Comparative Analysis of Biomaterial-Based Drug Delivery Systems: Efficiency, Applications, and Future Directions
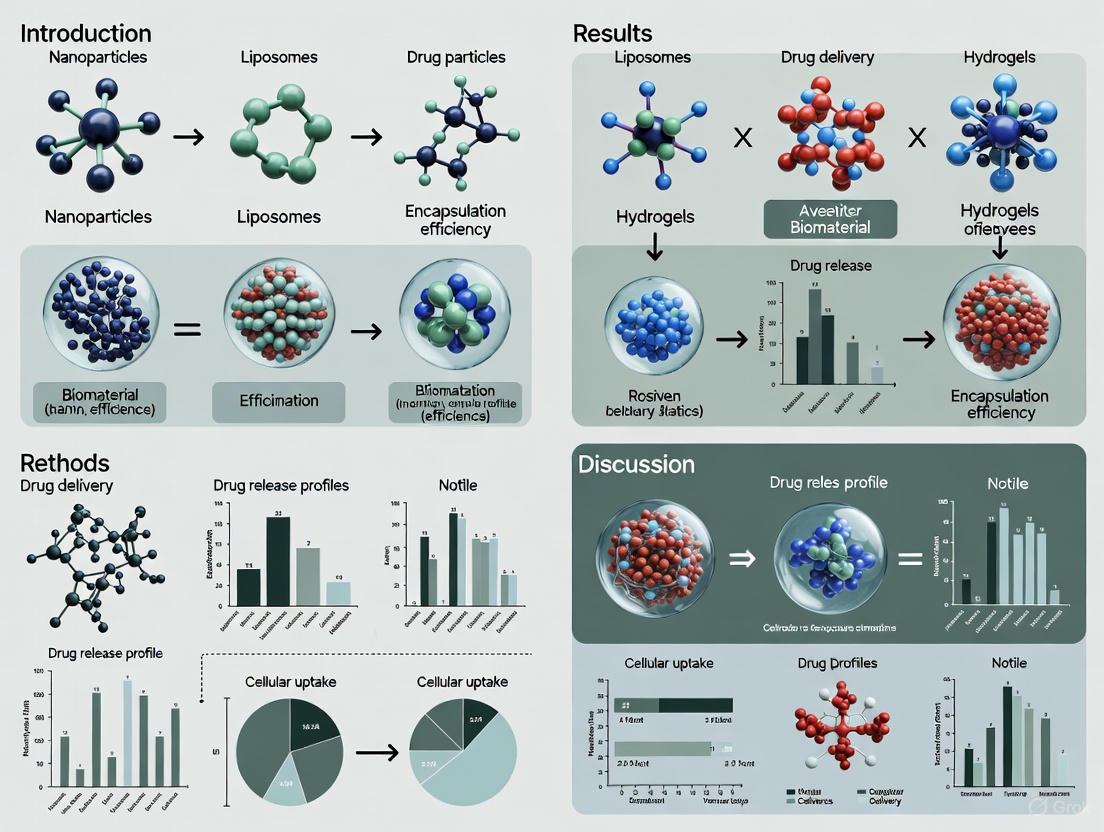
This article provides a comprehensive comparative analysis of the efficiency of various biomaterial-based drug delivery systems (DDS) for researchers and drug development professionals.
Comparative Analysis of Biomaterial-Based Drug Delivery Systems: Efficiency, Applications, and Future Directions
Abstract
This article provides a comprehensive comparative analysis of the efficiency of various biomaterial-based drug delivery systems (DDS) for researchers and drug development professionals. It explores the foundational principles of key biomaterial classes, including biobased nanomaterials, hydrogels, and biodegradable polymers. The analysis covers methodological advances in their application across diverse medical fields such as cancer therapy, CNS disorders, and regenerative medicine. The review systematically addresses major translational challenges, including scalability, biocompatibility, and overcoming biological barriers, while presenting optimization strategies. A quantitative comparison of system performance metrics—such as targeting precision, stability, controlled release, and patient compliance—offers a validated framework for material selection. By synthesizing current trends and data, this work aims to guide the development of next-generation, efficient, and clinically viable drug delivery platforms.
Biomaterials Unveiled: Exploring the Core Classes and Properties for Advanced Drug Delivery
The field of biomaterials has undergone a profound evolution, transitioning from simple, biocompatible passive structures to dynamic, intelligent systems capable of sophisticated interactions with biological environments. In modern pharmaceutical sciences, biomaterials are engineered substances designed to direct, through controlled interactions with biological systems, the therapeutic course of diagnostic or treatment regimens. This progression is largely driven by the limitations of conventional drug delivery, which often struggles with poor bioavailability, systemic toxicity, and an inability to target specific tissues effectively [1]. The contemporary definition of a biomaterial now encompasses a wide spectrum of substances—from naturally derived, sustainable polymers to synthetic, "smart" systems that respond to physiological stimuli. These advanced materials are foundational to creating targeted drug delivery systems that enhance therapeutic efficacy while minimizing adverse side effects, thereby revolutionizing the management of complex diseases such as cancer, diabetes, and neurological disorders [2] [1] [3]. This guide provides a comparative analysis of the performance of various biomaterial systems, underpinned by experimental data, to inform researchers and drug development professionals.
Comparative Analysis of Key Biomaterial Systems
The performance of drug delivery systems is critically dependent on the selection of biomaterials, which dictate properties such as drug release kinetics, targeting efficiency, and biocompatibility. The table below provides a structured comparison of three major classes of biomaterials used in advanced drug delivery applications.
Table 1: Comparative Analysis of Biomaterial Systems for Drug Delivery
| Biomaterial Class | Key Composition | Drug Loading & Release Mechanism | Targeting Efficiency & Key Findings | Reported Limitations |
|---|---|---|---|---|
| Polymeric Nanoparticles (PNPs) [4] | PLGA, Chitosan, Poly(lactic acid) | High drug loading capacity; Controlled release via polymer degradation and diffusion [4]. | Passive (EPR effect): High Active (with ligands): Enhanced→ Surface modification with PEG reduces non-specific tissue interaction; Ligands like antibodies enable specific tumor cell targeting [4]. | Potential toxicity of some polymers; Batch-to-batch consistency during scale-up; Regulatory hurdles for novel polymers [4] [1]. |
| Stimuli-Responsive Hydrogels [2] | Chitosan, PVA-CMC, PNIPAM | Fast-gelling at body temperature; Swelling/degradation or dynamic chemical bonds control release in response to pH, temperature, or enzymes [5] [2]. | Temporal/Spatial Control: High→ In a periodontitis model, a thermosensitive chitosan hydrogel provided a localized microenvironment for bone regeneration, reducing inflammatory cytokines (TNF-α, IL-6) and upregulating osteogenic markers (Collagen I, Runx2) [2]. | Limited mechanical strength for some applications; Response rate to stimuli can be slow; Potential for premature release. |
| Advanced Lipid & Polymeric Nanocarriers [6] [1] | Lipid Nanoparticles (LNPs), PLGA-RES, PO3Gn-b-PLA Triblock Copolymers | Encapsulation in lipid core or polymeric matrix; Release triggered by microenvironment (e.g., acidic pH) or external stimuli (e.g., NIR light) [6] [1]. | Tumor Targeting (e.g., with folate): Significant→ A bioinspired nano-prodrug (BiNp) with folic acid showed significant tumor-targeting and uptake, releasing active components in acidic tumor microenvironments to promote apoptosis [4]. → PLGA-RES nanocomposites significantly improved oocyte viability during cryopreservation by combating oxidative stress [2]. | Lipid-based systems may have stability issues; Immunogenicity concerns with PEG [7]; Complex manufacturing for some copolymer architectures. |
Experimental Protocols for Biomaterial Evaluation
To ensure the reliability and reproducibility of research in this field, standardized experimental protocols are essential. The following section details key methodologies for synthesizing and characterizing advanced biomaterial systems.
Synthesis of Bio-based Triblock Copolymer Nanoparticles
The development of sustainable and biocompatible polymers is a key research focus. The following protocol, adapted from Tinajero DÃaz et al., describes the synthesis of fully bio-based poly(lactide)-b-poly(1,3-trimethylene glycol)-b-poly(lactide) (PLA-b-PO3Gn-b-PLA) triblock copolymers, which are promising alternatives to PEG-based systems [7].
Table 2: Key Research Reagents for Triblock Copolymer Synthesis
| Reagent/Material | Function in the Experiment |
|---|---|
| Poly(trimethylene glycol) (PO3Gn) | Bio-based macroinitiator; forms the central, hydrophilic block of the copolymer, imparting "stealth" properties. |
| L-lactide or rac-lactide | Monomer; ring-opens to form the outer, hydrophobic polyester blocks (PLA) that influence crystallinity and degradation. |
| Stannous octoate (Sn(Oct)â‚‚ | Catalyst; accelerates the ring-opening polymerization of lactide. |
| Poly(vinyl alcohol) (PVA) | Stabilizer; used in the emulsion/solvent-evaporation method to form stable nanoparticles in water. |
| Dichloromethane (DCM) | Solvent; dissolves the copolymer for the nanoparticle self-assembly process. |
Detailed Workflow:
- Polymerization Setup: In a three-neck round-bottom flask equipped with a mechanical stirrer, nitrogen inlet, and vacuum outlet, combine the PO3Gn macroinitiator and L-lactide or rac-lactide at a predetermined molar feed ratio [7].
- Purging and Catalyst Addition: Purge the system with nitrogen. Heat the mixture to 120°C under vacuum for several minutes. Subsequently, increase the temperature to 180°C and add a catalytic amount of stannous octoate to initiate the ring-opening polymerization (ROP) [7].
- Bulk Polymerization: Allow the reaction to proceed under a nitrogen atmosphere at 180°C for a specified time until the desired molecular weight is achieved [7].
- Nanoparticle Formation via Self-Assembly: Purify the resulting PLA-b-PO3Gn-b-PLA triblock copolymer. Using the emulsion/solvent-evaporation method, dissolve the copolymer in dichloromethane. Emulsify this organic solution in an aqueous solution containing poly(vinyl alcohol) (PVA) as a stabilizer. Finally, evaporate the organic solvent to form solid, spherical nanoparticles with hydrodynamic diameters typically ranging from 95 to 158 nm [7].
Diagram 1: Triblock Copolymer Synthesis Workflow
Development and Testing of a Smart Theranostic System
The integration of diagnostics and therapy, known as theranostics, represents a frontier in personalized medicine. The following protocol is based on the work of Park et al., who developed a bifunctional tumor-targeting bioprobe [6].
Detailed Workflow:
- Bioprobe Fabrication: Synthesize or source a biocompatible nanoparticle core (e.g., gold nanorods, silica nanoparticles, or water-dispersible upconversion nanoparticles). Functionalize the nanoparticle surface with two key components: a) a tumor-targeting ligand (e.g., an antibody or peptide) for specific accumulation, and b) a combination of therapeutic and imaging agents, such as a photosensitizer for photodynamic therapy (PDT) and a near-infrared (NIR) fluorescent dye [6].
- In Vitro Validation: Incubate the bioprobe with target cancer cells and control cells. Use NIR fluorescence imaging to confirm specific cellular uptake and accumulation. Subsequently, apply a specific light stimulus (e.g., NIR laser) to activate the photosensitizer, generating reactive oxygen species (ROS) for photodynamic therapy and heat for photothermal therapy (PTT). Measure cell death to assess therapeutic efficacy [6].
- In Vivo Efficacy and Imaging: Administer the bioprobe to animal models with established tumors. Employ non-invasive NIR fluorescence imaging to track the bioprobe's biodistribution and real-time accumulation at the tumor site via the Enhanced Permeability and Retention (EPR) effect and active targeting. Apply targeted irradiation to trigger the therapeutic effects and monitor tumor regression over time. The system is designed for complete decomposition and clearance post-treatment [6].
Diagram 2: Smart Theranostic System Workflow
Emerging Trends and Future Perspectives
The next wave of innovation in biomaterials is being shaped by the convergence of materials science with digital technologies and a heightened focus on sustainability.
- AI-Driven Biomaterials Design: Artificial intelligence (AI) and machine learning (ML) are revolutionizing the development of new biomaterials. These technologies can analyze vast datasets to predict material properties, optimize nanoparticle design for specific drug release profiles, and even simulate nanoparticle degradation and interactions within the body. This significantly accelerates the discovery and optimization process, paving the way for highly personalized medicine approaches [4] [1] [8].
- Sustainable and Bio-based Polymers: The shift towards a circular economy is driving research into fully bio-based and biodegradable polymers. Examples include triblock copolymers of poly(lactide) and poly(trimethylene glycol) (derived from glucose fermentation), which serve as promising, potentially less immunogenic alternatives to conventional PEG in drug delivery formulations [7]. The use of natural extracts in hydrogels also aligns with this trend [2].
- Advanced Nanocarriers and Microrobots: The frontier of drug delivery is expanding to include sophisticated systems like magnetically propelled hydrogel microrobots for penetrating tumor sites [2] and exosome-based therapies that leverage the body's own intercellular communication systems for regenerative medicine [2]. The success of lipid nanoparticles (LNPs) in mRNA vaccine delivery has further validated the potential of nanocarriers for complex biologics [1].
The landscape of biomaterials for drug delivery is rich and diverse, spanning from sustainable biobased polymers to intelligently responsive smart systems. This comparative analysis demonstrates that while polymeric nanoparticles (PNPs) offer high versatility and drug loading capacity, stimuli-responsive hydrogels excel in providing localized and temporally controlled release. Meanwhile, advanced nanocarriers, including lipid nanoparticles and targeted theranostic probes, show unparalleled potential for precision delivery of complex therapeutics. The choice of biomaterial system is ultimately dictated by the specific therapeutic application, desired release profile, and targeting requirements. As the field advances, the integration of AI-driven design and a commitment to sustainable material sources will further empower researchers to develop next-generation, personalized drug delivery solutions that enhance therapeutic efficacy and patient outcomes.
In the evolving landscape of drug delivery and regenerative medicine, the selection of biomaterials—ranging from natural polymers like polysaccharides and proteins to synthetic polymeric carriers—is paramount for designing effective therapeutic systems. These materials form the foundational scaffold of nano-drug delivery systems (NDDS), influencing critical parameters such as biocompatibility, drug loading, release kinetics, and targeted delivery. Natural polymers, derived from biological sources, offer inherent biocompatibility and bioactivity, whereas synthetic polymers provide tunable mechanical properties and predictable degradation profiles. This comparative guide objectively analyzes the performance of these material classes, drawing on experimental data to inform researchers and drug development professionals. By examining their distinct advantages, limitations, and applications within a structured framework, this review aims to support the rational design of next-generation drug delivery platforms.
Comparative Analysis of Material Properties
The fundamental differences between natural and synthetic biomaterials directly influence their performance in drug delivery applications. The table below summarizes key properties based on experimental data.
Table 1: Comparative Properties of Natural and Synthetic Biomaterials for Drug Delivery
| Property | Natural Polysaccharides | Natural Proteins | Synthetic Polymers |
|---|---|---|---|
| Biocompatibility | Excellent; low toxicity and immunogenicity [9] | Excellent; high cell recognition [10] | Variable; can induce inflammatory responses [11] |
| Biodegradability | Enzymatically degradable; products are safe [9] | Highly biodegradable (e.g., collagen, silk) [10] | Tunable; but some by-products can be acidic (e.g., PLA, PLGA) [11] |
| Mechanical Strength | Generally moderate; often requires cross-linking [12] | Outstanding and diverse (e.g., high toughness in silk) [10] | Highly tunable and typically robust [11] [13] |
| Drug Loading Efficiency | High for various drugs; can be charge-dependent [12] | High; depends on protein structure and interactions [10] | High; can be engineered for specific drugs [4] |
| Release Kinetics | Can be responsive to pH, enzymes, or redox [9] | Can be controlled by cross-linking and degradation [10] | Predictable, diffusion-controlled release is common [11] |
| Targeting Capability | Inherent (e.g., lectin recognition by β-glucan) [14] | Can be functionalized with targeting ligands [10] | Requires surface functionalization (e.g., PEGylation, ligands) [4] |
| Cost & Scalability | Variable; sourcing and purification can be challenges [9] | Often high cost; batch-to-batch variability [10] | Good scalability and consistent quality [11] |
Experimental Data and Performance in Drug Delivery
Quantitative Formulation Screening Data
High-throughput screening of polysaccharide-based nanoparticles reveals how material selection impacts critical formulation parameters. The following table compiles experimental results from a combinatorial screen of cationic agents formulated with an anionic phosphorylated β-glucan (EEPG) framework for siRNA delivery [14].
Table 2: Experimental Screening Data for Polysaccharide-Based Nanoformulations [14]
| Cationic Material Category | Example Compounds | Optimal N/P Ratio for Formation | siRNA Encapsulation Efficiency (EE%) | Hydrodynamic Diameter (nm) |
|---|---|---|---|---|
| Cationic Polymers | Chitosan, Polyethyleneimine (PEI) | ~1/1 to 15/1 | 30-90% (PEI > Chitosan) | < 200 nm |
| Cationic Lipids | Lipid 2, Lipid 10 | < 0.04/1 to 15/1 | >80% (for Lipid 2/10 at N/P 15/1) | < 200 nm |
| Cell-Penetrating Peptides | K9, KALA, Penetratin | ~1/1 to 20/1 | >80% (at N/P 20/1) | < 200 nm |
| Small Molecules | Spermine | ~30/1 | >80% (comparable to PEI) | < 200 nm |
Experimental Drug Release Profiles
Comparative release studies using model drugs provide performance insights across different polymer classes. The data below summarizes findings from a study investigating ibuprofen (IBU) release from various polysaccharide-based hydrogels [12].
Table 3: Drug Release Kinetics of Ibuprofen from Polysaccharide Hydrogels [12]
| Hydrogel Type (Polymer) | Charge | Cumulative Release (%) | Release Kinetics Model | Key Influencing Factor |
|---|---|---|---|---|
| Sodium Carboxymethyl Cellulose (NaCMC) | Anionic | High | Fickian Diffusion | Swelling and electrostatic repulsion |
| Chitosan (CS) | Cationic | Low | Non-Fickian (Anomalous) transport | Electrostatic attraction to anionic drug |
| Tragacanth Gum (TRG) | Anionic | Moderate | Not Specified | Complex hetero-polysaccharide structure |
| Carrageenan (CRG) | Anionic | Moderate | Not Specified | Sulfated group interactions |
| Chitosan-Neutral Polymer Combination | Cationic/Neutral | Prolonged | Sustained Release | Modified diffusion path |
Detailed Experimental Protocols
High-Throughput Screening of Polysaccharide Nanoformulations
This protocol, adapted from a 2024 Nature Communications study, details a robotic-assisted screen for identifying optimal polysaccharide-based siRNA carriers [14].
- Primary Materials: Anionic polysaccharide (e.g., EEPG), diverse cationic compound library (polymers, lipids, peptides, small molecules), siRNA, microfluidics workstation, dynamic light scattering (DLS) instrument.
- Methodology:
- Solution Preparation: Prepare an aqueous solution of the anionic polysaccharide (EEPG) as the outer phase. Prepare solutions of cationic compounds in suitable buffers as the inner phase.
- Microfluidics-assisted Nanoprecipitation: Utilize a high-throughput microfluidics workstation with a co-flow device. Fix the flow conditions for the outer phase (EEPG). Systematically vary the flow rates of the inner phase (cationic compounds) to achieve a wide range of weight or N/P (Nitrogen/Phosphate) ratios.
- Automated Size and Formation Analysis: Direct the output from the microfluidic device to an integrated, automatic DLS system. Use the average derived counting rate (over 6000 kcps) as a primary indicator of successful nanoparticle formation. Record the hydrodynamic diameter and polydispersity index (PDI) for each formulation.
- siRNA Encapsulation Assay: For formulations with optimal physical characteristics (small size, PDI < 0.2), mix with siRNA at set N/P ratios (e.g., 15/1 and 20/1). Use a Ribogreen assay to quantify encapsulation efficiency (EE%). The fluorescent dye's signal is quenched upon encapsulation, allowing calculation of unencapsulated siRNA.
- Key Analysis: The optimal candidate, termed GluCARDIA, was identified through this screen and demonstrated efficient cardiac siRNA delivery in a murine model of myocardial ischemic/reperfusion injury [14].
Comparative Hydrogel Drug Release Kinetics
This standard protocol evaluates the drug release profiles from polymer-based hydrogels, as used in studies comparing polysaccharide excipients [12].
- Primary Materials: Polymer (e.g., Chitosan, NaCMC, Carrageenan), model drug (e.g., Ibuprofen), dissolution apparatus, Franz diffusion cells, HPLC system.
- Methodology:
- Hydrogel Preparation: Dissolve the polysaccharide in an appropriate solvent (e.g., aqueous acidic solution for chitosan). Incorporate the model drug uniformly into the polymer solution. Induce gelation via physical (e.g., pH change) or chemical (e.g., cross-linker) methods to form the drug-loaded hydrogel.
- In Vitro Release Study: Place a precise weight of the drug-loaded hydrogel in a receptor medium (e.g., phosphate buffer saline, PBS) under sink conditions. Maintain the system at a constant temperature (e.g., 37°C) with continuous agitation.
- Sample Collection and Analysis: At predetermined time intervals, withdraw aliquots from the receptor medium and replace with fresh medium to maintain sink conditions. Analyze the drug concentration in the aliquots using a validated analytical method (e.g., HPLC or UV-Vis spectrophotometry).
- Kinetic Modeling: Fit the cumulative drug release data to various mathematical models (e.g., Zero-order, First-order, Higuchi, Korsmeyer-Peppas) to determine the primary release mechanism.
- Key Analysis: The study found that cationic chitosan effectively prolonged the release of anionic ibuprofen, whereas anionic hydrogels like NaCMC showed higher, diffusion-driven release [12].
Visualization of Workflows and Mechanisms
High-Throughput Screening Workflow
The following diagram illustrates the automated, step-wise screening process for identifying optimal polysaccharide-based nanoformulations.
High-Throughput Screening Workflow for Optimal Nanoformulations
Mechanism of Targeted Drug Delivery
This diagram outlines the key mechanisms by which engineered polymeric carriers, particularly polysaccharide-based nanoparticles, achieve targeted drug delivery.
Mechanisms of Targeted Drug Delivery by Polymeric Carriers
The Scientist's Toolkit: Essential Research Reagents
This section details key materials and their functions for researchers developing and evaluating natural and synthetic polymeric carriers.
Table 4: Essential Reagents for Biomaterial-Based Drug Delivery Research
| Reagent / Material | Function in Research | Examples & Notes |
|---|---|---|
| Cationic Polysaccharides | Form polyelectrolyte complexes with nucleic acids; mucoadhesive properties. | Chitosan, Chitosan Oligomer (CS-O) [14] [12] |
| Anionic Polysaccharides | Ionic gelation framework; inherent targeting; responsive release. | Phosphorylated β-glucan (EEPG), Alginate, Hyaluronic Acid, NaCMC [9] [14] [12] |
| Cationic Lipids | Enhance encapsulation of anionic drugs/siRNA; improve cellular uptake. | Lipid 2, Lipid 10 (from combinatorial screens) [14] |
| Cell-Penetrating Peptides (CPPs) | Improve cellular internalization of nanoparticles. | K9, KALA, Penetratin, Transportan [14] |
| Cross-linkers | Stabilize hydrogels and nanoparticles; control degradation and release. | Genipin (natural), Glutaraldehyde, N,N'-Methylenebis(acrylamide) (MBA) [12] |
| Model Therapeutic Agents | For encapsulation and release studies. | Ibuprofen (small molecule), siRNA (genetic), Doxorubicin (chemotherapy) [14] [12] |
| Characterization Instruments | Determine size, charge, stability, and drug release profile. | Dynamic Light Scattering (DLS), HPLC, Franz Diffusion Cells [11] [14] [12] |
| Piperidine-3,3-diol | Piperidine-3,3-diol|High-Purity Research Chemical | Piperidine-3,3-diol is a versatile diol-substituted piperidine building block for pharmaceutical and organic synthesis. For Research Use Only. Not for human or veterinary use. |
| Lithium metagallate | Lithium metagallate, MF:GaLiO2, MW:108.7 g/mol | Chemical Reagent |
In the development of advanced drug delivery systems, the selection of biomaterials is governed by three critical performance metrics: biocompatibility, biodegradability, and functionalization. These properties collectively determine the safety, efficacy, and temporal control of therapeutic agent delivery. Biocompatibility ensures minimal adverse immune reactions and toxicity, biodegradability governs the rate of material breakdown and drug release kinetics, and functionalization enhances targeting capabilities and modulates interactions with biological systems. This guide provides a comparative analysis of prominent biomaterial systems, supported by experimental data and standardized testing methodologies, to inform rational material selection for specific therapeutic applications.
Comparative Analysis of Biocompatibility
Biocompatibility assessment evaluates the host response to a biomaterial, including its toxicity, immunogenicity, and potential to cause allergic reactions. Rigorous testing is required by regulatory bodies before clinical application [15] [16].
Quantitative Biocompatibility Metrics
Table 1: Standardized Biocompatibility and Toxicity Profiles of Selected Biomaterials
| Material | Test Model | Key Metrics | Results | Tolerated Dose/Concentration |
|---|---|---|---|---|
| Mesoporous Silica Nanoparticles (MSNs) [17] | Female nude mice (in vivo) | Serology, Hematology, Histopathology | No acute toxicity; Mild, transient elevation of liver enzymes (AST) at higher doses; No significant body weight change or histological lesions. | Up to 50 mg/kg (IV) |
| Polyethylene Glycol (PEG) [15] [16] | Immunoassay (in vitro) | Immunogenicity (Anti-PEG antibodies) | Presence of anti-PEG antibodies can alter nanocarrier biodistribution and trigger hypersensitivity. | Varies by formulation; immunogenicity is a key concern. |
| Polylactic Acid (PLA) [15] [16] | Cell culture & in vivo | Inflammatory response, Histocompatibility | Can provoke inflammatory reactions in vivo; modification with short-chain PEG enhances histocompatibility. | Dependent on application and modification. |
Experimental Protocols for Biocompatibility Assessment
- In Vivo Systemic Toxicity Profile (e.g., for MSNs) [17]:
- Administration: Intravenous injection of material suspended in saline via the tail vein in female nude mice. Doses are typically administered multiple times over a period (e.g., twice per week for 14 days).
- Monitoring: Daily observation for body weight change, visible signs of infection, ascites, grooming, and mobility. A Body Condition Scoring (BCS) system is used.
- Serological and Hematological Analysis: Blood collection at defined intervals (e.g., day 2 and day 14) for Complete Blood Count (CBC) and liver enzyme tests (AST, ALT).
- Histopathological Examination: Post-sacrifice, major organs (liver, spleen, kidney, heart, etc.) are harvested, sectioned, and examined for gross or pathological abnormalities.
- Immunogenicity Testing (e.g., for PEG) [15] [16]: Detection of pre-existing or induced antibodies via enzyme-linked immunosorbent assay (ELISA) or similar immunoassays. The impact on nanocarrier stability and biodistribution is assessed in relevant biological models.
Biocompatibility Assessment Workflow
Comparative Analysis of Biodegradability
Biodegradation involves the breakdown of materials into simpler substances through biological activity, primarily via hydrolysis or enzymatic action. The degradation rate is a crucial parameter for controlling drug release profiles [15].
