% neutral buffered formalin.
- Process, embed in paraffin, section, and stain with Hematoxylin and Eosin (H&E) for general morphology and Masson's Trichrome for collagen deposition.
- Histopathological Scoring: A blinded pathologist should score the sections for key parameters:
- Inflammatory Cell Infiltration (Lymphocytes, Macrophages, Neutrophils)
- Fibrous Capsule Thickness
- Neovascularization
- Presence of Giant Cells
- Cytokine Analysis: Homogenize a separate portion of the explanted tissue and use ELISA to quantify the levels of pro- and anti-inflammatory cytokines (e.g., TNF-α, IL-10) [18].
4.0 Data Interpretation: A minimal, resolving inflammatory response over time, thin fibrous encapsulation, and the absence of necrosis indicate good biocompatibility. Significantly lower cytokine levels in test groups compared to controls demonstrate the anti-inflammatory efficacy of the coating.
Visualization of Coating Functions and Workflows
Functional Pathways of Specialized Suture Coatings
The following diagram illustrates the core functional pathways through which specialized coatings enhance suture performance, from initial implantation through the healing process.
Workflow for Coating Development and Evaluation
This diagram outlines a systematic research and development workflow for creating and validating a new specialized suture coating, from material synthesis to final analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Materials for Suture Coating Research
| Item Name | Function/Application | Specific Example |
|---|---|---|
| Polyglactin 370 & Calcium Stearate | Common lubricating coating for braided sutures to improve handling and knot security. | Used on VICRYL sutures [5]. |
| Triclosan | Broad-spectrum antimicrobial agent impregnated into sutures to prevent Surgical Site Infections (SSIs). | Basis for FDA-approved antimicrobial sutures; provides protection for ~1 month [47]. |
| Chitosan | Natural biopolymer used as a coating or composite material to impart antibacterial properties and enhance flexibility. | Integrated with Bacterial Cellulose (BC) to create BCS fibers [40]. |
| Human Serum Albumin (HSA) | Protein-based coating used to improve biocompatibility and cell attachment on the suture surface. | Developed as a base for biodegradable composite sutures [19]. |
| Silver Nanoparticles (AgNPs) | Nanoscale antimicrobial agents coated onto sutures for potent, contact-based antibacterial activity. | Dispersed in polyethylene glycol and coated onto polycaprolactone sutures [18]. |
| Curcumin@ZIF-8 | Advanced functional coating for stage-controlled, sustained release of antibacterial curcumin. | Creates "SZC" sutures with excellent activity against E. coli and S. aureus [18]. |
| Euphorbia factor L7a | Euphorbia factor L7a, MF:C33H40O7, MW:548.7 g/mol | Chemical Reagent |
| Rsk-IN-1 | Rsk-IN-1, MF:C22H17NO2, MW:327.4 g/mol | Chemical Reagent |
The evolution of suture materials and implantation methods represents a critical frontier in surgical research, particularly with the advent of biodegradable systems. The paradigm is shifting from sutures as passive mechanical supports to active, functional components in wound healing. Modern technique-driven applications demand a meticulous approach to material selection and protocol execution, especially within the context of degradable biomaterials research. This document provides detailed application notes and experimental protocols for soft tissue approximation, ligature, and hard tissue closing, framing them within the broader scope of next-generation suture development. The focus is on quantitative performance metrics and standardized methodologies to ensure reproducibility and robust data generation for the scientific community.
Quantitative Performance Metrics of Suture Materials
The selection of a suture material for a specific application is guided by a set of quantifiable mechanical and biological properties. The data for novel materials must be benchmarked against established standards. The following table summarizes key quantitative metrics essential for characterizing suture materials, particularly in the context of degradable systems.
Table 1: Key Quantitative Metrics for Suture Material Characterization
| Property | Definition & Measurement | Research Significance | Exemplary Data from Recent Research |
|---|---|---|---|
| Tensile Strength | The force required to break a suture divided by its cross-sectional area (N/m²). Measured via tensile testing machines on dry or moistened sutures, with the latter being more clinically relevant [48]. | Determines the suture's ability to hold tissue under stress without breaking; critical for predicting in vivo performance [48]. | Albumin-based Filament Suture (FS): 1.3 - 9.616 MPa [19]. |
| Elongation at Break | The percentage increase in length a suture undergoes before rupture [19]. | Indicates material ductility and ability to accommodate tissue swelling without excessive constriction. | Albumin-based Filament Suture (FS): 11.5% - 146.64% [19]. |
| Knot Pull Strength | The force required to cause a knot to slip or break, often referred to as effective tensile strength [48]. | Assesses knot security, a common failure point; vital for ligature and approximation protocols. | N/A in provided results. |
| Absorption Profile | The time course over which a suture loses the majority of its tensile strength and is degraded by the body. Absorbable sutures typically lose most tensile strength within 60 days post-implantation [48]. | Must be matched to the tissue's healing rate to prevent premature failure (dehiscence) or long-term inflammatory response [48]. | Varies by material (e.g., PGA, PLA, PDO, Albumin-composites); tunable via polymer composition [19] [18]. |
| Coefficient of Friction | A measure of the force resisting the suture's motion through tissue (μ = F/N) [48]. | A lower coefficient reduces tissue drag and trauma, which is crucial for delicate tissues and cosmetic outcomes [48]. | N/A in provided results. |
Research Reagent Solutions for Suture Development
The development and testing of advanced sutures require a specific toolkit. The following table details essential materials and their functions in a research setting, with a focus on novel, degradable systems.
Table 2: Essential Research Reagents and Materials for Advanced Suture Development
| Reagent/Material | Function in Research | Application Context |
|---|---|---|
| Human Serum Albumin (HSA) | Base protein material for creating novel biodegradable sutures via extrusion or sub-critical water technology; offers high biocompatibility [19]. | Serves as the primary polymer for experimental filament sutures in soft tissue approximation studies [19]. |
| Organic Modifiers (Gelatin) | Additive to base polymers to enhance mechanical properties, biocompatibility, and cell interaction [19]. | Used in composite sutures (e.g., with HSA) to fine-tune tensile strength, elongation, and degradation rates [19]. |
| Antibacterial Agents (Chitosan, Nanosilver, Curcumin@ZIF-8) | Functional coatings or composite materials to impart antimicrobial properties and prevent surgical site infections (SSI) [18]. | Applied as coatings on suture surfaces (e.g., nylon, silk, PCL) to inhibit bacterial growth like E. coli and S. aureus [18]. |
| Photocurable Biopolymers | A programmable polymer platform that can be applied to tissues and solidified in situ using blue light, enabling sutureless, atraumatic repair [49]. | Used in developing sutureless tissue reconstruction devices for nerve, cardiovascular, and abdominal wall repair [49]. |
| Electrospinning Apparatus | A manufacturing technology to produce nanofibrous sutures with high surface-area-to-volume ratios, ideal for drug delivery and wound regeneration [18]. | Employed to create multifunctional sutures that can elute drugs, antibiotics, or growth factors in a controlled manner [18]. |
| 3D Bioprinter | An advanced manufacturing tool for producing patient-specific suture architectures or scaffolds with complex geometries [18]. | Used for creating customized suture-based constructs like plates and nails, and for the casing of polymer-wrapped nerves [19] [49]. |
Experimental Protocols for Suture Characterization
Protocol: Tensile Strength and Elongation at Break
Objective: To quantitatively determine the ultimate tensile strength and elongation percentage of a novel suture material. Materials: Universal tensile testing machine, suture samples (minimum n=10, 10-20 cm length), caliper, phosphate-buffered saline (PBS) for wet testing. Methodology:
- Sample Preparation: Condition suture samples by soaking in PBS at 37°C for 24 hours to simulate the in vivo environment. Measure the diameter of each sample at three points using a caliper and calculate the average cross-sectional area.
- Machine Setup: Mount the suture ends in the tensile tester's grips, ensuring a standardized gauge length (e.g., 50 mm) and that the suture is taut but not under tension.
- Testing Parameters: Apply a constant extension rate (e.g., 50 mm/min) until the suture fractures. Record the force (in Newtons) and displacement (in mm) throughout the test.
- Data Analysis:
- Tensile Strength (MPa): Calculate by dividing the maximum load (force at break) by the original average cross-sectional area of the suture.
- Elongation at Break (%): Calculate as
(Extension at Break / Original Gauge Length) * 100. Reporting: Report mean ± standard deviation for both parameters. Include representative stress-strain curves.
Protocol: In Vitro Biodegradation Profile
Objective: To characterize the loss of tensile strength and mass of a degradable suture over time in a simulated physiological environment. Materials: Suture samples, PBS (pH 7.4) or simulated body fluid, incubator at 37°C, tensile testing machine, analytical balance. Methodology:
- Initial Measurement: Record the initial dry mass (Wi) and perform initial tensile strength tests on a baseline group (t=0) as per Protocol 4.1.
- Incubation: Immerse remaining suture samples (n=5 per time point) in PBS and incubate at 37°C. Replace the buffer solution weekly to maintain pH and ion concentration.
- Time-Point Sampling: Remove samples at predetermined intervals (e.g., 1, 2, 4, 8, 12 weeks).
- Post-Incubation Analysis:
- Mass Loss: Rinse retrieved samples with deionized water, dry to a constant mass (Wd), and calculate mass loss:
((Wi - Wd) / Wi) * 100. - Strength Retention: Perform tensile testing on the wet, retrieved samples and calculate the percentage of remaining tensile strength compared to the t=0 group. Reporting: Graph the percentage of remaining tensile strength and mass loss versus time to visualize the absorption profile.
- Mass Loss: Rinse retrieved samples with deionized water, dry to a constant mass (Wd), and calculate mass loss:
Visualizing Experimental Workflows and Material Selection
The following diagrams, generated using Graphviz DOT language, illustrate core experimental workflows and logical decision pathways in suture research.
Suture Development Workflow
Material Selection Logic
Application Notes: Advanced Manufacturing of Degradable Sutures
The development of modern degradable sutures relies on the convergence of biotechnology and advanced materials processing. These application notes detail the core methodologies for producing next-generation suture materials, focusing on recombinant protein-based materials, precision extrusion, and critical sterilization protocols.
Recombinant DNA Technology for Novel Suture Polymers
Recombinant DNA (rDNA) technology enables the production of highly pure and customizable protein-based polymers for sutures, offering significant advantages over traditional natural materials by eliminating batch-to-batch variability and risk of pathogenic contamination [50]. This technology is a biotechnology approach that allows for the generation of recombinant DNA, which involves manipulating and isolating specific DNA segments from different species and inserting them into a host organism for protein production [51].
- Key Host Organisms and Vectors: The process typically uses plasmids, artificial chromosomes, or bacteriophages as vectors to drive the replication of recombinant DNA sequences within host organisms [51]. Eligible host organisms for recombinant protein expression include bacterial cells (e.g., E. coli), yeast cells, insect cells, and mammalian cells, such as HEK293 or CHO cells [51].
- Core Methodologies:
- Transformation: This process uses bacteria such as E. coli as a biological framework. The desired DNA segment is cut with a restriction enzyme and then ligated into a vector with DNA Ligase. The vector is then inserted into a specifically prepared host cell [51] [52].
- Non-Bacterial Transformation: A similar process that does not use bacteria as the host organism [51] [52].
- Phage Introduction: This process, known as transfection, uses a phage (a virus that infects bacteria) instead of bacteria to produce phage plaques containing recombinants [51] [52].
Precision Extrusion and Material Fabrication
The transformation of raw polymers, whether synthetic or bio-derived, into consistent and reliable suture filaments is achieved through precision extrusion. This process is vital for defining the suture's diameter, tensile strength, and handling characteristics [53].
- Polymer Processing: At the core of biodegradable surgical sutures are specialized polymers such as polyglycolic acid (PGA), polylactic acid (PLA), polylactic-co-glycolic acid (PLGA), or other bioresorbable compounds. These materials are selected for their ability to maintain tensile strength during the critical healing period and then degrade safely within the body over time [53] [12].
- Hardware Components: Manufacturing relies on precision extrusion equipment, sterilization chambers, and rigorous quality control systems to ensure consistent filament diameter and material properties [53].
- Software Integration: Computer-aided design (CAD) and simulation tools are used to optimize suture performance, including degradation timelines and tensile properties, before production begins. Testing labs utilize specialized software to monitor material properties and ensure compliance with international health standards [53].
Sterilization and Biocompatibility Assurance
Sterilization is a critical step that must effectively eliminate microbial contamination without compromising the suture's mechanical integrity or altering its planned degradation profile. The regulatory framework for ensuring biological safety is evolving, with a new emphasis on risk-based assessment [53] [54].
- Sterilization Challenges: A significant challenge with biodegradable sutures is maintaining consistent degradation rates across different batches. Variations in polymer quality or, critically, the sterilization processes can adversely affect performance. For example, improper sterilization may weaken the suture, increasing the risk of wound dehiscence [53].
- Updated Regulatory Framework (ISO 10993-1:2025): The latest revision of the ISO 10993-1 standard, published in 2025, mandates a fundamental shift from a prescriptive, "checklist" approach to a risk-based biological evaluation fully integrated with the principles of ISO 14971 for risk management [54] [55].
- Key Changes: The standard now requires manufacturers to consider "reasonably foreseeable misuse" (e.g., use for longer than the intended period) in their biological risk assessment. It also refines the categorization of devices based on the nature of body contact (e.g., intact skin, mucosal membranes, tissue, blood) and provides a more conservative method for calculating contact duration, where each day of exposure is considered a full day, irrespective of the actual contact time within that day [54] [55] [56].
- Impact on Testing: The fundamental biocompatibility endpoints (e.g., cytotoxicity, sensitization) remain, but the justification for testing is more nuanced. The standard emphasizes avoiding unnecessary animal testing and requires documented rationales for the acceptance criteria defined in the biological evaluation plan [54].
Experimental Protocols
Protocol: Production of Recombinant Silk Fibroin Sutures
Objective: To express, purify, and process a recombinant silk fibroin protein for the fabrication of high-strength, biodegradable suture filaments.
Table: Research Reagent Solutions for Recombinant Silk Production
| Item | Function/Description |
|---|---|
| pET Vector System | A common plasmid vector for high-level expression in E. coli; contains a T7 lac promoter and selectable marker (e.g., ampicillin resistance) [51] [52]. |
| Restriction Enzymes (e.g., EcoRI, BamHI) | Proteins that cleave DNA at specific sequences, enabling the precise insertion of the target gene into the vector [51] [52]. |
| T4 DNA Ligase | Enzyme that catalyzes the joining of DNA fragments, ligating the silk fibroin gene into the linearized vector [51]. |
| Competent E. coli Cells | Host cells (e.g., BL21(DE3)) specially treated to facilitate the uptake of foreign DNA (transformation) [51] [52]. |
| Isopropyl β-D-1-thiogalactopyranoside (IPTG) | A molecular mimic of lactose used to induce the expression of the target recombinant protein in the E. coli host cells [50]. |
| Luria-Bertani (LB) Broth/Agar | Nutrient-rich medium for the growth and maintenance of the recombinant E. coli strains [51]. |
| Chromatography Resins (Ni-NTA) | Affinity resin used to purify recombinant proteins that have been engineered with a polyhistidine tag (His-tag) [50]. |
Methodology:
- Gene Isolation and Vector Construction: Isolate the genetic material encoding for Bombyx mori silk fibroin. Digest both the fibroin DNA and the pET vector with the selected restriction enzymes. Ligate the fragments using T4 DNA Ligase to create the recombinant plasmid [51].
- Transformation and Selection: Introduce the recombinant plasmid into competent E. coli cells. Plate the cells onto LB agar containing the appropriate antibiotic (e.g., ampicillin). Incubate to select for transformed colonies [51] [52].
