Metallic vs. Polymeric Biomaterials: A Comprehensive Comparison of Mechanical Properties for Biomedical Applications
This article provides a detailed analysis of the mechanical properties of metallic and polymeric biomaterials, targeting researchers and professionals in biomedical engineering and drug development.
Metallic vs. Polymeric Biomaterials: A Comprehensive Comparison of Mechanical Properties for Biomedical Applications
Abstract
This article provides a detailed analysis of the mechanical properties of metallic and polymeric biomaterials, targeting researchers and professionals in biomedical engineering and drug development. It explores the fundamental characteristics of both material classes, examines their specific applications in orthopedics, cardiovascular devices, and tissue engineering, addresses key challenges such as stress shielding and degradation control, and offers a comparative validation of their performance. By synthesizing current research and emerging trends, including the use of explainable AI and additive manufacturing for material design, this review serves as a critical resource for the rational selection and development of next-generation biomaterials.
Fundamental Principles: Unraveling the Core Characteristics of Metallic and Polymeric Biomaterials
Biomaterials, traditionally defined as substances engineered to interact with biological systems for a medical purpose, have undergone a revolutionary transformation in both sophistication and application philosophy [1]. The field has evolved from the ancient use of naturally available materials like wood to replace tissues, to a highly interdisciplinary science that seamlessly integrates materials science, biology, and medicine [2]. This evolution is characterized by a fundamental shift from a paradigm of biological inertness to one of active interaction, where modern biomaterials are designed to elicit specific, therapeutic responses from host tissues [2]. The academic foundation of biomaterials has expanded precipitously; in the United States alone, there are now more than 75 departments of biomedical engineering, a dramatic increase from the 12 that existed in 1975, with over 16,000 enrolled students as of 2005 [2]. This growth underscores the critical role biomaterials play in a medical device market that generates approximately $200 billion annually in the U.S. [2]. This article places this evolution within the context of a broader thesis, focusing specifically on the comparison of mechanical properties between two dominant classes of biomaterials: metals and polymers.
Table 1: Historical Evolution of Biomaterials
| Era | Dominant Materials | Design Philosophy | Key Applications |
|---|---|---|---|
| Antiquity to Early 20th Century | Natural Materials (e.g., wood) | Structural replacement, availability | Primitive prosthetics [2] |
| Early to Mid-20th Century | Synthetic Polymers, Metal Alloys, Ceramics | Inertness, mechanical performance | Artificial hips, vascular stents, dental restoratives [2] |
| Late 20th Century to Present | Bioactive and Information-Rich Materials (e.g., composites, smart polymers) | Bioactivity, interaction with host biology, dynamic behavior | Drug-eluting stents, tissue engineering scaffolds, bioactive implants [2] [3] |
Modern Biomaterial Classifications and Properties
Today, biomaterials are broadly classified based on their interaction with host tissue and their chemical composition. The tissue response-based classification categorizes materials as close-to-inert (eliciting minimal tissue response), active (encouraging bonding to surrounding tissue), or degradable/resorbable (incorporated into tissue or dissolved over time) [4]. From a materials science perspective, the primary categories are metals, polymers, ceramics, and composites, each with distinct mechanical and biological properties that dictate their application.
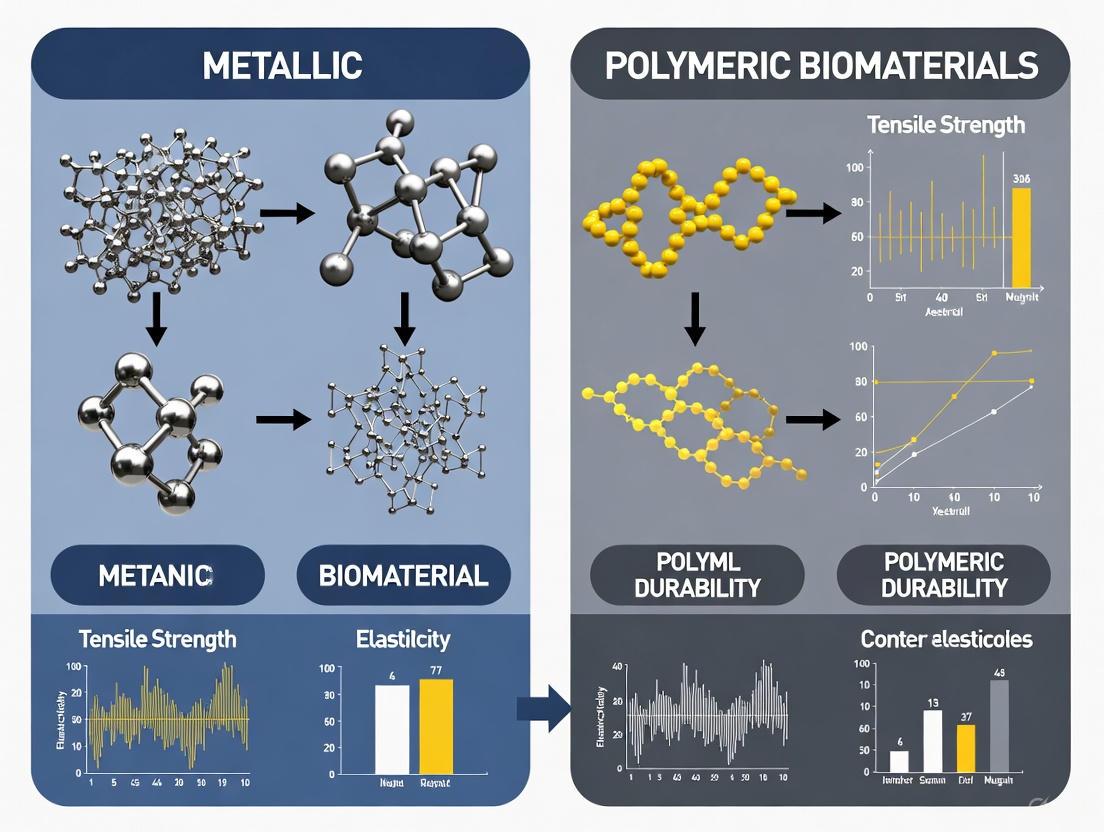
Metallic Biomaterials
Metals are predominantly used for load-bearing applications such as orthopedic and dental implants due to their superior strength, durability, and fatigue resistance [4] [5]. They are typically considered close-to-inert biomaterials. Key challenges for metallic implants include the risk of stress shielding due to a high elastic modulus compared to natural bone, aseptic loosening, and the release of metal ions through corrosion or wear [5] [6]. Consequently, research focuses on developing alloys with lower moduli and enhancing surfaces to improve biointegration.
Table 2: Mechanical Properties of Common Metallic Biomaterials
| Material | Young's Modulus (GPa) | Ultimate Tensile Strength (MPa) | Key Characteristics and Applications |
|---|---|---|---|
| 316L Stainless Steel | ~200 [7] | ~540 [7] | Cost-effective, good corrosion resistance; removable implants, fracture disks [4] |
| Co-Cr Alloys | ~230 [7] | ~900 [7] | Excellent wear resistance and biocompatibility; artificial hip joints, dental prostheses [4] |
| Commercially Pure Titanium | ~110 [7] | ~240 [7] | Excellent biocompatibility, osseointegration; dental implants [4] |
| Ti-6Al-4V Alloy | ~110 [7] | ~900 [7] | High strength-to-weight ratio, fatigue resistance; bone plates, joint replacements [4] |
| β-type Titanium Alloys | ~40-60 [8] | Varies | Low Young's modulus to reduce stress shielding; next-generation orthopedic implants [8] |
Polymeric Biomaterials
Polymers offer a wide range of properties, from flexible and biodegradable to durable and inert, making them suitable for applications from soft tissue engineering to cardiovascular devices [3] [9]. They can be natural (e.g., collagen, chitosan) or synthetic (e.g., PLA, PCL), and are frequently processed into forms such as hydrogels, porous sponges, and films [3]. A significant advancement is the development of "smart" polymers with self-healing or shape-memory properties, which are highly useful for minimally invasive implantation and creating dynamic tissue environments [3].
Table 3: Mechanical Properties of Common Polymeric Biomaterials
| Material | Young's Modulus | Ultimate Tensile Strength | Key Characteristics and Applications |
|---|---|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) | Wide range tunable by composition and MW [3] | Wide range tunable by composition and MW [3] | Biodegradable, used in drug delivery and as stent coatings [4] [3] |
| Polycaprolactone (PCL) | Wide range tunable by composition and MW [3] | Wide range tunable by composition and MW [3] | Biodegradable, used in electrospinning for tissue scaffolds [3] |
| Polyurethane (PU) | Varies by formulation | Varies by formulation | Biocompatible, resilient; used in breast implants, cardiac patches, and vascular grafts [4] |
| Acrylic Acid-co-HEMA Graft (Modified ePTFE) | 74-121 MPa [10] | 5-9 MPa [10] | Modified for reduced hydrophobicity; potential use in soft tissue replacement [10] |
Experimental Protocols for Biomaterial Characterization
To objectively compare the performance of metallic and polymeric biomaterials, standardized experimental protocols are essential. The following sections detail key methodologies cited in the literature for evaluating mechanical properties and corrosion behavior.
Static Immersion Test for Metal Release (Metallic Biomaterials)
This in vitro test is designed to quantitatively evaluate the corrosion and metal ion release from metallic biomaterials under simulated physiological conditions [6].
- Objective: To quantify the release of base and alloying elements from metallic biomaterials into various simulated body fluids and understand the effect of solution pH on metal release [6].
- Materials and Specimen Preparation: Specimens of materials like SUS316L stainless steel, Co-Cr-Mo alloy, and Ti-6Al-4V are prepared with a standardized surface finish. They are degreased, rinsed, dried, and sterilized before testing [6].
- Immersion Media: A range of solutions is used to simulate different body environments, including α-medium, phosphate-buffered saline (PBS), calf serum, 0.9% sodium chloride, artificial saliva, 1.2% L-cysteine (simulating inflammatory conditions), 1% lactic acid, and 0.01% HCl [6].
- Procedure: Specimens are immersed in the solutions at a consistent surface-area-to-volume ratio and maintained at 37°C for 7 days. The containers are sealed to prevent contamination and evaporation [6].
- Analysis: After the immersion period, the concentrations of released metal ions (e.g., Fe, Cr, Ni, Mo, Co, Ti, Al, V) in the solutions are quantified using analytical techniques like inductively coupled plasma-mass spectrometry (ICP-MS). The pH of each solution is also measured post-test [6].
Gamma Irradiation-Induced Grafting for Polymer Modification (Polymeric Biomaterials)
This protocol describes a method to modify the surface of a polymeric biomaterial to alter its physical and mechanical properties, using expanded polytetrafluoroethylene (ePTFE) as an example [10].
- Objective: To graft hydrophilic comonomers onto a hydrophobic polymer surface to improve biocompatibility and measure the resultant changes in mechanical properties [10].
- Materials: Base polymer (e.g., ePTFE film), hydrophilic comonomers (e.g., Acrylic Acid (AA), 2-hydroxyethyl methacrylate (HEMA), N-isopropylacrylamide (NIPAAM)), and a gamma irradiation source [10].
- Grafting Procedure:
- The ePTFE substrate is cut into standardized dumbbell shapes and cleaned with hot methanol to remove contaminants.
- The sample is immersed in a solution containing the comonomers and degassed with nitrogen.
- The container is sealed and irradiated at a specified dose (e.g., 0.5 to 2 kGy) using a gamma cell.
- Post-irradiation, the grafted samples are washed with hot methanol and deionized water to remove any ungrafted homopolymer and then dried [10].
- Mechanical Testing: The modified and unmodified samples are subjected to tensile testing using a universal testing machine (e.g., Instron) at a constant crosshead speed. Properties such as Young's modulus, ultimate tensile strength, and elongation at break are evaluated for both dry samples and samples soaked in deionized water (wet condition) [10].
Biomaterial Selection and Testing Workflow
The Scientist's Toolkit: Key Research Reagents and Materials
This table details essential materials and reagents used in the featured experiments and broader biomaterials research, providing researchers with a foundational list for experimental design.
Table 4: Essential Research Reagents and Materials in Biomaterials Science
| Item | Function in Research | Example Use Case |
|---|---|---|
| Simulated Body Fluids (SBFs) | To simulate the chemical environment of the human body for in vitro testing of corrosion, degradation, and bioactivity. | α-medium, PBS, and calf serum used in static immersion tests for metal release [6]. |
| Acrylic Acid (AA) & HEMA | Hydrophilic comonomers used to modify polymer surfaces via grafting. | Grafted onto ePTFE via gamma irradiation to reduce hydrophobicity and alter mechanical properties [10]. |
| Gamma Irradiation Source | Provides high-energy photons to initiate radical formation on polymer chains, enabling surface grafting without multiple chemicals. | Used in the gamma irradiation-induced grafting method for modifying ePTFE [10]. |
| Universal Testing Machine | Measures fundamental mechanical properties of materials, including tensile strength, elongation, and Young's modulus. | Used to characterize both metallic [7] and polymeric [10] biomaterials pre- and post-modification. |
| ICP-MS (Inductively Coupled Plasma Mass Spectrometry) | Highly sensitive analytical technique for quantifying trace levels of metal ions released from biomaterials. | Used to measure concentrations of released ions (Fe, Cr, Ni, Co, Ti, V) after immersion tests [6]. |
| Cyclopropanediazonium | Cyclopropanediazonium Ion Reagent for RUO | Cyclopropanediazonium ions for synthesizing cyclopropylazoarenes and studying radical intermediates. For Research Use Only. Not for human or veterinary use. |
| Butanal, 3,4-dihydroxy- | Butanal, 3,4-dihydroxy-, CAS:34764-22-2, MF:C4H8O3, MW:104.10 g/mol | Chemical Reagent |
The journey of biomaterials from inert structural replacements to dynamic, bioactive interfaces underscores a profound advancement in medical science. This comparison elucidates a clear dichotomy: metallic biomaterials are unparalleled for applications demanding high strength and fatigue resistance under load, while polymeric biomaterials offer unparalleled versatility, biodegradability, and the potential for sophisticated bio-instructive function. The future of the field lies not only in the continuous refinement of these individual material classes but also in the strategic development of hybrid and composite systems. By harnessing the strengths of both metals and polymers, researchers can create next-generation biomaterials that more perfectly recapitulate the complex mechanical and biological properties of native tissues, thereby improving patient outcomes across a vast spectrum of medical applications.
The selection of materials for biomedical applications, such as implants, stents, and tissue engineering scaffolds, hinges on a fundamental understanding of their intrinsic mechanical properties. These properties are dictated by the material's internal structure, from the type of atomic bonds to the microstructural architecture developed during processing. Within the field of biomaterials research, a central comparison lies between metallic alloys and synthetic polymers, two classes of materials with profoundly different characteristics. This guide provides an objective, data-driven comparison of metallic versus polymeric biomaterials, framing their performance within the context of their atomic bonding and microstructural foundations. It is designed to equip researchers and scientists with the experimental data and methodologies necessary for informed material selection in drug development and medical device innovation.
The global biomaterials market, a domain heavily reliant on these material classes, is projected to grow significantly, underscoring their critical role in advancing human health. These materials are integral to devices that repair or replace physiological functions, with key requirements including biocompatibility, appropriate mechanical properties, and controllable degradation rates for temporary implants. The interplay between a material's chemical structure, its processing history, and its resulting microstructure ultimately determines its success in a biological environment [11].
Atomic and Microstructural Fundamentals
The divergent mechanical behaviors of metals and polymers originate from the nature of their atomic and molecular bonds, which in turn dictate their microstructural organization.
Metallic Biomaterials: The structure of metals is defined by a crystalline lattice held together by metallic bonding, where valence electrons are delocalized and form a "sea" around positively charged ion cores. This bonding allows for plastic deformation without fracture, as planes of atoms can slide past one another via dislocations. This microstructure can be tailored through alloying and thermomechanical processing to control grain size and phase distribution. For instance, in titanium alloys, the stability of the alpha (HCP) and beta (BCC) phases, governed by the Molybdenum Equivalency (MoE), is a primary determinant of mechanical properties like strength and elastic modulus [12]. The quantum mechanical model of atomic structure explains how the arrangement of electrons in atoms leads to these strong, non-directional bonds [13].
Polymeric Biomaterials: Polymers are composed of long-chain molecules based on a carbon backbone, with chains held together by strong covalent bonds along their length and weaker secondary bonds (van der Waals forces, hydrogen bonding) between them. Their properties are heavily influenced by the degree of crystallinity and the glass transition temperature (Tg). A semi-crystalline polymer like Poly-l-lactic acid (PLLA) has regions of ordered chains (crystalline domains) embedded in a disordered amorphous matrix. Below its Tg, the amorphous regions are rigid and glassy; above it, they become flexible. The degradation of bioresorbable polymers like PLLA occurs primarily through hydrolysis of the covalent ester bonds in the backbone, a process that progresses from amorphous to crystalline regions [14].
The following diagram illustrates how these fundamental building blocks give rise to the observed material properties.
Comparative Mechanical Properties
The intrinsic differences in bonding and microstructure manifest as distinct mechanical performance profiles. The following tables provide a quantitative comparison of key properties.
Table 1: Comparative Mechanical Properties of Metallic and Polymeric Biomaterials
| Material | Young's Modulus (GPa) | Tensile Strength (MPa) | Flexural Modulus (GPa) | Strength-to-Weight Ratio | Key Characteristics |
|---|---|---|---|---|---|
| Metallic Biomaterials | |||||
| Titanium (Ti-6Al-4V) | 107 [15] | 900-1200 [16] | ~107 [15] | Extremely High (107) [16] | High strength, excellent corrosion resistance, biocompatible. |
| Cobalt-Chromium Alloys | N/A | N/A | N/A | N/A | Very high wear resistance, used in joint replacements. |
| Stainless Steel 316L | 193-200 [15] | 505-700 [16] | ~200 [15] | High (51) [16] | High strength, ductility, cost-effective. |
| Magnesium Alloys | N/A | 180-350 [16] | N/A | Very High (105) [16] | Biodegradable, low radiopacity, fast degradation. |
| Polymeric Biomaterials | |||||
| PLLA (Poly-l-lactic acid) | ~3.5 [14] | 50-70 [14] | 2.5-4.0 [17] [14] | N/A | Biodegradable, transparent, good biocompatibility. |
| PEEK (Polyether ether ketone) | 3.6-4.1 [15] | 90-100 | 3.6-4.1 [15] | N/A | High-performance, radiolucent, excellent chemical resistance. |
| UHMWPE (Ultra-high-molecular-weight polyethylene) | 0.5-1.5 | 39-48 | ~0.7 [17] | N/A | High wear resistance, used in bearing surfaces. |
| Nylon (PA 6, PA 66) | 2.5-3.5 [15] | 80-90 | 1.0-3.0 [17] | N/A | Tough, wear-resistant. |
Table 2: Clinical Performance and Degradation Profile
| Parameter | Metallic Biomaterials (e.g., Mg Alloys) | Polymeric Biomaterials (e.g., PLLA) |
|---|---|---|
| Biodegradation Mechanism | Corrosion (electrochemical) [14] | Hydrolysis (chain scission) [14] |
| Degradation Rate | Relatively fast (months) [14] | Slow (years); tunable via crystallinity & MW [14] |
| Degradation By-products | Metal ions (e.g., Mg²âº), hydrogen gas [14] | Lactic acid, enters Krebs cycle [14] |
| Radial Strength (in stents) | Good, allows for thinner struts [14] | Requires thicker struts to match metal strength [14] |
| Key Clinical Challenge | Potential for premature loss of mechanical support [14] | Thick struts can affect deliverability and flow [14] |
Experimental Protocols for Characterization
Robust experimental protocols are essential for generating comparable data on material properties. Below are standardized methodologies for key mechanical tests.
Tensile Testing for Young's Modulus (ASTM E8/E8M)
The Young's Modulus, or tensile modulus, is a fundamental property measured under uniaxial tension [15].
- Objective: To determine the stiffness of a material by measuring the relationship between tensile stress and strain within the elastic region.
- Procedure:
- A standardized dog-bone-shaped specimen is gripped in a universal testing machine.
- A controlled, increasing uniaxial tensile load is applied until the specimen yields or fractures.
- The elongation of a specific gauge length is measured using an extensometer.
- Data Analysis: Engineering stress (σ = Force / Original Cross-sectional Area) is plotted against engineering strain (ε = Change in Length / Original Gauge Length). Young's Modulus (E) is calculated as the slope of the initial linear-elastic portion of the stress-strain curve: E = σ / ε [15].
- Standards: ASTM E8/E8M (Standard Test Methods for Tension Testing of Metallic Materials), ISO 6892-1.
Three-Point Bending Test for Flexural Modulus (ASTM D790)
The flexural modulus measures a material's stiffness when subjected to bending forces, which is critical for many load-bearing applications [17] [18].
- Objective: To quantify a material's resistance to bending deformation.
- Procedure:
- A rectangular test bar is placed on two support spans, creating a specified length (L) between them.
- A loading nose applies a force (F) at the midpoint of the supports, deflecting the specimen at a constant rate.
- The test is continued until a set deflection (e.g., 5% as per ASTM D790) or specimen breakage is reached [17].
- Data Analysis: The flexural modulus (Ef) is calculated from the slope (m) of the linear portion of the load-deflection curve using the formula: Ef = (L³m) / (4bd³) where b is the width and d is the thickness of the specimen [17].
- Standards: ASTM D790 (Standard Test Methods for Flexural Properties of Unreinforced and Reinforced Plastics and Electrical Insulating Materials), ISO 178.
The workflow for this standard test is outlined below.
The Scientist's Toolkit: Research Reagent Solutions
A selection of essential materials, testing equipment, and software is critical for research in this field.
Table 3: Essential Research Tools for Biomaterials Characterization
| Tool / Material | Function | Example Use-Case |
|---|---|---|
| Universal Testing Machine | Applies controlled tensile, compressive, or flexural loads to measure mechanical properties. | Performing ASTM D790 three-point bend tests on PLLA scaffolds. |
| Titanium (Ti-6Al-4V) Alloy | A gold-standard metallic biomaterial for orthopedics due to its high strength, low modulus, and biocompatibility. | Control material for comparing mechanical performance of new biodegradable alloys. |
| Poly-l-lactic Acid (PLLA) Resin | A primary biodegradable polymer for fabricating temporary implants and tissue engineering scaffolds. | Studying the effect of molecular weight on the degradation rate and strength retention. |
| Talc Fillers (High Aspect Ratio) | Reinforcing filler for polymers to increase stiffness (flexural modulus). | Improving the load-bearing capacity of polyolefin-based composite biomaterials [17]. |
| Scanning Electron Microscope (SEM) | Provides high-resolution imaging of material microstructure, surface topography, and fracture surfaces. | Analyzing the fracture mechanism of a failed tensile specimen or observing polymer porosity. |
| Differential Scanning Calorimeter (DSC) | Measures thermal transitions such as glass transition temperature (Tg) and melting point (Tm). | Determining the crystallinity of a processed PLLA sample, which influences its degradation rate. |
| WebPlotDigitizer Software | Data extraction tool for digitizing data points from published graphs and images in literature. | Compiling mechanical property data from historical publications for meta-analysis [12]. |
| Acridinium, 9,10-dimethyl- | Acridinium, 9,10-dimethyl-|High-Purity Reagent | |
| Butyrophenonhelveticosid | Butyrophenonhelveticosid, CAS:35919-82-5, MF:C39H52O9, MW:664.8 g/mol | Chemical Reagent |
The selection of materials for biomedical implants is a critical decision that directly influences the success of medical interventions, from orthopedic implants to vascular scaffolds. The mechanical properties of these materials must be carefully matched to their biological environment to ensure both functionality and biocompatibility. This guide provides a comprehensive comparison of the key mechanical metrics—strength, modulus, ductility, and hardness—between two principal classes of biomaterials: metals and polymers. Understanding these properties is fundamental for researchers and material scientists developing next-generation medical devices, as mechanical mismatch can lead to complications such as stress shielding, implant failure, or adverse biological responses.
The inherent conflict between various mechanical properties presents a significant challenge in biomaterial design. For instance, high strength and low modulus are often mutually exclusive yet concurrently needed for optimal implant performance [19]. A low Young's modulus helps mitigate stress shielding—a phenomenon where the implant bears most of the load, leading to bone resorption and eventual implant loosening [20] [19]. Simultaneously, high yield strength ensures the implant can withstand physiological loads without permanent deformation [19]. This guide systematically compares metallic and polymeric biomaterials across these critical mechanical parameters, supported by experimental data and testing methodologies relevant to biomedical applications.
Comparative Analysis of Key Mechanical Properties
The mechanical behavior of biomaterials is characterized through standardized testing protocols that evaluate their response to applied forces. The following section provides a detailed comparison of metallic and polymeric biomaterials across four fundamental mechanical properties, supported by quantitative data from recent research.
Table 1: Mechanical Properties of Metallic Biomaterials
| Material Class | Specific Alloy/Type | Young's Modulus (GPa) | Tensile Strength (MPa) | Elongation at Break (%) | Key Applications |
|---|---|---|---|---|---|
| Titanium Alloys | Ti-10Nb-5Ta | ~40-50 [20] | >600 [19] | Not Specified | Dental implants |
| Titanium Alloys | Ti-13Nb-5Ta | ~40-50 [20] | >600 [19] | Not Specified | Dental implants |
| Complex Concentrated Alloys (CCAs) | Ti-Zr-Hf-Nb-Ta-Mo-Sn | 40-50 [19] | 600-915 [19] | Not Specified | Orthopedic implants |
| Magnesium Alloys | WE43 | 40-50 [21] | 220-330 [21] | 2-20 [21] | Bioresorbable stents |
| Stainless Steel | 316L | 193 [21] | 668 [21] | 40 [21] | Permanent stents, implants |
| Cobalt-Chromium | Co-Cr | 210 [21] | 235 [21] | 40 [21] | Load-bearing implants |
Table 2: Mechanical Properties of Polymeric Biomaterials
| Material Class | Specific Type | Young's Modulus (GPa) | Tensile Strength (MPa) | Elongation at Break (%) | Key Applications |
|---|---|---|---|---|---|
| PLLA (Polymer) | Semi-crystalline PLLA | 2-4 [21] [22] | 60-70 [21] | 2-6 [21] | Bioresorbable scaffolds |
| PLA (Polymer) | PLA Ingeo 4043D | 3.6 [22] | ~53 [22] | Not Specified | 3D printed medical devices |
| PLA Composite | PLA + 15wt% DE (Injection Molded) | Up to 4.65 [22] | Reduced vs. pure PLA [22] | Reduced vs. pure PLA [22] | Engineered biomedical constructs |
| PLA Composite | PLA + Metal Particles | 3.5-4 [23] | 50-70 [23] | Not Specified | Tissue engineering scaffolds |
| PDLLA | Amorphous PDLLA | 1-3.5 [21] | 40 [21] | 1-2 [21] | Drug delivery systems |
| PCL | Polycaprolactone | 0.34-0.36 [21] | 23 [21] | >4000 [21] | Soft tissue engineering |
Elastic Modulus: The Stiffness Factor
The elastic modulus (Young's modulus) quantifies a material's stiffness and its ability to resist elastic deformation under applied load. This property is particularly crucial for load-bearing implants to prevent stress shielding, where the implant bears most of the load, leading to bone resorption and eventual implant loosening [20].
Metallic biomaterials typically exhibit high modulus values, with stainless steel and cobalt-chromium alloys ranging from 193-210 GPa [21]. This is significantly higher than human cortical bone (7-30 GPa) [23], creating substantial modulus mismatch. Advanced titanium-based alloys like Ti-Nb-Ta systems and complex concentrated alloys (CCAs) have been developed with lower moduli (40-50 GPa) to better match bone mechanical properties [20] [19].
Polymeric biomaterials generally possess substantially lower modulus values. Semi-crystalline PLLA, used in bioresorbable vascular scaffolds, has a modulus of 2-4 GPa [21], while amorphous PDLLA is even lower (1-3.5 GPa) [21]. The modulus of polymeric materials can be enhanced through reinforcement strategies; for instance, adding 15wt% diatomaceous earth (DE) to semi-crystalline PLA increased its modulus to approximately 4.65 GPa [22].
Strength: Yield and Tensile Strength
Strength represents a material's resistance to permanent deformation and fracture, with yield strength indicating the onset of plastic deformation and tensile strength representing the maximum stress before fracture.
Metallic biomaterials generally offer superior strength properties. Stainless steel 316L exhibits a tensile strength of 668 MPa [21], while newly developed CCAs can achieve yield strengths of 600-915 MPa with lower modulus [19]. Magnesium alloys like WE43 provide intermediate tensile strength (220-330 MPa) [21] with the advantage of biodegradability.
Polymeric biomaterials demonstrate more moderate strength characteristics. Semi-crystalline PLLA used in vascular applications has a tensile strength of 60-70 MPa [21], while commercial PLA grades range between 45-53 MPa [22]. Reinforcement strategies can enhance these properties; metal particle-reinforced PLA composites show improved tensile strength compared to pure PLA [23], though the enhancement is highly dependent on interfacial bonding and filler distribution.
Ductility: Elongation at Break
Ductility, measured as elongation at break, indicates a material's ability to undergo plastic deformation before fracture, which is crucial for processing and certain implant applications like balloon-expandable stents.
Metallic biomaterials typically exhibit good ductility, with stainless steel 316L and cobalt-chromium alloys showing approximately 40% elongation [21]. Magnesium alloys display more variable ductility (2-20%) [21], reflecting their sensitivity to processing conditions and alloy composition.
Polymeric biomaterials show wide variation in ductility. Polycaprolactone (PCL) exhibits exceptional ductility with elongation exceeding 4000% [21], while PLLA is relatively brittle (2-6% elongation) [21]. Amorphous PDLLA shows even lower ductility (1-2% elongation) [21]. The addition of fillers generally reduces ductility; increasing diatomaceous earth content in PLA composites decreases elongation at break while increasing stiffness [22].
Hardness and Other Properties
Hardness represents a material's resistance to localized plastic deformation, which correlates with wear resistance—an important property for articulating joint replacements.
While specific hardness values for all materials weren't provided in the search results, metallic biomaterials generally exhibit superior hardness and wear resistance compared to polymers. The Vickers microhardness of newly developed Ti-Nb-Ta alloys is characterized as part of their comprehensive evaluation [20]. Polymeric biomaterials like PLA have relatively low surface hardness, which can be improved through composite strategies [23].
For bioresorbable materials, degradation behavior becomes a critical additional property. PLLA degrades over >24 months via hydrolysis of ester bonds, progressing from molecular weight reduction to mass loss and eventual resorption [21]. Magnesium alloys degrade more rapidly, typically within 3-12 months [21], with the challenge of controlling corrosion rates to match healing timelines.
Experimental Protocols for Biomaterial Characterization
Tensile Testing for Elastic Modulus and Strength
Tensile testing is the primary method for determining key mechanical properties including elastic modulus, yield strength, tensile strength, and ductility.
Protocol Overview: Tensile tests are performed according to international standards such as ISO 527-1 for plastics [22]. Specimens are machined or molded into standardized dog-bone shapes with specific gauge dimensions. The test involves applying uniaxial tension at a constant crosshead speed until fracture occurs.
Key Methodology Details:
- Specimens are conditioned at standard temperature and humidity before testing
- Strain is measured using extensometers or strain gauges for accurate modulus calculation
- Multiple specimens (typically n≥5) are tested to ensure statistical significance
- Tests are conducted at physiological temperature (37°C) for biomaterials
Data Analysis: The resulting stress-strain curve provides:
- Elastic Modulus: Calculated from the initial linear slope of the curve
- Yield Strength: Determined using the 0.2% offset method
- Tensile Strength: Maximum engineering stress on the curve
- Elongation at Break: Permanent strain at fracture
For composite materials like PLA + diatomaceous earth, tensile testing reveals how filler content affects mechanical properties, showing linear increases in stiffness but reductions in maximum tensile strength and elongation with increasing filler content [22].
