A Comprehensive Protocol for Validating Spinal Implant Computational Models: From Theory to Clinical Translation
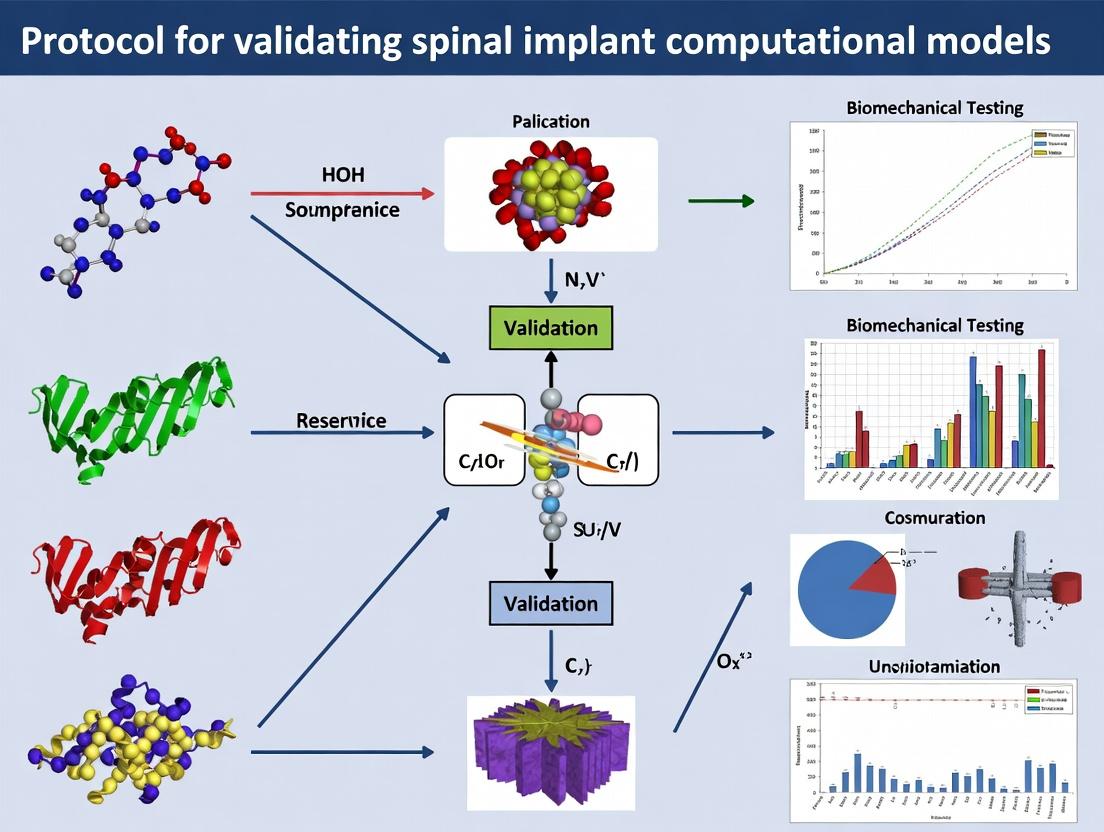
This article presents a detailed, step-by-step protocol for the rigorous validation of computational models used in spinal implant design and evaluation.
A Comprehensive Protocol for Validating Spinal Implant Computational Models: From Theory to Clinical Translation
Abstract
This article presents a detailed, step-by-step protocol for the rigorous validation of computational models used in spinal implant design and evaluation. Aimed at researchers and biomedical engineers, the content explores the foundational principles of biomechanical modeling, outlines methodological best practices for finite element analysis (FEA) and multi-body dynamics, provides solutions for common troubleshooting and optimization challenges, and establishes a robust framework for quantitative validation against experimental and clinical data. The protocol emphasizes standards like ASTM F2077 and ASME V&V 40 to ensure model credibility, ultimately bridging the gap between computational simulation and safe, effective implant development.
The Bedrock of Credibility: Core Principles and Standards for Spinal Implant Modeling
Defining Model Validation and Verification (V&V) in a Regulatory Context
In the context of regulatory submissions for spinal implants, computational model credibility is paramount. Validation and Verification (V&V) form the systematic process for assessing a model's accuracy and its predictive capability for the intended use. Regulatory bodies like the U.S. FDA and EU MDR require rigorous V&V as part of the computational modeling evidence for device safety and effectiveness.
Table 1: Key Regulatory Guidance Documents for Computational Model V&V
| Agency/Guideline | Document Title/Reference | Core V&V Principle Emphasized | Applicability to Spinal Implants |
|---|---|---|---|
| FDA | Reporting of Computational Modeling Studies in Medical Device Submissions | Credibility of computational models through V&V plans, evidence, and reports. | Directly applicable; recommends ASME V&V 40 framework. |
| ASME | V&V 40-2018: Assessing Credibility of Computational Modeling through Verification and Validation | Risk-informed credibility assessment framework (Credibility Factors). | Foundational framework referenced by regulators. |
| ISO | ISO/ASTM 52900:2021 Additive manufacturing — General principles | V&V for models used in design/ manufacturing (e.g., patient-specific implants). | Relevant for additively manufactured spinal devices. |
| EMA | Qualification of Novel Methodologies for Medicine Development | Defines "fit-for-purpose" model validation within a specific context of use. | Relevant for combination products (e.g., drug-eluting implants). |
Core Definitions in a Regulatory Context
- Verification: The process of ensuring that the computational model is implemented correctly and solves the underlying equations accurately. It answers: "Did we build the model right?"
- Validation: The process of determining the degree to which a model is an accurate representation of the real world from the perspective of the model's intended uses. It answers: "Did we build the right model?"
- Context of Use (COU): A definitive statement that fully and clearly describes the way the model will be used and the decisions it will inform. This is the critical first step defining the required level of credibility.
The ASME V&V 40 Risk-Informed Credibility Framework
The ASME V&V 40 framework is the industry standard for regulatory submissions. It ties the required level of V&V effort (Credibility) to the Risk of the Decision Informed by the Model.
Table 2: Relationship Between Model Risk and Required Credibility Evidence
| Model Risk Category (Per V&V 40) | Description | Example in Spinal Implant Research | Required Credibility Level |
|---|---|---|---|
| High | Model outcome directly impacts device safety/ efficacy decision; low prior knowledge. | Predicting novel implant's fatigue life in worst-case anatomical loading. | Very High. Extensive, multi-faceted V&V required. |
| Medium | Model informs design or supplements physical test data; some prior knowledge exists. | Comparing relative motion (stability) between two established implant designs. | Medium to High. Targeted V&V on key outputs. |
| Low | Model used for exploratory research or screening; not used for direct claims. | Preliminary scoping study of stress distribution in a vertebral body. | Low. Basic verification and rationale suffice. |
Credibility is built by accumulating evidence across six Credibility Factors: 1. Code Verification, 2. Solution Verification, 3. Conceptual Model Assessment, 4. Input Uncertainty Quantification, 5. Model Validation, 6. Results Uncertainty Quantification.
Title: The ASME V&V 40 Risk-Informed Credibility Process
Detailed V&V Application Notes & Protocols for Spinal Implant Models
Application Note 1: Verification Protocol for a Spinal Fusion Finite Element Model
- Context of Use: Predict segmental range of motion (ROM) and bone-implant interface stresses under physiological loading.
- Verification Activities:
- Code Verification: Use commercial FEA software (e.g., Abaqus, ANSYS) with prior qualification evidence. Document solver version and patch level.
- Solution Verification (Numerical Accuracy):
- Perform mesh convergence study on key outputs (ROM at treated level, peak von Mises stress in implant).
- Protocol: Refine global mesh size sequentially by factor of √2. Model is considered converged when change in key outputs is <5%.
Table 3: Example Mesh Convergence Study Data (L4-L5 Model)
| Mesh Size (mm) | No. of Elements | L4-L5 Flexion ROM (degrees) | % Change from Previous | Peak Implant Stress (MPa) | % Change from Previous |
|---|---|---|---|---|---|
| 2.0 | 45,200 | 3.85 | - | 142.5 | - |
| 1.4 | 92,500 | 4.12 | 7.0% | 155.8 | 9.3% |
| 1.0 | 181,300 | 4.28 | 3.9% | 162.1 | 4.0% |
| 0.7 | 350,000 | 4.31 | 0.7% | 163.5 | 0.9% |
| 0.5 | 680,000 | 4.32 | 0.2% | 164.0 | 0.3% |
Application Note 2: Validation Protocol Against Bench Test Data
- Context of Use: Predict fatigue performance of a pedicle screw construct.
- Validation Experiment: Correlate model-predicted strain/stress with physical strain gauge measurements on a polyurethane foam block (ASTM F1839) or cadaveric vertebra.
- Detailed Protocol:
- Bench Test Setup: Perform axial cyclic loading (e.g., 100-1000N, 5Hz) on a screw implanted in validated foam block. Attatch strain gauges at screw neck and shaft.
- Computational Model: Replicate exact test geometry, boundary conditions, and material properties (foam density matched to test certificate).
- Comparison Metric: Compare strain amplitude and pattern at identical gauge locations.
- Acceptance Criterion: Predicted vs. experimental strain hysteresis loops shall have a correlation coefficient (R²) > 0.85, and mean strain error < 15%.
Title: Model Validation Workflow Against Bench Test Data
The Scientist's Toolkit: Research Reagent Solutions for V&V
Table 4: Essential Materials & Tools for Spinal Implant Model V&V
| Item/Category | Example Product/Specification | Function in V&V Process |
|---|---|---|
| Standardized Test Substrate | Sawbones Polyurethane Foam Blocks (ASTM F1839, densities: 0.16g/cc, 0.32g/cc) | Provides consistent, repeatable mechanical properties for validation bench testing against computational models. |
| Cadaveric Tissue | Fresh-frozen human spinal segments (L1-L5) with documented bone mineral density. | Gold-standard biological substrate for highest-fidelity validation of models predicting bone-screw interaction or implant kinematics. |
| Digital Reference Data | Public corpus of spine CT/MRI datasets (e.g., Visible Human Project, SpineWeb). | Serves as anatomical input for developing and testing image segmentation and model generation pipelines (Conceptual Model Assessment). |
| Calibrated Sensors | Micro-strain gauges (e.g., FLA-2-11, Tokyo Sokki Kenkyujo); 6-DOF load cells. | Provides ground-truth mechanical data (strain, force, moment) from physical tests for quantitative model validation. |
| Software Verification Suite | NAFEMS FEA Benchmark Problems (e.g., LE10, LE11). | Standardized problems with known analytical solutions to verify correct implementation of element formulations and material models. |
| Uncertainty Quantification Tool | Dakota (SNL), or proprietary Monte Carlo modules in FEA packages. | Propagates input uncertainties (e.g., bone material properties, loading direction) to quantify uncertainty in model outputs. |
This document provides detailed application notes and protocols for biomechanical testing of the spine, framed within the context of validating computational models for spinal implants. The validation of finite element (FE) and multi-body dynamics models requires rigorous experimental benchmarking against controlled in vitro tests that quantify the spine's response to fundamental loads and motions, up to and including structural failure. These protocols are essential for researchers and engineers developing and certifying new spinal implant systems.
Quantification of Spinal Loads and Motions
Understanding the in vivo loading environment is critical for designing physiologically relevant computational models and experimental validation tests.
Table 1: RepresentativeIn VivoLoads on the Lumbar Spine
| Activity / Condition | Approximate Load (L4-L5) | Measurement Method | Key Reference |
|---|---|---|---|
| Standing at ease | 500 N | Telemeterized Implant | Rohlmann et al., 2013 |
| Walking | 650 - 850 N | Telemeterized Implant | Fagan et al., 2002 |
| Flexion (20°) | 1100 - 1200 N | Telemeterized Implant | Rohlmann et al., 2001 |
| Lifting 20kg (bent knees) | 1900 - 2400 N | Intra-Discal Pressure + Modeling | Wilke et al., 1999 |
| Sitting unsupported | 700 - 900 N | Intra-Discal Pressure | Sato et al., 1999 |
| Coughing / Sneezing | ~1000 N | Telemeterized Implant | Rohlmann et al., 2009 |
Protocol 1.1:In VitroRange of Motion (ROM) Testing
Purpose: To quantify the flexibility (angular motion per applied moment) of a spinal segment (FSU) in primary anatomical planes. This data is the primary benchmark for validating the kinematic response of computational models.
Materials (Research Reagent Solutions):
- Fresh-Frozen Human Spinal Segments (FSUs): Cadaveric functional spinal units (e.g., L2-L3). Primary biological substrate.
- Polymethyl Methacrylate (PMMA): For potting vertebral ends to ensure rigid fixation in testing fixtures.
- 6-Degree-of-Freedom Spinal Testing Machine: Electromechanical or servo-hydraulic system capable of applying pure moments.
- Optical Motion Capture System (IR cameras & markers): For high-fidelity, non-contact measurement of 3D vertebral kinematics.
- Environmental Chamber/Humidifier: To maintain tissue hydration with 0.9% saline spray during testing.
- Calibrated Moment-Angle Data Acquisition Software: Custom or commercial (e.g., LabVIEW) for real-time data collection.
Methodology:
- Specimen Preparation: Thaw FSU at 4°C. Carefully dissect paravertebral musculature while preserving ligaments, joints, and discs. Pot cranial and caudal vertebrae in PMMA blocks, ensuring the disc is oriented horizontally.
- Fixture & Instrumentation: Mount potted specimen in testing machine. Attach reflective marker triads rigidly to each vertebral body (not the potting blocks).
- Preconditioning: Apply 3-5 cycles of a low-magnitude pure moment (e.g., ±3 Nm) in flexion-extension, lateral bending, and axial rotation to establish a repeatable neutral zone.
- Load-Controlled Flexibility Test: Apply a pure moment in one primary plane (e.g., flexion-extension) at a slow rate (e.g., 1°/s or 0.1 Nm/s) to a target maximum (typically ±7.5 Nm or ±10 Nm). Hold at peak moment for a 10-second creep period. Record applied moment and the resulting angular displacement from the motion capture system throughout the cycle.
- Data Analysis: Plot moment vs. angle (hysteresis curve). Calculate neutral zone (NZ), range of motion (ROM), and stiffness (slope of the linear region) for the loading phase. Repeat steps 4-5 for lateral bending and axial rotation.
- Model Validation Benchmark: The experimental ROM at ±7.5 Nm serves as the direct validation target for the computational model under identical boundary conditions and loading.
In Vitro Flexibility Testing Workflow
Failure Modes and Injury Mechanisms
Validating a model's prediction of failure (e.g., vertebral fracture, ligament rupture) requires experimental protocols that induce and quantify damage.
Table 2: Common Spinal Failure Modes Under Specific Loading
| Failure Mode | Typical Loading Condition | Associated Injury / Pathology | Critical Biomechanical Parameter |
|---|---|---|---|
| Vertebral Body Fracture | Compression / Flexion | Osteoporotic Fracture, Burst Fracture | Ultimate Load (kN), Yield Stress (MPa) |
| Annular Tear / Disc Herniation | Complex Flexion-Compression-Torsion | Disc Prolapse, Radiculopathy | Intradiscal Pressure, Annulus Strain |
| Ligamentous Failure (e.g., PLL, SSL) | Hyperflexion / Hyperextension | Whiplash, Distraction Injury | Ligament Strain at Failure (%) |
| Facet Joint Fracture / Subluxation | Compression-Shear / Torsion | Spondylolisthesis, Facet Arthritis | Joint Contact Force (N) |
| Endplate Fracture | Rapid Compression | Schmorl's Nodes, Disc Degeneration | Endplate Strength (MPa) |
Protocol 2.1: Compressive Failure Testing of Vertebral Bodies
Purpose: To determine the ultimate compressive strength and failure mechanism of a vertebral body. This data validates the failure criteria of material models in FE analyses.
Materials:
- Isolated Vertebral Body: Prepared from a spinal segment.
- Bi-axial Materials Testing System: High-capacity load frame with a rigid, flat platen.
- Saline Spray System: For hydration.
- Digital Image Correlation (DIC) System: Two-camera setup with speckle pattern for full-field strain measurement.
- Acoustic Emission Sensors (Optional): To detect microfracture events.
Methodology:
- Specimen Preparation: Isolate the vertebral body by removing posterior elements and adjacent discs. Parallelize the superior and inferior endplates using a milling machine. Apply a fine speckle pattern on one lateral surface for DIC.
- Mounting: Place the vertebra between two rigid, flat platens. Ensure centric axial alignment.
- Testing: Apply a displacement-controlled axial compression at a slow rate (e.g., 1 mm/min) until a clear drop in load (>20% of peak) is observed, indicating structural failure. Continuously record load, displacement, DIC images, and acoustic emission.
- Post-Test Analysis: Calculate ultimate compressive strength (peak load / cross-sectional area). Use DIC to map strain localization leading to fracture. Correlate acoustic events with load steps. Visually classify fracture type (wedge, burst, etc.).
- Model Validation: The experimental load-displacement curve to failure and the observed fracture pattern are compared to the FE model prediction under identical conditions.
Pathways to Vertebral Body Failure Under Compression
Protocol for Implant-Spine Construct Validation
This integrated protocol combines principles from Sections 1 & 2 to validate a model of an instrumented spine.
Protocol 3.1: Hybrid Experimental-Computational Validation of a Spinal Fixation Construct
Purpose: To generate a comprehensive dataset for validating a computational model of a lumbar segment stabilized with pedicle screw-based instrumentation.
Materials:
- Instrumented Lumbar Specimen (e.g., L1-L3): With a destabilized L2-L3 segment (e.g., dissected disc, ligaments) and posterior fixation at L2-L3.
- Spinal Testing Machine & Motion Capture: As in Protocol 1.1.