Mechanisms and Kinetics of Biodegradation
Table 2: Biodegradation Mechanisms and Influencing Factors for Common Polymers
| Polymer | Primary Degradation Mechanism | Key Influencing Factors | Rate Modulation Example |
|---|---|---|---|
| Polylactic Acid (PLA) [15] | Hydrolysis of ester bonds | Temperature, Humidity, Catalysts | Hydrolysis rate increased by 30-50% with a 50°C temperature rise under >90% humidity. |
| Starch-based Polymers [15] | Enzymatic cleavage of α-1,4-glycosidic linkages | Enzymes (α-amylase, β-glucosidase), Temperature, Humidity | Degradation rate accelerates when temperature rises from 30°C to 50°C at >80% humidity. |
| Polycaprolactone (PCL) [18] | Hydrolytic cleavage of ester bonds | Crystallinity, Implant Environment, Blending | Blending with PLA in 3D printed scaffolds tailors degradation rate and flexibility [15]. |
Experimental Protocols for Degradation Profiling
- In Vitro Hydrolytic Degradation [15]:
- Sample Immersion: Incubate pre-weighed polymer samples (e.g., films, scaffolds) in phosphate-buffered saline (PBS) at a specific pH (e.g., 7.4) and temperature (commonly 37°C).
- Mass Loss Monitoring: At predetermined time points, remove samples, dry them thoroughly, and measure the mass loss. The percentage of mass loss is calculated as (Initial Dry Mass - Current Dry Mass) / Initial Dry Mass × 100.
- Media Analysis: Analyze the immersion media for degradation byproducts using techniques like Gel Permeation Chromatography (GPC) to track changes in molecular weight.
- Enzymatic Degradation Assay [15]:
- Solution Preparation: Prepare a buffer solution containing a specific, purified enzyme relevant to the polymer (e.g., lipase for PCL, proteinase K for PLA).
- Incubation and Sampling: Incubate the polymer sample in the enzyme solution under controlled conditions (e.g., 37°C). Monitor mass loss or molecular weight change over time as in the hydrolytic test.
- Kinetics Analysis: Compare the degradation rate against a control sample (without enzyme) to quantify the enzymatic contribution.
Biodegradation Pathways and Modulation
Comparative Analysis of Surface Functionalization
Surface functionalization enhances the bioactivity, targeting, and interfacial properties of biomaterials. It is particularly vital for synthetic polymers like PCL, which are inherently bioinert [18].
Performance of Functionalization Techniques
Table 3: Comparison of Surface Functionalization Methods for Polycaprolactone (PCL) Scaffolds
| Functionalization Method | Target Material/Application | Key Experimental Findings | Impact on Performance |
|---|---|---|---|
| TiCaPCON Coating (Magnetron Sputtering) [18] | PCL for Bone Tissue Regeneration | Enhanced MC3T3-E1 osteoblast cell adhesion/proliferation; Promoted formation of Ca-based mineralized layer in Simulated Body Fluid (SBF). | Induces bioactivity, improves bone regeneration potential. |
| COOH Plasma Polymerization [18] | PCL for Skin Repair | Improved IAR-2 epithelial cell adhesion and proliferation. | Enhances hydrophilicity and cytocompatibility for soft tissue applications. |
| PEGylation (Short-chain PEG) [15] [16] | PLA-based Microspheres | Reduced inflammatory reaction in vivo; Enhanced histocompatibility. | Improves stealth properties, reduces immune recognition. |
Experimental Protocols for Functionalization and Bioactivity Testing
- Atmospheric Pressure Plasma Copolymerization for COOH Groups [18]:
- Setup: Place electrospun PCL nanofibers in a plasma reactor.
- Process: Introduce precursor gases, typically COâ‚‚ and Câ‚‚Hâ‚„, into the chamber. Apply atmospheric pressure plasma to initiate copolymerization.
- Result: A thin, COOH-rich polymer layer is deposited on the PCL surface, increasing hydrophilicity.
- Magnetron Sputtering of TiCaPCON Film [18]:
- Target: Use a composite TiC–CaO–Ti₃POₓ target.
- Deposition: Place PCL scaffolds in a magnetron sputtering system (e.g., "UNICOAT 900"). Sputter the target in an atmosphere of Ar and Nâ‚‚ gases (e.g., 250 sccm Ar, 25 sccm Nâ‚‚) at an accelerating voltage of 450 V for a set duration (e.g., 10 min).
- In Vitro Bioactivity Assessment via SBF Immersion [18]:
- SBF Preparation: Prepare simulated body fluid (1× SBF) with ion concentrations nearly equal to human blood plasma.
- Immersion: Immerse the functionalized scaffolds in SBF at 37°C for a prolonged period (e.g., 21 days).
- Analysis: Post-immersion, characterize the scaffold surface using Scanning Electron Microscopy (SEM) and Fourier Transform Infrared (FTIR) spectroscopy to detect the formation of a calcium phosphate (apatite) layer, indicative of bioactivity.
Surface Functionalization and Evaluation Workflow
The Scientist's Toolkit: Essential Reagents and Materials
This section details key reagents, materials, and instruments essential for the experimental work discussed in this guide.
Table 4: Essential Research Reagents and Materials for Biomaterial Performance Evaluation
| Item Name | Function/Application | Specific Example / Note |
|---|---|---|
| Simulated Body Fluid (SBF) [18] | In vitro assessment of bioactivity and biomineralization potential. | Solution with ion concentration similar to human blood plasma. |
| Electrospinning Apparatus [18] | Fabrication of polymer nanofiber scaffolds that mimic the extracellular matrix. | e.g., Nanospider NSLAB 500. |
| Magnetron Sputtering System [18] | Deposition of thin, uniform, and adhesive bioactive coatings on polymers. | e.g., "UNICOAT 900" for TiCaPCON coating. |
| Differential Scanning Calorimetry (DSC) [15] [16] | Characterization of thermal properties of polymers (e.g., glass transition, melting point). | Informs processing conditions and stability. |
| Thermogravimetric Analysis (TGA) [15] [16] | Measurement of thermal stability and decomposition profile of materials. | |
| Enzymes (e.g., Lipases, Proteases) [15] | Study of enzymatic degradation pathways of biodegradable polymers. | Enzyme type selected based on polymer chemistry. |
| Cell Lines (e.g., MC3T3-E1, IAR-2) [18] | In vitro cytocompatibility and cell-material interaction studies. | MC3T3-E1 (osteoblasts), IAR-2 (epithelial cells). |
| Composite Sputtering Target (TiC–CaO–Ti₃POₓ) [18] | Source for depositing TiCaPCON bioactive films via magnetron sputtering. | Produced by self-propagating high-temperature synthesis. |
| Precursor Gases (COâ‚‚, Câ‚‚Hâ‚„) [18] | Used in plasma copolymerization to create COOH-rich functional surfaces. | |
| Anthra[2,3-b]thiophene | Anthra[2,3-b]thiophene, CAS:22108-55-0, MF:C16H10S, MW:234.3 g/mol | Chemical Reagent |
| 6-Hexadecenoic acid | 6-Hexadecenoic acid, MF:C16H30O2, MW:254.41 g/mol | Chemical Reagent |
The field of controlled drug delivery has undergone a revolutionary transformation, evolving from simple sustained-release formulations to sophisticated, intelligently targeted systems. This evolution represents a paradigm shift from one-size-fits-all release kinetics to precision medicine approaches that deliver therapeutics with spatial and temporal control. At the forefront of this transformation are poly(lactic-co-glycolic acid) (PLGA) based systems, which have served as the foundational backbone for controlled release technologies, and stimuli-responsive platforms that represent the next generation of intelligent drug delivery.
Traditional PLGA systems have demonstrated remarkable success by providing predictable, tunable drug release profiles through biodegradation kinetics. These systems leverage the well-understood hydrolysis of ester linkages in the PLGA backbone to release encapsulated therapeutics over periods ranging from days to months. The durability of PLGA as a drug delivery vehicle stems from its excellent biocompatibility, predictable erosion rates, and regulatory acceptance. However, the inherent passive diffusion mechanism and degradation-controlled release lack the responsiveness to dynamic physiological environments required for optimal therapeutic outcomes in complex disease states.
Stimuli-responsive platforms have emerged to address this critical limitation, integrating smart materials capable of sensing and responding to specific pathological triggers. These advanced systems bridge the gap between conventional sustained release and active pathological targeting, offering enhanced precision through both endogenous and exogenous activation mechanisms. The integration of PLGA with these responsive elements has created a new class of hybrid systems that merge the proven safety and controlled release properties of PLGA with the targeted activation capabilities of stimuli-responsive technologies.
This comparative analysis examines the technological evolution from conventional PLGA systems to advanced stimuli-responsive platforms, providing researchers with a systematic evaluation of their respective drug delivery efficiencies, experimental methodologies, and performance characteristics across key pharmaceutical metrics.
Material Foundations and System Architectures
PLGA-Based Controlled Release Systems
Poly(lactic-co-glycolic acid) (PLGA) has established itself as one of the most extensively utilized biodegradable polymers in controlled drug delivery, primarily due to its tunable physicochemical properties and excellent safety profile. The degradation mechanism of PLGA occurs through hydrolysis of ester bonds in an aqueous environment, generating lactic acid and glycolic acid as metabolic byproducts that enter the Krebs cycle and are eventually eliminated as carbon dioxide and water [19]. This biodegradation pathway minimizes systemic toxicity and underpins the regulatory acceptance of PLGA for numerous pharmaceutical applications.
The drug release profile from PLGA systems is governed by a complex interplay of polymer characteristics, including molecular weight, lactide-to-glycolide (L:G) ratio, blockiness, and end-group functionality. These parameters collectively influence hydration rates, degradation kinetics, and consequently, release duration. Specifically, higher molecular weight PLGA, increased lactide content, and ester end caps correlate with prolonged degradation times and extended release profiles [19]. This tunability has enabled the development of PLGA-based formulations spanning various administration routes, including injectable microspheres, implants, and nanoparticles.
The fabrication of PLGA nanoparticles typically employs emulsion-solvent evaporation, nanoprecipitation, or double-emulsion methods, with the selection dependent on the hydrophilicity or hydrophobicity of the encapsulated therapeutic. The double-emulsion technique (w/o/w) has proven particularly effective for hydrophilic compounds, allowing for high encapsulation efficiency through the formation of aqueous compartments within the polymeric matrix [20]. These methodological innovations have positioned PLGA as a versatile platform for delivering diverse therapeutic agents, including small molecules, proteins, peptides, and nucleic acids.
Stimuli-Responsive Platform Designs
Stimuli-responsive drug delivery systems represent a sophisticated advancement beyond conventional PLGA platforms, incorporating materials capable of sensing and responding to specific pathological cues or external triggers. These systems are broadly categorized as endogenous or exogenous responsive platforms, with some advanced architectures capable of responding to multiple stimuli simultaneously.
Endogenous stimuli-responsive systems leverage pathological abnormalities in the disease microenvironment, such as decreased pH, elevated reactive oxygen species (ROS), overexpression of specific enzymes, or redox potential gradients. For instance, pH-responsive systems exploit the acidic tumor microenvironment (pH ~6.5-7.0) or endosomal compartments (pH ~5.0-6.0) to trigger drug release through acid-labile bond cleavage or protonation-induced structural changes [21] [22]. Similarly, enzyme-responsive systems utilize pathological overexpression of matrix metalloproteinases (MMPs), hyaluronidases, or proteases to degrade specific peptide sequences or polysaccharide components, thereby releasing therapeutic payloads at the target site.
Exogenous stimuli-responsive systems respond to externally applied triggers such as magnetic fields, light, or ultrasound, offering precise spatiotemporal control over drug release. Magnetic-responsive platforms typically incorporate superparamagnetic iron oxide nanoparticles (e.g., maghemite, γ-Fe₂O₃) that generate localized heat under alternating magnetic fields, simultaneously enabling hyperthermia therapy and triggering drug release from thermosensitive carriers [21]. Light-responsive systems employ photosensitizers or gold nanoparticles that convert light energy to thermal energy or reactive oxygen species, while ultrasound-responsive systems utilize microbubbles or nanodroplets that cavitate upon ultrasonic exposure, disrupting carrier integrity and releasing encapsulated drugs.
Multi-stimuli responsive platforms represent the cutting edge of intelligent drug delivery, integrating responsiveness to multiple triggers for enhanced specificity. A notable example is the (maghemite/PLGA)/chitosan nanostructure that responds to pH, heat, and magnetic stimuli simultaneously [21]. In this tri-stimuli responsive system, the PLGA matrix provides pH-sensitive degradation through acid-accelerated hydrolysis, the embedded maghemite nanoparticles enable magnetic hyperthermia under external fields, and the chitosan shell offers additional pH-dependent solubility changes. This multi-functionality creates a sophisticated feedback system where drug release rates can be precisely modulated through combinatorial stimulation.
Table 1: Classification of Stimuli-Responsive Drug Delivery Platforms
| Stimulus Category | Specific Triggers | Responsive Mechanisms | Typical Applications |
|---|---|---|---|
| Endogenous (Internal) | pH (acidic tumor microenvironment, ~5.0-6.5) | Protonation of polyelectrolytes, acid-labile bond cleavage, polymer swelling | Tumor-targeted chemotherapy, inflammatory disease treatment |
| Redox potential (elevated glutathione in cancer cells) | Disulfide bond cleavage in high glutathione environments | Intracellular drug delivery to tumor cells | |
| Enzymes (MMPs, hyaluronidases, proteases) | Enzyme-specific substrate degradation | Tumor microenvironment-targeted release, inflammatory sites | |
| Reactive oxygen species (elevated Hâ‚‚Oâ‚‚ in inflammation) | Oxidation-sensitive bond cleavage (thioether, selenide) | Inflammatory diseases, cancer therapy | |
| Exogenous (External) | Magnetic fields | Hyperthermia from superparamagnetic nanoparticles, particle alignment | Deep-tumor targeting, combined hyperthermia-chemotherapy |
| Light (UV, visible, NIR) | Photothermal conversion, photoisomerization, photocleavage | Superficial and deep-tumor treatment (with NIR) | |
| Ultrasound | Cavitation-induced carrier disruption, thermal effects | Deep-tissue applications, blood-brain barrier opening | |
| Temperature | Polymer phase transition (e.g., LCST of thermosensitive polymers) | Localized hyperthermia-triggered release |
Comparative Performance Analysis
Quantitative Metrics of Drug Delivery Efficiency
Direct comparison of conventional PLGA systems and stimuli-responsive platforms reveals significant differences in key performance metrics, including drug loading capacity, encapsulation efficiency, release kinetics, and targeting precision. The following structured analysis synthesizes experimental data from multiple studies to provide researchers with a comprehensive efficiency assessment.
Table 2: Performance Comparison of PLGA vs. Stimuli-Responsive Platforms
| Performance Parameter | Conventional PLGA Systems | Stimuli-Responsive Platforms | Experimental Context |
|---|---|---|---|
| Drug Loading Capacity (%) | 5-15% (small molecules) [19] | 10-25% (small molecules) [21] | Cisplatin loading: PLGA (≤15%) vs. (γ-Fe₂O₃/PLGA)/CS (~15%) |
| Encapsulation Efficiency (%) | 50-80% (variable by method) [23] | 70-95% (enhanced with responsive elements) [21] | Double emulsion methods with magnetic incorporation |
| Release Duration | Days to months (tunable via polymer properties) [19] | Hours to weeks (stimulus-dependent) [21] | Programmable release profiles with on-demand bursts |
| Burst Release (Initial 24h) | 15-40% (significant in many formulations) [19] | 5-20% (reduced with chitosan coating) [21] | Chitosan shell as diffusion barrier in (γ-Fe₂O₃/PLGA)/CS |
| Release Rate Modulation | 1.5-2.5 fold (via polymer composition) [19] | Up to 4.7-fold with dual stimuli [21] | pH 5.0 + 45°C vs. pH 7.4 + 37°C in (γ-Fe₂O₃/PLGA)/CS |
| Targeting Specificity | Passive (EPR effect primarily) [20] | Active (pathological microenvironment response) [21] [24] | Magnetic guidance + pH responsiveness in tumor models |
| Therapeutic Efficacy (ICâ‚…â‚€) | Varies with drug potency | ~1.6-fold improvement vs. free drug [21] | Cisplatin against A-549 human lung adenocarcinoma cells |
The data reveal that stimuli-responsive platforms significantly outperform conventional PLGA systems in several key metrics. Most notably, the release rate modulation capability of stimuli-responsive systems demonstrates a substantial advantage, with dual pH- and temperature-responsive systems achieving up to 4.7-fold faster release under trigger conditions compared to physiological conditions [21]. This controlled release enhancement directly translates to improved therapeutic efficacy, as evidenced by the 1.6-fold lower ICâ‚…â‚€ value of cisplatin-loaded (maghemite/PLGA)/chitosan nanoparticles compared to free cisplatin against human lung adenocarcinoma cells [21].
Additionally, stimuli-responsive platforms address the persistent challenge of initial burst release common in conventional PLGA systems. The incorporation of functional barriers, such as chitosan shells in (maghemite/PLGA)/chitosan nanostructures, effectively mitigates this issue by creating an additional diffusion barrier that minimizes premature drug release during the initial exposure period [21]. This controlled initial release profile contributes to reduced systemic toxicity and enhanced accumulation at the target site.
Experimental Models and Methodologies
The evaluation of drug delivery system efficiency employs standardized in vitro and in vivo models to assess release kinetics, targeting accuracy, and therapeutic outcomes. The following experimental protocols represent methodologies commonly cited in the literature for both PLGA and stimuli-responsive platforms.
In Vitro Release Kinetics Protocol:
- Media Conditions: Phosphate-buffered saline (PBS) at varying pH (7.4 simulating physiological conditions, 5.0-6.5 simulating pathological environments) and temperatures (37°C vs. 45°C for hyperthermia conditions) [21]
- Sample Collection: Aliquots withdrawn at predetermined time points (0.5, 1, 2, 4, 8, 12, 24, 48, 72, 96 hours) with media replacement to maintain sink conditions
- Analysis Method: UV spectrophotometry at wavelength specific to drug absorbance maximum (e.g., 301 nm for cisplatin) [21]
- Additional Stimuli Application: For magnetic-responsive systems, alternating magnetic field (AMF) application (e.g., 100-400 kHz for 10-30 minutes at specific intervals) to trigger release [21]
Cellular Uptake and Cytotoxicity Assessment:
- Cell Lines: Human cancer cell lines (e.g., A-549 lung adenocarcinoma, T-84 colon carcinoma) and normal fibroblast lines (e.g., CCD-18 colon fibroblasts) for selectivity evaluation [21]
- Incubation Conditions: 24-72 hour exposure to nanoparticle formulations at equivalent drug concentrations
- Viability Assay: MTT or similar colorimetric assay measuring mitochondrial activity of treated cells versus untreated controls
- Internalization Analysis: Flow cytometry or fluorescence microscopy for fluorescently labeled nanoparticles
Hemocompatibility Testing:
- Protocol: Incubation of nanoparticle formulations with human blood samples (typically 1:9 ratio of nanoparticles to blood)
- Parameters: Hemolysis percentage, platelet activation, and complement system activation assessment
- Acceptance Criteria: <5% hemolysis generally considered compatible for intravenous administration [21]
The experimental workflow for evaluating stimuli-responsive systems incorporates additional validation steps for stimulus-specific responses, including pre- and post-stimulus release rate comparisons and imaging-guided localization assessment. These methodologies provide comprehensive data on both the baseline performance and activated response of advanced delivery platforms.
Diagram 1: Experimental workflow for evaluating drug delivery system performance, incorporating both standard characterization and stimulus-specific validation steps.
Advanced Applications and Theranostic Integration
Disease-Specific Implementation
The transition from conventional PLGA to stimuli-responsive platforms has enabled significant advances in disease-specific therapeutic applications, particularly in oncology, inflammatory disorders, and neurological conditions where targeted delivery is critical for efficacy and safety.
In oncology, stimuli-responsive platforms demonstrate superior performance in exploiting pathological hallmarks of the tumor microenvironment. The (maghemite/PLGA)/chitosan system exemplifies this approach, leveraging the acidic pH of tumors combined with externally applied magnetic fields to achieve spatially and temporally controlled drug release [21]. This dual-responsive behavior enables precise drug deployment at the target site while minimizing systemic exposure. Similarly, redox-responsive systems capitalize on the elevated glutathione concentrations in cancer cells (approximately 100-1000 times higher than extracellular levels) to trigger intracellular drug release through disulfide bond cleavage [24] [25].
For inflammatory bowel disease (IBD), pH- and enzyme-responsive nanomaterials have shown remarkable efficacy in achieving colon-specific drug delivery. These systems remain stable during transit through the upper gastrointestinal tract but selectively release their payload upon encountering the inflamed colonic microenvironment characterized by altered pH, elevated reactive oxygen species, and overexpression of specific enzymes [22]. This targeted approach enhances therapeutic efficacy while reducing systemic side effects common with conventional oral IBD treatments.
In neurological applications, the challenge of crossing the blood-brain barrier (BBB) has prompted the development of multifunctional PLGA-based nanoparticles that incorporate targeting ligands for receptor-mediated transcytosis. While still an area of active research, these systems show promise for enhancing drug delivery to central nervous system tumors by leveraging both passive and active targeting strategies [26] [20].
Theranostic Integration and Clinical Translation
The integration of therapeutic and diagnostic capabilities (theranostics) represents a significant advancement in stimuli-responsive platforms, enabling simultaneous treatment and monitoring of disease response. PLGA-based theranostic nanoparticles exemplify this approach by incorporating both therapeutic agents and imaging contrast materials (e.g., superparamagnetic iron oxide nanoparticles for MRI, fluorescent dyes for optical imaging) within a single platform [20].
These sophisticated systems allow researchers and clinicians to track nanoparticle distribution, monitor accumulation at target sites, visualize trigger activation, and assess therapeutic response in real-time. For instance, SPION (superparamagnetic iron oxide nanoparticle)-tagged macrophages have demonstrated utility as both therapeutic carriers and MRI contrast agents for hepatic tumor imaging [24]. Similarly, PLGA-PEG nanoparticles encapsulating doxorubicin and SPIONs have shown superior cytotoxicity against cancer cells while enabling dual-mode MRI-fluorescence imaging [20].
The clinical translation pathway for these advanced systems involves rigorous evaluation of biocompatibility, biodegradation, and manufacturing reproducibility. PLGA maintains an advantage in this regard due to its established regulatory approval history and well-characterized safety profile. However, emerging stimuli-responsive platforms incorporating novel materials face additional regulatory hurdles requiring comprehensive assessment of potential long-term toxicity, particularly for non-degradable components [26] [20].
Table 3: Research Reagent Solutions for Drug Delivery System Development
| Reagent/Chemical | Function in Formulation | Application Context |
|---|---|---|
| PLGA (50:50 to 85:15 L:G ratio) | Biodegradable polymer matrix providing controlled release kinetics | Core material for nanoparticle fabrication across all system types |
| Chitosan | Positively charged polysaccharide for surface functionalization | pH-responsive shell, mucoadhesive properties in (γ-Fe₂O₃/PLGA)/CS [21] |
| Maghemite (γ-Fe₂O₃) | Superparamagnetic iron oxide for hyperthermia and MRI contrast | Magnetic responsiveness in tri-stimuli systems [21] |
| Polyvinyl Alcohol (PVA) | Surfactant for emulsion stabilization during nanoparticle synthesis | Prevents aggregation in emulsion-based fabrication methods [19] [20] |
| Dichloromethane (DCM) | Organic solvent for PLGA dissolution in emulsion methods | Solvent for oil phase in single/double emulsion techniques [20] |
| Tin(II) bis(2-ethylhexanoate) [Sn(Oct)â‚‚] | Catalyst for ring-opening polymerization of PLGA | Synthesis of PLGA with specific molecular weights and end groups [19] |
| Glutathione | Reducing agent for evaluating redox-responsive systems | Simulating intracellular conditions for disulfide cleavage testing [24] |
| Matrix Metalloproteinases (MMPs) | Proteolytic enzymes for enzyme-responsive system validation | Testing substrate cleavage in disease-mimicking environments [24] |
Future Perspectives and Research Directions
The evolution from PLGA to stimuli-responsive platforms continues to advance with several emerging trends shaping the future of controlled drug delivery. Integration of artificial intelligence and machine learning in nanoparticle design is accelerating the optimization of formulation parameters, potentially reducing the traditional trial-and-error approach to development [23]. The growing availability of comprehensive datasets documenting PLGA nanoparticle formulations provides valuable resources for data-driven design and predictive modeling [23].
Multi-stimuli responsive systems represent another frontier, with research increasingly focused on platforms capable of responding to three or more distinct triggers for enhanced specificity. These systems aim to create sophisticated logic-gated release mechanisms that activate only when multiple disease biomarkers are present simultaneously, thereby minimizing off-target effects [21] [22].
Cell-mediated delivery approaches incorporating stimuli-responsive elements show particular promise for overcoming biological barriers. The use of erythrocytes, immune cells, stem cells, and exosomes as delivery vectors, combined with responsive release mechanisms, creates hybrid systems that leverage both biological targeting and engineered control [24]. For example, macrophage-mediated delivery of doxorubicin-loaded liposomes has demonstrated enhanced accumulation in triple-negative breast cancer models, while SPION-tagged macrophages enable MRI-guided delivery and imaging in hepatic tumors [24].
Despite these advancements, significant challenges remain in scaling up manufacturing processes, ensuring long-term stability, and addressing regulatory requirements for complex combination products. The transition from laboratory-scale synthesis to Good Manufacturing Practice (GMP) production presents particular hurdles for stimuli-responsive systems incorporating multiple functional components [26] [20]. Nevertheless, the continued convergence of materials science, pharmaceutical technology, and biological understanding promises to address these challenges and further advance the evolution of controlled release systems.
Diagram 2: Future research directions and technological convergence in advanced drug delivery systems, highlighting the multidisciplinary approach required for continued innovation.
The evolution from conventional PLGA systems to stimuli-responsive platforms represents a significant paradigm shift in controlled drug delivery, moving from passive sustained release to actively targeted, intelligence-based therapeutic deployment. While PLGA continues to provide a valuable foundation with its proven biocompatibility, tunable release kinetics, and regulatory acceptance, stimuli-responsive systems offer unprecedented precision through their ability to sense and respond to pathological cues.
The comparative analysis presented herein demonstrates that stimuli-responsive platforms consistently outperform conventional PLGA systems across multiple efficiency metrics, including drug release modulation, targeting specificity, and therapeutic efficacy. The experimental data confirm that multi-stimuli responsive systems, particularly those incorporating both endogenous and exogenous triggers, achieve superior control over spatiotemporal drug release profiles. These advanced platforms successfully address longstanding challenges in drug delivery, including premature release, off-target accumulation, and inadequate therapeutic concentrations at disease sites.
As the field continues to evolve, the integration of smart materials, biological targeting mechanisms, and diagnostic capabilities will further blur the boundaries between drug delivery systems and precision medicine tools. The ongoing convergence of materials science, pharmaceutical technology, and biological understanding promises to yield increasingly sophisticated platforms capable of adapting to dynamic disease states and patient-specific physiological conditions. This progression from simple controlled release to intelligently responsive therapeutic deployment ultimately heralds a new era in pharmaceutical technology, one characterized by enhanced efficacy, reduced side effects, and truly personalized treatment approaches.
From Bench to Bedside: Application Strategies and Material Innovations in Targeted Therapies
The evolution of nanomedicine has ushered in a new era for targeted drug delivery, particularly in treating challenging diseases like cancer and central nervous system (CNS) disorders. Among the most promising nanocarriers, lipid-based and polymeric nanoparticles have demonstrated exceptional capabilities in enhancing therapeutic efficacy while reducing systemic toxicity. These biomaterial systems address fundamental drug delivery challenges, including poor bioavailability, nonspecific biodistribution, and inability to cross biological barriers such as the blood-brain barrier (BBB). This comprehensive guide provides a comparative analysis of lipid and polymeric nanoparticle platforms, examining their distinct characteristics, performance metrics, and applications through synthesized experimental data and standardized methodologies to inform rational design choices for researchers and drug development professionals.
