Verification and Validation in Computational Biomechanics: A Comprehensive Guide for Building Credible Models
This article provides a comprehensive guide to Verification and Validation (V&V) processes essential for establishing credibility in computational biomechanics models.
Verification and Validation in Computational Biomechanics: A Comprehensive Guide for Building Credible Models
Abstract
This article provides a comprehensive guide to Verification and Validation (V&V) processes essential for establishing credibility in computational biomechanics models. Aimed at researchers and drug development professionals, it covers foundational principles distinguishing verification ('solving the equations right') from validation ('solving the right equations'). The scope extends to methodological applications across cardiovascular, musculoskeletal, and soft tissue mechanics, alongside troubleshooting techniques like sensitivity analysis and mesh convergence studies. Finally, it explores advanced validation frameworks and comparative pipeline analyses critical for clinical translation, synthesizing best practices to ensure model reliability in biomedical research and patient-specific applications.
The Core Principles of V&V: Building a Foundation for Model Credibility
In the field of computational biomechanics, where models are increasingly used to simulate complex biological systems and inform medical decisions, establishing confidence in simulation results is paramount. Verification and Validation (V&V) provide the foundational framework for building this credibility. These processes are particularly crucial when models are designed to predict patient outcomes, as erroneous conclusions can have profound effects beyond the mere failure of a scientific hypothesis [1]. The fundamental distinction between these two concepts is elegantly captured by their common definitions: verification is "solving the equations right" (addressing the mathematical correctness), while validation is "solving the right equations" (ensuring the model accurately represents physical reality) [1].
As computational models grow more complex to capture the intricate behaviors of biological tissues, the potential for errors increases proportionally. These issues were first systematically addressed in computational fluid dynamics (CFD), with publications soon following in solid mechanics [1]. While no universal standard exists due to the rapidly evolving state of the art, several organizations, including ASME, have developed comprehensive guidelines [1] [2]. The adoption of V&V practices is becoming increasingly mandatory for peer acceptance, with many scientific journals now requiring some degree of V&V for models presented in publications [1].
Core Definitions and Their Practical Application
The V&V Process Workflow
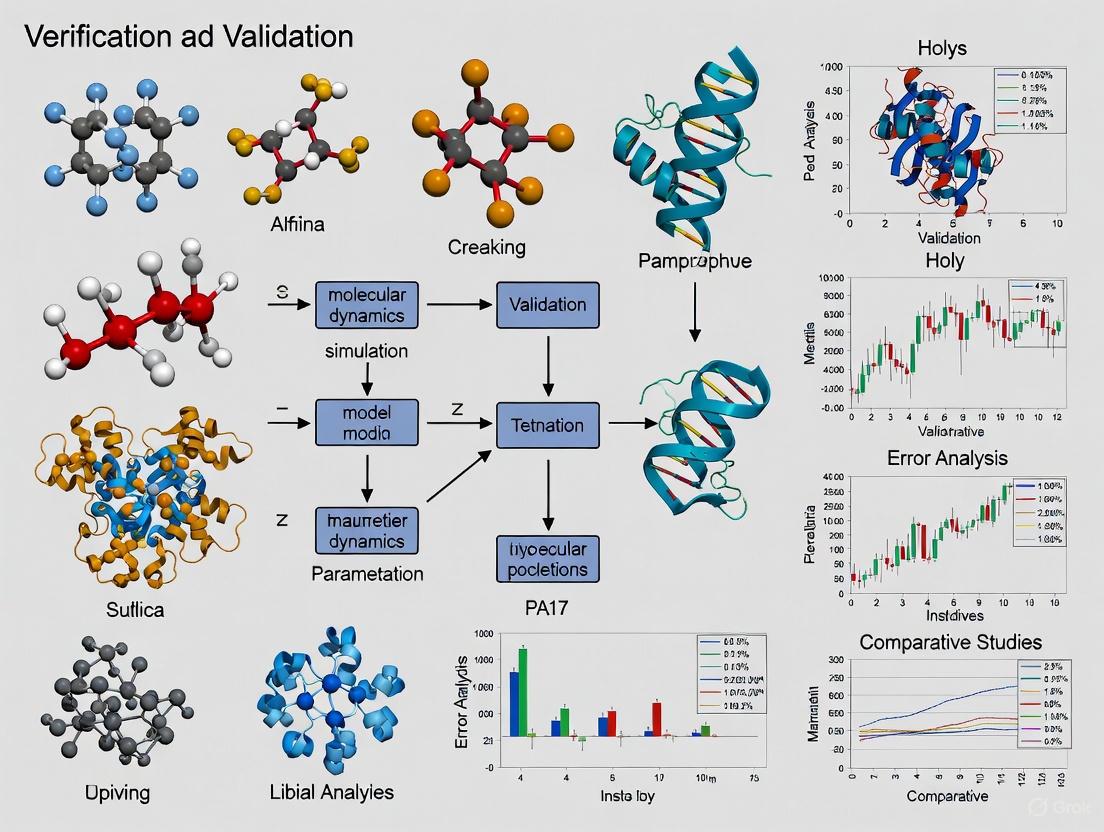
The relationship between the real world, mathematical models, and computational models, and how V&V connects them, can be visualized in the following workflow. Verification ensures the computational model correctly implements the mathematical model, while validation determines if the mathematical model accurately represents reality [1].
Comparative Analysis of V&V Concepts
The following table details the core objectives, questions, and key methodologies for Verification and Validation.
Table 1: Fundamental Concepts of Verification and Validation
| Aspect | Verification | Validation |
|---|---|---|
| Core Question | "Are we solving the equations correctly?" | "Are we solving the correct equations?" [1] |
| Primary Objective | Ensure the computational model accurately represents the underlying mathematical model and its solution [1]. | Determine the degree to which the model is an accurate representation of the real world from the perspective of its intended uses [1]. |
| Primary Focus | Mathematics and numerical accuracy. | Physics and conceptual accuracy. |
| Key Process | Code Verification: Ensuring algorithms work as intended.Calculation Verification: Assessing errors from domain discretization (e.g., mesh convergence) [1]. | Comparing computational results with high-quality experimental data for the specific context of use [1] [2]. |
| Error Type | Errors in implementation (e.g., programming bugs, inadequate iterative convergence). | Errors in formulation (e.g., insufficient constitutive models, missing physics) [1]. |
| Common Methods | Comparison to analytical solutions; mesh convergence studies [1]. | Validation experiments designed to tightly control quantities of interest [1]. |
Quantitative V&V Benchmarks and Experimental Protocols
Established Quantitative Benchmarks in the Literature
Successful application of V&V requires meeting specific quantitative benchmarks. The table below summarizes key metrics and thresholds reported in computational biomechanics research.
Table 2: Quantitative V&V Benchmarks from Computational Biomechanics Practice
| V&V Component | Metric | Typical Benchmark | Application Context |
|---|---|---|---|
| Code Verification | Agreement with Analytical Solution | ≤ 3% error [1] | Transversely isotropic hyperelastic model under equibiaxial stretch [1]. |
| Calculation Verification | Mesh Convergence Threshold | < 5% change in solution output [1] | Finite element studies of spinal segments [1]. |
| Validation | Comparison with Experimental Data | Context- and use-case dependent; requires statistical comparison and uncertainty quantification [1] [3]. | General practice for model validation against physical experiments. |
Detailed Experimental Protocols for V&V
Protocol for Mesh Convergence Study (Verification)
A mesh convergence study is a fundamental calculation verification activity to ensure that the discretization of the geometry does not unduly influence the simulation results.
- Problem Definition: Select a representative, well-defined problem relevant to the intended use of the full computational model.
- Baseline Mesh Generation: Create an initial mesh with a defined element size and type. The element size should be based on the geometric features of the model.
- Simulation Execution: Run the simulation using the baseline mesh and record the key output Quantity of Interest (QoI), such as peak stress or displacement.
- Systematic Refinement: Refine the mesh globally or in regions of high gradients (e.g., stress concentrations) by reducing the element size. The refinement ratio between subsequent meshes should be consistent (e.g., a factor of 1.5).
- Solution Tracking: Execute the simulation for each refined mesh and record the same QoI.
- Convergence Assessment: Calculate the relative difference in the QoI between successive mesh refinements. The study is considered complete when this relative difference falls below a pre-defined threshold (e.g., 5%) [1]. The solution from the finest mesh, or an extrapolated value, is typically taken as the converged result.
Protocol for a Model Validation Experiment
Validation requires a direct comparison of computational results with high-quality experimental data.
- Context of Use Definition: Clearly define the specific purpose of the model and the relevant QoIs for validation (e.g., ligament strain, joint contact pressure).
- Experimental Design: Design a physical experiment that can accurately measure the identified QoIs under well-controlled boundary conditions and loading scenarios. The experiment should be replicable.
- Specimen Characterization: Document all relevant characteristics of the physical specimen(s), including geometry, material properties, and any assumptions.
- Computational Model Setup: Develop a computational model (e.g., a Finite Element model) that replicates the exact geometry, boundary conditions, and loading of the physical experiment.
- Data Collection & Simulation: Conduct the physical experiment to collect empirical data for the QoIs. Run the simulation with the same inputs.
- Quantitative Comparison: Statistically compare the computational predictions with the experimental measurements. This goes beyond visual comparison and should assess both bias (systematic error) and random (statistical) errors [1].
- Uncertainty Quantification (UQ): Report the uncertainties associated with both the experimental data and the computational inputs. Use UQ methods to propagate these uncertainties and establish confidence bounds on the model predictions [3] [2]. The model is considered validated for its context of use if the simulation results fall within the agreed-upon confidence bounds of the experimental data.
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table catalogs key computational tools and methodologies that form the essential "reagents" for conducting V&V in computational biomechanics.
Table 3: Essential Research Reagents and Solutions for V&V
| Item / Solution | Function in V&V Process | Example Context |
|---|---|---|
| Analytical Solutions | Serves as a benchmark for Code Verification; provides a "known answer" to check numerical implementation [1]. | Verifying a hyperelastic material model implementation against an analytical solution for equibiaxial stretch [1]. |
| High-Fidelity Experimental Data | Provides the ground-truth data required for Validation; must be of sufficient quality and relevance to the model's context of use [1]. | Using video-fluoroscopy to measure in-vivo ligament elongation patterns for validating a subject-specific knee model [4]. |
| Mesh Generation/Refinement Tools | Enable Calculation Verification by allowing the systematic study of discretization error [1]. | Performing a mesh convergence study in a finite element analysis of a spinal segment [1]. |
| Uncertainty Quantification (UQ) Frameworks | Quantify and propagate uncertainties from various sources (e.g., input parameters, geometry) to establish confidence bounds on predictions [3] [2]. | Assessing the impact of variability in material properties derived from medical image data on stress predictions in a bone model [1]. |
| Sensitivity Analysis Tools | Identify which model inputs have the most significant influence on the outputs; helps prioritize efforts in UQ and Validation [1]. | Determining the relative importance of ligament stiffness, bone geometry, and contact parameters on knee joint mechanics. |
| 2,2,7-Trimethylnonane | 2,2,7-Trimethylnonane, CAS:62184-53-6, MF:C12H26, MW:170.33 g/mol | Chemical Reagent |
| 14,15-Ditridecyloctacosane | 14,15-Ditridecyloctacosane, CAS:61625-16-9, MF:C54H110, MW:759.4 g/mol | Chemical Reagent |
The Evolving Landscape: VVUQ and Digital Twins
The field is evolving from V&V to VVUQ, formally incorporating Uncertainty Quantification as a critical third pillar. This is especially vital for emerging applications like Digital Twins in precision medicine [3]. A digital twin is a virtual information construct that is dynamically updated with data from its physical counterpart and used for personalized prediction and decision-making [3].
For digital twins in healthcare, robust VVUQ processes are non-negotiable for building clinical trust. This involves new challenges, such as determining how often a continuously updated digital twin must be re-validated and how to effectively communicate the levels of uncertainty in predictions to clinicians [3]. The ASME standards, including V&V 40 for medical devices, provide risk-based frameworks for assessing the credibility of such models, ensuring they are "fit-for-purpose" in critical clinical decision-making [3] [2].
In computational biomechanics and systems biology, the credibility of simulation results is paramount for informed decision-making in research and drug development. The process of establishing this credibility rests on the pillars of Verification and Validation (V&V). Verification addresses the question "Are we solving the equations correctly?" and is concerned with identifying numerical errors. Validation addresses the question "Are we solving the correct equations?" and focuses on modeling errors [5]. For researchers and drug development professionals, confusing these two distinct error types can lead to misguided model refinements, incorrect interpretations of system biology, and ultimately, costly failures in translating computational predictions into real-world applications. This guide provides a structured comparison of these errors, supported by experimental data and methodologies, to equip scientists with the tools for robust model assessment within a rigorous V&V framework.
Defining the Error Types: A Comparative Basis
At its core, the distinction between numerical and modeling error is a distinction between solution fidelity and conceptual accuracy.
Modeling Error: This is a deficiency in the mathematical representation of the underlying biological or physical system. It arises from incomplete knowledge or deliberate simplification of the phenomena being studied. Sources include missed biological interactions, incorrect reaction kinetics, or uncertainty in model parameters [6] [7] [8]. In the context of V&V, modeling error is a primary target of validation activities [5].
Numerical Error: This error is introduced when the continuous mathematical model is transformed into a discrete set of equations that a computer can solve. It is the error generated by the computational method itself. Key sources include discretization error (from representing continuous space/time on a finite grid), iterative convergence error (from stopping an iterative solver too soon), and round-off error (from the finite precision of computer arithmetic) [7] [9] [8]. The process of identifying and quantifying these errors is known as verification [5].
The diagram below illustrates how these errors fit into the complete chain from a physical biological system to a computed result.
The chain of errors from a physical system to a computational result. Modeling error arises when creating the mathematical abstraction, while numerical and round-off errors occur during the computational solving process. Adapted from the concept of the "chain of errors" [8].
A Side-by-Side Comparison of Numerical and Modeling Errors
The following table summarizes the core characteristics that distinguish these two fundamental error types.
| Feature | Numerical Error | Modeling Error |
|---|---|---|
| Fundamental Question | Are we solving the equations correctly? (Verification) [5] | Are we solving the correct equations? (Validation) [5] |
| Primary Origin | Discretization and computational solution process [7] [9] | Incomplete knowledge or simplification of the biological system [6] [8] |
| Relation to Solution | Can be reduced by improving computational parameters (e.g., finer mesh, smaller time-step) [7] | Generally unaffected by computational improvements; requires changes to the model itself [6] |
| Key Subtypes | Discretization, Iterative Convergence, Round-off Error [7] | Physical Approximation, Physical Modeling, Geometry Modeling Error [7] [8] |
| Analysis Methods | Grid convergence studies, iterative residual monitoring [7] | Validation against high-quality experimental data, sensitivity analysis [10] [5] |
Deep Dive: Numerical Error Subtypes
Numerical errors can be systematically categorized and quantified. The table below expands on the primary subtypes.
| Error Subtype | Description | Mitigation Strategy |
|---|---|---|
| Discretization Error | Error from representing continuous PDEs as algebraic expressions on a discrete grid or mesh [7]. | Grid Convergence Studies: Refining the spatial mesh and temporal time-step until the solution shows minimal change [7]. |
| Local Truncation Error | The error committed in a single step of a numerical method by truncating a series approximation (e.g., Taylor series) [9]. | Using numerical methods with a higher order of accuracy, which causes the error to decrease faster as the step size is reduced [9]. |
| Iterative Convergence Error | Error from stopping an iterative solver (for a linear or nonlinear system) before the exact discrete solution is reached [7]. | Iterating until key solution residuals and outputs change by a negligibly small tolerance [7]. |
| Round-off Error | Error from the finite-precision representation of floating-point numbers in computer arithmetic [7] [11]. | Using higher-precision arithmetic (e.g., 64-bit double precision) and avoiding poorly-conditioned operations [7] [11]. |
Deep Dive: Modeling Error Subtypes
Modeling errors are often more insidious as they reflect the fundamental assumptions of the model.
| Error Subtype | Description | Example in Biological Systems |
|---|---|---|
| Physical Approximation Error | Deliberate simplifications of the full physical or biological description for convenience or computational efficiency [7] [8]. | Modeling a fluid flow as inviscid when viscous effects are small but non-zero; assuming a tissue is a single-phase solid when it is a porous, fluid-saturated material [8]. |
| Physical Modeling Error | Errors due to an incomplete understanding of the phenomenon or uncertainty in model parameters [7] [8]. | Using an incorrect reaction rate in a kinetic model of a signaling pathway; applying a linear model to a nonlinear biological process [6] [10]. |
| Geometry Modeling Error | Inaccuracies in the representation of the system's physical geometry [7]. | Using an idealized cylindrical vessel instead of a patient-specific, tortuous artery in a hemodynamic simulation. |
Experimental Protocols for Error Quantification
A rigorous V&V process requires standardized experimental and computational protocols to quantify both types of error.
Protocol for Quantifying Numerical (Discretization) Error
The most recognized method for quantifying spatial discretization error is the Grid Convergence Index (GCI) method, based on Richardson extrapolation.
- Generate a Series of Meshes: Create at least three geometrically similar computational grids with a systematic refinement ratio ( r ) (e.g., ( r = \sqrt{2} ) for a doubling of the number of grid elements in a 3D simulation). The grids should be as free of artifacts as possible.
- Compute Key Solutions: On each grid, compute the value of a key Quantity of Interest (QoI), such as the peak stress in a bone implant or the average velocity in a vessel. Denote these solutions as ( f1 ) (finest grid), ( f2 ), and ( f_3 ) (coarsest grid).
- Calculate Apparent Order: The observed convergence order ( p ) can be calculated using: ( p = \frac{1}{\ln(r{21})} \left| \ln \left| \frac{f3 - f2}{f2 - f1} \right| + q(p) \right| ), where ( r{21} ) is the refinement ratio between medium and fine grids, and ( q(p) ) is a term that can be solved iteratively [7].
- Extrapolate and Compute GCI: Use the observed order ( p ) to compute an extrapolated value ( f_{ext} ) and then the GCI for the fine grid solution, which provides an error band. The detailed equations for this step are standardized and available in references like the ASME V&V 20 standard [5].
Protocol for Quantifying and Correcting Modeling Error
The Dynamic Elastic-Net method is a powerful, data-driven approach for identifying and correcting modeling errors in systems of Ordinary Differential Equations (ODEs), common in modeling biological networks [6].
- Define the Nominal Model: Start with the preliminary ODE model: ( \frac{d\tilde{x}}{dt} = \tilde{f}(\tilde{x}, u, t) ), where ( \tilde{x} ) represents the state variables (e.g., protein concentrations) and ( u ) is a known input.
- Formulate the Observer System: Create a copy of the system that includes a hidden input ( \hat{w}(t) ) to represent the model error: ( \frac{d\hat{x}}{dt} = \tilde{f}(\hat{x}, u, t) + \hat{w}(t) ).
- Solve the Optimal Control Problem: Estimate the error signal ( \hat{w}(t) ) by minimizing an error functional ( J[\hat{w}] ) that balances the fit to the experimental data ( y(ti) ) with a regularization term that promotes a sparse solution. This functional is often of the form: ( J[\hat{w}] = \sum{i} \left\| y(ti) - h(\hat{x}(ti)) \right\|^2 + R(\hat{w}) ), where ( R(\hat{w}) ) is the regularization term [6].
- Analyze the Sparse Error Signal: The resulting estimate ( \hat{w}(t) ) will be non-zero primarily for the state variables and time periods most affected by model error, directly pointing to flaws in the nominal model structure.
- Reconstruct the True System State: Use the corrected model to obtain an unbiased estimate ( \hat{x}(t) ) of the true system state, which is valuable when not all states can be measured experimentally [6].
Workflow for the Dynamic Elastic-Net method, a protocol for identifying and correcting modeling errors in biological ODE models through inverse modeling and sparse regularization [6].
Case Study: JAK-STAT Signaling Pathway
The JAK-STAT signaling pathway, crucial in cellular responses to cytokines, provides a clear example where modeling error can be diagnosed and addressed.
Experimental Setup and Model
- Biological System: Erythropoietin receptor-mediated phosphorylation and nuclear transport of STAT5 in cells [6].
- Nominal ODE Model: A 4-state variable model (( \text{STAT5}u, \text{STAT5}m, \text{STAT5}d, \text{STAT5}n )) describing the phosphorylation, dimerization, and nuclear transport process [6].
- Experimental Data: Time-course measurements of phosphorylated and total cytoplasmic STAT5, obtained via techniques like flow cytometry or Western blotting [6].
- Observed Discrepancy: Despite parameter optimization, a systematic mismatch persisted between the nominal model's prediction and the experimental data, indicating a significant modeling error [6].
Application of the Dynamic Elastic-Net
Researchers applied the dynamic elastic-net protocol to this system. The method successfully [6]:
- Reconstructed the error signal ( \hat{w}(t) ), showing when and on which state variables the model was failing.
- Identified the target variables of the model error, pointing to specific processes (e.g., a missed feedback mechanism or incorrect transport rate) within the JAK-STAT pathway that were inaccurately modeled.
- Provided a corrected state estimate, allowing for a more accurate reconstruction of the true dynamic state of the system, even with the imperfect nominal model.
This case demonstrates how distinguishing and explicitly quantifying modeling error provides actionable insights for model improvement and more reliable biological interpretation.
The Scientist's Toolkit: Essential Reagents & Computational Tools
| Item / Solution | Function in Error Analysis |
|---|---|
| High-Fidelity Experimental Data | Serves as the ground truth for model validation and for quantifying modeling error [6] [10]. |
| BrdU (Bromodeoxyuridine) | A thymidine analog used in cell proliferation assays; its incorporation into DNA provides quantitative data for fitting and validating cell cycle models [10]. |
| MATLAB / Python (with SciPy) | Programming environments for implementing inverse modeling, performing nonlinear least-squares fitting, and running numerical error analyses [10] [12]. |
| Levenberg-Marquardt Algorithm | A standard numerical optimization algorithm for solving nonlinear least-squares problems, crucial for parameter estimation and inverse modeling [10]. |
| Monte Carlo Simulation | A computational technique used to generate synthetic data sets with known noise properties, enabling estimation of confidence intervals for fitted parameters (i.e., quantifying error in the inverse modeling process) [10]. |
| 5-Undecynoic acid, 4-oxo- | 5-Undecynoic acid, 4-oxo-, CAS:61307-46-8, MF:C11H16O3, MW:196.24 g/mol |
| 7-Methyloct-2-YN-1-OL | 7-Methyloct-2-yn-1-ol |
The journey toward credible and predictive computational models in biology demands a disciplined separation between numerical error and modeling error. Numerical error, addressed through verification, is a measure of how well our computers solve the given equations. Modeling error, addressed through validation, is a measure of how well those equations represent reality. By employing the structured protocols and comparisons outlined in this guide—such as grid convergence studies for numerical error and the dynamic elastic-net for modeling error—researchers can not only quantify the uncertainty in their simulations but also pinpoint its root cause. This critical distinction is the foundation for building more reliable models of biological systems, ultimately accelerating the path from in-silico discovery to clinical application in drug development.
In computational biomechanics, models are developed to simulate the mechanical behavior of biological systems, from entire organs down to cellular processes. The credibility of these models is paramount, especially when they inform clinical decisions or drug development processes. Verification and Validation (V&V) constitute a formal framework for establishing this credibility. Verification is the process of determining that a computational model accurately represents the underlying mathematical model and its solution ("solving the equations right"). In contrast, Validation is the process of determining the degree to which a model is an accurate representation of the real world from the perspective of its intended uses ("solving the right equations") [13].
The V&V process flow systematically guides analysts from a physical system of interest to a validated computational model capable of providing predictive insights. This process is not merely a final check but an integral part of the entire model development lifecycle. For researchers and drug development professionals, implementing a rigorous V&V process is essential for peer acceptance, regulatory approval, and ultimately, the translation of computational models into tools that can advance medicine and biology [13]. With the growing adoption of model-informed drug development and the use of in-silico trials, the ASME V&V 40 standard has emerged as a risk-based framework for establishing model credibility, even finding application beyond medical devices in biopharmaceutical manufacturing [14].
The V&V Process Flow: A Step-by-Step Guide
The journey from a physical system to a validated computational model follows a structured pathway. The entire V&V procedure begins with the physical system of interest and ends with the construction of a credible computational model to predict the reality of interest [13]. The flowchart below illustrates this comprehensive workflow.
Stages of the V&V Process Flow
Physical System to Conceptual Model: The process initiates with the physical system of interest (e.g., a vascular tissue, a bone joint, or a cellular process). Through observation and abstraction, a conceptual model is developed. This involves defining the key components, relevant physics, and the scope of the problem, while acknowledging inherent uncertainties due to a lack of knowledge or natural biological variation [13].
Conceptual Model to Mathematical Model: The conceptual description is translated into a mathematical model, consisting of governing equations (e.g., equations for solid mechanics, fluid dynamics, or reaction-diffusion), boundary conditions, and initial conditions. Assumptions and approximations are inevitable at this stage, leading to modeling errors [13].
Mathematical Model to Computational Model: The mathematical equations are implemented into a computational framework, typically via discretization (e.g., using the Finite Element Method). This step introduces numerical errors, such as discretization error and iterative convergence error [13]. The resulting software is the computational model.