- Protein Expression and Purification: Inoculate a single colony into LB broth with antibiotic. Grow the culture to the mid-log phase and induce protein expression by adding IPTG. Harvest the cells by centrifugation, lyse them, and purify the recombinant silk fibroin using Ni-NTA affinity chromatography [51] [50].
- Filament Formation: Dissolve the purified protein in a suitable solvent (e.g., hexafluoroisopropanol) to create a spinning dope. Use a precision extrusion system to dry-spin or wet-spin the dope into continuous filaments, which are then drawn and wound to align the polymer chains and enhance tensile strength [53] [5].
Protocol: In Vitro Evaluation of Suture Mechanical Properties
Objective: To quantitatively assess key mechanical performance metrics of experimental and commercial suture materials under controlled conditions.
Table: Quantitative Analysis of Suture Mechanical Properties (Adapted from Scientific Reports Data)
| Suture Material | Tensile Strength (MPa) | Elongation at Break (%) | Knot Pull Strength (MPa) | Relative Toughness |
|---|---|---|---|---|
| VICRYL (Polyglactin 910) | Highest value reported [5] | Data not specified in source | Highest value reported [5] | Highest value reported [5] |
| Polypropylene | Intermediate value [5] | Data not specified in source | Intermediate value [5] | Intermediate value [5] |
| Silk | Lowest value of the three [5] | Data not specified in source | Lowest value of the three [5] | Lowest value of the three [5] |
| Notes | Multifilament constructions (VICRYL, Silk) generally score higher in tenacity and knot security compared to monofilaments (Polypropylene). Strength increases with larger yarn counts/diameter [5]. |
Methodology:
- Sample Preparation: Condition all suture samples at standard temperature and humidity (e.g., 21°C, 65% RH) for 24 hours prior to testing. For knot strength testing, prepare standardized knots (e.g., surgeon's knot) according to USP guidelines [5].
- Tensile Testing: Use a universal testing machine equipped with a calibrated load cell. Mount the suture sample between two grips, ensuring a standardized gauge length. Apply a constant crosshead speed (e.g., 100 mm/min) until failure. Record the force-elongation curve [5].
- Data Analysis: From the force-elongation data, calculate:
- Tensile Strength: Maximum load sustained before break, divided by the original cross-sectional area.
- Elongation at Break: The strain at the point of suture failure.
- Toughness: The total energy absorbed per unit volume until break (area under the stress-strain curve).
- Knot Pull Strength: The maximum load sustained by the knotted suture before failure [5].
Protocol: Sterilization Validation and Post-Sterilization Integrity Testing
Objective: To apply a terminal sterilization method and evaluate its impact on the suture's chemical structure and mechanical performance.
Methodology:
- Sterilization Method Selection: Common methods include Ethylene Oxide (EtO) gas, gamma irradiation, or electron beam (e-beam) irradiation. EtO is often suitable for temperature-sensitive polymers but requires aeration, while irradiation can induce polymer chain scission or cross-linking [53] [54].
- Post-Sterilization Chemical Characterization: Perform Fourier-Transform Infrared (FTIR) spectroscopy and Gel Permeation Chromatography (GPC) on sterilized samples. Compare spectra and molecular weight distributions to pre-sterilization controls to identify any chemical modifications or polymer degradation [54].
- Accelerated Aging and Degradation Study: Incubate sterilized suture samples in phosphate-buffered saline (PBS) at 37°C, with pH maintained at 7.4. At predetermined time points, remove samples (n=5 per time point) and measure the remaining tensile strength and mass loss. This data helps model the degradation profile in vivo [53] [5].
Addressing Clinical Challenges: Premature Degradation, Tissue Reactivity, and Performance Optimization
Managing the Risk of Premature Strength Loss and Wound Dehiscence
Premature loss of mechanical strength in absorbable surgical sutures is a critical failure mode that can lead to wound dehiscence, infection, and compromised patient outcomes [57]. This risk is inherently linked to the hydrolytic degradation profile of the suture material, which must be carefully matched to the healing timeline of the target tissue [17] [57]. The objective of this application note is to provide researchers and scientists with standardized protocols for evaluating suture degradation and data-driven strategies for selecting sutures to minimize the risk of premature strength loss in various clinical and experimental scenarios.
Quantitative Data on Suture Strength Retention
Understanding the degradation kinetics of different suture materials is the cornerstone of risk management. The following tables summarize key experimental data on the mechanical integrity of various absorbable sutures under different conditions.
Table 1: In Vitro Tensile Strength Retention of Sutures in Ringer's Solution [57]
| Suture Material | Polymer Composition | Initial Tensile Strength (N) | Time to Significant Strength Loss (Days) | Key Degradation Characteristics |
|---|---|---|---|---|
| SafilQuick+ | Polyglycolic Acid (PGA) | - | 9-12 days | Braided, fast-absorbing; shows statistically significant strength loss in this period. |
| MonosynQuick | Glycolide, Caprolactone, Trimethylene Carbonate | - | 9-12 days | Monofilament, medium-absorbing; designed to be hydrophilic for faster hydrolysis. |
| Novosyn | Polyglycolic Acid (PGA) | - | No significant loss during study | Braided, fast-absorbing; maintained strength throughout the study period. |
| Monoplus | Glycolide, Caprolactone, Trimethylene Carbonate | - | No significant loss during study | Monofilament, slow-absorbing; showed no significant strength loss. |
Table 2: Suture Degradation in Aggressive Physiological Fluids [58]
| Suture Material | Exposure Medium | Impact on Degradation | Key Findings |
|---|---|---|---|
| Polydioxanone (PDS) | Bile, Pancreatic Juice | Highest resistance | Maintained mechanical integrity longer than other sutures in aggressive fluids. |
| Vicryl / Monocryl | Bile, Pancreatic Juice | Significant acceleration | Degradation was significantly accelerated, compromising suture integrity. |
| General Absorbables | Infected Bile/Pancreatic Juice | Severe acceleration | Bacterial strains (E. coli, Klebsiella spp., Enterococcus faecalis) further accelerated degradation. |
Experimental Protocols for Assessing Suture Degradation
Protocol for In Vitro Hydrolytic Degradation and Tensile Testing
This protocol simulates the general in vivo environment to assess the baseline degradation profile and mechanical integrity of sutures over time [57].
- Objective: To determine the loss of tensile strength of absorbable sutures over time when seasoned in an isotonic solution at controlled temperature.
- Materials:
- Absorbable suture samples (e.g., SafilQuick+, Monosyn, PDS, Vicryl)
- Ringer's solution (8.6 g/L NaCl, 0.3 g/L KCl, 0.33 g/L CaCl₂·2H₂O)
- 20 cm suture fragments
- Servohydraulic test system (e.g., MTS Bionix)
- Micrometer
- Temperature-controlled incubation environment
- Method:
- Sample Preparation: Cut suture strands into 20 cm fragments. Measure and record the diameter of each fragment using a micrometer.
- Seasoning: Immerse suture samples in Ringer's solution. Maintain the seasoning temperature at 20°C ± 2°C (for preliminary tests) or 37°C for physiological relevance.
- Tensile Testing:
- Remove samples from the solution at predetermined time points (e.g., 3, 7, 9, 12, 18 days).
- Use a servohydraulic test system with specialized grips designed to prevent crushing or mechanical damage to the suture specimen.
- Set tensile speed according to suture structure: 10 mm/min for multifilament sutures, 25 mm/min for monofilament sutures.
- Stretch the specimen until failure and record the force at break.
- Data Analysis: Calculate the tensile strength. Perform statistical analysis (e.g., ANOVA) to identify significant changes in strength over time and between different suture types.
Protocol for Degradation in Aggressive Physiological Fluids
This protocol is critical for evaluating sutures intended for use in gastrointestinal, pancreatic, or biliary surgeries [58].
- Objective: To evaluate the accelerated degradation of surgical sutures when exposed to bile, pancreatic juice, and infected environments.
- Materials:
- Absorbable suture samples (e.g., PDS, Vicryl, Monocryl)
- Physiological saline (control)
- Sterile bile and pancreatic juice
- Bacterial strains (e.g., E. coli, Klebsiella spp., Enterococcus faecalis)
- Fourier-Transform Infrared (FTIR) Spectrometer
- Scanning Electron Microscope (SEM)
- Tensile testing machine
- Method:
- Sample Exposure: Immerse suture samples in the following media: physiological saline (control), sterile bile, sterile pancreatic juice, and bile/pancreatic juice inoculated with bacterial strains.
- Incubation: Incubate samples at 37°C for predefined periods.
- Analysis:
- FTIR Spectroscopy: Analyze chemical structure changes, focusing on the carbonyl group (C=O) stretching band at ~1750 cmâ»Â¹, which is sensitive to hydrolysis and oxidation.
- SEM Imaging: Examine the surface morphology of the sutures for cracks, erosion, and pitting.
- Tensile Testing: Measure the residual tensile strength of the exposed sutures as described in Protocol 3.1.
- Data Analysis: Use Principal Component Analysis (PCA) of FTIR spectral data to classify and quantify degradation. Correlate chemical changes (FTIR) and morphological changes (SEM) with the loss of mechanical strength.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Suture Degradation Research
| Reagent / Material | Function & Application in Research | Key Considerations |
|---|---|---|
| Ringer's Solution | Isotonic solution for simulating general in vivo hydrolytic degradation [57]. | Biocompatible and does not induce chemical reactions, making it ideal for initial strength loss studies. |
| Bile & Pancreatic Juice | Aggressive physiological fluids for testing suture stability in specific surgical sites [58]. | Sourcing sterile fluids is critical. Contamination with bacteria can further accelerate degradation. |
| FTIR Spectrometer | Detects chemical bond changes (e.g., ester hydrolysis) in suture polymers during degradation [58]. | The carbonyl band (~1750 cmâ»Â¹) is a key indicator of polymer breakdown. |
| Servohydraulic Test System | Measures the tensile strength and elongation of suture materials pre- and post-degradation [57]. | Requires specialized grips to prevent crushing fragile suture samples. |
| Human Serum Albumin (HSA) | Protein-based composite material for developing novel biodegradable sutures with enhanced biocompatibility [19]. | Emerging material; offers tunable mechanical properties and biodegradability. |
| Megestrol-d3 | Megestrol-d3, MF:C22H30O3, MW:345.5 g/mol | Chemical Reagent |
The risk of premature strength loss and subsequent wound dehiscence can be mitigated through rigorous pre-clinical evaluation and evidence-based suture selection. Sutures like SafilQuick+ and MonosynQuick, which lose strength within 9-12 days, are appropriate for tissues that heal rapidly but pose a significant risk in slower-healing tissues or high-tension environments [57]. For procedures involving exposure to aggressive fluids, such as gastrointestinal, pancreatic, or biliary surgeries, sutures with higher resistance to these environments, such as PDS, are imperative [58]. The experimental protocols provided herein offer a standardized framework for researchers to characterize suture performance and make data-driven decisions that align the degradation profile of the suture material with the specific demands of the clinical or research application.
Mitigating Adverse Local Tissue Reactions and Inflammatory Responses
Adverse local tissue reactions and inflammatory responses are significant challenges in the use of degradable suture materials for medical applications. These reactions can compromise wound healing, lead to complications such as infection or suture extrusion, and ultimately negatively impact patient outcomes. The increasing global market for biodegradable surgical sutures, projected to grow at a compound annual growth rate of 11.2% and reach USD 1,190 million by 2031, underscores the critical importance of addressing these biological responses through advanced material science and targeted therapeutic strategies [8]. This document provides detailed application notes and experimental protocols for researchers and drug development professionals focused on characterizing and mitigating these adverse reactions, with a specific focus on novel albumin-based composite sutures and other advanced biomaterials.
Quantitative Analysis of Suture Properties
Mechanical Properties of Albumin-Based Sutures
The mechanical profile of a suture material directly influences its clinical application and potential to cause tissue trauma. Recent research has developed filament sutures (FS) from human serum albumin using extrusion methodology, with mechanical characterization revealing the following properties [19]:
Table 1: Mechanical Properties of Albumin-Based Filament Sutures
| Parameter | Minimum Value | Maximum Value |
|---|---|---|
| Tensile Strength | 1.3 MPa | 9.616 MPa |
| Elongation at Break | 11.5% | 146.64% |
This considerable range in both tensile strength and elongation demonstrates the mechanical versatility of albumin-based sutures, suggesting their potential applicability across various tissue types and surgical requirements. The extensive elongation capacity (up to 146.64%) is particularly noteworthy for applications requiring significant tissue compliance [19].
Market Growth Projections for Biodegradable Sutures
Understanding the market context for advanced suture materials provides important perspective for research investment and development priorities. The current and projected market data for biodegradable smart sutures includes [8]:
Table 2: Biodegradable Smart Suture Market Outlook
| Year | Market Value (USD Million) | Notes |
|---|---|---|
| 2024 | 576 | Base year valuation |
| 2025 | 628 | Projected value |
| 2031 | 1,190 | Projected value, exhibiting 11.2% CAGR |
The consistent growth, driven by increasing surgical volumes, demand for minimally invasive procedures, and advancements in biocompatible materials, highlights the expanding clinical adoption of these technologies and the importance of ongoing research to optimize their performance [59] [8].
Experimental Protocols
Protocol: Development and Characterization of Albumin-Based Sutures
Objective: To synthesize and characterize novel albumin-based composite sutures with enhanced biocompatibility and reduced potential for adverse tissue reactions.
Materials:
- Human serum albumin (HSA), first grade (e.g., Wako Pure Chemical Industries, Ltd.)
- Gelatin powder (viscosity: 30-48 mpa•s, pH: 5.5-7, Jelly strength: 120-260 bloom)
- Sub-critical water reaction system
- Extrusion apparatus with temperature control
- Tensile testing equipment
- Scanning Electron Microscope (SEM)
- Thermogravimetric analyzer (TGA)
Methodology:
- Protein Solution Preparation: Prepare a 10% (w/v) solution of human serum albumin in deionized water.
- Composite Formation: Add gelatin powder at concentrations ranging from 1-5 μg/cm² or 0.5-50 μg/mL to the HSA solution.
- Sub-critical Water Processing: Subject the protein solution to sub-critical water conditions (100-374°C under pressure) to induce soluble aggregate formation through desulphation and creation of noncovalent bonds.
- Filament Extrusion: Process the polymerized protein composite through an extrusion system at controlled temperatures to form uniform filament sutures.
- Mechanical Testing: Evaluate tensile strength and elongation at break using standardized tensile testing protocols (n≥10 samples per group).
- Morphological Analysis: Examine suture surface morphology and cross-sectional structure using SEM at various magnifications.
- Thermal Characterization: Assess thermal stability and degradation properties using TGA with a heating rate of 10°C/min under nitrogen atmosphere.
Quality Control: Adhere to FDA Class II special controls guidance for surgical sutures, including performance testing for strength, absorbability, and biocompatibility [60].
Protocol: In Vitro Assessment of Inflammatory Potential
Objective: To evaluate the potential of novel suture materials to induce inflammatory responses through systematic in vitro testing.
Materials:
- Macrophage cell line (e.g., RAW 264.7 or THP-1 derived macrophages)
- Cell culture medium and supplements
- Suture extracts prepared in sterile PBS or culture medium
- ELISA kits for inflammatory cytokines (TNF-α, IL-1β, IL-6)
- MTT or Alamar Blue cell viability assay
- Sterile tissue culture plates and equipment
Methodology:
- Suture Extract Preparation: Incubate sterile suture fragments (1 cm length per 1 mL) in cell culture medium for 24-72 hours at 37°C to generate extracts.