Comparative Structural and Functional Characteristics
Table 1: Fundamental Properties of Lipid and Polymeric Nanoparticles
| Property | Lipid Nanoparticles | Polymeric Nanoparticles |
|---|---|---|
| Typical Composition | Ionizable lipids, phospholipids, cholesterol, PEG-lipids [27] | PLGA, chitosan, PLA, gelatin, dendrimers [28] |
| Common Size Range | 5-200 nm [29] | 10-200 nm [28] |
| Structure Type | Amorphous or non-bilayer core-shell [27] | Nanospheres (matrix) or nanocapsules (reservoir) [28] |
| Drug Encapsulation | Hydrophilic & hydrophobic agents, nucleic acids [27] | Small molecules, proteins, nucleic acids [28] [30] |
| Surface Modification | PEG-lipids, targeting ligands [27] | PEG, antibodies, peptides, folates [28] [30] |
| Release Mechanism | pH-responsive, endosomal escape [27] | Controlled diffusion, polymer erosion, stimuli-responsive [28] [30] |
| Key Advantages | Biocompatibility, clinical validation for RNA delivery [27] | Versatile design, controlled release profiles, high stability [28] |
| Primary Limitations | Potential immunogenicity, limited drug loading for some compounds [27] | Complexity in reproducibility, polymer-specific toxicity concerns [28] |
CNS Drug Delivery Applications and Performance
Blood-Brain Barrier Penetration Mechanisms
The blood-brain barrier represents the fundamental challenge for CNS drug delivery, with its tight junctions, selective permeability, and active efflux mechanisms restricting over 98% of small-molecule drugs and nearly all large-molecule therapeutics [29] [31]. Both lipid and polymeric nanoparticles have demonstrated capabilities to overcome this barrier through multiple mechanisms:
Receptor-mediated transcytosis: Nanoparticles functionalized with targeting ligands (antibodies, peptides, transferrin) engage specific receptors on BBB endothelial cells to initiate vesicular transport into the brain parenchyma [29].
Cell-mediated transport: Some nanoparticle systems are taken up by immune cells like monocytes or macrophages, which subsequently carry them across the BBB in a "Trojan horse" approach [29].
Direct translocation: Certain surface-modified nanoparticles can temporarily disrupt tight junctions or fuse with cell membranes to facilitate paracellular or transcellular transport [29].
Intranasal delivery: Both lipid and polymeric nanoparticles can bypass the BBB completely when administered intranasally, traveling along olfactory and trigeminal nerve pathways directly to the CNS [31].
Figure 1: BBB Penetration Pathways for Lipid and Polymeric Nanoparticles
Quantitative Performance in CNS Delivery
Table 2: CNS Therapeutic Applications and Outcomes
| Nanoparticle Type | Therapeutic Application | Model System | Key Outcomes | Reference |
|---|---|---|---|---|
| Solid Lipid Nanoparticles | Alzheimer's disease, Parkinson's disease, glioblastoma | Preclinical animal models | Successful BBB crossing, improved therapeutic distribution, enhanced drug effectiveness | [29] |
| Polymeric (PLGA) NPs | Brain tumor therapy | White albino rats | Enhanced drug concentration in brain compared to conventional delivery | [28] |
| Lipid-based Nanoemulsions | CNS disorders | In vitro & in vivo models | Direct nose-to-brain delivery, bypassing hepatic first-pass metabolism | [31] |
| Chitosan Nanoparticles | CNS drug delivery | Experimental models | Demonstrated ability to cross BBB, protection against chemical degradation | [28] |
| Polymeric Micelles | CNS disorders | Experimental models | Potential to improve drug transport across BBB via EPR effect and active targeting | [30] |
Cancer Therapy Applications and Performance
Tumor Targeting Mechanisms
Both lipid and polymeric nanoparticles leverage unique pathophysiological features of tumors for enhanced drug delivery, primarily through the Enhanced Permeability and Retention (EPR) effect, where the leaky vasculature and impaired lymphatic drainage of tumors allow selective accumulation of nanoscale particles [27] [28]. Beyond this passive targeting, both platforms can be functionalized with active targeting ligands that recognize tumor-specific biomarkers, enabling precise cell-specific drug delivery [27] [30].
Table 3: Cancer Therapy Applications and Experimental Outcomes
| Nanoparticle Formulation | Cancer Model | Therapeutic Payload | Key Experimental Findings | Reference |
|---|---|---|---|---|
| Tumor-targeted Liposome (EY-L) | Renal cell carcinoma | Everolimus & YM155 | Significant tumor growth suppression, enhanced radiosensitivity in vitro and in vivo | [27] |
| PEG-HPMA Polymeric NPs | 4T1 and MCF-7 breast cancer | Doxorubicin | Enhanced cellular uptake and cytotoxicity compared to free doxorubicin | [28] |
| PLGA-PEG-PLGA NPs | HT29 colon cancer | 5-Fluorouracil & chrysin | High potent synergistic anticancer effect demonstrated | [28] |
| FA-L-PEG-PCL Polymeric NPs | MCF-7 breast cancer | Tamoxifen | Enhanced apoptosis of cancer cells, non-cytotoxic at high concentrations | [28] |
| LNP-mRNA Formulations | Various cancers | mRNA therapeutics | Efficient tumor-specific delivery, demonstrated in ongoing oncology clinical trials | [27] |
Experimental Protocols and Methodologies
Standardized Formulation Protocols
Lipid Nanoparticle Preparation (Ethanol Injection Method)
- Step 1: Prepare lipid phase by dissolving ionizable lipid, phospholipid, cholesterol, and PEG-lipid in ethanol at specific molar ratios (typical composition: 50:10:38.5:1.5 mol%) [27].
- Step 2: Prepare aqueous phase containing therapeutic payload (mRNA, siRNA, or small molecules) in citrate or acetate buffer (pH 4.0-5.0).
- Step 3: Rapidly mix lipid phase with aqueous phase using microfluidic device or rapid pipetting at 1:3 volume ratio (ethanolic:aqueous).
- Step 4: Dialyze against PBS (pH 7.4) to remove ethanol and establish neutral pH for storage.
- Step 5: Characterize particle size (target: 80-100 nm), polydispersity index (<0.2), encapsulation efficiency (>90%), and in vitro activity [27].
Polymeric Nanoparticle Preparation (Single Emulsion Solvent Evaporation)
- Step 1: Dissolve polymer (e.g., PLGA, PLA) and hydrophobic drug in organic solvent (dichloromethane or ethyl acetate).
- Step 2: Emulsify organic phase in aqueous solution containing stabilizer (e.g., polyvinyl alcohol) using probe sonication or high-pressure homogenization.
- Step 3: Stir continuously for 3-4 hours to evaporate organic solvent and allow nanoparticle hardening.
- Step 4: Centrifuge to collect nanoparticles, wash to remove stabilizer, and lyophilize for storage.
- Step 5: Characterize particle size, surface charge, drug loading, and in vitro release profile [28] [30].
Standardized Characterization Assays
- Size and Surface Charge: Dynamic light scattering for hydrodynamic diameter and polydispersity; laser Doppler electrophoresis for zeta potential [30].
- Morphology: Transmission electron microscopy or cryo-TEM for structural analysis [27].
- Drug Encapsulation and Loading: Ultracentrifugation followed by HPLC/UV-Vis quantification of encapsulated vs. free drug [28].
- In Vitro Release Profile: Dialysis method in physiologically relevant buffers (pH 7.4 and 5.5) with sampling at predetermined time points [28] [30].
- Cell Uptake and Cytotoxicity: Flow cytometry with fluorescently labeled nanoparticles; MTT assay for cell viability [27] [28].
Research Reagent Solutions
Table 4: Essential Research Reagents for Nanoparticle Development
| Reagent Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Ionizable Lipids | DLin-MC3-DMA, SM-102, ALC-0315 | LNP core structure, endosomal escape | Critical for nucleic acid delivery; protonate in acidic endosomes [27] |
| Structural Lipids | DSPC, DPPC, DOPE | Bilayer formation, stability | Phospholipids that provide structural integrity to nanoparticles [27] |
| Stabilizing Polymers | PEG-DMG, PEG-DSPE | Steric stabilization, circulation half-life | Reduce protein adsorption and macrophage uptake [27] |
| Biodegradable Polymers | PLGA, PLA, PCL | Polymeric matrix for drug encapsulation | Tunable degradation rates from weeks to months [28] |
| Natural Polymers | Chitosan, gelatin, alginate | Biocompatible nanoparticle matrix | Mucoadhesive properties beneficial for mucosal delivery [28] |
| Targeting Ligands | Folate, transferrin, RGD peptides, antibodies | Active targeting to specific cells/receptors | Enhance cellular uptake through receptor-mediated endocytosis [30] |
| Characterization Dyes | DiO, DiI, DiD, Cyanine dyes | Nanoparticle tracking and cellular uptake studies | Lipid-soluble dyes incorporate into hydrophobic regions [27] |
Lipid and polymeric nanoparticles represent complementary platforms in the targeted drug delivery landscape, each with distinctive advantages for specific applications. Lipid nanoparticles excel in nucleic acid delivery with proven clinical success, biocompatibility, and efficient endosomal escape mechanisms. Polymeric nanoparticles offer superior controlled release profiles, extensive tunability of properties, and high stability. The selection between these platforms depends critically on the specific therapeutic payload, target tissue, and desired release kinetics. Future directions include the development of hybrid systems that combine advantageous properties of both platforms, increased application of artificial intelligence for rational nanoparticle design, and continued focus on overcoming biological barriers for enhanced therapeutic outcomes in both CNS disorders and cancer.
The skin, being the largest organ of the human body, serves as a primary physiological barrier that prevents external substances from entering the system, thereby posing significant challenges for transdermal drug delivery. Conventional topical formulations, including creams and patches, often fail to penetrate the stratum corneum barrier effectively, especially when the skin thickens due to conditions like psoriasis or when biofilms form over infectious wounds [32]. Among the various strategies developed to overcome this barrier, microneedle (MN) technology has emerged as a transformative approach in biomedical applications, offering a painless, minimally invasive, and highly efficient method for drug delivery [32] [33]. Microneedles are micron-scale needle arrays that can painlessly penetrate the stratum corneum to deliver therapeutic agents directly to the epidermis or dermis, bypassing pain receptors and avoiding the discomfort associated with hypodermic needles [34] [35].
Hydrogel-forming microneedles (HFMs) represent a particularly advanced category within this technology. Composed of crosslinked, hydrophilic polymer networks, HFMs undergo rapid swelling upon insertion into the skin, absorbing interstitial fluid to form continuous hydrogel conduits that enable efficient drug transport into the dermal microcirculation [32] [33]. Unlike conventional microneedles that primarily rely on passive diffusion, HFMs create a gel matrix reservoir that facilitates controlled and sustained drug release, thereby maintaining therapeutic levels over extended periods while significantly reducing dosing frequency [32] [34]. This review provides a comprehensive comparative analysis of hydrogel microneedles against alternative drug delivery platforms, examining their mechanical properties, drug delivery efficiency, release kinetics, and therapeutic performance through structured experimental data and methodological protocols.
Comparative Analysis of Microneedle Platforms
Classification and Mechanism of Action
Microneedle platforms can be broadly categorized into five distinct types based on their design and drug delivery mechanisms: solid, coated, hollow, dissolving, and hydrogel-forming microneedles [34] [36] [35]. Each system employs a unique approach for transdermal drug delivery, with varying implications for drug loading capacity, release kinetics, and clinical applicability.
Solid microneedles (SMNs) function primarily as piercing devices to create microchannels in the skin, after which a drug-containing patch is applied for diffusion [35]. While they exhibit excellent mechanical properties and simple preparation methods, they require a two-step application process and offer poor control over drug dosage and administration timing [34]. Coated microneedles (CMNs) consist of solid microneedles coated with drug formulations, enabling rapid delivery of therapeutic agents as the coating dissolves upon skin insertion [32] [35]. Although this design allows for substantial drug loading and dosage control, the preparation process is complex, and there is a risk of coating loss in the stratum corneum [34].
Hollow microneedles (HMNs) feature internal bores through which liquid drug formulations can flow, typically driven by external pressure [35]. These systems enable rapid drug delivery with controllable dosing but are prone to clogging, needle fracture, and flow leakage issues [34]. Dissolving microneedles (DMNs) are fabricated from biodegradable, water-soluble polymers that encapsulate drugs and fully dissolve upon insertion into the skin, releasing their payload [32] [35]. While they offer manageable dosing and high biocompatibility, they often suffer from poor mechanical properties and prolonged action duration [34].
Hydrogel-forming microneedles (HFMs), the focus of this review, are composed of crosslinked hydrophilic polymers that swell upon skin insertion without dissolving, forming hydrogel conduits that enable controlled drug release [32] [33]. The key differentiator of HFMs is that drug delivery is governed primarily by the crosslinking density of the hydrogel matrix rather than the permeability of the stratum corneum, allowing for precise modulation of release kinetics [32]. This unique mechanism provides exceptional drug loading capacity and tunable release profiles while avoiding the generation of sharp biological waste [32] [34].
Table 1: Comparative Analysis of Microneedle Platforms for Transdermal Drug Delivery
| MN Type | Mechanism of Action | Advantages | Disadvantages | Primary Applications |
|---|---|---|---|---|
| Solid MN | Pre-treatment skin perforation followed by drug patch application | Simple preparation; Excellent mechanical properties [34] | Two-step process; Poor drug dosage control; Potential needle breakage [34] [35] | Vaccine delivery; Skin preconditioning [35] |
| Coated MN | Drug coating dissolves upon skin insertion | Large drug load; Controllable dosage [34] | Complex preparation; Coating loss in stratum corneum; Risk of premature drug release [34] [35] | Rapid delivery of vaccines; Macromolecular drugs [35] |
| Hollow MN | Pressure-driven flow through internal bore | Fast drug release; Dose control [34] | Clogging risk; Needle breakage; Low drug load; Flow leakage [34] [35] | Liquid drug formulations; Continuous infusion [35] |
| Dissolving MN | Needle dissolution releases encapsulated drug | Simple production; Biocompatible; No sharp waste [34] [35] | Poor mechanical strength; Prolonged action; Material limitations [34] | Sustained release; Vaccine delivery [35] |
| Hydrogel-forming MN | Skin insertion → hydrogel swelling → controlled drug diffusion | Large drug load; Tunable release; Excellent biocompatibility; Controlled by crosslink density [32] [34] [33] | Moderate mechanical strength; Formulation complexity [34] | Sustained drug delivery; Chronic conditions; ISF monitoring [32] [33] |
Performance Metrics and Experimental Data
Quantitative evaluation of microneedle performance encompasses multiple parameters, including mechanical strength, insertion capability, drug release efficiency, and biocompatibility. Experimental data derived from recent studies enables direct comparison between hydrogel-forming microneedles and alternative platforms.
Mechanical properties represent a critical performance indicator, as microneedles must possess sufficient strength to penetrate the stratum corneum (approximately 10-20 μm thick) and reach the viable epidermis and dermis (100-150 μm) without fracture [32] [36]. Research has demonstrated that optimized HFMs composed of polyvinyl alcohol (PVA) and polyvinylpyrrolidone (PVP) crosslinked with glutaraldehyde achieve a fracture force of 0.13 N per needle, substantially exceeding the minimum 0.058 N required for skin penetration [36]. Similarly, HFMs fabricated from PVA, PVP, and poly(ethylene glycol) diacid (PEGdiacid) exhibited minimal height reduction (7.67%) under 32 N compression pressure and successfully achieved insertion depths of 508-522 μm, effectively penetrating the stratum corneum while maintaining structural integrity [36].
Drug release kinetics vary significantly across microneedle platforms. Coated and dissolving microneedles typically exhibit rapid drug release, often within minutes to hours, while hydrogel-forming systems demonstrate extended release profiles ranging from days to weeks [32] [34]. For instance, a cyclosporine A-loaded HFM system for psoriatic treatment demonstrated sustained drug release over 72 hours, maintaining therapeutic concentrations with significantly enhanced skin deposition compared to conventional topical formulations [37]. Similarly, HFMs incorporating poly(ethylene glycol) (PEG) and PMVE/MA copolymers for acyclovir delivery achieved 75.56% drug release within 24 hours, with a transdermal absorption rate 39 times higher than conventional topical applications [36].
Drug loading capacity represents another distinguishing factor. While coated microneedles are limited by surface area and hollow microneedles by internal volume, hydrogel-forming systems utilize the entire polymer matrix for drug incorporation, enabling substantially higher payloads [32] [34]. This expanded capacity is particularly advantageous for macromolecular drugs, including proteins, peptides, and nucleic acids, which typically require frequent administration in conventional delivery systems [33].
Table 2: Experimental Performance Metrics of Microneedle Platforms
| Performance Parameter | Hydrogel-forming MNs | Dissolving MNs | Hollow MNs | Coated MNs |
|---|---|---|---|---|
| Typical Fracture Force (N/needle) | 0.13 [36] | 0.08-0.10 [34] | 0.15-0.20 [34] | 0.10-0.12 [34] |
| Insertion Depth (μm) | 500-522 [36] | 300-400 [34] | 500-1000 [34] | 200-300 [34] |
| Drug Release Profile | Sustained (hours to days) [32] | Rapid (minutes to hours) [34] | Immediate (minutes) [34] | Rapid (minutes) [34] |
| Transdermal Permeation Enhancement | 39-fold increase [36] | 10-20 fold increase [34] | 20-30 fold increase [34] | 5-15 fold increase [34] |
| Macromolecule Delivery Capacity | Excellent [32] [33] | Good [34] | Limited [34] | Limited [34] |
| Skin Recovery Time | 2-4 hours [32] | 4-8 hours [34] | 1-2 hours [34] | 2-4 hours [34] |
Experimental Protocols for HFM Evaluation
Fabrication Methodologies
The manufacturing process for hydrogel-forming microneedles significantly influences their structural integrity, mechanical properties, and drug delivery performance. Micro-molding represents the most widely employed fabrication technique, comprising several standardized steps [32] [34].
Master Mold Preparation: A negative mold containing the desired microneedle geometry (typically 100-1500 μm height, 50-250 μm base width) is fabricated using techniques such as hot embossing, micro-molding, thermal-drawing lithography, magneto-rheological lithography, laser drilling, or increasingly, 3D printing for enhanced customization [32] [38].
Hydrogel Formulation: Biocompatible polymers—including gelatin methacryloyl (GelMA), hyaluronic acid (HA), chitosan, silk fibroin (SF), polyvinyl alcohol (PVA), or combinations thereof—are dissolved in aqueous solution along with crosslinking agents [32] [34]. Active pharmaceutical ingredients are incorporated into this polymer mixture, with homogenization ensuring uniform drug distribution.
Mold Casting and Vacuum-assisted Filling: The hydrogel precursor solution is introduced into the master mold cavities, followed by vacuum or centrifugation application to eliminate air bubbles and ensure complete needle tip filling [32].
Crosslinking and Solidification: Structural integrity is established through chemical or physical crosslinking, typically initiated by ultraviolet irradiation (for photo-crosslinkable systems like GelMA), thermal treatment, or chemical catalysts [32] [36]. Crosslinking density is precisely controlled as it directly governs subsequent swelling behavior and drug release kinetics [32].
Demolding and Post-processing: The solidified HFM patch is carefully separated from the mold, followed by optional dehydration, sterilization (gamma irradiation or ethylene oxide), and packaging [32].
Performance Evaluation Protocols
Standardized experimental protocols enable quantitative assessment of HFM performance metrics and facilitate direct comparison with alternative platforms.
Mechanical Strength Testing:
- Compression Testing: Individual microneedles or complete arrays undergo axial compression using a texture analyzer or similar instrumentation, with progressive force application (typically 0.02-0.5 N/needle) until fracture occurs [36]. The force-displacement curve is recorded to determine fracture force and deformation behavior.
- Insertion Force Analysis: HFM arrays are applied to validated skin models (ex vivo porcine or human skin, or synthetic equivalents like Parafilm M layers) using a universal mechanical tester with controlled application force and velocity [36]. Successful penetration is confirmed through histological sectioning or dye-binding studies.
Drug Release Kinetics:
- In Vitro Release Profiling: HFM arrays are immersed in receptor medium (typically phosphate-buffered saline, pH 7.4) under sink conditions at 32°C to simulate skin temperature [32] [39]. Samples are withdrawn at predetermined intervals and analyzed via HPLC or UV-Vis spectroscopy to quantify drug release.
- Skin Permeation Studies: Using Franz diffusion cells with excised skin membranes, HFMs are applied to the stratum corneum side, with receptor medium sampling at scheduled timepoints to determine transdermal flux, permeation coefficients, and skin deposition [37].
Swelling Behavior and Hydration Kinetics:
- HFM arrays are weighed dry (Wâ‚€) before application to hydrated skin models or immersion in PBS.
- At predetermined intervals, arrays are removed, surface moisture is carefully blotted, and wet weight (Wₜ) is recorded.
- The swelling ratio is calculated as (Wₜ - W₀)/W₀ × 100%, providing insight into hydrogel conduit formation kinetics [32].
Biocompatibility Assessment:
- Cytotoxicity: HFM extracts are applied to fibroblast cultures (e.g., L929 or NIH/3T3 cells), with viability assessed via MTT or Alamar Blue assays after 24-72 hours [32] [33].
- Skin Irritation: HFMs are applied to reconstructed human epidermis models (EpiDerm, EpiSkin) or rabbit models, with irritation potential evaluated through morphological analysis and inflammatory mediator release [33].
Diagram 1: Comparative advantages and limitations of different microneedle platforms. Green connections indicate strengths, while red connections indicate limitations.
Advanced Hydrogel Microneedle Systems and Applications
Biomaterial Integration and Functional Enhancement
Recent innovations in hydrogel microneedle technology have focused on integrating advanced biomaterials to overcome inherent limitations and expand therapeutic applications. The incorporation of nanoparticles (NPs) within hydrogel matrices has demonstrated particular promise, creating hybrid systems that leverage the advantages of both components [40].
Nanoparticle-incorporated HFMs significantly enhance functionality through multiple mechanisms: (1) improved solubility and stability of hydrophobic therapeutic agents; (2) enhanced mechanical properties of the hydrogel matrix; (3) enabling intelligent, stimulus-responsive drug release; and (4) facilitating precise cellular targeting [40]. For instance, a silk fibroin-based HFM encapsulating Prussian blue nanozymes (PBNs) and vascular endothelial growth factor (VEGF) demonstrated exceptional biocompatibility, sustained drug release, pro-angiogenic, antioxidant, and antibacterial properties, offering a comprehensive therapeutic approach for diabetic wound healing [34].
Similarly, HFMs combining gelatin methacryloyl (GelMA) with polyethylene glycol diacrylate (PEGDA) have been developed for co-delivery of exosomes and tazarotene, promoting cell migration and angiogenesis through controlled release in deep skin layers [34]. These advanced composite systems effectively address the individual limitations of hydrogels (limited drug-loading capacity, suboptimal mechanical strength) and nanoparticles (penetration barriers, biocompatibility concerns), resulting in synergistic performance enhancements [37].
Therapeutic Applications and Clinical Performance
Hydrogel-forming microneedles have demonstrated exceptional efficacy across diverse medical applications, particularly in managing chronic conditions requiring sustained drug delivery.
Psoriasis Management: The thickened, hyperkeratotic psoriatic plaque presents significant challenges for conventional topical therapies. HFMs effectively bypass this compromised barrier, enabling targeted delivery of anti-psoriatic agents. A cross-linked hyaluronic acid microneedle system for localized delivery of an estrogen receptor alpha (ERα)-degrading PROTAC (ERD308) and Palbociclib demonstrated high rates of local drug retention (87%) with sustained release over at least 4 days, significantly inhibiting breast tumor growth in ER+ models with enhanced safety profiles [34]. Similarly, HFMs incorporating hydrolyzed collagen and sodium alginate have been developed for nicotinamide delivery, effectively reversing skin aging and treating related dermatological conditions [34].
Melanoma Therapy: HFMs have emerged as promising platforms for melanoma treatment, enabling localized delivery of chemotherapeutic, immunotherapeutic, and targeted therapeutic agents directly into the tumor microenvironment while minimizing systemic exposure [36]. A chitosan-based HMN patch loaded with 5-fluorouracil (5-FU) liposomes demonstrated significant anti-cancer activity with no appreciable toxicity to normal cells, highlighting the targeting precision of this approach [36]. Additionally, GelMA microneedles serving as delivery platforms for oncolytic viruses have opened new avenues in cancer immunotherapy [36].
Wound Healing: Multifunctional HFM patches have shown remarkable efficacy in promoting diabetic wound healing through coordinated action of multiple therapeutic components. A silk fibroin methacryloyl hydrogel microneedle patch (MN-PBN-VEGF) incorporating Prussian blue nanozymes and VEGF demonstrated superior pro-angiogenic, antioxidant, and antibacterial properties, significantly accelerating wound closure in diabetic models [34].
Diagram 2: Standardized fabrication workflow for hydrogel-forming microneedles, highlighting critical optimization points (yellow) and standardized procedures (green).
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and evaluation of advanced hydrogel-forming microneedles require specialized materials and characterization tools. The following table comprehensively details essential research reagents and their specific functions in HFM research protocols.
Table 3: Essential Research Reagents and Materials for Hydrogel Microneedle Development
| Category | Specific Material/Reagent | Function/Application | Experimental Notes |
|---|---|---|---|
| Natural Polymers | Gelatin Methacryloyl (GelMA) | Photo-crosslinkable hydrogel; retains RGD sequences and MMP-responsive sites [32] [34] | Tunable physical properties; concentration: 5-20% w/v; UV crosslinking: 365 nm, 5-15 mW/cm² |
| Hyaluronic Acid (HA) | Native or modified (MeHA); excellent biocompatibility; mimics extracellular matrix [34] [36] | Molecular weight impacts swelling and mechanical properties; concentration: 2-10% w/v | |
| Chitosan (CS) | Cationic polysaccharide; inherent antimicrobial properties [32] [33] | Soluble in weak acid solutions; degree of deacetylation affects properties | |
| Silk Fibroin (SF) | Exceptional mechanical strength; sustained release capability [34] [36] | Requires degumming process; concentration: 5-30% w/v | |
| Sodium Alginate (SA) | Ionic crosslinking with divalent cations (Ca²âº) [34] [36] | Rapid gelation; concentration: 1-5% w/v | |
| Synthetic Polymers | Polyvinyl Alcohol (PVA) | Excellent mechanical properties; freeze-thaw or chemical crosslinking [34] [36] | Degree of hydrolysis: 87-99%; concentration: 10-20% w/v |
| Polyvinyl Pyrrolidone (PVP) | Water solubility; film-forming ability [32] [34] | Molecular weight range: 10,000-1,000,000 Da; concentration: 5-30% w/v | |
| Poly(ethylene glycol) diacrylate (PEGDA) | Photo-polymerizable crosslinker; modulates mechanical properties [34] | Molecular weight: 700-10,000 Da; concentration: 1-10% w/v | |
| Crosslinking Agents | Glutaraldehyde | Chemical crosslinker for hydroxyl-containing polymers [36] | Concentration: 0.1-2% v/v; requires careful control due to cytotoxicity |
| Ammonium Persulfate (APS) / TEMED | Redox initiator system for radical polymerization [32] | Concentration: 0.1-1% w/v; degassing improves efficiency | |
| UV Photoinitiators (Irgacure 2959, LAP) | Free radical generation under UV exposure for photopolymerization [32] | Concentration: 0.1-0.5% w/v; wavelength: 365 nm for Irgacure 2959 | |
| Characterization Tools | Texture Analyzer | Mechanical property assessment (compression, fracture force) [36] | Typical settings: 0.5-1 mm/min compression rate; 0.02-0.5 N/needle force range |
| Franz Diffusion Cells | In vitro drug release and skin permeation studies [37] | Membrane options: ex vivo skin, synthetic membranes; temperature: 32°C | |
| HPLC-UV/FLD | Quantitative drug analysis in release studies [39] | Method validation required for each drug molecule | |
| Scanning Electron Microscopy (SEM) | Morphological characterization of microneedle structure [32] | Requires sputter coating for non-conductive polymers | |
| Fmoc-Glu-OMe-OH | Fmoc-Glu-OMe-OH, MF:C20H19NO6, MW:369.4 g/mol | Chemical Reagent | Bench Chemicals |
| Chrysene-5,6-diol | Chrysene-5,6-diol|Polycyclic Aromatic Hydrocarbon | Chrysene-5,6-diol is a dihydrodiol metabolite of Chrysene for research into PAH metabolic activation and genotoxicity. This product is For Research Use Only. Not for human or personal use. | Bench Chemicals |
Hydrogel-forming microneedles represent a paradigm shift in transdermal drug delivery, successfully addressing critical limitations of both conventional topical formulations and alternative microneedle platforms. Through their unique swelling mechanism and formation of continuous hydrogel conduits, HFMs enable precise control over drug release kinetics, exceptional loading capacity for macromolecular therapeutics, and minimally invasive application that significantly enhances patient compliance compared to hypodermic injections [32] [33]. The direct relationship between crosslinking density and release kinetics provides an unparalleled tool for tuning therapeutic profiles to match specific clinical requirements, from rapid onset to sustained delivery over several days [32].