Code Verification: This step asks, "Are we solving the equations right?" [13] It ensures that the governing equations are implemented correctly in the software, without programming mistakes. Techniques include the method of manufactured solutions and order-of-accuracy tests [15]. This is a check for acknowledged errors (like programming bugs) and is distinct from validation [13].
Solution Verification: This process assesses the numerical accuracy of the computed solution for a specific problem. It quantifies numerical errors like discretization error (by performing mesh convergence studies) and iterative error [15]. The goal is to estimate the uncertainty in the solution due to these numerical approximations.
Model Validation: This critical step asks, "Are we solving the right equations?" [13] It assesses the modeling accuracy by comparing computational predictions with experimental data acquired from the physical system or a representative prototype [13]. A successful validation demonstrates that the model can accurately replicate reality within the intended context of use. Discrepancies often require a return to the conceptual or mathematical model to refine assumptions.
Uncertainty Quantification and Sensitivity Analysis
Interwoven throughout the V&V process is Uncertainty Quantification (UQ). UQ characterizes the effects of input uncertainties (e.g., in material properties or boundary conditions) on model outputs [15]. A related activity, Sensitivity Analysis (SA), identifies which input parameters contribute most to the output uncertainty. This helps prioritize efforts in model refinement and experimental data collection [13] [15]. UQ workflows involve defining quantities of interest, identifying sources of uncertainty, estimating input uncertainties, propagating them through the model (e.g., via Monte Carlo methods), and analyzing the results [15].
Experimental Protocols for Model Validation
A robust validation plan requires high-quality, well-controlled experimental data for comparison with computational predictions. The following example from vascular biomechanics illustrates a detailed validation protocol.
Detailed Protocol: Experimental Validation of a Vascular Tissue Model
This protocol, adapted from a study comparing 3D strain fields in arterial tissue, outlines the key steps for generating experimental data to validate a finite element (FE) model [16].
Sample Preparation:
- Source: Porcine common carotid artery samples are acquired from animals 6-9 months of age.
- Preparation: Frozen specimens are thawed, and residual connective tissue is carefully removed.
- Mounting: A 35 mm section is excised and mounted onto a custom biaxial testing machine via barb fittings.
Equipment and Setup:
- Mechanical Testing: A computer-controlled biaxial testing system is used, which applies controlled axial force and internal pressure.
- Simultaneous Imaging: An Intravascular Ultrasound (IVUS) catheter is inserted into the vessel lumen, allowing for simultaneous mechanical testing and imaging. The system is equipped with a physiological bath (typically PBS at 37°C) to maintain tissue viability.
Experimental Procedure:
- Pre-conditioning: The vessel specimen undergoes cyclic mechanical loading (e.g., pressurization from 0 to 140 mmHg for 10 cycles) to achieve a repeatable mechanical state.
- Data Acquisition: The vessel is subjected to a defined pressure-loading protocol (e.g., 0 to 140 mmHg). IVUS image data is acquired at multiple axial positions (e.g., 15 slices) and at discrete pressure levels across the loading range.
- Strain Derivation: Experimental strains are derived from the IVUS image data across load states using a deformable image registration technique (e.g., "warping" analysis). This provides a 3D experimental strain field for comparison.
Computational Simulation:
- Model Construction: A 3D FE model of the artery is constructed directly from the IVUS image data acquired at a reference pressure state.
- Material Properties: Material parameters are often personalized by calibrating a constitutive model (e.g., an isotropic neo-Hookean model) to the experimental pressure-diameter data.
- Boundary Conditions: The FE model replicates the experimental boundary conditions (applied pressure and axial stretch).
- Analysis: The FE model is analyzed to predict the 3D strain field throughout the vessel wall.
Validation Comparison:
- Data Extraction: Model-predicted strains are extracted from the FE simulation at locations corresponding to the experimental measurements.
- Comparison Tiers: Strains are compared at multiple spatial evaluation tiers: slice-to-slice, circumferentially, and across transmural levels (from lumen to outer wall).
- Accuracy Assessment: The agreement between FE-predicted and experimentally-derived strains (e.g., circumferential, εₜₜ) is quantified using metrics like the Root Mean Square Error (RMSE) [16].
Quantitative Comparisons and Data Presentation
The core of model validation is the quantitative comparison between computational predictions and experimental data. The table below summarizes typical outcomes from a vascular strain validation study, demonstrating the level of agreement that can be achieved.
Table 1: Comparison of Finite Element (FE) Predicted vs. Experimentally Derived Strains in Arterial Tissue under Physiologic Loading (Systolic Pressure) [16]
| Analysis Tier | Strain Component | FE Prediction (Mean ± SD) | Experimental Data (Mean ± SD) | Agreement (RMSE) | Notes |
|---|---|---|---|---|---|
| Slice-Level | Circumferential (εₜₜ) | 0.110 ± 0.050 | 0.105 ± 0.049 | 0.032 | Good agreement across axial slices |
| Transmural (Inner Wall) | Circumferential (εₜₜ) | 0.135 ± 0.061 | 0.129 ± 0.060 | 0.039 | Higher strain at lumen surface |
| Transmural (Outer Wall) | Circumferential (εₜₜ) | 0.085 ± 0.038 | 0.081 ± 0.037 | 0.025 | Lower strain at outer wall |
The data shows that a carefully developed and validated model can bound experimental data and achieve close agreement, with RMSE values an order of magnitude smaller than the measured strain values. This non-linear mechanical behavior, where the model's predictions closely follow the experimental trends across the loading range, provides strong evidence for the model's descriptive and predictive capabilities [16].
The Scientist's Toolkit: Essential Research Reagents and Materials
Building and validating a credible computational model in biomechanics relies on a suite of specialized tools, both computational and experimental. The following table details key resources referenced in the featured studies.
Table 2: Key Research Tools for Computational Biomechanics V&V
| Tool / Reagent | Function in V&V Process | Example Use Case |
|---|---|---|
| Finite Element (FE) Software | Platform for implementing and solving the computational model. | Solving the discretized governing equations for solid mechanics (e.g., arterial deformation) [16]. |
| Custom Biaxial Testing System | Applies controlled multi-axial mechanical loads to biological specimens. | Generating experimental stress-strain data and enabling simultaneous imaging under physiologic loading [16]. |
| Intravascular Ultrasound (IVUS) | Provides cross-sectional, time-resolved images of vessel geometry under load. | Capturing internal vessel geometry and deformation for model geometry construction and experimental strain derivation [16]. |
| Deformable Image Registration | Computes full-field deformations by tracking features between images. | Deriving experimental 3D strain fields from IVUS image sequences for direct comparison with FE results [16]. |
| ASME V&V 40 Standard | Provides a risk-based framework for establishing model credibility. | Guiding the level of V&V rigor needed for a model's specific Context of Use, e.g., in medical device evaluation [14]. |
| Uncertainty Quantification (UQ) Tools | Propagates input uncertainties to quantify their impact on model outputs. | Assessing confidence in predictions using methods like Monte Carlo simulation or sensitivity analysis [15]. |
| 3-(Bromomethyl)selenophene | 3-(Bromomethyl)selenophene|Research Chemical | 3-(Bromomethyl)selenophene is a key synthetic intermediate for research applications in organic electronics and materials science. For Research Use Only. Not for human or veterinary use. |
| 10-Hydroxydec-6-en-2-one | 10-Hydroxydec-6-en-2-one, CAS:61448-23-5, MF:C10H18O2, MW:170.25 g/mol | Chemical Reagent |
The V&V process flow provides an indispensable roadmap for transforming a physical biological system into a credible, validated computational model. This structured journey—from conceptualization and mathematical formulation through code and solution verification to final validation against experimental data—ensures that models are both technically correct and meaningful representations of reality. For researchers and drug development professionals, rigorously applying this framework is not an optional extra but a fundamental requirement. It is the key to generating reliable, peer-accepted results that can safely inform critical decisions in drug development, medical device design, and ultimately, patient care. As the field advances, the integration of robust Uncertainty Quantification and adherence to standards like ASME V&V 40 will further solidify the role of computational biomechanics as a trustworthy pillar of biomedical innovation.
In computational biomechanics, Verification and Validation (V&V) represent a systematic framework for establishing model credibility. Verification is defined as "the process of determining that a computational model accurately represents the underlying mathematical model and its solution," while validation is "the process of determining the degree to which a model is an accurate representation of the real world from the perspective of the intended uses of the model" [1]. Succinctly, verification ensures you are "solving the equations right" (mathematics), and validation ensures you are "solving the right equations" (physics) [1]. This distinction is not merely academic; it forms the foundational pillar for credible simulation-based research and its translation into clinical practice.
The non-negotiable status of V&V stems from the escalating role of computational models in basic science and patient-specific clinical applications. In basic science, models simulate the mechanical behavior of tissues to supplement experimental investigations and define structure-function relationships [1]. In clinical applications, they are increasingly used for diagnosis and evaluation of targeted treatments [1]. The emergence of in-silico clinical trials, which use individualized computer simulations in the regulatory evaluation of medical devices, further elevates the stakes [17]. When model predictions inform scientific conclusions or clinical decisions, a rigorous and defensible V&V process is paramount. Without it, results can be precise yet misleading, potentially derailing research pathways or, worse, adversely impacting patient outcomes [18].
Comparative Analysis of V&V Approaches
The implementation of V&V is not a one-size-fits-all process. It is guided by the model's intended use and the associated risk of an incorrect prediction. The ASME V&V 40 standard provides a risk-informed framework for establishing credibility requirements, which has become a key enabler for regulatory submissions [19]. The following tables compare traditional and emerging V&V methodologies, highlighting their applications, advantages, and limitations.
Table 1: Comparison of V&V Statistical Methods for Novel Digital Measures
| Statistical Method | Primary Application | Performance Measures | Key Findings from Real-World Data |
|---|---|---|---|
| Pearson Correlation Coefficient (PCC) | Initial assessment of the relationship between a digital measure and a reference measure [20]. | Magnitude of the correlation coefficient [20]. | Serves as a baseline comparison; often weaker than other methods [20]. |
| Simple Linear Regression (SLR) | Modeling the linear relationship between a single digital measure and a single reference measure [20]. | R² statistic [20]. | Provides a basic measure of shared variance but may be overly simplistic [20]. |
| Multiple Linear Regression (MLR) | Modeling the relationship between digital measures and combinations of reference measures [20]. | Adjusted R² statistic [20]. | Accounts for multiple variables, but may not capture latent constructs effectively [20]. |
| Confirmatory Factor Analysis (CFA) | Assessing the relationship between a novel digital measure and a clinical outcome assessment (COA) reference measure when direct correspondence is lacking [20]. | Factor correlations and model fit statistics [20]. | Exhibited acceptable fit in most models and estimated stronger correlations than PCC, particularly in studies with strong temporal and construct coherence [20]. |
Table 2: Traditional Physical Testing vs. In-Silico Trial Approaches
| Aspect | Traditional Physical Testing | In-Silico Trial Approach |
|---|---|---|
| Primary Objective | Product compliance demonstration [21]. | Simulation model validation and virtual performance assessment [21]. |
| Resource Requirements | High costs and long durations (e.g., a comparative trial took ~4 years) [17]. | Significant time and cost savings (e.g., a similar in-silico trial took 1.75 years) [17]. |
| Regulatory Pathway | Often requires clinical evaluation, though many AI-enabled devices are cleared via 510(k) without prospective human testing [22]. | Emerging pathway; credibility must be established via frameworks like ASME V&V 40 [19]. |
| Key Challenges | Ethical implications, patient recruitment, high costs [17]. | Technological limitations, unmet need for regulatory guidance, need for model credibility [17]. |
| Inherent Risks | Recalls concentrated early after clearance, often linked to limited pre-market clinical evaluation [22]. | Potential for uncontrolled risks if VVUQ activities are limited due to perceived cost [21]. |
Essential V&V Experimental Protocols and Methodologies
The V&V Process Workflow
A standardized V&V workflow is critical for building model credibility. The process must begin with verification and then proceed to validation, thereby separating errors in model implementation from uncertainties in model formulation [1]. The following diagram illustrates the foundational workflow of the V&V process.
Core Verification Protocols
3.2.1 Code and Calculation Verification Verification consists of two interconnected activities: code verification and calculation verification [1]. Code verification ensures the computational model correctly implements the underlying mathematical model and its solution algorithms. This is typically achieved by comparing simulation results to problems with known analytical solutions. For example, a constitutive model implementation can be verified by showing it predicts stresses within 3% of an analytical solution for a simple loading case like equibiaxial stretch [1]. Calculation verification, also known as solution verification, focuses on quantifying numerical errors, such as those arising from the discretization of the geometry and time.
3.2.2 Mesh Convergence Studies A cornerstone of calculation verification is the mesh convergence study. This process involves progressively refining the computational mesh (increasing the number of elements) until the solution output (e.g., stress at a critical point) changes by an acceptably small amount. A common benchmark in biomechanics is to refine the mesh until the change in the solution is less than 5% [1]. An incomplete mesh convergence study risks a solution that is artificially too "stiff" [1]. Systematic mesh refinement is equally critical on unstructured meshes, as misleading results can arise if refinement is not applied systematically [19].
Core Validation Protocols
3.3.1 Validation Experiments and Metrics Validation is the process of determining how well the computational model represents reality by comparing its predictions to experimental data specifically designed for validation [1]. The choice of an appropriate validation metric is crucial. For scalar quantities, these can be deterministic (e.g., percent difference) or probabilistic (e.g., area metric, Z metric) [21]. For time-series data (waveforms), specialized metrics for comparing signals are required [21]. The entire validation process, from planning to execution, requires close collaboration between simulation experts and experimentalists [21].
3.3.2 Uncertainty Quantification and Sensitivity Analysis Uncertainty Quantification (UQ) is the process of characterizing and propagating uncertainties in model inputs (e.g., material properties, boundary conditions) to understand their impact on the simulation outputs [21]. UQ distinguishes between aleatory uncertainty (inherent randomness) and epistemic uncertainty (lack of knowledge) [21]. A critical component of UQ is sensitivity analysis, which scales the relative importance of model inputs on the results [1]. This helps investigators target critical parameters for more precise measurement and understand which inputs have the largest effect on prediction variability.
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 3: Essential Tools for V&V in Computational Biomechanics
| Tool or Resource | Category | Function and Application |
|---|---|---|
| ASME V&V 40 Standard | Credibility Framework | Provides a risk-based framework for establishing the credibility requirements of a computational model for a specific Context of Use [19]. |
| Open-Source Statistical Web App [17] | Analysis Tool | An open-source R/Shiny application providing a statistical environment for validating virtual cohorts and analyzing in-silico trials. It implements techniques to compare virtual cohorts with real datasets [17]. |
| Confirmatory Factor Analysis (CFA) | Statistical Method | A powerful statistical method for analytical validation, especially when validating novel digital measures against clinical outcome assessments where direct correspondence is lacking [20]. |
| Mesh Generation & Refinement Tools | Pre-processing Software | Tools for creating and systematically refining computational meshes to perform convergence studies for calculation verification [19] [1]. |
| Sensitivity Analysis Software | UQ Software | Tools (often built into simulation packages or as separate libraries) to perform sensitivity analyses and quantify how input uncertainties affect model outputs [1]. |
| Validation Database | Data Resource | A repository of high-quality experimental data specifically designed for model validation, providing benchmarks for comparing simulation results [21]. |
| 5,5-Dichloro-1,3-dioxane | 5,5-Dichloro-1,3-dioxane | 5,5-Dichloro-1,3-dioxane is a chemical building block for antimicrobial and synthetic chemistry research. For Research Use Only. Not for human or veterinary use. |
| 3-Butyl-1,3-oxazinan-2-one | 3-Butyl-1,3-oxazinan-2-one | 3-Butyl-1,3-oxazinan-2-one (C8H15NO2) is a versatile oxazinanone scaffold for antimicrobial and anticancer research. This product is For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Implications for Basic Science and Patient-Specific Outcomes
Implications for Basic Science Research
In basic science, the primary implication of rigorous V&V is the establishment of trustworthy structure-function relationships. Models that have been verified and validated provide a reliable platform for investigating "what-if" scenarios that are difficult, expensive, or ethically challenging to explore experimentally [1]. However, the adoption of V&V is not yet universal. While probabilistic methods and VVUQ were introduced to computational biomechanics decades ago, the community is still in the process of broadly adopting these practices as standard [18]. Failure to implement V&V risks building scientific hypotheses on an unstable computational foundation, potentially leading to erroneous conclusions and wasted research resources.
Implications for Patient-Specific Clinical Outcomes
The stakes for V&V are dramatically higher in the clinical realm, where models are used for patient-specific diagnosis and treatment planning. The consequences of an unvalidated model prediction can directly impact patient welfare [1]. The field is moving toward virtual human twins and in-silico trials, which hold the promise of precision medicine and accelerated device development [23] [17]. For example, the SIMCor project is developing a computational platform for the in-silico development and regulatory approval of cardiovascular implantable devices [17]. The credibility of these tools for clinical decision-making is inextricably linked to a robust V&V process that includes uncertainty quantification [23]. The recall of AI-enabled medical devices, concentrated early after FDA authorization and often associated with limited clinical validation, serves as a stark warning of the real-world implications of inadequate validation [22].
Verification and Validation are non-negotiable pillars of credible computational biomechanics. They are not isolated tasks but an integrated process that begins with the definition of the model's intended use and continues through verification, validation, and uncertainty quantification. As summarized in the workflow below, this process transforms a computational model from a theoretical exercise into a defensible tool for discovery and decision-making.
For basic science, V&V is a matter of scientific integrity, ensuring that computational explorations yield reliable insights. For patient-specific applications, it is a matter of patient safety and efficacy, ensuring that model-based predictions can be trusted to inform clinical decisions. The continued development of standardized frameworks like ASME V&V 40, open-source tools for validation, and a culture that prioritizes model credibility is essential for the future translation of computational biomechanics from the research lab to the clinic.
The field of computational biomechanics increasingly relies on models to understand complex biological systems, from organ function to cell mechanics. The credibility of these models hinges on rigorous Verification and Validation (V&V) processes. Verification ensures that computational models accurately solve their underlying mathematical equations, while validation confirms that these models correctly represent physical reality [13] [24]. The foundational principle is succinctly summarized as: verification is "solving the equations right," and validation is "solving the right equations" [13].
These V&V methodologies did not originate in biomechanics but were instead adapted from more established engineering disciplines. This guide traces the historical migration of V&V frameworks, beginning with their formalization in Computational Fluid Dynamics (CFD) and computational solid mechanics, to their current application in computational biomechanics, and finally to the emerging risk-based approaches for medical devices.
The Foundational Disciplines: CFD and Solid Mechanics
The development of formal V&V guidelines was pioneered by disciplines with longer histories of computational simulation.
Computational Fluid Dynamics (CFD)
The CFD community was the first to initiate formal discussions and requirements for V&V [13].
- Early Adoption: The Journal of Fluids Engineering instituted the first journal policy related to V&V in 1986, refusing papers that failed to address truncation error testing and accuracy estimation [13].
- Guideline Development: In 1998, the American Institute of Aeronautics and Astronautics (AIAA) published a comprehensive guide, establishing key V&V concepts and practices [24].
- Seminal Text: Roache's 1998 book provided a foundational text on V&V in CFD, solidifying key concepts for the community [13].
CFD's complex nature— involving strongly coupled non-linear partial differential equations solved in complex geometric domains—made the systematic assessment of errors and uncertainties particularly critical [24].
Computational Solid Mechanics
The computational solid mechanics community developed its V&V guidelines concurrently with the CFD field.
- ASME Leadership: The American Society of Mechanical Engineers (ASME) formed a committee in 1999, leading to the publication of the ASME V&V 10 standard in 2006 [13].
- Standardization: This standard provided the solid mechanics community with a common language, conceptual framework, and implementation guidance for V&V processes [25].
Table 1: Key Early V&V Guidelines in Foundational Engineering Disciplines
| Discipline | Leading Organization | Key Document / Milestone | Publication Year |
|---|---|---|---|
| Computational Fluid Dynamics (CFD) | AIAA | AIAA Guide (G-077) [13] | 1998 |
| Computational Fluid Dynamics (CFD) | - | Roache's Comprehensive Text [13] | 1998 |
| Computational Solid Mechanics | ASME | ASME V&V 10 Standard [13] | 2006 (First Published) |
Migration to Biomechanics and the Current State
The adoption of V&V principles in computational biomechanics followed a predictable but delayed trajectory, mirroring the field's own development.
The Time Lag and Initial Adoption
Computational simulations were used in traditional engineering in the 1950s but only appeared in tissue biomechanics in the early 1970s [13]. This 20-year time lag was reflected in the development of formal V&V policies. However, by the 2000s, active discussions were underway to adapt V&V principles for biological systems [13] [19]. Journals like Annals of Biomedical Engineering began instituting policies requiring modeling studies to "conform to standard modeling practice" [13].
The driving force for this adoption was the need for model credibility. As models grew more complex, analysts had to convince peers, experimentalists, and clinicians that the mathematical equations were implemented correctly, the model accurately represented the underlying physics, and an assessment of error and uncertainty was accounted for in the predictions [13].
Current Applications in Musculoskeletal Modeling
Modern applications show the mature integration of V&V concepts. In musculoskeletal (MSK) modeling of the spine, the ASME V&V framework provides a structured approach to ensure model suitability and credibility for a given "context of use" [26]. These models are used to study muscle recruitment, spinal disorders, and load distribution, relying on validation against often limited experimental data [26].
The modeling workflow now explicitly incorporates V&V, progressing from approach selection to morphological definition, incorporation of body weight, inclusion of passive structures, muscle modeling, kinematics description, and finally, validation through comparisons with literature data [26].
Figure 1: The historical evolution and specialization of V&V guidelines across engineering disciplines, culminating in modern biomedical applications.
The Rise of Risk-Based Frameworks: ASME V&V 40
A significant modern development is the shift towards risk-informed V&V processes, particularly for regulated industries like medical devices.
The ASME V&V 40 Standard
Published in 2018, the ASME V&V 40 standard provides a risk-based framework for establishing the credibility requirements of a computational model [2] [19]. Its core innovation is tying the level of V&V effort required to the model's risk in decision-making.
- Application to Medical Devices: V&V 40 has been a key enabler for the U.S. Food and Drug Administration (FDA) CDRH framework for using computational modeling and simulation data in regulatory submissions [19].
- Future Developments: The V&V 40 subcommittee continues to extend the framework, with ongoing technical reports on topics like a fictional tibial tray component and patient-specific femur-fracture prediction [19].
In Silico Clinical Trials
The push for higher-stakes applications continues with In Silico Clinical Trials (ISCT), where simulated patients augment or replace real human patients [19]. This application places the highest credibility demands on computational models, requiring extensive V&V to satisfy diverse stakeholders [19].
Table 2: Evolution of Key ASME V&V Standards for Solid and Biomechanics
| Standard | Full Title | Focus / Application Area | Key Significance |
|---|---|---|---|
| V&V 10 | Standard for Verification and Validation in Computational Solid Mechanics [2] [25] | General Solid Mechanics | Provided the foundational framework for the solid mechanics community. |
| V&V 40 | Assessing Credibility of Computational Modeling through Verification and Validation: Application to Medical Devices [2] | Medical Devices | Introduced a risk-based approach, crucial for regulatory acceptance. |
| VVUQ 40.1 | An Example of Assessing Model Credibility...: Tibial Tray Component... [19] | Medical Devices (Example) | Provides a detailed, end-to-end example of applying the V&V 40 standard. |
Successful implementation of V&V requires leveraging established resources, standards, and communities.
Key Standards and Frameworks
Researchers should consult and apply the following established guidelines:
- ASME V&V 10-2019: The current standard for verification and validation in computational solid mechanics, providing common language and guidance [25].
- ASME V&V 40-2018: The essential risk-based standard for applications in medical devices and biomedical simulations [2] [19].
- NASA-STD-7009: A comprehensive NASA standard covering requirements, verification, validation, and documentation for aerospace systems, with transferable principles [27].
Experimental Protocols for Validation
A robust validation protocol requires a direct comparison between computational predictions and experimental data.
- Gold Standard Comparison: Validation is a process by which computational predictions are compared to experimental data, which serves as the "gold standard," to assess modeling error [13].
- Combined Protocols: Models should be verified and validated using a combined computational and experimental protocol, integrating methodologies and data from both biomechanics domains [13].
- Uncertainty Quantification: The protocol must account for errors (e.g., discretization, geometry) and uncertainties (e.g., unknown material data, inherent property variation) [13] [2].
Professional Communities
Engagement with professional communities is vital for staying current.
- ASME VVUQ Standards Committees: Committees that develop and maintain V&V standards; participation is free and open to those with relevant expertise [2].
- NAFEMS: A worldwide community dedicated to engineering simulation, with working groups focused on simulation governance and VVUQ [27].
The evolution of V&V guidelines—from their origins in CFD and solid mechanics to their specialized application in biomechanics and medical devices—demonstrates a consistent trend toward greater formalization and risk-aware practices. The historical transition from fundamental concepts like "solving the equations right" to sophisticated, risk-based frameworks like ASME V&V 40 highlights the growing importance of computational model credibility. For researchers in biomechanics and drug development, leveraging these established guidelines is not merely a best practice but a fundamental requirement for producing clinically relevant and scientifically credible results. As the field advances toward in silico clinical trials and personalized medicine, rigorous V&V will remain the cornerstone of trustworthy computational science.