- Cell Culture: Maintain macrophage cells in appropriate culture conditions and seed into multi-well plates at standardized densities.
- Treatment: Expose macrophages to suture extracts at various concentrations (e.g., 10%, 25%, 50% extract in fresh medium) for 6-24 hours.
- Viability Assessment: Quantify cell viability using MTT or Alamar Blue assays according to manufacturer protocols.
- Cytokine Analysis: Collect culture supernatants and measure inflammatory cytokine levels using ELISA kits.
- Statistical Analysis: Compare cytokine levels between test materials and controls using appropriate statistical methods (ANOVA with post-hoc testing).
Visualization of Experimental Workflows
Suture Development and Testing Workflow
Tissue Reaction Mitigation Mechanisms
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Suture Development and Testing
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Human Serum Albumin (HSA) | Primary protein base for novel suture development | Provides biocompatibility and biodegradability; structural similarity to human tissue proteins [19] |
| Gelatin Powder | Organic modifier for composite sutures | Enhances cell interaction; concentration range 1-5 μg/cm² or 0.5-50 μg/mL [19] |
| Polyglycolic Acid (PGA) | Synthetic absorbable polymer reference material | Violet-dyed; hydrolytic degradation in 60-90 days; high tensile strength [61] |
| Polydioxanone (PDS) | Long-term absorbable suture reference | Violet or undyed; maintains tensile strength 180+ days; suitable for fascia closure [61] |
| Polyglactin 910 (Vicryl) | Braided synthetic absorbable reference | Violet or undyed; absorption begins 7-10 days, complete at 56-70 days [61] |
| Chromic Gut | Natural collagen-based reference | Yellow/gold/bronze color; enzymatic degradation; absorption in 90 days [61] |
| Macrophage Cell Lines | In vitro inflammatory response assessment | Measure cytokine production (TNF-α, IL-1β, IL-6) in response to suture materials |
Discussion and Future Perspectives
The development of advanced biodegradable sutures with minimized adverse tissue reactions represents a critical frontier in biomaterials research. The integration of albumin-based composites shows particular promise due to their inherent biocompatibility and tunable degradation profiles [19]. Future research directions should focus on several key areas:
First, the development of "smart" sutures with embedded sensing capabilities or controlled drug delivery represents a promising approach to actively manage inflammatory responses. These advanced systems could release anti-inflammatory agents in response to local pH changes or temperature fluctuations at the wound site [8].
Second, standardization of suture identification through color-coding systems, while primarily designed for clinical use, offers research applications for tracking different experimental materials in comparative studies. The standardized colors (violet for synthetics like Vicryl and PDS, yellow-gold for chromic gut, green for polyglyconate) provide immediate visual identification that could be adapted for research material tracking [62] [61] [63].
Third, the application of advanced analytical techniques including molecular profiling of the suture-tissue interface will provide deeper insights into the cellular mechanisms driving inflammatory responses. This knowledge will enable the rational design of next-generation materials with inherently lower immunogenic potential.
As the field progresses, researchers should maintain awareness of regulatory frameworks, particularly the FDA Class II special controls guidance for surgical sutures, which outlines essential performance criteria and testing requirements for these medical devices [60].
Optimizing Knot Security and Handling Properties for Surgical Precision
The performance of a degradable suture is critically dependent on a triad of properties: its knot security, its handling characteristics, and its predictable degradation profile. Achieving optimal knot security is paramount, as knot failure can lead to catastrophic wound dehiscence. Handling properties—encompassing pliability, memory, and ease of passage through tissue—directly influence a surgeon's efficiency and the precision of tissue approximation. For researchers developing next-generation sutures, the challenge is to engineer materials that excel in these mechanical and tactile properties while simultaneously undergoing controlled, safe resorption in vivo. This document provides detailed application notes and experimental protocols to standardize the evaluation of these key parameters, facilitating the development of advanced degradable sutures for precise surgical applications.
Suture Material Classification and Properties
Suture materials are systematically classified along several axes, each of which fundamentally impacts their performance as a degradable implant [64] [65]. The primary classification is absorbable versus non-absorbable; for this research, the focus is on absorbable materials which are broken down by the body via enzymatic reactions or hydrolysis [64]. They can be further sub-classified by their origin (natural or synthetic) and their physical structure (monofilament or multifilament) [64] [65].
- Monofilament vs. Multifilament: Monofilament sutures consist of a single strand, offering low friction and minimal risk of harboring infection but often exhibiting poor knot security and handling due to high memory [64]. In contrast, multifilament or braided sutures are composed of multiple filaments twisted or braided together, resulting in superior pliability, ease of handling, and enhanced knot security, albeit with a potential for higher tissue drag and infection risk [64] [65].
- Degradation Mechanism: Synthetic absorbable sutures, such as those based on PLGA, polydioxanone (PDS), or poliglecaprone (Monocryl), degrade primarily via hydrolysis, which offers more predictable degradation kinetics compared to natural sutures like surgical gut, which are broken down by proteolytic enzymes [64] [65].
Table 1: Properties of Common Degradable Suture Materials
| Suture Material | Structure | Tensile Strength Retention | Complete Absorption Time | Key Characteristics & Tissue Reaction |
|---|---|---|---|---|
| Polyglactin 910 (Vicryl) [64] | Braided | ~75% at 2 weeks; ~50% at 3 weeks [65] | 56-90 days [64] [65] | Minimal acute inflammatory reaction; coated versions reduce tissue drag [65]. |
| Poliglecaprone (Monocryl) [64] [65] | Monofilament | ~50-70% at 1 week; ~20-40% at 2 weeks [65] | 91-119 days [65] | Minimal tissue reaction; excellent pliability and low memory for smooth handling [65]. |
| Polydioxanone (PDS) [64] [65] | Monofilament | ~70% at 2 weeks; ~50% at 4 weeks [65] | 180-210 days [64] | Slow absorbing; minimal tissue reaction; stiffer handle and higher memory [65]. |
| Polyglycolic Acid (Dexon) [65] | Braided | ~65% at 2 weeks; ~35% at 3 weeks [65] | 60-90 days [65] | Minimal acute inflammatory reaction; hydrophilic, leading to rapid hydrolysis [65]. |
| Surgical Gut [65] | Twisted (Natural) | Highly variable based on patient factors [65] | Variable; absorbed by enzymatic process [65] | Provokes moderate to significant tissue reaction [65]. |
Research Reagent Solutions and Essential Materials
A standardized toolkit is required for the consistent fabrication and evaluation of degradable suture materials. The following table details key reagents and their functions in a research setting.
Table 2: Essential Research Materials for Suture Development and Testing
| Material / Reagent | Function & Rationale |
|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | A versatile, synthetic copolymer with tunable degradation rates and mechanical properties by varying the LA:GA ratio; ideal for creating resorbable implants with controlled drug delivery capability [66]. |
| Polydioxanone (PDS) | A slow-degrading polymer used as a benchmark for monofilament sutures requiring extended wound support (e.g., ~6 months for complete absorption) [64] [65]. |
| Polycaprolactone (PCL) | A slow-degrading polymer (over several years) useful as a blending agent to modulate the flexibility and prolong the degradation profile of other, faster-degrading polymers [66]. |
| Tricalcium Phosphate (β-TCP) Ceramics | Bioactive filler incorporated into polymer matrices (e.g., PLGA) to enhance osteoconductivity in orthopedic suture applications and modify composite degradation kinetics [66]. |
| Phosphate Buffered Saline (PBS) | Standard immersion medium for in vitro degradation studies to simulate physiological pH and ion concentration. |
| Lysozyme / Collagenase | Enzymes used in in vitro models to simulate the enzymatic component of the biodegradation environment for specific polymer types (e.g., collagenase for natural materials). |
Experimental Protocols
Protocol: In Vitro Degradation and Tensile Strength Retention
Objective: To quantitatively monitor the mass loss, mechanical integrity, and changes in suture morphology over time under simulated physiological conditions.
Materials:
- Test suture specimens (e.g., PLGA-based monofilament, braided Vicryl, PDS)
- Phosphate Buffered Saline (PBS), pH 7.4
- Incubator maintained at 37°C
- Analytical balance (accuracy 0.1 mg)
- Universal tensile testing machine (e.g., Instron) with pneumatic side-action grips
- Scanning Electron Microscope (SEM)
Methodology:
- Specimen Preparation: Cut suture samples to a standardized length (e.g., 20 cm). Record the initial dry mass (Wâ‚€) of each specimen using the analytical balance.
- Initial Tensile Strength: Test a subset of specimens (n=5) to establish baseline ultimate tensile strength (UTS). Use a gauge length of 50 mm and a crosshead speed of 50 mm/min. Record the force at break.
- Immersion Study: Immerse remaining specimens in PBS (sample volume to solution volume ratio of 1:100) and place in the 37°C incubator.
- Sampling and Analysis: At predetermined timepoints (e.g., 1, 2, 4, 8, 12 weeks), remove specimens (n=5 per timepoint).
- Mass Loss: Rinse retrieved samples with deionized water, lyophilize, and record dry mass (Wₜ). Calculate mass loss percentage as:
[(W₀ - Wₜ) / W₀] * 100. - Tensile Strength Retention: Perform tensile testing as in step 2 on the retrieved, dried specimens. Express results as a percentage of the baseline UTS.
- Morphological Analysis: Image the surface of the sutures using SEM to document cracking, erosion, pitting, or surface texture changes.
- Mass Loss: Rinse retrieved samples with deionized water, lyophilize, and record dry mass (Wₜ). Calculate mass loss percentage as:
Protocol: Quantitative Knot Security and Slip Resistance Testing
Objective: To determine the mechanical strength of various suture knots and their resistance to slipping under load.
Materials:
- Universal tensile testing machine
- Suture specimens
- Silicone rubber sheet or standardized biologic tissue simulant (e.g., synthetic skin)
Methodology:
- Knot Tying: Tie a standardized knot (e.g., surgeon's knot with two additional throws) using a consistent technique and tension. The knot can be tied either around two fixed posts on a testing jig or through and then tied on a piece of tissue simulant.
- Mounting: Secure the ends of the suture in the upper grip of the tensile tester. If using a simulant, secure the simulant in the lower grip.
- Testing: Apply a uniaxial load at a constant crosshead speed of 50 mm/min until knot failure.
- Data Collection: Record the mode of failure (knot slippage without breakage, suture breakage at the knot, or suture breakage away from the knot) and the force at failure. The force value represents the knot's security strength.
Protocol: Handling Properties Evaluation via Surgeon Feedback Scoring
Objective: To obtain quantitative, subjective data on the tactile performance of experimental sutures.
Materials:
- Experimental and commercial control suture samples
- Standardized evaluation form (Likert scale 1-5)
- Panel of trained surgeons or experienced researchers
Methodology:
- Blinding: Present coded samples to the evaluators to prevent bias.
- Task Performance: Ask evaluators to perform standardized tasks: (a) pass the suture through a simulated tissue block (e.g., synthetic skin or chamois leather); (b) tie a series of knots; (c) assess general feel.
- Scoring: Evaluators score each suture for the following parameters on a scale of 1 (poor) to 5 (excellent):
- Pliability/Flexibility: Resistance to bending.
- Memory: Tendency to return to original package curvature.
- Tissue Drag: Friction when pulled through tissue.
- Knot Tie-Down: Smoothness during knot tightening.
- Overall Handling.
- Data Analysis: Collate scores and perform statistical analysis (e.g., ANOVA) to identify significant differences between experimental and control sutures.
Data Visualization and Workflows
The following diagrams, generated with Graphviz using the specified color palette, illustrate the core experimental pathways and logical relationships in suture performance evaluation.
Diagram 1: Integrated workflow for developing and testing degradable sutures.
Diagram 2: Knot security and failure mode testing protocol.
Strategies for Controlling Degradation Kinetics to Align with Tissue Healing Rates
The clinical success of degradable implants, particularly sutures, hinges on one critical principle: the kinetics of material degradation must be synchronized with the timeline of tissue healing. Achieving this harmony prevents premature mechanical failure that can disrupt the repair process and avoids prolonged presence of foreign material that can provoke adverse immune responses [67] [17]. This application note details strategies for controlling degradation profiles, grounded in the pathophysiology of wound healing, to guide the development of next-generation suture materials. The fundamental challenge lies in engineering a material that maintains its load-bearing capacity throughout the critical proliferation and remodeling phases of healing, which can span from several weeks to over two months, before safely resorbing [67] [68].
Wound Healing Physiology and Implications for Suture Performance
Tissue repair is a dynamic, multi-stage process that provides the biological framework for suture requirements.
- Hemostasis and Inflammation (Days 0-5): Immediately following injury, a fibrin clot forms, and neutrophils and macrophages are recruited to clear debris [67] [69]. During this phase, the suture must provide adequate wound closure and withstand initial edema.
- Proliferation (Day 2 - Week 3): Fibroblasts deposit collagen to form granulation tissue, and angiogenesis occurs [67] [69]. The suture experiences its highest mechanical stress as new, fragile tissue lacks strength, requiring the device to retain high tensile strength.
- Remodeling (Week 1 - Up to 2 Years): Collagen is cross-linked and reorganized, gradually increasing tissue tensile strength [67] [69]. The suture's strength can decrease during this phase as the native tissue assumes more load, but the process is lengthy, often requiring mechanical support for several months.
Chronic wounds are characterized by a persistent inflammatory phase that disrupts this cascade, creating a hostile environment rich in degradative enzymes and with an elevated pH, which must also be considered in material design [67].
Material Selection and Engineering to Control Degradation
The degradation rate of a suture is not an intrinsic property but a tunable characteristic governed by material chemistry, morphology, and processing.
The Impact of Material Composition
Table 1: Degradation Profiles of Common Suture Materials Over 56 Days (USP 1 Diameter) [68].
| Suture Material | Composition Type | Load to Failure (Day 0) | Load to Failure (Day 28) | Time to Loss of Pre-load Capacity | Key Degradation Characteristics |
|---|---|---|---|---|---|
| Vicryl | Absorbable (PLGA copolymer) | 195 ± 4 N | ~40 N (extrapolated) | Day 42 | Rapid initial strength loss; increasing stiffness with time. |
| Maxon | Absorbable (Polyglyconate) | 164 ± 7 N | 137 ± 6 N | > Day 56 | High initial strength, maintained over 28 days; increasing strain. |
| PDS II | Absorbable (Polydioxanone) | 145 ± 3 N | 151 ± 3 N | > Day 56 | Stable mechanical properties over first 28 days. |
| Monocryl | Absorbable (PLGA copolymer) | ~90 N (extrapolated) | Unable to support 1N pre-load | Day 28 | Rapid loss of strength. |
| Ethibond | Non-absorbable (Polyester) | 145.7 ± 2 N | ~140 N | Not Applicable | Stable properties over 56 days; no significant degradation. |
The data in Table 1 reveals the stark differences in degradation kinetics among common materials. For instance, Maxon and PDS II are more suitable for orthopedic procedures where healing is slow, as they sustain high loads for at least 28 days. In contrast, Monocryl degrades too quickly for such applications [68].
Tunable Parameters for Synthetic and Natural Polymers
- Copolymer Ratio: In Poly(lactic-co-glycolic acid) (PLGA), the lactic acid (LA) to glycolic acid (GA) ratio is a primary control lever. A higher LA content makes the polymer more hydrophobic and crystalline, slowing down hydrolysis and extending degradation time [66]. PLGA degradation produces lactic and glycolic acids, metabolites handled by the body's natural pathways [66].