While challenges remain in optimizing mechanical strength for particularly thick or hyperkeratotic skin conditions, and in standardizing large-scale manufacturing processes, emerging technologies offer promising solutions [32] [41]. The integration of artificial intelligence and machine learning in material selection, design optimization, and manufacturing process control is accelerating the development of next-generation HFMs with enhanced performance characteristics [41]. Similarly, the incorporation of stimuli-responsive materials that react to pathological biomarkers or external triggers (pH, temperature, enzymes) is paving the way for intelligent, closed-loop drug delivery systems capable of autonomous therapeutic adjustment [36] [38].
As research advances, hydrogel-forming microneedles are poised to expand beyond dermatological applications into diverse fields including ocular drug delivery [38], cardiovascular therapy [34], and personalized medicine through combination with biosensing platforms [35]. Their unique combination of minimally invasive application, sustained release capabilities, and compatibility with diverse therapeutic agents establishes HFMs as a versatile and powerful platform that will continue to transform drug delivery paradigms across medical specialties.
The efficacy of a drug is profoundly influenced by its method of formulation and delivery within the body [42]. Conventional drug administration routes, such as oral ingestion or systemic injection, often face significant challenges due to specific anatomical and physiological barriers, leading to suboptimal therapeutic outcomes [43] [42]. Biomaterial-based drug delivery systems (DDS) are engineered to overcome these hurdles, offering enhanced control over release kinetics, improved bioavailability, and targeted delivery, thereby reducing systemic side effects [42] [44]. These systems are designed to interact with biological systems and can be tailored for diverse administration routes, each with unique advantages and limitations [42].
This guide provides a comparative analysis of biomaterial strategies tailored for three challenging delivery routes: the oral mucosa, the inner ear, and the pulmonary system. These routes exemplify the application of precision biomaterial engineering to solve distinct anatomical problems. For oral mucosal delivery, the focus is on overcoming salivary clearance and enzymatic degradation [45] [46]. For the inner ear, the primary challenge is bypassing the blood-labyrinth barrier to achieve sufficient local drug concentrations [43] [47]. Pulmonary delivery aims to maximize drug deposition in the deep lungs for rapid systemic absorption or local treatment [48] [49]. By comparing the key parameters, experimental models, and biomaterial solutions for these routes, this guide serves as a resource for researchers and drug development professionals working in advanced DDS.
Comparative Analysis of Key Parameters Across Delivery Routes
The following tables summarize the core challenges, biomaterial solutions, and key performance metrics for drug delivery via the oral mucosa, inner ear, and pulmonary routes.
Table 1: Anatomical Challenges and Biomaterial Solutions for Different Drug Delivery Routes
| Delivery Route | Primary Anatomical/Physiological Barriers | Common Biomaterial Solutions | Key Formulation Types |
|---|---|---|---|
| Oral Mucosal | Salivary washout, enzymatic degradation, limited permeability of stratified epithelium [45] [46] | Mucoadhesive polymers (e.g., Chitosan, Hyaluronic acid, Gelatin) [45] [46] | Mucoadhesive films, wafers, hydrogels, nanoparticles [45] |
| Inner Ear | Blood-labyrinth barrier, intricate and inaccessible anatomy, limited cochlear fluid volume [43] [47] | Hydrogels, polymeric nanoparticles, lipid-based carriers [43] [47] [50] | Biopolymer-coated implants, injectable hydrogels, nanoparticle suspensions [43] [47] |
| Pulmonary | Mucociliary clearance, alveolar macrophage phagocytosis, surfactant layer, variable patient inhalation technique [48] [49] | Engineered microparticles for aerosolization, phospholipids, biodegradable polymers [48] [49] | Metered-dose inhalers (MDIs), Dry powder inhalers (DPIs), Nebulizers [48] [49] |
Table 2: Key Performance Metrics and Experimental Data from Delivery System Studies
| Delivery Route | Typical Drug Payload | Release Duration | Key Efficacy Metrics (from experimental studies) |
|---|---|---|---|
| Oral Mucosal | Peptides, proteins, small molecules [45] | Hours to a few days (sustained-release) [45] | Enhancement in bioavailability vs. oral administration; Mucoadhesion strength (N/cm²); Permeation enhancement ratio [46] |
| Inner Ear | Neurotrophic factors (e.g., BDNF), antioxidants, genes [43] [47] | Weeks to months (long-term sustained release) [43] | Higher survival rate of hair cells/spiral ganglion neurons; Improved auditory brainstem response (ABR) thresholds [47] [50] |
| Pulmonary | Corticosteroids, bronchodilators, antibiotics [48] [49] | Minutes to hours (rapid release), or sustained over days [49] | Fine Particle Fraction (FPF %); Forced Expiratory Volume (FEV1) improvement; Reduced systemic side effects [48] [49] |
Experimental Protocols for Evaluating Drug Delivery Systems
Oral Mucosal Delivery: Mucoadhesion and Permeation Studies
Objective: To evaluate the bioadhesive strength and drug permeation enhancement of a chitosan-based film across porcine buccal mucosa [45] [46].
Materials:
- Test Formulation: Chitosan (CS) and Hyaluronic Acid (HA) composite film loaded with a model drug (e.g., Dexamethasone).
- Control: A simple drug solution.
- Biological Tissue: Fresh porcine buccal mucosa, excised and stored in Krebs buffer.
- Apparatus: Franz diffusion cell, texture analyzer, spectrophotometer or HPLC.
Methodology:
- Tissue Preparation: The porcine buccal mucosa is carefully mounted between the donor and receptor compartments of the Franz diffusion cell, with the epithelial side facing the donor compartment. The receptor compartment is filled with pH 7.4 buffer maintained at 37°C.
- Mucoadhesion Test: The film is hydrated with a drop of simulated saliva and attached to the probe of a texture analyzer. The probe is lowered to contact the mucosal tissue with a defined force for a set time. The force required to detach the film is measured, indicating the mucoadhesive strength [46].
- Permeation Study: The test film or control solution is placed in the donor compartment. Samples are periodically withdrawn from the receptor compartment and analyzed for drug concentration using UV-spectrophotometry or HPLC.
- Data Analysis: The cumulative amount of drug permeated per unit area is plotted against time. The slope of the linear portion gives the steady-state flux (Jss). The permeability coefficient (Papp) and enhancement ratio (ER) are calculated [45].
Inner Ear Delivery: Hydrogel-Based Hair Cell Protection Assay
Objective: To assess the protective efficacy of a GelMA-based hydrogel delivering an antioxidant (e.g., Uric Acid) on hair cells in an ototoxicity model using inner ear organoids [47] [50].
Materials:
- Biological Model: Inner ear organoids (IEOs) derived from mouse induced pluripotent stem cells (iPSCs) [50].
- Test Group: IEOs cultured in a GelMA hydrogel loaded with uric acid.
- Injury Control: IEOs exposed to a known ototoxin (e.g., Cisplatin) without treatment.
- Staining: Phalloidin (for F-actin in hair cell stereocilia) and Myosin VIIa antibodies (for hair cell bodies).
Methodology:
- Organoid Culture & Treatment: IEOs are generated and matured using established protocols [50]. The GelMA/uric acid hydrogel is prepared and applied to the organoid culture medium.
- Ototoxic Insult: Cisplatin is added to the culture medium of both the test and injury control groups for 24 hours to induce hair cell damage.
- Immunofluorescence and Quantification: After the exposure period, organoids are fixed, permeabilized, and stained with phalloidin and anti-Myosin VIIa. The samples are imaged using confocal microscopy.
- Data Analysis: The number of intact hair cells, identified by co-localized Phalloidin and Myosin VIIa staining, is counted in each group. The survival rate of hair cells in the test group is compared to the injury control group to determine the hydrogel's protective efficacy [47].
Pulmonary Delivery: Aerodynamic Particle Size Distribution
Objective: To characterize the aerosol performance and lung deposition potential of a dry powder inhaler (DPI) formulation [49].
Materials:
- Test Formulation: Spray-dried, engineered microparticles containing a drug (e.g., Tiotropium Bromide) and a carrier (e.g., Lactose).
- Apparatus: Next-Generation Impactor (NGI), high-capacity vacuum pump, DPI device.
Methodology:
- Impactor Setup: The NGI stages are assembled according to the manufacturer's instructions and cooled to 5°C to prevent particle bounce.
- Aerosolization: The DPI device, loaded with a single dose of the formulation, is actuated into a mouthpiece adapter attached to the NGI. A vacuum pump draws air through the system at a fixed flow rate (e.g., 60 L/min) for a specific time.
- Sample Collection: The drug deposited on each stage of the NGI, the induction port, and the device itself is carefully recovered using a suitable solvent and quantified using HPLC.
- Data Analysis: The mass of drug on each stage is used to calculate the Fine Particle Fraction (FPF), defined as the percentage of the emitted dose with an aerodynamic diameter smaller than 5 μm, which is considered respirable. The Mass Median Aerodynamic Diameter (MMAD) is also determined, indicating the particle size around which the mass distribution is centered [49].
Visualization of Experimental Workflows and Signaling Pathways
Inner Ear Organoid Mechanotransduction Pathway
The following diagram illustrates the signaling pathway by which mechanical properties of a hydrogel scaffold promote hair cell differentiation in inner ear organoids, a key mechanism explored in experimental models [50].
Mechanotransduction in Hair Cell Differentiation
Pulmonary DPI Testing Workflow
This workflow outlines the key steps for the experimental evaluation of Dry Powder Inhaler (DPI) formulations using a Next-Generation Impactor (NGI), a standard method in pulmonary drug development [49].
Aerosol Performance Testing Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Specialized Drug Delivery Research
| Item / Reagent Solution | Function / Application in Research |
|---|---|
| Chitosan (CS) | A natural mucoadhesive polymer used to create films and nanoparticles for oral mucosal delivery, extending residence time by bonding with mucosal glycoproteins [45] [46]. |
| Hyaluronic Acid (HA) | A glycosaminoglycan used in hydrogels for its biocompatibility, mucoadhesive properties, and ability to interact with CD44 receptors often upregulated in inflamed tissues [46] [50]. |
| Gelatin Methacrylate (GelMA) | A photopolymerizable hydrogel used as a 3D scaffold for inner ear organoids. Its stiffness can be tuned to influence stem cell differentiation toward hair cells [50]. |
| Matrigel | A complex, biologically-derived basement membrane matrix used traditionally for 3D culture of organoids, providing mechanical support and biochemical cues [50]. |
| Poly(Lactic-co-Glycolic Acid) (PLGA) | A biodegradable and biocompatible synthetic polymer widely used to create nanoparticles and microparticles for sustained drug release in inner ear and pulmonary delivery [43] [42]. |
| Lgr5+ Progenitor Cells | A population of Wnt-responsive inner ear stem cells that can be expanded and differentiated in 3D culture to generate inner ear organoids for ototoxicity testing and therapy development [50]. |
| Next-Generation Impactor (NGI) | The standard apparatus for characterizing the aerodynamic particle size distribution of inhaled formulations, critical for predicting lung deposition [49]. |
| Franz Diffusion Cell | An experimental setup used to study the permeation of drugs through biological membranes, such as buccal mucosa, and to test mucoadhesive properties [45] [46]. |
| 6-butyl-7H-purine | 6-Butyl-7H-purine|Research Use Only |
| Carbamic azide, cyclohexyl- | Carbamic azide, cyclohexyl-|C7H12N4O|For Research |
The field of drug delivery is undergoing a revolutionary transformation, moving away from the traditional "one-size-fits-all" approach toward a more personalized, patient-centric model. This paradigm shift is largely driven by advancements in additive manufacturing, commonly known as 3D printing, which enables the fabrication of customized drug delivery systems with precise control over geometry, composition, and release profiles [51]. Unlike conventional pharmaceutical manufacturing, 3D printing constructs dosage forms layer-by-layer based on digital designs, allowing for unprecedented customization to meet individual patient needs [52]. This technology has demonstrated significant potential for addressing the unique requirements of special populations, including pediatric and geriatric patients who often struggle with standardized medication formats [53] [52].
The convergence of 3D printing with biofabrication techniques has further expanded the horizons of personalized medicine, enabling the creation of sophisticated drug delivery devices that can control release kinetics, combine multiple therapeutics, and even incorporate living cells for tissue-specific targeting [54]. These innovations represent a significant departure from traditional drug delivery systems, offering solutions to long-standing challenges such as poor patient compliance, suboptimal therapeutic outcomes, and dose-dependent side effects [55] [56]. As the pharmaceutical industry embraces this technological disruption, comparative analysis of different 3D printing platforms and biomaterial systems becomes essential for guiding research and development efforts toward the most promising applications in personalized drug delivery.
Comparative Analysis of 3D Printing Technologies in Pharmaceutical Applications
Various 3D printing technologies have been adapted for pharmaceutical applications, each offering distinct advantages and limitations for manufacturing personalized drug delivery devices. The selection of an appropriate printing method depends on multiple factors, including the nature of the active pharmaceutical ingredient (API), desired release profile, structural complexity, and production requirements [53] [52]. The most prominent technologies currently being investigated include Material Extrusion (encompassing Fused Deposition Modeling (FDM) and Semi-Solid Extrusion (SSE), Binder Jetting (BJ-3DP), Vat Photopolymerization (including Stereolithography (SLA) and Digital Light Processing (DLP)), and Powder Bed Fusion (such as Selective Laser Sintering (SLS)) [52] [56].
Table 1: Comparison of Major 3D Printing Technologies for Drug Delivery Applications
| Printing Technology | Key Advantages | Major Limitations | Suitable Dosage Forms | Drug Loading Capacity |
|---|---|---|---|---|
| Fused Deposition Modeling (FDM) | Simple, inexpensive equipment; Ability to create complex 3D structures [52] | High printing temperatures; Requires drug-loaded filaments; Limited material options [52] | Immediate/sustained release tablets, implants, polypills [56] | Low to moderate [52] |
| Semi-Solid Extrusion (SSE) | Room temperature printing; Disposable syringes for easy material change [52] | Low printing accuracy; Often requires post-processing [52] | Pediatric formulations, multi-drug combinations [53] [52] | High |
| Binder Jetting (BJ-3DP) | Wide excipient range; High drug loading; No support material needed [52] | Complex post-processing; Large equipment size; Packaging challenges [52] | Immediate release, porous tablets [52] | High [52] |
| Stereolithography (SLA) | High printing accuracy; Room temperature operation [52] | Limited material options; Long pre-processing; Post-processing required [52] | Microneedles, implants, complex release systems [52] [56] | Moderate |
| Selective Laser Sintering (SLS) | High resolution; No need for support structures | Specialized equipment; Thermal stress on APIs | Orally disintegrating tablets, modified-release forms [56] | High |
The selection of an appropriate 3D printing technology fundamentally depends on the specific requirements of the drug delivery application. Fused Deposition Modeling (FDM), while limited by its need for thermally stable filaments and high processing temperatures, excels in producing complex geometric designs that enable controlled release profiles [52] [56]. Semi-Solid Extrusion (SSE) offers distinct advantages for heat-sensitive compounds due to its room-temperature operation and has been successfully deployed in hospital settings for point-of-care manufacturing of personalized medications [52]. Binder Jetting demonstrates superior capabilities for high-dose medications but presents challenges in post-processing and equipment scalability [52]. Emerging technologies such as Digital Light Processing (DLP) show promising resolution for micro-dosage forms but face limitations in biocompatible photoinitiator selection [56].
Experimental Protocols for Evaluating 3D-Printed Drug Delivery Systems
Performance Benchmarking Methodology
To objectively compare the efficiency of various 3D-printed drug delivery systems, researchers employ standardized experimental protocols that evaluate critical performance parameters. These methodologies typically include in vitro release testing, structural characterization, mechanical property assessment, and biocompatibility evaluation [55] [56]. The experimental workflow generally follows a systematic approach beginning with formulation design and proceeding through performance validation.
Diagram 1: Experimental workflow for evaluating 3D-printed drug delivery systems, illustrating the systematic approach from design to validation.
For drug release studies, the most common protocol involves using USP dissolution apparatus (Type I or II) under sink conditions at 37°C ± 0.5°C [56]. Samples are collected at predetermined time intervals and analyzed using validated analytical methods such as UV-Vis spectroscopy or high-performance liquid chromatography (HPLC) to determine drug concentration [56]. The dissolution media is selected based on the intended drug release site (e.g., simulated gastric fluid for immediate release, pH-shift media for enteric coatings). The resulting release data is then fitted to various mathematical models (zero-order, first-order, Higuchi, Korsmeyer-Peppas) to understand the release mechanisms and kinetics [56].
Structural and Mechanical Characterization Protocols
Structural characterization employs multiple analytical techniques to verify the quality and consistency of 3D-printed dosage forms. Scanning Electron Microscopy (SEM) provides high-resolution images of surface morphology and internal structure, allowing researchers to examine layer adhesion, pore distribution, and potential defects [56]. X-ray diffraction (XRD) and differential scanning calorimetry (DSC) are used to determine the physical state of the API (crystalline or amorphous) within the printed matrix, which significantly influences dissolution behavior and stability [56]. Mechanical testing through texture analysis evaluates hardness, friability, and disintegration behavior, particularly important for dosage forms requiring specific handling properties or rapid disintegration [53] [52].
Table 2: Key Experimental Parameters and Methodologies for Evaluating 3D-Printed Drug Delivery Systems
| Performance Parameter | Standard Experimental Method | Key Output Metrics | Significance in Drug Delivery |
|---|---|---|---|
| Drug Release Profile | USP dissolution apparatus with HPLC/UV analysis | Release rate constants, T50, T80, release mechanism | Predicts in vivo performance, guides dosing regimen |
| Structural Integrity | Scanning Electron Microscopy (SEM) | Layer adhesion, surface morphology, pore distribution | Affects drug release consistency and mechanical stability |
| Mechanical Properties | Texture analysis, friability testing | Hardness, friability, disintegration time | Determines handling capability and patient acceptability |
| Drug-Polymer Interaction | Differential Scanning Calorimetry (DSC), FTIR | Physical state of API, polymer-drug compatibility | Influences stability, dissolution, and bioavailability |
| Biocompatibility | Cell viability assays (MTT), hemocompatibility testing | Cell survival percentage, hemolysis rate | Ensures safety for physiological administration |
For specialized dosage forms such as floating gastro-retentive systems, additional specific tests are conducted, including buoyancy studies that measure the time required for the dosage form to float and the duration of floating in simulated gastric fluid [56]. Mucomimetic models using mucin solutions help evaluate the bioadhesive potential of formulations designed for prolonged gastric residence [56]. These specialized protocols provide critical insights into the functional performance of advanced drug delivery systems beyond conventional release characteristics.
Biomaterial Systems for 3D-Printed Drug Delivery: A Comparative Assessment
The performance of 3D-printed drug delivery devices is heavily influenced by the selection of appropriate biomaterials, which function as carriers for active pharmaceutical ingredients and control their release kinetics [55]. These biomaterial systems can be broadly categorized into polymers (both synthetic and natural), lipids, hydrogels, and composite materials, each offering distinct advantages for specific drug delivery applications [55] [52]. The ideal biomaterial for 3D printed drug delivery must satisfy multiple requirements, including printability, biocompatibility, appropriate degradation kinetics, and compatibility with the incorporated API [55].
Synthetic polymers such as polyvinyl alcohol (PVA), polylactic acid (PLA), polycaprolactone (PCL), and Eudragit series are widely used in FDM and SSE printing due to their predictable behavior and tunable properties [52] [56]. These polymers offer excellent mechanical properties and can be engineered to provide specific release profiles through matrix design, with PVA being particularly favored for immediate-release formulations and PCL for sustained-release applications due to its slower degradation rate [52] [56]. Natural polymers including alginate, chitosan, and gelatin are preferred for bioprinting applications and SSE processes where biocompatibility and mild processing conditions are paramount [55]. Hydrogels represent a particularly versatile class of biomaterials that can encapsulate drugs and even living cells, making them ideal for advanced applications in regenerative medicine and localized therapy [54].
Table 3: Comparative Analysis of Biomaterial Systems for 3D-Printed Drug Delivery
| Biomaterial Category | Representative Examples | Key Advantages | Release Mechanisms | Compatible Printing Technologies |
|---|---|---|---|---|
| Synthetic Polymers | PVA, PLA, PCL, Eudragit | Predictable properties, tunable degradation, mechanical strength | Diffusion, erosion, osmotic pressure | FDM, SSE, MED [52] [56] |
| Natural Polymers | Alginate, Chitosan, Gelatin | Excellent biocompatibility, mild processing | Swelling, diffusion, enzyme degradation | SSE, Bioprinting [55] |
| Lipids | Glyceryl dibehenate, Precirol | Solubility enhancement for BCS Class II drugs | Erosion, diffusion | SSE, MED [56] |
| Hydrogels | PEGDA, Alginate-PEG hybrids | High water content, cell encapsulation | Swelling, diffusion, stimulus-response | SLA, DLP, SSE [54] [56] |
| Composite Materials | Polymer-ceramic blends, Polymer-metal | Enhanced functionality, multi-modal release | Combined mechanisms | FDM, SLA, BJ-3DP [55] |
The relationship between material properties, printing technology, and drug release behavior follows predictable patterns that can be visualized through a logical framework. This understanding enables researchers to select optimal material-technology combinations for specific drug delivery requirements.
Diagram 2: Logical relationship between material selection, printing technology, structural attributes, and resulting drug release profiles in 3D-printed dosage forms.
The emergence of smart biomaterials that respond to physiological stimuli (pH, enzymes, temperature) represents the next frontier in personalized drug delivery [54] [51]. These advanced materials enable the development of dosage forms that release their payload in response to specific physiological conditions, such as the pH gradient along the gastrointestinal tract or enzyme concentrations at disease sites [55]. Additionally, bioinks—specially formulated materials incorporating biological components—have enabled the convergence of drug delivery with tissue engineering, creating opportunities for regenerative therapies that simultaneously administer drugs and facilitate tissue repair [54] [57].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and evaluation of 3D-printed drug delivery devices requires a specific set of research reagents and specialized materials. This toolkit encompasses printing materials, characterization reagents, bioactive agents, and analytical standards that enable researchers to fabricate, optimize, and validate personalized drug delivery systems [55] [52] [56].
Table 4: Essential Research Reagent Solutions for 3D Printing in Drug Delivery
| Reagent Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Pharmaceutical Polymers | PVA, PLA, PCL, HPMC, Eudragit series | Matrix former controlling drug release | PVA: Immediate release; PCL: Sustained release; Eudragit: Enteric coating [52] [56] |
| Bioinks | Gelatin methacryloyl, Alginate-PEG hybrids, Decellularized ECM | Cell-laden matrices for bioprinting | Enable fabrication of tissue constructs with embedded therapeutics [54] |
| Photoinitiators | 2,4,6-Trimethylbenzoyl, Lithium phenyl-2,4,6-trimethylbenzoyl | Crosslink hydrogels in vat polymerization | Critical for SLA/DLP processes; must demonstrate cytocompatibility [56] |
| Characterization Reagents | MTT, Alamar Blue, LDH assay kits | Biocompatibility and cytotoxicity assessment | Essential for safety profiling of printed dosage forms [55] |
| Dissolution Media | Simulated gastric/intestinal fluids, FaSSIF/FeSSIF | In vitro release testing | Biorelevant media for predicting in vivo performance [56] |
| Dimethoxy(dipropyl)stannane | Dimethoxy(dipropyl)stannane | C8H18O2Sn | Research Use | Dimethoxy(dipropyl)stannane is an organotin reagent for research, such as organic synthesis. For Research Use Only. Not for diagnostic or personal use. | Bench Chemicals |
Beyond the core materials listed above, specialized excipients play crucial roles in optimizing the performance of 3D-printed drug delivery systems. Plasticizers such as polyethylene glycol (PEG) and triethyl citrate are essential for modifying the mechanical properties of polymer filaments, particularly for FDM printing [56]. Porosity enhancers including mannitol and sodium chloride can be incorporated to create rapidly disintegrating formulations, especially beneficial for pediatric and geriatric populations [53] [52]. Release modifiers such as Kollidon VA64 and HPMC grades provide precise control over drug release kinetics, enabling the fabrication of dosage forms with tailored release profiles from immediate to sustained release over extended periods [56].
The selection of appropriate bioactive agents for research purposes must consider stability during the printing process. While small molecule drugs like acetaminophen, theophylline, and ibuprofen have been extensively studied in various 3D printing applications [56], researchers are increasingly exploring more complex biologics, including growth factors, therapeutic proteins, and even cells for advanced applications in regenerative medicine [54] [57]. The integration of nanoparticles and liposomes within 3D-printed structures represents another emerging frontier, combining the advantages of nanomedicine with the customization capabilities of additive manufacturing [55] [51].
The comparative analysis of 3D printing technologies and biomaterial systems for personalized drug delivery reveals a rapidly evolving landscape with significant potential to transform pharmaceutical development and patient care. Each printing technology offers distinct advantages—FDM for complex geometries, SSE for thermolabile compounds, BJ-3DP for high drug loading, and SLA for high-resolution structures—with the optimal choice dependent on the specific therapeutic requirements [52] [56]. The integration of artificial intelligence and machine learning approaches, as evidenced by studies predicting the printability of over 900 drug delivery systems, further enhances the capability to optimize formulations and printing parameters [58].
Future developments in this field will likely focus on several key areas: the expansion of biocompatible material libraries suitable for pharmaceutical printing, the advancement of multi-material printing capabilities for complex drug combination products, and the implementation of real-time quality control systems to ensure product consistency and safety [52] [51]. The emergence of 4D printing—where printed structures can change morphology or function in response to physiological stimuli—represents a particularly promising direction for creating intelligent drug delivery systems that dynamically interact with the biological environment [53]. Additionally, the regulatory framework for 3D-printed pharmaceuticals continues to evolve, with agencies like the FDA establishing pathways for approval as demonstrated by the landmark clearance of Spritam (levetiracetam) tablets in 2015 [53] [52].
As these technologies mature and overcome current challenges related to material selection, production speed, and regulatory standardization, 3D printing and biofabrication are poised to fundamentally reshape the pharmaceutical landscape. The transition from mass-produced medications to personalized drug delivery devices manufactured on-demand at hospital pharmacies or even local clinics represents the future of precision medicine, promising improved therapeutic outcomes, enhanced patient compliance, and more efficient healthcare delivery [53] [52] [51].
Navigating Translational Roadblocks: Scalability, Safety, and Barrier Penetration
The journey from a promising preclinical candidate to an approved clinical therapy is marked by a formidable challenge: high attrition rates. Current industry data reveals a stark reality, with the success rate for Phase 1 drugs plummeting to just 6.7% in 2024, a significant drop from 10% a decade ago [59]. This trend underscores a critical disconnect between preclinical success and clinical efficacy. The biopharmaceutical industry invests over $300 billion annually into research and development, supporting an unprecedented level of activity with over 23,000 drug candidates currently in development [59]. Despite this massive investment, diminishing R&D productivity threatens sustainable innovation, with the internal rate of return for R&D investment falling to 4.1% - well below the cost of capital [59].