From Theory to Practice: Implementing V&V Across Biomechanical Applications
In computational biomechanics, the credibility of model predictions is paramount, especially when simulations inform basic science or guide clinical decision-making. Verification and Validation (V&V) form the cornerstone of establishing this credibility. Within this framework, verification is defined as "the process of determining that a computational model accurately represents the underlying mathematical model and its solution," while validation determines "the degree to which a model is an accurate representation of the real world" [1]. Succinctly, verification ensures you are "solving the equations right" (mathematics), and validation ensures you are "solving the right equations" (physics) [1]. By definition, verification must precede validation to separate errors stemming from the implementation of the model from uncertainties inherent in the model's formulation itself [1]. This guide focuses on the critical practice of code and calculation verification, objectively comparing its methodologies and providing the experimental protocols for their rigorous application.
Foundational Concepts and Methodologies
Verification is composed of two interconnected categories: code verification and calculation verification [1].
Code verification ensures the mathematical model and its solution algorithms are implemented correctly within the software. It confirms that the underlying governing equations are being solved as intended, free from programming errors, inadequate iterative convergence, and lack of conservation properties [1]. The most rigorous method involves comparison to analytical solutions, which provide an exact benchmark. For complex problems where analytical solutions are unavailable, highly accurate numerical solutions or method of manufactured solutions are employed.
Calculation verification addresses errors arising from the discretization of the problem domain and its subsequent numerical solution. In the Finite Element Method (FEM), this primarily involves characterizing errors from the spatial discretization (the mesh) and the time discretization (time-stepping) [1]. A key process in calculation verification is the mesh convergence study, where the model is solved with progressively refined meshes until the solution changes by an acceptably small amount, indicating that the discretization error has been minimized.
The following diagram illustrates the hierarchical relationship and workflow between these verification concepts and their role within the broader V&V process.
Comparative Analysis of Verification Approaches
The table below summarizes the primary benchmarks and methods used for code and calculation verification, detailing their applications, outputs, and inherent limitations.
Table 1: Comparison of Verification Benchmarks and Methods
| Method Type | Primary Application | Key Measured Outputs | Advantages | Limitations |
|---|---|---|---|---|
| Analytical Solutions [1] | Code Verification | Stress, strain, displacement, flow fields | Provides exact solutions; most rigorous for code verification. | Seldom available for complex, non-linear biomechanics problems. |
| Method of Manufactured Solutions [1] | Code Verification | Any computable quantity from the model | Highly flexible; can be applied to any code and complex PDEs. | Does not verify model physics, only the solution implementation. |
| Mesh Convergence Studies [1] | Calculation Verification | Stress, strain, displacement, pressure | Essential for quantifying discretization error; standard practice in FE. | Computationally expensive; convergence can be difficult to achieve. |
| Numerical Benchmarks [28] | Code & Calculation Verification | Pressure-volume loops, stress, deformation | Provides community-agreed standards for complex physics (e.g., cardiac mechanics). | May not cover all features of a specific model of interest. |
Experimental Protocols for Verification
To ensure reproducibility and rigor, a standardized experimental protocol for verification must be followed. The workflow below details the logical sequence of steps for a comprehensive verification study, from defining the problem to final documentation.
Protocol for Code Verification via Analytical Benchmarks
This protocol is designed to test the fundamental correctness of a computational solver by comparing its results against a known exact solution.
Objective: To verify that the computational implementation accurately solves the underlying mathematical model for a simplified case with a known analytical solution [1].
Methodology:
- Problem Selection: Choose a simplified geometry and set of boundary conditions for which an exact analytical solution to the governing equations exists. An example from literature includes verifying a transversely isotropic hyperelastic constitutive model against an analytical solution for equibiaxial stretch [1].
- Simulation Setup: Implement the identical simplified problem in the computational code.
- Data Extraction & Comparison: Run the simulation and extract the relevant output fields (e.g., stress, strain). Quantitatively compare these results to the analytical solution.
- Error Quantification: Calculate the error, defined as the difference between the computational and analytical results. A common metric is the relative error norm. The code is considered verified for this specific case if errors fall below an acceptable threshold (e.g., <3% in the cited example) [1].
Protocol for Calculation Verification via Mesh Convergence
This protocol assesses and minimizes the numerical error introduced by discretizing the geometry into a finite element mesh.
Objective: To ensure that the solution is independent of the spatial discretization by systematically refining the mesh until the solution changes are negligible [1].
Methodology:
- Baseline Mesh: Create a baseline mesh with an initial element size deemed reasonably fine for the problem.
- Systematic Refinement: Generate a sequence of at least three meshes with progressively smaller element sizes (finer meshes). Global or local refinement techniques can be used.
- Solution Execution: Solve the same boundary value problem on each mesh in the sequence.
- Solution Monitoring: Track one or more key Quantities of Interest (QoIs) across the mesh series. QoIs are often maximum principal stress or strain at a critical location [1].
- Convergence Criterion: Determine that the solution has converged when the relative change in the QoI between successive mesh refinements is below a pre-defined tolerance. A common criterion in biomechanics is a change of <5% [1].
Table 2 provides a hypothetical example of how results from a mesh convergence study are tracked and analyzed.
Table 2: Example Results from a Mesh Convergence Study
| Mesh ID | Number of Elements | Max. Principal Stress (MPa) | Relative Change from Previous Mesh | Conclusion |
|---|---|---|---|---|
| Coarse | 15,000 | 48.5 | --- | Not Converged |
| Medium | 45,000 | 52.1 | 7.4% | Not Converged |
| Fine | 120,000 | 53.8 | 3.3% | Converged |
| Extra-Fine | 350,000 | 54.1 | 0.6% | Converged (Overkill) |
Emerging Benchmarking Efforts
The field is moving towards standardized community benchmarks to facilitate direct comparison between different solvers and methodologies. A prominent example is the development of a software benchmark for cardiac elastodynamics, which includes problems for assessing passive and active material behavior, viscous effects, and complex boundary conditions on both monoventricular and biventricular domains [28]. Utilizing such benchmarks is a best practice for demonstrating solver capability.
The Scientist's Toolkit: Research Reagent Solutions
Beyond software, a robust verification pipeline relies on specific computational tools and data. The following table details key "research reagents" essential for conducting verification studies.
Table 3: Essential Research Reagents for Verification Studies
| Item/Resource | Function in Verification | Application Example |
|---|---|---|
| Analytical Solution Repository | Provides ground-truth data for code verification. | Verifying a hyperelastic material model implementation against a known solution for uniaxial tension. |
| Mesh Generation Software | Creates the sequence of discretized geometries for calculation verification. | Generating coarse, medium, fine, and extra-fine tetrahedral meshes from a patient-specific bone geometry. |
| Robust FE Solver (e.g., FEBio) [29] | Computes the numerical solution to the boundary value problem; must be capable of handling complex biomechanical material models. | Solving a contact problem between two articular cartilage surfaces to predict contact pressure. |
| High-Performance Computing (HPC) Cluster | Provides the computational power required for running multiple simulations with high-fidelity models during convergence studies. | Executing a parameter sensitivity analysis or a large-scale 3D fluid-structure interaction simulation. |
| Numerical Benchmark Suite [28] | Offers standardized community-agreed problems for verifying solvers against established results for complex physics. | Testing a new cardiac mechanics solver against a benchmark for active contraction and hemodynamics. |
| 3-Methoxy-2,4-dimethylfuran | 3-Methoxy-2,4-dimethylfuran|High-Purity Reference Standard | 3-Methoxy-2,4-dimethylfuran: A high-purity chemical for research use only (RUO). Explore its applications in organic synthesis and fragrance development. Not for human or veterinary use. |
| GTP gamma-4-azidoanilide | GTP gamma-4-azidoanilide, CAS:60869-76-3, MF:C16H20N9O13P3, MW:639.3 g/mol | Chemical Reagent |
Code and calculation verification are non-negotiable prerequisites for building credibility in computational biomechanics. This guide has detailed the methodologies for benchmarking against analytical and numerical solutions, providing a direct comparison of approaches and the experimental protocols for their implementation. As the field advances towards greater clinical integration and the use of digital twins [30], the rigorous application of these verification practices, supported by community-driven benchmarks [28], will be the foundation upon which reliable and impactful computational discoveries are built.
In the field of computational biomechanics, the development of sophisticated models for simulating biological systems has advanced dramatically. However, the predictive value and clinical translation of these models are entirely dependent on rigorous experimental validation across multiple biological scales. Without systematic validation against experimental data, computational models remain unverified mathematical constructs of uncertain biological relevance. This guide provides a comprehensive comparison of the three principal experimental methodologies—in vitro, in vivo, and ex vivo testing—used to establish the credibility of computational biomechanics models for researchers and drug development professionals.
The choice of validation methodology directly influences the translational potential of computational findings. In vitro systems offer controlled reductionism, in vivo models provide whole-organism complexity, and ex vivo approaches bridge these extremes by maintaining tissue-level biology outside the living organism. Understanding the capabilities, limitations, and appropriate applications of each method is fundamental to building a robust validation framework that can withstand scientific and regulatory scrutiny.
Defining the Methodologies
In Vitro Testing
In vitro (Latin for "within the glass") testing encompasses experiments conducted with biological components isolated from their natural biological context using laboratory equipment such as petri dishes, test tubes, and multi-well plates [31]. These systems typically involve specific biological components such as cells, tissues, or biological molecules isolated from an organism, enabling precise manipulation and isolation of variables for detailed mechanistic studies [31].
- Key Characteristics: Controlled experimental conditions, simplified systems, isolation of specific variables, and suitability for high-throughput screening [31].
- Common Applications: Cell culture studies, cell viability and cytotoxicity assays, enzyme kinetics, biochemical assays, high-throughput drug screening, and molecular biology techniques [31].
In Vivo Testing
In vivo (Latin for "within a living organism") testing involves experiments conducted within intact living organisms, such as animals or humans [31]. These studies provide insights into physiological processes in their natural context, allowing for observation of complex interactions between different organ systems, physiological responses, and overall organismal behavior [31].
- Key Characteristics: Whole organism complexity, natural physiological environment, and observation of systemic effects and ecological interactions [31].
- Common Applications: Animal studies modeling disease progression, pathogenesis, and therapeutic strategies; clinical trials testing safety and efficacy of new drugs in humans; behavioral studies; and toxicology assessments [31].
Ex Vivo Testing
Ex vivo (Latin for "out of the living") testing involves experiments conducted on living tissue or biological systems outside the organism while attempting to maintain tissue structure and function. This approach bridges the gap between highly controlled in vitro systems and complex in vivo environments.
- Key Characteristics: Preservation of tissue-level architecture and cellular interactions, controlled experimental conditions, and limited systemic influences.
- Common Applications: Precision medicine platforms, tissue-specific drug response testing, and mechanistic studies requiring intact tissue microenvironment.
Comparative Analysis of Validation Methods
The table below provides a structured comparison of the three experimental methodologies, highlighting their distinct characteristics, applications, and value for computational model validation.
Table 1: Comprehensive Comparison of Experimental Validation Methods
| Aspect | In Vitro | In Vivo | Ex Vivo |
|---|---|---|---|
| System Complexity | Isolated cells or molecules in 2D/3D culture [31] | Whole living organism with all systemic interactions [31] | Living tissue or organs outside the organism [32] |
| Control Over Variables | High precision in manipulation of specific conditions [31] | Limited control due to inherent biological variability [31] | Moderate control while preserving tissue context |
| Physiological Relevance | Low - lacks natural microenvironment and systemic factors [31] | High - intact physiological environment and responses [31] | Intermediate - maintains tissue architecture but not systemic regulation |
| Throughput & Cost | High throughput, relatively low cost [31] | Low throughput, high cost and time requirements [31] | Moderate throughput and cost requirements |
| Ethical Considerations | Minimal ethical concerns [33] | Significant ethical considerations, especially in animal models [33] | Reduced ethical concerns compared to in vivo |
| Primary Validation Role | Initial model parameterization and mechanistic hypothesis testing | Holistic model validation and prediction of systemic outcomes [34] | Tissue-level validation and assessment of emergent tissue behaviors |
| Key Limitations | Unable to replicate complexity of whole organisms [33] | Interspecies differences, ethical constraints, high complexity [35] | Limited lifespan of tissues, absence of systemic regulation |
| Typical Duration | Hours to days | Weeks to months (animals); years (clinical trials) | Hours to weeks |
Experimental Protocols for Model Validation
Ex Vivo 3D Micro-Tumor Validation Platform
A clinically validated ex vivo approach for predicting chemotherapy response in high-grade serous ovarian cancer demonstrates the power of tissue-level validation systems [32].
Table 2: Key Research Reagent Solutions for Ex Vivo 3D Micro-Tumor Platform
| Reagent/Component | Function in Experimental Protocol |
|---|---|
| Malignant Ascites Samples | Source of patient-derived tumor material preserving native microenvironment [32] |
| Extracellular Matrix Components | Provides 3D support structure for micro-tumor growth and organization |
| Carboplatin/Paclitaxel | Standard of care chemotherapeutic agents for sensitivity testing [32] |
| Culture Medium with Growth Factors | Maintains tissue viability and function during ex vivo testing period |
| High-Content Imaging System | Quantifies morphological features and treatment responses in 3D micro-tumors [32] |
| Immunohistochemistry Markers | Validates preservation of tumor markers (PAX8, WT1) and tissue architecture [32] |
Step-by-Step Protocol:
- Sample Acquisition and Processing: Collect malignant ascites from ovarian cancer patients and enrich for micro-tumors using centrifugation and washing steps [32].
- 3D Culture Establishment: Embed micro-tumors in extracellular matrix components in multi-well plates to maintain 3D architecture and viability.
- Therapeutic Exposure: Expose micro-tumors to concentration gradients of standard-of-care chemotherapeutics (carboplatin/paclitaxel) and second-line agents for sensitivity profiling [32].
- High-Content Imaging and Analysis: Capture 3D images of micro-tumors over time using automated microscopy, followed by extraction of morphological features indicating viability and response [32].
- Response Modeling: Train linear regression models to correlate ex vivo sensitivity profiles with clinical CA125 decay rates, changes in tumor size, and progression-free survival [32].
- Clinical Correlation: Establish predictive thresholds for treatment response by correlating ex vivo results with patient outcomes, enabling stratification of responders versus non-responders [32].
This platform achieved a significant correlation (R=0.77) between predicted and clinical CA125 decay rates and correctly stratified patients based on progression-free survival, demonstrating its potential for informing treatment decisions [32].
In Vivo Target Validation Protocol
For validating computational models of disease mechanisms or therapeutic interventions, in vivo target validation provides the essential whole-organism context [34].
Step-by-Step Protocol:
- Animal Model Selection: Employ genetically engineered mouse models that recapitulate key disease pathologies, such as the TDP-43 mouse model for ALS research [34].
- Test Article Preparation: Prepare therapeutic agents (small molecules, biologics, gene therapies) with demonstrated safety at planned doses and confirmed brain penetrance [34].
- Experimental Dosing: Administer test articles via appropriate routes (systemic, intrathecal) using prophylactic/preventative or interventional dosing regimens over 4-8 weeks [34].
- Multimodal Endpoint Assessment:
- Clinical Measures: Monitor body weight, motor scores (grip strength), and perform anatomical MRI [34].
- Functional Measures: Conduct electromyography and longitudinal CT imaging of hindlimb muscle atrophy [34].
- Molecular Measures: Analyze tissue sections for target engagement markers, pathological protein mislocalization, and cellular stress responses [34].
- Data Integration: Correlate target modulation with functional improvements and survival outcomes to validate therapeutic mechanisms [34].
In Vitro Biomechanical Validation Protocol
For validating computational models of tissue biomechanics, in vitro systems allow precise control of mechanical conditions as shown in vascular tissue validation studies [16].
Step-by-Step Protocol:
- Tissue Preparation: Mount arterial specimens on custom biaxial testing systems that enable simultaneous mechanical loading and imaging [16].
- Experimental Setup: Insert intravascular ultrasound (IVUS) catheter into the lumen to capture cross-sectional images during controlled pressurization and axial extension [16].
- Mechanical Testing: Apply physiological pressure and axial stretch ratios while acquiring IVUS images at multiple axial positions and load states.
- Strain Quantification: Derive experimental strains using deformable image registration techniques applied to sequential IVUS images [16].
- Finite Element Model Development: Construct 3D finite element models from IVUS image data, incorporating material properties from literature and experimental measurements [16].
- Model-Experimental Comparison: Extract model-predicted strains at matching locations and compare with experimental measurements using correlation analyses and error quantification [16].
This approach demonstrated that FE-predicted strains bounded experimental data across spatial evaluation tiers, providing crucial validation of the modeling framework's ability to accurately predict artery-specific mechanical environments [16].
Integration with Computational Model Validation
Strategic Framework for Multiscale Validation
Each experimental methodology provides distinct but complementary value for computational model validation across biological scales. The following diagram illustrates the integrated relationship between computational modeling and experimental validation methods:
Figure 1: Integrated Workflow for Multiscale Model Validation. This framework illustrates how different experimental methods contribute sequentially to building credible computational models, from initial parameterization to final systemic validation.
Methodological Synergies for Comprehensive Validation
The most robust validation frameworks strategically combine methodologies to address their individual limitations:
In vitro to in vivo translation (IVIVC): In vitro assays provide high-throughput screening for model parameterization, while in vivo studies validate systemic predictions [31]. For example, in vitro cytotoxicity data can inform initial parameters for pharmacokinetic-pharmacodynamic models that are subsequently validated against in vivo efficacy outcomes.
Ex vivo bridging studies: Ex vivo platforms maintain tissue complexity while enabling controlled interventions, serving as intermediate validation steps between reductionist in vitro systems and complex in vivo environments [32]. The 3D micro-tumor platform exemplifies how ex vivo systems can predict in vivo clinical responses while enabling mechanistic investigation not feasible in intact organisms.
Quantitative validation metrics: Establishing standardized quantitative metrics for comparing computational predictions to experimental outcomes is essential across all methodologies. In vascular biomechanics, comparison of finite-element derived strain fields with experimental measurements provides rigorous validation of model accuracy [16].
Emerging Trends and Future Directions
Technological Innovations
The field of experimental validation is rapidly evolving with several technological innovations enhancing validation capabilities:
Organ-on-a-Chip and Microphysiological Systems: These advanced in vitro platforms incorporate microfluidics to create more physiologically relevant models that mimic human organ functionality, enabling more predictive toxicity testing and disease modeling [35] [36]. The integration of multiple organ systems on a single platform allows investigation of organ-organ interactions and systemic effects traditionally only assessable in in vivo models.
Humanized Mouse Models: Advanced in vivo models incorporating human cells and tissues bridge the translational gap between conventional animal models and human clinical responses, particularly in immunotherapy research [35]. These models better recapitulate human-specific biological processes and therapeutic responses.
Advanced Imaging and Sensing Technologies: Innovations in intravital microscopy, biosensors, and functional imaging enable more precise measurement of physiological parameters in all experimental systems, providing richer datasets for computational model validation [16].
Regulatory and Implementation Considerations
The global in vitro toxicity testing market, projected to grow from USD 10.04 billion in 2025 to USD 24.36 billion by 2032, reflects increasing regulatory acceptance and implementation of these methods [36]. Key trends include:
Regulatory shifts toward animal testing alternatives: Initiatives like the EU's REACH regulation and FDA's push for New Alternative Methods (NAMs) are driving adoption of sophisticated in vitro and ex vivo approaches for chemical safety assessment [36].
Quality control and standardization: As demonstrated in the ex vivo 3D micro-tumor platform, implementing rigorous quality control criteria (%CV < 25%, 3D gel quality assessment, positive control verification) is essential for generating reliable, reproducible validation data [32].
Validation against human data: Whenever possible, computational models should be ultimately validated against human clinical data, as demonstrated by the correlation between ex vivo drug sensitivity and clinical outcomes in ovarian cancer patients [32].
The strategic selection and implementation of in vitro, in vivo, and ex vivo experimental methods is fundamental to establishing credible, predictive computational models in biomechanics and drug development. Each methodology offers distinct advantages and addresses different aspects of the validation continuum, from molecular mechanisms to whole-organism physiology. The most robust validation frameworks strategically integrate multiple methodologies, leveraging their complementary strengths while acknowledging their limitations. As technological innovations continue to enhance the physiological relevance and precision of these experimental approaches, their power to validate and refine computational models will increasingly accelerate the development of safer, more effective therapeutic interventions.
The field of medicine is undergoing a significant transformation with the integration of computational modeling, enabling a shift from one-size-fits-all approaches to personalized treatment strategies. Patient-specific modeling involves creating detailed, personalized digital representations of a patient's anatomy and physiology using medical imaging data such as MRI or CT scans [37]. These models simulate various physiological processes, including blood flow, tissue mechanics, and drug delivery, providing clinicians with deeper insights into the underlying mechanisms of a patient's condition and facilitating more effective treatment strategies [37].
The generation of these models follows a structured pipeline, beginning with medical image acquisition and progressing through image segmentation, geometry reconstruction, and computational grid generation, ultimately enabling simulation and analysis. This process is particularly crucial in biomechanical applications such as blood flow in the cardiovascular system, air flow through the respiratory system, and tissue deformation in neurosurgery, where direct measurements of the phenomena of interest are often impossible or highly demanding through current in vivo examinations [38]. The credibility of computational models for medical devices and treatments is closely tied to their verification and validation (V&V), with validation being particularly challenging as it requires procedures that address the complexities of generating reliable experimental data for comparison with computational outputs [23].
Comparative Analysis of Grid Generation Techniques
The choice of computational grid type represents a fundamental technical decision in patient-specific modeling, significantly impacting solution accuracy, numerical diffusion, and computational efficiency. The table below compares the primary grid generation approaches based on key performance metrics.
Table 1: Comparison of Structured vs. Unstructured Grid Generation Techniques
| Feature | Structured Multi-block Grids | Unstructured Grids |
|---|---|---|
| Grid Element Alignment | Aligned with primary flow direction [38] | No specific alignment to flow [38] |
| Numerical Diffusion | Lower level [38] | Increased level [38] |
| Grid Convergence Index (GCI) | One order of magnitude less [38] | Higher [38] |
| Runtime Efficiency | Reduced by a factor of 3 [38] | Longer computation times [38] |
| Geometrical Accuracy | High, surface-conforming methods available [38] | Strong preservation of geometrical shape [38] |
| Generation Effort | Significant time and effort required [38] | Effortless generation in complex domains [38] |
| Typical Applications | CFD in bifurcations (e.g., carotid, aorta), FSI [38] | Initial studies in complex domains, rapid prototyping [38] |
Structured grids are typically composed of regular, ordered hexahedral elements, while unstructured grids use irregular collections of tetrahedral or polyhedral elements. The performance advantages of structured grids, particularly their alignment with flow direction and lower numerical diffusion, make them superior for simulating complex phenomena in branching geometries like those found in the cardiovascular system [38]. However, this advantage comes at the cost of significantly more complex and time-consuming grid generation processes.
For patient-specific modeling, a surface-conforming approach is essential for anatomical fidelity. A novel method for generating multi-block structured grids creates high-quality, surface-conforming grids from triangulated surfaces (STL format) derived from medical images, successfully applied to abdominal aorta bifurcations [38]. Similarly, in neurosurgery, patient-specific tetrahedral and regular hexahedral grids are generated from MRI and CT scans to solve the electrocorticography forward problem in a deforming brain [39].
Experimental Protocols and Methodologies
Protocol 1: Multi-block Structured Grid Generation for Arterial Bifurcations
This protocol outlines the methodology for generating high-quality structured grids from medical imaging data, specifically for arterial bifurcations [38].
- Step 1: Medical Image Acquisition and Processing: Acquire medical imaging data (e.g., MRI, CT) in DICOM format. Perform image segmentation to extract the Volume of Interest (VOI), creating a 3D triangulated surface representation of the anatomy in STL format [38].
- Step 2: Surface Processing and Domain Decomposition: Process the STL surface to ensure uniform triangulation. Decompose the complex bifurcation geometry into simpler topological blocks, often employing a "butterfly topology" to manage the branching region [38].
- Step 3: Block Assembly and Grid Generation: Assemble the decomposed blocks into a continuous multi-block structure. Generate a structured grid within each block, ensuring proper connectivity and smooth transitions between adjacent blocks [38].
- Step 4: Grid Enhancement and Quality Control: Apply elliptic smoothing techniques to enhance grid orthogonality and element quality. Conduct rigorous quality checks to ensure the grid is suitable for subsequent Computational Fluid Dynamics (CFD) or Fluid-Structure Interaction (FSI) analysis [38].
- Validation: Compare flow simulations against experimental data or results from commercial unstructured grid solvers (e.g., Ansys CFX) to validate the accuracy of the generated grid and flow solution [38].
Protocol 2: Patient-Specific Computational Grids for Brain Shift Analysis
This protocol details the creation of computational grids for solving the electrocorticography forward problem, accounting for brain deformation caused by surgical intervention [39].
- Step 1: Multi-Modal Image Acquisition and Co-registration: Obtain preoperative structural MRI, diffusion-weighted MRI (DWI), and postoperative CT images. Co-register these images into a common coordinate system [39].