- Strain Gauges: Miniature gauges applied to implant rods.
- Pressure-Sensitive Film or Tactile Sensor: For facet joint contact pressure measurement (optional).
Methodology:
- Native State Testing: Perform flexibility test (Protocol 1.1) on the intact L1-L3 specimen to establish baseline ROM.
- Destabilization: Create a standard injury model (e.g., complete discectomy, partial facetectomy) at L2-L3.
- Instrumentation: Implant the pedicle screw-rod system at L2-L3 according to surgical guidelines. Apply strain gauges to the rods.
- Instrumented State Testing: Repeat the flexibility test on the instrumented construct. Record simultaneously: a) segmental ROM (L2-L3), b) rod strain, c) adjacent segment ROM (L1-L2).
- Validation Data Generation: Create a table comparing experimental results (Intact vs. Instrumented) for ROM and rod strain. This forms the multi-modal validation dataset.
- Computational Model Calibration/Validation: The FE model of the intact spine is first calibrated to match the native state ROM. The model of the instrumented construct is then validated against the instrumented state data for ROM, rod strain (stress), and load-sharing characteristics.
Table 3: Key Research Reagent Solutions for Spinal Biomechanics
| Item / Solution | Function in Experiment | Key Consideration for Validation |
|---|---|---|
| Fresh-Frozen Cadaveric Spine | Gold-standard biological substrate for in vitro testing. | Segment (age, BMD), handling (freeze-thaw cycles) critically affect mechanical properties and must be documented for model input. |
| Polyurethane Foam Spines | Repeatable, isotropic synthetic models for feasibility studies. | Material properties are simplified and non-physiological; useful for initial implant fit/range checks, not final validation. |
| 6-DOF Spinal Simulator | Applies pure moments or follower loads to simulate in vivo motion. | Machine compliance and control algorithm (load vs. displacement) must be understood and replicated in the model's boundary conditions. |
| Optical Motion Capture (IR) | Provides high-accuracy 3D kinematics without contact artifacts. | Marker placement relative to vertebral bone (vs. potting block) is crucial; must be digitally replicated in the model. |
| Digital Image Correlation (DIC) | Measures full-field surface strains on bone, implants, or disc. | Provides rich spatial data for validating strain fields predicted by the FE model, moving beyond single-point comparisons. |
| Telemeterized Implant Data | In vivo force measurements from instrumented patients. | The ultimate validation target for load-prediction models, though rare and patient-specific. |
This document provides detailed application notes and experimental protocols for three core computational techniques—Finite Element Analysis (FEA), Multi-body Dynamics (MBD), and Computational Fluid Dynamics (CFD). The content is framed within the overarching research thesis: "Protocol for Validating Spinal Implant Computational Models." The objective is to establish rigorous, standardized methodologies for generating and validating computational models that predict the biomechanical performance, durability, and interaction of spinal implants with human physiology. These validated models are critical for researchers, scientists, and drug development professionals aiming to accelerate the design and regulatory evaluation of novel spinal implants and biologics.
Finite Element Analysis (FEA) for Spinal Implants
Application Notes
FEA is a numerical method for simulating the mechanical response of a structure to loads. In spinal implant research, it is used to predict stress distributions in implants and adjacent bone, assess risk of subsidence or fracture, and evaluate stability under physiological loading.
Key Applications:
- Stress-Shielding Analysis: Quantifying bone resorption due to altered load transfer.
- Fatigue Life Prediction: Estimating implant durability under cyclic loading.
- Patient-Specific Modeling: Using CT data to create subject-specific models for pre-surgical planning.
Protocol: FEA of a Lumbar Cage for Subsidence Risk
Objective: To validate an FEA model predicting the risk of vertebral body subsidence under static compression.
Materials & Software:
- µCT scan data of lumbar vertebral body (L3).
- CAD model of a PEEK interbody cage.
- FEA Software (e.g., ANSYS, Abaqus).
- Material property assignment tables from literature.
Methodology:
- Geometry Reconstruction:
- Segment the L3 vertebral body from µCT data using thresholding.
- Generate a 3D surface model, preserving cortical shell and trabecular architecture.
- Import and position the cage CAD model within the intervertebral space.
- Meshing:
- Mesh the cortical bone with 0.5 mm tetrahedral elements.
- Mesh the trabecular bone with 1.0 mm tetrahedral elements.
- Mesh the implant with 0.3 mm hexahedral elements.
- Perform a mesh convergence study.
- Material Properties & Boundary Conditions:
- Assign linear elastic, isotropic properties (See Table 1).
- Define a frictionless contact interface between cage and bone.
- Fix the inferior surface of the vertebral body in all degrees of freedom.
- Apply a 2000 N compressive load distributed on the superior surface.
- Solution & Validation:
- Run a static structural analysis.
- Validate by comparing predicted strain in the vertebral body against in vitro digital image correlation (DIC) data from a corresponding physical test.
- Calibrate the model by adjusting trabecular bone modulus if error >15%.
Table 1: Typical Material Properties for Lumbar FEA
| Material | Young's Modulus (MPa) | Poisson's Ratio | Source |
|---|---|---|---|
| Cortical Bone | 12,000 | 0.30 | Literature (Rho et al., 1993) |
| Trabecular Bone | 100 - 900 (Region-dependent) | 0.20 | Patient CT-derived (Bone Density) |
| PEEK Implant | 3,500 | 0.36 | Manufacturer Datasheet |
| Titanium Alloy (Ti-6Al-4V) | 110,000 | 0.33 | ASTM F136 |
Multi-body Dynamics (MBD) for Spinal Segment Kinematics
Application Notes
MBD simulates the motion of interconnected rigid or flexible bodies under force. It is used to analyze the kinematic and kinetic behavior of the spine as a system, evaluating range of motion, facet joint forces, and ligament tensions before and after implantation.
Key Applications:
- Implant Kinematic Performance: Assessing dynamic stability and constraint provided by pedicle screw systems or artificial discs.
- Wear Simulation: Predicting bearing surface wear in mobile-core implants.
- Whole-Spine Dynamics: Studying compensation mechanisms in adjacent segments.
Protocol: MBD Simulation of a Spinal Motion Segment with a Dynamic Stabilization Device
Objective: To validate an MBD model predicting L4-L5 range of motion (ROM) and facet contact forces after implantation of a posterior dynamic stabilization device.
Materials & Software:
- Geometrically accurate MBD model of L4-L5 vertebrae (from public database or reconstructed).
- CAD of the dynamic stabilization device (rods, screws, spacers).
- MBD Software (e.g., ADAMS LifeMOD, AnyBody).
- Kinematic input data from in vitro flexibility tests.
Methodology:
- Model Assembly:
- Define L4 and L5 as rigid bodies. Incorporate intervertebral disc as a 6-DOF nonlinear bushing element.
- Model major ligaments (ALL, PLL, LF, CL, ISL) as nonlinear tension-only spring elements.
- Model facet articulations as 3D contact elements.
- Assemble the implant model, defining joints between screws/vertebrae and compliant elements for the dynamic rod.
- Kinematic Driving & Loading:
- Apply pure moments (7.5 Nm) in flexion-extension, lateral bending, and axial rotation to the superior vertebra (L4) using a kinematic driver.
- Constrain the inferior vertebra (L5) in space.
- Apply a 500 N follower preload to simulate musculature.
- Simulation & Validation:
- Run dynamic simulation for each loading mode.
- Output L4-L5 angular ROM and L4-L5 facet joint contact forces.
- Validate by comparing simulation outputs to data from a matched in vitro experiment using a spinal testing machine and load-sensing facets. Correlation should be R² > 0.85.
Table 2: Key Ligament Properties for MBD (Wiltse et al.)
| Ligament | Stiffness (N/mm) | Pre-strain (%) | Cross-Sectional Area (mm²) |
|---|---|---|---|
| Anterior Longitudinal (ALL) | 30.0 | 0.0 | 40.2 |
| Posterior Longitudinal (PLL) | 50.0 | 0.0 | 13.1 |
| Ligamentum Flavum (LF) | 40.0 | 15.0 | 62.1 |
| Capsular Ligament (CL) | 35.0 | 0.0 | 60.1 |
| Interspinous (ISL) | 15.0 | 0.0 | 40.0 |
Computational Fluid Dynamics (CFD) for Biologics Transport
Application Notes
CFD analyzes fluid flow, heat transfer, and associated phenomena. In spinal research, it models the flow of blood, cerebrospinal fluid (CSF), or the diffusion of therapeutic agents (e.g., drugs, osteoinductive factors) within the spinal canal or implant-bone interface.
Key Applications:
- Drug Elution from Implants: Optimizing porous coating designs for controlled release of osteogenic drugs.
- CSF Flow Dynamics: Investigating shear stress on the spinal cord or drug dispersion in intrathecal delivery.
- Bone Ingrowth Simulation: Modeling interstitial fluid flow and nutrient transport in porous spinal implants.
Protocol: CFD of Osteogenic Drug Elution from a Porous Titanium Cage
Objective: To validate a CFD model predicting the concentration profile of a bone morphogenetic protein (BMP-2) analog eluting from a porous cage into the adjacent vertebral body.
Materials & Software:
- 3D CAD model of the porous cage and simplified bone region.
- CFD Software (e.g., STAR-CCM+, Fluent).
- Physicochemical properties of the carrier (e.g., collagen sponge) and drug.
Methodology:
- Geometry & Meshing:
- Create a fluid domain representing the porous carrier within the implant and the interconnected pore space of the adjacent trabecular bone.
- Generate a polyhedral volume mesh with prism layers at walls. Ensure mesh quality (skewness < 0.8).
- Physics & Boundary Conditions:
- Model the fluid (interstitial fluid) as incompressible and Newtonian.
- Model the porous carrier region using Darcy's Law with defined permeability.
- Define the drug as a dilute species. Set initial concentration in the carrier to 1.5 mg/mL.
- Set bone boundaries as no-slip walls. Set outer boundaries as zero-concentration outlets.
- Apply species diffusion coefficient (1e-10 m²/s) and carrier porosity (0.85).
- Solution & Validation:
- Run a transient simulation for 14 days.
- Output concentration contours and temporal release profile.
- Validate by comparing the simulated release curve (cumulative release vs. time) against data from an in vitro elution test (HPLC measurement) in a simulated body fluid bath. Normalized RMS error should be < 20%.
Table 3: Key Parameters for Drug Elution CFD
| Parameter | Value | Unit | Description |
|---|---|---|---|
| Fluid Density (ρ) | 1000 | kg/m³ | Assumed water-like |
| Fluid Viscosity (μ) | 0.001 | Pa·s | Assumed water-like |
| Carrier Permeability (κ) | 1.0e-12 | m² | From literature (collagen sponge) |
| Drug Diffusion Coefficient (D) | 1.0e-10 | m²/s | For BMP-2 in aqueous solution |
| Initial Drug Concentration | 1.5 | mg/mL | Typical clinical loading |
The Scientist's Toolkit: Research Reagent Solutions & Essential Materials
| Item | Function in Computational Model Validation |
|---|---|
| Polyurethane Foam Sawbones | Represents standardized bone material for in vitro bench tests. Used to validate FEA models of implant-bone interface mechanics under controlled, repeatable conditions. |
| Fresh-Frozen Human Cadaveric Spine Segments | Provides biologically accurate anatomy and material properties. The gold standard for in vitro validation of MBD and FEA models regarding kinematics, kinetics, and failure modes. |
| Digital Image Correlation (DIC) System | Non-contact optical method to measure full-field strain on bone or implant surfaces during mechanical testing. Critical for validating FEA-predicted strain fields. |
| Six-Degree-of-Freedom Spinal Testing Machine | Applies pure moments and follower loads to spine specimens. Generates kinematic and load data required to drive and validate MBD simulations. |
| Simulated Body Fluid (SBF) | Ion concentration similar to human blood plasma. Used in in vitro elution or corrosion studies to provide a biologically relevant fluid environment for CFD model validation. |
| High-Performance Computing (HPC) Cluster | Essential for solving high-fidelity, patient-specific FEA and CFD models with millions of elements and complex nonlinearities in a reasonable timeframe. |
| Bone Cement (PMMA) | Used to pot specimens for mechanical testing and to simulate osteolytic defects in validation models for implant stability. |
Visualization: Computational Validation Protocol Workflow
Diagram 1: Core Validation Workflow for Spinal Implant Models
Diagram 2: Computational Techniques Map for Spinal Implant Research
Within the research framework for a Protocol for Validating Spinal Implant Computational Models, understanding the regulatory and standardization landscape is paramount. This document provides Application Notes and detailed experimental Protocols based on three cornerstone guidance documents: ASTM, ISO, and ASME V&V 40. These standards provide the structured methodology required to establish credibility in computational model predictions used for evaluating spinal implant safety and performance.
The table below summarizes the key focus, scope, and quantitative requirements of each standard relevant to computational model validation.
Table 1: Comparative Overview of Key Standards for Computational Model Validation
| Standard / Guideline | Primary Focus & Scope | Key Quantitative Metrics / Tiers | Direct Application to Spinal Implant Models |
|---|---|---|---|
| ASME V&V 40-2018Assessing Credibility of Computational Modeling | Risk-informed credibility assessment framework. Defines Model Risk and Decision Risk. | Credibility Factors:1. Verification (Code, Calculation)2. Validation (Experimental)3. Application Inputs4. Results UncertaintyCredibility Scale: Low / Medium / High based on Decision Consequence. | Core framework for defining the required level of validation evidence based on the clinical risk of the spinal implant simulation (e.g., range of motion vs. fatigue fracture). |
| ASTM F3163-21Guide for Verification of Computational Solid Mechanics Models | Specific guidance for verification of finite element analysis (FEA) models. | Verification Activities:1. Code Verification (e.g., order of accuracy, P ≥ 2.0)2. Calculation Verification (Grid Convergence Index, GCI < 5-10% recommended). | Essential for ensuring the spinal implant FEA model is solving equations correctly and numerical errors are quantified. |
| ISO 19208:2017Framework for Verification, Validation of Computational Solid Mechanics Models | High-level framework aligning V&V activities with intended use. | Defines stages: Planning, Verification, Validation, Uncertainty Quantification. Recommends reporting of validation metrics (e.g., correlation metrics). | Provides the overarching process flow for the validation protocol, ensuring traceability from intended use to validation conclusion. |
Application Notes for Spinal Implant Model Validation
Note 1: Risk-Informed Credibility Plan (ASME V&V 40)
The Decision Consequence of the model dictates the required Credibility. For a spinal implant model predicting adjacent segment disc stress:
- High Decision Consequence: Model informs a pivotal preclinical safety test (e.g., implant fracture risk). Requires High Credibility – extensive validation under multiple loading conditions with stringent accuracy metrics.
- Low Decision Consequence: Model used for comparative design screening (e.g., comparing two screw thread designs). May require only Medium Credibility – validation against a single benchmark experiment.
Note 2: Hierarchical Validation Strategy
Leverage a multi-fidelity approach to build model credibility efficiently:
- Sub-model Validation: Validate material models (e.g., titanium elastoplasticity, bone plasticity) against simple coupon tests.
- Component Validation: Validate implant sub-assembly performance (e.g., screw pullout from a synthetic bone block).
- System Validation: Validate full spinal segment (e.g., L3-L5) response under flexion/extension against cadaveric or synthetic spine test data.
Note 3: Validation Metrics and Acceptance Criteria
Define quantitative metrics a priori based on the standard's guidance and clinical relevance.
- Correlation: Use Mean Absolute Percentage Error (MAPE) or Correlation Coefficient (R²).
- Difference Metrics: Use Root Mean Square Error (RMSE) normalized to a relevant physical quantity (e.g., range of motion in degrees).
- Example Acceptance Criterion: For a range of motion prediction in a lumbar model, MAPE < 15% may be deemed acceptable for a medium-consequence decision.
Detailed Experimental Protocols
Protocol 1: Validation of a Lumbar Spinal Fusion Construct FEA Model
Title: Experimental Validation of an L4-L5 Instrumented FEA Model Against Cadaveric Biomechanical Testing.
Objective: To validate the kinematic (range of motion) and kinetic (facet joint forces) predictions of a lumbar fusion model per ASME V&V 40 and ISO 19208.
Materials & Reagents: See Scientist's Toolkit below.
Workflow Diagram:
Diagram Title: Spinal Implant Model V&V Workflow
Methodology:
- Computational Model Setup:
- Develop a detailed L4-L5 FEA model including vertebrae (cortical/cancellous bone), intervertebral disc (annulus ground substance & fibers), ligaments (7 major ligaments), and the implant (pedicle screws & rods).
- Assign material properties from peer-reviewed literature.
- Verification (Per ASTM F3163): Perform mesh convergence study. Calculate the Grid Convergence Index (GCI) for maximum von Mises stress in the implant and L4 inferior endplate displacement. Refine mesh until GCI < 5%.
Validation Experiment Setup:
- Obtain N=6 fresh-frozen human L4-L5 specimens.
- Pot specimens in polymethyl methacrylate (PMMA) fixtures.
- Mount on a servo-hydraulic test system equipped with a 6-axis load cell.
- Apply pure moments of 7.5 Nm in flexion, extension, lateral bending, and axial rotation following a standard loading protocol (e.g., ISO 12189).
- Measure segmental range of motion (ROM) using an optical motion capture system.
- Measure facet joint contact forces using thin-film pressure sensors inserted in the facet joint capsule.
Simulation & Comparison:
- Run the FEA simulation replicating the exact experimental loading and boundary conditions.
- Extract the same output quantities: ROM for each loading mode and facet joint forces.
- Calculate validation metrics between experimental (E) and simulated (S) data for each specimen:
ROM_MAPE = (1/N) * Σ(|S_i - E_i| / E_i) * 100%(for each motion direction).Force_R²for facet force vs. applied moment curve.