This comparative analysis examines how advanced biomaterial systems for drug delivery can serve as a strategic tool to bridge this translational gap. By providing more controlled, targeted, and physiologically relevant therapeutic delivery, biomaterials offer the potential to enhance the predictive power of preclinical studies and improve clinical success rates. The following sections will quantitatively analyze attrition drivers, compare biomaterial platform efficacy, detail critical experimental methodologies, and visualize the integrated strategies needed to navigate the path from bench to bedside.
Quantitative Analysis of the Drug Development Pipeline
Understanding the precise points of failure within the drug development pipeline is essential for targeting improvement strategies. Attrition occurs at every stage, but the transition from preclinical to clinical phases presents particularly significant challenges. The table below summarizes key attrition metrics and their primary drivers across development phases.
Table 1: Drug Development Attrition Rates and Primary Causes
| Development Phase | Attrition Rate | Primary Causes of Failure |
|---|---|---|
| Preclinical Discovery | ~95% for novel drug discovery [60] | Inadequate physicochemical properties (e.g., poor solubility for ~90% of investigational compounds) [61]; Lack of efficacy in disease models |
| Phase I Transition | 93.3% (based on 6.7% success rate) [59] | Unexpected toxicity; Poor pharmacokinetics; Inadequate bioavailability |
| Clinical Phases (II-III) | ~50% due to lack of clinical efficacy [61] | Inefficacy in human populations; Safety issues emerging in larger cohorts; Suboptimal product profiles |
Beyond these overarching statistics, specific physicochemical challenges drive this attrition. Approximately 40% of marketed pharmaceuticals and nearly 90% of investigational compounds in the discovery pipeline exhibit poor water solubility, creating significant barriers to absorption and bioavailability [61]. This frequently results in inadequate plasma exposure, high inter-individual variability, and ultimate therapeutic failure despite promising preclinical results.
Comparative Analysis of Biomaterial Drug Delivery Systems
Advanced biomaterial systems are being engineered to specifically address the causes of clinical attrition by enhancing drug solubility, stability, targeting, and release kinetics. The following table provides a structured comparison of major biomaterial classes, their mechanisms, and their performance in addressing key translational challenges.
Table 2: Comparative Analysis of Biomaterial Platforms for Drug Delivery
| Biomaterial Platform | Key Mechanism of Action | Advantages for Translation | Documented Limitations |
|---|---|---|---|
| Nanocarriers(Liposomes, Dendrimers, PLGA NPs) | Target specific cells/tissues via EPR effect; Encapsulate drugs for protection [1] | Enhanced targeting accuracy; Minimized side effects; Improved therapeutic index [1] | Potential immune response; Bioaccumulation concerns; Scalability challenges [1] |
| Hydrogels(PEG, Hyaluronic Acid, Dextran) | 3D hydrophilic networks absorb water, enabling sustained drug release [62] | Minimally invasive application; Controlled release over time; Tunable properties [62] | Potential burst release; Harsh crosslinking components can damage protein therapeutics [62] |
| Bioresponsive Polymers & Nanogels(PNIPAM, PAA, Chitosan) | Respond to environmental stimuli (pH, temperature, enzymes) for triggered release [1] | Site-specific drug activation; Enhanced safety and efficacy; Adaptable to disease microenvironments [1] | Complex manufacturing; Batch-to-batch consistency challenges [1] |
| Amorphous Solid Dispersions(Spray-dried Dispersions) | Create high-energy amorphous drug forms to enhance dissolution [61] | Significantly improved bioavailability for poorly soluble compounds; Four-fold exposure increase documented [61] | Physical stability concerns; Conversion to crystalline form during storage |
| Lipid-Based Systems(SEDDS, SMEDDS) | Enhance solubilization and lymphatic transport of lipophilic drugs [61] | Improved absorption for BCS Class II/IV compounds; Reduced food effects | Drug loading limitations; Requires specialized manufacturing |
The translational impact of these systems is evidenced in clinical studies. For instance, in a first-in-human study for an ALS treatment, a spray-dried dispersion (SDD) formulation demonstrated a four-fold higher exposure compared to a conventional crystalline methylcellulose suspension, leading to its selection for further development [61]. Similarly, biomaterial-based protein delivery systems address critical stability challenges for biologics, protecting therapeutic proteins from enzymatic degradation and extending their circulation half-life [62].
Experimental Protocols for Evaluating Biomaterial Efficacy
Robust, predictive experimental models are essential for accurately assessing the clinical potential of biomaterial-based therapeutics before human trials. The following protocols represent state-of-the-art methodologies for evaluating biomaterial drug delivery systems.
Integrated Preclinical Screening Cascade
This multi-stage protocol leverages complementary models to build a comprehensive efficacy profile while validating biomarker hypotheses [60].
Initial High-Throughput Screening with PDX-Derived Cell Lines:
- Objective: Rapid assessment of compound efficacy across diverse genetic backgrounds and initial biomarker hypothesis generation.
- Methodology: Utilize panels of ≥500 genomically diverse cancer cell lines for drug response screening. Perform high-throughput cytotoxicity assays, drug combination studies, and correlate sensitivity with mutational status, copy number variation, and expression levels.
- Output: Dose-response curves (IC50 values); Correlation of genetic features with drug response to generate sensitivity/resistance biomarker hypotheses.
3D Validation Using Patient-Derived Organoids:
- Objective: Refine biomarker hypotheses and assess drug response in a more physiologically relevant 3D model that preserves tumor architecture.
- Methodology: Culture patient-derived tumor organoids in Matrigel or similar basement membrane matrix. Treat with therapeutic candidates across concentration ranges. Analyze using high-content imaging, viability assays, and multi-omics analysis (genomics, transcriptomics, proteomics) to validate and refine biomarker signatures.
- Output: 3D dose-response data; Mechanism of action confirmation; Refined predictive biomarker profiles.
In Vivo Validation Using Patient-Derived Xenograft (PDX) Models:
- Objective: Final preclinical validation of efficacy and biomarker strategy in an in vivo context that preserves tumor heterogeneity and microenvironment.
- Methodology: Implant patient tumor tissue into immunodeficient mice. Randomize mice into treatment and control groups upon established tumor growth. Administer biomaterial-formulated drug versus control. Monitor tumor volume, animal weight, and conduct pharmacokinetic/pharmacodynamic analyses.
- Output: In vivo efficacy data (tumor growth inhibition); Biodistribution and pharmacokinetic profiles; Final validated biomarker signatures for patient stratification.
Developability Classification System (DCS) Guided Formulation Screening
This systematic protocol addresses the pervasive challenge of poor solubility, a major cause of attrition [61].
Compound Classification:
- Objective: Categorize drug candidates based on their fundamental biopharmaceutical properties to guide formulation strategy.
- Methodology: Determine solubility and permeability parameters using biorelevant media. Classify compounds according to the Developability Classification System (DCS) as either dissolution-rate limited or solubility-limited.
Parallel Formulation Screening:
- Objective: Identify the optimal solubility-enhancement technology for the specific DCS class.
- Methodology: Screen multiple formulation approaches in parallel:
- Nano-milling: For particle size reduction of crystalline drugs.
- Amorphous Solid Dispersions: Evaluate both spray-dried dispersion (SDD) and hot-melt extrusion (HME).
- Lipidic Formulations: Screen self-emulsifying drug delivery systems (SEDDS) for highly lipophilic compounds.
In Vivo Pharmacokinetic Evaluation:
- Objective: Compare performance of lead formulations against a standard reference.
- Methodology: Conduct pharmacokinetic studies in relevant animal models. Administer equivalent doses of different formulations and measure plasma concentration over time. Key parameters: C~max~, T~max~, and AUC.
- Output: Relative bioavailability data; Selection of optimal clinical formulation.
Visualizing Workflows and Signaling Pathways
Integrated Preclinical Screening Workflow
The following diagram illustrates the multi-stage protocol for evaluating biomaterial drug delivery systems, from initial screening to in vivo validation.
Translational Pharmaceutics Development Pathway
This diagram outlines the integrated, adaptive approach to formulation development and clinical testing, which allows for real-time optimization.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development of biomaterial drug delivery systems requires specialized reagents and platforms. The following table details key solutions used in the featured experiments and this field of research.
Table 3: Essential Research Reagents for Biomaterial Drug Delivery Research
| Reagent / Material | Function in Research | Specific Application Example |
|---|---|---|
| PDX-Derived Cell Line Panels | Provide genetically diverse in vitro models for high-throughput drug screening [60] | Initial efficacy assessment and biomarker hypothesis generation [60] |
| Patient-Derived Organoids | 3D culture models that preserve tumor architecture and heterogeneity for intermediate validation [60] | Refining biomarker hypotheses and assessing drug response in a more physiologically relevant system [60] |
| Patient-Derived Xenograft (PDX) Models | In vivo models that closely mimic patient tumor biology for final preclinical validation [60] | Evaluating in vivo efficacy, pharmacokinetics, and final biomarker validation [60] |
| Biorelevant Media | Simulate gastrointestinal fluids for predicting in vivo solubility and dissolution [61] | Applying the Developability Classification System (DCS) to guide formulation strategy [61] |
| Spray-Dried Dispersion (SDD) Polymers | Matrix carriers for creating amorphous solid dispersions to enhance drug solubility [61] | Formulating poorly soluble compounds (e.g., BCS Class II) for improved exposure [61] |
| Lipid-Based Excipients | Components for self-emulsifying drug delivery systems (SEDDS) [61] | Enhancing absorption of highly lipophilic (high log P) drug compounds [61] |
| Stimuli-Responsive Polymers | Materials that undergo structural changes in response to biological stimuli (pH, enzymes) [1] | Designing bioresponsive nanogels for targeted drug release in specific disease microenvironments [1] |
The high attrition rate from preclinical success to clinical approval remains a formidable challenge in drug development. However, the strategic implementation of advanced biomaterial systems for drug delivery offers a promising path forward. As this comparative analysis demonstrates, platforms such as nanocarriers, hydrogels, and bioresponsive polymers can directly address the root causes of failure—inadequate bioavailability, poor targeting, and suboptimal pharmacokinetics.
The future of reducing attrition lies in the integration of predictive preclinical models, adaptive clinical trial designs like the Translational Pharmaceutics platform, and the application of artificial intelligence. AI and machine learning are already beginning to revolutionize biomaterial design by predicting nanoparticle degradation, optimizing drug release kinetics, and personalizing formulations based on patient-specific data [1]. Furthermore, regulatory evolution, such as the FDA's increased openness to advanced non-animal models, promises to accelerate the translation of these sophisticated delivery systems [60].
To truly bridge the translational gap, a holistic approach is essential. This involves leveraging the complementary strengths of various biomaterial platforms, employing cascading preclinical screening protocols, and maintaining flexibility to adapt formulations based on emerging clinical data. Through such integrated strategies, biomaterial drug delivery systems can significantly de-risk drug development, enhance therapeutic efficacy, and ultimately improve the probability that promising preclinical candidates will become approved clinical therapies.
The central nervous system (CNS) is protected by sophisticated biological barriers that maintain its homeostasis but also present a formidable challenge for drug delivery. The blood-brain barrier (BBB) and the blood-spinal cord barrier (BSCB) are the most well-studied of these interfaces, acting as highly selective gatekeepers that prevent most therapeutic agents from reaching their targets [63] [64]. These barriers are natural protective membranes that prevent toxins and pathogens in the blood from entering the CNS, but they also complicate pharmacotherapy for neurological disorders as an estimated >98% of small-molecule drugs and all macromolecular therapeutics are impeded from accessing the brain [63]. The BBB is considered the most restrictive endothelial barrier in the body, allowing passive diffusion primarily only for small (<400-600 Da), lipid-soluble molecules [65] [66].
While this review focuses primarily on the BBB and BSCB, it is important to note that similar barriers protect other sensory organs, including the blood-labyrinth barrier (BLB) of the inner ear, which shares many anatomical and functional characteristics with its CNS counterparts. Understanding the comparative structure and function of these barriers, along with the advanced strategies being developed to overcome them, is crucial for advancing the treatment of neurological and sensory disorders. Recent breakthroughs in materials science and nanotechnology have provided a powerful toolkit for targeted drug delivery, spurring the development of various functional materials and barrier-crossing strategies that will be explored in this comparative analysis [63] [55].
Anatomical and Physiological Comparison of Biological Barriers
The Blood-Brain Barrier (BBB)
The BBB is a spacious, multicellular, and dynamic semi-permeable membrane that isolates foreign substances in the blood from the CNS [63]. From a physiological perspective, the BBB is primarily composed of endothelial cells, astroglia, pericytes, and junctional complexes including tight junctions and adherens junctions [63]. The endothelial cells that form the core anatomical structure of the BBB differ significantly from peripheral endothelial cells in both morphology and function. They are fastened by extensive tight junctions, present no fenestrations (small transcellular pores), and contain higher numbers of mitochondria than peripheral endothelial cells, indicating greater energy requirements for transport [63]. These specialized endothelial cells also display a net negative surface charge, low expression of leukocyte adhesion molecules, and specialized transporters that collectively regulate the inflow and outflow of specific substrates [63].
Astrocytes, the most numerous glial cells in the CNS, connect with the basement membrane through their end feet and play a major role in dynamic signaling processes including waste clearance, blood flow regulation, ion homeostasis, and neuroimmune response balance [63]. Pericytes, embedded within the capillary basement membrane, are central to neurovascular unit function and play critical roles in modulating and maintaining the BBB, regulating cerebral blood flow, and managing vascular development and neuroinflammation [63]. The close communication between these cellular components through various signaling pathways ensures the integrity and proper function of the BBB.
The Blood-Spinal Cord Barrier (BSCB)
The BSCB is a semipermeable anatomical interface consisting of specialized small blood vessels that surround the spinal cord [64]. While similar to the BBB in both function and morphology, it is physiologically independent and possesses several distinct characteristics [64]. The BSCB shares the same basic cellular components as the BBB—endothelial cells, a basal membrane, pericytes, and astrocyte endfeet—but differs in their relative expression and functional properties [64].
In general, the BSCB is more permeable than the BBB, largely due to the relatively low expression of tight junction proteins like ZO-1 and occludin [64]. This increased permeability makes the BSCB more vulnerable to disruption and inflammation relative to the BBB, leaving the spinal cord susceptible to toxins that can inflict tissue damage [64]. This susceptibility is further exacerbated in BSCB endothelium through the relative downregulation of the critical efflux protein p-glycoprotein, thus slowing the elimination of toxins that penetrate the barrier [64]. These differences result in varying vulnerability to certain diseases and disorders affecting the CNS, with the BSCB playing a significant role in the development and progression of neurodegenerative diseases, spinal cord injury, pain conditions, and other neurological disorders [64].
Table 1: Comparative Anatomy and Physiology of CNS Barriers
| Characteristic | Blood-Brain Barrier (BBB) | Blood-Spinal Cord Barrier (BSCB) |
|---|---|---|
| Primary Cellular Components | Endothelial cells, astrocytes, pericytes, tight junctions | Endothelial cells, basal membrane, pericytes, astrocyte endfeet |
| Endothelial Tight Junctions | Extensive, high expression of ZO-1, occludin, claudin-5 | Less extensive, lower expression of ZO-1 and occludin |
| Basal Membrane | Present, contributes to cytoskeletal morphology | Present, similar composition and function |
| Overall Permeability | Highly restrictive | More permeable than BBB |
| Efflux Protein Expression | High P-glycoprotein expression | Relatively downregulated P-glycoprotein |
| Response to Cytokines | Less vulnerable to cytokine-mediated disruption | More vulnerable to disruption by cytokines |
| Key Transport Mechanisms | Passive diffusion, RMT, AMT, carrier-mediated transport | Similar mechanisms but with different efficiency |
Barrier Disruption in Pathological Conditions
Both the BBB and BSCB undergo significant changes under various pathological conditions that can alter their permeability and function. The BBB is known to be disrupted in conditions such as stroke, diabetes, seizures, multiple sclerosis, Parkinson's disease, and Alzheimer's disease [66]. This disruption often involves remodeling of the protein complexes in interendothelial junctions, leading to BBB breakdown [66]. Similarly, BSCB disruption plays an important role in primary and secondary injury processes related to spinal cord injury (SCI) [67]. After SCI, the structure of the BSCB breaks down, leading directly to leakage of blood components and increased permeability [67]. Within just five minutes following initial spinal cord injury, normally impermeable blood components like the large molecule albumin or red blood cells can be detected in spinal cord tissue, triggering an inflammatory response that extends the initial injury [64].
In neurodegenerative diseases, BSCB disruption has been found to precede and possibly initiate conditions like amyotrophic lateral sclerosis (ALS) and multiple sclerosis (MS) [64]. Patients with ALS have been shown to have decreased expression of tight junction proteins like ZO-1 and claudin-5, weakened tight junctions, and increased permeability of endothelial cell membranes [64]. These vasculature changes interestingly precede motor neuron death, indicating that BSCB breakdown may facilitate tissue damage rather than simply result from it [64].
Biomaterial Systems for Barrier Penetration
Classification and Properties of Drug Delivery Systems
The challenge of delivering therapeutic agents across biological barriers has spurred the development of various advanced drug delivery systems, particularly in the field of nanotechnology. These systems can be broadly classified into several categories based on their composition and physical properties, each with distinct advantages for CNS drug delivery.
Organic nanoparticles include systems composed of biodegradable polymers, proteins, carbohydrates, or lipids. Among these, poly(lactide-co-glycolide) (PLGA) nanoparticles have emerged as predominant polymeric drug carriers and are extensively investigated for biomedical applications in clinical studies [65]. PLGA nanoparticles have been shown to enhance drug penetration across the BBB in both in vitro and in vivo studies, with brain-targeted PLGA NPs reaching CNS neurons following systemic administration [65]. Albumin-based nanoparticles have also demonstrated significant potential in delivering drugs to target sites, enhancing drug accumulation, and overcoming drug resistance [65]. These are frequently utilized in brain research due to their enhanced permeability across the BBB, with chronic administration of oxytocin-loaded albumin-based NPs showing positive effects on hippocampal damage by enhancing neurogenesis and reducing apoptosis [65]. Lipid-based nanoparticles, particularly nanolipid carriers (NLCs), represent another frontrunner in drug delivery formulations, with high drug-loading capacity that makes them promising carriers for brain-targeted drug delivery [65].
Inorganic nanoparticles include systems composed of metals, metal oxides, ceramics, or semiconductors. While these offer unique properties for imaging and therapeutic applications, they often face greater challenges with biocompatibility and clearance compared to their organic counterparts. Recent research has focused on modifying these materials to improve their safety profiles while maintaining their functional advantages.
Table 2: Comparison of Biomaterial Systems for Barrier Penetration
| Biomaterial System | Composition | Size Range | Key Advantages | Limitations | BBB Penetration Efficiency |
|---|---|---|---|---|---|
| PLGA Nanoparticles | Biodegradable polyester copolymer | 100-300 nm | Biocompatible, controllable degradation, FDA-approved for some applications | Potential burst release, acidic degradation products | Enhanced penetration shown in vitro and in vivo |
| Albumin Nanoparticles | Natural protein (BSA/HSA) | 100-200 nm | Biocompatible, endogenous material, high drug loading | Stability challenges, potential immunogenicity | Significantly enhanced permeability across BBB |
| Nanolipid Carriers (NLC) | Lipid matrices with surfactants | 50-200 nm | High drug loading, improved stability, controlled release | Potential oxidation of lipids, production complexity | Promising for brain delivery, requires more investigation |
| Transferrin-Conjugated NPs | Albumin or other cores with Tf ligands | 150-400 nm | Active targeting through RMT, enhanced cellular uptake | More complex synthesis, potential receptor saturation | Significantly higher uptake in hBMECs in dose-dependent manner |
Active Targeting Strategies
Active targeting represents a sophisticated approach to enhance barrier penetration by functionalizing nanoparticles with specific ligands that interact with receptors naturally expressed on the barrier interfaces. One of the most extensively studied strategies is transferrin receptor (TfR)-mediated transcytosis, which facilitates the efficient delivery of therapeutic agents to the CNS [65]. This approach capitalizes on the natural mechanism by which transferrin crosses the BBB, hijacking this pathway for drug delivery.
Studies have demonstrated that transferrin-conjugated nanoparticles (BSA-Tf and HSA-Tf) show significantly higher uptake in human brain microvascular endothelial cells (hBMECs) compared to their non-targeted counterparts, with a clear dose-dependent relationship [65]. The internalization of these targeted systems occurs through receptor-mediated mechanisms, followed by transcytosis across the endothelial barrier. Beyond transferrin receptors, other targeting ligands have been explored, including peptides targeting specific CNS receptors, antibodies or antibody fragments against endothelial epitopes, and aptamers selected for their binding affinity to barrier components.
The effectiveness of active targeting strategies depends on multiple factors, including the density of receptors on the target cells, the affinity of the ligand-receptor interaction, the orientation and density of ligands on the nanoparticle surface, and the ability of the system to successfully navigate the transcytosis pathway without being trapped in endosomal compartments. Optimization of these parameters is crucial for developing successful targeted delivery systems for CNS applications.
Experimental Models and Methodologies for Barrier Assessment
In Vitro Models of Biological Barriers
Robust experimental models are essential for evaluating the penetration capacity of drug delivery systems across biological barriers. In vitro models using primary cells or cell lines have been developed to mimic the critical characteristics of these barriers while allowing for controlled experimentation. A common approach involves using human brain microvascular endothelial cells (hBMECs) as the primary barrier component, often in combination with other cell types to better recapitulate the native environment [65].
Advanced models incorporate multiple cell types in co-culture systems to more accurately represent the neurovascular unit. Triple co-culture models that include brain endothelial cells together with pericytes and astrocytes have been shown to develop tighter barriers with more physiological expression of transporters and junctional proteins compared to monocultures [68]. These systems provide a more comprehensive platform for evaluating how drug delivery systems interact with different cellular components of the barriers.
More recently, microfluidic systems and "brain-on-a-chip" technologies have emerged as sophisticated platforms that can incorporate fluid flow and mechanical stimuli to better mimic the in vivo conditions of biological barriers [68]. These systems allow for more realistic assessment of barrier permeability and nanoparticle transport while enabling real-time monitoring and high-resolution imaging of the interaction between delivery systems and barrier components.
Methodologies for Assessing Barrier Permeability and Nanoparticle Transport
Standardized methodologies are critical for obtaining comparable data on the permeability of biological barriers and the transport efficiency of drug delivery systems. Key techniques include:
Transendothelial Electrical Resistance (TEER) measurement is a widely used method to quantify the integrity and tightness of cellular barriers in real-time without causing damage. TEER values provide a quantitative measure of the formation and maintenance of tight junctions between endothelial cells, with higher values indicating tighter barriers [68].
Permeability assays using tracer molecules of various sizes provide direct measurement of barrier functionality. Commonly used tracers include fluorescently labeled or radio-labeled molecules such as sucrose, inulin, or albumin, which are applied to the apical compartment of transwell systems, and their appearance in the basolateral compartment is measured over time [68]. The permeability coefficient (Papp) can then be calculated to quantify barrier integrity.
Cellular uptake and internalization studies are performed using fluorescence-activated cell sorting (FACS) analysis, confocal microscopy, or electron microscopy to visualize and quantify the interaction between nanoparticles and barrier cells [65]. These studies can distinguish between surface-bound and internalized nanoparticles and provide insights into the mechanisms of uptake and intracellular trafficking.
Ultructural analysis using transmission electron microscopy (TEM) reveals detailed information about the subcellular localization of nanoparticles and their effects on cellular organelles. This approach has revealed notable differences between nanoparticle formulations and cell types, with autophagy emerging as a crucial mechanism for nanoparticle handling in pericytes and astrocytes [65].
Experimental Workflow for Barrier-NP Interaction Studies
Cytotoxicity and Biocompatibility Assessment
Ensuring the safety of drug delivery systems is paramount for their translational potential. Comprehensive assessment of cytotoxicity and biocompatibility is typically performed using a combination of methods:
Metabolic activity assays such as MTT, MTS, or WST-8 measure the activity of cellular enzymes involved in reduction reactions, providing an indication of cell viability and mitochondrial function after exposure to nanoparticles [65]. These colorimetric assays allow for high-throughput screening of nanoparticle toxicity across a range of concentrations.
Membrane integrity assays including lactate dehydrogenase (LDH) release measurement quantify the degree of cell membrane damage caused by nanoparticle exposure. Increased LDH in the culture medium indicates compromised membrane integrity and cytotoxic effects.
Oxidative stress assessment evaluates the generation of reactive oxygen species (ROS) in response to nanoparticle exposure, which can trigger inflammatory responses and compromise barrier integrity. Fluorescent probes such as DCFH-DA are commonly used for these measurements.
Studies have shown that at appropriate concentrations (e.g., 15.62 µg/mL, 31.25 µg/mL, and 62.5 µg/mL), various nanoparticle formulations including PLGA, albumin-based NPs, and nanolipid carriers caused no toxic effects on hBMECs, human brain vascular pericytes (hBVPs), or human astrocytes (hASTROs) after 3 hours of incubation [65]. However, the long-term effects and chronic exposure scenarios require more extensive investigation.
Key Research Reagents and Materials
The study of biological barriers and the development of strategies to overcome them relies on a specialized set of research reagents and materials. The following table summarizes essential tools and their applications in this field:
Table 3: Essential Research Reagents for Barrier Studies and Drug Delivery
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Primary Cells | In vitro barrier models | hBMECs, hBVPs, hASTROs [65] |
| PLGA | Biodegradable polymer for nanoparticles | Varying lactide:glycolide ratios (50:50, 75:25, 85:15) [65] |
| Albumin Proteins | Protein-based nanoparticle formulation | Bovine Serum Albumin (BSA), Human Serum Albumin (HSA) [65] |
| Transferrin | Active targeting ligand | Conjugated to nanoparticles for receptor-mediated transcytosis [65] |
| Lipid Formulations | Nanolipid carrier systems | Precirol, Compritol, Miglyol, surfactants [65] |
| TEER Measurement System | Barrier integrity assessment | Epithelial voltohmmeter, electrodes, transwell setups [68] |
| Tracer Molecules | Permeability studies | Fluorescent dextrans, sodium fluorescein, HRP, albumin [68] |
| Characterization Instruments | Nanoparticle physicochemical analysis | DLS (size, PDI), Zetasizer (zeta potential), TEM/SEM (morphology) [65] |
The comparative analysis of strategies for overcoming biological barriers, particularly the BBB and BSCB, reveals both challenges and opportunities in CNS drug delivery. While significant progress has been made in understanding the anatomical and physiological differences between these barriers, translating this knowledge into effective clinical treatments remains a work in progress. The development of advanced biomaterial systems, particularly various nanoparticle platforms, has provided powerful tools for enhancing drug delivery across these restrictive interfaces.
The future of this field lies in the continued refinement of targeted delivery systems that can selectively engage transport mechanisms without compromising barrier integrity. Combination approaches that leverage multiple crossing strategies simultaneously may offer enhanced efficacy, while personalized approaches based on individual barrier characteristics could optimize outcomes. Additionally, as our understanding of barrier biology in pathological conditions improves, opportunities for exploiting disease-specific changes in barrier properties will emerge.
Advanced imaging technologies and sophisticated in vitro models will continue to drive progress by enabling more accurate assessment of barrier penetration and therapeutic efficacy. The integration of artificial intelligence in designing and optimizing drug delivery systems represents another promising frontier. As these technologies mature, the goal of safely and effectively delivering therapeutics across biological barriers to treat CNS disorders appears increasingly attainable, potentially revolutionizing the treatment of neurological and sensory disorders that have long resisted conventional therapeutic approaches.