- Step 2: Brain Geometry Extraction and Tissue Classification: Extract the patient-specific brain geometry from the registered images. Perform tissue classification using both MRI-based (e.g., STAPLE) and DTI-based methods to define different material regions [39].
- Step 3: Electrode Localization and Projection: Identify the actual 3D positions of implanted subdural electrodes from the postoperative CT scan. For comparison, create a model with electrode positions projected onto the preoperative cortical surface, disregarding brain shift [39].
- Step 4: Multi-Grid Generation for Multi-Physics Simulation: Generate different computational grids tailored for specific solvers: a tetrahedral grid for the meshless solution of the biomechanical model to predict brain deformation, and a regular hexahedral grid for the finite element solution of the electrocorticography forward problem [39].
- Step 5: Biomechanical Prediction and Forward Problem Solution: Use the tetrahedral grid with a biomechanical model to predict the postoperative brain configuration (warped anatomy). Solve the electrocorticography forward problem on the hexahedral grid using both the original and predicted postoperative anatomy to quantify the impact of brain shift [39].
The following workflow diagram illustrates the core steps involved in generating patient-specific computational models from medical imaging data.
Diagram 1: Patient-specific model generation workflow, highlighting the critical role of VVUQ.
Verification, Validation, and Uncertainty Quantification (VVUQ)
Within computational biomechanics, the principles of Verification, Validation, and Uncertainty Quantification (VVUQ) are paramount for establishing model credibility [18]. Verification ensures that the computational model is solved correctly (solving the equations right), while Validation determines how accurately the model represents the real-world physical system (solving the right equations) [18]. Uncertainty Quantification characterizes the impact of inherent uncertainties in model inputs, parameters, and structure on the simulation outputs.
The community is increasingly adopting probabilistic methods and VVUQ to ensure that simulations informing research and engineering practice yield defensible, well-bounded inferences rather than precise yet misleading results [18]. This is especially critical when models are intended to support medical device design or clinical decision-making [23]. For cardiovascular devices, the validation phase must address complexities in generating in-vitro and/or in-vivo data for comparison with computational outputs, while also managing biological and environmental variability through robust uncertainty quantification methods [23].
A key challenge in complex patient-specific models, including Quantitative Systems Pharmacology (QSP) models, is avoiding overfitting and ensuring predictive performance surpasses that of simpler models. Benchmarking against simpler, context-specific heuristics is necessary to assess potential overfitting [40]. For instance, in predicting cardiotoxicity, a simple model based on the net block of repolarizing ion channels sometimes outperformed complex biophysical models with hundreds of parameters [40].
The Scientist's Toolkit: Essential Research Reagents and Software
The generation and analysis of patient-specific models rely on a suite of specialized software tools and data formats. The table below catalogs key resources used in advanced computational biomechanics studies.
Table 2: Essential Software and Data Resources for Patient-Specific Modeling
| Tool/Resource Name | Type/Category | Primary Function in Workflow |
|---|---|---|
| 3D Slicer [39] | Medical Imaging Platform | Core platform for image visualization, processing, and analysis. |
| SlicerCBM [39] | Software Extension (3D Slicer) | Provides tools for computational biophysics and biomechanics. |
| Gmsh [39] | Mesh Generator | Generates finite element meshes from geometric data. |
| MFEM [39] | C++ Library | A lightweight, scalable library for finite element method discretizations. |
| FreeSurfer [39] | Neuroimaging Toolkit | Processes, analyzes, and visualizes human brain MR images. |
| STL File Format [38] [39] | Data Format | Represents unstructured triangulated surface geometry. |
| NRRD File Format [39] | Data Format | Stores nearly raw raster image data from medical scanners. |
| VTK/VTU File Formats [39] | Data Format | Visualizes and stores computational grids and simulation results. |
| Abaqus FEA Input File (.inp) [39] | Data Format | Defines finite element models for commercial solvers like Abaqus. |
| Oxetane;heptadecahydrate | Oxetane;heptadecahydrate, CAS:60734-82-9, MF:C3H40O18, MW:364.34 g/mol | Chemical Reagent |
| 2-(But-2-en-1-yl)aniline | 2-(But-2-en-1-yl)aniline, CAS:60173-58-2, MF:C10H13N, MW:147.22 g/mol | Chemical Reagent |
This toolkit enables the end-to-end process from image to simulation. Open-source platforms like 3D Slicer and its SlicerCBM extension facilitate accessible and reproducible image analysis and model generation [39]. The use of widely accepted, open file formats (e.g., STL, NRRD, VTK) ensures interoperability between different software components and promotes data sharing and reuse within the research community [38] [39].
Patient-specific model generation from medical imaging has matured into a powerful paradigm for advancing personalized medicine. The technical comparison demonstrates a clear performance advantage for structured grids in specific applications like vascular simulation, though their adoption requires greater expertise and computational investment. The presented experimental protocols provide a replicable framework for generating high-fidelity models for both cardiovascular and neurosurgical applications.
The future of this field is intrinsically linked to robust VVUQ practices, which are essential for translating computational models into clinical tools [23] [18]. Key emerging trends include the integration of machine learning to analyze large datasets and inform model personalization, and the development of multi-scale modeling frameworks to simulate biological systems from the molecular to the whole-organ level [37]. Furthermore, the emergence of foundation models in AI, trained on vast medical image datasets, promises to enhance tasks like segmentation and classification, moving beyond the limitations of task-specific models and offering more robust solutions to critical clinical challenges [41]. As these technologies converge, patient-specific computational models are poised to become increasingly integral to clinical research, device design, and ultimately, personalized patient care.
This guide objectively compares the application of Verification and Validation (V&V) principles across three key domains of computational biomechanics. For researchers and drug development professionals, rigorous V&V is the critical bridge between computational models and clinically meaningful insights.
In computational biomechanics, verification and validation (V&V) are distinct but interconnected processes essential for establishing model credibility. Verification is the process of ensuring that a computational model accurately represents the underlying mathematical model and its solution ("solving the equations right"). Validation determines the degree to which the model is an accurate representation of the real world from the perspective of its intended uses ("solving the right equations") [1] [13]. The general V&V process flows from the physical reality of interest to a mathematical model (verification domain) and finally to a computational model that is compared against experimental data (validation domain) [1]. The required level of accuracy is dictated by the model's intended use, with clinical applications demanding the most stringent V&V [1].
V&V in Cardiovascular Biomechanics
Cardiovascular models are increasingly used to predict device performance and patient-specific treatments, making robust V&V protocols paramount.
Application Focus and Validation Challenges
A primary application is the digital simulation of cardiovascular devices, including structural and hemodynamic analysis of implants, device optimization, and modeling patient-specific treatments [23]. A significant V&V challenge is managing the inherent biological variability and complexities of generating high-quality in-vitro and in-vivo data for comparison with computational outputs [23]. Furthermore, for models aiming to become virtual human twins of the heart—which incorporate electrophysiology, mechanics, and hemodynamics—a critical focus is placed on verification, validation, and uncertainty quantification (VVUQ) to ensure predictive accuracy [23].
Experimental Protocols for Validation
Validation often involves multi-step workflows. For example, in developing models of the left atrium to study thrombosis in atrial fibrillation (AFib), validation may involve comparing simulated blood flow patterns against in-vivo imaging data from patients [23]. Another advanced protocol involves creating subject-specific cardiac digital twins. These models can be validated by comparing their predictions of cardiac output or wall motion against clinical MRI or echocardiography data collected under various conditions, such as during exercise or after caffeine consumption, which act as "stressors of daily life" [42].
V&V in Musculoskeletal Biomechanics
Musculoskeletal models estimate internal forces and stresses that are difficult to measure directly, necessitating rigorous V&V.
Application Focus and Validation Challenges
Applications range from neuromusculoskeletal (NMS) modeling for predicting limb forces [43] to subject-specific knee joint models for predicting ligament forces and kinematics [30]. A key challenge is the personalization of model parameters, such as ligament material properties. Many models use literature values, but direct calibration to subject-specific data is essential for accuracy [30]. Furthermore, obtaining true "passive" behavior data from living subjects is difficult, as even awake, instructed-to-relax volunteers exhibit involuntary muscle activity that influences kinematics [44].
Experimental Protocols for Validation
A detailed protocol for validating an NMS model of dorsiflexion involves:
- Data Collection: Participants perform isometric dorsiflexion contractions at various force levels (e.g., 5-60% of maximum voluntary contraction). Experimental force profiles are recorded simultaneously with high-density surface electromyography (HD-sEMG) from the tibialis anterior muscle [43].
- Motor Unit Decomposition: The HD-sEMG signals are decomposed offline using algorithms (e.g., Convolution Kernel Compensation in the DEMUSE tool) to identify the discharge times of individual motor units [43].
- Model Prediction & Comparison: A computational framework translates the experimental motor unit discharge characteristics into a subject-specific finite element musculoskeletal simulation. The simulated force profile is then validated against the experimentally measured force profile, with accuracy quantified using metrics like root mean square error (RMSE) and R² values [43] [45].
For joint models, a common protocol involves calibrating a finite element model to in-vivo knee laxity measurements obtained with a specialized device. The model's predictive ability is then validated by simulating activities like a pivot shift test and comparing the predicted kinematics against data from robotic knee simulators or other gold-standard methods [30].
V&V in Soft Tissue Biomechanics
Soft tissues exhibit complex, nonlinear behaviors, and their mechanical properties are critical for accurate modeling.
Application Focus and Validation Challenges
A major focus is on constitutive modeling and personalization of soft tissues, which can be nonlinear, time-dependent, and anisotropic [23]. The development of multiphase models based on porous media theory is a key approach for simulating tissues like intervertebral discs and menisci, which contain solid and fluid phases [23]. The central challenge is personalizing constitutive parameters and boundary conditions from clinical data to investigate normal physiology or disease onset [23]. Validating these models requires matching simulated mechanical responses against experimental tests on tissue samples.
Experimental Protocols for Validation
A protocol for validating passive soft tissue behavior highlights the difficulty of obtaining baseline data. To measure truly passive knee flexion kinematics:
- Subject Preparation: Knee flexion kinematics and muscle activity (EMG) of the vastus lateralis are measured in patients scheduled for surgery [44].
- Multi-Stage Testing: Tests are conducted under three conditions: while the patient is awake and instructed to relax, under propofol sedation, and after administration of a muscle relaxant (rocuronium) to ensure complete muscle paralysis [44].
- Data Analysis: The kinematic results from each condition are compared. Studies show significant differences in fall duration and joint angle between awake and fully relaxed states, providing crucial reference data for validating the passive behavior in computational models [44].
Comparative Analysis of V&V Applications
The table below summarizes the key V&V applications, metrics, and data sources across the three biomechanical domains.
Table 1: Comparative Analysis of V&V Applications in Biomechanical Domains
| Domain | Primary V&V Applications | Key Validation Metrics | Common Experimental Data Sources for Validation |
|---|---|---|---|
| Cardiovascular | Device implantation simulation, hemodynamics, virtual human twins [23] | Device deployment accuracy, flow rates/pressures, clot formation risk [23] | Medical imaging (MRI, CT), in-vitro benchtop flow loops, patient-specific clinical outcomes [23] [42] |
| Musculoskeletal | Neuromusculoskeletal force prediction, subject-specific joint mechanics [43] [30] | Joint kinematics/kinetics, muscle forces, ligament forces [43] [30] | Motion capture, force plates, electromyography (EMG), robotic joint simulators [43] [30] |
| Soft Tissue | Constitutive model personalization, multiphase porous media models [23] | Stress-strain response, fluid pressure, permeability [23] | Biaxial/tensile mechanical testing, indentation, in-vivo joint laxity measurements [23] [44] |
Another critical distinction lies in the methodologies for model personalization and the corresponding sources of uncertainty.
Table 2: Comparison of Model Personalization and Uncertainty in Biomechanics
| Domain | Personalization Focus | Primary Sources of Uncertainty |
|---|---|---|
| Cardiovascular | Patient-specific geometry from medical imaging, material properties of vascular tissue and blood [42] | Biological variability, boundary conditions (e.g., blood pressure), unmeasured stressors (e.g., exercise, caffeine) [23] [42] |
| Musculoskeletal | Subject-specific bone geometry, ligament properties, muscle activation patterns [43] [30] | Motor unit recruitment variability, difficulty in measuring true passive properties, soft tissue artifact in motion capture [43] [44] |
| Soft Tissue | Constitutive model parameters (e.g., stiffness, permeability) for specific tissues [23] | High inter-specimen variability, anisotropic and nonlinear material behavior, testing conditions [23] |
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for Biomechanical V&V
| Item | Function in V&V |
|---|---|
| High-Density Electromyography (HD-EMG) | Records muscle activity from multiple channels to decompose signals and identify individual motor unit discharge times for validating neural drive in NMS models [43]. |
| Robotic Knee Simulator (RKS) | Provides high-accuracy, multi-axis force-displacement measurements from cadaveric specimens, serving as a gold standard for validating subject-specific knee joint models [30]. |
| 3D Motion Capture System | Tracks the three-dimensional kinematics of body segments during movement for validating joint angles and positions predicted by musculoskeletal models [46]. |
| Finite Element Software | Provides the computational environment for implementing and solving complex mathematical models of biomechanical systems, from organs to implants [43] [1]. |
| Knee Laxity Apparatus (KLA) | A non-invasive device designed for in-vivo measurement of joint laxity in living subjects, used for calibrating ligament properties in personalized knee models [30]. |
| 1,2,4,5-Tetrahydropentalene | 1,2,4,5-Tetrahydropentalene|C8H10| |
| 8-Methylnonane-2,5-dione | 8-Methylnonane-2,5-dione|C10H18O2|RUO |
Workflow Diagrams
NMS Force Prediction Validation
The following diagram illustrates the integrated computational and experimental workflow for validating a neuromusculoskeletal model.
V&V Workflow for a Digital Twin
This diagram outlines the iterative V&V process essential for developing a credible digital twin, such as a cardiac model.
Verification and Validation (V&V) form the cornerstone of credible computational biomechanics, ensuring that models accurately represent biological reality. Verification confirms that models are solved correctly, while validation assesses how well they match real-world experimental data [47]. The integration of advanced imaging technologies—Magnetic Resonance Imaging (MRI), micro-Computed Tomography (micro-CT), and motion capture—has revolutionized tissue characterization by providing high-fidelity data for initializing, constraining, and validating computational models. This guide objectively compares the capabilities, performance metrics, and implementation considerations of these imaging modalities within a V&V framework, providing researchers and drug development professionals with evidence-based insights for selecting appropriate technologies for specific applications.
Technology Performance Comparison
Quantitative Performance Metrics
Table 1: Comparative performance metrics for advanced imaging technologies in tissue characterization
| Imaging Modality | Spatial Resolution | Temporal Resolution | Key Strength | Quantitative Accuracy | Primary Applications |
|---|---|---|---|---|---|
| Clinical MRI | ~1 mm | Seconds to minutes | Soft tissue contrast, functional imaging | AUC: 0.923 for iCCA diagnosis [48] | Tumor characterization, organ function |
| Micro-CT | ~10 μm | Minutes | Mineralized tissue microstructure | Identifies 110-734 reliable radiomic features [49] | Bone architecture, dental restorations |
| Optical Motion Capture | Sub-millimeter [50] | >200 Hz [50] | Multi-segment kinematics | Angular accuracy: 2-8° [50] | Joint kinematics, sports biomechanics |
| Markerless Motion Capture | Millimeter range [51] | 30-60 Hz | Ecological validity, convenience | Variable accuracy (sagittal: 3-15°) [50] | Clinical movement analysis, field studies |
V&V Credibility Assessment
Table 2: V&V credibility assessment across imaging modalities
| Credibility Attribute | MRI | Micro-CT | Motion Capture |
|---|---|---|---|
| Validation Data Quality | High soft tissue contrast [48] | Excellent for mineralized tissues [52] | Gold standard for kinematics [50] |
| Uncertainty Quantification | SNR≥40 maintains prediction accuracy [53] | ICC>0.8 for reliable features [49] | Environmental impacts performance [50] |
| Model Integration | Direct initialization of computational models [53] | Direct geometry for FEA [52] | Boundary condition specification |
| Standards Compliance | Emerging radiomics standards [49] | Preclinical validation [49] | ISO-guided validation [47] |
Experimental Protocols and Methodologies
MRI for Tumor Characterization
Protocol Overview: A 2025 study established a protocol for diagnosing intrahepatic cholangiocarcinoma (iCCA) within primary liver cancer using MRI-based deep learning radiomics [48].
Detailed Methodology:
- Patient Cohort: 178 pathologically confirmed PLC patients (training: n=124, test: n=54)
- Image Acquisition: T1-weighted imaging (T1WI), T2WI, DWI, and dynamic contrast-enhanced (DCE) sequences including optimal hepatic artery late phase (AP), venous phase (VP), and 3-minute delayed phase (DP)
- Tumor Segmentation: Two radiologists with >5 years experience delineated region of interest (ROI) on the largest tumor slice using ITK-SNAP software
- Feature Extraction: Employed residual convolutional neural network (Resnet-50) with migration learning
- Model Validation: 10-fold cross-validation with least absolute shrinkage and selection operator (LASSO) for feature refinement
- Performance Assessment: Receiver operating characteristic (ROC) curves, calibration curves, and decision curve analysis (DCA)
Key Results: The MRI-based deep learning radiomics-radiological (DLRRMRI) model achieved AUC of 0.923 in the test cohort, significantly outperforming CT-based models (AUC: 0.880) [48].
Micro-CT for Dental Biomechanics
Protocol Overview: Research published in 2025 developed a validated digital workflow integrating micro-CT with finite element analysis (FEA) for tooth-inlay systems [52].
Detailed Methodology:
- Sample Preparation: Human second molar with fused root, mechanically cleaned and stored in 0.1% thymol solution
- Initial Micro-CT Scanning: Nikon XT H 225 system, 100 kV, 110 µA, 700 ms exposure time, yielding 10×10×10 μm resolution
- Digital Reconstruction: Segmentation and surface model refinement using VGSTUDIO MAX, optimization with Meshmixer
- Physical Prototyping: 3D printing of typodonts using Anycubic Photon Mono 2 with water-wash resin at 50 μm layer height
- Cavity Preparation: Dentist-prepared cavities under dental operating microscope (6x magnification)
- Post-Preparation Scanning: Rescanning at 80 kV, 100 µA, maintaining 10 μm isotropic resolution
- FEA Integration: Virtual restoration design in Exocad, nonlinear FEA under masticatory loading
Output Metrics: Von Mises stress, strain energy density, and displacement distribution at tooth-restoration interfaces [52].
Motion Capture System Validation
Protocol Overview: A 2025 validation study compared the performance of a markerless stereoscopic camera (Zed 2i) against a gold-standard VICON system for balance assessment [51].
Detailed Methodology:
- Experimental Setup: Three conditions - quiet standing, anteroposterior sway, and mediolateral sway
- System Configuration: Zed 2i camera versus VICON marker-based system
- Data Processing: Calculation of center of mass displacement and velocities in x and y directions
- Statistical Analysis: Bland-Altman analysis for non-parametric data, coefficient of determination, and mean square error
Performance Outcome: The markerless system showed significant agreement with VICON in sway tasks, though static conditions were more influenced by sensor noise [51].
Integrated Workflow Visualization
V&V Imaging Integration Workflow
Research Reagent Solutions Toolkit
Table 3: Essential research reagents and materials for imaging-based tissue characterization
| Item | Function | Application Specifics |
|---|---|---|
| Phantom Materials | System calibration and validation | Quantitative radiomics feature validation across scanners [49] |
| Anycubic Water-Wash Resin | 3D printing of anatomical models | Fabrication of typodonts for dental biomechanics studies [52] |
| Thymol Solution (0.1%) | Tissue preservation | Maintains specimen integrity for ex vivo micro-CT studies [52] |
| Reflective Markers | Optical motion capture | Tracking anatomical landmarks with sub-millimeter accuracy [50] |
| Gadolinium-Based Contrast | Tissue enhancement in MRI | Improves soft tissue contrast for tumor characterization [48] |
| Radiomics Software | Image feature extraction | ITK-SNAP for segmentation, proprietary tools for feature calculation [48] |
| 4-Methoxy-4'-pentylbiphenyl | 4-Methoxy-4'-pentylbiphenyl | C18H22O | CAS 58244-49-8 |
Implementation Framework and Decision Guidance
Technology Selection Framework
The choice between imaging modalities should be guided by research questions, tissue properties, and V&V requirements:
Soft Tissue Characterization: MRI excels in soft tissue discrimination and functional assessment, with demonstrated efficacy in tumor classification (AUC: 0.923 for iCCA) [48]. Its multi-parametric capabilities (DWI, DCE) enable initialization of biophysical models for tumor growth prediction [53].
Mineralized Tissues: Micro-CT provides unmatched spatial resolution (~10 μm) for quantifying bone microstructure and biomaterial interfaces [52] [49]. The direct translation of micro-CT data to FEA geometries enables high-fidelity stress analysis in dental and orthopedic applications.
Dynamic Function Assessment: Motion capture technologies balance accuracy and ecological validity. Marker-based systems offer higher accuracy (2-8° angular accuracy) for controlled studies, while markerless systems facilitate field-based research despite reduced precision [50].
V&V Integration Strategies
Successful integration of imaging with computational models requires:
Uncertainty Quantification: Assess how imaging limitations (e.g., SNR, resolution) propagate through modeling pipelines. For MRI-informed tumor models, SNR≥40 maintains acceptable prediction accuracy despite resolution limitations [53].
Validation Experiment Design: Conduct multi-system validation studies, such as comparing markerless against marker-based motion capture [51] or establishing radiomics feature reliability across scanner platforms [49].
Standardized Protocols: Implement standardized imaging protocols and feature extraction methodologies to enhance reproducibility, particularly for radiomics studies where feature reliability varies significantly with acquisition parameters and tissue density [49].
The integration of V&V processes with advanced imaging technologies establishes a rigorous foundation for credible computational biomechanics. Each modality offers distinct advantages: MRI provides superior soft tissue characterization for tumor models, micro-CT enables microscopic geometric accuracy for hard tissue simulations, and motion capture delivers dynamic functional data for musculoskeletal models. The optimal selection depends on specific research questions, tissue properties, and validation requirements. By implementing robust V&V frameworks that acknowledge the capabilities and limitations of each imaging technology, researchers can enhance the predictive power and clinical translation of computational biomechanical models.
Navigating Uncertainty: Sensitivity Analysis and Error Reduction Strategies
Sensitivity Analysis (SA) is a critical methodology in computational biomechanics for quantifying how the uncertainty in the output of a model can be attributed to different sources of uncertainty in its inputs [54]. For researchers engaged in the verification and validation of computational models, SA provides a systematic approach to assess model robustness, identify influential parameters, and guide model simplification and personalization strategies [55] [56] [54]. In the context of drug development and biomedical research, where models often incorporate complex physiological interactions, SA helps to build confidence in model predictions and supports regulatory decision-making by thoroughly exploring the parameter space and its impact on simulated outcomes.
The fundamental mathematical formulation of SA treats a model as a function ( Y = f(X) ), where ( X = (X1, ..., Xp) ) represents the input parameters, and ( Y ) represents the model output [54]. SA methods then work to apportion the variability in the output ( Y ) to the different input parameters ( X_i ). In biomechanical applications, these inputs might include physiological parameters, material properties, kinematic measurements, or neural control signals, while outputs could represent joint torques, tissue stresses, or other clinically relevant quantities [55].
Key Sensitivity Analysis Methods: A Comparative Guide
Various SA methods have been developed, each with distinct strengths, limitations, and computational requirements. The choice of method depends on factors such as model complexity, computational cost, number of parameters, and the presence of correlations between inputs [54].
Table 1: Comparison of Primary Sensitivity Analysis Methods
| Method | Key Principle | Advantages | Limitations | Ideal Use Cases |
|---|---|---|---|---|
| One-at-a-Time (OAT) [54] | Changes one input variable at a time while keeping others fixed | Simple implementation and interpretation; Low computational cost; Direct attribution of effect | Cannot detect interactions between inputs; Does not explore entire input space; Unsuitable for nonlinear models | Initial screening of parameters; Models with likely independent inputs |
| Variance-Based (Sobol') [55] [54] | Decomposes output variance into contributions from individual inputs and their interactions | Measures main and interaction effects; Works with nonlinear models; Provides global sensitivity indices | Computationally expensive; Requires many model evaluations | Final analysis for important parameters; Models where interactions are suspected |
| Morris Method [54] | Computes elementary effects by traversing input space along various paths | More efficient than Sobol' for screening; Provides qualitative ranking of parameters | Does not precisely quantify sensitivity; Less accurate for ranking | Screening models with many parameters; Identifying insignificant parameters |
| Derivative-Based Local Methods [54] | Calculates partial derivatives of the output with respect to inputs at a fixed point | Computationally cheap per parameter; Adjoint methods can compute all derivatives efficiently | Only provides local sensitivity; Results depend on the chosen baseline point | Models with smooth outputs; Applications requiring a sensitivity matrix |
| Regression Analysis [54] | Fits a linear regression to model response and uses standardized coefficients | Simple statistical interpretation; Widely understood methodology | Only captures linear relationships; Can be misleading for nonlinear models | Preliminary analysis; Models with primarily linear relationships |
Advanced Considerations: Correlated Inputs and Computational Efficiency
A significant challenge in applying SA to biomechanical models is the presence of correlated inputs, which can alter the interpretation of SA results and impact model development and personalization [56]. Most traditional SA methods assume statistical independence between model inputs, but biomechanical parameters often exhibit strong correlations due to physiological constraints and interdependencies. Ignoring these correlations may lead to misleading sensitivity measures and suboptimal model reduction.