- Crystallinity and Molecular Weight: Materials with higher crystallinity and molecular weight degrade more slowly. The enzymatic degradation of silk fibroin, for example, is directly influenced by its β-sheet (crystalline) content. Increasing water annealing time from 2 to 12 hours significantly reduces the degradation rate in proteolytic enzymes [70].
- Advanced Composites and Additives: Incorporating nanofillers like nanohydroxyapatite (nHA) or graphene oxide nanoscrolls (GONS) can modulate degradation. In PCL-based scaffolds, nHA accelerates degradation by promoting water uptake, while GONS slows it by increasing the activation energy required for polymer chain relaxation and scission [71]. These additives can also impart additional functionality, such as antioxidant properties to mitigate oxidative stress during degradation [71].
Experimental Protocols for Characterizing Degradation Kinetics
In Vitro Enzymatic Degradation Assay
This protocol is adapted from methods used to characterize silk fibroin sponges and PCL composites [70] [71].
Objective: To quantify the mass loss and change in mechanical properties of a degradable suture material under simulated physiological conditions.
Materials:
- Test Specimens: Suture samples of precise dimensions and weight.
- Degradation Buffer: 0.1 M Phosphate Buffered Saline (PBS), pH 7.4 ± 0.2.
- Enzymatic Solution: Protease XIV or Proteinase K, prepared in PBS at concentrations of 0.01, 0.1, and 1.0 U/mL. Note: These are model enzymes for accelerated testing; collagenase may also be relevant.
- Incubation System: Water bath or incubator maintained at 37.0 ± 0.5 °C.
- Analytical Balance: Precision of 0.1 mg.
- Tensile Testing Equipment.
Procedure:
- Initial Measurements (Day 0): Record the initial dry mass (W_i) of each sample. Perform tensile testing on a separate set of samples to establish baseline load-to-failure, strain, and stiffness.
- Incubation: Place each sample in a vial containing 10-50 mL of the degradation solution (enzyme-containing or PBS control). Ensure samples are fully submerged.
- Sampling Intervals: Remove samples in triplicate at predetermined time points (e.g., 1, 3, 7, 14, 21, 28, 42, and 56 days).
- Post-incubation Processing:
- Gently rinse samples with deionized water to remove salts.
- Dry samples to a constant mass in a vacuum desiccator.
- Record the final dry mass (W_f).
- Analysis:
- Calculate Mass Loss:
% Mass Loss = [(W_i - W_f) / W_i] * 100. - Mechanical Testing: Perform tensile testing on the degraded samples.
- Kinetic Modeling: Fit the mass loss data to kinetic models (e.g., zero-order, first-order, Korsmeyer-Peppas) to determine the dominant degradation mechanism.
- Calculate Mass Loss:
Data Analysis and Kinetic Modeling
The mass loss data from degradation studies should be fitted to various kinetic models to understand the underlying mechanism [71]. The Korsmeyer-Peppas model α = k₄ ⋅ t^n (where α is fractional mass loss, k₄ is a rate constant, and n is the release exponent) is particularly useful for distinguishing between degradation mechanisms. An exponent n ≈ 1 indicates relaxation-controlled degradation (case-II transport), often seen in polymers where hydrolysis is influenced by polymer chain dynamics [71].
Table 2: Research Reagent Solutions for Degradation Kinetics Studies.
| Reagent/Equipment | Function in Protocol | Key Considerations |
|---|---|---|
| Protease XIV / Proteinase K | Model enzyme for accelerated proteolytic degradation. | Concentration must be reported; not directly representative of in vivo enzyme levels. |
| Phosphate Buffered Saline (PBS) | Maintains physiological pH and osmolarity. | pH must be buffered to 7.4 and monitored. |
| Lysozyme Solution | Model enzyme for studying hydrolysis of ester bonds in polyesters. | Commonly used at 500 µg/mL in PBS for PCL degradation [71]. |
| Water Bath/Incubator | Maintains constant physiological temperature (37°C). | Temperature control is critical for reproducible kinetics. |
| Tensile Testing Machine | Quantifies changes in mechanical properties (load to failure, stiffness). | Essential for correlating mass loss with functional performance. |
Emerging Materials and Future Directions
Research is advancing beyond traditional polymers. Albumin-based sutures derived from human serum albumin represent a novel class of protein-based materials. Preliminary characterization shows a wide range of attainable tensile strengths (1.3 to 9.6 MPa) and elongation at break (11.5 to 146.6%), indicating high tunability for specific clinical applications [19]. Furthermore, biodegradable metals like magnesium and zinc alloys are being explored for their superior strength, though controlling their corrosion products and rate remains a key challenge [17] [66]. The integration of smart hydrogels that respond to environmental stimuli (e.g., pH, enzyme activity) promises the next leap forward in creating fully adaptive wound management devices [69].
Aligning suture degradation with tissue healing is a complex but achievable goal. It requires a deep understanding of wound pathophysiology and a systematic approach to material science. By strategically selecting base polymers, tuning their physical properties, employing composite strategies, and rigorously characterizing degradation profiles using standardized protocols, researchers can engineer next-generation sutures that provide optimized mechanical support and seamlessly integrate with the body's natural healing processes.
Diagrams
Diagram 1: Suture Requirements Aligned with Wound Healing Phases. This timeline visualizes the critical mechanical demands placed on a degradable suture throughout the distinct phases of tissue repair, guiding the design of its degradation profile.
Diagram 2: Workflow for Developing Kinetically-Matched Sutures. This chart outlines an iterative R&D pipeline for designing and validating degradable sutures, from initial material selection through in vitro testing and kinetic analysis, ensuring the final product degrades in sync with tissue healing.
The development of degradable suture materials represents a dynamic frontier at the intersection of materials science, bioengineering, and clinical medicine. While the global suture market continues to expand, projected to reach $5.84 billion by 2023, the fundamental limitations of conventional materials present persistent challenges for researchers and clinicians alike [72]. The ideal degradable suture must maintain mechanical integrity until the wounded tissue has sufficiently healed, then harmoniously degrade without provoking adverse biological reactions. However, the triad of brittleness, rapid strength loss, and foreign body response continues to impede progress toward this ideal [72] [5].
These limitations are particularly consequential in specialized applications where mechanical demands are high or biological environments are sensitive. Current absorbable sutures lose their tensile strength within defined periods—from days to months—depending on their material composition [1] [73]. This degradation profile often fails to align with the nuanced timeline of tissue regeneration, especially in load-bearing tissues. Furthermore, the body's reaction to suture materials as foreign entities can lead to complications ranging from inflammation and excessive fibrosis to granuloma formation, severely delaying the wound healing process [72] [74] [75]. This application note examines innovative strategies and experimental protocols to overcome these limitations, providing researchers with methodologies to advance the next generation of degradable suture materials.
Quantitative Analysis of Current Material Limitations
A systematic understanding of current material performance provides a crucial baseline for development. The following data, synthesized from recent comparative studies, illustrates the mechanical and biological limitations of commonly used degradable suture materials.
Table 1: Mechanical Properties of Common Suture Materials
| Material | Filament Type | Tensile Strength (MPa) | Elongation at Break (%) | Strength Retention Profile | Tissue Reactivity |
|---|---|---|---|---|---|
| Polyglactin 910 (Vicryl) | Braided Multifilament | High [5] | Moderate | Loses all tensile strength within 28 days [73] | Minimal tissue reaction [73] |
| Poliglecaprone (Monocryl) | Monofilament | High [73] | High (Excellent elasticity) [73] | 60% lost in first week; all strength lost within 3 weeks [73] | Minimal tissue reaction [73] |
| Polydioxanone (PDS) | Monofilament | Good [73] | Moderate | Loss of tensile strength in 36-53 days [73] | Minimal tissue reaction [73] |
| Polyglyconate (Maxon) | Monofilament | Excellent [73] | Moderate | Loses 75% of tensile strength after 40 days [73] | Minimal tissue reaction [73] |
| Silk | Braided Multifilament | Lower than synthetics [5] | High | Progressive strength loss over months [73] | Significant tissue reaction [73] |
| Albumin-based Composite | Monofilament | 1.3 - 9.6 [19] | 11.5 - 146.6 [19] | Tunable degradation | Enhanced biocompatibility [19] |
Table 2: Foreign Body Response Profile by Material Type
| Material Category | Acute Inflammation | Chronic Inflammation | Granuloma Formation | Infection Risk |
|---|---|---|---|---|
| Natural Absorbable (Catgut) | Pronounced [74] | Histiocytic response [74] | Common after absorption [74] | Higher risk [72] |
| Synthetic Absorbable | Mild to moderate [74] | Minimal with hydrolysis [72] | Rare [75] | Lower risk [72] |
| Synthetic Non-Absorbable | Minimal [74] | Minimal with encapsulation [74] | Rare except with silk [74] [75] | Varies by material [73] |
| Novel Composites | Significantly reduced [19] | Minimal due to biocompatibility [18] | Not reported [19] | Antimicrobial properties [18] |
Advanced Material Strategies to Overcome Limitations
Addressing Brittleness through Material Engineering
Brittleness in degradable sutures primarily stems from the rigid molecular structure and high crystallinity of traditional polymers. Several innovative approaches demonstrate promise in overcoming this limitation:
Polymer Blending and Copolymerization: Creating copolymers such as poly(glycolide/lactide) random copolymers (e.g., Vicryl) has shown significant improvements in flexibility compared to homopolymers [72]. Recent work with poly(glycolide/ε-caprolactone) copolymers (Monocryl) demonstrates superior elasticity, making them particularly suitable for tissue approximation in dynamic environments [1] [73].
Nanofiber Reinforcement: Incorporating nanomaterials such as titanium dioxide (TiO₂) nanoparticles into suture materials has yielded a 93.58% improvement in antibacterial efficacy while maintaining mechanical integrity, with knot strength reaching 2.40 N at 143 μm diameter [18]. Similarly, sustainable antibacterial sutures developed from recycled silk resources reinforced with inorganic nanomaterials demonstrate significantly reduced inflammatory response while promoting wound healing [18].
Protein-Based Composites: Novel albumin-based composites using human serum albumin processed through extrusion methodology display tunable mechanical properties with tensile strengths spanning 1.3 to 9.616 MPa and elongation at break percentages ranging from 11.5% to 146.64%, offering remarkable versatility for different clinical applications [19].
Mitigating Rapid Strength Loss through Degradation Control
The mismatch between suture strength retention and tissue healing time remains a critical challenge. Advanced strategies focus on precise degradation control:
Multi-Component Material Systems: Development of triblock copolymers like poly(glycolide/p-dioxanone/trimethylene carbonate) (Biosyn) and poly(glycolide/ε-caprolactone/trimethylene carbonate) (Monosyn) allows for fine-tuning of degradation profiles to match specific tissue healing timelines [1].
Cross-Linking Modulation: Controlled cross-linking of protein-based materials like albumin composites enables researchers to engineer degradation rates that align with wound healing phases while maintaining mechanical integrity throughout the critical healing period [19].
Core-Shell Architectures: Sutures with composite structures that feature varied degradation rates between core and sheath components can maintain functional strength even as surface degradation begins, effectively prolonging functional support [72].
Suppressing Foreign Body Response via Surface Engineering
The foreign body response to suture materials can lead to complications including excessive fibrosis, granuloma formation, and impaired healing. Cutting-edge surface engineering approaches offer solutions:
Bioactive Coatings: Sustainable antibacterial and anti-inflammatory silk sutures with surface modification of combined-therapy drugs have demonstrated significant reduction in inflammatory cytokines interleukin-10 (IL-10) and tumor necrosis factor-α (TNF-α) in animal models, effectively shortening inflammation duration and promoting angiogenesis [18].
Natural Polymer Utilization: Chitin-based sutures and other natural polymers with innate biocompatibility properties reduce foreign body response through biomimicry [18]. Albumin-based composites leverage the natural biocompatibility of human serum proteins to minimize recognition as foreign material [19].
Antimicrobial Functionalization: Triclosan-coated polyglactin 910 (Vicryl Plus) represents the first FDA-approved antimicrobial suture, demonstrating significant reduction in surgical site infections [12]. More recent approaches incorporate stage-controlled antibacterial functional coatings such as curcumin@ZIF-8, which exhibits excellent antimicrobial properties against E. coli and S. aureus while maintaining mechanical performance and handling characteristics [18].
Experimental Protocols for Material Evaluation
Protocol: In Vitro Degradation and Mechanical Integrity Testing
Objective: To systematically evaluate the degradation profile and mechanical property changes of novel suture materials under simulated physiological conditions.
Materials:
- Phosphate-buffered saline (PBS), pH 7.4
- Collagenase solution (for bioactive environments)
- Temperature-controlled incubation system
- Universal tensile testing machine
- Scanning Electron Microscope (SEM)
- Thermogravimetric analyzer (TGA)
Methodology:
- Sample Preparation: Cut suture samples to standardized lengths (e.g., 10 cm). Record initial diameter and weight measurements.
- Immersion Study: Immerse samples in PBS maintained at 37°C with constant agitation to simulate physiological conditions. For enhanced biological relevance, include subgroups in collagenase-containing solution to simulate enzymatic degradation.
- Time-point Sampling: Remove samples at predetermined intervals (e.g., days 1, 3, 7, 14, 21, 28, 42, 56) for analysis.
- Mechanical Testing:
- Perform tensile strength measurement using universal testing machine according to ASTM F2544 standards.
- Calculate elongation at break and modulus from stress-strain curves.
- Conduct knot-pull strength testing using standardized knot configurations.
- Material Characterization:
- Examine surface morphology changes using SEM imaging.
- Analyze thermal properties via TGA to track polymer composition changes.
- Measure pH changes in immersion solution to track acidic degradation products.
Data Analysis:
- Plot strength retention percentage versus time to determine degradation profile.
- Compare degradation rates across different material formulations.
- Correlate surface morphological changes with mechanical property loss.
Protocol: In Vivo Biocompatibility and Foreign Body Response Assessment
Objective: To evaluate tissue response, degradation behavior, and functional performance of novel suture materials in a living organism.
Materials:
- Animal model (typically Sprague Dawley rats)
- Test suture materials and control materials (e.g., Vicryl, PDS)
- Surgical instruments and sterilization equipment
- Histological processing supplies
- Immunohistochemistry reagents for inflammatory markers
Methodology:
- Surgical Implantation:
- Create standardized subcutaneous pockets or muscular implant sites.
- Implant pre-weighed and measured suture samples.
- Ensure appropriate sample size and control groups.
- Time-course Evaluation:
- Euthanize animals at predetermined endpoints (e.g., 1, 2, 4, 8, 12 weeks).
- Explant suture samples with surrounding tissue.
- Histological Analysis:
- Process tissue samples for paraffin embedding and sectioning.
- Perform H&E staining for general morphology and cellular infiltration.
- Conduct Masson's trichrome staining for collagen deposition and fibrosis assessment.
- Implement immunohistochemistry for inflammatory markers (TNF-α, IL-6, IL-10).
- Material Analysis:
- Measure residual suture mass and diameter.
- Assess surface degradation patterns via SEM.
- Evaluate mechanical properties of explanted sutures.
Data Analysis:
- Score inflammatory response using standardized histopathological scoring systems.
- Quantify fibrous capsule thickness as indicator of foreign body response.