The advancement of biomaterial-based drug delivery systems represents a frontier in modern medicine, offering unprecedented control over therapeutic release and targeting. However, the clinical success of these systems hinges not only on their delivery efficiency but equally on their safety profile, particularly their potential to elicit toxic responses and undesirable immune activation. A comprehensive understanding of these aspects is crucial for selecting appropriate biomaterials for specific therapeutic applications.
When introduced into the biological environment, biomaterials interact with complex immune mechanisms that can determine their fate and functionality. These interactions range from acute inflammatory responses to chronic foreign body reactions that can compromise implant function and patient safety. Consequently, the field has evolved from developing merely bio-inert materials that minimize interaction to creating advanced bioactive and responsive systems that can actively modulate immune responses for improved integration and therapeutic outcomes [69] [70].
This guide provides a comparative analysis of toxicity and immune response profiles across major biomaterial classes, supported by experimental data and methodologies relevant to researchers and drug development professionals. By objectively evaluating these parameters, we aim to inform safer biomaterial selection and design strategies for next-generation drug delivery systems.
Comparative Toxicity and Immune Profiles of Biomaterial Systems
Different biomaterial classes exhibit distinct toxicity and immunogenicity profiles based on their composition, physical properties, and functionalization. The table below summarizes key experimental findings from comparative studies.
Table 1: Comparative toxicity and immune response profiles of selected biomaterials
| Biomaterial System | Experimental Model | Key Toxicity Findings | Immune Response Markers | Primary Organ Accumulation |
|---|---|---|---|---|
| Unconjugated Nanodiamonds | Female C57BL/6 mice (IV administration, 5-40 mg/kg) [71] | Favorable tolerability; Minimal inflammatory response [71] | Lowest CD69 expression in CD8+ T cells (0.12 ± 0.09); Minimal memory T cell activation [71] | Primarily heart tissue [71] |
| Gold Nanoparticles | Female C57BL/6 mice (IV administration, 5-40 mg/kg) [71] | Significant inflammatory response [71] | Highest CD69 expression in CD8+ T cells (0.40 ± 0.16); Elevated IL-6 and TNF-α at 2 hours [71] | Mainly left lung [71] |
| Quantum Dot Nanocarbons | Female C57BL/6 mice (IV administration, 5-40 mg/kg) [71] | Concentration-dependent toxicity concerns [71] | Highest CD25 expression (0.23 ± 0.04); Memory T cell activation [71] | Kidney, liver, blood, and heart [71] |
| Nanobody-Conjugated Nanodiamonds | Female C57BL/6 mice (IV administration, 5-40 mg/kg) [71] | Moderate inflammation at 2 hours post-dosing [71] | Highest total T cells (49.10% ± 6.99); Moderate inflammation [71] | Not specified in study [71] |
| Chitosan-based Systems | Preclinical models (varies by study) [72] [73] | Favorable biocompatibility; intrinsic antibacterial properties [72] [73] | Reduced inflammatory response; supports anti-inflammatory macrophage polarization [72] | Biodegradable; tissue-dependent clearance [73] |
| Polymeric Nanoparticles (PLGA) | Preclinical models (varies by study) [4] | Biocompatible with tunable degradation; potential acidity from degradation products [4] | Variable based on surface modification; generally low immunogenicity [4] | Liver and spleen (RES uptake) [4] |
Analysis of Comparative Data
The experimental data reveals significant differences in how various biomaterial systems interact with biological systems. Nanodiamonds, particularly unconjugated forms, demonstrate superior tolerability with minimal immune activation compared to other inorganic nanoparticles like gold and quantum dots [71]. This makes them promising candidates for applications where stealth properties are paramount.
Functionalization strategies significantly impact safety profiles, as evidenced by the increased immunogenicity of nanobody-conjugated nanodiamonds compared to their unconjugated counterparts [71]. This highlights the complex interplay between base material properties and surface modifications in determining overall biocompatibility.
Polymeric and natural biomaterials like chitosan generally exhibit favorable safety profiles, with the added benefit of intrinsic bioactive properties such as antimicrobial activity [72] [73]. However, their degradation kinetics and metabolic byproducts must be carefully considered in design parameters.
Methodologies for Assessing Toxicity and Immune Responses
Standardized experimental protocols are essential for generating comparable data on biomaterial safety profiles. The following section outlines key methodologies cited in the literature.
In Vivo Toxicity and Biodistribution Studies
The referenced study on nanodiamonds, gold nanoparticles, and quantum dot nanocarbons employed a comprehensive in vivo assessment protocol [71]:
- Animal Model: 22 female C57BL/6 mice
- Administration Route: Intravenous injection
- Dosing Strategy: Multiple concentrations (5, 10, 20, and 40 mg/kg) to evaluate dose-dependent effects
- Time Points: Sample collection at 2, 24, and 96 hours post-administration to assess acute and subacute responses
- Biodistribution Analysis: Tissue sampling to quantify nanoparticle accumulation in major organs
This protocol allows for comprehensive assessment of both immediate and delayed responses, providing insights into kinetic aspects of immune activation and clearance mechanisms.
Immune Cell Profiling via Flow Cytometry
Flow cytometry serves as a powerful tool for quantifying specific immune cell populations and activation states in response to biomaterial exposure [71]:
- T Cell Activation Markers: CD69 (early activation) and CD25 (interleukin-2 receptor) expression levels
- T Cell Subpopulations: Percentage of total T cells, CD4+ helper T cells, and CD8+ cytotoxic T cells
- Memory T Cell Activation: Assessment of memory T cell responses indicating adaptive immune engagement
- Cytokine Analysis: Measurement of pro-inflammatory cytokines (IL-6, TNF-α) as indicators of inflammatory responses
This methodology provides quantitative data on specific immune parameters rather than general inflammatory readouts, enabling precise characterization of immunomodulatory effects.
Computational Safety Assessment
Emerging computational approaches complement experimental methods in predicting biomaterial safety:
- Molecular Dynamics Simulations: Analyze nanoparticle stability in biological environments and predict interaction patterns with cellular components [74]
- AI-Driven Toxicity Prediction: Machine learning models trained on existing nanomaterial databases can forecast potential toxicity based on physicochemical properties [74]
- Molecular Docking Studies: Predict interactions between biomaterials and immune receptors to anticipate immunogenicity [74]
These in silico methods enable preliminary safety screening before extensive experimental investment, accelerating the development timeline for new biomaterials.
Table 2: Key methodologies for assessing biomaterial toxicity and immune responses
| Methodology | Key Parameters Measured | Applications in Biomaterial Assessment |
|---|---|---|
| In Vivo Dosing and Biodistribution | Organ accumulation, dose-dependent toxicity, clearance pathways [71] | Determination of pharmacokinetics, tissue-specific toxicity, and bioaccumulation potential |
| Flow Cytometry | Immune cell populations, activation markers (CD69, CD25), T cell subsets [71] | Quantitative analysis of specific immune responses, immunomodulatory effects |
| Cytokine Profiling | Inflammatory mediators (IL-6, TNF-α, IL-1β) [71] [69] | Assessment of inflammatory potential, both acute and chronic responses |
| Histopathological Analysis | Tissue structure, inflammatory cell infiltration, fibrosis [69] | Evaluation of tissue-level responses and foreign body reaction |
| Molecular Simulations | Binding affinities, interaction stability, release kinetics [74] | Prediction of biomaterial-behavior and potential immune interactions |
Strategic Mitigation of Toxicity and Immune Responses
Several strategic approaches have been developed to minimize adverse responses to biomaterials while maintaining therapeutic functionality.
Material Selection and Design Considerations
Surface Modification: PEGylation of nanoparticles reduces protein adsorption and opsonization, decreasing clearance by the reticuloendothelial system and minimizing non-specific immune activation [4] [75]
Biomimetic Approaches: Using marine-derived polymers like chitosan and alginate leverages their inherent biocompatibility and biodegradability, with additional bioactive benefits such as antimicrobial properties [73]
Smart Material Systems: Stimuli-responsive biomaterials that release immunomodulatory agents in response to specific environmental cues (pH, enzymes, temperature) enable localized immune modulation without systemic effects [70]
Active Immunomodulation Strategies
Advanced biomaterials can actively shape immune responses rather than simply avoiding detection:
Macrophage Polarization: Designing materials that promote a shift from pro-inflammatory M1 to anti-inflammatory M2 macrophage phenotypes to support tissue regeneration and reduce chronic inflammation [70]
Controlled Release of Immunomodulators: Incorporating anti-inflammatory cytokines (IL-4, IL-10) or small molecule inhibitors that can be released in a spatiotemporally controlled manner to dampen excessive immune activation [69]
Physical Property Modulation: Tailoring material stiffness, topography, and surface chemistry to influence immune cell adhesion, activation, and differentiation, leveraging the innate sensitivity of immune cells to physical cues [69]
Experimental Workflow and Signaling Pathways
The following diagrams visualize key experimental workflows and immune signaling pathways relevant to biomaterial safety assessment.
Biomaterial Immune Response Assessment Workflow
Biomaterial Immune Response Workflow
This workflow outlines the temporal progression of immune responses to biomaterials, from initial acute inflammation to potential chronic responses, along with key assessment methodologies at each phase.
Key Immune Signaling Pathways in Biomaterial Response
Immune Pathways in Biomaterial Response
This diagram illustrates key signaling pathways in immune responses to biomaterials, highlighting the divergence between pro-inflammatory (M1) and pro-regenerative (M2) macrophage polarization that significantly influences long-term outcomes.
Research Reagent Solutions for Safety Assessment
The table below catalogues essential research reagents and their applications in evaluating biomaterial toxicity and immune responses.
Table 3: Essential research reagents for assessing biomaterial safety
| Research Reagent | Function and Application | Experimental Context |
|---|---|---|
| Anti-CD69 Antibody | Flow cytometry marker for early T-cell activation [71] | Quantifying initial immune cell activation following biomaterial exposure |
| Anti-CD25 Antibody | Flow cytometry marker for IL-2 receptor (mid-stage T-cell activation) [71] | Assessing sustained T-cell response and proliferation capacity |
| IL-6 & TNF-α ELISA Kits | Quantification of pro-inflammatory cytokines in serum or tissue homogenates [71] | Measuring inflammatory response magnitude and kinetics |
| C57BL/6 Mouse Model | In vivo model for immunotoxicity and biodistribution studies [71] | Preclinical assessment of systemic responses and organ-specific accumulation |
| PLGA Nanoparticles | Biodegradable polymeric nanoparticle reference material [4] | Benchmarking against established biomaterial with known safety profile |
| Chitosan | Natural polysaccharide with intrinsic bioactive properties [72] [73] | Reference material for evaluating naturally-derived biomaterials |
The comparative analysis presented in this guide demonstrates significant differences in toxicity and immune response profiles across biomaterial classes. Nanodiamonds show particular promise with their favorable tolerability and minimal immune activation, while gold nanoparticles and quantum dots present greater challenges for clinical translation due to their inflammatory potential and organ-specific accumulation [71]. Natural polymers like chitosan offer an attractive balance of biocompatibility, biodegradability, and intrinsic bioactivity [72] [73].
Future directions in biomaterial safety optimization will likely involve increasingly sophisticated approaches to immune modulation, leveraging insights from immunology and materials science to design systems that actively promote tolerance and integration rather than merely avoiding detection. The combination of experimental assessment with computational prediction tools will accelerate the development of safer, more effective biomaterial-based drug delivery systems [74] [70].
By applying standardized assessment methodologies and leveraging the growing toolkit of immunomodulatory strategies, researchers can systematically advance the safety profile of biomaterial systems while maintaining their therapeutic efficacy, ultimately enabling more successful clinical translation.
Scalability and Manufacturing Hurdles in the Large-Scale Production of Biobased Nanomaterials
Biobased nanomaterials, derived from natural biological sources such as polysaccharides (cellulose, chitosan), proteins (albumin, silk fibroin), lipids, and other biomolecules, have emerged as a transformative platform in drug delivery systems [76]. These materials offer significant advantages including inherent biocompatibility, biodegradability, and reduced toxicity compared to conventional synthetic nanocarriers, making them particularly attractive for pharmaceutical applications [76]. The growing market for sustainable materials, predicted to surpass US$199.1 billion in 2025, underscores the increasing industrial interest in these materials [77]. However, a significant disconnect exists between laboratory-scale innovation and industrial-scale manufacturing, creating a critical bottleneck that impedes the clinical translation and commercial viability of these promising materials. This review provides a comparative analysis of the key scalability challenges and presents objective data on manufacturing hurdles that researchers must overcome to bridge this gap.
Core Scalability Challenges: A Comparative Analysis
The transition from laboratory synthesis to industrial production of biobased nanomaterials presents multifaceted challenges that impact both the economic viability and functional performance of the final product.
Technical and Operational Hurdles
Table 1: Comparative Analysis of Scalability Challenges for Biobased Nanomaterials
| Challenge Category | Laboratory-Scale Reality | Industrial-Scale Requirement | Impact on Final Product |
|---|---|---|---|
| Process Control | High degree of control over size, shape, and polydispersity [78] | Lack of reproducibility and control over intrinsic properties (size, morphology) during scale-up [78] | Batch-to-batch variability affecting drug loading, release kinetics, and biodistribution [79] |
| Synthesis Method | Bottom-up techniques (e.g., microfluidics) for high-quality nanomaterials [78] [80] | Dominance of top-down methods (e.g., mechanochemical milling) which can introduce defects [78] | Potential for heterogeneous size distributions, variable morphologies, and impurities [78] |
| Production Cost | Acceptable for research-grade materials (gram/hour possible with advanced methods) [81] | High costs of R&D and production for advanced smart materials [77] | Extremely high cost (e.g., gold nanoparticles at ~$80,000/gram vs. $50/gram for raw gold) [81] |
| Characterization & QA | Appropriate tools for assessing particle size, aggregation, and surface composition exist [82] | Need for enhanced quality control measures and consistent formulations with low variability [82] | Requires new data characterization methods and standards for nanoscale materials [82] |
The fundamental challenge lies in the "loss of control" phenomenon. While laboratory-scale synthesis, particularly through bottom-up approaches in the liquid phase, allows for precise engineering of nanomaterials with controlled size, morphology, and crystal structure, this precision diminishes significantly at the meso- and macro-scales required for industrial production [78] [81]. Techniques like microfluidics-assisted desolvation can produce uniform silk fibroin particles under 200 nm in a research setting [80], but maintaining this uniformity in large-volume reactors is exceptionally difficult. This reproducibility crisis is a primary barrier to regulatory approval and clinical translation, as batch-to-batch variability directly impacts critical quality attributes like drug loading efficiency, release profiles, and biological fate [79] [82].
Furthermore, the shift from sophisticated, control-oriented lab techniques to the more economically viable top-down methods like mechanical or mechanochemical milling for industrial production often results in nanomaterials with heterogeneous size distributions, variable morphologies, and introduced defects or impurities [78]. These compositional differences can alter the physicochemical properties that make nanomaterials desirable for drug delivery, such as their surface-area-to-volume ratio and reactivity [78].
Economic and Regulatory Hurdles
The high costs associated with research, development, and production of advanced nanomaterials present a significant market restraint [77]. The specialized equipment, pure starting materials, and energy-intensive processes required for synthesis contribute to exorbitant production costs, as illustrated by the dramatic price difference between raw gold and synthesized gold nanoparticles [81].
From a regulatory perspective, characterizing nanomaterials in medicines poses new challenges. Regulators like the FDA emphasize the need for appropriate tools to assess primary particle size, aggregation and agglomeration state, surface composition, and reactivity [82]. This necessitates enhanced quality control measures and robust evidence that a manufacturer can produce consistent formulations with low batch-to-batch variability—a requirement that is difficult to meet with current scaled processes [82]. The regulatory landscape is evolving from encouragement to enforcement, with initiatives like the EU's Ecodesign for Sustainable Products Regulation (ESPR) adding documentation overhead and turning sustainability attributes into mandatory specifications [77]. This environment often favors well-capitalized players with established data infrastructure, potentially squeezing out smaller innovators [77].
Synthesis and Scalability: Methodologies and Manufacturing Workflows
Understanding the fundamental synthesis approaches is crucial for diagnosing scalability issues. The following workflow illustrates the primary pathways for nanomaterial production and their associated scalability challenges.
Diagram 1: Nanomaterial Synthesis Pathways and Scalability. This workflow compares top-down and bottom-up manufacturing approaches, highlighting the inherent trade-off between production volume and material control.
Synthesis Methodologies: From Laboratory to Industry
Top-Down Methods involve reducing the size of bulk material until it reaches the nanoscale [78]. While relatively simple and capable of producing large quantities, these methods, including mechanical/mechanochemical milling and solid-state segregation, often result in significant environmental impact through waste generation and offer limited control over the final particle shape and structure [78]. For instance, mechanical milling can reduce average grain size from 50-100 µm down to 2-20 nm but typically yields products with heterogeneous sizes and morphologies containing impurities and defects [78].
Bottom-Up Techniques construct nanomaterials atom-by-atom or molecule-by-molecule through chemical reduction of molecular precursors [78]. These methods, including liquid phase (e.g., chemical synthesis, sol-gel) and vapor phase techniques (e.g., Chemical Vapor Deposition), are favored in research for producing high-quality nanomaterials with precisely controlled intrinsic properties [78]. They are fundamental for creating sophisticated drug carriers like lipid nanoparticles (LNPs) for mRNA delivery [80] and protein-based nanoparticles for anticancer therapy [80]. However, their translation to industrial scale is often hampered by complexity, cost, and low volumetric yield.
Emerging Scalable Production Technologies
Innovative approaches are being developed to overcome traditional scalability limitations:
- Microfluidics and Automated Platforms: The Langer group at MIT has devised a technique for producing gram amounts per hour of highly repeatable lipid-polymer nanoparticles using automated systems, representing a significant advancement toward therapeutic use [81].
- High-Throughput Robotic Synthesis: Initiatives like the BioPACIFIC MIP are integrating robotics and artificial intelligence to enable autonomous experimentation, dramatically reducing discovery timelines and accelerating the path from lab to application [83].
- Advanced Process Design: Companies like Cerion utilize a "design for manufacturing" (DFM) approach, which uses a phase/gate process to simplify, optimize, and improve nanomaterial design while preventing issues that impede scale-up or raise production costs [81].
Experimental Data: Quantifying the Scalability Challenge
Comparative Performance of Scalable Biobased Nanomaterials
Table 2: Experimental Performance Data of Biobased Nanomaterials in Drug Delivery
| Nanomaterial Type | Synthesis Method | Average Size (nm) | Drug Loading Capacity | Scale-Up Potential | Key Functional Findings |
|---|---|---|---|---|---|
| Silk Fibroin Particles (SFPs) [80] | Microfluidics-assisted desolvation | < 200 nm | Curcumin: 37%5-FU: 82% | Medium (requires specialized equipment) | Sustained release over 72 h; enhanced tumor necrosis with magnetic guidance in vivo. |
| Clarithromycin-Loaded Albumin NPs [80] | Bovine serum albumin nanoprecipitation | Not specified | Not specified | High (established protein chemistry) | Significant anticancer activity (A549 cells); minimal toxicity to healthy fibroblasts. |
| Chitosan-coated Lipid Vesicles [80] | Lipid film hydration & chitosan coating | Not specified | Not specified | Medium (multi-step process) | Superior anti-inflammatory & antioxidant effects vs. free drug in rat inflammation model. |
| Rutin-loaded Hyaluronic Acid NPs [80] | Modified nanoprecipitation | 179 - 209 nm | Not specified | Medium to High | Significant reduction in anthracycline-induced endothelial damage and inflammation markers. |
| Solid Lipid Nanoparticles (SLNs) [80] [75] | High-pressure homogenization / emulsion | 75 - 90 nm | mRNA: 95-100% | High (established methods) | Efficient mRNA delivery; vasoprotective effects; favorable biodistribution in models. |
The data reveals a critical pattern: nanomaterials with excellent drug delivery outcomes (e.g., high loading capacity, sustained release, enhanced efficacy) are often produced using sophisticated, control-oriented methods that present significant scale-up challenges. For instance, while SFPs show impressive functional performance, their production relies on microfluidics-assisted desolvation, which requires specialized equipment and may be difficult to implement at industrial scales [80].
Characterization and Biodistribution: The Critical Role of Physicochemical Properties
Table 3: Impact of Physicochemical Properties on Nanomaterial Biodistribution and Scalability
| Physicochemical Property | Impact on Drug Delivery Performance | Impact on Scalability & Characterization |
|---|---|---|
| Hydrodynamic Size [79] | Determines circulation time, tissue penetration, and cellular uptake. Optimal size often 10-150 nm for EPR effect. | Critical quality attribute; difficult to control uniformly at large scale; requires techniques like DLS, NTA. |
| Zeta Potential [79] | Affects colloidal stability, protein corona formation, and cellular interactions. | Key predictor in MLR-PBPK models; must be controlled for stability; batch-to-batch variation problematic. |
| Surface Coating [79] | (e.g., PEG) improves stability, reduces opsonization, and prolongs circulation. PEG is dominant coating type. | Adds complexity and cost to synthesis; requires precise conjugation chemistry; must be verified. |
| Particle Shape [79] | Influences margination, adhesion, and internalization. Spherical is most common (>50% in studies). | Difficult to control in top-down methods; affects flow and filtration behavior during manufacturing. |
Advanced modeling approaches, such as the Multivariate Linear Regression-Physiologically Based Pharmacokinetic (MLR-PBPK) framework, have demonstrated that key physicochemical properties including zeta potential, size, and coating are the most influential predictors of nanoparticle biodistribution, while core material and shape have lesser impacts [79]. This underscores the critical importance of precisely controlling these parameters during manufacturing—a major challenge in scale-up.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for Biobased Nanomaterial Development
| Reagent/Material Category | Specific Examples | Function in Development & Scaling |
|---|---|---|
| Biopolymer Building Blocks | Chitosan, Silk Fibroin, Albumin, Alginate, Hyaluronic Acid [76] [80] | Form the core matrix of the nanocarrier; provide biocompatibility and biodegradability. |
| Lipid Components | Phosphatidylcholine, Cholesterol, Poloxamers [80] | Form lipid bilayers (liposomes) or solid matrices (SLNs) for encapsulating diverse payloads. |
| Surface Modifiers | Polyethylene Glycol (PEG), Polysorbates, Hyaluronic Acid [80] [79] | Enhance stability, stealth properties, and targeting capability; reduce protein adsorption. |
| Crosslinkers & Stabilizers | Glutaraldehyde, Genipin, Tripolyphosphate | Improve mechanical stability of polymer nanoparticles and control drug release kinetics. |
| Characterization Standards | NIST Reference Materials, Fluorescent Dyes, ISO Protocols [82] | Enable accurate measurement of size, zeta potential, drug release, and biodistribution. |
This toolkit represents the foundational materials required for both initial development and subsequent scale-up of biobased nanodrug carriers. The selection of appropriate reagents, particularly bio-sourced polymers with consistent quality and scalable availability, is a critical first step in designing a translation-ready nanomedicine product.
The journey from laboratory innovation to commercially viable biobased nanomedicines is fraught with significant scalability hurdles. The core challenge remains the fundamental trade-off between the precise control achievable at small scales and the economic and practical demands of industrial manufacturing. Current data indicates that while sophisticated bottom-up synthesis methods yield nanomaterials with superior drug delivery performance, they often lack the scalability of less-controlled top-down approaches.
Future progress hinges on the adoption of innovative strategies that can bridge this divide. The integration of automation, artificial intelligence, and high-throughput experimentation [83], along with the implementation of "design for manufacturing" principles from the earliest stages of development [81], presents the most promising pathway forward. Furthermore, robust characterization and a deep understanding of the critical quality attributes that impact biological performance [79] will be essential for developing scalable processes that consistently produce safe and effective biobased nanomedicines. As these advanced manufacturing paradigms mature, they will ultimately accelerate the translation of these promising materials from the research bench to clinical applications, fully realizing their potential to revolutionize drug delivery.
Head-to-Head: A Data-Driven Comparison of Delivery System Efficacy and Performance
The efficacy of any therapeutic agent is profoundly influenced by the performance of its delivery system. For researchers and drug development professionals, selecting the appropriate biomaterial system requires a detailed, quantitative understanding of its stability, targeting accuracy, and controlled release profile. These parameters directly determine the therapeutic index, safety, and eventual clinical success of a drug product. This guide provides a comparative analysis of major advanced drug delivery systems—including nanoparticles, hydrogels, and extracellular vesicles (EVs)—by synthesizing experimental data on their key performance metrics. The objective is to offer a data-driven resource for the selection and development of biomaterial systems within the broader context of optimizing drug delivery efficiency.
Quantitative Performance Comparison of Drug Delivery Systems
The following tables summarize critical performance metrics for major drug delivery systems, based on recent experimental findings. These metrics provide a foundation for the comparative selection of platforms for specific therapeutic applications.
Table 1: Comparative Stability and Release Kinetics of Drug Delivery Systems
| Drug Delivery System | Encapsulation Efficiency (%) | Storage Stability | Release Kinetics | Key Stability Challenges |
|---|---|---|---|---|
| Polymeric Nanoparticles (e.g., PLGA) | 49-60% for coordinated drugs [84] | Varies by polymer degradation rate (e.g., PLGA degrades to lactic/glycolic acid) [85] | Controlled by polymer degradation; can be tailored from days to weeks [85] | Risk of drug leakage; batch-to-batch consistency during scale-up [85] |
| Liposomes | High for hydrophobic/amphiphilic drugs [84] | Membrane peroxidation can compromise stability [84] | Sustained release; can be triggered by ultrasound [84] | Susceptibility to oxidation; requires specialized storage conditions [84] |
| Extracellular Vesicles (EVs) | Dependent on parent cell and loading method [86] | Naturally stable in circulation; inherent lipid bilayer [86] | Sustained and targeted release via natural membrane fusion [86] | Heterogeneity of vesicle populations; standardization of isolation [86] |
| Stimuli-Responsive Hydrogels | High for hydrophilic drugs and biomolecules [87] | Swelling ratio and mechanical properties can change with environment [87] | Pulsatile or sustained release in response to specific stimuli (pH, enzyme) [2] [87] | Responsiveness must be finely tuned to pathological cues to avoid premature release [87] |
Table 2: Targeting Accuracy and Biodistribution Profiles
| Drug Delivery System | Targeting Mechanism | Evidence of Enhanced Permeability and Retention (EPR) | Active Targeting Strategies | Key Limitations in Targeting |
|---|---|---|---|---|
| Nanoparticles (General) | Passive (Size-dependent EPR) & Active (Ligand-functionalized) [84] | Gold-dendrigraft poly-l-lysine (DGL) nanoparticles (~200 nm) showed high tumor retention [84] | Surface conjugation of targeting ligands (e.g., peptides, antibodies) [84] [85] | Protein corona formation can mask targeting ligands [84] |
| Size-Switchable Nanoparticles | Initial small size for penetration, then aggregation for retention [84] | 200 nm particles degrade to sub-50 nm components for deep tumor penetration [84] | "Detachable PEG" coatings reveal cell-penetrating peptides after reaching target [84] | Aggregation may be influenced by in vivo environment and protein corona [84] |
| Extracellular Vesicles (EVs) | Innate homing to parent cell type; can be engineered [86] | MSC-EVs naturally target injured tissues (e.g., lung, liver, kidney) [86] | Engineered to display specific targeting proteins or peptides on their surface [86] | Off-target distribution depends on source cell and administration route [86] |
| Magnetic Hydrogel Microrobots | Externally guided by magnetic fields [2] | N/A (Active external steering) [2] | Directed to tumor site via external magnetic field for localized drug delivery [2] | Limited to relatively superficial tissues; requires specialized equipment [2] |
Experimental Protocols for Key Performance Assays
Protocol for Evaluating Controlled Release Profiles
Objective: To quantitatively measure the drug release kinetics from a delivery system under simulated physiological conditions, distinguishing between sustained and controlled release profiles. Sustained release is characterized by first-order kinetics (slow release over time), while controlled release follows zero-order kinetics (constant rate independent of drug concentration) [88].