To address the high computational cost of SA for complex models, surrogate modeling approaches offer an efficient alternative. These methods construct computationally inexpensive approximations (meta-models) of the original complex model, which can then be used for extensive SA at a fraction of the computational cost [56] [54]. For instance, a surrogate-based SA approach applied to a pulse wave propagation model achieved accurate results at a theoretical 27,000× lower computational cost compared to the direct approach [56].
Experimental Protocols for Sensitivity Analysis
Implementing a robust SA requires a structured methodology. The following protocols, drawn from recent biomechanics literature, provide a framework for conducting effective sensitivity studies.
Protocol 1: Global SA for Musculoskeletal Model Simplification
This protocol outlines the steps for performing a variance-based SA to guide the simplification of a musculoskeletal model, as demonstrated in recent research on knee joint torque estimation [55].
- Model Formulation: Establish a detailed musculoskeletal model incorporating relevant physiological components. For example, a knee-joint model might include four major muscles (Biceps Femoris, Rectus Femoris, Vastus Lateralis, Vastus Medialis) and combine advanced Hill-type muscle model components [55].
- Parameter Identification: Use an optimization algorithm (e.g., Genetic Algorithm) to identify personalizable parameters of the model based on experimental data (e.g., electromyography (EMG) signals and motion capture) [55].
- Global Sensitivity Analysis: Apply Sobol's method to compute global sensitivity indices. This involves:
- Sampling: Generating a sufficient number of input parameter sets using Quasi-Monte Carlo sequences.
- Model Evaluation: Running the model for each parameter set to compute the output(s) of interest (e.g., joint torque).
- Index Calculation: Calculating the first-order (main effect) and total-order (including interactions) Sobol' indices for each parameter [55].
- Model Simplification: Fix or remove parameters with low total-order sensitivity indices, as they contribute little to the output variance. The simplified model retains only the most influential parameters.
- Validation: Compare the output of the simplified model against the original model and experimental data to ensure performance is not significantly degraded (e.g., using metrics like Normalized Root Mean Square Error) [55].
SA Workflow for Model Simplification
Protocol 2: Correlated SA for Model Personalization
This protocol is designed for situations where model inputs are correlated, which is common in personalized biomechanical models [56].
- Define Input Uncertainty and Correlation: Specify probability distributions for all uncertain input parameters. Critically, define the correlation structure between parameters based on experimental data or literature.
- Surrogate Model Construction: To overcome computational constraints, build a surrogate model (e.g., a polynomial chaos expansion or Gaussian process emulator) that approximates the original complex model. This is trained on a limited set of model evaluations.
- Correlated Sensitivity Analysis: Perform the SA using the surrogate model. The method must account for the predefined input correlations to calculate accurate sensitivity indices that reflect the dependent nature of the inputs.
- Interpretation and Guidance: Interpret the correlated sensitivity indices to guide model development. This includes:
- Input Prioritization: Identifying which parameters, despite correlations, warrant precise measurement for personalization.
- Input Fixing: Determining which parameters can be fixed to nominal values without significant loss of model accuracy.
- Dependency Analysis: Understanding how the correlation structure itself influences model output [56].
Practical Application: Case Study in Lower-Limb Biomechanics
A recent study on a lower-limb musculoskeletal model provides a clear example of SA application [55]. The research established an EMG-driven model of the knee joint and used Sobol's global sensitivity analysis to examine the influence of parameter variations on joint torque output. The sensitivity results were used not just for analysis but to actively guide a model simplification process. By identifying parameters with low sensitivity indices, researchers reduced the model's complexity while maintaining comparable performance, as measured by the Normalized Root Mean Square Error (NRMSE). This sensitivity-based simplification is crucial for applications requiring real-time computation, such as human-robot interaction control in rehabilitation devices [55].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Materials for Sensitivity Analysis in Biomechanics
| Item / Solution | Function in Sensitivity Analysis |
|---|---|
| Surface Electromyography (sEMG) Sensors [55] | Non-invasive sensors to measure muscle activation signals, which serve as inputs to EMG-driven musculoskeletal models for parameter identification and validation. |
| Motion Capture (MoCap) System [55] | Provides kinematic data (joint angles, positions) necessary for calculating model-based outputs like joint torque, enabling comparison with model predictions. |
| Computational Model Optimization Software (e.g., GA, PSO implementations) [55] | Algorithms used to identify model parameters by minimizing the difference between model outputs and experimental measurements. |
| Global Sensitivity Analysis Library (e.g., Sobol' indices calculator) [55] [54] | Software tools for computing variance-based sensitivity indices from model input-output data, enabling quantification of parameter influence. |
| Surrogate Model Building Tools [56] | Software for constructing meta-models (e.g., polynomial chaos, Gaussian processes) that approximate complex models, making computationally expensive SA feasible. |
Sensitivity analysis is an indispensable component of the verification and validation workflow for computational biomechanics models. By systematically identifying critical parameters, SA helps researchers streamline model personalization, enhance robustness, and build justifiable confidence in model predictions. The choice of SA method—from efficient screening tools like the Morris Method to comprehensive variance-based approaches—must be aligned with the model's characteristics and the study's goals. As computational models play an increasingly vital role in drug development and medical device innovation, the rigorous application of sensitivity analysis will be paramount for generating reliable, actionable results that can effectively inform critical decisions in healthcare and biotechnology.
In computational biomechanics, the finite element method (FEM) has become a fundamental tool for investigating the mechanical function of biological structures, particularly in regions where obtaining experimental data is difficult or impossible [57]. However, model credibility must be established before clinicians and scientists can extrapolate information based on model predictions [57]. This process of establishing credibility falls under the framework of verification and validation (V&V) [58] [59].
Verification is defined as "the demonstration that the numerical model accurately represents the underlying mathematical model and its solution" [57]. A crucial aspect of solution verification is quantifying the discretization error, which arises from approximating a mathematical model with infinite degrees of freedom using a numerical model with finite degrees of freedom [57]. The accuracy of the discrete model solution improves as the number of degrees of freedom increases, with the discretization error approaching zero as the degrees of freedom become infinite [57]. Mesh convergence analysis serves as the primary methodology for estimating and controlling this discretization error.
This guide provides a comprehensive overview of mesh convergence analysis techniques, focusing on their critical role in the verification process within computational biomechanics. We compare different refinement strategies, present standardized protocols, and illustrate these concepts with examples from recent literature to help researchers produce reliable, credible computational results.
Fundamentals of Discretization Error and Convergence
The Mathematical Foundation of Discretization Error
In mechanical engineering, the mathematical model typically consists of coupled, nonlinear partial differential equations in space and time, subject to boundary and/or interface conditions [57]. Such models have an infinite number of degrees of freedom. The numerical model is a discretized version of these differential equations, introducing discretization parameters such as element size and type [57].
The formal method of estimating discretization errors requires plotting a critical result parameter (e.g., a specific stress or strain component) against a range of mesh densities [57]. When successive runs with different mesh densities produce differences smaller than a defined threshold, mesh convergence is achieved [57].
The Critical Role of Mesh Convergence in Model Verification
For computational models to gain acceptance in biomechanics, especially in clinical applications, rigorous verification practices are essential [59]. Discretization error represents one of the most significant numerical errors in finite element analysis, alongside iterative errors and round-off errors [57]. Mesh convergence analysis directly addresses this error source, ensuring that simulation results are not artifacts of mesh selection but accurate representations of the underlying mathematical model.
The importance of proper mesh convergence extends beyond mere academic exercise. Inadequate attention to discretization error can lead to false conclusions, particularly in clinical applications where computational models may inform treatment decisions [58]. For instance, in vascular biomechanics, accurate prediction of transmural strain fields depends on proper mesh refinement [60].
Mesh Convergence Techniques and Protocols
Core Methodological Approaches
Mesh convergence analysis follows a systematic process of refining the mesh until the solution stabilizes within an acceptable tolerance [61]. The fundamental approach involves:
- Selecting a Critical Response Parameter: Identify a specific, mechanically relevant output variable (e.g., maximal normal stress, strain at a specific location, or ultimate buckling resistance) that will serve as the convergence metric [57] [62].
- Iterative Refinement: Successively refine the mesh density and recalculate the critical parameter [61].
- Solution Monitoring: Track changes in the critical parameter across refinement levels [61].
- Convergence Determination: Establish a threshold (often 1-5% difference between successive runs) to determine when further refinement is unnecessary [62].
Table 1: Comparison of Mesh Refinement Strategies
| Refinement Type | Description | Applications | Advantages | Limitations |
|---|---|---|---|---|
| Global (h-refinement) | Uniform reduction of element size throughout the entire model [63] | Simple geometries; homogeneous stress fields | Simple implementation; predictable computational cost | Computationally inefficient for localized phenomena |
| Local Refinement | Selective mesh refinement only in regions of interest [61] | Stress concentrations; complex geometries; contact interfaces | Computational efficiency; focused accuracy | Requires prior knowledge of high-gradient regions |
| Adaptive Refinement | Automated refinement based on solution gradients [61] | Problems with unknown stress concentrations; automated workflows | Optimizes accuracy vs. computational cost | Complex implementation; may require specialized software |
| p-refinement | Increasing element order while maintaining mesh topology [63] | Smooth solutions; structural mechanics | Faster convergence for suitable problems | Limited by geometric representation |
Special Considerations for Biomechanical Applications
Biomechanical systems present unique challenges for mesh convergence due to complex geometries, material nonlinearities, and contact conditions [57]. For athermal fiber networks, researchers have found that modeling individual fibers as quadratic elements with length-based adaptive h-refinement provides the optimum balance between numerical accuracy and computational cost [63].
In cases involving complex interfaces, such as bone-screw systems, convergence behavior can be highly dependent on contact conditions, solution approaches (implicit or explicit), and convergence tolerance values [57]. These factors must be carefully considered when establishing convergence protocols for biomechanical systems.
Experimental Protocols for Convergence Analysis
Standardized Mesh Convergence Protocol
The following workflow provides a standardized protocol for performing mesh convergence analysis in biomechanical finite element studies:
Diagram 1: Mesh convergence analysis workflow
Step 1: Define Quantifiable Objectives
- Select critical response parameters based on the study's mechanical objectives (e.g., maximal principal stress in stress concentration regions, strain energy in deformation analysis, or ultimate buckling load in stability analysis) [57] [62].
- Establish convergence criteria (typically 1-5% difference for engineering applications, though stricter thresholds may be necessary for clinical applications) [62].
Step 2: Establish Baseline Simulation
- Create an initial mesh with coarse element sizing, ensuring proper geometric representation [62].
- Solve the baseline model and extract the critical response parameter(s).
- Document computational resources required for the baseline analysis.
Step 3: Implement Iterative Refinement
- Systematically refine the mesh using h-refinement (reducing element size), p-refinement (increasing element order), or a combination approach [63].
- For local refinement, identify regions of high stress or strain gradients from previous solutions to guide targeted mesh improvement [61].
- Solve each refined model and record the critical parameters and computational requirements.
Step 4: Analyze Convergence Behavior
- Plot the critical parameter values against mesh density (often represented as number of elements or degrees of freedom) [57] [62].
- Calculate the relative difference between successive refinements.
- Continue refinement until the established convergence criterion is met.
Step 5: Document and Report
- Report the final mesh density and the convergence behavior observed [59].
- For publication, include details on the convergence criterion, refinement strategy, and the relationship between mesh density and solution accuracy [59].
Case Study: Cantilever Beam Convergence Analysis
A practical example illustrates this protocol. Researchers performed mesh convergence on a cantilever beam model using both 4-node (QUAD4) and 8-node (QUAD8) plane elements, monitoring maximal normal stress as the critical parameter [62].
Table 2: Mesh Convergence Data for Cantilever Beam Study [62]
| Element Type | Number of Elements | Max Normal Stress (MPa) | Difference from Previous (%) | Computational Time (s) |
|---|---|---|---|---|
| QUAD4 | 1 | 180.0 | - | <1 |
| QUAD4 | 10 | 285.0 | 58.3 | <1 |
| QUAD4 | 50 | 297.0 | 4.2 | <1 |
| QUAD4 | 500 | 299.7 | 0.9 | <1 |
| QUAD8 | 1 | 300.0 | - | <1 |
| QUAD8 | 10 | 300.0 | 0.0 | <1 |
| QUAD8 | 500 | 300.0 | 0.0 | <1 |
The results demonstrate significantly different convergence behaviors between element types. QUAD8 elements achieved the correct solution (300 MPa) even with a single element, while QUAD4 elements required approximately 50 elements along the length to achieve reasonable accuracy (1% error) [62]. This highlights how element selection dramatically affects convergence characteristics and computational efficiency.
Advanced Applications in Biomechanics
Fiber Network Materials
In fiber network simulations, researchers systematically investigate methodological aspects with focus on output accuracy and computational cost [63]. Studies compare both p and h-refinement strategies with uniform and length-based adaptive h-refinement for networks with cellular (Voronoi) and fibrous (Mikado) architectures [63]. The analysis covers linear elastic and viscoelastic constitutive behaviors with initially straight and crimped fibers [63].
For these complex systems, the recommendation is to model individual fibers as quadratic elements discretized adaptively based on their length, providing the optimum balance between numerical accuracy and computational cost [63]. This approach efficiently handles the non-affine deformation of fibers and related non-linear geometric features due to large global deformation [63].
Vascular Biomechanics
In vascular applications, mesh convergence takes on added importance due to the clinical implications of computational results. In one IVUS-based FE study of arterial tissue, researchers selected mesh density according to a convergence test before comparing model-predicted strains with experimental measurements [60]. The accuracy of transmural strain predictions strongly depended on tissue-specific material properties, with proper mesh refinement being essential for meaningful comparisons between computational and experimental results [60].
Practical Implementation Guidelines
The Researcher's Toolkit for Convergence Analysis
Table 3: Essential Components for Mesh Convergence Studies
| Tool/Component | Function in Convergence Analysis | Implementation Considerations |
|---|---|---|
| Parameter Selection | Identifies critical response variables for monitoring convergence | Choose mechanically relevant parameters; avoid stress singularities [61] |
| Refinement Strategy | Determines how mesh improvement is implemented | Balance global and local refinement based on problem geometry [61] |
| Convergence Criterion | Defines acceptable solution stability threshold | Establish discipline-appropriate tolerances (1-5% for engineering) [62] |
| Computational Resources | Manages trade-off between accuracy and practical constraints | Monitor solution time relative to mesh density [63] |
| Documentation Framework | Records convergence process and results for verification | Follow reporting checklists for computational studies [59] |
Relationship Between Mathematical and Numerical Models
Diagram 2: Discretization error in model verification
Overcoming Common Challenges
Several persistent challenges affect mesh convergence studies in biomechanics:
Stress Singularities: These occur when the mesh cannot accurately capture stress concentrations at sharp corners or geometric discontinuities, resulting in unreasonably high stress values that diverge with mesh refinement [61]. Mitigation strategies include remeshing, stress smoothing, and recognizing that these are numerical artifacts rather than physical phenomena [61].
Computational Cost: For large-scale models, full convergence may be computationally prohibitive. Researchers must balance accuracy requirements with available resources, potentially using local refinement strategies and accepting slightly relaxed convergence criteria for less critical regions [63].
Complex Material Behaviors: Nonlinear materials, contact conditions, and large deformations complicate convergence behavior [57]. These require careful attention to both mesh convergence and iterative convergence parameters in nonlinear solution schemes [57].
Mesh convergence analysis represents a fundamental pillar of verification in computational biomechanics. As the field moves toward greater clinical integration and personalized medicine applications, rigorous attention to discretization error becomes increasingly critical. The methodologies outlined in this guide provide researchers with standardized approaches for quantifying and controlling these errors.
The comparison of techniques reveals that no single refinement strategy is optimal for all scenarios. Rather, researchers must select approaches based on their specific geometrical, material, and computational constraints. By implementing systematic convergence protocols and thoroughly documenting the process, the biomechanics community can enhance the credibility of computational models and facilitate their acceptance in scientific and clinical practice.
Future developments in adaptive meshing, error estimation, and high-performance computing will continue to evolve these methodologies, but the fundamental principle remains: mesh convergence analysis is not merely a technical exercise but an essential component of responsible computational biomechanics research.
Addressing Geometry and Material Property Uncertainty in Complex Tissues
Computational models have become indispensable tools in biomedical engineering, providing a non-invasive means to investigate complex tissue mechanics, such as those in the knee joint, and to predict the performance of biomedical implants [64]. However, the reliability of these models is inherently tied to how accurately they represent real-world biological systems. Uncertainty is omnipresent in all modeling approaches, and in bioengineering, its impact is particularly significant due to the clinical relevance of model outputs [65]. These uncertainties can be broadly categorized into two types: aleatory uncertainty, which is related to the intrinsic variation of the system caused by model input parameters, and epistemic uncertainty, which stems from a lack of knowledge about the real system behavior [65].
Geometry and material properties represent two of the most significant sources of uncertainty in models of complex tissues. Geometrical uncertainties arise from multiple factors, including the resolution of medical imaging modalities like MRI, the accuracy of segmentation techniques, and the natural anatomical variability between individuals [64] [65]. For instance, the slice thickness in MRI can introduce specific uncertainties in the direction of the slice, while segmentation errors can be as large as two pixels [64]. Similarly, material properties of biological tissues are inherently variable due to factors such as age, health status, and individual biological variation. Quantifying and managing these uncertainties is not merely an academic exercise; it is essential for supporting diagnostic procedures, pre-operative and post-operative decisions, and therapy treatments [65].
Geometric Uncertainties
Geometric uncertainties in complex tissues originate primarily from the processes of imaging and model reconstruction. A study on knee biomechanics highlighted that geometric uncertainties in cartilage and meniscus resulting from MRI resolution and segmentation accuracy cause considerable effects on predicted knee mechanics [64]. Even when mathematical geometric descriptors closely approximate image-based articular surfaces, the detailed contact pressure distribution they produce differs significantly. Even with high-resolution MRI (0.29 mm pixelâ»Â¹ and 1.5 mm slice thickness), the resulting geometric models contain uncertainties that substantially impact mechanical predictions like contact area and pressure distribution [64].
Table 1: Sources of Geometric Uncertainty in Tissue Modeling
| Source | Description | Impact Example |
|---|---|---|
| Medical Image Resolution | Limited spatial resolution of MRI/CT scanners. | Inability to capture subtle surface features of cartilage and meniscus [64]. |
| Segmentation Accuracy | Errors in delineating structures from images. | Can result in surface errors as large as two pixels; sub-pixel accuracy is challenging [64]. |
| Anatomical Variability | Natural morphological differences across a population. | Morphometrical variations significantly affect model outputs like stress distributions [65]. |
| Slice Thickness | The distance between consecutive image slices. | Introduces specific uncertainties in the direction of the slice, especially with large thickness [64]. |
Material Property Uncertainties
The material properties of biological tissues exhibit significant variability due to their complex, heterogeneous, and often subject-specific nature. Unlike engineered materials, properties like the elastic modulus of cartilage or the fiber stiffness in meniscus are not fixed values but exist within a probabilistic distribution across a population. This variability is a classic form of aleatory uncertainty [65]. For example, in knee models, the cartilage is often assumed to be linear isotropic with an elastic modulus of 15 MPa and a Poisson's ratio of 0.46, while the meniscus is modeled as transversely isotropic with different properties along and orthogonal to the fiber direction [64]. However, these values are typically population averages, and their actual value in any specific individual is uncertain.
A Unified Workflow for Uncertainty Management
Managing uncertainty in computational models requires a systematic pipeline that progresses from identification to analysis. A generalized workflow, adapted from probabilistic analysis in biomedical engineering, is illustrated below. This framework is applicable to both geometric and material property uncertainties.
Quantitative Comparison of Modeling Approaches
Polynomial-Based vs. Image-Based Geometric Descriptors
The method used to define geometry significantly influences model predictions. A comparative study of polynomial-based and image-based knee models reveals critical performance differences. Image-based models, derived directly from 3D medical images, capture detailed geometric features but are limited by MRI resolution and segmentation accuracy [64]. Polynomial-based models use mathematical functions to represent articular surfaces, offering easier generation and meshing, but may lack anatomical fidelity.
Table 2: Comparison of Polynomial-Based vs. Image-Based Knee Models
| Characteristic | Image-Based Model | Polynomial-Based Model (5th Degree) |
|---|---|---|
| Geometric Accuracy | Captures detailed features directly from anatomy. | Approximates surface (RMSE < 0.4 mm) [64]. |
| Contact Pressure Distribution | Provides detailed, localized pressure maps. | Different distribution from image-based model, even with low RMSE [64]. |
| Trend Prediction | Serves as a baseline for mechanical trends. | Predicts similar overall trends to image-based model [64]. |
| Development Workflow | Time-consuming, requires segmentation and 3D reconstruction. | Generally faster to develop and mesh [64]. |
| Meniscus Conformity | Based on actual anatomy. | Often created for perfect conformity with polynomial surfaces [64]. |
Uncertainty Propagation Methods
Once input uncertainties are characterized, they must be propagated through the computational model to determine their impact on the outputs. Propagation methods fall into two main categories: non-intrusive and intrusive. Non-intrusive methods are often preferred in biomedical engineering because they allow the use of commercial finite-element solvers as black-boxes, running ensembles of simulations created by a sampling scheme [65]. In contrast, intrusive approaches require reformulating the governing equations of the model and are typically implemented in specialized, in-house codes [65].
Table 3: Methods for Propagating and Analyzing Uncertainty
| Method | Type | Description | Application Example |
|---|---|---|---|
| Design of Experiments (DOE) | Non-intrusive | Uses predefined discrete values (levels) for input factors to explore combinations [65]. | Cervical cage evaluation (324 runs); foot orthosis design (1024 runs) [65]. |
| Random Sampling (Monte Carlo) | Non-intrusive | Uses numerous simulations with random input values drawn from statistical distributions. | Probabilistic analysis of implant failure across a patient population [65]. |
| Stochastic Collocation | Non-intrusive | Uses deterministic simulations at specific points (collocation points) in the random space. | Efficient propagation of material property variability in tissue models. |
| Stochastic Finite Element Method | Intrusive | Reformulates FE equations to include uncertainty directly in the solution formulation. | Specialized applications requiring integrated uncertainty analysis. |
Experimental Protocols for Model Validation
A Framework for Quantitative Validation
Moving beyond graphical comparisons, robust validation requires quantitative metrics that account for both computational and experimental uncertainties [66]. The concept of a validation metric provides a computable measure for comparing computational results and experimental data. These metrics should ideally incorporate estimates of numerical error, experimental uncertainty, and its statistical character [66]. For example, a confidence interval-based validation metric can be constructed to assess the agreement between a simulated system response quantity (SRQ) and its experimentally measured counterpart at a single operating condition or over a range of inputs [66].
Protocol 1: Sensitivity Analysis of Meniscal Geometry
This protocol is derived from studies investigating the effects of geometric uncertainties in knee joint models [64].
- Objective: To quantify the sensitivity of predicted knee contact mechanics to uncertainties in meniscal geometry arising from MRI resolution and segmentation inaccuracies.
- Materials:
- Computational Model: A validated finite-element model of the medial knee condyle.
- Parameter Variation: Systematically vary the meniscal dimensions, including height (±0.2 mm) and inner/outer radius (up to 1.0 mm), to cover a wide range of potential uncertainties [64].
- Methods:
- Use the intact model as a baseline.
- Create a series of perturbed models with altered meniscal geometry.
- Apply identical loading conditions (e.g., 400 N to simulate two-legged stance) to all models.
- Solve the FE models using a verified and mesh-converged setup.
- Extract output metrics of interest, specifically contact area and contact pressure distribution.
- Output Analysis: Compare the changes in contact area and pressure distribution relative to the baseline model. This quantifies the mechanical impact of geometric uncertainties in the meniscus.
Protocol 2: Dynamic Model Falsification through Time-Resolved Data
This advanced protocol uses a dynamic, multi-condition approach to rigorously test and falsify competing computational models [67].
- Objective: To distinguish between multiple computational models of endothelial cell network formation by comparing their predictions against time-lapse experimental data under varying conditions.
- Materials:
- In Vitro Experiment: Time-lapses of endothelial cell network formation.
- Computational Models: Multiple competing models based on different hypotheses (e.g., Cell Elongation Model, Contact-Inhibited Chemotaxis Model) [67].
- Analysis Pipeline: A custom time-lapse video analysis pipeline (e.g., in ImageJ) to extract dynamical network characteristics.
- Methods:
- Acquire high-quality time-lapse data of the biological process (e.g., angiogenesis).
- Extract a variety of dynamical characteristics (e.g., network remodeling metrics, lacunae size and number) from both the in vitro experiments and the computational simulations.
- Test the response of these dynamical characteristics to a change in initial conditions (e.g., cell density) in both the wet-lab and in silico environments.