Microhardness Testing
Microhardness testing evaluates a material's resistance to localized plastic deformation using diamond indenters under low loads.
Protocol Overview: The Vickers hardness test is commonly used for biomaterials, employing a pyramidal diamond indenter [20].
Key Methodology Details:
- Samples are meticulously polished to a mirror finish using progressively finer abrasives, with final polishing using 0.05 μm alumina powder [20]
- A load of 1000 gf is typically applied for 10 seconds [20]
- Multiple measurements are taken across the sample surface to account for heterogeneity
- For composites, measurements are taken in different phases to characterize reinforcement effects
Data Analysis: The Vickers hardness number (HV) is calculated from the indentation diagonals measured optically. Higher values indicate greater resistance to deformation.
Electrochemical Testing for Corrosion Behavior
Electrochemical testing is crucial for evaluating biomaterial stability in physiological environments, particularly for biodegradable metals and implants.
Protocol Overview: A standard three-electrode electrochemical cell system is used, consisting of a working electrode (test material), reference electrode (typically saturated calomel electrode), and counter electrode (platinum) [20].
Key Methodology Details:
- Tests are conducted in simulated body fluid (SBF) at pH 7.45 and 37°C to mimic physiological conditions [20]
- Multiple techniques are employed:
- Open Circuit Potential (OCP): Measures the steady-state corrosion potential
- Potentiodynamic Polarization: Scans potential to determine corrosion rates
- Electrochemical Impedance Spectroscopy (EIS): Evaluates interface characteristics and degradation processes
- Multiple measurements (n≥3) ensure statistical validation [20]
Data Analysis: Corrosion rates are calculated using Tafel extrapolation from polarization curves, while EIS data provides information about surface films and degradation mechanisms.
Advanced Research Tools and Reagent Solutions
Contemporary biomaterials research utilizes specialized reagents, materials, and computational tools to design and characterize novel materials with optimized mechanical and biological properties.
Table 3: Essential Research Reagents and Materials for Biomaterials Development
| Reagent/Material | Function/Application | Research Context |
|---|---|---|
| Poly-L-lactic Acid (PLLA) | Base polymer for bioresorbable scaffolds | Vascular scaffolds, orthopedic implants [21] |
| Ti-xNb-5Ta Alloys | Low-modulus titanium alloy system | Dental implants, load-bearing orthopedic applications [20] |
| Diatomaceous Earth (DE) | Silica-based reinforcement for polymers | PLA composite stiffening agent [22] |
| Simulated Body Fluid (SBF) | In vitro corrosion and degradation testing | Electrochemical evaluation of biomaterials [20] |
| Kroll's Reagent | Metallographic etching for microstructure | Revealing microstructure of titanium alloys [20] |
| Tin(II) Octoate (Sn(Oct)â‚‚) | Catalyst for ring-opening polymerization | PLA synthesis and processing [23] |
| Arc Melting System | Preparation of alloy ingots | Development of novel metallic biomaterials [20] |
Computational Design Tools
Machine learning approaches have emerged as powerful tools for multi-objective optimization of biomaterials. The XGBoost algorithm has been successfully applied to simultaneously predict Young's modulus and yield strength in complex concentrated alloy systems, enabling the design of materials with optimized modulus-strength combinations [19].
Key Features in ML Models:
- Electronic descriptors: Electronegativity, electron affinity, ionization energies
- Atomic descriptors: Atomic radius, size mismatch, lattice distortion energy
- Thermodynamic descriptors: Mixing enthalpy, configurational entropy, melting temperature
- Empirical parameters: VEC, Mo equivalent, bond order (Bo), d-orbital energy level (Md) [19]
These computational tools allow researchers to navigate the complex compositional space of multi-component alloys more efficiently than traditional trial-and-error approaches.
The comparative analysis of metallic and polymeric biomaterials reveals distinct advantages and limitations for each class. Metallic biomaterials generally provide superior strength, hardness, and fatigue resistance, making them suitable for permanent load-bearing applications. Advanced alloys, particularly titanium-based systems and complex concentrated alloys, offer improved modulus matching with biological tissues. Polymeric biomaterials, particularly biodegradable polyesters like PLLA, provide advantages in temporary implants where gradual load transfer to healing tissue is desired, with the additional benefit of eliminating long-term foreign body presence.
The emerging frontier in biomaterials development involves composite approaches and advanced manufacturing techniques. Metal-reinforced PLA composites attempt to bridge the property gap between these material classes [23], while additive manufacturing enables complex geometries tailored to patient-specific anatomy [22] [23]. Computational design tools, particularly multi-objective machine learning models, are accelerating the development of next-generation biomaterials with optimized mechanical-biological performance [19]. As research advances, the integration of material science, computational design, and advanced manufacturing will continue to produce innovative solutions to clinical challenges in regenerative medicine and medical device development.
The performance and longevity of biomedical implants are fundamentally governed by their interactions with the biological environment, primarily through the dual critical axes of biocompatibility and corrosion resistance. These properties determine the host tissue response and the material's structural integrity over time. For researchers and drug development professionals, understanding this biological interface is essential for selecting and developing next-generation implant materials. This guide provides a objective comparison between metallic and polymeric biomaterials, framing their performance within the broader context of mechanical properties research. It synthesizes current experimental data and methodologies to offer a clear, evidence-based resource for the scientific community.
The imperative for this comparison stems from a fundamental clinical challenge: the mismatch in mechanical properties between implant materials and native human tissue, which can lead to complications such as stress-shielding and implant failure [24]. Furthermore, the degradation profiles of materials—whether the slow, corrosive release of ions from metals or the controlled, enzymatic breakdown of polymers—directly influence their biocompatibility and functional lifespan [25] [26]. This analysis delves into the specific mechanisms, testing protocols, and performance data that define how metallic and polymeric systems navigate this complex interface.
Metallic Biomaterials: Performance and Data
Metallic biomaterials are predominantly used for load-bearing orthopaedic and dental applications due to their superior fatigue resistance, high strength-to-weight ratio, and excellent machinability [24] [27]. However, their performance is critically dependent on resisting corrosion in the harsh physiological environment and mitigating adverse biological reactions to corrosion byproducts.
Corrosion Mechanisms and Biocompatibility
The primary threat to metallic implants is localized corrosion, including pitting and fretting corrosion, which is accelerated by the complex, chloride-rich environment of the human body [27]. This process releases metal ions (e.g., Al, V, Co, Cr) that can provoke toxic responses, inflammatory reactions, and bone resorption, ultimately leading to aseptic loosening [24] [20]. The body's response to wear and corrosion debris often initiates a macrophage-mediated immune response, which can cause bone erosion (osteolysis) around the implant [24]. Therefore, the biocompatibility of metals is intrinsically linked to the stability and protectiveness of their surface passivation films.
Advancements in Alloy Design
Research has pivoted towards developing novel alloys that minimize these risks. Strategies include using non-toxic alloying elements like Nb, Zr, Ta, and Sn, and exploring new alloy systems such as Medium/High Entropy Alloys (M/HEAs) [27]. These designs aim to achieve a lower elastic modulus closer to that of bone to reduce stress shielding, while enhancing corrosion and wear resistance through unique microstructural properties [27] [20].
Table 1: Corrosion Performance of Selected Metallic Biomaterials
| Material | Experimental Environment | Corrosion Rate / Key Metric | Key Findings | Source |
|---|---|---|---|---|
| Ti40Zr40Nb5Ta12Sn3 MEA | Artificial Saliva (AS), Saline Buffer (SB), Simulated Body Fluid (SBF) | Superior corrosion resistance in AS; Metastable pitting in SBF | Passivation film in AS most stable. SBF's complex composition degrades film stability. | [27] |
| Ti-xNb-5Ta Alloys | Simulated Body Fluid (SBF) | Corrosion resistance improves with increasing Nb content. | Higher Nb content promotes stable passive film formation. | [20] |
| Mg-0.3Sr-0.4Mn (SM04) Alloy | In vitro biodegradation | 0.39 mm/year (54% reduction vs. SM0 alloy) | Optimal Mn content refines grains and improves corrosion resistance. | [28] |
Key Experimental Protocols for Metals
Standardized electrochemical tests are crucial for evaluating metallic biomaterials.
- Open Circuit Potential (OCP): Measures the inherent corrosion tendency of the material in a solution over time. An increasing OCP indicates the formation of a stable passivation film [27].
- Potentiodynamic Polarization: Scans through a range of potentials to determine key parameters like corrosion current density and breakdown potential, which quantify corrosion rate and resistance to pitting [27] [20].
- Electrochemical Impedance Spectroscopy (EIS): Assesses the protective quality and stability of the passive film on the metal surface by measuring its impedance to a range of AC frequencies [20].
Polymeric Biomaterials: Performance and Data
Polymeric biomaterials offer a distinct set of advantages, primarily their versatility in synthesis, ability to be biodegradable, and the capacity to mimic the properties of natural soft tissues [25]. Their biological interface is defined less by ionic release and more by their degradation products, surface chemistry, and mechanical mismatch.
Biocompatibility and Degradation Profiles
The biocompatibility of polymers is heavily influenced by their origin. Natural polymers (e.g., collagen, chitosan, hyaluronic acid) derive their excellent biocompatibility from their structural similarity to the native extracellular matrix (ECM), which minimizes chronic inflammation and immunological rejection [25]. Their degradation is typically controlled by enzymes [25]. Conversely, synthetic polymers (e.g., PLA, PGA, PCL, PEG) offer superior and tunable mechanical properties and reproducible, controlled degradation rates, but they often lack innate cell adhesion sites and may trigger immune responses, necessitating chemical modification [25].
A key challenge is the mechanical property mismatch between synthetic polymers and natural tissues, which can lead to inadequate load-bearing or adverse tissue responses [29]. Furthermore, the viscoelastic behavior of polymers means their mechanical properties are time-dependent, complicating long-term performance prediction under cyclical physiological loads [29].
Advanced Polymeric Systems
The field is advancing through the development of hybrid natural-synthetic systems, hydrogels with tunable mechanical properties, and nanocomposite polymers [25] [29]. These approaches aim to combine the bioactivity of natural polymers with the mechanical robustness and reproducibility of synthetic ones. For example, hydrogels can be engineered to match the stiffness of various soft tissues, while incorporating nanoparticles can significantly enhance the tensile strength and fracture toughness of polymers for load-bearing applications [25] [29].
Table 2: Mechanical & Biological Performance of Biomedical Polymers
| Polymer Class | Key Properties | Degradation Mechanism | Biocompatibility Considerations |
|---|---|---|---|
| Natural Polymers(e.g., Collagen, Chitosan) | Low mechanical strength, variable batch-to-batch. | Enzyme-controlled degradation in vivo. | Inherently high; mimics native ECM. Low chronic inflammation. |
| Synthetic Polymers(e.g., PLA, PLGA, PCL) | Tunable strength & degradation rate, high reproducibility. | Hydrolysis (controlled by polymer chemistry). | Can lack cell adhesion sites; may require surface modification. |
| Hydrogels(e.g., PEG-based) | Adjustable stiffness & elasticity, high water content. | Often responsive to stimuli (pH, temperature). | Can be designed to be non-immunogenic; excellent for soft tissue mimicry. |
Key Experimental Protocols for Polymers
Mechanical and biological testing for polymers addresses their unique characteristics.
- Dynamic Mechanical Analysis (DMA): Characterizes the viscoelastic behavior of polymers by applying oscillating forces, measuring properties like storage and loss moduli across a range of temperatures or frequencies [29].
- In Vitro Degradation Studies: Polymers are incubated in phosphate-buffered saline (PBS) or simulated body fluid at 37°C. Mass loss, molecular weight change, and mechanical property retention are tracked over time to predict in vivo performance [25].
- Cell Function Assays: Beyond viability, assays like alkaline phosphatase (ALP) activity are used quantitatively (e.g., with p-nitrophenyl phosphate) to assess the material's ability to promote osteogenic differentiation of stem cells, a key marker of bioactivity [28] [20].
Direct Comparison and Discussion
The choice between metallic and polymeric biomaterials is not a matter of superiority, but of application-specific suitability. The core trade-off lies between the high strength and toughness of metals and the tailorable degradation and potential for bioactivity of polymers.
The Stress Shielding Dilemma
A central theme in biomechanics is the elastic modulus mismatch. Metals like CoCrMo and Ti6Al4V have a Young's modulus (~110 GPa and ~110-120 GPa, respectively) significantly higher than human cortical bone (~10-30 GPa) [24] [30]. This disparity causes stress shielding, where the implant bears most of the load, leading to bone resorption and implant loosening [24]. While novel beta titanium alloys can achieve a lower modulus (~40-80 GPa), it remains higher than bone [24] [20]. Polymers, with a wider range of moduli, can be engineered to better match soft tissues, but their strength is often insufficient for major load-bearing bones.
Degradation: Corrosion vs. Controlled Resorption
The degradation pathways are fundamentally different. Metal degradation (corrosion) is an electrochemical process that can release toxic ions and particulate debris, provoking adverse biological reactions [24] [26]. In contrast, biodegradable polymers are designed to resorb through hydrolysis or enzymatic activity, and their degradation products can be metabolized. The ideal biodegradable metal, magnesium, occupies a middle ground, releasing non-toxic Mg²⺠ions that may actually promote bone formation, but controlling its rapid corrosion remains a challenge [28].
Table 3: Direct Comparison of Metallic vs. Polymeric Biomaterials
| Property | Metallic Biomaterials | Polymeric Biomaterials |
|---|---|---|
| Typical Young's Modulus | 40-200 GPa (often much higher than bone) | 0.1 MPa - 10 GPa (wide range, tunable) |
| Primary Degradation Form | Electrochemical Corrosion (ion release) | Hydrolysis/Enzymatic Degradation |
| Key Biocompatibility Concern | Inflammatory response to ions & wear debris | Inflammatory response to degradation products or lack of bioactivity |
| Primary Strength | High tensile & fatigue strength; Fracture toughness | Tunable strength; Good resilience for soft tissues |
| Biological Interaction | Typically bio-inert; surface can be functionalized | Can be designed to be bioactive or bio-instructive |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Reagents and Materials for Biomaterial Interface Research
| Reagent/Material | Function in Research | Example Use Case |
|---|---|---|
| Simulated Body Fluid (SBF) | In vitro solution mimicking ionic composition of human blood plasma. | Accelerated testing of apatite formation (bioactivity) and corrosion/degradation. |
| Phosphate Buffered Saline (PBS) | Isotonic buffer with stable pH. | Standard medium for in vitro degradation studies and as a control in biocompatibility tests. |
| Cell Culture Media (e.g., DMEM) | Nutrient-rich medium supporting cell growth. | Used in cytocompatibility assays to culture osteoblasts (e.g., MC3T3-E1) or stem cells (hBMSCs). |
| CCK-8 Assay Kit | Colorimetric kit for quantifying cell viability and proliferation. | Measures the metabolic activity of cells seeded on material extracts or surfaces. |
| p-Nitrophenyl Phosphate (pNPP) | Substrate for alkaline phosphatase (ALP) enzyme. | Used in semi-quantitative analysis of ALP activity, a key marker of osteogenic differentiation. |
| Kroll's Reagent | Etchant for titanium and its alloys. | Used in metallographic preparation to reveal microstructure for optical microscopy. |
| Potentiodynamic Polarization Setup | Standard three-electrode cell (working, reference, counter). | Electrochemical testing to determine corrosion rates and pitting susceptibility. |
| N-Acetylglycyl-D-alanine | N-Acetylglycyl-D-alanine | High-purity N-Acetylglycyl-D-alanine for research applications. This product is For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| 6-Methylhept-1-en-3-yne | 6-Methylhept-1-en-3-yne, CAS:28339-57-3, MF:C8H12, MW:108.18 g/mol | Chemical Reagent |
The field of biomedical implants is fundamentally defined by a material's relationship with the biological environment over time, creating a clear spectrum from permanent to fully transient devices. On one end, permanent implants are designed from biostable materials such as cobalt-chromium alloys, stainless steels, and certain titanium alloys, which remain in the body indefinitely to provide lifelong structural support for load-bearing applications like joint replacements [24]. These materials prioritize mechanical longevity, corrosion resistance, and biocompatibility over decades of service. Occupying the middle ground, bioactive implants interact with biological systems to promote healing while undergoing minimal degradation themselves; surface-modified metals and certain ceramics fall into this category, enhancing osseointegration through controlled surface interactions without significant bulk degradation [24]. At the far end of the spectrum, fully bioresorbable implants represent the most transformative approach, constructed from materials engineered to safely dissolve after fulfilling their temporary mechanical and biological functions [31]. These transient scaffolds—including magnesium-based alloys, polymers like polylactic acid (PLA) and poly(lactic-co-glycolic acid) (PLGA), and emerging hybrid systems—eliminate the need for secondary removal surgeries and can actively promote tissue regeneration by gradually transferring load to healing tissues and releasing bioactive substances during degradation [31] [32].
The fundamental thesis governing material selection in this spectrum revolves around the critical balance between mechanical properties and degradation kinetics. Metallic biomaterials generally provide the structural integrity required for load-bearing applications but have traditionally faced challenges with biodegradability, while polymeric materials offer superior degradation tunability and biological compatibility but often lack the mechanical strength for demanding orthopedic applications [31] [25] [24]. This comparison guide objectively examines the experimental data and performance metrics of metallic versus polymeric biomaterials across this biodegradability spectrum, providing researchers with a structured framework for material selection based on mechanical requirements, degradation timelines, and intended clinical applications.
Material Classes and Their Position on the Biodegradability Spectrum
Metallic Biomaterials
Metallic implants dominate applications requiring high load-bearing capacity and structural integrity, with their biodegradability characteristics varying significantly based on composition.
Permanent Metallic Implants: Traditional orthopedic implants utilize metals prized for their biostability and mechanical performance. Commercially pure titanium and Ti-6Al-4V alloy exhibit excellent corrosion resistance due to a stable surface oxide layer, with Young's modulus values ranging from 110-120 GPa—still significantly higher than cortical bone (10-30 GPa) but lower than other metals [12] [24]. CoCrMo alloys provide exceptional wear resistance necessary for articulating surfaces, with high strength (ultimate tensile strength > 900 MPa) and a Young's modulus of approximately 230 GPa, while stainless steel (316L) offers cost-effective manufacturing with good mechanical properties [24]. The primary limitation of these permanent metallic implants is the stress-shielding effect, where the significant modulus mismatch with bone leads to reduced mechanical stimulation of surrounding tissue, potentially causing bone resorption and implant loosening over time [24].
Biodegradable Metallic Implants: Emerging biodegradable metals represent a paradigm shift toward transient implant technology. Magnesium alloys demonstrate exceptional promise with their bone-like modulus (41-45 GPa), biocompatibility, and ability to completely degrade in physiological environments [31]. Magnesium's degradation rate can be tailored through alloying (with zinc, calcium, or rare earth elements) and processing techniques, creating implants that maintain mechanical integrity during initial bone healing (3-6 months) before gradually dissolving [31]. Similarly, iron and zinc-based alloys offer alternative degradation profiles, with zinc alloys typically degrading slower than magnesium but faster than iron [31]. These materials actively support the healing process during degradation, with in vivo studies showing enhanced osteogenesis and bone formation around degrading magnesium implants compared to inert counterparts [31].
Advanced Metallic Systems: Recent research explores niobium-based alloys as intermediate options, leveraging niobium's excellent corrosion resistance, biocompatibility, and lower elastic modulus (69-103 GPa) compared to traditional titanium alloys [33]. While not fully biodegradable, these alloys address stress-shielding concerns while maintaining long-term stability. Additionally, porous metallic structures created through advanced manufacturing techniques like 3D printing further reduce effective modulus while promoting bone ingrowth [24].
Polymeric Biomaterials
Polymeric biomaterials offer unparalleled versatility in degradation rate tuning and biological functionalization, positioning them predominantly at the biodegradable end of the spectrum.
Synthetic Biodegradable Polymers: This category provides precise control over degradation kinetics and mechanical properties. PLGA stands as the most extensively researched polymer system, with degradation rates controllable from weeks to months by adjusting the lactic to glycolic acid ratio [25] [32]. Polylactic acid (PLA) and polycaprolactone (PCL) offer longer degradation timelines (months to years), with mechanical properties suitable for various applications from sutures to bone fixation devices [25]. The key advantage of synthetic polymers is their reproducible manufacturing and tailorable properties, though they often require surface modification to enhance cell adhesion and may trigger mild inflammatory responses in certain applications [25].
Natural Polymers: Derived from biological sources, natural polymers excel in biological recognition and biocompatibility. Collagen, fibrin, chitosan, and silk fibroin provide innate cell adhesion motifs and enzymatic degradation pathways that closely mimic the natural extracellular matrix [31] [25]. For instance, silk fibroin scaffolds have demonstrated remarkable efficacy in enhancing the proliferation of bone marrow stem cells and chondrocytes in vitro [31]. However, these materials typically exhibit inferior mechanical properties compared to synthetic systems and face challenges with batch-to-batch variability during production [25].
Hybrid and Composite Systems: The most significant advancement in polymeric biomaterials involves creating hybrid natural-synthetic systems that leverage the strengths of both material classes [25]. These composites combine the mechanical robustness and manufacturing consistency of synthetic polymers with the bioactivity and biocompatibility of natural polymers. For example, PLGA-chitosan composites have been developed for nerve guidance conduits, demonstrating enhanced cellular interactions while maintaining structural integrity during the critical healing period [31] [25].
Table 1: Comparative Mechanical Properties of Metallic vs. Polymeric Biomaterials
| Material Class | Specific Examples | Young's Modulus (GPa) | Tensile Strength (MPa) | Degradation Timeline | Key Applications |
|---|---|---|---|---|---|
| Permanent Metals | Ti-6Al-4V [24] | 110-125 | 860-900 | Non-degradable | Joint replacements, dental implants |
| CoCrMo Alloy [24] | 200-230 | >900 | Non-degradable | Femoral heads, articulating surfaces | |
| 316L Stainless Steel [24] | 190-200 | 500-700 | Non-degradable | Fracture fixation, temporary devices | |
| Biodegradable Metals | Magnesium Alloys [31] | 41-45 | 250-350 | 3-12 months | Bone fixation, cardiovascular stents |
| Zinc Alloys [31] | 90-110 | 200-300 | 12-24 months | Cardiovascular stents, bone implants | |
| Iron-based Alloys [31] | 180-200 | 300-500 | >24 months | Bone defect scaffolds | |
| Synthetic Polymers | PLGA [25] [32] | 1.5-4.0 | 40-70 | Weeks to months | Drug delivery, tissue scaffolds |
| PLA [25] | 2.5-4.0 | 50-70 | 6 months to 2 years | Bone screws, sutures | |
| PCL [25] | 0.2-0.5 | 20-40 | 2-4 years | Soft tissue engineering | |
| Natural Polymers | Collagen [25] | 0.002-0.05 | 1-10 | Days to weeks | Wound healing, skin regeneration |
| Chitosan [25] | 0.5-2.0 | 20-40 | Weeks to months | Wound dressings, cartilage repair | |
| Silk Fibroin [31] | 5-15 | 50-100 | Months to years | Ligament repair, bone scaffolds |
Experimental Data and Performance Comparison
Mechanical Performance Under Physiological Conditions
The mechanical compatibility of implant materials with native tissues represents a critical performance metric, particularly for load-bearing applications. Experimental data compiled from extensive studies on Ti-alloys reveals a critical relationship between elastic modulus and β-phase stability, with metastable β-Ti alloys achieving moduli as low as 45-65 GPa—significantly closer to cortical bone (10-30 GPa) than conventional titanium alloys [12]. This reduction in modulus directly addresses the stress-shielding phenomenon, with in vivo studies demonstrating improved bone remodeling around lower modulus implants [24].
For biodegradable materials, the retention of mechanical properties during the degradation process presents the fundamental challenge. Experimental protocols typically involve monitoring mechanical properties of samples immersed in simulated body fluid (SBF) at 37°C over time. Magnesium alloys exhibit the most favorable initial mechanical properties among biodegradable metals, with AZ31 alloy maintaining approximately 80% of its yield strength after 28 days in SBF [31]. However, polymeric systems generally demonstrate more predictable degradation profiles, with PLGA scaffolds showing a linear relationship between molecular weight decrease and strength reduction over 12 weeks in physiological conditions [25].
Table 2: Degradation Characteristics and Biological Response of Biomaterials
| Material Type | Degradation Rate Control | Primary Degradation Byproducts | Tissue Response | Strength Retention During Degradation |
|---|---|---|---|---|
| Magnesium Alloys [31] | Composition, processing, coating | Mg(OH)â‚‚, Hâ‚‚ gas | Mild inflammation, enhanced osteogenesis | 60-80% at 4 weeks (varies by alloy) |
| Zinc Alloys [31] | Composition, microstructure | Zn²⺠ions, ZnO | Minimal inflammation, promotes mineralization | >80% at 12 weeks |
| Iron Alloys [31] | Composition, porosity | Fe²âº/Fe³⺠ions, oxides | Minimal inflammation, slow tissue integration | >90% at 24 weeks |
| PLGA [25] [32] | LA:GA ratio, molecular weight | Lactic acid, glycolic acid | Mild to moderate inflammation, predictable healing | 50-70% at 4 weeks (varies by composition) |
| PLA/PCL [25] | Crystallinity, molecular weight | Carboxylic acids, alcohols | Minimal to mild inflammation | 70-90% at 12 weeks |
| Natural Polymers (e.g., Silk) [31] | Crosslinking, structure | Amino acids, peptides | Excellent integration, minimal immune response | Highly variable based on processing |
Advanced Functional Integration
The convergence of material science with biomedical engineering has enabled sophisticated multifunctional implants that combine structural support with therapeutic capabilities. A pioneering example is the fully bioresorbable hybrid opto-electronic neural implant system, which integrates Mo/Si bilayer electrodes for neural recording with PLGA waveguides for optogenetic stimulation [32]. This system exemplifies the potential of transient implants, performing simultaneous electrophysiological monitoring and optical stimulation in mouse models for 2 weeks before complete biodegradation within 8 weeks [32].
The experimental methodology for such advanced systems involves layer-by-layer fabrication using transfer printing and soft lithography techniques, with precise control over material interfaces to prevent delamination during operation [32]. Performance validation includes in vitro degradation monitoring in phosphate-buffered saline at 37°C, electrochemical impedance spectroscopy for electrode functionality, and photoelectric artifact testing to ensure signal fidelity during optical stimulation [32]. In vivo assessment in transgenic mouse models demonstrates the system's capability to record evoked local field potentials while providing optogenetic stimulation, with histological analysis confirming minimal glial scarring and complete absorption of degradation products [32].
Experimental Methodologies for Biomaterial Evaluation
Standardized Testing Protocols
Mechanical Characterization: Standard ASTM protocols govern the mechanical evaluation of biomaterials. Tensile testing (ASTM E8/E8M) determines yield strength, ultimate tensile strength, and elongation at fracture using standardized dog-bone specimens tested at physiological temperature (37°C) in simulated body fluid when assessing biodegradable materials [12]. Compression testing (ASTM E9) evaluates performance under compressive loads relevant to orthopedic applications. Nanoindentation provides localized mechanical property mapping, particularly useful for composite and porous structures [12]. For fatigue assessment, specimens undergo cyclic loading at physiological frequencies (1-5 Hz) in simulated body fluid until failure or reaching 10 million cycles, with results presented as stress-number of cycles (S-N) curves [24].
Degradation Analysis: Immersion testing in simulated body fluid (SBF) at 37°C and pH 7.4 remains the standard for evaluating biodegradation kinetics [31]. Mass loss measurements at regular intervals quantify degradation rates, while solution analysis via inductively coupled plasma spectroscopy tracks ion release profiles. Electrochemical techniques including potentiodynamic polarization and electrochemical impedance spectroscopy provide accelerated corrosion data, with established correlations to actual in vivo performance [31] [33]. Surface characterization pre- and post-degradation using scanning electron microscopy, energy-dispersive X-ray spectroscopy, and profilometry documents morphological and compositional changes [33].
Biological Compatibility Assessment: In vitro cytotoxicity testing follows ISO 10993-5 standards, using direct contact and extract methods with fibroblast and osteoblast cell lines [24]. Cell adhesion and proliferation assays quantify cellular response to material surfaces, while specialized differentiation assays (alkaline phosphatase activity, calcium deposition) evaluate osteogenic potential [24]. Animal implantation studies in relevant models (rat femoral condyle, rabbit tibia) provide in vivo degradation and tissue response data, with histological scoring of inflammation, fibrosis, and tissue integration at multiple time points [31] [24].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Biomaterials Investigation
| Category | Specific Reagents/Materials | Research Function | Key Characteristics |
|---|---|---|---|
| Base Materials | Medical-grade Ti-6Al-4V, Mg-Zn-Ca alloys, PLGA (75:25), High-purity collagen | Fundamental implant fabrication | Controlled composition, reproducible properties, documented purity |
| Characterization Reagents | Simulated Body Fluid (SBF), Phosphate Buffered Saline (PBS), Alamar Blue, MTT assay kits | Degradation studies and biocompatibility screening | Standardized formulations, validated protocols, quantitative output |
| Cell Culture Systems | MC3T3-E1 osteoblast precursor cells, L929 fibroblasts, Human mesenchymal stem cells (hMSCs) | In vitro biocompatibility and functionality assessment | Well-characterized response, relevance to implant environment |
| Animal Models | Sprague-Dawley rats, New Zealand White rabbits, Transgenic mice (e.g., Thy-1: ChR2) | In vivo performance and degradation analysis | Established surgical models, predictable healing response |
| Analytical Tools | Scanning Electron Microscopy with EDS, ICP-OES, Electrochemical Impedance Spectroscopy | Material characterization and degradation monitoring | High sensitivity, quantitative data generation, surface specificity |
| 4-Azido-2-chloroaniline | 4-Azido-2-chloroaniline, CAS:33315-36-5, MF:C6H5ClN4, MW:168.58 g/mol | Chemical Reagent | Bench Chemicals |
| 2-Bromo-1,1-diethoxyoctane | 2-Bromo-1,1-diethoxyoctane, CAS:33861-21-1, MF:C12H25BrO2, MW:281.23 g/mol | Chemical Reagent | Bench Chemicals |
Material Selection Framework and Future Directions
The selection between metallic and polymeric biomaterials depends on a balanced consideration of mechanical requirements, degradation timeline, biological functionality, and manufacturing feasibility. The following decision framework visualizes the critical selection pathway for researchers navigating the biodegradability spectrum:
The field of biodegradable implants continues to evolve through several key research frontiers. Hybrid material systems that combine the mechanical advantages of metals with the biodegradability and bioactivity of polymers represent the most promising direction [31] [25]. These include polymer-coated magnesium alloys with controlled degradation profiles and natural-synthetic polymer composites with graded mechanical properties. Advanced manufacturing technologies, particularly 3D and 4D printing, enable patient-specific implants with complex architectures that optimize the balance between mechanical support and biodegradability [31] [24]. Surface functionalization techniques that incorporate bioactive molecules (peptides, growth factors) onto biodegradable scaffolds create implants that actively direct the healing process while gradually transferring load to regenerating tissues [24]. Finally, multifunctional implant systems that combine structural support with sensing, stimulation, and drug delivery capabilities represent the cutting edge of transient medical devices [32].