Materials:
- Research Reagent Solutions: Phosphate Buffered Saline (PBS) at various pH levels (7.4, 6.5, 5.5); simulated body fluid (SBF); specific enzymes (e.g., Hyaluronidase, Matrix Metalloproteinases) to mimic pathological microenvironments [84] [87].
- Equipment: Dialysis membrane tubes or Franz diffusion cells; thermostatic shaking water bath; UV-Vis spectrophotometer or HPLC system for drug quantification.
Methodology:
- Sample Preparation: Precisely weigh a quantity of the drug-loaded formulation (e.g., nanoparticles, hydrogel slice) and suspend it in a release medium within a dialysis bag.
- Incubation: Immerse the dialysis bag in a large volume of release medium (sink condition) and agitate in a water bath maintained at 37°C.
- Sampling: At predetermined time intervals, withdraw a fixed volume of the external release medium for analysis and replace it with an equal volume of fresh medium to maintain sink conditions.
- Analysis: Quantify the drug concentration in the samples using a pre-calibrated analytical method (e.g., HPLC for accuracy, UV-Vis for convenience).
- Data Modeling: Plot the cumulative drug release (%) versus time. Fit the data to kinetic models (e.g., zero-order, first-order, Higuchi) to determine the release mechanism [89] [88].
Protocol for Assessing Targeting Accuracy and Cellular Uptake
Objective: To validate the specificity of a targeted drug delivery system towards its intended cells or tissues and quantify its internalization efficiency.
Materials:
- Research Reagent Solutions: Fluorescent dyes (e.g., DiI, FITC, Cy5) for labeling the delivery system; cell culture media; flow cytometry buffer; paraformaldehyde for fixation.
- Cell Lines: Target cells (e.g., cancer cell lines) and non-target control cells (e.g., normal fibroblast lines).
- Equipment: Flow cytometer; confocal laser scanning microscope (CLSM).
Methodology:
- Labeling: Tag the drug delivery system with a fluorescent dye according to established protocols.
- Incubation with Cells: Seed target and non-target cells in multi-well plates. Upon reaching 70-80% confluence, incubate them with the fluorescently labeled delivery system for a set period (e.g., 1-4 hours).
- Quantification (Flow Cytometry):
- After incubation, wash the cells thoroughly with PBS to remove non-internalized particles.
- Trypsinize the cells, resuspend in flow cytometry buffer, and analyze using a flow cytometer to determine the percentage of fluorescent-positive cells and the mean fluorescence intensity, which correlates with uptake amount [84].
- Visualization (Confocal Microscopy):
- Culture cells on glass-bottom dishes. After incubation and washing, fix the cells with paraformaldehyde.
- Stain cell nuclei (e.g., with DAPI) and actin cytoskeleton (e.g., with phalloidin) for context.
- Image using CLSM to visually confirm the intracellular localization of the delivery system [84].
Protocol for Testing Stability
Objective: To evaluate the physical and chemical stability of the drug delivery system under storage conditions and in physiological environments.
Materials:
- Equipment: Dynamic Light Scattering (DLS) instrument; Nanoparticle Tracking Analysis (NTA); HPLC; refrigerators and stability chambers.
Methodology:
- Physical Stability:
- Size and Zeta Potential: Use DLS to measure the hydrodynamic diameter, polydispersity index (PDI), and zeta potential of the system at time zero and after storage under various conditions (e.g., 4°C, 25°C). Significant changes indicate aggregation or instability [86] [85].
- Morphology: Use transmission electron microscopy (TEM) to visually assess changes in morphology and confirm the absence of aggregation.
- Chemical Stability:
- Drug Integrity: Use HPLC to analyze the chemical integrity of the encapsulated drug after extraction from the system following storage. This identifies any degradation products.
- Carrier Integrity: For systems like liposomes, monitor for peroxidation by assessing thiobarbituric acid reactive substances (TBARS). For polymers like PLGA, monitor the pH of the suspension as degradation produces acidic byproducts [84] [85].
- For EVs: Utilize NTA for particle concentration and size distribution, and western blotting for the presence of specific EV marker proteins (e.g., CD63, TSG101) to confirm integrity [86].
Visualization of Key Concepts and Workflows
Signaling Pathways in Stimuli-Responsive Drug Release
Experimental Workflow for System Performance Evaluation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for Advanced Drug Delivery System Research
| Research Reagent / Material | Primary Function in Research | Key Considerations |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | A biodegradable and FDA-approved polymer for constructing nanoparticles and microspheres that provide sustained drug release [84] [85]. | The lactic acid to glycolic acid ratio (L:G) determines degradation rate and drug release kinetics [85]. |
| PEG (Poly(ethylene glycol)) | Used for "PEGylation" — coating the surface of delivery systems to reduce opsonization, prolong circulation time, and enhance stability [84]. | "Detachable PEG" systems can be designed to shed upon reaching the target site to improve cellular uptake [84]. |
| Phospholipids (e.g., DSPC, DOPC) | The fundamental building blocks of liposomal bilayers and lipid nanoparticles (LNPs), determining membrane fluidity and stability [84]. | Lipid purity and composition critically impact drug encapsulation efficiency and in vivo behavior [84] [85]. |
| Stimuli-Responsive Polymers (e.g., PNIPAM) | Form the basis of "smart" hydrogels and nanogels that undergo swelling/collapse in response to temperature, pH, or other triggers for controlled release [85] [87]. | The Lower Critical Solution Temperature (LCST) must be finely tuned to be relevant to physiological conditions [87]. |
| Hyaluronic Acid (HA) | A natural polysaccharide used in hydrogels and as a targeting ligand for CD44-overexpressing cancer cells; also degradable by hyaluronidase [84]. | Serves a dual function as both a structural matrix and an active targeting moiety [84]. |
| Cell-Penetrating Peptides (CPPs) | Short peptides (e.g., TAT) conjugated to delivery systems to enhance their cellular internalization and overcome bioavailability barriers [84]. | Can sometimes lack cell-type specificity and require careful design to minimize off-target uptake [84]. |
| Matrix Metalloproteinase (MMP) Substrates | Peptide linkers (e.g., cleavable by MMP-2/9) used as crosslinkers in hydrogels or between a drug and its carrier for enzyme-triggered release in diseased tissues [84]. | Specificity for the target enzyme is crucial to prevent unintended cleavage and release [84]. |
| Mesenchymal Stem Cells (MSCs) | A primary cell source for deriving natural extracellular vesicles (MSC-EVs) with inherent anti-inflammatory and tissue-homing properties [86]. | Source (e.g., umbilical cord, bone marrow), passage number, and culture conditions significantly influence EV properties [86]. |
The development of advanced drug delivery systems (DDS) represents a pivotal frontier in modern therapeutics, aiming to enhance drug efficacy, reduce side effects, and improve patient compliance. Among the most promising biomaterial-based platforms are nanoparticles, hydrogels, microneedles, and biodegradable polymers, each offering distinct mechanisms and advantages for targeted therapeutic delivery. This review provides a systematic comparative analysis of these four drug delivery systems, evaluating their unique characteristics, drug delivery efficiency, and applicability across various biomedical contexts. By synthesizing recent high-quality research, this article aims to serve as a reference for researchers and drug development professionals in selecting and optimizing biomaterial platforms for specific therapeutic challenges.
Comparative Characteristics of Drug Delivery Systems
The table below summarizes the core characteristics, advantages, and primary challenges of the four drug delivery systems based on current research.
Table 1: Comparative analysis of drug delivery systems
| Delivery System | Core Characteristics | Key Advantages | Primary Challenges |
|---|---|---|---|
| Nanoparticles [90] [91] [74] | • Size: 1-100 nm• High surface-to-volume ratio• Composed of lipids, polymers, or metals | • Enhanced cellular uptake• Tunable drug release kinetics• Ability to cross biological barriers (e.g., BBB)• Potential for active targeting | • Potential cytotoxicity without clear mechanisms [90]• Scalability and reproducibility issues [91]• Rapid clearance by the immune system |
| Hydrogels [92] [91] [93] | • 3D cross-linked polymer networks• High water content• Porosity: 5-200 μm [93] | • High biocompatibility• Mimics native extracellular matrix• Stimuli-responsive drug release (pH, temperature)• Injectable formulations for minimally invasive delivery | • Low mechanical stability [93]• Needle clogging in injectable forms [93]• Balancing biocompatibility & biodegradability [93] |
| Microneedles (MNs) [94] [95] [96] | • Height: 100-1500 μm• Arrayed needle tips• Various types: solid, coated, hollow, dissolving, hydrogel-forming | • Minimally invasive and painless• Bypasses stratum corneum barrier• High patient compliance• Avoids first-pass metabolism | • Poor control over delivery depth [96]• Inadequate regulation of immune effects [96]• Industrial-scale manufacturing |
| Biodegradable Polymers [97] | • Synthetic (e.g., PLGA, PCL, PLA) or natural (e.g., chitosan, collagen) origin• Degrade into biocompatible byproducts | • Controlled drug release via degradation• No need for surgical removal• Excellent tissue compatibility• Wide range of degradation rates | • In vivo degradation rate may not match drug release needs [97]• Potential local acidity from degradation byproducts (e.g., PLGA) |
Drug Delivery Mechanisms and Experimental Data
Quantitative Performance Metrics
Recent studies provide quantitative data on the performance of these systems. The following table compiles key experimental findings.
Table 2: Experimental performance data of different drug delivery systems
| Delivery System | Therapeutic Load | Key Experimental Findings | Reference Model |
|---|---|---|---|
| Nanoparticles | DNase I & Sivelestat | • Targeted delivery to >80% of lung neutrophils• Significant suppression of lung inflammation and early fibrosis | SARS-CoV-2 mouse model [98] |
| Hydrogel Nanoparticles | Chemotherapeutic drugs | • Enhanced drug solubility and bioavailability• pH-responsive release in tumor microenvironment | Cancer therapy models [91] |
| Dissolving Microneedles (MNs) | Peptide vaccine (TMV-PEP3) | • Effective induction of specific antibodies and cytotoxic T-cell responses | Triple-negative breast cancer model [96] |
| Hydrogel-Forming MNs | Nanoparticles | • Improved drug loading capacity and controlled-release kinetics• Enhanced stability of carried therapeutics | Transdermal drug delivery [95] |
| Injectable Hydrogel | Insulin | • Sustained release: 47.4%-53.36% over 6.5 hours• Non-Newtonian, shear-thinning rheology | Chronic wound therapy [92] |
| Biodegradable Polymer | Lornoxicam (LRX) | • Significant decrease in pro-inflammatory cytokines (IL-1β, TNF-α)• Promoted cartilage regeneration | Rat knee osteoarthritis model [97] |
Mechanisms of Action and Pathways
The following diagram illustrates the general workflow for developing and testing a novel drug delivery system, integrating key steps from the referenced studies.
Diagram 1: General workflow for developing and testing a novel drug delivery system, integrating key steps from the referenced studies.
Different systems employ distinct pathways for drug delivery. Nanoparticles designed for neurological applications utilize the nose-to-brain pathway, bypassing the blood-brain barrier (BBB) [90]. The diagram below details this mechanism.
Diagram 2: The nose-to-brain pathway utilized by nanoparticles for direct CNS delivery, bypassing the BBB.
Microneedles (MNs) create microchannels in the skin for enhanced drug delivery or biosensing [95] [96]. The following diagram classifies the main types of MNs and their fundamental drug release/fluid extraction mechanisms.
Diagram 3: Classification of microneedles and their primary mechanisms of action.
Detailed Experimental Protocols
Protocol: Fabrication of Nanoparticles-Incorporated Hydrogel Microneedles (NPs-HMN)
This protocol is adapted from studies on combining nanoparticles with hydrogel MNs to create synergistic systems [94].
Step 1: Nanoparticle Synthesis and Drug Loading
- Synthesize lipid or polymeric nanoparticles via nano-precipitation or emulsion methods.
- Load therapeutic agents (e.g., hydrophobic drugs, proteins) into the nanoparticles.
- Characterize the nanoparticles for size, zeta potential, and drug loading efficiency.
Step 2: Hydrogel Matrix Preparation
- Prepare an aqueous solution of hydrogel-forming polymers (e.g., hyaluronic acid, PVA).
- Mix the drug-loaded nanoparticles uniformly into the polymer solution.
Step 3: Microneedle Molding and Casting
- Pour the nanoparticle-polymer mixture into a polydimethylsiloxane (PDMS) mold containing microcavities.
- Apply centrifugation or vacuum to ensure the mixture fully fills the needle tips.
Step 4: Cross-Linking and Demolding
- Induce cross-linking physically (e.g., via cooling) or chemically (e.g., using cross-linkers) to solidify the hydrogel.
- Carefully demold the resulting NPs-HMN patch and dry for storage.
Protocol: Evaluating Intranasal Nanoparticle Delivery for Brain Targeting
This protocol outlines key steps for assessing the efficacy of nose-to-brain drug delivery [90].
Step 1: Formulation Optimization
- Engineer nanoparticles with appropriate size (typically < 200 nm) and surface charge.
- Modify the nanoparticle surface with mucoadhesive agents (e.g., chitosan) or targeting ligands.
Step 2: In Vivo Administration and Tracking
- Administer the fluorescently or radio-labeled nanoparticle formulation to animal models (e.g., mice) via the intranasal route.
- Compare with intravenous administration as a control.
Step 3: Biodistribution and Efficacy Analysis
- At predetermined time points, euthanize the animals and collect major organs (brain, liver, spleen, lungs).
- Quantify nanoparticle concentration in different brain regions (e.g., olfactory bulb, cortex) and other organs using imaging or analytical techniques.
- Measure the concentration of the delivered therapeutic agent in the same tissues and assess the resulting pharmacological effect.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key materials and reagents used in the development of the discussed drug delivery systems, as derived from the referenced studies.
Table 3: Key research reagents and materials for drug delivery system development
| Reagent/Material | Function in Research | Example Applications |
|---|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) [92] [97] | Biodegradable polymer for controlled drug release; forms microspheres and nanoparticles. | Dental surgery drug delivery [92]; knee osteoarthritis therapy [97] |
| Hyaluronic Acid (HA) [95] [97] | Natural polymer for hydrogels and dissolving MNs; biocompatible and similar to ECM. | Intervertebral disk regeneration [92]; wrinkle-removing MNs [95] |
| Lipid Nanoparticles (LNPs) [98] | Versatile carrier for encapsulating drugs and nucleic acids; enables cell-specific targeting. | Targeted delivery to lung neutrophils [98] |
| Polyvinyl Alcohol (PVA) [95] [97] | Water-soluble polymer used as a coating or matrix for MNs and hydrogels. | Coating for MNs to minimize post-use skin punctures [95]; modified PVA (PVAC) for KOA [97] |
| Sepineo P 600 / PHD 100 [92] | Commercial gelling polymers used to formulate dermatological hydrogels for sustained release. | Insulin hydrogel carrier for chronic wounds [92] |
| Chitosan (CS) [97] | Natural biodegradable polymer with antimicrobial properties; used in nanoparticles and scaffolds. | Bone tissue repair and treatment of KOA [97] |
| Poly(ε-caprolactone) (PCL) [97] | Synthetic, biodegradable polyester with slow degradation rate; used for long-term drug release. | Treatment of knee osteoarthritis [97] |
This comparative analysis demonstrates that nanoparticles, hydrogels, microneedles, and biodegradable polymers each occupy a unique and valuable niche in the drug delivery landscape. The optimal choice is contingent on the specific therapeutic application, target tissue, and desired release profile. Future advancements will likely focus on hybrid systems that combine the strengths of multiple platforms, such as nanoparticle-incorporated hydrogel microneedles [94] or injectable hydrogels containing drug-loaded biodegradable polymers [97]. Furthermore, the integration of computational design, artificial intelligence, and Quality by Design (QbD) principles [74] [92] will be crucial in optimizing these complex systems for clinical translation, ultimately enabling more precise, effective, and patient-friendly therapies.
Biomaterials science represents a cornerstone of modern therapeutic innovation, profoundly impacting drug delivery and regenerative medicine. The convergence of materials science, nanotechnology, and biotechnology has catalyzed the development of advanced systems capable of spatiotemporal control over therapeutic agent release, thereby enhancing treatment efficacy and patient outcomes. This interdisciplinary field has evolved from simple inert structures to sophisticated bioactive platforms that actively interact with biological systems [55] [99]. The global biomaterials market, valued at approximately $171.35 billion in 2024, is projected to expand at a compound annual growth rate of 11.82%, underscoring the field's rapid development and significant economic impact [99]. Despite exponential growth in research output, a comprehensive, data-driven overview of the scholarly landscape has been lacking. This vicennial bibliometric analysis systematically examines the evolution of biomaterials research from January 2005 to December 2024, mapping publication trends, geographical distributions, institutional contributions, and emerging frontiers. By providing a structured framework for navigating this complex landscape, this work aims to identify established paradigms and promising research directions, offering valuable insights for researchers, policymakers, and healthcare professionals invested in the future of biomaterial-driven therapies [100] [101].
Methodology: Bibliometric Data Collection and Analysis Framework
This analysis employed a rigorous bibliometric methodology to ensure comprehensive and reproducible mapping of the biomaterials research landscape. Data retrieval was conducted using the Science Citation Index Expanded (Web of Science Core Collection), encompassing articles and reviews published between January 1, 2005, and December 31, 2024 [100] [101]. The search strategy incorporated key terminology related to biomaterials, regenerative medicine, and drug delivery systems to capture the interdisciplinary nature of the field.
Analytical Tools and Techniques: Multiple software platforms were leveraged to extract and visualize different dimensions of the bibliometric data. The analytical workflow incorporated:
- Bibliometrix (R-package): For fundamental bibliometric indicators and descriptive statistics, including annual publication trends and citation analyses [101].
- VOSviewer: For constructing and visualizing collaborative networks among countries, institutions, and authors, as well as for mapping keyword co-occurrence patterns to identify research fronts [101].
- CiteSpace: For conducting temporal analyses of research contributions and detecting emerging trends through burst detection algorithms [101].
- Python and OriginPro: For data processing, cleaning, and generating high-quality visualizations of quantitative trends [102].
The analytical framework focused on several key metrics: publication volume and growth trajectory, geographical and institutional productivity, citation counts and H-index measurements, journal distribution and Bradford's Law zoning, and keyword evolution to track thematic shifts. This multi-faceted approach enabled both quantitative assessment of scholarly impact and qualitative interpretation of the field's intellectual structure and dynamic progression over the twenty-year period [100] [101].
Global Research Output and Geographical Distribution
The bibliometric analysis revealed a total of 885 scholarly publications on biomaterial-driven regenerative drug delivery between 2005 and 2024, demonstrating a remarkable acceleration in research activity. Annual publication output first exceeded 50 articles in 2017, surpassed 100 in 2024, and peaked at 116 publications in 2023. This trajectory reflects a maximum annual growth rate of 32.4%, with a particularly sharp increase observed during the COVID-19 pandemic, suggesting that global health challenges stimulated innovation in this domain [101]. Citation impact metrics indicated an average of 9.41 citations per publication annually, with the highest impact observed in 2010 at 16.71 citations per year, potentially signaling the publication of foundational works that continue to influence the field [101].
Table 1: Top 10 Most Productive Countries/Regions in Biomaterials Research (2005-2024)
| Rank | Country/Region | Publications | Total Citations | H-index |
|---|---|---|---|---|
| 1 | USA | 259 | Leading | 78 |
| 2 | China | 175 | Secondary | 51 |
| 3 | India | 76 | Secondary | - |
| 4 | Iran | - | - | 30 |
| 5 | Australia | - | High Average | - |
| 6 | Italy | - | High Average | - |
| 7 | Germany | Significant | - | - |
| 8 | United Kingdom | Significant | - | - |
| 9 | France | Significant | - | - |
| 10 | South Korea | Significant | - | - |
Seventy-seven countries/regions contributed to the global research output, with the United States establishing clear dominance in both productivity and influence. China emerged as a formidable second-tier contributor, followed by India. When measuring research impact through H-index metrics, the United States maintained leadership (H-index=78), with China (H-index=51) and Iran (H-index=30) completing the top tier [101]. Notably, Australia and Italy demonstrated exceptional performance in average citation rates, ranking second and third respectively, indicating highly influential research despite potentially lower publication volumes [101]. Network analysis identified the United States and China as central nodes in global research collaboration, with Germany, the United Kingdom, France, India, Italy, South Korea, and Australia comprising additional key contributors. This collaborative network exhibits extensive globalization patterns, featuring three principal knowledge exchange hubs: North America, Europe, and East Asia, highlighting the intercontinental nature of contemporary scientific cooperation in biomaterials research [101].
Leading Institutions and Their Collaborative Networks
The institutional landscape for biomaterials research encompasses over 1,300 participating organizations worldwide, with a clear hierarchy emerging among the most productive centers. Harvard University and the University of California System shared the top position as the most productive institutions, each with 26 publications during the analysis period [101]. They were closely followed by the Chinese Academy of Sciences (24 publications) and Universidade do Minho (20 publications), demonstrating the global distribution of research excellence.
Table 2: Top 10 Institutions in Biomaterials-Driven Regenerative Drug Delivery Research
| Rank | Institution | Publications | Collaboration Network |
|---|---|---|---|
| 1 | Harvard University | 26 | Extensive global ties |
| 2 | University of California System | 26 | Central node in North America |
| 3 | Chinese Academy of Sciences | 24 | Primary hub in East Asia |
| 4 | Universidade do Minho | 20 | European collaborator |
| 5 | Zhejiang University | - | Secondary hub in East Asia |
| 6 | National University of Singapore | - | Knowledge hub in Southeast Asia |
| 7 | Seoul National University | - | - |
| 8 | Yonsei University | - | - |
| 9 | Pusan National University | - | - |
| 10 | Korea University | - | - |
Collaborative network mapping revealed three predominant knowledge hubs centered around the Chinese Academy of Sciences, Zhejiang University, and the National University of Singapore [101]. Citation network analysis demonstrated dense interconnection patterns among high-output institutions, suggesting reciprocal citation behaviors that reinforce their disciplinary leadership. Temporal network visualization tracked the progressive expansion of research contributions, with China, the United States, and European nations driving biomaterial-focused advances in regenerative drug delivery systems [101]. Asian institutions demonstrated particularly strong growth, with several Korean universities, including Seoul National University, Yonsei University, Pusan National University, and Korea University, establishing significant research output as reflected in journal publications [103]. These multi-dimensional visualizations confirm two critical trends: the formation of self-reinforcing academic ecosystems among top-tier institutions, and the increasing globalization of interdisciplinary research in advanced therapeutic development [101].
Key Research Domains and Journal Dissemination
Biomaterials research disseminates through a diverse array of scholarly journals, with the analysis encompassing 324 journals that contributed to global research dissemination. ACTA Biomaterialia and Biomaterials emerged as the predominant sources in this domain, serving as core dissemination channels for high-impact research [101]. The remaining high-yield journals primarily concentrated on biomaterial engineering, molecular sciences, and pharmaceutical delivery systems. Application of Bradford's law of scattering stratified journals into three distinct zones, identifying 19 core dissemination channels within Zone 1 that accounted for the majority of impactful publications [101].
Table 3: Dominant Research Areas in Biomaterials Science
| Research Domain | Representative Topics | Significance |
|---|---|---|
| Materials Science | Polymer synthesis, Nanomaterial fabrication, Smart biomaterials | Foundation for developing novel delivery systems |
| Biomedical Engineering | Implantable devices, Tissue scaffolds, Medical devices | Application-focused research for clinical translation |
| Chemistry & Polymer Science | Biopolymer design, Hydrogel chemistry, Degradation kinetics | Enables controlled release and biocompatibility |
| Nanotechnology | Nanoparticles, Nanofibers, Liposomes | Enhances targeting and bioavailability of therapeutics |
| Tissue Engineering & Regenerative Medicine | 3D bioprinting, Organoids, Stem cell therapy | Promotes tissue repair and functional restoration |
Research domain analysis using VOSviewer revealed that the dominant research domains include Materials Science, Engineering, Chemistry, Polymer Science, and Science Technology Other Topics [101]. These focal areas underscore the primary directions of current research and point to promising avenues for future advancements in the field. The interdisciplinary nature of biomaterials research is evident in the convergence of these traditionally distinct domains, facilitating innovations such as bioactive glasses for drug delivery, biopolymer-based nanoparticles for targeted therapy, and conductive polymers for neural interfaces [55] [104]. The journal Biomaterials Research, with an Impact Factor of 8.1 and SCIMAGO SJR of 1.439, exemplifies this interdisciplinary focus, publishing primarily on nanotechnology, biomedical engineering, tissue engineering, and chemical engineering aspects of biomaterials [103]. This domain distribution highlights the field's evolution from fundamental material characterization toward application-driven research with strong clinical translation potential.
Experimental Protocols in Biomaterials Research
Bibliometric Analysis Workflow
The experimental protocol for conducting bibliometric analysis in biomaterials research involves a systematic, multi-stage process that ensures comprehensive data collection and robust analysis [101]. The first stage involves data retrieval from authoritative databases such as Web of Science and Scopus using carefully constructed search queries that incorporate key terminology related to biomaterials, drug delivery, and regenerative medicine. The second stage encompasses data cleaning and standardization, where records are deduplicated, metadata is harmonized (e.g., unifying institution names and country designations), and document types are categorized. The third stage implements quantitative analysis using specialized software tools like Bibliometrix, VOSviewer, and CiteSpace to examine publication trends, citation patterns, and collaboration networks. The final stage involves visualization and interpretation, where network maps, thematic evolution diagrams, and geographical distributions are generated to extract meaningful insights about the intellectual structure and dynamic progression of the research field [101] [102].
Biomaterials Characterization and Testing
Beyond bibliometric analysis, experimental research in biomaterials employs standardized methodologies to evaluate material properties and biological responses. Key techniques include:
- Mechanical Testing: Utilizing systems like the Mach-1 mechanical tester for multiaxial assessment of compression, tension, bending, shear, friction, and torsion properties of biomaterials and tissues [105].
- Surface Characterization: Employing contact angle goniometers and surface tensiometers to analyze wettability, surface energy, and adhesion properties that influence biocompatibility and cellular interactions [105].
- Biological Response Evaluation: Implementing molecular biology techniques including recombinant DNA technology, polymerase chain reaction (PCR), in situ hybridization, and immunocytochemistry to detect and quantify gene and protein expression related to inflammation and tissue regeneration [99].
- Microstructural Analysis: Leveraging advanced imaging technologies such as low-voltage electron microscopy (LVEM) and atomic force microscopy (AFM) for high-resolution characterization of material topography and cellular interactions at nano-scale resolutions [105].
Visualization of Research Networks and Conceptual Frameworks
The bibliometric analysis of biomaterials research reveals complex networks and conceptual relationships that can be visualized through structured diagrams. Below are Graphviz representations of key frameworks in the field.
Diagram 1: Interdisciplinary relationships between core research domains and primary applications in biomaterials science.
Diagram 2: Global collaboration patterns showing the primary knowledge exchange hubs in biomaterials research.
Advancing biomaterials research requires specialized instruments, materials, and analytical services that form the foundation of experimental investigations. The following table details key resources utilized across leading institutions.