- Perform a quantitative comparison of how well each model reproduces the experimental trends, not just a single endpoint.
- Output Analysis: Identify which model best captures the dynamic and multi-condition behavior of the biological system. A model is provisionally accepted only if it can reproduce the experimental trends across different conditions, while others are falsified [67].
The logical flow for this rigorous validation methodology is shown below.
The Scientist's Toolkit: Research Reagent Solutions
This table details key resources and computational tools essential for conducting uncertainty analysis in computational biomechanics.
Table 4: Essential Tools for Uncertainty Quantification in Tissue Modeling
| Tool / Reagent | Function | Application Note |
|---|---|---|
| Commercial FE Solver | Performs core mechanical simulations (e.g., Abaqus, FEBio). | Used as a "black-box" in non-intrusive uncertainty propagation methods [65]. |
| Statistical Sampling Software | Generates input parameter sets from defined distributions (e.g., MATLAB, Python). | Creates ensembles of simulations for Monte Carlo or DOE studies [64] [65]. |
| Medical Imaging Data | Provides the anatomical basis for geometry (e.g., MRI, CT). | Resolution and segmentation accuracy are primary sources of geometric uncertainty [64]. |
| Custom Image Analysis Pipeline | Extracts quantitative, time-resolved data for dynamic validation. | Crucial for falsification-based validation protocols (e.g., in ImageJ) [67]. |
| Polynomial Surface Fitting Tool | Generates mathematical approximations of anatomical surfaces. | Used to create simplified geometric models for comparison with image-based models [64]. |
| Validation Metric Scripts | Quantifies agreement between computation and experiment. | Implements statistical confidence intervals or other metrics for rigorous validation [66]. |
Strategies for Managing Inherent Variability in Biological Data and Boundary Conditions
The efficacy of computational models to predict the success of a medical intervention often depends on subtle factors operating at the level of unique individuals. The ability to predict population-level trends is hampered by significant levels of variability present in all aspects of human biomechanics, including dimensions, material properties, stature, function, and pathological conditions [68]. This biological variability presents a fundamental challenge for verification and validation (V&V) of computational biomechanics models, as model credibility is defined as "the trust, established through the collection of evidence, in the predictive capability of a computational model for a context of use" [69]. Quantifying and integrating physiological variation into modeling processes is therefore not merely an academic exercise but a prerequisite for clinical translation. Where engineered systems typically have a coefficient of variation (CV = σ/μ) of less than 20%, biological systems regularly exhibit coefficients of variation exceeding 50% [68], complicating the transition from traditional engineering to medical applications.
This comparison guide examines current computational strategies for managing biological variability, objectively comparing their performance, experimental requirements, and applicability across different modeling contexts. By framing this analysis within the broader thesis of V&V computational biomechanics research, we provide researchers, scientists, and drug development professionals with evidence-based guidance for selecting appropriate methods for their specific applications.
Quantitative Comparison of Biological vs. Engineered Material Variability
A fundamental distinction between traditional engineering and biomechanics lies in the inherent variability of biological materials. To quantify this difference, we compiled coefficient of variation (CV) values for material properties across multiple studies, contrasting biological tissues with standard engineering materials.
Table 1: Coefficient of Variation Comparison Between Biological and Engineered Materials
| Material Category | Specific Material/Property | Coefficient of Variation (CV) | Implications for Computational Modeling |
|---|---|---|---|
| Engineered Materials | Aluminum (Young's modulus) | 0.02-0.05 | Minimal uncertainty propagation required |
| Steel (yield strength) | 0.02-0.07 | Deterministic approaches typically sufficient | |
| Titanium (fatigue strength) | 0.04-0.08 | Well-characterized design envelopes | |
| Biological Tissues | Cortical bone (stiffness) | 0.10-0.25 | Requires statistical approaches |
| Cartilage (stiffness) | 0.20-0.40 | Significant uncertainty quantification needed | |
| Tendon (ultimate stress) | 0.25-0.45 | Population-based modeling essential | |
| Blood (density) | 0.02-0.04 | One of few biological "constants" |
The dramatic difference in variability levels has profound implications for modeling approaches. While engineered systems can often be accurately represented using deterministic models with safety factors, biological systems require statistical treatment and distribution-based predictions [68]. This variability necessitates specialized strategies throughout the modeling pipeline, from initial data acquisition to final validation.
Comparative Analysis of Variability Management Strategies
Virtual Population and Cohort Modeling
Virtual cohorts represent a paradigm shift from modeling an "average" individual to creating entire populations of models representative of clinical populations, enabling in silico clinical trials that account for biological variability [70]. This approach directly addresses the challenge that "subject-specific models are useful in some cases, but we typically are more interested in trends that can be reliably predicted across a population" [68].
Table 2: Virtual Cohort Generation Methodologies
| Generation Method | Technical Approach | Representative Study | Variability Captured | Validation Requirements |
|---|---|---|---|---|
| Parameter Sampling | Latin Hypercube Sampling, Monte Carlo methods | Cardiac electrophysiology virtual cohorts [70] | Model parameters (e.g., constitutive parameters) | Comparison to population experimental data |
| Model Fitting | Optimization to match individual subject data | Finite element model personalization [23] | Inter-individual geometric and material variations | Leave-one-out cross validation |
| Morphing | Statistical shape modeling | Bone geometry variations [71] | Anatomical shape variations | Comparison to medical imaging data |
| Experimental Integration | Incorporating multiple data modalities | Multiscale cardiac modeling [70] | Multi-scale and multi-physics variability | Hierarchical validation across scales |
The performance of virtual cohort approaches must be evaluated based on their ability to replicate population-level statistics while maintaining physiological plausibility. Successful implementation requires uncertainty quantification and careful consideration of species-specific, sex-specific, age-specific, and disease-specific factors [70].
Boundary Condition Formulation Strategies
Boundary conditions present particular challenges in biomechanical modeling due to the complex interactions between biological structures and their environment. A recent systematic comparison of femoral finite element analysis (FEA) boundary conditions during gait revealed significant differences in predicted biomechanics [71].
Table 3: Boundary Condition Method Performance Comparison for Femoral FEA
| Boundary Condition Method | Femoral Head Deflection (mm) | Peak von Mises Stress (MPa) | Cortical Strains (µε) | Physiological Realism | Implementation Complexity |
|---|---|---|---|---|---|
| Fixed Knee | 0.1-0.3 | 80-120 | 500-800 | Low | Low |
| Mid-shaft Constraint | 0.2-0.4 | 70-110 | 600-900 | Low | Low |
| Springs Method | 0.5-0.8 | 50-80 | 700-1000 | Medium | Medium |
| Isostatic Constraint | 0.7-1.0 | 45-75 | 800-1100 | Medium-High | Medium |
| Inertia Relief (Gold Standard) | 0.9-1.2 | 40-60 | 900-1200 | High | High |
| Novel Biomechanical Method | 0.8-1.1 | 42-62 | 850-1150 | High | Medium |
The novel biomechanical method proposed in the study demonstrated superior performance, with coefficient of determination = 0.97 and normalized root mean square error = 0.17 when compared to the inertia relief gold standard [71]. This method specifically addresses the limitation of directing deformation of the femur head along the femur's mechanical axis without accounting for rotational and anterior-posterior motions during gait [71].
Integrated Multiscale and Multiphysics Frameworks
Multiscale modeling frameworks provide a structured approach to managing variability across spatial and temporal scales. In cardiac electrophysiology, for example, a widely used multi-scale framework begins at the smallest scale with single ion channels, progresses to cellular models describing action potentials, and extends to tissue-level excitation propagation [70].
Diagram: Integrated Multiscale Framework for Managing Biological Variability
This hierarchical approach enables variability to be introduced at the appropriate scale, whether representing ion channel polymorphisms at the molecular level or geometric variations at the organ level. The PRC-disentangled architecture of Large Perturbation Models (LPMs) offers a complementary approach, representing perturbation, readout, and context as separate dimensions to integrate heterogeneous experimental data [72].
Experimental Protocols for Variability Management
Virtual Cohort Generation Protocol
The following detailed methodology outlines the generation of virtual cohorts for computational studies, based on established practices in the field:
Data Collection and Preprocessing: Assemble a comprehensive dataset of relevant biological parameters from experimental measurements, medical imaging, or literature sources. For femoral bone studies, this includes geometric parameters (neck-shaft angle, anteversion angle), material properties (cortical bone modulus, trabecular bone density), and loading conditions (hip contact force magnitude and direction) [71].
Statistical Analysis: Calculate distribution parameters (mean, standard deviation, correlation coefficients) for all collected parameters. Identify significant correlations between parameters to maintain physiological plausibility in generated virtual subjects.
Population Generation: Implement sampling algorithms (e.g., Latin Hypercube Sampling) to generate parameter sets that span the experimental distribution while maintaining correlation structures between parameters.
Model Instantiation: Create individual computational models for each parameter set in the virtual cohort. For finite element models of bone, this involves mesh generation, material property assignment, and application of subject-specific loading conditions [71].
Simulation and Analysis: Execute computational simulations for all virtual subjects and compile results for statistical analysis of outcome distributions.
This protocol directly addresses biological variability by replacing single-simulation approaches with distribution-based predictions that more accurately represent population responses.
Boundary Condition Optimization Protocol
Accurate boundary condition specification is essential for credible computational models. The following experimental protocol enables systematic evaluation of boundary condition formulations:
Systematic Review: Identify commonly used boundary condition approaches in the specific research domain through systematic literature review. For femoral FEA, this revealed five main groupings: fixed knee, springs, mid-shaft constraint, isostatic constraint, and inertia relief methods [71].
Benchmark Definition: Establish gold standard benchmarking metrics based on experimental measurements or highest-fidelity computational methods. For femoral studies, key benchmarks include femoral head deflection (<1 mm), strains (approaching 1000 µε), and stresses (<60 MPa) consistent with physiological observations [71].
Method Implementation: Implement all boundary condition methods in a consistent computational framework using the same underlying geometry, mesh, material properties, and loading conditions.
Comparative Analysis: Quantitatively compare model predictions across all boundary condition methods using established metrics (e.g., coefficient of determination, normalized root mean square error) [71].
Novel Method Development: Based on identified limitations of existing methods, develop improved boundary condition formulations that better replicate physiological behavior while maintaining practical implementation requirements.
This protocol emphasizes the importance of methodological rigor in boundary condition specification, which significantly influences model predictions but is often overlooked in computational biomechanics studies.
Research Reagent Solutions for Variability Management
Table 4: Essential Research Tools for Managing Biological Variability
| Tool Category | Specific Solution | Function in Variability Management | Representative Applications |
|---|---|---|---|
| Computational Modeling Platforms | FEBio, OpenSim | Implement boundary conditions and solve boundary value problems | Quasi-static FEA of bones and joints [71] |
| Statistical Analysis Tools | R, Python (scikit-learn) | Generate virtual cohorts, perform uncertainty quantification | Population-based modeling of cardiac function [70] |
| Medical Image Processing | 3D Slicer, ITK-SNAP | Extract patient-specific geometries for model personalization | Subject-specific musculoskeletal modeling [4] |
| Data Standardization | SBML, CellML | Enable model reproducibility and interoperability | Systems biology model encoding [69] |
| Uncertainty Quantification Libraries | UQLab, Chaospy | Propagate variability through computational models | Sensitivity analysis of constitutive parameters [68] |
| High-Performance Computing | SLURM, cloud computing platforms | Enable large-scale virtual cohort simulations | Multi-scale cardiac modeling [70] |
These research reagents form the foundation for implementing the variability management strategies discussed throughout this guide. Their selection should be guided by the specific context of use, available resources, and expertise within the research team.
Managing inherent variability in biological data and boundary conditions remains a fundamental challenge in computational biomechanics. The strategies compared in this guide demonstrate that no single approach is optimal for all applications; rather, selection depends on the specific context of use, available resources, and required predictive accuracy. Virtual cohort approaches excel when population-level predictions are needed, while advanced boundary condition methods are essential for tissue-level stress and strain predictions. The emerging integration of mechanistic and data-driven modeling approaches promises enhanced capability for managing biological variability while maintaining physiological fidelity [70].
As the field progresses toward increased model credibility and clinical translation, adherence to established standards such as the CURE principles (Credible, Understandable, Reproducible, and Extensible) becomes increasingly important [73]. By implementing the comparative strategies outlined in this guide and rigorously validating against experimental data, researchers can enhance the impact and trustworthiness of computational biomechanics models in biomedical applications.
In computational biomechanics, the relationship between model complexity and predictive accuracy is not linear. While increasing a model's sophistication often enhances its biological realism, it simultaneously escalates computational demands, data requirements, and the risk of overfitting. This creates a critical trade-off that researchers must navigate to develop models that are both scientifically valid and practically usable. The field is increasingly adopting a "fit-for-purpose" modeling philosophy, where optimal complexity is determined by the specific research question and context of use, rather than pursuing maximum complexity indiscriminately. This guide examines this balance through quantitative comparisons of contemporary modeling approaches, their validation methodologies, and performance metrics, providing researchers with evidence-based frameworks for selecting and optimizing biomechanical models.
Quantitative Comparison of Biomechanical Modeling Approaches
The table below synthesizes performance data for prominent biomechanical modeling approaches, highlighting the inherent trade-offs between computational expense and predictive capability across different application domains.
Table 1: Performance Comparison of Biomechanical Modeling Approaches
| Modeling Approach | Representative Tools/Platforms | Predictive Accuracy (Key Metrics) | Computational Cost & Implementation Requirements | Primary Applications & Validation Status |
|---|---|---|---|---|
| AI/ML for Sports Biomechanics | Custom CNN/RF implementations [74] | • CNN: 94% expert agreement (technique) [74]• Computer vision: ±15mm vs. marker-based [74]• Random Forest: 85% injury prediction [74] | • High data requirements• Significant preprocessing• Specialized ML expertise | • Athletic performance optimization• Injury risk prediction• Moderate-quality validation evidence |
| Reinforcement Learning (Postural Control) | Custom RL framework [75] | • Reproduces ankle-to-hip strategy transition [75]• Matches human kinematic patterns across perturbations [75] | • Nonlinear optimization demands• Complex reward structuring• Biomechanical constraint modeling | • Human movement strategy analysis• Neuromechanical control hypotheses• Single-study validation |
| Real-Time Musculoskeletal Modeling | Human Body Model (HBM) [76] | • Validated against OpenSim [76]• Real-time kinetics/kinematics [76]• Robust to marker dropout [76] | • Global optimization efficiency• Minimal anthropometrics needed [76]• Integrated hardware/software | • Clinical gait analysis• Real-time biofeedback• Multi-site validation |
| Computer Vision-Based Analysis | VueMotion [77] | • Scientifically validated algorithms [77]• Comprehensive biomechanical profiles [77] | • Smartphone accessibility [77]• Minimal equipment (5 cones) [77]• Cloud processing | • Field-based athletic assessment• Movement efficiency screening• Proprietary validation |
| Conventional Motion Capture | Cortex/Motion Analysis [78] | • Laboratory-grade precision [78]• Subtle movement tracking [78]• Integrated force platform data | • Marker-based system complexity• Fixed laboratory setting• High equipment investment | • Basic research validation• Robotics/animation• Extensive historical validation |
Experimental Protocols for Model Validation
AI Model Validation in Sports Biomechanics
The scoping review on AI in sports biomechanics employed rigorous methodology following PRISMA-ScR guidelines to assess model performance across 73 included studies [74]. The validation protocol included:
- Cross-Validation Framework: 10-fold cross-validation was implemented in multiple studies to optimize hyperparameters and prevent overfitting, with performance metrics calculated across all folds [74] [79].
- Comparison to Gold Standards: Computer vision systems were validated against marker-based motion capture (the laboratory gold standard), demonstrating mean accuracy within 15mm across 6 studies classified as moderate quality evidence [74].
- Expert Benchmarking: Convolutional Neural Networks (CNNs) for technique assessment were evaluated against international expert ratings, achieving 94% agreement based on moderate-quality evidence from 12 studies [74].
- Prospective Temporal Validation: Optimal Support Vector Machine (SVM) models for biomechanical prediction maintained high accuracy (AUC = 0.984) in prospective validation cohorts, demonstrating robustness beyond initial training data [79].
Reinforcement Learning for Postural Control Transitions
The investigation into postural control strategies employed a sophisticated reinforcement learning framework to model human responses to perturbations [75]. The experimental protocol included:
- Biomechanical Constraint Modeling: The CoP (Center of Pressure) range limitation was incorporated as a penalty function that increased exponentially as the CoP approached its biomechanical limit, creating a nonlinear optimization problem [75].
- Reward Function Design: The objective function combined three key components: upright posture recovery (rewarding minimal deviation from vertical), effort minimization (penalizing joint torques), and CoP constraint adherence [75].
- Human Validation Data: Model outputs were compared to experimental data from 13 healthy adults responding to backward support surface translations at seven magnitudes (3-15cm), with kinematic data captured at 120Hz and force data at 480Hz [75].
- Transition Quantification: Strategy transitions were quantified through coordinated changes in joint kinematics and corresponding joint torques of both ankle and hip joints in response to increasing perturbation magnitudes [75].
Visualization of Modeling Workflows and Relationships
Biomechanical Model Optimization Pathway
AI Model Validation Workflow
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Essential Research Tools for Computational Biomechanics
| Tool/Category | Specific Examples | Function & Application | Implementation Considerations |
|---|---|---|---|
| Motion Capture Systems | Cortex Software [78], HBM [76] | Provides kinematic and kinetic input data for model development and validation | • Laboratory vs. field deployment• Marker-based vs. markerless• Real-time capability requirements |
| AI/ML Frameworks | CNN [74], Random Forest [74], SVM [79] | Pattern recognition in complex biomechanical datasets; predictive modeling | • Data volume requirements• Explainability needs• Computational resource availability |
| Biomechanical Modeling Platforms | Human Body Model [76], BoB Software [80] | Musculoskeletal modeling and simulation; hypothesis testing | • Integration with experimental data• Customization capabilities• Validation requirements |
| Validation Methodologies | 10-fold cross-validation [79], Prospective temporal validation [79] | Assessing model generalizability and preventing overfitting | • Dataset partitioning strategies• Comparison to appropriate benchmarks• Clinical vs. statistical significance |
| Computer Vision Solutions | VueMotion [77] | Markerless motion capture; field-based assessment | • Accuracy vs. practicality trade-offs• Environmental constraints• Data processing pipelines |
Optimizing model complexity in computational biomechanics requires careful consideration of the intended application context and available resources. Evidence indicates that simpler, more interpretable models often outperform complex black-box approaches when data is limited, while sophisticated AI/ML methods excel in data-rich environments with appropriate validation. The most effective modeling strategy aligns technical capabilities with practical constraints, employing rigorous validation frameworks that include cross-validation, comparison to gold standards, and prospective testing. As the field advances, emphasis on explainable AI, standardized validation protocols, and reproducible workflows will be crucial for translating computational models into clinically and practically impactful tools. Researchers should select modeling approaches through this lens of "fit-for-purpose" optimization rather than defaulting to either maximally complex or minimally sufficient solutions.
Establishing Predictive Power: Validation Frameworks and Model Comparison
In computational biomechanics, the predictive power and clinical applicability of any model are contingent on the robustness of its validation. Verification and Validation (V&V) form the foundational framework for establishing model credibility, ensuring that simulations not only solve equations correctly (verification) but also accurately represent physical reality (validation) [81]. As these models increasingly inform clinical decision-making—from predicting aneurysm development to planning cryoballoon ablation procedures—the design of validation experiments spanning from simple benchmarks to complex clinical data becomes paramount [82] [83]. This guide systematically compares validation approaches across this spectrum, providing experimental protocols and quantitative comparisons to aid researchers in building trustworthy computational frameworks.
The critical importance of rigorous validation is particularly evident in cardiovascular applications, where even minor inaccuracies can significantly impact patient-specific treatment outcomes for conditions responsible for nearly 30% of global deaths [83]. Similarly, in forensic biomechanics, reconstructing injury-related movements requires biofidelic computational human body models validated against reliable passive kinematic data, which is notoriously challenging to acquire from awake volunteers due to involuntary muscle activity [84]. This article examines how validation strategies evolve across the complexity continuum, from controlled benchtop setups to the inherent variability of clinical and in-vivo environments.
Comparison of Validation Experiment Paradigms
Validation in computational biomechanics employs a multi-faceted approach, with each methodology offering distinct advantages and limitations. The table below provides a comparative overview of three primary validation paradigms.
Table 1: Comparison of Validation Experiment Paradigms in Computational Biomechanics
| Validation Paradigm | Key Applications | Data Outputs | Control Level | Biological Relevance | Primary Use in Validation |
|---|---|---|---|---|---|
| In-Vitro Benchmarks | Cardiovascular device hemodynamics [23], implant performance [85], material property characterization [86] | Pressure, flow rates, strain fields, durability cycles | High | Low-Medium | Component-level model validation under controlled boundary conditions |
| Pre-Clinical/Ex-Vivo Models | Bone mechanics [85], soft tissue constitutive laws [23], passive joint kinematics [84] | Force-displacement curves, structural stiffness, failure loads, kinematic trajectories | Medium | Medium-High | Subsystem-level validation of tissue mechanics and geometry |
| Clinical & In-Vivo Data | Patient-specific treatment planning [82] [83], disease progression (e.g., aneurysms) [83], human movement analysis [87] | Medical images (MRI, CT), motion capture kinematics, electromyography (EMG), clinical outcomes | Low | High | Whole-system validation and personalization of digital twins |
In-Vitro Benchmark Experiments
In-vitro experiments provide standardized, highly controlled environments ideal for isolating specific physical phenomena and performing initial model validation. In cardiovascular device development, for instance, benchtop setups are crucial for validating computational fluid dynamics (CFD) models of devices like flow diverters (FDs) or woven endo-bridges (WEB) used in aneurysm treatment [85]. These systems allow for precise measurement of hemodynamic variables such as wall shear stress and pressure gradients, which are critical for predicting device efficacy and thrombosis risk [23].
Typical Experimental Protocol: Cardiovascular Device Hemodynamics
- Setup: A transparent flow loop mimicking the patient-specific vasculature is created using 3D-printed or cast models from medical imaging data. The device (e.g., a flow diverter stent) is implanted in the model under fluoroscopic guidance.
- Flow Conditioning: A pulsatile flow pump circulates a blood-mimicking fluid with matched viscosity and density at physiological flow rates and waveforms.
- Data Acquisition: High-speed cameras paired with Digital Particle Image Velocimetry (DPIV) capture flow fields. Simultaneously, pressure transducers and flow sensors measure pressure drops and flow rates.
- Validation Metric: The computational model (e.g., a Fluid-Structure Interaction simulation) is validated by comparing the simulated velocity fields, pressure distributions, and shear stresses against the experimental measurements [23].
Pre-Clinical and Ex-Vivo Models
Ex-vivo models, including cadaveric tissues, offer a middle ground by preserving the complex material properties and hierarchical structure of biological tissues. A key application is validating the passive mechanical behavior of joints, which is essential for accurate musculoskeletal models. A 2025 study highlights the particular challenge of acquiring pure passive kinematics data from awake subjects, who cannot fully suppress muscle tone, leading to significant variability [84].
Detailed Experimental Protocol: Gravity-Induced Passive Knee Flexion This protocol, designed for validating computational human body models, quantifies the influence of muscle tone on passive joint behavior [84].
- Subject Preparation: Eleven patients scheduled for abdominal surgery were tested under three sequential conditions: awake (C), anesthetized with propofol (A), and anesthetized after administration of a muscle relaxant (AR). Surface EMG electrodes were placed on the vastus lateralis muscle.
- Test Setup: The patient lay supine with the right heel placed on a support, allowing the lower leg to hang freely. A consistent initial knee angle was established for reproducibility.
- Testing Procedure: The foot support was released via a manual switch, initiating a gravity-induced knee flexion. Kinematics were captured, and EMG activity was recorded simultaneously. Each patient underwent three trials per condition (C, A, AR).
- Key Quantitative Findings:
- The median time to reach 47° of knee flexion was longest in awake trials (404 ms), compared to anesthetized (355 ms) and anesthetized+relaxed trials (349 ms).
- Statistical analysis (p < 0.001) confirmed that kinematics under muscle relaxation differ significantly from both anesthetized and awake states.
- Only 15% of awake trials showed no measurable EMG activity, proving that true passive behavior is unattainable in awake volunteers [84].
This study provides crucial reference data for model validation, demonstrating that baseline passive kinematics for musculoskeletal models require data from subjects under anesthesia and muscle relaxation, not from self-reported relaxed, awake individuals.
Clinical and In-Vivo Data Integration
The ultimate test for many biomechanical models is their performance against real-world clinical data. This involves using patient-specific imaging, motion capture, and other in-vivo measurements to validate and personalize models, a cornerstone of the digital twin paradigm in medicine [23] [83]. For example, validating a computational heart model involves comparing simulated wall motions, blood flow patterns, and pressure-volume loops against clinical MRI and catheterization data [23].
Experimental Protocol: Patient-Specific Movement Analysis
- Data Collection: Participants perform functional tasks (e.g., gait, hopping) while their movement is recorded by a 3D motion capture system and ground reaction forces are measured with force platforms. EMG data may be collected concurrently [87].