As research progresses, the distinction between permanent and transient implants continues to blur, with functionally graded materials that exhibit controlled transitions from structural to degradable regions. The future of biomedical implants lies not in a single material solution, but in rationally designed material systems precisely engineered across the biodegradability spectrum to address specific clinical needs and healing timelines.
From Bench to Bedside: Application-Oriented Performance in Medical Devices
Orthopedic implants are critical for restoring function and alleviating pain in millions of patients suffering from musculoskeletal injuries and degenerative diseases. The global orthopaedic implant market, projected to reach $79.5 billion by 2030, reflects the substantial demand for these devices [34]. The fundamental purpose of load-bearing implants—including joint replacements, fracture fixation plates, and spinal implants—is to withstand the complex mechanical forces encountered during daily activities while facilitating biological integration and long-term stability. However, the mechanical environment presents significant challenges, as inadequate load-bearing capacity can lead to catastrophic failure through mechanisms such as implant fracture, loosening, or stress shielding that compromises surrounding bone [34].
The ongoing debate in biomaterials research centers on selecting optimal materials that balance mechanical performance with biological compatibility. Metallic biomaterials have historically dominated load-bearing applications due to their exceptional strength and fatigue resistance, but they present limitations including stress shielding, ion release, and artifacts in medical imaging [34] [11]. Polymeric biomaterials offer advantages such as radiolucency and modulus closer to bone, though their mechanical strength often remains inferior to metals [14]. This comparison guide objectively examines the mechanical properties, experimental methodologies, and clinical performance of metallic versus polymeric biomaterials for orthopaedic applications, providing researchers with a comprehensive framework for material selection and development.
Material Classes and Key Properties
Metallic Biomaterials
Metallic biomaterials represent the most extensively used class in load-bearing orthopaedic applications, with a service lifetime of approximately twenty years [11]. These materials are preferred for their excellent mechanical strength, durability, and biocompatibility under demanding physiological conditions [34]. Titanium and its alloys have gained prominence due to their favorable strength-to-weight ratio, corrosion resistance, and elastic modulus lower than stainless steel or cobalt-chromium alloys, thus reducing stress shielding effects [34] [12]. Advanced β-Ti alloys with molybdenum, niobium, and tantalum as alloying elements have been developed to further decrease elastic modulus to levels closer to bone (10-30 GPa) while maintaining strength [12]. Magnesium alloys represent an emerging category of biodegradable metallic materials that offer the potential to eliminate secondary removal surgeries, though their rapid degradation kinetics in physiological environments requires careful alloying and surface modification to match resorption rates with bone healing [34].
Polymeric Biomaterials
Polymeric biomaterials provide distinct advantages for orthopaedic applications, including radiolucency, lighter weight, and elastic modulus closer to bone, which helps reduce stress shielding [34] [25]. Polyether ether ketone (PEEK) has emerged as a leading high-performance polymer for spinal implants and other load-bearing applications due to its excellent mechanical properties, biocompatibility, and inherent radiolucency that enables clear postoperative imaging [34]. Bioabsorbable polymers such as polylactic acid (PLA), polyglycolic acid (PGA), and their copolymers (PLGA) are used for fracture fixation devices that gradually transfer load to healing bone while eliminating the need for hardware removal [34] [11]. Recent advancements in polymer science have led to composite materials such as carbon fiber-reinforced PEEK (CFR-PEEK), which offers enhanced strength and stiffness tailored to match bone's mechanical properties more closely [34]. Natural polymers including collagen, chitosan, and hyaluronic acid are also being investigated for tissue engineering scaffolds, though their mechanical properties generally require reinforcement for load-bearing applications [25].
Table 1: Mechanical Properties of Major Biomaterial Classes for Orthopedic Implants
| Material Category | Specific Materials | Elastic Modulus (GPa) | Tensile Strength (MPa) | Fatigue Strength | Key Clinical Advantages |
|---|---|---|---|---|---|
| Metallic | Titanium Alloys (Ti-6Al-4V) | 110-125 [12] | 860-900 [34] | High | Excellent strength-to-weight ratio, osseointegration |
| Stainless Steel (316L) | 190-200 [34] | 640-750 [34] | High | Cost-effective, high strength | |
| Cobalt-Chromium Alloys | 200-250 [34] | 900-1500 [34] | Very High | Extreme wear resistance | |
| Magnesium Alloys (biodegradable) | 41-45 [14] | 200-300 [14] | Moderate | Biodegradable, prevents stress shielding | |
| Polymeric | PEEK | 3-4 [34] [14] | 90-100 [34] | Moderate | Radiolucent, bone-like stiffness |
| CFR-PEEK | 10-18 [34] | 200-300 [34] | Good | Tailorable anisotropy, strength | |
| UHMWPE | 0.5-1.0 [25] | 30-40 [25] | Moderate | Excellent wear resistance, bearing surfaces | |
| PLLA (bioresorbable) | 2.7-4.1 [14] | 50-70 [14] | Low | Biodegradable, eliminates removal surgery |
Composite and Advanced Biomaterials
Composite biomaterials represent a promising approach to overcome limitations of single-material systems by combining advantageous properties from multiple constituents [34] [11]. Carbon fiber-reinforced PEEK (CFR-PEEK) exemplifies this strategy, marrying PEEK's biocompatibility with carbon fibers for enhanced strength and stiffness closer to bone, while maintaining MRI compatibility for postoperative imaging [34]. Nanocomposites incorporating hydroxyapatite, titanium nanoparticles, or other nanoscale reinforcements offer further opportunities to tailor mechanical properties and biological responses [34] [11]. These advanced materials can be engineered with graded or anisotropic properties that more closely mimic the complex structure of natural bone, potentially reducing stress concentrations and improving long-term performance [34].
Experimental Characterization of Mechanical Properties
Standardized Mechanical Testing Protocols
The mechanical characterization of biomaterials for orthopedic implants follows standardized protocols to ensure reproducibility, clinical relevance, and regulatory compliance. Quasi-static tensile testing according to ASTM F2516 or ISO 7206 standards provides fundamental mechanical properties including elastic modulus, yield strength, ultimate tensile strength, and elongation to failure [35] [12]. For orthopaedic applications, compression testing is equally critical, particularly for materials intended for spinal implants or joint replacement components that experience compressive loads [35]. Fatigue testing conducted per ASTM F1800 or ISO 14879 standards evaluates the material's resistance to cyclic loading, which simulates the physiological loading conditions encountered during walking or other daily activities [35]. Wear testing using pin-on-disk or joint simulators (ASTM F732) is essential for bearing surfaces in joint replacements, where particulate wear debris can trigger inflammatory responses and osteolysis [34].
Specialized Methodologies for Biomaterials
Beyond standard mechanical tests, specialized methodologies have been developed to address the unique challenges of orthopaedic biomaterials. Microcompression and nanoindentation techniques enable mechanical characterization at the microstructural level, providing insights into local variations in properties and their relationship to microstructure [36]. These techniques are particularly valuable for porous scaffolds and surface-modified implants where bulk properties may differ significantly from local characteristics [36]. Atomic force microscopy (AFM) has emerged as a powerful tool for mapping nanomechanical properties of biomaterials and even living cells, with applications in understanding cell-material interactions [36]. For biodegradable materials, immersion testing in simulated body fluids (SBS) at physiological temperature (37°C) and pH (7.4) allows researchers to monitor changes in mechanical properties over time, simulating the degradation process that occurs in vivo [14].
Diagram 1: Comprehensive workflow for mechanical characterization of orthopedic biomaterials, covering from material selection through performance evaluation with key standardized tests.
Computational Modeling Approaches
Computational modeling has become an indispensable tool for complementing experimental characterization of biomaterials. Finite element analysis (FEA) enables researchers to predict stress distributions and potential failure points in complex implant geometries under physiological loading conditions [36]. This approach allows for virtual prototyping and optimization of implant designs before manufacturing, reducing development time and costs [36]. Recent advances in multiscale modeling facilitate the bridging of phenomena across different length scales, from atomic interactions in biomaterials to macroscopic implant performance [36]. Additionally, computational modeling of tissue-scaffold systems helps predict how mechanical stimuli influence tissue regeneration, guiding the design of implants that promote optimal bone ingrowth and remodeling [36].
Table 2: Standard Experimental Protocols for Biomaterial Mechanical Characterization
| Test Method | Applicable Standards | Key Parameters Measured | Clinical Significance | Typical Sample Requirements |
|---|---|---|---|---|
| Tensile Test | ASTM F2516, ISO 6892-1 | Elastic modulus, yield strength, UTS, elongation | Predicts resistance to stretching forces | Dog bone specimens, 3-5 mm diameter |
| Compression Test | ASTM F451, ISO 5832 | Compressive yield strength, modulus | Relevant for spinal implants & joint replacements | Cylindrical specimens, L/D ratio 2:1 |
| Fatigue Test | ASTM F1800, ISO 14879 | Fatigue strength, S-N curves | Predicts long-term durability under cyclic loads | Smooth or notched specimens |
| Hardness Test | ASTM E384, ISO 6507 | Vickers, Rockwell, or Brinell hardness | Correlates with wear resistance | Polished cross-sections |
| Wear Test | ASTM F732, ISO 14242 | Wear rate, friction coefficient | Critical for bearing surfaces in joint replacements | Pin-on-disk or joint simulator |
| Micro-CT Analysis | N/A | 3D pore structure, connectivity | Relates scaffold architecture to bone ingrowth | Small samples (<10 mm cubes) |
Comparative Performance Analysis
Load-Bearing Capacity and Mechanical Stability
The load-bearing capacity of orthopaedic implants is paramount for their clinical success, particularly in lower extremity applications where forces can exceed five times body weight during normal activities. Metallic implants consistently demonstrate superior mechanical properties for high-load applications such as primary hip and knee replacements, with titanium alloys exhibiting tensile strengths of 860-900 MPa and fatigue limits sufficient to withstand millions of loading cycles [34] [12]. The high strength of metals enables thinner implant profiles while maintaining safety margins, which is particularly advantageous for minimally invasive surgical approaches [34]. In contrast, polymeric implants like PEEK exhibit tensile strengths of approximately 90-100 MPa, requiring thicker cross-sections to achieve comparable load-bearing capacity, which can compromise surgical maneuverability and increase bone resection requirements [34] [14]. For fracture fixation plates, metallic materials provide immediate stability necessary for early weight-bearing, though their high stiffness can shield underlying bone from physiological stresses, potentially leading to disuse osteoporosis over time [34].
Bone-Implant Interface and Long-Term Stability
The bone-implant interface critically determines long-term stability and clinical success of orthopaedic implants. Metallic implants typically require surface modifications such as porous coatings, plasma spraying, or bioactive hydroxyapatite coatings to enhance bone integration [34]. Additive manufacturing has enabled the creation of titanium implants with controlled porous architectures that mimic trabecular bone, promoting bone ingrowth and biological fixation [34]. Polymeric materials like PEEK are inherently bioinert and often require surface activation or composite strategies to improve their osteoconductivity [34] [25]. Bioabsorbable polymers such as PLLA facilitate gradual load transfer to healing bone, potentially stimulating more natural bone remodeling, though their initial mechanical strength limits application to low-load scenarios [14]. Surface engineering approaches including nanoscale topographies and bioactive coatings are being applied to both metallic and polymeric implants to create favorable microenvironments for bone cell adhesion, proliferation, and differentiation [34].
Clinical Performance and Complication Profiles
The clinical performance of orthopaedic implants reveals distinct complication profiles for metallic versus polymeric materials. Aseptic loosening remains a primary failure mechanism for metallic implants, often initiated by wear debris-induced inflammation and osteolysis [34]. Metal-on-polyethylene bearing couples generate particulate debris that triggers inflammatory cascades, potentially leading to bone resorption and implant instability [34]. Metallic implants also carry risks of ion release and hypersensitivity reactions in susceptible patients [34]. Polymeric implants mitigate some metal-related complications but introduce different challenges, including potential for polymer debris-induced inflammation and concerns regarding fatigue failure under high-cycle loading [14] [25]. Recent advances in highly cross-linked UHMWPE have significantly improved wear resistance for bearing surfaces, while carbon fiber reinforcement has enhanced the strength and fatigue performance of PEEK constructs [34]. Infection represents a devastating complication for all implant types, spurring development of antimicrobial coatings such as the recently FDA-approved NanoCept technology that utilizes quaternary ammonium compounds to mechanically disrupt bacterial cell walls [34].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials and Reagents for Orthopedic Biomaterials Research
| Item/Category | Specific Examples | Research Function | Key Characteristics |
|---|---|---|---|
| Reference Materials | Ti-6Al-4V ELI, CoCrMo (ASTM F1537), Medical-grade PEEK | Positive controls & calibration | Standardized composition & properties, traceable source |
| Simulated Body Fluids | Phosphate-buffered saline (PBS), SBF (Kokubo recipe) | In vitro corrosion & degradation studies | Physiologically relevant ion concentrations, pH 7.4 |
| Cell Culture reagents | Osteoblast cell lines (MG-63, SaOS-2), Osteoblast Differentiation Media | Biocompatibility assessment | Standardized protocols (ISO 10993), quantify cell viability & differentiation |
| Histological Stains | Alizarin Red S, Von Kossa, Hematoxylin & Eosin (H&E) | Bone formation & mineralization assessment | Specific binding to calcium deposits, visualizes tissue structure |
| Mechanical Testing Equipment | ElectroForce test instruments, Microindentation testers, AFM | Quantification of mechanical properties | Controlled displacement/force, environmental chambers, micro-newton sensitivity |
| Surface Characterization Tools | SEM with EDS, XPS, White Light Interferometry | Surface topography & chemistry analysis | Nanoscale resolution, elemental composition, 3D surface mapping |
| Antibacterial Testing Materials | S. aureus, E. coli cultures, Live/Dead bacterial viability kits | Efficacy evaluation of antimicrobial coatings | Standardized bacterial strains (ISO 22196), quantitative analysis |
| 2-(Decyloxy)benzaldehyde | 2-(Decyloxy)benzaldehyde|C17H26O2|262.39 g/mol | Bench Chemicals | |
| 1,2,3-Triisocyanatobenzene | 1,2,3-Triisocyanatobenzene, CAS:29060-61-5, MF:C9H3N3O3, MW:201.14 g/mol | Chemical Reagent | Bench Chemicals |
Future Directions and Emerging Technologies
The field of orthopaedic biomaterials is rapidly evolving with several promising technologies poised to address current limitations. Additive manufacturing (3D printing) enables patient-specific implants with complex porous architectures that promote bone ingrowth while matching the mechanical properties of native bone [34]. This technology facilitates the creation of functionally graded materials that optimize both biological and mechanical performance across different regions of an implant [34]. "Smart" implants equipped with sensors and wireless connectivity represent another frontier, allowing real-time monitoring of biomechanical parameters and healing progression [34]. These intelligent systems could potentially deliver therapeutic agents in response to specific physiological signals, creating dynamic treatment platforms rather than static implants [34]. Biodegradable metallic materials, particularly magnesium alloys, continue to advance with modified compositions and surface treatments that control degradation rates to match bone healing timelines [34] [14]. The integration of artificial intelligence in implant design processes promises to accelerate the development of optimized structures that would be impossible to create through conventional design approaches [34].
Diagram 2: Decision framework for biomaterial selection based on load-bearing requirements, connecting mechanical demands with appropriate material options.
The comparative analysis of metallic and polymeric biomaterials for orthopaedic implants reveals a complex landscape where material selection represents a series of trade-offs between mechanical performance, biological response, and long-term clinical outcomes. Metallic biomaterials currently dominate high-load applications such as joint replacements and fracture fixation plates where superior strength and fatigue resistance are paramount. However, concerns regarding stress shielding, artifacts in medical imaging, and ion release continue to drive innovation in this space. Polymeric biomaterials offer compelling advantages for specific applications, including radiolucency, bone-like stiffness that reduces stress shielding, and the potential for biodegradability that eliminates the need for removal surgeries. The emergence of advanced composites and additive manufacturing technologies promises to bridge the gap between these material classes, enabling patient-specific implants with functionally graded properties.
Future advancements in orthopaedic biomaterials will likely focus on creating "smart" systems that actively participate in the healing process through controlled drug delivery, biosensing capabilities, and tailored degradation profiles. The integration of bioactive molecules, stem cell technologies, and immunomodulatory strategies represents the next frontier in biomaterial development, potentially leading to implants that not only provide mechanical support but also actively orchestrate tissue regeneration. As these technologies mature, the traditional boundaries between metallic and polymeric biomaterials will continue to blur, giving rise to hybrid systems that leverage the strengths of multiple material classes to achieve optimal clinical outcomes for patients requiring orthopaedic interventions.
The evolution of percutaneous coronary intervention has been marked by the continuous innovation of stent technology, aimed at overcoming the limitations of previous generations. The central dichotomy in contemporary stent design lies between metallic drug-eluting stents (DES) with durable or biodegradable polymers and fully bioresorbable polymeric scaffolds (BRS). Each approach presents a distinct philosophy: metallic DES provide permanent structural support, while polymeric BRS offer temporary scaffolding that subsequently dissolves, potentially restoring natural vascular physiology. This comparison guide objectively analyzes these technologies through the critical lens of mechanical properties, degradation behavior, and clinical performance, providing researchers and drug development professionals with experimental data and methodologies essential for informed evaluation.
Metallic Drug-Eluting Stents (DES)
Metallic DES represent the current clinical mainstay, comprising a permanent metallic backbone—typically cobalt-chromium (CoCr) or platinum-chromium—coated with a thin polymer layer that elutes an anti-proliferative drug (e.g., sirolimus, everolimus) to suppress neointimal hyperplasia [37]. The polymer, which controls drug release kinetics, may be durable (permanent) or biodegradable. The fundamental design principle centers on providing permanent structural support to the vessel wall, with the drug component addressing the primary failure mode of bare-metal stents—in-stent restenosis.
Durable polymer DES (DP-DES) maintain their polymer coating indefinitely, which has been historically associated with persistent inflammatory responses and very late stent thrombosis in first-generation devices [38]. Biodegradable polymer DES (BP-DES) were developed to mitigate this risk; after the drug elutes (typically 3-6 months), the polymer resorbs, leaving behind a bare metal stent intended to reduce long-term polymer-induced inflammation [39] [40].
Polymeric Bioresorbable Scaffolds (BRS)
Polymeric BRS, most commonly fabricated from poly-L-lactide (PLLA) or its copolymers, represent a paradigm shift by providing transient vessel support before fully resorbing over 1-3 years [41] [42]. The core hypothesis is that after the critical period of vessel healing and positive remodeling, the permanent implant becomes superfluous, and its elimination may mitigate long-term complications such as late stent thrombosis, restore vasomotion, and eliminate vessel caging [43].
First-generation BRS faced significant challenges, particularly thick struts (≥150 μm) required to compensate for PLLA's inferior mechanical properties compared to metals, which impeded deliverability and caused disturbed flow dynamics [42]. Next-generation devices are exploring advanced material blends, such as fully amorphous PLLA/PLGA (poly-L-lactide/poly-L-glycolide), to enhance mechanical performance and reduce inflammatory responses [42].
Comparative Mechanical Properties Analysis
The mechanical behavior of stent platforms is paramount to their procedural success and long-term clinical performance. The inherent material properties of metals versus polymers dictate fundamental differences in device design and capability.
Table 1: Fundamental Material Properties Comparison
| Property | Metallic DES (CoCr) | Polymeric BRS (PLLA) | Clinical Significance |
|---|---|---|---|
| Radial Strength | High (>300 MPa UTS) [44] | Moderate (Inferior to metals) [41] | Determines resistance to vessel recoil. |
| Strut Thickness | Thin (∼60-81 μm) [39] | Thicker (≥100-150 μm) [41] [42] | Impacts deliverability, flow disruption, and restenosis risk. |
| Elastic Recoil | Low (<4%) [44] | Higher (requires design mitigation) [41] | Post-deployment lumen loss. |
| Bending Flexibility | Modifiable via stent design [44] | Generally lower due to thicker struts [41] | Ability to navigate tortuous anatomy and conform to vessel curvature. |
Structural Design and Performance Enhancement
Finite Element Analysis (FEA) reveals that strategic geometric modifications can significantly enhance the mechanical performance of polymeric BRS. A 2025 computational study on PLA stents demonstrated that widening the ring bends by 40% (from 0.2 mm to 0.28 mm) increased radial stiffness and radial strength while minimizing elastic recoil, albeit at the cost of reduced bending flexibility [41]. This illustrates the critical trade-offs inherent in BRS design optimization. Furthermore, the same study found that such widening also improved volumetric integrity during degradation, enhancing lumen preservation [41].
For metallic DES, the evolution has focused on alloy refinement, thinner struts, and enhanced polymer/drug kinetics. Modern ultrathin-strut DES (struts <81 μm) have demonstrated excellent clinical outcomes in complex lesions, including left main and bifurcation disease [39].
Degradation Characteristics and Vascular Response
The degradation profile is a critical differentiator with direct implications for vascular healing and long-term safety.
Table 2: Degradation Behavior and Biological Response
| Characteristic | Biodegradable Polymer DES | Polymeric BRS (PLLA) | Notes |
|---|---|---|---|
| Polymer Resorption | 6-9 months [40] [38] | 1-3 years (full mass loss) [41] [42] | BRS requires longer structural integrity. |
| Inflammation Profile | Generally low; varies by polymer [42] | Higher risk with crystalline polymers; improved with amorphous blends (e.g., PLLA/PLGA) [42] | Polymer crystallinity is a key driver of inflammation. |
| Vascular Healing | Favorable, with low stent thrombosis in newer generations [40] | Potential for positive remodeling and late lumen gain post-resorption [42] | "Leave nothing behind" hypothesis is unique to BRS. |
Preclinical Evidence of Enhanced Biocompatibility
Preclinical models are vital for assessing the vascular response to these devices. A 2025 porcine study compared a novel, fully amorphous PLLA/PLGA BRS against crystalline PLLA controls. The PLLA/PLGA scaffold demonstrated a 7.2-fold higher proportion of struts with no inflammation at 30 days and exhibited positive remodeling with significant late lumen enlargement at 90 days (lumen area increased from 1.86 mm² to 3.40 mm², p=0.02) [42]. This underscores how material science advancements—shifting from crystalline to amorphous polymers—can directly address the inflammatory limitations of early BRS.
Clinical Performance Data
Clinical endpoints from randomized trials and registries provide the ultimate measure of a device's safety and efficacy.
Table 3: Comparative Clinical Outcomes from Key Studies
| Study / Device | Follow-up | TLR (%) | MACE (%) | Stent Thrombosis (%) | Notes |
|---|---|---|---|---|---|
| RAIN Registry (BP-DES vs DP-DES) [39] | 16 months | 2.9 vs 3.7 (p=0.22) | 11.6 vs 12.3 (p=0.74) | Not Specified | No significant difference in complex patients. |
| DESTINY Trial (SES vs BES) [40] | 5 years | Component of MACE | 12.5 vs 17.9 (p=0.4) | 0.0 vs 0.0 (Definite/Probable) | Both BP-DES showed excellent long-term safety. |
| Meta-analysis (Various BP-DES) [38] | 1 year | Varied by drug | Not Specified | Not significantly different from PermPol-DES | Performance varies among different BP-DES. |
The RAIN registry, focusing on complex PCI using ultrathin stents, found that BP-DES and DP-DES performed similarly for most endpoints. However, a sensitivity analysis revealed that in complex bifurcations requiring a two-stent strategy, BP-DES were associated with significantly lower MACE (10% vs. 20.4%, p=0.03) and target vessel revascularization (4.6% vs. 12%, p=0.05), suggesting potential advantages in high-risk subsets [39].
Long-term data from the DESTINY randomized trial at five years showed no definite or probable stent thrombosis in the Inspiron sirolimus-eluting BP-DES group and no events after the first year in the Biomatrix Flex biolimus-eluting BP-DES control group, confirming the long-term safety of modern BP-DES [40].
Experimental Protocols for Preclinical Evaluation
Rigorous preclinical assessment is mandatory for regulatory approval and provides critical insights into device performance before clinical trials.
In Vivo Porcine Coronary Stent Model
The domestic swine model is the standard for evaluating stent safety and vascular response [42] [45].
Methodology Details:
- Animal Preparation: Juvenile domestic farm pigs are acclimatized. Pre-medication includes dual antiplatelet therapy (e.g., aspirin and clopidogrel) and anti-spasmodics [45].
- Stent Implantation: Under general anesthesia and via femoral or carotid access, stents are implanted in coronary arteries (LAD, LCx, RCA) with a target overstretch of approximately 10% relative to the reference vessel diameter [42] [45].
- Terminal Endpoints: Animals are sacrificed at predetermined timepoints (e.g., 14, 28, 90 days). Vessels are pressure-perfused with fixative for subsequent analysis [45].
Key Analytical Endpoints:
- Histopathology: Vessels are embedded in resin, sectioned, and stained (e.g., H&E, Verhoeff van Gieson). Morphometric analysis quantifies lumen area, internal elastic lamina (IEL) area, and percent area stenosis. Inflammatory and fibrin scores are assessed semi-quantitatively [45].
- Scanning Electron Microscopy (SEM): Used to evaluate the completeness of endothelial strut coverage at early time points, a key marker of vascular healing and thrombogenic potential [45].
- Optical Coherence Tomography (OCT): Performed in-life at follow-up to assess strut apposition, tissue coverage, and lumen dimensions [42].
In Vitro Degradation and Mechanical Testing
Mechanical Performance Bench Testing: Standards include radial compression testing to measure radial strength and recoil, and three-point bend testing to assess flexibility [44]. In Vitro Dynamic Immersion Test: Stents are immersed in simulated physiological solutions (e.g., Hank's solution) at 37°C, often with dynamic flow conditions. The degradation rate is monitored by measuring mass loss, molecular weight change, and the release of degradation products into the medium over time [44].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for Stent Research
| Item | Function / Application | Examples / Notes |
|---|---|---|
| Polymer Materials | Scaffold fabrication or drug-eluting coating. | PLLA, PLGA: For BRS or biodegradable polymer DES. Amorphous PLLA/PLGA blends show reduced inflammation [42]. |
| Anti-proliferative Drugs | Suppress smooth muscle cell proliferation to prevent restenosis. | Limus family drugs: Sirolimus, Everolimus, Biolimus A9. Paclitaxel: Used in some peripheral DES [37] [38]. |
| Probucol Matrix | Polymer-free excipient for controlled drug release. | Used in novel polymer-free DES to avoid polymer-related complications, showing improved strut coverage [45]. |
| Cell Culture Systems (in vitro) | Assess biocompatibility and cellular responses. | Human vascular endothelial and smooth muscle cells. Must replicate human vasculature for predictive value [46]. |
| Simulated Body Fluid | In vitro degradation and corrosion testing. | Mimics ionic composition of blood; used for dynamic immersion tests to predict in vivo degradation [44]. |
| Staining Reagents (Histology) | Evaluate vascular healing and tissue response. | H&E: General morphology. Verhoeff van Gieson: Elastic laminae. Semi-quantitative scoring for inflammation/fibrin [45]. |
| Thiirane, phenyl-, (R)- | Thiirane, phenyl-, (R)-, CAS:33877-15-5, MF:C8H8S, MW:136.22 g/mol | Chemical Reagent |
| Phosphorothious acid | Phosphorothious acid, CAS:25758-73-0, MF:H3O2PS, MW:98.06 g/mol | Chemical Reagent |
The choice between metallic DES and polymeric BRS involves a complex trade-off between the proven, superior mechanical performance and long-term durability of metals and the theoretical long-term benefits of vascular restoration offered by bioresorbable polymers. Current evidence strongly supports modern metallic BP-DES as the benchmark for safety and efficacy across a wide spectrum of coronary disease. The future of polymeric BRS is contingent upon material science breakthroughs that successfully bridge the mechanical and degradation performance gap. Key research directions include developing stronger, more flexible amorphous polymers, refining stent design via computational modeling to optimize the strength-degradation relationship, and exploring polymer-free metallic DES that eliminate the polymer component entirely. For researchers and developers, the integration of robust preclinical testing—encompassing advanced mechanical bench testing, insightful in vitro degradation models, and comprehensive in vivo histological assessment—remains paramount for guiding the next generation of cardiovascular stent technology.
In the field of tissue engineering, scaffolds serve as temporary three-dimensional structures that mimic the native extracellular matrix (ECM), providing mechanical support and biological cues to guide cell proliferation, differentiation, and new tissue formation [47]. The quest to optimally replicate the mechanical environment of natural tissues represents a fundamental challenge, with the choice between metallic and polymeric biomaterials constituting a central research focus. These material classes offer distinct advantages and limitations in their ability to provide appropriate structural integrity, degradation profiles, and bioactive signaling while matching the mechanical properties of the target tissue [14] [21].
The mechanical properties of a scaffold—including its stiffness, strength, and modulus—directly influence critical biological processes. Stiffness mismatches between implants and native tissues can lead to detrimental effects such as stress shielding in bone applications, where the scaffold bears disproportionate load, effectively shielding the surrounding bone from mechanical stresses and leading to bone resorption [48]. Furthermore, the mechanical environment affects cell adhesion, migration, and differentiation through mechanotransduction pathways [47]. Consequently, the comparison between metallic and polymeric systems extends beyond mere mechanical performance to encompass how these materials integrate with biological systems throughout the tissue regeneration process.
Material Comparison: Metallic vs. Polymeric Biomaterials
Mechanical and Physical Properties
The intrinsic mechanical properties of base materials fundamentally influence scaffold design requirements. Metallic biomaterials generally exhibit superior strength and modulus values compared to biodegradable polymers, which directly translates to differences in scaffold architecture and performance.
Table 1: Mechanical Properties of Biomaterials Used in Tissue Engineering Scaffolds
| Material | Tensile/Young's Modulus (GPa) | Tensile Strength (MPa) | Elongation at Break (%) | Degradation Time |
|---|---|---|---|---|
| PLLA | 2–4 | 60–70 | 2–6 | >24 months |
| PLGA | 1–4.3 | 45 | 1–4 | 1–18 months |
| PCL | 0.34–0.36 | 23 | >4000 | 24–36 months |
| Mg alloy (WE43) | 40–50 | 220–330 | 2–20 | 3–12 months |
| SS 316L | 193 | 668 | 40 | Biostable |
| Co-Cr | 210 | 235 | 40 | Biostable |
Data compiled from polymer and metallic stent research [14] [21]
Metallic materials like stainless steel 316L and cobalt-chromium alloys provide permanent, biostable solutions with high strength and modulus, making them suitable for load-bearing applications [48] [14]. Bioresorbable metals, particularly magnesium alloys, offer an intermediate solution with higher initial strength than polymers and complete degradation over time [21]. Polymeric materials like PLLA, PLGA, and PCL provide significantly lower mechanical properties but offer greater tunability in degradation rates and easier processing into complex porous structures [14] [21].
Scaffold Performance and Architectural Influence
Beyond base material properties, scaffold architecture plays a crucial role in determining overall performance. Different internal designs significantly influence mechanical behavior, permeability, and surface characteristics.
Table 2: Comparison of Scaffold Architectures at Constant Porosity (75-85%)
| Scaffold Type | Compressive Strength (MPa) | Permeability (10â»â¸ m²) | Specific Surface Area | Key Characteristics |
|---|---|---|---|---|
| Sheet TPMS | Higher than skeletal types | Lower than skeletal types | Moderate | Superior mechanical properties, saddle-like curvature |
| Skeletal TPMS | Lower than sheet types | Higher than sheet types | Higher | Greater fluid flow performance |
| MFCC | Intermediate | Intermediate | Higher | Concave spherical pores promoting cell growth |
Data from metallic bone scaffold study using 316L stainless steel [48]
Triply periodic minimal surface (TPMS) scaffolds represent an architecturally advanced approach, with sheet-type structures exhibiting superior mechanical properties while skeletal-types offer enhanced permeability [48]. Modified face-centered cubic (MFCC) scaffolds with spherical concave pores have demonstrated potential as alternatives to TPMS structures, with tunable internal architectures that promote cell growth due to their favorable curvature [48]. The optimal permeability range for bone scaffolds is approximately 0.5–5.0 × 10â»â¸ m², which ensures effective nutrient and waste transfer without causing cell washout [48].