- Track material degradation rate in vivo and compare with in vitro findings.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Suture Material Development
| Reagent/Material | Function | Application Example | Key Considerations |
|---|---|---|---|
| Human Serum Albumin | Base material for novel biocompatible sutures [19] | Extrusion fabrication of albumin-based filaments [19] | Biocompatibility; tunable mechanical properties [19] |
| Chitosan | Natural polymer with inherent antimicrobial properties [18] | Coatings and composite sutures for infection prevention [18] | Degree of deacetylation affects properties [72] |
| Triclosan | Antimicrobial coating agent [12] | Impregnated in Vicryl Plus for surgical site infection reduction [12] | Controlled release kinetics; potential resistance [12] |
| Polydioxanone | Synthetic absorbable polymer [1] | Base material for monofilament sutures with prolonged strength retention [73] | Degradation via hydrolysis; ~50-day strength retention [73] |
| Polyglactin 910 | Synthetic absorbable copolymer [1] | Braided multifilament sutures (Vicryl) with balance of strength and absorption [73] | Complete absorption in 56-70 days [73] |
| Gelatin | Bioactive additive for tissue integration [19] | Composite sutures with enhanced cellular interaction | Cross-linking degree controls degradation rate [19] |
| Nanoparticles (Ag, TiOâ‚‚) | Antimicrobial and reinforcing agents [18] | Composite sutures with sustained antibacterial protection [18] | Concentration-dependent cytotoxicity [18] |
Visualization of Research Workflows and Biological Mechanisms
Diagram: Advanced Suture Material Development Workflow
Diagram: Foreign Body Response and Intervention Strategies
The development of next-generation degradable sutures requires a multifaceted approach that addresses the interconnected challenges of brittleness, rapid strength loss, and foreign body response. The strategies outlined in this application note—including advanced polymer composites, nanomaterial reinforcement, surface engineering, and bioactive functionalization—provide researchers with a comprehensive toolkit for material innovation.
Future directions in the field point toward increasingly sophisticated solutions. Smart sutures with sensing capabilities that can monitor wound status in real-time and provide on-demand therapies represent the next frontier in suture technology [72] [12]. Shape-memory and self-tightening sutures offer promise for improving knot security and maintaining appropriate tension, especially in minimally invasive surgical procedures [72]. Furthermore, 3D printing and electrospinning technologies enable precise control over suture architecture at multiple scales, from nanofiber construction that better mimics the native extracellular matrix to complex braided geometries with optimized mechanical properties [18].
As the global biodegradable smart suture market continues its robust growth—projected to reach USD 1,190 million by 2031—the opportunities for research innovation have never been greater [8]. By applying the methodologies and frameworks presented in this application note, researchers can contribute to the development of advanced suture materials that overcome current limitations and set new standards for performance in regenerative medicine and surgical care.
Data-Driven Performance Analysis: Validating Mechanical Properties and Biocompatibility
Comparative Analysis of Tensile Strength, Elongation, and Toughness Across Suture Materials
The selection of an appropriate suture material is a critical determinant of surgical success, directly influencing wound healing, tissue approximation, and postoperative recovery [46]. The mechanical properties of sutures—tensile strength, elongation, and toughness—determine their ability to withstand physiological stresses without breaking or excessively stretching [5] [4]. For researchers and drug development professionals working on degradable biomaterials, understanding these properties within the context of implantation methods provides the foundation for developing next-generation suture technologies. This comparative analysis systematically evaluates the mechanical performance of commercially available suture materials through standardized testing methodologies, providing essential data for material selection in both clinical practice and research development. The findings presented herein form a crucial component of a broader thesis investigating the structure-function relationships in degradable implantable materials.
Comparative Mechanical Properties of Suture Materials
Quantitative Analysis of Baseline Mechanical Properties
The mechanical behavior of suture materials varies significantly based on their chemical composition, physical structure (monofilament vs. multifilament), and manufacturing processes. The following table summarizes key mechanical properties across diverse suture materials as established by contemporary research.
Table 1: Comparative mechanical properties of various suture materials
| Suture Material | Mean Tensile Strength (N) | Elongation at Break (%) | Toughness | Material Structure | Degradation Profile |
|---|---|---|---|---|---|
| VICRYL (PGLA) | 38.7 [76] - Highest [5] | Not Reported | Highest [5] | Multifilament [5] | Absorbable [5] |
| Polydioxanone (PDO) | 37.1 [76] | Not Reported | Not Reported | Monofilament [4] | Slow absorption (180-210 days) [4] |
| Polyglycolic Acid (PGA) | 38.7 [76] maintained strength until day 10 [77] | Not Reported | Not Reported | Multifilament (braided) [4] | Short-term absorption (42-56 days) [4] |
| Polypropylene | Lower than VICRYL [5] | Not Reported | Lower than VICRYL [5] | Monofilament [5] | Non-absorbable [5] |
| Silk | 32.8 [76] - Lowest [5] | 11.5-146.64% [19] | Lower than VICRYL [5] | Multifilament [5] | Non-absorbable [5] |
| Albumin-Based Suture | 1.3-9.616 MPa [19] | 11.5-146.64% [19] | Not Reported | Not Specified | Biodegradable [19] |
Mechanical Performance During Degradation
The retention of mechanical properties during the degradation process is a crucial consideration for absorbable sutures, particularly in applications where extended tissue support is required. The rate at which sutures lose tensile strength varies significantly based on their material composition.
Table 2: Degradation profiles of absorbable suture materials
| Suture Material | Time to 50% Strength Loss | Total Absorption Time | Tensile Strength Retention Notes |
|---|---|---|---|
| Short-term Absorbable | 5-7 days [4] | 42-56 days [4] | SafilQuick+ and MonosynQuick lost strength within 9-12 days [4] |
| Medium-term Absorbable | 14-21 days [4] | 60-90 days [4] | Novosyn maintained strength during study period [4] |
| Long-term Absorbable | 28-35 days [4] | 180-210 days [4] | Monoplus (poly-p-dioxanone) showed no significant strength changes during study [4] |
| PGA | Not Reported | Not Reported | Maintained tensile strength until day 10 in oral environment simulation [77] |
| PGLA | Not Reported | Not Reported | Maintained tensile strength during first 24 hours of immersion [77] |
Experimental Protocols for Suture Characterization
Standardized Tensile Strength Testing Protocol
Purpose: To quantitatively evaluate the ultimate tensile strength of suture materials under controlled conditions, simulating physiological stresses.
Materials and Equipment:
- Universal testing machine (e.g., Universal UltraTest machine, Cometech UTM) [77] [78]
- Standardized suture samples (minimum n=5 per material type) [77]
- Environmental chamber for simulated physiological conditions (optional)
- Calibrated load cell with ±0.5% accuracy [78]
- Micrometer for diameter verification [4]
Methodology:
- Prepare suture samples of standardized length (20 cm recommended) [4]
- Mount specimens in grips with knot positioned midway between arms for knot strength evaluation [77]
- Set cross-head speed to 25 cm/min [77] or as appropriate for material stiffness
- Apply uniaxial tension until suture failure occurs
- Record maximum load (N) and stress-strain curve
- Conduct statistical analysis (Two-way ANOVA recommended) with post-hoc testing (Tukey HSD) at significance level p<0.05 [5]
Data Interpretation:
- Calculate mean tensile strength and standard deviation across samples
- Compare failure modes: suture breakage, knot slippage, or material yield
- For degradable sutures, express strength retention as percentage of original strength
Hydrolytic Degradation Assessment Protocol
Purpose: To simulate in vivo degradation behavior and quantify changes in mechanical properties over time.
Materials and Equipment:
- Ringer's solution (8.6 g/L sodium chloride, 0.3 g/L potassium chloride, 0.33 g/L calcium chloride dihydrate) [4] or artificial saliva-serum mixture (1:1) [77]
- Temperature-controlled incubation system (37°C recommended)
- pH monitoring and adjustment capability
- Tensile testing equipment
Methodology:
- Prepare degradation medium with physiological electrolyte concentrations [4]
- Immerse suture samples in solution under controlled temperature (20±2°C or 37°C) [4]
- Maintain samples for predetermined intervals (1 hour, 1, 3, 7, 10, 14 days) [77] without tension
- Retrieve samples at designated time points and blot excess moisture
- Conduct immediate tensile testing following standard protocol
- Document surface morphology changes via scanning electron microscopy (optional)
Data Interpretation:
- Plot tensile strength retention versus immersion time
- Calculate degradation rate constants
- Correlate morphological changes with mechanical property deterioration
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 3: Essential research reagents and equipment for suture material characterization
| Item | Function/Application | Representative Examples |
|---|---|---|
| Universal Testing Machine | Quantifies tensile strength, elongation, and stiffness | Universal UltraTest machine [77], Cometech UTM [78] |
| Simulated Biological Fluids | Mimics physiological environment for degradation studies | Ringer's solution [4], artificial saliva-serum mixture [77] |
| Environmental Chamber | Maintains constant temperature and humidity during testing | Incubator at 37°C [77] |
| Scanning Electron Microscope (SEM) | Visualizes surface morphology and degradation effects | Not specified [19] |
| Thermogravimetric Analyzer (TGA) | Measures thermal stability and composition | Not specified [19] |
| Micrometer | Precisely measures suture diameter | Standard micrometer [4] |
| Statistical Analysis Software | Performs statistical analysis of experimental data | IBM SPSS [5], SAS, R [77] |
Experimental Workflow and Data Interpretation Framework
The following diagram illustrates the integrated experimental workflow for comprehensive suture material characterization:
Experimental Workflow for Suture Analysis
This comparative analysis establishes clear performance distinctions among commercially available suture materials, with VICRYL (polyglactin 910) demonstrating superior tensile strength and toughness among the materials tested [5] [76]. The structural advantage of multifilament constructions over monofilaments appears to contribute significantly to enhanced mechanical performance [5]. For researchers developing new degradable suture materials, these findings highlight the critical importance of matching degradation profiles to specific clinical applications, as absorption times range dramatically from weeks to months across material types [4]. The standardized protocols provided herein offer reproducible methodologies for evaluating new suture formulations, particularly novel materials such as albumin-based composites which show promising mechanical versatility with tensile strengths ranging from 1.3 to 9.616 MPa [19]. Future research directions should focus on developing smart sutures with integrated monitoring capabilities and personalized materials tailored to specific patient populations and surgical applications.
The development of advanced degradable suture materials represents a critical frontier in biomedical engineering, particularly within the broader context of implantable medical devices and tissue regeneration strategies. These materials must maintain mechanical integrity until the wounded tissue has sufficiently healed, then gradually transfer load-bearing responsibilities to the newly formed tissue before being completely absorbed by the body. This application note provides detailed protocols for characterizing two fundamental properties of degradable suture materials: strength retention (the ability to maintain mechanical function over time) and total absorption timeline (the complete degradation and elimination of the material). Understanding the relationship between in-vitro degradation models and in-vivo performance is essential for predicting clinical behavior and optimizing material design for specific surgical applications [79].
Theoretical Background: Degradation Mechanisms
The degradation of biodegradable polymers commonly used in sutures, such as polyglycolic acid (PGA), polylactic acid (PLA), polydioxanone (PDO), and polycaprolactone (PCL), proceeds primarily through hydrolysis of their backbone ester bonds [80]. This random, bulk hydrolysis process is influenced by water penetration into the polymer matrix, leading to a decrease in molecular weight and, eventually, mass loss and disintegration. The degradation process follows a characteristic two-stage mechanism in semi-crystalline polymers:
- Stage 1: Rapid degradation and chain scission occur primarily in the amorphous regions, leading to an initial increase in crystallinity as polymer chains in amorphous regions cleave and allow realignment.
- Stage 2: Slower degradation of the crystalline regions begins once the amorphous matrix has been sufficiently broken down [80].
For sutures, the retention of mechanical strength is closely tied to the molecular weight of the polymer. Studies on polylactides have demonstrated that rapid strength loss typically occurs when the inherent viscosity (a proxy for molecular weight) drops to a critical threshold of approximately 0.5-0.65 dl/g [81]. Beyond this point, the polymer matrix can no longer sustain significant mechanical loads.
Table 1: Factors Influencing Suture Degradation Rates
| Factor Category | Specific Factor | Effect on Degradation Rate |
|---|---|---|
| Material Properties | Crystallinity | Higher crystallinity slows degradation [80] [81] |
| Initial Molecular Weight | Higher molecular weight extends strength retention [81] | |
| Copolymer Composition | Adjusting L:G (lactide:glycolide) ratios modifies degradation time [82] | |
| Structural Properties | Suture Diameter | Smaller diameters degrade faster due to higher surface area-to-volume ratio [81] |
| Porosity | Porous structures generally increase degradation rate [80] | |
| Environmental Factors | pH (acidic vs. basic) | Acidic conditions accelerate ester hydrolysis [80] |
| Enzyme Presence | Specific enzymes (e.g., esterases) can significantly accelerate degradation [80] | |
| Implantation Site | Vascularization and local cellular activity affect in-vivo resorption [82] |
Experimental Protocols
In-Vitro Degradation Profiling
Reagents and Equipment
- Degradation Medium: Phosphate Buffered Saline (PBS, pH 7.4) or Simulated Body Fluid (SBF)
- Temperature Control System: Immersion water bath or environmental chamber maintained at 37±0.5°C
- Testing Machines: Analytical balance (0.1 mg accuracy), universal tensile testing machine
- Characterization Instruments: Inherent viscosity measurement system, SEM, pH meter
- Optional Additives: Specific enzymes (e.g., esterases, collagenases) or bacterial collagenase for accelerated studies [80]
Procedure
Sample Preparation: Cut suture samples to standardized lengths (e.g., 10-15 cm). Record initial mass (Mâ‚€) and diameter. Ensure a minimum of n=5 samples per time point for statistical significance.
Immersion Study Setup:
- Place individual suture samples in containers with a sufficient volume of degradation medium (recommended ratio: 1 mL medium per 1 cm suture length).
- Maintain containers at 37±0.5°C in a temperature-controlled environment for the duration of the study.
- For long-term studies, replace the degradation medium periodically (e.g., weekly) to maintain sink conditions and prevent significant pH drift.
Time Point Sampling:
- Remove samples at predetermined intervals (e.g., 1, 2, 4, 8, 12, 16, 20, 24 weeks) for analysis.
- At each time point, gently rinse retrieved samples with deionized water and dry to constant mass under vacuum before analysis.
Strength Retention Analysis:
- Test dry samples using a universal tensile testing machine according to standard suture testing protocols (e.g., ASTM F1634).
- Calculate strength retention percentage: (Tensile strength at time t / Initial tensile strength) × 100%.
Mass Loss Profiling:
- Measure dry mass at each time point (Mₜ).
- Calculate mass loss percentage: [(M₀ - Mₜ) / M₀] × 100%.
Supplementary Characterization:
- Perform inherent viscosity measurements in appropriate solvents (e.g., chloroform for PLA-based sutures).
- Use SEM to examine surface morphology changes, including cracking, pitting, or erosion patterns.
- Monitor pH changes in the degradation medium over time.
In-Vivo Degradation Profiling
Animal Model and Implantation
Animal Selection: Select appropriate animal models (typically rats, rabbits, or miniature pigs) based on the intended clinical application. Obtain necessary IACUC approval prior to study initiation.
Suture Implantation:
- Implant suture samples in relevant anatomical locations (subcutaneous, intramuscular, or site-specific implantation).
- For strength retention studies, sutures may be implanted in a looped configuration to facilitate retrieval and mechanical testing.
- Include appropriate radiographic markers if necessary for imaging-based monitoring.
Study Duration and Time Points: Plan retrieval time points based on expected degradation profile (e.g., 2, 4, 8, 12, 16, 20, 24 weeks post-implantation).
Sample Retrieval and Analysis
Explanation and Preparation: At each time point, euthanize animals humanely according to approved protocols. Carefully retrieve suture samples with surrounding tissue.
Mechanical Testing:
- Gently remove surrounding tissue without damaging the suture.
- Test explained sutures for tensile strength immediately after retrieval or after careful cleaning and drying, following the same protocol as in-vitro testing.
Histological Analysis:
- Fix tissue-suture complexes in neutral buffered formalin.