- Compare metrics to pre-defined acceptance criteria (e.g., ROM_MAPE < 20%; R² > 0.85).
Credibility Assessment:
- Following ASME V&V 40, given the model's use for a medium-consequence decision (supporting a 510(k) submission), the achieved validation evidence, combined with completed verification and uncertainty quantification, supports a Medium to High Credibility rating for predicting ROM.
Protocol 2: Verification of a Standalone Cervical Disc Implant Fatigue Model
Title: Code and Calculation Verification for an FEA Model of a Cervical Disc Fatigue Life Prediction.
Objective: To perform rigorous verification of the numerical solution for a dynamic fatigue analysis of a cervical disc implant as per ASTM F3163.
Workflow Diagram:
Diagram Title: FEA Model Verification Process
Methodology:
- Code Verification (Software):
- Use the Method of Manufactured Solutions (MMS). Apply a simple, known displacement field to a coarse mesh of a single implant component (e.g., the core).
- Calculate the corresponding body forces and boundary conditions required to satisfy the momentum equations.
- Input these forces/BCs into the FEA solver and run the analysis.
- Compare the solver's displacement output to the manufactured solution. The observed order of accuracy should approach the theoretical order of the elements used (e.g., ≥ 2.0 for quadratic elements).
- Calculation Verification (Specific Model):
- Develop three mesh densities for the full cervical disc implant assembly: Coarse, Medium, and Fine (e.g., increasing element count by a factor of ~1.5-2 each time).
- Run a static load step simulating peak load in the fatigue cycle.
- Monitor a key output, such as the maximum principal stress in the ultra-high molecular weight polyethylene (UHMWPE) core.
- Perform a Richardson Extrapolation on the results from the three meshes to estimate the asymptotic numerical value.
- Calculate the Grid Convergence Index (GCI) for the Fine mesh solution.
GCI_fine = (F_s * |ε|) / (r^p - 1), where ε is the relative error between fine and medium solutions, r is the refinement ratio, p is the observed order of accuracy, and F_s is a safety factor (1.25 for 3+ grids). - Acceptance: GCI < 10% for the region of interest (stress concentration area). Document this as the numerical uncertainty.
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions for Spinal Implant Model Validation
| Item / Solution | Function in Validation Context | Example Product / Specification |
|---|---|---|
| Synthetic Bone Blocks | Provides standardized, repeatable medium for component validation (e.g., screw pullout, rod bending). Mimics cancellous bone density. | Sawbones (Pacific Research Labs) foam blocks of specified density (e.g., 15 pcf or 30 pcf). |
| Fresh-Frozen Cadaveric Spines | The gold-standard biological substrate for system-level validation. Provides realistic anatomy and material properties. | Sourced from accredited tissue banks. Stored at -20°C, thawed in saline at 4°C prior to testing. |
| Biocompatible Potting Material | Secures bone specimens into testing fixtures for biomechanical testing. Provides rigid fixation without damaging the tissue. | Poly-methyl methacrylate (PMMA) dental acrylic or low-melt alloy. |
| 6-Axis Load Cell | Precisely measures applied forces and moments during biomechanical testing, providing input validation for simulations. | ATI Mini-45 or similar. Calibrated for Fx, Fy, Fz, Tx, Ty, Tz. |
| Optical Motion Capture System | Accurately measures 3D kinematic output (range of motion, center of rotation) for comparison with FEA predictions. | Vicon or OptiTrack systems with retroreflective markers. |
| Finite Element Analysis Software | Platform for developing and solving computational solid mechanics models. Must have robust solvers and element libraries. | Abaqus (Dassault Systèmes), Ansys Mechanical, or FEBio. |
| Thin-Film Pressure Sensor | Measures contact force/pressure in joints (e.g., facet joints) or between implant components for kinetic validation. | Tekscan K-Scan or I-Scan sensors, calibrated within appropriate pressure range. |
The Role of Validation in the Implant Design Lifecycle and Regulatory Submissions
1. Introduction Within the thesis framework of Protocol for validating spinal implant computational models research, validation is the critical process determining if a computational model accurately represents the physical reality of implant performance. It is not a single event but an iterative activity integrated throughout the design lifecycle, culminating in evidence for regulatory submissions. This document outlines application notes and detailed protocols to formalize this process.
2. Application Notes: Integrating Validation Milestones Validation activities must be synchronized with key design and regulatory stages, as summarized in Table 1.
Table 1: Validation Integration in the Implant Lifecycle
| Lifecycle Phase | Primary Validation Objective | Key Inputs | Output for Regulatory File |
|---|---|---|---|
| Concept & Feasibility | Assess model conceptual accuracy. | Literature data, material properties. | Report on model rationale and scope. |
| Design & Development | Correlate model predictions with benchtop tests (e.g., static, fatigue). | CAD geometry, ASTM test protocols, prototype test data. | Correlation plots and statistical analysis (e.g., R², error margins). |
| Verification & Validation (V&V) | Execute formal model V&V per ASME V&V 40. | Final test data from standardized mechanical tests. | Comprehensive V&V report documenting credibility. |
| Regulatory Submission | Demonstrate model credibility for specific Context of Use (COU). | All prior reports, risk analysis, COU statement. | Integrated summary for FDA/EMA, justifying model use in lieu of certain tests. |
3. Experimental Protocols for Validation Benchmarking The following protocol details a core experiment for validating a finite element analysis (FEA) model of a lumbar spinal implant under static compression.
Protocol 3.1: Physical Benchmark Test for Computational Model Validation
- Objective: To generate empirical data for validating a computational model predicting implant subsidence and strain under compressive load.
- Materials: See "Research Reagent Solutions" below.
- Methods:
- Specimen Preparation: Use polyurethane foam blocks (Grade 20, 0.32 g/cm³) as standardized surrogate bone material. Machine blocks to dimensions per ASTM F1839.
- Implant Placement: Assemble the titanium alloy (Ti-6Al-4V) implant per surgical technique guide. Insert it into the prepared foam block using a fixture ensuring consistent alignment.
- Instrumentation: Affix a minimum of three uniaxial strain gauges (e.g., 350-ohm) to critical locations on the implant. Connect to a calibrated data acquisition system.
- Mechanical Testing: Mount the construct in a servo-hydraulic test frame. Apply a pre-load of 50N. Then, apply a quasi-static compressive load at a rate of 25 N/s to a maximum of 2000N, holding for 30 seconds. Record load, displacement, and strain data at 100 Hz.
- Data Collection: Perform five (n=5) replicate tests. Record (i) Load vs. Displacement (subsidence) and (ii) Load vs. Microstrain for each gauge location.
- Deliverables: A dataset of mean displacement and strain values with standard deviations at key load intervals (e.g., 500N, 1000N, 2000N) for direct comparison to computational predictions.
4. Visualization of the Validation Workflow
Diagram 1: Validation workflow for spinal implant models.
Table 2: Sample Validation Metric Table (Compression at 2000N)
| Data Source | Subsidence (mm) | Strain at Location A (με) | Strain at Location B (με) |
|---|---|---|---|
| Experimental Mean (n=5) | 1.52 ± 0.18 | 1250 ± 95 | 980 ± 110 |
| Computational Prediction | 1.48 | 1190 | 1015 |
| Absolute Error | 0.04 | 60 | 35 |
| Error (%) | 2.6% | 4.8% | 3.6% |
5. The Scientist's Toolkit: Research Reagent Solutions Table 3: Essential Materials for Validation Testing
| Item | Function & Rationale |
|---|---|
| Polyurethane Foam Blocks (Grade 10/20) | Standardized surrogate for cancellous bone with consistent properties, reducing biological variability in benchtop tests. |
| Ti-6Al-4V ELI Alloy Rods/Implants | Medical-grade titanium alloy representing final implant material for testing; essential for accurate strain measurement. |
| Uniaxial Strain Gauges (350-ohm) | Sensors bonded to implant surface to measure local surface strain, providing direct comparison to FEA node results. |
| Servo-hydraulic Test Frame | Provides precise, controlled application of mechanical loads (compression, shear, fatigue) per ASTM standards. |
| Optical 3D Digital Image Correlation (DIC) System | Non-contact method to measure full-field displacement and strain on implant or surrogate bone surface. |
| ASTM F1717 / F2077 Standards | Definitive protocols for testing spinal constructs; provide the experimental framework for generating validation data. |
Diagram 2: Evidence hierarchy for regulatory acceptance.
Building the Digital Twin: A Step-by-Step Methodological Protocol
Within the broader thesis "Protocol for Validating Spinal Implant Computational Models," the accurate reconstruction of patient-specific spinal anatomy from medical imaging data is the foundational step. This application note details protocols for creating high-fidelity 3D anatomical models from CT or MRI scans, which serve as the geometric basis for subsequent finite element analysis (FEA) and computational validation of implant performance. The precision of this step directly impacts the predictive validity of the entire computational modeling pipeline.
Imaging Modality Selection
The choice between CT and MRI is dictated by the anatomical and tissue features of interest for implant validation.
| Modality | Optimal Use Case in Spinal Implant Research | Typical Resolution | Key Advantage | Primary Limitation |
|---|---|---|---|---|
| Computed Tomography (CT) | Bony anatomy (vertebrae, pedicles, endplates), implant-bone interface, porous structures. | 0.25 - 0.625 mm slice thickness | Excellent bone contrast; high spatial resolution; fast acquisition. | Poor soft tissue contrast; ionizing radiation. |
| Magnetic Resonance Imaging (MRI) | Soft tissues (intervertebral discs, ligaments, spinal cord, nerve roots), cartilage, bone marrow edema. | 0.5 - 1.5 mm slice thickness (3D sequences) | Superior soft tissue contrast; no ionizing radiation. | Lower bone definition; longer scan times; more sensitive to motion. |
Recommended Imaging Parameters for Research-Grade Reconstruction
Based on current literature and best practices for computational model generation, the following acquisition parameters are recommended.
| Parameter | CT Protocol (Cortical Bone) | MRI Protocol (Disc/Ligament) |
|---|---|---|
| Slice Thickness | ≤ 0.625 mm | ≤ 1.0 mm (3D isotropic voxels preferred) |
| In-Plane Pixel Spacing | ≤ 0.4 mm | ≤ 0.5 mm |
| Scan Field of View | Focused on target spinal segment(s) | Encompasses relevant soft tissue structures |
| Kernel/Sequence | Bone (sharp) kernel | T2-weighted 3D SPACE or equivalent |
| Dose/Contrast | As Low As Reasonably Achievable (ALARA) | N/A (non-contrast typically sufficient) |
Experimental Protocol: Anatomical Model Reconstruction Workflow
Materials & Software Requirements
Research Reagent Solutions & Essential Materials
| Item | Function/Description | Example Products/Tools |
|---|---|---|
| DICOM Image Dataset | Raw, unprocessed medical images in standard Digital Imaging and Communications in Medicine format. | Output from CT/MRI scanners. |
| Image Processing Software | For initial image enhancement, filtering, and format conversion. | ImageJ, Horos, 3D Slicer. |
| Segmentation Software | Core tool for labeling and isolating anatomical structures of interest from image data. | Mimics (Materialise), Simpleware ScanIP (Synopsys), ITK-SNAP, 3D Slicer. |
| 3D Model Editor (CAD) | For smoothing, repairing mesh defects, and preparing geometry for simulation. | Geomagic Wrap, Blender, MeshLab. |
| Reference Anatomical Atlas | Digital or literature-based guide for accurate structural identification during segmentation. | Visible Human Project, published anatomical studies. |
| High-Performance Workstation | Computer with significant RAM (≥32 GB), multi-core CPU, and dedicated GPU for handling large datasets. | Custom-built or commercial scientific workstations. |
Detailed Stepwise Protocol
Step 1: Data Acquisition & Import
- Acquire DICOM datasets per the parameters specified in Tables 1 & 2.
- Import the DICOM series into segmentation software. Ensure correct orientation (anatomical planes) and verify scale using embedded pixel spacing metadata.
Step 2: Image Pre-processing
- Apply noise reduction filters (e.g., non-local means, median filter) to improve signal-to-noise ratio, especially for MRI data.
- Enhance contrast using histogram equalization or contrast-limited adaptive histogram equalization (CLAHE) to better differentiate tissue boundaries.
- For multi-specimen studies, consider spatial normalization to a standard coordinate system.
Step 3: Multi-Structure Segmentation This is the most critical and time-intensive step.
- Thresholding: Use Hounsfield Unit (HU) ranges for CT data to create an initial mask for bone.
- Typical Cortical Bone HU: > 300
- Typical Trabecular Bone HU: 100 - 300
- Region Growing: Seed within a target vertebra and apply connectivity constraints to isolate it from adjacent structures.
- Manual Correction & Refinement: Use manual slice-by-slice editing tools to correct errors at boundaries with low contrast (e.g., disc-vertebra interface, posterior elements).
- Separate Segmentation: Repeat the process for each anatomical structure required for the model (e.g., individual vertebrae, intervertebral discs, ligament attachments).
- Label Fields: Assign each segmented structure a unique label.
Step 4: 3D Model Generation (Meshing)
- Calculate a 3D surface mesh (typically STL format) from each label field using the marching cubes algorithm.
- Adjust mesh quality parameters: target triangle count (balancing detail and computational load), smoothing iterations, and hole-filling.
Step 5: Post-Processing & Validation
- Import surface meshes into a 3D editor or CAD software.
- Perform mesh repair: fix non-manifold edges, remove self-intersections, and close holes.
- Apply minimal smoothing to reduce stair-step artifacts from voxel data without losing anatomical accuracy.
- Geometric Validation: Compare key dimensions (e.g., vertebral body width, pedicle diameter, disc height) of the 3D model against direct measurements from the source images or physical specimens. Document discrepancies.
Step 6: Preparation for Simulation
- Convert surface mesh to a volumetric mesh (tetrahedral or hexahedral elements) suitable for FEA within dedicated pre-processor software (e.g., ANSYS, Abaqus, FEBio).
- Assign material properties and boundary conditions in subsequent steps of the broader validation protocol.
Workflow Diagram
Workflow for Anatomical Model Reconstruction
Data Presentation & Metrics for Validation
Quantitative Validation Metrics
The accuracy of the reconstructed model must be assessed against a ground truth. Common metrics are summarized below.
| Validation Metric | Description | Acceptance Criterion (Typical) | Measurement Tool |
|---|---|---|---|
| Dice Similarity Coefficient (DSC) | Measures spatial overlap between segmented model and ground truth mask (2D or 3D). Range: 0 (no overlap) to 1 (perfect overlap). | DSC > 0.90 for bone; >0.85 for soft tissue. | Image analysis software (e.g., ITK-SNAP). |
| Average Surface Distance (ASD) | The average of all distances from points on model A to the closest point on model B. | ASD < 0.5 mm for bony anatomy. | Mesh comparison software (e.g., CloudCompare, Meshlab). |
| Hausdorff Distance (HD) | The maximum distance from points on model A to model B (measures worst-case error). | HD < 1.5 mm for bony anatomy. | Mesh comparison software. |
| Geometric Dimension Comparison | Linear measurements (e.g., disc height, vertebral width) compared to caliper measurements on specimen or image. | Difference < 5% of measured value. | CAD software / Image ruler tool. |
A rigorous and reproducible protocol for anatomical model reconstruction from CT/MRI data is essential for generating valid computational models for spinal implant research. Adherence to high-resolution imaging parameters, meticulous multi-structure segmentation, and quantitative geometric validation forms the critical first step in the thesis pipeline, ensuring that subsequent biomechanical simulations are based on a faithful representation of patient anatomy.
Within the protocol for validating spinal implant computational models, the accurate assignment of material properties and the biomechanical representation of spinal tissues are foundational. This step directly dictates the predictive fidelity of Finite Element Analysis (FEA) or Computational Fluid Dynamics (CFD) models under physiological loading. This document outlines contemporary approaches, data, and experimental protocols essential for this phase.
Quantitative Material Property Data for Spinal Tissues
Material properties are typically derived from experimental testing and integrated into computational models as linear/non-linear elastic, hyperelastic (e.g., Mooney-Rivlin, Ogden), or viscoelastic constitutive models.
Table 1: Representative Material Properties for Spinal Tissues
| Tissue/Component | Constitutive Model | Key Parameters (Mean ± SD or Range) | Source / Testing Method |
|---|---|---|---|
| Cortical Bone | Linear Elastic (Orthotropic) | E₁ = 11.4 ± 3.1 GPa, E₂ = E₃ = 5.9 ± 1.2 GPa, ν = 0.28 ± 0.06 | Uniaxial tensile/compression test on machined specimens. |
| Cancellous Bone | Non-linear Elastic (Crushable Foam) | Apparent Density: 0.1-0.3 g/cm³, Elastic Modulus: 50-500 MPa, Plateau Stress: 1-10 MPa | Quasi-static compression of core samples, density-modulus correlation. |
| Annulus Fibrosus (Ground Substance) | Hyperelastic (Mooney-Rivlin) | C10=0.12 MPa, C01=0.09 MPa, Bulk Modulus (K)=1.0 GPa | Biaxial or confined compression testing of hydrated tissue. |
| Nucleus Pulposus | Hyperelastic (Neo-Hookean) / Incompressible Fluid | Shear Modulus (μ) = 0.005 - 0.02 MPa, K = 1.67 GPa | Indentation or confined compression; often modeled as fluid cavity in FEA. |
| Spinal Ligaments (ALL, PLL, LF) | Non-linear Tension-Only (Viscoelastic) | Toe Region: E=5-10 MPa, Linear Region: E=50-150 MPa, Failure Strain: 15-30% | Uniaxial tensile test at low strain rates (0.01-0.1 /s). |
| Cartilage Endplate | Poroelastic | Permeability: k = 1e-15 ± 0.5e-15 m⁴/Ns, Elastic Modulus: 20-30 MPa | Confined compression stress-relaxation test. |
Experimental Protocols for Property Determination
These protocols provide the empirical data required for model inputs in Table 1.