Experimental Protocols for Biomaterial Evaluation
Mechanical Testing Methodologies
Standardized mechanical testing provides critical data for comparing metallic and polymeric scaffold performance. These tests simulate the various loading conditions scaffolds encounter in physiological environments.
Experimental Workflow for Mechanical Characterization
Compressive Testing Protocol
Compressive testing is particularly relevant for bone tissue engineering applications where scaffolds must withstand significant loading forces.
- Sample Preparation: Fabricate cylindrical scaffold specimens (typically 10-15mm height × 10mm diameter) using appropriate manufacturing techniques (e.g., selective laser melting for metallic scaffolds, 3D printing for polymeric scaffolds) [48].
- Testing Conditions: Place specimens in a universal testing machine equipped with compression plates. Maintain physiological temperature (37°C) and immerse in simulated body fluid (SBF) to replicate in vivo conditions [48] [49].
- Loading Protocol: Apply uniaxial compressive load at a constant strain rate (typically 1 mm/min) until specimen failure or deformation reaches 50% of original height [48].
- Data Analysis: Calculate compressive strength from the maximum load sustained before failure. Determine compressive modulus from the slope of the initial linear portion of the stress-strain curve [48].
Flexural Testing Protocol
Flexural strength measures a material's resistance to deformation under bending loads, which is critical for applications experiencing complex loading conditions [50] [51].
- Test Selection: Choose between 3-point and 4-point bending configurations based on material homogeneity. The 3-point test is suitable for homogeneous materials, while the 4-point test is preferred for non-homogeneous materials like composites as it subjects a larger volume to stress [51].
- Specimen Preparation: Prepare rectangular specimens with specific dimensions according to ASTM D790 standards. For scaffold materials, typical dimensions are 80mm × 10mm × 4mm [51].
- Testing Procedure:
- Measurement: Measure deflection at the loading point(s) while applying force at a constant rate. Continue testing until specimen failure or until a predetermined deflection is reached [51].
- Calculations: Calculate flexural strength using standard beam equations. For a 3-point bend setup: σ = (3FL)/(2bd²), where F is the maximum load, L is the support span, b is the specimen width, and d is the specimen thickness [51].
Degradation Assessment Methods
Evaluating biomaterial degradation is essential for predicting in vivo performance and ensuring degradation products are non-toxic and properly metabolized [49].
Biomaterial Degradation Assessment Protocol
In Vitro Degradation Protocol
- Initial Characterization: Before degradation, document initial sample mass, dimensions, mechanical properties, and molecular weight [49].
- Degradation Media: Immerse scaffolds in phosphate-buffered saline (PBS) at pH 7.4 or simulated body fluid (SBF) maintained at 37°C to mimic physiological conditions. For accelerated degradation studies or specific material systems, enzymatic solutions or adjusted pH conditions may be employed [49] [52].
- Sample Maintenance: Change degradation media periodically (e.g., weekly) to maintain constant pH and ion concentrations, preventing saturation of degradation products [49].
- Periodic Assessment: Remove samples at predetermined time points (e.g., 1, 7, 14, 28, 42, and 60 days) for comprehensive analysis [53] [49].
Degradation Measurement Techniques
- Gravimetric Analysis: Rinse retrieved samples with deionized water, dry to constant weight, and measure mass loss percentage: Mass Loss (%) = [(Wâ‚€ - Wâ‚)/Wâ‚€] × 100, where Wâ‚€ is initial mass and Wâ‚ is dry mass after degradation [49].
- Morphological Examination: Examine surface and internal morphology using scanning electron microscopy (SEM) to observe pore structure changes, surface erosion, crack formation, and degradation patterns [48] [49].
- Mechanical Property Monitoring: Track changes in compressive strength, flexural strength, and modulus throughout degradation to determine strength retention profiles [49] [52].
- Chemical Analysis:
- Molecular Weight Changes: Use size exclusion chromatography (SEC) or solution viscosity measurements to track polymer chain scission and molecular weight reduction [49].
- Chemical Structure Analysis: Employ Fourier transform infrared spectroscopy (FTIR) and nuclear magnetic resonance (NMR) to identify chemical bond cleavage and degradation byproducts [49] [52].
- Ion Release Monitoring: For metallic or composite scaffolds, use techniques like inductively coupled plasma spectroscopy to measure metal ion release rates (e.g., Siâ´âº from biosilica composites or Mg²⺠from magnesium alloys) [52].
Biological Integration and Therapeutic Considerations
Bioactivity and Surface Interactions
Surface characteristics and bioactivity significantly influence scaffold integration with native tissues. Surface curvature at the microscale level directly affects cell proliferation and new bone formation, with concave surfaces demonstrating superior tissue regeneration compared to convex and flat surfaces [48]. This understanding has driven the development of advanced architectures like MFCC scaffolds with spherical concave pores and TPMS scaffolds with saddle-like curvatures [48].
The incorporation of therapeutic metallic ions (e.g., cobalt, copper, strontium, zinc, silver) creates opportunities for enhanced biofunctionality. These metallic ions as therapeutic agents (MITAs) can be released during scaffold degradation to stimulate specific cellular responses, including angiogenesis and osteogenesis [47]. For instance, incorporating biosilica from diatoms into PDLGA scaffolds has demonstrated controlled Siâ´âº ion release, which is known to enhance osteogenic activity [52].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Scaffold Evaluation
| Reagent/Material | Function/Application | Research Context |
|---|---|---|
| Poly-L-lactic acid (PLLA) | Biodegradable polymer for scaffold fabrication; provides structural support with tunable degradation | Primary material for polymer-based bioresorbable scaffolds [14] [21] |
| 316L Stainless Steel | Metallic scaffold material with high strength and corrosion resistance | Used in load-bearing bone scaffold applications [48] |
| Magnesium Alloys (e.g., WE43) | Biocorrodible metal with intermediate degradation time and good mechanical properties | Material for metallic bioresorbable scaffolds [21] |
| Phosphate Buffered Saline (PBS) | Simulates physiological ionic environment for in vitro degradation studies | Standard degradation medium for in vitro testing [49] |
| Simulated Body Fluid (SBF) | Mimics ion concentration of human blood plasma for bioactivity assessment | Testing apatite formation on bioactive surfaces [49] |
| Glutaraldehyde | Crosslinking agent for biopolymer scaffolds (e.g., chitosan-gelatin) | Improves mechanical stability and reduces degradation rate [53] |
| Diatom Biosilica | Natural source of silicon for enhancing bioactivity in composite scaffolds | Incorporated into PDLGA to improve mechanical retention during degradation [52] |
| Zeolite | Inorganic additive to improve mechanical properties and stability | Incorporated into chitosan-gelatin scaffolds to enhance cell proliferation [53] |
| Cycloheptane;titanium | Cycloheptane;titanium|Reagent for Research | Cycloheptane;titanium reagent for research (RUO). Explore its applications in organic synthesis and catalysis. For Research Use Only. Not for human use. |
| lithium;4H-quinolin-4-ide | Lithium;4H-quinolin-4-ide|CAS 30412-49-8|Supplier |
The comparison between metallic and polymeric biomaterials for tissue engineering scaffolds reveals a complex landscape where mechanical properties, degradation behavior, and biological activity must be balanced for specific applications. Metallic systems offer superior strength and are advantageous for load-bearing scenarios, with biodegradable magnesium alloys providing an intermediate solution between permanent implants and fully resorbable polymers [14] [21]. Polymeric materials, while mechanically inferior, provide greater tunability of degradation rates and easier functionalization [14] [49].
Advanced architectural designs like TPMS and MFCC structures enable more precise control over mechanical and biological properties regardless of base material [48]. The incorporation of therapeutic ions creates new opportunities for enhancing biofunctionality beyond structural support [47] [52]. As standardization in degradation assessment improves [49], researchers are better equipped to make informed material selections based on comprehensive performance data. The optimal scaffold solution increasingly involves hybrid approaches that combine material strengths with architectural innovation to more effectively mimic the native extracellular matrix.
The advent of advanced manufacturing technologies, particularly 3D printing and additive manufacturing (AM), has revolutionized the development of biomaterials for medical applications. While often used interchangeably, 3D printing typically refers to consumer-focused or prototyping contexts, whereas additive manufacturing encompasses industrial-scale, production-grade technologies used in regulated sectors like healthcare [54]. This technological paradigm enables the layer-by-layer fabrication of complex geometries directly from digital models, offering unprecedented design freedom and customization capabilities for biomedical implants and devices [55].
Within the field of biomaterials research, a fundamental mechanical comparison exists between metallic and polymeric materials, each offering distinct advantages for different clinical applications. Metallic biomaterials typically provide superior strength and durability for load-bearing implants, while polymeric materials offer tunable biodegradation and often better biocompatibility [20] [23]. This guide objectively compares the performance of metallic versus polymeric biomaterials manufactured through advanced AM technologies, providing researchers with experimental data and methodologies to inform material selection for specific biomedical applications.
Comparative Analysis of Metallic and Polymeric Biomaterials
Mechanical Properties of 3D-Printed Polymeric Biomaterials
Polymeric biomaterials, particularly photopolymer resins used in various 3D printing technologies, exhibit significantly different mechanical properties based on the printing technology employed. A recent comparative study evaluated three common vat polymerization technologies: stereolithography (SLA), digital light processing (DLP), and liquid crystal display (LCD) [56].
Table 1: Mechanical Properties of Polymers from Different 3D Printing Technologies
| Property | SLA | DLP | LCD |
|---|---|---|---|
| Flexural Strength (MPa) | 93.39 ± 5.57 | 69.97 ± 8.48 | 64.69 ± 8.98 |
| Surface Hardness (kgf/mm²) | 18.80 ± 0.57 | 17.80 ± 1.85 | 18.27 ± 0.93 |
| Surface Roughness (nm) | 14.79 ± 7.96 | 24.59 ± 9.76 | 89.87 ± 28.26 |
The experimental data reveal that SLA technology produces polymers with significantly superior flexural strength compared to DLP and LCD methods. Furthermore, SLA demonstrates the smoothest surface finish, a critical factor for biomedical applications where surface roughness can influence bacterial adhesion, cellular response, and overall biocompatibility [56].
For biodegradable polymers, polylactic acid (PLA) has gained significant attention due to its biodegradability and biocompatibility. However, neat PLA exhibits limitations for load-bearing applications, with tensile strength of 50–70 MPa, compressive strength of 60–70 MPa, and elastic modulus of 3.5–4 GPa [23]. These properties fall short of human cortical bone requirements, which has motivated the development of reinforced PLA composites.
Mechanical Properties of Metallic Biomaterials for Implants
Metallic biomaterials remain indispensable for load-bearing orthopedic and dental implants where mechanical integrity is paramount. Recent research has focused on developing novel titanium-based alloys with improved biocompatibility and mechanical properties closer to natural bone.
Table 2: Properties of Ti-xNb-5Ta Alloys for Biomedical Implants
| Alloy Composition | Ultimate Tensile Strength (MPa) | Elastic Modulus (GPa) | Elongation at Break (%) | Corrosion Resistance |
|---|---|---|---|---|
| Ti-5Nb-5Ta | Data not available in source | Data not available in source | Data not available in source | Improves with Nb content |
| Ti-7Nb-5Ta | Data not available in source | Data not available in source | Data not available in source | Improves with Nb content |
| Ti-10Nb-5Ta | Exceeds TA4G surgical standard | Lower than conventional Ti alloys | Greater than conventional Ti alloys | Improves with Nb content |
| Ti-13Nb-5Ta | Exceeds TA4G surgical standard | Lower than conventional Ti alloys | Greater than conventional Ti alloys | Improves with Nb content |
The Ti-xNb-5Ta alloy series demonstrates that strategic alloying with niobium and tantalum can create materials that surpass standard surgical implant requirements while offering a lower elastic modulus – a critical factor for reducing stress shielding effects [20]. The corrosion resistance of these alloys improves with increasing niobium content, enhancing their long-term biocompatibility and performance in the physiological environment.
Direct Comparison: Metallic vs. Polymeric Biomaterials
When selecting materials for specific biomedical applications, researchers must consider the fundamental trade-offs between metallic and polymeric systems:
Mechanical Performance: Metallic biomaterials consistently outperform polymers in tensile strength, fatigue resistance, and fracture toughness, making them essential for permanent load-bearing implants [20]. Enhanced polymers like metal-reinforced PLA composites bridge this gap but remain limited to lower-stress applications.
Biocompatibility and Bioactivity: Both material classes can demonstrate excellent biocompatibility. Polymers like PLA degrade into non-toxic byproducts, while properly formulated titanium alloys show exceptional tissue integration with minimal adverse reactions [20] [23].
Manufacturing Considerations: Polymers generally require lower processing temperatures and energy inputs. Material extrusion of PLA occurs at approximately 170-220°C, while metal alloys like Ti-xNb-5Ta require arc-melting and often subsequent thermal treatments [20] [23].
Customization Potential: Both material systems benefit significantly from AM's design freedom. Polymers excel in producing complex scaffolds with fine features, while metals provide durability in patient-specific implants [57] [23].
Experimental Protocols and Methodologies
Methodology for Evaluating 3D-Printed Polymers
The comparative study of SLA, DLP, and LCD technologies followed a rigorous experimental protocol to ensure reliable and reproducible results [56]:
Specimen Preparation:
- Bar-shaped specimens (25 × 2 × 2 mm) were designed for flexural strength testing according to ISO 10477:2020 standards.
- Disc-shaped specimens (9 mm diameter × 2 mm thickness) were fabricated for surface hardness and roughness assessments following ISO 20795-1:2013.
- All specimens were printed with a consistent layer thickness of 50 μm and 90-degree build orientation.
- Post-processing included washing with 99% isopropyl alcohol for 10 minutes using an ultrasonic cleaner, followed by post-curing for 30 minutes at 40°C.
Testing Protocols:
- Flexural Strength: Measured using a universal testing machine with a three-point bending setup, 20 mm span length, and 5 mm/min crosshead speed.
- Surface Hardness: Evaluated using a micro-Vickers hardness tester with a 300 g load applied for 15 seconds.
- Surface Roughness: Quantified using atomic force microscopy with probes having nominal spring constants of 10 N/m and resonance frequencies of 250 kHz.
Statistical Analysis:
- Sample size was determined through a power analysis using G*Power software.
- Data normality was assessed with Shapiro-Wilk test, and variance homogeneity with Levene's test.
- One-way ANOVA and Tukey's post-hoc tests were applied with significance set at p < 0.05.
Diagram 1: Experimental workflow for polymer evaluation
Methodology for Developing and Testing Metallic Alloys
The research on Ti-xNb-5Ta alloys employed metallurgical processing and comprehensive characterization techniques [20]:
Alloy Design and Preparation:
- Alloys were designed using d-electron theory and molybdenum equivalent calculations to target near-β-type titanium alloys.
- Ingots were prepared via arc-melting high-purity elements in an argon atmosphere.
- Each ingot was remelted five times to ensure compositional homogeneity.
- Actual composition was verified according to GB/T 4698 standards.
Material Characterization:
- Microstructural Analysis: Samples were mirror-polished and etched with Kroll's reagent for optical microscopy. Phase constituents were examined using X-ray diffraction.
- Mechanical Testing: Tensile properties and elastic modulus were determined using an electronic universal material testing machine. Vickers microhardness was measured at 1000 gf load for 10 seconds.
- Electrochemical Evaluation: Corrosion performance was assessed in simulated body fluid using open circuit potential, polarization curves, and electrochemical impedance spectroscopy.
- Biological Assessment: In vitro performance was evaluated through CCK-8 assay, ALP semi-quantitative analysis, and RT-PCR to assess osteogenic differentiation of human bone marrow stromal cells.
Diagram 2: Metallic alloy development and testing methodology
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Biomaterials Development
| Material/Reagent | Function | Application Context |
|---|---|---|
| Photopolymer Resins | Base material for vat polymerization | SLA, DLP, and LCD 3D printing of polymeric specimens [56] |
| Polylactic Acid (PLA) | Biodegradable thermoplastic polymer | Material extrusion printing, tissue engineering scaffolds [23] |
| Titanium, Niobium, Tantalum | Metallic elements for alloy development | Arc-melting of novel implant alloys (Ti-xNb-5Ta) [20] |
| Isopropyl Alcohol (99%) | Solvent for post-processing | Cleaning residual resin from 3D-printed polymers [56] |
| Simulated Body Fluid (SBF) | Simulates physiological environment | Corrosion testing and bioactivity assessment [20] |
| Kroll's Reagent | Metallographic etchant | Revealing microstructure of titanium alloys [20] |
| Cell Culture Reagents (CCK-8) | Cell viability assessment | In vitro biocompatibility testing [20] |
| Sydnone, 3-(dimethylamino)- | Sydnone, 3-(dimethylamino)-, CAS:27430-80-4, MF:C4H7N3O2, MW:129.12 g/mol | Chemical Reagent |
| Dihydroxy(oxo)vanadium | Dihydroxy(oxo)vanadium|CAS 30486-37-4|RUO | Dihydroxy(oxo)vanadium for research applications. Explore its use in insulin-mimetic studies, enzyme inhibition, and anticancer research. For Research Use Only. Not for human use. |
The comparative analysis of metallic and polymeric biomaterials for advanced manufacturing reveals a complementary relationship rather than outright superiority of either material class. Metallic biomaterials,
particularly novel titanium alloys like Ti-xNb-5Ta, offer superior mechanical properties for load-bearing applications where strength and fatigue resistance are paramount, while polymeric systems provide advantages in biodegradability, processability, and design flexibility for custom implants and tissue engineering scaffolds.
The choice between material systems ultimately depends on the specific clinical application, mechanical requirements, and desired biological response. Future developments in multi-material additive manufacturing and functional grading may further blur the lines between these material classes, enabling optimized designs that leverage the advantages of both metallic and polymeric biomaterials within a single integrated implant [57] [55]. This evolution will continue to advance personalized medicine through patient-specific implants with tailored mechanical and biological properties.
The field of orthopedic biomaterials is increasingly focused on developing implants that closely mimic the natural properties of human bone to enhance clinical outcomes. Two leading material strategies have emerged: polyether ether ketone (PEEK) polymers for spinal interbody fusion cages and porous titanium alloys for bone substitution. This guide provides a comprehensive, data-driven comparison of these material platforms, framing the analysis within the broader research thesis of metallic versus polymeric biomaterials for orthopedic applications. We examine their fundamental properties, experimental performance data, and clinical outcomes to inform researchers and development professionals in the field.
Material Properties and Design Philosophies
The fundamental distinction between PEEK and titanium alloys lies in their mechanical properties and biological interaction capabilities.
PEEK polymers are high-performance thermoplastics with an elastic modulus (~3.8 GPa) similar to that of cancellous bone, which reduces the risk of stress shielding—a phenomenon where excessive stiffness of the implant shields the surrounding bone from mechanical load, leading to bone resorption [58]. However, PEEK is biologically inert, which can inhibit bone-implant osseointegration, and may be prone to biofilm formation [58].
Porous Titanium Alloys are typically manufactured using additive manufacturing techniques such as selective laser melting (SLM) or electron beam melting (EBM). The key innovation is the introduction of controlled porosity, which serves two critical functions: reducing the effective elastic modulus to match that of cortical bone (thereby mitigating stress shielding) and creating a scaffold for bone ingrowth and vascularization [59] [60]. The elastic modulus of solid titanium alloy (110 GPa) can be reduced to approximately 10 GPa with 35% porosity [59].
Table 1: Fundamental Properties of Biomaterials Compared to Bone
| Material | Elastic Modulus (GPa) | Key Advantages | Inherent Limitations |
|---|---|---|---|
| Cortical Bone | 12-18 [58] | Biological remodeling | Limited healing capacity for large defects |
| Cancellous Bone | 0.1-1.0 [60] | Osteoconductive | Low mechanical strength |
| PEEK | ~3.8 [58] | Radiolucency, bone-like stiffness | Bioinert, inhibits osseointegration |
| Solid Titanium Alloy | 90-115 [60] | Excellent strength, osseointegration | Stress shielding, high stiffness |
| Porous Titanium Alloy | 10-20 [59] [60] | Tunable stiffness, bone ingrowth | Potential for fretting corrosion [61] |
Experimental Data and Performance Comparison
Biomechanical Performance in Spinal Fusion
Finite element analysis and machine learning optimization studies reveal significant differences in biomechanical behavior. Research on titanium-PEEK composite cages demonstrates their ability to effectively reduce stress shielding compared to traditional titanium cages. One study showed that an optimized circular hole inner core (M2) fusion cage reduced the peak von Mises stress in the L4 lower endplate and L5 upper endplate by 54.2% and 27.7%, respectively, compared to a solid titanium device [58]. Furthermore, the strain energy in the M2 model increased by 49.7%, indicating a more favorable transfer of mechanical load to the surrounding bone structures [58].
Table 2: Clinical Outcomes from Meta-Analysis: 3D-Printed Porous Titanium vs. PEEK Cervical Cages
| Outcome Measure | 3D-Printed Porous Titanium | PEEK Cage | P-value | Source/Study |
|---|---|---|---|---|
| Operative Time (min) | Significantly Shorter | Longer | < 0.00001 | [62] |
| Intraoperative Blood Loss (ml) | Significantly Less | More | 0.006 | [62] |
| Hospital Stay (days) | Significantly Shorter | Longer | 0.0001 | [62] |
| Postoperative Complications | Lower Rate (OR: 0.35) | Higher Rate | 0.01 | [62] |
| Fusion Rate (Atlantoaxial) | 100% | 80.6% | Not Significant | [63] |
| Maintenance of Cervical Curvature | Superior | Inferior | < 0.0001 | [62] |
Preclinical Evaluation in Large Animal Models
Preclinical studies in sheep models comparing 3D-printed porous PEEK and 3D-printed titanium cages with posterior instrumentation have shown that both designs support successful interbody fusion when used with autograft [64]. A critical finding is the superior imaging compatibility of 3D-printed PEEK. Its radiolucent nature allows for clear assessment of fusion via radiographs and microCT, whereas 3D-printed titanium cages can appear solid in radiographs and produce significant artifacts in microCT scans, complicating postoperative evaluation [64].
Experimental Protocols and Methodologies
Finite Element Analysis with Machine Learning Optimization
A developed framework integrating finite element (FE) simulation with machine learning provides a robust methodology for optimizing implant design [58].
Figure 1: Integrated Workflow for Intelligent Implant Design. This diagram illustrates the "finite element simulation-machine learning-postoperative model biomechanical validation and evaluation" framework [58].
Detailed Protocol Steps:
- Model Establishment: Obtain CT scan images of the spine (L4-L5 segment) from a healthy volunteer. Import Dicom 3.0 files into Mimics Research 21.0 for 3D surface reconstruction. Use Geomagic Studio for surface smoothing and fitting to create a 3D solid model. Assemble the model in Siemens NX 10.0, establishing intervertebral discs and facet joint cartilage [58].
- Material Property Assignment: Define material properties for various spinal structures as detailed in Table 1 of the source, including cortical bone (12,000 MPa), cancellous bone (100 MPa), and bony endplate (2,000 MPa). Model the annulus fibrosus using a Mooney-Rivlin hyperelastic material model [58].
- Finite Element Simulation: Perform FE compression simulations using Abaqus software. The analysis should simulate physiological loading conditions to calculate stress distributions and strain energy.
- Machine Learning Optimization: Use the simulation data to train a Back Propagation Neural Network (BPNN). The model learns the relationship between the fusion cage's structural parameters (e.g., pore size, strut thickness) and its resulting equivalent elastic modulus. The BPNN then intelligently optimizes these parameters to achieve a target elastic modulus matching cortical bone [58].
- Validation: The optimized designs are implanted into a traditional Posterior Lumbar Interbody Fusion (PLIF) postoperative finite element model for static and transient dynamic analysis to evaluate the biomechanical response [58].
Manufacturing and Characterization of Porous Titanium
Space Holder Technique: This powder metallurgy method involves blending angular Ti powders (e.g., Grade 2) with space-holding particles (e.g., urea). The mixture is uniaxially pressed and then heated to remove the space holder and sinter the titanium, creating a highly porous structure [61].
Additive Manufacturing (Selective Laser Melting - SLM): This process involves four key steps: 1) acquiring patient imaging data (CT/MRI), 2) creating a digital model (CAD) and converting it to STL format, 3) computer-controlled, layer-by-layer melting of titanium alloy powder to print the implant, and 4) post-processing through grinding and surface modification [60].
Mechanical and Tribological Testing: Characterize the elastoplastic properties of the porous samples via compression testing. Furthermore, evaluate the fretting-corrosion behavior in simulated body fluids (e.g., foetal bovine serum) using a triboelectrochemical setup, applying varying normal loads and displacement amplitudes to study the synergy between mechanical wear and electrochemical corrosion [61].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Materials and Reagents for Biomaterials Research
| Item | Function/Application | Specific Examples / Notes |
|---|---|---|
| CP Ti Grade 2 Powder | Raw material for fabricating porous titanium substrates | Particle size D50 = 36 μm [61] |
| Urea Particles | Space holder for creating controlled macro-porosity in titanium | Angular shaped, <500 μm [61] |
| Foetal Bovine Serum (FBS) | Electrolyte for in-vitro tribocorrosion testing | Simulates the organic constituents of body fluid [61] |
| Mooney-Rivlin Model | Hyperelastic material model for simulating soft tissues | Used for annulus fibrosus in finite element models [58] |
| Back Propagation Neural Network (BPNN) | Machine learning algorithm for optimizing implant design parameters | Used to predict and optimize structural parameters for target elastic modulus [58] |
| Autograft | Gold standard bone graft material in preclinical and clinical studies | Used to fill cages in spinal fusion studies [64] |
| (2-Thienyl)-methylsilane | (2-Thienyl)-methylsilane|Research Use Only | (2-Thienyl)-methylsilane is a silane reagent for organic synthesis and materials science research. This product is for Research Use Only. Not for human or veterinary use. |
The comparison between PEEK and porous titanium alloys reveals a trade-off between mechanical compatibility and biological integration. PEEK cages offer an excellent modulus match to bone and superior imaging capabilities, reducing complications like stress shielding and allowing clear postoperative assessment. However, their biological inertness remains a limitation. Porous titanium alloys address this through enhanced osseointegration and bone ingrowth, leading to superior fusion rates and mechanical stability in the long term, albeit with challenges related to imaging artifacts and potential corrosion. The choice between these materials is therefore application-specific. The future of orthopedic implants lies in the continued development of composite structures, such as titanium-PEEK combinations, and the refinement of surface modification techniques, all accelerated by integrated computational approaches like FE-ML frameworks that reduce design cycles and enable patient-specific solutions.
Overcoming Clinical Challenges: Stress Shielding, Degradation, and Failure Analysis
Stress shielding remains a significant challenge in orthopaedic implants, leading to aseptic loosening and implant failure. This phenomenon arises from a mismatch in elastic modulus between native bone and traditional implant materials, causing reduced mechanical stimulation in the surrounding bone tissue and subsequent bone resorption. This review systematically compares metallic and polymeric biomaterials for orthopaedic applications, evaluating their efficacy in mitigating stress shielding through advanced engineering strategies. We examine experimental data on novel material solutions including porous metals, biodegradable alloys, polymer composites, and additive-manufactured structures. The analysis incorporates quantitative mechanical property comparisons, detailed experimental methodologies, and emerging research trends to provide researchers and clinicians with evidence-based guidance for material selection in next-generation orthopaedic implants.
Stress shielding represents a critical biomechanical phenomenon in orthopaedic surgery where high-stiffness implants bear the majority of physiological loads, effectively "shielding" the surrounding bone from its normal mechanical environment [65]. According to Wolff's Law, bone remodeling is exquisitely sensitive to mechanical stimulation, and reduced loading leads to progressive bone resorption through imbalanced osteoclast and osteoblast activity [66] [67]. This bone loss can ultimately result in implant loosening, periprosthetic fracture, and the need for revision surgery, with stress shielding accounting for a substantial proportion of aseptic failures in joint arthroplasty [68] [24].
The fundamental mechanism driving stress shielding is the mismatch in elastic modulus between implant materials and native bone tissue. Cortical bone exhibits a highly anisotropic structure with elastic modulus values ranging from 5-10 GPa transversely to approximately 18 GPa along the longitudinal direction, while trabecular bone modulus can be below 3 GPa [66]. In contrast, conventional metallic implant materials possess substantially higher modulus values: titanium alloys (~116 GPa), cobalt-chromium alloys (~190-230 GPa), and stainless steel (~210 GPa) [66] [67]. This 4-10x stiffness disparity causes implants to carry disproportionate load shares, creating the periprosthetic bone resorption observed in stress shielding [24] [66].
The growing prevalence of joint replacement surgeries amplifies the clinical significance of stress shielding. With primary total hip arthroplasties projected to increase by 284% and knee arthroplasties by 401% by 2040, optimizing implant longevity through improved material selection becomes increasingly imperative [68]. This review comprehensively examines current biomaterials solutions focused on modulus-matching strategies, providing comparative experimental data and methodological insights to guide future research and clinical applications.
The Modulus Mismatch Problem
Fundamental Mechanisms
The biomechanical consequences of modulus mismatch manifest through two primary mechanisms: stress shielding-induced bone loss and stress concentration-induced device failure [66]. When a high-stiffness implant is fixated to bone, it disrupts normal stress-strain trajectories, redirecting mechanical loading along the implant itself rather than through the surrounding bone tissue. This redistribution occurs because the structural stiffness of the implant-bone construct becomes dominated by the implant material, whose higher elastic modulus translates to greater load carriage under identical deformation conditions [65] [66].
Bone remodeling responds to this altered mechanical environment through a coordinated cellular process. Osteocytes embedded within the bone matrix function as mechanosensors, detecting reduced fluid flow and strain energy density under diminished loading [67]. This mechanosensation triggers biochemical signaling that promotes osteoclast differentiation and activity while suppressing osteoblast function, leading to net bone resorption [66] [67]. The resorptive process typically initiates at the endosteal surface, progressively enlarging the medullary cavity and reducing cortical thickness, particularly in regions adjacent to the stiffest portions of implants [65].
Clinical Consequences and Evaluation
The clinical manifestations of stress shielding present significant challenges in orthopaedic practice. Periprosthetic bone loss compromises implant stability through diminished bone-implant contact, increasing susceptibility to micromotion and aseptic loosening [68] [67]. Severe bone resorption also elevates fracture risk during revision procedures or trauma, complicating surgical outcomes [65]. In total hip arthroplasty, characteristic patterns of proximal femoral bone loss occur with distally fixed stems, while retroacetabular stress shielding manifests following press-fit acetabular component implantation [67].
Radiographic assessment remains the primary clinical method for monitoring stress shielding, with computed tomography (CT) and dual-energy X-ray absorptiometry (DEXA) providing quantitative bone mineral density measurements [67]. The Wilkinson classification system divides the retroacetabular region into four zones of interest for standardized BMD tracking, demonstrating the precision required for clinical evaluation of periprosthetic bone changes [67]. Lucent lines visible in profile indicate implant loosening, while more diffuse decreases in bone density beneath implant components suggest stress shielding effects [65].
Figure 1: Stress Shielding Pathway. This diagram illustrates the sequential biological events from implant placement to potential revision surgery, highlighting key mechanisms in stress shielding-induced bone loss.