Table 4: Essential Research Tools and Services in Biomaterials Science
| Resource Category | Specific Tools/Products | Primary Research Functions |
|---|---|---|
| Mechanical Testing | Mach-1 Multiaxial Tester (Biomomentum) | Comprehensive mechanical characterization of tissues and biomaterials under various loading conditions [105]. |
| Microscopy & Imaging | Bruker Bio AFM, Delong LVEM | High-resolution imaging and mechanical property mapping at nano-scale resolutions [105]. |
| Biomaterials Supply | RESOMER polymers (Evonik), Calcium phosphate powders (CaP Biomaterials) | Source of bioresorbable polymers and ceramic materials with certified quality for medical devices [105]. |
| Surface Analysis | DataPhysics Contact Angle Goniometers | Measurement of surface tension, wettability, and surface energy critical for biocompatibility [105]. |
| 3D Bioprinting | Allevi Bioprinters, Bioinks | Fabrication of complex tissue constructs and scaffolds with precise architectural control [105]. |
| Molecular Analysis | PCR systems, Electrophoresis equipment | Detection and quantification of gene expression related to inflammatory responses and tissue regeneration [99]. |
The integration of these tools enables comprehensive characterization of biomaterial properties from macro-scale mechanical performance to nano-scale surface interactions and biological responses. For instance, the combination of mechanical testing with molecular biology techniques allows researchers to correlate material properties with cellular behaviors, facilitating the design of biomaterials that elicit specific regenerative responses [105] [99]. Commercial availability of specialized biomaterials like RESOMER polymers and calcium phosphate ceramics provides researchers with standardized materials that streamline comparative studies and enhance reproducibility across different laboratories [105]. Furthermore, advanced bioprinting platforms enable the fabrication of complex, three-dimensional tissue constructs that more accurately mimic native tissue architecture, accelerating the translation of biomaterials research into clinical applications [105].
Emerging Frontiers and Future Perspectives
The biomaterials landscape is rapidly evolving toward increasingly sophisticated and intelligent systems. Several promising frontiers are poised to define the next decade of research and development. Personalized medicine approaches are gaining traction, enabled by advances in 3D bioprinting and patient-specific modeling that allow for custom-tailored implants and drug delivery systems [100] [55]. Organoid and organ-on-chip technologies represent another transformative frontier, providing more physiologically relevant platforms for drug screening and disease modeling while reducing reliance on animal testing [100]. These systems increasingly incorporate biomaterial scaffolds that mimic native extracellular matrices, enhancing their biological relevance.
The integration of artificial intelligence and machine learning with biomaterials research is accelerating materials discovery and optimization. AI algorithms are being employed to predict material properties, optimize fabrication parameters for 3D printing, and analyze complex biological responses to material cues [102]. Additionally, smart biomaterials with responsive capabilities are emerging, designed to react to specific physiological stimuli such as pH changes, enzyme activity, or mechanical stress to release therapeutics in a precisely controlled manner [55] [104]. The convergence of these technologies points toward a future where biomaterials function not merely as passive carriers but as active participants in therapeutic processes, capable of sensing their environment and adapting their function accordingly to optimize treatment outcomes [100] [55].
Despite these promising advances, significant challenges remain in scalability, safety assessment, and regulatory translation. Fewer than 10% of preclinical biomaterial-based delivery systems progress to Phase III trials, highlighting the translational gap between laboratory innovation and clinical implementation [101]. Addressing these challenges will require enhanced collaboration between materials scientists, biologists, clinicians, and regulatory experts to establish standardized evaluation protocols and safety criteria tailored to the unique properties of advanced biomaterials. The continued growth of global research networks, particularly strengthened collaborations between North American, European, and Asian institutions, will be crucial for overcoming these barriers and fully realizing the potential of biomaterials to transform healthcare delivery [100] [101].
This vicennial bibliometric analysis provides a comprehensive examination of the evolving landscape of biomaterials research from 2005 to 2024, revealing a field characterized by robust growth, increasing globalization, and accelerating interdisciplinary integration. The United States and China have emerged as dominant forces in both research productivity and impact, with extensive collaboration networks spanning North America, Europe, and East Asia. The intellectual structure of the field encompasses core domains of materials science, biomedical engineering, chemistry, and nanotechnology, converging to advance applications in drug delivery, regenerative medicine, and medical implants. Emerging frontiers including personalized biomaterials, organ-on-chip technologies, AI-driven design, and smart responsive systems represent the next wave of innovation. However, the translation of these advances into clinical practice faces persistent challenges in scalability, safety validation, and regulatory approval. By mapping these trends and patterns, this analysis provides researchers, policymakers, and industry stakeholders with a structured framework for navigating the complex biomaterials landscape, identifying collaboration opportunities, and prioritizing research investments to address unmet medical needs through innovative biomaterial solutions.
The evolution of drug delivery systems (DDS) represents a paradigm shift in therapeutic interventions across diverse medical fields. This comparative analysis examines the efficacy of advanced biomaterial-based delivery platforms within three distinct domains: cancer immunotherapy, neurological disease management, and regenerative medicine. The strategic engineering of these systems enables precise spatiotemporal control over therapeutic agent delivery, addressing fundamental challenges in bioavailability, target specificity, and off-target effects. By synthesizing experimental data and clinical outcomes across these disciplines, this guide provides a framework for researchers and drug development professionals to evaluate the performance characteristics of various delivery platforms, informing the design of next-generation therapeutic strategies.
Comparative Efficacy Across Therapeutic Domains
The efficacy of advanced drug delivery systems varies significantly based on their application domain, mechanism of action, and the physiological barriers they are designed to overcome. The following comparative analysis synthesizes performance metrics across cancer immunotherapy, neurological, and regenerative applications.
Table 1: Comparative Efficacy of Drug Delivery Systems Across Therapeutic Domains
| Therapeutic Domain | Delivery System | Key Therapeutic Agent | Efficacy Metrics | Reported Outcome | Clinical Context |
|---|---|---|---|---|---|
| Cancer Immunotherapy | Biomimetic nanoparticle [106] | Doxorubicin + Sorafenib | Tumor growth inhibition | 68% inhibition in Lewis lung carcinoma [106] | Preclinical (mouse model) |
| Cancer Immunotherapy | Gold nanoparticle with PD-L1 siRNA [106] | hPD-L1 siRNA | Gene downregulation + Photothermal therapy | Successful hPD-L1 downregulation & tumor cell death [106] | Preclinical |
| Cancer Immunotherapy | Inhalable immunoliposomes [106] | Afatinib | Tumor growth inhibition | Significant inhibition of lung tumors [106] | Preclinical (tumor-bearing mice) |
| Neurological (MS) | High-Efficacy DMTs [107] | Ocrelizumab, Natalizumab, etc. | No Evidence of Disease Activity (NEDA) | 57-61% lower probability of losing NEDA over 2 years [107] | Real-world study (Human) |
| Neurological (MS) | High-Efficacy DMTs [107] | Ocrelizumab, Natalizumab, etc. | Relapse probability | 71-94% lower relapse probability at years 1 & 2 [107] | Real-world study (Human) |
| Regenerative (Joint Repair) | Platelet-Rich Plasma (PRP) [108] | Autologous growth factors | Pain reduction, functional improvement | Symptom improvement for ≥6 months [108] | Clinical observation |
| Regenerative (Cartilage Repair) | MACI [108] | Autologous chondrocytes | Structural cartilage repair | 80-90% success rate over time [108] | Clinical procedure |
| Regenerative (DFU) | PRP + Conventional [109] | Autologous growth factors | Wound healing time | Significantly earlier healing vs. control [109] | Network Meta-analysis (RCTs) |
| Regenerative (DFU) | Stem Cell + Conventional [109] | Stem cells | Wound healing time | No significant difference vs. PRP/EGF [109] | Network Meta-analysis (RCTs) |
Experimental Protocols and Methodologies
Cancer Immunotherapy: Evaluation of Biomimetic Nanoparticles
Objective: To assess the efficacy of a cell membrane-derived biomimetic drug delivery platform co-encapsulating doxorubicin and sorafenib in modulating the tumor microenvironment and inhibiting tumor growth in a Lewis lung carcinoma model [106].
Materials:
- Nanoparticle Formulation: Cell membrane-derived vesicles loaded with doxorubicin and sorafenib.
- Cell Line: Lewis lung carcinoma cells.
- Animal Model: Mice implanted with Lewis lung carcinoma.
- Key Reagents: Antibodies for flow cytometry (CD8, CD4, FoxP3), ELISA kits for cytokine analysis.
Methodology:
- Nanoparticle Synthesis & Characterization: Prepare biomimetic nanoparticles via co-encapsulation. Characterize size, zeta potential, drug loading efficiency, and release profile using dynamic light scattering and HPLC.
- In Vitro Analysis: Treat Lewis lung carcinoma cells with nanoparticles. Assess immunogenic cell death markers (e.g., ATP, HMGB1 release) via ELISA.
- In Vivo Tumor Model: Randomize tumor-bearing mice into groups receiving: (i) biomimetic nanoparticles, (ii) free drug combination, (iii) placebo control.
- Tumor Monitoring: Measure tumor volume regularly with calipers. Calculate percent tumor growth inhibition relative to control.
- TME Immunophenotyping: At endpoint, analyze tumor infiltrating lymphocytes by flow cytometry to quantify CD8+ cytotoxic T cells and regulatory T cells (Tregs).
- Cytokine Analysis: Measure pro-inflammatory cytokines in tumor homogenates.
Key Findings: The biomimetic platform achieved 68% tumor growth inhibition, significantly enhanced CD8+ T cell infiltration, and reduced immunosuppressive factors in the TME [106].
Neurological Disease: Assessing High-Efficacy DMTs in Multiple Sclerosis
Objective: To compare treatment outcomes, including No Evidence of Disease Activity (NEDA), between treatment-naïve Relapsing-Remitting MS (RRMS) patients commencing high-efficacy therapies (HET) versus non-high-efficacy therapies (non-HET) using real-world data [107].
Materials:
- Patient Cohorts: Treatment-naïve RRMS patients initiated on HET or non-HET.
- HET Definition: Fingolimod, natalizumab, ocrelizumab, cladribine, alemtuzumab.
- Non-HET Definition: Dimethyl fumarate, glatiramer acetate, interferons.
- Key Tools: Expanded Disability Status Scale, MRI.
Methodology:
- Study Design: Prospective, observational, longitudinal study of two single-center cohorts.
- Patient Selection & Matching: Include treatment-naïve patients with ≥2 years of follow-up. Use propensity score matching to balance baseline characteristics between HET and non-HET groups.
- Outcome Measures:
- NEDA: A composite endpoint defined as no relapses, no confirmed disability progression, and no new MRI activity.
- Relapse Rate: Annualized relapse rate.
- Disability Progression: Change in EDSS score from baseline.
- Statistical Analysis: Use Cox proportional hazards models for time-to-event outcomes (losing NEDA) and logistic regression for binary outcomes (relapse). Analyze at years 1 and 2.
Key Findings: The probability of losing NEDA was 57% and 39% lower in the HET group at years 1 and 2, respectively. Relapse probability was 94% and 71% lower in the HET group at the same time points [107].
Regenerative Medicine: Network Meta-Analysis of Diabetic Foot Ulcer Therapies
Objective: To compare the efficacy of regenerative therapies—Platelet-Rich Plasma, stem cell therapy, and epidermal growth factor—for treating diabetic foot ulcers in terms of ulcer healing and healing time [109].
Materials:
- Data Sources: PubMed, Cochrane Library, EMBASE.
- Study Selection: Randomized Controlled Trials comparing conventional treatment combined with PRP, EGF, or stem cell therapy vs. conventional treatment alone for DFUs.
- Interventions: PRP, EGF, Stem Cell Therapy.
Methodology:
- Systematic Review: Conduct a systematic literature search based on PRISMA guidelines.
- Study Inclusion & Data Extraction: Include RCTs reporting complete ulcer healing or wound healing time. Extract data on patient demographics, intervention details, and outcomes.
- Network Meta-Analysis: Perform a frequentist network meta-analysis to compare treatments directly and indirectly. Rank treatments using the surface under the cumulative ranking curve.
- Outcome Measures:
- Primary: Proportion of completely healed ulcers.
- Secondary: Mean wound healing time.
- Risk of Bias & Certainty of Evidence: Assess study quality using the Cochrane risk-of-bias tool. Evaluate publication bias with funnel plots.
Key Findings: No significant difference was found in the number of healed ulcers between PRP, stem cells, and EGF. However, the PRP group achieved significantly earlier ulcer healing than the other groups. The ranking probability showed stem cells as the best for complete healing, followed by PRP and EGF [109].
Signaling Pathways and Workflows
Diagram 1: Nano-Drug Delivery Enhances Cancer Immunotherapy
Diagram 2: MS Treatment Escalation Pathway
Diagram 3: Regenerative Medicine Healing Cascade
Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for Drug Delivery System Development
| Research Reagent / Material | Primary Function | Application Context |
|---|---|---|
| Matrigel | Tumor-derived extracellular matrix used as a 3D scaffold for cell culture. | Liver organoid development; in vitro disease modeling [110]. |
| Synthetic Hydrogels | Defined, xeno-free biomaterials serving as scaffolds for 3D cell culture and organoid growth. | Engineering next-generation, clinically relevant liver organoid models [110]. |
| Polymeric Nanoparticles | Biodegradable nanocarriers (e.g., PLGA) for controlled drug encapsulation and release. | Passive/active tumor targeting in cancer immunotherapy [106] [111]. |
| Lipid Nanoparticles | Nanocarriers with high biocompatibility for encapsulating various therapeutic cargoes. | Pulmonary drug delivery for lung cancer; mRNA/siRNA delivery [112]. |
| Gold Nanoparticles | Versatile metal nanoparticles serving as drug carriers, imaging agents, and photothermal therapy agents. | Constructing artificial antigen-presenting cells; delivering siRNA (e.g., PD-L1) [106]. |
| Immune Checkpoint Inhibitors | Monoclonal antibodies (e.g., anti-PD-1, anti-CTLA-4) that block inhibitory pathways on T-cells. | Key therapeutic agents delivered via nanocarriers to enhance anti-tumor immunity [113] [111]. |
| Ferroptosis Inducers | Agents that trigger iron-dependent, non-apoptotic cell death characterized by lipid peroxidation. | Combined with ICIs in nano-delivery systems to potentiate cancer immunotherapy [113]. |
| Mesenchymal Stem Cells | Multipotent adult stem cells with immunomodulatory and tissue-reparative properties. | Cellular therapy for autoimmune, inflammatory, and degenerative conditions [108] [114]. |
| Platelet-Rich Plasma | Autologous concentration of platelets containing a high dose of growth factors. | Treatment of musculoskeletal conditions and chronic wounds like diabetic foot ulcers [108] [109]. |
Conclusion
This comparative analysis underscores that no single biomaterial system universally outperforms others; rather, each class—nanoparticles, hydrogels, microneedles, and biodegradable polymers—offers a unique profile of advantages tailored to specific therapeutic needs. The future of biomaterial-driven drug delivery lies in the strategic integration of these systems into hybrid platforms, leveraging their complementary strengths. Key trends such as personalization via 3D printing, the development of intelligent stimuli-responsive materials, and the application of AI for design optimization are poised to address current translational challenges. For researchers and clinicians, this evolving landscape promises a new era of precision medicines capable of improved targeting, reduced side effects, and enhanced therapeutic outcomes across a broad spectrum of diseases. The continued convergence of materials science with biology will be crucial in transforming these promising platforms into mainstream clinical realities.
References
- 1. Revolutionizing Drug Delivery: The Impact of Advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944361/]
- 2. Editorial: Functional biomaterials for drug delivery [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1550444/full]
- 3. Biomaterials in Drug Delivery: Advancements in Cancer ... [https://www.mdpi.com/1422-0067/25/6/3126]
- 4. Polymeric Nanoparticles in Targeted Drug Delivery: Unveiling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11991310/]
- 5. Biomaterials-mediated sequential drug delivery: emerging ... [https://www.sciencedirect.com/science/article/pii/S1818087625000728]
- 6. Smart Biomaterials for Delivery of Drugs and Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311304/]
- 7. Bio-based poly(1,3-trimethyleneglycol- co -lactide) triblock ... [https://pubs.rsc.org/en/content/articlehtml/2025/py/d5py00594a]
- 8. The synergy of artificial intelligence in biomaterials ... [https://www.sciencedirect.com/science/article/pii/S305072352500001X]
- 9. Review Natural polysaccharide-based nano-drug delivery ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025066383]
- 10. Bioinspired and biomimetic protein-based fibers and their ... [https://www.nature.com/articles/s43246-024-00488-2]
- 11. Comparative Stability of Synthetic and Natural Polymeric ... [https://www.mdpi.com/1999-4923/17/11/1439]
- 12. Comparative Study of Polysaccharide-Based Hydrogels [https://pmc.ncbi.nlm.nih.gov/articles/PMC8951473/]
- 13. A Comparative Review of Natural and Synthetic ... [https://www.mdpi.com/2073-4360/13/7/1105]
- 14. Comparative optimization of polysaccharide-based ... [https://www.nature.com/articles/s41467-024-49804-x]
- 15. Advanced Biocompatible and Biodegradable Polymers [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611034/]
- 16. Advanced Biocompatible and Biodegradable Polymers [https://www.mdpi.com/2073-4360/17/21/2901]
- 17. Biocompatibility, Biodistribution, and Drug-Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2952648/]
- 18. Comparison of Different Approaches to Surface ... [https://www.mdpi.com/2079-4991/9/12/1769]
- 19. Recent Applications of PLGA in Drug Delivery Systems [https://www.mdpi.com/2073-4360/16/18/2606]
- 20. Multifunctional PLGA nanosystems: enabling integrated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488692/]
- 21. A Tri-Stimuli Responsive (Maghemite/PLGA)/Chitosan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8401782/]
- 22. Stimuli-responsive nanomaterials for targeted drug delivery ... [https://www.sciencedirect.com/science/article/abs/pii/S2590238525002929]
- 23. A formulation dataset of poly(lactide-co-glycolide ... [https://www.nature.com/articles/s41597-025-05520-9]
- 24. Stimuli-Responsive, Cell-Mediated Drug Delivery Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389507/]
- 25. Polymeric nanocarriers as stimuli-responsive systems for ... [https://www.sciencedirect.com/science/article/pii/S1319016420300050]
- 26. Challenges and material innovations in drug delivery to ... [https://pubmed.ncbi.nlm.nih.gov/39985979]
- 27. Translational Advances in Lipid Nanoparticle Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567512/]
- 28. Polymeric nanomaterials as a drug delivery system for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417996/]
- 29. Precision targeting of the CNS: recent progress in brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278267/]
- 30. Polymeric Nanoparticles in Targeted Drug Delivery [https://www.mdpi.com/2073-4360/17/7/833]
- 31. Recent Advances in Intranasal Administration for Brain-Targeting... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10898487/]
- 32. Hydrogel-forming microneedles for the treatment of skin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590443/]
- 33. Hydrogel-Forming Microneedles in the Management of ... [https://www.mdpi.com/2310-2861/10/11/719]
- 34. Advances in Research of Hydrogel Microneedle-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11676655/]
- 35. Recent advances and perspectives of MicroNeedles for ... [https://link.springer.com/article/10.1007/s12551-025-01317-7]
- 36. Enhancing melanoma therapy with hydrogel microneedles [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1590534/full]
- 37. Research progress of biomaterial-based hydrogels in the ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325011901]
- 38. Microneedles for controlled and sustained intraocular drug ... [https://www.nature.com/articles/s41427-025-00614-7]
- 39. Engineering and in vitro evaluation of semi-dissolving ... [https://www.sciencedirect.com/science/article/pii/S0378517325007690]
- 40. Nanoparticles-incorporated hydrogel microneedle for ... [https://pubmed.ncbi.nlm.nih.gov/40777846/]
- 41. Developmental Framework and Umbrella Review of AI ... [https://www.preprints.org/manuscript/202504.2168]
- 42. Advances in Biomaterials for Drug Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6261797/]
- 43. Biomaterial-based drug delivery systems in the treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12004832/]
- 44. Biomaterials for Drug Delivery and Human Applications [https://www.mdpi.com/1996-1944/17/2/456]
- 45. Biomaterial-based drug delivery strategies for oral mucosa [https://www.sciencedirect.com/science/article/abs/pii/S0927776525001110]
- 46. Targeting the Oral Mucosa: Emerging Drug Delivery Platforms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473735/]
- 47. Therapeutic potential of biomaterials in rescuing ... [https://www.sciencedirect.com/science/article/abs/pii/S0306452225010309]
- 48. Pulmonary Drug Delivery System Market Size to Worth ... [https://finance.yahoo.com/news/pulmonary-drug-delivery-system-market-150000192.html]
- 49. Pulmonary Drug Delivery Systems Analysis 2025 and ... [https://www.archivemarketresearch.com/reports/pulmonary-drug-delivery-systems-545295]
- 50. Inner Ear Organoids: A Hydrogel-Based Platform for Drug ... [https://link.springer.com/article/10.1007/s12264-025-01479-0]
- 51. Empowering Precision Medicine: The Impact of 3D Printing ... [https://link.springer.com/article/10.1208/s12249-023-02682-w]
- 52. A Review of 3D Printing Technology in Pharmaceutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC9962448/]
- 53. 3D Printing in Oral Drug Delivery - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299587/]
- 54. Innovative applications of 3D printing in personalized ... [https://www.sciencedirect.com/science/article/pii/S2589004225017663]
- 55. Biomaterials for Drug Delivery and Human Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10817481/]
- 56. 3D printing processes in precise drug delivery for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11164598/]
- 57. Recent applications of three-dimensional bioprinting in ... [https://www.sciencedirect.com/science/article/pii/S0169409X24002783]
- 58. Machine learning predicts 3D printing performance of over ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365921003977]
- 59. Biopharma RD Faces Productivity And Attrition Challenges ... [https://www.clinicalleader.com/doc/biopharma-r-d-faces-productivity-and-attrition-challenges-in-2025-0001]
- 60. Transforming Cancer Therapy: Insights from 2025 H1 FDA ... [https://blog.crownbio.com/transforming-cancer-therapy-insights-from-2025-h1-fda-approvals-and-preclinical-drug-discovery]
- 61. From Preclinical Screening to Clinical Optimization [https://drug-dev.com/preclinical-screening-platform-from-preclinical-screening-to-clinical-optimization-accelerating-poorly-soluble-drug-development/]
- 62. Biomaterials for Protein Delivery: Opportunities and ... [https://www.mdpi.com/2072-666X/15/4/533]
- 63. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 64. Blood–spinal cord barrier [https://en.wikipedia.org/wiki/Blood%E2%80%93spinal_cord_barrier]
- 65. Comparison of Drug Delivery Systems with Different Types of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11679882/]
- 66. Current Strategies for Brain Drug Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5858162/]
- 67. Blood-Spinal Cord Barrier in Spinal Cord Injury: A Review [https://pubmed.ncbi.nlm.nih.gov/33292072/]
- 68. Blood brain barrier: An overview on strategies in drug delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4836458/]
- 69. Engineering the Immune Response to Biomaterials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12097135/]
- 70. Smart biomaterials: as active immune modulators to shape ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1669399/full]
- 71. Toxicity and biodistribution comparison of functionalized ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1512622/full]
- 72. Chitosan based smart injectable hydrogels for biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595387/]
- 73. Marine Biomaterials for Drug Delivery and Wound Healing [https://www.mdpi.com/1424-8247/18/8/1093]
- 74. Nanotechnologyâ€Driven Drug Delivery Systems for Lung Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274165/]
- 75. Advances in nanoparticles in targeted drug delivery–A review [https://www.sciencedirect.com/science/article/pii/S2666845925001163]
- 76. Biobased Nanomaterials in Drug Delivery System [https://www.sciencepublishinggroup.com/article/10.11648/j.nano.20251302.12]
- 77. Smart & Sustainable Materials Market Report 2025-2035: [https://www.globenewswire.com/news-release/2025/11/18/3189801/0/en/Smart-Sustainable-Materials-Market-Report-2025-2035-Opportunities-Through-Strategic-Partnerships-Cross-Regional-Manufacturing-Expansion-and-Adoption-of-Smart-Material-Technologies.html]
- 78. Towards Sustainable Scaling-Up of Nanomaterials ... [https://www.mdpi.com/2673-4117/6/7/149]
- 79. Data-Driven Prediction of Nanoparticle Biodistribution from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312149/]
- 80. Advances in Nanotechnology-Based Drug Delivery Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389492/]
- 81. The Challenges Behind Scaling Up Nanomaterials [https://www.azonano.com/article.aspx?ArticleID=6126]
- 82. Nanotechnology Creates Opportunities, Challenges for ... [https://www.biopharminternational.com/view/nanotechnology-creates-opportunities-challenges-biotech-manufacturers]
- 83. UCLA, UC Santa Barbara's BioPACIFIC MIP earns renewed ... [https://cnsi.ucla.edu/august-19-2025-ucla-uc-santa-barbaras-biopacific-mip-earns-renewed-nsf-support-to-accelerate-ai-driven-biobased-materials-innovation/]
- 84. Recent progress in drug delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6900554/]
- 85. Revolutionizing Drug Delivery: The Impact of Advanced ... [https://www.mdpi.com/1999-4923/17/3/375]
- 86. Extracellular vesicle-based drug overview: research ... [https://www.nature.com/articles/s41392-025-02312-w]
- 87. Advancements in Hydrogels: A Comprehensive Review of ... [https://www.mdpi.com/2073-4360/17/15/2026]
- 88. Controlled Release vs. Sustained Release [https://oakwoodlabs.com/sustained-release-drugs-vs-controlled-release-drugs-whats-the-difference/]
- 89. Controlled Drug Delivery Systems: Current Status and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8512302/]
- 90. Recent advancements in nanoparticle drug delivery ... [https://www.sciencedirect.com/science/article/abs/pii/S1853002825000254]
- 91. Hydrogel Nanoparticles in Drug Delivery: A Review [https://www.sciencedirect.com/science/article/pii/S2949866X25000644]
- 92. Hydrogel Materials for Drug Delivery and Tissue Engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609469/]
- 93. Recent advances and challenges of injectable hydrogels in ... [https://www.sciencedirect.com/science/article/abs/pii/S016836592500642X]
- 94. Nanoparticles-incorporated hydrogel microneedle for ... [https://www.sciencedirect.com/science/article/pii/S1818087625000534]
- 95. Recent advances and perspectives of MicroNeedles for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12290160/]
- 96. Advances in clinical applications of microneedle [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1607210/full]
- 97. Research progress on biodegradable polymer-based drug ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1561708/full]
- 98. Novel Drug Delivery Platform Targets Lung Neutrophils ... [https://jabsom.hawaii.edu/news-events/news/2025/05/verma-park-drug-delivery-platform.html]
- 99. Essential molecular biology methods in biomaterials ... [https://www.explorationpub.com/Journals/ebmx/Article/101344]
- 100. Biomaterial-driven regenerative drug delivery: a vicennial ... [https://pubmed.ncbi.nlm.nih.gov/40727534/]
- 101. Biomaterial-driven regenerative drug delivery: a vicennial ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1593985/full]
- 102. Insights from Scopus and Web of Science (2015-2025) [https://pubmed.ncbi.nlm.nih.gov/40978403/]
- 103. Biomaterials Research - Impact Factor & Score 2025 [https://research.com/journal/biomaterials-research]
- 104. Their role in drug delivery systems and comparison of ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224722010322]
- 105. Resource Guide | Society for Biomaterials (SFB) [https://biomaterials.org/about-society/resource-guide]
- 106. Drug Delivery System for Cancer Immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12035301/]
- 107. Real-World Comparison of High-Efficacy Versus Non- ... [https://pubmed.ncbi.nlm.nih.gov/40670294/]
- 108. How successful is regenerative medicine [https://californiapain.com/how-successful-is-regenerative-medicine/]
- 109. Comparative Efficacy of Regenerative Therapies for ... [https://pubmed.ncbi.nlm.nih.gov/39996539/]
- 110. Current advances and prospects in biomaterials-guided ... [https://www.sciencedirect.com/science/article/pii/S2666138125000131]
- 111. Targeted nano-drug delivery systems for tumor ... [https://www.sciencedirect.com/science/article/pii/S2095177925002254]
- 112. Global research trends and emerging hotspots in nano-drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11724832/]
- 113. Boosting cancer immunotherapy: drug delivery systems ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1611299/full]
- 114. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]