Protocol 2.1: Uniaxial Tensile Testing for Spinal Ligaments
- Objective: To obtain non-linear stress-strain curves and failure parameters for ligaments (e.g., Ligamentum Flavum).
- Materials: Fresh-frozen human cadaveric spinal segments, saline solution, tensile testing machine with environmental chamber, cryo-clamps, digital image correlation (DIC) system.
- Procedure:
- Dissect ligament, ensuring minimal damage. Maintain hydration with 0.9% saline.
- Machine ends are potted in polymethylmethacrylate (PMMA) blocks for secure gripping.
- Mount specimen in testing machine equipped with a saline bath or spray system at 37°C.
- Apply a pre-load of 0.5 N to remove slack.
- Conduct a preconditioning cycle (10 cycles at 0.5% strain).
- Perform tensile test to failure at a quasi-static strain rate of 0.1%/s.
- Simultaneously, use DIC to measure full-field strain, accounting for grip artifacts.
- Record force (N) and displacement (mm). Calculate engineering stress (Force/initial cross-sectional area) and strain (Displacement/original gauge length).
- Data Analysis: Fit stress-strain data to a Fung-type exponential or piecewise linear model. Extract toe-region modulus, linear-region modulus, and failure stress/strain.
Protocol 2.2: Confined Compression for Intervertebral Disc Properties
- Objective: To determine the compressive modulus and hydraulic permeability of the nucleus pulposus/annulus ground substance.
- Materials: Isolated disc or tissue plug, confined compression chamber with porous platen, phosphate-buffered saline (PBS), load cell, displacement transducer.
- Procedure:
- Place a cylindrical tissue sample (e.g., nucleus) into the impermeable chamber fitted with a porous platen at the top.
- Submerge the chamber in 37°C PBS.
- Apply a small pre-strain (2-5%) and allow stress to equilibrate (30 mins).
- Apply a rapid step increase in compressive strain (e.g., 5%).
- Record the resulting stress as it relaxes over time (typically 30-60 mins).
- Repeat for multiple strain increments.
- Data Analysis: Fit the stress relaxation data to a linear biphasic (poroelastic) theory model (e.g., using the Hayes equation) to extract the aggregate modulus (Ha) and hydraulic permeability (k).
Tissue Modeling Approaches: Workflow & Logical Relationships
Title: Workflow for Assigning Material Properties in Spinal Implant Models
Title: Forward vs Inverse Material Parameter Identification
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Spinal Tissue Biomechanical Testing
| Item / Reagent | Function / Application | Key Consideration |
|---|---|---|
| Phosphate-Buffered Saline (PBS), 0.1M | Hydration and ionic balance maintenance for soft tissues during testing and storage. | Must be isotonic and used at 37°C to prevent tissue degeneration. |
| Protease Inhibitor Cocktail Tablets | Added to storage solution to inhibit enzymatic degradation of collagen and proteoglycans in soft tissues. | Critical for maintaining native mechanical properties in cadaveric tissues. |
| Polymethylmethacrylate (PMMA) Resin | For potting bone or ligament ends to ensure uniform load distribution and prevent slippage in grips. | Low exotherm versions preferred to avoid thermal damage to tissue. |
| Silicone-based Mold Release Agent | Prevents tissue samples from adhering to potting molds or compression chambers. | Must be biocompatible and not diffuse into tissue. |
| Digital Image Correlation (DIC) System | Non-contact, full-field 3D strain measurement on tissue surfaces during mechanical testing. | Requires application of a high-contrast speckle pattern to the tissue surface. |
| Porous Titanium or Sintered Bronze Platens | Used in confined/indentation tests to allow fluid exudation while applying compressive load. | Pore size must be small enough to support tissue but allow fluid flow. |
| Environmental Chamber with Temperature Control | Encloses the test setup to maintain physiological temperature (37°C) and humidity. | Prevents tissue drying, which significantly alters mechanical properties. |
| Calibrated Microsphere Suspensions | Used for permeability measurement in poroelastic testing via tracer methods. | Sphere size must be larger than proteoglycan mesh size to track fluid flow. |
Within the protocol for validating spinal implant computational models, Step 3 is the core of translating a conceptual implant design into a robust Finite Element (FE) model capable of predictive biomechanical analysis. The accuracy of this step directly dictates the validity of subsequent verification and validation steps. This application note details methodologies for geometric modeling, mesh generation, and contact definition for implants like cervical plates, lumbar pedicle screw systems, and interbody cages.
Implant Modeling and Geometric Idealization
Implant geometry is sourced from CAD designs or 3D scanned physical specimens. A critical decision is the level of geometric idealization required for the simulation objectives.
| Geometric Feature | High-Fidelity Model | Idealized Model | Rationale for Choice |
|---|---|---|---|
| Threads (Screws) | Explicit 3D threads modeled. | Smoothed cylindrical shaft with adjusted friction coefficients. | Explicit threads increase elements by >300% and require nonlinear contact. Use for pull-out studies. |
| Surface Texturing | Micro-scale roughness features included. | Macroscale geometry with averaged surface properties. | Critical for osseointegration studies; often omitted for macro-mechanics. |
| Small Fillets/Chamfers | Precisely modeled. | Simplified to sharp edges. | Simplification reduces mesh complexity with minimal impact on global stiffness. |
| Porosity (e.g., Ti/Ta lattice) | Homogenized material properties. | Explicit strut modeling. | Explicit modeling is computationally prohibitive for full assembly; homogenization is standard. |
Protocol 2.1: CAD Preparation for FE
- Import solid geometry (STEP or IGES format) into pre-processor (e.g., ANSYS SpaceClaim, Altair HyperMesh).
- Defeaturing: Remove non-structural details (logo engraving, minute fillets <0.1mm).
- Healing: Repair any gaps, overlaps, or non-manifold edges from translation.
- Partitioning: Split complex volumes into simpler, mappable regions for structured meshing (e.g., separate screw head from shaft).
- Export the cleaned geometry as a Parasolid (.x_t) file for meshing.
Meshing Strategies and Quality Metrics
Meshing converts geometry into discrete elements. A convergence analysis is mandatory within the broader thesis validation protocol.
| Mesh Type | Element Formulation | Typical Size at Implant | Application & Notes |
|---|---|---|---|
| Tetrahedral (Tet10) | Quadratic, 10-node | 0.5 - 1.0 mm | Complex geometries. Softer than hexahedral; use with caution in bending. |
| Hexahedral (Hex8/Hex20) | Linear/Quadratic, 8/20-node | 0.3 - 0.7 mm | Preferred for accuracy and efficiency. Requires geometry partitioning. |
| Mixed (Hex-Dominant) | Hybrid | Varies | Hex in bulk regions, tets in complex zones. Practical compromise. |
Protocol 3.1: Mesh Convergence Analysis Objective: Determine mesh density where solution (e.g., peak von Mises stress in implant) changes by <5%.
- Generate 4 mesh sets with global element sizes progressively refined by a factor of ~1.5 (e.g., 2.0mm, 1.3mm, 0.9mm, 0.6mm).
- Apply identical boundary conditions and a representative load case (e.g., flexion moment).
- Solve each model and extract a key output parameter (P):
P_max_stress_implant,P_max_strain_bone. - Calculate relative error between successive meshes:
Error (%) = |(P_fine - P_coarse) / P_fine| * 100. - Select the mesh density one level coarser than the point where error falls below 5% as the converged mesh.
Protocol 3.2: Mesh Quality Assurance Check Before solution, validate mesh quality against these thresholds in the pre-processor:
- Jacobian Ratio (Quad/Hex): > 0.6
- Skewness: < 0.7 (Tet), < 0.5 (Hex)
- Aspect Ratio: < 10 for bone-implant interface regions
- Element Warping (Quad/Hex): < 15 degrees
Contact Definitions and Interface Modeling
This defines mechanical interactions between implant components and between implant and bone.
| Contact Type | Formulation | Friction Coefficient (μ) | Application |
|---|---|---|---|
| Bonded | No separation/slip. | N/A | Cemented interfaces, locked screw-plate junctions. |
| Frictional | Slip allowed after friction overcome. | 0.2 - 0.6 (Ti-Ti) | Bone-implant interface (primary stability), screw-plate lag. |
| Frictionless | Free slip, no shear resistance. | 0.0 | Conservative simplification of lubricated contact. |
| No Separation | Allows slip, prevents gap opening. | N/A | Model of retained but not bonded components. |
Protocol 4.1: Defining Bone-Implant Interface Contact
- Surface Preparation: Designate the implant outer surface as the "Contact" body and the adjacent bone cavity surface as the "Target".
- Type Selection: For primary stability simulation, select "Frictional".
- Parameter Definition:
- Set friction coefficient (
μ) to 0.4 as a baseline for Titanium-Trabecular bone. - Define normal behavior as "Augmented Lagrange" for robustness.
- Set pinball region to automatically handle initial gaps/penetrations.
- Set friction coefficient (
- Advanced Controls: Enable "Adjust to Touch" to ensure initial contact. Use a symmetric bilateral contact for scenarios where either body can be contact/target.
Protocol 4.2: Modeling Threaded Contacts in Pedicle Screws
For explicit threads, a frictional contact (μ=0.2) is defined between all thread flanks and bone. For idealized smooth shafts:
- Define a bonded contact zone in the predicted region of osseointegration (proximal 1/3 of shaft).
- Define a frictional contact (
μ=0.3-0.5) over the remaining shaft to simulate initial mechanical interlock.
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function in Computational Modeling |
|---|---|
| CAD Software (SolidWorks, Creo) | Generates the initial, precise 3D geometry of the implant design. |
| FE Pre-processor (ANSYS, Abaqus/CAE, HyperMesh) | Platform for geometry healing, partitioning, meshing, and contact definition. |
| High-Performance Computing (HPC) Cluster | Enables running large, nonlinear contact models with fine meshes in feasible time. |
| ISO 5832 / ASTM F136 Titanium Alloy Material Data | Provides validated elastic-plastic material properties for implant material definition. |
| Mesh Convergence Script (Python/Matlab) | Automates the process of batch meshing, solving, and result extraction for convergence studies. |
| Medical Image Data (μCT of cadaveric bone) | Source for generating accurate 3D bone geometry (vertebrae) to model the implant's environment. |
This protocol details the critical step of applying physiological boundary conditions and load cases within the broader thesis framework, "Protocol for Validating Spinal Implant Computational Models." This step transforms a generic finite element model into a validated, predictive tool by simulating in vivo mechanical environments. Accurate application is paramount for predicting implant performance, adjacent segment effects, and bone remodeling.
Core Principles & Quantitative Data
Boundary conditions (BCs) constrain model displacement, while load cases represent physiological forces. Key quantitative data for the lumbar spine (L1-L5) are summarized below.
Table 1: Representative Physiological Loads for Lumbar Spine Analysis
| Load Case | Magnitude (N) | Direction | Application Point | Primary Physiological Activity |
|---|---|---|---|---|
| Compression | 500 - 1200 | Axial (Inferior-Superior) | Superior Endplate | Standing, Weight-Bearing |
| Flexion | 7.5 - 10 Nm | Sagittal Plane Moment | L3 Vertebral Body | Forward Bending |
| Extension | 7.5 - 10 Nm | Sagittal Plane Moment | L3 Vertebral Body | Backward Bending |
| Lateral Bending | 7.5 - 10 Nm | Coronal Plane Moment | L3 Vertebral Body | Side Bending |
| Axial Rotation | 5 - 7.5 Nm | Axial Plane Moment | L3 Vertebral Body | Twisting/Torsion |
| Combined Loading (Gait) | 400-800 N + Variable Moments | Multi-Axial | Superior Endplate | Walking |
Table 2: Common Boundary Condition Definitions
| Constraint Type | Degrees of Freedom Constrained | Typical Anatomical Application | Rationale |
|---|---|---|---|
| Fixed (Encastered) | All (UX, UY, UZ, ROTX, ROTY, ROTZ) | Inferior Endplate of Lowest Vertebra (e.g., L5/S1) | Simulates fixation to immobile pelvis. |
| Frictionless Support | Translations (UX, UY, UZ) | Inferior Endplate | Allows rotation but prevents rigid body motion. |
| Symmetry BC | UX=0, ROTY=0, ROTZ=0 | Mid-sagittal Plane | Reduces model size for symmetric analyses. |
Experimental Protocols
Protocol 3.1: Application of Pure Moment Loading for Range-of-Motion (ROM) Simulation
Objective: To simulate standard flexion, extension, lateral bending, and axial rotation for implant comparison.
- Model Setup: Isolate the spinal segment (e.g., L4-L5) with implant. Fix all degrees of freedom at the inferior endplate of the lower vertebra (L5).
- Load Application: Apply a pure moment up to the target value (e.g., 10 Nm) incrementally to the superior endplate of the upper vertebra (L4). Use a coupling constraint or reference point (RP) tied to the superior endplate to apply the moment.
- Data Acquisition: At each load increment, record the angular rotation (in degrees) of the superior vertebra relative to the inferior vertebra in the plane of the applied moment.
- Output: Generate a moment-rotation curve. Calculate the Neutral Zone (NZ) and Elastic Zone (EZ) from the hysteresis loop. Compare ROM to intact spine and other implant models.
Protocol 3.2: Application of Combined Compression-Flexion Loading
Objective: To simulate a more physiologically demanding activity, such as lifting.
- Model Setup: As per Protocol 3.1.
- Load Application: a. First, apply a static axial preload of 500 N to the superior endplate RP to simulate body weight. b. Subsequently, apply a linearly increasing flexion moment (0 to 10 Nm) to the same RP, superimposed on the preload.
- Data Acquisition: Record intradiscal pressure (if modeled), facet joint contact forces, implant stresses, and segmental rotation.
- Output: Report peak von Mises stress in implant components, contact forces at the facet joints, and total angular displacement.
Protocol 3.3: Kinematic Validation via Displacement-Control Loading
Objective: To validate the model against in vitro biomechanical testing data.
- Input Data: Obtain experimental rotation data from a cadaveric study for a specific load (e.g., 8 Nm flexion).
- Model Setup: Apply boundary conditions identical to the experimental setup (e.g., potting of inferior vertebra).
- Load Application: Instead of applying a moment, prescribe the angular displacement (from experiment) to the superior vertebra.
- Data Acquisition: Compute the reaction moment generated by the model at the fixed boundary.
- Output: Compare the model-predicted reaction moment to the experimental applied moment (8 Nm). Calculate correlation coefficient (R²) and relative error.
Visualizations
Diagram 1: BC & Load Application Workflow
Diagram 2: Multi-Step Load Case for Gait
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Boundary Condition & Load Application
| Item / Solution | Function in Protocol | Example Product / Specification |
|---|---|---|
| Finite Element Software | Platform for applying BCs, loads, and solving. | Abaqus, ANSYS, FEBio. |
| Material Property Datasets | Defines nonlinear, isotropic/orthotropic behavior for bone, ligaments, and implant. | Published data for cortical/cancellous bone, titanium alloy (Ti-6Al-4V), PEEK. |
| Kinematic Coupling Constraint | Applies moments/forces to a reference point tied to a vertebral surface. | Abaqus: Coupling/MPC constraint. ANSYS: Remote Displacement/Force. |
| Nonlinear Solver | Essential for solving large deformations and contact under complex loads. | Abaqus/Standard, ANSYS Mechanical APDL, FEBio's Newton-Raphson solver. |
| Validation Dataset (Benchmark) | In vitro cadaveric ROM data for intact and implanted states. | Published data from Wilke et al. (1998) or subsequent studies. |
| High-Performance Computing (HPC) Cluster | Reduces solution time for complex, nonlinear, multi-step analyses. | Local cluster or cloud-based solutions (AWS, Azure). |
| Python/Matlab Scripting | Automates the application of multi-step load cases and batch post-processing. | Custom scripts for Abaqus Python API or ANSYS ACT. |
Within the broader thesis on a Protocol for Validating Spinal Implant Computational Models, the design of physical bench tests is the critical translational step. These tests provide empirical, quantitative data to assess the predictive accuracy of finite element analysis (FEA) and computational biomechanics models. This application note details the design principles and specific protocols for corresponding physical bench tests, ensuring a rigorous validation framework.
Core Principles for Corresponding Test Design
The physical test must be the biomechanical analogue of the computational model. Correspondence is defined by:
- Identical Boundary Conditions: Fixturing in the physical test must replicate the model's constraints.
- Identical Loading Profiles: Magnitude, rate, direction, and application point of loads must match.
- Identical Outcome Measures: The measured physical parameters (e.g., strain, displacement, load) must be the direct counterparts of the model's output variables.
- Use of Identical Constructs: The implant, screw, and surrogate bone (e.g., polyurethane foam block) specifications must be the same in both realms.
Key Experimental Protocols
Protocol 1: Quasi-Static Axial Compression/Bending Test for a Lumbar Vertebral Body Replacement (VBR) Construct
Objective: To validate computational model predictions of stiffness, subsidence risk, and load distribution under physiological loading.
Detailed Methodology:
- Construct Preparation:
- Use a standardized rigid polyurethane foam block (Grade: 20 pcf / 0.32 g/cm³) to simulate osteoporotic cancellous bone, per ASTM F1839.
- Machine a block to representative vertebral body dimensions (e.g., 25mm height x 40mm width x 40mm depth).
- Prepare the VBR implant per manufacturer instructions.
- Assemble the VBR implanted centrally within the foam block, ensuring uniform endplate contact. Pot the ends in dental stone or low-melting-point alloy within loading platens to ensure even load distribution.
Instrumentation & Setup:
- Mount the construct onto a servo-hydraulic or electro-mechanical materials testing system (e.g., Instron, MTS).