- Model Personalization: A subject-specific musculoskeletal model is created by scaling a generic model based on the individual's anthropometry, derived from motion capture marker positions or medical images.
- Inverse Dynamics: The experimental kinematics and kinetics data are used to compute joint angles, moments, and forces.
- Validation: The outputs of a forward-dynamics simulation (e.g., a finite element knee model) are compared against the experimentally derived joint kinematics and kinetics. A study on multiple-hop tests found that kinetic variables (e.g., forces, impulses) were far more sensitive in detecting movement asymmetries (asymmetries up to 95.4%) than kinematic outcome variables like hop distance (asymmetries below 28.9%), highlighting the importance of selecting appropriate validation metrics [87].
The Validation Workflow and Its Components
The following diagram illustrates the hierarchical and iterative process of designing robust validation experiments, moving from simple benchmarks to clinical data.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of validation experiments requires specific tools and methodologies. The table below catalogs key solutions and their applications, as evidenced in the search results.
Table 2: Key Research Reagent Solutions for Biomechanics Validation
| Tool/Material | Function in Validation | Application Example |
|---|---|---|
| Blood-Mimicking Fluid | Replicates viscosity and density of blood for in-vitro hemodynamic studies | Validating CFD models of cardiovascular devices [23] |
| Propofol & Muscle Relaxants | Induces general anesthesia and muscle paralysis for measuring true passive kinematics | Acquiring baseline passive joint data for musculoskeletal model validation [84] |
| High-Speed Cameras & Motion Capture | Captures high-frame-rate kinematic data for dynamic movement analysis | Validating joint kinematics and kinetics in sports biomechanics and gait [86] [87] |
| Force Platforms | Measures ground reaction forces and moments during movement | Input and validation data for inverse dynamics simulations [87] |
| Micro-CT / Nano-CT | Provides high-resolution 3D images of tissue microstructure (bone, vessels) | Generating geometric models and validating simulated strain distributions [86] |
| Advanced MRI (DTI, MRE) | Characterizes in-vivo tissue properties like fiber orientation and mechanical stiffness | Personalizing and validating material properties in finite element models [86] |
| Surface Electromyography (EMG) | Records electrical activity produced by skeletal muscles | Quantifying muscle activation levels in volunteer studies for model input/validation [84] |
Designing robust validation experiments is a progressive and multi-stage endeavor fundamental to building credibility in computational biomechanics. As explored, this journey navigates from the high-control, component-level focus of in-vitro benchmarks, through the biologically relevant complexity of ex-vivo and pre-clinical models, to the ultimate challenge of clinical data integration. The quantitative data and detailed protocols presented here, from the validation of passive knee kinematics to cardiovascular device performance, provide a framework for researchers. Adherence to this rigorous, hierarchical approach to validation, underscored by uncertainty quantification and standardized reporting, is what ultimately transforms a computational model from an interesting research tool into a reliable asset for scientific discovery and clinical translation.
In the field of computational biomechanics, model validation is the critical process of determining the degree to which a computational model accurately represents the real world from the perspective of its intended uses [1]. This process fundamentally involves quantifying the agreement between model predictions and experimental data to establish credibility for model outputs [13]. As computational models increasingly inform scientific understanding and clinical decision-making—from estimating hip joint contact forces to predicting tissue-level stresses—the need for robust, quantitative validation metrics has become paramount [88]. Without rigorous validation, model predictions remain speculative, potentially leading to erroneous conclusions in basic science or adverse outcomes in clinical applications [1].
Validation is distinctly different from verification, though both are essential components of model credibility. Verification addresses whether "the equations are solved right" from a mathematical standpoint, while validation determines whether "the right equations are solved" from a physics perspective [1] [13]. This guide focuses specifically on the latter, presenting a structured approach to assessing predictive accuracy through quantitative comparison methodologies. The increasing complexity of biological models, which often incorporate intricate solid-fluid interactions and complex material behaviors not found in traditional engineering materials, makes proper validation both more challenging and more essential [1].
Foundational Concepts of Model Validation
The validation process begins with recognizing that all models contain some degree of error, defined as the difference between a simulated or experimental value and the truth [1]. In practice, "absolute truth" is unattainable for biological systems, so the engineering approach relies on statistically meaningful comparisons between computational and experimental results to assess both random (statistical) and bias (systematic) errors [1] [13]. The required level of accuracy for any given model depends fundamentally on its intended use, with clinical applications typically demanding more stringent validation than basic science investigations [1].
A crucial conceptual framework in validation is that it must precede through a logical progression, beginning with the physical system of interest and proceeding through conceptual, mathematical, and computational model stages before culminating in the validation assessment itself [13]. This systematic approach ensures that errors are properly identified and attributed to their correct sources, whether in model formulation (conceptual), implementation (mathematical), or solution (computational). By definition, verification must precede validation to separate errors due to model implementation from uncertainty due to model formulation [1].
Quantitative Metrics for Assessing Agreement
Statistical Comparison Metrics
Table 1: Primary Quantitative Metrics for Validation
| Metric | Calculation | Interpretation | Application Context |
|---|---|---|---|
| Correlation Coefficient | Measures linear relationship between predicted and experimental values | Values接近 1 indicate strong agreement; used in musculoskeletal model validation [88] | Time-series data comparison (e.g., joint forces, muscle activations) |
| Root Mean Square Error (RMSE) | $\sqrt{\frac{1}{n}\sum{i=1}^{n}(y{pred,i}-y_{exp,i})^2}$ | Lower values indicate better agreement; absolute measure of deviation | Overall error assessment in continuous data |
| Normalized RMSE | RMSE normalized by range of experimental data | Expresses error as percentage of data range; facilitates cross-study comparison | When experimental data ranges vary significantly |
| Kullback-Leibler Divergence | $\int\Theta\pi1(\theta)\log\frac{\pi1(\theta)}{\pi2(\theta)}d\theta$ [89] | Measures information loss when one distribution approximates another; zero indicates identical distributions | Comparing probability distributions rather than point estimates |
Advanced Bayesian Approaches
Beyond traditional statistical metrics, Bayesian methods offer powerful approaches for quantitative validation, particularly when dealing with epistemic uncertainty (uncertainty due to lack of knowledge) as opposed to aleatory uncertainty (uncertainty due to randomness) [89]. The Data Agreement Criterion (DAC), based on Kullback-Leibler divergences, measures how one probability distribution diverges from a second probability distribution, providing a more nuanced assessment than simple point-to-point comparisons [89]. This approach is especially valuable when comparing expert beliefs or prior distributions with experimental outcomes, as it naturally incorporates uncertainty estimates into the validation process.
Bayes factors represent another advanced approach, where different experts' beliefs or model formulations are treated as competing hypotheses [89]. The marginal likelihood of the data under each prior distribution provides an indication of which expert's prior belief gives most probability to the observed data. The Bayes factor, as a ratio of marginal likelihoods, provides odds in favor of one set of beliefs over another, creating a rigorous quantitative framework for model selection and validation [89].
Experimental Protocols for Validation
General Validation Methodology
A robust validation protocol requires carefully designed experiments that capture the essential physics the model intends to simulate. The general workflow involves: (1) establishing the physical system of interest with clearly defined quantities to be measured; (2) designing and executing controlled experiments to collect high-quality benchmark data; (3) running computational simulations of the experimental conditions; and (4) performing quantitative comparisons using the metrics described in Section 3 [13]. This process should be repeated across multiple loading scenarios, boundary conditions, and specimens to establish the generalizability of validation results.
Case Study: Hip Joint Model Validation
Table 2: Validation Protocol for Musculoskeletal Hip Model
| Protocol Component | Implementation Details | Quantitative Outcomes |
|---|---|---|
| Experimental Data Collection | In vivo measurement from instrumented total hip arthroplasty patients during dynamic tasks [88] | Hip contact forces (HCFs) in body weights (N/BW); electromyography (EMG) data for muscle activations |
| Model Prediction | Modified 2396Hip musculoskeletal model simulating same dynamic tasks with increased range of motion capacity [88] | Estimated HCFs and muscle activation patterns |
| Comparison Metrics | Difference in minimum and maximum resultant HCFs; correlation coefficients for muscle activation patterns [88] | HCF differences of 0.04-0.08 N/BW; "strong correlations" for muscle activations |
| Validation Conclusion | Model deemed "valid and appropriate" for estimating HCFs and muscle activations in young healthy population [88] | Model suitable for simulating dynamic, multiplanar movement tasks |
The hip joint validation study exemplifies key principles of effective validation protocols. First, it uses direct in vivo measurements as the gold standard rather than proxy measures. Second, it validates multiple output quantities—both joint forces and muscle activations—across dynamic, multiplanar tasks rather than simple single-plane motions. Third, it establishes quantitative criteria for acceptable agreement rather than relying on qualitative assessments [88]. This comprehensive approach provides greater confidence in model predictions when applied to clinical questions or research investigations.
Sensitivity Analysis in Validation
An often overlooked but critical component of validation is sensitivity analysis, which assesses how variations in model inputs affect outputs [1]. Sensitivity studies help identify critical parameters that require tight experimental control and provide assurance that validation results are robust to expected variations in model inputs [1]. These analyses are particularly important in patient-specific models where unique combinations of material properties and geometry are coupled, introducing additional sources of uncertainty [1]. Sensitivity analysis can be performed both before validation (to identify critical parameters) and after validation (to ensure experimental results align with initial estimates) [1].
Conceptual Framework of Validation Metrics
The relationship between different validation approaches and their mathematical foundations can be visualized as a hierarchical structure, with increasing statistical sophistication from basic point comparisons to full distributional assessments. This progression represents the evolution of validation methodology from simple quantitative comparisons to approaches that fully incorporate uncertainty quantification.
Essential Research Reagents and Tools
Table 3: Research Toolkit for Validation Studies
| Tool/Reagent Category | Specific Examples | Function in Validation |
|---|---|---|
| Computational Platforms | OpenSim (v4.4) [88], Finite Element Software | Provides environment for implementing and solving computational models |
| Experimental Measurement Systems | Instrumented implants [88], Motion capture, Force plates | Collects in vivo biomechanical data for comparison with model predictions |
| Statistical Analysis Tools | R, Python (SciPy, NumPy), MATLAB | Implements quantitative validation metrics and statistical comparisons |
| Sensitivity Analysis Methods | Monte Carlo simulation [13], Parameter variation studies | Quantifies how input uncertainties propagate to output variability |
| Data Collection Protocols | Dynamic multiplanar tasks [88], Controlled loading scenarios | Generates consistent, reproducible experimental data for validation |
Quantitative validation through rigorous assessment of agreement between predictions and experimental data remains the cornerstone of credible computational biomechanics research. The metrics and methodologies presented in this guide—from traditional correlation coefficients and error measures to advanced Bayesian approaches—provide researchers with a comprehensive toolkit for establishing model credibility. As the field continues to evolve toward more complex biological systems and increased clinical application, the importance of robust, quantitative validation will only grow. By adopting these systematic approaches and clearly documenting validation procedures, researchers can enhance peer acceptance of computational models and accelerate the translation of biomechanics research to clinical impact.
Computational biomechanics has become an indispensable tool for understanding human movement, diagnosing pathologies, and developing treatment strategies. Within this field, the prediction of joint forces and kinematics is fundamental for applications in rehabilitation, sports science, and surgical planning. As the complexity of these models grows, ensuring their reliability through rigorous verification and validation (V&V) processes becomes paramount. Verification ensures that "the equations are solved right" (mathematical correctness), while validation determines that "the right equations are solved" (physical accuracy) [1]. This guide provides a comparative analysis of contemporary modeling pipelines for joint force and kinematic predictions, framing the evaluation within the critical context of V&V principles to assist researchers in selecting and implementing robust computational approaches.
Comparative Performance of Modeling Pipelines
Different computational approaches offer varying advantages in terms of prediction accuracy, computational efficiency, and implementation requirements. The table below summarizes the quantitative performance of several prominent methods based on experimental data.
Table 1: Performance Comparison of Joint Force and Kinematic Prediction Models
| Modeling Approach | Primary Input Data | Key Outputs | Performance Metrics | Computational Context |
|---|---|---|---|---|
| Artificial Neural Networks (ANN) [90] [91] | Ground Reaction Forces (GRFs), Motion Capture | Joint Moments, EMG Signals, Knee Contact Forces (KCFs) | Joint Moments: R = 0.97 [91]EMG Signals: R = 0.95 [91]KCFs: Pearson R = 0.89-0.98 (Leave-Trials-Out) [90] | High speed, suitable for real-time applications; eliminates need for complex musculoskeletal modeling [90] [91]. |
| Random Forest (RF) [92] | IMUs, EMG Signals | Joint Kinematics, Kinetics, Muscle Forces | Outperformed SVM and MARS; comparable to CNN with lower computational cost [92]. | Effective for both intra-subject and inter-subject models; handles non-linear relationships well [92]. |
| Convolutional Neural Networks (CNN) [92] | IMUs, EMG Signals | Joint Kinematics, Kinetics, Muscle Forces | High accuracy; outperformed classic neural networks in gait time-series prediction [92]. | Requires automatic feature extraction (e.g., Tsfresh package); higher computational cost than RF [92]. |
| Support Vector Regression (SVR) [90] | Motion Capture, Musculoskeletal Modeling-derived variables | Medial and Lateral Knee Contact Forces | Demonstrated promising prediction performance but was outperformed by ANNs in KCF prediction [90]. | Notable generalization ability to unseen datasets [90]. |
Key Insights from Comparative Data
- ANN Dominance for Real-Time Prediction: ANNs demonstrate exceptional accuracy in predicting lower limb joint moments and EMG signals directly from GRF data, with high correlation coefficients (R ≥ 0.95) [91]. This approach bypasses traditional, computationally intensive musculoskeletal modeling, enabling real-time applications such as clinical gait analysis and dynamic assistive device control [90] [91].
- Wearable Sensor Integration with RF and CNN: For predictions based on wearable sensors (IMUs and EMG), both Random Forest and Convolutional Neural Networks deliver high performance [92]. RF is notable for its balance of high accuracy and lower computational cost, making it a practical choice for clinical settings with limited resources [92].
- Performance Variation with Data Splitting Strategy: The methodology for partitioning training and test data significantly impacts model performance. For instance, ANN predictions for Knee Contact Forces showed high accuracy (R = 0.89-0.98) when tested on new trials from the same subjects (
LeaveTrialsOut) but lower accuracy (R = 0.45-0.85) when tested on entirely new subjects (LeaveSubjectsOut) [90]. This underscores the challenge of model generalizability across diverse populations.
Experimental Protocols and Methodologies
A critical understanding of the experimental protocols behind the data is essential for assessing model validity and reproducibility.
Protocol for ANN-based Joint Moment and EMG Prediction
This protocol [91] aimed to predict joint moments and EMG signals using only ground reaction force (GRF) data.
- Data Collection: A large dataset of 363 trials from 4 datasets was used for joint moment prediction, and 63 trials from 2 datasets for EMG prediction. The input features were the three-dimensional GRF signals. The target outputs were the joint moment timeseries for the ankle, knee, and hip, and the EMG timeseries for six major lower-limb muscles.
- Model Training and Validation: An Artificial Neural Network (ANN) was trained to establish the non-linear relationship between the input GRFs and the target outputs. Model performance was validated using correlation analysis (R-value) between the predicted and experimentally measured timeseries.
Diagram: Workflow for ANN-Based Joint Moment Prediction
Protocol for Wearable Sensor-Based Gait Analysis
This protocol [92] compared multiple ML models for estimating full-body kinematics, kinetics, and muscle forces using IMU and EMG data.
- Participants and Trials: Seventeen healthy adults performed over-ground walking trials. Data included marker trajectories (optical motion capture), ground reaction forces (force plates), IMU data (7 sensors), and EMG data (16 muscles).
- Target Calculation and Feature Extraction: The gold-standard "targets" (joint angles, moments, muscle forces) were calculated from the motion capture and force plate data using biomechanical software. Features from the IMU and EMG signals were automatically extracted using the
TsfreshPython package, which generates a comprehensive set of temporal and spectral features. - Model Training and Comparison: The extracted features were used to train four non-linear regression models: CNN, RF, SVM, and MARS. Performance was evaluated for both intra-subject (model personalized to an individual) and inter-subject (general model for new individuals) contexts, based on prediction error and computational time.
Protocol for Tensor Decomposition in Ageing Studies
This study [93] employed a novel methodology to investigate age-related differences in motor patterns during object lifting, which illustrates an alternative analytical pipeline.
- Experimental Task: Younger and older adults performed a bimanual grasp-lift-replace task with objects of different weights. Muscle activity (EMG) of arm and hand muscles, along with grip and load forces, were recorded simultaneously from both limbs.
- Data Structure and Analysis: The multi-faceted data (muscles/forces × time × object weight × participant × trial) was organized into a 5-way array (tensor). A Non-negative Canonical Polyadic (NCP) tensor decomposition was applied to extract cohesive patterns (components) that capture the spatial (muscle/force), temporal, and participant-specific characteristics of the lifting movement.
- Validation and Interpretation: The resulting components were linked to functional outcomes. For example, a component representing high grip force coupled with specific muscle synergies was found to be significantly more activated in older adults, predicting age group with high accuracy (AUC=0.83) [93]. This demonstrates a direct mapping between computational patterns and physiological phenomena.
Diagram: Tensor Decomposition for Movement Analysis
Verification and Validation in Computational Biomechanics
The credibility of any computational model hinges on a rigorous V&V process, a framework that is especially critical in biomechanics where models inform clinical decisions [1].
Verification: Solving the Equations Right: Verification ensures the computational model correctly implements its underlying mathematical formulation. This involves code verification against benchmark problems with known analytical solutions and calculation verification, typically through mesh convergence studies in Finite Element Analysis (FEA) to ensure results are independent of discretization choices. A change of <5% in the solution upon mesh refinement is often considered adequate for convergence [1] [59].
Validation: Solving the Right Equations: Validation assesses how accurately the computational model represents reality by comparing its predictions with experimental data. For joint force and kinematic models, this entails comparing model outputs (e.g., predicted knee contact force) against gold-standard experimental measurements. However, such direct in vivo measurements are often invasive and impractical [90] [1]. Therefore, models are frequently validated against indirect measures or in laboratory settings, with the understanding that all models have inherent errors and uncertainties.
Sensitivity Analysis: A crucial adjunct to V&V is sensitivity analysis, which quantifies how uncertainty in model inputs (e.g., material properties, geometry) affects the outputs. This helps identify critical parameters that require precise estimation and ensures that validation results are robust to input variations [1].
Diagram: The Verification & Validation Process in Biomechanics
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the modeling pipelines discussed requires a suite of computational and experimental tools. The table below details key resources referenced in the comparative studies.
Table 2: Essential Research Reagents and Computational Tools
| Tool Name | Type/Category | Primary Function in Pipeline | Example Use Case |
|---|---|---|---|
| OpenSim [90] | Software Platform | Musculoskeletal Modeling & Simulation | Generating gold-standard data for joint kinematics, kinetics, and muscle forces for model training [90]. |
| VICON System [90] [92] | Hardware & Software | Optical Motion Capture | Recording high-accuracy 3D marker trajectories for biomechanical analysis and target calculation [90] [92]. |
| IMUs (Inertial Measurement Units) [92] | Wearable Sensor | Measuring 3D Acceleration and Angular Velocity | Serving as input features for machine learning models predicting joint angles and moments outside the lab [92]. |
| EMG (Electromyography) [92] [93] | Wearable Sensor/Biosensor | Measuring Muscle Electrical Activity | Used as input for predicting muscle forces [92] or decomposed with forces to study muscle synergies [93]. |
| Tsfresh (Python Package) [92] | Software Library | Automated Feature Extraction from Time Series | Extracting relevant features from raw IMU and EMG data for training ML models like RF and CNN [92]. |
| drc R Package [94] | Software Library | Dose-Response Curve Analysis | Fitting parametric models for benchmark concentration (BMC) analysis in biostatistical pipelines (related context) [94]. |
| Non-negative CP Decomposition [93] | Computational Algorithm | Multi-dimensional Pattern Recognition | Factorizing complex data tensors (e.g., EMG, forces, time) to identify interpretable motor components [93]. |
This comparison guide elucidates a paradigm shift in biomechanical modeling from traditional, physics-based simulations towards data-driven machine learning pipelines. ANNs and RF models have demonstrated remarkable accuracy and efficiency in predicting joint forces and kinematics, showing particular promise for real-time clinical application. However, the choice of pipeline is contingent on the specific research question, available data, and required computational efficiency. Across all approaches, the foundational principles of verification and validation remain non-negotiable. They are the critical processes that separate a computationally interesting result from a biologically credible and clinically actionable prediction. Future work should focus on improving the generalizability of these models across diverse populations and standardizing V&V reporting practices to foster reproducibility and clinical translation.
In computational biomechanics, the creation of digital models to simulate biological systems is no longer a novelty but a cornerstone of modern research and development. These models are increasingly used to predict complex phenomena, from the mechanical behavior of arterial walls to the efficacy of orthopedic implants. However, a model's prediction is only as reliable as the confidence one can place in it. Uncertainty Quantification (UQ) provides the mathematical framework to assess this confidence, integrating statistical methods directly into model predictions to evaluate how uncertainties in inputs—such as material properties, boundary conditions, and geometry—propagate through computational analyses to affect the final results [95] [96]. The formal process of Verification and Validation (V&V) is the bedrock upon which credible models are built; verification ensures the equations are solved correctly, while validation determines if the right equations are being solved against experimental benchmarks [44] [30].
The push towards personalized medicine and digital twins—virtual replicas of physical assets or processes—has made UQ not just an academic exercise but a clinical imperative. A patient-specific finite element model of a knee, for instance, must reliably predict joint kinematics and ligament forces to be considered for surgical planning [30]. Similarly, computational models of cardiovascular devices require robust validation against in-vitro and in-vivo data to manage the inherent variability introduced by biological systems [23]. This guide objectively compares the performance of different UQ methodologies and their integration into experimental protocols, providing a framework for researchers to enhance the predictive power of their computational models.
Core Principles and Methodologies of Uncertainty Quantification
Foundational Concepts and Terminology
Understanding UQ requires familiarity with its core concepts. Uncertainty Quantification itself is the comprehensive process of characterizing and reducing uncertainties in both computational and real-world applications. It involves two primary types of uncertainty: aleatoric uncertainty, which arises from inherent, irreducible variability in a system (e.g., differences in bone density across a population), and epistemic uncertainty, which stems from a lack of knowledge and is theoretically reducible through more data or improved models [96]. A critical application of UQ is sensitivity analysis, a systematic process for ranking the influence of input parameters on model outputs, thereby identifying which parameters require precise characterization and which can be approximated [95].
The credibility of any computational model hinges on its Verification and Validation. Verification addresses the question "Are the equations being solved correctly?" by ensuring that the computational model accurately represents the underlying mathematical model and its solution. Validation, on the other hand, answers "Are the right equations being solved?" by assessing how accurately the computational model replicates real-world phenomena, typically through comparison with physical experiments [44] [30]. Finally, a digital twin is a subject-specific computational model that is continuously updated with data from its physical counterpart to mirror its current state and predict its future behavior, a concept heavily reliant on UQ for clinical translation [30].
A Generalized Workflow for UQ in Biomechanics
The process of integrating UQ into computational biomechanics can be visualized as a structured workflow that connects experimental data, computational modeling, and statistical analysis.
Diagram 1: UQ workflow in biomechanics.
Comparative Analysis of UQ Experimental Protocols
This section objectively compares the experimental methodologies and quantitative outcomes of three distinct approaches to model validation and UQ in biomechanics. The table below synthesizes key performance data from recent studies, highlighting how different protocols address uncertainty.
Table 1: Comparison of Experimental Protocols for Model Validation and UQ
| Study Focus & Reference | Experimental Protocol Summary | Key Quantitative Findings & UQ Outcomes | Strengths in UQ Approach | Limitations / Unaddressed Uncertainties |
|---|---|---|---|---|
| Vascular Strain Validation [16] | - Porcine carotid arteries (n=3) mounted on a biaxial tester.- Simultaneous intravascular ultrasound (IVUS) imaging during pressurization.- Strains from 3D FE models compared to experimental strains derived from deformable image registration. | - FE model strain predictions bounded experimental data at systolic pressure.- Higher variability in model-predicted strains (up to 10%) versus experimental (up to 5%).- Models incorporating material property variability successfully captured the range of experimental outcomes. | - Direct, focal comparison of transmural strain fields.- Acknowledges and incorporates biological variability into model predictions. | - Small sample size (n=3) limits statistical power.- Uncertainty from image registration technique not fully quantified. |
| Passive Knee Kinematics [44] | - Gravity-induced knee flexion tests on patients (n=11) in three states: awake, anesthetized, and anesthetized + muscle relaxant.- Kinematics and EMG activity of the vastus lateralis were measured. | - Median time to 47° flexion: 404 ms (awake) vs. 349 ms (anesthetized + relaxed).- Significant difference (p < 0.001) between awake and fully relaxed states.- Only 15% of awake trials showed no measurable EMG activity. | - Provides crucial data on "baseline passive kinematics" for model validation.- Quantifies the inherent muscle tone in "relaxed" awake subjects, a key uncertainty in musculoskeletal modeling. | - Study focused on providing validation data rather than implementing a full UQ framework on a specific model. |
| Knee Model Calibration [30] | - Compared two calibration methods for subject-specific knee FEMs using cadaveric specimens.- Calibration sources: 1) Robotic Knee Simulator (RKS - in vitro), 2) Knee Laxity Apparatus (KLA - in vivo). | - Model predictions (anterior-posterior laxity) differed by < 2.5 mm between RKS and KLA models.- During pivot shift simulation, kinematics were within 2.6° and 2.8 mm.- Despite similar kinematics, predicted ligament loads differed. | - Directly quantifies the impact of calibration data source on model output uncertainty.- Highlights that kinematic accuracy does not guarantee force prediction accuracy. | - Ligament force predictions remain unvalidated due to lack of in vivo force measurements. |
Key Insights from Comparative Data
The comparative data reveals that a one-to-one match between model predictions and experimental data is often not achieved, nor is it necessarily the goal. A robust UQ process, as demonstrated in the vascular strain study, aims for the model to bound the experimental data, meaning its predictions encompass the range of physical measurements when input variability is considered [16]. Furthermore, the knee calibration study underscores a critical principle: validation is context-dependent. A model calibrated for excellent kinematic predictions may still perform poorly in predicting tissue-level loads, emphasizing the need for validation against the specific outputs of interest [30].