Material Solutions and Comparative Performance
Metallic Biomaterials: Traditional and Advanced Approaches
Traditional orthopaedic metals including stainless steel, cobalt-chromium alloys, and titanium alloys have dominated load-bearing applications due to their superior strength, fatigue resistance, and biocompatibility [69] [24]. However, their high elastic modulus relative to bone has driven the development of advanced metallic solutions focused on modulus reduction.
Porous metals represent a transformative approach to addressing modulus mismatch. Through additive manufacturing techniques like Laser Powder Bed Fusion, researchers have created lattice structures with controlled porosity that significantly lower effective stiffness [68] [70]. Experimental studies with CoCrMo scaffolds demonstrate that increasing pore size from 500μm to 1000μm enhances mechanical compatibility, with 1000μm porous scaffolds reducing bone strain shielding compared to full-density equivalents [68]. Titanium alloys (particularly Ti6Al4V) have shown superior performance in porous configurations, generating bone strain and reaction forces closer to intact bone than CoCrMo alternatives in finite element analysis [68].
Novel alloy compositions offer another pathway to modulus optimization. Beta titanium alloys incorporating biocompatible elements such as niobium, zirconium, and tantalum demonstrate significantly reduced modulus (55-85 GPa) while maintaining necessary strength [24]. These advanced compositions more closely approximate bone's mechanical properties but face limited clinical adoption due to regulatory hurdles and manufacturing complexities [24].
Table 1: Mechanical Properties of Metallic Biomaterials Compared to Bone
| Material | Elastic Modulus (GPa) | Tensile Strength (MPa) | Compressive Strength (MPa) | Key Advantages | Stress Shielding Concerns |
|---|---|---|---|---|---|
| Cortical Bone | 5-20 (direction-dependent) | 50-150 | 100-200 | Natural tissue | Reference standard |
| Trabecular Bone | 0.1-3 | 1-20 | 2-20 | Natural tissue | Reference standard |
| Stainless Steel (316L) | ~210 | 500-700 | 500-700 | High strength, cost-effective | Severe mismatch (>10x) |
| CoCr Alloys | 190-230 | 600-1500 | 600-1500 | Wear resistance | Severe mismatch (>10x) |
| Ti6Al4V | ~116 | 900-1100 | 900-1100 | Biocompatibility | Moderate mismatch (6-8x) |
| Porous Titanium | 1.5-20 (porosity-dependent) | 100-500 | 100-600 | Modulus tunability | Minimal mismatch possible |
| Beta Ti Alloys | 55-85 | 600-1000 | 600-1000 | Lower modulus | Reduced mismatch (3-5x) |
Polymeric and Composite Biomaterials
Polymeric materials offer inherent advantages in modulus matching due to their lower stiffness profiles. While traditional polymers lack sufficient strength for load-bearing applications, advanced composites and reinforced formulations have expanded their utility in orthopaedic implant design.
Polyetheretherketone (PEEK) possesses an elastic modulus (~3-4 GPa) considerably closer to bone than metals, potentially reducing stress shielding effects [69]. However, its limited osseointegration capacity and wear resistance have restricted widespread adoption in major joint arthroplasty components [69].
Polylactic acid (PLA) biocomposites represent an emerging category with particular relevance to biodegradable applications. PLA's inherent modulus (~3.5-4 GPa) closely approximates the lower range of cortical bone, but its mechanical limitations for load-bearing applications have driven the development of metal-reinforced composites [23]. Incorporating titanium, stainless steel, magnesium, or silver particles enhances tensile strength, durability, and overall mechanical performance while maintaining favorable modulus characteristics [23]. These composites can be processed via additive manufacturing to create patient-specific geometries optimized for mechanical compatibility.
Ultra-high-molecular-weight polyethylene (UHMWPE) remains the gold standard for articulating surfaces in joint arthroplasty due to its exceptional wear characteristics, though its application as a structural component remains limited by creep resistance and long-term deformation concerns [69].
Table 2: Performance Comparison of Polymeric and Composite Biomaterials
| Material | Elastic Modulus (GPa) | Tensile Strength (MPa) | Key Advantages | Limitations | Stress Shielding Potential |
|---|---|---|---|---|---|
| PEEK | 3-4 | 90-100 | Excellent biocompatibility, modulus matching | Poor osseointegration, wear concerns | Low |
| PLA | 3.5-4 | 50-70 | Biodegradable, biocompatible | Brittleness, low impact resistance | Low |
| PLA-Ti Composite | 4-8 (reinforcement-dependent) | 80-120 | Enhanced strength, modulus tuning | Interfacial adhesion challenges | Low to Moderate |
| UHMWPE | 0.5-1.5 | 40-50 | Superior wear resistance | Creep deformation, low strength | Very Low |
| Magnesium Alloys | 41-45 | 150-350 | Biodegradable, modulus matching | Rapid corrosion, gas formation | Moderate |
Bioabsorbable Metals
Bioabsorbable metals represent a revolutionary approach to stress shielding elimination by temporarily providing mechanical support before gradually transferring load to healing bone. Magnesium alloys demonstrate particular promise with an elastic modulus (~41-45 GPa) substantially closer to bone than traditional metals [71]. This improved modulus matching, combined with complete biodegradation, theoretically enables optimal load transfer during the critical bone remodeling phase [72] [71].
Current research focuses on corrosion rate modulation to maintain mechanical integrity during early healing while ensuring complete absorption post-recovery. Surface modifications and alloying with elements like zinc have demonstrated corrosion reduction efficiencies up to 85%, addressing a primary limitation in magnesium-based implants [71]. Iron-based biodegradable metals offer alternative corrosion kinetics but require porosity engineering via additive manufacturing to achieve clinically relevant degradation rates [72].
Experimental Approaches and Methodologies
Standardized Mechanical Testing Protocols
Rigorous mechanical characterization forms the foundation for evaluating stress shielding potential in novel biomaterials. Standardized compression, tension, and fatigue testing according to ASTM and ISO standards provide essential data on yield strength, ultimate tensile strength, elastic modulus, and fatigue resistance [68] [70]. These fundamental properties determine initial implant suitability for load-bearing applications.
For porous structures, compression testing reveals distinctive deformation behavior characterized by three distinct regions: linear elastic response, plastic plateau with pore collapse, and final densification [70]. Testing should be conducted at physiological strain rates (0.001-0.1 sâ»Â¹) to simulate in vivo conditions, with samples hydrated at body temperature (37°C) to account for environmental effects on material performance [68].
Digital Image Correlation for Strain Analysis
Digital Image Correlation (DIC) has emerged as a powerful experimental technique for quantifying strain distributions at bone-implant interfaces [68]. This non-contact optical method tracks the displacement of a stochastic speckle pattern applied to specimen surfaces, generating full-field strain maps with high spatial resolution.
Experimental Protocol:
- Sample Preparation: Fresh-frozen bovine cortical bone specimens are machined to standardized dimensions (e.g., 18 × 18 × 6 mm) with precisely milled cavities for scaffold insertion [68]. Bone samples are maintained hydrated with physiological saline throughout preparation and testing.
- Speckle Pattern Application: A high-contrast random speckle pattern is created using white spray paint background with black speckles, ensuring optimal pattern recognition while minimizing paint penetration into bone pores [68].
- Mechanical Testing with Synchronized Imaging: Bone-implant compounds are loaded under displacement control (0.003 mm/s) in a servo-hydraulic testing machine while a high-resolution monochrome camera captures sequential images at predetermined load increments (e.g., 1000 N increments) [68].
- Strain Analysis: Commercial DIC software (e.g., GOM Correlate) processes image sequences to compute displacement vectors and strain tensors across defined regions of interest (ROI). Multiple ROIs (typically 3×3 mm) enable comprehensive characterization of strain gradients at the bone-implant interface [68].
DIC validation studies demonstrate exceptional repeatability in bone strain measurements, with coefficients of variation below 5% across replicate samples, establishing this methodology as a robust approach for quantifying stress shielding effects in vitro [68].
Figure 2: Experimental Workflow for DIC Strain Analysis. This diagram outlines the key methodological steps in assessing bone-implant mechanical interactions using Digital Image Correlation.
Finite Element Analysis and Computational Modeling
Finite Element Analysis (FEA) provides complementary computational assessment of stress shielding potential, enabling detailed evaluation of complex geometries and loading scenarios difficult to replicate experimentally [68] [66]. Validated against experimental DIC data, FEA models predict stress and strain distributions throughout bone-implant constructs with high spatial resolution.
Advanced modeling approaches incorporate anisotropic bone properties, interfacial conditions, and physiological loading profiles to simulate in vivo performance. Spring-based analytical models offer simplified alternatives for initial assessment of reaction forces and load-sharing characteristics in bone-scaffold compounds [68]. These computational tools enable rapid iteration during the design phase, optimizing pore architecture, material selection, and geometric parameters before physical prototyping.
The Research Toolkit: Essential Materials and Methods
Table 3: Essential Research Reagents and Materials for Stress Shielding Investigation
| Category | Specific Items | Function/Application | Key Considerations |
|---|---|---|---|
| Test Materials | CoCrMo powder (LPBF) | Porous scaffold fabrication | Particle size distribution, flowability |
| Ti6Al4V powder (LPBF) | Porous scaffold fabrication | Oxygen content, sphericity | |
| Magnesium alloys | Biodegradable implant research | Corrosion rate modulation | |
| PLA polymer filament | Polymer composite studies | Molecular weight, crystallinity | |
| Bone Models | Fresh-frozen bovine cortical bone | Biomechanical testing | Age, anatomical location, storage |
| Synthetic bone analogs | Standardized testing | Composition matching, porosity | |
| Cadaveric human bone | Clinical relevance studies | Donor variability, preservation | |
| Testing Equipment | Servo-hydraulic testing machine | Mechanical characterization | Load cell capacity, control accuracy |
| High-resolution monochrome camera | DIC analysis | Resolution, frame rate, stability | |
| Environmental chamber | Physiological conditions | Temperature control, hydration | |
| Software Tools | DIC analysis software (GOM Correlate) | Full-field strain measurement | Algorithm accuracy, processing speed |
| Finite element software (Abaqus, ANSYS) | Computational modeling | Mesh sensitivity, material models | |
| Statistical analysis packages | Data validation | Significance testing, power analysis |
The persistent challenge of stress shielding in orthopaedic implants continues to drive biomaterials innovation toward improved modulus matching with native bone tissue. Traditional metallic implants, while providing excellent mechanical strength, create significant modulus mismatches that precipitate periprosthetic bone resorption. Advanced solutions including porous metals, novel alloy compositions, polymer composites, and biodegradable systems each offer distinct advantages and limitations in addressing this fundamental biomechanical problem.
Experimental evidence confirms that porous titanium scaffolds with optimized architecture (1000μm pores) significantly improve strain transfer to adjacent bone compared to solid implants [68] [70]. Additive manufacturing enables unprecedented control over implant microarchitecture, facilitating patient-specific designs with tuned mechanical properties [72] [67]. Emerging biodegradable materials, particularly magnesium alloys and their composites, present promising opportunities for transient load-bearing applications where gradual load transfer to healing bone is desirable [71] [23].
Future research directions should prioritize long-term in vivo validation of novel material systems, with particular emphasis on the biological response to degradation products and the dynamics of bone remodeling in the presence of modulus-gradient implants. Multifunctional designs incorporating bioactive coatings, drug delivery capabilities, and optimized surface textures for enhanced osseointegration represent the next frontier in orthopaedic biomaterials research. As additive manufacturing technologies evolve and our understanding of bone mechanobiology deepens, the goal of eliminating stress shielding through intelligent material design appears increasingly attainable.
In the field of biomaterials, the long-term performance and safety of medical implants are critically dependent on how the material degrades within the body. For polymeric biomaterials, the primary degradation mechanism is hydrolysis, a chemical process where water breaks the backbone chains of the polymer. For metallic biomaterials, the dominant failure mode is corrosion, an electrochemical process that leads to the oxidation and dissolution of the metal. Both processes determine the functional lifespan of an implant, its integration with biological tissue, and its overall biocompatibility. Understanding and controlling these degradation mechanisms is therefore a fundamental objective in biomaterials research and development [21] [73].
This guide provides a comparative analysis of these degradation pathways. It outlines the underlying mechanisms, summarizes key material properties, details standard experimental methods for evaluation, and presents strategies for controlling degradation rates. The information is structured to serve researchers and scientists engaged in the selection, design, and testing of biomaterials for medical applications.
Hydrolysis in Polymeric Biomaterials
Mechanism and Key Factors
Hydrolysis is the chemical cleavage of polymer chains by water. For the polyesters commonly used in bioresorbable implants, such as poly-L-lactic acid (PLLA), this occurs via a reaction at the ester bonds [21]. The process is influenced by several intrinsic and extrinsic factors:
- Chemical Structure: The identity of the chemical bonds in the polymer backbone is the primary determinant. Ester bonds in polyesters are highly susceptible to hydrolysis, while carbon-carbon bonds in polyolefins are not [74] [75].
- Crystallinity and Morphology: The tightly packed molecular chains in crystalline regions are less accessible to water than the disordered amorphous regions. Therefore, hydrolysis initiates predominantly in the amorphous phases [21].
- Hydrophilicity/Hydrophobicity: Polymers with hydrophilic backbones or side chains allow for greater water penetration, accelerating hydrolysis.
- Molecular Weight: Higher molecular weight polymers generally degrade more slowly as more chain scissions are required to cause significant material loss [75].
The bioresorption of a polymer like PLLA follows a multi-stage process, as illustrated in the workflow below.
Strategies for Controlling Hydrolysis
Material scientists employ several strategies to tailor the hydrolysis rate of polymers for specific applications:
- Copolymerization: Incorporating different monomer units (e.g., glycolide or caprolactone with lactide) disrupts the polymer's crystallinity, making it more accessible to water and altering the degradation profile [21].
- Blending and Additives: The inclusion of acidic or basic additives can catalyze the hydrolysis reaction. Conversely, stabilizers can be added to slow it down [74].
- Material Processing: Techniques like annealing can increase the crystallinity of a polymer, thereby reducing its hydrolysis rate [21].
- Surface Modification: Applying coatings can create a barrier that limits water diffusion to the polymer surface, delaying the onset of bulk degradation.
Corrosion in Metallic Biomaterials
Mechanism and Key Factors
Corrosion is an electrochemical process where a metal oxidizes and dissolves in an aqueous environment. In the human body, this occurs in the presence of electrolytes like chloride ions. The process involves the establishment of anodic (oxidation) and cathodic (reduction) sites on the metal surface [73]. Key factors influencing corrosion include:
- Electrochemical Potential: The inherent tendency of a metal to oxidize, which is fundamental to its position in the electrochemical series.
- Microstructure and Defects: Inhomogeneities in the metal's microstructure, such as grain boundaries or inclusions, can create localized anodic sites, leading to pitting corrosion [73].
- Environmental Conditions: The body's environment is particularly aggressive due to its temperature, pH, and the presence of chloride ions and proteins that can influence corrosion kinetics [73].
- Mechanical Stress: The combination of corrosive environments and cyclic mechanical load can lead to corrosion-fatigue, a common failure mode in load-bearing implants.
Strategies for Controlling Corrosion
Controlling metallic corrosion is essential for implant longevity and biocompatibility. Key protection strategies include:
- Alloying: Creating alloys is a primary method for enhancing corrosion resistance. For example, Magnesium (Mg) alloys are developed for biocorrodible implants, while stainless steels contain chromium, which forms a passive protective layer [21] [73].
- Surface Modifications and Coatings: Applying a protective layer is a highly effective strategy. Recent advances include TiB2 coatings on molybdenum for molten zinc environments, phytic acid-based films on copper foils for batteries, and superhydrophobic surfaces on aluminum created via chemical etching and silane grafting [73].
- Corrosion Inhibitors: These are chemicals that, when added in small concentrations, significantly slow down corrosion. Recent research focuses on biosourced inhibitors, such as oxazoline molecules for carbon steel or Ruta graveolens leaf extract for 304 stainless steel in acidic environments [73].
Comparative Analysis: Data and Methodologies
Quantitative Comparison of Material Properties
The fundamental differences between polymers and metals are reflected in their mechanical and degradation properties, which directly influence their selection for biomedical applications. The table below summarizes key characteristics of common biomaterials.
Table 1: Mechanical and Degradation Properties of Biomaterials
| Material | Tensile Modulus (GPa) | Tensile Strength (MPa) | Elongation at Break (%) | Degradation Time | Key Degradation Mode |
|---|---|---|---|---|---|
| PLLA (Polymer) | 2 - 4 | 60 - 70 | 2 - 6 | >24 months [21] | Hydrolysis |
| PGA (Polymer) | 6 - 7 | 90 - 110 | 1 - 2 | 4 - 6 months [21] | Hydrolysis |
| WE43 (Mg Alloy) | 40 - 50 | 220 - 330 | 2 - 20 | 3 - 12 months [21] | Corrosion |
| SS 316L (Metal) | 193 | 668 | 40 | Biostable [21] | Corrosion (if passive layer fails) |
| Co-Cr (Metal) | 210 | 235 | 40 | Biostable [21] | Corrosion (if passive layer fails) |
Standard Experimental Protocols
Evaluating degradation requires standardized, reproducible experimental protocols. The following methodologies are central to research in this field.
Evaluating Polymer Hydrolysis and Biodegradation
A comprehensive understanding of polymer degradation requires testing that goes beyond traditional standards. A modern sequential workflow that captures both abiotic and biotic phases provides a more complete picture [75].
Table 2: Key Reagents for Polymer Degradation Studies
| Research Reagent | Function/Explanation |
|---|---|
| Phosphate Buffered Saline (PBS) | Simulates the ionic strength and pH of the physiological environment for hydrolysis studies. |
| Marine Microbial Inoculum | A mixed culture of marine bacteria used as the biotic medium to assess biodegradation in marine environments. |
| 1,5,7-triazabicyclo[4.4.0]dec-5-ene (TBD) | An organic catalyst that mediates efficient degradation of condensation polymers via transesterification [74]. |
| Documentation of Dissolved Organic Carbon (DOC) | A critical metric that quantifies the bioavailable carbon released during abiotic degradation, often missed by CO2-only measurements [75]. |
Experimental Workflow Explanation:
- Polymer samples are prepared and characterized for initial mass, molecular weight, and thermal properties.
- The Abiotic Phase involves exposing samples to simulated sunlight to initiate photodegradation, or incubating them in aqueous solutions (e.g., PBS at 37°C) to study hydrolysis. The release of Dissolved Organic Carbon (DOC) is quantified, as this represents a major, often overlooked, degradation product [75].
- The Biotic Phase follows, where the abiotically treated samples are inoculated with a relevant microbial community (e.g., marine inoculum). The system is monitored for microbial consumption of the DOC, conversion into biomass, and ultimate mineralization into CO2.
Evaluating Metallic Corrosion
Electrochemical techniques are the cornerstone of metallic corrosion assessment, allowing for accelerated and predictive testing.
Key Experimental Protocol: Electrochemical Corrosion Testing [73]
- Sample Preparation: Metal specimens are cut to a specific geometry, mounted to define an exposed surface area, and polished to a standardized finish to ensure reproducibility.
- Electrolyte Selection: An appropriate corrosive medium is chosen. For biomedical applications, this is often a simulated body fluid (SBF) or a hydrochloric acid (HCl) solution to simulate an aggressive inflammatory environment.
- Setup: A standard three-electrode cell is used, consisting of:
- Working Electrode: The metal sample under test.
- Reference Electrode: (e.g., Saturated Calomel or Ag/AgCl) to provide a stable potential reference.
- Counter Electrode: (e.g., Platinum) to complete the circuit.
- Testing Techniques:
- Open Circuit Potential (OCP): Measures the steady-state potential of the metal in the electrolyte, indicating its thermodynamic tendency to corrode.
- Potentiodynamic Polarization: The potential of the working electrode is systematically varied, and the resulting current is measured. This data is used to generate a Tafel plot, from which key parameters like corrosion current density (Icorr) and corrosion potential (Ecorr) are extracted.
- Electrochemical Impedance Spectroscopy (EIS): Applies a small AC potential over a range of frequencies to characterize the resistance of the surface film and the corrosion reactions.
Table 3: Essential Reagents for Metallic Corrosion Studies
| Research Reagent | Function/Explanation |
|---|---|
| Simulated Body Fluid (SBF) | A solution with inorganic ion concentrations nearly equal to human blood plasma, used to mimic the in vivo environment. |
| Potentiodynamic Polarization Kit | Standardized electrodes and electrochemical cells for measuring corrosion rates. |
| Ruta graveolens Leaf Extract | An example of a green, biosourced corrosion inhibitor for stainless steel in acidic environments [73]. |
| Phytic Acid Solution | Used to form a thin, protective conversion coating on metals like copper to improve corrosion resistance [73]. |
The management of degradation is a pivotal aspect of biomaterials science. For polymers, control is exerted through molecular design—manipulating the polymer's chemical structure, crystallinity, and composition to program a specific hydrolysis rate. For metals, control is achieved primarily through surface engineering—using alloys, coatings, and inhibitors to protect against electrochemical corrosion. The choice between a polymeric or metallic biomaterial is thus not a matter of superiority, but one of application-specific suitability. Resorbable polymers offer the ultimate advantage of disappearing after fulfilling their temporary function, ideal for sutures, tissue scaffolds, and pediatric implants. Permanent, corrosion-resistant metals provide the necessary long-term mechanical support for load-bearing applications like joint replacements and fracture fixation plates. Understanding the distinct mechanisms of hydrolysis and corrosion, and the methodologies to evaluate them, empowers researchers to make informed decisions and drive innovation in the development of safer, more effective, and longer-lasting medical devices.
The long-term performance of biomedical implants is critically dependent on their ability to withstand cyclic physiological loads over extended periods. Fatigue and fracture resistance therefore become paramount material selection criteria, determining whether an implant will maintain structural integrity throughout its intended service life. This guide provides a systematic comparison of metallic and polymeric biomaterials, focusing on their fatigue and fracture behavior in vivo. We examine fundamental failure mechanisms, present quantitative performance data, and detail standardized experimental methodologies used for assessing mechanical integrity in simulated physiological conditions.
Comparative Fatigue Performance of Biomaterial Classes
The fatigue behavior of biomaterials is characterized through stress-life (S-N) curves, which relate the cyclic stress amplitude to the number of cycles until failure. Metallic and polymeric biomaterials exhibit fundamentally different fatigue responses due to their distinct material structures and damage mechanisms.
Table 1: Comparative Fatigue Properties of Metallic and Polymeric Biomaterials
| Material | Fatigue Limit/Strength (MPa) | Testing Conditions | Key Influencing Factors | Primary Failure Mechanisms |
|---|---|---|---|---|
| Ti-based MMCs [72] | High (Not specified) | Not specified | Microarchitecture, reinforcement distribution | Crack propagation from stress concentrators |
| PEEK [76] | Approaches fatigue limit under lateral/oblique loads | Finite element analysis, oral environment | Loading configuration (stress vs. strain-controlled), frequency, amplitude | Crack initiation from notch-like defects, brittle fracture |
| PEKK [76] | Approaches fatigue limit under lateral/oblique loads | Finite element analysis, oral environment | Loading configuration, notch sensitivity | Crack initiation from stress concentrators |
| CF/PEEK Composites [77] | 81.83 (at 25°C) | Tensile testing, ISO 527 standard | Temperature, fiber-matrix interface bonding | Fiber pull-out, matrix cracking, delamination |
| Metallic Meta-biomaterials [78] | Varies with topology | Cyclic loading in physiological conditions | Topological structures, base material, manufacturing defects | Crack propagation from nodal points, stress concentrators |
Table 2: Fracture Mechanics Parameters for Biomaterials with Defects
| Material System | Critical Defect Size (mm) | Threshold Stress Intensity Factor Range, ΔKth (MPa·√m) | Crack Propagation Behavior | Influence of Manufacturing Defects |
|---|---|---|---|---|
| Metallic Alloys [79] | 0.1-0.5 | 10 (for 2.25Cr1Mo steel) | Small crack regime, closure mechanisms | Defects eliminate crack initiation phase |
| Additively Manufactured Metals [79] | Process-dependent | Material-dependent | Propagation-dominated | Inherent defects act as crack precursors |
| Polymer Matrix Composites [80] | Not specified | Not applicable | Self-heating accelerated degradation | Voids, fiber misalignment |
Experimental Protocols for Fatigue Assessment
Fatigue Testing of Metallic Biomaterials
Standardized fatigue testing of metallic biomaterials involves cyclic loading under physiologically relevant conditions until failure or predetermined runout cycles (typically 10â· cycles). The methodology focuses on characterizing both crack initiation and propagation phases [79].
Specimen Preparation: Metallic specimens are machined according to ASTM E466 standards, with careful attention to surface finish to minimize unintended stress concentrators. For additively manufactured materials, specimens are often built in orientations representing actual implant manufacturing directions [72].
Testing Parameters:
- Loading Profile: Axial loading with stress ratios (R = σmin/σmax) typically between 0.1 and -1.0 to simulate various physiological loading conditions
- Frequency: 5-30 Hz to balance testing duration with minimal hysteretic heating
- Environment: Testing in physiological saline (0.9% NaCl) at 37°C to simulate in vivo conditions
- Data Collection: Continuous monitoring of load cycles, crack length measurements (using potential drop or optical methods), and periodic interruption for replica methods to measure small cracks [79]
Fracture Mechanics Approach: For metals containing inherent defects, a damage tolerance methodology is employed where:
- Initial defect size is characterized through non-destructive evaluation
- Fatigue life is calculated via integration of crack growth laws from initial to critical crack size
- The threshold stress intensity factor range (ΔK_th) is determined for small crack regimes [79]
Fatigue Evaluation of Polymeric Biomaterials
Polymer fatigue testing requires special considerations for viscoelastic effects, self-heating, and frequency sensitivity. The Increasing Amplitude Test (IAT) methodology is particularly valuable for rapid determination of fatigue limits in polymeric systems [80].
Specimen Fabrication: For CFR/PEEK composites, specimens are fabricated using Fused Deposition Modeling (FDM) with standardized process parameters:
- Nozzle temperature: 360-400°C
- Bed temperature: 140°C
- Printing speed: 10 mm/s
- Layer height: 0.2 mm
- Fiber content: 10 wt% carbon fiber in PEEK matrix [77]
IAT Protocol:
- Sequential loading at progressively increasing stress levels
- Constant number of cycles at each stress level (e.g., 5000 cycles)
- Monitoring of self-heating temperature using infrared thermography
- Construction of stress-temperature plot
- Determination of fatigue limit as the point of rapid temperature increase [80]
Self-Heating Monitoring:
- Measurement of surface temperature using calibrated infrared cameras
- Identification of critical self-heating temperature corresponding to global crack formation
- Correlation of thermal signals with stiffness degradation measurements [80]
Failure Analysis:
- Scanning Electron Microscopy (SEM) of fracture surfaces to identify failure mechanisms
- Analysis of fiber-matrix debonding, fiber pull-out, and matrix cracking
- Assessment of interfacial bonding quality between fibers and polymer matrix [77]
Visualization of Fatigue Testing Methodologies
Fatigue Testing Workflow Comparison: This diagram illustrates the standardized experimental approaches for evaluating fatigue behavior in metallic versus polymeric biomaterials, highlighting key methodological differences.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials and Equipment for Biomaterial Fatigue Research
| Item | Function/Application | Specifications/Standards |
|---|---|---|
| Electromechanical Testing Systems [80] | Cyclic loading application | 100 kN capacity, environmental chamber, temperature control |
| Infrared Thermography Camera [80] | Self-heating temperature monitoring | High sensitivity (0.05°C), rapid response, calibration for material surfaces |
| Scanning Electron Microscope [77] | Fracture surface analysis | High vacuum mode, 5-20 kV accelerating voltage, gold/palladium sputter coating |
| Physiological Saline Solution [79] | Simulated biological environment | 0.9% NaCl, pH buffered to 7.4, 37°C temperature maintenance |
| Fused Deposition Modeling Printer [77] | Polymer composite specimen fabrication | High-temperature capability (400°C), enclosed build chamber, precision ±0.05 mm |
| CF/PEEK Filament [77] | Raw material for composite specimens | 1.75 mm diameter, 10 wt% carbon fiber, uniform dispersion, moisture-controlled |
| Potential Drop Crack Measurement [79] | Non-destructive crack length monitoring | Calibrated for material conductivity, resolution < 0.1 mm |
The fatigue and fracture performance of biomaterials is a critical determinant of long-term implant success. Metallic biomaterials demonstrate superior fatigue resistance under high-cycle loading conditions but are susceptible to defect-induced failure, necessitating rigorous fracture mechanics approaches. Polymeric systems offer favorable bone-matched mechanical properties but require careful consideration of viscoelastic effects, self-heating, and environmental degradation. Researchers must select testing methodologies aligned with material-specific failure mechanisms and intended in vivo application environments to accurately predict clinical performance.
The pursuit of advanced biomaterials represents a critical frontier in modern medicine, driven by the need to repair or replace damaged human tissue and organs. Within this field, metallic and polymeric biomaterials are two predominant classes, each with distinct advantages and limitations. The strategic enhancement of these materials through composites, alloying, and novel processing techniques is paramount to overcoming their inherent weaknesses and tailoring their properties for specific biomedical applications. This guide objectively compares the performance of enhanced metallic and polymeric biomaterials, framing the analysis within a broader thesis on their mechanical properties. It synthesizes current research to provide researchers, scientists, and drug development professionals with a clear comparison of material alternatives, supported by experimental data and methodologies.
Material Classifications and Fundamental Properties
Biomaterials are broadly classified based on their composition and the biological response they elicit. The principal categories include metals, polymers, ceramics, and composites, each with unique characteristics. According to the European Society of Biomaterials, a biomaterial is defined as a substance, other than a drug, of synthetic or natural origin that can be used to treat, enhance, or restore body functions [11]. The tissue response to these materials varies: metals are typically close-to-inert, ceramics can be inert, active, or resorbable, and polymers may be inert or resorbable [4].
- Metallic Biomaterials: These are renowned for their excellent mechanical properties, including high strength, ductility, fatigue resistance, and load-bearing capacity, making them indispensable for orthopedic and dental implants [11] [4]. Common examples include 316L stainless steel, cobalt-chromium alloys (Co-Cr), and titanium and its alloys (e.g., Ti6Al4V) [4]. A key challenge is their high elastic modulus, which can lead to a "stress shielding" effect, causing bone resorption and implant loosening [20].
- Polymeric Biomaterials: These materials are characterized by their versatility, biocompatibility, and often biodegradability [11] [4]. They range from synthetic polymers like ultra-high molecular weight polyethylene (UHMWPE), polyurethane (PU), and polylactic acid (PLA) to natural polymers such as chitosan [4]. Their mechanical properties are generally inferior to those of metals, featuring lower strength and rigidity, and are more susceptible to time-dependent deformation and environmental factors [81].
- Composite Biomaterials: Composites are engineered by combining two or more distinct materials to achieve a synergistic effect that overcomes the limitations of single-component systems [4]. A prominent research area involves reinforcing polymeric matrices with natural fibers, such as pine needles or recycled paper, to create more sustainable and eco-friendly composite materials [82].