- Calibrate the system's load cell and actuator displacement transducer.
- Affix a minimum of three uniaxial strain gauges (e.g., 350Ω) or a digital image correlation (DIC) system to the implant surface and/or foam block to map strain fields.
- Position a displacement sensor (LVDT) to measure inter-segmental compression.
Loading Protocol:
- Pre-condition the construct with 10 cycles of compression from 50N to 500N at 1 Hz.
- Perform a quasi-static compression test to failure or to a predefined limit (e.g., 5000N) at a displacement rate of 1 mm/min.
- Continuously record load (N), actuator displacement (mm), strain gauge microstrain (µε), and LVDT displacement (mm).
Data Analysis:
- Calculate construct stiffness (N/mm) as the slope of the linear region of the load-displacement curve.
- Identify yield load from the 0.2% offset method.
- Correlate experimental strain maps with FEA-predicted strain contours.
Table 1: Representative Data from VBR Compression Validation Study
| Metric | Computational Model Prediction | Physical Bench Test Result (Mean ± SD, n=5) | Percent Difference | Validation Criterion Met? |
|---|---|---|---|---|
| Construct Stiffness (N/mm) | 2450 | 2310 ± 185 | 5.7% | Yes (<10%) |
| Yield Load (N) | 4150 | 3880 ± 310 | 6.5% | Yes (<15%) |
| Peak Strain at Location A (µε) | -1250 | -1180 ± 95 | 5.6% | Yes (<10%) |
Protocol 2: Dynamic Cyclic Fatigue Test for a Pedicle Screw-Rod Construct
Objective: To validate model predictions of fatigue life and failure mode under cyclic physiological loading.
Detailed Methodology:
- Construct Preparation:
- Use ultra-high molecular weight polyethylene (UHMWPE) or composite test blocks with pre-drilled pilot holes as a consistent surrogate for bone.
- Instrument the block with two pedicle screws (per manufacturer technique) connected by a titanium rod (5.5mm diameter).
- Secure the block in a custom fixture that allows pure moment application.
Setup & Fixturing:
- Mount the fixture on a dynamic biaxial testing system capable of applying simultaneous axial and torsional loads.
- The fixture must allow unconstrained motion along the loading axis to apply pure moments via follower load principles.
Loading Protocol (Based on ASTM F1717):
- Apply a constant compressive pre-load of 200N.
- Superimpose a cyclic sinusoidal flexion-extension moment at a frequency of 2-5 Hz.
- Load magnitude: ±5 Nm to ±10 Nm (based on model simulation loads).
- Cycle until construct failure (defined as screw fracture, rod fracture, or catastrophic loosening) or to 5 million cycles (run-out).
Data Analysis:
- Record cycles to failure.
- Document failure mode via macroscopic and microscopic imaging.
- Compare predicted high-stress locations from FEA with actual failure initiation sites.
Table 2: Example Fatigue Test Validation Matrix
| Loading Condition | FEA Predicted Fatigue Life (Cycles) | Experimental Mean Life (Cycles, n=3) | Observed Failure Mode | Predicted High-Stress Location |
|---|---|---|---|---|
| ±7.5 Nm, 4 Hz | 1.2 x 10⁶ | 0.9 x 10⁶ | Screw fracture at shank-neck junction | Screw shank-neck junction |
| ±10 Nm, 4 Hz | 3.5 x 10⁵ | 2.8 x 10⁵ | Rod fracture near screw interface | Rod at set-screw contact |
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions & Materials
| Item | Specification / Example | Primary Function in Validation |
|---|---|---|
| Surrogate Bone | Rigid Polyurethane Foam (20 pcf) | Provides a consistent, isotropic material with known properties to simulate cancellous bone for screw pull-out/insertion and implant subsidence tests. |
| Composite Test Blocks | Fiber-reinforced epoxy (e.g., Sawbones) | Mimics the anisotropic properties of cortical bone for more realistic pedicle screw fixation testing. |
| Strain Gauges | Uniaxial or Rosette, 350Ω | Precisely measures surface strain on implants or bone surrogates for direct comparison with FEA nodal strain outputs. |
| Digital Image Correlation (DIC) System | Aramis, Vic-3D | Non-contact, full-field 3D strain and displacement mapping; crucial for validating complex strain fields predicted by models. |
| Servo-Hydraulic Test System | MTS Bionix, Instron 8874 | Applies precise, programmable static and dynamic (cyclic) loads to simulate in-vivo biomechanics. |
| Optical Motion Tracking | Qualisys, Vicon | Measures 3D kinematics of multi-segment spine constructs under load, validating kinematic model predictions. |
| Low-Melting-Point Alloy | Cerrobend | Used for potting irregular test specimens to ensure repeatable and uniform load application in fixtures. |
| Calibration Standards | NIST-traceable load cells, dimensional blocks | Ensures traceability, accuracy, and repeatability of all physical measurements for credible validation. |
Validation Workflow Diagram
Subsidence Test Pathway
Navigating Pitfalls: Common Errors, Convergence Issues, and Sensitivity Analysis
Resolving FEA Convergence Problems in Complex Contact Simulations
Within the broader thesis on Protocol for Validating Spinal Implant Computational Models, the verification of Finite Element Analysis (FEA) models against experimental benchmarks is paramount. Complex contact simulations, such as those between a spinal implant (cage, screw, rod) and vertebral bone, are critical for predicting micromotion, stress shielding, and long-term stability. However, these simulations are notoriously prone to non-convergence, undermining model validity. This application note details systematic protocols for diagnosing and resolving convergence issues in this specific research context.
The table below summarizes prevalent convergence issues, their indicators, and typical impact severity based on a review of recent literature and software documentation.
Table 1: Primary Sources of FEA Convergence Failure in Spinal Implant Contact Simulations
| Source Category | Specific Issue | Common Numerical Indicator | Typical Impact on Solution (Severity) |
|---|---|---|---|
| Contact Formulation | Initial penetration / gaps > element size | Negative residual forces, immediate divergence. | High |
| Inappropriate contact stiffness (too high/low) | Oscillating residual norms, cutbacks. | High | |
| Choice of penalty vs. augmented Lagrange method | Convergence rate, contact pressure accuracy. | Medium | |
| Material & Geometric Nonlinearity | High plasticity in cancellous bone without proper hardening. | Lack of equilibrium in force residuals. | High |
| Large deformation of ligamentous tissues without updated contact. | Extreme mesh distortion, negative Jacobian. | High | |
| Mesh & Discretization | Incompatible mesh densities at contact surfaces. | Abrupt stress jumps, failure to reduce residuals. | Medium |
| Poorly shaped elements (aspect ratio >10) in contact zone. | Ill-conditioned stiffness matrix. | Medium | |
| Solver Settings | Overly aggressive incremental/step sizes. | Repeated cutback, minimal progress. | Medium |
| Insufficient equilibrium iterations per increment. | Premature termination, high residuals. | Low |
Experimental Protocols for Convergence Diagnosis & Resolution
Protocol 3.1: Systematic Diagnosis of Non-Convergence
Objective: To identify the root cause of convergence failure in a spinal implant-bone contact simulation. Workflow:
- Run a single increment, small load step simulation (e.g., 1% of nominal load).
- Examine the message file for error codes (e.g., "too many attempts," "negative eigenvalues").
- Plot the residual force norm vs. iteration number for the failed increment. A diverging plot suggests contact/instability; an oscillating plot suggests stiffness issues.
- Visualize contact status and pressure at the last converged increment. Look for excessive penetration, abrupt changes in contact status, or singularities.
- Check mesh quality metrics (Jacobian, aspect ratio, skew) specifically within the contact region and highly deformed volumes.
- Output reaction forces at boundary conditions to verify global equilibrium is being sought.
Protocol 3.2: Stepwise Resolution of Contact-Induced Non-Convergence
Objective: To achieve a stable, converging solution for a vertebroplasty cement-implant interface model. Methodology:
- Initial Condition Stabilization:
- Apply a small "stabilization" or "smoothing" step with artificial damping (available in solvers like Abaqus) to establish initial contact without dynamics.
- Alternatively, use "contact controls" to soften contact stiffness for the initial increment.
- Contact Formulation Tuning:
- Begin with a "softened" penalty contact (e.g., "soft contact" in Abaqus with exponential pressure-overclosure).
- If oscillations persist, switch to an Augmented Lagrange formulation, which enforces contact constraints more strictly but may require more iterations.
- Set contact stiffness based on underlying material stiffness. A guideline:
KN ≈ 10 * (E / h), where E is Young's modulus of the softer material and h is characteristic element length. Adjust via trial.
- Incrementation Strategy:
- Use automatic incrementation with a small initial increment size (0.01).
- Set a high maximum number of increments (e.g., 1000).
- Allow a moderate number of equilibrium iterations per increment (e.g., 15-20).
- Verification:
- After successful run, perform an energy balance check (ALLWK vs. ALLIE). Ensure artificial strain energy (ALLAE) is < 5-10% of internal strain energy (ALLIE) for quasi-static analyses.
Protocol 3.3: Mesh Sensitivity and Compatibility Protocol
Objective: To ensure mesh discretization does not cause convergence failure in a pedicle screw-bone thread contact simulation. Methodology:
- Create a mesh compatibility region: On the master surface (e.g., implant thread), seed a fine mesh. On the slave surface (e.g., bone thread), seed a mesh of similar density. A ratio of slave element size to master of 1:1 to 2:1 is ideal.
- Use bias meshing to gradually coarsen the mesh away from the contact interface.
- Employ secondary surface offset or "adjust" settings to ensure nodes are within a reasonable search distance at the start of the analysis.
- Run a convergence study: Refine the global mesh size by factors of √2 until key outputs (peak contact pressure, relative micromotion) change by < 2-5%.
Visualization: Convergence Troubleshooting Workflow
Diagram Title: FEA Contact Convergence Troubleshooting Logic Flow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for Robust Spinal Implant Contact FEA
| Item / Solution | Function & Rationale |
|---|---|
| Abaqus/Standard (Implicit) | Primary solver for quasi-static, nonlinear contact problems. Its robust Newton-Raphson method with automatic incrementation is industry-standard for implant analysis. |
| Augmented Lagrange Contact | A contact formulation that combines penalty and Lagrange multiplier methods. Reduces penetration compared to pure penalty without the numerical stiffness of pure Lagrange, crucial for accurate interface pressure. |
| Automatic Surface-to-Surface Contact | Defines contact between deformable bodies using surface integrals, generally more accurate than node-to-surface, especially for sliding and curved interfaces like screw threads. |
| Material Calibration Data (e.g., Bone Plasticity) | Experimentally-derived yield stress and hardening parameters for cancellous/cortical bone are essential to model permanent deformation under implant insertion, preventing non-convergence from unrealistic material response. |
| High-Performance Computing (HPC) License | Enables parallel processing of contact algorithms and matrix inversion, drastically reducing solution time for the high iteration counts required in resolving difficult contact. |
| Python Scripting Interface | Allows for parametric modeling, automated batch submission of multiple simulations with varying contact properties, and post-processing of convergence metrics (residuals, energies). |
| Validation Dataset (DIC, Biomechanical Test) | Digital Image Correlation (DIC) strain maps and load-displacement curves from physical implant testing are required to tune contact parameters and validate the final converging model. |
This application note details protocols for mesh optimization within a broader thesis research program focused on validating computational models of spinal implants. Achieving a balance between simulation fidelity and practical computational expense is paramount for enabling efficient, predictive in silico testing of implant designs. Mesh optimization is the critical process of refining the finite element (FE) mesh—the discretized representation of the geometry—to ensure solution accuracy without incurring prohibitive computational cost.
Foundational Principles
The core challenge lies in minimizing the discretization error introduced when a continuous physical domain is divided into finite elements. Key concepts include:
- Convergence: The process of sequentially refining the mesh until the solution (e.g., stress, strain, displacement) changes by less than an acceptable tolerance.
- Mesh Sensitivity: The degree to which the simulation results depend on mesh density and quality.
- Adaptive Mesh Refinement (AMR): An automated process where the mesh is refined in regions of high solution gradients (e.g., stress concentrations near implant edges) and coarsened in areas of low gradients.
Quantitative Data on Mesh Parameters & Performance
Table 1: Impact of Global Mesh Size on Lumbar Spinal Segment (L3-L4) FE Model Performance
| Mesh Size (Avg. Element Edge, mm) | Number of Elements (Nodes) | Max Von Mises Stress at Implant (MPa) | Computational Time (min) | RAM Usage (GB) | Recommended Application |
|---|---|---|---|---|---|
| 2.5 | ~45,000 (~85,000) | 185.4 | 12 | 3.2 | Preliminary design screening |
| 1.2 | ~250,000 (~420,000) | 213.7 (+15.3%) | 68 | 8.5 | Standard design analysis |
| 0.8 | ~850,000 (~1.4M) | 221.1 (+19.3%) | 245 | 24.1 | High-fidelity validation |
| 0.5 (Reference) | ~3.2M (~5.1M) | 225.0 | 1,120 | 87.3 | Benchmark/Convergence study |
Table 2: Error and Cost Trade-off for Different Mesh Optimization Strategies
| Optimization Strategy | Error vs. Dense Mesh (Displacement, %) | Computational Cost vs. Uniform Fine Mesh (%) | Key Benefit | Key Limitation |
|---|---|---|---|---|
| Uniform Coarse Mesh | 8.5 | 15 | Speed | Misses stress risers |
| Uniform Fine Mesh | 0.5 (ref) | 100 (ref) | Accuracy | High resource use |
| Manual Local Refinement | 2.1 | 40 | Control | User expertise required |
| h-Adaptive Refinement | 1.8 | 35 | Automated efficiency | Setup complexity |
| p-Adaptive Refinement | 1.5 | 50 | Exponential convergence | Software support limited |
Experimental Protocols for Mesh Convergence Studies
Protocol 4.1: Standard Mesh Convergence Analysis for Spinal Implant Models
Objective: To determine the mesh density required for a solution accuracy within a pre-defined tolerance (e.g., <5% change in peak stress).
Materials: CAD model of spinal implant and vertebral bodies (L3-L4), FE software (e.g., Abaqus, ANSYS, FEBio), high-performance computing (HPC) workstation.
Procedure:
- Mesh Generation (Iteration 1): Generate an initial, relatively coarse, high-quality mesh (primarily tetrahedral or hexahedral elements) for the complete assembly (vertebrae, implant, ligaments). Record the global average element size (h₁) and total element count.
- Boundary Conditions & Solving: Apply physiological loading conditions (e.g., 1000N axial compression + 7.5Nm flexion). Solve the linear or non-linear static FE problem. Extract key outcome measures: peak Von Mises stress in the implant (σ_vm), maximum bone-implant interface stress, and segmental range of motion.
- Data Recording: Log (σ_vm)₁, computational time, and RAM usage.
- Systematic Refinement: Globally refine the mesh by reducing the average element size by a factor (e.g., 0.75*h₁) to create a new mesh (h₂). Ensure mesh quality metrics (aspect ratio, skewness, Jacobian) remain acceptable.
- Iteration & Comparison: Repeat steps 2-4 for at least 3-4 mesh densities. For each refinement i, calculate the relative change in peak outcome measures: Δ = |(Valuei - Value{i-1}) / Value_{i-1}| * 100%.
- Convergence Criterion: Plot key outcomes (σ_vm) versus element count or computational cost. The converged mesh is identified when Δ for all primary outcomes falls below the acceptable threshold (e.g., 5%) between two successive refinements.
Protocol 4.2: Protocol for Adaptive Mesh Refinement (AMR) in Stress Concentration Zones
Objective: To automate mesh refinement in regions of high stress gradient to improve accuracy efficiently.
Procedure:
- Initial Coarse Solution: Run an initial FE analysis on a coarse, uniform mesh (Protocol 4.1, Iteration 1).
- Error Estimation: Use the software's built-in error estimator (typically based on stress or strain energy density gradients) to calculate a spatial error field across the model.
- Refinement Criterion Definition: Set a threshold for the error estimator (e.g., refine elements where the relative error is >15%).
- Automated Refinement: The AMR algorithm subdivides (h-refinement) or increases element order (p-refinement) for elements meeting the criterion.
- Re-solution: The FE problem is solved on the adapted mesh.
- Iteration Check: The error estimation process is repeated. Steps 4-5 are iterated until the global error estimate or the maximum local error falls below a target value, or for a set number of cycles.
Visualizations
Title: Mesh Convergence Study Workflow
Title: Adaptive Mesh Refinement (AMR) Cycle
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials & Software for Mesh Optimization Studies
| Item | Category | Example/Supplier | Function in Protocol |
|---|---|---|---|
| FE Software with AMR | Software | Abaqus/Standard (SIMULIA), ANSYS Mechanical, FEBio | Primary platform for meshing, solving, and automated adaptive refinement. |
| HPC Cluster/Workstation | Hardware | Local HPC, Cloud (AWS, Azure), WS with >64GB RAM, multi-core CPU | Enables solving of large, high-fidelity models within practical timeframes. |
| Anatomical Geometry Database | Data | SpineWeb, The Open Science Framework (OSF) | Provides validated, segmentable 3D models of vertebral bodies for patient-specific or generalized studies. |
| Mesh Quality Tool | Software Plugin | MeshAssess (FEBio), ANSYS Meshing Metrics | Quantifies element quality (Jacobian, skew, aspect ratio) to ensure solution stability. |
| Python/Matlab Scripts | Custom Code | In-house developed scripts | Automates batch processing of convergence studies, data extraction, and result plotting. |
| Standardized Load Cases | Protocol Data | ISO 12189, ASTM F1717 | Provides benchmark axial compression/flexion moments for comparative validation of implant models. |
Addressing Uncertainties in Material Properties and Boundary Conditions
Within the thesis on Protocol for validating spinal implant computational models, addressing uncertainties in material properties and boundary conditions (BCs) is a critical step for ensuring model predictive fidelity. Computational models, primarily Finite Element Analysis (FEA), are indispensable for evaluating spinal implant biomechanics, stress shielding, and long-term performance. However, the validity of these models is contingent upon accurate inputs. This document provides application notes and detailed experimental protocols to characterize these inputs and quantify their associated uncertainties, thereby strengthening the validation framework.