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of UQ requires a suite of specialized tools, from physical devices to computational resources. The table below details key solutions used in the featured studies.
Table 2: Key Research Reagent Solutions for UQ in Biomechanics
| Item Name / Category | Function in UQ/Validation Workflow | Specific Example from Literature |
|---|---|---|
| Custom Biaxial Testing Systems | Applies controlled multiaxial mechanical loads to biological tissues to generate data for constitutive model calibration and validation. | System for pressurizing arterial tissue while simultaneously conducting IVUS imaging [16]. |
| Knee Laxity Apparatus (KLA) | Measures in vivo joint laxity (displacement under load) to provide subject-specific data for ligament material property calibration in musculoskeletal models. | Device used to apply anterior-posterior drawer tests and pivot-shift loads on cadaveric specimens and living subjects [30]. |
| Robotic Knee Simulator (RKS) | Provides high-accuracy, high-volume force-displacement data from cadaveric specimens, serving as a "gold standard" for validating models calibrated with in vivo data. | Used to collect extensive laxity measurements for model calibration in a controlled in vitro environment [30]. |
| Medical Imaging & Analysis Software | Generates subject-specific geometry and enables non-invasive measurement of internal strains for direct model validation. | Intravascular Ultrasound (IVUS) and deformable image registration to measure transmural strains in arterial tissue [16]. |
| Finite Element Analysis Software with UQ Capabilities | Platform for building computational models and running simulations (e.g., Monte Carlo) to propagate input uncertainties and perform sensitivity analysis. | Used to create specimen-specific knee finite element models and calibrate ligament properties [30]. Specialized sessions at CMBBE 2025 discussed such tools [23]. |
Application Workflow for Knee Model Validation
The tools listed in Table 2 are integrated into a cohesive workflow for developing and validating a computational model, as exemplified by the subject-specific knee model study [30]. This process can be visualized as follows.
Diagram 2: Tool integration for model validation.
The integration of statistical methods for Uncertainty Quantification is what separates a suggestive computational model from a credible tool for scientific and clinical decision-making. As the field progresses, UQ is becoming deeply embedded in emerging areas like digital twins for personalized medicine and in-silico clinical trials [97] [30]. Future advancements will likely be driven by the coupling of physics-based models with machine learning, where UQ will be vital for understanding the limitations of data-driven approaches, and by the exploration of quantum computing for tackling the computational expense of UQ in high-fidelity models [95]. The consistent theme across all studies is that a model's true value is determined not by its complexity, but by a transparent and rigorous quantification of its predictive confidence.
Verification and validation (V&V) are fundamental pillars of computational biomechanics, ensuring that models are solved correctly (verification) and accurately represent real-world physics (validation). Within orthopaedic biomechanics, patient-specific musculoskeletal (MSK) models offer the potential to predict individual joint mechanics non-invasively, with applications in surgical planning, implant design, and personalized intervention strategies [98] [99]. However, the translation of these models from research tools to clinical decision-support systems hinges on rigorous validation and a clear understanding of their predictive limitations. This case study focuses on the comparative validation of two distinct patient-specific modeling pipelines developed to predict knee joint contact forces (KCFs) during level walking, a primary activity of daily living. By examining their methodologies, predictive performance, and computational efficiency, this analysis contributes to the broader thesis on establishing robust V&V standards for computational biomechanics models.
Methodology: Modeling Pipelines and Experimental Protocols
This case study objectively compares two patient-specific modeling pipelines for predicting KCFs:
- The INSIGNEO Pipeline: An established, detailed workflow for developing image-based skeletal models of the lower limb. This pipeline is characterized by a high degree of manual input and customization, requiring a niche computational skillset [98].
- The STAPLE/nmsBuilder Pipeline: A semi-automated pipeline that combines the STAPLE toolbox for the rapid generation of image-based skeletal models with the nmsBuilder software for adding musculotendon units and performing simulations. This approach is designed to streamline and expedite model development with minimal user input [98].
Both pipelines aim to create subject-specific MSK models from medical images (e.g., MRI), which are then used within simulation frameworks like OpenSim to calculate muscle forces and subsequent joint loading during dynamic tasks [100].
Experimental Validation Protocol
The gold standard for validating predicted KCFs involves direct comparison with in vivo measurements from instrumented knee implants. The following protocol is representative of rigorous validation efforts:
- Data Source: Publicly available datasets, such as the CAMS-Knee project, provide essential validation data. These datasets include measurements from patients with instrumented tibial implants, capturing six load components (three forces and three moments) at the knee joint during activities like level walking [100].
- Complementary Data: The datasets also typically include synchronized whole-body marker kinematics (measured via motion capture), ground reaction forces (measured via force plates), and electromyography (EMG) signals from major lower limb muscles [100].
- Simulation Workflow: The generic MSK model is scaled to match the patient's anthropometry based on a static trial. Inverse kinematics calculates joint angles from marker trajectories, and inverse dynamics computes intersegmental moments. Muscle activations are then estimated using tools like static optimization, which minimizes the sum of squared muscle activations. Finally, a joint reaction force analysis computes the KCFs [100].
- Analysis Metrics: Predicted and measured KCFs are compared using metrics such as:
- Root Mean Square (RMS) Error: Quantifies the magnitude of the prediction error.
- R² Pearson Correlation Coefficient: Assesses the similarity in the waveform shape between predicted and measured forces.
- Peak Force Comparison: Evaluates the model's accuracy in predicting the magnitude of maximum loading [100].
The diagram below illustrates the logical workflow for creating and validating a patient-specific knee model.
Quantitative Performance Comparison
The following table summarizes the key quantitative findings from the comparative validation of the two pipelines against experimental implant data.
Table 1: Quantitative Comparison of Modeling Pipeline Performance for Predicting Knee Contact Forces during Level Walking
| Performance Metric | INSIGNEO Pipeline | STAPLE/nmsBuilder Pipeline | Notes |
|---|---|---|---|
| Total KCF Prediction | Similar force profiles and average values to STAPLE [98] | Similar force profiles and average values to INSIGNEO [98] | Both showed a moderately high level of agreement with experimental data. |
| Statistical Difference | Statistically significant differences were found between the pipelines (Student t-test) [98] | Statistically significant differences were found between the pipelines (Student t-test) [98] | Despite similar profiles, differences were statistically significant. |
| Computational Time (Model Generation) | ~160 minutes [98] | ~60 minutes [98] | STAPLE-based pipeline offered a ~62.5% reduction in time. |
| Representative Generic Model RMS Error (Total KCF) | Not directly reported in study | Not directly reported in study | For context, a generic OpenSim model showed an RMS error of 47.55%BW during gait [100]. |
| Representative Generic Model R² (Total KCF) | Not directly reported in study | Not directly reported in study | For context, a generic OpenSim model showed an R² of 0.92 during gait [100]. |
Analysis of Results and Broader Validation Challenges
Interpretation of Comparative Findings
The comparative study indicates that the semi-automated STAPLE/nmsBuilder pipeline can achieve a level of accuracy in predicting KCFs that is comparable to the established, but more time-consuming, INSIGNEO pipeline [98]. The fact that both pipelines showed similar agreement with experimental data is promising for the use of streamlined workflows. However, the presence of statistically significant differences underscores that the choice of modeling pipeline can introduce systematic variations in predictions, even when overall agreement is good. The substantial reduction in model generation time with the STAPLE-based pipeline (60 minutes vs. 160 minutes) is a critical advantage, potentially making patient-specific modeling more feasible in clinical settings where time is a constraint [98].
Critical Limitations in Model Validation
A paramount consideration in the validation of MSK models is that accurate prediction of KCFs alone is insufficient to guarantee a correct representation of the complete joint biomechanics. A recent sensitivity analysis demonstrated that simulations producing acceptable KCF estimates could still exhibit large inaccuracies in joint kinematics—with uncertainties reaching up to 8 mm in translations and 10° in rotations [101]. This dissociation between kinetic and kinematic accuracy highlights a significant limitation of using KCFs as a sole validation metric, particularly for applications like implant design or soft-tissue loading analysis where precise motion is critical [101].
Furthermore, the predictive capacity of models can vary dramatically across different activities. While models may perform reasonably well during gait, they often show substantially larger errors during more demanding tasks like squatting, where RMS errors for generic models can exceed 105%BW [100]. This activity-dependent performance necessitates validation across a spectrum of movements relevant to the clinical or research question.
Advancing Model Personalization with In Vivo Data
The pursuit of greater predictive accuracy is driving innovation in model personalization. A key frontier is the calibration of ligament material properties using in vivo data. Traditionally, this has required measurements from cadaveric specimens. However, new devices are now capable of performing knee laxity tests on living subjects [30]. Research has demonstrated that computational models calibrated with these in vivo laxity measurements can achieve accuracy comparable to models calibrated with gold-standard in vitro robotic simulator data, with predictions during simulated clinical tests differing by less than 2.5 mm and 2.6° [30]. This workflow is a crucial step toward developing truly subject-specific "digital twins" of the knee.
Successful development and validation of patient-specific knee models rely on a suite of computational and experimental resources. The table below details key solutions and their functions.
Table 2: Key Research Reagent Solutions for Knee Joint Modeling and Validation
| Tool / Resource | Type | Primary Function |
|---|---|---|
| OpenSim [100] | Software Platform | Open-source software for building, simulating, and analyzing MSK models and dynamic movements. |
| STAPLE [98] | Software Toolbox | Semi-automated toolbox for rapidly generating image-based skeletal models of the lower limb. |
| nmsBuilder [98] | Software Tool | Used to add musculotendon units to skeletal models and perform simulations. |
| CAMS-Knee Dataset [100] | Validation Dataset | A public dataset containing in vivo knee contact forces, kinematics, ground reaction forces, and EMG from instrumented implants. |
| Finite Element (FE) Software (e.g., ABAQUS) [99] | Software Platform | Used for creating detailed finite element models of the knee to predict contact mechanics, pressures, and stresses. |
| Knee Laxity Apparatus (KLA) [30] | Experimental Device | A device designed to measure knee joint laxity in living subjects, providing data for subject-specific model calibration. |
This case study demonstrates that while semi-automated pipelines like STAPLE/nmsBuilder can dramatically improve the efficiency of generating patient-specific models without severely compromising predictive accuracy for KCFs during walking, significant validation challenges remain. The core thesis reinforced here is that comprehensive validation in computational biomechanics must extend beyond a single metric, such as total knee contact force. Future work must prioritize:
- Multi-modal Validation: Incorporating both kinetic (forces) and kinematic (motion) data into the validation framework [101].
- Activity-Specific Assessment: Validating model performance across a range of functionally relevant activities [100].
- Deep Personalization: Advancing the calibration of model parameters, such as ligament properties, using data obtainable from living subjects to improve individual accuracy [30].
The continued refinement of these pipelines, coupled with robust and critical validation practices, is essential for bridging the gap between research-grade simulations and reliable clinical tools for personalized medicine.
Conclusion
Verification and Validation are indispensable, interconnected processes that form the bedrock of credibility in computational biomechanics. This synthesis of core intents demonstrates that rigorous V&V, coupled with systematic sensitivity analysis, transforms models from research tools into reliable assets for scientific discovery and clinical decision-making. The future of the field hinges on developing standardized V&V protocols for patient-specific applications, enhancing uncertainty quantification methods, and fostering deeper collaboration between computational scientists, experimentalists, and clinicians. As modeling pipelines become more efficient and accessible, their successful translation into clinical practice will be directly proportional to the robustness of their underlying V&V frameworks, ultimately paving the way for personalized medicine and predictive healthcare solutions.
References
- 1. Validation of Computational Models in Biomechanics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2941217/]
- 2. Verification, Validation and Uncertainty Quantification ... [https://www.asme.org/codes-standards/publications-information/verification-validation-uncertainty]
- 3. Survey and perspective on verification, validation, and ... [https://www.nature.com/articles/s41746-025-01447-y]
- 4. Computational Biomechanics [https://movement.ethz.ch/research/computational-biomechanics.html]
- 5. Verification, Validation, Uncertainty Quantification in ... [https://www.nafems.org/events/nafems/2025/verification-and-validation-in-engineering-simulation-online-01/?srsltid=AfmBOor00Rdle_bNqZNTdqYzfA_Z3X7Hwe8pDA_Rvr3xRZ4k05na5V6n]
- 6. Learning (from) the errors of a systems biology model [https://www.nature.com/articles/srep20772]
- 7. Uncertainty and Error in CFD Simulations [https://www.grc.nasa.gov/www/wind/valid/tutorial/errors.html]
- 8. Modeling Error - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/engineering/modeling-error]
- 9. Local truncation error - (Biomedical Engineering II) [https://fiveable.me/key-terms/biomedical-engineering-ii/local-truncation-error]
- 10. Biomedical Model Fitting and Error Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3272496/]
- 11. a surprising instance of catastrophic floating point errors in ... [https://arxiv.org/abs/2304.02365]
- 12. Practical considerations for data exploration in quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12045597/]
- 13. Verification, Validation and Sensitivity Studies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3361760/]
- 14. Verification and Validation of Computational Models Used ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354921000319]
- 15. Verification, Validation, Uncertainty Quantification in ... [https://www.nafems.org/events/nafems/2025/verification-and-validation-in-engineering-simulation-online-01/?srsltid=AfmBOopCCj8Sbr2DT7HoVlq_rlnrY_kKhYkZDn_vwwUZ-I2iSH1lhRIh]
- 16. Journal of Biomechanics [https://www.sciencedirect.com/science/article/abs/pii/S0021929025002015]
- 17. An open source statistical web application for validation ... [https://www.nature.com/articles/s41598-025-99720-3]
- 18. Co-chairing CMBBE 2025 on VVUQ in Barcelona [https://www.linkedin.com/posts/dan-nicolella-2b9a146_cmbbe2025-computationalbiomechanics-vvuq-activity-7368971806633832450-C7sS]
- 19. Current Applications and Future Developments of the ASME ... [https://dmd.umn.edu/2025/vv40]
- 20. Methods for Analytical Validation of Novel Digital Clinical ... [https://www.jmir.org/2025/1/e70314/]
- 21. Verification, Validation, Uncertainty Quantification in ... [https://www.nafems.org/events/nafems/2025/verification-and-validation-in-engineering-simulation-online-01/?srsltid=AfmBOoo4vSMaRZqDxnLZoKbD41mADF3mzJSVa97dehTRv5AxN_bc16qv]
- 22. Keep an Eye on Clinical Validation Gaps in AI-Enabled ... [https://www.aha.org/aha-center-health-innovation-market-scan/2025-09-16-keep-eye-clinical-validation-gaps-ai-enabled-medical-devices]
- 23. Special sessions | CMBBE 2025 [https://www.cmbbe-symposium.com/2025/special-sessions/]
- 24. Overview of CFD Verification & Validation [https://www.grc.nasa.gov/www/wind/valid/tutorial/overview.html]
- 25. ASME V&V 10-2019 - Standard for Verification and ... [https://webstore.ansi.org/standards/asme/asme102019?srsltid=AfmBOopTGj0GwKimWuMn2j6BnQrz9g4UIpaAqSvSF8N4AZbWYhHZqs7F]
- 26. Advances in Musculoskeletal Modeling of the Thoraco ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575568/]
- 27. Solid Mechanics & Aerospace: VVUQ References [https://eikosim.com/en/technical-articles/vvuq-references-aerospace-solid-mechanics/]
- 28. A software benchmark for cardiac elastodynamics [https://www.sciencedirect.com/science/article/pii/S0045782524007394]
- 29. Focal comparison of experimental and finite element ... [https://pubmed.ncbi.nlm.nih.gov/40359618/]
- 30. Validating subject-specific knee models from in vivo ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1554836/full]
- 31. vs. In : Choosing the Right Experimental Model... - Cusabio Vivo In Vitro [https://www.cusabio.com/c-21169.html]
- 32. Ex vivo 3D micro-tumour testing platform for predicting ... [https://www.nature.com/articles/s41698-025-01080-8]
- 33. $32.88 Bn In-vitro Toxicology Testing Market Trends and ... [https://finance.yahoo.com/news/32-88-bn-vitro-toxicology-092400584.html]
- 34. In Vivo Target Validation [https://www.targetals.org/in-vivo-target-validation-2025/]
- 35. Preclinical ex vivo and in vivo models to study immunotherapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574409/]
- 36. In Vitro Toxicity Testing Market Size & Forecast, 2025-2032 [https://www.coherentmarketinsights.com/market-insight/in-vitro-toxicity-testing-market-3855]
- 37. Patient-Specific Modelling and Personalized Medicine with ... [https://vias3d.com/blogs/patient-specific-modelling-and-personalized-medicine-with-finite-element-method-fem/]
- 38. A novel method for the generation of multi-block ... [https://www.sciencedirect.com/science/article/abs/pii/S1350453311003183]
- 39. Image data and computational grids for computing brain shift ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10147975/]
- 40. Benchmarking QSP Models Against Simple Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC6118293/]
- 41. Artificial intelligence in medical imaging: From task-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11925424/]
- 42. Developing cardiac biomechanical models beyond the clinic [https://link.springer.com/article/10.1007/s10237-025-01982-3]
- 43. Verification Through Experimental Neuromuscular Dynamics [https://link.springer.com/article/10.1007/s10439-025-03783-2]
- 44. Validation of computational models simulating injury ... [https://link.springer.com/article/10.1007/s00414-025-03577-0]
- 45. Neuromusculoskeletal Modeling and Force Prediction - PubMed [https://pubmed.ncbi.nlm.nih.gov/40627083/]
- 46. Biomechanics, Volume 5, Issue 2 (June 2025) – 24 articles [https://www.mdpi.com/2673-7078/5/2]
- 47. Verification, Validation, Uncertainty Quantification in ... [https://www.nafems.org/events/nafems/2025/verification-and-validation-in-engineering-simulation-online-01/?srsltid=AfmBOoqyLWK6-vjJIwIlkuQIko-Yzy_c3cSD8nKcfb7VKfHJVBB_Vnkz]
- 48. Comparison of MRI and CT based deep learning ... - Nature [https://www.nature.com/articles/s41598-025-92263-7]
- 49. A comparative analysis of preclinical computed ... [https://www.sciencedirect.com/science/article/pii/S240563162400085X]
- 50. Motion Capture Technologies for Athletic Performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299843/]
- 51. Validation of a markerless motion capture system for centre ... [https://www.sciencedirect.com/science/article/pii/S0208521625000233]
- 52. The Integration of Micro-CT Imaging and Finite Element ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12295181/]
- 53. Investigating the Limits of Predictability of Magnetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564088/]
- 54. Sensitivity analysis [https://en.wikipedia.org/wiki/Sensitivity_analysis]
- 55. Parameter identification and sensitivity analysis of a lower- ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1566381/full]
- 56. Efficient sensitivity analysis for biomechanical models with ... [https://research.tue.nl/en/publications/efficient-sensitivity-analysis-for-biomechanical-models-with-corr/]
- 57. Discretization error when using finite element models [https://www.sciencedirect.com/science/article/abs/pii/S0021929009002826]
- 58. Validation of Computational Models in Biomechanics ... [https://www.scribd.com/document/899651372/Validation-of-Computational-Models-in-Biomechanics-4fkakyjeth]
- 59. Reporting checklist for verification and validation of finite ... [https://www.sciencedirect.com/science/article/pii/S1350453321000345]
- 60. Focal Comparison of Experimental and Finite Element ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288764/]
- 61. Ansys Mechanical in 2025R1 - Mesh Convergence [https://blog.cadfem.ai/ansys-mechanical-in-2025r1/]
- 62. Mesh convergence with examples [https://enterfea.com/examples-mesh-convergence/]
- 63. Methodological Aspects and Mesh Convergence in ... [https://www.mdpi.com/2079-6439/12/1/9]
- 64. The effects of geometric uncertainties on computational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5579124/]
- 65. Analysis of Uncertainty and Variability in Finite Element ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2016.00085/full]
- 66. Measures of agreement between computation and ... [https://www.sciencedirect.com/science/article/abs/pii/S0021999106001860]
- 67. Falsifying computational models of endothelial cell network ... [https://pubmed.ncbi.nlm.nih.gov/40305554/]
- 68. Biological variability in biomechanical engineering research [https://www.sciencedirect.com/science/article/abs/pii/S0021929014000712]
- 69. Adapting modeling and simulation credibility standards to ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04290-5]
- 70. Computational modelling of biological systems now and then [https://pmc.ncbi.nlm.nih.gov/articles/PMC12105733/]
- 71. Effect of different constraining boundary conditions on ... [https://www.nature.com/articles/s41598-024-61305-x]
- 72. In silico biological discovery with large perturbation models [https://www.nature.com/articles/s43588-025-00870-1]
- 73. From FAIR to CURE: Guidelines for Computational Models ... [https://ui.adsabs.harvard.edu/abs/2025arXiv250215597S/abstract]
- 74. Artificial Intelligence in Sports Biomechanics: A Scoping ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383302/]
- 75. Biomechanical optimization and reinforcement learning ... [https://www.nature.com/articles/s41598-025-97637-5]
- 76. HBM - Motekmedical.com [https://www.motekmedical.com/software/hbm/]
- 77. VueMotion: AI-Powered Athletic Performance Analysis Platform [https://www.vuemotion.com/]
- 78. Motion Capture Systems for Biomechanics and Movement ... [https://www.motionanalysis.com/movement-analysis/]
- 79. Machine learning predictive model based on the corneal ... [https://www.sciencedirect.com/science/article/pii/S1572100025007938]
- 80. The Biomechanics of Bodies (BoB) Software [https://www.bob-biomechanics.com/]
- 81. of Validation models in computational biomechanics [https://pubmed.ncbi.nlm.nih.gov/20839648/]
- 82. Computational Biomechanics - Research Groups [https://researchgroups.msu.edu/compbiomech/]
- 83. PhD Position University of Glasgow – Computational ... [https://esbiomech.org/phd-position-university-of-glasgow-computational-biomechanics-research-group-2/]
- 84. Validation of computational models simulating injury- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532759/]
- 85. ICBT 2025 (17-November 18, 2025): Scientific Program [https://konferenz.uni-hannover.de/event/152/program]
- 86. Advanced Biomechanical Testing Techniques [https://www.numberanalytics.com/blog/advanced-biomechanical-testing-techniques]
- 87. Biomechanics, Volume 5, Issue 3 (September 2025) [https://www.mdpi.com/2673-7078/5/3]
- 88. Validation of a musculoskeletal model to investigate hip ... [https://www.sciencedirect.com/science/article/abs/pii/S0021929023003378]
- 89. Using the Data Agreement Criterion to Rank Experts' Beliefs [https://pmc.ncbi.nlm.nih.gov/articles/PMC7513104/]
- 90. Real-Time Prediction of Joint Forces by Motion Capture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7730598/]
- 91. Predicting lower body joint moments and ... [https://www.sciencedirect.com/science/article/pii/S096663622500013X]
- 92. A comparison of machine learning models' accuracy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10049990/]
- 93. A tensor decomposition reveals ageing-induced ... [https://www.nature.com/articles/s41598-024-62768-8]
- 94. A comparative study of biostatistical pipelines for ... [https://www.sciencedirect.com/science/article/abs/pii/S2468111325000209]
- 95. Conference on Computational and Artificial Intelligence for ... [https://ccaimb.wordpress.com/]
- 96. UNCECOMP 2025 / 6th International Conference on ... [https://2025.uncecomp.org/]
- 97. Sparking translational modelling at CMBBE 2025 in ... [https://sano.science/sparking-translational-modelling-at-cmbbe-2025-in-barcelona/]
- 98. Comparative validation of two patient - specific pipelines for... modelling [https://pubmed.ncbi.nlm.nih.gov/37659354/]
- 99. Development and validation of a computational model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4047624/]
- 100. The Capacity of Generic Musculoskeletal Simulations to Predict Knee ... [https://link.springer.com/article/10.1007/s10439-020-02465-5]
- 101. Knee contact force alone is insufficient to validate joint ... [https://www.sciencedirect.com/science/article/pii/S0021929025004920]