Table 1: Fundamental Properties and Typical Applications of Biomaterial Classes
| Material Class | Key Characteristics | Common Examples | Typical Applications |
|---|---|---|---|
| Metallic | High strength, ductility, good fatigue resistance, prone to corrosion | 316L Stainless Steel, Co-Cr Alloys, Ti6Al4V | Orthopedic implants (hip, knee joints), dental implants, bone plates [11] [4] |
| Polymeric | Biocompatible, often biodegradable, tunable properties, lower mechanical strength | Polyurethane (PU), Polylactic acid (PLA), Polyethylene (PE) | Drug delivery systems, tissue engineering scaffolds, sutures, cardiovascular stents [11] [4] |
| Ceramic | High compressive strength, inert or bioactive, brittle | Alumina, Zirconia, Hydroxyapatite | Dental crowns, bone tissue engineering scaffolds, joint replacements [11] [4] |
| Composite | Combines properties of constituents, designable performance | Polymer matrix with natural fiber reinforcement, Metal-polymer blends | Lightweight implants, eco-friendly materials, enhanced structural components [82] [4] |
Performance Comparison of Enhanced Materials
Enhanced Metallic Biomaterials via Alloying
Alloying is a fundamental strategy for improving the performance of metallic biomaterials. Recent research focuses on developing novel alloys with non-toxic elements to enhance mechanical compatibility and corrosion resistance.
A 2025 study designed and evaluated a series of novel Ti-xNb-5Ta (x = 5, 7, 10, 13 wt.%) alloys for dental implant applications [20]. The ingots were prepared via arc-melting under an argon atmosphere and were remelted five times to ensure compositional homogeneity. Their microstructure, mechanical properties, and corrosion resistance were comprehensively characterized.
Table 2: Mechanical and Electrochemical Properties of Ti-xNb-5Ta Alloys [20]
| Alloy Composition | Ultimate Tensile Strength (MPa) | Elongation at Break (%) | Elastic Modulus (GPa) | Corrosion Resistance Trend |
|---|---|---|---|---|
| Ti-5Nb-5Ta | Data specific to this alloy was not isolated in the provided text. | |||
| Ti-7Nb-5Ta | Data specific to this alloy was not isolated in the provided text. | |||
| Ti-10Nb-5Ta | Surpassed TA4G surgical implant standard | Greater elongation | Lower elastic modulus | Improves with increasing Nb content |
| Ti-13Nb-5Ta | Surpassed TA4G surgical implant standard | Greater elongation | Lower elastic modulus | Improves with increasing Nb content |
The key findings from this study demonstrate that alloying titanium with Nb and Ta successfully creates materials with a more desirable combination of properties than conventional CP-Ti. The Ti-10Nb-5Ta and Ti-13Nb-5Ta alloys surpassed the strength requirements of a common surgical implant standard (TA4G) while offering a lower elastic modulus and greater elongation [20]. This lower modulus is crucial for reducing stress shielding. Furthermore, electrochemical experiments confirmed that corrosion resistance improved with increasing Nb content, and in vitro biological tests showed that these alloys enhanced the early osteogenic differentiation of human bone marrow stromal cells (hBMSCs) [20].
Enhanced Polymeric and Composite Biomaterials
The enhancement of polymeric biomaterials often involves creating composites with natural reinforcements or developing novel polymer blends and nanocomposites.
A 2024 study investigated the mechanical behavior of PLA/OLA/MgO electrospun fibers [81]. The researchers used the Box-Wilson surface response methodology to optimize the amounts of magnesium oxide nanoparticles (MgO) and an oligomer of lactic acid (OLA) used as a plasticizer. This approach allowed for the design of tailor-made electrospun nanocomposites with specific mechanical requirements, demonstrating how additives can finely tune material properties [81].
Another research effort focused on creating environmentally friendly composites using pine needles and recovered paper as reinforcement in a matrix of natural dammar resin blended with synthetic resins [82]. The composites were manufactured using the lay-up hand technique, and samples were tested for tensile strength, compression, bending, and hardness. The results indicated that as the percentage of dammar resin in the matrix increased, the strength and rigidity of the material decreased, while its elasticity and ductility increased [82]. This trade-off highlights the ability to tailor the mechanical profile of a composite by adjusting the matrix composition.
Table 3: Performance of Enhanced Polymeric/Composite Biomaterials
| Material System | Enhancement Strategy | Key Outcome | Reference |
|---|---|---|---|
| PLA/OLA/MgO Fibers | Electrospinning with nanoparticles (MgO) and a plasticizer (OLA) | Tailor-made mechanical properties achievable via response surface methodology | [81] |
| Dammar Resin Composite | Matrix blending (natural dammar with synthetic resins); reinforcement with pine needles/paper | Higher dammar content increases elasticity/ductility but reduces strength/rigidity | [82] |
| VESTAKEEP Fusion PEEK | Incorporation of biphasic calcium phosphate additives into a PEEK filament for 3D printing | Creates an osteoconductive material that enhances bone cell adhesion and healing | [83] |
Advanced Manufacturing and Experimental Protocols
Novel Processing Techniques: Additive Manufacturing
Additive manufacturing (AM) has revolutionized the fabrication of biomaterials by enabling the production of complex, patient-specific geometries that are difficult or impossible to achieve with traditional methods.
- For Metallic Biomaterials: Techniques like Selective Laser Melting (SLM) and Electron Beam Melting (EBM) are commonly used. SLM has been applied to alloys of titanium, zinc, magnesium, and cobalt, while EBM is particularly noted for producing titanium implants with fine structures and minimal contaminants [4]. These techniques allow for the creation of porous structures that can mimic bone and reduce the effective elastic modulus of the implant.
- For Polymeric Biomaterials: Fused Deposition Modeling (FDM) is widely employed. For instance, a study on shape memory PLA parts found that the extruder temperature and nozzle diameter were the most significant FDM parameters for achieving optimal mechanical properties [81]. Furthermore, companies like Evonik have developed specialized osteoconductive PEEK filaments (VESTAKEEP Fusion) compatible with extrusion-based 3D printing for creating customized implants [83].
Detailed Experimental Protocol: Metallic Alloy Assessment
The following workflow, derived from the Ti-Nb-Ta alloy study [20], provides a template for the comprehensive evaluation of a novel metallic biomaterial.
Diagram 1: Metal Biomaterial Evaluation Workflow
1. Alloy Design and Ingot Preparation:
- Theory: Alloys are designed using the d-electron theory and molybdenum equivalent (Moeq) to predict phase stability and properties. For biomedical use, the bond order (Bo) typically targets 2.75-2.85 and the metal d-orbital energy level (Md) 2.35-2.45 eV [20].
- Fabrication: Ingots are prepared via arc-melting in an inert argon atmosphere using high-purity elemental components. Each ingot is remelted multiple times (e.g., five times) to ensure chemical homogeneity [20].
2. Microstructural Characterization:
- Sample Preparation: Samples are mirror-polished using a series of abrasive papers and final polished with alumina powder. Kroll's reagent may be applied as an etchant to reveal microstructural features [20].
- Analysis: Optical Microscopy (OM) and X-ray Diffraction (XRD) are used to examine the microstructure, identify constituent phases (e.g., α, β, α"), and assess homogeneity [20].
3. Mechanical Testing:
- Tensile Properties: Tensile strength, elongation, and elastic modulus are determined using an electronic universal testing machine. The elastic modulus is calculated using the tensile method [20].
- Hardness: Vickers microhardness is measured with a hardness tester at a specified load (e.g., 1000 gf) and dwell time (e.g., 10 s) [20].
4. Electrochemical Experiment:
- Setup: A standard three-electrode electrochemical cell system is used with a saturated calomel reference electrode, a platinum counter electrode, and the alloy as the working electrode.
- Testing: Tests are conducted in simulated body fluid (SBF) at room temperature. Key tests include:
- Open Circuit Potential (OCP): Measures the steady-state potential.
- Potentiodynamic Polarization: Generates a polarization curve to assess corrosion rate and behavior.
- Electrochemical Impedance Spectroscopy (EIS): Evaluates the characteristics of the passive film on the alloy surface [20].
5. In Vitro Biocompatibility:
- Cell Viability: Assessed using assays like CCK-8 to measure cell proliferation and health.
- Osteogenic Potential: Alkaline Phosphatase (ALP) activity is measured as an early marker of osteogenic differentiation. Reverse Transcription-Polymerase Chain Reaction (RT-PCR) is used to analyze the expression of osteogenic genes [20].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for Biomaterials Research
| Item | Function/Application | Example Context |
|---|---|---|
| High-Purity Metal Elements (Ti, Nb, Ta) | Raw materials for synthesizing novel alloy compositions with controlled purity. | Fabrication of Ti-xNb-5Ta alloy ingots via arc-melting [20]. |
| Simulated Body Fluid (SBF) | An in vitro solution that mimics the ion concentration of human blood plasma for corrosion and bioactivity testing. | Electrochemical corrosion testing of metallic implants [20]. |
| Dammar Resin | A natural resin used as a matrix component in eco-friendly composite materials. | Creating biodegradable composites with pine needle reinforcement [82]. |
| Magnesium Oxide (MgO) Nanoparticles | A nanoscale additive used to modify the thermal and mechanical responses of polymers. | As an additive in PLA/OLA electrospun fibers to tailor mechanical properties [81]. |
| Kroll's Reagent | A chemical etchant used to reveal the microstructure of titanium and its alloys for metallographic observation. | Microstructural characterization of Ti-Nb-Ta alloys [20]. |
| CCK-8 Assay Kit | A colorimetric kit for quantifying cell viability and proliferation in cytocompatibility studies. | In vitro biocompatibility testing of new alloy surfaces [20]. |
The strategic enhancement of metallic and polymeric biomaterials is a dynamic and multifaceted endeavor critical to advancing biomedical engineering. For metallic biomaterials, alloying with non-toxic elements like Nb and Ta proves highly effective in optimizing the crucial balance between strength, a reduced elastic modulus, and corrosion resistance, as demonstrated by the Ti-Nb-Ta system. For polymeric biomaterials, strategies such as creating nanocomposites, using natural reinforcements, and developing smart polymers allow for extensive tuning of their mechanical and biological properties. Furthermore, additive manufacturing emerges as a transformative processing technique across both material classes, enabling unparalleled design freedom and functional integration. The continuous refinement of these strategies—compositing, alloying, and novel processing—ensures that the next generation of biomaterials will offer improved performance, greater personalization, and enhanced clinical outcomes for patients.
The Role of Explainable AI and Data-Driven Frameworks in Material Optimization
The development of advanced biomaterials for orthopedic and medical applications has traditionally relied on iterative experimental processes, presenting a significant bottleneck in creating implants with ideal mechanical properties, biodegradability, and biocompatibility. The integration of Explainable Artificial Intelligence (XAI) and data-driven frameworks is fundamentally transforming this paradigm, enabling the precise optimization of both metallic and polymeric biomaterials [84] [85]. These approaches leverage machine learning (ML), active learning, and high-throughput experimentation to navigate complex multi-variable design spaces, accelerating the discovery of materials tailored for specific clinical needs [86] [87]. Within the context of biomaterials research, a critical comparison between metallic and polymeric systems reveals distinct mechanical advantages and challenges, which these advanced computational frameworks are uniquely positioned to address.
This guide objectively compares the performance of newly developed biomaterials—from innovative magnesium alloys to advanced polymers—by synthesizing experimental data generated through these AI-driven methodologies. It details the specific experimental protocols, reagent solutions, and workflows that underpin this new era of intelligent materials optimization.
Material Performance Comparison: Metallic vs. Polymeric Biomaterials
The following tables summarize key properties of recently developed metallic and polymeric biomaterials, highlighting their performance for orthopedic and biomedical applications.
Table 1: Mechanical Properties and Degradation Behavior of Metallic Biomaterials
| Material System | Yield Strength (MPa) | Ultimate Tensile Strength (MPa) | Elongation (%) | Corrosion Rate (mm/year) | Key Findings |
|---|---|---|---|---|---|
| Extruded Mg-0.3Sr-0.4Mn (SM04) Alloy [28] | 205 | 242 | Data Not Provided | 0.39 | 28% higher yield strength and 54% lower corrosion rate than binary Mg-0.3Sr alloy. |
| Rolled Mg-2Sr Alloy [28] | ~150 | 213 | ~3 | 0.37 | Strength and degradation rate fall short of clinical benchmarks for load-bearing applications. |
| Pure Magnesium [28] | Insufficient | Insufficient | Data Not Provided | High (Rapid) | Rapid in vivo degradation leads to premature mechanical failure. |
Table 2: Properties and Functions of Polymeric Biomaterials
| Polymer Name | Polymer Type | Key Properties | Specific Medical Applications |
|---|---|---|---|
| Polylactic Acid (PLA) [25] | Synthetic | Biodegradable, Biocompatible | Bone screws, sutures, vascular stents, drug delivery. |
| Polyurethanes (PU) [25] | Synthetic | Hemocompatible, Tough, Versatile | Catheters, wound dressings, artificial hearts, adhesives. |
| Chitosan [25] | Natural | Biocompatible, Biodegradable, Antimicrobial | Wound healing, tissue engineering, drug delivery. |
| Hyaluronic Acid (HA) [25] | Natural | Biocompatible, Mimics ECM | Wound healing, cartilage scaffolds, drug carriers. |
| Poly(ethylene glycol) (PEG) [25] | Synthetic | Non-immunogenic, Hydrophilic | Hydrogels, drug conjugates, device coatings. |
Table 3: Clinical Benchmark Comparison for Orthopedic Implants
| Performance Metric | Clinical Target [28] | Mg-Sr-Mn (SM04) Alloy [28] | Representative Polymer (PLA) [25] |
|---|---|---|---|
| Yield Strength | >200 MPa | 205 MPa | Varies by form/processing; used in sutures and screws. |
| Degradation Rate | <0.5 mm/year | 0.39 mm/year | Controllable degradation profile, enzyme-mediated for natural polymers. |
| Elastic Modulus | ~20 GPa (Natural Bone) | 41-45 GPa | Typically 1-3 GPa, significantly lower than metals, reducing stress shielding. |
Experimental Protocols for AI-Driven Material Development
Protocol for Metallic Alloy Development and Testing
The development of the Mg-Sr-Mn alloy series followed a structured, data-driven workflow [28]:
- Alloy Design and Synthesis: A series of Mg-0.3Sr-xMn (where x = 0, 0.4, 1.2, and 2.0 wt.%) alloys were prepared. A fixed Sr content of 0.3 wt.% was used to leverage its grain-refining and osteogenic properties while avoiding detrimental effects on corrosion resistance. The alloys were processed using extrusion to obtain a refined microstructure.
- Microstructural and Phase Analysis: The microstructures of the extruded samples were characterized using Scanning Electron Microscopy (SEM) and Transmission Electron Microscopy (TEM). Energy-Dispersive X-ray Spectroscopy (EDS) was used for elemental mapping, and X-ray Diffraction (XRD) was employed to identify phases (α-Mg, Mgâ‚₇Srâ‚‚, and α-Mn).
- Mechanical Testing: Tensile tests were conducted to determine yield strength (YS) and ultimate tensile strength (UTS).
- In Vitro Degradation Behavior: The corrosion rate was assessed by immersing samples in a simulated physiological environment and measuring the hydrogen evolution or mass loss.
- Biocompatibility Assessment: Cell viability was evaluated using a standard MTT assay with osteoblast cell lines (e.g., MC3T3-E1). Alkaline phosphatase (ALP) activity was measured as a marker for osteogenic differentiation.
Protocol for AI-Optimized Material Discovery
The CRESt (Copilot for Real-world Experimental Scientists) platform exemplifies a comprehensive AI-driven experimental protocol [86]:
- Multimodal Data Integration: The system ingests diverse data sources, including scientific literature, chemical compositions, and microstructural images, to create a knowledge base.
- Knowledge-Embedded Active Learning: An AI model performs principal component analysis (PCA) on a knowledge-embedding space to define a reduced search space. Bayesian optimization (BO) is then used within this space to propose the most promising next experiment.
- High-Throughput Robotic Synthesis: Proposed material recipes (e.g., up to 20 precursor molecules) are autonomously synthesized using a liquid-handling robot and a carbothermal shock system.
- Automated Characterization and Testing: The synthesized materials are automatically characterized using techniques like electron microscopy and tested for target properties (e.g., electrochemical performance in a fuel cell).
- Iterative Feedback and Computer Vision: Results are fed back into the active learning model. Cameras and visual language models monitor experiments in real-time to detect issues (e.g., sample misplacement) and suggest corrections, improving reproducibility.
Visualization of AI-Driven Workflows
XAI-Driven Biomaterial Optimization Workflow
Material Selection Logic for Implants
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagent Solutions for Biomaterial Development and Testing
| Reagent/Material | Function in Research | Example Application |
|---|---|---|
| Strontium (Sr) Metal [28] | Alloying element to refine grains, improve strength/corrosion resistance, and promote osteogenesis. | Mg-Sr-Mn alloy development for bone implants. |
| Manganese (Mn) Metal [28] | Alloying element to form nanoscale precipitates, enhance strength, and improve corrosion resistance. | Optimization of Mg-Sr-Mn ternary alloys. |
| Polylactic Acid (PLA) [25] | A synthetic, biodegradable polymer for creating scaffolds and temporary implants. | Bone screws, sutures, drug delivery systems. |
| Chitosan [25] | A natural polymer used for its biocompatibility, biodegradability, and inherent antimicrobial properties. | Wound dressings, tissue engineering scaffolds. |
| Cell Culture Media (e.g., for MC3T3-E1) [28] | To support the growth of osteoblast cells for in vitro biocompatibility testing. | Assessing cell viability and ALP activity on alloy surfaces. |
| Simulated Body Fluid (SBF) [28] | A solution mimicking human blood plasma for in vitro degradation and bioactivity studies. | Measuring corrosion rate of biodegradable metals. |
Head-to-Head: A Data-Driven Validation of Mechanical and Clinical Performance
The selection of biomaterials for medical implants and devices is critically dependent on their mechanical properties, which must closely match the biological environment of the target tissue to ensure long-term functionality and biocompatibility. Among the most crucial mechanical properties are tensile strength, elastic modulus, and toughness, which collectively determine a material's ability to withstand structural loads, resist deformation, and absorb energy before failure [11]. The ongoing research in biomaterials science is largely focused on addressing the fundamental trade-offs between these properties, particularly in the context of metallic versus polymeric biomaterials [88] [89].
Metallic biomaterials have traditionally dominated load-bearing applications such as joint replacements and bone fixation devices due to their superior strength and fatigue resistance. However, their high elastic modulus often leads to stress-shielding phenomena, where the implant bears most of the load, leading to bone resorption and eventual implant loosening [90]. In contrast, polymeric biomaterials offer closer modulus matching to biological tissues and greater design flexibility but often lack the required strength for demanding load-bearing applications [23]. This comprehensive review systematically compares the tensile strength, elastic modulus, and toughness of metallic and polymeric biomaterials, providing researchers with objective experimental data and methodologies to guide material selection for specific biomedical applications.
Fundamental Properties and Measurement Methodologies
Defining Key Mechanical Properties
Tensile Strength: This property represents the maximum stress a material can withstand while being stretched or pulled before necking or failing. It is a critical parameter for implants that experience tensile loads, such as ligament anchors or bone plates. Tensile strength is typically reported in megapascals (MPa) or gigapascals (GPa) [11] [90].
Elastic Modulus (Young's Modulus): This is a measure of a material's stiffness, representing the ratio of stress to strain in the elastic deformation region. For biomaterials, matching the elastic modulus of the surrounding tissue is essential to prevent stress shielding in bone implants or undesirable mechanical mismatch in soft tissue applications. It is also measured in GPa or MPa [90] [89].
Toughness: Toughness quantifies a material's ability to absorb energy and plastically deform without fracturing. It is typically measured as the area under the stress-strain curve and is reported in megajoules per cubic meter (MJ/m³). High toughness is crucial for implants subject to impact loads or cyclic loading [88] [89].
Standardized Testing Protocols
The reliable comparison of mechanical properties across different studies requires adherence to standardized testing methodologies. The following experimental approaches are most commonly employed in biomaterials characterization:
Uniaxial Tensile Testing: This is the primary method for determining tensile strength and elastic modulus. Specimens with standardized dimensions (typically dog-bone shaped) are subjected to controlled tension until failure while measuring the applied load and elongation. The elastic modulus is calculated from the slope of the initial linear portion of the stress-strain curve [89] [91].
Three-Point Bending Tests: Frequently used for evaluating dental materials and bone scaffolds, this method places a specimen on two supports and applies a load at the center. The test measures flexural strength and modulus, which are particularly relevant for applications like fixed partial dentures (FPDs) and spinal implants [91].
Cyclic Fatigue Testing: To simulate in vivo loading conditions, materials undergo repeated loading-unloading cycles to determine fatigue strength and lifetime. This is especially important for cardiovascular and orthopedic implants that experience cyclic stresses [89].
The experimental workflow for comprehensive mechanical characterization typically follows a systematic process, as illustrated below:
Comparative Analysis of Metallic Biomaterials
Conventional Metallic Biomaterials
Metallic biomaterials represent the most widely used class of materials for load-bearing implants due to their exceptional combination of strength, fracture toughness, and durability. The global biomaterials market, valued at USD 35.5 billion in 2020, is projected to reach USD 47.5 billion by 2025, with metallic biomaterials maintaining a significant share [11]. Traditional metallic implants have a service life of approximately twenty years, making them the preferred choice for permanent implants [11]. The most common metallic biomaterials include stainless steel, cobalt-chromium alloys, and titanium and its alloys, each offering distinct mechanical advantages for specific clinical applications.
Table 1: Mechanical Properties of Conventional Metallic Biomaterials
| Material | Tensile Strength (MPa) | Elastic Modulus (GPa) | Toughness Characteristics | Primary Applications |
|---|---|---|---|---|
| Stainless Steel (316L) | 540-750 | 190-200 | High fracture toughness | Temporary bone fixtures, fracture plates, screws |
| Cobalt-Chromium Alloys | 900-1540 | 210-230 | Excellent wear resistance | Dental implants, joint replacements, orthopedic screws |
| Titanium (CP) | 240-550 | 100-110 | Good fatigue resistance | Dental implants, cranial plates, maxillofacial surgery |
| Ti-6Al-4V | 860-965 | 110-115 | High strength-to-weight ratio | Load-bearing orthopedic and dental implants |
| Magnesium Alloys | 250-350 | 41-45 | Biodegradable, moderate toughness | Biodegradable bone screws, cardiovascular stents |
Advanced and Novel Metallic Alloys
Recent developments in metallic biomaterials have focused on addressing the significant mismatch between the modulus of conventional metals (100-230 GPa) and human cortical bone (7-30 GPa) [90] [89]. This modulus mismatch leads to stress shielding, where the implant bears most of the mechanical load, resulting in bone resorption and potential implant failure. Magnesium alloys have emerged as promising biodegradable materials with an elastic modulus (41-45 GPa) closer to bone, but their relatively low tensile strength (250-350 MPa) and rapid degradation kinetics have limited their application in load-bearing scenarios [92].
A groundbreaking development is the Ti-50.8 at.% Ni dual-seed strain glass (DS-STG) alloy, which demonstrates an unprecedented combination of ultrahigh yield strength (σy ≈ 1.8 GPa) and polymer-like low Young's modulus (E ≈ 10.5 GPa) [89]. This alloy overcomes the traditional strength-flexibility trade-off that has long plagued materials science, achieving a flexibility figure of merit (σy/E ≈ 0.17) that significantly exceeds existing structural materials. The DS-STG alloy also exhibits super-large rubber-like elastic strain of approximately 8% and maintains these properties across a wide temperature range (-80°C to +80°C), making it suitable for aerospace medical applications and extreme environments [89].
Comparative Analysis of Polymeric Biomaterials
Conventional Medical-Grade Polymers
Polymeric biomaterials offer distinct advantages in biomedical applications, including lower elastic moduli closer to biological tissues, ease of processing, and potential for biodegradation. The primary limitation of most medical polymers has been their insufficient mechanical strength for load-bearing applications, leading to the development of various reinforcement strategies [23].
Table 2: Mechanical Properties of Polymeric Biomaterials
| Material | Tensile Strength (MPa) | Elastic Modulus (GPa) | Toughness Characteristics | Primary Applications |
|---|---|---|---|---|
| PEEK | 90-100 | 3-4 | High fracture strength, fatigue resistance | Dental frameworks, spinal implants, trauma fixation |
| PLA | 50-70 | 3.5-4 | Brittle, low impact resistance | Tissue engineering scaffolds, sutures, drug delivery |
| PMMA | 55-75 | 2-3 | Low toughness, brittle | Bone cements, dental restorations, cranial implants |
| UHMWPE | 39-48 | 0.5-1.8 | Excellent impact strength | Bearing surfaces in joint replacements |
| PVA/HCPA Composite | ~104 (48% increase) | Not specified | 370% toughness improvement | Self-healing medical devices, flexible implants |
Enhanced and Composite Polymeric Systems
Significant research efforts have focused on improving the mechanical performance of polymeric biomaterials through composite strategies and structural modifications. Polyetheretherketone (PEEK) has gained prominence as a high-performance polymer for load-bearing applications, with studies demonstrating its superiority over zirconia in fixed partial dentures (FPDs) under experimental loading conditions [91]. Zirconia-ceramic FDPs exhibited lower values of vertical displacement compared to PEEK-based samples, indicating PEEK's better ability to withstand functional loads without catastrophic failure [91].
Polylactic acid (PLA), while biocompatible and biodegradable, suffers from inherent brittleness and low impact resistance, with tensile strength ranging between 50-70 MPa and elastic modulus of 3.5-4 GPa [23]. These properties fall short of the requirements for high-stress or weight-bearing environments without reinforcement. To address these limitations, researchers have developed metal-reinforced PLA biocomposites incorporating titanium, stainless steel, magnesium, or silver particles. These composites demonstrate significantly enhanced tensile strength and durability while maintaining biocompatibility [23].
A notable advancement in polymer science involves the use of multiple hydrogen-bonded networks to simultaneously enhance strength and toughness. The incorporation of small molecules like HCPA (N,N'-Bis(2,6-diisopropylphenyl)-1,4,5,8-naphthalenetetracarboxydiimide) into polyvinyl alcohol (PVA) matrices has demonstrated remarkable improvements: 48% increase in tensile strength, 173% increase in strain at break, and 370% improvement in toughness [88]. This approach overcomes the classic dilemma of mutually exclusive strength and toughness by creating dynamic cross-links that can dissociate and reform under mechanical strain, effectively dissipating energy and preventing crack propagation [88].
Experimental Data and Case Studies
Direct Comparative Studies
A compelling in vitro study directly compared the biomechanical behavior of zirconia-ceramic and PEEK-composite fixed partial dentures (FPDs) under experimental loading conditions using a prototypal simulator [91]. The research employed a three-point bending mechanical test on FPDs screwed into a biomimetic mandible model, with load to fracture evaluated while generating point-by-point graphics of speed/load and time/deformation relationships.
The experimental protocol involved:
- Sample Preparation: Ten titanium fixtures were screwed into resin mandibular section simulators, divided into two groups: Group A (zirconia-ceramic FPDs) and Group B (PEEK-composite FPDs).
- Testing Configuration: A three-point bending test was applied to simulate functional loading conditions.
- Analysis Methods: Fracture resistance was measured, and samples were further analyzed by micro-computed tomography (micro-CT) to assess structural integrity post-loading.
Results demonstrated that zirconia-ceramic FDPs showed lower values of vertical displacement compared to PEEK-based samples, indicating PEEK's superior ability to undergo deformation without failure—a key characteristic for withstanding the cyclic loading experienced in dental applications [91]. Micro-CT analysis further confirmed these findings, showing more favorable fracture patterns in the PEEK-composite materials.
Advanced Material Performance
The exceptional properties of the Ti-50.8 at.% Ni DS-STG alloy were characterized through a comprehensive experimental protocol [89]:
- Thermomechanical Processing: The alloy underwent a three-step thermomechanical treatment creating a unique "dual-seed strain glass" microstructure.
- Mechanical Testing: Uniaxial tensile tests revealed the alloy's J-shaped stress-strain curve with ultralow initial modulus (E ≈ 10.5 GPa) and super-large recoverable strain (εre ≈ 8%).
- Temperature Stability: Testing across -80°C to +80°C confirmed property retention over an aviation-relevant temperature range.
- Fatigue Resistance: The alloy demonstrated excellent high-strain fatigue resistance, with fatigue-free behavior (>5×10ⶠcycles) at 1.6% strain.
The microstructure of this innovative alloy, composed of a strain glass matrix embedded with aligned R and B19′ martensite "seeds," enables a nucleation-free reversible transition during loading and unloading, responsible for its unique mechanical behavior [89].
The mechanism behind hydrogen-bonding enhancement in polymers is illustrated below, showing how dynamic cross-links create enhanced mechanical properties:
The Scientist's Toolkit: Essential Research Materials and Methods
Table 3: Key Research Reagents and Equipment for Biomaterials Mechanical Testing
| Item | Function/Application | Experimental Context |
|---|---|---|
| HCPA Cross-linker | Small molecule forming multiple H-bonds with polymer chains | Enhancing strength and toughness of PVA-based biomaterials [88] |
| Bluzirkon Simex Zirconia | Yttria-stabilized tetragonal zirconia polycrystal (3Y-TZP) | Dental framework fabrication for biomechanical testing [91] |
| VICTREX PEEK | High-performance polymer for medical applications | Comparative studies with ceramics in load-bearing dental applications [91] |
| Ti-50.8 at.% Ni Alloy | Shape memory alloy with unique strain glass behavior | Developing strong yet flexible metallic biomaterials [89] |
| Three-Point Bending Fixture | Simulates functional loading on dental/orthopedic constructs | Evaluating fracture resistance of FPDs in biomimetic environments [91] |
| Micro-CT Scanner | Non-destructive 3D structural analysis | Examining internal damage and fracture patterns post-loading [91] |
| Dynamic Mechanical Analyzer | Measures viscoelastic properties under cyclic loading | Characterizing self-healing behavior in hydrogen-bonded networks [88] |
The direct comparison of tensile strength, elastic modulus, and toughness between metallic and polymeric biomaterials reveals a complex landscape where material selection must be carefully matched to specific application requirements. Metallic biomaterials generally offer superior tensile strength and fracture toughness, making them indispensable for high-load applications such as joint replacements and dental implants. However, their high elastic modulus creates challenges with stress shielding, driving research toward novel alloys like the Ti-Ni DS-STG system that combines ultrahigh strength (1.8 GPa) with polymer-like modulus (10.5 GPa) [89].
Polymeric biomaterials provide better modulus matching to biological tissues and greater design flexibility but typically require reinforcement strategies to achieve sufficient strength for load-bearing applications. Advanced approaches using multiple hydrogen-bonded networks [88] and metal-particle reinforcements [23] have demonstrated remarkable improvements in simultaneously enhancing strength, modulus, and toughness—properties traditionally governed by mutually exclusive mechanisms.
The future of biomaterials development lies in creating multifunctional systems that provide not only appropriate mechanical properties but also bioactive surfaces, controlled degradation profiles, and immune-modulatory capabilities. As additive manufacturing technologies continue to advance, the integration of computational design with hierarchical material architectures will further enable the development of patient-specific implants with optimized mechanical performance for enhanced clinical outcomes.
Radial strength and recoil are fundamental mechanical properties determining the clinical success of coronary stents. Radial strength refers to a stent's ability to resist compression and maintain vessel patency after deployment, while recoil describes the percentage reduction in stent diameter immediately following expansion. These properties are critically influenced by the choice of biomaterial—whether metallic or polymeric—and the specific stent design.
The permanent implantation of metallic stents, while effective initially, presents long-term limitations including vessel caging, impaired vasomotion, and risk of late adverse events [21]. These concerns have driven the development of bioresorbable polymeric scaffolds that provide temporary support before degrading. This analysis benchmarks the radial strength and recoil properties of metallic versus polymeric stent platforms, providing researchers with comparative experimental data and methodologies essential for advancing cardiovascular biomaterials research.