Table 1: Reported Ranges for Key Material Properties in Spinal Modeling
| Material / Tissue | Property | Typical Range (Mean ± SD) | Coefficient of Variation (%) | Key Source of Uncertainty |
|---|---|---|---|---|
| Cortical Bone | Elastic Modulus (E) | 12.0 - 20.0 GPa | 15-25% | Donor age, health, anatomic site, testing method (tensile vs. nanoindentation). |
| Cancellous Bone | Elastic Modulus (E) | 50 - 500 MPa | 30-50% | High porosity variation, site-specific density, loading direction (anisotropy). |
| Intervertebral Disc (Annulus) | Elastic Modulus (E) | 3.5 - 6.5 MPa | 20-35% | Hydration state, degeneration grade, fiber orientation. |
| Titanium Alloy (Ti-6Al-4V) | Elastic Modulus (E) | 110 - 115 GPa | 1-3% | Manufacturing process (forged vs. printed), post-processing. |
| PEEK | Elastic Modulus (E) | 3.0 - 4.0 GPa | 5-10% | Crystallinity, filler content (e.g., carbon fiber). |
| Spinal Ligament (e.g., ALL) | Stiffness (K) | 20 - 70 N/mm | 40-60% | Pre-strain, viscoelasticity, testing strain rate. |
Table 2: Common Boundary Condition Uncertainties in Spinal FEA
| BC Type | Typical Implementation | Uncertainty Source | Impact on Model Output (e.g., Range of Motion, Implant Stress) |
|---|---|---|---|
| Load Application | Force/Moment at top vertebra | Point of application, direction, magnitude. | ±15-30% change in segmental ROM. |
| Inferior Fixation | Fully fixed (encastre) | Realistic constraint at lower vertebra is not perfect fixation. | Overestimation of implant stresses by up to 20%. |
| Contact Definitions | Friction coefficient at implant-bone interface | Assumed value (e.g., 0.2-0.8); changes with surface texture, coating. | ±25% variation in micromotion predictions. |
| Muscle Forces | Often simplified or omitted | Complex force directions and magnitudes in vivo. | Alters load sharing, can affect facet joint forces by >40%. |
| Pre-stress/Pre-strain | Often neglected in ligaments | Alters neutral zone and stiffness response. | Significant impact on initial stability predictions. |
Experimental Protocols for Parameter Characterization
Protocol 3.1: Nanoindentation for Site-Specific Bone Modulus
Objective: To determine the elastic modulus of cortical and cancellous bone at micro-scale from donor specimens, informing patient-specific FEA inputs. Materials: Fresh-frozen human vertebral bodies, microtome, embedding resin, nanoindenter (e.g., Bruker Hysitron), phosphate-buffered saline (PBS). Methodology:
- Specimen Preparation: Section vertebral body into sagittal slices (∼3mm thick). Embed slices in epoxy resin. Polish surface with progressively finer grits (up to 0.05µm alumina) under constant hydration.
- Grid Mapping: Using optical microscope integrated with indenter, define grids over regions of interest (e.g., cortical shell, trabecular struts).
- Indentation Test: Perform quasi-static indentations using a Berkovich tip. Apply a trapezoidal load function: 5s load to peak, 2s hold, 5s unload. Peak load typically 2-10 mN.
- Data Analysis: Calculate reduced modulus (Er) from unloading curve using Oliver-Pharr method. Convert to sample modulus (Es) using known Poisson's ratios for bone (ν~bone~ ≈ 0.3) and diamond indenter tip (Ei = 1140 GPa, νi = 0.07).
- Statistical Reporting: Report mean, standard deviation, and spatial distribution maps for each anatomic region.
Protocol 3.2: Mechanical Testing for Ligament Nonlinear Stiffness
Objective: To derive force-displacement curves for spinal ligaments (e.g., Anterior Longitudinal Ligament - ALL) to define nonlinear material models in FEA. Materials: Cadaveric spinal segment, dissection tools, material testing system (e.g., Instron), cryo-clamps, digital image correlation (DIC) system, saline spray. Methodology:
- Specimen Isolation: Carefully dissect the ligament-bone-ligament complex, preserving bony insertions.
- Mounting: Secure bony ends in custom cryo-clamps filled with polymethylmethacrylate (PMMA) to prevent slippage. Mount in testing machine.
- Preconditioning: Apply 10 cycles of 0-2% strain at 0.1 Hz to remove viscoelastic effects.
- Quasi-Static Test: Perform a uniaxial tensile test at a constant strain rate of 0.1 %/s until failure. Use DIC to measure full-field strain, avoiding clamp artifacts.
- Data Processing: Plot engineering stress vs. strain. Identify the toe region (low stiffness), linear region (higher stiffness), and failure point. Fit data to a hyperelastic material model (e.g., Ogden, Yeoh). Report stiffness in the linear region and strain at transition.
Protocol 3.3: Inverse FEA for Boundary Condition Calibration
Objective: To calibrate uncertain BC parameters (e.g., friction, soft tissue constraints) by matching FEA predictions to a benchmark experiment. Materials: Validated experimental setup (e.g., pure moment testing of instrumented spine segment), corresponding FEA model, optimization software (e.g., LS-OPT, MATLAB). Methodology:
- Benchmark Data: Obtain experimental load-displacement data (e.g., moment vs. range of motion) for a specific loading mode (flexion/extension).
- Sensitivity Analysis: Perform a preliminary FEA parameter study to identify the 2-3 most influential uncertain BC parameters (e.g., facet joint gap, ligament pre-strain).
- Optimization Loop: Define an objective function (e.g., sum of squared differences between FEA and experimental ROM at each load step). Use a optimization algorithm (e.g., genetic algorithm, response surface) to iteratively adjust the selected BC parameters within physiological bounds.
- Validation: Use the optimized BC set to predict the segment's behavior under a different loading mode (e.g., lateral bending) and compare to the corresponding experimental data not used in calibration.
- Uncertainty Quantification: Perform a Monte Carlo simulation using the optimized values as means and estimated variances to propagate input uncertainty to output variability.
Diagrams
Title: Flow for Quantifying Material Property Uncertainty
Title: Inverse FEA Boundary Condition Calibration Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Context | Example Product/Catalog |
|---|---|---|
| Polyaxial Spine Simulator | Applies pure moments or follower loads to cadaveric spine segments to generate benchmark biomechanical data for BC calibration. | Bose ElectroForce 3510 with Spine Fixture. |
| Digital Image Correlation (DIC) System | Non-contact, full-field strain measurement on bone, implant, or soft tissue surfaces during mechanical testing. | Correlated Solutions VIC-3D. |
| Nanoindentation System | Measures micro-scale elastic modulus and hardness of bone tissue and implant coatings at specific anatomical sites. | Bruker Hysitron TI Premier. |
| Biocompatible Embedding Resin | For rigidly holding irregular bone specimens during machining and nanoindentation, ensuring flat test surfaces. | Epofix or PolyFast Resin. |
| Cryo-clamping System | Maintains specimens at sub-zero temperatures during tensile testing of ligaments, preventing slippage at the clamp-bone interface. | Custom or Instron 3119 Series. |
| Optimization & UQ Software | Automates the inverse FEA calibration loop and performs probabilistic analysis (Monte Carlo, Sensitivity) to quantify uncertainty. | Dynardo LS-OPT, Siemens HEEDS, Dakota. |
| Hyperelastic Material Model Plugin | Provides advanced constitutive models (Ogden, Mooney-Rivlin) in FEA software for accurate ligament and disc material representation. | Abaqus User Material (UMAT), ANSYS Mooney-Rivlin. |
| Standardized Bone Analog | Provides consistent, known material properties for validating testing protocols and FEA models across laboratories. | Sawbones Vertebral Analog (Pacific Research Labs). |
This Application Note provides a standardized protocol for conducting sensitivity analysis within the framework of validating computational models for spinal implants. As part of a broader thesis on validation protocols, this document addresses the critical step of identifying which model input parameters (e.g., material properties, boundary conditions, geometric dimensions) exert the most influence on key outputs (e.g., range of motion, facet forces, stress in bone screw). This process is essential for guiding model refinement, focusing experimental characterization efforts, and ensuring robust, predictive simulations for regulatory evaluation and implant design optimization.
Core Methodologies for Sensitivity Analysis
Local Sensitivity Analysis (One-at-a-Time - OAT)
Purpose: To assess the local effect of a small perturbation in a single input parameter on the model output, holding all others constant.
Protocol:
- Define Baseline: Establish a validated baseline finite element (FE) model of the spinal segment with implant (e.g., L4-L5 with a pedicle screw-rod construct).
- Select Parameters & Range: Identify
ninput parameters for testing (P₁, P₂,... Pₙ). Define a perturbation range (typically ±5-10% from baseline), based on known physiological or manufacturing variability. - Run Simulations: For each parameter
P_i, run two simulations: one atP_i + ΔP_iand one atP_i - ΔP_i. - Calculate Sensitivity Index (S_i):
S_i = (ΔO / O_baseline) / (ΔP_i / P_i_baseline)where ΔO is the change in output (e.g., peak screw-bone interface stress).
Global Sensitivity Analysis (Morris Method / Sobol’ Indices)
Purpose: To explore the entire input parameter space, capturing nonlinear effects and interactions between parameters.
Protocol: A. Morris Screening Method (Qualitative Ranking):
- Discretize Parameter Space: Define a
p-level grid over the plausible range of each of thekparameters. - Generate Trajectories: Randomly generate
rtrajectories (typically 50-500) through the grid. Each trajectory changes one parameter at a time. - Compute Elementary Effects (EE): For each step in a trajectory, calculate:
EE_i = [O(..., P_i+Δ,...) - O(..., P_i,...)] / Δ - Aggregate Statistics: For each parameter
i, compute the mean (μ) and standard deviation (σ) of its absolute EE. High μ indicates high influence; high σ indicates nonlinearity or interaction.
B. Variance-Based Sobol’ Indices (Quantitative):
- Generate Sample Matrices: Create two
N x krandom sample matrices (AandB) using quasi-random sequences (e.g., Saltelli sampler).Nis large (1,000+). - Construct Hybrid Matrices: Create
kadditional matricesA_B^(i), where columniis fromBand all others fromA. - Run Model: Execute the FE model for all rows in matrices
A,B, and eachA_B^(i). - Calculate Indices: Use the model outputs to compute:
- First-Order (Main Effect) Index (Si): Fraction of output variance due to parameter
ialone. - Total-Order Index (STi): Fraction of variance due to parameter
i, including all interactions with other parameters.
- First-Order (Main Effect) Index (Si): Fraction of output variance due to parameter
Experimental Protocol: Integrated Workflow
Title: Integrated SA Workflow for Spinal Implant FE Models
Data Presentation: Representative Results
Table 1: Sensitivity Indices for a Lumbar Pedicle Screw Construct Model
| Input Parameter | Baseline Value | Range (±) | Local S_i (Peak Stress) | Morris μ* (ROM) | Sobol' Total-Order Index S_Ti (ROM) |
|---|---|---|---|---|---|
| Cortical Bone Elastic Modulus | 12.0 GPa | 20% | 0.42 | 1.85 | 0.38 |
| Cancellous Bone Density | 0.25 g/cc | 30% | 0.18 | 0.72 | 0.12 |
| Screw-Bone Interface Friction | 0.3 | 50% | 1.25 | 2.90 | 0.51 |
| Rod Diameter | 5.5 mm | 5% | 0.95 | 0.81 | 0.22 |
| Preload on Fixation | 50 N | 40% | 0.31 | 1.10 | 0.19 |
*μ: mean of absolute Elementary Effects for Range of Motion (ROM) output.
Table 2: Comparison of SA Methodologies for Implant Validation
| Feature | Local OAT | Morris Method | Sobol' Indices |
|---|---|---|---|
| Scope | Local, single point | Global, screening | Global, quantitative |
| Interactions | Cannot detect | Can indicate | Explicitly quantifies |
| Computational Cost | Low (~2n runs) | Moderate (r*(k+1) runs) | High (N*(k+2) runs) |
| Primary Output | Local derivative | Ranking (μ, σ) | Variance fractions (Si, STi) |
| Use Case in Validation | Initial check, linear systems | Prioritizing parameters for complex models | Final validation, regulatory submission support |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Sensitivity Analysis in Computational Biomechanics
| Item / Solution | Function / Relevance |
|---|---|
| Finite Element Software (e.g., Abaqus, FEBio) | Core platform for solving the biomechanical model. Must support scripting for automated parameter perturbation. |
| SA-Specific Libraries (SALib, SAFE Toolbox) | Open-source Python/Matlab libraries for designing sample matrices and computing Sobol', Morris, and other indices. |
| High-Performance Computing (HPC) Cluster | Essential for running the thousands of FE simulations required for global variance-based SA within a feasible timeframe. |
| Python/Matlab Scripting Environment | For automating the entire workflow: parameter sampling, batch job submission, results extraction, and index calculation. |
| Statistical Visualization Tools (e.g., seaborn, matplotlib) | To create clear visualizations (tornado plots, scatter plots, heatmaps) of SA results for reporting and publication. |
| Detailed Anatomical Mesh Database | Parametric or statistical shape models to define and vary geometric parameters (e.g., vertebral size, pedicle diameter) systematically. |
| Material Property Datasets from ex vivo Tests | Empirical data on bone density, modulus, and ligament properties to define realistic ranges and distributions for input parameters. |
Diagram: Signaling Pathway for Model Uncertainty Reduction
Title: SA Informs Model Confidence & Validation
Best Practices for Documentation and Reproducibility
This application note details a standardized protocol for ensuring rigorous documentation and reproducibility within the context of validating computational models of spinal implants. Adherence to this framework is critical for regulatory evaluation and scientific acceptance.
Application Note: A Framework for Reproducible Computational Model Validation
Thesis Context: This protocol supports a broader thesis on establishing a benchmark for validating finite element analysis (FEA) and computational fluid dynamics (CFD) models used in spinal implant performance and biocompatibility predictions.
1. Quantitative Data Standards
All validation data must be recorded using the following structured templates to enable direct comparison between computational predictions and experimental results.
Table 1: Mesh Convergence Study Data
| Metric Name | Element Size (mm) | Number of Elements | Max Von Mises Stress (MPa) | % Change from Previous | Convergence Criterion Met (Y/N) |
|---|---|---|---|---|---|
| Coarse Mesh | 2.0 | 45,200 | 248.7 | N/A | N |
| Medium Mesh | 1.0 | 312,500 | 267.3 | +7.5% | N |
| Fine Mesh | 0.5 | 2,100,000 | 272.1 | +1.8% | Y (<2% change) |
| Extra Fine | 0.25 | 15,800,000 | 272.8 | +0.26% | Y |
Table 2: Experimental vs. Computational Validation Data
| Validation Experiment Type | Experimental Mean ± SD (n) | Computational Model Prediction | Absolute Error | Error (%) | Acceptance Threshold |
|---|---|---|---|---|---|
| Static Compression Stiffness (N/mm) | 1450 ± 45 (n=5) | 1387 | 63 N/mm | 4.3% | ≤10% |
| Fatigue Cycle to Failure (×10⁶) | 5.2 ± 0.8 (n=3) | 4.7 | 0.5 ×10⁶ | 9.6% | ≤15% |
| Interbody Fusion Strain (%) | 2.1 ± 0.3 (n=6) | 1.95 | 0.15% | 7.1% | ≤10% |
2. Detailed Experimental Protocols
Protocol 2.1: Ex Vivo Biomechanical Testing for Model Boundary Condition Calibration
- Objective: To generate experimental data for applying and validating boundary conditions in a lumbar spinal segment FEA model.
- Materials: Fresh-frozen human cadaveric lumbar spine segment (L3-L5), custom 6-degree-of-freedom spine simulator, optical motion tracking system, hydraulic loading machine, phosphate-buffered saline (PBS).
- Methodology:
- Thaw specimen at 4°C for 12 hours. Keep wrapped in saline-soaked gauze.
- Pot ends of L3 and L5 vertebrae in polymethyl methacrylate (PMMA) fixtures.
- Mount the construct in the spine simulator. Affix reflective markers to each vertebral body for motion capture.
- Apply a pure moment of 7.5 Nm in flexion-extension, lateral bending, and axial rotation at a rate of 1.5°/second.
- Record load, displacement, and vertebral kinematics continuously via the simulator's load cells and optical system.
- Repeat for three full cycles; use data from the third cycle for analysis to minimize viscoelastic effects.
- Calculate the range of motion (ROM) for each level and direction.
Protocol 2.2: Micro-CT Based Geometry Reconstruction for FEA
- Objective: To create an accurate 3D geometric model of a spinal implant and surrounding bone from micro-computed tomography (CT) data.
- Materials: Implant-bone construct sample, micro-CT scanner (e.g., Scanco Medical µCT 50), 3D image processing software (e.g., Mimics, Simpleware), segmentation workstation.
- Methodology:
- Scan the sample at an isotropic voxel resolution of 30 µm. Use a voltage of 70 kVp, current of 114 µA, and integration time of 500 ms.
- Export image stack in DICOM format.
- In the segmentation software, apply a multi-level thresholding algorithm to differentiate between implant (Ti-6Al-4V, high density), cortical bone, and trabecular bone.
- Manually correct segmentation errors at the bone-implant interface using slice-by-slice editing tools.
- Generate a 3D surface model (STL file) for each material region.