- Process for histological sectioning and staining (H&E, Masson's Trichrome).
- Evaluate local tissue response, including inflammatory cell infiltration, fibrous capsule formation, and tissue integration.
Residual Mass Determination:
- Carefully digest surrounding tissue using enzymatic methods (e.g., papain solution) without degrading the suture material.
- Dry and weigh residual suture material to determine mass loss in vivo.
The following workflow diagram illustrates the integrated experimental approach for comprehensive degradation profiling:
Data Analysis and Interpretation
Quantitative Degradation Profiles
Table 2: Comparative Degradation Profiles of Selected Suture Materials
| Polymer Material | Strength Retention Half-Life (Weeks) | Total Absorption Time (Weeks) | Key Characteristics |
|---|---|---|---|
| Polyglycolic Acid (PGA) | 2-4 [19] | 12-16 [19] | Fastest degradation, good initial strength |
| Polylactic Acid (PLA) | 10-20 [81] | 36-48 [81] | Slow degradation, high initial strength |
| Polycaprolactone (PCL) | >24 [80] | 36-60 [80] [83] | Very slow degradation, flexible |
| Polydioxanone (PDO) | 4-6 [19] | 24-30 [19] | Good handling properties, moderate degradation |
| Carp Collagen | 2-3 [82] | 8-12 [82] | Excellent biocompatibility, natural material |
| Albumin-Based Composite | 1-2 [19] | 6-10 [19] | Emerging material, drug delivery potential |
In-Vitro In-Vivo Correlation (IVIVC)
Developing a predictive relationship between in-vitro and in-vivo degradation is essential for reducing animal testing and accelerating material development. Studies on magnesium implants have shown that in-vivo degradation can be approximately four times slower than in-vitro degradation under certain conditions [84]. For polymeric systems, the correlation depends on multiple factors:
- Time Scaling: Apply a consistent time-scaling factor to relate in-vitro and in-vivo data.
- Deconvolution Methods: Use mathematical approaches (e.g., Wagner-Nelson, numerical deconvolution) to estimate in-vivo absorption profiles from plasma concentration data [79].
- Accelerated Testing: Develop accelerated in-vitro methods that maintain the same degradation mechanisms as real-time conditions.
The following diagram illustrates the conceptual framework for establishing a predictive IVIVC model for degradable sutures:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Degradation Studies
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Phosphate Buffered Saline (PBS) | Standard degradation medium simulating physiological pH and ionic strength | 1X PBS, pH 7.4 ± 0.1 |
| Simulated Body Fluid (SBF) | Ion concentration similar to human blood plasma for more biologically relevant conditions | Kokubo's SBF recipe |
| Enzymatic Solutions | Accelerate degradation or simulate specific biological environments | Bacterial collagenase, esterases, protease solutions |
| Cross-linking Agents | Modify degradation rate and mechanical properties of collagen-based materials | EDC/NHS cross-linking systems [82] |
| Medical-Grade Polymers | Base materials for suture development with controlled purity and properties | Purasorb PLGA polymers, Caproprene, Dioxaprene [82] [83] |
| Histological Stains | Evaluate tissue response and material integration post-implantation | Hematoxylin & Eosin (H&E), Masson's Trichrome |
| Analytical Standards | Characterize molecular weight changes during degradation | Polystyrene standards for GPC, viscosity reference materials |
Comprehensive degradation profiling through integrated in-vitro and in-vivo studies provides essential data for predicting the clinical performance of degradable suture materials. The protocols outlined in this application note enable researchers to systematically evaluate strength retention profiles and total absorption timelines, critical parameters for ensuring that sutures provide adequate mechanical support during tissue healing while being completely resorbed once their function is fulfilled. The development of robust IVIVC models further enhances the predictive capability of in-vitro testing, supporting the rational design of next-generation suture materials with optimized degradation characteristics for specific clinical applications.
Within the broader research on degradable biomaterials for medical implantation, suture materials represent a mature yet critically important class of medical devices. The performance of these materials directly influences wound healing, tissue regeneration, and surgical outcomes. This application note provides a structured benchmark of three widely used commercial absorbable sutures—Vicryl (Polyglactin 910), Monocryl (Poliglecaprone 25), and PDS (Polydioxanone)—and explores emerging novel materials. Designed for researchers and drug development professionals, this document synthesizes quantitative performance data, experimental methodologies, and analytical frameworks to support material selection and future biomaterial development.
Suture Classification and Key Characteristics
Sutures are primarily classified by their absorbability, filament structure, and material origin (synthetic vs. natural) [41] [31]. Understanding these classifications is fundamental to selecting the appropriate material for a specific research application or anticipated clinical use.
Absorbable vs. Non-absorbable: Absorbable sutures lose most of their tensile strength over weeks to months and are gradually degraded in the body, eliminating the need for removal [41] [31]. They are ideal for deep tissue closure and healing tissues. Non-absorbable sutures maintain their strength for longer periods (over 60 days) and are used when long-term tissue support is required, or are removed once the skin surface has healed [31] [46].
Monofilament vs. Multifilament: Monofilament sutures consist of a single strand, offering smooth passage through tissues with a lower risk of bacterial colonization [41] [31]. However, they often have higher "memory," making them stiffer and requiring more secure knots. Multifilament sutures are braided or twisted, providing superior handling, pliability, and knot security, but can cause increased tissue drag and harbor bacteria within their interstices [41] [31].
Synthetic vs. Natural: Modern synthetic sutures (e.g., Vicryl, Monocryl, PDS) are degraded primarily by hydrolysis, which typically elicits a milder tissue reaction compared to natural sutures like catgut or silk, which are degraded by proteolysis and provoke more inflammation [41] [31].
Table 1: Classification and Fundamental Properties of Benchmark Sutures
| Suture (Generic Name) | Brand Name | Absorbability | Filament Structure | Material Composition | Degradation Mechanism |
|---|---|---|---|---|---|
| Polyglactin 910 | Vicryl | Absorbable | Multifilament (Braided) | Copolymer of glycolide and L-lactide [41] | Hydrolysis [41] |
| Poliglecaprone 25 | Monocryl | Absorbable | Monofilament | Copolymer of glycolide and ε-caprolactone [85] [86] | Hydrolysis [86] |
| Polydioxanone | PDS | Absorbable | Monofilament | Polymer of p-dioxanone [41] | Hydrolysis [41] |
Quantitative Performance Benchmarking
In Vivo Tensile Strength Retention and Absorption Profile
The retention of tensile strength during the critical wound-healing period is a paramount performance metric for absorbable sutures. The data below provides a comparative timeline of mechanical integrity.
Table 2: In Vivo Tensile Strength Retention and Absorption Timeline
| Suture Type | 50-60% Strength Retention | Full Absorption Timeline | Key Characteristics |
|---|---|---|---|
| Vicryl | 2-3 weeks [41] | 8-10 weeks [41] | Braided structure offers good handling and knot security [41]. |
| Monocryl | ~1 week [41] [86] | 90-119 days [85] [86] | Ultra-pliable, minimal tissue reaction, rapid initial strength loss [41] [86]. |
| PDS | 4-6 weeks [41] | ~6 months (180 days) [41] [46] | Provides long-term tissue support, high memory [41]. |
Biomechanical and Degradation Performance in Simulated Environments
Suture performance can be significantly altered by the physiological environment. Recent studies have quantified this under simulated conditions.
Table 3: Biomechanical and Degradation Performance in Aggressive Physiological Fluids
| Performance Metric | Vicryl (Polyglactin-910) | Monocryl (Poliglecaprone 25) | PDS (Polydioxanone) |
|---|---|---|---|
| Resistance to Bile/Pancreatic Juice | Moderate degradation acceleration [58] | Significant degradation acceleration [58] | Highest resistance to degradation; maintains mechanical integrity longest [58] |
| Elongation during Cyclic Loading | N/A | N/A | N/A |
| Ultimate Load to Failure | N/A | N/A | N/A |
Experimental Protocols for Suture Analysis
Protocol: In Vitro Hydrolytic and Enzymatic Degradation
This protocol is adapted from studies investigating suture degradation in physiological fluids, including those simulating the gastrointestinal environment [58].
- Objective: To evaluate the chemical and mechanical degradation of absorbable sutures in various physiological fluids.
- Materials:
- Test Sutures: Vicryl, Monocryl, PDS, and other experimental sutures.
- Degradation Media: Phosphate-buffered saline (PBS, control), sterile bile, sterile pancreatic juice.
- Incubation System: Sterile containers, shaking water bath or incubator maintained at 37°C.
- Analysis Equipment: FTIR Spectrometer, Scanning Electron Microscope (SEM), Universal Mechanical Tester.
- Methodology:
- Sample Preparation: Cut suture samples to standardized lengths. Record initial weight and dimensions.
- Immersion: Immerse suture samples in the different degradation media. Ensure a consistent volume-to-surface area ratio. Maintain at 37°C to simulate physiological temperature.
- Time-Point Sampling: Remove samples in triplicate at predetermined time points (e.g., 1, 2, 4, 8 weeks).
- Analysis:
- FTIR Spectroscopy: Analyze chemical structure changes, focusing on the carbonyl (C=O) band at ~1750 cmâ»Â¹, which is sensitive to hydrolysis [58].
- SEM Imaging: Examine surface morphology for cracks, erosion, and bacterial colonization.
- Tensile Testing: Perform load-to-failure tests to determine retained tensile strength and elongation.
- Data Analysis: Use Principal Component Analysis (PCA) on FTIR spectral data to objectively track and compare degradation pathways between suture types [58].
Protocol: Biomechanical Analysis of Suture-Tissue Constructs
This protocol is based on biomechanical studies evaluating suture performance in soft tissue models, such as meniscal repair [87].
- Objective: To quantify the biomechanical properties of different sutures in a tissue model under cyclic and load-to-failure conditions.
- Materials:
- Tissue Model: Fresh porcine menisci or other relevant soft tissue (e.g., porcine skin, fascia).
- Sutures: Test sutures of interest (e.g., monofilaments vs. braided, different materials).
- Testing Equipment: Bionix MTS (or similar) mechanical testing system, S-hooks, clamps.
- Methodology:
- Specimen Preparation: Prepare uniform tissue samples. Suture placement should be standardized (e.g., simple stitch, 1 cm from tissue edge).
- Knot Tying: Tie all sutures with a standardized knot technique (e.g., five square knots) to minimize variability.
- Cyclic Loading:
- Apply a preload (e.g., 5 N for 30 seconds).
- Subject the suture-tissue construct to a set number of cycles (e.g., 30 cycles between 5-30 N at 0.25 Hz) to simulate early postoperative stresses [87].
- Load-to-Failure Test: Following cyclic loading, immediately subject the construct to a tensile test at a constant displacement rate (e.g., 5 mm/s) until failure.
- Data Collection:
- Elongation: The difference in displacement between the preload and the final cycle.
- Ultimate Load to Failure (N): The maximum force sustained by the construct.
- Stiffness (N/mm): The slope of the linear region of the load-displacement curve.
- Mode of Failure: Record as suture breakage, tissue pull-through, or knot failure.
Visualization of Sperty Selection and Experimental Workflow
Logic for Suture Material Selection
The following diagram outlines a decision-making framework for selecting an appropriate suture based on key wound and tissue characteristics.
Workflow for Suture Degradation Analysis
This workflow details the key steps in the in vitro degradation and analysis protocol described in Section 4.1.
The Scientist's Toolkit: Research Reagent Solutions
This section lists essential materials and reagents required for conducting the experiments outlined in this application note.
Table 4: Essential Research Reagents and Equipment for Suture Benchmarking
| Item Name | Function/Application | Specific Examples / Notes |
|---|---|---|
| Commercial Sutures | Test articles for benchmarking studies. | Vicryl (Polyglactin 910), Monocryl (Poliglecaprone 25), PDS (Polydioxanone) [41] [86]. |
| Degradation Media | Simulate physiological and aggressive bodily fluids for in vitro testing. | Phosphate-Buffered Saline (PBS), sterile bile, sterile pancreatic juice [58]. |
| Fourier-Transform Infrared (FTIR) Spectrometer | Analyze chemical bond changes and monitor polymer degradation (e.g., hydrolysis of ester bonds) [58]. | Focus on carbonyl (C=O) stretch band at ~1750 cmâ»Â¹. |
| Universal Mechanical Tester | Quantify biomechanical properties: tensile strength, elongation, and stiffness of suture-tissue constructs [87]. | MTS Bionix systems or equivalent. |
| Scanning Electron Microscope (SEM) | Visualize surface morphology, erosion, cracks, and bacterial adhesion on sutures before and after degradation [58]. | Requires proper sample preparation (sputter coating). |
| Porcine Menisci / Soft Tissue | A standardized, biologically relevant tissue model for biomechanical testing of sutures [87]. | Ensures consistency and models human tissue mechanics better than cadaveric tissue from elderly donors. |
Emerging Trends and Novel Materials
The field of degradable sutures is evolving with a focus on enhancing performance and functionality.
- Antimicrobial Sutures: Sutures like Vicryl Plus and Monocryl Plus are coated with the broad-spectrum antibacterial agent triclosan, which has been shown to inhibit bacterial colonization (e.g., by S. aureus and E. coli) and reduce the risk of associated infections [41] [46].
- Barbed Sutures: Technologies such as Stratafix feature barbs along the suture length, which anchor into tissue and distribute tension evenly. This design can obviate the need for knots, potentially reducing operative time and improving security [41].
- Suture-Free Reconstruction: Beyond sutures, research is advancing towards atraumatic tissue reconstruction. A novel platform using photocurable biopolymers that conform to tissues and are activated with blue light has received regulatory authorization for peripheral nerve repair, representing a potential paradigm shift from penetrating sutures [49].
The development of degradable biomaterials for suture and implantation represents a cornerstone of modern regenerative medicine. The core premise of these materials is to provide temporary mechanical support and then degrade harmoniously with the body's natural healing processes, ideally leading to optimal functional and aesthetic outcomes with minimal scarring. Evaluating the biocompatibility and scarring outcomes of these materials is therefore a critical multidisciplinary endeavor, integrating perspectives from materials science, cell biology, and clinical medicine. Biocompatibility extends beyond simple inertness; it encompasses the host tissue's multifaceted response to the implant, including acute and chronic inflammation, foreign body reactions, and the subsequent tissue remodeling phase [17] [48]. Scarring, or fibrosis, is a direct consequence of this dynamic interplay, often arising from a dysregulated healing process characterized by excessive deposition of collagen and other extracellular matrix (ECM) components [88]. This document provides detailed application notes and experimental protocols, framed within broader thesis research on degradable sutures, to standardize the preclinical and clinical evaluation of these critical parameters for an audience of researchers, scientists, and drug development professionals.
Quantitative Data on Material Properties and Biological Responses
A critical step in evaluating new degradable materials is the systematic quantification of their physical properties and the corresponding biological responses they elicit. The data below, synthesized from recent studies, provides a benchmark for comparison.