Comparative Analysis of Metallic and Polymeric Stents
Fundamental Material Properties
The intrinsic mechanical properties of biomaterials directly determine stent performance characteristics. Metallic alloys used in stents, such as Cobalt-Chromium (Co-Cr) and Stainless Steel (SS 316L), possess significantly higher tensile modulus (193-210 GPa) and strength (235-668 MPa) compared to polymeric alternatives [21]. This substantial mechanical advantage enables thinner strut designs while maintaining radial strength.
Biodegradable polymers, particularly poly-L-lactic acid (PLLA), exhibit a tensile modulus of only 2-4 GPa and strength of 60-70 MPa [21]. The inferior mechanical properties of PLLA necessitate substantially thicker struts (often >150 μm) to achieve radial strength comparable to metallic stents, which can impact deliverability and cause flow disturbances. Magnesium alloys represent an intermediate option with a modulus of 40-50 GPa and complete biodegradation within 3-12 months [21].
Table 1: Mechanical Properties of Stent Biomaterials
| Material | Tensile Modulus (GPa) | Tensile Strength (MPa) | Elongation at Break (%) | Degradation Time |
|---|---|---|---|---|
| SS 316L | 193 | 668 | 40 | Biostable |
| Co-Cr | 210 | 235 | 40 | Biostable |
| WE43 (Mg alloy) | 40-50 | 220-330 | 2-20 | 3-12 months |
| PLLA | 2-4 | 60-70 | 2-6 | >24 months |
| PDLLA | 1-3.5 | 40 | 1-2 | 3-4 months |
| PLGA (82/12) | 3.3-3.5 | 65 | 2-6 | 12-18 months |
Radial Strength and Recoil Performance
Metallic Stents
A comprehensive 1999 comparative study of 17 coronary stents revealed appreciable variation in resistance to local compression [93]. The tested stents demonstrated minimal purely elastic behavior, with most exhibiting plastic deformation above very small force thresholds (<0.4 Newtons). The study distinguished between stent families based on the presence or absence of this elastic region.
In a specialized test where stents were deployed in 3.0-mm elastic tubes with controlled pressure gradients, significant deformation differences emerged after 0.3 × 10ⵠPa [93]. The Crossflex stent demonstrated the highest radial resistance, while the BeStent BEL-15 was the least resistant, highlighting substantial design-dependent performance variations despite similar material composition.
Polymeric Bioresorbable Stents
Bioresorbable vascular scaffolds (BRS) face inherent challenges in balancing radial strength with biodegradation profiles. First-generation polymeric BRS required strut profiles 240% thicker than metallic DES to compensate for PLLA's lower tensile modulus [21]. Newer generation technologies address this through hybrid designs and improved materials:
- Hybrid metal-polymer scaffolds combine metallic strength with resorbable benefits [94]
- Thin-strut BRS with struts <70 μm maintain adequate radial strength while minimizing flow disturbances [94]
- Accelerated resorption profiles complete degradation within 12-18 months versus earlier 2-3 year timelines [94]
Bench testing has revealed that despite material property differences, optimized PLLA scaffolds like the ABSORB BVS can achieve comparable radial strength and recoil to metallic DES when measured using standard methods [21].
Table 2: Clinical Performance Metrics of Stent Technologies
| Stent Technology | Radial Strength | Acute Recoil | Chronic Recoil Incidence | TLR Association |
|---|---|---|---|---|
| Metallic DES (2nd gen+) | High | Low (<5%) | 7.8% (non-TLR lesions) | Moderate |
| Polymer BRS (1st gen) | Moderate | Moderate | N/A | Higher |
| Polymer BRS (2nd gen+) | Moderate-High | Low-Moderate | 21.5% (TLR lesions) | Significant |
| Mg Alloy BRS | Moderate | Low | N/A | Evolving evidence |
Chronic Stent Recoil: Clinical Impact and Predictive Factors
Chronic stent recoil represents a significant clinical concern, particularly for bioresorbable platforms. A 2025 serial optical coherence tomography (OCT) study found chronic recoil occurring in 21.5% of lesions undergoing target lesion revascularization (TLR), compared to only 7.8% in non-TLR lesions [95]. Multivariable analysis identified several factors significantly associated with chronic recoil:
- Larger maximum calcium arc (per 90°, OR: 1.64; 95% CI: 1.17-2.29)
- Greater baseline stent expansion (per 10%, OR: 1.41; 95% CI: 1.19-1.83)
- Greater stent eccentricity index (per 0.1, OR: 0.61; 95% CI: 0.39-0.92) [95]
The study concluded that greater chronic stent recoil (per 1 mm², OR: 3.86; 95% CI: 1.57-9.48) was independently associated with TLR, along with greater in-stent tissue growth and baseline smaller minimum stent area [95].
Experimental Methodologies for Stent Benchmarking
Radial Force Compression Testing
The deformation-controlled dynamometer method provides precise measurement of local compression resistance [93]. This approach involves:
- Apparatus: Precision dynamometer with 1-micron precision
- Method: Compression applied along a longitudinal generatrix
- Measurement: Force-displacement relationship throughout compression
- Analysis: Identification of elastic deformation limits and plastic deformation region
This method effectively characterizes the transition from elastic to plastic deformation, which occurs at remarkably low forces (<0.4N) for most stent designs [93]. The resulting force-displacement curves enable quantitative comparison between stent platforms and identification of design-specific mechanical behaviors.
Figure 1: Radial Force Compression Testing Workflow
Elastic Tube Pressure Testing
This methodology evaluates stent performance under clinically relevant conditions [93]:
- Apparatus: 3.0-mm elastic tube with controlled pressure gradient
- Precision: 50-micron measurement capability
- Method: Creation of pressure differential between interior and exterior of tube
- Measurement: Pressure-diameter relationship throughout expansion
This test reveals performance differences not apparent under baseline conditions, with significant divergence occurring after 0.3 × 10ⵠPa pressure [93]. The methodology generates characteristic pressure-diameter curves for each stent type, enabling direct comparison of deformation resistance in a simulated vascular environment.
Comprehensive Mechanical Deformation Testing
For peripheral arterial stents, more extensive testing is required to evaluate performance under multiple deformation modes [96]:
- Axial tension and compression: Measures resistance to longitudinal forces
- Three-point bending: Quantifies flexibility and bending stiffness
- Radial compression: Directly assesses radial strength
- Torsion: Evaluates resistance to twisting forces
This comprehensive approach revealed that no single stent design demonstrates superior characteristics under all deformation modes, with many experiencing global buckling and diameter pinching under extreme conditions [96].
Figure 2: Comprehensive Stent Mechanical Testing Methodology
Serial Optical Coherence Tomography (OCT) Imaging
For clinical assessment of chronic stent recoil, serial OCT provides detailed volumetric analysis [95]:
- Timeline: Baseline post-procedure and follow-up (>6 months)
- Parameters: Stent volume, cross-sectional area, fracture assessment
- Definition of Chronic Recoil: >10% stent volume reduction over 10-mm length without fracture, or >10% reduction in cross-sectional area with fracture/deformation
This methodology enables precise quantification of long-term stent performance and identification of factors predictive of clinical failure.
The Scientist's Toolkit: Essential Research Materials
Table 3: Essential Research Reagents and Materials for Stent Mechanical Testing
| Category | Specific Materials | Research Function |
|---|---|---|
| Stent Platforms | Metallic DES (Co-Cr, SS), PLLA BRS, Mg alloy BRS | Experimental subjects for comparative benchmarking |
| Polymer Materials | PLLA, PDLLA, PLGA, PCL, Polycarbonates | Bioresorbable scaffold fabrication and coating development |
| Testing Equipment | Dynamometer, Elastic tube systems, OCT imaging, CellScale biotester | Radial force measurement, simulated vascular testing, clinical imaging |
| Analytical Tools | Finite element analysis software, Computational fluid dynamics | Predictive modeling of stent performance and hemodynamic effects |
| Biocompatibility Assays | Cell culture models, Protein adsorption assays, Inflammation markers | Assessment of biological response to stent materials |
Emerging Technologies and Future Directions
Next-Generation Biodegradable Stents
The integration of advanced technologies is transforming stent functionality beyond simple mechanical scaffolding [97]:
- Biosensor integration: Real-time monitoring of endothelial healing, inflammatory response, and local drug concentrations
- Personalized drug delivery: Adjustable release profiles based on patient-specific characteristics and comorbidities
- Advanced biomaterials: Smart polymers with programmable degradation kinetics and enhanced biocompatibility
These innovations address fundamental limitations of current biodegradable stents, including suboptimal degradation timing and implantation complexity [97].
Drug-Eluting Balloon Alternatives
For treating in-stent restenosis, drug-eluting balloons (DEB) present a metal-free alternative [98]. The SELUTION4ISR trial demonstrated that sirolimus-eluting balloons perform comparably to standard care (16.2% vs. 13.5% target lesion failure at one year), offering a promising approach for patients with multiple stent layers who cannot tolerate additional metal implants [98].
Advanced Material Technologies
Fourth-generation stent technologies incorporate several groundbreaking approaches [94]:
- Gradient-release polymers: Variable drug elution rates tailored to temporal healing requirements
- Biomimetic polymers: Extracellular matrix-mimicking materials promoting endothelialization
- Nanoporous surface technologies: Polymer-free drug delivery with controlled elution kinetics
- 3D-printed personalized stents: Patient-specific designs based on individual anatomy
These innovations have contributed to remarkable improvements in clinical outcomes, with contemporary DES platforms demonstrating target lesion failure rates below 3% at one year and very late stent thrombosis rates declining to unprecedented lows (<0.1% per year) [94].
This benchmarking analysis demonstrates that radial strength and recoil performance remain critically important determinants of stent success, with significant differences between metallic and polymeric platforms. Metallic stents continue to offer superior mechanical properties and predictable long-term performance, while bioresorbable polymeric scaffolds provide the advantage of temporary support and eventual restoration of vascular physiology.
The optimal stent platform selection involves balancing acute mechanical performance with long-term biological response. Emerging technologies integrating biosensing, personalized drug delivery, and advanced biomaterials promise to transform stent functionality from passive scaffolding to active therapeutic systems. For researchers developing next-generation cardiovascular devices, comprehensive mechanical characterization using standardized methodologies remains essential for translating novel biomaterial concepts into clinically viable technologies that improve patient outcomes.
The selection between metallic and polymeric biomaterials is a fundamental decision in medical device design, directly influencing long-term clinical success and patient outcomes. These material classes exhibit profoundly different mechanical properties, degradation behaviors, and biological interactions that dictate their performance in physiological environments. This guide provides an objective comparison of metallic versus polymeric biomaterials, synthesizing recent experimental data to evaluate their clinical outcomes across orthopedic, cardiovascular, and tissue engineering applications. By examining mechanical integrity, degradation profiles, biocompatibility, and complication rates, this analysis aims to equip researchers and clinicians with evidence-based insights for material selection in therapeutic development.
Table 1: Fundamental Characteristics of Metallic and Polymeric Biomaterials
| Property | Metallic Biomaterials | Polymeric Biomaterials |
|---|---|---|
| Primary Materials | Magnesium alloys, Niobium alloys, Titanium alloys, Stainless Steel [11] [33] [28] | Poly-L-lactic acid (PLLA), Polyglycolic acid (PGA), Polycaprolactone (PCL), Polyurethane (PU), Chitosan [25] [14] |
| Typical Young's Modulus | 41-110 GPa (Mg alloys: 41-45 GPa; Nb alloys: ~69-103 GPa) [33] [28] | 0.5-3 GPa (PLLA: ~2.7 GPa) [14] |
| Tensile Strength | 200-250 MPa (Mg-Sr-Mn alloy: 242 MPa) [28] | 50-70 MPa (PLLA) [14] |
| Degradation Mechanism | Corrosion (aqueous/electrochemical) [28] | Hydrolysis and enzymatic cleavage [14] |
| Degradation Timeline | Months to years (Mg alloys: targeted <0.5 mm/year) [28] | Months to years (PLLA: complete resorption ~2-3 years) [14] |
| Key Clinical Advantages | High strength, fracture toughness, bioactivity (Mg²âº, Sr²âº) [11] [28] | Tailorable degradation, drug delivery capacity, biomimicry of ECM [99] [25] |
Mechanical Properties and Structural Performance
The mechanical compatibility of an implant with native tissue is critical for long-term functional integration. Metallic biomaterials typically provide superior tensile strength, yield strength, and fracture toughness, making them indispensable for load-bearing applications such as orthopedic fixation and joint replacement [11]. For instance, advanced magnesium alloys like Mg-0.3Sr-0.4Mn (SM04) demonstrate yield strength of 205 MPa and ultimate tensile strength of 242 MPa, exceeding the minimum thresholds required for bone implants [28]. The elastic modulus of metals, however, often significantly exceeds that of bone, leading to a phenomenon known as "stress shielding." This mismatch can cause bone resorption and implant loosening over time. Niobium alloys present an advantage with a lower elastic modulus (69-103 GPa) closer to bone, thereby reducing this risk [33].
Polymeric biomaterials, particularly biodegradable polyesters like PLLA, exhibit significantly lower mechanical strength and stiffness [14]. While this limits their use in high-load environments, their flexibility and compliance make them excellent for soft tissue applications, including vascular scaffolds and hernia repair meshes [99]. To achieve sufficient radial strength in a bioresorbable vascular scaffold (BRS), PLLA typically requires strut thicknesses approximately 240% greater than those of metallic drug-eluting stents [14]. This structural compromise can affect device deliverability and hemodynamics. The mechanical integrity of polymers is also transient; semicrystalline polymers like PLLA experience a rapid decline in strength during the second stage of degradation when hydrolytic scission of the amorphous tie chains occurs [14].
Table 2: Experimentally Measured Mechanical Properties of Select Biomaterials
| Material | Yield Strength (MPa) | Ultimate Tensile Strength (MPa) | Elongation at Break (%) | Young's Modulus (GPa) | Source/Alloy |
|---|---|---|---|---|---|
| Metallic Alloy | 205 | 242 | Not Specified | 41-45 | Mg-0.3Sr-0.4Mn (SM04) [28] |
| Metallic Alloy | ~150 | 213 | ~3 | Not Specified | Mg-2Sr (Rolled) [28] |
| Pure Metal | Not Specified | Not Specified | 25 | 103 | Pure Niobium [33] |
| Metallic Alloy | Not Specified | Not Specified | Not Specified | 69 | Nb-1Zr Alloy [33] |
| Polymer | Not Specified | 50-70 | 2-6 | ~2.7 | Poly-L-lactic Acid (PLLA) [14] |
Degradation Behavior and Mass Transport Properties
Controlled degradation is the cornerstone of next-generation "bioresorbable" implants, which aim to provide temporary support and then disappear, restoring native tissue function.
Metallic Biomaterials Degradation: Biocorrodible metals like magnesium degrade via an electrochemical corrosion process in the aqueous physiological environment. The degradation rate is a critical performance metric. For orthopedic applications, a target corrosion rate of <0.5 mm/year is ideal to maintain mechanical integrity until sufficient bone healing has occurred [28]. The Mg-Sr-Mn alloy SM04 demonstrates a corrosion rate of 0.39 mm/year, a 54% reduction compared to the binary Mg-Sr alloy, achieved by grain refinement and the formation of protective surface layers [28]. The degradation products, including Mg²⺠and Sr²⺠ions, are not only biocompatible but also bioactive, playing roles in promoting osteogenesis and bone metabolism [28].
Polymeric Biomaterials Degradation: Biodegradable polymers like PLLA degrade through hydrolysis, a bimolecular nucleophilic substitution reaction that cleaves ester bonds in the polymer backbone [14]. This process occurs in three distinct stages: (I) hydration and cleavage of amorphous tie chains, causing a drop in molecular weight without mass loss; (II) loss of mechanical strength due to scission of load-bearing amorphous chains, leading to structural fragmentation; and (III) mass loss and eventual resorption of low-molecular-weight fragments via metabolic pathways [14]. The degradation rate can be tailored by adjusting crystallinity, copolymer composition, and molecular weight.
Biocompatibility and Biological Response
The biological response to an implant determines its long-term success and defines the rate of complications such as inflammation, fibrosis, and foreign body rejection.
Metallic biomaterials are generally considered bio-tolerant. However, the release of metal ions due to corrosion can sometimes lead to chronic allergies, toxicity, or excessive inflammation [11] [28]. Niobium stands out for its exceptional biocompatibility, forming a passive Nbâ‚‚Oâ‚… oxide layer that minimizes ion release and elicits no rejection response from human tissues [33]. Furthermore, specific alloying elements are chosen for their bio-positive effects. Strontium (Sr) in Mg alloys has been shown to enhance osteoblast activity and bone mineralization [28], while manganese (Mn) is an essential trace element involved in antioxidant defense and osteoblast differentiation [28].
Polymeric biomaterials can be broadly categorized into synthetic and natural polymers, each with distinct biocompatibility profiles. Natural polymers like collagen, chitosan, and hyaluronic acid exhibit excellent inherent biocompatibility and biomimicry of the native extracellular matrix (ECM), which minimizes chronic inflammation [25]. Their main drawbacks are potential immunogenicity and batch-to-batch variability. Synthetic polymers like PLA, PGA, and PCL offer reproducible and tailorable properties but often lack cell adhesion sites and can trigger a foreign body reaction, sometimes leading to fibrotic encapsulation [25]. This is a significant issue with traditional polypropylene hernia meshes, which can cause chronic inflammation and pain [99].
Clinical Outcomes and Complication Rates by Application
Orthopedic Applications
In orthopedics, metallic biomaterials dominate the market for load-bearing implants like joint replacements and fracture fixation plates, largely due to their strength and durability [100]. The emergence of biodegradable Mg alloys aims to eliminate the need for a second surgery for implant removal and reduce long-term stress shielding. The key challenge is balancing the degradation rate with the bone healing timeline. An alloy that degrades too quickly loses mechanical integrity prematurely, while one that degrades too slowly may impede complete bone remodeling [28]. The Mg-Sr-Mn SM04 alloy demonstrates a promising balance, with a corrosion rate of 0.39 mm/year and a 2.46-fold increase in alkaline phosphatase (ALP) activity—a marker for osteogenesis—compared to the control, indicating enhanced bone-forming potential [28].
Polymeric materials are widely used in orthopedics in a non-load-bearing capacity, such as porous scaffolds for bone tissue engineering. These scaffolds are designed to be biomimetic, providing a 3D template that guides cell adhesion, proliferation, and differentiation [25]. Their composition and architecture can be tailored to deliver growth factors and promote vascularization, addressing the critical challenge of integrating large engineered tissue constructs [25].
Cardiovascular Applications (Stents)
The performance of bioresorbable stents (BRS) highlights the direct trade-off between the mechanical strength of metals and the tailored degradability of polymers.
Polymer-based BRS, most notably the PLLA-based Absorb BVS, pioneered the concept of providing transient vessel support. However, their thick strut profiles (necessary to compensate for PLLA's low radial strength) were associated with higher rates of acute thrombotic events and late scaffold thrombosis compared to modern metallic drug-eluting stents (DES) [14]. The scaffold's degradation process itself can be pro-thrombogenic during the period of mass loss and structural disintegration [14].
Magnesium-based BRS represent a metallic approach to bioresorption. Mg alloys like Magmaris (Mg with Rare Earth elements) offer superior radial strength and thinner struts than their polymeric counterparts, leading to more favorable hemodynamics and a lower thrombogenic profile [14]. The primary limitation of Mg alloys has been their relatively rapid degradation, which can lead to premature loss of mechanical support and early vessel recoil. Ongoing research focuses on alloying and processing to further slow the corrosion rate and extend the functional support window.
Soft Tissue Repair (Hernia Meshes)
The evolution of hernia repair meshes illustrates the shift from inert, permanent materials to regenerative, bioresorbable scaffolds. Traditional polypropylene meshes, while effective at reducing recurrence, are biologically inert and often trigger chronic inflammation, fibrosis, pain, and a foreign body sensation [99]. This is a classic example of a long-term complication arising from a permanent synthetic material.
The new generation of tissue-engineered scaffolds uses biodegradable polymers, both synthetic (e.g., PLA, PCL) and natural (e.g., chitosan, ECM-derived proteins), to transition from passive reinforcement to active regeneration [99]. These biomimetic scaffolds are designed to mimic the native ECM, facilitating cell integration and degrading at a rate that allows for the formation of new, functional tissue while minimizing chronic complications [99]. The integration of nanotechnology allows for the controlled release of anti-inflammatory or antimicrobial agents, further improving the biocompatibility and long-term outcomes [99].
Essential Research Reagents and Methodologies
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Materials and Reagents for Biomaterials Research
| Reagent/Material | Function in Research | Application Example |
|---|---|---|
| Simulated Body Fluid (SBF) | In vitro assessment of biodegradation and bioactivity [28] | Electrochemical corrosion testing; observing apatite formation on surfaces |
| MC3T3-E1 Cell Line | Pre-osteoblast model for in vitro cytocompatibility and osteogenesis assays [28] | Testing cell adhesion, proliferation, and differentiation (e.g., ALP activity) on new alloys |
| Alkaline Phosphatase (ALP) Assay Kit | Quantitative measurement of osteoblast differentiation activity [28] | Evaluating the osteo-inductive potential of Mg-Sr-Mn alloys |
| Poly-L-lactic Acid (PLLA) Resin | Raw material for fabricating biodegradable polymeric scaffolds and devices [14] | Manufacturing bioresorbable vascular scaffolds (BRS) or tissue engineering matrices |
| SEM/EDS (Scanning Electron Microscopy/Energy Dispersive X-ray Spectroscopy) | Characterization of surface morphology, corrosion products, and elemental composition [28] | Analyzing the microstructure and corrosion layer of Mg alloys after immersion in SBF |
Standard Experimental Protocols
In Vitro Degradation Testing (Metallic Alloys):
- Methodology: Electrochemical tests including potentiodynamic polarization and electrochemical impedance spectroscopy (EIS) are conducted in a standard three-electrode cell filled with simulated body fluid (SBF) at 37°C. Immersion tests are performed by placing samples in SBF for set durations, with the solution refreshed periodically to mimic in vivo conditions [28].
- Data Analysis: The corrosion rate is calculated from polarization curves using the Tafel extrapolation method. Hydrogen evolution is monitored during immersion, and the degraded surface is analyzed using SEM/EDS to observe pitting and the composition of the corrosion layer [28].
In Vitro Degradation Testing (Polymers):
- Methodology: PLLA-based scaffold samples are immersed in phosphate-buffered saline (PBS) at 37°C in a controlled incubator. The pH of the solution may be monitored as the degradation of polyesters releases acidic byproducts [14].
- Data Analysis: At predetermined time points, samples are removed, dried, and weighed to track mass loss. Gel permeation chromatography (GPC) is used to monitor the reduction in molecular weight over time, which is the primary indicator of the first stage of degradation [14].
Mechanical Property Evaluation (Radial Strength for Stents):
- Methodology: A radial expansion force gauge (e.g., MSI RX550) is used. The scaffold or stent is mounted on a holder and subjected to compressive forces. The test measures the force required to cause a defined diametric compression [14].
- Data Analysis: Radial strength is reported as the pressure (in MPa) at which the device yields or fractures. This data allows for direct comparison of the mechanical support provided by different BRS and traditional metallic DES [14].
Visual Experimental Workflows
Biomaterial Degradation Analysis Workflow
(Biomaterial Degradation Analysis Workflow)
Biomaterial Development and Evaluation Pathway
(Biomaterial Development and Evaluation Pathway)
The selection between metallic and polymeric biomaterials represents a critical strategic decision in medical device development, influencing everything from initial manufacturing to long-term clinical performance. Biomaterials are defined as substances (other than drugs) of synthetic or natural origin that can be used to treat, enhance, or restore body functions [11]. The global biomaterials market, estimated to reach $47.5 billion by 2025, reflects the significance of these materials in medical advancement [11]. This guide provides an objective comparison of metallic and polymeric biomaterials, focusing on their mechanical performance, manufacturing considerations, and lifecycle costs to inform researchers, scientists, and drug development professionals.
Metallic biomaterials, including stainless steels, cobalt-chromium alloys, and titanium alloys, have traditionally dominated load-bearing applications due to their exceptional strength and durability [101]. Meanwhile, polymeric biomaterials—both biodegradable varieties like poly-l-lactic acid (PLLA) and permanent ones like ultra-high molecular weight polyethylene—offer distinct advantages in tissue integration, drug delivery capabilities, and design flexibility [11] [4]. The following sections provide a detailed comparative analysis of these material classes to support evidence-based selection for specific biomedical applications.
Comparative Mechanical Properties
Essential Mechanical Properties for Biomaterials
Biomaterials for load-bearing applications must satisfy multiple mechanical requirements to ensure clinical success. Key properties include adequate strength to withstand physiological loads, appropriate modulus of elasticity to prevent stress shielding (where the implant bears too much load, causing bone resorption), high wear resistance to minimize debris generation, and long fatigue life to endure cyclic loading [101]. Stress shielding can be prevented by matching the modulus of elasticity of biomaterials to that of bone, which varies from 4 to 30 GPa [101]. Additionally, the material should have a low modulus combined with high strength to prolong the service period of the implant and prevent loosening, thereby preventing the need for revision surgery [101].
Table 1: Comparative Mechanical Properties of Biomaterials and Natural Tissues
| Material Category | Specific Material | Tensile Strength (MPa) | Tensile Modulus (GPa) | Fatigue Life | Fracture Toughness |
|---|---|---|---|---|---|
| Metallic Biomaterials | 316L Stainless Steel | 465-950 | 200 | High | High |
| Co-Cr Alloys | 655-1896 | 210-230 | High | High | |
| Ti-6Al-4V | 897-1200 | 110-125 | High | High | |
| Magnesium Alloys | 100-300 | 41-45 | Moderate | Moderate | |
| Polymeric Biomaterials | PLLA | 50-70 | 3-4 | Low to Moderate | Low |
| UHMWPE | 40 | 0.5-1.4 | Moderate | Moderate | |
| Polyurethane | 30-40 | 0.002-0.5 | Moderate | High | |
| Natural Tissues | Cortical Bone | 50-150 | 4-30 | N/A | N/A |
| Articular Cartilage | 10-40 | 0.001-0.01 | N/A | N/A |
Specialized Performance Characteristics
Beyond basic mechanical properties, specialized performance characteristics critically influence biomaterial selection. Wear resistance is particularly crucial for articulating surfaces in joint replacements. Metallic biomaterials generally exhibit excellent wear resistance, though wear debris from metal-on-metal implants can cause adverse tissue reactions [101]. Polymeric materials like UHMWPE offer good wear characteristics when paired with metallic or ceramic counter surfaces, though their relatively low mechanical strength has limited their use in load-bearing applications without reinforcement [102].
Fatigue behavior represents another critical differentiation factor. Metals typically demonstrate superior fatigue resistance under cyclic loading conditions, making them suitable for applications like bone plates and spinal fixation devices [101]. Polymers exhibit more variable fatigue performance, with factors including molecular weight, crystallinity, and reinforcement strategies significantly influencing endurance limits [102]. For biodegradable polymeric scaffolds, fatigue resistance becomes particularly crucial as the material must maintain mechanical integrity while degrading over time [102].
Manufacturing Processes and Considerations
Traditional and Advanced Manufacturing Techniques
Manufacturing approaches for metallic and polymeric biomaterials differ significantly, impacting both cost and performance outcomes. Traditional metal processing techniques include investment casting (particularly for cobalt-chromium alloys), forging, and machining [101]. These processes often require secondary operations to achieve desired surface finishes and mechanical properties, adding to manufacturing complexity and cost.
Additive manufacturing (AM) has revolutionized biomaterial processing, enabling patient-specific implants with complex geometries. For metallic biomaterials, selective laser melting (SLM) and electron beam melting (EBM) are commonly employed, particularly for titanium and its alloys [4]. These techniques produce fine structures with minimal contaminants and can be followed by post-processing steps such as hydrothermal treatment to improve surface properties [4]. Polymer processing techniques include injection molding, extrusion, and various AM approaches such as fused deposition modeling (FDM) for biodegradable polymers like PLLA and PCL [11] [4].
Table 2: Manufacturing Methods for Metallic vs. Polymeric Biomaterials
| Manufacturing Aspect | Metallic Biomaterials | Polymeric Biomaterials |
|---|---|---|
| Traditional Methods | Investment casting, forging, machining | Injection molding, extrusion, compression molding |
| Additive Manufacturing | Selective laser melting (SLM), Electron beam melting (EBM) | Fused deposition modeling (FDM), Stereo-lithography (SLA) |
| Post-processing | Heat treatment, surface grinding, electrophishing | Surface modification, sterilization, drug incorporation |
| Design Flexibility | High with AM, limited with traditional methods | Generally high across methods |
| Customization Cost | High for traditional, moderate for AM | Low to moderate |
Manufacturing Impact on Material Properties
Manufacturing processes profoundly influence final material properties. For metallic biomaterials, techniques like severe plastic deformation can enhance strength and fatigue resistance while maintaining biocompatibility [101]. For polymers, processing parameters significantly affect crystallinity, molecular orientation, and ultimately, mechanical performance [102] [14]. The degradation profile of biodegradable polymers like PLLA is particularly sensitive to processing conditions, as factors like thermal history influence crystallinity, which subsequently affects hydrolysis rates [14].
Advanced manufacturing approaches also enable composite structures that overcome individual material limitations. For example, incorporating magnesium into polymer matrices provides higher mechanical strength and fracture toughness, while the polymer prevents premature degradation of the composite [11]. Similarly, 3D-printed polymeric scaffolds can be reinforced with ceramic nanoparticles to improve both mechanical properties and biological activity [11] [4].
Figure 1: Comparative Manufacturing Workflows for Metallic and Polymeric Biomaterials
Experimental Assessment Methodologies
Standardized Testing Protocols
Rigorous experimental assessment is essential for evaluating biomaterial performance. Standardized mechanical testing protocols include tensile testing (ASTM F2516), compression testing (ASTM F2077), and fatigue testing (ASTM F1800, ASTM F2118) [101]. These tests provide quantitative data on fundamental mechanical properties under controlled conditions. For wear assessment, specialized equipment simulates in vivo conditions, with parameters like load, frequency, and lubrication controlled to mimic physiological environments [101].
For biodegradable materials, additional testing must monitor property evolution during degradation. Accelerated degradation models in simulated body fluid at elevated temperatures provide preliminary data, though correlation with real-time degradation at 37°C remains essential for clinical prediction [14]. Chemical analysis techniques including gel permeation chromatography (for molecular weight), mass loss measurements, and pH monitoring track degradation progression [102] [14].
Advanced Characterization Techniques
Advanced characterization techniques provide deeper insight into biomaterial behavior. Scanning electron microscopy (SEM) reveals surface topography, wear mechanisms, and degradation patterns at micro- to nanoscale resolution [101]. Fourier-transform infrared spectroscopy (FTIR) monitors chemical changes during polymer degradation, while differential scanning calorimetry (DSC) tracks thermal property transitions that influence mechanical performance [102] [14].
For in vitro biological assessment, cell culture studies evaluate cytotoxicity (per ISO 10993-5), cell adhesion, and proliferation on material surfaces [11]. Bio-reactors simulating physiological mechanical stimulation provide more clinically relevant conditions for evaluating tissue-engineered constructs [102]. These comprehensive assessment methodologies enable researchers to establish structure-property-performance relationships essential for biomaterial optimization.
Lifecycle Cost-Benefit Analysis
Comprehensive Cost Assessment Framework
Lifecycle cost-benefit analysis (CBA) provides a systematic approach to evaluate the economic viability of biomaterials throughout their entire lifespan—from raw material acquisition to eventual implant removal or resorption [103]. A comprehensive CBA for biomaterials should consider direct costs (raw materials, manufacturing, sterilization), indirect costs (research and development, regulatory compliance), intangible costs (potential risks, learning curve), and opportunity costs [103]. The cost-benefit ratio formula compares the present value of benefits to costs: Cost-Benefit Ratio = Sum of Present Value Benefits / Sum of Present Value Costs [103]. A result greater than 1 indicates a positive return on investment.