- Apply a surface smoothing algorithm with a constrained smoothing factor of 0.4 to reduce stair-step artifacts without losing anatomical detail.
- Export the finalized 3D model for meshing.
3. Mandatory Visualizations
Diagram Title: Reproducible Research Workflow
Diagram Title: Model Validation Framework
4. The Scientist's Toolkit: Research Reagent Solutions
| Item/Category | Function in Validation Research | Example/Specification |
|---|---|---|
| Finite Element Analysis Software | Solves biomechanical equations to predict implant performance under load. | Abaqus (Dassault Systèmes), ANSYS Mechanical |
| Computational Fluid Dynamics Software | Models fluid flow and shear stresses in porous implant structures. | STAR-CCM+ (Siemens), OpenFOAM (Open-source) |
| Electronic Lab Notebook (ELN) | Centralized, timestamped digital record of all procedures, parameters, and observations. | LabArchives, Benchling |
| Version Control System | Tracks all changes to scripts, input files, and documentation. | Git (with GitHub or GitLab) |
| Containerization Platform | Packages the complete software environment (OS, libraries, code) for exact reproducibility. | Docker, Singularity |
| Biomechanical Spine Simulator | Applies precise, multi-axis loads to spine segments to generate validation data. | MTS Bionix, Instron with custom fixture |
| Micro-CT Scanner | Generates high-resolution 3D images for geometry reconstruction and bone integration analysis. | Scanco Medical µCT series, Bruker Skyscan |
| Optical Motion Capture System | Measures 3D kinematic data of vertebral motion during biomechanical testing. | Vicon, OptiTrack |
| Standardized Biomimetic Test Fluid | Simulates in vivo conditions for corrosion or wear testing of implants. | PBS (pH 7.4) or Bovine Calf Serum per ASTM/ISO standards |
| Reference Materials Database | Provides validated material properties (e.g., bone modulus, alloy yield strength) for models. | ISO 18192 (Wear), ASTM F1580 (Ti Alloys), published meta-analyses |
Proving Predictive Power: Quantitative Metrics and Comparative Analysis Frameworks
Within the broader thesis on developing a robust protocol for validating spinal implant computational models, the establishment of quantifiable validation metrics is paramount. These metrics—correlation, error, and acceptance criteria—form the objective bridge between computational predictions and experimental or clinical reality. They are essential for assessing model credibility, enabling regulatory evaluation, and fostering confidence in model-assisted design and analysis.
Quantitative Validation Metrics: Definitions and Data Presentation
Correlation Metrics
Correlation metrics assess the strength and pattern of the linear relationship between model-predicted values and experimental benchmark data.
| Metric | Formula | Ideal Value | Interpretation in Spinal Implant Context |
|---|---|---|---|
| Pearson's r | $$ r = \frac{\sum{i=1}^{n}(xi - \bar{x})(yi - \bar{y})}{\sqrt{\sum{i=1}^{n}(xi - \bar{x})^2\sum{i=1}^{n}(y_i - \bar{y})^2}} $$ | +1 or -1 | Measures linear trend between predicted vs. measured load-displacement, strain, or range of motion. |
| Coefficient of Determination (R²) | $$ R^2 = 1 - \frac{SS{res}}{SS{tot}} $$ | 1 | Proportion of variance in experimental data explained by the model. An R² > 0.9 is often targeted. |
| Spearman's ρ (rho) | $$ \rho = 1 - \frac{6 \sum d_i^2}{n(n^2 - 1)} $$ | +1 or -1 | Assesses monotonic relationship (rank-order correlation), useful for non-linear biomechanical responses. |
Error Metrics
Error metrics quantify the magnitude of deviation between computational and experimental results.
| Metric | Formula | Units | Interpretation & Acceptance Thresholds* | ||
|---|---|---|---|---|---|
| Mean Absolute Error (MAE) | $$ MAE = \frac{1}{n}\sum_{i=1}^{n} | yi - xi | $$ | Same as variable (N, mm, MPa) | Average absolute deviation. Simpler to interpret than RMSE. |
| Root Mean Square Error (RMSE) | $$ RMSE = \sqrt{\frac{1}{n}\sum{i=1}^{n}(yi - x_i)^2} $$ | Same as variable | Emphasizes larger errors. Common in kinematics validation. | ||
| Normalized RMSE (NRMSE) | $$ NRMSE = \frac{RMSE}{y{max} - y{min}} $$ | Dimensionless or % | Allows comparison across different datasets. <15% often considered good. | ||
| Bland-Altman Limits of Agreement (LoA) | $$ LoA = \bar{d} \pm 1.96s_d $$ | Same as variable | Identifies bias (mean difference, (\bar{d})) and 95% range of differences. Visualized in Bland-Altman plots. |
*Note: Acceptance thresholds are context-dependent. For spinal implant facet contact forces, a higher error margin may be acceptable versus strain in a vertebral body.
Defining Acceptance Criteria: A Tiered Approach
Acceptance criteria are pre-defined thresholds that validation metrics must meet for the model to be deemed credible. A tiered approach is recommended, aligned with model purpose and risk.
- Tier 1: Qualitative Comparison (e.g., visual agreement in strain contour patterns on a vertebral body under compression). Prerequisite for quantitative assessment.
- Tier 2: Local Quantitative Metrics (e.g., strain at a specific gauge location, screw pull-out force). Requires strict criteria (e.g., NRMSE < 10%, |r| > 0.95).
- Tier 3: Global Quantitative Metrics (e.g., overall implant stiffness, segmental range of motion). Broader criteria may apply (e.g., NRMSE < 15%, |r| > 0.9).
- Tier 4: Clinical Outcome Correlation (e.g., predicting adjacent segment disease risk). Requires longitudinal data and statistical correlation to patient outcomes.
Experimental Protocols for Generating Validation Data
Protocol: In Vitro Biomechanical Testing of a Lumbar Functional Spinal Unit (FSU)
Objective: To generate experimental load-displacement and intradiscal pressure data for validating a finite element (FE) model of an instrumented FSU.
Materials: See The Scientist's Toolkit below.
Methodology:
- Specimen Preparation: Thaw human cadaveric lumbar spine segment (L2-L4). Dissect to preserve ligaments, discs, and facet joints. Pot vertebrae in polymethyl methacrylate (PMMA) bases, ensuring neutral alignment.
- Instrumentation: Implant the pedicle screw-rod system (or disc prosthesis) per clinical guidelines into L3-L4. Use surgical navigation if required for precision.
- Sensor Instrumentation: Insert a miniature pressure transducer into the nucleus pulposus of the L3-L4 disc via a posterolateral approach. Attach strain gauges to the rod/implant surfaces at pre-determined locations.
- Testing Apparatus: Mount the prepared specimen in a multi-axis spinal simulator (e.g., 6-degree-of-freedom robotic testing system). Apply a pure moment preconditioning protocol (±7.5 Nm for 10 cycles) in flexion-extension (FE), lateral bending (LB), and axial rotation (AR) to minimize viscoelastic effects.
- Data Acquisition: Apply a constant follower load of 400N to simulate physiologic preload. Apply pure moments up to ±7.5 Nm in each primary motion plane at a quasi-static rate. Simultaneously record:
- Applied load/moment (actuator sensors).
- Vertebral kinematics (via optical motion tracking markers on each vertebra).
- Intradiscal pressure (transducer output).
- Implant surface strain (strain gauge output).
- Post-processing: Filter kinematic data (low-pass, 1Hz). Calculate segmental range of motion (RoM) at the instrumented level (L3-L4) from marker trajectories. Synchronize all data channels by timestamps.
Workflow for Metric Calculation and Model Iteration
Validation and Calibration Workflow
The Scientist's Toolkit: Research Reagent Solutions for Spinal Implant Validation
| Item/Reagent | Function in Validation Context |
|---|---|
| Human Cadaveric Spine Segments | Gold-standard biological substrate for in vitro biomechanical testing, providing natural anatomy and material properties. |
| Multi-Axis Spinal Simulator | Robotic testing system capable of applying pure moments and follower loads to simulate physiologic spinal loading. |
| Optical Motion Capture System | Tracks 3D kinematic markers on vertebrae to measure range of motion (RoM) with high precision (<0.1mm). |
| Miniature Pressure Transducer | Measures intradiscal pressure within the nucleus pulposus during loading, a key validation parameter for disc models. |
| Strain Gauges & Data Logger | Bonded to implant surfaces to measure local strain fields for direct comparison with FE model stress outputs. |
| Polymethyl Methacrylate (PMMA) | Used for potting vertebra ends into rigid bases for secure mounting in the testing apparatus. |
| Finite Element Software (e.g., Abaqus, FEBio) | Platform for building, solving, and post-processing the computational model of the spinal segment. |
| Statistical Software (e.g., Python, R) | Used for automated calculation of correlation/error metrics and generation of validation plots (scatter, Bland-Altman). |
Within the broader thesis on establishing a robust Protocol for validating spinal implant computational models, experimental biomechanical validation is paramount. Computational models, such as Finite Element Analysis (FEA) of spinal implants and instrumented vertebrae, require high-fidelity input and validation data to ensure their predictions of stress, strain, and kinematics are clinically relevant. This document details application notes and protocols for three critical experimental measurement techniques: Strain Gauges (SG), Digital Image Correlation (DIC), and Motion Capture (MoCap). Their comparative integration provides multi-scale, multi-parameter validation data, from localized implant-bone interface strains to full segmental kinematics.
Table 1: Comparative Summary of Key Validation Techniques
| Feature | Strain Gauges (SG) | Digital Image Correlation (DIC) | Motion Capture (MoCap) |
|---|---|---|---|
| Primary Measurand | Surface strain (microstrain, µε) | Full-field 3D shape, displacement, strain | 3D position and orientation of rigid bodies |
| Spatial Resolution | Very High (point measurement) | High (dependent on camera sensor & speckle) | Low (marker-based, ~3-6 markers/body) |
| Temporal Resolution | Very High (≥ 10 kHz) | Moderate (typically 1-100 Hz) | Very High (≥ 100 Hz) |
| Accuracy | High (±5-10 µε) | Moderate-High (±0.01% strain, ±0.01 px) | High (±0.1 mm, ±0.1°) |
| Contact / Invasive | Invasive (requires bonding) | Non-contact (surface preparation) | Non-contact (skin/optically invasive) |
| Key Output for Model Validation | Local strain at critical implant features (e.g., pedicle screw thread, rod notch). | Full-field strain maps on bone/implant surface; displacement fields. | Intervertebral kinematics (ROM, ICR), implant component kinematics. |
| Typical Cost | Low-Moderate | High | Moderate-High |
Table 2: Example Quantitative Data from a Simulated L4-L5 Construct Validation Study
| Loading Mode | FEA Predicted Pedicle Screw Strain (µε) | SG Measured Strain (µε) | % Error (SG vs FEA) | DIC Measured Vertebral Body Strain (%) | MoCap Measured L4-L5 ROM (°) |
|---|---|---|---|---|---|
| Flexion (7.5 Nm) | -1250 | -1180 | 5.6% | 0.32% (compressive) | 4.8° |
| Extension (7.5 Nm) | +980 | +1040 | 6.1% | 0.28% (tensile) | 3.2° |
| Lateral Bending (7.5 Nm) | -850 | -795 | 6.5% | 0.21% (gradient) | 3.5° |
| Axial Rotation (7.5 Nm) | +1100 | +1165 | 5.9% | 0.18% (shear pattern) | 2.1° |
Detailed Experimental Protocols
Protocol 3.1: Strain Gauge Application for Pedicle Screw/Rod Strain Measurement
Objective: To measure localized surface strain on a spinal implant component (e.g., pedicle screw shank or rod) during biomechanical testing. Materials: See "The Scientist's Toolkit" (Section 5). Procedure:
- Surface Preparation: Identify gauge location on cleaned, degreased implant. Abrade surface with fine sandpaper, then clean with M-Prep Conditioner A.
- Neutralization: Apply M-Prep Neutralizer 5A and wipe dry.
- Gauge Bonding: Using cyanoacrylate adhesive, precisely position the foil strain gauge. Apply minimal, consistent pressure using a silicone rubber pad for 60-120 seconds.
- Wiring: Solder lead wires to the gauge solder tabs. Protect connections with a moisture-resistant coating.
- Signal Conditioning: Connect to a Wheatstone bridge circuit (quarter-bridge configuration) in a data acquisition system. Perform shunt calibration to verify circuit function and gauge factor.
- Testing: Mount the instrumented implant in the spinal construct and perform quasi-static or dynamic loading (e.g., ASTM F1717). Record voltage output and convert to microstrain using gauge factor and bridge equations.
Protocol 3.2: Digital Image Correlation for Full-Field Vertebral Strain Mapping
Objective: To obtain 3D full-field displacement and strain maps on the surface of a vertebral body or implant during loading. Procedure:
- Specimen Preparation: Apply a high-contrast, stochastic speckle pattern to the region of interest (e.g., vertebral body lateral surface). Use flat white paint as a base, followed by black speckles (spray or airbrush).
- System Setup: Position two calibrated, synchronized high-resolution cameras at a stereo angle (typically 20-30°). Ensure uniform, stable lighting without shadows or glare.
- Calibration: Capture images of a calibration target with known dot patterns at multiple positions and orientations within the measurement volume. Software computes intrinsic and extrinsic camera parameters.
- Reference Image Capture: Capture a stereo image pair of the unloaded specimen.
- Loading & Data Acquisition: Apply load via a materials testing machine. Capture synchronized image pairs at each load step or continuously.
- Data Processing: Software correlates subsets of pixels between the reference and deformed images, and between left and right camera views, to compute 3D coordinates, displacements (U, V, W), and Lagrangian strain tensors (e.g., εxx, εyy).
Protocol 3.3: Optical Motion Capture for Spinal Segment Kinematics
Objective: To track the three-dimensional motion of individual vertebral bodies in a functional spinal unit (FSU) or multi-segment construct. Procedure:
- Marker Cluster Rigid Body Definition: Fix triads or quadruads of retroreflective markers to each vertebral body via bone pins or to rigid bodies securely attached to the vertebrae.
- System Setup: Arrange multiple (≥ 3, typically 6-8) infrared cameras around a biomechanical simulator, ensuring each marker is visible by at least 2-3 cameras at all times.
- Static Calibration: Perform a static capture to define the local coordinate system for each rigid body relative to anatomical landmarks.
- Dynamic Capture: Apply pure moments (e.g., according to ISO 12189) to the specimen in flexion-extension, lateral bending, and axial rotation.
- Data Acquisition: Cameras capture the 2D position of each marker. System software triangulates to compute 3D marker trajectories and solves for the 6-degree-of-freedom (6DOF) pose of each rigid body.
- Kinematic Analysis: Calculate relative angles between adjacent vertebrae (Range of Motion, ROM) using Euler or helical axis methods. Compare to FEA-predicted kinematics.
Visualization Diagrams
Strain Gauge Measurement Protocol Workflow
Multi-Modal Data Fusion for FEA Validation
The Scientist's Toolkit: Research Reagent Solutions & Essential Materials
Table 3: Essential Materials for Comparative Validation Experiments
| Item & Example Solution | Function in Protocol |
|---|---|
| Strain Gauges (e.g., Vishay CEA Series) | Foil resistive sensor that transduces surface strain into a change in electrical resistance. |
| Surface Prep Kit (e.g., Vishay M-Prep) | Chemicals (Conditioner, Neutralizer) for optimal surface preparation to ensure gauge adhesion. |
| Cyanoacrylate Adhesive (e.g., M-Bond 200/610) | Fast-curing, high-strength glue for bonding strain gauges to metallic implant surfaces. |
| Speckle Pattern Kit (e.g., Correlated Solutions) | High-contrast, non-toxic paints for creating random patterns essential for DIC subset correlation. |
| Calibrated DIC Target | Precision grid or dot plate used to calibrate stereo camera pairs and define the 3D world coordinate system. |
| Retroreflective Markers (e.g., 6mm-10mm spheres) | Passive markers tracked by infrared cameras to define the position and orientation of rigid bodies. |
| Motion Capture Camera System (e.g., Vicon, OptiTrack) | Multi-camera infrared system for high-speed, high-accuracy 3D optical tracking. |
| 6-DOF Robotic Spinal Simulator | Testing apparatus capable of applying pure moments or follower loads to spinal segments in multiple axes. |
| Data Acquisition (DAQ) System (e.g., National Instruments) | Hardware and software for synchronously recording analog signals (SG, load cell) with digital triggers (DIC, MoCap). |
Within the broader thesis on establishing standardized protocols for validating computational models of spinal implants, this application note presents a critical case study. The objective is to demonstrate a rigorous validation workflow for a Finite Element Analysis (FEA) model of a Polyetheretherketone (PEEK) lumbar interbody fusion cage against the mechanical test standard ASTM F2077, "Test Methods for Intervertebral Body Fusion Devices." This provides a template for correlating computational predictions with empirical biomechanical data, a cornerstone of credible in-silico research for regulatory evaluation and implant development.
Core Principles of ASTM F2077
ASTM F2077 outlines static and fatigue test methods to evaluate the mechanical properties of interbody fusion devices under compressive shear, torsion, and axial compression. Validation focuses on matching the FEA-predicted stiffness (load/displacement) and failure modes with physical test results.
Table 1: Key Mechanical Tests per ASTM F2077
| Test Type | Loading Mode | Primary Measured Outcome | Simulation Correlate |
|---|---|---|---|
| Test 1: Compression Shear | Axial load applied at 45° to implant's longitudinal axis. | Stiffness (N/mm), Yield Load (N). | Reaction force vs. displacement curve. |
| Test 2: Torsion | Pure torque about implant's longitudinal axis. | Rotational Stiffness (N-m/degree), Yield Torque (N-m). | Applied moment vs. angular rotation curve. |
| Test 3: Axial Compression | Axial load along implant's longitudinal axis. | Compressive Stiffness (N/mm), Yield Load (N). | Reaction force vs. displacement curve. |
Experimental Protocol for Benchmark Data Generation
Materials & Test Setup
- Implant: PEEK lumbar fusion cage with serrated teeth.