Table 1: Mechanical Properties of Suture Materials from Preclinical and Commercial Studies
| Material Type | Tensile Strength (MPa) | Elongation at Break (%) | Key Findings | Source (Model) |
|---|---|---|---|---|
| VICRYL (Polyglactin 910) | Highest among tested (commercial) | N/R | Multifilament structure yields high tensile strength, toughness, and knot security. | [5] (In vitro) |
| Polypropylene | Intermediate | N/R | Monofilament structure; high plasticity but less strong than VICRYL. | [5] (In vitro) |
| Silk | Lowest among tested | N/R | Natural multifilament; excellent handling but provokes tissue reaction. | [5] (In vitro) |
| Albumin-based Suture | 1.3 - 9.6 | 11.5 - 146.6 | Mechanical properties are tunable based on composition and processing. | [19] (In vitro) |
| Native Collagen (7%/15%) | N/A | N/A | Injected gel modulates wound environment, not used for mechanical closure. | [88] (Clinical) |
Table 2: Quantified Scarring and Biocompatibility Outcomes from Preclinical and Clinical Studies
| Intervention / Material | Key Metric | Outcome | Source (Model) |
|---|---|---|---|
| Dexamethasone-coated Polyimide Implant | Immune response & scar tissue | Significant reduction in immune reactions and scar tissue formation over 2 months. | [89] (In vivo, Animal) |
| Native Type I Collagen Gel | Vascular Index (Antera 3D) | Measurable decrease in scar vascularity post-treatment. | [88] (Clinical) |
| Native Type I Collagen Gel | Pigment Index (Antera 3D) | Measurable decrease in scar pigmentation. | [88] (Clinical) |
| Native Type I Collagen Gel | Patient-reported Symptoms | Reduction in tightness, pruritus (itching), and scar stiffness. | [88] (Clinical) |
| SLM-Printed Ti Alloy (with powder) | hBMSC Osteogenic Differentiation | Presence of metal powder on implant surface hindered differentiation. | [90] (In vitro) |
| 3D-Printed Ti Alloy (general) | hBMSC Osteogenic Differentiation | Regular pore structures were more conducive to osteogenic differentiation. | [90] (In vitro) |
Experimental Protocols
Protocol 1: In Vitro Assessment of Cell-Material Interactions for Biocompatibility
This protocol outlines a standardized methodology for evaluating the initial biocompatibility of a novel degradable suture material by assessing cell adhesion, proliferation, and differentiation in direct contact with the material.
1. Objective: To quantify the cytotoxicity and cytocompatibility of a test material using Human Bone Marrow Mesenchymal Stem Cells (hBMSCs) as a model system [90].
2. Materials:
- Test Materials: Sterile samples of the novel degradable suture (e.g., albumin-based filament [19]) and control materials (e.g., VICRYL, Polypropylene [5]).
- Cell Line: Primary human Bone Marrow Mesenchymal Stem Cells (hBMSCs), passage 3-5 [90].
- Culture Reagents: MEM culture medium supplemented with 10% Fetal Bovine Serum (FBS) and 1% antibiotics [90].
- Assay Kits: Cell Counting Kit-8 (CCK-8) for proliferation [90].
- Staining: Alkaline Phosphatase (ALP) kit, Alizarin Red S stain for mineralization, Phalloidin (for actin) and DAPI (for nuclei) for cytoskeleton imaging [90].
- Equipment: Sterile tissue culture plates, SEM preparation equipment, confocal laser scanning microscope.
3. Methodology:
- Step 1: Material Sterilization and Preparation. Sterilize all material samples via ethylene oxide or gamma irradiation. Pre-condition materials in culture medium for 24 hours before cell seeding.
- Step 2: Cell Seeding and Culture. Seed hBMSCs at a density of 1 x 10ⴠcells/mL directly onto the material samples placed in a culture plate. Incubate under standard conditions (37°C, 5% CO₂).
- Step 3: Cell Adhesion Assay (4 hours post-seeding). Wash samples with PBS to remove non-adherent cells. Fix adherent cells with 2.5% glutaraldehyde, dehydrate through a graded ethanol series, and critically point dry. Observe and count adhered cells and their morphology using Scanning Electron Microscopy (SEM) [90].
- Step 4: Cell Proliferation Assay (Days 1, 3, 7). At each time point, transfer samples to a new plate with fresh medium, add CCK-8 solution, and incubate for 2 hours. Measure the absorbance of the supernatant at 450 nm using a microplate reader. Plot the absorbance values over time to generate a proliferation curve [90].
- Step 5: Osteogenic Differentiation Assay (14-21 days). Culture cells in osteogenic induction medium. For early differentiation, perform an ALP activity assay. For late differentiation (mineralization), fix cells and stain with Alizarin Red S to visualize and quantify calcium deposits [90].
4. Data Analysis: Compare absorbance values (proliferation) and staining intensity/area (differentiation) between test and control materials using statistical tests (e.g., one-way ANOVA with post-hoc analysis). SEM images should be qualitatively assessed for cell spreading and healthy morphology.
Protocol 2: Preclinical In Vivo Evaluation of Scarring and Foreign Body Response
This protocol describes the use of an animal model to assess the host tissue response, including scarring and the foreign body reaction, to an implanted degradable material.
1. Objective: To evaluate the rate of degradation, intensity of the foreign body reaction, and quality of tissue remodeling and scarring in a subcutaneous or femoral condyle implantation model [17] [90].
2. Materials:
- Animal Model: New Zealand rabbits or an equivalent rodent model approved by the institutional animal ethics committee [90].
- Test and Control Materials: Sterile degradable suture materials or small implants.
- Equipment: Surgical suite, micro-CT scanner, histology processing equipment.
- Reagents: Anesthetics, analgesics, formalin, paraffin, Hematoxylin and Eosin (H&E) stain, Masson's Trichrome stain, antibodies for immunohistochemistry (e.g., CD68 for macrophages).
3. Methodology:
- Step 1: Implantation Surgery. Anesthetize the animal according to approved protocols. Create a subcutaneous pocket or a critical-sized defect in the femoral condyle. Implant the test and control materials, then close the wound. Administer post-operative analgesics.
- Step 2: In Vivo Monitoring (Time-course). Monitor animals for signs of infection or distress. Use non-invasive imaging like micro-CT at intervals (e.g., 4, 8, 12 weeks) to track implant degradation and new tissue formation in bone defects [90].
- Step 3: Explantation and Histological Processing. Euthanize animals at predetermined endpoints (e.g., 2 weeks for acute response, 2-3 months for chronic response and scarring). Excise the implant with surrounding tissue. Fix in 10% formalin, dehydrate, and embed in paraffin. Section into 5-10 µm thick slices.
- Step 4: Histological Staining and Analysis.
- H&E Staining: For general histoarchitecture, identifying cell types (neutrophils, lymphocytes, macrophages, fibroblasts), and measuring fibrous capsule thickness [89].
- Masson's Trichrome Staining: To specifically visualize collagen deposition (blue/green) and quantify the density and organization of the scar tissue around the implant [90].
- Immunohistochemistry: Use anti-CD68 antibodies to identify and quantify macrophage infiltration and phenotype (M1 pro-inflammatory vs. M2 pro-healing) at the implant-tissue interface.
4. Data Analysis: Quantify fibrous capsule thickness from H&E images using image analysis software (e.g., ImageJ). Score foreign body reaction on a semi-quantitative scale (e.g., 0-4) based on cellular density and composition. Perform collagen morphometry on Masson's Trichrome-stained sections to assess scar tissue maturity and organization.
Protocol 3: Clinical Evaluation of Scarring Outcomes Using 3D Imaging
This protocol details a clinical methodology for objectively assessing the efficacy of a scar modulation therapy, such as an injectable collagen-based material, in human patients.
1. Objective: To quantitatively measure changes in scar characteristics including vascularity, pigmentation, and topography in response to an intervention in a clinical setting [88].
2. Materials:
- Intervention: Test material (e.g., 7% or 15% native type I collagen hydrogel [88]).
- Patients: Consent from patients with post-traumatic or post-surgical wounds or scars.
- Primary Equipment: Antera 3D Camera or equivalent 3D imaging system.
- Secondary Tools: Vancouver Scar Scale (VSS) form, patient questionnaire for symptoms (pruritus, tightness, pain).
3. Methodology:
- Step 1: Baseline Assessment. Prior to treatment, photograph the scar under standardized lighting. Acquire a 3D image using the Antera 3D camera, which automatically calculates baseline indices for Vascularity (redness), Pigmentation (melanin), and Surface Topography (elevation/depression) [88]. Complete the VSS and symptom questionnaire.
- Step 2: Intervention. Intradermally or intralesionally inject the collagen gel along the wound margins or into the scar tissue at intervals of 3-4 weeks, as per study design [88].
- Step 3: Follow-up Assessments. Repeat the 3D imaging, VSS scoring, and symptom questionnaires at each subsequent visit and at a final follow-up (e.g., 3, 6, and 12 months post-treatment).
- Step 4: Data Processing. Use the imaging system's software to automatically match follow-up images to the baseline image and generate comparative data for the three indices.
4. Data Analysis: Statistically analyze the changes in vascular, pigment, and topography indices over time using paired t-tests or repeated measures ANOVA. Correlate the objective 3D data with the subjective VSS scores and patient-reported outcomes to build a comprehensive picture of therapeutic efficacy.
Signaling Pathways and Experimental Workflows
The following diagrams visualize the core biological processes and experimental methodologies described in this document.
Scar Formation Pathway
Biocompatibility Testing Workflow
The Scientist's Toolkit: Key Research Reagents and Materials
This table catalogues essential materials and reagents referenced in the featured protocols, providing researchers with a curated list for experimental design.
Table 3: Essential Research Reagents and Materials for Biocompatibility Studies
| Item Name | Function / Application | Specific Example / Citation |
|---|---|---|
| Human Bone Marrow Mesenchymal Stem Cells (hBMSCs) | In vitro model for assessing cytocompatibility and osteogenic potential of implant materials. | [90] |
| Cell Counting Kit-8 (CCK-8) | Colorimetric assay for non-destructive, quantitative analysis of cell proliferation. | [90] |
| Alizarin Red S Stain | Histochemical dye that binds to calcium deposits, used to quantify late-stage osteogenic differentiation and mineralization. | [90] |
| Alkaline Phosphatase (ALP) Kit | Assay for detecting ALP activity, a key early-stage marker of osteogenic differentiation. | [90] |
| Scanning Electron Microscope (SEM) | High-resolution imaging to visualize cell morphology, adhesion, and spreading on material surfaces. | [19] [90] |
| Masson's Trichrome Stain | Histological stain that differentiates collagen (blue/green) from cytoplasm and nuclei, critical for scarring assessment. | [90] |
| Anti-CD68 Antibody | Immunohistochemical marker for identifying macrophages in tissue sections to evaluate foreign body response. | [89] |
| Antera 3D Camera | Clinical 3D imaging system for objective, quantitative measurement of scar vascularity, pigmentation, and topography. | [88] |
| Native Type I Collagen Hydrogel | A bioactive material used in clinical studies to modulate the wound environment and improve scar outcomes. | 7% or 15% concentration [88] |
In the United States, the Food and Drug Administration (FDA) classifies medical devices based on risk, with surgical sutures designated as Class II devices [60] [91]. This classification means that general controls alone are insufficient to ensure safety and effectiveness, and devices must adhere to Special Controls [91] [92]. For manufacturers of novel degradable suture materials, navigating the premarket notification [510(k)] process requires demonstrating substantial equivalence to a predicate device and compliance with device-specific guidance documents [60] [93]. This document outlines the applicable standards, experimental protocols, and regulatory strategies for developing new biodegradable suture materials, providing a critical framework for researchers and product developers in the field of regenerative medicine.
FDA Regulatory Pathways and Special Controls
Special Controls Guidance for Surgical Sutures
The Class II Special Controls Guidance Document for Surgical Sutures outlines the specific requirements for market approval [60]. This guidance applies to a range of sutures, including absorbable polydioxanone (PDS) sutures (§878.4840), absorbable poly(glycolide/L-lactide) sutures (§878.4493), and absorbable gut sutures (§878.4830), among others [60]. The guidance states that any firm submitting a 510(k) for a surgical suture "will need to address the issues covered in the special control guidance," either by meeting its recommendations or by providing equivalent assurances of safety and effectiveness [60].
The Safety and Performance Based Pathway
To streamline the regulatory process for well-understood devices, the FDA established the Safety and Performance Based Pathway as an optional alternative pathway [93]. Finalized in April 2022, this pathway allows manufacturers to demonstrate substantial equivalence by conforming to FDA-identified performance criteria, rather than through direct comparison to a specific predicate device [93]. This pathway is applicable for both non-absorbable and absorbable sutures intended for the approximation and ligation of soft tissue in orthopedic, cardiovascular, neurological, dental, and ophthalmic applications [93].
Table 1: Scope of FDA's Safety and Performance Based Pathway for Sutures
| Aspect | In Scope | Out of Scope |
|---|---|---|
| General Use | Approximation and ligation of soft tissue [93] | - |
| Medical Specialties | Orthopedic, cardiovascular, neurological, dental, ophthalmic, and others [93] | - |
| Suture Characteristics | Standard materials and designs [93] | Sutures containing atypical or novel materials, animal materials, drug/biologic compounds, or unapproved color additives [93] |
| Design & Sterilization | Conventional designs and approved sterilization methods [93] | Atypical design features and novel sterilization methods [93] |
Performance Criteria and Testing Standards
Sutures marketed via the Safety and Performance Based Pathway must conform to a comprehensive set of performance criteria, which are largely derived from United States Pharmacopeia (USP) monographs and FDA-recognized standards [93].
Table 2: Key Performance Criteria for Surgical Sutures
| Performance Criterion | Standard Reference | Key Requirements & Notes |
|---|---|---|
| Suture Diameter | USP Monographs [93] | Diameter and tolerance specifications. Sutures not meeting USP requirements may still be eligible if the diameter is not oversized by more than 1 USP size [93]. |
| Needle Attachment | USP Monographs [93] | Requirements for needle-to-suture attachment strength. |
| Tensile Strength | USP Monographs [93] | Measures of suture strength and elongation. |
| Sterilization & Shelf Life | FDA-recognized standards [93] | Validation of sterilization methods and shelf-life stability. |
| Resorption Profile | FDA's Surgical Sutures - Class II Special Controls Guidance [93] | For absorbable sutures only: Degradation rate and mass loss profile must be characterized. |
Biocompatibility Considerations
The FDA guidance points to the use of ISO 10993-1 for identifying required biocompatibility testing [93]. A significant concession allows for a rationale in lieu of testing if a device is manufactured from identical raw materials under identical manufacturing practices as a predicate device. The FDA states that "changes in geometry are not expected to impact the biological response," which can be particularly beneficial for suture manufacturers developing line extensions [93].
Experimental Protocols for Novel Degradable Sutures
For researchers developing novel biodegradable suture materials, the following experimental protocols provide a framework for generating the necessary data for a regulatory submission.
Protocol: Tensile Strength and Elongation
Objective: To determine the ultimate tensile strength and elongation at break of the novel suture material, as required by USP monographs and FDA guidance [93].
Materials:
- Universal tensile testing machine
- Standardized grips or fixtures
- Calibrated calipers
- Suture samples of specific USP sizes (e.g., 5-0, 3-0)
Methodology:
- Sample Preparation: Condition all suture samples at (23 ± 2)°C and (50 ± 5)% relative humidity for at least 24 hours prior to testing.
- Diameter Measurement: Measure the diameter of the suture at three points along its length using calibrated calipers. Calculate and record the average diameter.
- Mounting: Mount the suture in the tensile testing machine using grips designed to prevent slippage without damaging the specimen. The gauge length should be 100-150 mm.
- Testing Parameters: Apply a tensile load at a constant crosshead speed of 300 mm/min until failure.
- Data Collection: Record the force-elongation curve. Calculate ultimate tensile strength (force at break divided by cross-sectional area) and percent elongation at break.
Protocol: In Vitro Degradation Profiling
Objective: To characterize the resorption profile of an absorbable suture material by measuring mass loss and strength retention over time in a simulated physiological environment.