For biomaterials, the benefit component must extend beyond simple financial metrics to include clinical outcomes such as reduced rehabilitation time, improved quality of life, and decreased revision surgery rates [103] [104]. Polymeric biomaterials often present higher initial manufacturing costs but may offer long-term benefits through reduced follow-up interventions, particularly for biodegradable systems that eliminate the need for implant removal [14].
Table 3: Lifecycle Cost-Benefit Analysis of Metallic vs. Polymeric Biomaterials
| Cost-Benefit Factor | Metallic Biomaterials | Polymeric Biomaterials |
|---|---|---|
| Raw Material Cost | High (especially for Ti, Co-Cr alloys) | Low to Moderate |
| Manufacturing Cost | Moderate to High | Low to Moderate |
| Device Longevity | 10-20+ years | Varies (months to permanent) |
| Revision Risk | Moderate (mainly due to wear/loosening) | Variable (higher for early-generation BRS) |
| Biointegration Potential | Moderate (requires surface modification) | High (especially porous/resorbable) |
| Drug Delivery Capability | Limited (requires coatings) | High (intrinsic capability) |
| Removal Surgery Cost | High (if required) | None for resorbable materials |
Clinical and Economic Outcomes
The ultimate validation of biomaterial selection comes from clinical and economic outcomes data. Metallic implants generally offer excellent long-term durability in load-bearing applications, with survival rates exceeding 90% at 10 years for joint replacements [101]. However, complications including wear debris-induced osteolysis, stress shielding, and corrosion products may necessitate revision surgery with substantial associated costs [101].
Polymeric biomaterials present a different value proposition. While early-generation bioresorbable vascular scaffolds demonstrated higher acute thrombotic events potentially linked to thick struts and flow disturbances [14], advanced formulations address these limitations through improved material processing and design optimization [102] [14]. The economic benefit of avoiding permanent implants is particularly significant for younger patients who might otherwise require multiple revision surgeries over their lifespan [14].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Materials for Biomaterials Investigation
| Research Material | Category | Research Function | Example Applications |
|---|---|---|---|
| Poly-L-lactic acid (PLLA) | Biodegradable Polymer | Primary material for resorbable constructs | Bioresorbable scaffolds, tissue engineering matrices |
| Ti-6Al-4V ELI | Metallic Alloy | Gold standard for metallic implants | Orthopedic implants, dental roots |
| Simulated Body Fluid (SBF) | Testing Reagent | In vitro bioactivity and corrosion assessment | Evaluating apatite formation, degradation kinetics |
| Cell Culture Media | Biological Reagent | In vitro biocompatibility assessment | Cytotoxicity testing, cell-material interaction studies |
| Phosphate Buffered Saline (PBS) | Biochemical Reagent | Degradation studies, control medium | Hydrolytic degradation acceleration |
| Scanning Electron Microscope | Characterization Equipment | Surface topography and failure analysis | Wear mechanism identification, degradation morphology |
| Gel Permeation Chromatography | Analytical Instrument | Molecular weight distribution analysis | Polymer degradation tracking |
Figure 2: Biomaterial Selection Logic Based on Application Requirements
The choice between metallic and polymeric biomaterials involves nuanced trade-offs between mechanical performance, biological response, manufacturing complexity, and lifecycle economics. Metallic biomaterials remain the gold standard for high load-bearing applications where longevity and mechanical reliability are paramount, despite limitations including permanent implantation, stress shielding effects, and potential ion release [101]. Polymeric biomaterials offer superior opportunities for biological integration, drug delivery, and resorbability, though early mechanical limitations are being addressed through material engineering and processing innovations [102] [14].
Future advancements in both material classes will focus on overcoming current limitations. For metallic biomaterials, developments include biodegradable metals (magnesium, iron alloys) [11] [14] and surface modifications to enhance biointegration. For polymers, research directions include advanced composites with nanoreinforcements [102], smart responsive materials [4], and improved processing techniques for enhanced mechanical properties. The growing polymer biomaterial market, projected to reach $94.98 billion in 2025 [83], reflects the increasing importance of these materials in medical advancement.
The optimal biomaterial selection ultimately depends on the specific clinical application, patient factors, and economic considerations. Through continued research and development, both metallic and polymeric biomaterials will evolve to better address the complex challenges of modern medical device design and tissue engineering, ultimately improving patient outcomes through evidence-based material selection.
The field of materials science is undergoing a revolutionary transformation driven by the development of smart polymers, multi-principal element alloys (MPEAs), and sophisticated hybrid materials. These advanced materials are redefining performance boundaries across biomedical, aerospace, and sustainable technology applications. Smart polymers, also known as stimuli-responsive polymers, represent a novel class of high-performance materials that undergo reversible structural changes at the molecular level in response to minimal environmental variations [105]. Simultaneously, MPEAs (also referred to as high-entropy alloys) defy traditional alloy design principles by incorporating multiple principal elements in near-equiatomic proportions, creating exceptional mechanical properties and corrosion resistance [106]. The global biomaterials market, valued at $35.5 billion in 2020, is projected to reach $47.5 billion by 2025, reflecting the significant economic and technological importance of these material advances [11].
This comparison guide examines the fundamental characteristics, experimental performance data, and application potential of these material systems within the specific context of mechanical properties for biomedical applications. The content is structured to provide researchers, scientists, and drug development professionals with objective experimental comparisons and methodologies to inform material selection for specific biomedical applications.
Smart Polymers: Responsive Materials for Biomedical Applications
Fundamental Characteristics and Classification
Smart polymers are characterized by their unique ability to undergo reversible physical or chemical changes in response to external stimuli such as temperature, pH, magnetic fields, or light [105]. These transformations occur at the functional polymer segments, manifesting macroscopically as changes in solubility in aqueous solutions or alterations in the volume and water content of polymer hydrogels. This responsiveness enables precise control over material behavior in biological environments, making them particularly valuable for drug delivery, tissue engineering, and separation science applications.
The classification of smart polymers is based on their stimulus response mechanisms:
- Thermo-responsive Systems: Respond to temperature changes with reversible phase transitions (e.g., poly(N-isopropylacrylamide) [105]
- pH-responsive Systems: React to alterations in environmental pH [105]
- Magnetically-responsive Systems: Contain magnetic components that respond to external magnetic fields [105]
- Dual-stimuli-responsive Systems: Combine multiple responsiveness mechanisms for enhanced control [105]
Key Research Reagent Solutions
Table 1: Essential Research Reagents for Smart Polymer Systems
| Reagent/Material | Function/Application | Key Characteristics |
|---|---|---|
| Poly(N-isopropylacrylamide) | Thermo-responsive polymer | Exhibits lower critical solution temperature (LCST) around 32°C [105] |
| N-vinylcaprolactam | Thermo-responsive monomer | Used in synthesis of thermo-sensitive hydrogels and microgels [105] |
| Ethylene oxide-propylene oxide copolymers | Thermo-separating polymers | Enable phase separation with temperature changes for protein recovery [105] |
| Eudragit S100 | pH-responsive polymer | Anionic polymer for pH-dependent precipitation and purification [105] |
| Magnetic ionic liquids | Magnetically-responsive solvents | Enable magnetic separation in aqueous two-phase systems [105] |
Experimental Methodologies for Smart Polymer Analysis
Thermo-responsive Phase Separation Protocol: A standard methodology for evaluating thermo-responsive polymers involves preparing aqueous solutions at specific concentrations (typically 5-15% w/w) and subjecting them to controlled temperature cycles. The phase separation behavior is monitored spectrophotometrically by measuring turbidity at 600 nm while gradually increasing temperature (0.5-1.0°C/min) across the expected transition range. The cloud point is determined as the temperature at which 50% reduction in transmittance occurs [105].
Stimuli-Responsive Aqueous Two-Phase System (ATPS) Extraction: This protocol involves constructing ATPS using smart polymers that respond to external stimuli. For thermo-responsive systems, the polymer and target compounds are dissolved in aqueous buffer and mixed at temperature below the cloud point. The temperature is then raised above the transition point to induce phase separation. The polymer-rich phase can be recovered and the polymer recycled by simply reversing the stimulus. This method has been successfully applied for protein recovery, enzyme separation, and biopharmaceutical purification [105].
Multi-Principal Element Alloys: Revolutionizing Metallic Biomaterials
Fundamental Principles and Core Effects
Multi-principal element alloys represent a paradigm shift from traditional alloy design, which typically features one predominant base element with minor additions. MPEAs consist of five or more principal elements in equiatomic or near-equiatomic proportions (typically 5-35% atomic concentration each) [106]. This innovative approach creates four distinctive core effects that govern their exceptional properties:
- High-entropy effect: The random distribution of multiple elements significantly increases configurational entropy, stabilizing solid solution phases and inhibiting intermetallic compound formation [106]
- Severe lattice distortion effect: Atomic size differences among constituent elements create pronounced lattice strain, enhancing dislocation pinning capability and increasing hardness and wear resistance [106]
- Sluggish diffusion effect: The varied melting points and bond strengths of different atoms retard diffusion processes, improving microstructural stability at elevated temperatures [106]
- "Cocktail" effect: Synergistic interactions between constituent elements produce unexpected property combinations not seen in conventional alloys [106]
Classification and Biomedical Applications
MPEAs for biomedical applications typically form simple solid solutions with face-centered cubic (FCC), body-centered cubic (BCC), or hexagonal close-packed (HCP) crystal structures despite their complex compositions [106]. Notable biomedical MPEA systems include TiZrNbTa, CrNbTiVZr, and FeNiCrCuCo alloys, which demonstrate excellent biocompatibility, corrosion resistance, and mechanical properties suitable for orthopedic and dental implants [106]. The global orthopedic implant market, valued at $45.19 billion in 2023 and projected to reach $71.74 billion by 2032, provides significant impetus for MPEA development in biomedical applications [106].
Key Research Reagent Solutions
Table 2: Essential Research Materials for MPEA Development
| Material/Equipment | Function/Application | Key Characteristics |
|---|---|---|
| Cantor alloy (CoCrFeNiMn) | Baseline MPEA system | One of the first MPEAs; extensively studied for fundamental properties [106] |
| Refractory MPEAs (NbMoTaW) | High-temperature applications | Exhibit superior high-temperature strength but contain CRMs [107] |
| CALPHAD (Thermo-Calc) | Computational phase prediction | Uses thermodynamic databases to predict phase formation in complex systems [107] |
| Critical Raw Materials (CRMs) | Elements with supply chain risks | Includes Ta, W, Nb, Hf; focus on developing reduced-CRM MPEAs [107] |
| Machine Learning Models | Property prediction | Extra Trees Regressor shows superior performance for hardness prediction [107] |
Experimental Methodologies for MPEA Characterization
MPEA Synthesis via Arc Melting: Standard laboratory-scale production of MPEAs employs vacuum arc melting with a water-cooled copper hearth under inert atmosphere (typically argon). High-purity constituent elements (≥99.9%) are weighed in equiatomic or near-equiatomic proportions and melted repeatedly (minimum five times) to ensure chemical homogeneity. The resulting ingots are subsequently homogenized in vacuum quartz tubes at temperatures ranging from 1000°C to 1300°C for several hours, followed by water quenching or controlled cooling [106].
Vickers Hardness Testing Protocol: Microhardness evaluation follows ASTM E384 standards using a Vickers hardness tester with a diamond pyramid indenter. Specimens are mounted, ground, and polished to a mirror finish. A minimum of ten indentations are performed per specimen using appropriate loads (typically 0.3-0.5 kgf) with a dwell time of 10-15 seconds. The diagonal lengths of the resulting impressions are measured to calculate Vickers hardness values (HV), reported as mean ± standard deviation [107].
Comparative Analysis of Mechanical Properties
Quantitative Performance Comparison
Table 3: Mechanical Properties Comparison of Metallic vs. Polymeric Biomaterials
| Material System | Tensile Strength (MPa) | Hardness | Elastic Modulus (GPA) | Key Applications |
|---|---|---|---|---|
| Traditional Ti-6Al-4V | 850-1000 [106] | 30-36 HRC [106] | 110-125 [106] | Orthopedic implants, dental components |
| CoCrFeNb₀.₃₀₉Ni MPEA | N/A | 480 HV [107] | N/A | High-strength biomedical implants |
| Reduced-CRM MPEA (Tiâ‚€.â‚€â‚â‚â‚â‚NiFeâ‚€.â‚„Cuâ‚€.â‚„) | N/A | 488 HV [107] | N/A | Sustainable alternative to CRM-containing MPEAs |
| Natural Fiber Composite (JF/CC/PALF) | 85.8 [108] | 72.6 Shore D [108] | N/A | Eco-friendly structural composites |
| Jute Fiber Composite | 28.26 [108] | N/A | N/A | Sustainable polymer reinforcement |
Material Property Trade-offs and Selection Criteria
The comparative data reveals significant trade-offs between different material classes. MPEAs demonstrate superior hardness values (480-488 HV) compared to traditional titanium alloys, making them suitable for high-wear applications such as joint replacements [107]. However, the presence of critical raw materials (CRMs) like Co, Ta, W, Nb, and Hf in many high-performance MPEAs creates supply chain vulnerabilities and environmental concerns [107]. This has motivated research into reduced-CRM MPEAs that maintain comparable mechanical performance while mitigating supply chain risks.
Natural fiber-reinforced polymers offer substantially lower mechanical properties but provide advantages in sustainability, biodegradability, and reduced health risks [108]. The alkaline treatment of natural fibers (e.g., jute, banana, coir) significantly improves fiber-matrix interfacial bonding by reducing hydroxyl groups and enhancing surface roughness, leading to improved mechanical and thermal performance [108].
Hybrid Material Systems and Future Directions
Integrated Material Solutions
The convergence of smart polymers, MPEAs, and hybrid composites represents the next frontier in advanced materials development. Hybrid natural fiber composites combining jute fiber (20%), coconut coir (20%), and pineapple leaf fiber (10%) in epoxy matrices have demonstrated optimized mechanical properties with tensile strength of 85.8 MPa, flexural strength of 134.5 MPa, and hardness of 72.6 Shore D [108]. Machine learning approaches, particularly random forest models, have shown exceptional predictive capability for these hybrid systems with R² values of 0.968 for tensile strength and 0.962 for hardness [108].
Machine Learning and Computational Materials Design
Data-driven approaches are revolutionizing materials development by reducing redundant experiments and trial-and-error processes. For epoxy polymers, integrating multi-algorithm outlier detection with selective re-experimentation of unreliable cases has been shown to significantly improve prediction accuracy for key mechanical properties (glass transition temperature, tan δ peak, and crosslinking density) while requiring only about 5% of the dataset to be re-measured [109]. For MPEAs, the Extra Trees Regressor machine learning model has demonstrated superior performance in predicting alloy hardness and guiding the development of reduced-CRM compositions [107].
Additive Manufacturing and Processing Innovations
Additive manufacturing (AM) technologies, particularly laser powder bed fusion (L-PBF), have enabled the production of complex, customized implants from both metallic and polymeric biomaterials [90]. The medical devices market for AM with metal powders was valued at $800 million in 2018 and is projected to reach $5.65 billion by 2025, reflecting the growing importance of these manufacturing technologies [90]. AM allows for the creation of porous scaffold structures that mimic the complex architecture of natural bone, promoting osseointegration and reducing stress-shielding effects through optimized mechanical properties [90].
The comparative analysis of smart polymers, multi-principal element alloys, and hybrid materials reveals distinct advantages and limitations for biomedical applications. MPEAs offer exceptional mechanical properties, corrosion resistance, and potential for high-temperature performance, though concerns regarding critical raw materials and supply chain sustainability must be addressed through continued development of reduced-CRM alternatives. Smart polymers provide unparalleled responsiveness to environmental stimuli, enabling advanced drug delivery, separation science, and tissue engineering applications. Hybrid material systems leverage the strengths of multiple material classes to achieve balanced performance profiles that can be tailored to specific application requirements.
Future developments in this field will be increasingly driven by integrated computational materials design approaches, including machine learning and computational thermodynamics, coupled with advanced manufacturing technologies like additive manufacturing. These methodologies will accelerate the discovery and optimization of next-generation materials with tailored properties for specific biomedical applications, ultimately enhancing patient outcomes through improved implant performance, biocompatibility, and functionality.
Visual Synthesis: Experimental Workflow for Advanced Materials Development
Diagram 1: Integrated workflow for advanced materials development, combining computational design, synthesis, characterization, and validation with machine learning refinement.
Conclusion
The choice between metallic and polymeric biomaterials is not a matter of superiority, but of strategic application based on a deep understanding of their distinct mechanical profiles. Metals generally offer superior tensile strength and durability for permanent, high-load-bearing applications, while polymers provide advantages in weight, radiolucency, biodegradability, and a closer match to native tissue modulus, which helps prevent stress shielding. The emergence of advanced manufacturing, novel composite strategies, and data-driven design using explainable AI is blurring the traditional boundaries, enabling the development of biomaterials with previously unattainable combinations of properties. The future of biomaterials lies in this multi-functional, patient-specific design paradigm, which promises to yield implants and scaffolds that not only repair but actively promote regeneration, ultimately improving clinical outcomes across medicine.
References
- 1. Biomaterial [https://en.wikipedia.org/wiki/Biomaterial]
- 2. Inspiration and application in the evolution of biomaterials [https://pmc.ncbi.nlm.nih.gov/articles/PMC2848528/]
- 3. A Critical Review on Polymeric Biomaterials for Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8433665/]
- 4. An Overview of Biomaterials: Advancements and ... [https://www.azom.com/article.aspx?ArticleID=108]
- 5. Metallic Biomaterials: Current Challenges and Opportunities [https://pmc.ncbi.nlm.nih.gov/articles/PMC5578250/]
- 6. Comparison of metal release from various ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961204001267]
- 7. Characterization of Mechanical of Properties Metal Biomaterials [https://link.springer.com/chapter/10.1007/978-3-319-68025-5_23]
- 8. Design and development of metallic with biological and... biomaterials [https://pubmed.ncbi.nlm.nih.gov/30861312/]
- 9. Recent perspective of polymeric biomaterial in tissue ... [https://www.sciencedirect.com/science/article/abs/pii/S2468519423004457]
- 10. Mechanical properties of polymeric biomaterials: Modified... [https://www.degruyterbrill.com/document/doi/10.1515/chem-2021-0112/html?lang=en&srsltid=AfmBOoqwftRXo6eiSZyzuTtZU3DBTOdmol6kqyPeFfZEsDFDo8tb2dP6]
- 11. Advances in Biodegradable Polymers and Biomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10488517/]
- 12. A compilation of experimental data on the mechanical ... [https://www.nature.com/articles/s41597-022-01283-9]
- 13. Chemical bonding - Atomic Structure, Intermolecular ... [https://www.britannica.com/science/chemical-bonding/Atomic-structure-and-bonding]
- 14. Mechanical behavior of polymer-based vs. metallic-based ... [https://jtd.amegroups.org/article/view/14531/html]
- 15. Flexural vs. Young's Modulus: Definitions & Formulas [https://welleshaft.com/en/flexural-modulus-vs-youngs-modulus-vs-elastic-modulus/]
- 16. Metal Strength Chart - A Pro Guide 2025! [https://www.partmfg.com/metal-strength-chart-a-pro-guide-2025/]
- 17. Flexural Modulus: Units, Formula & Material Table [https://www.specialchem.com/plastics/guide/stiffness]
- 18. Understanding Flexural Modulus: Guide to Material Rigidity [https://www.atlasfibre.com/understanding-flexural-modulus-guide-to-material-rigidity/]
- 19. A multi-objective synergistic design for low modulus and ... [https://www.nature.com/articles/s41524-025-01713-3]
- 20. The Mechanical Properties, Corrosion Resistance, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11818253/]
- 21. Mechanical behavior of polymer-based vs. metallic- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5583085/]
- 22. Effect of Fabrication Route on the Mechanical Properties ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389703/]
- 23. Recent Advances in Metal Particle Reinforced Polylactic ... [https://link.springer.com/article/10.1007/s13369-025-10555-6]
- 24. Improving Biocompatibility for Next Generation of Metallic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9851385/]
- 25. Polymeric Materials in Biomedical Engineering: A Bibliometric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608308/]
- 26. Exploring the future of metallic implants: a review of bi... [https://www.degruyterbrill.com/document/doi/10.1515/corrrev-2024-0125/html?lang=en&srsltid=AfmBOoqB5caW1le6LEZECNgbdA4JTZdOoeJa1OnJyIzAJQfU-QTXPthO]
- 27. Evaluation of wear, corrosion, and biocompatibility of a ... [https://www.sciencedirect.com/science/article/abs/pii/S1751616125000670]
- 28. Controllable degradation behavior, mechanical properties ... [https://www.nature.com/articles/s41529-025-00658-8]
- 29. Analysis of Mechanical Properties in Biomedical Polymers [https://eureka.patsnap.com/report-analysis-of-mechanical-properties-in-biomedical-polymers]
- 30. Comparison of engineering materials and biomaterials [https://www.doitpoms.ac.uk/tlplib/optimisation-biomaterials/comparison.php]
- 31. Biodegradable Medical Implants: Reshaping Future Medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462970/]
- 32. Fully bioresorbable hybrid opto-electronic neural implant ... [https://www.nature.com/articles/s41467-024-45803-0]
- 33. Bio-functional niobium-based metallic biomaterials [https://www.sciencedirect.com/science/article/abs/pii/S1742706124007554]
- 34. Current developments in orthopaedic implant technology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560316/]
- 35. Mechanical Characterization of Biomaterials [https://www.sciencedirect.com/science/article/abs/pii/B9780124158009000036]
- 36. Recent Advances in Experimental Testing and ... [https://link.springer.com/chapter/10.1007/978-981-10-4361-1_112]
- 37. Drug delivery, development, and technological aspects for ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X25001632]
- 38. Clinical performance of drug-eluting stents with biodegradable ... [https://eurointervention.pcronline.com/article/clinical-performance-of-drug-eluting-stents-with-biodegradable-polymeric-coating-a-meta-analysis-and-systematic-review]
- 39. Comparison of bioresorbable vs durable polymer drug- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7227223/]
- 40. Comparative clinical performance of two types of drug ... [https://www.revportcardiol.org/en-comparative-clinical-performance-two-types-articulo-S2174204921000398]
- 41. Influence of Stent Structure on Mechanical and Degradation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12295491/]
- 42. Improved vascular response to a novel polymeric blend ... [https://www.nature.com/articles/s41598-025-15997-4]
- 43. 3D printing of biodegradable polymer vascular stents to ... [https://www.sciencedirect.com/science/article/pii/S2214860425003483]
- 44. Biodegradable Metal-Based Stents: Advances, Challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470573/]
- 45. Preclinical Assessment of a Novel Polymer-Free Hybrid ... [https://link.springer.com/article/10.1007/s12265-025-10680-5]
- 46. Preclinical research models for evaluating the ... [https://www.sciencedirect.com/science/article/pii/S2452199X25004098]
- 47. Metallic ions as therapeutic agents in tissue engineering ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3262432/]
- 48. Simultaneous optimization of stiffness, permeability, and ... [https://www.sciencedirect.com/science/article/abs/pii/S0020722523001520]
- 49. A review of biomaterial degradation assessment ... [https://www.nature.com/articles/s41529-024-00487-1]
- 50. Flexural Strength vs Tensile Strength: What are the ... [https://www.testresources.net/blog/flexural-strength-vs-tensile-strength-what-are-the-similarities]
- 51. Guide to Flexural Strength in Materials [https://www.atlasfibre.com/understanding-flexural-strength-guide-to-flexural-strength-in-materials/]
- 52. A comparison of the degradation behaviour of 3D printed ... [https://www.sciencedirect.com/science/article/abs/pii/S0928493120336742]
- 53. Evaluation of bioactivity and biodegradability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10538513/]
- 54. Additive Manufacturing vs 3D Printing: Key Differences [https://amfasinternational.com/newsroom/additive-manufacturing-vs-3d-printing-are-they-the-same-or-different/]
- 55. Recent Advances in Additive Manufacturing: A Review of ... [https://www.mdpi.com/2075-1702/13/9/813]
- 56. Comparison of mechanical properties of different 3D ... [https://www.nature.com/articles/s41598-025-03632-1]
- 57. 3D printing: What does 2025 hold for additive manufacturing? [https://roboticsandautomationnews.com/2025/01/15/predictions-on-3d-printing-what-does-2025-hold-for-additive-manufacturing/88570/]
- 58. Biomechanical design of titanium-PEEK combined fusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12558872/]
- 59. Development and mechanical characterization of porous ... [https://www.sciencedirect.com/science/article/abs/pii/S1751616112000288]
- 60. The rational design, biofunctionalization and biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897010/]
- 61. Highly porous Ti as a bone substitute: Triboelectrochemical ... [https://www.sciencedirect.com/science/article/abs/pii/S0010938X21004625]
- 62. Application of 3D‑printed porous titanium interbody fusion [https://www.spandidos-publications.com/10.3892/etm.2024.12579]
- 63. Comparison of outcomes between 3D-printed porous ... [https://pubmed.ncbi.nlm.nih.gov/40614266/]
- 64. Preclinical evaluation of lateral interbody fusions using 3D ... [https://www.sciencedirect.com/science/article/pii/S2666548425001763]
- 65. Stress Shielding - an overview [https://www.sciencedirect.com/topics/veterinary-science-and-veterinary-medicine/stress-shielding]
- 66. The role of stiffness-matching in avoiding stress shielding ... [https://www.sciencedirect.com/science/article/abs/pii/S174270612300658X]
- 67. Stress-shielding in aseptic loosening on the 3D printed ... [https://www.explorationpub.com/Journals/ebmx/Article/101317]
- 68. implications for stress shielding in orthopedic implants [https://pmc.ncbi.nlm.nih.gov/articles/PMC12014715/]
- 69. Biomaterials as Implants in the Orthopedic Field for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10303232/]
- 70. implications for stress shielding of orthopaedic implants [https://pubmed.ncbi.nlm.nih.gov/34077904/]
- 71. Biomaterials for orthopedic applications and techniques to ... [https://link.springer.com/article/10.1007/s10853-023-08237-5]
- 72. Additively manufactured metal-matrix composites and their ... [https://pubs.rsc.org/en/content/articlehtml/2025/ma/d5ma00537j]
- 73. Recent Advances in the Corrosion and Protection of ... [https://www.mdpi.com/2075-4701/15/6/654]
- 74. Degradation technologies for condensation polymers ... [https://www.nature.com/articles/s41428-025-01069-x]
- 75. the importance of considering biotic and abiotic polymer ... [https://pubs.rsc.org/en/content/articlehtml/2025/em/d5em00079c]
- 76. Influence of different polymeric materials of implant and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11783779/]
- 77. Effect of low temperature on mechanical properties and ... [https://www.nature.com/articles/s41598-025-20220-5]
- 78. Metallic meta-biomaterials: A critical review of fatigue ... [https://www.sciencedirect.com/science/article/pii/S2468217923000540]
- 79. Fracture mechanics analysis of the fatigue strength curves ... [https://www.sciencedirect.com/science/article/abs/pii/S0167844225003519]
- 80. Fatigue response and fracture mechanisms of polymer ... [https://www.sciencedirect.com/science/article/abs/pii/S0263822325003721]
- 81. Mechanical Behavior of Polymeric Materials: Recent Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC11478764/]
- 82. Mechanical properties of composites reinforced with recycled ... [https://bioresources.cnr.ncsu.edu/resources/mechanical-properties-of-composites-reinforced-with-recycled-paper-and-pine-needles-using-polymer-matrices-containing-50-to-70-dammar-resin/]
- 83. Polymer Biomaterial Global Market Report 2025 [https://www.thebusinessresearchcompany.com/report/polymer-biomaterial-global-market-report]
- 84. An explainable data-driven framework for material processing [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.21203/rs.3.rs-7857002/v1]
- 85. Virginia Tech researchers develop new metallic materials ... [https://news.vt.edu/articles/2025/05/eng-che-researchers-develop-new-metallic-materials-using-data-driven-frameworks-and-AI.html]
- 86. AI system learns from many types of scientific information ... [https://news.mit.edu/2025/ai-system-learns-many-types-scientific-information-and-runs-experiments-discovering-new-materials-0925]
- 87. AI can transform innovation in materials design – here's how [https://www.weforum.org/stories/2025/06/ai-materials-innovation-discovery-to-design/]
- 88. Recent advances in polymeric materials with exceptional ... [https://pubs.rsc.org/en/content/articlehtml/2025/lp/d5lp00189g]
- 89. A polymer-like ultrahigh-strength metal alloy [https://www.nature.com/articles/s41586-024-07900-4]
- 90. Additive manufacturing of metallic and polymeric load ... [https://www.sciencedirect.com/science/article/abs/pii/S1005030221003972]
- 91. Comparative in vitro study on biomechanical behavior ... [https://www.medsci.org/v20p0639.htm]
- 92. Comprehensive review of Mg-based alloys: Mechanical, ... [https://www.sciencedirect.com/science/article/pii/S2238785425002157]
- 93. Radial force of coronary stents: a comparative analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/10348145/]
- 94. 2025 Guide: Drug-Eluting Coronary Stent Innovations ... [https://invamed.com/2025-guide-drug-eluting-coronary-stent-innovations-transforming-patient-outcomes/]
- 95. Factors Associated With Chronic Stent Recoil and its ... [https://pubmed.ncbi.nlm.nih.gov/40272344/]
- 96. COMPARISON OF FEMOROPOPLITEAL ARTERY STENTS UNDER AXIAL AND RADIAL COMPRESSION, AXIAL TENSION, BENDING, AND TORSION DEFORMATIONS - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5623954/]
- 97. Next-generation biodegradable cardiovascular stents [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578071/]
- 98. New Drug-Eluting Balloon May Be as Safe and Effective as ... [https://www.mountsinai.org/about/newsroom/2025/new-drug-eluting-balloon-may-be-as-safe-and-effective-as-conventional-metal-stents-for-repeat-percutaneous-coronary-interventions]
- 99. Nanocomposite Biomaterials for Tissue-Engineered Hernia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467858/]
- 100. 2025 Biomaterials Global Market Overview, 2021-2030 - [https://www.globenewswire.com/news-release/2025/02/27/3033608/28124/en/2025-Biomaterials-Global-Market-Overview-2021-2030-Collaborative-Research-and-Smart-Biomaterials-Drive-Industry-Growth.html]
- 101. Wear Characteristics of Metallic Biomaterials: A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC5455551/]
- 102. Fatigue behaviour of load-bearing polymeric bone scaffolds [https://pubmed.ncbi.nlm.nih.gov/37797705/]
- 103. Cost-Benefit Analysis: A Quick Guide with Examples and ... [https://www.projectmanager.com/blog/cost-benefit-analysis-for-projects-a-step-by-step-guide]
- 104. Cost-benefit assessment of manufacturing system using ... [https://www.sciencedirect.com/science/article/abs/pii/S0306261922000812]
- 105. Current developments and applications of smart polymers ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X24012827]
- 106. A new era for applications of multi-principal element alloys ... [https://www.sciencedirect.com/science/article/abs/pii/S2772950825000718]
- 107. Critical raw material-free multi-principal alloy design for a ... [https://www.nature.com/articles/s41598-025-87784-0]
- 108. Investigation and machine learning-based prediction of ... [https://www.nature.com/articles/s41598-025-18944-5]
- 109. a Novel Method to Enhance Data-driven Prediction of ... [https://arxiv.org/abs/2506.01994]