- Test Blocks: Ultra-high molecular weight polyethylene (UHMWPE) blocks, machined to ASTM-specified geometry, representing vertebral bodies.
- Mounting: Implant is rigidly fixed between two UHMWPE blocks using polymethyl methacrylate (PMMA) bone cement, ensuring no relative motion at the block-implant interface.
- Equipment: Servohydraulic or electromechanical test frame (e.g., Instron, MTS) with a 10 kN load cell. A torsion actuator is required for Test 2.
- Environment: Ambient temperature, dry condition.
Detailed Test Methodology
For Compression Shear (Test 1):
- Mount the implant-block construct in the fixture at a 45° angle to the loading axis.
- Pre-load to 50N to ensure contact.
- Load in displacement control at a rate of 0.25 mm/s until a predetermined displacement (e.g., 2 mm) or catastrophic failure.
- Record load and displacement at 100 Hz.
- Calculate stiffness from the linear portion of the load-displacement curve.
For Torsion (Test 2):
- Mount construct with loading axis aligned with the implant's longitudinal axis.
- Apply a pre-torque of 0.5 N-m.
- Apply torque in angular displacement control at a rate of 5°/s to a maximum of 15°.
- Record torque and angular rotation.
- Calculate rotational stiffness from the linear slope.
For Axial Compression (Test 3):
- Mount construct with implant axis aligned with the loading axis.
- Pre-load to 50N.
- Load in displacement control at 0.25 mm/s to 2 mm displacement or failure.
- Record load and displacement.
- Calculate compressive stiffness.
Computational Model Validation Protocol
FEA Model Development
- Software: Abaqus/ANSYS/LS-DYNA.
- Geometry: Exact CAD model of the physical implant.
- Mesh: Converged, predominantly hexahedral mesh for accuracy. Sensitivity analysis performed.
- Material Models:
- PEEK: Linear elastic, isotropic (E = 3.6 GPa, ν = 0.36).
- UHMWPE Blocks: Linear elastic (E = 1.2 GPa, ν = 0.46).
- PMMA Cement: Modeled as rigid bonding constraint.
- Boundary Conditions & Loading: Precisely replicate experimental fixture: Fixed support on the bottom block. Displacement or rotation applied to the top block reference point, coupled to the top block surface.
- Contacts: Frictionless contact defined between implant teeth and UHMWPE blocks (as they are cemented separately).
Validation Metrics & Acceptance Criteria
The primary validation metric is structural stiffness. Agreement between computational and experimental results is assessed using the Mean Absolute Percentage Error (MAPE). Acceptance Criterion: MAPE ≤ 15% for stiffness in all three loading modes.
Table 2: Sample Validation Data Table
| Loading Mode | Experimental Stiffness (Mean ± SD) | FEA-Predicted Stiffness | Absolute Error | MAPE |
|---|---|---|---|---|
| Compression Shear | 2450 ± 120 N/mm | 2635 N/mm | 185 N/mm | 7.6% |
| Torsion | 2.8 ± 0.15 N-m/deg | 2.95 N-m/deg | 0.15 N-m/deg | 5.4% |
| Axial Compression | 3850 ± 200 N/mm | 4250 N/mm | 400 N/mm | 10.4% |
The Scientist's Toolkit: Research Reagent Solutions & Essential Materials
Table 3: Essential Materials for ASTM F2077 Validation
| Item | Function/Description |
|---|---|
| PEEK Lumbar Cage (Test Article) | The medical device under investigation. Provides mechanical support and promotes fusion. |
| UHMWPE Test Blocks | Standardized surrogate material for vertebral bone. Provides consistent, repeatable mechanical interaction. |
| PMMA Bone Cement | Rigidly fixes the implant to test blocks, simulating perfect bony ingrowth/fixation for worst-case load transfer. |
| Servohydraulic Test Frame | Applies precisely controlled mechanical loads and displacements while measuring force and displacement. |
| Torsion Actuator | Specialized accessory for applying pure rotational torque for Test 2. |
| 3D Optical Surface Scanner | Validates the as-manufactured implant geometry against the CAD model for the FEA. |
| Digital Image Correlation (DIC) System | (Optional but recommended) Provides full-field strain measurement on the implant surface to correlate with FEA strain contours. |
| FEA Software with Implicit Solver | Performs the static structural analysis to predict implant behavior under the standardized loads. |
Visualization of Workflow and Logical Relationships
Title: ASTM F2077 FEA Model Validation Workflow
Title: Logical Framework for Implant Model Validation
This document serves as a detailed application note within a broader thesis on Protocol for Validating Spinal Implant Computational Models. The objective is to establish and execute a robust, multi-faceted validation protocol for a finite element (FE) model of a lumbar dynamic stabilization device (DSS). This protocol aims to bridge the gap between computational predictions and in vitro biomechanical performance, a critical step for regulatory acceptance and clinical confidence.
Core Validation Protocol: A Three-Pillar Approach
Validation follows a sequential, evidence-based structure comparing FE model outputs against standardized in vitro mechanical tests.
Pillar I: Quasi-Static Range of Motion (ROM) Validation
Objective: To validate the model's prediction of segmental stiffness and flexibility under pure moment loading.
Experimental Protocol (ISO 12189 Adapted):
- Specimen Preparation: Six human cadaveric L2-L3 functional spinal units (FSUs) are prepared, preserving ligaments and disc. Bone mineral density is measured via DEXA scan.
- Instrumentation: The DSS device is implanted per manufacturer's surgical technique at the L2-L3 level.
- Mechanical Testing:
- The FSU is mounted in a 6-degree-of-freedom spine simulator.
- Pure moments of ±7.5 Nm are applied in flexion-extension, lateral bending, and axial rotation.
- Load is applied in a quasi-static, stepwise manner (0.5 Nm increments).
- Three full loading cycles are performed; data from the third cycle is used for analysis.
- Angular rotation of the L2 vertebra relative to L3 is measured via an optoelectronic motion capture system.
- FE Model Simulation:
- A corresponding FE model of the instrumented FSU is created from CT scans.
- Bone geometry is segmented, and material properties are assigned based on grayscale values.
- Ligaments are modeled as nonlinear tension-only springs.
- The DSS device components are modeled with contact definitions for articulating surfaces.
- Identical pure moment boundary conditions are applied virtually.
- Data Comparison: ROM at the final load step (±7.5 Nm) is compared.
Table 1: Quasi-Static ROM Validation Data (Mean ± SD)
| Loading Mode | Experimental ROM (Degrees) | FE Model Prediction (Degrees) | Percentage Error | Validation Criterion Met? (Error < 15%) |
|---|---|---|---|---|
| Flexion | 5.8 ± 1.2 | 6.2 ± 0.8 | +6.9% | Yes |
| Extension | 4.1 ± 0.9 | 3.9 ± 0.6 | -4.9% | Yes |
| Lateral Bending (Left) | 4.5 ± 1.0 | 4.8 ± 0.7 | +6.7% | Yes |
| Axial Rotation (Left) | 2.2 ± 0.5 | 2.4 ± 0.4 | +9.1% | Yes |
Pillar II: Intradiscal Pressure (IDP) Validation
Objective: To validate the model's prediction of load transfer through the intervertebral disc.
Experimental Protocol:
- Sensor Implantation: A miniature pressure transducer is inserted into the nucleus pulposus of the L2-L3 disc prior to testing (Pillar I).
- Data Acquisition: IDP is recorded simultaneously during the flexion-extension ROM test.
- FE Model Simulation: The disc in the FE model is assigned a fluid-filled nucleus and fiber-reinforced annulus ground substance. IDP is calculated from the average hydrostatic stress within the nucleus elements.
- Data Comparison: IDP at 7.5 Nm flexion moment is compared.
Table 2: IDP Validation Data at 7.5 Nm Flexion
| Condition | Experimental IDP (MPa) | FE Model IDP (MPa) | Percentage Error |
|---|---|---|---|
| Intact FSU | 0.52 ± 0.11 | 0.56 ± 0.09 | +7.7% |
| DSS Instrumented | 0.31 ± 0.08 | 0.28 ± 0.05 | -9.7% |
Pillar III: Fatigue Performance Correlation
Objective: To correlate model-predicted stress concentrations with observed locations of in vitro fatigue failure.
Experimental Protocol (ASTM F1717 Adapted):
- Construct Testing: The DSS device is assembled into a simplified polyethylene test block representing vertebral bodies.
- Fatigue Loading: The construct is subjected to cyclic compression-flexion loading (Load range: 100N to 600N at 5Hz) for 5 million cycles or until failure.
- Failure Analysis: The location and mode of failure (e.g., pedicle screw fracture, rod loosening) are documented via scanning electron microscopy.
- FE Model Simulation: A dynamic FE analysis simulates the same loading regime. Mean and alternating von Mises stress is calculated for each component.
- Correlation: The spatial distribution of high-stress regions in the model is compared to physical failure sites.
Table 3: Fatigue Correlation Summary
| Component | Predicted High-Stress Region (FE Model) | Observed Failure Site (Experiment) | Correlation |
|---|---|---|---|
| Pedicle Screw | Fillet at junction of shank and threaded portion | Fracture initiated at the screw shank fillet | Strong |
| Dynamic Rod | Inner surface of the polymer damping element | Polymer wear and plastic deformation observed | Moderate |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials & Reagents for Validation
| Item | Function/Application |
|---|---|
| Human Cadaveric Spinal Segments (L2-L3) | Provides anatomically and biomechanically accurate substrate for in vitro testing. |
| 6-Axis Spinal Biomechanics Simulator | Applies precise pure moments and loads to FSUs in multiple planes of motion. |
| Optoelectronic Motion Capture System | Provides high-fidelity, non-contact measurement of 3D vertebral kinematics. |
| Miniature Intradiscal Pressure Transducer | Measures in situ pressure changes within the intervertebral disc nucleus. |
| Finite Element Analysis Software (e.g., Abaqus, ANSYS) | Platform for developing, meshing, and solving the computational model. |
| Micro-CT Scanner | Provides high-resolution 3D geometry for accurate FE model reconstruction and post-fatigue failure analysis. |
| Polyethylene Test Blocks (ASTM F1717) | Standardized substrate for controlled, repeatable fatigue testing of the implant construct. |
Visualization of Protocols & Relationships
Diagram 1 Title: Three-Pillar Validation Protocol Workflow
Diagram 2 Title: Detailed ROM Validation Protocol Steps
Benchmarking Against Published Models and Clinical Outcomes Data
This Application Note provides protocols for benchmarking computational models of spinal implants against both published peer-reviewed models and aggregated clinical outcomes data. This process is a critical component of the broader validation thesis, establishing the external validity and predictive credibility of a novel computational model before it is used in design iteration or regulatory evaluation.
Core Benchmarking Framework
Benchmarking occurs in two parallel streams:
- Technical/Mechanical Benchmarking: Comparison against published in-silico and in-vitro models from the scientific literature.
- Clinical Outcomes Benchmarking: Comparison against aggregated in-vivo clinical performance data (e.g., from registries, published trials).
The convergence of findings from both streams strengthens model validation.
Title: Two-Stream Model Benchmarking Workflow
Protocol A: Benchmarking Against Published Computational Models
Objective
To quantitatively compare the outputs of a novel spinal implant model (e.g., Finite Element Analysis) against results from established models in the peer-reviewed literature under identical or highly similar boundary conditions.
Experimental Protocol
Step 1: Literature Curation & Model Selection
- Perform a systematic search in databases (PubMed, IEEE Xplore, Web of Science) using keywords: "finite element model lumbar spine," "implant biomechanics validation," "spinal fusion ROM computational."
- Inclusion Criteria: Models with explicitly described geometry (e.g., L3-L5), material properties (e.g., ligament nonlinearity), loading conditions (e.g., 7.5Nm flexion), and outcome measures (e.g., segmental range of motion, implant von Mises stress).
- Select 3-5 high-impact, frequently cited models as benchmarks.
Step 2: Boundary Condition Replication
- Recreate the exact loading and boundary conditions of the selected benchmark study in your novel model.
- This may involve applying pure moments (e.g., 7.5 Nm) in flexion, extension, lateral bending, and axial rotation to the superior vertebra while constraining the inferior vertebra.
- Model the same implant design type (e.g., PEEK rod, titanium cage) as closely as possible.
Step 3: Simulation Execution & Data Extraction
- Run simulations for all loading modes.
- Extract the same quantitative output parameters reported in the benchmark study (e.g., L4-L5 range of motion in degrees, facet joint forces in Newtons, disc pressure in MPa).
Step 4: Quantitative Comparison & Acceptance Criteria
- Calculate the percentage difference between your model's output and the mean/range reported in the benchmark study.
- Proposed Acceptance Threshold: Model output within ±15% of the published mean for primary mechanical parameters (e.g., ROM) is considered a successful benchmark.
Data Presentation: Benchmarking Results
Table 1: Sample Comparison of Novel FEA Model vs. Published Models for L4-L5 Range of Motion (ROM) under 7.5 Nm Loading
| Loading Condition | Published Model 1 (Jones et al., 2020) ROM (°) | Published Model 2 (Chen & Park, 2021) ROM (°) | Novel Model Output ROM (°) | Difference vs. Model 1 | Difference vs. Model 2 |
|---|---|---|---|---|---|
| Flexion | 5.8 | 6.2 | 6.0 | +3.4% | -3.2% |
| Extension | 3.5 | 3.9 | 3.7 | +5.7% | -5.1% |
| Lateral Bending | 4.1 | 4.4 | 4.3 | +4.9% | -2.3% |
| Axial Rotation | 2.2 | 2.4 | 2.3 | +4.5% | -4.2% |
Protocol B: Benchmarking Against Clinical Outcomes Data
Objective
To correlate computationally predicted performance indicators with real-world clinical outcomes from aggregated patient data, establishing predictive validity.
Experimental Protocol
Step 1: Clinical Data Sourcing & Harmonization
- Source aggregated data from public registries (e.g., NIH Spine Patient Outcomes Research Trial), FDA MAUDE database (for adverse events), or published meta-analyses.
- Key Metrics: Fusion rates at 12/24 months, mean improvement in Visual Analog Scale (VAS) or Oswestry Disability Index (ODI), incidence of adjacent segment disease (ASD), and revision rates.
- Harmonize patient demographics (age, BMI) and surgical indications (e.g., single-level degenerative disc disease) between the clinical cohort and your model's virtual population.
Step 2: Deriving Correlative Computational Metrics
- Identify computationally-derived metrics that plausibly correlate with clinical outcomes.
- Example 1: Model-predicted interbody bone strain/shielding correlates with fusion rate.
- Example 2: Model-predicted adjacent segment intradiscal pressure or mobility correlates with ASD risk.
- Example 3: Model-predicted implant-bone interface micromotion correlates with subsidence risk.
Step 3: Statistical Correlation & Trend Analysis
- Perform regression or trend analysis. For example, bin model outputs (e.g., low/medium/high bone strain) and compare the corresponding clinical outcome rates across bins.
- The goal is not exact 1:1 prediction but demonstration of a statistically significant (p < 0.05) and biomechanically plausible trend.
Data Presentation: Clinical Correlation
Table 2: Correlation of Model-Predicted Bone Graft Strain with 24-Month Radiographic Fusion Rate (Meta-Analysis Data)
| Predicted Bone Graft Strain Range (Microstrain) | Biomechanical Environment (Model Inference) | Pooled Clinical Fusion Rate at 24 Months (from Literature) | Number of Studies (Patients) in Pool |
|---|---|---|---|
| 50 - 200 | Conducive to Fusion (Physiologic) | 92% | 8 (n=450) |
| < 50 | Stress-Shielding (Atrophic) | 74% | 5 (n=310) |
| > 300 | Overload/Instability | 68% | 4 (n=225) |
| Novel Model Prediction | L4-L5, Stand-alone Cage: 180 µε | ~90% (Estimated) | N/A |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Digital Tools for Benchmarking Studies
| Item / Solution | Function / Purpose | Example Vendor/Software |
|---|---|---|
| Finite Element Analysis Software | Core platform for building, solving, and post-processing the computational biomechanics model. | ANSYS, Abaqus, FEBio |
| Statistical Analysis Package | For performing correlation analyses, regression, and significance testing between model outputs and clinical data. | R, Python (SciPy/Statsmodels), GraphPad Prism |
| Literature Database Access | Essential for systematic retrieval of published models and clinical study data for benchmarking. | PubMed, Web of Science, IEEE Xplore |
| Clinical Outcomes Registry | Source of real-world, aggregated patient data for clinical benchmark correlation. | NIH Spine Patient Outcomes Research Trial (SPORT), institutional registries |
| Anatomical Model Repository | Provides standardized, high-quality 3D geometry of spinal segments for model construction. | The Open Science Framework (OSF), Visible Human Project, commercial image libraries |
| Material Property Library | Curated database of bone, ligament, disc, and implant material properties for accurate model definition. | Published compendiums (e.g., Journal of Biomechanics datasets), supplier datasheets |
Conclusion
A robust, standardized validation protocol is non-negotiable for transforming spinal implant computational models from research tools into credible evidence for design decisions and regulatory evaluation. By systematically addressing foundational principles, methodological rigor, troubleshooting, and quantitative validation, researchers can significantly enhance model predictive power. This not only accelerates the development of safer and more effective implants but also strengthens the case for regulatory acceptance of in silico trials. Future directions will involve integrating probabilistic analysis, patient-specific modeling powered by AI, and the creation of open-source validation benchmarks to advance the entire field toward more reliable clinical translation.