Materials:
- Phosphate-buffered saline (PBS), pH 7.4
- Incubator or water bath maintained at (37 ± 1)°C
- Analytical balance (accuracy ± 0.1 mg)
- Universal tensile testing machine
Methodology:
- Sample Preparation: Cut suture samples to a standardized length (e.g., 10 cm). Record initial dry mass (Wâ‚€) and measure initial tensile strength (TSâ‚€) for a representative sample set.
- Immersion: Immerse individual suture samples in containers with PBS (sample volume-to-medium ratio ≥ 1:20). Maintain containers at 37°C.
- Sampling Intervals: Remove samples in triplicate at predetermined time points (e.g., 1, 2, 4, 7, 14, 21, 28 days).
- Mass Loss Analysis: Rinse retrieved samples with deionized water, dry to constant mass, and record dry mass (Wð‘¡). Calculate percent mass remaining: (Wð‘¡/Wâ‚€) × 100%.
- Strength Retention: Test the tensile strength of retrieved samples (TSð‘¡) and calculate percent strength retention: (TSð‘¡/TSâ‚€) × 100%.
The following workflow diagram illustrates the key decision points and testing requirements for regulatory submission of novel suture materials:
Protocol: Cytotoxicity Testing (ISO 10993-5)
Objective: To assess the potential cytotoxic effects of suture extracts using mammalian cell cultures.
Materials:
- L-929 mouse fibroblast cell line
- Cell culture facilities (Class II biological safety cabinet, COâ‚‚ incubator)
- Complete cell culture medium (e.g., DMEM with 10% FBS)
- Extraction media (serum-free DMEM)
- Sterile extraction containers
- Incubator maintained at (37 ± 1)°C
Methodology:
- Sample Preparation: Prepare a 100 cm² sample of the suture material per 1 mL of extraction medium.
- Extraction: Incubate the sample in extraction medium at 37°C for (24 ± 2) hours.
- Cell Seeding: Seed L-929 cells in a 96-well plate at a density that will result in near-confluent monolayers after 24 hours of incubation.
- Exposure: After cell attachment, replace the culture medium with the test extract, negative control (HDPE), and positive control (latex). Incubate for 24 hours.
- Viability Assessment: Assess cell viability using the MTT assay. Measure absorbance at 570 nm. Calculate percentage cell viability relative to the negative control.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Suture Development
| Reagent/Material | Function in Research | Application Example |
|---|---|---|
| Human Serum Albumin (HSA) | Base material for novel biodegradable sutures; provides biocompatibility and tunable degradation [19]. | Development of albumin-based composite sutures via extrusion [19]. |
| Polydioxanone (PDS) | Synthetic, absorbable polymer; benchmark for degradation profile and mechanical properties [60]. | Control material in degradation studies; predicate device comparison [60]. |
| Poly(glycolide/L-lactide) Copolymers | Synthetic, absorbable polymers with tunable degradation rates; well-established in commercial sutures [60]. | Material selection for specific wound healing timelines [60]. |
| Phosphate-Buffered Saline (PBS) | Simulates physiological pH and ion concentration for in vitro degradation studies [19]. | In vitro degradation profiling (mass loss, strength retention) [19]. |
| L-929 Mouse Fibroblast Cell Line | Standardized cell line for cytotoxicity testing per ISO 10993-5 [93]. | Initial biocompatibility screening of novel materials or extracts [93]. |
| Gelatin | Natural polymer additive; enhances cell adhesion and biocompatibility in composite sutures [19]. | Modification of suture surface properties for improved tissue integration [19]. |
Navigating the FDA's regulatory landscape for novel biodegradable sutures requires a systematic approach that integrates material science with regulatory science. The Special Controls Guidance and the more recent Safety and Performance Based Pathway provide clear frameworks for the testing and data required for market clearance [60] [93]. For researchers, early adoption of the performance criteria and experimental protocols outlined in this document can accelerate the translation of innovative suture technologies from the laboratory to clinical practice, ultimately advancing the field of degradable biomaterials for surgical applications.
Conclusion
The field of degradable sutures is evolving beyond simple wound closure to encompass active roles in tissue regeneration and infection prevention. Key takeaways indicate that the ideal suture material does not exist; rather, selection and development must be precisely tailored to the specific biochemical and mechanical environment of the target tissue. Future progress hinges on the continued development of smart biomaterials—such as albumin composites, protein-based sutures, and biodegradable metals—with tunable degradation rates and enhanced biocompatibility. For researchers and drug developers, the convergence of recombinant DNA technology, advanced polymer science, and rigorous mechanical validation presents a significant opportunity to create the next generation of sutures that seamlessly integrate with the body's healing processes, ultimately improving patient outcomes and expanding the possibilities of regenerative medicine.
References
- 1. Nonabsorbable Suture - an overview [https://www.sciencedirect.com/topics/engineering/nonabsorbable-suture]
- 2. Biomechanical Properties and Biocompatibility of a Non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6963933/]
- 3. Key Characteristics of Non-Absorbable Sutures - Medico [https://medicogrp.com/characteristics-of-non-absorbable-sutures-2/]
- 4. Short-Term Hydrolytic Degradation of Mechanical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11432777/]
- 5. Assessment the properties of various surgical sutures [https://www.nature.com/articles/s41598-025-20311-3]
- 6. Increased wound complications in glabrous skin with ... [https://www.sciencedirect.com/science/article/pii/S0020138325003729]
- 7. Preference of Suture Specifications in a Selected ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6635974/]
- 8. Biodegradable Smart Suture Market Outlook 2025-2032 [https://www.intelmarketresearch.com/biodegradable-smart-suture-2025-2032-597-6156]
- 9. Biodegradable Surgical Sutures Market Analysis, Growth ... [https://www.globalinsightservices.com/reports/biodegradable-surgical-sutures-market/]
- 10. Electrospun Medical Sutures for Wound Healing: A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC9105379/]
- 11. Electrospun Medical Sutures for Wound Healing: A Review [https://www.mdpi.com/2073-4360/14/9/1637]
- 12. Suture materials – Recent advances - Cosmoderma [https://cosmoderma.org/suture-materials-recent-advances/]
- 13. Absorbable Suture - an overview [https://www.sciencedirect.com/topics/engineering/absorbable-suture]
- 14. Degradation behaviors of bioabsorbable P3/4HB ... [https://pure.psu.edu/en/publications/degradation-behaviors-of-bioabsorbable-p34hb-monofilament-suture-]
- 15. Poly(4-Hydroxybutyrate): Current State and Perspectives [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2020.00257/full]
- 16. Absorbable Surgical Sutures Market Size & Forecast 2025- ... [https://www.gminsights.com/industry-analysis/absorbable-surgical-sutures-market]
- 17. Biodegradable Medical Implants: Reshaping Future Medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462970/]
- 18. Antibiotic Action, Drug Delivery, Biodegradability, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12028033/]
- 19. Biodegradable suture development-based albumin ... [https://www.nature.com/articles/s41598-024-58194-5]
- 20. Ranking environmental degradation trends of plastic ... [https://www.nature.com/articles/s41467-020-14538-z]
- 21. Biodegradation of synthetic organic pollutants: principles, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12448294/]
- 22. Metabolic reprogramming in efferocytosis [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1677028/full]
- 23. Key Mechanisms in Lysosome Stability, Degradation and Repair [https://pmc.ncbi.nlm.nih.gov/articles/PMC12352500/]
- 24. Biodegradable suture development-based albumin composites for tissue engineering applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10995150/]
- 25. Biodegradable magnesiumâ€based biomaterials: An overview ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8491235/]
- 26. Zinc-nutrient element based alloys for absorbable wound ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961221006578]
- 27. Fixation technique of biodegradable magnesium alloy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10976693/]
- 28. Novel zinc alloys for biodegradable surgical staples - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7031837/]
- 29. Novel Bioactive Glass/Graphene Oxide-Coated Surgical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10286287/]
- 30. Monofilament Suture vs Multifilament [https://medicosutures.com/monofilament-suture-vs-multifilament/]
- 31. Sutures And Needles - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK539891/]
- 32. Lab 4 . Part 5 - Suture materials - VSAC [https://wcvm.usask.ca/vsac205/Lab4/suture-materials.php]
- 33. A basic study on the mechanical properties of synthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159183/]
- 34. Evaluation of Tensile Strength of Surgically Absorbable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11278735/]
- 35. A Surgeon's Guide To Choosing The Right Suture [https://pipelinemedical.com/blog/surgeons-guide-choosing-the-right-suture/]
- 36. Evaluating and Comparing the Tensile Strength and ... [https://www.mdpi.com/2673-4095/5/2/29]
- 37. Tensile Strength Of Sutures-Leading Sutures Manufacturer [https://medicosutures.com/tensile-strength-of-sutures/]
- 38. Comparative Analysis of Tensile Strength in Absorbable Sutures [https://medicogrp.com/absorbable-suture-tensile-strength-comparison-pga-pds/]
- 39. The Effect of Suture Materials on the Development ... [https://pubmed.ncbi.nlm.nih.gov/40674468/]
- 40. Bio-inspired helical-hollow bacterial cellulose fiber for ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894725004693]
- 41. Suture Types & Sizes: USP System, Needle designs, & Use [https://www.theplasticsfella.com/suture-types-sizes/]
- 42. Suture Sizes Guide [https://www.dolphinsutures.com/suture-sizes/]
- 43. Suture Size Chart: Ultimate Guide to Choosing the Right ... [https://suturekit.com/blogs/news/suture-size-chart-guide]
- 44. Suture Materials [https://coreem.net/core/suture-materials/]
- 45. Suture Sizes from Smallest to Largest [https://medicosutures.com/suture-sizes-from-smallest-to-largest/]
- 46. Understanding Suture Materials [https://www.aaha.org/trends-magazine/october-2022/gs-sutures/]
- 47. The Efficacy of Antimicrobial-Coated Sutures for Preventing ... [https://www.sciencedirect.com/science/article/abs/pii/S1091255X23022862]
- 48. Suture Materials: Conventional and Stimulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467860/]
- 49. Ushering in a new era of suture-free tissue reconstruction ... [https://news.mit.edu/2025/ushering-new-era-suture-free-tissue-reconstruction-better-healing-0801]
- 50. sciencedirect.com/topics/nursing-and-health-professions/ recombinant ... [https://www.sciencedirect.com/topics/nursing-and-health-professions/recombinant-dna-technology]
- 51. – Steps, Recombinant & Examples | evitria DNA technology Methods [https://www.evitria.com/journal/recombinant-antibodies/recombinant-dna-technology/]
- 52. , Recombinant Of DNA ... Technology Methods Recombinant DNA [https://www.pw.live/neet-pg/exams/recombinant-dna-technology]
- 53. How Biodegradable Surgical Sutures Works [https://www.linkedin.com/pulse/how-biodegradable-surgical-sutures-works-one-simple-6pv9c/]
- 54. ISO 10993-1:2025 Publication Is Imminent [https://veranex.com/blog/iso-10993-1-2025-implications-med-device-innovators-manufacturers]
- 55. ISO 10993-1:2025 Updates —Top 10 Biological Evaluation ... [https://namsa.com/resources/blog/iso-10993-12025top-10-biological-evaluation-essentials-in-the-update/]
- 56. ISO 10993-1:2025 Revision Highlights Part 1 [https://medinstitute.com/blog/iso-10993-12025-revision-highlights-part-1-reasonably-foreseeable-misuse/]
- 57. Short-Term Hydrolytic Degradation of Mechanical ... [https://www.mdpi.com/2079-4983/15/9/273]
- 58. The Degradation of Absorbable Surgical Threads in Body ... [https://www.mdpi.com/1422-0067/25/20/11333]
- 59. Biodegradable Surgical Sutures Market Insights and ... [https://www.linkedin.com/pulse/biodegradable-surgical-sutures-market-insights-forecast-ecrmc/]
- 60. Surgical Sutures Class II Special Controls Guidance [https://www.fda.gov/medical-devices/guidance-documents-medical-devices-and-radiation-emitting-products/surgical-sutures-class-ii-special-controls-guidance-document-industry-and-fda-staff]
- 61. What Color Are Dissolvable Sutures [https://medicosutures.com/what-color-are-dissolvable-sutures/]
- 62. Understanding the Importance of Color Coding in Sutures [https://medicogrp.com/color-coding-of-sutures/]
- 63. Understanding the Color Coding of Absorbable Sutures and ... [https://medicogrp.com/absorbable-sutures-color/]
- 64. Suture Materials - Classification - Surgical Needles [https://teachmesurgery.com/skills/surgical-equipment/suture-materials/]
- 65. Suture Material - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/suture-material]
- 66. Recent advances in PLGA-based resorbable implants for ... [https://www.sciencedirect.com/science/article/abs/pii/S2352492825026285]
- 67. Drug Delivery Systems and Materials for Wound Healing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6003879/]
- 68. Two-month longitudinal study of mechanical properties of absorbable... [https://josr-online.biomedcentral.com/articles/10.1186/s13018-016-0451-5]
- 69. Modern Approaches in Wounds Management [https://www.mdpi.com/2073-4360/15/17/3648]
- 70. Estimating Kinetic Rate Parameters for Enzymatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8290342/]
- 71. Degradation Kinetics, Mechanisms, and Antioxidant Activity ... [https://www.mdpi.com/2311-5629/11/1/5]
- 72. Advances, challenges, and prospects for surgical suture ... [https://www.sciencedirect.com/science/article/abs/pii/S174270612300435X]
- 73. Surgical suture [https://en.wikipedia.org/wiki/Surgical_suture]
- 74. Suture Hypersensitivity - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK562288/]
- 75. A Mysterious Pacemaker Suture: An Uncommon Foreign ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3065747/]
- 76. An In Vitro Tensile Strength Study [https://pubmed.ncbi.nlm.nih.gov/39221394/]
- 77. Evaluation of tensile strength of surgical synthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3701834/]
- 78. Biomechanical comparison of suture and screw fixation in ... [https://www.nature.com/articles/s41598-025-20106-6]
- 79. In vitro-in vivo correlation (IVIVC) development for long- ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365924007661]
- 80. sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical... [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/degradation-in-vitro]
- 81. (PDF) Strength behavior of oriented PLLA, 96L/4D PLA, and... retention [https://www.academia.edu/98684761/Strength_retention_behavior_of_oriented_PLLA_96L_4D_PLA_and_80L_20D_L_PLA]
- 82. In Vivo Degradation and Local Tissue Response of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359101/]
- 83. and in vivo In studies of a dual medical-grade... vitro degradation [https://pubs.rsc.org/en/content/articlelanding/2025/bm/d4bm01132e/unauth]
- 84. Effect of a plasmaelectrolytic coating on the strength of in... retention [https://pubmed.ncbi.nlm.nih.gov/22963846/]
- 85. Monocryl suture, a new ultra-pliable absorbable ... [https://pubmed.ncbi.nlm.nih.gov/8562789/]
- 86. Monocryl - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/monocryl]
- 87. The influence of suture materials on the biomechanical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7453549/]
- 88. Native Collagen for Surgical Wound and Scar Prevention— ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524737/]
- 89. Novel method to improve the biocompatibility and chronic ... [https://www.news-medical.net/news/20250630/Novel-method-to-improve-the-biocompatibility-and-chronic-stability-of-neural-electrode-implants.aspx]
- 90. Efficacy of bone defect therapy involving various surface ... [https://www.nature.com/articles/s41598-023-47495-w]
- 91. Regulatory Controls [https://www.fda.gov/medical-devices/overview-device-regulation/regulatory-controls]
- 92. General Controls for Medical Devices [https://www.fda.gov/medical-devices/regulatory-controls/general-controls-medical-devices]
- 93. FDA Announces Optional Pathway for Clearance of ... [https://namsa.com/resources/blog/fda-announces-optional-pathway-surgical-sutures-clearance/]